- Open access
- Published: 26 December 2019

The relationship between physical activity, mental wellbeing and symptoms of mental health disorder in adolescents: a cohort study
- Sarah Louise Bell ORCID: orcid.org/0000-0003-1181-9591 1 ,
- Suzanne Audrey 1 ,
- David Gunnell 1 , 2 ,
- Ashley Cooper 2 , 3 &
- Rona Campbell 1
International Journal of Behavioral Nutrition and Physical Activity volume 16 , Article number: 138 ( 2019 ) Cite this article
97k Accesses
113 Citations
23 Altmetric
Metrics details
Mental illness is a worldwide public health concern. In the UK, there is a high prevalence of mental illness and poor mental wellbeing among young people. The aim of this study was to investigate whether physical activity is associated with better mental wellbeing and reduced symptoms of mental health disorder in adolescents.
A cohort of 928 12–13 year olds (Year 8) from six secondary schools in England, who had participated in the AHEAD trial, ‘Activity and Healthy Eating in Adolescence’, were followed up three years later (when 15–16 years old, Year 11). At baseline, physical activity was measured using accelerometers. At follow-up, mental wellbeing was measured using the ‘Warwick Edinburgh Mental Wellbeing Scale’ (WEMWBS) and symptoms of mental health disorder using the ‘Strengths and Difficulties Questionnaire’ (SDQ). Multivariable linear regression analyses were used to investigate associations between physical activity and both mental wellbeing and symptoms of mental health disorder.
794 (86%) of the eligible 928 young people provided valid accelerometer data at baseline. 668 (72%) provided complete mental wellbeing data and 673 (73%) provided complete symptoms of mental health disorder data at follow-up. The multivariable analyses showed no evidence of an association between physical activity volume (counts per minute (cpm)) or intensity (Moderate to Vigorous Physical Activity (MVPA)) and mental wellbeing (WEMWBS overall score) or overall symptoms of mental health disorder (SDQ Total Difficulties Score). However, higher levels of physical activity volume at age 12–13 years were associated with lower scores on the emotional problems subscale of the SDQ at age 15–16 years.
Conclusions
This cohort study found no strong evidence that physical activity is associated with better mental wellbeing or reduced symptoms of mental health disorder in adolescents. However, a protective association between physical activity and the emotional problems subscale of the SDQ was found. This suggests that physical activity has the potential to reduce symptoms of depression and anxiety in adolescents. Future cohort study designs should allow for repeated measures to fully explore the temporal nature of any relationship.
Mental illness is a worldwide public health concern [ 1 ]. It is currently the largest single cause of disability in the UK representing an estimated 28% of the total disease burden (compared to 16% each for cancer and heart disease) [ 2 ]. The World Health Organization (2013) estimates that, worldwide, 20% of adolescents in any given year may experience mental illness. In England, the most recent population survey (2017) reported 14.4% (1 in 7) of young people aged 11–16 years were identified with a mental health disorder [ 3 ]. Emotional disorders (present in 9%) were the most common type at this age followed by behavioural (conduct) disorders (6.2%) [ 3 ]. Mental health disorder has diverse and long-term negative effects on individuals, their families, and wider society [ 4 ].
Population surveys have also found increased levels of low wellbeing in young people [ 3 ]. Mental wellbeing is conceptualised as more than the absence of mental illness [ 5 ]. It has been described as encompassing hedonic (happiness, life satisfaction, and affect) and eudaimonic (positive functioning, sense of purpose, and self-acceptance) wellbeing [ 6 , 7 , 8 , 9 , 10 ]. Mental wellbeing is protective for a range of health outcomes [ 11 , 12 , 13 , 14 ] and found to be associated with higher educational outcomes in adolescence and better occupational functioning in adulthood [ 15 , 16 , 17 ]. Correlates of young peoples’ mental illness and mental wellbeing are reported to be largely distinct, stressing the importance of considering these concepts separately and avoiding their conflation [ 18 ].
While mental illness and mental wellbeing may be related, they are not necessarily distinct ends of a continuum [ 19 , 20 , 21 ]. The dual continuum model views mental illness (or mental health disorder) and mental health (or mental wellbeing) as two separate continua rather than as opposite ends of the same continuum [ 20 ]. Keyes and Lopez (2002) depicted the dual continuum model of mental illness and mental health and described four states: struggling (incomplete mental illness i.e. mental illness and high wellbeing), floundering (complete mental illness i.e. mental illness and low wellbeing), languishing (incomplete mental health i.e. no mental illness and low wellbeing), and flourishing (complete mental health i.e. no mental illness and high wellbeing). A large number of adolescents are thought to suffer from poor mental wellbeing despite being free from mental illness [ 4 , 22 ]. Therefore, promoting mental wellbeing alongside preventing and treating the symptoms of mental illness, is a growing priority. The recent Green Paper (2018) focuses on schools finding low cost and low risk interventions to promote mental wellbeing and prevent symptoms of mental health disorder [ 23 ].
Although there is evidence of physical activity improving mental wellbeing [ 24 , 25 ] and having the potential to prevent symptoms of mental health disorder [ 26 , 27 ] in adults, the evidence of any relationship in adolescents is weaker. The studies lack measurement consistency, having defined and assessed physical activity, mental wellbeing, and symptoms of mental health disorder in a variety of ways. Furthermore, few studies have used a multi-dimensional measure of mental wellbeing or symptoms of mental health disorder (most capture only one component of mental wellbeing such as self-esteem [ 28 ] or self-efficacy [ 29 ] or a specific mental health problem such as depression [ 30 , 31 , 32 , 33 , 34 ]), and studies that have used an objective measure of physical activity to assess any relationship are limited [ 35 , 36 , 37 ].
Several reviews have attempted to analyse any association in young people [ 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 ]. A review of reviews by Biddle et al. (2011) [ 48 ] showed that physical activity has beneficial effects on mental health in children and adolescents. More recently there has been a significant increase in the number and quality of studies exploring any association, and when the review of reviews was updated in 2019 [ 49 ], physical activity continued to be shown to be associated with certain mental health outcomes in young people (a causal association was found with cognitive functioning, a partial association for depression, no association for self-esteem, and research focusing on the association of physical activity with anxiety was reported to be variable but generally showed small beneficial effects) [ 49 ]. A review by Rodriguez-Ayllon et al. (2019) [ 50 ] analysed the effects of physical activity interventions (randomised controlled trials and non-randomised controlled trials) on mental health outcomes of adolescents and also synthesised the observational evidence (both longitudinal and cross-sectional). Their review included studies that had at least one ‘psychological illbeing’ (i.e. depression, anxiety, stress or negative effect) and/or ‘psychological wellbeing’ (self-esteem, self-concept, self-efficacy, self-image, positive affect, optimism, happiness and satisfaction with life) outcome. They concluded that there was a small positive effect of physical activity interventions on mental health outcomes in adolescents [ 50 ].
The SDQ is a unique screening tool of symptoms indicating overall mental health disorder in young people. This composite measure identifies symptoms of emotional problems, hyperactivity, and behavioural/conduct problems and has been used in the UK series of surveys of the mental health of children and young people (1999, 2004 and 2017) [ 3 ] alongside other significant population surveys [ 52 ]. Despite this, few studies have used this measure when looking at the association between physical activity and symptoms of mental health disorder [ 31 , 53 , 54 , 55 ]. Of the studies identified, neither of the two longitudinal studies used an objective measure of physical activity [ 31 , 53 ].
The WEMWBS is a relatively new scale, also used in the series of surveys in the UK [ 3 ], designed to capture population mental wellbeing. The reviews that have included studies assessing the relationship between physical activity and various aspects of mental wellbeing [ 38 , 39 , 40 , 41 , 42 , 43 , 44 ; 46 , 47 , 48 , 49 , 50 ] have concluded that there is evidence of promise, but further studies are needed that use a multi-dimensional measure such as the WEMWBS.
Given the limitations of the evidence base, the aim of this study was to determine whether physical activity is associated with mental wellbeing and symptoms of mental health disorder in adolescents. This is the first study to investigate any potential relationship longitudinally using an objective measure of physical activity and valid and reliable self-report measures of both mental wellbeing, using the WEMWBS, and symptoms of mental health disorder, using the SDQ, in adolescents.
A prospective cohort was formed based on the 928 participants from six secondary schools in the South West of England who took part in a two-year school-based exploratory randomised controlled trial (RCT) of an Activity and Healthy Eating intervention for use in ADolescence: the AHEAD trial [ 56 ]. All state secondary schools in the selected local authorities were invited to participate in the study. Schools first to express an interest (ensuring variation in size, geographical area, Ofsted rating, Free School Meal entitlement, and achievement rating) were recruited to the study. Physical activity was measured in 2008 when the participants were aged 12–13 years (Year 8); mental wellbeing and symptoms of mental health disorder was measured three years later (2011) when the participants were aged 15–16 years (Year 11). The inclusion criteria were participation in the AHEAD trial and continued attendance at a study school three years later. Data collections at baseline (2008) and follow-up (2011) were conducted by a team of researchers in the schools (classrooms or school halls) during a usual lesson (approximately 60 min). There was no evidence of promise that the AHEAD intervention improved physical activity or diet.
Physical activity measure
The ActiGraph GT1M accelerometer (ActiGraph, LLC, Penscola, FL) was used to measure physical activity. Participants were instructed in the use of the accelerometers in school, and then asked to wear the instrument for seven days during waking hours, except for water-based activities such as bathing and swimming. Accelerometer data were downloaded using ActiLife software (Lifestyle Monitor System software Version 3.3.0) and processed using Kinesoft software (Version 3.3.62; Kinesoft, Saskatchewan, Canada) to generate outcome variables (10 s epochs were used to capture the sporadic nature of adolescent physical activity). Physical activity volume was computed as mean accelerometer counts per minute (cpm), and physical activity intensity (mean minutes per day of Moderate to Vigorous Physical Activity (MVPA)) was computed using established thresholds [ 57 ]. A valid day of measurement was defined as recording at least 480 min (8 h) of data (monitoring period from 7 am until 11 pm; periods of ≥60 min of consecutive zeros, with allowance for 2 min of interruption, was classed as nonwear time) and at least three valid days were required for inclusion in analyses.
Mental wellbeing and symptoms of mental health disorder measures
The ‘Warwick Edinburgh Mental Wellbeing Scale’ (WEMWBS) [ 58 ], validated for use in adolescents aged 13–16 years, was used to measure mental wellbeing. The WEMWBS has 14 positively worded items with a five-point Likert scoring scale for each item (with scores ranging from 1 = none of the time to 5 = all of the time). The responses to each item were summed to give an overall WEMWBS score; a minimum score of 14 (i.e. poor mental wellbeing) and a maximum of 70 (i.e. good mental wellbeing). The higher score, indicative of better mental wellbeing, reflects more positive thoughts, feelings and behaviours. Where scores for three or less items were missing the mean value of responses for completed items for that individual was used to replace the score for missing items, enabling a total score for that individual to be computed [ 59 ]. If more than three items were missing the data for that participant were not used. The WEMWBS was selected due to it being the first multi-dimensional scale to measure population mental wellbeing in adolescents, based on established indicators. It covers most aspects of mental wellbeing including both hedonic and eudaimonic perspectives and is suitable for looking at the relationship between physical activity and mental wellbeing.
The ‘Strengths and Difficulties Questionnaire’ (SDQ) [ 60 ] was used to measure symptoms of mental health disorder. It is a behavioural screening tool used to assess social, emotional, and physical aspects of behaviour in young people [ 61 ] and has been shown to be valid and reliable for completion by 11–16 year olds [ 62 ]. The questionnaire has 25 items which comprise five subscales: (i) emotional symptoms (anxiety and depressive symptoms); (ii) conduct problems; (iii) hyperactivity/inattention; (iv) peer relationship problems; and (v) pro-social behaviour (positive behaviours such as being kind and helpful, scored in reverse of the other subscales). Response options are ‘not true, somewhat true, or certainly true’ (scored 0, 1 or 2). The SDQ ‘Total Difficulties Score’ (SDQ TDS) was generated by adding together the scores from the first four subscales and can range from 0 (low difficulties) to 40 (high difficulties). The five subscales whose scores can vary from 0 to 10 were also investigated independently. Items scores which were missing were imputed only if at least three out of five items were complete on each subscale. In this case the total subscale score for each participant was divided by the number of complete items to get the mean score and used to replace the missing item score [ 60 , 63 ]. If more than two items were missing from any sub scale the data for that subscale for that participant were not used. Participants required a score for each of the SDQ subscales to be able to compute their SDQ TDS. The SDQ was selected as the SDQ TDS provides a useful indicator of the level of symptoms of mental health disorder overall. Furthermore, the subscale items may be used to indicate specific clinical disorders in adolescents: depression, anxiety, hyperactivity attention deficit disorder (ADHD) and behavioural/conduct disorder. The SDQ is a useful screening tool for identifying young people with raised scores thus potentially at risk.
Possible confounders and mediators
The self-report behavioural questionnaires recorded a number of potential confounders and mediators of any potential relationship: age; gender; ethnicity; socioeconomic status (SES) (measured using the ‘Family Affluence Scale’ FAS II [ 64 ]); study school; number of daylight minutes (a proxy for season); baseline symptoms of mental health disorder (SDQ TDS); sleep (frequency of feeling tired when going to school in the morning); number of friends; belonging to teams and clubs; smoking; drinking alcohol; and intervention arm of the AHEAD trial [ 56 ] (the participants were randomised into two groups - the intervention arm received a physical activity and healthy eating intervention and the control arm continued with usual practice).
Confounders included were determined by the construction of a directed acyclic graph (DAG) and the availability of relevant data on study participants. Accelerometer wear time was computed from the participants accelerometer data.
Data from the self-report behavioural questionnaires were entered into a secure Access database and the accelerometer data were stored as anonymised files on a secure drive. All analyses were conducted using Stata 13 MP [ 65 ].
Statistical analysis
The analyses assessed the association between physical activity and the measures of mental wellbeing and symptoms of mental health disorder. Multivariable linear regression analyses were used to estimate exposure effects controlling for potential confounders and mediators which were investigated by grouping them as clusters of related factors in the models: i.e. socioeconomic factors (ethnic group, SES, study school); factors that may influence the physical activity data processing (daylight minutes (when volume or MVPA exposure), minutes of wear time (when MPVA exposure only); lifestyle factors (sleep, friends, belonging to teams or clubs, drinking alcohol, smoking; measured at follow-up only); baseline symptoms of mental health disorder); and then by producing a fully adjusted model containing all of these factors. Where there was evidence of confounding or mediation (associations weakened or enhanced), further models were fitted to investigate this in more detail. Confounders adjusted for were determined by the availability of relevant data on study participants. This somewhat crude epidemiological approach was used due to there being no clear evidence of associations (and whether confounders or mediators in the relationship) in the literature. Coefficients represent the linear relationship- change in WEMWBS overall score, SDQ TDS or SDQ subscale score per unit increase in physical activity (volume or intensity). Physical activity volume was defined by accelerometer counts (a dimensionless output from the accelerometer) per minute of recording (computed as total counts recorded divided by the total minutes of valid recording over the measurement period, described as counts per minute (cpm)), whilst physical activity intensity was defined as daily minutes of Moderate to Vigorous Physical Activity (MVPA). The relationship was quantified as the change in mental wellbeing or symptoms of mental health disorder score associated with an increase of 100 cpm (e.g. an increase from 508 cpm to 608 cpm, an approximately 20% increase in physical activity volume from baseline mean of the sample); or an additional 60 min of daily MVPA. Tests for interactions were carried out to investigate whether observed associations differed by gender. There was no evidence that associations between physical activity (volume and MVPA) and either mental wellbeing or symptoms of mental health disorder (WEMWBS and SDQ) differed in males and females. The test for interaction p -value ranged from p = 0.19–0.97 so all models were based on data for males and females combined.
Ethics approval and consent to participate
The University of Bristol Faculty of Medicine and Dentistry Ethics Committee gave full approval in 2007 for the AHEAD feasibility study and pilot trial (reference number 060702) and in 2011 for the cohort study (reference number 101119).
Consent procedures were the same in the original feasibility study and pilot trial and in the subsequent cohort study. Firstly, written consent to participation was sought from each schools’ headteacher. Secondly, letters were posted by school staff to the parents/carers of all eligible school pupils explaining the study and enclosing a reply slip to be returned if parents/carers did not want their child to participate. This ‘opt-out’ method of consent has been found to be an ethical and appropriate procedure in low-risk prevention research and avoids the low response rates and potential sampling bias when opt-in parental consent procedures are used [ 66 , 67 ]. At all data collections, the young people were provided with information about the study and informed that they could ‘opt-out’ of some or all the study activities at any point and were asked to sign individual assent forms.
Cohort study profile and baseline characteristics
794 (86%) of the 928 pupils provided complete, valid baseline physical activity data and were followed-up three years later to complete mental wellbeing and symptoms of mental health disorder measures. 673 (73%) completed the SDQ and 668 (72%) completed the WEMWBS at follow-up. Those lost to follow-up were more likely to be older, male and from one particular school (due to a new headteacher using alternative educational placements for a large number of the school’s more challenging pupils). Table 1 shows the baseline characteristics of the participants included and excluded from the cohort. Figure 1 displays the study profile for the cohort study and Table 2 describes the baseline characteristics of the participants.
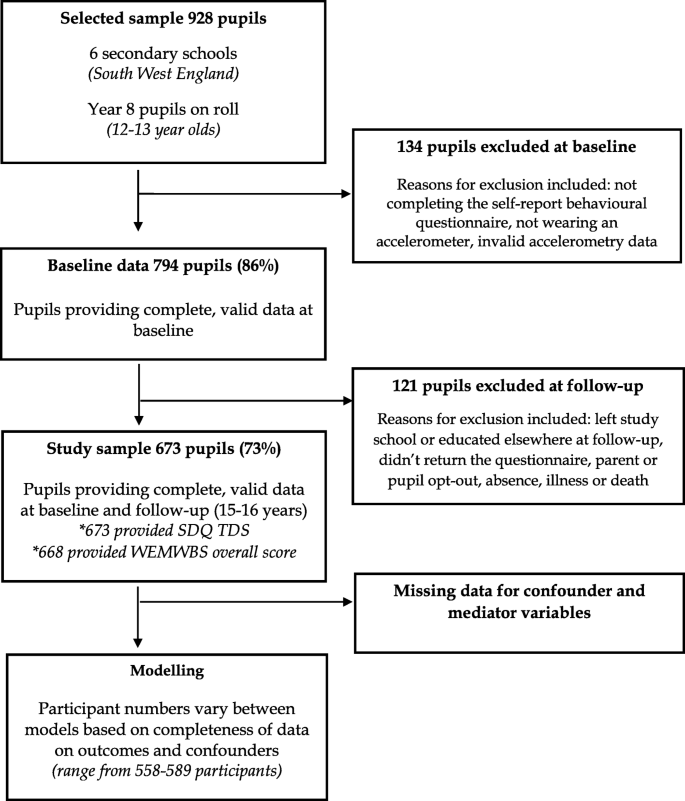
Study profile for cohort study
Physical activity at baseline
At baseline, overall physical activity volume (mean (SD) counts per minute (cpm)) was 508.3 cpm (169.42) and participants recorded 55.6 (21.5) (mean (SD)) daily minutes of MVPA). Females were less active than males with regard to both physical activity volume (mean difference 86.39 cpm (95% CI 111.2 cpm to 61.6 cpm, p < 0.001) and intensity (mean difference 11.7 min (95% CI − 15.41 to − 8.82), p < 0.001).
Mental wellbeing and symptoms of mental health disorder at follow-up
There was a negative association between the WEMWBS overall score and the SDQ TDS (r = − 0.41) at follow-up. This relatively weak correlation indicates the scales are measuring different things (the WEMWBS overall score only accounts for 16% of the total variation in the SDQ TDS). At follow-up, the participants’ WEMWBS overall mean (SD) score was 48.74 (8.66) (data from a similar study (13–16 year olds) 48.8 (8.66) [ 58 ]; females ( n = 342) 46.93 (8.90) and males ( n = 326) 50.63 (7.99) with strong evidence of a gender difference in WEMWBS overall score (mean difference in WEMWBS overall score − 3.70 (95% CI − 4.99 to − 2.24) p < 0.001). Females had a lower WEMWBS overall score indicating poorer mental wellbeing than males. The participants’ SDQ TDS mean score was 12.17 (5.56) (normative data (for 11–15 years) 10.3 (5.2)) [ 60 ]; females ( n = 343) 12.66 (5.36) and males ( n = 330) 11.66 (5.73). Again there was evidence of a gender difference in SDQ TDS (mean difference in SDQ TDS 1.00 (95% CI 0.16 to 1.84) p = 0.02). Females had a higher SDQ TDS indicating higher symptoms of mental health disorder than males.
Main findings
The univariable (adjusted for gender, age and intervention arm of the AHEAD trial) and multivariable analyses showed no evidence of an association between physical activity (volume or intensity) and mental wellbeing (WEMWBS overall score) or overall symptoms of mental health disorder (SDQ TDS) (Table 3 ). When the five SDQ subscales were analysed independently, an association was found between both physical activity volume and intensity and the emotional problems subscale of the SDQ (scale range 0–10). However, the association found between MVPA and the emotional problems subscale of the SDQ was slightly attenuated in the fully adjusted model (when controlling for symptoms of mental health disorder at baseline (SDQ TDS)), such that confidence intervals included the null value.
For physical activity volume, a mean increase of 100 cpm (~ 20% increase in physical activity volume) was associated with a decrease in the emotional problems subscale score of 0.12 (unadjusted model) and 0.11 (fully adjusted model). The confidence intervals (95% CI) ranged from − 0.23 to − 0.00 in the fully adjusted model implying that a potential reduction in the emotional problems subscale score of 0.23 could be achieved with an additional 100 mean cpm of physical activity (the extreme end of the effect estimate). For physical activity intensity, an additional 60 min of mean daily MVPA was associated with a decrease in the emotional problems subscale score of 0.54 (unadjusted model) and 0.49 (fully adjusted model; however confidence intervals crossed zero).
To the best of our knowledge, this is the first longitudinal study to investigate the relationship between physical activity, mental wellbeing and symptoms of mental health disorder in adolescents. We also believe this is the first study to use an objective measure of physical activity (accelerometers) and composite measures of both mental wellbeing (WEMWBS) and symptoms of mental health disorder (SDQ) validated for use with young people alongside each other, to investigate any potential associations. We found no evidence of an association between physical activity (volume or MVPA) and mental wellbeing (WEMWBS overall score) or overall symptoms of mental disorder (SDQ TDS). However, a protective association was found between physical activity volume and the emotional problems subscale of the SDQ. This finding suggests that increasing physical activity volume in adolescents may have the potential to reduce their risk of emotional problems (items on the SDQ emotional problems subscale include: worrying a lot; having fears and being easily scared; being nervous in new situations and easily losing confidence; often feeling unhappy, down-hearted or tearful; and getting a lot of headaches, stomach-aches or sickness). Those adolescents accumulating more daily MVPA minutes may have more beneficial effects. Physical activity could provide an acceptable, low risk and cost-effective intervention for young people showing symptoms of depression and anxiety.
Strengths and limitations of the study
The study was based on a relatively large number of secondary school pupils drawn from six schools of different sizes and characteristics (e.g. rural schools, inner city schools) [ 56 , 68 ]; participants are likely to be broadly representative of secondary school pupils in England. Loss to follow-up was largely due to participants no longer attending a study school and this is unlikely to have biased the patterns of associations found.
A strength of this study was its use of accelerometers, which provide an objective measure of physical activity increasing the precision of measurement. However, it is important to note that accelerometers have known limitations such as not accurately measuring cycling and not being waterproof, so do not measure physical activity from water-based activities.
This study contributes to the evolving debate concerning mental wellbeing and mental illness terminology and measurement. The findings from this study support the notion that mental wellbeing and symptoms of mental health disorder are two separate concepts, captured using different measurement scales. Using validated measures of both mental wellbeing and symptoms of mental health disorder was a strength and novel aspect of this study. This study demonstrated that physical activity is not associated with mental wellbeing or overall symptoms of mental health disorder, but has a protective relationship with regards to risk of emotional problems.
The cohort study would have benefited from repeated measures of physical activity, mental wellbeing and symptoms of mental health disorder, to fully explore the temporal nature of any relationship and take account of changing patterns of physical activity. If an effect of physical activity on mental wellbeing and symptoms of mental health disorder is short-lived, then a three-year time lag would be inappropriate to investigate any association [ 69 ].
We were able to control for a wide range of possible confounders and assess the effect of possible mediators of the relationship. However, some confounders were only measured at follow-up (sleep, number of friends, smoking, drinking alcohol, belonging to teams and clubs). The possible effects of some of the confounders may be different at baseline and follow-up (e.g. smoking and drinking behaviours would be more common at follow-up). Due to the WEMWBS not being available at the time of baseline measures, the SDQ TDS was used to control for baseline wellbeing. We were only able to adjust for confounders measured as part of the AHEAD trial. This study would have been strengthened if Body Mass Index (BMI) [ 70 ] and screen viewing behaviour [ 71 ] were measured and controlled for. The possible mechanisms underlying any association between physical activity, mental wellbeing and symptoms of mental health disorder in adolescents are complex [ 41 ]. It is possible that an integrative model that combined components of different hypotheses (biochemical e.g. release of endorphins, or psychosocial e.g. distraction, sense of mastery, social interaction) offers the most likely, full explanation [ 41 ]. Also, the effects may vary between individuals. Further research needs to consider confounding and mediating factors and exploration of potential mechanisms at the study design stage, to ensure candidate variables are measured appropriately.
Findings in the context of existing research
Studies that have explored the relationship between physical activity and symptoms of overall mental health disorder (using the SDQ) are scarce, and of those identified, no association was reported overall [ 31 ; 53 , 54 , 55 ]. However, Sagatun et al. (2007) [ 53 ] found that for males (but not females) the number of weekly hours (self-reported weekly hours of physical activity that makes them breathless) the boys spent on physical activity per week at age 15–16 years was negatively associated with emotional problems and peer problems at age 18–19 years. Similarly, Wiles et al. (2008) [ 31 ] reported young people (aged 11–14 years) who met recommended levels for physical activity (1 h per day) had, on average, a score on the emotional problems sub-scale of the SDQ that was 0.29 units lower (− 0.29 (95%CI − 0.61 to 0.022)) at 1 year follow-up compared to those who did not undertake recommended levels of physical activity. The association found in our study between physical activity volume and the emotional problems subscale of the SDQ (− 0.11 (95% CI − 0.23 to − 0.00)) (overall but not when gender stratified) is similar to the findings of both these studies, and supports evidence from the recent physical activity and mental health in young people reviews [ 49 , 50 ].
As noted at the outset, there are no longitudinal studies or RCTs that have used a multi-dimensional scale to investigate the relationship between physical activity and mental wellbeing in adolescents with which to compare our findings. Reviews have suggested evidence of promise [ 41 , 50 ] but studies included only used single component measures of mental wellbeing outcomes such as self-image, satisfaction with life and happiness. In the review of reviews by Biddle et al. (2019) [ 49 ] evidence for support of a causal relationship was reported for cognitive function outcome measures, as well as academic achievement and brain structure and function. Although showing an association between physical activity and cognitive function is important to emphasis the role of physical activity in schools, this literature needs to be considered alongside further studies using a composite measure of mental wellbeing.
Implications
There is no strong evidence of any relationship between physical activity, mental wellbeing and overall symptoms of mental health disorder in adolescents. However the findings from this study, together with that from two other studies, suggests a relationship between physical activity volume and emotional problems. Cohort studies, designed specifically to look at the relationship between physical activity and both mental wellbeing and symptoms of mental health disorder, are needed to confirm and explore any potential associations further. Measurement scales that focus on more than one aspect of mental health disorder or mental wellbeing should be used in population level school-based research, and both the SDQ and WEMWBS scales warrant further exploration. Alongside this literature, the association between physical activity and specific mental health disorders should continue to be explored. Measures that can confirm an International Statistical Classification of Diseases and Related Health Problems (ICD- 10 ) or Diagnostic and Statistical Manual of Mental Disorders ( DSM - 5 ) diagnosis in young people, such as the DAWBA (Development and Well-being Assessment), should be considered. Further studies that focus on mental health disorders common in adolescents, other than anxiety and depression, are needed. An objective measure of physical activity used alongside a standardised self-report physical activity questionnaire may be the best approach to understand the context of the physical activity data (e.g. physical activity outdoors may be better for mental wellbeing and team sports may prevent a particular type of mental health disorder). It is important that the self-report measure of physical activity incorporates information on general daily living activities, such as walking to and from school or playing outdoors, and captures any relevant contextual information [ 70 ]. Future study designs should allow for repeated measures to fully explore the temporal nature of any relationship, take account of changing patterns of physical activity and look at short-term associations.
This cohort study provided no strong evidence that physical activity is a protective factor for mental wellbeing or symptoms of mental health disorder in adolescents, as measured by the WEMWBS overall score and SDQ TDS. There was, however, evidence of an association between physical activity volume and the emotional problems subscale of the SDQ. This indicates that emotional problems (such as symptoms of depression and anxiety) in adolescents could be reduced by increasing their physical activity levels.
Availability of data and materials
The datasets during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Activity and Health Eating in ADolescence
Body Mass Index
Confidence Interval
Counts Per Minute
Development and Well-being Assessment
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) FAS (Family Affluence Scale)
International Statistical Classification of Diseases and Related Health Problems
Moderate to Vigorous Physical Activity
Standard Deviation
Strengths and Difficulties Questionnaire Total Difficulties Score
Strengths and Difficulties Questionnaire
Social Economic Status
Warwick Edinburgh Mental Wellbeing Scale
World Health Organization. The global burden of disease: 2004 update. Geneva; 2014.
Ferrari A, Charlson F, Norman R, Patten S, Freedman G, Murray C, Vos T, Whiteford H. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS med. 2013;10(11):e1001547.
Article PubMed PubMed Central Google Scholar
Sadler K, Vizard T, Ford T, Marcheselli F, Pearce N, Mandalia D, Davis J, Brodie E, Forbes N, Goodman A, Goodman R, McManus S. Mental health of children and young people in England, 2017. London: NHS digital; 2018.
Google Scholar
Davies S. Annual report of the chief medical officer 2013, public mental health priorities: investing in the evidence. London: Department of Health; 2014.
Ryan RM, Deci EL. On happiness and human potentials: a review of research on hedonic and eudaimonic well-being. Annu Rev Psychol. 2001;52(1):141–66. https://doi.org/10.1146/annurev.psych.52.1.141.f .
Article CAS PubMed Google Scholar
Pollard EL, Lee PD. Child well-being: a systematic review of the literature. Soc Indic Res. 2003;61(1):59–78.
Article Google Scholar
Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57(6):1069.
Diener E, Suh E. Measuring quality of life: economic, social, and subjective indicators. Soc Indic Res. 1997;40(1–2):189–216.
Seligman ME. Authentic happiness: using the new positive psychology to realize your potential for lasting fulfilment: Simon and Schuster; 2004.
Foresight. Foresight mental capital and wellbeing project: final project report. London: The Government Office for Science; 2008.
National Statistics: The Scottish Health Survey 2008:ISBN 978 0 7559 8107 6. accessed 16/01/2011.
Davidson R. Well-being and affective style: neural substrates and biobehavioural correlates. Philosophical transactions of the Royal Society of London. Series B: Biological Sci. 2004;359(1449):1395–411.
Singh-Manoux A, Martikainen P, et al. What does self rated health measure? Results from the British Whitehall II and French Gazel cohort studies. J Epidemiol Community Health. 2006;60(4):364–9.
Keyes CL. The nexus of cardiovascular disease and depression revisited: the complete mental health perspective and the moderating role of age and gender. Aging Ment Health. 2004;8(3):266–74.
Stewart-Brown S. Promoting health in children and young people: identifying priorities. J R Soc Promot Health. 2005;125(2):61.
Article PubMed Google Scholar
Barlow J, Underdown A. Promoting the social and emotional health of children: where to now? J R Soc Health. 2005;125(2):64–70.
Currie C, Roberts C, Settertobulte W, Morgan A, Smith R, Samdal O, Barnekow RV. Young People's health in context: health behaviour in school-aged children (HSBC) study: international report from the 2001/2002 survey. WHO Regional Office for Europe: Copenhagen; 2004.
Patalay P, Fitzsimons E. Correlates of mental illness and wellbeing in children: are they the same? Results from the UK millennium cohort study. J Am Acad Child Adolesc Psychiatry. 2016;55(9):771–83.
Tudor K. Mental health promotion: paradigms and practice: psychology press; 1996.
Keyes CL. Lopez SJ. Toward a science of mental health. 2002:45–59.
Holder MD. Happiness in children: measurement, correlates and enhancement of positive subjective well-being. London: Springer Science and Business Media; 2012.
Book Google Scholar
Roberts RE, Attkisson CC, Rosenblatt A. Prevalence of psychopathology among children and adolescents. Am J Psychiatr. 1998;155(6):715–25.
CAS PubMed Google Scholar
Department of Health and Social Care and Department for Education. Transforming children and young people’s mental health provision: A green paper. London; 2018.
Scully D, Kremer J, Meade MM, Graham R, Dudgeon K. Physical exercise and psychological well being: a critical review. Br J Sports Med. 1998;32(2):111–20.
Article CAS PubMed PubMed Central Google Scholar
Fox KR. The influence of physical activity on mental well-being. Public Health Nutr. 1999;2(3a):411–8.
Paluska SA, Schwen TL. Physical activity and mental health. Sports Med. 2000;29(3):167–80.
Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, McMurdo M, Mead GE. Exercise for depression. Cochrane Database of Systematic Reviews 2013, Issue 9. Art. No.: CD004366. DOI: https://doi.org/10.1002/14651858.CD004366.pub6 .
Tremblay MS, Inman JW, Willms JD. The relationship between physical activity, self-esteem, and academic achievement in 12-year-old children. Pediatr Exerc Sci. 2000;12(3):312–23.
Valois RF, Umstattd MR, Zullig KJ, Paxton RJ. Physical activity behaviors and emotional self-efficacy: is there a relationship for adolescents? J Sch Health. 2008;78(6):321–7.
Wiles NJ, Haase AM, Lawlor DA, Ness A, Lewis G. Physical activity and depression in adolescents: cross-sectional findings from the ALSPAC cohort. Soc Psychiatry Psychiatr Epidemiol. 2012;47(7):1023–33.
Wiles NJ, Jones GT, Haase AM, Lawlor DA, Macfarlane GJ, Lewis G. Physical activity and emotional problems amongst adolescents. Soc Psychiatry Psychiatr Epidemiol. 2008;43(10):765–72.
Motl RW, Birnbaum AS, Kubik MY, Dishman RK. Naturally occurring changes in physical activity are inversely related to depressive symptoms during early adolescence. Psychosom Med. 2004;66(3):336–42.
PubMed Google Scholar
Birkeland MS, Torsheim T, Wold B. A longitudinal study of the relationship between leisure-time physical activity and depressed mood among adolescents. Psychol Sport Exerc. 2009;10(1):25–34.
Rothon C, Edwards P, Bhui K, Viner RM, Taylor S, Stansfeld SA. Physical activity and depressive symptoms in adolescents: a prospective study. BMC Med. 2010;8(1):32.
Opdal IM, Morseth B, Handegård BH, Lillevoll K, Ask H, Nielsen CS, Horsch A, Furberg AS, Rosenbaum S, Rognmo K. Change in physical activity is not associated with change in mental distress among adolescents: the Tromsø study: fit futures. BMC Public Health. 2019;19(1):916.
Van Dijk ML, Savelberg HH, Verboon P, Kirschner PA, De Groot RH. Decline in physical activity during adolescence is not associated with changes in mental health. BMC Public Health. 2016;16(1):300.
Toseeb U, Brage S, Corder K, Dunn VJ, Jones PB, Owens M, et al. Exercise and depressive symptoms in adolescents: a longitudinal cohort study. JAMA Pediatr. 2014;168(12):1093–100.
Gruber JJ. Physical activity and self-esteem development in children: a meta-analysis. American Academy of Physical Education Papers. 1986;19:30–48.
Ekeland E, Heian F, Hagen KB, Abbott JM, Nordheim L. Exercise to improve self-esteem in children and young people. Cochrane Database Syst Rev. 2004;1.
Liu M, Wu L, Ming Q. How does physical activity intervention improve self-esteem and self-concept in children and adolescents? Evidence from a meta-analysis. PLoS One. 2015;10(8):e0134804.
Article PubMed PubMed Central CAS Google Scholar
Whitelaw S, Teuton J, Swift J, Scobie G. The physical activity–mental wellbeing association in young people: a case study in dealing with a complex public health topic using a ‘realistic evaluation’ framework. Ment Health Phys Act. 2010;3(2):61–6.
Burkhardt J, Brennan C. The effects of recreational dance interventions on the health and well-being of children and young people: a systematic review. Arts Health. 2012;4(2):148–61.
Lees C, Hopkins J. Peer reviewed: effect of aerobic exercise on cognition, academic achievement, and psychosocial function in children: a systematic review of randomized control trials. Prev Chronic Dis. 2013;10.
Ferreira-Vorkapic C, Feitoza JM, Marchioro M, Simões J, Kozasa E, Telles S. Are there benefits from teaching yoga at schools? A systematic review of randomized control trials of yoga-based interventions. Evid Based Complement Alternat Med. 2015.
Larun L, Nordheim L, Ekeland E, Hagen K, Heian F. Exercise in prevention and treatment of anxiety and depression among children and young people. Cochrane Database Syst Rev. 2006;4.
Ahn SA, Fedewa J. Meta-analysis of the relationship between physical activity and mental health. J Pediatr Psychol. 2011;10:22–8.
Das JK, Salam RA, Lassi ZS, Khan MN, Mahmood W, Patel V, Bhutta ZA. Interventions for adolescent mental health: an overview of systematic reviews. J Adolesc Health. 2016 Oct 1;59(4):S49–60.
Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. British J Sports Med. 2011;45(11):886–95.
Biddle SJ, Ciaccioni S, Thomas G, Vergeer I. Physical activity and mental health in children and adolescents: an updated review of reviews and an analysis of causality. Psychol Sport Exerc. 2019 May 1;42:146–55.
Rodriguez-Ayllon M, Cadenas-Sanchez C, Estevez-Lopez F, Muñoz NE, Mora-Gonzalez J, Migueles JH, Molina-Garcia P, Henriksson H, Mena-Molina A, Martinez-Vizcaino V, Catena A. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. 2019;16:1–28.
Caldwell DM, Davies SR, Hetrick SE, Palmer JC, Caro P, López-López JA, Gunnell D, Kidger J, Thomas J, French C, Stockings E. School-based interventions to prevent anxiety and depression in children and young people: a systematic review and network meta-analysis. Lancet Psychiatry. 2019;14.
Duinhof EL, Lek KM, de Looze ME, Cosma A, Mazur J, Gobina I, Wüstner A, Vollebergh WA, Stevens GW. Revising the self-report strengths and difficulties questionnaire for cross-country comparisons of adolescent mental health problems: the SDQ-R. Epidemiol psychiatric sci 2019 3:1–0.
Sagatun A, Søgaard AJ, Bjertness E, Selmer R, Heyerdahl S. The association between weekly hours of physical activity and mental health: a three-year follow-up study of 15–16-year-old students in the city of Oslo. Norway BMC Public Health. 2007;7(1):155.
Eather N, Morgan PJ, Lubans DR. Effects of exercise on mental health outcomes in adolescents: findings from the CrossFit™ teens randomized controlled trial. Psychol Sport Exerc. 2016;26:14–23.
Bunketorp Käll L, Malmgren H, Olsson E, Lindén T, Nilsson M. Effects of a curricular physical activity intervention on children's school performance, wellness, and brain development. J Sch Health. 2015;85(10):704–13.
Bell SL, Audrey S, Cooper AR, Noble S, Campbell R. Lessons from a peer-led obesity prevention programme in English schools. Health Promot Int. 2017;32(2):250–9.
Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–65.
Clarke A, Friede T, Putz R, Ashdown J, Martin S, Blake A, et al. Warwick-Edinburgh Mental Well-being Scale (WEMWBS): validated for teenage school students in England and Scotland. A mixed methods assessment. BMC Public Health. 2011;11(1):487.
Bartram DJ, Yadegarfar G, Sinclair JM, Baldwin DS. Validation of the Warwick–Edinburgh mental well-being scale (WEMWBS) as an overall indicator of population mental health and well-being in the UK veterinary profession. Vet J. 2011;187(3):397–8.
Goodman R. Youth in Mind 2010 http://www.sdqinfo.com/py/sdqinfo/c0.py . Accessed 09/02/2016.
Muris P, Meesters C, Eijkelenboom A, Vincken M. The self-report version of the strengths and difficulties questionnaire: its psychometric properties in 8-to 13-year-old non-clinical children. Br J Clin Psychol. 2004;43(4):437–48.
Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1337–45.
Goodman A, Lamping DL, Ploubidis GB. When to use broader internalising and externalising subscales instead of the hypothesised five subscales on the strengths and difficulties questionnaire (SDQ): data from British parents, teachers and children. J Abnorm Child Psychol. 2010;38(8):1179–91.
Boyce W, Torsheim T, Currie C, Zambon A. The family affluence scale as a measure of national wealth: validation of an adolescent self-report measure. Soc Indic Res. 2006;78(3):473–87.
StataCorp L. Stata 13. StataCorp LP., College Station, Texas, United States. http://www.stata.com ; 2013.
Campbell R, Starkey F, Holliday J, Audrey S, Bloor M, Parry-Langdon N, Hughes R, Moore L. An informal school-based peer-led intervention for smoking prevention in adolescence (ASSIST): a cluster randomised trial. Lancet. 2008;371(9624):1595–602.
Audrey S, Cordall K, Moore L, Cohen D, Campbell R. The development and implementation of a peer-led intervention to prevent smoking among secondary school students using their established social networks. Health Educ J. 2004;63(3):266–84.
Audrey S, Holliday J, Campbell R. It's good to talk: adolescent perspectives of an informal, peer-led intervention to reduce smoking. Soc Sci Med. 2006;63(2):320–34.
Clark C, Haines MM, Head J, Klineberg E, Arephin M, Viner R, et al. Psychological symptoms and physical health and health behaviours in adolescents: a prospective 2-year study in East London. Addiction. 2006;102(1):126–35.
Kimm SY, Glynn NW, Obarzanek E, Kriska AM, Daniels SR, Barton BA, Liu K. Relation between the changes in physical activity and body-mass index during adolescence: a multicentre longitudinal study. Lancet. 2005;366(9482):301–7.
Page AS, Cooper AR, Griew P, Jago R. Children's screen viewing is related to psychological difficulties irrespective of physical activity. Pediatrics. 2010;126(5):e1011–7.
Download references
Acknowledgements
Thanks are due to the schools and young people involved as this research would not have been possible without their support and willing participation.
The AHEAD trial (during which the baseline data was collected) was funded by the Department of Health Policy Research Programme (Project Number 0600002). SB was funded by a doctoral research fellowship from the National Institute for Health Research (NIHR-DRF-2010-03-51) to complete the follow-up study. The work was undertaken with the support of The Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UKCRC Public Health Research Centre of Excellence. Joint funding (MR/KO232331/1) from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the Welsh Government and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged. The funding sources were not involved in the design of the study and collection, analysis, and interpretation of data or in writing the manuscript. DG and AC are supported by the NIHR Biomedical Research Centre at University Hospitals Bristol NHS Foundation Trust and the University of Bristol, England. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
Author information
Authors and affiliations.
Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, BS8 2PS, UK
Sarah Louise Bell, Suzanne Audrey, David Gunnell & Rona Campbell
National Institute of Health Research Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust, Bristol, UK
David Gunnell & Ashley Cooper
Centre for Exercise, Nutrition and Health Sciences, School for Policy Studies, University of Bristol, Bristol, BS8 1TZ, UK
Ashley Cooper
You can also search for this author in PubMed Google Scholar
Contributions
SB planned and carried out the study, conducted the data analysis and wrote the manuscript. DG and RC advised on the data analysis and reviewed the manuscript. SA led the AHEAD trial and reviewed the manuscript. AC advised on the physical activity measurement and analysis and reviewed the manuscript.
Corresponding author
Correspondence to Sarah Louise Bell .
Ethics declarations
Consent for publication.
Not applicable.
Competing interests
The authors declare that they have no competing interests. RC is an NIHR Senior Investigator and member of the NIHR-PHR research funding committee. SA is a member of the NIHR-PHR research finding committee.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Bell, S.L., Audrey, S., Gunnell, D. et al. The relationship between physical activity, mental wellbeing and symptoms of mental health disorder in adolescents: a cohort study. Int J Behav Nutr Phys Act 16 , 138 (2019). https://doi.org/10.1186/s12966-019-0901-7
Download citation
Received : 23 April 2019
Accepted : 12 December 2019
Published : 26 December 2019
DOI : https://doi.org/10.1186/s12966-019-0901-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Physical activity
- Mental wellbeing/mental health/mental illness/mental health disorder
- Adolescents/young people
- Cohort study
International Journal of Behavioral Nutrition and Physical Activity
ISSN: 1479-5868
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 01 February 2022
The association between physical activity and mental health during the first year of the COVID-19 pandemic: a systematic review
- Priscila Marconcin 1 , 2 ,
- André O. Werneck 3 ,
- Miguel Peralta 2 , 4 ,
- Andreas Ihle 5 , 6 , 7 ,
- Élvio R. Gouveia 8 , 9 ,
- Gerson Ferrari 10 ,
- Hugo Sarmento 11 &
- Adilson Marques 2 , 3
BMC Public Health volume 22 , Article number: 209 ( 2022 ) Cite this article
30k Accesses
106 Citations
153 Altmetric
Metrics details
Introduction
The Coronavirus disease-19 (COVID-19) pandemic affected countries worldwide and has changed peoples’ lives. A reduction in physical activity and increased mental health problems were observed, mainly in the first year of the COVID-19 pandemic. Thus, this systematic review aims to examine the association between physical activity and mental health during the first year of the COVID-19 pandemic.
In July 2021, a search was applied to PubMed, Scopus, and Web of Science. Eligibility criteria included cross-sectional, prospective, and longitudinal study designs and studies published in English; outcomes included physical activity and mental health (e.g., depressive symptoms, anxiety, positive and negative effects, well-being).
Thirty-one studies were included in this review. Overall, the studies suggested that higher physical activity is associated with higher well-being, quality of life as well as lower depressive symptoms, anxiety, and stress, independently of age. There was no consensus for the optimal physical activity level for mitigating negative mental symptoms, neither for the frequency nor for the type of physical activity. Women were more vulnerable to mental health changes and men were more susceptive to physical activity changes.
Physical activity has been a good and effective choice to mitigate the negative effects of the COVID-19 pandemic on mental health during the first year of the COVID-19 pandemic. Public health policies should alert for possibilities to increase physical activity during the stay-at-home order in many countries worldwide.
Peer Review reports
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is a highly contagious virus that infects humans and causes coronavirus disease-19 (COVID-19), which is currently having a damaging impact on almost all countries worldwide [ 1 ]. To bring this pandemic to an end, a large share of the world needs to be immune to the virus, and the safest way to achieve this is with a vaccine. Fortunately, in December 2020 the vaccination started in the United Kingdom [ 2 ] and is currently pursued in different countries [ 3 ]. Until November 2021, 53.3% of the world population has received at least one dose of a COVID-19 vaccine [ 4 ]. However, the number of infected people and deaths continues to grow [ 5 ]. The World Health Organization (WHO) published a weekly report and on 16th of November 2021 it was observed a increasing trend in new global weekly cases [ 6 ]. From the beginning of the pandemic, as a community mitigation strategy used to reduce the spread of COVID-19, most countries adopted the stay-at-home order as well as the stimulation of facemask wearing and hygiene habits [ 7 , 8 ].
As a consequence of the stay-at-home strategies, mainly during the first year of the COVID-19 pandemic, studies had reported multiple behaviour changes. Some common impacts include disturbed eating behaviours [ 9 ], changes in alcohol consumption [ 10 ], and substance use [ 11 ]. A wide range of psychological outcomes has been observed during the virus outbreak, including a reduction in well-being as well as increases in depressive and anxiety symptoms [ 12 , 13 ]. Considering the need for social distancing measures, the investigation of possible factors that can mitigate the negative effects of social distancing on mental health should help the promotion of intervention strategies.
Physical activity (PA) is well recognised as a key factor for the prevention and management of mental illness, including mental disorders such as depression and anxiety as well as the promotion of mental health such as well-being [ 14 , 15 ]. Nevertheless, globally, approximately 23% of adults and 81% of adolescents do not meet the WHO recommendations regarding PA for maintaining health [ 16 , 17 , 18 ]. This situation even worsened with the COVID-19 pandemic. Studies have demonstrated that PA declined and sedentary behaviour increased during the COVID-19 pandemic stay at home order in many countries, regardless of the subpopulation [ 19 ]. Different studies sought to investigate whether these changes in PA were associated with mental health indicators during the COVID-19 pandemic and a previous systematic review synthetised that PA is an effective strategy to face the psychological effects of the COVID-19 pandemic [ 20 ]. However, the previous review included articles published between 1 January 2019, and 15 July 2020, before the second wave of the COVID-19 pandemic. Therefore, our systematic review aimed to update those findings and clarify if PA is associated with mental health during the first full year of the COVID-19 pandemic and to analyse if PA mitigates the effects of the stay-at-home order on mental health. We aimed to explore the first year of the COVID-19 pandemic because it was the period when restrictive orders were strictest when people were strongly encouraged to comply with the stay-at-home order.
This systematic review focuses on peer-reviewed journal articles on the relationship of PA to mental health during the COVID-19 pandemic published until 30 July 2021.
Data sources and searches
A systematic review protocol was registered with the PROSPERO database on the 29th of January 2021 (IDCRD42021233921). A broad search strategy was employed. Searches were conducted on the 30th of January 2021, in the following electronic databases: PubMed, Scopus, and Web of Science. The search was performed in the three databases using the terms: (physical activity OR physical inactivity OR exercise OR training OR sport* OR fitness OR physical function* OR movement behavio* OR sedentary behavio*) AND (mental health OR psychological health OR depress* OR anxiety OR psychological function* OR mental function* OR wellbeing OR well-being OR burnout OR burn-out OR fear OR fears OR worries OR worry) AND (coronavirus disease OR COVID-19 OR SARS-CoV-2 OR lockdown OR shutdown OR quarantine OR confinement OR social isolation). These terms were searched in title and abstract of scientific articles. Additionally, cross-referencing search was performed in the full-text read of potentially included articles.
Study selection
Observational studies (cross-sectional, prospective, or longitudinal) were eligible for this review. Furthermore, studies were also required to meet the following criteria: (1) assessing PA by a validated instrument, (2) assessing mental health by a validated instrument, (3) presenting an analysis on the association between PA and mental health. Studies with samples including pregnant women, chronic disease patients, athletes, COVID-19 survivors, and frail older adults were excluded. Besides, studies reporting PA as a moderate or mediated variable were also excluded. Two co-authors screened titles and abstracts to identify articles that met the inclusion criteria. Two co-authors read the articles and decided whether they should be included in the analysis or excluded. The inclusion decision was consensual and in cases of disagreement, the decision was made by mutual agreement.
Data extraction and synthesis of results
Data extraction was completed independently by one co-author. Data extracted from all studies included study details (author, year of publication, study design, recruitment processes, and date and location of the study); participant characteristics (sex, mean age); outcome and instruments, and main findings. A table was made for articles that analysed the association between PA and mental health among adults, and another table for the analyses of the association between PA and mental health among children and adolescents.
Quality assessment
The risk of bias was assessed by two independent reviewers, using the Newcastle-Ottawa Scale (NOS) [ 21 ] which was also adapted for cross-sectional studies [ 22 ]. Therefore, we used the original scale for cohort studies and the adapted scale for the cross-sectional studies. The original scale varies between 0 and 9, while the adapted scale for cross-sectional studies varies between 0 and 10, with higher scores indicating research of better quality.
Narrative synthesis
Considering the heterogeneity of methods used for the estimation of the exposures and outcomes, it was not possible to conduct a meta-analysis. Therefore, we compared the findings across the included articles according to each outcome.
Results of the search
From the database search, 734 records were identified. After removing duplicates, the titles and abstracts of 328 articles were screened concerning the eligibility criteria, and 205 were excluded. The full texts of the remaining 1237 articles were evaluated and 92 were excluded for the following reasons: sample characteristics ( n = 24), data were not analysed regarding the association between PA and mental health variables ( n = 23), review studies ( n = 4), no valid instruments to assess PA ( n = 31) and mental health ( n = 6), the study was not in the period of the COVID-19 pandemic ( n = 4). Thirty-one studies were included in this review, 27 about adults and old adults and 4 about children and adolescents. The flow diagram of study search and selection was created according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 23 ] and is presented in Fig. 1 . The mean score of quality was 5.7 ± 1.5. More details are presented in Tables 1 and 2 .
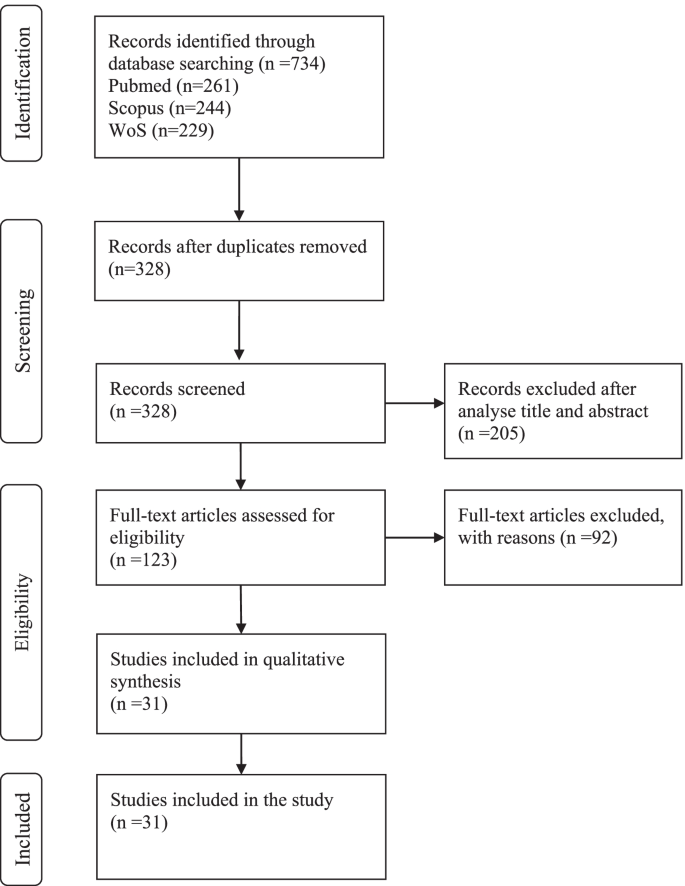
Flow diagram of study selection
The association between physical activity and mental health among adults and old adults
The details of the association between PA and mental health among adults and old adults are summarised in Table 1 , 27 studies were included [ 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 51 ].
Participants characteristics and date of filling the questionnaires
The number of participants in the 27 included studies varied between 66 [ 50 ] and 14,715 [ 40 ] participants. Regarding sex, with exception of four studies [ 24 , 31 , 40 , 48 ] the majority included more women than men. Concerning age, most articles presented the mean age range between 20 and 30 years [ 24 , 25 , 36 , 37 , 44 , 48 , 49 , 50 , 56 , 57 ], two article presented mean age between 30 and 40 years [ 33 , 43 ]; five articles presented mean age between 40 and 50 years [ 28 , 32 , 35 , 41 , 42 ]; and seven articles presented mean age above 50 years [ 26 , 27 , 34 , 45 , 46 , 47 , 51 ]. Four articles did not present mean age [ 31 , 38 , 39 , 40 ], for one article the age ranged between 21 and 35 years [ 31 ], for another, the age ranged between 21 and 40 years [ 38 ], for another, the age ranged between 17 and 69 years [ 40 ], and in one the age ranged between 27 and 53 years [ 39 ]. The majority of studies reported, the sample filled out online questionnaires. One study used interviewed by telephone call [ 34 ]. Twenty four studies conducted a cross-sectional analysis and four a longitudinal analysis.
Study location
The studies were carried out on five different continents. Ten studies from Europe [ 24 , 25 , 26 , 27 , 28 , 38 , 39 , 43 , 44 , 49 ], foure studies from Asia [ 36 , 40 , 46 , 48 , 50 ], seven studies from America [ 33 , 34 , 35 , 37 , 41 , 51 , 57 ] two studies from Africa [ 31 , 56 ], two study from Oceania [ 42 , 45 ], and two multi-centre study [ 32 , 47 ].
Outcomes and instruments
Concerning outcomes and instruments, 12 articles used the International Physical Activity Questionnaire (IPAQ) to assess PA and one article calculated an estimate of cardiorespiratory fitness (algorithm includes age, body composition, resting heart rate and PA) [ 57 ]. The others articles assessed PA with different instruments. Mental health included analyses of subjective well-being, sleep quality, depressive symptoms, anxiety, quality of life, psychological distress, motivation, resilience, affects (positive and negative), and health-related quality of life.
Main findings
Overall, all articles found a positive association between PA and better outcomes of mental health (e. g., depression, anxiety, well-being). Physical activity was explanatory variable for mental health [ 25 ]. Physical activity was positive associated with mental health [ 42 , 49 ]. Articles that observed a decrease in PA during the stay-at-home order also observed a decrease in well-being [ 47 , 56 ], negative changes in depressive symptoms [ 57 ], and negative changes in anxiety and stress symptoms [ 45 ]. This relationship seems to be bidirectional, since participants who decrease in mental health had greater reduction in physical activity [ 37 ]. Inactive people had worse well-being, highest depression and enxiety compared with moderately active and very active participants [ 24 , 51 ]. Also, inactive old adults had more depressive symptoms [ 26 ]. On the other hand, participants sufficiently active reported significantly lower depression and anxiety and higher life satisfaction. Moreover, it was found that exercise intensity seems to be important. Two studies founded that depression was significantly negatively correlated with moderate-intensity PA but not vigorous and walking/light exeeercuse [ 36 , 40 ]. Another one found that vigorous PA better predicted depressive symptoms than moderate PA [ 27 ]. Three studies suggested that the threshold of PA should be done to fells the benefits on mental health [ 28 , 39 , 50 ]. At least 4 h of MVPA reduced by 49% odds of depressive symptoms [ 28 ], and at leas 477 METs-min/week was associated with a 33% decrease in the probability of depressive symptoms [ 39 ]. On the other hand, a non-significant association was found between PA and anxiety [ 35 ], and between PA and health-related quality of life [ 46 ]. One study found that the decrease in mental wellbeing and increase in perceived stress was not related to changes in PA [ 44 ].
The association between physical activity and mental health among children and adolescents
The details of the association between PA and mental health among children and adolescents are shown in Table 2 , four studies were included [ 52 , 53 , 54 , 55 ].
The number of participants ranged between 64 and 4898 children and adolescents. More girls than boys participated in the studies. The mean ages were 11, 14, 15, and 16 years old. One study was longitudinal and presents two moments of assessment, also opting for phone or video calls to collect the data [ 52 ]. The other three studies were cross-sectional, and collected data by online surveys.
One study was from the USA [ 52 ], one from Greece [ 54 ] and the other two were from China [ 53 , 55 ].
Three studies assessed PA by the International physical activity questionnaire (IPAQ) questionnaire [ 53 , 54 , 55 ], and another one used a 24-h physical activity recall [ 52 ]. Regarding mental health, different outcomes were assessed, such as anxiety, positive and negative affect, insomnia, depressive symptoms, psychological well-being and mood states.
Moderate physical activity was associated with less state anxiety [ 52 , 53 ]. Positive affect was not related to physical activity [ 52 ]. Higher levels of physical activity were also significantly associated with lower levels of total mood disturbance [ 55 ]. Regarding the dose of physical activity, days of physical activity per week was stronger predictor of well-being than minutes of physical activity per week [ 54 ].
This systematic review focuses on the association between PA and mental health during the first year of the COVID-19 pandemic. In particular, we sought to answer if PA mitigates the effects of the stay-at-home order on mental health. The COVID-19 pandemic generated numerous challenges for public health, particularly the significant burden of mental health in the population [ 58 , 59 ]. In addition, PA has been recognized as an effective mitigation strategy for improving mental health [ 60 ]. The COVID-19 pandemic has been affecting all continents in the world, at different scales. This study analysed 31 research articles, 27 about adults and old adults and 4 about children and adolescents. The articles are mainly based on cross-sectional studies and five are longitudinal studies. In nearly all of the studies comprised in the present systematic review, investigators used online surveys as the main procedure to collect data. Overall, the studies suggested that higher PA is associated with less negative mental health symptoms, such as depression, anxiety, well-being, and fear, independently of age.
The studies observed that women showed more depressive symptoms than men [ 28 , 39 , 50 , 53 , 55 ], and this trend increases with age [ 24 ] Furthermore, individuals with a lower level of masculinity traits (not specifically females) increased risk of developing depression [ 36 ], and women experienced more generalised anxiety [ 41 ]. The reduction of PA levels may mostly influence the mental well-being of females [ 38 , 49 ]. Those findings are expected since the literature is consistent in signalising sex differences in most mental disorders [ 61 ]. On the whole, the prevalence rates of anxiety and depression were both higher than the rates found in previous studies before the COVID-19 pandemic [ 36 , 37 , 43 , 45 , 48 , 57 ], which highlights a worsening in mental health during the first year of the COVID-19 pandemic. Regarding age, younger individuals experienced significantly higher anxiety and depression, also income influenced mental health, lower-income participants present worse mental health [ 37 ].
Five articles conducted a longitudinal study. Among those studies, four enrolled adults and old adults [ 28 , 44 , 46 , 50 , 51 ] and in one the sample comprised children [ 52 ]. Among the studies that have collected measures before and after the stay-at-home order, both observed a significant reduction in PA [ 44 , 46 ]. Two study collected measures after the stay-at-home order and during this period physical activity mean score decreased minimally [ 51 ], and depressive symptoms increase as the weeks of isolation go [ 28 ]. Other studies also reported a reduction in self-reported PA [ 26 , 33 , 34 , 37 , 38 , 42 , 43 , 45 , 56 , 57 ] and increase in sedentary behaviour [ 25 , 26 , 34 ]. Individuals who reported larger decrease in MVPA pre to during COVID-19 reported relatively poorer mental health [ 33 ]. Participants whose mental health got “worse” or “much worse” had greater reductions in physical activity [ 37 ]. Also, increased levels of physical activity were associated with stronger effects on wellbeing [ 42 ]. The reduction was more pronounced in men than women [ 32 , 38 , 44 ], in vigorous PA [ 38 ], and between those with lower health-related quality of life scores before the COVID-19 pandemic [ 46 ]. The possible explanation for this sex-difference is that men are more engaged in group/community PA and sports in clubs or gyms, and those were more impacted by the COVID-19 restrictions. Also, women are more engaged in low and moderate physical activities, which can be done at home. Besides, women spent more time in housework activities. Women without changes in childcare provision reported more opportunities to be physically active [ 41 ]. The same sex-differences were observed in an Italian study [ 62 ]. Increases in PA were observed for a minority, but the majority of the respective study samples demonstrating a positive change were individuals who did not meet recommended PA guidelines before the COVID-19 pandemic [ 32 , 38 ]. Additional reasons could be an increase in awareness for health issues and more time to pursue PA during the stay-at-home order [ 32 ]. These behaviour changes can help to maintain a more active lifestyle during the pandemic. Another study found an increase of 40% in PA in a sample that was already active before the COVID-19 pandemic [ 35 ]. PA could be used as a coping strategy to deal with the consequences of the pandemic. The place where individuals prefer to practice PA seems to be important, since active participants reported greater connectedness to nature and nature relatedness than the inactive population [ 35 ].
There was no consensus across studies for the optimal PA levels for mitigating negative mental symptoms. The more the physical activity is frequent and vigorous, the best people feel themselves [ 24 ]. Among Chinese students, 2500 METs minute/week of PA every week was the optimal dose to alleviate negative emotion [ 50 ]. On the other hand, a Spanish community sample study showed that 477 METs-minute/week was associated with a 33% decrease in the probabilities of notable depressive symptoms [ 39 ]. The difference between the values must be relativised considering the samples’ characteristics. The first one concerns students with a mean age of 20 years [ 50 ], and the second one concerns a community sample with a mean age of 43.2 years for women and 40.5 years for men [ 39 ]. In addition, it is claimed that at least 3000 METs-minute/week reduce the odds of depressive symptoms by 47% [ 39 ]. These studies used the IPAQ to assess PA, and according to IPAQ, to reach a minimally active category at least 600 METs minute/week is needed [ 63 ]. The American College of Sports Medicine also recommends for healthy adults aged 18–65 years at least 600 METs minute/week but did not specify the minimum dose to prevent depressive symptoms [ 14 , 64 ].
Studies also examined the association between PA and mental health according to PA intensity. Moderate-intensity PA (e.g., walking or jogging on a treadmill, using an elliptical trainer, cleaning house) is associated with better mental health outcomes than vigorous-intensity PA [ 36 , 40 ], and light-intensity PA [ 40 ]. On the other hand, vigorous-intensity PA better predicted depressive symptoms than moderate-intensity PA; also the effect size was higher for the association between vigorous-intensity PA and level of resilience compared with moderate-intensity PA [ 27 ]. One study found that performing high PA levels has no positive effect on depressive symptoms [ 39 ]. Another study explored the type of PA and showed that stretching and resistance training were associated with lower anxiety, and three types of PA (household chores, stretching, and resistance training) were associated with lower depression symptoms [ 48 ].
One study explored the association of specific types of physical exercise and mental health, and founded that home-based group entertainment exercise, rope skipping and badminton, Chinese traditional sports, video dancing and sensory-motor games present a greater reduction in mental health than others types [ 40 ].
Sedentary behaviour was observed in few studies and contradictory findings were observed. No association between sedentary time and depressive symptoms was observed [ 26 , 36 ]. However, other studies have shown that sedentary behaviour was associated with poorer mental health [ 25 ], well-being [ 32 ] and perceived stress [ 44 ].
Concerning the association between PA and mental health outcomes among children and adolescents, only four articles were selected. Some issues must be highlighted. This population had to face, beyond the reality that changed from the COVID-19 pandemic, the changes in the education system such as online learning became the main learning method for students and uncertainty of academic development, which probably caused more anxiety level [ 52 , 53 ]. Both moderate and highly active groups were significantly associated with less depressive symptoms [ 53 ] and anxiety [ 52 , 53 ], and only the most active adolescents reported significantly lower insomnia symptoms [ 53 ] and better mood states [ 55 ]. Days of physical activity per week was stronger predictor of well-being than minutes of physical activity per week [ 54 ].
Regarding old-age samples, the studies mentioned the particular vulnerability to changes in social circumstances, and highlight the importance of health-related quality of life [ 46 ] and levels of resilience [ 27 ] to deal with the consequences of the COVID-19 pandemic on the PA level. The stay-at-home order can cause greater distress and feelings of sadness, considered specific risk factor for depressive symptoms [ 34 ]. Mental health and physical activity decrease pre to during stay-at-home order [ 47 ]. In a group that were previously regular participants of a formal exercise program, MVPA was significantly higher within the non-depressed group compared with depressed group [ 26 ]. Being active previously of COVID-19 confinement did not prevent 30.4% of Brazilian older adults from having depressive symptoms, but these results is much lower than prevalence of depression in Brazilian general population, which is 68% [ 34 ].
The present systematic review had some limitations that must be mentioned. First, the studies present correlative analyses, not causal ones, thus randomised controlled trials must be conducted in the context of the COVID-19 pandemic and the stay-at-home order to clarify the direction of the association. However, beyond the COVID-19 context, randomised controlled trials showed that PA interventions show beneficial effects on mental health outcomes such as depression and anxiety [ 65 ]. Thus, a nuanced perspective particularly during the COVID-19 context in future research is needed. Moreover, the included studies with community samples were limited, and the analyses were mostly based on convenience samples with college students, which had specific characteristics and low mean age. Thus, future research needs to focus on representative study samples.
This review helps to clarify the positive association between PA and mental health during the first year of the COVID-19 pandemic, especially considering the effects of the stay-at-home order worldwide. Although there is an association between increased PA and improved mental health, further studies are needed, specifically randomised clinical trials, to identify the direction of this relationship, and what kind of PA, intensity, and frequency are most indicated to maximise the effects. Also, an investigation to examine the association during the second year of the COVID-19 pandemic is needed. The impact of the COVID-19 pandemic on mental health may be continuous and long-term [ 66 , 67 ]. Thus, public health agencies must provide timely and effective interventions, in which PA and exercise should be a priority.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
Coronavirus disease-19
Severe acute respiratory syndrome coronavirus-2
Physical activity
World Health Organization
International physical activity questionnaire
Metabolic equivalent
Conti P, Caraffa A, Gallenga CE, Kritas SK, Frydas I, Younes A, et al. The British variant of the new coronavirus-19 (Sars-Cov-2) should not create a vaccine problem. J Biol Regul Homeost Agents. 2020;35(1).
Ritchie H, Ortiz-Ospina E.; Beltekian D., Mathieu E., Hasell J., Macdonald B., Giattino C. and Roser M. Coronavirus (COVID-19) Vaccinations 2021 Available from: https://ourworldindata.org/covid-vaccinations .
Google Scholar
Organization WH. Coronavirus disease (COVID-19): Vaccines 2021 [Available from: https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccines?adgroupsurvey={adgroupsurvey}&gclid=CjwKCAiA1eKBBhBZEiwAX3gqlwcwqCmOIN-6welx1Msuxpy-YUyvsWAV-BYZOJ1g1qS0oUYbLEPiZxoC9uQQAvD_BwE .
Our World in Data. Coronavirus (COVID-19) Vaccinations. 2021.
Organization WH. WHO Coronavirus Disease (COVID-19) Dashboard 2021 [Available from: https://covid19.who.int/?gclid=CjwKCAiAmrOBBhA0EiwArn3mfDVdryFCBj-_lYP99HuMas-LYQzoVDYdfWMBkTmfFA8QVtmS0ncCTRoCiFIQAvD_BwE .
WHO. Weekly epidemiological update on COVID-19 16 November 2021. 2021.
European Centre for Disease Prevention and Control. Data on country response measures to COVID-19 2021 [Available from: https://www.ecdc.europa.eu/en/publications-data/download-data-response-measures-covid-19 .
Moreland A, Herlihy C, Tynan MA, Sunshine G, McCord RF, Hilton C, et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement—United States, march 1–may 31, 2020. Morb Mortal Wkly Rep. 2020;69(35):1198.
Article CAS Google Scholar
Valentin F, Sylvain I, Oulmann Z, Rachel FR, Joël B, Pierre-Michel L, et al. COVID-19 pandemic lockdown and problematic eating behaviors in a student population. J Behav Addict. 2020;9(3):826–35.
Article Google Scholar
Chodkiewicz J, Talarowska M, Miniszewska J, Nawrocka N, Bilinski P. Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int J Environ Res Public Health. 2020;17(13):4677.
Article CAS PubMed Central Google Scholar
Wei Y, Shah R. Substance use disorder in the COVID-19 pandemic: a systematic review of vulnerabilities and complications. Pharmaceuticals. 2020;13(7):155.
Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. 2020;16(1):57.
Chen Q, Li M, Wang Y, Zhang L, Tan X. Changes in anxiety, depression, and stress in one week and one month later after the Wuhan shutdown against the COVID-19 epidemic. Disast Med Public Health Prepared. 2021;1-8.
Teychenne M, White RL, Richards J, Schuch FB, Rosenbaum S, Bennie JA. Do we need physical activity guidelines for mental health: what does the evidence tell us? Ment Health Phys Act. 2020;18:100315.
Marques A, Peralta M, Martins J, Catunda R, Matos MG, Saboga NL. Associations between physical activity and self-rated wellbeing in European adults: a population-based, cross-sectional study. Prev Med. 2016;91:18–23.
Article PubMed Google Scholar
WHO. Physical Inactivity: a global public health problem 2021 [Available from: https://www.who.int/ncds/prevention/physical-activity/inactivity-global-health-problem/en/ .
Marques A, Henriques-Neto D, Peralta M, Martins J, Demetriou Y, Schönbach DMI, et al. Prevalence of physical activity among adolescents from 105 low, middle, and high-income countries. Int J Environ Res Public Health. 2020;17(9).
Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health. 2018;6(10):e1077–e86.
Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. 2021;7(1):e000960.
Violant-Holz V, Gallego-Jiménez MG, González-González CS, Muñoz-Violant S, Rodríguez MJ, Sansano-Nadal O, et al. Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2020;17(24):9419.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm [cited 2021 Dec 28].
Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, et al. Panethnic differences in blood pressure in Europe: a systematic review and Meta-analysis. PLoS One. 2016;11(1):e0147601.
Article PubMed PubMed Central Google Scholar
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Abate Daga F, Agostino S, Peretti S, Beratto L. The impact of physical activity rate on subjective well-being among North-Western Italian population during COVID-19 nationwide lockdown. J Sports Med Phys Fitness. 2021.
Bird JM, Karageorghis CI, Hamer M. Relationships among behavioural regulations, physical activity, and mental health pre- and during COVID-19 UK lockdown. Psychol Sport Exerc. 2021;55:101945.
Carvalho J, Borges-Machado F, Pizarro AN, Bohn L, Barros D. Home confinement in previously active older adults: a cross-sectional analysis of physical fitness and physical activity behavior and their relationship with depressive symptoms. Front Psychol. 2021;12:643832.
Carriedo A, Cecchini JA, Fernandez-Rio J, Méndez-Giménez A. COVID-19, psychological well-being and physical activity levels in older adults during the Nationwide lockdown in Spain. Am J Geriatr Psychiatry. 2020;28(11):1146–55.
Cecchini JA, Carriedo A, Fernández-Río J, Méndez-Giménez A, González C, Sánchez-Martínez B, et al. A longitudinal study on depressive symptoms and physical activity during the Spanish lockdown. Int J Clin Health Psychol. 2021;21(1):100200.
Chouchou F, Augustini M, Caderby T, Caron N, Turpin NA, Dalleau G. The importance of sleep and physical activity on well-being during COVID-19 lockdown: Reunion island as a case study. Sleep Med. 2021;77:297–301.
Coughenour C, Gakh M, Pharr JR, Bungum T, Jalene S. Changes in depression and physical activity among college students on a diverse campus after a COVID-19 stay-at-home order. J Community Health. 2021;46(4):758–66.
Eric NO, Oghenebrorien AE, Onogimesike AT, Suoke OP. Mental wellbeing and exercise participation during covid-19 pandemic among adult residents of Nigeria's Niger delta. Int J Hum Move Sports Sci. 2020;8(6):534–42.
Faulkner J, O'Brien WJ, McGrane B, Wadsworth D, Batten J, Askew CD, et al. Physical activity, mental health and well-being of adults during initial COVID-19 containment strategies: a multi-country cross-sectional analysis. J Sci Med Sport. 2020;24(4):320–6.
Gierc M, Riazi NA, Fagan MJ, Di Sebastiano KM, Kandola M, Priebe CS, et al. Strange days: adult physical activity and mental health in the first two months of the COVID-19 pandemic. Front Public Health. 2021;9:567552.
Lage A, Carrapatoso S, de Queiroz S, Neto E, Gomes S, Soares-Miranda L, et al. Associations between depressive symptoms and physical activity intensity in an older adult population during COVID-19 lockdown. Front Psychol. 2021;12:644106.
Lesser IA, Nienhuis CP. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int J Environ Res Public Health. 2020;17(11):3899.
Lin J, Guo T, Becker B, Yu Q, Chen ST, Brendon S, et al. Depression is associated with moderate-intensity physical activity among college students during the COVID-19 pandemic: differs by activity level, gender and gender role. Psychol Res Behav Manag. 2020;13:1123–34.
Marashi MY, Nicholson E, Ogrodnik M, Fenesi B, Heisz JJ. A mental health paradox: mental health was both a motivator and barrier to physical activity during the COVID-19 pandemic. PLoS One. 2021;16(4):e0239244.
Article CAS PubMed PubMed Central Google Scholar
Maugeri G, Castrogiovanni P, Battaglia G, Pippi R, D'Agata V, Palma A, et al. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon. 2020;6(6):e04315.
Méndez-Giménez A, Cecchini JA, Fernández-Río J, Carriedo A. Physical activity and prevention of depressive symptoms in the Spanish population during confinement due to COVID-19. Psicothema. 2021;33(1):111–7.
PubMed Google Scholar
Nie YJ, Ma YY, Wu YK, Li JH, Liu T, Zhang C, et al. Association between physical exercise and mental health during the COVID-19 outbreak in China: a Nationwide cross-sectional study. Front Psychiatry. 2021;12:722448.
Nienhuis CP, Lesser IA. The Impact of COVID-19 on Women's Physical Activity Behavior and Mental Well-Being. Int J Environ Res Public Health. 2020;17(23):9036.
O'Brien L, Forster J. Physical activity supporting connection to nature, and helping to maintain wellbeing during the Covid-19 restrictions in England. Int J Environ Res Public Health. 2021;18(9):4585.
Ozdemir F, Cansel N, Kizilay F, Guldogan E, Ucuz I, Sinanoglu B, et al. The role of physical activity on mental health and quality of life during COVID-19 outbreak: a cross-sectional study. Eur J Integrat Med. 2020;40:101248.
Savage MJ, James R, Magistro D, Donaldson J, Healy LC, Nevill M, et al. Mental health and movement behaviour during the COVID-19 pandemic in UK university students: prospective cohort study. Ment Health Phys Act. 2020;19.
Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int J Environ Res Public Health. 2020;17(11):4065.
Suzuki Y, Maeda N, Hirado D, Shirakawa T, Urabe Y. Physical Activity Changes and Its Risk Factors among Community-Dwelling Japanese Older Adults during the COVID-19 Epidemic: Associations with Subjective Well-Being and Health-Related Quality of Life. Int J Environ Res Public Health. 2020;17(18):6591.
Trabelsi K, Ammar A, Masmoudi L, Boukhris O, Chtourou H, Bouaziz B, et al. Sleep quality and physical activity as predictors of mental wellbeing variance in older adults during COVID-19 lockdown: ECLB COVID-19 international online survey. Int J Environ Res Public Health. 2021;18(8):4329.
Xiang MQ, Tan XM, Sun J, Yang HY, Zhao XP, Liu L, et al. Relationship of physical activity with anxiety and depression symptoms in Chinese college students during the COVID-19 outbreak. Front Psychol. 2020;11:582436.
Zalewska A, Gałczyk M, Sobolewski M, Białokoz-Kalinowska I. Depression as compared to level of physical activity and internet addiction among polish physiotherapy students during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(19):10072.
Zhang Y, Zhang H, Ma X, Di Q. Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int J Environ Res Public Health. 2020;17(10):3722.
Young DR, Hong BD, Lo T, Inzhakova G, Cohen DA, Sidell MA. The longitudinal associations of physical activity, time spent outdoors in nature and symptoms of depression and anxiety during COVID-19 quarantine and social distancing in the United States. Prev Med. 2021;154:106863.
Alves JM, Yunker AG, DeFendis A, Xiang AH, Page KA. Associations between affect, physical activity, and anxiety among US children during COVID-19. medRxiv. 2020.
Chi X, Liang K, Chen ST, Huang Q, Huang L, Yu Q, et al. Mental health problems among Chinese adolescents during the COVID-19: the importance of nutrition and physical activity. Int J Clin Health Psychol. 2020;21:100218.
Morres ID, Galanis E, Hatzigeorgiadis A, Androutsos O, Theodorakis Y. Physical activity, sedentariness, eating behaviour and well-being during a COVID-19 lockdown period in Greek adolescents. Nutrients. 2021;13(5):1449.
Kang S, Sun Y, Zhang X, Sun F, Wang B, Zhu W. Is physical activity associated with mental health among Chinese adolescents during isolation in COVID-19 pandemic? J Epidemiol Global Health. 2020;11(1):26–33.
Chouchou F, Augustini M, Caderby T, Caron N, Turpin NA, Dalleau G. The importance of sleep and physical activity on well-being during COVID-19 lockdown: Reunion island as a case study. Sleep Med. 2020:297–301.
Coughenour C, Gakh M, Pharr JR, Bungum T, Jalene S. Changes in depression and physical activity among college students on a diverse campus after a COVID-19 stay-at-home order. J Community Health. 2020:758–66.
Lima CKT, Carvalho PMM, Lima I, Nunes J, Saraiva JS, de Souza RI, et al. The emotional impact of coronavirus 2019-nCoV (new coronavirus disease). Psychiatry Res. 2020;287:112915.
Hahad O, Gilan DA, Daiber A, Münzel T. Public mental health as one of the key factors in dealing with COVID-19. Gesundheitswesen. 2020;82(5):389–91.
PubMed PubMed Central Google Scholar
Jakobsson J, Malm C, Furberg M, Ekelund U, Svensson M. Physical activity during the coronavirus (COVID-19) pandemic: prevention of a decline in metabolic and immunological functions. Front Sports Active Living. 2020;2:57.
Riecher-Rössler A. Sex and gender differences in mental disorders. Lancet Psychiatry. 2017;4(1):8–9.
Giustino V, Parroco AM, Gennaro A, Musumeci G, Palma A, Battaglia G. Physical activity levels and related energy expenditure during COVID-19 quarantine among the Sicilian active population: a cross-sectional online survey study. Sustainability. 2020;12(11):4356.
Committee IR. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ)-short and long forms. http://www.ipaq.ki.se/scoring.pdf . 2005.
Thompson PD, Arena R, Riebe D, Pescatello LS. ACSM’s new preparticipation health screening recommendations from ACSM’s guidelines for exercise testing and prescription. Curr Sports Med Rep. 2013;12(4):215–7.
Neill RD, Lloyd K, Best P, Tully MA. The effects of interventions with physical activity components on adolescent mental health: systematic review and meta-analysis. Ment Health Phys Act. 2020;19:100359.
Gan Y, Ma J, Wu J, Chen Y, Zhu H, Hall BJ. Immediate and delayed psychological effects of province-wide lockdown and personal quarantine during the COVID-19 outbreak in China. Psychol Med. 2020:1–12.
Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113(10):707–12.
Article CAS PubMed Google Scholar
Download references
Acknowledgements
AI acknowledges support from the Swiss National Centre of Competence in Research LIVES – Overcoming vulnerability: life course perspectives, granted by the Swiss National Science Foundation (grant number: 51NF40-185901). AI acknowledges support from the Swiss National Science Foundation (grant number: 10001C_189407). André Werneck is supported by the São Paulo Research Foundation (FAPESP) with a PhD scholarship (FAPESP process: 2019/24124-7). This paper presents independent research. The views expressed in this publication are those of the authors and not necessarily those of the acknowledged institutions.
No funding.
Author information
Authors and affiliations.
KinesioLab, Research Unit in Human Movement Analysis, Insituto Piaget, Almada, Portugal
Priscila Marconcin
CIPER, Faculdade de Motricidade Humana, Universidade de Lisboa, Lisbon, Portugal
Priscila Marconcin, Miguel Peralta & Adilson Marques
Center for Epidemiological Research in Nutrition and Health, Department of Nutrition, School of Public Health, São Paulo, Brazil
André O. Werneck & Adilson Marques
ISAMB, Universidade de Lisboa, Lisbon, Portugal
Miguel Peralta
Center for the Interdisciplinary Study of Gerontology and Vulnerability, University of Geneva, Geneva, Switzerland
Andreas Ihle
Swiss National Centre of Competence in Research LIVES – Overcoming vulnerability: Life course perspectives, Lausanne and Geneva, Switzerland
Department of Psychology, University of Geneva, Geneva, Switzerland
Universidade da Madeira, Funchal, Portugal
Élvio R. Gouveia
Interactive Technologies Institute, LARSyS, Funchal, Portugal
Laboratorio de Rendimiento Humano, Grupo de Estudio en Educación, Actividad Física y Salud (GEEAFyS), Universidad Católica del Maule, Talca, Chile
Gerson Ferrari
University of Coimbra, Research Unit for Sport and Physical Activity (CIDAF). Faculty of Sport Sciences and Physical Education, Coimbra, Portugal
Hugo Sarmento
You can also search for this author in PubMed Google Scholar
Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. PM, MP and AM had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. PM, MP and AM, study conception and design. PM and MP acquisition of data. PM, MP and AM, analysis and interpretation of data.
Corresponding author
Correspondence to Priscila Marconcin .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Marconcin, P., Werneck, A.O., Peralta, M. et al. The association between physical activity and mental health during the first year of the COVID-19 pandemic: a systematic review. BMC Public Health 22 , 209 (2022). https://doi.org/10.1186/s12889-022-12590-6
Download citation
Received : 28 October 2021
Accepted : 17 January 2022
Published : 01 February 2022
DOI : https://doi.org/10.1186/s12889-022-12590-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health

BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Research Review: Childhood chronic physical illness and adult emotional health - a systematic review and meta-analysis
Affiliations.
- 1 EDGE Lab, School of Psychology, University of Sussex, Brighton, UK.
- 2 Department of Psychology, Indiana University-Purdue University Indianapolis, Indianapolis, IN, USA.
- 3 MRC Unit for Lifelong Health & Ageing at UCL, London, UK.
- PMID: 28449285
- DOI: 10.1111/jcpp.12727
Background: Childhood chronic physical illness is associated with a greater vulnerability for emotional problems (i.e. depression and anxiety) in childhood. However, little is known about life-long effects of childhood chronic physical illness on mental health. The present study aims to systematically review evidence for associations between eight chronic physical illnesses with childhood onset (arthritis, asthma, cancer, chronic renal failure, congenital heart disease, cystic fibrosis, type 1 diabetes, and epilepsy) and adult emotional problems.
Methods: A database search of MEDLINE, PsycARTICLES, PsycINFO, and ScienceDirect was undertaken, and random effects meta-analyses were used to synthesise evidence from eligible studies.
Results: In total, 37 studies were eligible for the systematic review (n = 45,733) and of these, 34 studies were included in the meta-analyses (n = 45,358). There were overall associations between childhood chronic physical illness and adult depression (OR = 1.31; 95% CI [1.12, 1.54]) and anxiety (OR = 1.47; 95% CI [1.13, 1.92]). Separate meta-analyses for childhood asthma, type 1 diabetes and cancer were also conducted, with cancer being significantly associated with adult depression (OR = 1.19; 95% CI [1.00, 1.42]).
Conclusions: The effects of childhood chronic physical illness on the risk of emotional problems persist beyond childhood and adolescence. Mental health prevention and intervention strategies targeting children with chronic physical illnesses can have long-term benefits.
Keywords: Depression; anxiety; chronic disorders; meta-analysis; paediatrics.
© 2017 Association for Child and Adolescent Mental Health.
PubMed Disclaimer
Similar articles
- The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Bedaso A, Adams J, Peng W, Sibbritt D. Bedaso A, et al. Reprod Health. 2021 Jul 28;18(1):162. doi: 10.1186/s12978-021-01209-5. Reprod Health. 2021. PMID: 34321040 Free PMC article. Review.
- Association Between Maternal Perinatal Depression and Anxiety and Child and Adolescent Development: A Meta-analysis. Rogers A, Obst S, Teague SJ, Rossen L, Spry EA, Macdonald JA, Sunderland M, Olsson CA, Youssef G, Hutchinson D. Rogers A, et al. JAMA Pediatr. 2020 Nov 1;174(11):1082-1092. doi: 10.1001/jamapediatrics.2020.2910. JAMA Pediatr. 2020. PMID: 32926075 Free PMC article.
- The relationship between childhood trauma and the severity of adulthood depression and anxiety symptoms in a clinical sample: The mediating role of cognitive emotion regulation strategies. Huh HJ, Kim KH, Lee HK, Chae JH. Huh HJ, et al. J Affect Disord. 2017 Apr 15;213:44-50. doi: 10.1016/j.jad.2017.02.009. Epub 2017 Feb 7. J Affect Disord. 2017. PMID: 28189964
- Childhood maltreatment: A predictor of mental health problems among adolescents and young adults. Badr HE, Naser J, Al-Zaabi A, Al-Saeedi A, Al-Munefi K, Al-Houli S, Al-Rashidi D. Badr HE, et al. Child Abuse Negl. 2018 Jun;80:161-171. doi: 10.1016/j.chiabu.2018.03.011. Epub 2018 Apr 5. Child Abuse Negl. 2018. PMID: 29609135
- Exploring the relationship between cognitive illness representations and poor emotional health and their combined association with diabetes self-care. A systematic review with meta-analysis. Hudson JL, Bundy C, Coventry PA, Dickens C. Hudson JL, et al. J Psychosom Res. 2014 Apr;76(4):265-74. doi: 10.1016/j.jpsychores.2014.02.004. Epub 2014 Feb 21. J Psychosom Res. 2014. PMID: 24630175 Review.
- Testing a model of benefit-finding and growth in youths with chronic health conditions. von Rezori RE, Baumeister H, Holl RW, Minden K, Müller-Stierlin AS, Reinauer C, Temming S, Warschburger P. von Rezori RE, et al. BMC Pediatr. 2024 Jan 5;24(1):19. doi: 10.1186/s12887-023-04467-3. BMC Pediatr. 2024. PMID: 38183031 Free PMC article.
- Establishing an International Interdisciplinary Research Network in Craniofacial Microsomia: The CARE Program. Stock NM, Crerand CE, Johns AL, McKinney CM, Koudstaal MJ, Drake AF, Heike CL. Stock NM, et al. Cleft Palate Craniofac J. 2024 Sep;61(9):1470-1479. doi: 10.1177/10556656231176904. Epub 2023 May 29. Cleft Palate Craniofac J. 2024. PMID: 37248561
- Risk of Psychiatric Disorders in Juvenile Idiopathic Arthritis: Population- and Sibling-Controlled Cohort and Cross-Sectional Analyses. Delcoigne B, Horne A, Reutfors J, Askling J. Delcoigne B, et al. ACR Open Rheumatol. 2023 May;5(5):277-284. doi: 10.1002/acr2.11549. Epub 2023 May 12. ACR Open Rheumatol. 2023. PMID: 37170883 Free PMC article.
- "They go hand in hand": a patient-oriented, qualitative descriptive study on the interconnectedness between chronic health and mental health conditions in transition-age youth. Allemang B, Samuel S, Pintson K, Patton M, Greer K, Farias M, Schofield K, Sitter KC, Patten SB, Mackie AS, Dimitropoulos G. Allemang B, et al. BMC Health Serv Res. 2023 Jan 2;23(1):2. doi: 10.1186/s12913-022-09002-1. BMC Health Serv Res. 2023. PMID: 36593502 Free PMC article.
- Health-Related Quality of Life and mental health of families with children and adolescents affected by rare diseases and high disease burden: the perspective of affected children and their siblings. Wiegand-Grefe S, Liedtke A, Morgenstern L, Hoff A, Csengoe-Norris A, Johannsen J, Denecke J, Barkmann C, Grolle B, Daubmann A, Wegscheider K, Boettcher J. Wiegand-Grefe S, et al. BMC Pediatr. 2022 Oct 14;22(1):596. doi: 10.1186/s12887-022-03663-x. BMC Pediatr. 2022. PMID: 36229869 Free PMC article.
Publication types
- Search in MeSH
Grants and funding
- MC_UU_12019/3/MRC_/Medical Research Council/United Kingdom
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
Other Literature Sources
- scite Smart Citations
- MedlinePlus Consumer Health Information
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Become a member
Psychological Health, Well-Being, and the Mind-Heart-Body Connection: A Scientific Statement From the American Heart Association
Information & authors, metrics & citations, view options, methodology, negative psychological health and cvd, chronic stress and social stressors, anger and hostility, summary of findings: negative psychological health and cvd.
| Negative psychological factors | Parameter/end point | Effect estimates (95% CI) |
|---|---|---|
| Depression | Incident MI | RR, 1.30 (1.22–1.40) |
| Incident CHD | RR, 1.30 (1.18–1.44) | |
| Stroke | RR, 1.45 (1.31–1.61) | |
| Obesity | RR, 1.37 (1.17–1.48) | |
| Hypertension | RR, 1.42 (1.09–1.86) | |
| Diabetes | RR, 1.32 (1.18–1.47) | |
| Anxiety | CVD mortality | RR, 1.41 (1.13–1.76) |
| Incident CHD | RR, 1.41 (1.23–1.61) | |
| Coronary artery spasm | RR, 5.20 (4.72–5.40) | |
| Incident stroke | RR, 1.71 (1.18–2.50) | |
| Heart failure | RR, 1.35 (1.11–1.64) | |
| Work-related stress | Incident CVD events | RR, 1.4 (1.2–1.8) |
| Any-cause stress | Incident CHD/CHD mortality | RR, 1.27 (1.12–1.45) |
| PTSD | Incident CHD | RR, 1.61 (1.46–1.77) |
| Social isolation and loneliness | Incident CVD events | RR, 1.5 (1.2–1.9) |
| Pessimism | CHD mortality | OR, 2.17 (1.21–3.89) (highest vs lowest quartile) |
| Anger and hostility | Incident CHD | HR, 1.19 (1.05–1.35) |
| Recurrent CHD | HR, 1.24 (1.08–1.42) |
Positive Psychological Health and CVD
Sense of purpose, happiness and positive affect, mindfulness, other positive factors, summary of findings: positive psychological factors and cardiovascular health.
| Positive psychological factors | Parameter/end point | Effect estimates (95% CI) |
|---|---|---|
| Optimism | Incident CVD | RR, 0.65 (0.51–0.78) |
| Hospital readmission after ACS | HR, 0.92 (0.86–0.98) | |
| All-cause mortality | RR, 0.86 (0.80–0.92) | |
| Sense of purpose | CVD risk | RR, 0.83 (0.75–0.92) |
| All-cause mortality | RR, 0.83 (0.75–0.91) | |
| Happiness/more positive affect | Incident CHD | HR, 0.78 (0.63–0.96) |
| Mindfulness | Good cardiovascular health | PR, 1.83 (1.07–3.13) |
| Nonsmoking | PR, 1.37 (1.06–1.76) | |
| Body mass index <25 kg/m | PR, 2.17 (1.16–4.07) | |
| Fasting glucose <100 mg/dL | PR, 1.47 (1.06–2.04) | |
| High level of physical activity | PR, 1.56 (1.04–2.35) | |
| Higher emotional vitality | Incident CHD | RR, 0.81 (0.69–0.94) |
| Psychological well-being | Cardiovascular mortality | OR, 0.71 (0.59–0.84) |
Pathways Linking Psychological Health and CVD
Biological processes, behavioral and psychosocial processes, summary of findings.

Interventions for Psychiatric Disorders or Symptoms
Antidepressants, psychotherapy, care management, interventions to promote positive psychological health, psychotherapy and stress management programs, positive psychology programs, meditation training and mindfulness-based interventions, implications for clinical practice.
| Over the past 2 wk, how often have you been bothered by any of the following problems? | Not at all | Several days | More than half the days | Nearly every day |
|---|---|---|---|---|
| Little interest or pleasure in doing things | 0 | 1 | 2 | 3 |
| Feeling down, depressed, or hopeless | 0 | 1 | 2 | 3 |
| Well-being parameter | Question |
|---|---|
| Health-related optimism | “How do you think things will go with your health moving forward?” |
| Positive affect | “How often do you experience pleasure or happiness in your life?” |
| Gratitude | “Do you ever feel grateful about your health? Do you ever feel grateful about other things in your life?” |
| Sample statements to address depression “It seems like feeling down or even a little hopeless might be affecting the way you are taking care of yourself. Let’s think about how we can tackle this problem together.” |
| Sample statements to address anxiety “It seems like your level of anxiety and worry is really wearing on you, and that can really affect your health and the way you take care of yourself. Let’s think about how we can tackle this problem together.” |
| Sample statements to support optimism “I have taken care of many patients with this kind of heart problem before, and many of them have done very well. I think you can, too.” |
| Sample statements to support positive affect “There is a lot of research finding connections between feeling happy and satisfied with your life and your heart health. I want to really support you in taking time for yourself and engaging in _________ [fill in as appropriate such as “hobbies” or “meaningful activities”]. Let’s think together about that.” |
| Sample statements to support gratitude “We were lucky to catch your heart problem when we did, and there are some good treatments. I think that means that we have a lot to be grateful for here, and there is a good chance that your health can remain strong if we work together.” |
Future Research
Conclusions.
| Writing group member | Employment | Research grant | Other research support | Speakers’ bureau/honoraria | Expert witness | Ownership interest | Consultant/advisory board | Other |
|---|---|---|---|---|---|---|---|---|
| Glenn N. Levine | Baylor College of Medicine | None | None | None | None | None | None | None |
| Beth E. Cohen | University of California, San Francisco | None | None | None | None | None | None | None |
| Yvonne Commodore-Mensah | Johns Hopkins University School of Public Health and Nursing | None | None | None | None | None | None | None |
| Julie Fleury | Arizona State University | None | None | None | None | None | None | None |
| Jeff C. Huffman | Massachusetts General Hospital | NIH (well-being research in cardiac patients) | None | None | None | None | None | None |
| Umair Khalid | Baylor College of Medicine | None | None | None | None | None | None | None |
| Laura D. Kubzansky | Harvard T.H. Chan School of Public Health, Social and Behavioral Sciences | NIH (principal investigator, optimism and exceptional longevity) | Lee Kum Sheung Center for Health and Happiness (codirector) | None | None | None | None | None |
| Darwin R. Labarthe | Northwestern University | None | None | None | None | None | None | None |
| Helen Lavretsky | Semel Institute for Neuroscience and Human Behavior | None | None | None | None | None | None | None |
| Erin D. Michos | Johns Hopkins University School of Medicine, Johns Hopkins Hospital | None | None | None | None | None | None | None |
| Erica S. Spatz | Yale University School of Medicine, Yale-New Haven Hospital | None | None | None | None | None | None | Medtronic Vascular, Inc |
| Reviewer | Employment | Research grant | Other research support | Speakers’ bureau/honoraria | Expert witness | Ownership interest | Consultant/advisory board | Other |
|---|---|---|---|---|---|---|---|---|
| Julia K. Boehm | Chapman University | AHA (grant 18AIREA33960394 that investigates how childhood psychosocial resources, including well-being, are related to cardiometabolic risk in adulthood) | None | None | None | None | None | None |
| Robert M. Carney | Washington University | NIH (RO1s) | None | None | None | Pfizer, Inc | None | None |
| Sidney C. Smith Jr | University of North Carolina | None | None | None | None | None | None | None |
Supplemental Material
Eletters (0).
eLetters should relate to an article recently published in the journal and are not a forum for providing unpublished data. Comments are reviewed for appropriate use of tone and language. Comments are not peer-reviewed. Acceptable comments are posted to the journal website only. Comments are not published in an issue and are not indexed in PubMed. Comments should be no longer than 500 words and will only be posted online. References are limited to 10. Authors of the article cited in the comment will be invited to reply, as appropriate.
Comments and feedback on AHA/ASA Scientific Statements and Guidelines should be directed to the AHA/ASA Manuscript Oversight Committee via its Correspondence page.
Information
Published in.

Permissions
- AHA Scientific Statements
- Statements and Guidelines
Affiliations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Select your manager software from the list below and click Download.
- Pawel Borkowski,
- Natalia Borkowska,
- Anna A. Kuzyukova,
- Irina A. Belyaeva,
- Yana G. Pekhova,
- Olga V. Yurova,
- Anatoliy D. Fesyun,
- Filippo Luca Gurgoglione,
- Luigi Vignali,
- Rocco Antonio Montone,
- Riccardo Rinaldi,
- Giorgio Benatti,
- Emilia Solinas,
- Antonio Maria Leone,
- Domenico Galante,
- Gianluca Campo,
- Simone Biscaglia,
- Italo Porto,
- Stefano Benenati,
- Giampaolo Niccoli,
- Elena Bandieri,
- Eleonora Borelli,
- Sarah Bigi,
- Claudia Mucciarini,
- Fabio Gilioli,
- Umberto Ferrari,
- Sonia Eliardo,
- Mario Luppi,
- Leonardo Potenza,
- Zsofia Ocsovszky,
- Blanka Ehrenberger,
- Blanka Berenyi,
- Alexandra Assabiny,
- Jozsef Otohal,
- Tamas Martos,
- Orsolya Papp-Zipernovszky,
- Fanni Hegedus,
- Bela Merkely,
- Marta Csabai,
- Zsolt Bagyura,
- Alisa Auer,
- Norbert K. Semmer,
- Roland von Känel,
- Livia Thomas,
- Claudia Zuccarella-Hackl,
- Roland Wiest,
- Petra H. Wirtz,
- Francesco Bottaccioli,
- Anna Giulia Bottaccioli,
- Huijing Zou,
- Sek Ying Chair,
- Bilong Feng,
- Yu Jia Liu,
- Yu Xin Cheng,
- Xiao Qin Wang,
- Leiqing Huang,
- Yunyan Xianyu,
- Bing Xiang Yang,
- Łukasz Pietrzykowski,
- Agata Kosobucka-Ozdoba,
- Piotr Michalski,
- Michał Kasprzak,
- Jakub Ratajczak,
- Alicja Rzepka-Cholasińska,
- Joanna Siódmiak,
- Klaudyna Grzelakowska,
- Aldona Kubica,
- Jacob P. DeBlois,
- Andrew S. London,
- Kevin S. Heffernan,
View options
Pdf and all supplements, login options.
Check if you have access through your login credentials or your institution to get full access on this article.
Purchase Options
Purchase this article to access the full text.
Purchase access to this journal for 24 hours
Restore your content access
Enter your email address to restore your content access:
Note: This functionality works only for purchases done as a guest. If you already have an account, log in to access the content to which you are entitled.
Share article link
Copying failed.
Submit a Response to This Article
Compose eletter, contributors, statement of competing interests, previous article, next article, comment response.
The Science of Mindfulness: Research and Benefits
- First Online: 25 September 2024
Cite this chapter

- Rajat Chand 3 &
- Greg Sazima 4
This chapter delves into the scientific underpinnings of mindfulness, showcasing its transformative effects on mental and physical health through neural mechanisms and empirical research. It explores how mindfulness practices influence key brain networks, including the Default Mode, Salience, and Central Executive Networks, promoting neural coherence and enhancing attentional control. The chapter highlights mindfulness’s ability to modulate the limbic system, fostering improved emotional regulation and reducing stress responses. Additionally, it outlines the positive impacts of mindfulness on attention, demonstrating increased cognitive flexibility and reduced distractibility. The clinical benefits of mindfulness are emphasized, with evidence supporting its efficacy in managing pain, anxiety, and stress-related hormonal responses. By integrating mindfulness into healthcare, individuals can cultivate resilience, empathy, and a more compassionate approach to both self-care and patient care, leading to improved overall well-being and quality of life.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Goleman D, Davidson RJ. Altered traits: science reveals how meditation changes your mind, brain, and body. New York, NY: Avery; 2017.
Google Scholar
Michael Sayers W, et al. The emerging neurobiology of mindfulness and emotion processing. Springer EBooks; 2015. p. 9–22. https://doi.org/10.1007/978-1-4939-2263-5_2 . Accessed 3 Jan 2024
Book Google Scholar
Sharma H. Meditation: process and effects. Ayu. 2015;36(3):233–7. https://doi.org/10.4103/0974-8520.182756 .
Article PubMed PubMed Central Google Scholar
Wynne A. The origin of Buddhist meditation; 2007. https://doi.org/10.4324/9780203963005 .
Kabat-Zinn J. Mindfulness-based stress reduction (MBSR). Construct Hum Sci. 2003;8(2):73–107.
Tang Y-Y, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015;16(4):213–25. https://doi.org/10.1038/nrn3916 .
Article PubMed Google Scholar
Brandmeyer T, Delorme A, Wahbeh H. The neuroscience of meditation: classification, phenomenology, correlates, and mechanisms. In: Progress in brain research. Elsevier; 2019. p. 1–29. https://doi.org/10.1016/bs.pbr.2018.10.020 .
Chapter Google Scholar
Changde D, Li J, Huang L, He H. Brain encoding and decoding in fMRI with bidirectional deep generative models. Engineering. 2019;5(5):948–53.
Article Google Scholar
Weder BJ. Mindfulness in the focus of the neurosciences—the contribution of neuroimaging to the understanding of mindfulness. Front Behav Neurosci. 2022;16:928522. https://doi.org/10.3389/fnbeh.2022.928522 .
Farb NA, Anderson AK, Segal ZV. The mindful brain and emotion regulation in mood disorders. Can J Psychiatr. 2012;57(2):70–7. https://doi.org/10.1177/070674371205700203 . PMID: 22340146; PMCID: PMC3303604
Kral TRA, Schuyler BS, Mumford JA, Rosenkranz MA, Lutz A, Davidson RJ. Impact of short- and long-term mindfulness meditation training on amygdala reactivity to emotional stimuli. Neuroimage. 2018;181:301–13. https://doi.org/10.1016/j.neuroimage.2018.07.013 . Epub 2018 Jul 7. PMID: 29990584; PMCID: PMC6671286
Rathore M, Verma M, Nirwan M, Trivedi S, Pai V. Functional connectivity of prefrontal cortex in various meditation techniques—a mini-review. Int J Yoga. 2022;15(3):187–94. https://doi.org/10.4103/ijoy.ijoy_88_22 . Epub 2023 Jan 16. PMID: 36949839; PMCID: PMC10026337
Siew S, Yu J. Mindfulness-based randomized controlled trials led to brain structural changes: an anatomical likelihood meta-analysis. Sci Rep. 2023;13:18469. https://doi.org/10.1038/s41598-023-45765-1 .
Lazar SW, Kerr CE, Wasserman RH, Gray JR, Greve DN, Treadway MT, McGarvey M, Quinn BT, Dusek JA, Benson H, Rauch SL, Moore CI, Fischl B. Meditation experience is associated with increased cortical thickness. Neuroreport. 2005;16(17):1893–7. https://doi.org/10.1097/01.wnr.0000186598.66243.19 . PMID: 16272874; PMCID: PMC1361002
Hölzel BK, Carmody J, Vangel M, Congleton C, Yerramsetti SM, Gard T, Lazar SW. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. 2011;191(1):36–43. https://doi.org/10.1016/j.pscychresns.2010.08.006 . Epub 2010 Nov 10. PMID: 21071182; PMCID: PMC3004979
Taren AA, Gianaros PJ, Greco CM, Lindsay EK, Fairgrieve A, Brown KW, Rosen RK, Ferris JL, Julson E, Marsland AL, Bursley JK, Ramsburg J, Creswell JD. Mindfulness meditation training alters stress-related amygdala resting state functional connectivity: a randomized controlled trial. Soc Cogn Affect Neurosci. 2015;10(12):1758–68. https://doi.org/10.1093/scan/nsv066 . Epub 2015 Jun 5. PMID: 26048176; PMCID: PMC4666115
Tang Y-Y, Lu Q, Feng H, Tang R, Posner MI. Short-term meditation increases blood flow in anterior cingulate cortex and insula. Front Psychol. 2015;6:212. https://doi.org/10.3389/fpsyg.2015.00212 .
Haase L, Thom NJ, Shukla A, Davenport PW, Simmons AN, Stanley EA, Paulus MP, Johnson DC. Mindfulness-based training attenuates insula response to an aversive interoceptive challenge. Soc Cogn Affect Neurosci. 2016;11(1):182–90. https://doi.org/10.1093/scan/nsu042 . Epub 2014 Apr 8. PMID: 24714209; PMCID: PMC4692309
Zeidan F, Grant JA, Brown CA, McHaffie JG, Coghill RC. Mindfulness meditation-related pain relief: evidence for unique brain mechanisms in the regulation of pain. Neurosci Lett. 2012;520(2):165–73. https://doi.org/10.1016/j.neulet.2012.03.082 . Epub 2012 Apr 6. PMID: 22487846; PMCID: PMC3580050
Roxo MR, Franceschini PR, Zubaran C, Kleber FD, Sander JW. The limbic system conception and its historical evolution. ScientificWorldJournal. 2011;11:2428–41. https://doi.org/10.1100/2011/157150 . Epub 2011 Dec 8. PMID: 22194673; PMCID: PMC3236374
Buckner RL. The brain’s default network: origins and implications for the study of psychosis. Dialogues Clin Neurosci. 2013;15(3):351–8. https://doi.org/10.31887/DCNS.2013.15.3/rbuckner . PMID: 24174906; PMCID: PMC3811106
Carroll J. Imagination, the Brain’s default mode network, and imaginative verbal artifacts. In: Carroll J, Clasen M, Jonsson E, editors. Evolutionary perspectives on imaginative culture. Cham: Springer; 2020. https://doi.org/10.1007/978-3-030-46190-4 .
Schimmelpfennig J, Topczewski J, Zajkowski W, Jankowiak-Siuda K. The role of the salience network in cognitive and affective deficits. Front Hum Neurosci. 2023;17:1133367. https://doi.org/10.3389/fnhum.2023.1133367 . PMID: 37020493; PMCID: PMC10067884
Na H, et al. The modulation of salience and central executive networks by acute stress in healthy males: an EEG microstates study. Int J Psychophysiol. 2021;169:63–70. ISSN 0167-8760. https://doi.org/10.1016/j.ijpsycho.2021.09.001 .
Bremer B, et al. Mindfulness meditation increases default mode, salience, and central executive network connectivity. Sci Rep. 2022;12(1):13219. https://doi.org/10.1038/s41598-022-17325-6 . PMID: 35918449; PMCID: PMC9346127
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15(10):483–506. https://doi.org/10.1016/j.tics.2011.08.003 . Epub 2011 Sep 9
Anselm D, Hölzel Britta K, Boucard Christine C, Wohlschläger Afra M, Christian S. Mindfulness is associated with intrinsic functional connectivity between default mode and salience networks. Front Hum Neurosci. 2015;9:461. https://doi.org/10.3389/fnhum.2015.00461 .
Raffone A, Marzetti L, Del Gratta C, Perrucci MG, Romani GL, Pizzella V. Toward a brain theory of meditation. Prog Brain Res. 2019;244:207–32. https://doi.org/10.1016/bs.pbr.2018.10.028 . Epub 2019 Jan 3
Lin Y, Gloe LM, Louis CC, Eckerle WD, Fisher ME, Moser JS. An electrophysiological investigation on the emotion regulatory mechanisms of brief open monitoring meditation in novice non-meditators. Sci Rep. 2020;10(1):14252. https://doi.org/10.1038/s41598-020-71122-7 . PMID: 32860004; PMCID: PMC7455688
McGilchrist I. The master and his emissary. Yale University Press; 2009. ISBN 978-0-300-14878-7 .
Austin JH. Zen and the brain: toward an understanding of meditation and consciousness. Boston, MA: MIT Press; 1998. ISBN 0-262-51109-6
Austin JH. Meditating selflessly : practical neural zen. Boston, MA: MIT Press; 2013. ISBN 978-0-262-01587-5
Jha AP, Stanley EA, Kiyonaga A, Wong L, Gelfand L. Examining the protective effects of mindfulness training on working memory capacity and affective experience. Emotion. 2010;10(1):54–64. https://doi.org/10.1037/a0018438 .
Kozasa EH, et al. Meditation training increases brain efficiency in an attention task. NeuroImage. 2012;59(1):745–9. www.sciencedirect.com/science/article/pii/S1053811911007531 . https://doi.org/10.1016/j.neuroimage.2011.06.088 .
Chiesa A, Calati R, Serretti A. Does mindfulness training improve cognitive abilities? A systematic review of neuropsychological findings. Clin Psychol Rev. 2011;31(3):449–64. https://doi.org/10.1016/j.cpr.2010.11.003 .
Malinowski P. Neural mechanisms of attentional control in mindfulness meditation. Front Neurosci. 2013;7:8. https://doi.org/10.3389/fnins.2013.00008 .
Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends Cogn Sci. 2008;12(4):163–9. https://doi.org/10.1016/j.tics.2008.01.005 .
van den Hurk PAM, Giommi F, Gielen SC, Speckens AEM, Barendregt HP. Greater efficiency in attentional processing related to mindfulness meditation. Q J Exp Psychol. 2010;63(6):1168–80. https://doi.org/10.1080/17470210903249365 .
Turakitwanakan W, Mekseepralard C, Busarakumtragul P. Effects of mindfulness meditation on serum cortisol of medical students. J Med Assoc Thail. 2013;96(Suppl 1):S90–5.
Jung Y-H, et al. The effects of mind–body training on stress reduction, positive affect, and plasma catecholamines. Neurosci Lett. 2010;479(2):138–42. https://doi.org/10.1016/j.neulet.2010.05.048 .
Sanada K, et al. Effects of mindfulness-based interventions on biomarkers in healthy and cancer populations: a systematic review. BMC Complement Altern Med. 2017;17(1):125. https://doi.org/10.1186/s12906-017-1638-y .
Walsh E, et al. Brief mindfulness training reduces salivary IL-6 and TNF-α in young women with depressive symptomatology. J Consult Clin Psychol. 2016;84(10):887–97. https://doi.org/10.1037/ccp0000122 .
Bellosta-Batalla M, et al. Brief mindfulness session improves mood and increases salivary oxytocin in psychology students. Stress Health. 2020;36(4):469–77. https://doi.org/10.1002/smi.2942 .
Jørgensen MA, et al. Effect of mindfulness-based stress reduction on dehydroepiandrosterone-sulfate in adults with self-reported stress. A randomized trial. Clin Transl Sci. 2021;14(6):2360–9. https://doi.org/10.1111/cts.13100 . Accessed 22 Sept. 2021
Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. Delta Trade Paperbacks; 1991. ISBN 0-385-30312-2.
Sipe WEB, Eisendrath SJ. Mindfulness-based cognitive therapy: theory and practice. Can J Psychiatry. 2012;57(2):63–9. https://doi.org/10.1177/070674371205700202 . ISSN 1497-0015 . PMID 22340145 . S2CID 63436 61
Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, Berger Z, Sleicher D, Maron DD, Shihab HM, Ranasinghe PD, Linn S, Saha S, Bass EB, Haythornthwaite JA. Meditation programs for psychological stress and Well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357–68. https://doi.org/10.1001/jamainternmed.2013.13018 . PMID: 24395196; PMCID: PMC4142584
Khoury B, Sharma M, Rush SE, Fournier C. Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J Psychosom Res. 2015;78(6):519–28. https://doi.org/10.1016/j.jpsychores.2015.03.009 . Epub 2015 Mar 20
Hofmann SG, et al. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. 2010;78(2):169–83., www.ncbi.nlm.nih.gov/pmc/articles/PMC2848393/ . https://doi.org/10.1037/a0018555 .
Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 2008;31:23–33.
Gotink RA, et al. 8-week mindfulness based stress reduction induces brain changes similar to traditional long-term meditation practice—a systematic review. Brain Cogn. 2016;108:32–41., www.sciencedirect.com/science/article/abs/pii/S0278262616301312 . https://doi.org/10.1016/j.bandc.2016.07.001 .
Marchand WR. Neural mechanisms of mindfulness and meditation: evidence from neuroimaging studies. World J Radiol. 2014;6(7):471. www.ncbi.nlm.nih.gov/pmc/articles/PMC4109098/ . https://doi.org/10.4329/wjr.v6.i7.471 .
Kuyken W, et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. Lancet. 2015;386(9988):63–73., www.thelancet.com/journals/lancet/article/PIIS0140-6736(14)62222-4/fulltext . https://doi.org/10.1016/s0140-6736(14)62222-4 .
Gotink RA, et al. Standardised mindfulness-based interventions in healthcare: an overview of systematic reviews and meta-analyses of RCTs. PLoS One. 2015;10(4):e0124344., www.ncbi.nlm.nih.gov/pmc/articles/PMC4400080/ . https://doi.org/10.1371/journal.pone.0124344 .
Nakata H, et al. Meditation reduces pain-related neural activity in the anterior cingulate cortex, insula, secondary somatosensory cortex, and thalamus. Front Psychol. 2014;5:117291. https://doi.org/10.3389/fpsyg.2014.01489 .
Lindsay EK, David Creswell J. Mechanisms of mindfulness training: monitor and acceptance theory (MAT). Clin Psychol Rev. 2017;51:48–59. https://doi.org/10.1016/j.cpr.2016.10.011 .
Rahl HA, et al. Brief mindfulness meditation training reduces mind wandering: the critical role of acceptance. Emotion. 2017;17(2):224–30. www.ncbi.nlm.nih.gov/pmc/articles/PMC5329004/ . https://doi.org/10.1037/emo0000250 .
Langen WH, Smith SL. A systematic review of mindfulness practices for improving outcomes in chronic low Back pain. Int J Yoga. 2020;13(3):177. https://doi.org/10.4103/ijoy.ijoy_4_20 .
Pérez-Aranda A, et al. A randomized controlled efficacy trial of mindfulness-based stress reduction compared with an active control group and usual care for fibromyalgia: the EUDAIMON study. Pain. 2019;160(11):2508–23. pubmed.ncbi.nlm.nih.gov/31356450 /. https://doi.org/10.1097/j.pain.0000000000001655 .
Anheyer D, et al. Mindfulness-based stress reduction for treating low back pain. Ann Intern Med. 2017;166(11):799. https://doi.org/10.7326/m16-1997 .
Zeidan F, et al. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci. 2011;31(14):5540–8. www.ncbi.nlm.nih.gov/pmc/articles/PMC3090218/ . https://doi.org/10.1523/jneurosci.5791-10.2011 .
Pei J-H, et al. Mindfulness-based cognitive therapy for treating chronic pain: a systematic review and meta-analysis. Psychol Health Med. 2020;26(3):333–46. https://doi.org/10.1080/13548506.2020.1849746 .
Zeidan F, et al. Mindfulness-meditation-based pain relief is not mediated by endogenous opioids. J Neurosci. 2016;36(11):3391–7. https://doi.org/10.1523/jneurosci.4328-15.2016 .
Download references
Author information
Authors and affiliations.
Diagnostic and Interventional Radiology, Austin Radiological Association, Austin, TX, USA
Rajat Chand
Senior Behavioral Faculty, Stanford-O’Connor Family Medicine Residency Program, San Jose, CA, USA
Greg Sazima
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Chand, R., Sazima, G. (2024). The Science of Mindfulness: Research and Benefits. In: Mindfulness in Medicine. Springer, Cham. https://doi.org/10.1007/978-3-031-66166-2_3
Download citation
DOI : https://doi.org/10.1007/978-3-031-66166-2_3
Published : 25 September 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-66165-5
Online ISBN : 978-3-031-66166-2
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Frontiers in Sports and Active Living
- Physical Education and Pedagogy
- Research Topics
Building Health Through Physical Activity in Schools - Volume II
Total Downloads
Total Views and Downloads
About this Research Topic
This is the second volume of the Research Topic "Building" Health Through Physical Activity in Schools, please see the first volume here . Physical activity in the school context refers to the various ways in which students engage in physical activity during the school day. This can include physical education classes, recess and lunch breaks, and extracurricular sports and activities. The importance of physical activity in schools can be seen in the numerous benefits it can provide for students' physical and mental health, academic performance, and overall well-being. Physical education classes are a key component of physical activity in schools, providing students with structured physical activity opportunities and helping them to develop the knowledge and skills needed to be physically active throughout their lives. Additionally, recess and lunch breaks can provide students with the opportunity to engage in unstructured physical activity, allowing them to socialize with their peers and blow off steam. Extracurricular sports and activities can also provide students with opportunities to be physically active, while also helping them to develop important social and teamwork skills. Research has shown that students who are physically active tend to have better academic performance, are less likely to experience obesity and related health issues and have better mental health. However, despite the many benefits of physical activity, many students do not engage in enough physical activity. Factors such as a lack of access to physical activity opportunities, limited time for recess and physical education, and a focus on academics over physical activity can all contribute to this problem. In order to promote physical activity among students, it is important for schools to provide a variety of opportunities for physical activity, and to make physical activity an integral part of the school day. Therefore, high quality articles of different types (e.g., original research, clinical trials, systematic reviews) are strongly recommended. Potential topics include, but are not limited to: • The impact of physical activity programs on the academic performance of school-aged children • Examine the effectiveness of school interventions to increase physical activity levels in children • The relationship between physical activity levels and mental health in school-aged children • Examine the influence of school policies and facilities on physical activity levels in children • The role of physical education in promoting lifelong physical activity habits in children • Investigate the impact of technology use on physical activity levels in school-aged children • Examine the effectiveness of community-based approaches to increasing physical activity levels among school-aged children • The impact of socioeconomic status on physical activity levels among school-aged children • The relationship between physical activity levels and body weight in school-aged children • Investigate the impact of school physical activity programs on reducing childhood obesity
Keywords : physical education, healthy behaviors, pedagogy, active methodologies, motivation
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, submission deadlines.
| Manuscript Summary | |
| Manuscript |
Participating Journals
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
Physical health and well-being: Experiences and perspectives of young adult mental health consumers
- February 2016
- International Journal of Mental Health Nursing 25(4)

- The University of Sydney

- Australian Catholic University
- This person is not on ResearchGate, or hasn't claimed this research yet.
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Jonah Kynan Murray

- Graeme Browne

- Talia Wigod

- Alec L. Miller

- Zhenhua Han

- Int J Ment Health Nurs

- Christina Aggar
- Kerith Duncanson

- Issues Ment Health Nurs

- Nikka Marabong

- Helen Lester
- David Shiers
- Patrick D. McGorry
- Rosemary Purcell

- PSYCHIAT SERV
- Liam Stanbury
- Vicky Cheeseman

- John W. Creswell
- Vicki L. Plano Clark

- Vladimir Olshanskiy

- S.M. Grundy
- World Health Organization
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
The impact of stress on body function: A review
Habib yaribeygi.
1 Neurosciences Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran
Yunes Panahi
2 Clinical Pharmacy Department, Faculty of Pharmacy, Baqiyatallah University of Medical Sciences, Tehran, Iran
Hedayat Sahraei
Thomas p. johnston.
3 Division of Pharmaceutical Sciences, School of Pharmacy, University of Missouri-Kansas City, Kansas City, Missouri, USA
Amirhossein Sahebkar
4 Biotechnology Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
Any intrinsic or extrinsic stimulus that evokes a biological response is known as stress. The compensatory responses to these stresses are known as stress responses. Based on the type, timing and severity of the applied stimulus, stress can exert various actions on the body ranging from alterations in homeostasis to life-threatening effects and death. In many cases, the pathophysiological complications of disease arise from stress and the subjects exposed to stress, e.g. those that work or live in stressful environments, have a higher likelihood of many disorders. Stress can be either a triggering or aggravating factor for many diseases and pathological conditions. In this study, we have reviewed some of the major effects of stress on the primary physiological systems of humans.
Abbreviations
ACTH: Adrenocorticotropic hormone
CNS: Central nervous system
CRH: Corticotropin releasing hormone
GI: Gastrointestinal
LTP: Long-term potentiation
NMDA : N-methyl-D-aspartate
VTA: Ventral tegmental area
Stress and the Brain Function Complications
For a long time, researchers suggested that hormones have receptors just in the peripheral tissues and do not gain access to the central nervous system (CNS) (Lupien and Lepage, 2001[ 63 ]). However, observations have demonstrated the effect of anti-inflammatory drugs (which are considered synthetic hormones) on behavioral and cognitive disorders and the phenomenon called “Steroid psychosis” (Clark et al., 1952[ 16 ]). In the early sixties, neuropeptides were recognized as compounds devoid of effects on the peripheral endocrine system. However, it was determined that hormones are able to elicit biological effects on different parts of the CNS and play an important role in behavior and cognition (De Kloet, 2000[ 22 ]). In 1968, McEven suggested for the first time that the brain of rodents is capable of responding to glucocorticoid (as one of the operators in the stress cascade). This hypothesis that stress can cause functional changes in the CNS was then accepted (McEwen et al., 1968[ 74 ]). From that time on, two types of corticotropic receptors (glucocorticosteroids and mineralocorticoids) were recognized (de Kloet et al., 1999[ 23 ]). It was determined that the affinity of glucocorticosteroid receptors to cortisol and corticosterone was about one tenth of that of mineralocorticoids (de Kloet et al., 1999[ 23 ]). The hippocampus area has both types of receptors, while other points of the brain have only glucocorticosteroid receptors (de Kloet et al., 1999[ 23 ]).
The effects of stress on the nervous system have been investigated for 50 years (Thierry et al., 1968[ 115 ]). Some studies have shown that stress has many effects on the human nervous system and can cause structural changes in different parts of the brain (Lupien et al., 2009[ 65 ]). Chronic stress can lead to atrophy of the brain mass and decrease its weight (Sarahian et al., 2014[ 100 ]). These structural changes bring about differences in the response to stress, cognition and memory (Lupien et al., 2009[ 65 ]). Of course, the amount and intensity of the changes are different according to the stress level and the duration of stress (Lupien et al., 2009[ 65 ]). However, it is now obvious that stress can cause structural changes in the brain with long-term effects on the nervous system (Reznikov et al., 2007[ 89 ]). Thus, it is highly essential to investigate the effects of stress on different aspects of the nervous system (Table 1 (Tab. 1) ; References in Table 1: Lupien et al., 2001[ 63 ]; Woolley et al., 1990[ 122 ]; Sapolsky et al., 1990[ 99 ]; Gould et al., 1998[ 35 ]; Bremner, 1999[ 10 ]; Seeman et al., 1997[ 108 ]; Luine et al., 1994[ 62 ]; Li et al., 2008[ 60 ]; Scholey et al., 2014[ 101 ]; Borcel et al., 2008[ 9 ]; Lupien et al., 2002[ 66 ]).

Stress and Memory
Memory is one of the important functional aspects of the CNS and it is categorized as sensory, short term, and long-term. Short term memory is dependent on the function of the frontal and parietal lobes, while long-term memory depends on the function of large areas of the brain (Wood et al., 2000[ 121 ]). However, total function of memory and the conversion of short term memory to long-term memory are dependent on the hippocampus; an area of the brain that has the highest density of glucocorticosteroid receptors and also represents the highest level of response to stress (Scoville and Milner, 1957[ 107 ]; Asalgoo et al., 2015[ 1 ]). Therefore, during the past several decades, the relationship between the hippocampus and stress have been hotly debated (Asalgoo et al., 2015[ 1 ]; Lupien and Lepage, 2001[ 63 ]). In 1968, it was proven that there were cortisol receptors in the hippocampus of rats (McEwen et al., 1968[ 74 ]). Later, in 1982, by using specific agonists of glucocorticosteroid and mineralocorticoid receptors, the existence of these two receptors in the brain and hippocampus area of rats was proven (Veldhuis et al., 1982[ 119 ]). It should also be noted that the amygdala is very important to assessing the emotional experiences of memory (Roozendaal et al., 2009[ 91 ]).
The results of past studies have demonstrated the effect of stress on the process of memory (Ghodrat et al., 2014[ 32 ]). Various studies have shown that stress can cause functional and structural changes in the hippocampus section of the brain (McEwen, 1999[ 72 ]). These structural changes include atrophy and neurogenesis disorders (Lupien and Lepage, 2001[ 63 ]). Also, chronic stress and, consequently, an increase in plasma cortisol, leads to a reduction in the number of dendritic branches (Woolley et al., 1990[ 122 ]) and the number of neurons (Sapolsky et al., 1990[ 99 ]), as well as structural changes in synaptic terminals (Sapolsky et al., 1990[ 99 ]) and decreased neurogenesis in the hippocampus tissue (Gould et al., 1998[ 35 ]). Glucocorticosteroids can induce these changes by either effecting the cellular metabolism of neurons (Lawrence and Sapolsky, 1994[ 58 ]), or increasing the sensitivity of hippocampus cells to stimulatory amino acids (Sapolsky and Pulsinelli, 1985[ 98 ]) and/or increasing the level of extracellular glutamate (Sapolsky and Pulsinelli, 1985[ 98 ]).
High concentrations of stress hormones can cause declarative memory disorders (Lupien and Lepage, 2001[ 63 ]). Animal studies have shown that stress can cause a reversible reduction in spatial memory as a result of atrophy of the hippocampus (Luine et al., 1994[ 62 ]). In fact, high plasma concentrations of glucocorticosteroids for extended periods of time can cause atrophy of the hippocampus leading to memory disorders (Issa et al., 1990[ 45 ]). Additionally, people with either Cushing's syndrome (with an increased secretion of glucocorticosteroids), or people who receive high dosages of exogenous synthetic anti-inflammatory drugs, are observed to have atrophy of the hippocampus and associated memory disorders (Ling et al., 1981[ 61 ]). MRI images taken from the brains of people with post-traumatic stress disorder (PTSD) have demonstrated a reduction in the volume of the hippocampus along with neurophysiologic effects such as a weak verbal memory (Bremner, 1999[ 10 ]). Several human studies have suggested that even common therapeutic doses of glucocorticosteroids and dexamethasone can cause problems with explicit memory (Keenan et al., 1995[ 49 ]; Kirschbaum et al., 1996[ 53 ]). Thus, there is an inverse relationship between the level of cortisol and memory (Ling et al., 1981[ 61 ]), such that increasing levels of plasma cortisol following prolonged stress leads to a reduction in memory (Kirschbaum et al., 1996[ 53 ]), which improves when the level of plasma cortisol decreases (Seeman et al., 1997[ 108 ]).
Stress also has negative effects on learning. Results from hippocampus-dependent loading data demonstrate that subjects are not as familiar with a new environment after having been exposed to a new environment (Bremner, 1999[ 10 ]). Moreover, adrenal steroids lead to alteration in long-term potentiation (LTP), which is an important process in memory formation (Bliss and Lømo, 1973[ 7 ]).
Two factors are involved in the memory process during stress. The first is noradrenaline, which creates emotional aspects of memories in the basolateral amygdala area (Joëls et al., 2011[ 47 ]). Secondly, this process is facilitated by corticosteroids. However, if the release of corticosteroids occurs a few hours earlier, it causes inhibition of the amygdala and corresponding behaviors (Joëls et al., 2011[ 47 ]). Thus, there is a mutual balance between these two hormones for creating a response in the memory process (Joëls et al., 2011[ 47 ]).
Stress does not always affect memory. Sometimes, under special conditions, stress can actually improve memory (McEwen and Lupien, 2002[ 71 ]). These conditions include non-familiarity, non-predictability, and life-threatening aspects of imposed stimulation. Under these specific conditions, stress can temporarily improve the function of the brain and, therefore, memory. In fact, it has been suggested that stress can sharpen memory in some situations (Schwabe et al., 2010[ 105 ]). For example, it has been shown that having to take a written examination can improve memory for a short period of time in examination participants. Interestingly, this condition is associated with a decrease in the level of cortisol in the saliva (Vedhara et al., 2000[ 118 ]). Other studies have shown that impending stress before learning occurs can also lead to either an increase in the power of memory (Domes et al., 2002[ 27 ]; Schwabe et al., 2008[ 102 ]), or decrease in the capacity for memory (Diamond et al., 2006[ 26 ]; Kirschbaum et al., 1996[ 53 ]). This paradox results from the type of imposed stress and either the degree of emotional connection to the stressful event (Payne et al., 2007[ 83 ]; Diamond et al., 2007[ 25 ]), or the period of time between the imposing stress and the process of learning (Diamond et al., 2007[ 25 ]).
The process of strengthening memory is usually reinforced after stress (Schwabe et al., 2012[ 103 ]). Various studies on animal and human models have shown that administration of either glucocorticosteroids, or stress shortly after learning has occurred facilitates memory (Schwabe et al., 2012[ 103 ]). Also, it has been shown that glucocorticosteroids (not mineralocorticoids) are necessary to improve learning and memory (Lupien et al., 2002[ 66 ]). However, the retrieval of events in memory after exposure to stress will be decreased (Schwabe et al., 2012[ 103 ]), which may result from the competition of updated data for storage in memory in a stressful state (de Kloet et al., 1999[ 23 ]). Some investigations have shown that either exposure to stress, or injection of glucocorticosteroids before a test to assess retention, decreases the power of memory in humans and rodents (Schwabe and Wolf, 2009[ 104 ]).
In summary, it has been concluded that the effect of stress on memory is highly dependent on the time of exposure to the stressful stimulus and, in terms of the timing of the imposed stress, memory can be either better or worse (Schwabe et al., 2012[ 103 ]). Moreover, recent studies have shown that using a specific-timed schedule of exposure to stress not only affects hippocampus-dependent memory, but also striatum-dependent memory, which highlights the role of timing of the imposed stressful stimulus (Schwabe et al., 2010[ 105 ]).
Stress, Cognition and Learning
Cognition is another important feature of brain function. Cognition means reception and perception of perceived stimuli and its interpretation, which includes learning, decision making, attention, and judgment (Sandi, 2013[ 95 ]). Stress has many effects on cognition that depend on its intensity, duration, origin, and magnitude (Sandi, 2013[ 95 ]). Similar to memory, cognition is mainly formed in the hippocampus, amygdala, and temporal lobe (McEwen and Sapolsky, 1995[ 73 ]). The net effect of stress on cognition is a reduction in cognition and thus, it is said that any behavioral steps undertaken to reduce stress leads to increase in cognition (Scholey et al., 2014[ 101 ]). In fact, stress activates some physiological systems, such as the autonomic nervous system, central neurotransmitter and neuropeptide system, and the hypothalamus-pituitary-adrenal axis, which have direct effects on neural circuits in the brain involved with data processing (Sandi, 2013[ 95 ]). Activation of stress results in the production and release of glucocorticosteroids. Because of the lipophilic properties of glucocorticosteroids, they can diffuse through the blood-brain barrier and exert long-term effects on processing and cognition (Sandi, 2013[ 95 ]).
It appears that being exposed to stress can cause pathophysiologic changes in the brain, and these changes can be manifested as behavioral, cognitive, and mood disorders (Li et al., 2008[ 60 ]). In fact, studies have shown that chronic stress can cause complications such as increased IL-6 and plasma cortisol, but decreased amounts of cAMP responsive element binding protein and brain-derived neurotrophic factor (BDNF), which is very similar to what is observed in people with depression and mood disorders that exhibit a wide range of cognitive problems (Song et al., 2006[ 114 ]). Additionally, the increased concentrations of inflammatory factors, like interleukins and TNF-α (which play an important role in creating cognitive disorders), proves a physiologic relationship between stress and mood-based cognitive disorders (Solerte et al., 2000[ 113 ]; Marsland et al., 2006[ 68 ]; Li et al., 2008[ 60 ]). Studies on animals suggest that cognitive disorders resulting from stress are created due to neuroendocrine and neuroamine factors and neurodegenerative processes (Li et al., 2008[ 60 ]). However, it should be noted that depression may not always be due to the over activation of the physiological-based stress response (Osanloo et al., 2016[ 81 ]).
Cognitive disorders following exposure to stress have been reported in past studies (Lupien and McEwen, 1997[ 64 ]). Stress has effects on cognition both acutely (through catecholamines) and chronically (through glucocorticosteroids) (McEwen and Sapolsky, 1995[ 73 ]). Acute effects are mainly caused by beta-adrenergic effects, while chronic effects are induced in a long-term manner by changes in gene expression mediated by steroids (McEwen and Sapolsky, 1995[ 73 ]). In general, many mechanisms modulate the effects of stress on cognition (McEwen and Sapolsky, 1995[ 73 ]; Mendl, 1999[ 75 ]). For instance, adrenal steroids affect the function of the hippocampus during cognition and memory retrieval in a biphasic manner (McEwen and Sapolsky, 1995[ 73 ]). In chronic stress, these steroids can destroy neurons with other stimulatory neurotransmitters (Sandi, 2013[ 95 ]). Exposure to stress can also cause disorders in hippocampus-related cognition; specifically, spatial memory (Borcel et al., 2008[ 9 ]; Sandi et al., 2003[ 96 ]). Additionally, stress can halt or decrease the genesis of neurons in the dentate gyrus area of the hippocampus (this area is one of the limited brain areas in which neurogenesis occurs in adults) (Gould and Tanapat, 1999[ 34 ]; Köhler et al., 2010[ 54 ]). Although age is a factor known to affect cognition, studies on animals have demonstrated that young rats exposed to high doses of adrenal steroids show the same level of decline in their cognition as older adult animals with normal plasma concentrations of glucocorticoids (Landfield et al., 1978[ 57 ]). Also, a decrease in the secretion of glucocorticosteroids causes preservation of spatial memory in adults and has also been shown to have neuroprotective effects (Montaron et al., 2006[ 78 ]). Other studies have shown that stress (or the injection of adrenal steroids) results in varied effects on cognition. For instance, injection of hydrocortisone at the time of its maximum plasma concentration (in the afternoon) leads to a decrease in reaction time and improves cognition and memory (Lupien et al., 2002[ 66 ]).
In summary, the adverse effects of stress on cognition are diverse and depend on the type, timing, intensity, and duration (Sandi, 2013[ 95 ]). Generally, it is believed that mild stress facilitates an improvement in cognitive function, especially in the case of virtual or verbal memory. However, if the intensity of stress passes beyond a predetermined threshold (which is different in each individual), it causes cognitive disorders, especially in memory and judgment. The disruption to memory and judgment is due to the effects of stress on the hippocampus and prefrontal cortex (Sandi, 2013[ 95 ]). Of course, it must be realized that factors like age and gender may also play a role in some cognitive disorders (Sandi, 2013[ 95 ]). Importantly, it should be emphasized that different people may exhibit varied responses in cognition when exposed to the very same stressful stimulus (Hatef et al., 2015[ 39 ]).
Stress and Immune System Functions
The relationship between stress and the immune system has been considered for decades (Khansari et al., 1990[ 50 ]; Dantzer and Kelley, 1989[ 21 ]). The prevailing attitude between the association of stress and immune system response has been that people under stress are more likely to have an impaired immune system and, as a result, suffer from more frequent illness (Khansari et al., 1990[ 50 ]). Also, old anecdotes describing resistance of some people to severe disease using the power of the mind and their thought processes, has promoted this attitude (Khansari et al., 1990[ 50 ]). In about 200 AC, Aelius Galenus (Galen of Pergamon) declared that melancholic women (who have high levels of stress and, thus, impaired immune function) are more likely to have cancer than women who were more positive and exposed to less stress (Reiche et al., 2004[ 88 ]). This may be the first recorded case about the relationship between the immune system and stress. In an old study in the early 1920's, researchers found that the activity of phagocytes in tuberculosis decreased when emotional stress was induced. In fact, it was also suggested that living with stress increases the risk of tuberculosis by suppressing the immune system (Ishigami, 1919[ 44 ]). Following this study, other researchers suggested that the probability of disease appearance increases following a sudden, major, and extremely stressful life style change (Holmes and Rahe, 1967[ 41 ]; Calabrese et al., 1987[ 12 ]).
Over the past several decades, there have been many studies investigating the role of stress on immune system function (Dantzer and Kelley, 1989[ 21 ]; Segerstrom and Miller, 2004[ 109 ]). These studies have shown that stress mediators can pass through the blood-brain barrier and exert their effects on the immune system (Khansari et al., 1990[ 50 ]). Thus, the effect of stress on the immune system is now an accepted relationship or association.
Stress can affect the function of the immune system by modulating processes in the CNS and neuroendocrine system (Khansari et al., 1990[ 50 ]; Kiecolt-Glaser and Glaser, 1991[ 51 ]). Following stress, some neuroendocrine and neural responses result in the release of corticotropin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH), and other stress mediators (Carrasco and Van de Kar, 2003[ 13 ]). However, evidence suggests that the lymphatic system, which is a part of the immune system, also plays a role in releasing these mediators (Khansari et al., 1990[ 50 ]). For instance, thymus peptides, such as thymopentine, thymopoietin, and thymosin fraction-5, cause an increase in ACTH production (Goya et al., 1993[ 36 ]). Additionally, the existence of CRH in thymus has been proven (Redei, 1992[ 87 ]). It has also been proven that interleukin-1 released from phagocytes has a role in ACTH secretion (Berkenbosch et al., 1987[ 4 ]). On the other hand, natural or synthetic glucocorticosteroids (which are the final stress operators) are known as anti-inflammatory drugs and immune suppressants and their role in the inhibition of lymphocytes and macrophages has been demonstrated as well (Elenkov et al., 1999[ 28 ]; Reiche et al., 2004[ 88 ]). Moreover, their role in inhibiting the production of cytokines and other immune mediators and decreasing their effect on target cells during exposure to stress has also been determined (Reiche et al., 2004[ 88 ]).
In addition to adrenal steroids, other hormones are affected during stress. For example, the secretion of growth hormone will be halted during severe stress. A study showed that long-term administration of CRH into the brain ventricles leads to a cessation in the release of growth hormone (Rivier and Vale, 1985[ 90 ]). Stress also causes the release of opioid peptides to be changed during the time period over which the person is exposed to stress (McCarthy et al., 2001[ 70 ]). In fact, stress modifies the secretion of hormones that play a critical role in the function of the immune system (Khansari et al., 1990[ 50 ]). To date, it has been shown that various receptors for a variety of hormones involved in immune system function are adversely affected by stress. For example, ACTH, vasoactive intestinal peptide (VIP), substance P, growth hormone, prolactin, and steroids all have receptors in various tissues of the immune system and can modulate its function (De la Fuente et al., 1996[ 24 ]; Gala, 1991[ 30 ]; Mantyh, 1991[ 67 ]). In addition, active immune cells are also able to secrete several hormones; thus, some researchers believe that these hormones, as mediators of immune system, play a significant role in balancing its function (Blalock et al., 1985[ 6 ]).
Severe stress can lead to malignancy by suppressing the immune system (Reiche et al., 2004[ 88 ]). In fact, stress can decrease the activity of cytotoxic T lymphocytes and natural killer cells and lead to growth of malignant cells, genetic instability, and tumor expansion (Reiche et al., 2004[ 88 ]). Studies have shown that the plasma concentration of norepinephrine, which increases after the induction stress, has an inverse relationship with the immune function of phagocytes and lymphocytes (Reiche et al., 2004[ 88 ]). Lastly, catecholamines and opioids that are released following stress have immune-suppressing properties (Reiche et al., 2004[ 88 ]).
Stress and the Function of the Cardiovascular System
The existence of a positive association between stress and cardiovascular disease has been verified (Rozanski et al., 1999[ 93 ]). Stress, whether acute or chronic, has a deleterious effect on the function of the cardiovascular system (Rozanski et al., 1999[ 93 ]; Kario et al., 2003[ 48 ]; Herd, 1991[ 40 ]). The effects of stress on the cardiovascular system are not only stimulatory, but also inhibitory in nature (Engler and Engler, 1995[ 29 ]). It can be postulated that stress causes autonomic nervous system activation and indirectly affects the function of the cardiovascular system (Lazarus et al., 1963[ 59 ]; Vrijkotte et al., 2000[ 120 ]). If these effects occur upon activation of the sympathetic nervous system, then it mainly results in an increase in heart rate, strength of contraction, vasodilation in the arteries of skeletal muscles, a narrowing of the veins, contraction of the arteries in the spleen and kidneys, and decreased sodium excretion by the kidneys (Herd, 1991[ 40 ]). Sometimes, stress activates the parasympathetic nervous system (Pagani et al., 1991[ 82 ]). Specifically, if it leads to stimulation of the limbic system, it results in a decrease, or even a total stopping of the heart-beat, decreased contractility, reduction in the guidance of impulses by the heart stimulus-transmission network, peripheral vasodilatation, and a decline in blood pressure (Cohen et al., 2000[ 17 ]). Finally, stress can modulate vascular endothelial cell function and increase the risk of thrombosis and ischemia, as well as increase platelet aggregation (Rozanski et al., 1999[ 93 ]).
The initial effect of stress on heart function is usually on the heart rate (Vrijkotte et al., 2000[ 120 ]). Depending upon the direction of the shift in the sympatho-vagal response, the heart beat will either increase or decrease (Hall et al., 2004[ 38 ]). The next significant effect of stress on cardiovascular function is blood pressure (Laitinen et al., 1999[ 56 ]). Stress can stimulate the autonomic sympathetic nervous system to increase vasoconstriction, which can mediate an increase in blood pressure, an increase in blood lipids, disorders in blood clotting, vascular changes, atherogenesis; all, of which, can cause cardiac arrhythmias and subsequent myocardial infarction (Rozanski et al., 1999[ 93 ]; Vrijkotte et al., 2000[ 120 ]; Sgoifo et al., 1998[ 111 ]). These effects from stress are observed clinically with atherosclerosis and leads to an increase in coronary vasoconstriction (Rozanski et al., 1999[ 93 ]). Of course, there are individual differences in terms of the level of autonomic-based responses due to stress, which depends on the personal characteristics of a given individual (Rozanski et al., 1999[ 93 ]). Thus, training programs for stress management are aimed at reducing the consequences of stress and death resulting from heart disease (Engler and Engler, 1995[ 29 ]). In addition, there are gender-dependent differences in the cardiovascular response to stress and, accordingly, it has been estimated that women begin to exhibit heart disease ten years later that men, which has been attributed to the protective effects of the estrogen hormone (Rozanski et al., 1999[ 93 ]).
Studies have shown that psychological stress can cause alpha-adrenergic stimulation and, consequently, increase heart rate and oxygen demand (Rozanski et al., 1998[ 92 ], 1999[ 93 ]; Jiang et al., 1996[ 46 ]). As a result, coronary vasoconstriction is enhanced, which may increase the risk of myocardial infarction (Yeung et al., 1991[ 124 ]; Boltwood et al., 1993[ 8 ]; Dakak et al., 1995[ 20 ]). Several studies have demonstrated that psychological stress decreases the microcirculation in the coronary arteries by an endothelium-dependent mechanism and increases the risk of myocardial infarction (Dakak et al., 1995[ 20 ]). On the other hand, mental stress indirectly leads to potential engagement in risky behaviors for the heart, such as smoking, and directly leads to stimulation of the neuroendocrine system as part of the autonomic nervous system (Hornstein, 2004[ 43 ]). It has been suggested that severe mental stress can result in sudden death (Pignalberi et al., 2002[ 84 ]). Generally, stress-mediated risky behaviors that impact cardiovascular health can be summarized into five categories: an increase in the stimulation of the sympathetic nervous system, initiation and progression of myocardial ischemia, development of cardiac arrhythmias, stimulation of platelet aggregation, and endothelial dysfunction (Wu, 2001[ 123 ]).
Stress and Gastrointestinal Complications
The effects of stress on nutrition and the gastrointestinal (GI) system can be summarized with two aspects of GI function.
First, stress can affect appetite (Bagheri Nikoo et al., 2014[ 2 ]; Halataei et al., 2011[ 37 ]; Ranjbaran et al., 2013[ 86 ]). This effect is related to involvement of either the ventral tegmental area (VTA), or the amygdala via N-methyl-D-aspartate (NMDA) glutamate receptors (Nasihatkon et al., 2014[ 80 ]; Sadeghi et al., 2015[ 94 ]). However, it should also be noted that nutrition patterns have effects on the response to stress (Ghanbari et al., 2015[ 31 ]), and this suggests a bilateral interaction between nutrition and stress.
Second, stress adversely affects the normal function of GI tract. There are many studies concerning the effect of stress on the function of the GI system (Söderholm and Perdue, 2001[ 112 ]; Collins, 2001[ 18 ]). For instance, studies have shown that stress affects the absorption process, intestinal permeability, mucus and stomach acid secretion, function of ion channels, and GI inflammation (Collins, 2001[ 18 ]; Nabavizadeh et al., 2011[ 79 ]). Stress also increases the response of the GI system to inflammation and may reactivate previous inflammation and accelerate the inflammation process by secretion of mediators such as substance P (Collins, 2001[ 18 ]). As a result, there is an increase in the permeability of cells and recruitment of T lymphocytes. Lymphocyte aggregation leads to the production of inflammatory markers, activates key pathways in the hypothalamus, and results in negative feedback due to CRH secretion, which ultimately results in the appearance of GI inflammatory diseases (Collins, 2001[ 18 ]). This process can reactivate previous silent colitis (Million et al., 1999[ 76 ]; Qiu et al., 1999[ 85 ]). Mast cells play a crucial role in stress-induced effects on the GI system, because they cause neurotransmitters and other chemical factors to be released that affect the function of the GI system (Konturek et al., 2011[ 55 ]).
Stress can also alter the functional physiology of the intestine (Kiliaan et al., 1998[ 52 ]). Many inflammatory diseases, such as Crohn's disease and other ulcerative-based diseases of the GI tract, are associated with stress (Hommes et al., 2002[ 42 ]). It has been suggested that even childhood stress can lead to these diseases in adulthood (Schwartz and Schwartz, 1983[ 106 ]). Irritable bowel syndrome, which is a disease with an inflammatory origin, is highly related to stress (Gonsalkorale et al., 2003[ 33 ]). Studies on various animals suggest the existence of inflammatory GI diseases following induction of severe stress (Qiu et al., 1999[ 85 ]; Collins et al., 1996[ 19 ]). Additionally, pharmacological interventions, in an attempt to decrease the response of CRH to stress, have been shown to result in an increase in GI diseases in rats (Million et al., 1999[ 76 ]).
Altering the permeability of the mucosal membrane by perturbing the functions of mucosal mast cells may be another way that stress causes its effects on the GI system, since this is a normal process by which harmful and toxic substances are removed from the intestinal lumen (Söderholm and Perdue, 2001[ 112 ]). Also, stress can both decrease the removal of water from the lumen, as well as induce sodium and chloride secretion into the lumen. This most likely occurs by increasing the activity of the parasympathetic nervous system (Barclay and Turnberg, 1987[ 3 ]). Moreover, physical stress, such as trauma or surgery, can increase luminal permeability (Söderholm and Perdue, 2001[ 112 ]) (Table 2 (Tab. 2) ; References in Table 2: Halataei et al., 2011[ 37 ]; Ranjbaran et al., 2013[ 86 ]; Mönnikes et al., 2001[ 77 ]; Collins, 2001[ 18 ]; Nabavizadeh et al., 2011[ 79 ]; Barclay and Turnberg, 1987[ 3 ]; Million et al., 1999[ 76 ]; Gonsalkorale et al., 2003[ 33 ]).

Stress also affects movement of the GI tract. In this way, it prevents stomach emptying and accelerates colonic motility (Mönnikes et al., 2001[ 77 ]). In the case of irritable bowel syndrome, stress increases the movement (contractility and motility) of the large intestine (Mönnikes et al., 2001[ 77 ]). Previous studies have revealed that CRH increases movement in the terminal sections of the GI tract and decreases the movements in the proximal sections of the GI tract (Mönnikes et al., 2001[ 77 ]). A delay in stomach emptying is likely accomplished through CRH-2 receptors, while type 1 receptors affect the colon (Mönnikes et al., 2001[ 77 ]). The effects produced by CRH are so prominent that CRH is now considered an ideal candidate for the treatment of irritable bowel syndrome (Martinez and Taché, 2006[ 69 ]). When serotonin is released in response to stress (Chaouloff, 2000[ 14 ]), it leads to an increase in the motility of the colon by stimulating 5HT-3 receptors (Mönnikes et al., 2001[ 77 ]). Moreover, it has also been suggested that stress, especially mental and emotional types of stress, increase visceral sensitivity and activate mucosal mast cells (Mönnikes et al., 2001[ 77 ]). Stimulation of the CNS by stress has a direct effect on GI-specific nervous system ( i.e. , the myenteric system or plexus) and causes the above mentioned changes in the movements of the GI tract (Bhatia and Tandon, 2005[ 5 ]). In fact, stress has a direct effect on the brain-bowel axis (Konturek et al., 2011[ 55 ]). Various clinical studies have suggested a direct effect of stress on irritable bowel syndrome, intestinal inflammation, and peptic ulcers (Konturek et al., 2011[ 55 ]).
In conclusion, the effects of stress on the GI system can be classified into six different actions: GI tract movement disorders, increased visceral irritability, altered rate and extent of various GI secretions, modified permeability of the intestinal barrier, negative effects on blood flow to the GI tract, and increased intestinal bacteria counts (Konturek et al., 2011[ 55 ]).
Stress and the Endocrine System
There is a broad and mutual relationship between stress and the endocrine system. On one hand, stress has many subtle and complex effects on the activity of the endocrine system (Sapolsky, 2002[ 97 ]; Charmandari et al., 2005[ 15 ]), while on the other hand, the endocrine system has many effects on the response to stress (Ulrich-Lai and Herman, 2009[ 117 ]; Selye, 1956[ 110 ]). Stress can either activate, or change the activity of, many endocrine processes associated with the hypothalamus, pituitary and adrenal glands, the adrenergic system, gonads, thyroid, and the pancreas (Tilbrook et al., 2000[ 116 ]; Brown-Grant et al., 1954[ 11 ]; Thierry et al., 1968[ 115 ]; Lupien and McEwen, 1997[ 64 ]). In fact, it has been suggested that it is impossible to separate the response to stress from the functions of the endocrine system. This premise has been advanced due to the fact that even a minimal amount of stress can activate the hypothalamic-pituitary-adrenal axis, which itself is intricately involved with the activation of several different hormone secreting systems (Sapolsky, 2002[ 97 ]). In different locations throughout this article, we have already discussed the effects of stress on hormones and various endocrine factors and, thus, they will not be further addressed.
Altogether, stress may induce both beneficial and harmful effects. The beneficial effects of stress involve preserving homeostasis of cells/species, which leads to continued survival. However, in many cases, the harmful effects of stress may receive more attention or recognition by an individual due to their role in various pathological conditions and diseases. As has been discussed in this review, various factors, for example, hormones, neuroendocrine mediators, peptides, and neurotransmitters are involved in the body's response to stress. Many disorders originate from stress, especially if the stress is severe and prolonged. The medical community needs to have a greater appreciation for the significant role that stress may play in various diseases and then treat the patient accordingly using both pharmacological (medications and/or nutraceuticals) and non-pharmacological (change in lifestyle, daily exercise, healthy nutrition, and stress reduction programs) therapeutic interventions. Important for the physician providing treatment for stress is the fact that all individuals vary in their response to stress, so a particular treatment strategy or intervention appropriate for one patient may not be suitable or optimal for a different patient.
Yunes Panahi and Amirhossein Sahebkar (Department of Medical Biotechnology, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran, P.O. Box: 91779-48564, Iran; Tel: 985118002288, Fax: 985118002287, E-mail: [email protected], [email protected]) contributed equally as corresponding authors.
Conflict of interest
The authors declare that have no conflict of interest in this study.
Acknowledgement
The authors would like to thank the "Neurosciences Research Center of Baqiyatallah University of Medical Sciences" and the “Clinical Research Development Center of Baqiyatallah (a.s.) Hospital” for providing technical supports.
This site uses session cookies and persistent cookies to improve the content and structure of the site.
By clicking “ Accept All Cookies ”, you agree to the storing of cookies on this device to enhance site navigation and content, analyse site usage, and assist in our marketing efforts.
By clicking ' See cookie policy ' you can review and change your cookie preferences and enable the ones you agree to.
By dismissing this banner , you are rejecting all cookies and therefore we will not store any cookies on this device.
AMRC briefing paper on embedding research in the NHS
On 19 September 2024 the Association of Medical Research Charities (AMRC) published a briefing paper on embedding research in the NHS .
The briefing outlined why research and innovation must be a central part of the solution in the NHS 10-year health plan, and how we can ensure that research is embedded effectively in the NHS by prioritising three areas:
- supporting a thriving clinical research workforce
- maximising opportunities for everyone to take part in research
- making it easy to deliver research throughout the NHS.
We welcome the briefing from AMRC and our Director of Approvals Service, Janet Messer has responded below.

“We were pleased to see the helpful briefing from AMRC following on from the publication of Lord Darzi’s review last week. It provides a further reminder of the importance of research in the NHS. “We agree that charities play a vital role in health and social care research and the AMRC briefing highlights the wide range of benefits non-commercially funded research brings to UK. “The briefing highlights three priorities to ensure research is embedded effectively in the NHS and the Health Research Authority is already working with our partners to support work in these key areas. “We are pleased to see that the HRA’s work with others to champion the importance of diversity and inclusion in research has been recognised. The UK’s diverse population, alongside the well-established research infrastructure in the NHS, provides a unique opportunity for properly representative research to be carried out. This is a key way to tackling health inequalities and to support this we will soon be asking for feedback on our draft inclusion and diversity plan and guidance which is designed to support the research community to design inclusive research. “We are also working with others to clarify how data can be used to identify and invite people to take part in research, to help increase recruitment to clinical studies and trials. “Our aim is to make it easy to do research that people can trust. This briefing makes it clear that more needs to be done to make it easier to deliver research in the NHS, and we are committed to doing everything we can to support this. We are working with others on a range of actions to speed up the set-up of research in the NHS. Across the NHS we have already made a difference to the set-up of commercial research through the National Contract Value Review (NCVR) process which removes the duplication in costing by individual NHS organisations. Thanks to NCVR in 2023 we saw that participating commercial study set-up times were over 100 days quicker compared to pre-pandemic levels. “We understand that the research community is keen to know about the upcoming changes to Clinical Trials Legislation and we have committed to ensuring that we share guidance well in advance of any changes coming into effect so that everyone understands what they need to do.”
- Privacy notice
- Terms & conditions
- Accessibility statement
- Feedback or concerns

IMAGES
VIDEO
COMMENTS
Background Sedentary lifestyle is a major risk factor for noncommunicable diseases such as cardiovascular diseases, cancer and diabetes. It has been estimated that approximately 3.2 million deaths each year are attributable to insufficient levels of physical activity. We evaluated the available evidence from Cochrane systematic reviews (CSRs) on the effectiveness of exercise/physical activity ...
Because physical activity is increasingly executed in an organized manner [17,18,19], sport's role in society has become increasingly important over the years, not only for the individual but also for public health. In this paper, we describe the health effects of sport from a physiological and psychological perspective, related both to ...
In addition, several papers assessing the role of physical fitness on mental health were based on a correlational study design [11,12] often using univariate or small multivariate models, showing a direct association of physical activity or fitness indicators, and a plethora of psychological features and measures. However, correlational studies ...
A chronic disease is an illness that is not contagious, usually of long duration, progresses slowly, and is typically a result of genetics, environment, or poor lifestyle. 1 In 1990, more than 28 million (57%) of all global deaths were caused by chronic disease. 2 This number increased to 36 million (63%) of all global deaths in 2008 3 and 39 million (72%) of all global deaths in 2016 4 (Fig. 1).
Objective. This article aims to provide a brief overview and summary of the evidence on: 1) the preventive effects of physical activity on a wide range of mental disorders; 2) the role of physical activity in promoting the physical health of people with mental disorders; 3) the role of exercise as a strategy to manage mental health symptoms in ...
The prevalence of common mental disorders is on the rise among the populations of western industrial nations (Twenge et al., 2010, Hidaka, 2012).A strong link has been found between mental and physical health (Nabi et al., 2008, Surtees et al., 2008).Ohrnberger, Fichera and Sutton (2017) find strong cross-effects between physical and mental health even after controlling for confounders.
In The Lancet Psychiatry, Chekroud and colleagues1 presented a large cross-sectional examination of physical activity and mental health. Despite imprecision about the terms mental health and exercise in the study—and the cross-sectional design—the findings overall match the existing body of longitudinal research showing that regular physical activity is associated with better mental health.2
Background The treatment of noncommunicable diseases (NCD), like coronary heart disease or type 2 diabetes mellitus, causes rising costs for the health system. Physical activity is supposed to reduce the risk for these diseases. Results of cross-sectional studies showed that physical activity is associated with better health, and that physical activity could prevent the development of these ...
Physical activity (PA) takes a particularly key position in health promotion and prevention. It reduces risks for several diseases, overweight, and all-cause mortality [] and is beneficial for physical, psychological and social health [2,3,4,5] as well as for academic achievement [6, 7].However, PA levels decrease from childhood through adolescence and into adulthood [8,9,10].
Moreover, we produced the analysis of burstness for the top references of the 1988-2021, 2016-2021, and 2021 time periods (Supplementary Tables 2P-R).The analysis of burstness revealed that the top three references with the latest and strongest beginning of citation burst were the Warburton and Bredin paper on health benefits of physical activity (), the Brooks et al. paper on the ...
Abstract. Exercise has long been recognized for its physical health benefits, but its impact on mental health has gained increasing attention in recent years. This paper provides a comprehensive ...
to face the decline or deterioration that occurs in old age with better physical and mental health 11 the sedentary life continues to a ff ect a wide range of the adult population [ 12 ].
Mental illness is a worldwide public health concern. In the UK, there is a high prevalence of mental illness and poor mental wellbeing among young people. The aim of this study was to investigate whether physical activity is associated with better mental wellbeing and reduced symptoms of mental health disorder in adolescents. A cohort of 928 12-13 year olds (Year 8) from six secondary ...
It is well known that physical and mental health are closely related, with growing evidence for biological and behavioural pathways. Mostly the research has focussed on mental health as the key driver of this inter-connection; the extent physical health shapes mental health has received less attention. We aim to derive robust estimates of the unique role physical health may play in shaping ...
Physical Activity and Health concluded that "physical inactivity is causally linked to atherosclerosis and coronary heart disease". A recent research summary indicates that the effects of physical activity on blood pressure are more dramatic than previously thought and are independent of age, body fatness, and other factors.
Introduction and background. Physical activity has its origins in ancient history. It is thought that the Indus Valley civilization created the foundation of modern yoga in approximately 3000 B.C. during the early Bronze Age [].The beneficial role of physical activity in healthy living and preventing and managing health disorders is well documented in the literature.
Physical activity is an important determinant of both physical and psychological health. Regular physical. activity exerts beneficial effects on onset and progression of a number chronic diseases ...
The Coronavirus disease-19 (COVID-19) pandemic affected countries worldwide and has changed peoples' lives. A reduction in physical activity and increased mental health problems were observed, mainly in the first year of the COVID-19 pandemic. Thus, this systematic review aims to examine the association between physical activity and mental health during the first year of the COVID-19 pandemic.
Background: Childhood chronic physical illness is associated with a greater vulnerability for emotional problems (i.e. depression and anxiety) in childhood. However, little is known about life-long effects of childhood chronic physical illness on mental health. The present study aims to systematically review evidence for associations between eight chronic physical illnesses with childhood ...
Several terms have been used to describe and capture an overall state of health. Wellness is more than simply the absence of disease. It is an active process directed toward a healthier, happier, and more fulfilling life and includes not only physical but also psychological and emotional dimensions. 2 The related term well-being can be defined as one's cognitive and affective evaluation and ...
Far from its roots in ancient wisdom traditions, mindfulness is being described today in the context of science—as an expressed trait, relatable to changes in the brain, and with those changes supported by neurobiological and neuroimaging research [1, 2].Understanding mindfulness scientifically can be compared to understanding any other physiological capability of the human body.
Associations of "Weekend Warrior" Physical Activity With Incident Disease and Cardiometabolic Health. Circulation , 2024; DOI: 10.1161/CIRCULATIONAHA.124.068669
Keywords: physical education, healthy behaviors, pedagogy, active methodologies, motivation . Important Note: All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements.Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer ...
This Working Group has been requested: a) to identify areas of promising work related to comorbidity of mental and physical disorders, and to develop recommendations for WPA's involvement in research, education and service development concerning problems related to that comorbidity; b) to identify individuals and centres interested and willing ...
Compromised physical health and raised levels of morbidity and mortality are experienced by young people (16-24 years) with mental illness, and are compounded by psychotropic medication ...
At the University of Florida College of Public Health and Health Professions, several faculty members in the departments of physical therapy and speech, language, and hearing sciences are investigating strategies to enhance the health and wellbeing of people with spinal cord injury. These approaches are designed to improve a wide range of ...
The annual Military Health System Research Symposium brought researchers from across the globe to Kissimmee, Florida, to showcase their cutting-edge science. The international event, known as the ...
Based on the type, timing and severity of the applied stimulus, stress can exert various actions on the body ranging from alterations in homeostasis to life-threatening effects and death. In many cases, the pathophysiological complications of disease arise from stress and the subjects exposed to stress, e.g. those that work or live in stressful ...
On 19 September 2024 the Association of Medical Research Charities (AMRC) published a briefing paper on embedding research in the NHS.. The briefing outlined why research and innovation must be a central part of the solution in the NHS 10-year health plan, and how we can ensure that research is embedded effectively in the NHS by prioritising three areas: