

Mental Health
On This Page: -->
Mental Health During the COVID-19 Pandemic
Frequently asked questions, mental health resources.

NIH has compiled a library of resources related to COVID-19 and mental illnesses and disorders, including condition-specific and population-specific resources.

An Urgent Issue
Both SARS-CoV-2 and the COVID-19 pandemic have significantly affected the mental health of adults and children. In a 2021 study, nearly half of Americans surveyed reported recent symptoms of an anxiety or depressive disorder, and 10% of respondents felt their mental health needs were not being met. Rates of anxiety, depression, and substance use disorder have increased since the beginning of the pandemic. And people who have mental illnesses or disorders and then get COVID-19 are more likely to die than those who don’t have mental illnesses or disorders.
Mental health is a focus of NIH research during the COVID-19 pandemic. Researchers at NIH and supported by NIH are creating and studying tools and strategies to understand, diagnose, and prevent mental illnesses or disorders and improve mental health care for those in need.
How COVID-19 Can Impact Mental Health
If you get COVID-19, you may experience a number of symptoms related to brain and mental health, including:
Cognitive and attention deficits (brain fog)
Anxiety and depression
Suicidal behavior
Data suggest that people are more likely to develop mental illnesses or disorders in the months following infection, including symptoms of post-traumatic stress disorder (PTSD). People with Long COVID may experience many symptoms related to brain function and mental health.
How the Pandemic Affects Developing Brains
The impact of the COVID-19 pandemic on the mental health of children is not yet fully understood. NIH-supported research is investigating factors that may influence the cognitive, social, and emotional development of children during the pandemic, including:
Changes to routine
Virtual schooling
Mask wearing
Caregiver absence or loss
Financial instability
Not Everyone Is Affected Equally
While the COVID-19 pandemic can affect the mental health of anyone, some people are more likely to be affected than others. People who are more likely to experience symptoms of mental illnesses or disorders during the COVID-19 pandemic include:
People from racial and ethnic minority groups
Mothers and pregnant people
People with financial or housing insecurity
People with disabilities
People with preexisting mental illnesses or substance use problems
Health care workers
People who belong to more than one of these groups may be at an even greater risk for mental illness.
Telehealth’s Potential to Help
The pandemic has prevented many people from visiting health care professionals in person, and as a result, telehealth has been more widely adopted during this time. Telehealth visits for mental health and substance use disorders increased significantly from 2020 to 2021 and now make up nearly half of all total visits for behavioral health.
Widespread adoption of telehealth services may help people who otherwise would not be able to access mental health support, such as people in rural areas or places with few providers.

I have a preexisting mental illness. Is COVID-19 more dangerous to me?
COVID-19 can be worse for people with mental illnesses. Data suggest that people who reported symptoms of anxiety or depression had a greater chance of being hospitalized after a COVID-19 diagnosis than people without those symptoms.
The Centers for Disease Control and Prevention (CDC) reports that having mood disorders and schizophrenia spectrum disorders can increase a person’s chances of having severe COVID-19. People with mental illnesses who belong to minority groups are also more likely to get COVID-19. And people with schizophrenia are significantly more likely to get COVID-19 and more likely to die from it.
Despite these risks, effective treatments are available. If you have a preexisting mental illness and get COVID-19, talk to your health care professional to determine the treatment plan that’s appropriate for you.
I’m experiencing symptoms of a mental illness or disorder. What should I do?
If you are experiencing symptoms of anxiety, depression, or any other mental illness or disorder, there are ways you can get help. For immediate help:
Call or text the 988 Suicide & Crisis Lifeline at 988 (para ayuda en español, llame al 988)
Call or text the Disaster Distress Helpline , 1-800-985-5990 (press 2 for Spanish)
The Substance Abuse and Mental Health Services Administration can help you find mental health or substance use specialists.
Talk to your health care professional or mental health care professional. Together, you can work on a plan to manage or reduce your symptoms.
What research is NIH doing on the mental health impacts of COVID-19?
The National Institute of Mental Health (NIMH) and other NIH Institutes have created research initiatives to address mental health for people in general and for the most vulnerable people specifically. Examples of this research include:
NIH's Researching COVID to Enhance Recovery (RECOVER) Initiative has launched RECOVER-NEURO , a clinical trial that will test interventions to combat cognitive problems caused by Long COVID, including brain fog, memory problems, difficulty with attention, thinking clearly, and problem solving.
NIMH launched a five-year research study called RECOUP-NY to promote the mental health of New Yorkers from communities hard-hit by COVID-19. The study will test the use of a new care model called Problem Management Plus (PM+) that can be used by non-specialists.
A study funded by NIMH is examining the use of mobile apps to address mental health disparities .
The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) is funding research to understand the effects of mask usage for children , including any impacts on their emotional and brain development.
NIMH is funding research on the impacts of the pandemic on underserved and vulnerable populations and on the cognitive, social, and emotional development of children .
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) is funding research on how COVID-19 and SARS-CoV-2 affect the causes and consequences of alcohol misuse .
A collaborative study supported by NIMH and the National Center for Complementary and Integrative Health (NCCIH) enrolled more than 3,600 people from all 50 U.S. states to understand the stressors affecting people during the pandemic.
Mental Health Resources by Topic
A library of resources related to COVID-19 and mental illnesses and disorders
Page last updated: September 28, 2023
- High Contrast
- Increase Font
- Decrease Font
- Default Font
- Turn Off Animations
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment case
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Publications detail /
Mental Health and COVID-19: Early evidence of the pandemic’s impact: Scientific brief, 2 March 2022

The COVID-19 pandemic has had a severe impact on the mental health and wellbeing of people around the world while also raising concerns of increased suicidal behaviour. In addition access to mental health services has been severely impeded. However, no comprehensive summary of the current data on these impacts has until now been made widely available.
This scientific brief is based on evidence from research commissioned by WHO, including an umbrella review of systematic reviews and meta-analyses and an update to a living systematic review. Informed by these reviews, the scientific brief provides a comprehensive overview of current evidence about:
- the impact of the COVID-19 pandemic on the prevalence of mental health symptoms and mental disorders
- the impact of the COVID-19 pandemic on prevalence of suicidal thoughts and behaviours
- the risk of infection, severe illness and death from COVID-19 for people living with mental disorders
- the impact of the COVID-19 pandemic on mental health services
- the effectiveness of psychological interventions adapted to the COVID-19 pandemic to prevent or reduce mental health problems and/or maintain access to mental health services
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 07 March 2024
The impact of COVID-19 lockdowns on mental health patient populations in the United States
- Ibtihal Ferwana 1 &
- Lav R. Varshney ORCID: orcid.org/0000-0003-2798-5308 1
Scientific Reports volume 14 , Article number: 5689 ( 2024 ) Cite this article
2436 Accesses
19 Altmetric
Metrics details
- Health care economics
- Health policy
During the start of the COVID-19 pandemic in 2020, lockdowns and movement restrictions were thought to negatively impact population mental health, since depression and anxiety symptoms were frequently reported. This study investigates the effect of COVID-19 mitigation measures on mental health across the United States, at county and state levels using difference-in-differences analysis. It examines the effect on mental health facility usage and the prevalence of mental illnesses, drawing on large-scale medical claims data for mental health patients joined with publicly available state- and county-specific COVID-19 cases and lockdown information. For consistency, the main focus is on two types of social distancing policies, stay-at-home and school closure orders. Results show that lockdown has significantly and causally increased the usage of mental health facilities in regions with lockdowns in comparison to regions without such lockdowns. Particularly, resource usage increased by 18% in regions with a lockdown compared to 1% decline in regions without a lockdown. Also, female populations have been exposed to a larger lockdown effect on their mental health. Diagnosis of panic disorders and reaction to severe stress significantly increased by the lockdown. Mental health was more sensitive to lockdowns than to the presence of the pandemic itself. The effects of the lockdown increased over an extended time to the end of December 2020.
Similar content being viewed by others

The WHO estimates of excess mortality associated with the COVID-19 pandemic

The real-time infection hospitalisation and fatality risk across the COVID-19 pandemic in England
Risk of COVID-19 death in adults who received booster COVID-19 vaccinations in England
Introduction.
As the COVID-19 pandemic began, confirmed cases rose, and mandated policy responses were enacted, mental health concerns started to be alarming 1 , 2 , 3 . The deterioration of mental health was observed during the first few months of the COVID-19 pandemic, March–June 2020 4 , 5 , especially among women and college students 6 , 7 , 8 . Further, people with preexisting psychiatric disorders 9 , 10 and people that encountered COVID-19 itself 4 developed more mental health issues during the pandemic.
In the early stage of the COVID-19 pandemic, people voluntarily stayed at home and limited their trips for weeks before public policy interventions were imposed 11 . Subsequently, social distancing policies were issued globally as a form of non-pharmaceutical intervention, including limiting people’s gatherings, closing schools, and fully restricting movements by lockdown orders (also called stay-at-home or shelter-in-place orders) 12 , so as to contain virus spread in light of the increasing number of COVID-19 cases and fatalities.
Given that various intertwined events took place during the COVID-19 pandemic, the cause of mental health deterioration is not clear. One possible explanation is the increased severity of COVID-19 which led to increased anxiety, worry, and depression 13 . Another explanation is that policy responses to the pandemic, particularly the lockdown orders, contributed to worsening mental health.
Previous studies observing the decline in mental health have faced a challenge in determining possible causes or selecting direct measures. For example, Refs. 14 , 15 found that depression and anxiety symptoms almost quadrupled from 2019 to June 2020, but could not infer causality given the study design. Other studies found that reduced physical activity resulting from restricted mobility led to higher rates of depression during the pandemic, but could not establish causality since they lacked pre-COVID-19 data 10 , 16 , 17 . Two other important studies by Refs. 18 , 19 used Google search data and found that the timing of lockdown policies has been significantly associated with searches of terms related to worry , sadness , and boredom revealing negative feelings. A recent study established causality of the effect of lockdown restrictions on worsening mental health using a clinical mental health questionnaire in Europe 20 . Although these studies considered pre-COVID-19 trends and have established causality on the lockdown orders, they lacked measures that reflect the rising need for mental health treatment and lacked a large representative population.
Examining the use of mental health resources and the prevalence of mental illnesses would further help in measuring the actual cost of COVID-19 lockdowns on mental health and inform mental health treatment resource planning for future lockdowns. Mental disorders have been more economically costly than any other disease, in which mental disorders were the leading segment of healthcare spending in the United States 21 , with the potential cause of a global economic burden 22 . Mental health has been related to social capital on individual and community levels 23 , 24 . Indeed, good social capital plays a role in promoting healthier public behaviors, especially during COVID-19 25 . The risk of mental health degradation goes beyond to impact the advantage of social capital in the face of viral diseases. Given these consequences of poor mental health on health care systems 26 , it has been essential to mitigate additional mental degradation and avoid potential future economic and social costs.
In this work, we consider measures that reflect the actual seeking of mental health services covering a large fraction of the United States population. To the best of our knowledge, there is no large-scale study that has investigated the effect of lockdown on the usage of mental health resources across the country. We empirically estimate the causal effect of COVID-19 social distancing policies on mental health across counties and states in the United States by comparing the differences in changes between locked and non-locked down regions using a large-scale medical claims dataset that covers most hospitals in the country. Specifically, we are interested to know whether the increase in mental health patients can be explained by COVID-19 lockdowns. Causal inference gives us the tools to uncover causal relationships rather than correlational relationships 27 , in order to understand the impact of COVID-19 policies on mental health.
We use the daily number of patients who visit mental health facilities as a measure for the usage of mental health resources, and we consider emergency department (ED) visits for mental health issues as a proxy for the development of new mental diseases, here, so severe that treatment could not be avoided. We consider ED visits to reflect the utilization of hospital resources under the shortage of medical staff. During COVID-19 there were patients with acute conditions reaching ED in which they have not been in regular outpatient visits 28 . Also, given the shortage in in-patient beds during the pandemic, mental health patients were admitted to ED instead 29 . Therefore, ED visits were of interest to indicate unmet mental health needs. The usage of mental health resources can further trigger analysis of economic costs borne by health care systems and the country as a whole. Mental health ED treatment visits might further reflect the mental health cost on an individual level.
Our results show that extended lockdown measures significantly increase the usage of mental health resources and ED visits. In particular, mental health resource usage in regions with lockdown orders has significantly increased compared to regions without a lockdown. The effect size of lockdowns was not only positive and significant but was also increasing till the end of December 2020. Our results further imply that mental health is more sensitive to policy interventions rather than the evolution of the pandemic itself.
The University of Illinois Urbana-Champaign Institutional Review Board declared this work to be exempt from review. The University of Illinois Urbana-Champaign Institutional Review Board waived the need for informed consent for the current study. All methods were carried out in accordance with relevant guidelines and regulations.
We used three sets of data to conduct our study: mental health claims data including emergency department (ED) claims, COVID-19 cases data, and lockdown dates data.
The mental health data is a large de-identified medical claims corpus provided by Change Healthcare for years 2019 and 2020. Change Healthcare serves 1 million providers covering 5500 hospitals with 220 million patients (which is roughly two-thirds of the US population) and represents over 50% of private insurance claims across the United States. It covers 51 states/territories and a total of 3141 counties (and equivalent jurisdictions like parishes). The data set includes millions of claims per month from the private insurance marketplace, and some Medicare Advantage programs and Medicaid programs using private insurance carriers, excluding Medicare and Medicaid indemnity claims, which is a limitation in the dataset coverage.
Given that different age and gender groups were affected differently during the pandemic 6 , 7 , 8 , we consider a variety of population subgroups in our analysis. Specifically, we consider subgroups of different age, gender, and mental health conditions. Not only do we look at the total mental health claims, but we also select specific mental health conditions, such as anxiety disorders, major depressive disorder, bipolar disorder. Our selected mental health conditions have been also been examined by others 30 during the COVID-19 pandemic. More details on the used clinical codes of mental health records are found in Supplementary Appendix Table 1 . We show summary statistics of the data and its subset representing gender, age, and mental disorders in Table 1 .
For COVID-19 cases, we considered state-level and county-level cases reported in the United States taken from the New York Times database 31 from the first case date in late January 2020 to December 31, 2020, covering 3218 counties in 51 states/territories. Given that reported cases depend on the testing results, thus, the data is limited by the fact that there was a widespread shortage of available tests in different regions at different times. The undercounts of COVID-19 cases used in this study would only weaken the effect we present, and so fixing the data would only strengthen the resultant effect.
For lockdown data, we used the data from the COVIDVis project URL: https://covidvis.berkeley.edu/ led by the University of California Berkeley to track policy interventions on state and county levels, in which they depended on government pandemic responses to construct the dataset. We considered the dates of two order types, shelter-in-place and K-12 school closure at state and county levels. The earliest and latest shelter-in-place orders were on March 14 and April 7, 2020, covering 2598 counties in 43 states. The earliest K-12 school closure was on March 10 and the latest was on April 28, 2020, covering 2465 counties in 39 states. The data is comprehensive, in which states and counties that do not appear in the dataset are considered without officially imposed lockdown. We focus on the impact of the initial shutdowns to avoid complications related to re-opening and repeated closures. Given that in some regions people tend to voluntarily isolate themselves at home and limit their trips before official lockdown orders 11 , therefore, lockdown dates might be limited to reflect the actual social distancing behavior across regions during the pandemic. However, lockdown dates would better reflect the beginning of persistent social distancing behaviors for a larger population group, which is useful to our study, unlike voluntary behaviors.
Difference-in-differences analysis
To estimate the effects of COVID-19 mitigation policies on mental health patients at county and state levels, we conducted a difference-in-differences (DID) analysis, which allows for inferring causality based on parallel trends assumption. For DID analysis we considered daily mental health patients’ visits from the date of September 1, 2019, till December 31, 2020, to observe the prolonged effects since mental health disorders may appear sometime after a trauma 32 . We aim to have balanced periods for pre- and post-lockdown interventions, and this is achievable with this selected range of dates. We used two outcomes, weighted and raw numbers of daily patient visits, weighted outcomes are normalized by the region population.
Our approach leveraged the variation of policy-mandated dates in different counties or states with 8 states that did not declare an official lockdown. Accordingly, we constructed both treated and control groups to implement the analysis. We estimated the following regression as our main equation:
where \(Y_{cd}\) is the outcome in a given region c (county or state) on a date d , \(policy_{jcd}\) indicates whether a policy j has been mandated for a region c on a date d , \(\beta _j\) is the DID interaction coefficient, representing the effect of introducing policy j , and \(\delta _c\) and \(\delta _{d}\) are fixed effects for region and date respectively. The region fixed-effect is included to adjust for time-invariant (independent of time) unobserved regional characteristics that might affect the outcome. For example, each county/state has its local health care system, social capital index, age profile, and socioeconomic status that the fixed effect controls for. Further, the date fixed effect \(\delta _{d}\) is included to adjust for factors that vary over time, such as COVID-19 rates or social behavioral change.
Control by the evolution of COVID-19 cases
Even though DID avoids the bias encountered in time-invariant factors, the bias of time-varying confounders may still be present 33 . Therefore, we consider the COVID-19 confirmed cases \(x_{cd}\) as a main confounder factor in counties or states and we control for it. We follow 34 to use a time-varying adjusted (TVA) model, based on the assumption that the confounding variable affects both treated and untreated groups regardless of policy intervention. We measured the interaction of time and the confounding \(x_{cd}\) covariate at county- and state-levels
Therefore, to mitigate the effect of potential confounders, e.g. socio-economic status and COVID-19 growth, we use several techniques from econometrics 35 . Specifically, we use the fixed effects \(\delta _c\) and \(\delta _d\) in ( 1 ) to adjust for time-invariant confounders related to location and time. Additionally, we use TVA 34 to adjust for time-varying confounders such as COVID-19 growth.
Event-study model
DID models rely on the assumption of parallel pre-treatment trends to exist in both treated and untreated groups. Hence, in the absence of a policy, treated counties or states would evolve similarly as untreated counties or states. To assess equal pre-policy trends, we designed an event-study type model 36 . We calculated k periods before policy implementation and used an event-study coefficient to indicate whether an outcome in specific date d and county/state c is within k periods before the policy implementation 18 , 37 . We estimated the following regression model:
where \(policy_{hsd}^k\) , a dummy variable, equals 1 if policy h took place k periods before the mandate, and zero otherwise. Period k is calculated in months, \(k=\{- 6, - 5, - 4, - 2, - 1, 0\}\) months, and the month of the policy implementation ( \(k=0\) ) is considered as the omitted category. Here, \(\beta _h^k\) is the event-study coefficient and we included all control variables as defined in ( 1 ).
Descriptive analysis
Before we delve into the causal DID inference, we report some statistics to describe the data of mental health patients. Among 16.7 million mental health patients in the United States, the mean age was 38.7 years and 56% were female. As seen in Fig. 1 , the distribution of mental health patients in states and counties shifted between 2019 and 2020. The total increase is 22% of all mental health patients of any mental health disorder as seen in Table 2 in the Supplementary Appendix.
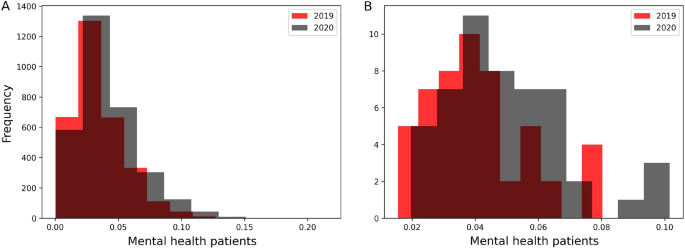
Distributions of mental health patients weighted by regions’ populations in years of 2019 and 2020 in counties ( A ) and states ( B ). The total population increase is 22% in 2020.
Figure 2 shows the increasing trend of the number of mental health daily patients’ visits, though it decreased between March and April 2020, during lockdown mandates.
An obvious increase was during June 2020, which can be attributed to telemedicine options or relaxed lockdown measures.
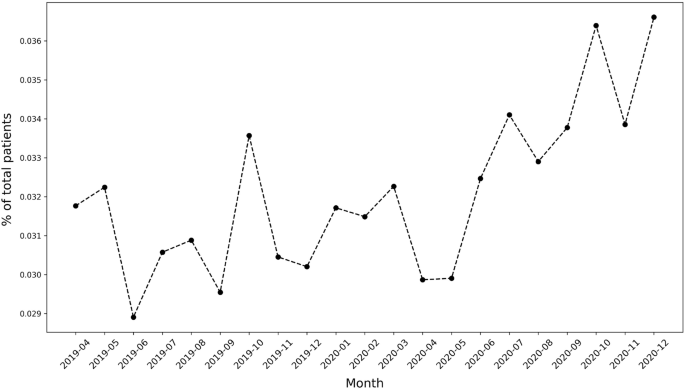
Mental health patients over time.
Parallel trend assumption
To apply DID, first, we validate the pre-policy parallel trends assumption. We tested the equality of pre-policy trends for counties and states using ( 3 ). We plot the event-study coefficients for 6 months before policy implementation from the models of stay-at-home and school-closure orders and the corresponding 95 % confidence intervals. Figure 1 (in Supplementary Appendix) shows that the event-study coefficients are generally non-significant, therefore we cannot reject the null hypothesis of parallel trends. Accordingly, the key assumption of parallel trends of DID is satisfied for both counties and states.
Correlation to COVID-19
Given the possibility that COVID-19 increasing cases act as a confounding factor to the increasing mental health burden, we adjusted our main DID regression to COVID-19 cases using the TVA model in ( 2 ). First, we validate that a correlation exists between mental health visits number and COVID-19 increasing cases. Figure 3 shows that a significant correlation between COVID-19 and mental health patients populations (R \(^2\) = 0.77, p-value < 2 \(\times 10^{-16}\) ) with an increase of 0.043 mental health visits for each new COVID-19 confirmed case. Adjusting for the COVID-19 cases acts as a proxy for adjusting for the pandemic effect itself.
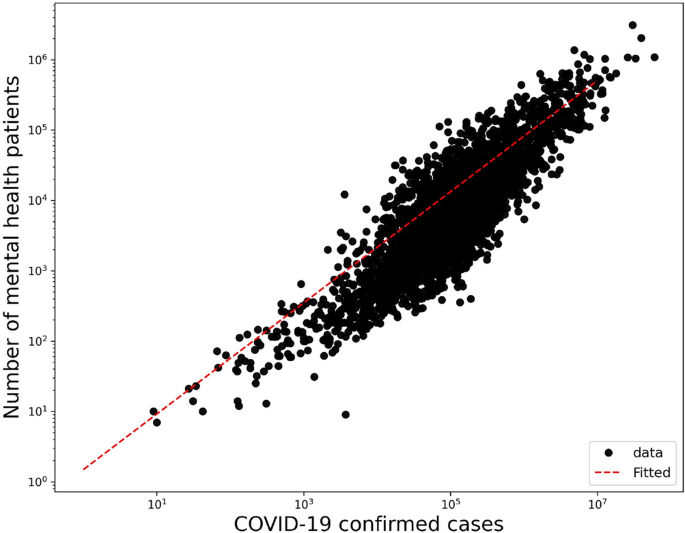
Correlation of mental health daily visits and COVID-19 confirmed cases in a log-log plot with an increase of 0.043 mental health visits for each confirmed COVID-19 case in counties (R \(^2\) = 0.77, p-value < \(2 \times 10^{-16}\) ).
Effects on the usage of mental health resources
We consider daily visits of mental health patients for the causal DID inference model from September 1, 2019, to December 31, 2020. Figure 4 shows the monthly average mental health visits in counties with stay-at-home orders and without. In general, there is an increase in monthly visits in months after COVID-19 lockdowns in regions with enacted lockdowns. There is also a clear similar trend of visits between regions with and without lockdowns. This pre-COVID-19 trend has been validated in the previously mentioned event study. Figure 2 (in Supplementary Appendix) shows the monthly average visits in counties with and without school closure orders. Similarly, Figs. 3 and 4 (in Supplementary Appendix) show the average monthly visits at the state level.
We further investigate the causality relationship between daily visits and lockdown measures. In Tables 2 and 3 we summarize the estimated effects of COVID-19 lockdown measures on the weighted outcomes for counties and states respectively for different population groups with the adjusted results after controlling for COVID-19 cases. Tables 5 and 6 (in Supplementary Appendix) summarize the raw outcomes. Along with regression estimates, we include significance measures of p-value, 95% confidence intervals of standard errors, and R-squared ( \(R^2\) ). We will further discuss results for each population group in both counties and states in the following sections.
Tables 11 and 12 (in Supplementary Appendix) summarize the estimated effects of Eq. ( 1 ) at different periods of time k where k = {1, 5, 9}-months after lockdowns, to show the dynamic effect of stay-at-home and school closures in counties and states respectively.
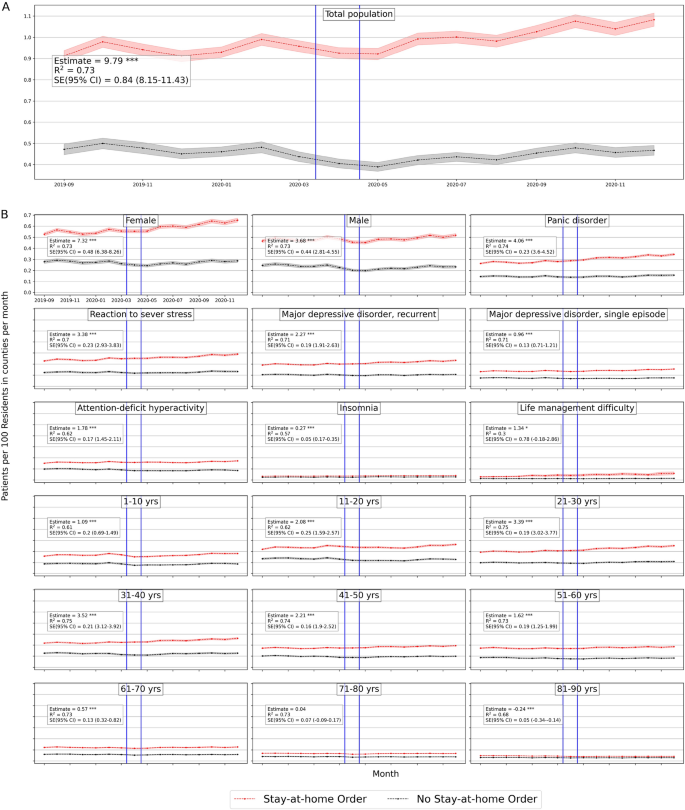
Average number of mental health patients over time (September 2019–December 2020) in counties with stay-at-home orders and without. Vertical lines show the first stay-at-home order on 3/14/2020 and last on 4/07/2020 across United States. Difference-in-differences estimates are included for each population. (Detailed average percentage changes are listed in Table 3 ). \(***p < 0.01\) , \(**p < 0.05\) , \(*p < 0.1\) .
Effects on total population
We consider the overall mental health population including all mental health disorders with clinical codes defined in Supplementary Table 1 . Based on Table 2 there is a significant positive effect of stay-at-home order across counties on the weighted population of mental health patients’ daily visits, with a mean difference of 1 in 10,000 daily patient visits between counties with stay-at-home orders and counties without. On average, mental health patients increased by 18.7% but declined by 1% in counties without lockdown (Fig. 4 ). Adjusting for COVID-19 confounding effect preserves the positive effect significant on the mental health population with a similar effect size. School closure has also a significant, but a lower effect on the mental health patient population (estimated mean difference = 8.8 in 100,000 population), with a percentage increase of 17% and 16% in counties with closed schools and without respectively (Table 3 in Supplementary Appendix), with significant similar size effect while adjusted for COVID-19 cases.
Similar results are found at the state level, Table 3 shows that the effect of stay-at-home order is positively significant for total mental health patients (difference estimate is 8.8 and 8.6 when adjusted in 10 \(^5\) population) with 22% increase by December 2020 as compared to less than 2% increase in states without lockdown (Table 4 in Supplementary Appendix). However, school closures have no significant effect at the state level.
We further investigate whether the effect on mental health differs if we shorten the period of observation after lockdown interventions. We applied our main regression model ( 1 ) on outcomes after a 1-month of lockdown (maximum mid-May) and 5-month of lockdown (maximum mid-August) for each region. The sizes of the lockdown effects are positive and significant at different times. Also, they keep increasing from the first month after the lockdown date until the end of the year 2020, for both stay-at-home orders and school closures in counties (Table 11 in Supplementary Appendix) and states (Table 12 in Supplementary Appendix).
We further examined the sensitivity of our DID results by sequentially adding controls to the baseline DID model. Table 7 in the Supplementary Appendix shows results are robust and neither COVID-19 growth nor the social capital index contributed to the effect of lockdowns on mental health populations.
Gender effects
In counties, the estimated effects of stay-at-home orders on both women and men are 6.8 (6.6 when adjusted) and 5.7 (5.7 when adjusted) respectively (Table 2 ). Female patients’ daily visits increased by 24% in counties with stay-at-home orders in comparison with 3% in counties without (Table 3 in Supplementary Appendix). Male patients declined by 5% in counties without stay-at-home orders. Whereas the estimated effects of school closures are negative for females (mean difference = − 1.67, and − 3.89 when adjusted) and significant when adjusted. While for men, school closure effects were significantly positive (mean difference = 4.5 and 3.4 when adjusted) (Table 2 ). This implies that women have been affected more by stay-at-home orders than by school closures across counties.
Similarly in states, the estimated mean difference for women is 5.1 (5.6 when adjusted) and for men is 3.8 (4.1 when adjusted) in 10 \(^5\) population (Table 3 ). Female patients’ daily visits increased by 29% and 6% in states with stay-at-home orders and without respectively, while male patients’ daily visits decreased in states without stay-at-home lockdown (Table 4 in Supplementary Appendix). School closure did not show significant effects on women or men at the state level.
Even at an early stage of the COVID-19 lockdown, mental health visits for female and male patients were larger than in non-locked regions, which they were increasing significantly throughout the year 2020 in counties and states (Tables 11 , 12 in Supplementary Appendix)
Diagnosis effects
We selected the top five mental disorders (e.g. panic disorder ) that peaked in 2020, and other disorders of interest ( insomnia and life management difficulty ) to investigate the effect of lockdowns on patient populations for specific diagnosis. We provide the definition of each considered mental condition in Table 1 in Supplementary Appendix.
In counties, all disorders were positively and significantly affected by stay-at-home orders and by school closures with lower effect sizes. Patients diagnosed with panic disorder (ICD-10: F41) had the largest difference among other mental illnesses and increased in both county groups (31.8% vs 8.88%) with an estimated effect of 3.3 (3.2 when adjusted in 10 \(^5\) population). Patients with attention-deficit hyperactivity disorder (ICD-10: F90) decreased in counties without stay-at-home orders by − 13.6% with an estimated effect of 3.2 (3.1 when adjusted) in 10 \(^5\) population.
Unlikely, patients with insomnia , with a significant estimated effect of \(-\,0.053\) in 10 \(^5\) population when adjusted, increased more in counties without school closures by 24% compared to 17% in counties with closures, which implies that insomnia was more in counties without school closures. Patients diagnosed with life management difficulty disorder increased more in counties without school closures as well by 127.85% compared with 94.64% with closures, and the estimated effect is − 0.6 (in 10 \(^5\) population) when adjusted (Tables 2 , 3 in Supplementary Appendix).
Similarly, at the state level, panic disorder (ICD-10: F41) increased by 38.4% in states with stay-at-home orders (Table 4 in Supplementary Appendix) and had the largest difference effect size with a mean difference of 2 in 10 \(^{5}\) population, similarly when adjusted (Table 3 ). Daily visits of patients with life management difficulty increased more in states without a school closure by 161.49% compared to 123.36% in states with closures with a significant estimated effect of \(-\,0.2\) (in 10 \(^{5}\) population) similarly when adjusted.
Over time, the effect of stay-at-home order kept increasing significantly for all selected mental disorders across counties (Table 11 in Supplementary Appendix) and states (Table 12 in Supplementary Appendix). While school closure effect is significantly increasing for most diagnoses except for life management difficulty diagnosis where the effect kept declining.
Age effects
At the county level, all age groups, both lockdowns have positive significant effects on the mental health patients’ daily visits. Based on Table 2 , the two largest significant differences were for adults between 31 and 40 years old and adults between 21 and 30 years old. Adults in their thirties increased by 20.47% in counties with stay-at-home orders but declined by − 0.1% in counties without, with a mean difference of 3.2 (in 10 \(^5\) population, similarly when adjusted). Adults in their twenties increased more in counties with stay-at-home orders by 30.01% compared to 11% in counties without, with an estimated effect of 1.5 (in 10 \(^5\) population, similarly when adjusted). Daily visits of young patients under 11 and adolescent patients under 21 are lower in counties without stay-at-home orders with significant positive effects of stay-at-home lockdown (Table 2 ).
Similarly, school closures affected patients in their thirties but with lower mean differences of 1.9 in 10 \(^5\) population (not significant when adjusted) (Table 3 ). They increased by 18.75 vs. 18.62 in regions with and without closures respectively. While daily visits of teenagers and adolescent (11 to 20) patients increased more in counties with school closures by 27.16%, compared to 19.17% in counties without closures, with estimated effect 2.2 in 10 \(^5\) population (not significant when adjusted) (Fig. 2 in Supplementary Appendix).
Similar observations are found at the state-level based on Table 3 . For most age groups both stay-at-home and school closure orders show significant positive effects, with the largest effect size for people in their thirties. Mental health patients who are in their thirties increased by 28% and 1% in states with stay-at-home orders and without respectively. Similarly, patients in their twenties increased by 40% and 15% in states with stay-at-home order and without respectively (Table 4 in Supplementary Appendix).
The effect sizes of both lockdowns on most age groups kept increasing significantly throughout the year of 2020. Children less than 11 years old had the largest change of estimation size, which indicates a greater effect on children appeared later on in counties with stay-at-home orders (Table 11 in Supplementary Appendix).
Effects on urgent treatment-seeking
We consider daily emergency department (ED) visits to reflect the emergent need to seek a mental health facility during the COVID-19 pandemic such that the condition is so severe to avoid treatment. The ED visits are defined according to the codes in Table 1 in Supplementary Appendix.
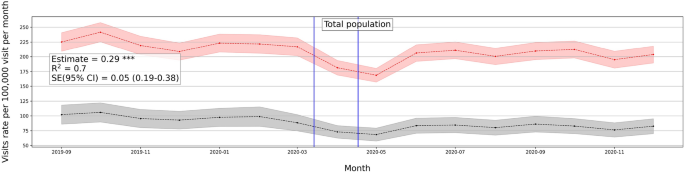
Average number of mental health ED visits over time (September 2019–December 2020) in counties with stay-at-home orders and without. Vertical lines show the first stay-at-home order on 3/14/2020 and last on 4/07/2020 across United States. Difference-in-differences estimates are included for each population. \(***p < 0.01\) , \(**p < 0.05\) , \(*p < 0.1\) .
ED visits decreased at the beginning of the pandemic, with a further finding that only patients with serious medical conditions were seeking care in ED 38 . One reason is that some patients were more willing to self-treat a variety of medical conditions than risk being exposed to COVID-19 in emergency rooms 39 . Given the role played by the ED during the first few months of the pandemic, it is linked with acute conditions for which patients could not avoid treatment
ED visits show a similar increasing positive trend in response to the lockdown measures (see Fig. 5 ). We also investigated ED visits outcomes on different population groups and the trend is consistent (Fig. 5 in Supplementary Appendix).
The effect of stay-at-home order on the overall ED visits is positive and significant with a magnitude of 0.29 weighted by population on state-level, and 0.32 when adjusted to the pandemic factor. Similarly, the effect of school closure is positive and significant with a value of 0.12 weighted by state population, same when adjusted (see Table 9 in Supplementary Appendix). Women and men groups show similar effect sizes with regard to ED visits, with an effect size of 0.2 for both groups even with adjusting for the pandemic factor. Similarly for psychiatric diagnosis, the effects are positive and significant with the largest effect size on panic disorder patients with a magnitude of 0.1 and 0.09 when adjusted. Age groups also show a similar trend of increasing daily ED visits with the largest effect size on the 21–30 age group of 0.07 and 0.05 when adjusted. Younger group ages did not show a significant effect on daily ED visits (Table 9 in Supplementary Appendix). Similar results appear for the school closures and county-level outcomes (Table 8 in Supplementary Appendix).
Robustness check
Given the differences in regions with respect to the number of hospitals, facilities, and patients, we conducted robustness checks of our main analysis to show that dropping multiple states does not change the estimates and that our results are not driven by specific regions. We dropped New York and Ohio states which were two states with the largest patient volume relative to population, and we apply our DID regression model to the weighted outcomes in states. The estimates remained robust, significant, and positive (Table 4 ). We also added all 2019 samples to expand the control group and the pre-intervention period. The relationship inferred from our analysis stayed significant and positive with this expansion.
We also conducted a similar check for ED analysis and found a similar observation of consistent robustness (Table 10 in Supplementary Appendix).
Early in March 2020, non-pharmaceutical interventions, such as social distancing policies, were imposed around the world to contain the spread of COVID-19 and proved to reduce the number of COVID-19 cases and fatalities 3 , 40 , 41 . Mitigation policies come with both costs and benefits, which may be further analyzed to help determine the optimal time to release or stop a policy intervention 42 . Prior research showed significant mental health degradation associated with the COVID-19 pandemic 6 , 7 , 18 , 19 , however, no research investigated the causal relation between COVID-19 mitigation policies and the usage of mental health resources. Yet the effects on the usage of mental health resources can further reflect the economic and health costs brought by the pandemic interventions. In our study, using large-scale medical claims data, we estimated the effects of lockdowns on the usage of mental health facilities and the prevalence of mental health issues at the state- and county levels in the United States.
Our findings demonstrate a statistically significant causal effect of lockdown measures (stay-at-home and school closure orders) on the usage of mental health facilities represented by an increasing number of issued medical claims for mental health appointments during COVID-19 pandemic. Also, ED visits were statistically significant and positive in locked-down regions which reflects the increase in emergent mental help-seeking due to the COVID-19 lockdowns. Results further emphasize the cost brought by extra months of lockdowns, in which effect sizes keep increasing through the end of 2020 in both mental health visits and ED visits. Some sub-population groups were exposed to a larger deterioration effect than other groups, such as women and adolescent groups.
Some mental health conditions were of particular interest to investigate during the COVID-19 lockdown. For example, sleep disturbance have been widely observed 43 specifically being a large concern in Italy 44 and China 45 during COVID-19 lockdown. Our results showed a similar observation, in which insomnia visits increased in counties with lockdowns. Similarly, burnout has been observed among health providers 46 and some working parents 47 during lockdown measures. Life-management difficulty disorder reflects burn-out and mental health issues in the workplace. Although this is not classified as a medical condition, but rather as an occupational phenomenon 48 , it is certainly a public health challenge 49 . Our results show that life management difficulty disorder, including burnout, increased with lockdowns at the state-level.
There have been several observations on the relation of school closures with increased mental health risks. Specifically, it was observed that some children were more likely to suffer from attention-deficit hyperactivity disorder (ADHD) symptoms during the COVID-19 pandemic 50 . This further confirms our findings of increased ADHD visits with school closures.
Our findings were observed at two granularity levels, county and state levels, with very similar trends of observations of increasing daily patient visits to mental health facilities. This further strengthens the established relationship of the effect of lockdowns on the mental health population with controlled possible sources of confoundedness. We also note our results stay the same when controlling for the evolution of the pandemic. This adds to the validity and robustness of the effects of lockdown measures on mental health despite the presence of the pandemic. It also implies that mental health is more sensitive to policy measures rather than to the evolution of the pandemic.
Given the various intertwined events and causes during the COVID-19 pandemic, our analysis is limited by several factors. First, it is important to point out that the adoption of lockdowns across states did not happen at random. Differences in shutdown orders’ timings and adoption across regions were associated with the differences in COVID-19 confirmed cases and fatality rates across those regions 51 , 52 and the differences in their health systems capacity 53 . Also, there exist other political, economical, and institutional factors that affect the adoption of COVID-19 measures and their strictness level across countries 54 . Even though the lockdown timing may be affected by regional factors related to the virus, such as the number of cases or institutional factors, however, there is no reason to believe that lockdown timing was affected by the prevalence of mental health in regions. Given that, we have also encountered regional fixed effects in our model to adjust for regional differences. Second, though mental illnesses have a negative economic impact 55 , the opposite is true as well, in which economic disadvantage may lead to a greater mental illness 56 . During COVID-19, there have been negative consequences on individuals in different industry sectors who were more likely to lose their jobs due to the lockdown measures 57 with significant employment loss in occupations that require interpersonal contact 58 . Therefore, the loss of employment due to shutdowns may have a confounding effect on increased mental health issues.
In addition, the medical claims used in this study do not cover Medicare and Medicaid health insurance programs which creates a limitation on our data. Medicare covers most aged and disabled populations across the US, while Medicare covers a wider range of populations including low-income beneficiaries covering 30% of US population 59 . This limitation would impact the representativeness of results since our data misses some population groups in the US. We also note that our medical claims dataset does not provide demographics information such as race and ethnicity. This limitation restricts our analysis to only age and gender demographics information.
Despite the mentioned limitations, our results provide important policy implications from economic and social impacts. There is a notable mental health cost brought by non-pharmaceutical interventions, especially interventions that are extended to longer duration. Our results suggest that there should be considerations to the mental health cost through ensuring mental health treatment capacity.
Furthermore, we showed that number of patients’ daily visits had dropped right after lockdowns and then progressively increased in June and July 2020, supporting the findings of Refs. 60 , 61 . This suggests that people with mental health afflictions did not have the ability to seek immediate care during restrictive lockdowns. Findings suggest that policy interventions should be accompanied by strategies that facilitate mental health treatment reachability despite restrictive lockdowns, in order to avoid the exacerbated effect of delayed treatment.
Data availability
There is a Research Data Access and Services Agreement between Change Healthcare Operations, LLC and the Board of Trustees of the University of Illinois, through which data access was granted. This work is exempt from review, as per the University of Illinois Urbana-Champaign institutional review board process. Medical claims data analyzed during the current study are not publicly available because it is under the agreement between Change Healthcare, LLC and the University of Illinois Urbana-Champaign. The NYTimes data analyzed during the current study is available in the NYTiems repository, https://github.com/nytimes/covid-19-data . The COVID-19 data analyzed during the current study is available in the COVIDVis repository, https://github.com/covidvis/covid19-vis/tree/master/data .
Thunström, L., Newbold, S. C., Finnoff, D., Ashworth, M. & Shogren, J. F. The benefits and costs of using social distancing to flatten the curve for COVID-19. J. Benefit-Cost Anal. 11 , 179–195. https://doi.org/10.1017/bca.2020.12 (2020).
Article Google Scholar
Anderson, R. M., Heesterbeek, H., Klinkenberg, D. & Hollingsworth, T. D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? The Lancet 395 , 931–934. https://doi.org/10.1016/S0140-6736(20)30567-5 (2020).
Article CAS Google Scholar
Fowler, J. H., Hill, S. J., Levin, R. & Obradovich, N. The effect of stay-at-home orders on COVID-19 cases and fatalities in the United States. MedRxiv 1 , 628. https://doi.org/10.1101/2020.04.13.20063628 (2020).
Pfefferbaum, B. & North, C. S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 383 , 510–512. https://doi.org/10.1056/NEJMp2008017 (2020).
Article CAS PubMed Google Scholar
File, T. & Marlay, M. Living Alone has More Impact on Mental Health of Young Adults than Older Adults (United States Census Bureau, 2021).
Google Scholar
Elmer, T., Mepham, K. & Stadtfeld, C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 15 , e0236337. https://doi.org/10.1371/journal.pone.0236337 (2020).
Article CAS PubMed PubMed Central Google Scholar
Adams-Prassl, A., Boneva, T., Golin, M. & Rauh, C. The Impact of the Coronavirus Lockdown on Mental Health: Evidence from the US. Cambridge Working Papers in Economics 2037 (University of Cambridge, 2020).
Wathelet, M. et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw. Open 3 , e2025591. https://doi.org/10.1001/jamanetworkopen.2020.25591 (2020).
Article PubMed PubMed Central Google Scholar
Zhu, Y. et al. The risk and prevention of novel coronavirus pneumonia infections among inpatients in psychiatric hospitals. Neurosci. Bull. 36 , 299–302. https://doi.org/10.1007/s12264-020-00476-9 (2020).
Melamed, O. C. et al. Physical health among people with serious mental illness in the face of COVID-19: Concerns and mitigation strategies. Gen. Hosp. Psychiatry 66 , 30–33. https://doi.org/10.1016/j.genhosppsych.2020.06.013 (2020).
Lee, M. et al. Human mobility trends during the early stage of the COVID-19 pandemic in the United States. PLoS ONE 15 , 1–15. https://doi.org/10.1371/journal.pone.0241468 (2020).
Musinguzi, G. & Asamoah, B. O. The science of social distancing and total lock down: Does it work? Whom does it benefit? Electron. J. Gen. Med. 17 , 230. https://doi.org/10.29333/ejgm/7895 (2020).
Le, K. & Nguyen, M. The psychological burden of the covid-19 pandemic severity. Econom. Hum. Biol. 41 , 100979 (2021).
Czeisler, M. É. et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report 32 (Centers for Disease Control and Prevention, 2020).
Abbott, A. COVID’s mental-health toll: How scientists are tracking a surge in depression. Nature 590 , 194–195. https://doi.org/10.1038/d41586-021-00175-z (2021).
Article CAS PubMed ADS Google Scholar
Giuntella, O., Hyde, K., Saccardo, S. & Sadoff, S. Lifestyle and mental health disruptions during COVID-19. Proc. Natl. Acad. Sci. U.S.A. 118 , e2016632118. https://doi.org/10.1073/pnas.2016632118 (2021).
Devaraj, S. & Patel, P. C. Change in psychological distress in response to changes in reduced mobility during the early 2020 COVID-19 pandemic: Evidence of modest effects from the US. Soc. Sci. Med. 270 , 113615. https://doi.org/10.1016/j.socscimed.2020.113615 (2021).
Article PubMed Google Scholar
Farkhad, B. F. & Albarracín, D. Insights on the implications of COVID-19 mitigation measures for mental health. Econom. Hum. Biol. 40 , 100963. https://doi.org/10.1016/j.ehb.2020.100963 (2021).
Brodeur, A., Clark, A. E., Fleched, S. & Powdthavee, N. COVID-19, lockdowns and well-being: Evidence from Google Trends. J. Public Econ. 193 , 104346. https://doi.org/10.1016/j.jpubeco.2020.104346 (2021).
Serrano-Alarcón, M., Kentikelenis, A., Mckee, M. & Stuckler, D. Impact of covid-19 lockdowns on mental health: Evidence from a quasi-natural experiment in England and Scotland. Health Econ. 31 , 284–296 (2022).
Roehrig, C. Mental disorders top the list of the most costly conditions in the United States: \$201 billion. Health Aff. 35 , 1130–1135. https://doi.org/10.1377/hlthaff.2015.1659 (2016).
Bloom, D. et al. The Global Economic Burden of Noncommunicable Diseases. Geneva. Tech. Rep (World Economic Forum, 2011).
McKenzie, K. W. S. & Whitley, R. Social capital and mental health. Br. J. Psychiatry 181 , 280–283 (2002).
Berkman, L. F. & Syme, S. L. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. Am. J. Epidemiol. 109 , 186–204 (1979).
Ferwana, I. & Varshney, L. R. Social capital dimensions are differentially associated with COVID-19 vaccinations, masks, and physical distancing. PLoS ONE 16 , e0260818 (2021).
Simon, N. M., Saxe, G. N. & Marmar, C. R. Mental health disorders related to COVID-19-related deaths. JAMA 324 , 1493–1494 (2020).
Ross, L. & Bassett, D. Causation in neuroscience: Keeping mechanism meaningful. Nat. Rev. Neurosci. 1 , 81–90 (2024).
Bommersbach, T. J., McKean, A. J., Olfson, M. & Rhee, T. G. National trends in mental health-related emergency department visits among youth, 2011–2020. JAMA 329 , 1469–1477 (2023).
Kuehn, B. M. Clinician shortage exacerbates pandemic-fueled “mental health crisis’’. JAMA 327 , 2179–2181 (2022).
Cantor, J. H., McBain, R. K., Ho, P. C., Bravata, D. M. & Whaley, C. Telehealth and in-person mental health service utilization and spending, 2019 to 2022. JAMA Health Forum 4 , e232645. https://doi.org/10.1001/jamahealthforum.2023.2645 (2023).
Times, T. N. Y. Coronavirus (Covid-19) Data in the United States. Dataset (2021).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet 395 , 912–920. https://doi.org/10.1016/S0140-6736(20)30460-8 (2020).
Keele, L. J., Small, D. S., Hsu, J. Y. & Fogarty, C. B. Patterns of effects and sensitivity analysis for differences-in-differences. http://arxiv.org/abs/1901.01869 (2019).
Zeldow, B. & Hatfield, L. A. Confounding and regression adjustment in difference-in-differences studies. Health Serv. Res. 56 , 932–941 (2021).
Angrist, J. D. & Pischke, J.-S. Mostly Harmless Econometrics: An Empiricist’s Companion (Princeton University Press, 2008).
Book Google Scholar
Goodman-Bacon, A. & Marcus, J. Using difference-in-differences to identify causal effects of COVID-19 policies. Survey Res. Methods 14 , 153–158. https://doi.org/10.18148/srm/2020.v14i2.7723 (2020).
Rambachan, A. & Roth, J. An Honest Approach to Parallel Trends. Unpublished (2020).
Hartnett, K. P. et al. Impact of the covid-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. Morb. Mortal. Wkly. Rep. 23 , 699–704 (2020).
Kocher, K. E. & Macy, M. L. Emergency department patients in the early months of the coronavirus disease 2019 (covid-19) pandemic-what have we learned? JAMA Health Forum 6 , e200705 (2020).
Friedson, A. I., McNichols, D., Sabia, J. J. & Dave, D. Did California’s Shelter-in-Place Order Work? Early Coronavirus-Related Public Health Effects. Working Paper 26992 (National Bureau of Economic Research, 2020).
Cucinotta, D. WHO declares COVID-19 a pandemic. Acta Bio-med. 91 , 157–160. https://doi.org/10.23750/abm.v91i1.9397 (2020).
Layard, R. et al. When to Release the Lockdown? A Wellbeing Framework for Analysing Costs and Benefits IZA. Discussion Papers 13186 (Institute of Labor Economics, 2020).
Gupta, R. et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J. Psychiatry 62 , 370–378. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_523_20 (2020).
Gualano, M. R., Lo Moro, G., Voglino, G., Bert, F. & Siliquini, R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int. J. Environ. Res. Public Health 17 , 4779. https://doi.org/10.3390/ijerph17134779 (2020).
Xiao, H., Zhang, Y., Kong, D., Li, S. & Yang, N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 26 , 1–8. https://doi.org/10.12659/MSM.923549 (2020).
Joshi, G. & Sharma, G. Burnout: A risk factor amongst mental health professionals during COVID-19. Asian J. Psychiatry 54 , 102300 (2020).
Aguiar, J. et al. Parental burnout and the COVID-19 pandemic: How Portuguese parents experienced lockdown measures. Fam. Relat. 70 , 927–938 (2021).
Murthy, V. H. Confronting health worker burnout and well-being. N. Engl. J. Med. 387 , 577–579 (2022).
Bailhache, M., Monnier, M. & Moulin, F. E. A. Emotional and attention-deficit/hyperactivity disorder symptoms of preterm vs full-term children during covid-19 pandemic restrictions. Pediatr. Res. 92 , 1749–1756 (2022).
Huang, X. et al. The impact of lockdown timing on COVID-19 transmission across US counties. EClinicalMedicine 38 , 101035 (2021).
Loewenthal, G. et al. COVID-19 pandemic-related lockdown: Response time is more important than its strictness. EMBO Mol. Med. 12 , e13171. https://doi.org/10.15252/emmm.202013171 (2020).
Gutkowski, V. A. Lockdown Responses to COVID-19. Tech. Rep. (Federal Reserve Bank of St. Louis, 2021).
Ferraresi, M., Kotsogiannis, C., Rizzod, L. & Secomandi, R. The ‘Great Lockdown’ and its determinants. Econ. Lett. 197 , 109628. https://doi.org/10.1016/j.econlet.2020.109628 (2020).
JoAnn, P., Dooley, D. & Huh, J. Income volatility and psychological depression. Am. J. Community Psychol. 43 , 57–70. https://doi.org/10.1007/s10464-008-9219-3 (2009).
Knapp, M. & Wong, G. Economics and mental health: The current scenario. World Psychiatry 19 , 3–14 (2020).
Fana, M., Pérez, S. T. & Fernández-Macías, E. Employment impact of Covid-19 crisis: From short term effects to long terms prospects. J. Ind. Bus. Econom. 47 , 391–410. https://doi.org/10.1007/s40812-020-00168-5 (2020).
Montenovo, L. et al. Determinants of Disparities in COVID-19 Job Losses NBER. Working Paper 27132 (National Bureau of Economic Research, 2021).
Klees, B. S. & Curtis, C. A. Brief Summaries of Medicare & Medicaid. Summary Report (Centers for Medicare & Medicaid Services, Department of Health and Human Services, 2020).
Trinkl, J. & Muñoz del Río, A. Effect of COVID-19 Pandemic on Visit Patterns for Anxiety and Depression (2020).
Patel, S. Y. et al. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern. Med. 181 , 388–391. https://doi.org/10.1001/jamainternmed.2020.5928 (2020).
Article PubMed Central Google Scholar
Download references
Acknowledgements
The authors thank the Change Healthcare team, Craig Midgett, Mina Atia, Andrew Harris, Anil Konda, Tim Suther, and Jaideep Kulkarni for facilitating our access to medical claims data and for their help in large-scale analysis.
Author information
Authors and affiliations.
Coordinated Science Laboratory, University of Illinois Urbana-Champaign, Urbana, IL, 61801, USA
Ibtihal Ferwana & Lav R. Varshney
You can also search for this author in PubMed Google Scholar
Contributions
IF was responsible for data curation, formal analysis, writing an original draft, and reviewing. LV was responsible for conceptualization, funding acquisition, methodology, reviewing, and editing.
Corresponding author
Correspondence to Ibtihal Ferwana .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Ferwana, I., Varshney, L.R. The impact of COVID-19 lockdowns on mental health patient populations in the United States. Sci Rep 14 , 5689 (2024). https://doi.org/10.1038/s41598-024-55879-9
Download citation
Received : 14 April 2023
Accepted : 27 February 2024
Published : 07 March 2024
DOI : https://doi.org/10.1038/s41598-024-55879-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Many Americans continue to experience mental health difficulties as pandemic enters second year

Note: For the latest information on this topic, read our 2022 post .
One year into the societal convulsions caused by the coronavirus pandemic , about a fifth of U.S. adults (21%) are experiencing high levels of psychological distress, including nearly three-in-ten (28%) among those who say the outbreak has changed their lives in “a major way.” The share of the public experiencing psychological distress has edged down slightly since March 2020 but remains elevated among some groups in the population. Concerns about both the personal health and the financial threats from the pandemic are associated with high levels of psychological distress.
This assessment of the public’s psychological reaction to the COVID-19 outbreak is based on surveys of members of Pew Research Center’s American Trends Panel (ATP) conducted online several times since March 2020. The mental health questions were included on three surveys. The first survey was conducted with 11,537 U.S. adults March 19-24, 2020; a second survey with the question series was conducted April 20-26, 2020, with a sample of 10,139 adults; and the most recent survey was conducted Feb. 16-21, 2021, among 10,121 adults. This analysis also includes questions asked in a survey conducted Jan. 19-24, 2021, with a sample of 10,334 adults.
The ATP is an online survey panel that is recruited through national random sampling of residential addresses. This way nearly all U.S. adults have a chance of selection. The surveys are weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Here is more information about the ATP.
The psychological distress index used here measures the total amount of mental distress that individuals reported experiencing in the past seven days. The low distress category in the index includes about half of the sample; very few in that group said they were experiencing any of the types of distress most or all of the time. The middle category includes roughly one-quarter of the sample, while the high distress category includes 21%, down slightly from 24% in March 2020. A large majority of those in the high distress group reported experiencing at least one type of distress most or all of the time in the past seven days.
The questions used to measure the levels of psychological distress were developed with the help of the COVID-19 and mental health measurement group from Johns Hopkins Bloomberg School of Public Health (JHSPH): M. Daniele Fallin (JHSPH), Calliope Holingue (Kennedy Krieger Institute, JHSPH), Renee Johnson (JHSPH), Luke Kalb (Kennedy Krieger Institute, JHSPH), Frauke Kreuter (University of Maryland, Ludwig-Maximilians University of Munich), Elizabeth Stuart (JHSPH), Johannes Thrul (JHSPH) and Cindy Veldhuis (Columbia University).
Here are the mental health questions used for this analysis, along with responses, and the detailed survey methodology statements for March 2020 , late April 2020 and February 2021 .
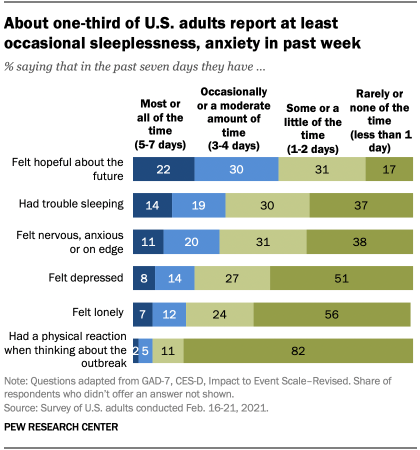
The index of psychological distress is based on a set of five questions asking about anxiety, sleeplessness, depression, loneliness and physical symptoms of distress. Except for the last item, the questions do not explicitly mention the pandemic. But experts have documented that fear and isolation associated with the pandemic have been responsible for a surge of anxiety and depression over the past year. And on the one item that asks about physical reactions when thinking about coronavirus outbreak – such as sweating, trouble breathing, nausea or a pounding heart – 17% report having such reactions at least “some or a little of the time” in the past week.
The five items were combined to create an index, which was then grouped into three categories: high, medium and low distress. The questions were part of a survey conducted online Feb. 16-21 among 10,121 members of Pew Research Center’s American Trends Panel. Most of those interviewed had also participated in last year’s surveys about reactions to the pandemic.
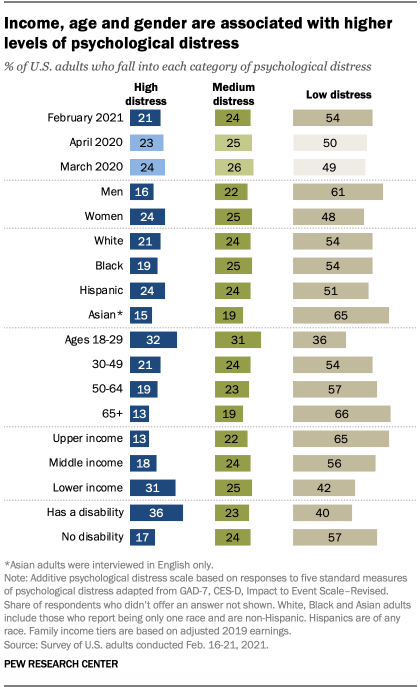
High levels of distress are being experienced by those who say the coronavirus outbreak is a major threat to their personal financial situation (34% high distress) or to their personal health (28%). Psychological distress is especially common among adults ages 18 to 29 (32%), those with lower family incomes (31%) and those who have a disability or health condition that keeps them from participating fully in work, school, housework or other activities (36%).
The share of adults falling into the high distress group (21%) is now slightly lower than in March of last year: It was 24% then, near the beginning of coronavirus-related lockdowns in the U.S.
Underneath the relative stability of the index, considerable change has occurred. About six-in-ten (61%) of those interviewed in both April 2020 and February 2021 remained in the same category of the index. Just over a fifth (22%) moved from a higher to a lower category of distress, while 16% moved from a lower to a higher category. Of all panelists interviewed in both April 2020 and February 2021, 12% were classified as high in psychological distress in both interviews and 40% were low in both.
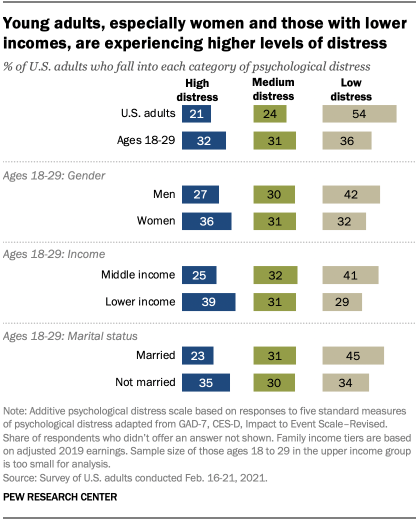
Young people have been a particular group of concern during the pandemic for mental health professionals, and young adults stand out in the current survey for exhibiting higher levels of psychological distress than other age groups. The shutdowns have disrupted job opportunities, college experiences, and the mixing and mingling that marks the transition to adulthood. Among adults ages 18 to 29, women (36%) and those with lower incomes (39%) are especially likely to be in the high distress group. In this age group, those who are unmarried fare worse than the married (35% vs. 23% experienced high levels of distress, respectively).
Adults ages 18 to 29 are especially likely to report anxiety, depression or loneliness compared with other age groups. For example, 45% of those under 30 describe being “nervous, anxious or on edge” at least “occasionally or a moderate amount of time” during the past seven days; among those 30 and older, 28% do so.
Not surprisingly, psychological distress is higher among those who express concern about becoming ill with COVID-19 or believe that the disease is a major threat to their personal health. Among those who are “very concerned” that they might get infected and require hospitalization, 27% score high in psychological distress, compared with just 14% among those who are not too or not at all concerned. Similarly, 27% of those who see the disease as a major threat to their personal health score high in psychological distress, compared with 11% who say it is not a threat. Distress levels are also higher among those who perceive the sign-up process for a coronavirus vaccine in their area as unfair or who say that it has not been easy to find information about the process.
As much as concern about the health implications of the pandemic may be affecting the mental health status of many Americans, financial troubles are also a strong correlate of psychological distress. Pew Research Center surveys, including this one, have documented the substantial negative impact of the pandemic on the financial situation of many Americans. A January survey found that more than four-in-ten adults said that they or someone in their household had lost a job or wages since the beginning of the outbreak, and significant shares of the unemployed acknowledged the emotional toll it had taken.
Among those interviewed in the current survey who say that the pandemic is a major threat to their personal financial situation, 34% are classified as being in high psychological distress. Even greater levels of distress are observed among those who said in a January interview that they worry about how to pay their bills “every day” (40% high psychological distress) or who said they are in “poor” shape financially (44%).
Note: Here are the mental health questions used for this analysis, along with responses, and the detailed survey methodology statements for March 2020 , late April 2020 and February 2021 .
- Coronavirus (COVID-19)
- COVID-19 & Science
- Happiness & Life Satisfaction
Scott Keeter is a senior survey advisor at Pew Research Center .
How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, mental health and the pandemic: what u.s. surveys have found, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
© 2024 Pew Research Center
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and respiratory illness
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.
Large study reveals clearer links between COVID-19, mental health risks

Marcos Calvo / iStock
In a large US study that tracked people for as long as a year, COVID-19 patients had a 60% higher risk of mental disorders such as anxiety, depression, or substance abuse compared with those who weren't sickened by the virus.
Given the large number of people infected with COVID-19, the findings suggest that nations should take more steps to tackle the growing challenge of managing mental health conditions in survivors. Researchers based at the Veterans Administration (VA) and Washington University in St. Louis published their findings yesterday in The BMJ .
Senior author Ziyad Al-Aly, MD , clinical epidemiologist at Washington University in St. Louis, said in a news release from the school, "But while we've all suffered during the pandemic, people who have had COVID-19 fare far worse mentally. We need to acknowledge this reality and address these conditions now before they balloon into a much larger mental health crisis."
Probing a range of mental health impacts
Earlier studies have drawn links between COVID-19 illness and mental health conditions, but the new study is the largest known to date, harnessing information from 153,848 patients who tested positive for COVID-19 from Mar 1, 2020, to Jan 15, 2021, in a database from the Department of Veterans Affairs, which is the nation's largest integrated health delivery system.
For comparison, the researchers assessed mental health conditions in two control groups: 5.6 million who weren't sick with COVID-19 during the same period, and more than 5.6 million patients who were in the VA system before the pandemic began.
The authors emphasized that the study period they focused on came before vaccines were widely available and before the Delta and Omicron variant waves took place. And though most of the patients in the dataset are older white men, its large size included more than 1.3 million women, more than 2.1 million Blacks, and large numbers of people of different age-groups.
When the team drilled down into specific mental health issues, they found a 35% higher risk of anxiety in the COVID-19 group, a 39% higher risk of depression, and a 41% higher risk of sleep disorders. People who recovered from COVID-19 were 80% more likely to experience neurocognitive decline—a constellation of symptoms known as "brain fog."
And for treatment for mental health conditions, the investigators found a 55% increase in the use of antidepressants and a 65% jump in benzodiazepines for treating anxiety. They also found a 76% higher risk of opioid use, 34% higher risk of opioid use disorder, and a 20% higher risk for the use of other substances.
Unique to COVID? Typical after hospitalization?
To assess patterns that they found were unique to COVID-19, the researchers compared the COVID-19 patients with those in the database who had flu, including hospitalization for the condition, in the three flu seasons leading up to start of the pandemic.
The risk of mental health conditions was still significantly higher in COVID-19 patients: 27% in those with mild infection and 45% in those who were hospitalized.
Al-Aly said, "My hope is that this dispels the notion that COVID-19 is like the flu. It's so much more serious."
Because hospital stays are known to provoke anxiety, depression, and other conditions, the team compared those hospitalized for COVID-19 during the first 30 days of infection with those hospitalized for any other cause. Mental health conditions were 86% more likely in those who were hospitalized for COVID-19.
Though the findings suggest a link between COVID-19 and mental health disorders, Al-Aly said a leading hypothesis is that the virus can enter the brain and disrupt cellular and neuron pathways, leading to mental disorders.
Take-home messages from the study are that the best defense against long COVID is to avoid contracting COVID-19 in the first place by getting vaccinated and wearing quality masks, the authors said. First author Yan Xie, PhD, an epidemiologist with the VA St Louis Epidemiology Center, said she hopes the study's findings will raise awareness to make the conditions easier for health providers to identify and treat.
Prioritizing mental health with COVID-19
In a related editorial in the same issue, Scott Weich, MD, professor of mental health at the University of Sheffield in England, said the study paints a clearer picture of COVID-19's mental health impacts.
For the general population, the pandemic setting and lockdown caused transient distress related to the threat. But those who contracted the virus had a moderately increased risk of anxiety and depression, mainly for the first 6 months but greatest in the first month.
He said the bulk of the research on the mental health impact of COVID-19 represents more hindsight than insight and that, moving forward, investigations need to focus on understanding the causes and evaluating treatments for mental health conditions more generally.
"We do not yet know the true incidence and consequences of long covid, and we are still witnessing the unfolding toll of the pandemic on healthcare staff," he wrote. "And while epidemiological research has flourished—at least in terms of scientific publications—we are guilty of failing to prioritise evaluations of mental healthcare interventions, including clinical trials, just when these are most needed."
Related news
Ahrq survey: 7% of us adults reported having long covid by early 2023.

Paxlovid fails to improve long-COVID symptoms in small study

FDA panel supports switch to JN.1 for fall COVID vaccines

Report: More than 200 symptoms tied to long COVID

Placing COVID patients in skilled nursing facilities led to increased cases, deaths, study finds

N95 respirator gets top billing in stopping SARS-CoV-2 viral leakage into the air

WHA approves new IHR amendments, resets timeline for pandemic agreement negotiations

Early use of antivirals linked to reduced risk of long COVID


This week's top reads
Man dies after h5n2 avian flu in mexico; minnesota reports first case in dairy cow.
Minnesota and Iowa report infected dairy herds.

H5 influenza wastewater dashboard launches
Though the test can't pinpoint the virus subtype or source, most of the detections are from states hard hit by H5N1 in dairy herds.

The report "offers a comprehensive review of the evidence base for how Long COVID may impact a patient's ability to engage in normal activities."

Report describes emerging sexually transmitted fungal infection
The infection is caused by Trichophyton mentagrophytes type VII, a fungus that may spread via sexual contact.
The "duckbill" N95 stopped 98% of the virus that causes COVID-19, the authors say.

CDC: Cucumber-linked Salmonella outbreak sickens 162 in 25 states, Washington DC
Fifty-four people have been hospitalized, with no deaths reported.

Though the vote was unanimous, discussions were complicated by the diversity of JN.1 viruses.

Early oral antiviral drug administration was associated with a 23% reduction in long COVID overall.

Excess death rates due to pandemic persisted in Western countries
In 2020, 1,033,122 excess deaths were recorded, and that number rose in 2021 to 1,256, 942.
Although a 15-day course of Paxlovid was found to be safe, it didn't demonstrate a significant benefit in improving symptoms.

Our underwriters
Unrestricted financial support provided by.

- Antimicrobial Resistance
- Chronic Wasting Disease
- All Topics A-Z
- Resilient Drug Supply
- Influenza Vaccines Roadmap
- CIDRAP Leadership Forum
- Roadmap Development
- Coronavirus Vaccines Roadmap
- Antimicrobial Stewardship
- Osterholm Update
- Newsletters
- About CIDRAP
- CIDRAP in the News
- Our Director
- Osterholm in the Press
- Shop Merchandise
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Measuring Mental Distress Amid a Pandemic
Understanding COVID-19’s Psychological Effects Over Time
The disruptions of the COVID-19 pandemic—mandatory masks, social distancing, remote school and work—have touched every facet of our lives, including our mental health.
In the early days of the outbreak, mental health experts at Johns Hopkins Bloomberg School of Public Health saw a need to better understand and measure mental distress in the context of a pandemic. To that end, a working group within the School’s Department of Mental Health developed key questions to add to existing large domestic and international surveys to measure the mental health impact of the pandemic.
Some of the initial results of the surveys, which began in March and are continuing, indicate that mental distress has increased in the current coronavirus pandemic, with particularly large increases early on in the states hardest hit.
Contributors to the effort discuss the rationale behind the research initiative and share preliminary results below.
Why is understanding mental distress important?
“We collect these data because we know that stressful things like pandemics affect population mental health,” says Calliope Holingue, PhD, MPH, postdoctoral fellow in Mental Health and the Department of Neuropsychology at the Kennedy Krieger Institute. “The purpose of capturing longitudinal data across time, across sociodemographics, is to see who gets better and why, which helps us design and implement better interventions and treatments.”
“We need to ensure that individuals with need for services receive those, in the current environment,” says Elizabeth Stuart, PhD , associate dean for Education and professor in Mental Health. “To help identify where that need will be, we need good measurement of distress in communities.”
How did the research team develop the survey questions?
The survey questions draw on mental health studies during other large-scale disasters, including the 2003 SARS epidemic. Questions about feelings of anxiety, depression, loneliness, hopelessness, physical reactions to stressors, and existing diagnoses of a mental disorder were adapted and submitted to a number of research surveys, including the Pew Research Center American Trends Panel, the Understanding America Study, and others in the U.S. and abroad.
“The benefit of embedding these measures into existing surveys is that they already collect important data including race, socioeconomic status, employment, even measures on social media use,” says Johannes Thrul, PhD , assistant professor in Mental Health. “Adapting established questions by simply changing the look-back period to seven days, for example, is a very efficient way to look at predictors of higher mental distress during a rapidly evolving situation like this.”
What do the preliminary results show?
- Mental distress in the general population is rising. In early March, hotspot states like California, Washington, New York, and Massachusetts, saw that mental distress significantly increased even after adjusting for factors like age and income. This was a critical time frame to start to understand mental health in the population: a national emergency had just been declared, schools were closing, and workplaces were shutting down. Other states had a smaller increase in distress at that time. However, these geographic differences in mental distress may become less pronounced as the pandemic continues.
- Mental distress is higher in younger individuals than in older populations. Because of medical complications related to COVID-19 among older individuals, researchers expected to see the opposite. Continued data collection is needed to see how age is related to changes in mental health symptoms due to the pandemic.
- The initial survey results also showed that individuals with more frequent use of traditional media (newspapers, TV, radio) and social media had higher levels of mental distress. The findings suggest spending more time engaged with the media may contribute to distress during the pandemic. However, given the restrictions imposed on in-person interactions by social distancing, more research is needed to understand what types of media engagement might be helpful for supporting mental health.
- Individuals who had consumed cannabis and alcohol more frequently in the past week had significantly higher mental distress. Whether the cannabis and alcohol use led to the mental distress, or vice versa, cannot be determined from the current data, but these early results suggest that substance use is not an effective strategy for coping with COVID-19-related stressors.
How do we move forward?
Collecting longitudinal data will be particularly helpful.
“Over time, some people who reported distress earlier on may have other characteristics that allow them to cope better than others,” says Thrul. “Long-term research will help understand and differentiate what may be predictors of a more adverse outcome versus a more positive outcome after an initial distress signal.”
Stuart says other key questions include: “Are there preventive actions we can take right now to improve mental health? How do we ensure individuals get the services they need as the situation evolves? And ultimately, what are the services and treatments that help people manage their current distress, and prevent future problems? That is the type of information we want to learn.”
The Johns Hopkins COVID-19 Mental Health Measurement Working Group includes M. Daniele Fallin, Mental Health chair, Renee M. Johnson, Kira Riehm, Elizabeth Stuart, and Johannes Thrul (Johns Hopkins Bloomberg School of Public Health, Department of Mental Health); Calliope Holingue and Luke Kalb (Johns Hopkins Bloomberg School of Public Health, Department of Mental Health, and Kennedy Krieger Institute); Frauke Kreuter (University of Maryland and University of Mannheim); and Cindy Veldhius (Columbia University School of Nursing).
RELATED CONTENT
- COVID-19 Mental Health Care Q&A With a Clinical Psychologist
Related Content

How to Offer Support and Find Strength on a Trauma Anniversary

Mental Health in the Workplace: A Conversation Bridging Research and Practice

Activity, Sleep & Dementia

Rev. Pamula Yerby-Hammack Breaking the Stigma of Mental Health

Inside the Movement to Transform Mental Health in Sierra Leone
Depression and Anxiety in Long COVID: Why Interdisciplinary Treatment Is Needed
BY BROOKS LEITNER June 10, 2024
In the spring of 2022, Helen C.* began experiencing a strange mental "fogginess." Simple words slipped from her grasp during conversations, her job became a challenge, and fatigue was a constant companion. She started losing weight and found it harder and harder to concentrate.
Not long thereafter, Helen, with no prior history of mental health issues and a supportive family, ended up in a psychiatric hospital for severe depression, pronounced weight loss, significant weakness, and a sudden onset of anxiety based on a false belief that she had cancer. After an inpatient stay, she left with a prescription for antidepressants. The sudden downturn of her mental health puzzled those close to her. The only noteworthy events in her recent medical history? Two bouts of COVID-19.
This scenario is not unique. Ebony Dix , MD, assistant professor of psychiatry at Yale School of Medicine (YSM), who oversaw the Inpatient COVID Psychiatry Unit at Yale New Haven Hospital in 2022, observed a similar pattern in some of her patients. Dr. Dix often found herself asking, "Could their new depression or anxiety be linked to COVID-19 and, if so, when did they have it?"
Does COVID-19 raise the risk for depression and anxiety?
For Helen, whose condition was detailed in a case report published in Frontiers in Psychiatry , a combination of antidepressant medication and various non-drug therapies—including visual art, music, physical therapy, and psychotherapy—relieved her depressive symptoms. But how common is a story like hers?
Research suggests that as many as 90% of individuals hospitalized with COVID-19 and 25% of non-hospitalized adults experience at least one brain or mind-related symptom, including fatigue, headache, sleep disturbances, depression, or anxiety, six months after the illness. Symptoms of depression, which have been shown to generally decrease as more time passes following COVID-19, can include a loss of interest in activities, feeling down or hopeless, difficulty sleeping, low energy, and trouble concentrating. Anxiety symptoms, which also have been found to ease as more time passes post-COVID-19, involve constant worrying, feeling nervous or on edge, irritability, and finding it difficult to relax. With a significant portion of patients experiencing these symptoms, the question arises: Is COVID-19 causing changes to the brain?
Does COVID-19 cause inflammation in the brain?
An article published in Neuron notes that SARS-CoV-2, the virus that causes COVID-19, may trigger inflammation in the brain through various potential pathways. For example, COVID-19 can induce severe inflammation in the body that may lead to the spillover of inflammatory molecules into the brain, causing damage from inflammation originating outside of the brain. The virus may also directly affect the brain, in particular causing damage to two types of cells crucial for brain activity and repair: neurons (the brain cells) and glial cells (the support cells). This damage may contribute to such symptoms as fatigue, brain fog, memory issues, as well as depression and anxiety. Other potential mechanisms are also being explored to explain COVID-19’s effect on the brain.
Additional research has identified another piece of the puzzle concerning the development of depression and anxiety. Scientists comparing blood samples from hundreds of individuals both with and without Long COVID discovered that patients experiencing persistent Long COVID symptoms had low levels of serotonin. Often referred to as a “natural mood booster,” serotonin is a vital neurotransmitter that regulates mood, memory, and other brain functions. Notably, popular antidepressant medications like Prozac or Zoloft, known as selective serotonin reuptake inhibitors (SSRIs), aim to boost serotonin levels in the brain. This research suggests a potential link between serotonin and Long COVID-associated depression.
COVID-19 can impair normal metabolism in the brain
Scientists, using a brain-imaging technique called a PET scan, have discovered another oddity . In a study of 35 patients with Long COVID, researchers at the Aix-Marseille University, in Marseille, France, found that patients with persistent cognitive symptoms three weeks after infection, including pain, insomnia, and memory impairments, had a reduction in the level of glucose uptake (hypometabolism) in their brain. This impaired glucose metabolism, which fuels normal brain function, could specifically be linked to depressive symptoms, including insomnia.
Another study conducted in France involved 143 patients with Long COVID at an average of 11 months after their COVID infection. The study showed that about half of patients had reduced glucose metabolism in the brain. This additional piece of evidence not only links impaired brain metabolism to neuropsychiatric symptoms, but also demonstrates the heterogeneity in the patient biology underlying Long COVID.
How do we treat depression and anxiety related to Long COVID?
As was the case for Helen, treating depression and anxiety often involves a combination of approaches. While there are various medications, like SSRIs, available to address symptoms, patients may also engage in a range of behavior changes and therapies. These include cognitive behavioral therapy (CBT), which can be done in person with a therapist or online through telehealth services. Patients may also explore mind-body approaches, such as meditation, yoga, or relaxation techniques, to relieve anxiety symptoms.
The U.S. Department of Health and Human Services (HHS) has also recognized the toll that Long COVID can take on one’s mental health. In an advisory issued in June 2023, HHS warned that Long COVID can have "devastating effects on the mental health of those who experience it, as well as their families," stemming not only from the illness itself but also from “social isolation, financial insecurity, caregiver burnout, and grief.”
The Substance Abuse and Mental Health Services Administration (SAMHSA) has also issued an advisory , which encourages doctors to look for psychiatric symptoms as well as physical symptoms to identify and diagnose Long COVID. The SAMHSA recommends an interdisciplinary treatment approach that may include physical medicine and rehabilitation, individual and group psychotherapy, and neurorehabilitation.
Indeed, effectively dealing with Long COVID-related depression and anxiety often requires different tools from the healthcare toolkit. The most successful outcomes usually stem from a strong partnership between the patient and their care team. Dr. Dix emphasizes the importance of "collaboration between psychiatry and other medical disciplines" for impactful treatment. This comprehensive approach ensures that the whole person is cared for.
*Not her real name.
Brooks Leitner is an MD/PhD candidate at Yale School of Medicine.
The last word from Lisa Sanders, MD:
Depression and anxiety are two of the most common symptoms of Long COVID. While many may think it is reasonable to be depressed or anxious when you continue to feel bad weeks, months, or even years after an infection, research suggests that for some of these patients, the depression or anxiety isn’t caused by Long COVID but is, instead, part of it. As with so many of the symptoms of Long COVID, the emotional turmoil caused by the disease seems to respond to the same medical and therapeutic approach that has been used for others with these diseases.
Perhaps a better understanding of what causes the depression and anxiety of Long COVID will provide us with other more targeted treatments. And perhaps that understanding will not only reveal something about SARS-CoV-2’s effect on the brain, but also about the physiology of depression and anxiety in the rest of us.
Read other installments of Long COVID Dispatches here .
If you’d like to share your experience with Long COVID for possible use in a future post (under a pseudonym), write to us at: LongCovid [email protected]
Information provided in Yale Medicine content is for general informational purposes only. It should never be used as a substitute for medical advice from your doctor or other qualified clinician. Always seek the individual advice of your health care provider with any questions you have regarding a medical condition.
More news from Yale Medicine
- Research article
- Open access
- Published: 31 May 2022
Mental health provider perspectives of the COVID-19 pandemic impact on service delivery: a focus on challenges in remote engagement, suicide risk assessment, and treatment of psychosis
- Lindsay A. Bornheimer 1 , 2 ,
- Juliann Li Verdugo 1 ,
- Joshua Holzworth 1 ,
- Fonda N. Smith 1 &
- Joseph A. Himle 1 , 2
BMC Health Services Research volume 22 , Article number: 718 ( 2022 ) Cite this article
2851 Accesses
9 Citations
7 Altmetric
Metrics details
The COVID-19 pandemic has been impacting the need, utilization, and delivery of mental health services with greater challenges being faced by clients and providers. With many clients facing reduced access to services and social isolation, a focus on suicide risk assessment and prevention is critical. Concern is particularly increased for clients with schizophrenia spectrum disorders given data show suicide rates are disproportionately high for those with psychosis in comparison to the general population. Provider perspectives of challenges in service delivery are needed to inform efforts to improve access, feasibility, and quality of mental health care throughout the evolving pandemic. This study explored mental health provider perspectives of client challenges in service utilization and provider challenges in service delivery, including remote engagement, suicide risk assessment, and treatment of psychosis.
Data were collected from social work mental health providers ( n = 12) in United States community mental health setting. Providers consented to participate and responded to questions about service delivery experiences in late 2020 and in relation to COVID-19. Demographic and practice-related provider data were explored descriptively using SPSS and qualitative data using open coding and grounded theory methods in Dedoose.
Among the 9 providers who engaged in remote service delivery, 7 (77.8%) experienced challenges in remote engagement with clients and 8 (88.9%) experienced challenges in treatment of psychosis. Among the 7 providers who engaged in remote suicide assessment, 4(57%) experienced challenges. Qualitative themes emerged including logistic (e.g., technology access and use), engagement (e.g., virtual rapport-building and limited remote services), and clinical (e.g., difficulty assessing suicide risk, internal stimuli, abnormal involuntary movement, and affect) challenges in service delivery.
Conclusions
Provider perspectives are essential to inform efforts to build resources and problem-solve challenges and barriers that both providers and clients face throughout various shifts in mental health service delivery. Findings emphasize the need to troubleshoot client access to technology, bolster support for providers to prevent burnout, and greater provider training to improve skills in remote engagement, assessment, and treatment, particularly in relation to psychosis and suicide prevention. Study implications are not only critical for the evolving COVID-19 pandemic, but also in preparation for ongoing shifts in service delivery as technology evolves.
Peer Review reports
Introduction
The COVID-19 pandemic has led to substantial psychological impact in the United States and worldwide [ 1 , 2 , 3 ]. For many individuals, mental health needs have been rising throughout the pandemic’s progression [ 4 ], with adjustment-related impacts of quarantine, health anxiety, economic and financial stressors, social isolation, and more [ 5 , 6 ]. Aligning with preexisting epidemic and outbreak-related studies [ 7 , 8 , 9 ], the COVID-19 pandemic has prompted greater anxiety and depression [ 10 ], social isolation [ 11 ], and risk for suicide [ 12 ]. While the pandemic’s impact on mental health has been increasingly investigated, greater understandings of its impact on mental health services and delivery are needed from the perspective of mental health providers. Furthermore, and importantly, less is known to date about challenges providers community mental health (CMH) face in remote assessment and treatment of psychosis and suicide risk in the United States.
Suicide is a critical public health problem and leading cause of preventable death among individuals with schizophrenia spectrum and other psychotic disorders [ 13 ], Bornheimer, 2020) [ 14 ]. Data estimate the risk for suicide among individuals with schizophrenia spectrum disorders is over eight times greater than the general population [ 15 ]. It is predicted that short- and long-term impact of the COVID-19 pandemic may disproportionately affect individuals with psychosis [ 16 ] and given the potential for worsening mental health symptoms [ 6 ], there are rising concerns of suicide risk within this population [ 17 ]. As a result, it is essential that mental health providers gain skills to effectively conduct comprehensive suicide-risk assessments, formulate levels of risk, and deliver treatments and services to reduce risk and prevent death. Furthermore, CMH settings are well-positioned to engage in suicide prevention efforts as they are among the largest providers of outpatient behavioral health in the United States, and particularly so for clients with serious mental illness and psychosis [ 18 ].
Service delivery has increasingly shifted to telehealth and virtual formats throughout the COVID-19 pandemic with notable impact on individuals seeking care, mental health providers adjusting to remote service delivery, and an increased need for mental health services [ 19 , 20 ]. In the United States in particular, the demand for mental health services have remarkably increased [ 21 ]. Across the globe and within numerous individual contexts, there are varying perceptions about and experiences with virtual healthcare services among providers and clients. For some clients, virtual services increase accessibility to care, and for others, technology barriers have made care more inaccessible when face-to-face services are not an option [ 22 ]. Among providers, there is a similar spread of virtual services being experienced as acceptable and effective in practice, yet also challenging given technology access and clinical barriers (e.g., not being able to observe certain nonverbal cues and less privacy) that may arise [ 1 , 23 , 24 ]. One qualitative study exploring healthcare provider experiences during the pandemic yielded themes of a prevailing sense of helplessness, overwhelming workloads for providers, and increased mental health decline among clients [ 25 ]. It is evident that providers have been impacted throughout the onset and progression of the COVID-19 pandemic. While the pandemic’s overall impact on mental health services is increasingly investigated, greater understandings are needed from provider perspectives regarding the impact on service delivery in United States CMH settings, such as perceived challenges of clients receiving treatment and provider challenges in workload, engagement, assessment, and treatment. The CMH context in the United States is particularly important, given many clients engaging in community-based mental health services reside in low-income, underserved, or rural areas with less access to technology [ 22 ]. Additionally, there are gaps in knowledge about the pandemic’s impact on provider assessment and treatment of both symptoms of psychosis and suicide risk. In particular, the remote nature of service delivery likely poses complexities in client engagement, assessment of mental status and symptoms, and delivery of behavioral interventions.
Given ongoing changes in mental health service delivery and increased need for care, emerging research from the perspective of providers in CMH is particularly vital to inform clinical practice and future research aiming to disseminate mental health services in mental health service systems. The current study explored provider perspectives of mental health services and delivery challenges in relation to the COVID-19 pandemic with specific focus on providing services to individuals with psychosis symptoms and at risk for suicide.
Data were collected as part of a National Institute of Mental Health (NIMH)-funded study (R34MH123609; PI: Bornheimer) focused on suicide prevention among adults with psychosis in a CMH setting. As a first step in the study, survey data were collected in the fall of 2020 to explore the impact of the COVID-19 pandemic on providers delivering mental health services. This manuscript presents our pandemic-related demographic and qualitative data among social work mental health providers in a CMH setting and aligns with the consolidated criteria for reporting qualitative studies (COREQ; [ 26 ].
Setting, Participants, and Procedures
A total of 12 mental health providers in a midwestern CMH setting of the United States participated in this study. Using purposive sampling methods, providers were recruited through informational presentations given in virtual provider staff meetings. This CMH setting provides mental health services to adults with severe mental illness and developmental disability, offering a breadth of programs including crisis residential services, case management, outpatient mental health, medication management, assertive community treatment (ACT), and more. Prior to the pandemic, the majority of services in this CMH setting were delivered in-person (e.g., individual and group psychotherapy, psychiatric evaluations, medication management, and case management), with few services being delivered outside of CMH facilities (e.g., ACT for clients with serious and persistent mental illness involving multidisciplinary care in their home and community). The range of attendance in the CMH facility ranged by service type, with some clients attending multiple times a week for therapeutic services, many attending once or twice a month for case management and medication management, and a smaller subset attending every few months. Once the pandemic began to impact this region of the United States in early 2020, many services became limited for CMH clients (e.g., case management, medication management, and therapy sessions occurred less often than typical) and some services were temporarily discontinued (e.g., group psychotherapy). Importantly, and uncommon in CMH prior to the pandemic, teletherapy and virtual service delivery became a standard approach to care when local lockdowns occurred, and safety protocols were put in place with less in-person access to the CMH facility to prevent the spread of COVID-19. ACT continued in the community with home visits being completed less frequently, while the remaining CMH services were primarily virtual with clients having limited in-person access to the CMH facility for more than 1 year. This CMH setting also represents a public mental health system encompassing the diversity of the midwestern United States (race, ethnicity, socioeconomic status, organizational services, insurance/payment types, etc.). Currently the site is serving over 700 clients with schizophrenia spectrum disorders and this region of the United States has a rate of 14.3 deaths per 100,000 total population suicide, which is a 33% increase since 1999 [ 27 ].
Providers were given a link to view and sign a written consent form via Research Electronic Data Capture (REDCap) software and subsequently responded to qualitative questions related to the COVID-19 pandemic (described in the measurement section below). Recruitment and data collection continued until saturation was reached [ 28 ]. All data were collected between November and December of 2020 and Institutional Review Board approval was obtained.
Measurement
Qualitative COVID-19-related questions were preceded by introductory questions about demographic characteristics (e.g., provider age and gender) and practice-related characteristics (e.g., provider license type and duration of practice experience) to increase understandings of the sample. Data collection involved approximately 30 min of time for providers. Prior to question design, it was apparent in conversations with staff and leadership in the CMH setting that many challenges were being faced by clients and providers, thus, questions were focused on challenges with the goal of gaining understandings of potential barriers to service delivery to develop potential solutions and strategies for challenge mitigation. A total of 5 qualitative questions were established by the investigative team, with prior experience in developing qualitative questions, and sought to explore the following within the COVID-19 pandemic-context: 1) provider observations of challenges related to telehealth and virtual services, 2) provider workload changes, 3) challenges experienced in remote engagements with clients, 4) challenges related to engagement with clients who experience symptoms of psychosis, and 5) challenges related to remote suicide assessment. As shown in Fig. 1 , qualitative questions were preceded by introductory yes/no questions related to challenges being present, and an additional qualitative question was asked at the end of the survey to gather any additional information, experiences, or observations.
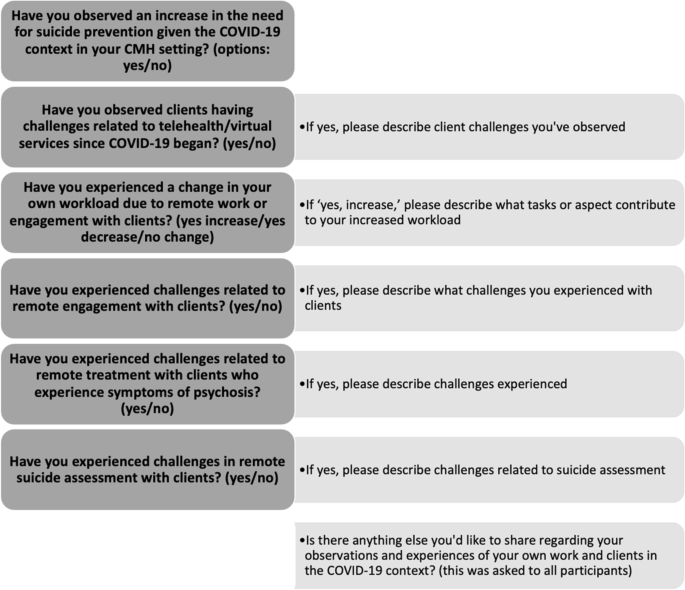
Questions given to providers
Data Analysis
Demographic and practice-related data were viewed using SPSS27 (e.g., number and percentage for categorical information, means and standard deviations for continuous information) and qualitative question data analyzed using Dedoose. We first viewed demographic and practice-related data to better understand the sample, followed by qualitative question data analysis with an aim of expanding on descriptive details of the sample (Creswell et al., 2017) [ 29 ]. For open-ended qualitative questions, responses were independently coded by two Master’s-level research assistants (JLV and JH) in preparation for codebook development. An open coding technique was used to generate themes across the 6 qualitative questions (Saldana, 2016) [ 30 ] and grounded theory methods were utilized for analysis [ 31 ]. After an initial round of coding, the lead author (LAB) met with both research assistants to discuss emerging themes from the qualitative data, reviewed field notes from the coding process, and agreed upon a codebook. The research assistants conducted a second round of coding with use of the established codebook and the lead author resolved any disagreements to achieve inter-coder consistency. Themes were ultimately organized into a final framework and findings are presented in the results section below. Strategies for qualitative rigor [ 32 ] in the current study include: 1) analytic triangulation (i.e., more than one qualitative coder was involved), 2) audit trail, and 3) member checking.
Demographic and practice-related provider data are presented in Table 1 . Providers ( n = 12) were on average 35.67 years of age (SD = 6.387), most often identified as female ( n = 8, 66.7%), and all ( n = 12) identified as White and non-Hispanic/Latinx. As is common in CMH settings in the US, all providers identified as social workers with 11 having a master’s degree in social work and 1 reporting being currently enrolled in a social work master’s degree program. Providers either had a social work license (LMSW or LCSW; n = 9, 75%), limited social work license (LLMSW; n = 2, 16.67%), or were a Master of Social Work Student in training (MSW student; n = 1. 8.33%). All providers ( n = 12) endorsed having direct contact with clients with the majority in a mental health therapist, clinician, or case manager role ( n = 10, 83.3%). The average duration of work experience providing services in the mental health field was 5 years and 10 months (SD = 4 years and 1 month) with a range from 6 months to 14 years. The average duration of work experience in their current CMH setting was 4 years and 6 months (SD = 3 years and 1 month).
Provider Observations of Client Challenges
All qualitative data findings are presented in Table 2 . The majority of providers (66.7%, n = 8) observed clients having challenges related to diminished access to telehealth and virtual mental health services during the COVID-19 pandemic. Challenges observed by providers resulted in 3 themes: 1) logistic challenges (qualitative responses: limited availability of a device capable for video and internet, government-supported phones do not always accept restricted calls from providers who use a blocked number), 2) engagement challenges (less ability to engage in individual and group therapy, less comfort engaging with providers remotely, lower therapeutic rapport), and 3) clinical challenges (more agitation, more physical altercations, heightened anxiety, and increased social isolation). Providers shared the following:
“Clients have limited access to devices capable of all telehealth modalities. Also, doc [doctor] phone numbers come through restricted numbers and some government-supported phones do not accept restricted phone numbers, so when docs are working remotely, certain clients cannot be contacted for even a phone visit by a prescriber.” -provider 1
“I’ve seen more agitation in general with clients, specifically during the actual ‘stay home’ period of the pandemic. I had incidents of physical altercations? between residents in homes where there had been little or no signs of aggression in several years.” -provider 3
“Prior to the pandemic, our clients were socially isolated due to the nature of severe mental illness. Now they are even more so now as they are not able to attend psychosocial activities or group therapy which has led to worsening of symptoms.” -provider 7
Provider Workload Changes
Slightly more than half of the 12 providers (58.3%, n = 7) noted their workload increased within the context of the pandemic. Of those who noted an increase, the following 4 themes emerged pertaining to tasks or aspects of service delivery were negatively impacting workload: 1) logistic challenges (assisting clients with telehealth, capturing signatures from clients on documentation, separating services previously grouped together), 2) service need (greater caseload due to increased need for services), 3) staffing challenges (providers not passing COVID-19 screening questionnaire, needing to quarantine, becoming ill, and taking sick days to manage mental health and stress), and 4) new tasks (assessing more for physical health symptoms). Providers shared the following:
“Many people have been off due to quarantining or taking sick days off for mental health to deal with the stress of COVID-19's repercussions. This understaffing leads to a cycle of workers having to see more clients daily, spending less time with each client, having less time available for paperwork and more paperwork, and causes more stress to the workers/interns. Since this makes it so less time is spent with each client, it increases the risk for crisis situations which also creates more stress/work for the team.” -provider 2
“We are having to assess for additional health concerns because of COVID-19 and have had to separate services that are typically grouped together. Such as, medication reviews and injections, and shopping groups with multiple consumers.” -provider 9
“In most circumstances, clients are needing telehealth and virtual services to facilitate medication reviews, and many clients don’t have phones or devices for telehealth, which means I assist with facilitation of telehealth services by seeing them with a tablet so they can attend the virtual medication review.” -provider 12
Provider Challenges in Remote Client Engagement
Of all participants, 7 (58.3%) endorsed challenges related to telehealth/remote engagement with clients. Importantly, only 9 of the 12 participants provided remote services to clients, therefore among the 9 who engaged remotely, a total of 7 experienced challenges (77.8%). Challenges experienced by providers resulted in 3 themes: 1) logistic challenges (clients have limited to technology and devices for telehealth, clients don’t respond to phone or phone is not on, clients are less likely to reach out because it is more difficult remotely), 2) health concerns (clients concerned about COVID-19 and do not want to go in for in person services), and 3) service delivery challenges (harder for providers to engage/build rapport with clients remotely, some services are not possible to deliver remotely, accuracy of information provided by client in assessment). Providers shared the following:
“Clients often do not have phones, do not reliably answer their phones, or their phone service is shut off. Also, clients rarely have access to video capable devices for telehealth.” -provider 4
“Many of our clients who state virtually that they’re doing well were not actually doing well so the lack of eyes through engagement is impactful.” -provider 8
Provider Challenges in Remote Treatment of Psychosis
Of the 9 providers who remotely provided services to clients during the pandemic, 88.9% ( n = 8) endorsed challenges with remote treatment among clients who experience symptoms of psychosis. Challenges experienced by providers resulted in 3 themes: 1) assessment challenges (administering the Abnormal Involuntary Movement Scale [AIMS] via telehealth is very challenging, responses to internal stimuli are hard to assess for remotely, the mental status exam [MSE] is hard to administer remotely, Activities of Daily Living (ADLs) are hard to assess for remotely), 2) symptomatology (psychosis symptoms make it difficult to engage in telehealth, paranoia may limit desire to engage), and 3) service delivery challenges (some services are not possible to deliver remotely). Providers shared the following:
“If they are not in person, it is hard to assess all the aspects of a mental status exam…or to assess for ADLs when using a phone or tablet.” -provider 5
“It’s more challenging for clients experiencing internal stimuli to maintain engagement generally. Being remote limits the ability to redirect or re-engage when clients are experiencing symptoms.” -provider 10
“It is difficult for providers to get a sense of symptomatology through telehealth services. Paranoia may limit desire to engage.” -provider 12
Provider Challenges in Remote Suicide Assessment
Of the 9 providers who remotely provided services to clients during the pandemic, 7 endorsed engaging in remote suicide assessments with clients, and of whom, 4 (57%) experienced challenges in conducting remote suicide assessments with clients during the pandemic. Challenges resulted in 2 themes: 1) assessment challenges (difficult to conduct mental status exam, hard to assess without seeing facial expressions and/or body movements, easier for clients to evade questions) and 2) rapport challenges (hard to build report well and find relatable environmental factors). Providers shared the following:
“Over the phone it has been harder to assess clients’ symptomology without seeing body and facial expressions.” -provider 2
“Clients may be more likely not to share their thoughts or feelings when there isn’t face-to-face contact.” -provider 5
“It is easier for people to dodge your questions on the phone, you can’t build rapport as well, find relatable environmental factors, and it is hard to get to linking and information sharing.” -provider 11
Literature of the evolving COVID-19 pandemic highlight an impact on mental health service need, utilization, and delivery (Ardebili et. al, 2020; [ 25 , 10 , 19 ], Vizeh et al., 2020). Given the prediction that COVID-19 may disproportionately impact individuals with psychosis [ 16 ], a population that is at greater risk for suicide in comparison to the general population (Adyin et al., 2019,Bornheimer, 2020) [ 14 ], it is critical that mental health providers can effectively engage, conduct suicide-risk assessments, and deliver services to individuals with psychosis. As a result, greater understandings of the COVID-19 impact on services and delivery are needed from the perspective of providers in CMH with specific attention to challenges in assessing and treating psychosis and suicide risk. Data of the current study indicate CMH providers observed a greater need for suicide prevention, clients facing challenges with telehealth and virtual services, an increase in workload, and challenges with remote engagement, treatment of psychosis, and suicide assessment since the COVID-19 pandemic began. Provider responses to qualitative questions further underscore and expand upon the logistic, engagement, and clinical challenges emerging within the pandemic context.
Logistic challenges emerged as a theme including provider observations of clients facing technology barriers in remote service use, clients reaching out less to providers, some services not being offered remotely due to the need for technology, and provider challenges in engaging with clients due to limited technology. These technology challenges further reinforce the disparaging impact of COVID-19 with technology access for remote engagement with mental health services presenting an inequality gap [ 33 ]. While many may have access to smart phones, computers, and reliable internet connections, clients engaging in community-based mental health services often reside in low-income, underserved, or rural areas with limited access to technology that is now needed for virtual services [ 22 ]. Some providers shared that they tried to increase access by allowing clients to use their device to meet virtually with psychiatrists and primary care providers. Though providing a device for clients as a method of problem-solving aligns with social work values of compassion, justice, and beneficence, this is also unlikely a standard practice due to resources (e.g., availability of technology and cost) and provider time (e.g., increased caseloads due to greater service needs and staffing challenges). Beaunoyer and colleagues (2020) propose a multi-layer strategy to mitigate digital inequalities involving government, organizations, corporations, and communities. It is suggested that offering alternatives to technology (e.g., allowing a phone call visit instead of a teleconference visit which requires a camera and internet), increasing coverage and capabilities of networks, public funding for increased network access, and donating technology devices to low-income households may increase access to technology. It is also recommended to increase digital literacy with household, family, and community support for device use, tutorials and trainings, and adding digital literacy to public school curriculums.
Limited technology access also serves as a foundation for the rapport and engagement challenges that providers noted. This engagement theme includes provider observations of clients engaging less in services, clients facing challenges in remote engagement due to psychosis symptoms, and provider challenges in remotely building rapport with clients. Findings align with recent literature client and provider engagement challenges since the COVID-19 pandemic began due to technology and service access [ 25 , 34 ]. These engagement challenges are likely influenced and exacerbated by increased levels of social isolation during the pandemic, already an extant problem for individuals experiencing negative symptoms within psychosis (e.g., reduction in emotional experience and loss of volition; [ 35 ]. It is also possible these challenges are influenced by variations in digital literacy, and service delivery organizations may benefit from offering training to their clients in how to engage with providers via smartphones and computers as they navigate online service system portals, audio and video telehealth sessions, setting up calendar reminders for virtual appointments, and more [ 36 ]. If the technology gap can be improved by increasing access to remote services (e.g., offering both telephone and videoconferencing options for care) and training for clients to engage in remote services, providers could integrate greater opportunities for individual and group virtual engagement to foster a sense of community and belonging.
In addition to logistic and engagement themes, findings also revealed clinical and service delivery challenges. Providers described clients having increased agitation and anxiety, provider challenges with remote assessment, new tasks of assessing for COVID-related symptoms, and increased caseloads due to greater mental health needs in the community and provider staffing challenges. Assessment was a common theme in which providers shared difficulties in conducting mental status exams in relation to suicide risk and symptoms of psychosis, administering the Abnormal Involuntary Movement Scale (AIMS), and assessing for Activities of Daily Living (ADLs). For example, providers described challenges in assessing affect without seeing facial expressions, client experience and response to internal stimuli, and overall noted greater question evasion by clients. The challenges of assessing a client without being able to observe them are also echoed in recent literature [ 24 ], and for those treating psychosis, observation of symptoms is an essential component [ 37 ]. Related to service delivery, it was apparent that provider shortage was common due COVID-19 symptoms or illness, quarantine, and using sick time to manage stress and mental health,all of which increased workloads and caseloads.
Beyond troubleshooting technology barriers, findings point towards the need for support and training among providers who have been navigating challenges and practice unknowns in CMH settings and beyond. The COVID-19 pandemic arrived in 2020 with overwhelming demands for mental health providers and healthcare workers overall, raising concerns of trauma exposure, stress, and mental illness (i.e., depression, anxiety, and post-traumatic stress disorder) among providers delivering services [ 38 ]. In the current study, providers shared that workload changes were challenging to manage and given it may not be feasible to hire more staff, strategizing for how to manage increased caseloads with bolstered support for providers to prevent burnout is essential. Burnout prevention approaches often involve self-care (e.g., sleep, breaks from work, movement), stress management (e.g., mindfulness, exercise), emotional support and professional mental health treatment [ 39 ]. Such approaches can be integrated into service delivery settings like CMH, with the potential to improve provider support and quality of life [ 40 ]. In addition to provider-focused strategies to prevent burnout, it is also imperative for agencies and organizations to foster supportive environments for staff. For example, establishing health and safety protocols with monitoring for mental health, efforts to de-stigmatize provider mental health, collaborating with providers and staff on what is needed to improve working conditions, and mindfulness of the disproportionate impact of COVID-19 on poverty-impacted individuals and racial and ethnic minority groups [ 39 ]. For specific focus on mental health and trauma, Psychological First Aid for mental health providers may be beneficial to implement in CMH settings as suggested from prior pandemic-related studies (e.g., SARS) focused on healthcare workers [ 41 ].
Though providers undergo training in educational programs, during licensure obtainment, and continuing education, most focus on in-person engagement and service delivery as opposed to telehealth and virtual forms of service delivery. An international survey ( n = 1206) across 100 countries revealed that approximately 49.1% of clinicians reported that they had not received any training in teletherapy (i.e., telephone and videoconference; [ 42 ]. In the United States, studies prior to the COVID-19 pandemic show approximately 25% of clinicians used telehealth with a lack of available training being cited as a barrier [ 43 , 44 ]. Therefore, it is essential for trainings to be established and implemented for providers to gain skills and confidence in remote engagement, assessment, and service delivery including the nuances of mental status and emotion expression. Assessing for symptoms of psychosis and suicide risk, particularly of focus in the current study, are challenging to do remotely (e.g., AIMS) and likely require additional clinical training and skills. In addition to the shift towards virtual service delivery with clients, many providers have also navigated a shift to virtual supervision [ 39 ]. Therefore, approaches to practice and supervision must be adjusted with space for real-time processing of changes and subsequent modifications as needed. Overall, new and additional training for clinicians both in the context of continuing education and also provided at service delivery sites like CMH may alleviate some of the clinical challenges faced resulting from telehealth and virtual service delivery.
Limitations
First, the findings emerged from a small sample of providers in a CMH setting of a northern midwestern region of the United States. Thus, social work provider perspectives in the sample may differ from providers of other disciplines, other mental health settings, and geographical areas across the world. It is essential for future investigations to examine a range of experiences and impacts of the COVID-19 pandemic among mental health providers across characteristics, contexts, and settings. Second, providers shared observations of client challenges within the pandemic context who were reportedly engaged in CMH services, therefore emerging themes of pandemic-related challenges may differ for clients who are not engaged with services. Third, providers most often identified as female, White, and non-Hispanic/Latinx, thus the sample is not representative of all providers across the United States and the globe. Fourth, although themes did not emerge in the data about positive changes or outcomes in relation to the pandemic, our interview did not specifically ask or probe for positive aspects of the pandemic context. We did, however, have an open-ended question asking for any additional observations or experiences at the end of the interview, with no positive responses emerging. It is important to be mindful that while many challenges emerged, it is also very possible that there are benefits to the pandemic context and virtual service delivery for providers (e.g., some people may enjoy working remotely from home or not having to drive to work). Lastly, data were qualitative, cross-sectional in nature, and collected between November and December of 2020. As a result, statistical investigations of findings did not occur and fluctuations or patterns of provider experiences were not examined across various points of time and waves of the COVID-19 pandemic.
Despite growing literature of the COVID-19 pandemic’s impact on mental health, less is known about changes in mental health services and delivery from the perspective of mental health providers and related to service delivery among individuals with psychosis and risk for suicide. Study findings highlight the logistic, engagement, and clinical challenges of clients and providers in a CMH setting. Provider perspectives are essential to inform efforts to build resources and problem-solve challenges and barriers with an overall goal of improving access, feasibility, and quality of mental health service delivery in CMH settings and beyond. The recommendations informed by the study’s findings are not only vital for the unfolding and evolving COVID-19 pandemic, but also in preparation for ongoing shifts in service delivery as technology evolves.
Availability of data and materials
Data will be made available through the NIH Data Archive (NDA) upon completion of the study.
Abbreviations
Assertive Community Treatment
Community Mental Health
National Institute of Mental Health
Center for Disease Control
Master of Social Work
Licensed Master of Social Work
Licensed Clinical Social Worker
Standard Deviation
Abnormal Involuntary Movement Scale
Activity of Daily Living
Cole CL, Waterman S, Stott J, Saunders R, Buckman JEJ, Pilling S, Wheatley J. Adapting IAPT services to support frontline NHS staff during the Covid-19 pandemic: the Homerton Covid Psychological Support (HCPS) pathway. Cogn Behav Ther. 2020;13:e12.
Ivbijaro G, Brooks C, Kolkiewicz L, Sunkel C, Long A. Psychological impact and psychosocial consequences of the COVID 19 pandemic: Resilience, mental well-being, and the coronavirus pandemic. Indian J. Psychiatry. 2020;62(Suppl 3):S395–403.
Article Google Scholar
Rahul P, Chander KR, Murugesan M, Anjappa AA, Parthasarathy R, Manjunatha N, Math SB. Accredited Social Health Activist (ASHA) and her role in district mental health program: Learnings from the COVID 19 pandemic. Community Ment Health J. 2021;57:442–5.
Kontoangelos K, Economou M, Papageorgiou C. Mental health effects of COVID-19 pandemia: a review of clinical and psychological traits. Psychiatry Investig. 2020;17(6):491.
Article CAS Google Scholar
Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiat. 2020;7(4):300–2.
Sanderson WC, Arunagiri V, Funk AP, Ginsburg KL, Krychiw JK, Limowski AR, Stout Z. The nature and treatment of pandemic-related psychological distress. J Contemp Psychother. 2020;50(4):251–63.
Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: Address mental health care to empower society. The Lancet. 2020;395(10224):e37–8.
Ferrando SJ, Klepacz L, Lynch S, Shahar S, Dornbush R, Smiley A, Bartell A. Psychiatric emergencies during the height of the COVID-19 pandemic in the suburban New York City area. J Psychiatr Res. 2020;136:552–9.
Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, Ng CH. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiat. 2020;7(3):228–9.
Reading Turchioe M, Grossman LV, Myers AC, Pathak J, Creber RM. Correlates of Mental Health Symptoms Among US Adults During COVID-19, March–April 2020. Public Health Rep. 2021;136(1):97–106.
Thakur V, Jain A. COVID 2019-suicides: A global psychological pandemic. Brain Behav Immun. 2020;88:952-953.
Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, Yip PS. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiat. 2020;7(6):468–71.
Aydin M, Ilhan BC, Tekdemir R, Çokünlü Y, Erbasan V, Altınbaş K. Suicide attempts and related factors in schizophrenia patients. Saudi Med J. 2019;40(5):475.
Bornheimer LA, Zhang A, Li J, Hiller M, Tarrier N. Effectiveness of suicide-focused psychosocial interventions in psychosis: a systematic review and meta-analysis. Psychiatr Serv. 2020;71(8):829–38.
Jacobs DG, Baldessarini RJ, Conwell Y, Fawcett JA, Horton L, Meltzer H, ... & Simon RI. Assessment and treatment of patients with suicidal behaviors. APA Practice Guidelines. 2010:1–183.
Anglin DM, Galea S, Bachman P. Going upstream to advance psychosis prevention and improve public health. JAMA Psychiat. 2020;77(7):665–6.
Brown E, Gray R, Monaco SL, O'Donoghue B, Nelson B, Thompson A, ... & McGorry P. The potential impact of COVID-19 on psychosis: a rapid review of contemporary epidemic and pandemic research. Schizophr Res. 2020;222:79-87.
Adamou M. Community service models for schizophrenia: evidence-based implications and future directions. Psychiatry (Edgmont). 2005;2(2):24.
Google Scholar
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976–e203976.
Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J Diabetes Metab Disord. 2020;19(2):1–12.
Pierce, B. S., Perrin, P. B., Tyler, C. M., McKee, G. B., & Watson, J. D. (2021). The COVID-19 telepsychology revolution: A national study of pandemic-based changes in U.S. mental health care delivery. American Psychologist, 76 (1), 14–25.
Weigel G, Ramaswamy A, Sobel L, Salganicoff A, Cubanski J, Freed M. Opportunities and barriers for telemedicine in the US during the COVID-19 emergency and beyond. Women’s Health Policy. 2020. Accessed 1 Mar 2022. https://www.kff.org/womens-health-policy/issue-brief/opportunities-and-barriers-for-telemedicine-in-the-u-s-during-the-covid-19-emergency-and-beyond/ .
Buckman JE, Saunders R, Leibowitz J, Minton R. The barriers, benefits and training needs of clinicians delivering psychological therapy via video. Behav Cogn Psychother. 2021;49(6):696–720.
Uscher-Pines L, Sousa J, Raja P, Mehrotra A, Barnett ML, Huskamp HA. Suddenly becoming a “virtual doctor”: Experiences of psychiatrists transitioning to telemedicine during the COVID-19 pandemic. Psychiatr Serv. 2020;71(11):1143–50.
Ardebili M, Naserbakht M, Bernstein C, Alazmani-Noodeh F, Hakimi H, Ranjbar H. Healthcare providers experience of working during the COVID-19 pandemic: A qualitative study. Am J Infect Control. 2020;S0196–6553(20):30896–8.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
CDC. (2019). Suicide Mortality by State: Michigan. Accessed May 1, 2021. https://www.cdc.gov/nchs/pressroom/sosmap/suicide-mortality/suicide.htm .
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, Jinks C. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907.
Creswell JW, Clark VLP. Designing and conducting mixed methods research. Thousand Oaks, CA: Sage publications; 2017.
Saldaña J. The coding manual for qualitative researchers. Thousand Oaks, CA: Sage publications; 2021.
Charmaz K. Constructing grounded theory. Thousand Oaks, CA: Sage publications; 2014.
Padgett DK. Qualitative methods in social work research (Vol. 36). Thousand Oaks, CA: Sage publications; 2016.
Beaunoyer E, Dupéré S, Guitton MJ. COVID-19 and digital inequalities: Reciprocal impacts and mitigation strategies. Comput Hum Behav. 2020;111: 106424.
Cadel L, Marcinow M, Sandercock J, Dowedoff P, Guilcher SJ, Maybee A, Kuluski K. A scoping review of patient engagement activities during COVID-19: More consultation, less partnership. PLoS ONE. 2021;16(9): e0257880.
Lysaker PH, Shea AM, Buck KD, Dimaggio G, Nicolò G, Procacci M, Rand KL. Metacognition as a mediator of the effects of impairments in neurocognition on social function in schizophrenia spectrum disorders. Acta Psychiatrica Scandanavia. 2010;122(5):405–13.
Hoffman L, Wisniewski H, Hays R, Henson P, Vaidyam A, Hendel V, Torous J. Digital opportunities for outcomes in recovery services (DOORS): A pragmatic hands-on group approach toward increasing digital health and smartphone competencies, autonomy, relatedness, and alliance for those with serious mental illness. J Psychiatr Pract. 2020;26(2):80–8.
Sharp IR, Kobak KA, Osman DA. The use of videoconferencing with patients with psychosis: a review of the literature. Ann Gen Psychiatry. 2011;10(1):14.
Søvold LE, Naslund JA, Kousoulis AA, Saxena S, Qoronfleh MW, Grobler C, Münter L. Prioritizing the mental health and well-being of healthcare workers: an urgent global public health priority. Front Public Health. 2021;9:1-12.
Gruber J, Prinstein MJ, Clark LA, Rottenberg J, Abramowitz JS, Albano AM, ... & Weinstock LM. Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am Psychol. 2020;76(3):409-426.
Dyrbye LN, Shanafelt TD, Sinsky CA, Cipriano PF, Bhatt J, Ommaya A, West CP, et al. Burnout among health care professionals: A call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspectives. Discussion Paper. Washington DC: National Academy of Medicine; 2017.
Maunder RG, Peladeau N, Leszcz M, Romano D, Savage D, Rose M, Reg O, et al. Applying the Lessons of SARS to Pandemic Influenza An Evidence-based Approach to Mitigating the Stress Experienced by Healthcare Workers. Can J Public Health. 2008;99(6):486-88.
Montoya MI, Kogan CS, Rebello TJ, Sadowska K, Garcia-Pacheco JA, Khoury B, Reed GM. An international survey examining the impact of the COVID-19 pandemic on telehealth use among mental health professionals. J Psychiatr Res. 2022;148:188–96.
Pierce BS, Perrin PB, McDonald SD. Demographic, organizational, and clinical practice predictors of US psychologists’ use of telepsychology. Prof Psychol Res Pract. 2020;51(2):184.
Perle JG, Burt J, Higgins WJ. Psychologist and physician interest in telehealth training and referral for mental health services: An exploratory study. J Technol Hum Serv. 2014;32(3):158–85.
Download references
Acknowledgements
Data were collected as part of a National Institute of Mental Health (NIMH)-funded pilot effectiveness clinical trial (R34MH123609; PI: Bornheimer). The contents of this article are solely the responsibility of the authors and do not necessarily represent the views of NIH.
Author information
Authors and affiliations.
University of Michigan, School of Social Work, Ann Arbor, MI, USA
Lindsay A. Bornheimer, Juliann Li Verdugo, Joshua Holzworth, Fonda N. Smith & Joseph A. Himle
University of Michigan, Department of Psychiatry, Ann Arbor, MI, USA
Lindsay A. Bornheimer & Joseph A. Himle
You can also search for this author in PubMed Google Scholar
Contributions
LAB and JAH conceptualized and designed the study. LAB, JLV, JH, and FS collected and analyzed the data, and all authors were involved in interpretation of findings. LAB, JLV, and JH conducted literature reviews and drafted the first version of the manuscript. All authors contributed to subsequent drafts of the manuscript, preparations for submission, revisions, and resubmission. All authors read and approved the final manuscript.
Authors’ information
Lindsay A. Bornheimer, PhD, LCSW is an Assistant Professor in the University of Michigan School of Social Work and Department of Psychiatry. Juliann Li Verdugo, MSW, LMSW is a project coordinator at the University of Michigan School of Social Work. Joshua Holzworth, MSW was a research assistant at the University of Michigan School of Social Work. Fonda Smith, MSW was a research assistant at the University of Michigan School of Social Work. Joseph A. Himle, PhD is a Professor in the University of Michigan School of Social Work and Department of Psychiatry.
Corresponding author
Correspondence to Lindsay A. Bornheimer .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the University of Michigan Institutional Review Board and all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bornheimer, L.A., Li Verdugo, J., Holzworth, J. et al. Mental health provider perspectives of the COVID-19 pandemic impact on service delivery: a focus on challenges in remote engagement, suicide risk assessment, and treatment of psychosis. BMC Health Serv Res 22 , 718 (2022). https://doi.org/10.1186/s12913-022-08106-y
Download citation
Received : 11 October 2021
Accepted : 18 May 2022
Published : 31 May 2022
DOI : https://doi.org/10.1186/s12913-022-08106-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Service delivery
- Risk assessment
- Community mental health
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine (2021)
Chapter: 8 major findings and research questions, 8 major findings and research questions, introduction.
The COVID-19 pandemic, which began in late 2019, created unprecedented global disruption and infused a significant level of uncertainty into the lives of individuals, both personally and professionally, around the world throughout 2020. The significant effect on vulnerable populations, such as essential workers and the elderly, is well documented, as is the devastating effect the COVID-19 pandemic had on the economy, particularly brick-and-mortar retail and hospitality and food services. Concurrently, the deaths of unarmed Black people at the hands of law enforcement officers created a heightened awareness of the persistence of structural injustices in U.S. society.
Against the backdrop of this public health crisis, economic upheaval, and amplified social consciousness, an ad hoc committee was appointed to review the potential effects of the COVID-19 pandemic on women in academic science, technology, engineering, mathematics, and medicine (STEMM) during 2020. The committee’s work built on the National Academies of Sciences, Engineering, and Medicine report Promising Practices for Addressing the Underrepresentation of Women in Science, Engineering, and Medicine: Opening Doors (the Promising Practices report), which presents evidence-based recommendations to address the well-established structural barriers that impede the advancement of women in STEMM. However, the committee recognized that none of the actions identified in the Promising Practices report were conceived within the context of a pandemic, an economic downturn, or the emergence of national protests against structural racism. The representation and vitality of academic women in STEMM had already warranted national attention prior to these events, and the COVID-19
pandemic appeared to represent an additional risk to the fragile progress that women had made in some STEMM disciplines. Furthermore, the future will almost certainly hold additional, unforeseen disruptions, which underscores the importance of the committee’s work.
In times of stress, there is a risk that the divide will deepen between those who already have advantages and those who do not. In academia, senior and tenured academics are more likely to have an established reputation, a stable salary commitment, and power within the academic system. They are more likely, before the COVID-19 pandemic began, to have established professional networks, generated data that can be used to write papers, and achieved financial and job security. While those who have these advantages may benefit from a level of stability relative to others during stressful times, those who were previously systemically disadvantaged are more likely to experience additional strain and instability.
As this report has documented, during 2020 the COVID-19 pandemic had overall negative effects on women in academic STEMM in areas such productivity, boundary setting and boundary control, networking and community building, burnout rates, and mental well-being. The excessive expectations of caregiving that often fall on the shoulders of women cut across career timeline and rank (e.g., graduate student, postdoctoral scholar, non-tenure-track and other contingent faculty, tenure-track faculty), institution type, and scientific discipline. Although there have been opportunities for innovation and some potential shifts in expectations, increased caregiving demands associated with the COVID-19 pandemic in 2020, such as remote working, school closures, and childcare and eldercare, had disproportionately negative outcomes for women.
The effects of the COVID-19 pandemic on women in STEMM during 2020 are understood better through an intentionally intersectional lens. Productivity, career, boundary setting, mental well-being, and health are all influenced by the ways in which social identities are defined and cultivated within social and power structures. Race and ethnicity, sexual orientation, gender identity, academic career stage, appointment type, institution type, age, and disability status, among many other factors, can amplify or diminish the effects of the COVID-19 pandemic for a given person. For example, non-cisgender women may be forced to return to home environments where their gender identity is not accepted, increasing their stress and isolation, and decreasing their well-being. Women of Color had a higher likelihood of facing a COVID-19–related death in their family compared with their white, non-Hispanic colleagues. The full extent of the effects of the COVID-19 pandemic for women of various social identities was not fully understood at the end of 2020.
Considering the relative paucity of women in many STEMM fields prior to the COVID-19 pandemic, women are more likely to experience academic isolation, including limited access to mentors, sponsors, and role models that share gender, racial, or ethnic identities. Combining this reality with the physical isolation stipulated by public health responses to the COVID-19 pandemic,
women in STEMM were subject to increasing isolation within their fields, networks, and communities. Explicit attention to the early indicators of how the COVID-19 pandemic affected women in academic STEMM careers during 2020, as well as attention to crisis responses throughout history, may provide opportunities to mitigate some of the long-term effects and potentially develop a more resilient and equitable academic STEMM system.
MAJOR FINDINGS
Given the ongoing nature of the COVID-19 pandemic, it was not possible to fully understand the entirety of the short- or long-term implications of this global disruption on the careers of women in academic STEMM. Having gathered preliminary data and evidence available in 2020, the committee found that significant changes to women’s work-life boundaries and divisions of labor, careers, productivity, advancement, mentoring and networking relationships, and mental health and well-being have been observed. The following findings represent those aspects that the committee agreed have been substantiated by the preliminary data, evidence, and information gathered by the end of 2020. They are presented either as Established Research and Experiences from Previous Events or Impacts of the COVID-19 Pandemic during 2020 that parallel the topics as presented in the report.
Established Research and Experiences from Previous Events
| Leading up to the COVID-19 pandemic, the representation of women has slowly increased in STEMM fields, from acquiring Ph.D.s to holding leadership positions, but with caveats to these limited steps of progress; for example, women representation in leadership positions tends to be at institutions with less prestige and fewer resources. While promising and encouraging, such progress is fragile and prone to setbacks especially in times of crisis (see ). | |
| Social crises (e.g., terrorist attacks, natural disasters, racialized violence, and infectious diseases) and COVID-19 pandemic-related disruptions to workload and schedules, added to formerly routine job functions and health risks, have the potential to exacerbate mental health conditions such as insomnia, depression, anxiety, and posttraumatic stress. All of these conditions occur more frequently among women than men. As multiple crises coincided during 2020, there is a greater chance that women will be affected mentally and physically (see and ). |
___________________
1 This finding is primarily based on research on cisgender women and men.
| Structural racism is an omnipresent stressor for Women of Color, who already feel particularly isolated in many fields and disciplines. Attempts to ensure equity for all women may not necessarily create equity for women across various identities if targeted interventions designed to promote gender equity do not account for the racial and ethnic heterogeneity of women in STEMM (see , , and ). |
Impacts of the COVID-19 Pandemic during 2020
| While some research indicates consistency in publications authored by women in specific STEMM disciplines, like Earth and space sciences, during 2020, several other preliminary measures of productivity suggest that COVID-19 disruptions have disproportionately affected women compared with men. Reduced productivity may be compounded by differences in the ways research is conducted, such as whether field research or face-to-face engagement with human subjects is required (see ). | |
| Many administrative decisions regarding institutional supports made during 2020, such as work-from-home provisions and extensions on evaluations or deliverables, are likely to exacerbate underlying gender-based inequalities in academic advancement rather than being gender neutral as assumed. For example, while colleges and universities have offered extensions for those on the tenure track and federal and private funders have offered extensions on funding and grants, these changes do not necessarily align with the needs expressed by women, such as the need for flexibility to contend with limited availability of caregiving and requests for a reduced workload, nor do they generally benefit women faculty who are not on the tenure track. Furthermore, provision of institutional support may be insufficient if it does not account for the challenges faced by those with multiple marginalized identities (see and ). | |
| Organizational-level approaches may be needed to address challenges that have emerged as a result of the COVID-19 pandemic in 2020, as well as those challenges that may have existed before the pandemic but are now more visible and amplified. Reliance on individual coping strategies may be insufficient (see and ). | |
| The COVID-19 pandemic has intensified complications related to worklife boundaries that largely affect women. Preliminary evidence |
| from 2020 suggests women in academic STEMM are experiencing increased workload, decreased productivity, changes in interactions, and difficulties from remote work caused by the COVID-19 pandemic and associated disruptions. Combined with the gendered division of nonemployment labor that affected women before the pandemic, these challenges have been amplified, as demonstrated by a lack of access to childcare, children’s heightened behavioral and academic needs, increased eldercare demands, and personal physical and mental health concerns. These are particularly salient for women who are parents or caregivers (see ). | |
| During the COVID-19 pandemic, technology has allowed for the continuation of information exchange and many collaborations. In some cases technology has facilitated the increased participation of women and underrepresented groups. However, preliminary indicators also show gendered impacts on science and scientific collaborations during 2020. These arise because some collaborations cannot be facilitated online and some collaborations face challenges including finding time in the day to engage synchronously, which presents a larger burden for women who manage the larger share of caregiving and other household duties, especially during the first several months of the COVID-19 pandemic (see ). | |
| During the COVID-19 pandemic in 2020, some professional societies adapted to the needs of members as well as to broader interests of individuals engaged in the disciplines they serve. Transitioning conferences to virtual platforms has produced both positive outcomes, such as lower attendance costs and more open access to content, and negative outcomes, including over-flexibility (e.g., scheduling meetings at non-traditional work hours; last-minute changes) and opportunities for bias in virtual environments (see ). | |
| During the COVID-19 pandemic in 2020, many of the decision-making processes, including financial decisions like lay-offs and furloughs, that were quickly implemented contributed to unilateral decisions that frequently deviated from effective practices in academic governance, such as those in crisis and equity-minded leadership. Fast decisions greatly affected contingent and nontenured faculty members—positions that are more often occupied by women and People of Color. In 2020, these financial decisions already had negative, short-term effects and may portend long-term consequences (see ). | |
| Social support, which is particularly important during stressful situations, is jeopardized by the physical isolation and restricted social interactions that have |
| been imposed during the COVID-19 pandemic. For women who are already isolated within their specific fields or disciplines, additional social isolation may be an important contributor to added stress (see ). | |
| For women in the health professions, major risk factors during the COVID-19 pandemic in 2020 included unpredictability in clinical work, evolving clinical and leadership roles, the psychological demands of unremitting and stressful work, and heightened health risks to family and self (see ). |
RESEARCH QUESTIONS
While this report compiled much of the research, data, and evidence available in 2020 on the effects of the COVID-19 pandemic, future research is still needed to understand all the potential effects, especially any long-term implications. The research questions represent areas the committee identified for future research, rather than specific recommendations. They are presented in six categories that parallel the chapters of the report: Cross-Cutting Themes; Academic Productivity and Institutional Responses; Work-Life Boundaries and Gendered Divisions of Labor; Collaboration, Networking, and Professional Societies; Academic Leadership and Decision-Making; and Mental Health and Well-being. The committee hopes the report will be used as a basis for continued understanding of the impact of the COVID-19 pandemic in its entirety and as a reference for mitigating impacts of future disruptions that affect women in academic STEMM. The committee also hopes that these research questions may enable academic STEMM to emerge from the pandemic era a stronger, more equitable place for women. Therefore, the committee identifies two types of research questions in each category; listed first are those questions aimed at understanding the impacts of the disruptions from the COVID-19 pandemic, followed by those questions exploring the opportunities to help support the full participation of women in the future.
Cross-Cutting Themes
- What are the short- and long-term effects of the COVID-19 pandemic on the career trajectories, job stability, and leadership roles of women, particularly of Black women and other Women of Color? How do these effects vary across institutional characteristics, 2 discipline, and career stage?
2 Institutional characteristics include different institutional types (e.g., research university, liberal arts college, community college), locales (e.g., urban, rural), missions (e.g., Historically Black Colleges and Universities, Hispanic-Serving Institutions, Asian American/Native American/Pacific Islander-Serving Institutions, Tribal Colleges and Universities), and levels of resources.
- How did the confluence of structural racism, economic hardships, and environmental disruptions affect Women of Color during the COVID-19 pandemic? Specifically, how did the murder of George Floyd, Breonna Taylor, and other Black citizens impact Black women academics’ safety, ability to be productive, and mental health?
- How has the inclusion of women in leadership and other roles in the academy influenced the ability of institutions to respond to the confluence of major social crises during the COVID-19 pandemic?
- How can institutions build on the involvement women had across STEMM disciplines during the COVID-19 pandemic to increase the participation of women in STEMM and/or elevate and support women in their current STEMM-related positions?
- How can institutions adapt, leverage, and learn from approaches developed during 2020 to attend to challenges experienced by Women of Color in STEMM in the future?
Academic Productivity and Institutional Responses
- How did the institutional responses (e.g., policies, practices) that were outlined in the Major Findings impact women faculty across institutional characteristics and disciplines?
- What are the short- and long-term effects of faculty evaluation practices and extension policies implemented during the COVID-19 pandemic on the productivity and career trajectories of members of the academic STEMM workforce by gender?
- What adaptations did women use during the transition to online and hybrid teaching modes? How did these techniques and adaptations vary as a function of career stage and institutional characteristics?
- What are examples of institutional changes implemented in response to the COVID-19 pandemic that have the potential to reduce systemic barriers to participation and advancement that have historically been faced by academic women in STEMM, specifically Women of Color and other marginalized women in STEMM? How might positive institutional responses be leveraged to create a more resilient and responsive higher education ecosystem?
- How can or should funding arrangements be altered (e.g., changes in funding for research and/or mentorship programs) to support new ways of interaction for women in STEMM during times of disruption, such as the COVID-19 pandemic?
Work-Life Boundaries and Gendered Divisions of Labor
- How do different social identities (e.g., racial; socioeconomic status; culturally, ethnically, sexually, or gender diverse; immigration status; parents of young children and other caregivers; women without partners) influence the management of work-nonwork boundaries? How did this change during the COVID-19 pandemic?
- How have COVID-19 pandemic-related disruptions affected progress toward reducing the gender gap in academic STEMM labor-force participation? How does this differ for Women of Color or women with caregiving responsibilities?
- How can institutions account for the unique challenges of women faculty with parenthood and caregiving responsibilities when developing effective and equitable policies, practices, or programs?
- How might insights gained about work-life boundaries during the COVID-19 pandemic inform how institutions develop and implement supportive resources (e.g., reductions in workload, on-site childcare, flexible working options)?
Collaboration, Networking, and Professional Societies
- What were the short- and long-term effects of the COVID-19 pandemic-prompted switch from in-person conferences to virtual conferences on conference culture and climate, especially for women in STEMM?
- How will the increase in virtual conferences specifically affect women’s advancement and career trajectories? How will it affect women’s collaborations?
- How has the shift away from attending conferences and in-person networking changed longer-term mentoring and sponsoring relationships, particularly in terms of gender dynamics?
- How can institutions maximize the benefits of digitization and the increased use of technology observed during the COVID-19 pandemic to continue supporting women, especially marginalized women, by increasing accessibility, collaborations, mentorship, and learning?
- How can organizations that support, host, or facilitate online and virtual conferences and networking events (1) ensure open and fair access to participants who face different funding and time constraints; (2) foster virtual connections among peers, mentors, and sponsors; and (3) maintain an inclusive environment to scientists of all backgrounds?
- What policies, practices, or programs can be developed to help women in STEMM maintain a sense of support, structure, and stability during and after periods of disruption?
Academic Leadership and Decision-Making
- What specific interventions did colleges and universities initiate or prioritize to ensure that women were included in decision-making processes during responses to the COVID-19 pandemic?
- How effective were colleges and universities that prioritized equity-minded leadership, shared leadership, and crisis leadership styles at mitigating emerging and potential negative effects of the COVID-19 pandemic on women in their communities?
- What specific aspects of different leadership models translated to more effective strategies to advance women in STEMM, particularly during the COVID-19 pandemic?
- How can examples of intentional inclusion of women in decision-making processes during the COVID-19 pandemic be leveraged to develop the engagement of women as leaders at all levels of academic institutions?
- What are potential “top-down” structural changes in academia that can be implemented to mitigate the adverse effects of the COVID-19 pandemic or other disruptions?
- How can academic leadership, at all levels, more effectively support the mental health needs of women in STEMM?
Mental Health and Well-being
- What is the impact of the COVID-19 pandemic and institutional responses on the mental health and well-being of members of the academic STEMM workforce as a function of gender, race, and career stage?
- How are tools and diagnostic tests to measure aspects of wellbeing, including burnout and insomnia, used in academic settings? How does this change during times of increased stress, such as the COVID-19 pandemic?
- How might insights gained about mental health during the COVID-19 pandemic be used to inform preparedness for future disruptions?
- How can programs that focus on changes in biomarkers of stress and mood dysregulation, such as levels of sleep, activity, and texting patterns, be developed and implemented to better engage women in addressing their mental health?
- What are effective interventions to address the health of women academics in STEMM that specifically account for the effects of stress on women? What are effective interventions to mitigate the excessive levels of stress for Women of Color?
This page intentionally left blank.
The spring of 2020 marked a change in how almost everyone conducted their personal and professional lives, both within science, technology, engineering, mathematics, and medicine (STEMM) and beyond. The COVID-19 pandemic disrupted global scientific conferences and individual laboratories and required people to find space in their homes from which to work. It blurred the boundaries between work and non-work, infusing ambiguity into everyday activities. While adaptations that allowed people to connect became more common, the evidence available at the end of 2020 suggests that the disruptions caused by the COVID-19 pandemic endangered the engagement, experience, and retention of women in academic STEMM, and may roll back some of the achievement gains made by women in the academy to date.
The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine identifies, names, and documents how the COVID-19 pandemic disrupted the careers of women in academic STEMM during the initial 9-month period since March 2020 and considers how these disruptions - both positive and negative - might shape future progress for women. This publication builds on the 2020 report Promising Practices for Addressing the Underrepresentation of Women in Science, Engineering, and Medicine to develop a comprehensive understanding of the nuanced ways these disruptions have manifested. The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine will inform the academic community as it emerges from the pandemic to mitigate any long-term negative consequences for the continued advancement of women in the academic STEMM workforce and build on the adaptations and opportunities that have emerged.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Household Pulse Survey

As part of an ongoing partnership with the Census Bureau, the National Center for Health Statistics (NCHS) recently added questions to assess the prevalence of post-COVID-19 conditions (long COVID), on the experimental Household Pulse Survey. This 20-minute online survey was designed to complement the ability of the federal statistical system to rapidly respond and provide relevant information about the impact of the coronavirus pandemic in the U.S. Data collection began on April 23, 2020.
Beginning in Phase 3.5 (on June 1, 2022), NCHS included questions about the presence of symptoms of COVID that lasted three months or longer. Beginning in Phase 3.6 (on September 14, 2022), NCHS included a question about whether long-term symptoms among those reporting symptoms lasting three months or longer reduced the ability to carry out day-to-day activities compared with the time before having COVID-19. Phase 3.6 will continue with a two-weeks on, two-weeks off collection and dissemination approach.
Estimates on this page are derived from the Household Pulse Survey and show the following outcomes for adults aged 18 and over:
- The percentage of all U.S. adults who EVER experienced post-COVID conditions (long COVID). These adults had COVID and had some symptoms that lasted three months or longer.
- The percentage of adults who EVER experienced post-COVID conditions (long COVID) among those who ever had COVID .
- The percentage of all U.S. adults who are CURRENTLY experiencing post-COVID conditions (long COVID). These adults had COVID, had long-term symptoms, and are still experiencing symptoms.
- The percentage of adults who are CURRENTLY experiencing post-COVID conditions (long COVID) among those who ever had COVID.
Beginning in Phase 3.6:
- The percentage of any activity limitations (either ‘yes, a little’ or ‘yes, a lot’ responses) from long COVID, among adults who are currently experiencing long COVID and among all adults
- The percentage of significant activity limitations (‘yes, a lot’ response) from long COVID, among adults who are currently experiencing long COVID and among all adults
The percentage of all U.S. adults who ever said they had COVID is also included to provide context for the other percentages. It should be noted that the percentage of adults who said they ever had COVID based on the Household Pulse Survey is lower than other estimates based on seroprevalence studies .
See the technical notes for more information on these measures.
Questions on post-COVID conditions (long COVID) were also included on the National Health Interview Survey (NHIS) in 2022. The NHIS, conducted by NCHS, is the major source for high-quality data used to monitor the nation’s health. NHIS data collection will continue through December 2024.
- Anxiety and Depression
- Health Insurance Coverage
- Lack of Social Connection
- Functioning and Disability
- Telemedicine Use
- Mental Health Care
- Reduced Access to Care
Long COVID or Post COVID Conditions
Use the drop-down menus to show data for selected indicators or categories. Select the buttons at the bottom of the dashboard to view national and state estimates. The data table may be scrolled horizontally and vertically to view additional estimates.
Access Dataset on Data.CDC.gov (Export to CSV, JSON, XLS, XML) [?]
Beginning in Phase 4.1 (April 2, 2024) of data collection and reporting, the answer choices for the third question in the series changed to Yes, my symptoms lasted between 3 and 6 months; Yes, my symptoms lasted 6 months to a year; Yes, my symptoms lasted more than a year; No. The definitions of ever and currently have Long COVID remain the same.
Technical Notes
Survey questions.
Have you ever tested positive for COVID-19 (using a rapid point-of-care test, self-test, or laboratory test) or been told by a doctor or other health care provider that you have or had COVID-19?
Answer Choices: yes, no
How would you describe your coronavirus symptoms when they were at their worst?
Answer choices: I had no symptoms, I had mild symptoms, I had moderate symptoms, I had severe symptoms.
Did you have any symptoms lasting 3 months or longer that you did not have prior to having coronavirus or COVID-19?
Long term symptoms may include: Tiredness or fatigue, difficulty thinking, concentrating, forgetfulness, or memory problems (sometimes referred to as “brain fog”), difficulty breathing or shortness of breath, joint or muscle pain, fast-beating or pounding heart (also known as heart palpitations), chest pain, dizziness on standing, menstrual changes, changes to taste/smell, or inability to exercise.
Answer choices: yes, no
Do you have symptoms now?
Do these long-term symptoms reduce your ability to carry out day-to-day activities compared with the time before you had COVID-19?
Answer choices: Yes, a lot; Yes, a little; Not at all
Data Source
The U.S. Census Bureau, in collaboration with multiple federal agencies, launched the Household Pulse Survey to produce data on the social and economic impacts of COVID-19 on American households. The Household Pulse Survey was designed to gauge the impact of the pandemic on employment status, consumer spending, food security, housing, education disruptions, and dimensions of physical and mental wellness.
The survey was designed to meet the goal of accurate and timely weekly estimates. It was conducted by an internet questionnaire, with invitations to participate sent by email and text message. The sample frame is the Census Bureau Master Address File Data. Housing units linked to one or more email addresses or cell phone numbers were randomly selected to participate, and one respondent from each housing unit was selected to respond for him or herself. Estimates are weighted to adjust for nonresponse and to match Census Bureau estimates of the population by age, sex, race and ethnicity, and educational attainment. All estimates shown meet the NCHS Data Presentation Standards for Proportions .
Limitations
The Household Pulse Survey is different from other surveys. NCHS, the Census Bureau, and other federal statistical agencies are considered the preeminent source of the nation’s most important benchmark surveys. Many of these surveys have been in production for decades and provide valuable insight on health, social, and economic trends. However, the production of benchmark data requires a relatively long lead time, and personal interviews (face-to-face or telephone) require additional time. While efforts are underway to introduce COVID-19 questions into these surveys, that process can take months, sometimes years, before data are made available.
The Household Pulse Survey is different: It was designed to go into the field quickly, to be administered via the web, and to disseminate data in near real-time, providing data users with information they can use now to help ease the burden on American households and expedite post-pandemic recovery. The Census Bureau is fielding the Household Pulse Survey as a demonstration project, with data released as part of its Experimental Statistical Products Series.
Confidence intervals included in the tables on this page only reflect the potential for sampling error. Nonsampling errors can also occur and are more likely for surveys that are implemented quickly, achieve low response rates, and rely on online response. Nonsampling errors for the Household Pulse Survey may include:
- Measurement error: The respondent provides incorrect information, or an unclear survey question is misunderstood by the respondent. The Household Pulse Survey schedule offered only limited time for testing questions.
- Coverage error: Individuals who otherwise would have been included in the survey frame were missed. The Household Pulse Survey only recruited households for which an email address or cell phone number could be identified.
- Nonresponse error: Responses are not collected from all those in the sample or the respondent is unwilling to provide information. The response rate for the Household Pulse Survey was substantially lower than most federally sponsored surveys.
- Processing error: Forms may be lost, data may be incorrectly keyed, coded, or recoded. The real-time dissemination of the Household Pulse Survey provided limited time to identify and fix processing errors.
For more information on nonresponse bias for the Household Pulse Survey, please visit https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/2020_HPS_NR_Bias_Report-final.pdf .
For more information on the Household Pulse Survey, please visit https://www.census.gov/data/experimental-data-products/household-pulse-survey.html .
Suggested Citation
National Center for Health Statistics. U.S. Census Bureau, Household Pulse Survey, 2022–2024. Long COVID. Generated interactively: from https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

IMAGES
COMMENTS
The impact of the COVID-19 pandemic on the mental health of children is not yet fully understood. NIH-supported research is investigating factors that may influence the cognitive, social, and emotional development of children during the pandemic, including: Changes to routine. Virtual schooling. Mask wearing.
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic ...
In this section. The COVID-19 pandemic has had a huge impact on public health around the globe in terms of both physical and mental health, and the mental health implications of the pandemic may continue long after the physical health consequences have resolved. This research area aims to contribute to our understanding of the COVID-19 ...
Mental health professionals can help craft messages to be delivered by trusted leaders. 4. The Covid-19 pandemic has alarming implications for individual and collective health and emotional and ...
In these times of rapid change, with high levels of uncertainty, anxiety, social isolation, and financial pressure, mental health worldwide is likely to be at risk. Researchers are rightly ensuring that mental health research is included in the response to the coronavirus disease 2019 (COVID-19) pandemic.1 Here, we reflect on ethical issues to consider when conducting research on self-harm ...
The coronavirus disease 2019 (COVID-19) pandemic is having a profound effect on all aspects of society, including mental health and physical health. We explore the psychological, social, and neuroscientific effects of COVID-19 and set out the immediate priorities and longer-term strategies for mental health science research.
The COVID-19 pandemic has had a severe impact on the mental health and wellbeing of people around the world while also raising concerns of increased suicidal behaviour. In addition access to mental health services has been severely impeded. However, no comprehensive summary of the current data on these impacts has until now been made widely ...
Three years into the COVID-19 outbreak in the United States, Pew Research Center published this collection of survey findings about Americans' challenges with mental health during the pandemic.All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
As the COVID-19 pandemic began, confirmed cases rose, and mandated policy responses were enacted, mental health concerns started to be alarming 1,2,3.The deterioration of mental health was ...
Members of the COVID-19 Mental Health Measurement Working Group are working to ensure that measurement of mental health measures is a key part of large-scale national and international data collections relative to COVID-19 and then conducting research studies on mental health during the pandemic. Read more about our current measurements.
COVID-19 has a significant impact on mental health. It is creating a destructive mentality and increasing depression in regular life. As a result, suicidal attempts are increasing. Life of people are becoming more irritable, and people have social anxiety. For COVID-19 social distance has increased. So, physical contact is decreasing.
The mental health questions were included on three surveys. The first survey was conducted with 11,537 U.S. adults March 19-24, 2020; a second survey with the question series was conducted April 20-26, 2020, with a sample of 10,139 adults; and the most recent survey was conducted Feb. 16-21, 2021, among 10,121 adults.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020. Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19.
Marcos Calvo / iStock. In a large US study that tracked people for as long as a year, COVID-19 patients had a 60% higher risk of mental disorders such as anxiety, depression, or substance abuse compared with those who weren't sickened by the virus. Given the large number of people infected with COVID-19, the findings suggest that nations should ...
Mental Health. The disruptions of the COVID-19 pandemic—mandatory masks, social distancing, remote school and work—have touched every facet of our lives, including our mental health. In the early days of the outbreak, mental health experts at Johns Hopkins Bloomberg School of Public Health saw a need to better understand and measure mental ...
Note: This brief was updated on March 20, 2023 to incorporate the latest available data. Concerns about mental health and substance use remain elevated three years after the onset of the COVID-19 ...
Research suggests that as many as 90% of individuals hospitalized with COVID-19 and 25% of non-hospitalized adults experience at least one brain or mind-related symptom, including fatigue, headache, sleep disturbances, depression, or anxiety, six months after the illness. Symptoms of depression, which have been shown to generally decrease as ...
The COVID-19 pandemic has been impacting the need, utilization, and delivery of mental health services with greater challenges being faced by clients and providers. With many clients facing reduced access to services and social isolation, a focus on suicide risk assessment and prevention is critical. Concern is particularly increased for clients with schizophrenia spectrum disorders given data ...
Major Findings and Research Questions INTRODUCTION. The COVID-19 pandemic, which began in late 2019, created unprecedented global disruption and infused a significant level of uncertainty into the lives of individuals, both personally and professionally, around the world throughout 2020. ... Mental Health and Well-being: For women in the health ...
In 2019-2020, 20.78% of adults were experiencing a mental illness. That is equivalent to over 50 million Americans. The vast majority of individuals with a substance use disorder in the U.S. are not receiving treatment. 15.35% of adults had a substance use disorder in the past year. Of them, 93.5% did not receive any form of treatment.
The COVID-19 pandemic has taken a disproportionate toll on the health and well-being of people of color and other underserved groups. Cumulative age-adjusted data showed that AIAN and Hispanic ...
In 2021 and 2022, 21% and 18% of adolescents reported living with a household member experiencing mental illness or substance use issues, respectively; 17% reported emotional abuse by a parent or ...
As part of an ongoing partnership with the Census Bureau, the National Center for Health Statistics (NCHS) recently added questions to assess the prevalence of post-COVID-19 conditions (long COVID), on the experimental Household Pulse Survey. This 20-minute online survey was designed to complement the ability of the federal statistical system to rapidly respond and provide relevant information ...