Health risks and issues
Featured health risks and issues.
As part of the Global Burden of Disease (GBD) study, we produce estimates for more than 80 risk factors along with in-depth analysis for the world's most pressing health issues.

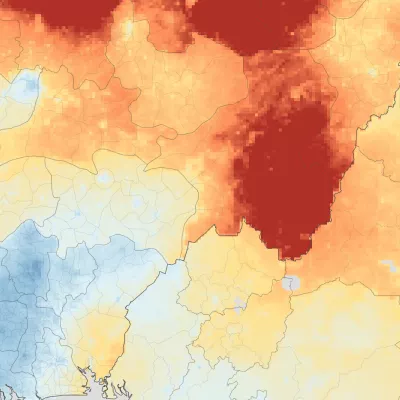
Air pollution
Air pollution affects millions of people worldwide. Both household and outdoor air pollution pose severe threats related to cardiovascular and respiratory diseases, cancers, and other conditions.
Alcohol use
Alcohol use is a major risk factor for death and disability worldwide. In some countries, it is the number one risk factor for men.
Antimicrobial resistance (AMR)
AMR poses a major threat to human health around the world. AMR occurs when microorganisms, such as bacteria, adapt in ways that make currently available treatments for infections less effective.
Child health
Despite notable advancements and progress made by many countries in reducing child mortality rates, millions of children continue to lose their lives before turning five.
How much disease burden can be attributed to diet, and what components of our diet are most harmful? We explore the link between dietary changes and population health.
Maternal health
Maternal health refers to the health of women and childbearing people during pregnancy, childbirth, and the post-natal months. Despite overall improvement in maternal outcomes since 1990, disparities remain.
Mental health
Mental health conditions are among the top 10 leading causes of health loss worldwide, with anxiety and depression ranked as the most common across all age groups and locations.
Smoking and tobacco
While smoking prevalence has decreased over the past 30 years, the total number of smokers worldwide has continued to increase due to population growth, contributing significantly to disease burden.
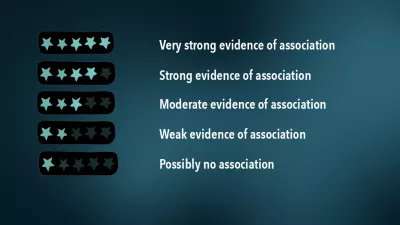
Which health studies are supported by strong evidence?
We investigated which popular health recommendations have the biggest impact, so everyone from health-conscious individuals to policymakers can better understand the strength of evidence behind certain risks and outcomes.
Publications
Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021, a burden of proof study on alcohol consumption and ischemic heart disease, estimating the subnational prevalence of antimicrobial resistant salmonella enterica serovars typhi and paratyphi a infections in 75 endemic countries, 1990–2019, health effects associated with chewing tobacco: a burden of proof study, interactive data visuals.

Burden of Proof
Compare strength of evidence for health risks and outcomes.
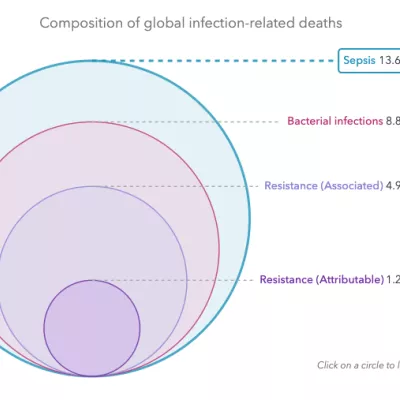
The MICROBE (Measuring Infectious Causes and Resistance Outcomes for Burden Estimation) tool visualizes the fatal and nonfatal health outcomes of infections, pathogens, and antimicrobial resistance across different countries and regions.
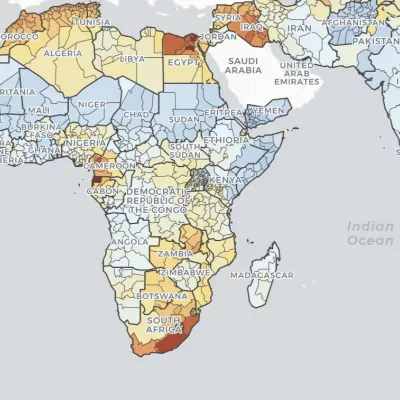
Double Burden of Malnutrition
With this dynamic map visualization tool, explore local patterns in child overweight and wasting, from 2000 to 2019. Observe trends at multiple spatial scales and search to view trends in specific countries and local areas.
Child Growth Failure
Delve into local patterns in child stunting, wasting, and underweight across all low- and middle-income countries from 2000 to 2017.
Data input sources
The Global Health Data Exchange (GHDx) is home to the world's most comprehensive catalog of surveys, censuses, vital statistics, and other health-related data. Use our data input sources tool to explore the sources used in the latest round of the Global Burden of Disease (GBD) estimation.
Open data catalog
Subscribe to our newsletter
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 May 2021
Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis
- Surapon Nochaiwong ORCID: orcid.org/0000-0003-1100-7171 1 , 2 ,
- Chidchanok Ruengorn ORCID: orcid.org/0000-0001-7927-1425 1 , 2 ,
- Kednapa Thavorn ORCID: orcid.org/0000-0003-4738-8447 2 , 3 , 4 , 5 ,
- Brian Hutton ORCID: orcid.org/0000-0001-5662-8647 3 , 4 , 5 ,
- Ratanaporn Awiphan ORCID: orcid.org/0000-0003-3628-0596 1 , 2 ,
- Chabaphai Phosuya 1 ,
- Yongyuth Ruanta ORCID: orcid.org/0000-0003-4184-0308 1 , 2 ,
- Nahathai Wongpakaran ORCID: orcid.org/0000-0001-8365-2474 6 &
- Tinakon Wongpakaran ORCID: orcid.org/0000-0002-9062-3468 6
Scientific Reports volume 11 , Article number: 10173 ( 2021 ) Cite this article
56k Accesses
321 Citations
117 Altmetric
Metrics details
- Post-traumatic stress disorder
To provide a contemporary global prevalence of mental health issues among the general population amid the coronavirus disease-2019 (COVID-19) pandemic. We searched electronic databases, preprint databases, grey literature, and unpublished studies from January 1, 2020, to June 16, 2020 (updated on July 11, 2020), with no language restrictions. Observational studies using validated measurement tools and reporting data on mental health issues among the general population were screened to identify all relevant studies. We have included information from 32 different countries and 398,771 participants. The pooled prevalence of mental health issues amid the COVID-19 pandemic varied widely across countries and regions and was higher than previous reports before the COVID-19 outbreak began. The global prevalence estimate was 28.0% for depression; 26.9% for anxiety; 24.1% for post-traumatic stress symptoms; 36.5% for stress; 50.0% for psychological distress; and 27.6% for sleep problems. Data are limited for other aspects of mental health issues. Our findings highlight the disparities between countries in terms of the poverty impacts of COVID-19, preparedness of countries to respond, and economic vulnerabilities that impact the prevalence of mental health problems. Research on the social and economic burden is needed to better manage mental health problems during and after epidemics or pandemics. Systematic review registration : PROSPERO CRD 42020177120.
Similar content being viewed by others
Three-year outcomes of post-acute sequelae of COVID-19

Long COVID: major findings, mechanisms and recommendations

The serotonin theory of depression: a systematic umbrella review of the evidence
Introduction.
After the World Health Organisation (WHO) declared the rapid worldwide spread of coronavirus disease-2019 (COVID-19) to be a pandemic, there has been a dramatic rise in the prevalence of mental health problems both nationally and globally 1 , 2 , 3 . Early international evidence and reviews have reported the psychological effects of the COVID-19 outbreak on patients and healthcare workers, particularly those in direct contact with affected patients 4 , 5 , 6 , 7 , 8 . Besides patients with COVID-19, negative emotions and psychosocial distress may occur among the general population due to the wider social impact and public health and governmental response, including strict infection control, quarantine, physical distancing, and national lockdowns 2 , 9 , 10 .
Amid the COVID-19 pandemic, several mental health and psychosocial problems, for instance, depressive symptoms, anxiety, stress, post-traumatic stress symptoms (PTSS), sleep problems, and other psychological conditions are of increasing concern and likely to be significant 5 , 10 , 11 . Public psychological consequences can arise through direct effects of the COVID-19 pandemic that are sequelae related to fear of contagion and perception of danger 2 . However, financial and economic issues also contribute to mental health problems among the general population in terms of indirect effects 12 , 13 . Indeed, economic shutdowns have disrupted economies worldwide, particularly in countries with larger domestic outbreaks, low health system preparedness, and high economic vulnerability 14 , 15 , 16 .
The COVID-19 pandemic may affect the mental health of the general population differently based on national health and governmental policies implemented and the public resilience and social norms of each country. Unfortunately, little is known about the global prevalence of mental health problems in the general population during the COVID-19 pandemic. Previous systematic reviews have been limited by the number of participants included, and attention has been focussed on particular conditions and countries, with the majority of studies being conducted in mainland China 5 , 8 , 11 , 17 , 18 . To the best of our knowledge, evidence on mental health problems among the general population worldwide has not been comprehensively documented in the current COVID-19 pandemic. Therefore, a systematic review and meta-analysis at a global level is needed to provide robust and contemporary evidence to inform public health policies and long-term responses to the COVID-19 pandemic.
As such, we have performed a rigorous systematic review and meta-analysis of all available observational studies to shed light on the effects of the global COVID-19 pandemic on mental health problems among the general population. We aimed to: (1) summarise the prevalence of mental health problems nationally and globally, and (2) describe the prevalence of mental health problems by each WHO region, World Bank income group, and the global index and economic indices responses to the COVID-19 pandemic.
This systematic review and meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines 19 and reported in line with the Meta-analysis of Observational Studies in Epidemiology statement (Appendix, Table S1 ) 20 . The pre-specified protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42020177120).
Search strategy
We searched electronic databases in collaboration with an experienced medical librarian using an iterative process. PubMed, Medline, Embase, PsycINFO, Web of Science, Scopus, CINAHL, and the Cochrane Library were used to identify all relevant abstracts. As the WHO declared the COVID-19 outbreak to be a public health emergency of international concern on January 30, 2020, we limited the search from January 1, 2020, to June 16, 2020, without any language restrictions. The main keywords used in the search strategy included “coronavirus” or “COVID-19” or “SARS-CoV-2”, AND “mental health” or “psychosocial problems” or “depression” or “anxiety” or “stress” or “distress” or “post-traumatic stress symptoms” or “suicide” or “insomnia” or “sleep problems” (search strategy for each database is provided in the Appendix, Table S2 ). Relevant articles were also identified from the reference lists of the included studies and previous systematic reviews. To updated and provide comprehensive, evidence-based data during the COVID-19 pandemic, grey literature from Google Scholar and the preprint reports from medRxiv, bioRxiv, and PsyArXiv were supplemented to the bibliographic database searches. A targeted manual search of grey literature and unpublished studies was performed through to July 11, 2020.
Study selection and data screening
We included observational studies (cross-sectional, case–control, or cohort) that (1) reported the occurrence or provided sufficient data to estimate the prevalence of mental health problems among the general population, and (2) used validated measurement tools for mental health assessment. The pre-specified protocol was amended to permit the inclusion of studies the recruited participants aged 12 years or older and college students as many colleges and universities were closed due to national lockdowns. We excluded studies that (1) were case series/case reports, reviews, or studies with small sample sizes (less than 50 participants); (2) included participants who had currently confirmed with the COVID-19 infection; and (3) surveyed individuals under hospital-based settings. If studies had overlapping participants and survey periods, then the study with the most detailed and relevant information was used.
Eligible titles and abstracts of articles identified by the literature search were screened independently by two reviewers (SN and CR). Then, potentially relevant full-text articles were assessed against the selection criteria for the final set of included studies. Potentially eligible articles that were not written in English were translated before the full-text appraisal. Any disagreement was resolved by discussion.
The primary outcomes were key parameters that reflect the global mental health status during the COVID-19 pandemic, including depression, anxiety, PTSS, stress, psychological distress, and sleep problems (insomnia or poor sleep). To deliver more evidence regarding the psychological consequences, secondary outcomes of interest included psychological symptoms, suicidal ideation, suicide attempts, loneliness, somatic symptoms, wellbeing, alcohol drinking problems, obsessive–compulsive symptoms, panic disorder, phobia anxiety, and adjustment disorder.
Data extraction and risk of bias assessment
Two reviewers (SN and YR) independently extracted the pre-specified data using a standardised approach to gather information on the study characteristics (the first author’s name, study design [cross-sectional survey, longitudinal survey, case–control, or cohort], study country, article type [published article, short report/letters/correspondence, or preprint reporting data], the data collection period), participant characteristics (mean or median age of the study population, the proportion of females, proportion of unemployment, history of mental illness, financial problems, and quarantine status [never, past, or current]), and predefined outcomes of interest (including assessment outcome definitions, measurement tool, and diagnostic cut-off criteria). For international studies, data were extracted based on the estimates within each country. For studies that had incomplete data or unclear information, the corresponding author was contacted by email for further clarification. The final set of data was cross-checked by the two reviewers (RA and CP), and discrepancies were addressed through a discussion.
Two reviewers (SN and CR) independently assessed and appraised the methodological quality of the included studies using the Hoy and colleagues Risk of Bias Tool-10 items 21 . A score of 1 (no) or 0 (yes) was assigned to each item. The higher the score, the greater the overall risk of bias of the study, with scores ranging from 0 to 10. The included studies were then categorised as having a low (0–3 points), moderate (4–6 points), or high (7 or 10 points) risk of bias. A pair of reviewers (RA and CP) assessed the risk of bias of each study. Any disagreements were resolved by discussion.
Data synthesis and statistical methods
A two-tailed P value of less than 0.05 was considered statistically significant. We used Stata software version 16.0 (StataCorp, College Station, TX, USA) for all analyses and generated forest plots of the summary pooled prevalence. Inter-rater agreements between reviewers for the study selection and risk of bias assessment were tested using the kappa (κ) coefficient of agreement 22 . Based on the crude information data, we recalculated and estimated the unadjusted prevalence of mental health and psychological problems using the crude numerators and denominators reported by each of the included studies. Unadjusted pooled prevalence with corresponding 95% confidence intervals (CIs) was reported for each WHO regions (Africa, America, South-East Asia, Europe, Eastern Mediterranean, and Western Pacific) and World Bank income group (low-, lower-middle-, upper-middle-, and high-income).
We employed the variance of the study-specific prevalence using the Freeman–Tukey double arcsine methods for transforming the crude data before pooling the effect estimates with a random-effect model to account for the effects of studies with extreme (small or large) prevalence estimates 23 . Heterogeneity was evaluated using the Cochran’s Q test, with a p value of less than 0.10 24 . The degree of inconsistency was quantified using I 2 values, in which a value greater than 60–70% indicated the presence of substantial heterogeneity 25 .
Pre-planned subgroup analyses were performed based on the participant (i.e., age, the proportion of female sex, the proportion of unemployment, history of mental illness, financial problems, and quarantine status) and study characteristics (article type, study design, data collection, and sample size). To explore the inequality and poverty impacts across countries, subgroup analyses based on the global index and economic indices responses to the COVID-19 pandemic were performed, including (1) human development index (HDI) 2018 (low, medium, high, and very high) 26 ; (2) gender inequality index 2018 (below vs above world average [0.439]) 27 ; (3) the COVID-19-government response stringency index during the survey (less- [less than 75%], moderate- [75–85%], and very stringent [more than 85%]) according to the Oxford COVID-19 Government Response Tracker reports 28 ; (4) the preparedness of countries in terms of hospital beds per 10,000 people, 2010–2018 (low, medium–low, medium, medium–high, and high) 15 ; (5) the preparedness of countries in terms of current health expenditure (% of gross domestic product [GDP] 2016; low, medium–low, medium, medium–high, and high) 15 ; (6) estimated percent change of real GDP growth based on the International Monetary Fund, April 2020 (below vs above world average [− 3.0]) 29 ; (7) the resilience of countries’ business environment based on the 2020 global resilience index reports (first-, second-, third-, and fourth-quartile) 30 ; and (8) immediate economic vulnerability in terms of inbound tourism expenditure (% of GDP 2016–2018; low, medium–low, medium, medium–high, and high) 15 .
To address the robustness of our findings, we conducted a sensitivity analysis by restricting the analysis to studies with a low risk of bias (Hoy and Colleagues-Tool, 0–3 points). Furthermore, a random-effects univariate meta-regression analysis was used to explore the effect of participant and study characteristics, and the global index and economic indices responses to the COVID-19 pandemic as described above on the prevalence estimates.
The visual inspection of funnel plots was performed when there was sufficient data and tested for asymmetry using the Begg’s and Egger’s tests for each specific. A P value of less than 0.10 was considered to indicate statistical publication bias 31 , 32 . If the publication bias was detected by the Begg’s and Egger’s regression test, the trim and fill method was then performed to calibrate for publication bias 33 .
Initially, the search strategy retrieved 4642 records. From these, 2682 duplicate records were removed, and 1960 records remained. Based on the title and abstract screening, we identified 498 articles that seemed to be relevant to the study question (the κ statistic for agreement between reviewers was 0.81). Of these, 107 studies fulfilled the study selection criteria and were included in the meta-analysis (Appendix, Figure S1 ). The inter-rater agreement between reviewers on the study selection and data extraction was 0.86 and 0.75, respectively. The reference list of all included studies in this review is provided in the Appendix, Table S3 .
Characteristics of included studies
In total, 398,771 participants from 32 different countries were included. The mean age was 33.5 ± 9.5 years, and the proportion of female sex was 60.9% (range, 16.0–51.6%). Table 1 summarises the characteristics of all the included studies according to World Bank income group, the global index of COVID-19 pandemic preparedness, and economic vulnerability indices. The included studies were conducted in the Africa (2 studies 34 , 35 [1.9%], n = 723), America (12 studies 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 [11.2%], n = 18,440), South-East Asia (10 studies 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 [9.4%], n = 11,953), Europe (27 studies 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 [25.2%], n = 148,430), Eastern Mediterranean (12 studies 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 [11.2%], n = 23,396), and Western Pacific WHO regions (44 studies 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 [41.1%], n = 195,829). Most of the included studies were cross-sectional (96 studies, 89.7%), used an online-based survey (101 studies, 95.3%), conducted in mainland China (34 studies, 31.8%), and were conducted in countries with upper-middle (49 studies, 45.8%) and high-incomes (44 studies, 41.1%). Detailed characteristics of the 107 included studies, measurement tools for evaluating the mental health status and psychological consequences, and the diagnostic cut-off criteria are described in Appendix, Table S4 . Of the 107 included studies, 76 (71.0%) had a low risk, 31 (29.0%) had a moderate risk, and no studies had a high risk of bias (Appendix, Table S5 ).
Global prevalence of mental health issues among the general population amid the COVID-19 pandemic
Table 2 presents a summary of the results of the prevalence of mental health problems among the general population amid the COVID-19 pandemic by WHO region and World Bank country groups. With substantial heterogeneity, the global prevalence was 28.0% (95% CI 25.0–31.2) for depression (75 studies 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 60 , 61 , 64 , 66 , 67 , 68 , 69 , 70 , 71 , 73 , 74 , 75 , 76 , 77 , 80 , 81 , 82 , 83 , 87 , 88 , 91 , 93 , 96 , 97 , 99 , 101 , 104 , 105 , 106 , 107 , 108 , 109 , 112 , 113 , 114 , 116 , 117 , 119 , 120 , 122 , 124 , 125 , 126 , 127 , 129 , 130 , 131 , 132 , 133 , 134 , 136 , 138 , 139 , 140 , n = 280,607, Fig. 1 ); 26.9% (95% CI 24.0–30.0) for anxiety (75 studies 35 , 37 , 38 , 40 , 42 , 43 , 44 , 46 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 60 , 61 , 64 , 66 , 67 , 68 , 69 , 71 , 73 , 74 , 75 , 76 , 77 , 80 , 81 , 82 , 83 , 87 , 88 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 104 , 105 , 107 , 108 , 109 , 112 , 113 , 114 , 115 , 116 , 117 , 119 , 120 , 122 , 124 , 125 , 126 , 129 , 130 , 131 , 132 , 133 , 134 , 136 , 138 , 139 , 140 , n = 284,813, Fig. 2 ); 24.1% (95% CI 17.0–32.0) for PTSS (28 studies 35 , 44 , 56 , 59 , 62 , 64 , 66 , 69 , 75 , 78 , 80 , 81 , 82 , 89 , 90 , 91 , 106 , 109 , 110 , 111 , 119 , 123 , 124 , 125 , 127 , 131 , 135 , 138 , n = 56,447, Fig. 3 ); 36.5% (95% CI 30.0–43.3) for stress (22 studies 37 , 50 , 51 , 52 , 53 , 54 , 57 , 58 , 71 , 73 , 75 , 76 , 80 , 114 , 117 , 119 , 120 , 122 , 125 , 129 , 131 , 136 , n = 110,849, Fig. 4 ); 50.0% (95% CI 41.8–58.2) for psychological distress (18 studies 39 , 47 , 52 , 59 , 63 , 65 , 70 , 72 , 78 , 79 , 85 , 86 , 88 , 102 , 110 , 118 , 121 , 128 , n = 81,815, Fig. 5 ); and 27.6% (95% CI 19.8–36.1) for sleep problems (15 studies 35 , 53 , 58 , 80 , 84 , 103 , 106 , 107 , 109 , 119 , 120 , 125 , 134 , 136 , 137 , n = 99,534, Fig. 6 ). The prevalence of mental health problems based on different countries varied (Appendix, Table S6 ), from 14.5% (South Africa) to 63.3% (Brazil) for depressive symptoms; from 7.7% (Vietnam) to 49.9% (Mexico) for anxiety; from 10.5% (United Kingdom) to 52.0% (Egypt) for PTSS; from 19.7% (Portugal) to 72.8% (Thailand) for stress; from 23.9% (China) to Jordan (92.9%) for psychological distress; from 9.2% (Italy) to 53.9% (Thailand) for sleep problems.
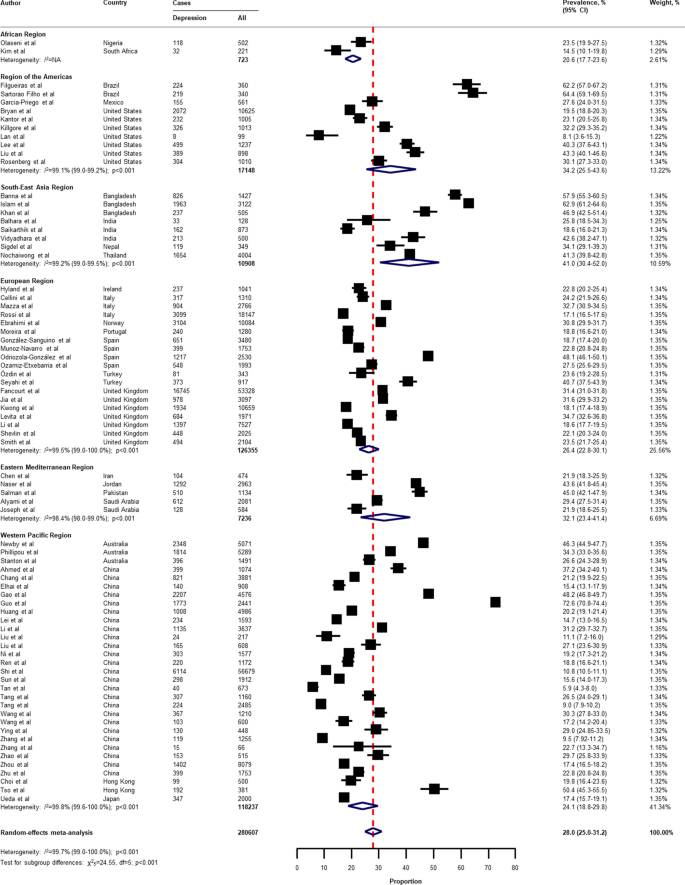
Pooled prevalence of depression among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
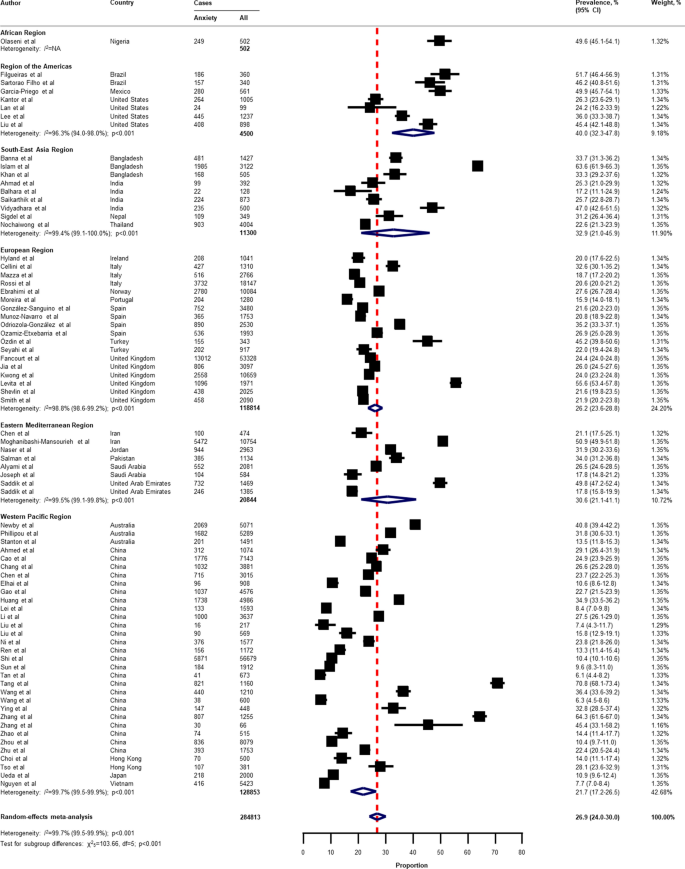
Pooled prevalence of anxiety among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
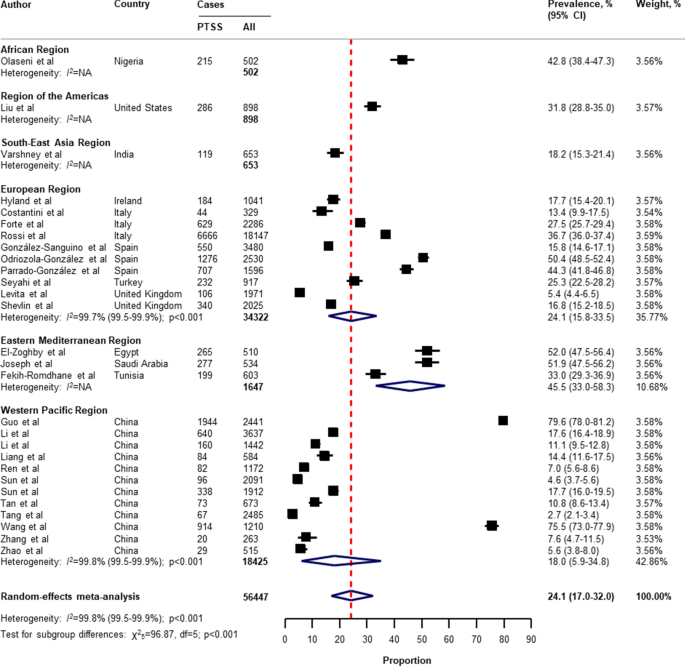
Pooled prevalence of PTSS among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable, PTSS post-traumatic stress symptoms. References are listed according to WHO region in the appendix, Table S3 .
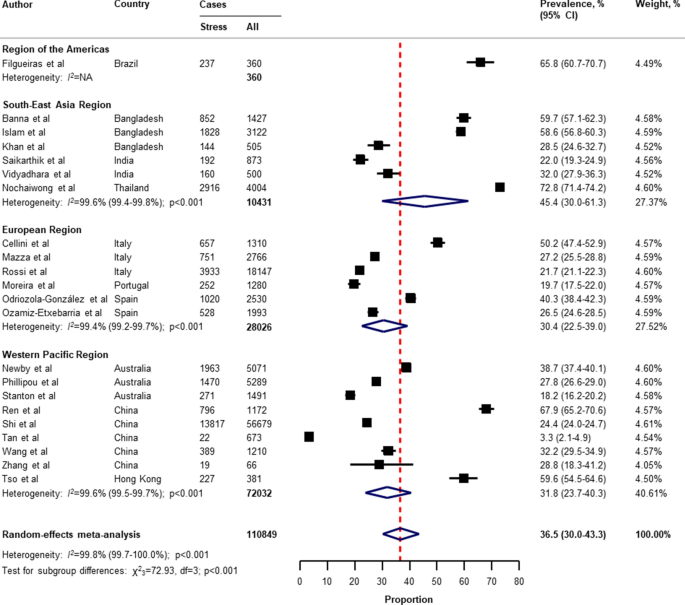
Pooled prevalence of stress among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
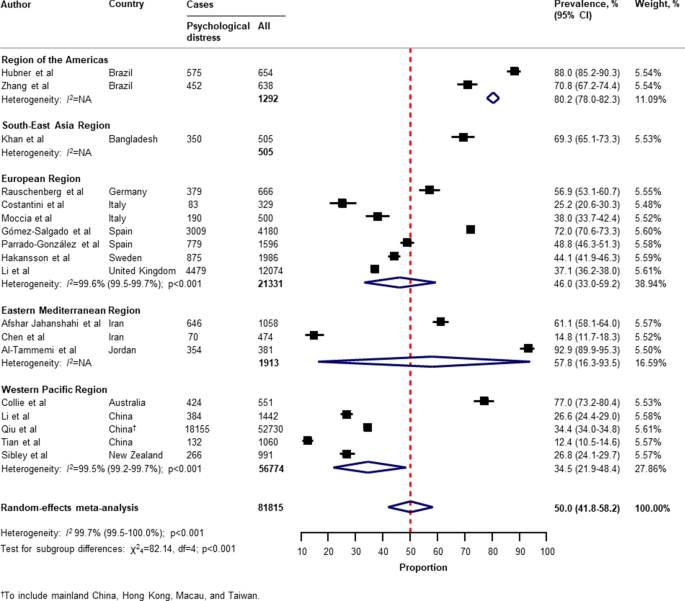
Pooled prevalence of psychological distress among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
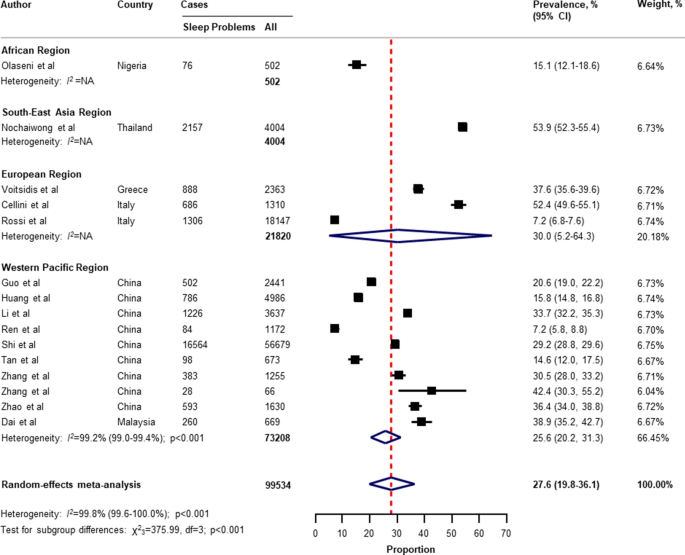
Pooled prevalence of sleep problems among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
With respect to the small number of included studies and high degree of heterogeneity, the pooled secondary outcome prevalence estimates are presented in Appendix, Table S7 . The global prevalence was 16.4% (95% CI 4.8–33.1) for suicide ideation (4 studies 36 , 41 , 53 , 124 , n = 17,554); 53.8% (95% CI 42.4–63.2) for loneliness (3 studies 41 , 44 , 45 , n = 2921); 30.7% (95% CI 2.1–73.3) for somatic symptoms (3 studies 53 , 69 , 134 , n = 7230); 28.6% (95% CI 9.2–53.6) for low wellbeing (3 studies 53 , 68 , 97 , n = 15,737); 50.5% (95% CI 49.2–51.7) for alcohol drinking problems (2 studies 97 , 114 , n = 6145); 6.4% (95% CI 5.5–7.4) for obsessive–compulsive symptoms (2 studies 73 , 134 , n = 2535); 25.7% (95% CI 23.7–27.8) for panic disorder (1 study 74 , n = 1753); 2.4% (95% CI 1.6–3.4) for phobia anxiety (1 study 134 , n = 1255); 22.8% (95% CI 22.1–23.4) for adjustment disorder (1 study 80 , n = 18,147); and 1.2% (95% CI 1.0–1.4) for suicide attempts (1 study 36 , n = 10,625).
Subgroup analyses, sensitivity analyses, meta-regression analyses, and publication bias
In the subgroup analyses (Appendix, Table S8 , Table S9 , Table S10 , Table S1 , Table S12 ), the prevalence of mental health problems was higher in countries with a low to medium HDI (for depression, anxiety, PTSS, and psychological distress), high HDI (for sleep problems), high gender inequality index (for depression and PTSS), very stringent government response index (for PTSS and stress), less stringent government response index (for sleep problems), low to medium hospital beds per 10,000 people (for depression, anxiety, PTSS, stress, psychological distress, and sleep problems), low to medium current health expenditure (for depression, PTSS, and psychological distress), estimated percent change of real GDP growth 2020 below − 3.0 (for psychological distress), low resilience (fourth-quartile) of business environment (for depression, anxiety, and PTSS), medium resilience (second-quartile) of business environment (for psychological distress, and sleep problems), high economic vulnerability-inbound tourism expenditure (for psychological distress, sleep problems), article type-short communication/letter/correspondence (for stress), cross-sectional survey (for PTSS and psychological distress), longitudinal survey (for anxiety and stress), non-mainland China (for depression, anxiety, and psychological distress), sample size of less than 1000 (for psychological distress), sample size of more than 5000 (for PTSS), proportion of females more than 60% (for stress and sleep problems), and measurement tools (for depression, anxiety, stress, and sleep problems). However, several pre-planned subgroup analyses based on participant characteristics and secondary outcomes reported could not be performed due to limited data in the included studies.
Findings from the sensitivity analysis were almost identical to the main analysis (Appendix, Table S14 ). The pooled prevalence by restricting the analysis to studies with a low risk of bias was 28.6% (95% CI 25.1–32.3) for depression, 27.4% (95% CI 24.1–30.8) for anxiety, 30.2% (95% CI 20.3–41.1) for PTSS, 40.1% (95% CI 32.5–47.9) for stress, 45.4% (95% CI 32.0–59.2) for psychological distress, and 27.7% (95% CI 19.4–36.9) for sleep problems.
On the basis of univariate meta-regression, the analysis was suitable for the primary outcomes (Appendix, Table S15 ). The increased prevalence of mental health problems was associated with the WHO region (for depression, anxiety, and psychological distress), female gender inequality index (for depression and anxiety), the COVID-19-government response stringency index during the survey (for sleep problems), hospital beds per 10,000 people (for depression and anxiety), immediate economic vulnerability-inbound tourism expenditure (for sleep problems), study design (cross-sectional vs longitudinal survey; for stress), surveyed country (mainland China vs non-mainland China; for depression and psychological distress), and risk of bias (for PTSS).
The visual inspection of the funnel plots, and the p values tested for asymmetry using the Begg’s and Egger’s tests for each prevalence outcome, indicated no evidence of publication bias related to the sample size (Appendix, Table S16 , and Figure S2 ).
This study is, to the best of our knowledge, the first systematic review and meta-analysis on the overall global prevalence of mental health problems and psychosocial consequences among the general population amid the COVID-19 pandemic. Overall, our findings indicate wide variability in the prevalence of mental health problems and psychosocial consequences across countries, particularly in relation to different regions, the global index of COVID-19 pandemic preparedness, inequalities, and economic vulnerabilities indices.
Two reports examined the global prevalence of common mental health disorders among adults prior to the COVID-19 outbreak. The first study was based on 174 surveys across 63 countries from 1980 to 2013. The estimated lifetime prevalence was 29.1% for all mental disorders, 9.6% for mood disorders, 12.9% for anxiety disorders, and 3.4% for substance use disorder 141 . Another report which was conducted as part of the Global Health Estimates by WHO in 2015, showed that the global estimates of depression and anxiety were 4.4% and 3.6% (more common among females than males), respectively 142 . Despite the different methodological methods used, our findings show that the pooled prevalence of mental health problems during the COVID-19 pandemic is higher than before the outbreak.
Previous studies on the prevalence of mental health problems during the COVID-19 pandemic have had substantial heterogeneity. Three systematic reviews reported the prevalence of depression, anxiety, and stress among the general population (mainly in mainland China). The first of these by Salari et al. 11 , was based on 17 included studies (from ten different countries in Asia, Europe, and the Middle East), the pooled prevalence of depression, anxiety, and stress were 33.7% (95% CI 27.5–40.6), 31.9% (95% CI 27.5–36.7), and 29.6% (95% CI 24.3–35.4), respectively. A review by Luo et al. 8 , which included 36 studies from seven different countries, reported a similar overall prevalence of 27% (95% CI 22–33) for depression and 32% (95% CI 25–39) for anxiety. However, a review by Ren et al. 17 , which focussed on only the Chinese population (8 included studies), found that the pooled prevalence was 29% (95% CI 16–42) and 24% (95% CI 16–32), respectively. Nevertheless, previous systematic reviews have been mainly on investigating the prevalence of PTSS, psychological distress, and sleep problems among the patients or healthcare workers that are limited to the general population during the COVID-19 pandemic. With regard to the general population, a review by Cénat et al. 143 , found that the pooled prevalence of PTSS, psychological distress, and insomnia were 22.4% (95% CI 7.6–50.3; 9 included studies), 10.2% (95% CI 4.6–21.0; 10 included studies), and 16.5% (95% CI 8.4–29.7; 8 included studies), respectively.
In this systematic review and meta-analysis, we updated and summarised the global prevalence of mental health problems and psychosocial consequences during the COVID-19 pandemic using information from 32 different countries, and 398,771 participants. A range of problems, including depression, anxiety, PTSS, stress, psychological distress, and sleep problems were reported. The global prevalence of our findings was in line with the previous reviews mentioned above in terms of depression (28.0%; 95% CI 25.0–31.2), anxiety (26.9%; 95% CI 24.0–30.0), and stress (36.5%; 95% CI 30.0–43.3). Interestingly, our findings highlight the poverty impacts of COVID-19 in terms of inequalities, the preparedness of countries to respond, and economic vulnerabilities on the prevalence of mental health problems across countries. For instance, our results suggest that countries with a low or medium HDI had a higher prevalence of depression and anxiety compared to countries with a high or very high HDI (Appendix, Table S8 , and Table S9 ). The prevalence of depression was higher among countries with a gender inequality index of 0.439 or greater (39.6% [95% CI 30.3–49.3] vs 26.2% [95% CI 23.1–29.3]; P = 0.020; Appendix, Table S8 ). Likewise, the prevalence of depression and anxiety was higher among countries with low hospital beds per 10,000 people (Appendix, Table S8 , and Table S9 ). Our findings suggest that the poverty impacts of COVID-19 are likely to be quite significant and related to the subsequent risk of mental health problems and psychosocial consequences. Although we performed a comprehensive review by incorporating articles published together with preprint reports, there was only limited data available on Africa, low-income groups, and secondary outcomes of interest (psychological distress, suicide ideation, suicide attempts, loneliness, somatic symptoms, wellbeing, alcohol drinking problems, obsessive–compulsive symptoms, panic disorder, phobia anxiety, and adjustment disorder).
Strengths and limitations of this review
From a methodological point of view, we used a rigorous and comprehensive approach to establish an up-to-date overview of the evidence-based information on the global prevalence of mental health problems amid the COVID-19 pandemic, with no language restrictions. The systematic literature search was extensive, comprising published peer-reviewed articles and preprints reporting data to present all relevant literature, minimise bias, and up to date evidence. Our findings expanded and addressed the limitations of the previous systematic reviews, such as having a small sample size and number of included studies, considered more aspects of mental health circumstance, and the generalisability of evidence at a global level 5 , 6 , 11 , 17 , 18 . To address biases from different measurement tools of assessment and the cultural norms across countries, we summarised the prevalence of mental health problems and psychosocial consequences using a random-effects model to estimate the pooled data with a more conservative approach. Lastly, the sensitivity analyses were consistent with the main findings, suggesting the robustness of our findings. As such, our data can be generalised to individuals in the countries where the included studies were conducted.
There were several limitations to this systematic review and meta-analysis. First, despite an advanced comprehensive search approach, data for some geographical regions according to the WHO regions and World Bank income groups, for instance, the Africa region, as well as the countries in the low-income group, were limited. Moreover, the reporting of key specific outcomes, such as suicide attempts and ideation, alcohol drinking or drug-dependence problems, and stigma towards COVID-19 infection were also limited. Second, a subgroup analysis based on participant characteristics (that is, age, sex, unemployment, history of mental illness, financial problems, and quarantine status), could not be performed as not all of the included studies reported this data. Therefore, the global prevalence of mental health problems and psychosocial consequences amid the COVID-19 pandemic cannot be established. Third, it should be noted that different methods, for example, face-to-face interviews or paper-based questionnaires, may lead to different prevalence estimates across the general population. Due to physical distancing, the included studies in this review mostly used online surveys, which can be prone to information bias and might affect the prevalence estimates of our findings. Fourth, a high degree of heterogeneity between the included studies was found in all outcomes of interest. Even though we performed a set of subgroup analyses concerning the participant characteristics, study characteristics, the global index, and economic indices responses to the COVID-19 pandemic, substantial heterogeneity persisted. However, the univariate meta-regression analysis suggested that the WHO region, gender inequality index, COVID-19-government response stringency index during the survey, hospital beds, immediate economic vulnerability (inbound tourism expenditure), study design, surveyed country (mainland China vs non-mainland China), and risk of bias were associated with an increased prevalence of mental health problems and psychosocial consequences amid the COVID-19 pandemic. Finally, we underline that the diagnostic cut-off criteria used were not uniform across the measurement tools in this review, and misclassification remains possible. The genuine variation in global mental health circumstances across countries cannot be explained by our analyses. Indeed, such variation might be predisposed by social and cultural norms, public resilience, education, ethnic differences, and environmental differences among individual study populations.
Implications for public health and research
Despite the limitations of our findings, this review provides the best available evidence that can inform the epidemiology of public mental health, implement targeted initiatives, improving screening, and reduce the long-term consequences of the COVID-19 pandemic, particularly among low-income countries, or those with high inequalities, low preparedness, and high economic vulnerability. Our findings could be improved by further standardised methods and measurement tools of assessment. There is a need for individual country-level data on the mental health problems and psychosocial consequences after the COVID-19 pandemic to track and monitor public health responses. There are a number network longitudinal surveys being conducted in different countries that aim to improve our understanding of the long-term effects of the COVID-19 pandemic 144 . To promote mental wellbeing, such initiatives could also be advocated for by public health officials and governments to increase awareness and provide timely proactive interventions in routine practice.
Conclusions
In conclusion, this systematic review and meta-analysis provides a more comprehensive global overview and evidence of the prevalence of mental health problems among the general population amid the COVID-19 pandemic. The results of this study reveal that the mental health problems and psychosocial consequences amid the COVID-19 pandemic are a global burden, with differences between countries and regions observed. Moreover, equality and poverty impacts were found to be factors in the prevalence of mental health problems. Studies on the long-term effects of the COVID-19 pandemic on the mental health status among the general population at a global level is needed. Given the high burden of mental health problems during the COVID-19 pandemic, an improvement of screening systems and prevention, prompt multidisciplinary management, and research on the social and economic burden of the pandemic, are crucial.
Data sharing
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Mahase, E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ 368 , m1036 (2020).
Article PubMed Google Scholar
Pfefferbaum, B. & North, C. S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 383 , 510–512 (2020).
Article CAS PubMed Google Scholar
Burki, T. K. Coronavirus in China. Lancet Respir. Med. 8 , 238 (2020).
Article CAS PubMed PubMed Central Google Scholar
Chen, Q. et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 7 , e15–e16 (2020).
Article PubMed PubMed Central Google Scholar
Vindegaard, N. & Benros, M. E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 89 , 531–542. https://doi.org/10.1016/j.bbi.2020.05.048 (2020).
Pappa, S. et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 88 , 901–907 (2020).
Salazar de Pablo, G. et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 275 , 48–57 (2020).
Luo, M., Guo, L., Yu, M., Jiang, W. & Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public: a systematic review and meta-analysis. Psychiatry Res. 291 , 113190 (2020).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 , 912–920 (2020).
Kaufman, K. R., Petkova, E., Bhui, K. S. & Schulze, T. G. A global needs assessment in times of a global crisis: world psychiatry response to the COVID-19 pandemic. BJPsych Open 6 , e48 (2020).
Article PubMed CAS Google Scholar
Salari, N. et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health 16 , 57 (2020).
Article Google Scholar
Kawohl, W. & Nordt, C. COVID-19, unemployment, and suicide. Lancet Psychiatry 7 , 389–390 (2020).
Frasquilho, D. et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health 16 , 115 (2016).
World Bank. Global Economic Prospects, June 2020 (World Bank, 2020).
Book Google Scholar
Kovacevic, M. & Jahic, A. COVID-19 and Human Development: Exploring Global Preparedness and Vulnerability (Human Development Report Office, UNDP, 2020).
Google Scholar
Conceicao, P. et al. COVID-19 and Human Development: Assessing the Crisis, Envisioning the Recovery (Human Development Report Office, UNDP, 2020).
Ren, X. et al. Mental health during the Covid-19 outbreak in China: a meta-analysis. Psychiatr. Q. 91 (4), 1033–1045. https://doi.org/10.1007/s11126-020-09796-5 (2020).
Rogers, J. P. et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 7 , 611–627 (2020).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339 , b2535 (2009).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283 , 2008–2012 (2000).
Hoy, D. et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J. Clin. Epidemiol. 65 , 934–939 (2012).
Viera, A. J. & Garrett, J. M. Understanding interobserver agreement: the kappa statistic. Fam. Med. 37 , 360–363 (2005).
PubMed Google Scholar
Nyaga, V. N., Arbyn, M. & Aerts, M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health 72 , 39 (2014).
Cochran, W. G. The combination of estimates from different experiments. Biometrics 10 , 101–129 (1954).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21 , 1539–1558 (2002).
Human Development Report Office. Human Development Report 2019–Beyond Income, Beyond Averages, Beyond Today: Inequalities in Human DEVELOPMENT in the 21st century (United Nations Development Programme (UNDP), 2019).
Human Development Report Office. 2020 Human Development Persepctives: Tackling Social Norms–A game changer for gender inequalities (United National Development Programme (UNDP), 2020).
Hale, T. et al. Variation in government responses to COVID-19. Version 6.0. Blavatnik School of Government Working Paper. https://www.bsg.ox.ac.uk/covidtracker (2020).
International Monetary Fund (IMF). World Economic Outlook (April 2020), Real GDP growth Annual percent change . Accessed 29 July 2020. https://www.imf.org/external/datamapper/NGDP_RPCH@WEO/OEMDC/ADVEC/WEOWORLD (2020).
FM Global. 2020 FM Global Resilience Index: Make a Resilient Decision . Accessed 30 July 2020. https://www.fmglobal.com/research-and-resources/tools-and-resources/resilienceindex (2020).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50 , 1088–1101 (1994).
Article CAS PubMed MATH Google Scholar
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315 , 629–634 (1997).
Duval, S. & Tweedie, R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56 , 455–463 (2000).
Kim, A. W., Nyengerai, T. & Mendenhall, E. Evaluating the mental health impacts of the COVID-19 pandemic in urban South Africa: perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms. medRxiv. 2020.2006.2013.20130120 (2020).
Olaseni, A., Akinsola, O., Agberotimi, S. & Oguntayo, R. Psychological distress experiences of Nigerians amid COVID-19 pandemic. PsyArXiv May 6. 1031234/osfio/9v78y (2020).
Bryan, C., Bryan, A. O. & Baker, J. C. Associations among state-level physical distancing measures and suicidal thoughts and behaviors among U.S. adults during the early COVID-19 pandemic. PsyArXiv May 29 . 1031234/osfio/9bpr4 (2020).
Filgueiras, A. & Stults-Kolehmainen, M. Factors linked to changes in mental health outcomes among Brazilians in quarantine due to COVID-19. medRxiv. 2020.2005.2012.20099374 (2020).
Garcia-Priego, B. A. et al. Anxiety, depression, attitudes, and internet addiction during the initial phase of the 2019 coronavirus disease (COVID-19) epidemic: a cross-sectional study in Mexico. medRxiv. 2020.2005.2010.20095844 (2020).
Hubner, C. v. K., Bruscatto, M. L. & Lima, R. D. Distress among Brazilian university students due to the Covid-19 pandemic: survey results and reflections. medRxiv. 2020.2006.2019.20135251 (2020).
Kantor, B. N. & Kantor, J. Mental health outcomes and associations during the coronavirus disease 2019 pandemic: a cross-sectional survey of the US general population. medRxiv. 2020.2005.2026.20114140 (2020).
Killgore, W. D. S., Cloonan, S. A., Taylor, E. C. & Dailey, N. S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 290 , 113117 (2020).
Lan, F.-Y., Suharlim, C., Kales, S. N. & Yang, J. Association between SARS-CoV-2 infection, exposure risk and mental health among a cohort of essential retail workers in the United States. medRxiv. 2020.2006.2008.20125120 (2020).
Lee, S. A., Jobe, M. C. & Mathis, A. A. Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol. Med. 1–2. https://doi.org/10.1017/S003329172000121X (2020).
Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S. & Hahm, H. C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 290 , 113172 (2020).
Rosenberg, M., Luetke, M., Hensel, D., Kianersi, S. & Herbenick, D. Depression and loneliness during COVID-19 restrictions in the United States, and their associations with frequency of social and sexual connections. medRxiv. 2020.2005.2018.20101840 (2020).
Sartorao Filho, C. I. et al. Impact of COVID-19 pandemic on mental health of medical students: a cross-sectional study using GAD-7 and PHQ-9 questionnaires. medRxiv. 2020.2006.2024.20138925 (2020).
Zhang, S. X., Wang, Y., Afshar Jahanshahi, A., Li, J. & Haensel Schmitt, V. G. Mental distress of adults in Brazil during the COVID-19 crisis. medRxiv. 2020.2004.2018.20070896 (2020).
Ahmad, A., Rahman, I. & Agarwal, M. Factors influencing mental health during COVID-19 outbreak: an exploratory survey among Indian population. medRxiv. 2020.2005.2003.20081380 (2020).
Balhara, Y. P. S., Kattula, D., Singh, S., Chukkali, S. & Bhargava, R. Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J. Public Health. 64 , S172-176 (2020).
Banna, H. A. et al. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. PsyArXiv May 24 . 1031234/osfio/chw5d. (2020).
Islam, M. S. et al. Psychological eesponses during the COVID-19 outbreak among university students in Bangladesh. PsyArXiv June 2 . 1031234/osfio/cndz7. (2020).
Khan, A. H. et al. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. PsyArXiv May 15 . 1031234/osfio/97s5r. (2020).
Nochaiwong, S. et al. Mental health circumstances among health care workers and general public under the pandemic situation of COVID-19 (HOME-COVID-19). Medicine (Baltimore) 99 , e20751 (2020).
Article CAS Google Scholar
Saikarthik, J., Saraswathi, I. & Siva, T. Assessment of impact of COVID-19 outbreak & lockdown on mental health status & its associated risk and protective factors in adult Indian population. medRxiv. 2020.2006.2013.20130153 (2020).
Sigdel, A. et al. Depression, anxiety and depression-anxiety comorbidity amid COVID-19 pandemic: an online survey conducted during lockdown in Nepal. medRxiv. 2020.2004.2030.20086926 (2020).
Varshney, M., Parel, J. T., Raizada, N. & Sarin, S. K. Initial psychological impact of COVID-19 and its correlates in Indian Community: an online (FEEL-COVID) survey. PLoS ONE 15 , e0233874 (2020).
Vidyadhara, S., Chakravarthy, A., Pramod Kumar, A., Sri Harsha, C. & Rahul, R. Mental health status among the South Indian pharmacy students during Covid-19 pandemic quarantine period: a cross-sectional study. medRxiv. 2020.2005.2008.20093708 (2020).
Cellini, N., Canale, N., Mioni, G. & Costa, S. Changes in sleep pattern sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 29 , e13074 (2020).
Costantini, A. & Mazzotti, E. Italian validation of CoViD-19 Peritraumatic Distress Index and preliminary data in a sample of general population. Riv. Psichiatr. 55 , 145–151 (2020).
Ebrahimi, O., Hoffart, A. & Johnson, S. U. The mental health impact of non-pharmacological interventions aimed at impeding viral transmission during the COVID-19 pandemic in a general adult population and the factors associated with adherence to these mitigation strategies. PsyArXiv May 9 . 1031234/osfio/kjzsp. (2020).
Fancourt, D., Steptoe, A. & Bu, F. Trajectories of depression and anxiety during enforced isolation due to COVID-19: longitudinal analyses of 59,318 adults in the UK with and without diagnosed mental illness. medRxiv. 2020.2006.2003.20120923 (2020).
Forte, G., Favieri, F., Tambelli, R. & Casagrande, M. COVID-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int. J. Environ. Res. Public Health 17 , 4151 (2020).
Article CAS PubMed Central Google Scholar
Gómez-Salgado, J., Andrés-Villas, M., Domínguez-Salas, S., Díaz-Milanés, D. & Ruiz-Frutos, C. Related health factors of psychological distress during the COVID-19 pandemic in Spain. Int. J. Environ. Res. Public Health 17 , 3947 (2020).
Article PubMed Central CAS Google Scholar
González-Sanguino, C. et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 87 , 172–176 (2020).
Article PubMed PubMed Central CAS Google Scholar
Håkansson, A. Changes in gambling behavior during the COVID-19 pandemic: a web survey study in Sweden. Int. J. Environ. Res. Public Health 17 , 4013 (2020).
Hyland, P. et al. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. PsyArXiv April 22. 1031234/osfio/8yqxr. (2020).
Jia, R. et al. Mental health in the UK during the COVID-19 pandemic: early observations. medRxiv. 2020.2005.2014.20102012 (2020).
Kwong, A. S. F. et al. Mental health during the COVID-19 pandemic in two longitudinal UK population cohorts. medRxiv. 2020.2006.2016.20133116 (2020).
Levita, L. et al. Impact of Covid-19 on young people aged 13–24 in the UK- preliminary findings. PsyArXiv June 30. 1031234/osfio/uq4rn. (2020).
Li, L. Z. & Wang, S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom: results from the Understanding Society UKHLS. medRxiv. 2020.2006.2009.20120139 (2020).
Mazza, C. et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health 17 , 3165 (2020).
Moccia, L. et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 87 , 75–79 (2020).
Moreira, P. S. et al. Protective elements of mental health status during the COVID-19 outbreak in the Portuguese population. medRxiv. 2020.2004.2028.20080671 (2020).
Munoz-Navarro, R., Cano-Vindel, A., Schmitz, F., Cabello, R. & Fernandez-Berrocal, P. Emotional distress and associated sociodemographic risk factors during the COVID-19 outbreak in Spain. medRxiv. 2020.2005.2030.20117457 (2020).
Odriozola-González, P., Planchuelo-Gómez, Á., Irurtia, M. J. & de Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 290 , 113108 (2020).
Ozamiz-Etxebarria, N., Idoiaga Mondragon, N., Dosil Santamaría, M. & Picaza Gorrotxategi, M. Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: an investigation in a sample of citizens in Northern Spain. Front. Psychol. 11 , 1491 (2020).
Özdin, S. & Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatry 66 , 504–511 (2020).
Parrado-González, A. & León-Jariego, J. C. Covid-19: factors associated with emotional distress and psychological morbidity in Spanish population. Rev. Esp. Salud Publica 94 , e202006058 (2020).
Rauschenberg, C. et al. Social isolation, mental health and use of digital interventions in youth during the COVID-19 pandemic: a nationally representative survey. PsyArXiv June 29 . 1031234/osfio/v64hf (2020).
Rossi, R. et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N = 18147 web-based survey. medRxiv. 2020.2004.2009.20057802 (2020).
Seyahi, E., Poyraz, B. C., Sut, N., Akdogan, S. & Hamuryudan, V. The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey. Rheumatol. Int. 40 , 1229–1238 (2020).
Shevlin, M. et al. Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 pandemic. PsyArXiv April 18. 1031234/osfio/hb6nq (2020).
Smith, L. E. et al. Factors associated with self-reported anxiety, depression, and general health during the UK lockdown; a cross-sectional survey. medRxiv. 2020.2006.2023.20137901 (2020).
Voitsidis, P. et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 289 , 113076 (2020).
Afshar Jahanshahi, A., Mokhtari Dinani, M., Nazarian Madavani, A., Li, J. & Zhang, S. X. The distress of Iranian adults during the Covid-19 pandemic: more distressed than the Chinese and with different predictors. medRxiv. 2020.2004.2003.20052571 (2020).
Al-Tammemi, A. a. B., Akour, A. & Alfalah, L. Is it just about physical health? An internet-based cross-sectional study exploring the psychological impacts of COVID-19 pandemic on university students in Jordan using Kessler psychological distress scale. medRxiv. 2020.2005.2014.20102343 (2020).
Alyami, H. S. et al. Depression and anxiety during 2019 coronavirus disease pandemic in Saudi Arabia: a cross-sectional study. medRxiv. 2020.2005.2009.20096677 (2020).
Chen, J. et al. The curvilinear relationship between the age of adults and their mental health in Iran after its peak of COVID-19 cases. medRxiv. 2020.2006.2011.20128132 (2020).
El-Zoghby, S. M., Soltan, E. M. & Salama, H. M. Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. J. Community Health 45 , 689–695 (2020).
Fekih-Romdhane, F., Ghrissi, F., Abbassi, B., Cherif, W. & Cheour, M. Prevalence and predictors of PTSD during the COVID-19 pandemic: findings from a Tunisian community sample. Psychiatry Res. 290 , 113131 (2020).
Joseph, R., Alshayban, D., Lucca, J. M. & Alshehry, Y. A. The immediate psychological response of the general population in Saudi Arabia during COVID-19 pandemic: a cross-sectional study. medRxiv. 2020.2006.2019.20135533 (2020).
Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatr. 51 , 102076 (2020).
Naser, A. Y. et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. 10 (8), e01730. https://doi.org/10.1002/brb3.1730 (2020).
Saddik, B. et al. Assessing the influence of parental anxiety on childhood anxiety during the COVID-19 pandemic in the United Arab Emirates. medRxiv. 2020.2006.2011.20128371 (2020).
Saddik, B. et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. medRxiv. 2020.2005.2010.20096933 (2020).
Salman, M. et al. Psychological impact of COVID-19 on Pakistani university students and how they are coping. medRxiv. 2020.2005.2021.20108647 (2020).
Ahmed, M. Z. et al. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatr. 51 , 102092 (2020).
Cao, W. et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 287 , 112934 (2020).
Chang, J., Yuan, Y. & Wang, D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao 40 , 171–176 (2020).
Chen, S. H. et al. Public anxiety and its influencing factors in the initial outbreak of COVID-19. Fudan Univ. J. Med. Sci. 47 , 385–391 (2020).
Choi, E. P. H., Hui, B. P. H. & Wan, E. Y. F. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 17 , 3740 (2020).
Collie, A. et al. Psychological distress among people losing work during the COVID-19 pandemic in Australia. medRxiv. 2020.2005.2006.20093773 (2020).
Dai, H., Zhang, S. X., Looi, K. H., Su, R. & Li, J. Health condition and test availability as predictors of adults' mental health during the COVID-19 pandemic. medRxiv. 2020.2006.2021.20137000 (2020).
Elhai, J. D., Yang, H., McKay, D. & Asmundson, G. J. G. COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. J. Affect. Disord. 274 , 576–582 (2020).
Gao, J. et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 15 , e0231924 (2020).
Guo, J., Feng, X. L., Wang, X. H. & van IJzendoorn, M. H. Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int. J. Environ. Res. Public Health 17 , 3857 (2020).
Huang, Y. & Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 288 , 112954 (2020).
Lei, L. et al. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med. Sci. Monit. 26 , e924609 (2020).
Li, Y. et al. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin. Sleep Med. https://doi.org/10.5664/jcsm.8524 (2020).
Li, Y. et al. Psychological distress among health professional students during the COVID-19 outbreak. Psychol. Med. 1–3. https://doi.org/10.1017/S0033291720001555 (2020).
Liang, L. et al. The effect of COVID-19 on youth mental health. Psychiatr. Q. 91 (3), 841–852. https://doi.org/10.1007/s11126-020-09744-3 (2020).
Liu, J. et al. Online mental health survey in a medical college in China during the COVID-19 outbreak. Front. Psychiatry 11 , 459 (2020).
Liu, X. et al. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect. Dis. Poverty 9 , 58 (2020).
Newby, J., O'Moore, K., Tang, S., Christensen, H. & Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. medRxiv. 2020.2005.2003.20089961 (2020).
Nguyen, H. T. et al. Fear of COVID-19 scale-associations of its scores with health literacy and health-related behaviors among medical students. Int. J. Environ. Res. Public Health 17 , 4164 (2020).
Ni, M. Y. et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Ment. Health 7 , e19009 (2020).
Phillipou, A. et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: initial results from the COLLATE project. Int. J. Eat. Disord. 53 , 1158–1165 (2020).
Qiu, J. et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 33 , e100213 (2020).
Ren, Y. et al. Letter to the Editor “A longitudinal study on the mental health of general population during the COVID-19 epidemic in China”. Brain Behav. Immun. 87 , 132–133 (2020).
Shi, L. et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open 3 , e2014053 (2020).
Sibley, C. G. et al. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am. Psychol. 75 , 618–630 (2020).
Stanton, R. et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health 17 , 4065 (2020).
Sun, L. et al. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. medRxiv. 2020.2003.2006.20032425 (2020).
Sun, S., Goldberg, S. B., Lin, D., Qiao, S. & Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. medRxiv. 2020.2007.2003.20144931 (2020).
Tan, W. et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 87 , 84–92 (2020).
Tang, F. et al. COVID-19 related depression and anxiety among quarantined respondents. Psychol. Health 36 (2), 164–178. https://doi.org/10.1080/08870446.2020.1782410 (2020).
Tang, W. et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 274 , 1–7 (2020).
Tian, F. et al. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 288 , 112992 (2020).
Tso, I. F. & Sohee, P. Alarming levels of psychiatric symptoms and the role of loneliness during the COVID-19 epidemic: a case study of Hong Kong. PsyArXiv published online June 27. 1031234/osfio/wv9y2 (2020).
Ueda, M., Stickley, A., Sueki, H. & Matsubayashi, T. Mental health status of the general population during the COVID-19 pandemic: a cross-sectional national survey in Japan. medRxiv. 2020.2004.2028.20082453 (2020).
Wang, C. et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17 , 1729 (2020).
Wang, Y., Di, Y., Ye, J. & Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 26 (1), 13–22. https://doi.org/10.1080/13548506.2020.1746817 (2020).
Ying, Y. et al. Mental health status among family members of health care workers in Ningbo, China during the Coronavirus Disease 2019 (COVID-19) outbreak: a Cross-sectional Study. medRxiv. 2020.2003.2013.20033290 (2020).
Zhang, W. R. et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 89 , 242–250 (2020).
Zhang, Y. & Ma, Z. F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int. J. Environ. Res. Public Health 17 , 2381 (2020).
Zhang, Y., Zhang, H., Ma, X. & Di, Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int. J. Environ. Res. Public Health 17 , 3722 (2020).
Zhao, X., Lan, M., Li, H. & Yang, J. Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: a moderated mediation model. Sleep Med. S1389–9457 (1320), 30224–30220. https://doi.org/10.1016/j.sleep.2020.05.021 (2020).
Zhao, Y., An, Y., Tan, X. & Li, X. Mental health and its influencing factors among self-isolating ordinary citizens during the beginning epidemic of COVID-19. J. Loss Trauma https://doi.org/10.1080/15325024.15322020.11761592 (2020).
Zhou, S. J. et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 29 , 749–758 (2020).
Zhu, S. et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav.. Immun. 87 , 56–58 (2020).
Steel, Z. et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 43 , 476–493 (2014).
World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates (World Health Organization, 2017).
Cénat, J. M. et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 295 , 113599 (2021).
COVID-MINDS Network. COVID-MINDS network: global mental health in the COVID-19 pandemic , https://www.covidminds.org/ (2020).
Download references
Acknowledgements
The authors thank the research assistances and all staff of Pharmacoepidemiology and Statistics Research Center (PESRC), Chiang Mai, Thailand. This work reported in this manuscript was partially supported by a grant by the Chiang Mai University, Thailand. The funder of the study had no role in the study design collection, analysis, or interpretation of the data, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit it for publication.
Author information
Authors and affiliations.
Department of Pharmaceutical Care, Faculty of Pharmacy, Chiang Mai University, Chiang Mai, 50200, Thailand
Surapon Nochaiwong, Chidchanok Ruengorn, Ratanaporn Awiphan, Chabaphai Phosuya & Yongyuth Ruanta
Pharmacoepidemiology and Statistics Research Center (PESRC), Faculty of Pharmacy, Chiang Mai University, Chiang Mai, 50200, Thailand
Surapon Nochaiwong, Chidchanok Ruengorn, Kednapa Thavorn, Ratanaporn Awiphan & Yongyuth Ruanta
Ottawa Hospital Research Institute, Ottawa Hospital, Ottawa, ON, K1H 8L6, Canada
Kednapa Thavorn & Brian Hutton
Institute of Clinical and Evaluative Sciences, ICES uOttawa, Ottawa, ON, K1Y 4E9, Canada
School of Epidemiology and Public Health, Faculty of Medicine, University of Ottawa, Ottawa, ON, K1G 5Z3, Canada
Department of Psychiatry, Faculty of Medicine, Chiang Mai University, Chiang Mai, 50200, Thailand
Nahathai Wongpakaran & Tinakon Wongpakaran
You can also search for this author in PubMed Google Scholar
Contributions
S.N. conceived the study and, together with C.R., K.T., R.A., C.P., and Y.R. developed the protocol. S.N. and C.R. did the literature search, selected the studies. S.N. and Y.R. extracted the relevant information. S.N. synthesised the data. S.N. wrote the first draft of the paper. K.T., B.H., N.W., and T.W. critically revised successive drafts of the paper. All authors approved the final draft of the manuscript. SN is the guarantor of the study.
Corresponding author
Correspondence to Surapon Nochaiwong .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary figures and tables., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Nochaiwong, S., Ruengorn, C., Thavorn, K. et al. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci Rep 11 , 10173 (2021). https://doi.org/10.1038/s41598-021-89700-8
Download citation
Received : 11 January 2021
Accepted : 29 April 2021
Published : 13 May 2021
DOI : https://doi.org/10.1038/s41598-021-89700-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Advancing Health Equity, Eliminating Health Disparities, and Improving Population Health
EDITORIAL — Volume 18 — August 12, 2021
Leonard Jack Jr, PhD, MSc 1 ( View author affiliations )
Suggested citation for this article: Jack L Jr. Advancing Health Equity, Eliminating Health Disparities, and Improving Population Health. Prev Chronic Dis 2021;18:210264. DOI: http://dx.doi.org/10.5888/pcd18.210264 .
Non-Peer Reviewed
Author Information
In June 2017, Preventing Chronic Disease (PCD) invited a panel of 7 nationally recognized experts in scientific publishing to respond to key questions about the journal’s mission, quality of scientific content, scope of operations, intended audience, and future direction (1). PCD and the panel of experts recognized that chronic disease is a major contributor to poor health outcomes, an increase in health care costs, and a reduction in quality of life. Reducing the burden of chronic disease is a challenge requiring diverse collaborations and dissemination and adoption of effective interventions in multiple settings. The expert panel strongly encouraged the journal to focus more on complementing its rich body of published work on epidemiological studies with content that is attentive to evaluating population-based interventions and policies.
Since its inception in 2004, PCD’s mission has been to promote dialogue among researchers, practitioners, and policy makers worldwide on the integration and application of research findings and practical experience to address health disparities, advance health equity, and improve population health. To better advance that mission, PCD used the panel’s recommendations to refine the journal’s focus, addressing 4 main areas of public health research, evaluation, and practice:
Behavioral, psychological, genetic, environmental, biological, and social factors that influence health
Development, implementation, and evaluation of population-based interventions to prevent chronic diseases and control their effect on quality of life, illness, and death
Interventions that reduce the disproportionate incidence of chronic diseases among at-risk populations
Development, implementation, and evaluation of public health law and health policy–driven interventions
Refining the focus on these 4 areas has allowed PCD to receive a wide range of content from authors around the world. In addition to manuscripts received through the journal’s regular submission process, PCD has issued calls for papers on topics that bring to the forefront timely public health issues and targeted public health responses to improve population health.
Advancing health equity and eliminating health disparities have been and continue to be critical factors to PCD in addressing these topic areas. Healthy People 2020 defines health equity as the attainment of the highest level of health for all people (2). According to Healthy People 2020, “Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and health care disparities” (2). Healthy People 2020 defines health disparities as “a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage” (2).
As part of its mission to address these important issues, PCD is excited to release this collection, “Advancing Health Equity, Eliminating Health Disparities, and Improving Population Health.” Of the 17 articles in the collection, 10 were submitted in response to PCD’s call for papers for the collection and 7 were previously published in the journal. All articles underwent the journal’s rigorous peer-review process. In addition, this collection features a position statement on the journal’s commitment to advancing diversity, equity, and inclusion in its scientific leadership, peer review process, research focus, training, and continuing education (3).
Over the past decade, there has been a range of community-based, technically innovative, and clinically driven prevention strategies in public health to prevent and reduce the burden of chronic conditions among diverse populations worldwide. Articles in this collection describe innovative and successful work to address factors contributing to advancing health equity, eliminating health disparities, and improving population health. They provide the latest information on ways to better understand contextual factors responsible for influencing health outcomes (both negatively and positively) and effective approaches to improve population health among diverse populations in various settings. The 18 articles address these core themes from multiple perspectives:
PCD’s Commitment to Advancing Diversity, Equity, and Inclusion in Its Scientific Leadership, Peer Review Process, Research Focus, Training, and Continuing Education (3)
Engaging With Communities — Lessons (Re)Learned From COVID-19 (4)
Global Perspectives on Improving Chronic Disease Prevention and Management in Diverse Settings (5)
Reaching the Hispanic Community About COVID-19 Through Existing Chronic Disease Prevention Programs (6)
Community Engagement of African Americans in the Era of COVID-19: Considerations, Challenges, Implications, and Recommendations for Public Health (7)
Addressing Racial and Ethnic Disparities in COVID-19 Among School-Aged Children: Are We Doing Enough? (8)
A Framework for Mobilizing Health Care to Respond to the Community Within the COVID-19 Pandemic (9)
Addressing Emotional Wellness During the COVID-19 Pandemic: The Role of Promotores in Delivering Integrated Mental Health Care and Social Services (10)
COVID-19 and Chronic Disease: The Impact Now and in the Future (11)
Screening and Referral Care Delivery Services and Unmet Health-Related Social Needs: A Systematic Review (12)
Community and Research Perspectives on Cancer Disparities in Wisconsin (13)
Urban–Rural Disparities in Access to Low-Dose Computed Tomography Lung Cancer Screening in Missouri and Illinois (14)
Quantification of Potential Inequities in Breast Cancer Incidence in New Mexico Through Bayesian Disease Mapping (15)
HbA 1c Performance in African Descent Populations in the United States With Normal Glucose Tolerance, Prediabetes, or Diabetes: A Scoping Review (16)
Reducing Tobacco Use in Oregon Through Multisector Collaboration: Aligning Medicaid and Public Health Programs (17)
“We’re, Like, the Most Unhealthy People in the Country”: Using an Equity Lens to Reduce Barriers to Healthy Food Access in Rural Appalachia (18)
Oral Health Behaviors in Very Young Children in Low-Income Urban Areas in Chicago, Illinois, 2018–2019 (19)
A Randomized Trial to Improve Adherence to Follow-up Eye Examinations Among People With Glaucoma (20)
Positioning a scientific journal to address matters related to diversity, equity, and inclusion requires careful and intentional thinking and action. Going back to PCD’s inaugural issue in 2004, featuring an essay on social determinants of health by Dr Leonard Symes, professor emeritus of epidemiology at the University of California, Berkeley, the journal has created a space to highlight the importance of these topics in chronic disease prevention and health promotion. Since that first issue, PCD has continued to demonstrate a dedication to these issues at all levels: through its leadership and staff, the content it publishes, its expanding pool of talented volunteers (PCD’s external review panel, editorial board, associate editors, statistics review committee), the rigorous peer-review process, a comprehensive and inclusive variety of article types, calls for papers related to these issues, and more. In its 18 years of publication, PCD has consistently worked to assure the public of its commitment to achieving diversity, equity, and inclusion.
Peer-reviewed journals around the world are also focusing attention on these issues. In keeping with this movement, as PCD’s editor in chief I have authored the first article featured in this collection, which is a position statement on the steps already taken by the journal, steps planned for the next 5 years, and key measurable outcomes (3). PCD hopes to serve as a model in identifying and implementing best practices for diversity, equity, and inclusion to build an even stronger trust with the public.
And trust is needed: mistrust of the health care system has emerged as a primary barrier among members of communities of color to seeking care in health care systems (21). Mistrust stems from historical events, including the Tuskegee syphilis study, and is reinforced by health system issues and discriminatory events that continue to this day (21). This collection includes an article by Michener and colleagues, which posits that COVID-19 has underscored long-standing societal differences in drivers of health (4). The authors offer insights into this historical reality and suggest using a health equity lens to engage communities at risk of poor health outcomes, improve bidirectional communication, establish data sharing, and improve involvement in program implementation, dissemination, and evaluation. Authors share concrete ways these can be achieved by presenting successful examples around the US.
The global impact of COVID-19 among people at risk or living with a chronic condition in multicultural communities necessitates that health communication messages are created and delivered from a health equity perspective (22). Airhihenbuwa and coauthors, in their commentary, discuss the importance of culture in unpacking messages that may be the same globally (eg, physical/social distancing) yet different across cultures and communities (individualist vs collectivist) (5). Authors discuss how use of the PEN-3 framework can facilitate a community-engaged communication response to COVID-19.
Populations with low socioeconomic status and certain racial and ethnic groups (eg, Native American, Hispanic, and African American people) have historically been disproportionately affected by chronic disease, COVID-19 diagnosis, hospitalization, and mortality (23). Calo and associates discuss how COVID-19 has disproportionately affected Hispanic communities throughout the US (6). This commentary describes how Better Together REACH, a community–academic coalition promoting chronic disease prevention, and Project ECHO (a telementoring program based at Penn State University), were adopted to support a coordinated COVID-19 response in the Hispanic community in Pennsylvania. Authors provide insights into how the existing infrastructure of chronic disease programs can be used to leverage resources and provide trusted and continuous services to reach Hispanic populations during the pandemic.
African Americans, like the Hispanic population, are more likely to contract COVID-19, be hospitalized, and die of the disease (24). Akintobi et al describe how psychosocial, sociocultural, and environmental vulnerabilities, compounded by preexisting health conditions, exacerbate the burden of COVID-19 among African Americans (7). Authors share important information based on their years of experience on ways to create and implement approaches to intentionally engage African Americans at higher risk of COVID-19. Insights and recommendations can advance community leadership and be used to prepare public health practitioners, researchers, and evaluators for future pandemics — both assisting in advancing health equity and addressing historical aspects of health disparities among African Americans.
The disproportionate impact of COVID-19 and associated disparities among Hispanic, non-Hispanic Black, and non-Hispanic American Indian/Alaska Native children and teenagers has been widely reported (25). Children from some racial and ethnic minority groups have a higher prevalence of obesity, asthma, type 2 diabetes, and hypertension; were diagnosed more frequently with COVID-19; and had more severe outcomes compared with their non-Hispanic White counterparts (26). In addition, a higher proportion of children from some racial and ethnic minority groups, compared with White children, live in families with incomes less than 200% of the federal poverty level or in households lacking secure employment (8). White et al argue that the COVID-19 pandemic reemphasizes the importance of implementing policy, systems, and environmental changes in school systems to support emergency preparedness and recovery, as well as resilience, through collaborations among local health departments, local school systems, and other public and private organizations (8). Topics addressed in this article include disparities in underlying medical conditions and social determinants of health, inequities in social determinants of health, and community-based approaches to reducing COVID-19 disparities. The article concludes by discussing ways to implement strategies to advance health equity through partnership.
It has long been recognized that disparities in health care access and patient outcomes are associated with factors related to race, sex, gender, sexual orientation, primary language, and socioeconomic status (27). Epps and coauthors recognize that African Americans and other underrepresented racial and ethnic groups are often not included in health decision making and policy development (9). As a result, these public health experts describe steps undertaken to improve participation, joint decision making, and capacity building between an integrated academic health system and a community coalition to address complex health challenges with the aim of increasing the capacity of health systems to reduce the burden of COVID-19. This article describes a call to action by the chair of a health care board of trustees to its board members consisting of clinicians, researchers, educators, and health advocates to identify ways to mitigate disparities and determine how the health care system could play a role in advancing and implementing effective strategies to reduce the disproportionate burden of COVID-19 among communities of color. Authors provide insight into the organizational planning process to generate a community outreach and health disparities collaborative with goals for governance, messaging and education, community partnerships, data, and research and evaluation.
COVID-19 has exacted a tremendous toll on the physical, emotional, and psychological well-being of many Americans, thus requiring a population health response (28). The disproportionate impact of the COVID-19 pandemic on Hispanic communities has resulted in a greater burden of depression, anxiety, and stress along with the need for increased assistance with housing, access to food, and supplemental income (29). Moon and colleagues offer original research that reports findings on demographic characteristics and factors associated with service volume, types of services, and referrals in the pre-COVID-19 and COVID-19 periods (10). They report that referrals shifted from primarily mental health services and disease management during the prepandemic period to affordable housing support, food assistance, and supplemental income during the COVID-19 period. This study presents findings on how a community-based organization with a long-standing presence in the Hispanic community effectively expanded its emotional wellness program, using promotores to provide integrated mental health care and social services to clients disproportionately affected by COVID-19.
Hacker et al discuss the problem of COVID-19 and chronic disease in their essay (11). They describe 3 categories of challenges facing public health professionals and identify solutions needed to improve health outcomes and lessen health inequities among people at risk or living with a chronic disease. Authors also discuss the evolving response by the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion to implement a multipronged approach to enhance access to data at the local level, focus on addressing social determinants of health through a health equity lens, and expand partnerships and communication about the impact of COVID-19 on chronic disease.
Unmet health-related social support needs among people being served by health care systems can contribute to high patient morbidity and poor population health (30,31). However, little is known about the overall impact of screening and referral programs that address unmet health-related social needs on outcomes related to experience of care, population health, and cost. Ruiz Escobar et al conducted a systematic review of peer-reviewed articles in PubMed published over the past 10 years (as of March 2020) to determine the impact of screening and referral care delivery services on unmet health-related social needs (12). Thirty-five articles met the systematic review’s inclusion criteria. After conducting their review, the authors concluded that although evidence exists of a positive influence of screening and referral program outcomes related to experience of care and population health, no definitive conclusions could be made on the overall impact on changes in patient connection to resources, patient satisfaction, and patient-reported outcomes because of the potential high risk of bias across studies. Their findings can inform the use of screening and referral programs in health care organizations, including ways to strengthen future studies to examine their effectiveness.
Qualitative research is an important methodological tool that provides critical insights in identifying subjective meaning in the context of health (32). Qualitative research is a necessary exploratory approach that can be used to better understand and improve health equity research and practice. Olson and her team of researchers conducted 10 listening sessions and 28 interviews with people from diverse backgrounds to identify themes in causes, solutions, and opportunities to collaborate across sectors to address cancer disparities (13). Researchers validated the use of qualitative approaches to engage diverse participants representing many different sectors. Qualitative findings identified medical mistrust, the need for equitable multilevel partnerships, influences of environmental threats on cancer burden, and location of cancer disparities as key concerns among people participating in the listening sessions and interviews. The researchers describe how these findings will be used to form multisector teams to address local social, cultural, and biological influences of cancer disparities and achieve health equity in Wisconsin.
Geographic location continues to be an important contributor in shaping access to timely and necessary screening and treatment options (33). Rohatgi et al conducted original research examining relationships among rurality, sociodemographic characteristics, and access to low-dose computed tomography (LDCT) screening for lung cancer and screening access and lung cancer mortality (14). This study revealed that more than 97% of metropolitan residents had access to LCDT screening, compared with just over 40% of nonmetropolitan residents. Researchers learned that residents of southeastern Missouri, a rural and impoverished area, had low screening access, high smoking prevalence, and high lung cancer mortality. Researchers concluded that targeted strategies to implement rural LDCT screening could reduce geographic disparities in access, and future research could help identify factors that increase access to screening to eliminate rural-related disparities in lung cancer mortality.
Breast cancer is the most frequently diagnosed cancer and a leading cause of cancer mortality among American Indian/Alaska Native (AI/AN) women (34). Despite having a lower incidence of breast cancer than White women, AI/AN women are more likely to be diagnosed at younger ages and later stages (35). Breast cancer incidence among non-AI/AN women has largely been quantified in large geographic regions in the US, and substantial regional variation in breast cancer inequities in non-Hispanic AI/AN populations has been reported. Zahrieh and colleagues conducted research to obtain a deeper understanding at a granular level to identify potential inequities in breast cancer incidence by applying county-level Bayesian disease mapping (a model-based approach that offers a means to improve county-level incidence estimates) to population surveillance data from 2005 through 2014 in New Mexico (30). They found a significant overall disparity effect across New Mexico, evidenced by the age-adjusted rate of breast cancer among non-Hispanic AI/AN women being appropriately 0.38 times the corresponding age-adjusted rate among non-Hispanic White women. Researchers also suggest that findings can be used to facilitate targeted statewide and county-level cancer control interventions to mitigate breast cancer disparities among AI/AN women in New Mexico.
Historically, type 2 diabetes has disproportionately affected racial and ethnic minority groups (31). To ensure accurate detection of type 2 diabetes, we must understand the ability of hemoglobin A 1c (HbA 1c ) to correctly classify type 2 diabetes status and evaluate intra-ethnic variation. Toward this end, Khosla et al conducted a scoping review to determine HbA 1c performance in African descent populations in the US with normal glucose tolerance, prediabetes, and diabetes (16). Results included 7 studies that analyzed HbA 1c performance among African Americans, 1 study that analyzed HbA 1c performance in Afro-Caribbean people, and 4 studies that analyzed HbA 1c performance among Africans. Researchers found that current HbA 1c cutoffs for prediabetes and type 2 diabetes may overestimate glycemic status in African Americans and underestimate glycemic status in Afro-Caribbean and African people. Researchers indicated that alternating testing, such as the oral glucose tolerance test, fasting plasma glucose, and other glycated blood proteins in place of or in combination with HbA 1c may better assess glycemic status in populations of African descent.
Tobacco use remains the leading cause of preventable morbidity and mortality in the US (33). Livingston and colleagues evaluated changes in tobacco cessation benefits, patient access, and cigarette smoking prevalence before and after 16 coordinated care organizations began providing comprehensive cessation benefits for reducing tobacco use prevalence among Medicaid members in Oregon (17). This implementation evaluation identified changes in tobacco cessation benefits, patient–provider discussions of smoking cessation, and cigarette smoking prevalence before and after the introduction of statewide incentives for reducing cigarette smoking. Evaluators reported that statewide effort accelerated progress toward tobacco use reduction among members of coordinated care organizations.
Obesity among adults living in Appalachia continues to be a major problem, and policy, systems, and environmental interventions may help to address long-standing underlying factors that have historically contributed to this persistent public health concern (35). Cardarelli and associates reported findings from a qualitative study that used a grounded theory approach to identify barriers and facilitators for healthy food access in a rural county in Kentucky (18). The goal was to design interventions responsive to social, cultural, and historical contexts from an equity perspective. Focus group participants were asked, for example, if it was easy to get fruits and vegetable at locations where they purchase food, if many people in their community purchase food at farmers markets, and what factors in their community make it easier or harder to eat healthy. The authors concluded that efforts to address food access through policy, systems, and environmental interventions must be sensitive to characteristics of the rural setting, acknowledge social inequities in the region, and proactively engage community members throughout all stages of intervention planning, implementation, and evaluation.
Oral health disparities among children have been linked to socioeconomic inequalities, access to care, health systems barriers, and lack of access to foods that promote optimal oral health outcomes (39). Martin et al conducted original research that explored the frequency of tooth brushing among children with a mean age 21.5 months (19). Their results indicated that the frequency of brushing among children, as reported by guardians, was higher when the correct amount of toothpaste was used, brushing occurred for a longer duration, and other family members helped children with brushing. Their findings strongly suggest that parental and family support for brushing are critically important in promoting and sustaining tooth-brushing behaviors.
According to the Lancet Global Health Commission on Global Eye Health, women, rural populations, and racial/ethnic minority groups are more likely to have vision impairment, a pervasive inequality that needs to be addressed (40). This PCD collection on advancing health equity and reducing health disparities concludes with a research study by Leiby et al investigating the effectiveness of an enhanced intervention among people with glaucoma: using patient navigators and social workers to improve patient adherence to follow-up eye care in community settings (20). The study compared the intervention group with a group of patients in usual care. Participants in usual care were provided with a local ophthalmologist’s contact information and a copy of their eye examination results; they were not provided access to patient navigators or social workers. Study participants, who were randomly assigned to either the enhanced or usual care intervention, were a diverse group of participants aged over 40 with a family history of glaucoma or currently diagnosed with diabetes. Only participants who had not seen an ophthalmologist in the previous 12 months were permitted to enroll in the study. Study participants consisted largely of African Americans, followed by White, Asian American, and Hispanic residents of Philadelphia, Pennsylvania. The study found that the use of patient navigators and social workers doubled the rate of adherence to annual recommended eye care follow-up, compared with participants assigned to the study’s usual care intervention. The study highlights that formalized use of social support in partnership with local ophthalmologists can be an effective approach to increasing access to local ophthalmological services.
At the center of this collection of articles is a shared commitment to the goal of eliminating health disparities, particularly those that continue to persist despite aggressive efforts to ameliorate them. The collection describes a range of diverse and timely examples of efforts to eliminate health disparities and advance health equity among racial and ethnic groups in the US. Articles appearing here represent various types of PCD articles that encompass multiple perspectives, from original research and systematic reviews to implementation evaluation to expert commentaries to tools that can be used in public health practice. As a discipline, we have important work to do, not only to better understand how social determinants of health and other contextual factors impact health but also to design, implement, and evaluate effective multilevel systems approaches that create optimal conditions to promote health for all. PCD will continue to move forward in its commitment to these goals, and we encourage authors to visit the journal’s Author’s Corner website (https://www.cdc.gov/pcd/for_authors/index.htm) to learn more about article types that best fit their research addressing population-based approaches to eliminating health disparities and advancing health equity.
Corresponding Author: Leonard Jack, Jr, PhD, MSc, Editor in Chief, Preventing Chronic Disease: Public Health Research, Practice, and Policy, Office of Medicine and Science, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, 4770 Buford Hwy, NE, Mailstop S107–8, Atlanta, GA 30341. Email: [email protected] .
Author Affiliations: 1 Office of Medicine and Science, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, Georgia.
- Jack L Jr. Using PCD’s first-ever external review to enhance the journal’s worldwide usefulness to researchers, practitioners, and policy makers. Prev Chronic Dis 2018;15:E41. CrossRef PubMed
- US Department of Health and Human Services. Section IV: Advisory Committee findings and recommendation. In: The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I report: recommendations for the framework and format of Healthy People 2020. http://www.healthypeople.gov/sites/default/files/phaseI_0.pdf. Accessed July 8, 2021.
- Jack L Jr. PCD’s commitment to advancing diversity, equity, and inclusion in its scientific leadership, peer review process, research focus, training, and continuing education. Prev Chronic Dis 2021;18:210269.
- Michener L, Aguilar-Gaxiola S, Alberti PM, Castaneda MJ, Castrucci BC, Harrison LM, et al. Engaging with communities — lessons (re)learned from COVID-19. Prev Chronic Dis 2020;17:E65. CrossRef PubMed
- Airhihenbuwa CO, Tseng TS, Sutton VD, Price L. Global perspectives on improving chronic disease prevention and management in diverse settings. Prev Chronic Dis 2021;18:E33. CrossRef PubMed
- Calo WA, Murray A, Francis E, Bermudez M, Kraschnewski J. Reaching the Hispanic community about COVID-19 through existing chronic disease prevention programs. Prev Chronic Dis 2020;17:E49. CrossRef PubMed
- Akintobi HT, Jacobs T, Sabbs D, Holden K, Braithwaite R, Johnson LN, et al. Community engagement of African Americans in the era of COVID-19: considerations, challenges, implications, and recommendations for public health. Prev Chronic Dis 2020;17:E83. CrossRef PubMed
- White A, Liburd LC, Coronado F. Addressing racial and ethnic disparities in COVID-19 among school-aged children: are we doing enough? Prev Chronic Dis 2021;18:E55. CrossRef PubMed
- Epps F, Wiley Z, Teunis LJ, Johnson TM 2d, Patzer RE, Ofotokun I, et al. A framework for mobilizing health care to respond to the community within the COVID-19 pandemic. Prev Chronic Dis 2021;18:E30. CrossRef PubMed
- Moon KJ, Montiel GI, Cantero PJ, Nawaz S. Addressing emotional wellness during the COVID-19 pandemic: the role of promotores in delivering integrated mental health care and social services. Prev Chronic Dis 2021;18:E53. CrossRef PubMed
- Hacker KA, Briss PA, Richardson L, Wright J, Petersen R. COVID-19 and chronic disease: the impact now and in the future. Prev Chronic Dis 2021;18:210086. CrossRef PubMed
- Ruiz Escobar R, Pathak H, Blanchard C. Screening and referral care delivery services and unmet health-related social needs: a systematic review. Prev Chronic Dis 2021;18:2000569.
- Olson J, Cawthra T, Beyer K, Frazer D, Ignace L, Maurana C, et al. Community and research perspectives on cancer disparities in Wisconsin. Prev Chronic Dis 2020;17:E122. CrossRef PubMed
- Rohatgi KW, Marx CM, Lewis-Thames MW, Liu J, Colditz GA, James AS. Urban–rural disparities in access to low-dose computed tomography lung cancer screening in Missouri and Illinois. Prev Chronic Dis 2020;17:E140. CrossRef PubMed
- Zahrieh D, Golafshar MA, Patel SH, DeWees TA. Quantification of potential inequities in breast cancer incidence in New Mexico through Bayesian disease mapping. Prev Chronic Dis 2021;18:E23. CrossRef PubMed
- Khosla L, Bhat S, Fullington LA, Horlyck-Romanovsky MF. HbA1c performance in African descent populations in the United States with normal glucose tolerance, prediabetes, or diabetes: a scoping review. Prev Chronic Dis 2021;18:E22. CrossRef PubMed
- Livingston CJ, Bartelmann SE, Goff NM, Aird KG. Reducing tobacco use in Oregon through multisector collaboration: aligning Medicaid and public health programs. Prev Chronic Dis 2020;17:E155. CrossRef PubMed
- Cardarelli K, DeWitt E, Gillespie R, Norman-Burgdolf H, Jones N, Mullins JT. “We’re, like, the most unhealthy people in the country”: using an equity lens to reduce barriers to healthy food access in rural Appalachia. Prev Chronic Dis 2020;17:E165. CrossRef PubMed
- Martin M, Pugach O, Avenetti D, Lee H, Salazar S, Rosales G, et al. Oral health behaviors in very young children in low-income urban areas in Chicago, Illinois, 2018–2019. Prev Chronic Dis 2020;17:E152. CrossRef PubMed
- Leiby BE, Hegarty SE, Zhan T, Myers JS, Katz LJ, Haller JA, et al. A randomized trial to improve adherence to follow-up eye examinations among people with glaucoma. Prev Chronic Dis 2021;18:E52. CrossRef PubMed
- Webb Hooper M, Mitchell C, Marshall VJ, Cheatham C, Austin K, Sanders K, et al. Understanding multilevel factors related to urban community trust in healthcare and research. Int J Environ Res Public Health 2019;16(18):3280. CrossRef PubMed
- Finset A, Bosworth H, Butow P, Gulbrandsen P, Hulsman RL, Pieterse AH, et al. Effective health communication — a key factor in fighting the COVID-19 pandemic. Patient Educ Couns 2020;103(5):873–6. CrossRef PubMed
- Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the US. J Clin Med 2020;9(8):2442. CrossRef PubMed
- Vahidy FS, Nicolas JC, Meeks JR, Khan O, Pan A, Jones SL, et al. Racial and ethnic disparities in SARS-CoV-2 pandemic: analysis of a COVID-19 observational registry for a diverse US metropolitan population. BMJ Open 2020;10(8):e039849. CrossRef PubMed
- Bassett MT, Chen JT, Krieger N. The unequal toll of COVID-19 mortality by age in the United States: quantifying racial/ethnic disparities. Working paper. Cambridge (MA): Harvard T.H. Chang School of Public Health; 2020.https://www.hsph.harvard.edu/social-and-behavioral-sciences/2020/06/23/the-unequal-toll-of-covid-19-mortality-by-age-in-the-united-states-quantifying-racial-ethnic-disparities/. Accessed July 13, 2021.
- Kim L, Whitaker M, O’Halloran A, Kambhampati A, Chai SJ, Reingold A, et al. ; COVID-NET Surveillance Team. Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory-confirmed COVID-19 — COVID-NET, 14 states, March 1–July 25, 2020. MMWR Morb Mortal Wkly Rep 2020;69(32):1081–8. CrossRef PubMed
- Okoro CA, Zhao G, Fox JB, Eke PI, Greenlund KJ, Town M. Surveillance for health care access and health services use, adults aged 18–64 years — Behavioral Risk Factor Surveillance System, United States, 2014. MMWR Surveill Summ 2017;66(7):1–42. CrossRef PubMed
- Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun 2020;89:531–42. CrossRef PubMed
- Waitzkin H, Getrich C, Heying S, Rodríguez L, Parmar A, Willging C, et al. Promotoras as mental health practitioners in primary care: a multi-method study of an intervention to address contextual sources of depression. J Community Health 2011;36(2):316–31. CrossRef PubMed
- Tough H, Siegrist J, Fekete C. Social relationships, mental health and wellbeing in physical disability: a systematic review. BMC Public Health 2017;17(1):1414. Erratum in BMC Public Health 2017;17(1)580. CrossRef PubMed
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med 2010;7(7):e1000316. CrossRef PubMed
- Mykhalovskiy E, Eakin J, Beagan B, Beausoleil N, Gibson BE, Macdonald ME, et al. Beyond bare bones: critical, theoretically engaged qualitative research in public health. Can J Public Health 2018;109(5-6):613–21. CrossRef PubMed
- Tsui J, Hirsch JA, Bayer FJ, Quinn JW, Cahill J, Siscovick D, et al. Patterns in geographic access to health care facilities across neighborhoods in the United States based on data from the National Establishment Time-Series between 2000 and 2014. JAMA Netw Open 2020;3(5):e205105. CrossRef PubMed
- White MC, Espey DK, Swan J, Wiggins CL, Eheman C, Kaur JS. Disparities in cancer mortality and incidence among American Indians and Alaska Natives in the United States. Am J Public Health 2014;104(Suppl 3):S377–87. CrossRef PubMed
- Melkonian SC, Jim MA, Haverkamp D, Wiggins CL, McCollum J, White MC, et al. Disparities in cancer incidence and trends among American Indians and Alaska Natives in the United States, 2010–2015. Cancer Epidemiol Biomarkers Prev 2019;28(10):1604–11. CrossRef PubMed
- Lin J, Thompson TJ, Cheng YJ, Zhuo X, Zhang P, Gregg E, et al. Projection of the future diabetes burden in the United States through 2060. Popul Health Metr 2018;16(1):9. CrossRef PubMed
- Creamer MR, Wang TW, Babb S, Cullen KA, Day H, Willis G, et al. Tobacco product use and cessation indicators among adults — United States, 2018. MMWR Morb Mortal Wkly Rep 2019;68(45):1013–9. CrossRef PubMed
- Smith LH, Laurent D, Baumker E, Petosa RL. Rates of obesity and obesogenic behaviors of rural Appalachian adolescents: how do they compare to other adolescents or recommendations? J Phys Act Health 2018;15(11):874–81. CrossRef PubMed
- Shen A, Bernabé E, Sabbah W. Systematic review of intervention studies aiming at reducing inequality in dental caries among children. Int J Environ Res Public Health 2021;18(3):1300. CrossRef PubMed
- Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health 2021;9(4):e489–551. CrossRef PubMed
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Fact sheets
- Facts in pictures
Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment case
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Science Division /
- Research for health
Research for Health
WHO’s goal: Forward looking and prioritized global health research
Research for health is a global endeavour, and WHO has a unique role to play in ensuring that these efforts can help improve health for all.
WHO provides leadership, calling on the wider scientific community to engage behind global health concerns. This is based on a deep understanding of the needs of countries, and rigorous assessment by international experts.
WHO has three key objectives to promote forward-looking and prioritized global health research:

Anticipating scientific, technological, and epidemiological shifts
To stay on top of scientific and technological advancements and epidemiological trends, WHO must anticipate new trends, technologies, research, and discoveries in medical and public health.
Through continuous, rigorous, and systematic horizon scanning, the Science Division assesses and identifies emerging issues, for early identification of potential health benefits or threats. It actively prospects for scientific and technological innovations that could change the equation on advancing health.
Science in action: the WHO Advisory Committee on Developing Global Standards for Governance and Oversight of Human Genome Editing
This committee examines the scientific, ethical, social, and legal challenges associated with human genome editing, and makes recommendations on the ethical framework for research and application of this technology.

Setting a global research agenda to address gaps, emerging areas, and country priorities
Truly useful innovations are not simply new; they are designed explicitly with the needs of the user in mind. By analyzing gaps, inequities, emerging areas and country priorities, the WHO research agenda anticipates the complex issues affecting people’s health and supports the discovery of innovative solutions to address them.
Science in action: R&D Blueprint for dementia research.
In 2017, the World Health Assembly adopted a Global Action Plan on the Public Health Response to Dementia. A key component of this plan was a call to action for research and innovation. To move this forward, the Science Division is developing an R&D Blueprint for dementia research.

Strengthening confidence in science
The Science Division supports countries in developing their scientific expertise and research capacities and facilitating the development of new and innovative research methodologies. This will improve understanding of the determinants of health, health systems, and the transformative potential of innovations in health.
Science in action: WHO Science Council
At WHO, Research for Health covers five key functions , which are integrated to apply research and innovation and achieve impact for people’s health around the world.

Foresight and emerging technologies
We try to get ahead of the curve by understanding what is needed to improve health for all in the future, and where the best new ideas are emerging.
Advances in science and technology hold great promise for new ways to address global health and support healthier populations worldwide. WHO engages in horizon scanning across the science and technology landscape. It also supports countries in doing their own futures and foresight exercises to understand their future needs. The aim of foresight is to identify and connect known, new, or emerging issues that could significantly impact global health within the next two decades.
Emerging technologies offer great health opportunities but also pose potentially significant challenges. The WHO Foresight function provides ongoing monitoring of emerging technologies to spot potential risks and come up with strategies for prevention and mitigation.

Research prioritization and support, R&D optimization
We identify gaps in current research priorities, and promote and support research that can best address unmet needs.
WHO has a unique role in supporting research for health , because we can help ensure health research is directed towards the biggest unmet needs in global health. We do this by sharing upstream research information from clinical trials , and research and development pipelines , and by providing guidance for research priority setting exercises.
WHO can determine strategic public health areas and identify key research and development needs. It then produces a clear target product profile to promote research and development that will be of most benefit. By mapping existing target product profiles in the Target Product Profile Directory and developing new ones based on identified public health needs, WHO steers innovation in support of improved health for all.
Product developers seek advice from WHO on whether or not their product likely has value for public health. In this way, WHO, expedites development of health related products, including novel therapeutics, diagnostics, and repurposing existing products.
Research for Health works with researchers and innovators to ensure they are aligned with the Prequalification Team and WHO’s technical departments on the package of evidence that will be needed to secure prequalification or a WHO policy recommendation. This process informs clinical trials on life-saving medical products, technologies and processes. A coordinated scientific advice process is currently in pilot phase.
Health ethics and governance
By putting ethics at the heart of decision-making and providing guidance on governance, WHO promotes this ethos within WHO and throughout the global health community.
In addition to supporting projects conducted by WHO, we are often called upon by development partners at country level for our expertise in global health ethics. Our Health Ethics and Governance unit produces guidance and tools for Member States on ethics in research and public health. Inside and outside WHO, it also helps researchers and public health specialists navigate ethical challenges posed by their projects.

Research policy for access
The best ideas are not just the brightest, but the one that actually get implemented and make an impact. WHO provides leadership on policies in research to ensure access and scale-up.
Having the right research policy is a key step towards ensuring health research has actual impact. This means that research priorities match real-world problems. At WHO, Research for Health works to ensure that the needs of countries are clearly articulated, and then communicated to the research community.
At WHO we promote an end-to-end approach in research policy. Working with local health systems and communities is needed to better understand the delivery and uptake of new products and to achieve widespread and equitable access. WHO can help broker multinational studies, foster regulatory harmonization, and promote dialogue among all stakeholders.

Taking knowledge from evidence to impact
Through a global network for evidence-informed health policy-making and tailored country support, WHO brings together researchers, policy-makers and implementers to translate evidence into improved health policies and programmes.
Public health problems are often complex and require nuanced, context-specific solutions and tailored implementation strategies. To make a difference for patients, communities and medical professionals, reliable evidence on how to tackle a health issue needs to be synthesized, reflected in a local context, and effectively communicated between researchers and decision-makers.
Through a set of field-tested and user-friendly tools, the Evidence to Policy and Impact Unit supports countries in bridging the gap between public health research, policy, and programme. Evidence briefs for policy and rapid response mechanisms put key research findings into context and place them at the fingertips of decision-makers. Policy dialogues provide researchers, policy-makers, and partner organizations with a forum to rally behind evidence-informed policy options and effective health interventions, discuss the findings, and share their own experiences and values. Citizen engagement strategies give voice to the beliefs and perspectives of individuals and communities, upholding accountability and democratic deliberation as core principles of equitable health care.
WHO’s global Evidence-informed Policy Network (EVIPNet) is a key initiative building sustainable and resilient capacity for evidence-informed decision-making and knowledge translation with Member States and in WHO offices at country, regional and international level. With over 15 years of experience and active teams in close to 50 countries, EVIPNet has successfully strengthened national health systems and emergency response capacity around the globe. The network also forms a vivid community of practice, facilitating decentralized peer-support among members and offering a treasure trove of successful strategies in evidence-informed health policy-making.

Research for Health within WHO
WHO’s Research for Health Department supports teams and units across the entire organization to establish their own research priorities . It helps people working in different parts of our global network connect the dots and create a better coordinated research response. This in turns helps keep WHO on track, ensuring that the research done within WHO is aligned with the health-related Sustainable Development Goals (SDGs) and our own Triple Billion Targets of 1 billion more people benefitting from universal health coverage, 1 billion more people better protected from health emergencies, and 1 billion more people enjoying better health and well-being.
Research for Health: our role in the global public health research community
WHO’s technical units are just one part of a global web of research for health, encompassing academia, national and regional research bodies, product development partnerships and the private sector. WHO helps to provide global guidance for research priority setting. Our global, regional and country-level reach means we can help to clearly articulate the needs of the countries, and we are uniquely well-placed to broker multinational research efforts.
WHO advisory group convenes its first meeting on responsible use of the life sciences in Geneva
Stakeholders convene in Uganda on responsible use of the life sciences
Global Research Agenda on Knowledge Translation and Evidence-informed Policy-making
Public consultation
CLOSED - Call for Experts – Technical Advisory Group on the responsible use of the life sciences and dual-use research
Public consultation on WHO guidance for best practices for clinical trials

Protocol: using data to drive governance
This document introduces a collaboratively developed study protocol to identify what data and information is currently being collected by governments and...

Evidence generation for development of health products: a practical guide for WHO staff
This document describes the main elements that World Health Organization (WHO) technical departments should elaborate on when providing guidance on evidence...

Report of the fifth meeting of the WHO Diagnostic Technical Advisory Group for Neglected Tropical Diseases:...
The WHO Department of Control of Neglected Tropical Diseases (WHO/NTD) manages a diverse portfolio of 20 diseases and disease groups, each with its own...

Performing a landscape analysis: understanding health product research and development
A landscape analysis related to health products aims to identify and characterize all the products that exist or are being developed in a specific topic...
- Open access
- Published: 20 September 2022
Factors that influence mental health of university and college students in the UK: a systematic review
- Fiona Campbell 1 ,
- Lindsay Blank 1 ,
- Anna Cantrell 1 ,
- Susan Baxter 1 ,
- Christopher Blackmore 1 ,
- Jan Dixon 1 &
- Elizabeth Goyder 1
BMC Public Health volume 22 , Article number: 1778 ( 2022 ) Cite this article
110k Accesses
56 Citations
92 Altmetric
Metrics details
Worsening mental health of students in higher education is a public policy concern and the impact of measures to reduce transmission of COVID-19 has heightened awareness of this issue. Preventing poor mental health and supporting positive mental wellbeing needs to be based on an evidence informed understanding what factors influence the mental health of students.
To identify factors associated with mental health of students in higher education.
We undertook a systematic review of observational studies that measured factors associated with student mental wellbeing and poor mental health. Extensive searches were undertaken across five databases. We included studies undertaken in the UK and published within the last decade (2010–2020). Due to heterogeneity of factors, and diversity of outcomes used to measure wellbeing and poor mental health the findings were analysed and described narratively.
We included 31 studies, most of which were cross sectional in design. Those factors most strongly and consistently associated with increased risk of developing poor mental health included students with experiences of trauma in childhood, those that identify as LGBTQ and students with autism. Factors that promote wellbeing include developing strong and supportive social networks. Students who are prepared and able to adjust to the changes that moving into higher education presents also experience better mental health. Some behaviours that are associated with poor mental health include lack of engagement both with learning and leisure activities and poor mental health literacy.
Improved knowledge of factors associated with poor mental health and also those that increase mental wellbeing can provide a foundation for designing strategies and specific interventions that can prevent poor mental health and ensuring targeted support is available for students at increased risk.
Peer Review reports
Poor mental health of students in further and higher education is an increasing concern for public health and policy [ 1 , 2 , 3 , 4 ]. A 2020 Insight Network survey of students from 10 universities suggests that “1 in 5 students has a current mental health diagnosis” and that “almost half have experienced a serious psychological issue for which they felt they needed professional help”—an increase from 1 in 3 in the same survey conducted in 2018 [ 5 ]. A review of 105 Further Education (FE) colleges in England found that over a three-year period, 85% of colleges reported an increase in mental health difficulties [ 1 ]. Depression and anxiety were both prevalent and widespread in students; all colleges reported students experiencing depression and 99% reported students experiencing severe anxiety [ 5 , 6 ]. A UK cohort study found that levels of psychological distress increase on entering university [ 7 ], and recent evidence suggests that the prevalence of mental health problems among university students, including self-harm and suicide, is rising, [ 3 , 4 ] with increases in demand for services to support student mental health and reports of some universities finding a doubling of the number of students accessing support [ 8 ]. These common mental health difficulties clearly present considerable threat to the mental health and wellbeing of students but their impact also has educational, social and economic consequences such as academic underperformance and increased risk of dropping out of university [ 9 , 10 ].
Policy changes may have had an influence on the student experience, and on the levels of mental health problems seen in the student population; the biggest change has arguably been the move to widen higher education participation and to enable a more diverse demographic to access University education. The trend for widening participation has been continually rising since the late 1960s [ 11 ] but gained impetus in the 2000s through the work of the Higher Education Funding Council for England (HEFCE). Macaskill (2013) [ 12 ] suggests that the increased access to higher education will have resulted in more students attending university from minority groups and less affluent backgrounds, meaning that more students may be vulnerable to mental health problems, and these students may also experience greater challenges in making the transition to higher education.
Another significant change has been the introduction of tuition fees in 1998, which required students to self fund up to £1,000 per academic year. Since then, tuition fees have increased significantly for many students. With the abolition of maintenance grants, around 96% of government support for students now comes in the form of student loans [ 13 ]. It is estimated that in 2017, UK students were graduating with average debts of £50,000, and this figure was even higher for the poorest students [ 13 ]. There is a clear association between a student’s mental health and financial well-being [ 14 ], with “increased financial concern being consistently associated with worse health” [ 15 ].
The extent to which the increase in poor mental health is also being seen amongst non-students of a similar age is not well understood and warrants further study. However, the increase in poor mental health specifically within students in higher education highlights a need to understand what the risk factors are and what might be done within these settings to ensure young people are learning and developing and transitioning into adulthood in environments that promote mental wellbeing.
Commencing higher education represents a key transition point in a young person’s life. It is a stage often accompanied by significant change combined with high expectations of high expectations from students of what university life will be like, and also high expectations from themselves and others around their own academic performance. Relevant factors include moving away from home, learning to live independently, developing new social networks, adjusting to new ways of learning, and now also dealing with the additional greater financial burdens that students now face.
The recent global COVID-19 pandemic has had considerable impact on mental health across society, and there is concern that younger people (ages 18–25) have been particularly affected. Data from Canada [ 16 ] indicate that among survey respondents, “almost two-thirds (64%) of those aged 15 to 24 reported a negative impact on their mental health, while just over one-third (35%) of those aged 65 and older reported a negative impact on their mental health since physical distancing began” (ibid, p.4). This suggests that older adults are more prepared for the kind of social isolation which has been brought about through the response to COVID-19, whereas young adults have found this more difficult to cope with. UK data from the National Union of Students reports that for over half of UK students, their mental health is worse than before the pandemic [ 17 ]. Before COVID-19, students were already reporting increasing levels of mental health problems [ 2 ], but the COVID-19 pandemic has added a layer of “chronic and unpredictable” stress, creating the perfect conditions for a mental health crisis [ 18 ]. An example of this is the referrals (both urgent and routine) of young people with eating disorders for treatment in the NHS which almost doubled in number from 2019 to 2020 [ 19 ]. The travel restrictions enforced during the pandemic have also impacted on student mental health, particularly for international students who may have been unable to commence studies or go home to see friends and family during holidays [ 20 ].
With the increasing awareness and concern in the higher education sector and national bodies regarding student mental health has come increasing focus on how to respond. Various guidelines and best practice have been developed, e.g. ‘Degrees of Disturbance’ [ 21 ], ‘Good Practice Guide on Responding to Student Mental Health Issues: Duty of Care Responsibilities for Student Services in Higher Education’ [ 22 ] and the recent ‘The University Mental Health Charter’ [ 2 ]. Universities UK produced a Good Practice Guide in 2015 called “Student mental wellbeing in higher education” [ 23 ]. An increasing number of initiatives have emerged that are either student-led or jointly developed with students, and which reflect the increasing emphasis students and student bodies place on mental health and well-being and the increased demand for mental health support: Examples include: Nightline— www.nightline.ac.uk , Students Against Depression— www.studentsagainstdepression.org , Student Minds— www.studentminds.org.uk/student-minds-and-mental-wealth.html and The Alliance for Student-Led Wellbeing— www.alliancestudentwellbeing.weebly.com/ .
Although requests for professional support have increased substantially [ 24 ] only a third of students with mental health problems seek support from counselling services in the UK [ 12 ]. Many students encounter barriers to seeking help such as stigma or lack of awareness of services [ 25 ], and without formal support or intervention, there is a risk of deterioration. FE colleges and universities have identified the need to move beyond traditional forms of support and provide alternative, more accessible interventions aimed at improving mental health and well-being. Higher education institutions have a unique opportunity to identify, prevent, and treat mental health problems because they provide support in multiple aspects of students’ lives including academic studies, recreational activities, pastoral and counselling services, and residential accommodation.
In order to develop services that better meet the needs of students and design environments that are supportive of developing mental wellbeing it is necessary to explore and better understand the factors that lead to poor mental health in students.
Research objectives
The overall aim of this review was to identify, appraise and synthesise existing research evidence that explores the aetiology of poor mental health and mental wellbeing amongst students in tertiary level education. We aimed to gain a better understanding of the mechanisms that lead to poor mental health amongst tertiary level students and, in so doing, make evidence-based recommendations for policy, practice and future research priorities. Specific objectives in line with the project brief were to:
To co-produce with stakeholders a conceptual framework for exploring the factors associated with poorer mental health in students in tertiary settings. The factors may be both predictive, identifying students at risk, or causal, explaining why they are at risk. They may also be protective, promoting mental wellbeing.
To conduct a review drawing on qualitative studies, observational studies and surveys to explore the aetiology of poor mental health in students in university and college settings and identify factors which promote mental wellbeing amongst students.
To identify evidence-based recommendations for policy, service provision and future research that focus on prevention and early identification of poor mental health
Methodology
Identification of relevant evidence.
The following inclusion criteria were used to guide the development of the search strategy and the selection of studies.
We included students from a variety of further education settings (16 yrs + or 18 yrs + , including mature students, international students, distance learning students, students at specific transition points).
Universities and colleges in the UK. We were also interested in the context prior to the beginning of tertiary education, including factors during transition from home and secondary education or existing employment to tertiary education.
Any factor shown to be associated with mental health of students in tertiary level education. This included clinical indicators such as diagnosis and treatment and/or referral for depression and anxiety. Self-reported measures of wellbeing, happiness, stress, anxiety and depression were included. We did not include measures of academic achievement or engagement with learning as indicators of mental wellbeing.
Study design
We included cross-sectional and longitudinal studies that looked at factors associated with mental health outcomes in Table 5 .
Data extraction and quality appraisal
We extracted and tabulated key data from the included papers. Data extraction was undertaken by one reviewer, with a 10% sample checked for accuracy and consistency The quality of the included studies were evaluated using the Newcastle-Ottawa Scale [ 26 ] and the findings of the quality appraisal used in weighting the strength of associations and also identifying gaps for future high quality research.
Involvement of stakeholders
We recruited students, ex-students and parents of students to a public involvement group which met on-line three times during the process of the review and following the completion of the review. During a workshop meeting we asked for members of the group to draw on their personal experiences to suggest factors which were not mentioned in the literature.
Methods of synthesis
We undertook a narrative synthesis [ 27 ] due to the heterogeneity in the exposures and outcomes that were measured across the studies. Data showing the direction of effects and the strength of the association (correlation coefficients) were recorded and tabulated to aid comparison between studies.
Search strategy
Searches were conducted in the following electronic databases: Medline, Applied Social Sciences Index and Abstracts (ASSIA), International Bibliography of Social Sciences (IBSS), Science,PsycINFO and Science and Social Sciences Ciatation Indexes. Additional searches of grey literature, and reference lists of included studies were also undertaken.
The search strategy combined a number of terms relating to students and mental health and risk factors. The search terms included both subject (MeSH) and free-text searches. The searches were limited to papers about humans in English, published from 2010 to June 2020. The flow of studies through the review process is summarised in Fig. 1 .
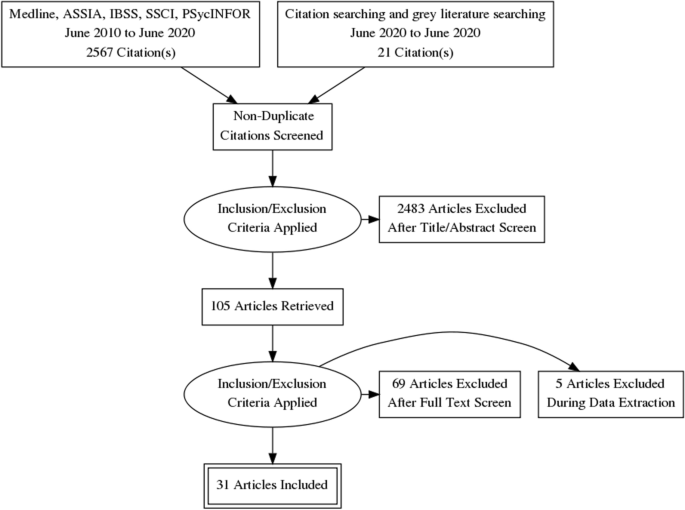
Flow diagram
The full search strategy for Medline is provided in Appendix 1 .
Thirty-one quantitative, observational studies (39 papers) met the inclusion criteria. The total number of students that participated in the quantitative studies was 17,476, with studies ranging in size from 57 to 3706. Eighteen studies recruited student participants from only one university; five studies (10 publications) [ 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ] included seven or more universities. Six studies (7 publications) [ 35 , 36 , 37 , 38 , 39 , 40 , 41 ] only recruited first year students, while the majority of studies recruited students from a range of year groups. Five studies [ 39 , 42 , 43 , 44 , 45 ] recruited only, or mainly, psychology students which may impact on the generalisability of findings. A number of studies focused on students studying particular subjects including: nursing [ 46 ] medicine [ 47 ], business [ 48 ], sports science [ 49 ]. One study [ 50 ] recruited LGBTQ (lesbian, gay, bisexual, transgender, intersex, queer/questioning) students, and one [ 51 ] recruited students who had attended hospital having self-harmed. In 27 of the studies, there were more female than male participants. The mean age of the participants ranged from 19 to 28 years. Ethnicity was not reported in 19 of the studies. Where ethnicity was reported, the proportion that were ‘white British’ ranged from 71 – 90%. See Table 1 for a summary of the characteristics of the included studies and the participants.
Design and quality appraisal of the included studies
The majority of included studies ( n = 22) were cross-sectional surveys. Nine studies (10 publications) [ 35 , 36 , 39 , 41 , 43 , 50 , 51 , 52 , 53 , 62 ] were longitudinal in design, recording survey data at different time points to explore changes in the variables being measured. The duration of time that these studies covered ranged from 19 weeks to 12 years. Most of the studies ( n = 22) only recruited participants from a single university. The use of one university setting and the large number of studies that recruited only psychology students weakens the wider applicability of the included studies.
Quantitative variables
Included studies ( n = 31) measured a wide range of variables and explored their association with poor mental health and wellbeing. These included individual level factors: age, gender, sexual orientation, ethnicity and a range of psychological variables. They also included factors that related to mental health variables (family history, personal history and mental health literacy), pre-university factors (childhood trauma and parenting behaviour. University level factors including social isolation, adjustment and engagement with learning. Their association was measured against different measures of positive mental health and poor mental health.
Measurement of association and the strength of that association has some limitations in addressing our research question. It cannot prove causality, and nor can it capture fully the complexity of the inter-relationship and compounding aspect of the variables. For example, the stress of adjustment may be manageable, until it is combined with feeling isolated and out of place. Measurement itself may also be misleading, only capturing what is measureable, and may miss variables that are important but not known. We included both qualitative and PPI input to identify missed but important variables.
The wide range of variables and different outcomes, with few studies measuring the same variable and outcomes, prevented meta-analyses of findings which are therefore described narratively.
The variables described were categorised during the analyses into the following categories:
Vulnerabilities – factors that are associated with poor mental health
Individual level factors including; age, ethnicity, gender and a range of psychological variables were all measured against different mental health outcomes including depression, anxiety, paranoia, and suicidal behaviour, self-harm, coping and emotional intelligence.
Six studies [ 40 , 42 , 47 , 50 , 60 , 63 ] examined a student’s ages and association with mental health. There was inconsistency in the study findings, with studies finding that age (21 or older) was associated with fewer depressive symptoms, lower likelihood of suicide ideation and attempt, self-harm, and positively associated with better coping skills and mental wellbeing. This finding was not however consistent across studies and the association was weak. Theoretical models that seek to explain this mechanism have suggested that older age groups may cope better due to emotion-regulation strategies improving with age [ 67 ]. However, those over 30 experienced greater financial stress than those aged 17-19 in another study [ 63 ].
Sexual orientation
Four studies [ 33 , 40 , 64 , 68 ] examined the association between poor mental health and sexual orientation status. In all of the studies LGBTQ students were at significantly greater risk of mental health problems including depression [ 40 ], anxiety [ 40 ], suicidal behaviour [ 33 , 40 , 64 ], self harm [ 33 , 40 , 64 ], use of mental health services [ 33 ] and low levels of wellbeing [ 68 ]. The risk of mental health problems in these students compared with heterosexual students, ranged from OR 1.4 to 4.5. This elevated risk may reflect the greater levels of isolation and discrimination commonly experienced by minority groups.
Nine studies [ 33 , 38 , 39 , 40 , 42 , 47 , 50 , 60 , 63 ] examined whether gender was associated mental health variables. Two studies [ 33 , 47 ] found that being female was statistically significantly associated with use of mental health services, having a current mental health problem, suicide risk, self harm [ 33 ] and depression [ 47 ]. The results were not consistent, with another study [ 60 ] finding the association was not significant. Three studies [ 39 , 40 , 42 ] that considered mediating variables such as adaptability and coping found no difference or very weak associations.
Two studies [ 47 , 60 ] examined the extent to which ethnicity was associated with mental health One study [ 47 ] reported that the risks of depression were significantly greater for those who categorised themselves as non-white (OR 8.36 p = 0.004). Non-white ethnicity was also associated with poorer mental health in another cross-sectional study [ 63 ]. There was no significant difference in the McIntyre et al. (2018) study [ 60 ]. The small number of participants from ethnic minority groups represented across the studies means that this data is very limited.
Family factors
Six studies [ 33 , 40 , 42 , 50 , 60 ] explored the association of a concept that related to a student’s experiences in childhood and before going to university. Three studies [ 40 , 50 , 60 ] explored the impact of ACEs (Adverse Childhood Experiences) assessed using the same scale by Feletti (2009) [ 69 ] and another explored the impact of abuse in childhood [ 46 ]. Two studies examined the impact of attachment anxiety and avoidance [ 42 ], and parental acceptance [ 46 , 59 ]. The studies measured different mental health outcomes including; positive and negative affect, coping, suicide risk, suicide attempt, current mental health problem, use of mental health services, psychological adjustment, depression and anxiety.
The three studies that explored the impact of ACE’s all found a significant and positive relationship with poor mental health amongst university students. O’Neill et al. (2018) [ 50 ] in a longitudinal study ( n = 739) showed that there was in increased likelihood in self-harm and suicidal behaviours in those with either moderate or high levels of childhood adversities (OR:5.5 to 8.6) [ 50 ]. McIntyre et al. (2018) [ 60 ] ( n = 1135) also explored other dimensions of adversity including childhood trauma through multiple regression analysis with other predictive variables. They found that childhood trauma was significantly positively correlated with anxiety, depression and paranoia (ß = 0.18, 0.09, 0.18) though the association was not as strong as the correlation seen for loneliness (ß = 0.40) [ 60 ]. McLafferty et al. (2019) [ 40 ] explored the compounding impact of childhood adversity and negative parenting practices (over-control, overprotection and overindulgence) on poor mental health (depression OR 1.8, anxiety OR 2.1 suicidal behaviour OR 2.3, self-harm OR 2.0).
Gaan et al.’s (2019) survey of LGBTQ students ( n = 1567) found in a multivariate analyses that sexual abuse, other abuse from violence from someone close, and being female had the highest odds ratios for poor mental health and were significantly associated with all poor mental health outcomes [ 33 ].
While childhood trauma and past abuse poses a risk to mental health for all young people it may place additional stresses for students at university. Entry to university represents life stage where there is potential exposure to new and additional stressors, and the possibility that these students may become more isolated and find it more difficult to develop a sense of belonging. Students may be separated for the first time from protective friendships. However, the mechanisms that link childhood adversities and negative psychopathology, self-harm and suicidal behaviour are not clear [ 40 ]. McLafferty et al. (2019) also measured the ability to cope and these are not always impacted by childhood adversities [ 40 ]. They suggest that some children learn to cope and build resilience that may be beneficial.
McLafferty et al. (2019) [ 40 ] also studied parenting practices. Parental over-control and over-indulgence was also related to significantly poorer coping (OR -0.075 p < 0.05) and this was related to developing poorer coping scores (OR -0.21 p < 0.001) [ 40 ]. These parenting factors only became risk factors when stress levels were high for students at university. It should be noted that these studies used self-report, and responses regarding views of parenting may be subjective and open to interpretation. Lloyd et al.’s (2014) survey found significant positive correlations between perceived parental acceptance and students’ psychological adjustment, with paternal acceptance being the stronger predictor of adjustment.
Autistic students may display social communication and interaction deficits that can have negative emotional impacts. This may be particularly true during young adulthood, a period of increased social demands and expectations. Two studies [ 56 ] found that those with autism had a low but statistically significant association with poor social problem-solving skills and depression.
Mental health history
Three studies [ 47 , 51 , 68 ] investigated mental health variables and their impact on mental health of students in higher education. These included; a family history of mental illness and a personal history of mental illness.
Students with a family history or a personal history of mental illness appear to have a significantly greater risk of developing problems with mental health at university [ 47 ]. Mahadevan et al. (2010) [ 51 ] found that university students who self-harm have a significantly greater risk (OR 5.33) of having an eating disorder than a comparison group of young adults who self-harm but are not students.
Buffers – factors that are protective of mental wellbeing
Psychological factors.
Twelve studies [ 29 , 39 , 40 , 41 , 42 , 43 , 46 , 49 , 54 , 58 , 64 ] assessed the association of a range of psychological variables and different aspects of mental wellbeing and poor mental health. We categorised these into the following two categories: firstly, psychological variables measuring an individual’s response to change and stressors including adaptability, resilience, grit and emotional regulation [ 39 , 40 , 41 , 42 , 43 , 46 , 49 , 54 , 58 ] and secondly, those that measure self-esteem and body image [ 29 , 64 ].
The evidence from the eight included quantitative studies suggests that students with psychological strengths including; optimism, self-efficacy [ 70 ], resilience, grit [ 58 ], use of positive reappraisal [ 49 ], helpful coping strategies [ 42 ] and emotional intelligence [ 41 , 46 ] are more likely to experience greater mental wellbeing (see Table 2 for a description of the psychological variables measured). The positive association between these psychological strengths and mental well-being had a positive affect with associations ranging from r = 0.2–0.5 and OR1.27 [ 41 , 43 , 46 , 49 , 54 ] (low to moderate strength of association). The negative associations with depressive symptoms are also statistically significant but with a weaker association ( r = -0.2—0.3) [ 43 , 49 , 54 ].
Denovan (2017a) [ 43 ] in a longitudinal study found that the association between psychological strengths and positive mental wellbeing was not static and that not all the strengths remained statistically significant over time. The only factors that remained significant during the transition period were self-efficacy and optimism, remaining statistically significant as they started university and 6 months later.
Parental factors
Only one study [ 59 ] explored family factors associated with the development of psychological strengths that would equip young people as they managed the challenges and stressors encountered during the transition to higher education. Lloyd et al. (2014) [ 59 ] found that perceived maternal and paternal acceptance made significant and unique contributions to students’ psychological adjustment. Their research methods are limited by their reliance on retrospective measures and self-report measures of variables, and these results could be influenced by recall bias.
Two studies [ 29 , 64 ] considered the impact of how individuals view themselves on poor mental health. One study considered the impact of self-esteem and the association with non-accidental self-injury (NSSI) and suicide attempt amongst 734 university students. As rates of suicide and NSSI are higher amongst LGBT (lesbian, gay, bisexual, transgender) students, the prevalence of low self-esteem was compared. There was a low but statistically significant association between low self-esteem and NSSI, though not for suicide attempt. A large survey, including participants from seven universities [ 42 ] compared depressive symptoms in students with marked body image concerns, reporting that the risk of depressive symptoms was greater (OR 2.93) than for those with lower levels of body image concerns.
Mental health literacy and help seeking behaviour
Two studies [ 48 , 68 ] investigated attitudes to mental illness, mental health literacy and help seeking for mental health problems.
University students who lack sufficient mental health literacy skills to be able to recognise problems or where there are attitudes that foster shame at admitting to having mental health problems can result in students not recognising problems and/or failing to seek professional help [ 48 , 68 ]. Gorcyznski et al. (2017) [ 68 ] found that women and those who had a history of previous mental health problems exhibited significantly higher levels of mental health literacy. Greater mental health literacy was associated with an increased likelihood that individuals would seek help for mental health problems. They found that many students find it hard to identify symptoms of mental health problems and that 42% of students are unaware of where to access available resources. Of those who expressed an intention to seek help for mental health problems, most expressed a preference for online resources, and seeking help from family and friends, rather than medical professionals such as GPs.
Kotera et al. (2019) [ 48 ] identified self-compassion as an explanatory variable, reducing social comparison, promoting self-acceptance and recognition that discomfort is an inevitable human experience. The study found a strong, significant correlation between self-compassion and mental health symptoms ( r = -0.6. p < 0.01).
There again appears to be a cycle of reinforcement, where poor mental health symptoms are felt to be a source of shame and become hidden, help is not sought, and further isolation ensues, leading to further deterioration in mental health. Factors that can interrupt the cycle are self-compassion, leading to more readiness to seek help (see Fig. 2 ).
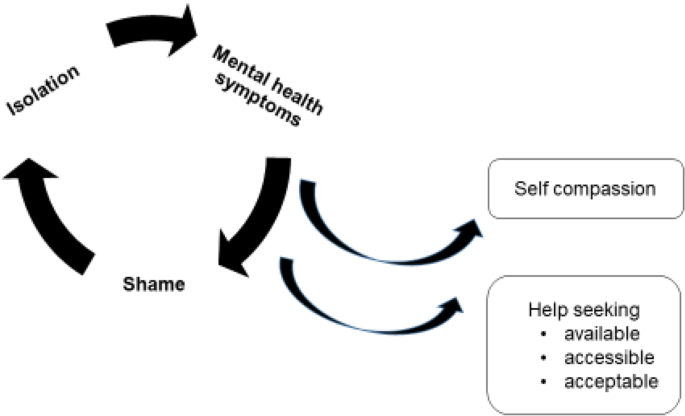
Poor mental health – cycles of reinforcement
Social networks
Nine studies [ 33 , 38 , 41 , 46 , 51 , 54 , 60 , 64 , 65 ] examined the concepts of loneliness and social support and its association with mental health in university students. One study also included students at other Higher Education Institutions [ 46 ]. Eight of the studies were surveys, and one was a retrospective case control study to examine the differences between university students and age-matched young people (non-university students) who attended hospital following deliberate self-harm [ 51 ].
Included studies demonstrated considerable variation in how they measured the concepts of social isolation, loneliness, social support and a sense of belonging. There were also differences in the types of outcomes measured to assess mental wellbeing and poor mental health. Grouping the studies within a broad category of ‘social factors’ therefore represents a limitation of this review given that different aspects of the phenomena may have been being measured. The tools used to measure these variables also differed. Only one scale (The UCLA loneliness scale) was used across multiple studies [ 41 , 60 , 65 ]. Diverse mental health outcomes were measured across the studies including positive affect, flourishing, self-harm, suicide risk, depression, anxiety and paranoia.
Three studies [ 41 , 60 , 62 ] measuring loneliness, two longitudinally [ 41 , 62 ], found a consistently positive association between loneliness and poor mental health in university students. Greater loneliness was linked to greater anxiety, stress, depression, poor general mental health, paranoia, alcohol abuse and eating disorder problems. The strength of the correlations ranged from 0–3-0.4 and were all statistically significant (see Tables 3 and 4 ). Loneliness was the strongest overall predictor of mental distress, of those measured. A strong identification with university friendship groups was most protective against distress relative to other social identities [ 60 ]. Whether poor mental health is the cause, or the result of loneliness was explored further in the studies. The results suggest that for general mental health, stress, depression and anxiety, loneliness induces or exacerbates symptoms of poor mental health over time [ 60 , 62 ]. The feedback cycle is evident, with loneliness leading to poor mental health which leads to withdrawal from social contacts and further exacerbation of loneliness.
Factors associated with protecting against loneliness by fostering supportive friendships and promoting mental wellbeing were also identified. Beliefs about the value of ‘leisure coping’, and attributes of resilience and emotional intelligence had a moderate, positive and significant association with developing mental wellbeing and were explored in three studies [ 46 , 54 , 66 ].
The transition to and first year at university represent critical times when friendships are developed. Thomas et al. (2020) [ 65 ] explored the factors that predict loneliness in the first year of university. A sense of community and higher levels of ‘social capital’ were significantly associated with lower levels of loneliness. ‘Social capital’ scales measure the development of emotionally supportive friendships and the ability to adjust to the disruption of old friendships as students transition to university. Students able to form close relationships within their first year at university are less likely to experience loneliness (r-0.09, r- 0.36, r- 0.34). One study [ 38 ] investigating the relationship between student experience and being the first in the family to attend university found that these students had lower ratings for peer group interactions.
Young adults at university and in higher education are facing multiple adjustments. Their ability to cope with these is influenced by many factors. Supportive friendships and a sense of belonging are factors that strengthen coping. Nightingale et al. (2012) undertook a longitudinal study to explore what factors were associated with university adjustment in a sample of first year students ( n = 331) [ 41 ]. They found that higher skills of emotion management and emotional self-efficacy were predictive of stable adjustment. These students also reported the lowest levels of loneliness and depression. This group had the skills to recognise their emotions and cope with stressors and were confident to access support. Students with poor emotion management and low levels of emotional self-efficacy may benefit from intervention to support the development of adaptive coping strategies and seeking support.
The positive and negative feedback loops
The relationship between the variables described appeared to work in positive and negative feedback loops with high levels of social capital easing the formation of a social network which acts as a critical buffer to stressors (see Fig. 3 ). Social networks and support give further strengthening and reinforcement, stimulating positive affect, engagement and flourishing. These, in turn, widen and deepen social networks for support and enhance a sense of wellbeing. Conversely young people who enter the transition to university/higher education with less social capital are less likely to identify with and locate a social network; isolation may follow, along with loneliness, anxiety, further withdrawal from contact with social networks and learning, and depression.
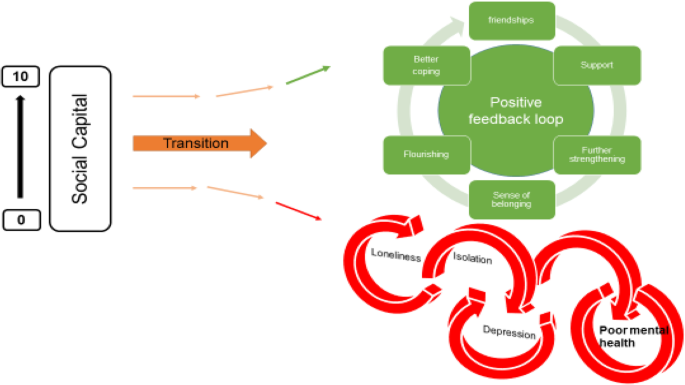
Triggers – factors that may act in combination with other factors to lead to poor mental health
Stress is seen as playing a key role in the development of poor mental health for students in higher education. Theoretical models and empirical studies have suggested that increases in stress are associated with decreases in student mental health [ 12 , 43 ]. Students at university experience the well-recognised stressors associated with academic study such as exams and course work. However, perhaps less well recognised are the processes of transition, requiring adapting to a new social and academic environment (Fisher 1994 cited by Denovan 2017a) [ 43 ]. Por et al. (2011) [ 46 ] in a small ( n = 130 prospective survey found a statistically significant correlation between higher levels of emotional intelligence and lower levels of perceived stress ( r = 0.40). Higher perceived stress was also associated with negative affect in two studies [ 43 , 46 ], and strongly negatively associated with positive affect (correlation -0.62) [ 54 ].
University variables
Eleven studies [ 35 , 39 , 47 , 51 , 52 , 54 , 60 , 63 , 65 , 83 , 84 ] explored university variables, and their association with mental health outcomes. The range of factors and their impact on mental health variables is limited, and there is little overlap. Knowledge gaps are shown by factors highlighted by our PPI group as potentially important but not identified in the literature (see Table 5 ). It should be noted that these may reflect the focus of our review, and our exclusion of intervention studies which may evaluate university factors.
High levels of perceived stress caused by exam and course work pressure was positively associated with poor mental health and lack of wellbeing [ 51 , 52 , 54 ]. Other potential stressors including financial anxieties and accommodation factors appeared to be less consistently associated with mental health outcomes [ 35 , 38 , 47 , 51 , 60 , 62 ]. Important mediators and buffers to these stressors are coping strategies and supportive networks (see conceptual model Appendix 2 ). One impact of financial pressures was that students who worked longer hours had less interaction with their peers, limiting the opportunities for these students to benefit from the protective effects of social support.
Red flags – behaviours associated with poor mental health and/or wellbeing
Engagement with learning and leisure activities.
Engagement with learning activities was strongly and positively associated with characteristics of adaptability [ 39 ] and also happiness and wellbeing [ 52 ] (see Fig. 4 ). Boulton et al. (2019) [ 52 ] undertook a longitudinal survey of undergraduate students at a campus-based university. They found that engagement and wellbeing varied during the term but were strongly correlated.
Engagement and wellbeing
Engagement occurred in a wide range of activities and behaviours. The authors suggest that the strong correlation between all forms of engagement with learning has possible instrumental value for the design of systems to monitor student engagement. Monitoring engagement might be used to identify changes in the behaviour of individuals to assist tutors in providing support and pastoral care. Students also were found to benefit from good induction activities provided by the university. Greater induction satisfaction was positively and strongly associated with a sense of community at university and with lower levels of loneliness [ 65 ].
The inte r- related nature of these variables is depicted in Fig. 4 . Greater adaptability is strongly associated with more positive engagement in learning and university life. More engagement is associated with higher mental wellbeing.
Denovan et al. (2017b) [ 54 ] explored leisure coping, its psychosocial functions and its relationship with mental wellbeing. An individual’s beliefs about the benefits of leisure activities to manage stress, facilitate the development of companionship and enhance mood were positively associated with flourishing and were negatively associated with perceived stress. Resilience was also measured. Resilience was strongly and positively associated with leisure coping beliefs and with indicators of mental wellbeing. The authors conclude that resilient individuals are more likely to use constructive means of coping (such as leisure coping) to proactively cultivate positive emotions which counteract the experience of stress and promote wellbeing. Leisure coping is predictive of positive affect which provides a strategy to reduce stress and sustain coping. The belief that friendships acquired through leisure provide social support is an example of leisure coping belief. Strong emotionally attached friendships that develop through participation in shared leisure pursuits are predictive of higher levels of well-being. Friendship bonds formed with fellow students at university are particularly important for maintaining mental health, and opportunities need to be developed and supported to ensure that meaningful social connections are made.
The ‘broaden-and-build theory’ (Fredickson 2004 [ 85 ] cited by [ 54 ]) may offer an explanation for the association seen between resilience, leisure coping and psychological wellbeing. The theory is based upon the role that positive and negative emotions have in shaping human adaptation. Positive emotions broaden thinking, enabling the individual to consider a range of ways of dealing with and adapting to their environment. Conversely, negative emotions narrow thinking and limit options for adapting. The former facilitates flourishing, facilitating future wellbeing. Resilient individuals are more likely to use constructive means of coping which generate positive emotion (Tugade & Fredrickson 2004 [ 86 ], cited by [ 54 ]). Positive emotions therefore lead to growth in coping resources, leading to greater well-being.
Health behaviours at university
Seven studies [ 29 , 31 , 38 , 45 , 51 , 54 , 66 ] examined how lifestyle behaviours might be linked with mental health outcomes. The studies looked at leisure activities [ 63 , 80 ], diet [ 29 ], alcohol use [ 29 , 31 , 38 , 51 ] and sleep [ 45 ].
Depressive symptoms were independently associated with problem drinking and possible alcohol dependence for both genders but were not associated with frequency of drinking and heavy episodic drinking. Students with higher levels of depressive symptoms reported significantly more problem drinking and possible alcohol dependence [ 31 ]. Mahadevan et al. (2010) [ 51 ] compared students and non-students seen in hospital for self-harm and found no difference in harmful use of alcohol and illicit drugs.
Poor sleep quality and increased consumption of unhealthy foods were also positively associated with depressive symptoms and perceived stress [ 29 ]. The correlation with dietary behaviours and poor mental health outcomes was low, but also confirmed by the negative correlation between less perceived stress and depressive symptoms and consumption of a healthier diet.
Physical activity and participation in leisure pursuits were both strongly correlated with mental wellbeing ( r = 0.4) [ 54 ], and negatively correlated with depressive symptoms and anxiety ( r = -0.6, -0.7) [ 66 ].
Thirty studies measuring the association between a wide range of factors and poor mental health and mental wellbeing in university and college students were identified and included in this review. Our purpose was to identify the factors that contribute to the growing prevalence of poor mental health amongst students in tertiary level education within the UK. We also aimed to identify factors that promote mental wellbeing and protect against deteriorating poor mental health.
Loneliness and social isolation were strongly associated with poor mental health and a sense of belonging and a strong support network were strongly associated with mental wellbeing and happiness. These associations were strongly positive in the eight studies that explored them and are consistent with other meta-analyses exploring the link between social support and mental health [ 87 ].
Another factor that appeared to be protective was older age when starting university. A wide range of personal traits and characteristics were also explored. Those associated with resilience, ability to adjust and better coping led to improved mental wellbeing. Better engagement appeared as an important mediator to potentially explain the relationship between these two variables. Engagement led to students being able to then tap into those features that are protective and promoting of mental wellbeing.
Other important risk factors for poor mental wellbeing that emerged were those students with existing or previous mental illness. Students on the autism spectrum and those with poor social problem-solving also were more likely to suffer from poor mental health. Negative self-image was also associated with poor mental health at university. Eating disorders were strongly associated with poor mental wellbeing and were found to be far more of a risk in students at university than in a comparative group of young people not in higher education. Other studies of university students also found that pre-existing poor mental health was a strong predictor of poor mental health in university students [ 88 ].
At a family level, the experience of childhood trauma and adverse experiences including, for example, neglect, household dysfunction or abuse, were strongly associated with poor mental health in young people at university. Students with a greater number of ‘adverse childhood experiences’ were at significantly greater risk of poor mental health than those students without experience of childhood trauma. This was also identified in a review of factors associated with depression and suicide related outcomes amongst university undergraduate students [ 88 ].
Our findings, in contrast to findings from other studies of university students, did not find that female gender associated with poor mental health and wellbeing, and it also found that being a mature student was protective of mental wellbeing.
Exam and course work pressure was associated with perceived stress and poor mental health. A lack of engagement with learning activities was also associated with poor mental health. A number of variables were not consistently shown to be associated with poor mental health including financial concerns and accommodation factors. Very little evidence related to university organisation or support structures was assessed in the evidence. One study found that a good induction programme had benefits for student mental wellbeing and may be a factor that enables students to become a part of a social network positive reinforcement cycle. Involvement in leisure activities was also found to be associated with improved coping strategies and better mental wellbeing. Students with poorer mental health tended to also eat in a less healthy manner, consume more harmful levels of alcohol, and experience poorer sleep.
This evidence review of the factors that influence mental health and wellbeing indicate areas where universities and higher education settings could develop and evaluate innovations in practice. These include:
Interventions before university to improve preparation of young people and their families for the transition to university.
Exploratory work to identify the acceptability and feasibility of identifying students at risk or who many be exhibiting indications of deteriorating mental health
Interventions that set out to foster a sense of belonging and identify
Creating environments that are helpful for building social networks
Improving mental health literacy and access to high quality support services
This review has a number of limitations. Most of the included studies were cross-sectional in design, with a small number being longitudinal ( n = 7), following students over a period of time to observe changes in the outcomes being measured. Two limitations of these sources of data is that they help to understand associations but do not reveal causality; secondly, we can only report the findings for those variables that were measured, and we therefore have to support causation in assuming these are the only factors that are related to mental health.
Furthermore, our approach has segregated and categorised variables in order to better understand the extent to which they impact mental health. This approach does not sufficiently explore or reveal the extent to which variables may compound one another, for example, feeling the stress of new ways of learning may not be a factor that influences mental health until it is combined with a sense of loneliness, anxiety about financial debt and a lack of parental support. We have used our PPI group and the development of vignettes of their experiences to seek to illustrate the compounding nature of the variables identified.
We limited our inclusion criteria to studies undertaken in the UK and published within the last decade (2009–2020), again meaning we may have limited our inclusion of relevant data. We also undertook single data extraction of data which may increase the risk of error in our data.
Understanding factors that influence students’ mental health and wellbeing offers the potential to find ways to identify strategies that enhance the students’ abilities to cope with the challenges of higher education. This review revealed a wide range of variables and the mechanisms that may explain how they impact upon mental wellbeing and increase the risk of poor mental health amongst students. It also identified a need for interventions that are implemented before young people make the transition to higher education. We both identified young people who are particularly vulnerable and the factors that arise that exacerbate poor mental health. We highlight that a sense of belonging and supportive networks are important buffers and that there are indicators including lack of engagement that may enable early intervention to provide targeted and appropriate support.
Availability of data and materials
Further details of the study and the findings can be provided on request to the lead author ([email protected]).
Association of Colleges. Association of Colleges’ survey on students with mental health conditions in further education. London: 2017.
Google Scholar
Hughes G, Spanner L. The University Mental Health Charter. Leeds: Student Minds; 2019.
Sivertsen B, Hysing M, Knapstad M, Harvey AG, Reneflot A, Lønning KJ, et al. Suicide attempts and non-suicidal self-harm among university students: prevalence study. BJPsych Open. 2019;5(2):e26.
Article PubMed PubMed Central Google Scholar
Storrie K, Ahern K, Tuckett A. A systematic review: students with mental health problems—a growing problem. Int J Nurs Pract. 2010;16(1):1–6.
Article PubMed Google Scholar
Pereira S, Reay K, Bottell J, Walker L, Dzikiti C, Platt C, Goodrham C. Student Mental Health Survey 2018: A large scale study into the prevalence of student mental illness within UK universities. 2019.
Bayram N, Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc Psychiatry Psychiatr Epidemiol. 2008;43(8):667–72.
Bewick B, Koutsopoulou G, Miles J, Slaa E, Barkham M. Changes in undergraduate students’ psychological well-being as they progress through university. Stud High Educ. 2010;35(6):633–45.
Article Google Scholar
Thorley C. Not By Degrees: Not by degrees: Improving student mental health in the UK’s universities. London: IPPR; 2017.
Eisenberg D, Golberstein E, Hunt JB. Mental health and academic success in college. BE J Econ Anal Pol. 2009;9(1):1–37.
Hysenbegasi A, Hass SL, Rowland CR. The impact of depression on the academic productivity of university students. J Ment Health Policy Econ. 2005;8(3):145.
PubMed Google Scholar
Chowdry H, Crawford C, Dearden L, Goodman A, Vignoles A. Widening participation in higher education: analysis using linked administrative data. J R Stat Soc A Stat Soc. 2013;176(2):431–57.
Macaskill A. The mental health of university students in the United Kingdom. Br J Guid Couns. 2013;41(4):426–41.
Belfield C, Britton J, van der Erve L. Higher Education finance reform: Raising the repayment threshold to£ 25,000 and freezing the fee cap at £ 9,250: Institute for Fiscal Studies Briefing note. London: Institute for Fiscal Studies; 2017. Available from https://ifs.org.uk/publications/9964 .
Benson-Egglenton J. The financial circumstances associated with high and low wellbeing in undergraduate students: a case study of an English Russell Group institution. J Furth High Educ. 2019;43(7):901–13.
Jessop DC, Herberts C, Solomon L. The impact of financial circumstances on student health. Br J Health Psychol. 2005;10(3):421–39.
(2020) SCSC. Canadians’ mental health during the COVID-19 pandemic. 2020.
(NUS) NUoS. Coronavirus Student Survey phase III November 2020. 2020.
Hellemans K, Abizaid A, Gabrys R, McQuaid R, Patterson Z. For university students, COVID-19 stress creates perfect conditions for mental health crises. The Conversation. 2020. Available from: https://theconversation.com/for-university-students-covid-19-stress-creates-perfect-conditions-for-mental-health-crises-149127 .
England N. Children and Young People with an Eating Disorder Waiting Times: NHS England; 2021 [Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/cyped-waiting-times/
King JA, Cabarkapa S, Leow FH, Ng CH. Addressing international student mental health during COVID-19: an imperative overdue. Australas Psychiatry. 2020;28(4):469.
Rana R, Smith E, Walking J. Degrees of disturbance: the new agenda; the Impact of Increasing Levels of Psychological Disturbance Amongst Students in Higher Education. England: Association for University and College Counselling Rugby; 1999.
AMOSSHE. Responding to student mental health issues: 'Duty of Care' responsibilities for student services in higher education. https://www.amosshe.org.uk/resources/Documents/AMOSSHE_Duty_of_Care_2001.pdf [accessed 24.12.2020]. (2001).
Universities UK. Student mental wellbeing in higher education. Good practice guide. London: Universities UK; 2015.
Williams M, Coare P, Marvell R, Pollard E, Houghton A-M, Anderson J. 2015. Understanding provision for students with mental health problems and intensive support needs: Report to HEFCE by the Institute for Employment Studies (IES) and Researching Equity, Access and Partnership (REAP). Institute for Employment Studies.
Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. 2010;46(1):3–10.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. In.: Oxford; 2000.
Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890.
El Ansari W, Adetunji H, Oskrochi R. Food and mental health: relationship between food and perceived stress and depressive symptoms among university students in the United Kingdom. Cent Eur J Public Health. 2014a;22(2):90–7.
El Ansari W, Dibba E, Stock C. Body image concerns: levels, correlates and gender differences among students in the United Kingdom. Cent Eur J Public Health. 2014b;22(2):106–17.
Ansari EL, W, Oskrochi R, Stock C. Symptoms and health complaints and their association with perceived stress: Students from seven universities in England, Wales and Northern Ireland. J Public Health. 2013;21(5):413–25.
El Ansari W, Sebena R, Stock C. Do importance of religious faith and healthy lifestyle modify the relationships between depressive symptoms and four indicators of alcohol consumption? A survey of students across seven universities in England, Wales, and Northern Ireland. Subst Use Misuse. 2014c;49(3):211–20.
El Ansari W, Stock C. Is the health and wellbeing of university students associated with their academic performance? Cross sectional findings from the United Kingdom. International Journal of Environmental Research & Public Health [Electronic Resource]. 2010;7(2):509–27.
Gnan GH, Rahman Q, Ussher G, Baker D, West E, Rimes KA. General and LGBTQ-specific factors associated with mental health and suicide risk among LGBTQ students. J Youth Stud. 2019;22(10):1393–408.
Jackson SL, Dritschel B. Modeling the impact of social problem-solving deficits on depressive vulnerability in the broader autism phenotype. Res Aut Spectr Disord. 2016;21:128–38.
Richardson T, Elliott P, Roberts R. The impact of tuition fees amount on mental health over time in British students. J Public Health. 2015;37(3):412–8.
Article CAS Google Scholar
Richardson T, Mma Y, Jansen M, Elliott P, Roberts R. Financial difficulties and psychosis risk in British undergraduate students: a longitudinal analysis. J Public Ment Health. 2018;17(2):61–8.
Thomas L, Briggs P, Hart A, Kerrigan F. Understanding social media and identity work in young people transitioning to university. Comput Hum Behav. 2017;76:541–53.
Hixenbaugh P, Dewart H, Towell T. What enables students to succeed? An investigation of socio-demographic, health and student experience variables. Psychodyn Pract. 2012;18(3):285–301.
Holliman A, Martin A, Collie R. Adaptability, engagement, and degree completion: a longitudinal investigation of university students. Educ Psychol. 2018;38(6):785–99.
McLafferty M, Armour C, Bunting B, Ennis E, Lapsley C, Murray E, et al. Coping, stress, and negative childhood experiences: the link to psychopathology, self-harm, and suicidal behavior. Psychic J. 2019;8(3):293–306.
Nightingale S, Roberts S, Tariq V, Appleby Y, Barnes L, Harris R, et al. Trajectories of university adjustment in the United Kingdom: EMOTION management and emotional self-efficacy protect against initial poor adjustment. Learn Individ Differ. 2013;27:174–81.
Berry K, Kingswell S. An investigation of adult attachment and coping with exam-related stress. Br J Guid Couns. 2012;40(4):315.
Denovan A, Macaskill A. Stress and subjective well-being among first year UK undergraduate students. J Happiness Stud. 2017a;18(2):505–25.
Hassel S, Ridout N. An investigation of first-year students’ and lecturers’ expectations of university education. Front Psychol. 2018;8:2218.
Norbury R, Evans S. Time to think: subjective sleep quality, trait anxiety and university start time. Psychiatry Res. 2019;271:214–9.
Por J, Barriball L, Fitzpatrick J, Roberts J. Emotional intelligence: its relationship to stress, coping, well-being and professional performance in nursing students. Nurse Educ Today. 2011;31(8):855.
Honney K, Buszewicz M, Coppola W, Griffin M. Comparison of levels of depression in medical and non-medical students. Clin Teach. 2010;7(3):180–4.
Kotera Y, Conway E, Van Gordon W. Mental health of UK university business students: Relationship with shame, motivation and self-compassion. Journal of Education for Business. 2019;94(1):11–20.
Oliver EJ, Markland D, Hardy J. Interpretation of self-talk and post-lecture affective states of higher education students: a self-determination theory perspective. Br J Educ Psychol. 2010;80(Pt 2):307–23.
O’Neill S, McLafferty M, Ennis E, Lapsley C, Bjourson T, Armour C, et al. Socio-demographic, mental health and childhood adversity risk factors for self-harm and suicidal behaviour in College students in Northern Ireland. J Affect Disord. 2018;239:58–65.
Mahadevan S, Hawton K, Casey D. Deliberate self-harm in Oxford University students, 1993–2005: a descriptive and case-control study. Soc Psychiatry Psychiatr Epidemiol. 2010;45(2):211–9.
Boulton CA, Hughes E, Kent C, Smith JR, Williams HTP. Student engagement and wellbeing over time at a higher education institution. PLoS One [Electronic Resource]. 2019;14(11): e0225770.
Davies EL, Paltoglou AE. Public self-consciousness, pre-loading and drinking harms among university students. Subst Use Misuse. 2019;54(5):747–57.
Denovan A, Macaskill A. Stress, resilience and leisure coping among university students: Applying the broaden-and-build theory. Leisure Studies. 2017b;36(6):852–65.
El Ansari W, Vallentin-Holbech L, Stock C. Predictors of illicit drug/s use among university students in Northern Ireland, Wales and England. Glob J Health Sci. 2015;7(4):18–29.
Freeth M, Bullock T, Milne E. The distribution of and relationship between autistic traits and social anxiety in a UK student population. Autism. 2013;17(5):571–81.
Jessop DC, Reid M, Solomon L. Financial concern predicts deteriorations in mental and physical health among university students. Psychology Health. 2020;35(2):196–209.
Kannangara CS, Allen RE, Waugh G, Nahar N, Khan SZN, Rogerson S, Carson J. All that glitters is not grit: Three studies of grit in university students. Front Psychol. 2018;9:1539.
Lloyd J, Ward T, Young J. Do parental interpersonal power and prestige moderate the relationship between parental acceptance and psychological adjustment in U.K. Students? Cross-Cultural Research. The Journal of Comparative Social Science. 2014;48(3):326–35.
McIntyre JC, Worsley J, Corcoran R, Harrison Woods P, Bentall RP. Academic and non-academic predictors of student psychological distress: the role of social identity and loneliness. J Ment Health. 2018;27(3):230–9.
Ribchester C, Ross K, Rees EL. Examining the impact of pre-induction social networking on the student transition into higher education. Innov Educ Teach Int. 2014;51(4):355–65.
Richardson T, Elliott P, Roberts R. Relationship between loneliness and mental health in students. J Public Ment Health. 2017a;16(2):48–54.
Richardson T, Elliott P, Roberts R, Jansen M. A Longitudinal Study of Financial Difficulties and Mental Health in a National Sample of British Undergraduate Students. Community Ment Health J. 2017;53(3):344–52.
Taylor PJ, Dhingra K, Dickson JM, McDermott E. Psychological Correlates of Self-Harm within Gay, Lesbian and Bisexual UK University Students. Arch Suicide Res. 2020;24(sup1):41–56.
Thomas L, Orme E, Kerrigan F. Student loneliness: The role of social media through life transitions. Comput Educ. 2020;146:103754.
Tyson P, Wilson K, Crone D, Brailsford R, Laws K. Physical activity and mental health in a student population. J Ment Health. 2010;19(6):492–9.
Folkman S. The Oxford handbook of stress, health, and coping. Oxford: Oxford University Press; 2011.
Gorczynski P, Sims-schouten W, Hill D, Wilson JC. Examining mental health literacy, help seeking behaviours, and mental health outcomes in UK university students. J Ment Health Train Educ Pract. 2017;12(2):111–20.
Felitti VJ. Adverse childhood experiences and adult health. Acad Pediatr. 2009;9(3):131–2.
Denovan A, Macaskill A. An interpretative phenomenological analysis of stress and coping in first year undergraduates. Br Educ Res J. 2013;39(6):1002–24.
Bandura A. Self-efficacy: The foundation of agency. Control of human behavior, mental processes, and consciousness: Essays in honor of the 60th birthday of August Flammer. 2000;16.
Martin AJ, Nejad H, Colmar S, Liem GAD. Adaptability: Conceptual and empirical perspectives on responses to change, novelty and uncertainty. J Psychol Couns Sch. 2012;22(1):58–81.
Lazarus RS, Folkman S. Stress, appraisal, and coping: Springer publishing company; 1984.
Gross JJ. Emotion regulation: Past, present, future. Cogn Emot. 1999;13(5):551–73.
Mayer JD, Salovey P, Caruso DR. TARGET ARTICLES:" Emotional Intelligence: Theory, Findings, and Implications". Psychol Inq. 2004;15(3):197–215.
Duckworth AL, Peterson C, Matthews MD, Kelly DR. Grit: perseverance and passion for long-term goals. J Pers Soc Psychol. 2007;92(6):1087.
Snyder CR, Ilardi SS, Cheavens J, Michael ST, Yamhure L, Sympson S. The role of hope in cognitive-behavior therapies. Cognit Ther Res. 2000;24(6):747–62.
Scheier MF, Carver CS, Bridges MW. Optimism, pessimism, and psychological well-being. 2001.
Seligman ME. Positive psychology in practice: Wiley; 2012.
Masten AS. Ordinary magic: Lessons from research on resilience in human development. Education Canada. 2009;49(3):28–32.
Rosenberg M, Schooler C, Schoenbach C, Rosenberg F. Global self-esteem and specific self-esteem: Different concepts, different outcomes. Am Sociol Rev. 1995:141–56.
Oliver EJ, Markland D, Hardy J. Interpretation of self-talk and post-lecture affective states of higher education students: A self-determination theory perspective. Br J Educ Psychol. 2010;80(2):307–23.
Hofmann W, Friese M, Strack F. Impulse and self-control from a dual-systems perspective. Perspect Psychol Sci. 2009;4(2):162–76.
Aceijas C, Waldhausl S, Lambert N, Cassar S, Bello-Corassa R. Determinants of health-related lifestyles among university students. Perspect Public Health. 2017;137(4):227–36.
Fredrickson BL. The broaden–and–build theory of positive emotions. Philos Trans R Soc Lond B Biol Sci. 2004;359(1449):1367–77.
Tugade MM, Fredrickson BL, Feldman Barrett L. Psychological resilience and positive emotional granularity: Examining the benefits of positive emotions on coping and health. J Pers. 2004;72(6):1161–90.
Harandi TF, Taghinasab MM, Nayeri TD. The correlation of social support with mental health: A meta-analysis. Electron physician. 2017;9(9):5212.
Sheldon E, Simmonds-Buckley M, Bone C, Mascarenhas T, Chan N, Wincott M, Gleeson H, Sow K, Hind D, Barkham M. Prevalence and risk factors for mental health problems in university undergraduate students: A systematic review with meta-analysis. J Affect Disord. 2021;287:282–92.
Download references
Acknowledgements
We acknowledge the input from our public advisory group which included current and former students, and family members of students who have struggled with their mental health. The group gave us their extremely valuable insights to assist our understanding of the evidence.
This project was supported by funding from the National Institute for Health Research as part of the NIHR Public Health Research Programme (fuding reference 127659 Public Health Review Team). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
University of Sheffield, Sheffield, UK
Fiona Campbell, Lindsay Blank, Anna Cantrell, Susan Baxter, Christopher Blackmore, Jan Dixon & Elizabeth Goyder
You can also search for this author in PubMed Google Scholar
Contributions
All of the included authors designed the project methods and prepared a protocol. A.C. designed the search strategy. F.C, L.B and C.B screened the identified citations and undertook data extraction. S.B. led the PPI involvement. JD participated as a member of the PPI group. F.C and L.B undertook the analysis. F.C. and L.B wrote the main manuscript text. All authors reviewed the manuscript. F.C designed Figs. 2 , 3 and 4 . The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Fiona Campbell .

Ethics declarations
Ethics approval and consent to participate.
Not applicable as this was secondary research.
Consent for publication
Not applicable.
Competing interests
None of the authors have competing interests or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Campbell, F., Blank, L., Cantrell, A. et al. Factors that influence mental health of university and college students in the UK: a systematic review. BMC Public Health 22 , 1778 (2022). https://doi.org/10.1186/s12889-022-13943-x
Download citation
Received : 03 February 2022
Accepted : 25 July 2022
Published : 20 September 2022
DOI : https://doi.org/10.1186/s12889-022-13943-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Student mental health
- Mental wellbeing
- Risk factors
- Rapid review
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]

How stress affects your health
Stress can be brief, situational, and a positive force motivating performance, but if experienced over an extended period of time it can become chronic stress, which negatively impacts health and well-being.
- Chronic Illness

Stress : We’ve all felt it. Sometimes stress can be a positive force, motivating you to perform well at your piano recital or job interview. But often—like when you’re stuck in traffic—it’s a negative force. If you experience stress over a prolonged period of time, it could become chronic—unless you take action.
A natural reaction
Have you ever found yourself with sweaty hands on a first date or felt your heart pound during a scary movie? Then you know you can feel stress in both your mind and body.
This automatic response developed in our ancient ancestors as a way to protect them from predators and other threats. Faced with danger, the body kicks into gear, flooding the body with stress hormones such as adrenaline and cortisol that elevate your heart rate, increase your blood pressure, boost your energy, and prepare you to deal with the problem.
These days, you’re not likely to face the threat of being eaten. But you probably do confront multiple challenges every day, such as meeting deadlines, paying bills, and juggling childcare that make your body react the same way. As a result, your body’s natural alarm system—the “fight or flight” response—may be stuck in the on position. And that can have serious consequences for your health.
Pressure points
Even short-lived, minor stress can have an impact. You might get a stomachache before you have to give a presentation, for example. More major acute stress, whether caused by a fight with your spouse or an event like an earthquake or terrorist attack, can have an even bigger impact.
Repeated acute stress may also contribute to inflammation in the circulatory system , particularly in the coronary arteries, and this is one pathway that is thought to tie stress to a heart attack. It also appears that how a person responds to stress can affect cholesterol levels.
Chronic stress
When stress starts interfering with your ability to live a normal life for an extended period, it becomes even more dangerous. The longer the stress lasts, the worse it is for both your mind and body. You might feel fatigued, unable to concentrate, or irritable for no good reason, for example. But chronic stress causes wear and tear on your body, too.
The long-term activation of the stress response system and the overexposure to cortisol and other stress hormones that come with it can disrupt almost all of your body's processes. This can put you at increased risk for a variety of physical and mental health problems, including anxiety, depression, digestive issues, headaches, muscle tension and pain, heart disease, heart attack, high blood pressure, stroke, sleep problems, weight gain, and memory and concentration impairment.
Chronic stress may also cause disease, either because of changes in your body or the overeating, smoking, and other bad habits people use to cope with stress. Job strain—high demands coupled with low decision-making latitude—is associated with increased risk of coronary disease , for example. Other forms of chronic stress, such as depression and low levels of social support, have also been implicated in increased cardiovascular risk.
Chronic stress also suppresses the body's immune system , making it harder to recover from illnesses.
What you can do
Reducing your stress levels can not only make you feel better right now, but may also protect your health long-term. Several research studies have demonstrated, for example, that interventions to improve psychological health can have a beneficial impact on cardiovascular health . As a result, researchers recommend boosting your positive affect—feelings like happiness, joy, contentment, and enthusiasm—by making time for enjoyable activities every day.
Other strategies for reducing stress include:
- Identify what’s causing stress. Monitor your state of mind throughout the day. If you feel stressed, write down the cause, your thoughts, and your mood. Once you know what’s bothering you, develop a plan for addressing it. That might mean setting more reasonable expectations for yourself and others or asking for help with household responsibilities, job assignments, or other tasks. List all your commitments, assess your priorities, and then eliminate any tasks that are not absolutely essential.
- Build strong relationships. Relationships can be a source of stress. Research has found that negative, hostile reactions with your spouse cause immediate changes in stress-sensitive hormones, for example. But relationships can also serve as stress buffers. Reach out to family members or close friends and let them know you’re having a tough time. They may be able to offer practical assistance and support, useful ideas, or just a fresh perspective as you begin to tackle whatever’s causing your stress.
- Walk away when you’re angry. Before you react, take time to regroup by counting to 10. Then reconsider. Walking or other physical activities can also help you work off steam. Plus, exercise increases the production of endorphins, your body’s natural mood booster. Commit to a daily walk or other form of exercise—a small step that can make a big difference in reducing stress levels.
- Rest your mind. To help ensure you get the recommended seven or eight hours of shut-eye, cut back on caffeine, remove distractions such as television or computers from your bedroom, and go to bed at the same time each night. Research shows that activities like yoga and relaxation exercises not only help reduce stress, but also boost immune functioning .
- Get help. If you continue to feel overwhelmed, consult with a psychologist or other licensed mental health professional who can help you learn how to manage stress effectively. They can help you identify situations or behaviors that contribute to your chronic stress and then develop an action plan for changing them.
Recommended Reading

Related reading
- Stress effects on the body
- Stress in America
You may also like
Participating in Health Research Studies
What is health research.
- Is Health Research Safe?
- Is Health Research Right for Me?
- Types of Health Research
The term "health research," sometimes also called "medical research" or "clinical research," refers to research that is done to learn more about human health. Health research also aims to find better ways to prevent and treat disease. Health research is an important way to help improve the care and treatment of people worldwide.
Have you ever wondered how certain drugs can cure or help treat illness? For instance, you might have wondered how aspirin helps reduce pain. Well, health research begins with questions that have not been answered yet such as:
"Does a certain drug improve health?"
To gain more knowledge about illness and how the human body and mind work, volunteers can help researchers answer questions about health in studies of an illness. Studies might involve testing new drugs, vaccines, surgical procedures, or medical devices in clinical trials . For this reason, health research can involve known and unknown risks. To answer questions correctly, safely, and according to the best methods, researchers have detailed plans for the research and procedures that are part of any study. These procedures are called "protocols."
An example of a research protocol includes the process for determining participation in a study. A person might meet certain conditions, called "inclusion criteria," if they have the required characteristics for a study. A study on menopause may require participants to be female. On the other hand, a person might not be able to enroll in a study if they do not meet these criteria based on "exclusion criteria." A male may not be able to enroll in a study on menopause. These criteria are part of all research protocols. Study requirements are listed in the description of the study.
A Brief History
While a few studies of disease were done using a scientific approach as far back as the 14th Century, the era of modern health research started after World War II with early studies of antibiotics. Since then, health research and clinical trials have been essential for the development of more than 1,000 Food and Drug Administration (FDA) approved drugs. These drugs help treat infections, manage long term or chronic illness, and prolong the life of patients with cancer and HIV.
Sound research demands a clear consent process. Public knowledge of the potential abuses of medical research arose after the severe misconduct of research in Germany during World War II. This resulted in rules to ensure that volunteers freely agree, or give "consent," to any study they are involved in. To give consent, one should have clear knowledge about the study process explained by study staff. Additional safeguards for volunteers were also written in the Nuremberg Code and the Declaration of Helsinki .
New rules and regulations to protect research volunteers and to eliminate ethical violations have also been put in to place after the Tuskegee trial . In this unfortunate study, African American patients with syphilis were denied known treatment so that researchers could study the history of the illness. With these added protections, health research has brought new drugs and treatments to patients worldwide. Thus, health research has found cures to many diseases and helped manage many others.
Why is Health Research Important?
The development of new medical treatments and cures would not happen without health research and the active role of research volunteers. Behind every discovery of a new medicine and treatment are thousands of people who were involved in health research. Thanks to the advances in medical care and public health, we now live on average 10 years longer than in the 1960's and 20 years longer than in the 1930's. Without research, many diseases that can now be treated would cripple people or result in early death. New drugs, new ways to treat old and new illnesses, and new ways to prevent diseases in people at risk of developing them, can only result from health research.
Before health research was a part of health care, doctors would choose medical treatments based on their best guesses, and they were often wrong. Now, health research takes the guesswork out. In fact, the Food and Drug Administration (FDA) requires that all new medicines are fully tested before doctors can prescribe them. Many things that we now take for granted are the result of medical studies that have been done in the past. For instance, blood pressure pills, vaccines to prevent infectious diseases, transplant surgery, and chemotherapy are all the result of research.
Medical research often seems much like standard medical care, but it has a distinct goal. Medical care is the way that your doctors treat your illness or injury. Its only purpose is to make you feel better and you receive direct benefits. On the other hand, medical research studies are done to learn about and to improve current treatments. We all benefit from the new knowledge that is gained in the form of new drugs, vaccines, medical devices (such as pacemakers) and surgeries. However, it is crucial to know that volunteers do not always receive any direct benefits from being in a study. It is not known if the treatment or drug being studied is better, the same, or even worse than what is now used. If this was known, there would be no need for any medical studies.
- Next: Is Health Research Safe? >>
- Last Updated: May 27, 2020 3:05 PM
- URL: https://guides.library.harvard.edu/healthresearch
| | |

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
JavaScript appears to be disabled on this computer. Please click here to see any active alerts .
Research on Health Effects from Air Pollution
Decades of research have shown that air pollutants such as ozone and particulate matter (PM) increase the amount and seriousness of lung and heart disease and other health problems. More investigation is needed to further understand the role poor air quality plays in causing detrimental effects to health and increased disease, especially in vulnerable populations. Children, the elderly, and people living in areas with high levels of air pollution are especially susceptible.
Results from these investigations are used to support the nation's air quality standards under the Clean Air Act and contribute to improvements in public health.
On this page:
Health Effects of Air Pollutants on Vulnerable Populations
Long-term and short-term effects from exposure to air pollutants.
- Multipollutant Exposures and Changes in Environmental Conditions
- Leveraging Big Data for Innovations in Health Science
Health Effects of Wildfire Smoke
Public health intervention and communications strategies, integrated science assessments for air pollutants.

Research has shown that some people are more susceptible than others to air pollutants. These groups include children, pregnant women, older adults, and individuals with pre-existing heart and lung disease. People in low socioeconomic neighborhoods and communities may be more vulnerable to air pollution because of many factors. Proximity to industrial sources of air pollution, underlying health problems, poor nutrition, stress, and other factors can contribute to increased health impacts in these communities.
There is a need for greater understanding of the factors that may influence whether a population or age group is at increased risk of health effects from air pollution. In addition, advances to analytical approaches used to study the health effects from air pollution will improve exposure estimates for healthy and at-risk groups.
The research by EPA scientists and others inform the required reviews of the primary National Ambient Air Quality Standards (NAAQS), which is done with the development of Integrated Science Assessments (ISAs). These ISAs are mandated by Congress every five years to assess the current state of the science on criteria air pollutants and determine if the standards provide adequate protection to public health.
Research is focused on addressing four areas:
- Identifying and characterizing whether there are key reproductive factors and critical stages of development that are impacted by air pollution exposures;
- Determining the role of acute and chronic sociodemographic factors in air pollution health disparities;
- Understanding how diet modifies responses to air pollution;
- Evaluating long-term lifestyle and chronic disease effects on air pollution-induced respiratory and cardiovascular responses
A multi-disciplinary team of investigators is coordinating epidemiological, human observational, and basic toxicological research to assess the effects of air pollution in at-risk populations and develop strategies to protect these populations, particularly those with pre-existing disease. The results from these products will improve risk assessments by clarifying the role of modifying factors such as psychosocial stress (e.g. noise) and diet, and determining the impact of individual susceptibility on the relationship between air pollutant exposures and health.
Related Links
- Healthy Heart Research
- Integrated Science Assessments
- Criteria Air Pollutants

People can experience exposure to varying concentrations of air pollution. Poor air quality can impact individuals for a short period of time during the day, or more frequently during a given day. Exposure to pollutants can also occur over multiple days, weeks or months due to seasonal air pollution, such as increased ozone during the summer or particulate matter from woodstoves during the winter.
The health impact of air pollution exposure depends on the duration and concentrations, and the health status of the affected populations. Studies are needed to increase knowledge of the exposure duration and the possible cumulative increase in risk.
The research is focused on three main areas:
- Short-term peak exposures, such as wildfires, traffic-related sources, or other episodic events;
- Intermittent and cumulative exposures;
- Mechanisms underlying the exposure risks
Researchers are evaluating the health responses of intermittent multiple days versus one-day air pollution exposure in controlled human exposure, animal, and in vitro models and associated cellular and molecular mechanisms. They are employing population-based models and electronic health records to assess the health effects of short-term and long-term exposures and identifying populations at greatest risk of health effects. The work is improving our understanding of the possible cumulative effects of multiple short-term peak exposures and the relationship of these exposures to longer-term exposures and risks.
Multipollutant Exposures and Changes in Environmental Conditions

EPA research is providing information to understand how individuals may respond to two or more pollutants or mixtures and how environmental conditions may impact air quality. While risk estimates for exposure to individual criteria air pollutants such as PM and ozone are well established, the acute and cumulative effects of combinations of pollutants is not well understood. In addition, research is needed to determine how changes in the environment affect both pollutant formation and subsequent responsiveness to exposures in healthy and susceptible individuals.
The research is focused on three specific questions:
- What is the role of temperature and photochemical aging on the health impact of wildfire smoke and air pollution mixtures?
- What is the effect of changing environmental conditions (i.e., temperature and humidity) on responsiveness to air pollution?
- Does prior pollutant exposure modify responsiveness to subsequent exposures?
The integrated, multi-disciplinary research includes:
- Epidemiologic analyses of environmental influences on morbidity and mortality in populations,
- Simulations of changing environmental conditions in multi-pollutant formation in atmospheric chamber studies coupled with clinical and toxicological assessments in healthy and at-risk populations,
- Evaluation of pre-exposure as a modifying effect on subsequent exposures
The results are revealing how changes in environmental conditions affect pollutant formation and subsequent health impact in at-risk populations. The research findings are informing EPA’s Integrated Science Assessments for criteria air pollutants and assisting with future regulatory decisions on the National Ambient Air Quality Standards (NAAQS).
Leveraging Big Data for Innovations in Health Science

EPA is at the cutting edge of health science, using electronic health records, novel data systems, tissue-like advanced cellular models, molecular approaches, and animal models to evaluate the health impacts of air pollution. Researchers are using these powerful new techniques to identify factors that may increase sensitivity and vulnerability to air pollution effects.
The research is building capacity for future risk assessment and regulatory analyses that go beyond traditional lines of evidence to more clearly define populations and lifestages at increased risk of health effects from air pollution.
To continue to protect public health from poor air quality, researchers must consider new epidemiological, toxicological and clinical approaches to understand the health risks of poor air quality and the biological mechanisms responsible for these risks. At the center of these new research approaches is an explosion of data availability and methodological approaches for handling large clinical and molecular datasets, also known as "big data."
While data of increasing size, depth, and complexity have accelerated research for many industries and scientific fields, big data is sometimes less recognized for the impacts it is having on environmental health studies. Increasingly, researchers are able to examine vulnerable populations with unprecedented precision and detail while also evaluating hundreds of thousands of molecular biomarkers in order to understand biological mechanisms associated with exposure.
- Development of the InTelligence And Machine LEarning (TAME) Toolkit for Introductory Data Science, Chemical-Biological Analyses, Predictive Modeling, and Database Mining for Environmental Health Research (Journal Article)

Larger and more intense wildfires are creating the potential for greater smoke production and chronic exposures in the United States, particularly in the West. Wildfires increase air pollution in surrounding areas and can affect regional air quality.
The health effects of wildfire smoke can range from eye and respiratory tract irritation to more serious disorders, including reduced lung function, exacerbation of asthma and heart failure, and premature death. Children, pregnant women, and the elderly are especially vulnerable to smoke exposure. Emissions from wildfires are known to cause increased visits to hospitals and clinics by those exposed to smoke.
It is important to more fully understand the human health effects associated with short- and long-term exposures to smoke from wildfires as well as prescribed fires, together referred to as wildland fires. EPA is conducting research to advance understanding of the health effects from different types of fires as well as combustion phases. Researchers want to know:
- What is the full extent of health effects from smoke exposure?
- Who is most at risk?
- Are there differences in health effects from different wildfire fuel types or combustion phases (burning versus flaming)?
- What strategies and approaches are most effective in protecting public health?
- What are the environmental, social and economic impacts of wildfire emissions?
- Wildland Fire Research
- Smoke-Ready Toolbox for Wildfires
- Smoke Sense Project and App

Many communities throughout the United States face challenges in providing advice to residents about how best to protect their health when they are exposed to elevated concentrations of air pollutants from motor vehicle and industrial emissions and other sources of combustion, including wildland fire smoke.
Researchers are studying intervention strategies to reduce the health impacts from exposure to air pollution as well as ways to effectively communicate these health risks. To translate the science for use in public health communication and community empowerment, EPA is collaborating with other federal agencies, such as the Centers for Disease Control and Prevention (CDC) and the National Heart, Lung, and Blood Institute (NHLBI), and state and local agencies and tribes. The objectives are to identify ways to lower air pollution exposure or mitigate the biological responses at individual, community or ecosystem levels, and ultimately evaluate whether such interventions have benefits as measured by indicators of health, well-being or economics.
Studies are evaluating the interactions between behavior and social and economic factors to more thoroughly understand how these factors may influence health and well-being outcomes, which can inform effective and consistent health risk messaging.
- Healthy Heart Toolkit and Research
- Video: Air Quality Impacts on Public Health

EPA sets National Ambient Air Quality Standards (NAAQS) for six principal criteria air pollutants —nitrogen oxides, sulfur oxides, particulate matter, carbon monoxide, ozone and lead—all of which have been shown to be harmful to public health and the environment.
The Agency’s Integrated Science Assessments (ISAs) form the scientific foundation for the review of the NAAQS standards by providing the primary (human health-based) assessments and secondary (welfare-based, e.g. ecology, visibility, materials) assessments. The ISAs are assessments of the state of the science on the criteria pollutants. They are conducted as mandated under the Clean Air Act.
- Air Research Home
- Air Monitoring & Emissions
- Air Quality Modeling
- Wildland Fires
- Health Effects from Air Pollution
- Air & Energy
- Outreach, Tools & Resources
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
- Black Americans’ Views of and Engagement With Science
- 3. Black Americans’ views about health disparities, experiences with health care
Table of Contents
- Compared with other professions, fewer Black adults see people of their race at highest levels of success in science, engineering
- A majority of Black high school graduates recall a positive experience in STEM classes, but sizable shares also recall mistreatment
- Half or more Black Americans see mentors as especially influential to how many young people pursue STEM degrees
- Large majorities of Black adults have at least some trust in medical scientists or scientists, generally
- Black Americans generally hold positive views of medical researchers’ competence, skeptical of whether they own up to mistakes
- 75% of Black adults have heard about the Tuskegee study; a majority are skeptical that research procedures today will prevent serious misconduct
- About half of Black Americans say they’ve talked about the coronavirus outbreak multiple times a week
- Black Americans report mix of positive and negative reactions to science news, express frustration over political disagreements
- Acknowledgments
- Methodology
- Appendix: Detailed charts and tables
CORRECTION (Jan. 12, 2024): Chapter 3 of a previous version of this report included an incorrect percentage because one survey question was asked only of women. Among Black adults, 55% say they have ever had at least one of six negative experiences with doctors or other health care providers.
Black Americans offer a mixed assessment of the progress that has been made improving health outcomes for Black people: 47% say health outcomes for Black people have gotten better over the past 20 years, while 31% say they’ve stayed about the same and 20% think they’ve gotten worse.
Less access to quality medical care is the top reason Black Americans see contributing to generally worse health outcomes for Black people in the U.S. Large shares also see other factors as playing a role, including environmental quality problems in Black communities, and hospitals and medical centers giving lower priority to the well-being of Black people.
Asked about their own health care experiences, most Black Americans have positive assessments of the quality of care they’ve received most recently. However, a majority (55%) say they’ve had at least one of six negative experiences, including having to speak up to get the proper care and being treated with less respect than other patients. (A seventh issue asked about applied only to women.)
By and large, Black Americans do not express a widespread preference to see a Black health care provider for routine care: 64% say this makes no difference to them, though 31% say they would prefer to see a Black health care provider for care.
The experiences of younger Black women in the medical system stand out in the survey. A large majority of Black women ages 18 to 49 report having had at least one of seven negative health care experiences included in the survey. They are also more likely than other Black adults to say they would prefer a Black health care provider for routine care and to say a Black doctor or other health care provider would do a better job than medical professionals of other races and ethnicities at providing them with quality medical care.
Beliefs about key factors in health disparities for Black Americans
There are long-standing differences in health outcomes for Black people. Disproportionate mortalities from COVID-19 have heightened disparities between Black and other racial and ethnic populations in the U.S. The most recent estimates from the U.S. Census bureau projects life expectancy at 71.8 years for non-Hispanic Black Americans, the lowest since 2000 and below that estimated for other racial and ethnic groups. The White, non-Hispanic population experienced a smaller decline and, as a result, the gap between expected lifespans for Black and White Americans has widened in the past few years.
Experts have pointed to a number of contributing factors to disparities in health outcomes for Black Americans. The Center survey asked Black Americans for their own views about the reasons behind these disparities and their sense of whether there has been progress over time.
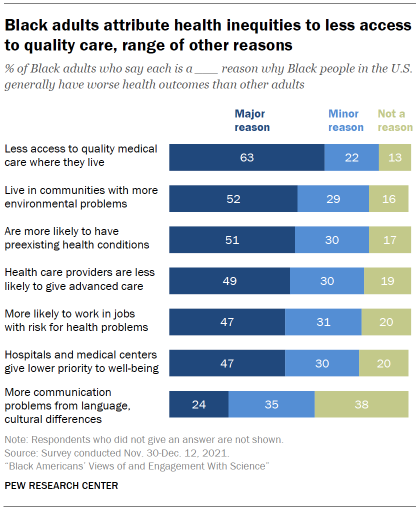
A majority of Black adults say less access to quality medical care where they live is a major reason why Black people in the U.S. generally have worse health outcomes than other adults. About two-in-ten (22%) say this is a minor reason, while just 13% say it is not a reason.
Black adults see a range of other factors – including environmental problems and less-advanced care from health care providers – as contributing to worse health outcomes for Black adults, though somewhat smaller shares cite these as major reasons than point to access issues.
About half (51%) say a major reason why Black people generally have worse health outcomes than others is because they are more likely to have preexisting health conditions. Issues with home and work environments also are seen as playing a role: 52% say a major reason why Black people have worse health outcomes than others is because they live in communities with more environmental problems that cause health issues; 47% say a major reason is that Black people are more likely to work in jobs that put them at risk for health problems.
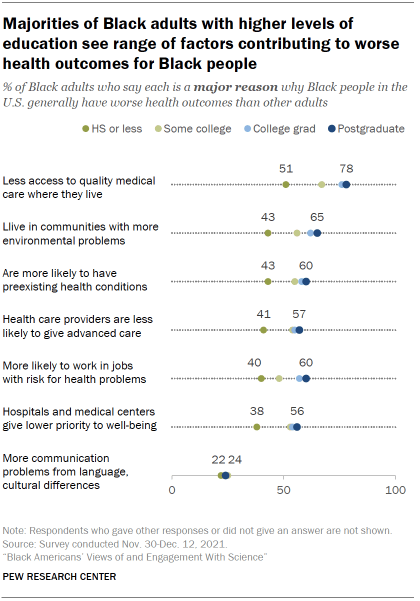
The health care system is also seen as contributing to the problem: 49% say a major reason why Black people generally have worse health outcomes is because health care providers are less likely to give Black people the most advanced medical care. A roughly equal share (47%) says hospitals and medical centers giving lower priority to their well-being is a major reason for differing health outcomes.
A smaller share (24%) views communication problems from language or cultural differences as a major reason why Black people generally have worse health outcomes than other adults in the U.S.
Black adults with higher levels of education are more likely than those with lower levels of education to point to a variety of factors as major reasons for worse health outcomes among Black people.
For instance, large majorities of Black postgraduates (78%) and college graduates (76%) say less access to quality medical care is a major reason Black people have worse health outcomes than other adults in the U.S., compared with 67% of those with some college experience and 51% of Black adults with a high school diploma or less education.
There are also differences in views by age. A majority of Black adults ages 50 and older (58%) say that being more likely to have preexisting health conditions is a major reason why Black people have worse health outcomes than others. Fewer of those under age 50 (46%) see this as a major reason.
Conversely, younger Black adults are more likely than older adults to cite actions from hospitals and medical centers: 50% of those under age 50 say hospitals and medical centers giving lower priority to their well-being is a major reason why Black people have worse health outcomes; 43% of Black adults 50 and older say the same.
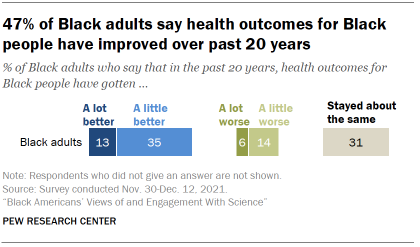
Overall, 47% think health outcomes for Black people have gotten a lot or a little better over the last 20 years. Still, 31% say they have stayed about the same and 20% think they have gotten a lot or a little worse.
For the most part, Black adults’ views on this question are fairly similar across characteristics such as age, gender and levels of educational attainment.
A majority of Black Americans give positive ratings of their recent health care, but can also point to negative experiences in the past
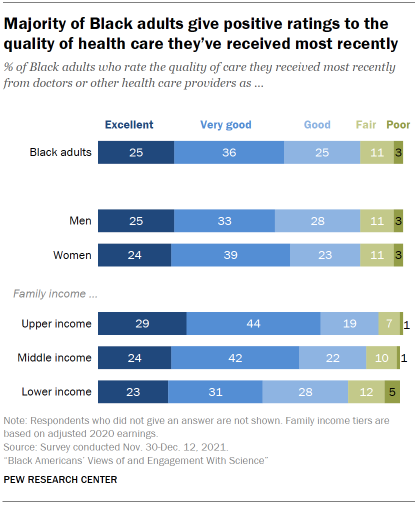
Black adults have generally positive impressions of their most recent experience with health care. A majority (61%) rate the quality of care they’ve received from doctors or other health care providers recently as excellent (25%) or very good (36%). A quarter describe the quality as good, while just 11% say it was fair and only 3% describe the quality of care they’ve received most recently as poor. These ratings are nearly identical to those of all U.S. adults.
Those with higher incomes report more positive recent experiences with doctors and other health care providers than do those with lower incomes.
When it comes to cost, 51% of Black adults describe the out-of-pocket cost of their most recent medical care as ‘about what is fair.’ About a quarter (27%) say they paid more than what’s fair, while 19% say they paid less than what’s fair. For more details, see the Appendix .
A majority of Black adults report at least one negative interaction with doctors and other health care providers at some point in the past
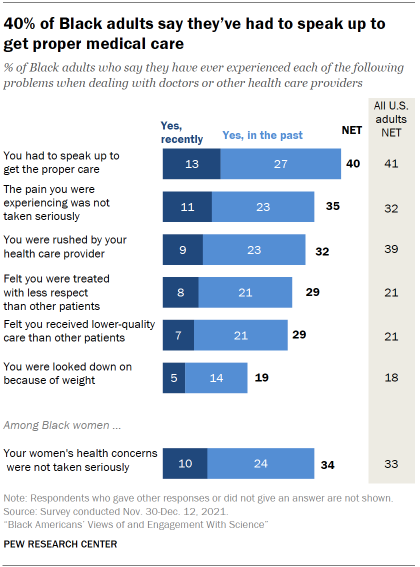
While Black adults generally offer positive ratings of the quality of care they’ve received most recently, a majority (55%) say they’ve had at least one of six negative experiences with doctors or other health care providers at some point in their lives. (A seventh issue asked about applied only to women.)
Overall, 40% of Black adults say they have had to speak up to get the proper care either recently (13%) or in the past (27%). This is the most frequently cited negative experience with medical care across the items included in the survey.
One focus group respondent described their experience this way:
“I had a situation where I had to go through about two different doctors until I was able to get the results that I was requesting, because they did not believe that the issues that I had were valid, or that they were as serious as I made them out to be. It’s kind of been an ongoing thing, so I’m always leery when I’m talking to physicians. I don’t trust them just because they are doctors. I know they have the Hippocratic Oath, but it feels like it’s a little different when they deal with African American patients. And I don’t care if it’s an African American physician or White physicians.” – Black woman, 25-39
When it comes to treatments for pain, 35% of Black adults say they’ve felt the pain they were experiencing was not taken seriously either recently (11%) or in past interactions (23%) with doctors and other health care providers.
About three-in-ten Black adults (32%) say they’ve felt rushed by their health care provider and 29% say they’ve felt they were treated with less respect than other patients, either recently or in past experiences with doctors and other health care providers. Similarly, 29% say they’ve felt they’ve received lower quality medical care at some point; 70% of Black adults say this has not happened to them.
Relatively fewer (19%) say they’ve been looked down on because of their weight or eating habits; 79% say this hasn’t happened to them.
Among Black women, 34% say their women’s health concerns or symptoms were not taken seriously in interactions with doctors and other health care providers.
Black adults at all family income levels are about equally likely to report having at least one of these experiences.
The frequency of negative experiences with the health care system are mostly similar between Black adults and all U.S. adults. However, greater shares of Black adults than all U.S. adults say they’ve felt they’ve received lower-quality care (29% vs. 21% of all U.S. adults) or been treated with less respect than other patients (29% vs. 21%). And fewer Black adults say they were rushed by a health care provider (32% vs. 39% of all U.S. adults).
Black women, especially younger Black women, stand out for the frequency with which they report having had negative health care experiences. Taken together, 63% of Black women say they’ve experienced at least one of the seven negative health care experiences measured in the survey. Among Black men, 46% say they’ve had at least one of six negative experiences with doctors or other health care providers. Black women were asked one more item than men, but the gap between men and women on the six experiences in common is almost identical (62% vs. 46%).
In their own words: Focus group participants on difficulties getting treatment for pain management
There are long-standing concerns about racial biases in pain management. A study in 2020 of emergency room patients experiencing acute appendicitis found wide racial disparities in pain management for both children and adults. The growing use of artificial intelligence algorithms to determine a patient’s need for pain management is raising new questions about how to address systematic bias in pain management treatments.
Here are a few of the comments from focus group participants about getting treatment for pain.
“Well, my husband’s condition (trigeminal neuralgia), it requires a narcotic. And before we got [to current health care provider] for so long, a lot of people just assumed that he was a junkie, like he was just coming in and trying to get pain medication and they wanted to put him on this rotation that just didn’t work, wanted him to take this Tylenol. And it was so frustrating.” – Black woman, age 25-39
“My mom, and I can’t think of it specifically, she has complained to me about being at the hospital and feeling as though they were treating her like she was a drug addict. When they would have to give her pain medication, or she would need something for pain – having her fill out forms, only allotting a certain amount, or cutting it, when her pain is … she goes through pain more times a day, they’ll cut it to less. Less than what she needs to get through the day and not be in pain.” – Black man, age 25-39
“At what point are you going to educate your nurses, your doctors, your ER team that, ‘Hey, this is the protocol when we have sickle cell’? Now, the ironic thing is, when she was going to the children’s hospital, they did have a sickle cell protocol and their treatment of their kids was a little bit different. Most of the time, … 85% of the time … because they were kids, they took their word for it. But when they transitioned over to the adult care, it’s terrible. It’s terrible with the pain, it’s terrible with pain management.” – Black woman, age 40-65
“I was in pain, like in my abdomen. Come to find out I had a fibroid. But I went to the emergency room. ‘Oh, no. You’re fine.’ Something like, ‘Your insurance won’t cover this emergency visit’ or something. ‘Just go to Walgreens and get some Tylenol.’ And I’m like, ’I’m in severe pain. Like I have abdominal pain.’ I ended up going to my doctor, the one I eventually found. He ended up getting me an ultrasound. We did blood work. It was just totally different.” – Black woman, age 25-39
A large majority of younger Black women ages 18 to 49 report negative interactions with health care providers: 71% say they’ve had at least one negative experience in the past. By comparison, a smaller share of Black women ages 50 and older say this (54%).
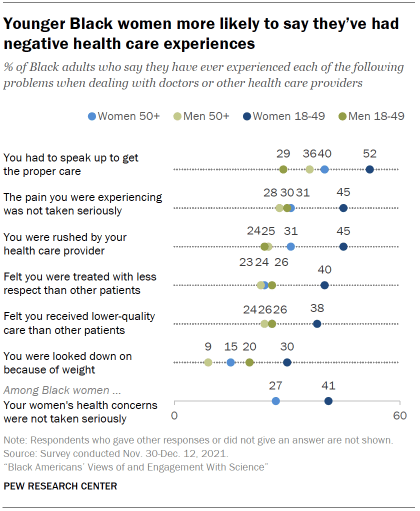
Among Black men, differences by age are more modest than among women, and the pattern runs in the opposite direction: 51% of men ages 50 and older report experiencing at least one of six negative experiences with health care providers, compared with a somewhat smaller share of men ages 18 to 49 (43%).
The experiences of younger Black women stand out across each individual item on health care interactions. For instance, 52% of younger Black women say they’ve had to speak up to get the proper care, compared with 40% of older women, 36% of older men and 29% of younger men.
Among U.S. adults, women ages 18 to 49 are also more likely than older women or than men to say they have had at least one of these negative experiences in a health care visit.
31% of Black adults say they would prefer to see a Black health care provider; a majority have no preference
The share of Black adults working in health-related jobs is roughly equal to their share in the overall workforce, although just 5% of physicians and surgeons are Black. The new survey asked people for their preferences and thoughts about what, if any, difference it makes to have a health care provider who shares their racial background.
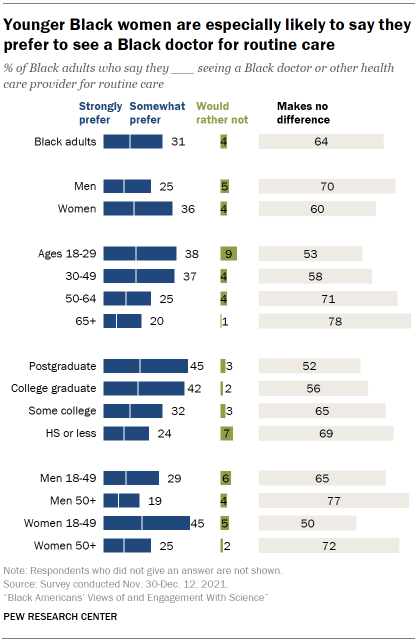
Overall, 31% of Black adults say they would strongly (14%) or somewhat prefer (17%) to see a Black doctor or other health care provider for routine medical care. About two-thirds (64%) say it makes no difference to them, and just 4% say they’d rather not do so for routine care.
Younger Black women stand out from their elders and from Black men in their preferences for seeing a Black health care provider.
Among Black women, a much greater share of those ages 18 to 49 than those 50 and older say they’d prefer to see a Black health care provider for routine care (45% vs. 25%). A majority of older Black women (72%) say it wouldn’t make a difference to them.
There’s a similar pattern in views among Black men, though the gap between younger and older Black men is not as large as among Black women: 29% of Black men ages 18 to 49 would prefer to see a Black health care provider for routine care, compared with 19% of Black men ages 50 and older.
There’s hardly any difference in views on this question between those who have seen a Black doctor or health care provider in the past and those who have not. Among the roughly two-thirds of Black adults who say they’ve seen a Black health care provider for routine care in the past, 32% say they would prefer to see a Black health care provider; among those who have not seen a Black health care provider previously, 30% express this view. See the Appendix for details .
Younger Black women are more likely to see benefits for the quality of medical care from health care treatment with same-race providers
When it comes to key aspects of medical care, majorities of Black adults view a Black doctor and other health care providers as about the same as providers who do not share their race or ethnicity at meeting their needs.
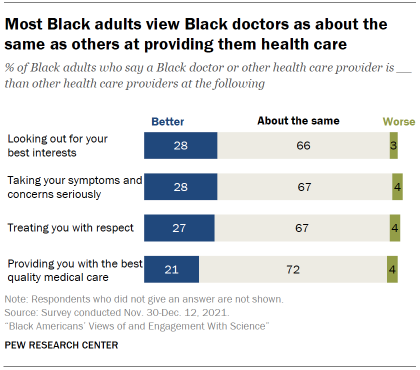
For instance, 72% of Black adults think a Black health care provider is about the same as other health professionals when it comes to the quality of medical care they provide; 21% think a Black health care provider is better than others at this, while just 4% say worse.
Roughly two-thirds view a Black health care provider as about the same as others when it comes to taking their symptoms and concerns seriously, treating them with respect, and looking out for their best interests. Roughly three-in-ten see a Black doctor or health care professional as better than other providers for each of these elements of care.
Among the 31% of Black Americans who say they would prefer to see a Black health care provider for routine matters, majorities think a Black health care provider is better than others at looking out for their best interests (64%), taking their symptoms seriously (64%), treating them with respect (60%) and providing the best quality medical care (53%).
It is unclear whether personal experience lies behind these beliefs. Black adults who have seen a Black health care provider in the past hold similar views on this as those who have not. See Appendix for more details .
Younger Black women are more inclined than older women and men to see an advantage from routine care with a Black health care provider. Still, the majority viewpoint across groups – including among younger Black women – is that a Black health care provider is about the same as others at providing key aspects of care.
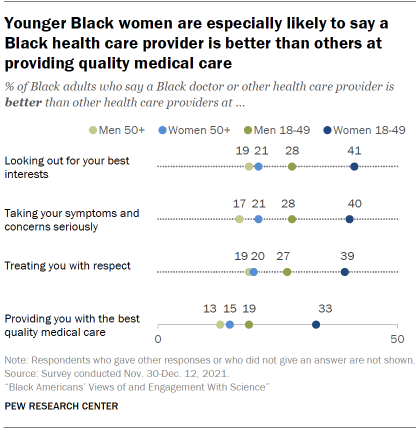
About four-in-ten Black women ages 18 to 49 (41%) say a Black health care provider is better than others at looking out for their best interests, compared with 53% who say they are about the same as other health care providers.
Smaller shares of Black women ages 50 and older (21%), Black men 18 to 49 (28%) and Black men ages 50 and older (19%) view a Black health care provider as better than others at looking out for their best interests. Majorities say they are about the same as others at this.
Age and gender patterns among Black adults are similar across the other aspects of care included in the survey.
When it comes to education, Black adults with higher levels of education tend to be more likely to view a Black doctor or health care provider as better than others when it comes to these key aspects of care. But as with patterns by age and gender, the majority view across levels of educational attainment remains that a Black health care provider is about the same as other healthcare professionals at providing routine health and medical care. See the Appendix for details.
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Sign up for The Briefing
Weekly updates on the world of news & information
- Black Americans
- Coronavirus (COVID-19)
- COVID-19 & Science
- COVID-19 in the News
- Medicine & Health
- Racial Bias & Discrimination
- Science News & Information
- STEM Education & Workforce
- Trust in Science
Most Black Americans Believe Racial Conspiracy Theories About U.S. Institutions
An early look at black voters’ views on biden, trump and election 2024, a look at black-owned businesses in the u.s., 8 facts about black americans and the news, black americans’ views on success in the u.s., most popular, report materials.
- American Trends Panel Wave 100
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
© 2024 Pew Research Center
Addressing the unprecedented behavioral-health challenges facing Generation Z
Nearly two years after the COVID-19 pandemic began in the United States, Gen Zers, ranging from middle school students to early professionals, are reporting higher rates of anxiety, depression, and distress than any other age group. 1 Ages for Generation Z can vary, with some analysis including ages as young as nine. In this article, we focus on those between the ages of 16 and 24, and define millennials as 25 to 40; Ramin Mojtabai and Mark Olfson, “National trends in mental health care for US adolescents,” JAMA Psychiatry , March 25, 2020, Volume 77, Number 7; Martin Seligman, The Optimistic Child: A Revolutionary Approach to Raising Resilient Children , Boston, MA: Mariner Books, 2007; Gen Z respondents are 1.5 times as likely to report having felt anxious or depressed, compared with the average respondent, according to the McKinsey Consumer Health Insights Survey, conducted in June 2021—a nationally representative survey of 2,906 responses, including 316 Gen Z responses. The mental-health challenges among this generation are so concerning that US surgeon general Vivek Murthy issued a public health advisory on December 7, 2021, to address the “youth mental health crisis” exacerbated by the COVID-19 pandemic. 2 Protecting youth mental health: US surgeon general’s advisory , Office of the Surgeon General, December 7, 2021.
About the authors
The article is a collaborative effort by Erica Coe , Jenny Cordina , Kana Enomoto , Raelyn Jacobson , Sharon Mei, and Nikhil Seshan, representing views of the McKinsey’s Healthcare Systems & Services and Public & Social Sector Practices.
A series of consumer surveys and interviews conducted by McKinsey indicate stark differences among generations, with Gen Z reporting the least positive life outlook, including lower levels of emotional and social well-being than older generations. One in four Gen Z respondents reported feeling more emotionally distressed (25 percent), almost double the levels reported by millennial and Gen X respondents (13 percent each), and more than triple the levels reported by baby boomer respondents (8 percent). 3 These research efforts have been focused on Gen Zers between the ages of 16 and 24 when compared with samples of millennials (aged 25 to 40), Gen Xers (aged 41 to 56), and baby boomers (aged 57 to 76). And the COVID-19 pandemic has only amplified this challenge (see sidebar, “The disproportionate impact of the COVID-19 pandemic”). While consumer surveys are, of course, subjective and Gen Z is not the only generation to experience distress, employers, educators, and public health leaders may want to consider the sentiment of this emerging generation as they plan for the future.
The disproportionate impact of the COVID-19 pandemic
While Gen Z is less vulnerable to the physical impacts of the COVID-19 pandemic, they bear unique burdens due to their life stage, including emotional stress and grief from the pandemic, high rates of job loss and unemployment, and educational challenges from remote or interrupted learning. The effects of the pandemic may be especially felt by recent college graduates, many of whom have encountered difficulties finding jobs, had their previously secured job offers rescinded, or were unable to apply to graduate school due to the timing of the lockdowns in March 2020. In April 2020, workers aged 18 to 24 faced 27 percent unemployment, with 13 percent of this segment ceasing to look for work. While employment has largely recovered, this segment has exited the workforce at twice the rate of other age groups since the start of the pandemic. The inequitable impact of the pandemic by race extends to Gen Z employment as well, where Black, Hispanic/Latino, and Asian American and Pacific Islander (AAPI) workers aged 18 to 24 faced up to 1.8 times the unemployment rates of their White counterparts. 1 McKinsey analysis of the US Census Bureau Current Population Survey as of November 2020.
In our sample, Gen Z respondents were more likely to report having been diagnosed with a behavioral-health condition (for example, mental or substance use disorder) than either Gen Xers or baby boomers. 4 Gen Z respondents were 1.4 to 2.3 times more likely to report that they had been diagnosed with a mental-health condition and 1.9 to 4.1 times more likely to be diagnosed with a substance-use disorder than both Gen Xers and baby boomers. Based on the McKinsey Consumer Behavioral Health Survey conducted in November–December 2020—a nationally representative survey of 1,523 responses, including an oversample of Gen Z respondents (aged 16 to 24, n = 874). Gen Z respondents were also two to three times more likely than other generations to report thinking about, planning, or attempting suicide in the 12-month period spanning late 2019 to late 2020.
Gen Z also reported more unmet social needs than any other generation. 5 Also referred to as social determinants of health or social needs, including income, employment, education, food, housing, transportation, social support, and safety. These basic needs, if unmet, can negatively affect health. In addition, factors such as race, ethnicity, gender and sexual orientation, disability, and age can influence health status. Fifty-eight percent of Gen Z reported two or more unmet social needs, compared with 16 percent of people from older generations. These perceived unmet social needs, including income, employment, education, food, housing, transportation, social support, and safety, are associated with higher self-reported rates of behavioral-health conditions. As indicated in a recent nationwide survey, people with poor mental health were two times as likely to report an unmet basic need as those with good mental health, and four times as likely to have three or more unmet basic needs. 6 2019 McKinsey Social Determinants of Health Survey, n = 2,010, where respondents included those with Medicare or Medicaid coverage, individuals with coverage through the individual market who had household incomes below 250 percent of the federal poverty level, and individuals who were uninsured and had household income below 250 percent of the federal poverty level.
As these young adults work to develop their resilience, Gen Zers may seek out the holistic approach to health they have come to expect, which includes physical health, behavioral health, and social needs, as future students, employees, and customers.
Characteristics of Gen Z consumers in the healthcare ecosystem
Gen Z’s specific needs suggest that improving their behavioral healthcare will require stakeholders to increase access and deliver appropriate, timely services.
Gen Z is less likely to seek help
Gen Z respondents were more likely to report having a behavioral-health diagnosis but less likely to report seeking treatment compared with other generations (Exhibit 1). For instance, Gen Z is 1.6 to 1.8 times more likely to report not seeking treatment for a behavioral-health condition than millennials. There are several factors that may account for Gen Z’s lack of seeking help: developmental stage, disengagement from their healthcare, perceived affordability, and stigma associated with mental or substance use disorders within their families and communities. 7 Before age 25, the human brain is not fully developed. Awareness of long-term consequences and the ability to curb impulsive behavior are some of the last functions to mature. Thus, adolescents and young adults, across generations and not just Gen Z, may be less likely to engage in activities such as routine or preventive healthcare. For more, see Investing in the health and well-being of young adults , Institute of Medicine and National Research Council, 2015.
Gen Z respondents identified as less engaged in their healthcare than other respondents (Exhibit 2). About two-thirds of Gen Z respondents fell into lower engagement segments of healthcare consumers, compared with one-half of respondents from other generations. Gen Z and other people in these less engaged segments reported that they feel less in control of their health and lifespan, are less health-conscious, and are less proactive about maintaining good health. One-third of Gen Z respondents fell into the least engaged segment, who reported the lowest motivation to improve their health and the least comfort talking about behavioral-health challenges with doctors. 8 Disadvantaged, disconnected users are more resigned to their health and less engaged and active in improving it. They value convenience but are often not engaged digitally.
Another driver for Gen Z’s reduced help-seeking may be the perceived affordability of mental-health services. One out of four Gen Z respondents said they could not afford mental-health services, which had the lowest perceived affordability of all services surveyed. 9 Services surveyed include healthcare, health insurance, internet services, necessary transportation, financial services, housing, and nutritious food. Across the board, Americans with mental and substance use disorders bear a disproportionate share of out-of-pocket healthcare costs for a range of reasons, including the fact that many behavioral-health providers do not accept insurance . “I found the perfect therapist for me but I couldn’t afford her, even with insurance,” said one Gen Z respondent. “The absolute biggest barrier to gaining mental-health treatment has been financial,” added another.
In addition, stigma associated with mental and substance use disorders and a lack of family support may be a substantial barrier in seeking mental healthcare. Many Gen Zers rely on parents for transportation or health insurance and may fear interacting with their parents about mental-health topics. This factor is particularly relevant for communities of color, who report perceiving a higher level of stigma associated with behavioral-health conditions. 10 Mental health: Culture, race, and ethnicity; A supplement to mental health; A report of the surgeon general , US Department of Health and Human Services, August 2001: A 1998 study cited in the supplement found that only 12 percent of Asians would mention their mental-health problems to a friend or relative (compared with 25 percent of Whites), only 4 percent of Asians would seek help from a psychiatrist or specialist (compared with 26 percent of Whites), and only 3 percent of Asians would seek help from a physician (compared with 13 percent of Whites). Children of immigrants also may internalize guilt because of their parents’ sacrifices or may have behavioral-health concerns minimized by their parents, who may state or think their children “have it much easier” than they did growing up. 11 Mental Health America , “To be the child of an immigrant,” blog entry by Kenna Chick, accessed December 1, 2021.
Gen Z relies on emergency care, social media, and digital tools when they do seek help
When they do seek support for behavioral-health issues, Gen Z may not be turning to regular outpatient mental-health services and instead may rely on emergency care, social media, and digital tools .
Gen Zers rely on acute sites of care more often than older generations, with Gen Z respondents one to four times more likely to report using the ER, and two to three times more likely to report using crisis services or behavioral-health urgent care in the past 12 months. Gen Z also makes up nearly three-quarters of Crisis Text Line’s users. 12 Everybody hurts 2020: What 48 million messages say about the state of mental health in America , Crisis Text Line, February 10, 2020. One Gen Z respondent expressed her frustration, saying, “Seems [like the] only option is an emergency room visit, otherwise I have to wait weeks to see a psychiatrist.”
Almost one in four Gen Zers also reported that it is “extremely” or “very” challenging to get help during a behavioral-health crisis. This lack of access is concerning for a generation two to three times more likely to report seeking treatment in the past 12 months for suicidal ideation or attempted suicide, than any other generation.
Many Gen Zers also indicated their first step in managing behavioral-health challenges was going to TikTok or Reddit for advice from other young people, following therapists on Instagram, or downloading relevant apps. This reliance on social media may be due, in part, to the provider shortages in many parts of the country: 64 percent of counties in the United States have a shortage of mental-health providers. Furthermore, 56 percent of counties in the United States are without a psychiatrist (corresponding to 9 percent of the total population), and 73 percent of counties are without a child and adolescent psychiatrist (corresponding to 19 percent of the total population). 13 Oleg Bestsennyy, Greg Gilbert, Alex Harris, and Jennifer Rost, “ Telehealth: A quarter-trillion-dollar post-COVID-19 reality ?,” McKinsey, July 9, 2021; Vulnerable Populations dashboard, McKinsey’s Center for Societal Benefit through Healthcare, accessed December 1, 2021.
Gen Z is less satisfied with the behavioral-health services they receive
Gen Zers say the behavioral healthcare system overall is not meeting their expectations—Gen Zers who received behavioral healthcare were less likely to report being satisfied with the services they received than other generations. For example, compared with older generations, Gen Z reports lower satisfaction with behavioral-health services received through outpatient counseling/therapy (3.7 out of 5.0 for Gen Z, compared with 4.1 for Gen X) or intensive outpatient (3.1 for Gen Z, compared with 3.8 for older generations). 14 Mean differences are significantly different, at a 90 percent confidence level. One Gen Z respondent said, “Struggling to find a psychologist whom I was comfortable with and cared enough to remember my name and what we did the week before” was the most significant barrier to care. Another said, “I have trust issues and find it difficult to talk with therapists about my problems. I also had a very bad experience with a therapist, which made this problem worse.”
Although we have seen high penetration of telehealth in psychiatry (share of telehealth outpatient and office visits claims were at 50 percent in February 2021), 15 Vulnerable Populations: Data Over Time Database, McKinsey Center for Societal Benefit through Healthcare, April 2021. Gen Z has the lowest satisfaction with tele-behavioral health (Gen Z rates their satisfaction with telehealth at a 3.8 out of 5.0, compared with older generations, who rate it 4.1) and digital app/tools (3.5 out of 5.0 for Gen Z, compared with 4.0 for older generations). 16 Mean differences are significantly different, at a 90 percent confidence level. Around telehealth, Gen Zers cited reasons for dissatisfaction such as telehealth therapy feeling “less official” or “less professional,” as well as more difficult to form a trusting connection with a therapist. For apps, Gen Z respondents noted a lack of personalization, as well as a lack of diversity—both in terms of the racial and ethnic diversity of the stories they presented, and in the problems that the apps offered tools to address. In creating and improving behavioral-health tools, it is crucial to employ a user-centered design approach to develop functionality and experiences that Gen Zers actually want.
In creating and improving behavioral-health tools, it is crucial to employ a user-centered design approach to develop functionality and experiences that Gen Zers actually want.
Gen Z cares about diversity when choosing a healthcare provider
Racial and ethnic diversity in the behavioral-health workforce is also important. According to McKinsey’s COVID-19 Consumer Survey, racial and ethnic minority respondents reported valuing racial and ethnic diversity when choosing a physician, citing their physician’s race more frequently than White respondents as a consideration. 17 Thirteen percent of Black respondents, 9 percent of Asian respondents, and 8 percent of Hispanic/Latino respondents cited their physician’s race when selecting the physicians that they see, compared with 4 percent of Whites. Because Gen Z cares deeply about diversity, there are opportunities to integrate care and early intervention by offering a more racially and ethnically diverse behavioral-health workforce and culturally relevant digital tools. 18 According to surveys conducted by the Pew Research Center, most Gen Zers see the country’s growing racial and ethnic diversity as a good thing: Ruth Igielnik and Kim Parker, “On the cusp of adulthood and facing an uncertain future: What we know about Gen Z so far,” Pew Research Center, May 14, 2020.
Potential stakeholder actions to address the needs of Generation Z
In our article “ Unlocking whole person care through behavioral health ,” we outline six potential actions integral to improving the quality of care and experience for millions with behavioral-health conditions. Many of those levers apply to Gen Z, but further tailoring is needed to best meet the needs of this emerging generation. Promising areas to explore could include the emerging role of digital and telehealth; the need for stronger community-based response to behavioral-health crises; better meeting the needs of Gen Z where they live, work, and go to school; promoting mental-health literacy; investing in behavioral health at parity with physical health; and supporting a holistic approach that embraces behavioral, physical, and social aspects of health.
Need for action now
Gen Z is our next generation of leaders, activists, and politicians; many of them have already taken on adult responsibilities as they start climate movements, lead social justice marches, and drive companies to align more closely with their values. Healthcare leaders, educators, and employers all have a role to play in supporting the behavioral health of Gen Z. By taking a tailored, generational approach to designing messages, products, and services, stakeholders can meaningfully improve the behavioral health of Gen Z and help them achieve their full potential. This investment could be viewed as a down payment on our future that will bear social and economic returns for years to come.
Erica Coe is a partner in McKinsey’s Atlanta office and coleads the Center for Societal Benefit through Healthcare, Jenny Cordina is a partner in the Detroit office and leads McKinsey’s Consumer Health Insights research, Kana Enomoto is a senior expert in the Washington, DC, office and coleads the Center for Societal Benefit through Healthcare, Raelyn Jacobson is an associate partner in the Seattle office, Sharon Mei is an expert in the New York office, and Nikhil Seshan is a consultant in the Philadelphia office.
The authors wish to thank Tamara Baer, Eric Bochtler, Emma Dorn, Erin Harding, Brad Herbig, Jimmy Sarakatsannis, and Boya Wang for their contributions to this paper.
Explore a career with us
Related articles.

How affordable is mental healthcare? The long-term impact on financial health

Unlocking whole person care through behavioral health

Children’s health during the COVID-19 pandemic: What have we learned?

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Surgeon General Issues New Advisory About Effects Social Media Use Has on Youth Mental Health
Surgeon General Dr. Vivek Murthy Urges Action to Ensure Social Media Environments are Healthy and Safe, as Previously-Advised National Youth Mental Health Crisis Continues
Today, United States Surgeon General Dr. Vivek Murthy released a new Surgeon General’s Advisory on Social Media and Youth Mental Health . While social media may offer some benefits, there are ample indicators that social media can also pose a risk of harm to the mental health and well-being of children and adolescents. Social media use by young people is nearly universal, with up to 95% of young people ages 13-17 reporting using a social media platform and more than a third saying they use social media “almost constantly.”
With adolescence and childhood representing a critical stage in brain development that can make young people more vulnerable to harms from social media, the Surgeon General is issuing a call for urgent action by policymakers, technology companies, researchers, families, and young people alike to gain a better understanding of the full impact of social media use, maximize the benefits and minimize the harms of social media platforms, and create safer, healthier online environments to protect children. The Surgeon General’s Advisory is a part of the Department of Health and Human Services’ (HHS) ongoing efforts to support President Joe Biden’s whole-of-government strategy to transform mental health care for all Americans.
“The most common question parents ask me is, ‘is social media safe for my kids’. The answer is that we don't have enough evidence to say it's safe, and in fact, there is growing evidence that social media use is associated with harm to young people’s mental health,” said U.S. Surgeon General Dr. Vivek Murthy . “Children are exposed to harmful content on social media, ranging from violent and sexual content, to bullying and harassment. And for too many children, social media use is compromising their sleep and valuable in-person time with family and friends. We are in the middle of a national youth mental health crisis, and I am concerned that social media is an important driver of that crisis – one that we must urgently address.”
Usage of social media can become harmful depending on the amount of time children spend on the platforms, the type of content they consume or are otherwise exposed to, and the degree to which it disrupts activities that are essential for health like sleep and physical activity. Importantly, different children are affected by social media in different ways, including based on cultural, historical, and socio-economic factors. Among the benefits, adolescents report that social media helps them feel more accepted (58%), like they have people who can support them through tough times (67%), like they have a place to show their creative side (71%), and more connected to what’s going on in their friends’ lives (80%).
However, social media use can be excessive and problematic for some children. Recent research shows that adolescents who spend more than three hours per day on social media face double the risk of experiencing poor mental health outcomes, such as symptoms of depression and anxiety; yet one 2021 survey of teenagers found that, on average, they spend 3.5 hours a day on social media. Social media may also perpetuate body dissatisfaction, disordered eating behaviors, social comparison, and low self-esteem, especially among adolescent girls. One-third or more of girls aged 11-15 say they feel “addicted” to certain social media platforms and over half of teenagers report that it would be hard to give up social media. When asked about the impact of social media on their body image, 46% of adolescents aged 13-17 said social media makes them feel worse, 40% said it makes them feel neither better nor worse, and only 14% said it makes them feel better. Additionally, 64% of adolescents are “often” or “sometimes” exposed to hate-based content through social media. Studies have also shown a relationship between social media use and poor sleep quality, reduced sleep duration, sleep difficulties, and depression among youth.
While more research is needed to determine the full impact social media use has on nearly every teenager across the country, children and adolescents don’t have the luxury of waiting years until we know the full extent of social media’s effects. The Surgeon General’s Advisory offers recommendations stakeholders can take to help ensure children and their families have the information and tools necessary to make social media safer for children:
- Policymakers can take steps to strengthen safety standards and limit access in ways that make social media safer for children of all ages, better protect children’s privacy, support digital and media literacy, and fund additional research.
- Technology companies can better and more transparently assess the impact of their products on children, share data with independent researchers to increase our collective understanding of the impacts, make design and development decisions that prioritize safety and health – including protecting children’s privacy and better adhering to age minimums – and improve systems to provide effective and timely responses to complaints.
- Parents and caregivers can make plans in their households such as establishing tech-free zones that better foster in-person relationships, teach kids about responsible online behavior and model that behavior, and report problematic content and activity.
- Children and adolescents can adopt healthy practices like limiting time on platforms, blocking unwanted content, being careful about sharing personal information, and reaching out if they or a friend need help or see harassment or abuse on the platforms.
- Researchers can further prioritize social media and youth mental health research that can support the establishment of standards and evaluation of best practices to support children’s health.
In concert with the Surgeon General’s Advisory, leaders at six of the nation’s medical organizations have expressed their concern on social media’s effects on youth mental health:
“Social media can be a powerful tool for connection, but it can also lead to increased feelings of depression and anxiety – particularly among adolescents. Family physicians are often the first stop for parents and families concerned about the physical and emotional health of young people in their lives, and we confront the mental health crisis among youth every day. The American Academy of Family Physicians commends the Surgeon General for identifying this risk for America's youth and joins our colleagues across the health care community in equipping young people and their families with the resources necessary to live healthy, balanced lives.” – Tochi Iroku-Malize, M.D., MPH, MBA, FAAFP, President, American Academy of Family Physicians
“Today’s children and teens do not know a world without digital technology, but the digital world wasn’t built with children’s healthy mental development in mind. We need an approach to help children both on and offline that meets each child where they are while also working to make the digital spaces they inhabit safer and healthier. The Surgeon General’s Advisory calls for just that approach. The American Academy of Pediatrics looks forward to working with the Surgeon General and other federal leaders on Youth Mental Health and Social Media on this important work.” – Sandy Chung, M.D., FAAP, President, American Academy of Pediatrics
“With near universal social media use by America’s young people, these apps and sites introduce profound risk and mental health harms in ways we are only now beginning to fully understand. As physicians, we see firsthand the impact of social media, particularly during adolescence – a critical period of brain development. As we grapple with the growing, but still insufficient, research and evidence in this area, we applaud the Surgeon General for issuing this important Advisory to highlight this issue and enumerate concrete steps stakeholders can take to address concerns and protect the mental health and wellbeing of children and adolescents.We continue to believe in the positive benefits of social media, but we also urge safeguards and additional study of the positive and negative biological, psychological, and social effects of social media.”— Jack Resneck Jr., M.D., President, American Medical Association
“The first principle of health care is to do no harm – that’s the same standard we need to start holding social media platforms to. As the Surgeon General has pointed out throughout his tenure, we all have a role to play in addressing the youth mental health crisis that we now face as a nation. We have the responsibility to ensure social media keeps young people safe. And as this Surgeon General’s Advisory makes clear, we as physicians and healers have a responsibility to be part of the effort to do so.” – Saul Levin, M.D., M.P.A., CEO and Medical Director, American Psychiatric Association
“The American Psychological Association applauds the Surgeon General's Advisory on Social Media and Youth Mental Health, affirming the use of psychological science to reach clear-eyed recommendations that will help keep our youth safe online. Psychological research shows that young people mature at different rates, with some more vulnerable than others to the content and features on many social media platforms. We support the advisory's recommendations and pledge to work with the Surgeon General's Office to help build the healthy digital environment that our kids need and deserve.” – Arthur Evans, Jr., Ph.D., Chief Executive Officer and Executive Vice President, American Psychological Association.
“Social media use by young people is pervasive. It can help them, and all of us, live more connected lives – if, and only if, the appropriate oversight, regulation and guardrails are applied. Now is the moment for policymakers, companies and experts to come together and ensure social media is set up safety-first, to help young users grow and thrive. The Surgeon General’s Advisory about the effects of social media on youth mental health issued today lays out a roadmap for us to do so, and it’s critical that we undertake this collective effort with care and urgency to help today’s youth.” – Susan L. Polan, Ph.D., Associate Executive Director, Public Affairs and Advocacy, American Public Health Association
The National Parent Teacher Association shared the following:
“Every parent’s top priority for their child is for them to be happy, healthy and safe. We have heard from families who say they need and want information about using social media and devices. This Advisory from the Surgeon General confirms that family engagement on this topic is vital and continues to be one of the core solutions to keeping children safe online and supporting their mental health and well-being.” – Anna King, President of the National Parent Teacher Association .
In December 2021, Dr. Murthy issued a Surgeon General’s Advisory on Protecting Youth Mental Health calling attention to our national crisis of youth mental health and well-being. Earlier this month, he released a Surgeon General’s Advisory on Our Epidemic of Loneliness and Isolation , where he outlined the profound health consequences of social disconnection and laid out six pillars to increase connection across the country, one of which being the need to reform our digital environments. The new Surgeon General’s Advisory on Social Media and Youth Mental Health is a continuation of his work to enhance the mental health and well-being of young people across the country.
The full Surgeon General’s Advisory can be read here . For more information about the Office of the Surgeon General, visit www.surgeongeneral.gov/priorities .
Sign Up for Email Updates
Receive the latest updates from the Secretary, Blogs, and News Releases
Subscribe to RSS
Receive latest updates

Related News Releases
Biden-harris administration expands access to mental health and substance use services with addition of 10 new states to ccbhc medicaid demonstration program, readout of federal interagency working group on arts, health, and civic infrastructure meeting, hhs mental health accomplishments by the numbers, related blog posts.

The HHS Office for Civil Rights Celebrates National Recovery Month
Media inquiries.
For general media inquiries, please contact [email protected] .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J MCH AIDS
- v.9(1); 2020

Current and Emerging Issues in Global Health: An Introduction to Special Journal Collection
Hamisu m. salihu.
1 Center of Excellence in Health Equity, Training and Research, Baylor College of Medicine, 3701 Kirby Drive, 700 Houston, Texas 77098, USA
Romuladus E. Azuine
2 The Center for Global Health and Health Policy, Global Health and Education Projects, Inc., P. O. Box 234, Riverdale, Maryland 20738, USA
We are thrilled to present this special collection of articles entitled “ Current and Emerging Issues in Global Health .” This special collection pursued three main goals. First, the collection presents an opportunity for innovation. Second, it presents an opportunity to engage the field and community around a common theme. Finally, the collection provides a reality-check for the journal editors to support the field in evaluating the extent to which we have collectively attempted to confront the global maternal and child health (MCH) issues of our time regardless of where in the world we live. Unique to this special collection is the geographical spread of the article submissions. We have articles and contributions from researchers and research groups from three continents in a single edition: Africa, Asia and North America, making the articles opportunities for cross-fertilization of ideas across the global North and South. Public health is passing through a seismic transformation. Whether at the global, national, state, and local levels, disease outbreaks, patient demographics, and health technology have changed the global health landscape in a way never imagined. Our hope is that papers in this special collection will spark new ideas for invention, improved patient care, and transform population health.
We are thrilled to present this special collection of articles on “Current and Emerging Issues in Global Health.” Over the last six months when the call for papers for this special collection was issued, the field of global maternal and child health (MCH) and HIV/AIDS has been agog with interest. The support from leading researchers, graduate students, pre-and-post-doctoral researchers from far and near bore testimony on the need for a curated, cutting-edge, collection of peer-reviewed articles around a common and shared theme. The International Journal of Maternal and Child Health and AIDS (IJMA) is an applied and translational global health journal; so the idea of a special collection is at the center of the journal’s global health mission and objectives. 1 The collection captures three main goals for the journal. First, it presents an opportunity for innovation; second, it presents an opportunity to engage the field and community around a common theme; and finally, it is a moment of reality-check for the journal editors to support the field in evaluating the extent to which we have collectively attempted to confront the global MCH issues of our time.
The idea of a special journal collection on emerging global health issues was timely. At the beginning of 2019, the World Health Organization (WHO) released a list of 10 threats to global health for the year. 2 They include: (1) air pollution and climate change, (2) non-communicable diseases, (3) threat of a global influenza pandemic, (4) fragile and vulnerable settings, such as regions affected by drought and conflict, (5) antimicrobial resistance, (6) Ebola and high-threat pathogens, (7) weak primary care, (8) vaccine hesitancy, (9) Dengue, and (10) Human immunodeficiency virus (HIV).
Each of the above global threats is real, far-reaching, and supported by overwhelming data and evidence. Few examples. Climate change, natural and human-made health stressors, influence human health and disease in multiple ways. The health effects of climate change include increased respiratory and cardiovascular disease, injuries and premature deaths related to extreme weather events, changes in the prevalence and geographical distribution of food- and water-borne illnesses and other infectious diseases, and threats to mental health. 3 An American Academy of Pediatrics’ primary care research network study reported that almost 12% of caregivers had moderate or high vaccine hesitancy and that a high proportion of caregivers held inaccurate beliefs about vaccines. 4 These are but a few of the real issues confronting global health.
Public health is passing through a seismic transformation. Whether at the global, national, state, and local levels, disease outbreaks, patient demographics, and health technology have changed the global health landscape in a way never imagined. Diverse health outbreaks have transformed global health. There is no doubt that shifting boundaries, ennobled by migration, have lifted the boundaries for disease outbreaks, such as Ebola, Zika virus, measles, and the pandemic flu. 5 From Avian Flu, to Zika, to drug-resistant bacteria, the world faces a host of dangerous pathogens and potential epidemics. 5 Consequently, public health is now center-stage at national security discourses culminating in the burgeoning field of global health security preparedness. With about 70% of the world’s countries not fully prepared for an outbreak, it is evident that we face dangerous gaps in public health systems across the globe. 5
In total realization of these changing landscapes, we now have a cadre of public health professionals who found themselves engaging a changed demographics like never before. Demographic shifts and societal changes are intensifying pressures on health systems and demanding new directions in the delivery of healthcare. 6 In addition, aging populations in both emerging and developed nations are driving up the demand for healthcare. Health care professionals, unlike ever known in history, now agree that the “patient is king.” The “Google-ennobled patients” come to medical visits armed with questions for their healthcare practitioners making dialogue and a meeting of the minds inevitable. Given that all information is not always accurate, evidence-informed, or simply ready for patient consumption, the healthcare professional goes the extra mile of further empowering the patient with accurate information and bursts prevalent myths and misinformation. The empowered-patient-era has led to the realization that one-size-fits-all no longer suffices. It bears testimony to the long-held aspirations for precision medicine and precision healthcare practice that addresses the needs of patients according to their individual circumstances, which is pertinent in accelerating biomedical research and improving population health and health disparities. 7 The Google-ennobled patient is but one of the realities of technological incursion into healthcare presenting phenomenal opportunities but significant unanswered questions that warrant continued investigations.
The purpose of the special collection was to highlight and support emerging scientific innovations in the fields of global MCH and HIV/AIDS. The articles in the special collection lived up to this goal. They are diverse and make for a good reading touching on a wide range of contemporary topics dealing with issues that directly or indirectly influence MCH populations or people living with HIV/AIDS. Accordingly, we have high-quality articles that discuss childhood obesity and their social determinants; maternal and feto-infant survival in both developing (Nigeria, India and Malawi) and in developed (United States) settings. The role of the father during pregnancy, a concept that is increasingly gaining acceptance as an essential ingredient for favorable pregnancy outcomes, is also highlighted in this edition. Articles on HIV/AIDS report findings regarding two very important issues that determine success or failure of current efforts toward control of the HIV epidemic: stigma and HIV vaccine. The article by Aliyu et al., for example, demonstrates that stigma prevented sufficient adherence to anti-retroviral treatment among pregnant women enrolled in a prevention of mother to child transmission (PMTCT) trial in rural North Central Nigeria. A paper by Alio et al. explores factors that could influence HIV vaccine acceptance among black men and transgender persons in Western New York. Unique to this special collection is the geographical spread of the article submissions. We have articles and contributions from research groups from three continents in a single edition: Africa, Asia and North America.
Our profound gratitude goes to the editorial management and support teams in Washington, DC led by Mr. Brownmagnus U. Olivers for their diligence and indefatigable work in helping us make this special collection a reality. We thank all our authors for their painstaking commitment in addressing the multiple reviews from the guardianship of Guest Editor Dr. Salihu to assemble a profound collection of papers that will stand the test of time and challenge existing paradigms in global health policy and practice. Our ultimate hope is that papers in this collection spark new ideas for invention, improved patient care, and transformation of population health. We are grateful to reviewers for their diligence and support of this special collection. We invite you to enjoy the read. We look forward to receiving your letters and comments on the papers in this collection.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
March 14, 2023
Erythritol and cardiovascular events
At a glance.
- Higher blood levels of the artificial sweetener erythritol were associated with increased risk of heart attack and stroke.
- The results highlight the need for further study of erythritol’s long-term risks for cardiovascular health.

Artificial sweeteners have become a widespread way to reduce sugar and calorie intake. Regulatory agencies generally consider artificial sweeteners to be safe. But little is known about their long-term health consequences. Growing evidence points to a link between certain artificial sweeteners and cardiovascular problems. But the connection hasn’t yet been proven.
Erythritol is a common artificial sweetener. Low amounts occur naturally in fruits and vegetables. It is also made inside our cells as part of normal metabolism. But when used as a sweetener, erythritol levels are typically more than 1,000-fold greater than levels found naturally in foods. Erythritol is in an ingredient category called “sugar alcohols,” which are not required to be listed individually on Nutrition Facts labels.
An NIH-funded research team led by Dr. Stanley Hazen at the Cleveland Clinic examined the relationship between erythritol and heart attacks and stroke. In an initial study with more than 1,000 people, the team looked for compounds in blood whose levels were linked to future cardiac risk. They tracked major adverse cardiovascular events over three years, including death and nonfatal heart attack or stroke. Results appeared in Nature Medicine on February 27, 2023.
The team found that elevated levels of erythritol and several related artificial sweeteners were associated with the risk for cardiovascular events. To confirm this result, the researchers examined two more groups of people in the U.S. and Europe totaling almost 3,000. They also developed a method to better distinguish erythritol from related compounds.
These measurements reproduced the association between erythritol and cardiovascular events. People with the highest erythritol levels (top 25%) were about twice as likely to have cardiovascular events over three years of follow-up as those with the lowest (bottom 25%).
Next, the team wanted to better understand how erythritol might increase these health risks. So, they exposed human platelets, which control blood clotting, to erythritol. Doing so increased the platelets’ sensitivity to blood clotting signals. Increasing blood erythritol levels also sped up blood clot formation and artery blockage in mice.
The scientists next asked how diet affects erythritol levels in people. To find out, they measured blood erythritol levels in eight healthy volunteers after drinking a beverage sweetened with erythritol. Blood erythritol levels increased 1,000-fold and remained substantially elevated for several days. For at least two days, the erythritol levels grew more than high enough to trigger changes in platelet function.
These results suggest that consuming erythritol can increase blood clot formation. This, in turn, could increase the risk of heart attack or stroke. Given the prevalence of erythritol in artificially sweetened foods, further safety studies of the health risks of erythritol are warranted.
“Sweeteners like erythritol have rapidly increased in popularity in recent years, but there needs to be more in-depth research into their long-term effects,” Hazen says. “Cardiovascular disease builds over time, and heart disease is the leading cause of death globally. We need to make sure the foods we eat aren’t hidden contributors.”
—by Brian Doctrow, Ph.D.
Related Links
- Gut Cells Distinguish Between Sugar and Artificial Sweeteners
- Irregular Sleep Patterns May Raise Risk of Heart Disease
- Stress Links Poverty to Inflammation and Heart Disease
- Prescribing Healthy Foods Could Bring Cost-Effective Benefits
- Eating Red Meat Daily Triples Heart Disease-Related Chemical
- How Dietary Factors Influence Disease Risk
- Healthy Body, Happy Heart: Improve Your Heart Health
- Coronary Heart Disease
- The Heart Truth®
References: The artificial sweetener erythritol and cardiovascular event risk. Witkowski M, Nemet I, Alamri H, Wilcox J, Gupta N, Nimer N, Haghikia A, Li XS, Wu Y, Saha PP, Demuth I, König M, Steinhagen-Thiessen E, Cajka T, Fiehn O, Landmesser U, Tang WHW, Hazen SL. Nat Med . 2023 Feb 27. doi: 10.1038/s41591-023-02223-9. Online ahead of print. PMID: 36849732.
Funding: NIH’s National Heart, Lung, and Blood Institute (NHLBI) and Office of Dietary Supplements (ODS); Leducq Foundation; Deutsche Forschungsgemeinschaft; Charité—Universitätsmedizin Berlin; Berlin Institute of Health; Sanofi-Aventis Deutschland GmbH; American Heart Association.
Connect with Us
- More Social Media from NIH
Racism can spark depression and anxiety in Black adolescents, study finds
Studies of brain activity suggest that the way Black youths cope with racial discrimination can affect their mental health.
Black adolescents’ experiences with racial discrimination may put them at higher risk of depression and anxiety, according to a study published this week in JAMA Network Open that sheds light on the long-term impact of racism.
The study from researchers at the University of Georgia calls attention to the complex ways in which Black youths process and respond to discrimination. Its findings can potentially improve the resources designed to help Black adolescents cope with racism.
Assaf Oshri, lead author of the study, is an associate professor whose research focuses on child development. He and his team pulled data from the Adolescent Brain Cognitive Development Study , a nationwide project funded by the National Institutes of Health that collects data on children’s health and brain development. Oshri and his colleagues analyzed data from more than 1,500 participants, gathered over three years.
“We know discriminatory experiences are associated with a range of negative health outcomes,” Oshri said. “This study is showing that some brain patterns that are trying to process threats … can help [participants] cope with these types of experiences, but there might be an emotional toll.”
By studying the amygdala — the emotion center of the brain — the authors were able to better understand the role it plays in Black youths’ responses to threats such as racism.
The amygdala’s activity was assessed using data collected during functional MRIs, widely known as fMRIs. During fMRI scans, participants were shown neutral and negative facial expressions — a commonly used test in neuroscience known as the Emotional N-Back Task. The test can simulate how participants respond to negative stimuli.
The authors also evaluated surveys in which Black adolescents self-reported experiences with racial discrimination and categorized their behaviors.
If a participant indicated on a survey that they were feeling scared or anxious, or sad or depressed, the researchers noted these feelings as internalizing symptoms, which are inner problems a person can face. If a participant noted they argued frequently or threw temper tantrums, Oshri and his team categorized these behaviors as externalizing symptoms, which are problems that present outwardly and affect the individual and people around them.
Internalizing and externalizing symptoms can tell researchers how participants are responding to stressors in their environment.
Taking the brain and survey data together, Oshri and his team found a correlation between youths whose amygdala shut down in response to negative stimuli and increased reporting of internalizing symptoms — including anxiety and depression.
Many of those adolescents also expressed feelings of marginalization in their surveys and fewer externalizing symptoms. The authors noticed these trends in about 1 in every 5 participants. So, while some youths may be less likely to act out in response to stressors, they might be at a higher risk of internalizing them and feeling sad or anxious as a result.
The amygdala shutting down in response to negative stimuli may be the brain’s way of protecting Black adolescents when they confront discrimination, though it may also be a sign of avoidant coping, which can harm their mental health over time.
“There’s a lot of implications,” Oshri said. He highlighted the importance of using data to document that “discriminatory experiences are harming our children and [their] development.”
Ryan DeLapp agreed. DeLapp, who was not involved in the study, is a psychologist and the creator of the Racial, Ethnic, and Cultural Healing program , which is designed to help youths of color navigate and heal from experiences with racial discrimination.
“Looking at biological data can further substantiate what has been shown for decades, [which is] that individuals are significantly impacted by these experiences,” DeLapp said. He added that quantitative studies should not stand alone: “These studies are needed in addition to … anecdotes of people’s lived experiences.”
Howard Stevenson, professor of Africana studies at the University of Pennsylvania, said scientific studies influence and inform intervention strategies all the time, including his own as a leader in the field of intervention work. He spearheads the Racial Empowerment Collaborative , a training and research center that explores how racism affects people’s lives.
Stevenson, who was not involved in the University of Georgia study, said that work such as Oshri’s shows why mindfulness is an important practice to teach youths, especially youths of color who are likely to experience discrimination.
“That’s like vitamins for your amygdala,” Stevenson said. Much like Oshri’s findings, Stevenson emphasized the importance of adolescents acknowledging their feelings rather than constantly suppressing them.
“The practice of noticing what’s happening to your body, thoughts and feelings” is central to intervention work, Stevenson said.

Common Comorbidities with Substance Use Disorders Research Report Part 1: The Connection Between Substance Use Disorders and Mental Illness
Many individuals who develop substance use disorders (SUD) are also diagnosed with mental disorders, and vice versa. 2,3 Although there are fewer studies on comorbidity among youth, research suggests that adolescents with substance use disorders also have high rates of co-occurring mental illness; over 60 percent of adolescents in community-based substance use disorder treatment programs also meet diagnostic criteria for another mental illness. 4
Data show high rates of comorbid substance use disorders and anxiety disorders—which include generalized anxiety disorder, panic disorder, and post-traumatic stress disorder. 5–9 Substance use disorders also co-occur at high prevalence with mental disorders, such as depression and bipolar disorder, 6,9–11 attention-deficit hyperactivity disorder (ADHD), 12,13 psychotic illness, 14,15 borderline personality disorder, 16 and antisocial personality disorder. 10,15 Patients with schizophrenia have higher rates of alcohol, tobacco, and drug use disorders than the general population. 17 As Figure 1 shows, the overlap is especially pronounced with serious mental illness (SMI). Serious mental illness among people ages 18 and older is defined at the federal level as having, at any time during the past year, a diagnosable mental, behavior, or emotional disorder that causes serious functional impairment that substantially interferes with or limits one or more major life activities. Serious mental illnesses include major depression, schizophrenia, and bipolar disorder, and other mental disorders that cause serious impairment. 18 Around 1 in 4 individuals with SMI also have an SUD.
Data from a large nationally representative sample suggested that people with mental, personality, and substance use disorders were at increased risk for nonmedical use of prescription opioids. 19 Research indicates that 43 percent of people in SUD treatment for nonmedical use of prescription painkillers have a diagnosis or symptoms of mental health disorders, particularly depression and anxiety. 20
Youth—A Vulnerable Time
Although drug use and addiction can happen at any time during a person’s life, drug use typically starts in adolescence, a period when the first signs of mental illness commonly appear. Comorbid disorders can also be seen among youth. 21–23 During the transition to young adulthood (age 18 to 25 years), people with comorbid disorders need coordinated support to help them navigate potentially stressful changes in education, work, and relationships. 21
Drug Use and Mental Health Disorders in Childhood or Adolescence Increases Later Risk
The brain continues to develop through adolescence. Circuits that control executive functions such as decision making and impulse control are among the last to mature, which enhances vulnerability to drug use and the development of a substance use disorder. 3,24 Early drug use is a strong risk factor for later development of substance use disorders, 24 and it may also be a risk factor for the later occurrence of other mental illnesses. 25,26 However, this link is not necessarily causative and may reflect shared risk factors including genetic vulnerability, psychosocial experiences, and/or general environmental influences. For example, frequent marijuana use during adolescence can increase the risk of psychosis in adulthood, specifically in individuals who carry a particular gene variant. 26,27
It is also true that having a mental disorder in childhood or adolescence can increase the risk of later drug use and the development of a substance use disorder. Some research has found that mental illness may precede a substance use disorder, suggesting that better diagnosis of youth mental illness may help reduce comorbidity. One study found that adolescent-onset bipolar disorder confers a greater risk of subsequent substance use disorder compared to adult-onset bipolar disorder. 28 Similarly, other research suggests that youth develop internalizing disorders, including depression and anxiety, prior to developing substance use disorders. 29
Untreated Childhood ADHD Can Increase Later Risk of Drug Problems
Numerous studies have documented an increased risk for substance use disorders in youth with untreated ADHD, 13,30 although some studies suggest that only those with comorbid conduct disorders have greater odds of later developing a substance use disorder. 30,31 Given this linkage, it is important to determine whether effective treatment of ADHD could prevent subsequent drug use and addiction. Treatment of childhood ADHD with stimulant medications such as methylphenidate or amphetamine reduces the impulsive behavior, fidgeting, and inability to concentrate that characterize ADHD. 32
That risk presents a challenge when treating children with ADHD, since effective treatment often involves prescribing stimulant medications with addictive potential. Although the research is not yet conclusive, many studies suggest that ADHD medications do not increase the risk of substance use disorder among children with this condition. 31,32 It is important to combine stimulant medication for ADHD with appropriate family and child education and behavioral interventions, including counseling on the chronic nature of ADHD and risk for substance use disorder. 13,32
Advertisement
Supported by
Ozempic Cuts Risk of Chronic Kidney Disease Complications, Study Finds
A major clinical trial showed such promising results that the drug’s maker halted it early.
- Share full article

By Dani Blum
Dani Blum has reported on Ozempic and similar drugs since 2022.
Semaglutide, the compound in the blockbuster drugs Ozempic and Wegovy , dramatically reduced the risk of kidney complications, heart issues and death in people with Type 2 diabetes and chronic kidney disease in a major clinical trial, the results of which were published on Friday. The findings could transform how doctors treat some of the sickest patients with chronic kidney disease, which affects more than one in seven adults in the United States but has no cure.
“Those of us who really care about kidney patients spent our whole careers wanting something better,” said Dr. Katherine Tuttle, a professor of medicine at the University of Washington School of Medicine and an author of the study. “And this is as good as it gets.” The research was presented at a European Renal Association meeting in Stockholm on Friday and simultaneously published in The New England Journal of Medicine .
The trial, funded by Ozempic maker Novo Nordisk, was so successful that the company stopped it early . Dr. Martin Holst Lange, Novo Nordisk’s executive vice president of development, said that the company would ask the Food and Drug Administration to update Ozempic’s label to say it can also be used to reduce the progression of chronic kidney disease or complications in people with Type 2 diabetes.
Diabetes is a leading cause of chronic kidney disease, which occurs when the kidneys don’t function as well as they should. In advanced stages, the kidneys are so damaged that they cannot properly filter blood. This can cause fluid and waste to build up in the blood, which can exacerbate high blood pressure and raise the risk of heart disease and stroke, said Dr. Subramaniam Pennathur, the chief of the nephrology division at Michigan Medicine.
The study included 3,533 people with kidney disease and Type 2 diabetes, about half of whom took a weekly injection of semaglutide, and half of whom took a weekly placebo shot.
Researchers followed up with participants after a median period of around three and a half years and found that those who took semaglutide had a 24 percent lower likelihood of having a major kidney disease event, like losing at least half of their kidney function, or needing dialysis or a kidney transplant. There were 331 such events among the semaglutide group, compared with 410 in the placebo group.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Common sugar substitute linked to increased risk of heart attack and stroke
The safety of sugar substitutes is once again being called into question.
Researchers led by the Cleveland Clinic linked the low-calorie sugar substitute xylitol to an increased risk of heart attack, stroke or cardiovascular-related deaths, according to a study published today in the European Heart Journal.
Xylitol is a sugar alcohol that is found in small amounts in fruit and vegetables, and the human body also produces it. As an additive, it looks and tastes like sugar but has 40% fewer calories. It is used, at much higher concentrations than found in nature, in sugar-free gum, candies, toothpaste and baked goods. It can also be found in products labeled "keto-friendly," particularly in Europe.
The same research team found a similar association last year to the popular sugar substitute erythritol. The use of sugar substitutes has increased significantly over the past decade as concerns about rising obesity rates mount.
“We’re throwing this stuff into our food pyramid, and the very people who are most likely to be consuming it are the ones who are most likely to be at risk” of heart attack and stroke, such as people with diabetes, said lead author Dr. Stanely Hazen, chair of cardiovascular and metabolic sciences at Cleveland Clinic’s Lerner Research Institute.
Latest heart health news
- How a surge of anger could raise your risk of heart attack.
- A stealthy cholesterol is killing people and most don't know they have it.
- 'Surprisingly' high number of adults, even younger ones, in the U.S. are at risk of a heart syndrome.
Many heart attacks and strokes occur in people who do not have known risk factors, like diabetes, high blood pressure or elevated cholesterol levels. The research team began studying sugar alcohols found naturally in the human body to see if the compounds might predict cardiovascular risk in these people.
In the study, the investigators measured the level of naturally occurring xylitol in the blood of more than 3,000 participants after overnight fasting. They found that people whose xylitol levels put them in the top 25% of the study group had approximately double the risk for heart attack, stroke or death over the next three years compared to people in the bottom quarter.
The researchers also wanted to understand the mechanism at work, so they fed xylitol to mice, added it to blood and plasma in a lab and gave a xylitol-containing drink to 10 healthy volunteers. In all these cases, xylitol seemed to activate platelets, which are the blood component that controls clotting, said Hazen. Blood clots are the leading cause of heart attack and stroke.
“All it takes is xylitol to interact with platelets alone for a very brief period of time, a matter of minutes, and the platelet becomes supercharged and much more prone to clot,” Hazen said.
The next question is what causes naturally-occurring xylitol to be elevated in some people and how do you lower it, said Dr. Sadiya Khan, a cardiologist at Northwestern Medicine Bluhm Cardiovascular Institute and a professor of cardiovascular epidemiology at Northwestern Feinberg School of Medicine who was not involved in the new study.
Much more research needs to be done, said Hazen. In the meantime, he is telling patients to avoid eating xylitol and other sugar alcohols, whose spelling all end in ‘itol.’ Instead, he recommends using modest amounts of sugar, honey or fruit to sweeten food, adding that toothpaste and one stick of gum are probably not a problem because so little xylitol is ingested.
The report had key limitations.
First, the study of naturally occurring xylitol in people’s blood was observational and can show only an association between the sugar alcohol and heart risk. It does not show that xylitol caused the higher incidence of heart attack, stroke or death.
Nevertheless, given the totality of the evidence presented in the paper, “it’s probably reasonable to limit intake of artificial sweeteners,” said Khan. “Perhaps the answer isn’t replacing sugar with artificial sweeteners but thinking about more high quality dietary components, like vegetables and fruits, as natural sugars.”
Artificial sweeteners shouldn’t be difficult to avoid, said Joanne Slavin, PhD, RDN, a professor of food science and nutrition at the University of Minnesota-Twin Cities. They are listed on the ingredient list of packaged goods.
“Would I say never eat xylitol?” asked Slavin, who had no connection to the study. For some people who struggle to reduce sugar in their diet, sugar substitutes are one tool, and it comes down to personal choice, she said.
While Slavin found the study interesting and cause for some concern, she noted that sugar alcohols are expensive and are generally used in very small amounts in gum and sugar-free candies.
Another limitation of the study is that the participants whose xylitol levels in the blood were measured were at high risk for or had documented heart disease, and so the results may not apply to healthy individuals.
Still, many people in the general public share the characteristics of the study participants, said Hazen.
“In middle-aged or older America, it’s common to have obesity and diabetes or high cholesterol or high blood pressure,” he said.
Barbara Mantel is an NBC News contributor. She is also the topic leader for freelancing at the Association of Health Care Journalists, writing blog posts, tip sheets and market guides, as well as producing and hosting webinars. Barbara’s work has appeared in CQ Researcher, AARP, Undark, Next Avenue, Medical Economics, Healthline, Today.com, NPR and The New York Times.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.
Testing fitness of aging brain

DNR orders for Down syndrome patients far exceeded pandemic norm

Researchers reverse hair loss caused by alopecia

Women who follow Mediterranean diet live longer
Large study shows benefits for cancer, cardiovascular mortality, also identifies likely biological drivers of better health
BWH Communications
In a study that followed more than 25,000 U.S. women for up to 25 years, researchers from Harvard-affiliated Brigham and Women’s Hospital found that participants who closely followed the Mediterranean diet had up to a 23 percent lower risk of all-cause mortality, with benefits for both cancer and cardiovascular health. The researchers found evidence of biological changes that may help explain the longevity gains. Results are published in JAMA.
“For women who want to live longer, our study says watch your diet,” said senior author Samia Mora , a cardiologist and a professor of medicine at Harvard Medical School. “Following a Mediterranean dietary pattern could result in about one-quarter reduction in risk of death over more than 25 years with benefit for both cancer and cardiovascular mortality, the top causes of death in women and men in the U.S. and globally.”
The Mediterranean diet is rich in plants (nuts, seeds, fruits, vegetables, whole grains, legumes). The main fat is olive oil, usually extra-virgin. The regimen includes moderate intake of fish, poultry, dairy, eggs, and alcohol, and rare consumption of meats, sweets, and processed foods.
The authors of the current study investigated the long-term benefit of adherence to a Mediterranean diet in a U.S. population recruited as part of the Women’s Health Study , and illuminated biological mechanisms that may explain the diet’s health benefits. Investigators evaluated a panel of approximately 40 biomarkers representing various biological pathways and clinical risk factors.
Biomarkers of metabolism and inflammation were most important, followed by triglyceride-rich lipoproteins, adiposity, and insulin resistance.
“Our research provides significant public health insight: Even modest changes in established risk factors for metabolic diseases — particularly those linked to small-molecule metabolites, inflammation, triglyceride-rich lipoproteins, obesity, and insulin resistance — can yield substantial long-term benefits from following a Mediterranean diet,” said lead author Shafqat Ahmad , an associate professor of epidemiology at Uppsala University Sweden and a researcher in the Center for Lipid Metabolomics and the Division of Preventive Medicine at the Brigham.
The authors noted some key limitations of the study, including that it was limited to middle-aged and older, well-educated female health professionals who were predominantly non-Hispanic and white. The study relied on food-frequency questionnaires and other self-reported measures, such as height, weight, and blood pressure. But the study’s strengths include its large scale and long follow-up period.
The authors also note that as the concept of the Mediterranean diet has gained popularity, the diet has been adapted in different countries and cultures.
“The health benefits of the Mediterranean diet are recognized by medical professionals, and our study offers insights into why the diet may be so beneficial,” said Mora. “Public health policies should promote the healthful dietary attributes of the Mediterranean diet and should discourage unhealthy adaptations.”
The Women’s Health Study is supported by the National Institutes of Health. More information on funding for individual researchers here .
Get the best of the Gazette delivered to your inbox
By subscribing to this newsletter you’re agreeing to our privacy policy
Share this article
You might like.
Most voters back cognitive exams for older politicians. What do they measure?

Co-author sees need for additional research and earlier, deeper conversations around care

Treatment holds promise for painlessly targeting affected areas without weakening immune system
Bringing back a long extinct bird
Scientists sequence complete genome of bush moa, offering insights into its natural history, possible clues to evolution of flightless birds
More than a planetary fender-bender
New study finds Earth collided with dense interstellar cloud, possibly affecting life on planet
Alzheimer’s disease indicators track with biological changes in brain, study finds
Researchers see self-reported memory loss may be early, preclinical warning
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Weight Management
- Understanding Adult Overweight & Obesity
- Health Risks
- Español
Health Risks of Overweight & Obesity
In this section:
Type 2 diabetes
High blood pressure, heart disease, metabolic syndrome, fatty liver diseases, some cancers, breathing problems, osteoarthritis, diseases of the gallbladder and pancreas, kidney disease, pregnancy problems, fertility problems, sexual function problems, mental health problems.
Overweight and obesity may increase your risk for many health problems—especially if you carry extra fat around your waist. Reaching and staying at a healthy weight can help prevent these problems, stop them from getting worse, or even make them go away.
Type 2 diabetes is a disease that occurs when your blood glucose , also called blood sugar, is too high. Nearly 9 in 10 people with type 2 diabetes have overweight or obesity. 12 Over time, high blood glucose can lead to heart disease , stroke, kidney disease , eye problems , nerve damage , and other health problems .
If you are at risk for type 2 diabetes, you may be able to prevent or delay diabetes by losing at least 5% to 7% of your starting weight. 13,14 For instance, if you weigh 200 pounds, your goal would be to lose about 10 to 14 pounds.

High blood pressure , also called hypertension, is a condition in which blood flows through your blood vessels with a force greater than normal. Having a large body size may increase blood pressure because your heart needs to pump harder to supply blood to all your cells. Excess fat may also damage your kidneys , which help regulate blood pressure.
High blood pressure can strain your heart, damage blood vessels, and raise your risk of heart attack , stroke , kidney disease , and death. 10 Losing enough weight to reach a healthy body mass index range may lower high blood pressure and prevent or control related health problems.
Heart disease is a term used to describe several health problems that affect your heart, such as a heart attack , heart failure , angina , or an abnormal heart rhythm. Having overweight or obesity increases your risk of developing conditions that can lead to heart disease, such as high blood pressure, high blood cholesterol , and high blood glucose. In addition, excess weight can also make your heart have to work harder to send blood to all the cells in your body. Losing excess weight may help you lower these risk factors for heart disease.
A stroke happens when a blood vessel in your brain or neck is blocked or bursts, cutting off blood flow to a part of your brain. A stroke can damage brain tissue and make you unable to speak or move parts of your body.
Overweight and obesity are known to increase blood pressure—and high blood pressure is the leading cause of strokes. Losing weight may help you lower your blood pressure and other risk factors for stroke, including high blood glucose and high blood cholesterol.
Metabolic syndrome is a group of conditions that increase your risk for heart disease, diabetes , and stroke. To be diagnosed with metabolic syndrome, you must have at least three of the following conditions
- large waist size
- high level of triglycerides in your blood
- high blood pressure
- high level of blood glucose when fasting
- low level of HDL cholesterol —the “good” cholesterol—in your blood
Metabolic syndrome is closely linked to overweight and obesity and to a lack of physical activity. Healthy lifestyle changes that help you control your weight may help you prevent and reduce metabolic syndrome.
Fatty liver diseases develop when fat builds up in your liver , which can lead to severe liver damage, cirrhosis , or even liver failure . These diseases include nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) .
NAFLD and NASH most often affect people who have overweight or obesity. People who have insulin resistance , unhealthy levels of fat in the blood, metabolic syndrome , type 2 diabetes, and certain genes can also develop NAFLD and NASH.
If you have overweight or obesity, losing at least 3% to 5% of your body weight may reduce fat in the liver. 15
Cancer is a collection of related diseases. In all types of cancer, some of the body’s cells begin to grow abnormally or out of control. The cancerous cells sometimes spread to other parts of the body.
Overweight and obesity may raise your risk of developing certain types of cancer . Men with overweight or obesity are at a higher risk for developing cancers of the colon , rectum , and prostate . 10 Among women with overweight or obesity, cancers of the breast , lining of the uterus , and gallbladder are more common.

Adults who gain less weight as they get older have lower risks of many types of cancer, including colon, kidney , breast, and ovarian cancers . 16
Overweight and obesity can also affect how well your lungs work, and excess weight increases your risk for breathing problems. 17
Sleep apnea
Sleep apnea is a common problem that can happen while you are sleeping. If you have sleep apnea, your upper airway becomes blocked, causing you to breathe irregularly or even stop breathing altogether for short periods of time. Untreated sleep apnea may raise your risk for developing many health problems, including heart disease and diabetes.
Obesity is a common cause of sleep apnea in adults. 18 If you have overweight or obesity, you may have more fat stored around your neck, making the airway smaller. A smaller airway can make breathing difficult or cause snoring. If you have overweight or obesity, losing weight may help reduce sleep apnea or make it go away.
Asthma is a chronic, or long-term, condition that affects the airways in your lungs. The airways are tubes that carry air in and out of your lungs. If you have asthma, the airways can become inflamed and narrow at times. You may wheeze, cough, or feel tightness in your chest.
Obesity can increase your risk of developing asthma, experiencing worse symptoms, and having a harder time managing the condition. 19 Losing weight can make it easier for you to manage your asthma. For people who have severe obesity, weight-loss surgery—also called metabolic and bariatric surgery—may improve asthma symptoms. 17
Osteoarthritis is a common, long-lasting health problem that causes pain, swelling, stiffness, and reduced motion in your joints . Obesity is a leading risk factor for osteoarthritis in the knees, hips, and ankles. 20
Having overweight or obesity may raise your risk of getting osteoarthritis by putting extra pressure on your joints and cartilage. If you have excess body fat, your blood may have higher levels of substances that cause inflammation . Inflamed joints may raise your risk for osteoarthritis.

If you have overweight or obesity, losing weight may decrease stress on your knees, hips, and lower back and lessen inflammation in your body. If you have osteoarthritis, losing weight may improve your symptoms. Research shows that exercise is one of the best treatments for osteoarthritis. Exercise can improve mood, decrease pain, and increase flexibility.
Gout is a kind of arthritis that causes pain and swelling in your joints. Gout develops when crystals made of a substance called uric acid build up in your joints. Risk factors include having obesity, being male, having high blood pressure, and eating foods high in purines . 21 These foods include red meat, liver, and anchovies.
Gout is treated mainly with medicines. Losing weight may also help prevent and treat gout. 22
Overweight and obesity may raise your risk of getting gallbladder diseases, such as gallstones and cholecystitis . People who have obesity may have higher levels of cholesterol in their bile , which can cause gallstones. They may also have a large gallbladder that does not work well.
Having a large amount of fat around your waist may raise your risk for developing gallstones. But losing weight quickly also increases your risk. If you have obesity, talk with your health care professional about how to lose weight safely .
Obesity can also affect your pancreas , a large gland behind your stomach that makes insulin and enzymes to help you digest food. People who have obesity have a higher risk of developing inflammation of the pancreas, called pancreatitis . High levels of fat in your blood can also raise your risk of having pancreatitis. You can lower your chances of getting pancreatitis by sticking with a low-fat, healthy eating plan.
Kidney disease means your kidneys are damaged and can’t filter your blood as they should. Obesity raises the risk of developing diabetes and high blood pressure, which are the most common causes of chronic kidney disease (CKD). Even if you don’t have diabetes or high blood pressure, having obesity may increase your risk of developing CKD and speed up its progress. 23
If you have overweight or obesity, losing weight may help you prevent or delay CKD. If you are in the early stages of CKD, consuming healthy foods and beverages , being active, and losing excess weight may slow the progress of the disease and keep your kidneys healthier longer. 24

Overweight and obesity raise the risk of developing health problems during pregnancy that can affect the pregnancy and the baby’s health. Pregnant people who have obesity may have a greater chance of 10
- developing gestational diabetes , or diabetes that occurs during pregnancy
- having preeclampsia , or high blood pressure during pregnancy, which can cause severe health problems for the pregnant person and baby if left untreated
- needing a caesarean delivery —or c-section—and, as a result, taking longer to recover after giving birth
- having complications from surgery and anesthesia , especially if they have severe obesity
- gaining more weight or continuing to have overweight or obesity after the baby is born
Having obesity or gaining too much weight during pregnancy can also increase health risks for the baby, including 25
- being born larger than expected based on the sex of the baby or the duration of the pregnancy
- developing chronic diseases as adults, including type 2 diabetes, obesity, heart disease, and asthma
Talk with your health care professional about how to
- reach a healthy weight before pregnancy
- gain a healthy amount of weight during pregnancy
- safely lose weight after your baby is born
Obesity increases the risk of developing infertility . Infertility in women means not being able to get pregnant after a year of trying, or getting pregnant but not being able to carry a pregnancy to term. For men, it means not being able to get a woman pregnant. 26
Obesity is linked to lower sperm count and sperm quality in men. 27 In women, obesity is linked to problems with the menstrual cycle and ovulation . 26 Obesity can also make it harder to become pregnant with the help of certain infertility treatments or procedures. 26
Women with obesity who lose 5% of their body weight may increase their chances of having regular menstrual periods, ovulating, and becoming pregnant. 28
Obesity may also increase the risk of developing sexual function problems. 29 Having overweight or obesity increase the risk of developing erectile dysfunction (ED) , a condition in which males are unable to get or keep an erection firm enough for satisfactory sexual intercourse.
Few studies have looked at how obesity may affect female sexual function by contributing to problems such as loss of sexual desire, being unable to become or stay aroused, being unable to have an orgasm, or having pain during sex. 30 But research suggests that healthy eating, increased physical activity, and weight loss may help reduce sexual function problems in people with obesity. 29,30
In addition to increasing the risk for developing physical health problems, obesity can also affect mental health, increasing the risk for developing 31
- long-term stress
- body image problems
- low self-esteem
- eating disorders
Studies show that people with overweight or obesity are also likely to face weight-related bias at school and work, which may cause long-term harm to their quality of life. 31 Losing excess weight has been found to improve body image and self-esteem and reduce symptoms of depression. 32
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Nearly One-Third of U.S. Adults Know Someone Who’s Died of Drug Overdose
Survey also finds ‘overdose loss’ bolsters recognition of addiction as an important policy issue that spans party lines
Losing a loved one to drug overdose has been a common experience for many Americans in recent years, crossing political and socioeconomic divides and boosting the perceived importance of the overdose crisis as a policy issue, according to a new survey led by researchers at the Johns Hopkins Bloomberg School of Public Health.
A nationally representative survey of more than 2,300 Americans, fielded in spring 2023, suggests that 32 percent of the U.S. adult population, or an estimated 82.7 million individuals, has lost someone they know to a fatal drug overdose. For nearly one-fifth of survey respondents—18.9 percent, representing an estimated 48.9 million adults—the person they knew who died of overdose was a family member or close friend.
The rates of reported loss due to overdose did not differ significantly by political party affiliation, but those who experienced overdose loss were more likely to view addiction as an extremely or very important policy issue.
The study was published online May 31 in JAMA Health Forum .
“The drug overdose crisis is a national tragedy,” says Alene Kennedy-Hendricks, PhD, assistant professor in the Department of Health Policy and Management at the Bloomberg School, who led the analysis. “Although large numbers of U.S. adults are bereaved due to overdose, they may not be as visible as other groups who have lost loved ones to less stigmatized health issues. Movements to build support for policy change to overcome the devastating toll of the overdose crisis should consider the role of this community.”
Over one million Americans have died from drug overdoses since the late 1990s, including more than 100,000 per year in the last few years, according to the Centers for Disease Control and Prevention. Last year, overdose deaths declined slightly for the first time in five years, decreasing three percent from 2022, according to preliminary data from the CDC’s National Center for Health Statistics. At about 108,000 estimated deaths, the CDC 2023 preliminary numbers remain near historic highs.
The overdose crisis has evolved over several phases, beginning with prescription opioids such as oxycodone playing a key role, followed by heroin and, more recently, powerful synthetic opioids like illicitly manufactured fentanyl and polysubstance use. Opioids can suppress breathing as a side effect, and the unpredictability of the illicit drug supply and the potency of fentanyl have dramatically increased the risk of overdose.
While the survey questions did not specifically identify opioids, the majority of overdose deaths over the last two decades have been opioid-related.
The overdose crisis has not only impacted its direct victims but also their relatives, friends, and acquaintances. Kennedy-Hendricks and her colleagues at the Bloomberg School’s Center for Mental Health and Addiction Policy set up the study to help illuminate this wider impact, which otherwise has been little studied.
The paper was co-written with colleagues from Boston University School of Public Health, the University of Minnesota, and the de Beaumont Foundation. The study’s senior author is Sandro Galea, MD, DrPH, MPH, dean of Boston University School of Public Health.
The survey is part of the CLIMB (COVID-19 and Life Stressors Impact on Mental Health and Well-being) study. Led by Catherine Ettman, PhD, an assistant professor in the Bloomberg School’s Department of Health Policy and Management, the CLIMB study has surveyed a nationally representative sample of adult Americans annually since 2020. For this overdose loss study, questions to participants from March 28 to April 17, 2023—CLIMB Wave 4—included “Do you personally know anyone who has died from a drug overdose?” A total of 2,326 participants responded to the question. Participants answering “yes” were then asked “Who do you know that has died from a drug overdose?”
Overdose losses were reported across all income groups. Forty percent of lower-income respondents (defined as annual household incomes less than $30,000) reported overdose loss. Over one-quarter—26 percent—of respondents in the $100,000 and higher annual household income category reported an overdose loss.
The rate of reported overdose loss was not significantly different across self-described Republicans, Democrats, and Independents, adding to the picture of a far-reaching phenomenon.
The data suggested a high level of endorsement across all groups—greater than 60 percent, even among those reporting no overdose loss—that addiction is an extremely or very important policy issue. Respondents who reported overdose loss had 37 percent greater odds of viewing addiction as a very or extremely important policy priority.
“This study contributes new evidence that the addiction crisis and the losses that come with it are common across Americans, but the burden is greater among those who are more economically precarious,” says Ettman. “Addressing addiction can be a unifying theme in increasingly divided times.”
The researchers plan to follow up with further studies in future CLIMB survey waves, looking at associations between overdose loss and other social variables such as trust in institutions.
“ Experience of Personal Loss Due to Drug Overdose Among U.S. Adults ” was co-authored by Alene Kennedy-Hendricks, Catherine Ettman, Sarah Gollust, Sachini Bandara, Salma Abdalla, Brian Castrucci, and Sandro Galea.
CLIMB Study Wave 4 was funded by a grant from the de Beaumont Foundation.
Media contacts: Kate Sam [email protected] or Kris Henry [email protected]
Related Content

From the Classroom to the Capitol: Gretchen Jacobson, PhD’s Journey in Public Health Policy

Health in All Policies

A Brief History of Traffic Deaths in the U.S.

The Hunger Gap

Rewriting the Story of Life’s Later Years

IMAGES
VIDEO
COMMENTS
Abstract. Social media are responsible for aggravating mental health problems. This systematic study summarizes the effects of social network usage on mental health. Fifty papers were shortlisted from google scholar databases, and after the application of various inclusion and exclusion criteria, 16 papers were chosen and all papers were ...
We desperately need more research to find effective treatments as well as preventive measures to reduce the risk of developing long COVID." — Sarah Wulf Hanson, lead research scientist of the non-fatal and risk quality enhancement team and lead author of the JAMA paper on long COVID . 2. Mental health
Health research entails systematic collection or analysis of data with the intent to develop generalizable knowledge to understand health challenges and mount an improved response to them. The full spectrum of health research spans five generic areas of activity: measuring the health problem; understanding its cause(s); elaborating solutions; translating the solutions or evidence into policy ...
Featured health risks and issues. As part of the Global Burden of Disease (GBD) study, we produce estimates for more than 80 risk factors along with in-depth analysis for the world's most pressing health issues. View all risks. Health topic.
Globally, the problem is many times worse, making homelessness a global public health and environmental problem. The facts [ 1] are staggering: On a single night in January 2020, 580,466 people (about 18 out of every 10,000 people) experienced homelessness across the United States—a 2.2% increase from 2019.
To provide a contemporary global prevalence of mental health issues among the general population amid the coronavirus disease-2019 (COVID-19) pandemic. We searched electronic databases, preprint ...
Need for Mental Health (MH) Prevention. Longitudinal studies suggest that individuals with a lower level of positive wellbeing are more likely to acquire mental illness ().Conversely, factors that promote positive wellbeing and resilience among individuals are critical in preventing mental illnesses and better outcomes among those with mental illness (10, 11).
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022. Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began ...
A systems perspective provides new lenses through which we can study mental health problems: by using theories and methods from other fields with rich traditions, including network and systems sciences (Barabási, 2012; Von Bertalanffy, 1972). I introduce a few concepts below that may help to advance understanding of mental health problems.
With NIH support, scientists across the United States and around the world conduct wide-ranging research to discover ways to enhance health, lengthen life, and reduce illness and disability. Groundbreaking NIH-funded research often receives top scientific honors. In 2021, these honors included Nobel Prizes to five NIH-supported scientists.
And trust is needed: mistrust of the health care system has emerged as a primary barrier among members of communities of color to seeking care in health care systems (21). Mistrust stems from historical events, including the Tuskegee syphilis study, and is reinforced by health system issues and discriminatory events that continue to this day (21).
Research for health is a global endeavour, and WHO has a unique role to play in ensuring that these efforts can help improve health for all. WHO provides leadership, calling on the wider scientific community to engage behind global health concerns. This is based on a deep understanding of the needs of countries, and rigorous assessment by ...
There was inconsistency in the study findings, with studies finding that age (21 or older) was associated with fewer depressive symptoms, lower likelihood of suicide ideation and attempt, self-harm, and positively associated with better coping skills and mental wellbeing. ... The risk of mental health problems in these students compared with ...
This can put you at increased risk for a variety of physical and mental health problems, including anxiety, depression, digestive issues, headaches, muscle tension and pain, heart disease, heart attack, high blood pressure, stroke, sleep problems, weight gain, and memory and concentration impairment. Chronic stress may also cause disease ...
The term "health research," sometimes also called "medical research" or "clinical research," refers to research that is done to learn more about human health. Health research also aims to find better ways to prevent and treat disease. Health research is an important way to help improve the care and treatment of people worldwide.
Increasing demands on ecosystems, decreasing biodiversity, and climate change are among the most pressing environmental issues of our time. As changing weather conditions are leading to increased vector-borne diseases and heat- and flood-related deaths, it is entering collective consciousness: environmental issues are human health issues. In public health, the field addressing these issues is ...
Research on Health Effects from Air Pollution. Decades of research have shown that air pollutants such as ozone and particulate matter (PM) increase the amount and seriousness of lung and heart disease and other health problems. More investigation is needed to further understand the role poor air quality plays in causing detrimental effects to ...
Among Black adults, 55% say they have ever had at least one of six negative experiences with doctors or other health care providers. Black Americans offer a mixed assessment of the progress that has been made improving health outcomes for Black people: 47% say health outcomes for Black people have gotten better over the past 20 years, while 31% ...
Loneliness may be harmful to our daily health, according to a new study led by researchers in the Penn State College of Health and Human Development and Center for Healthy Aging focused on ...
This factor is particularly relevant for communities of color, who report perceiving a higher level of stigma associated with behavioral-health conditions. 10 Mental health: Culture, race, and ethnicity; A supplement to mental health; A report of the surgeon general, US Department of Health and Human Services, August 2001: A 1998 study cited in ...
Recent research shows that adolescents who spend more than three hours per day on social media face double the risk of experiencing poor mental health outcomes, such as symptoms of depression and anxiety; yet one 2021 survey of teenagers found that, on average, they spend 3.5 hours a day on social media.
The idea of a special journal collection on emerging global health issues was timely. At the beginning of 2019, the World Health Organization (WHO) released a list of 10 threats to global health for the year. 2 They include: (1) air pollution and climate change, (2) non-communicable diseases, (3) threat of a global influenza pandemic, (4 ...
Results appeared in Nature Medicine on February 27, 2023. The team found that elevated levels of erythritol and several related artificial sweeteners were associated with the risk for cardiovascular events. To confirm this result, the researchers examined two more groups of people in the U.S. and Europe totaling almost 3,000.
He and his team pulled data from the Adolescent Brain Cognitive Development Study, a nationwide project funded by the National Institutes of Health that collects data on children's health and ...
Many individuals who develop substance use disorders (SUD) are also diagnosed with mental disorders, and vice versa. 2,3 Although there are fewer studies on comorbidity among youth, research suggests that adolescents with substance use disorders also have high rates of co-occurring mental illness; over 60 percent of adolescents in community-based substance use disorder treatment programs also ...
May 24, 2024. Semaglutide, the compound in the blockbuster drugs Ozempic and Wegovy, dramatically reduced the risk of kidney complications, heart issues and death in people with Type 2 diabetes ...
The safety of sugar substitutes is once again being called into question. Xylitol is associated with an increased risk of heart attack and stroke, according to new Cleveland Clinic research.
June 3, 2024 3 min read. In a study that followed more than 25,000 U.S. women for up to 25 years, researchers from Harvard-affiliated Brigham and Women's Hospital found that participants who closely followed the Mediterranean diet had up to a 23 percent lower risk of all-cause mortality, with benefits for both cancer and cardiovascular health.
Few studies have looked at how obesity may affect female sexual function by contributing to problems such as loss of sexual desire, being unable to become or stay aroused, being unable to have an orgasm, or having pain during sex. 30 But research suggests that healthy eating, increased physical activity, and weight loss may help reduce sexual ...
The study was published online May 31 in JAMA Health Forum. "The drug overdose crisis is a national tragedy," says Alene Kennedy-Hendricks, PhD, assistant professor in the Department of Health Policy and Management at the Bloomberg School, who led the analysis.