- Search Menu
- Sign in through your institution
- Volume 2024, Issue 6, June 2024 (In Progress)
- Volume 2024, Issue 5, May 2024
- Case of the Year
- MSF Case Reports
- Audiovestibular medicine
- Cardiology and cardiovascular systems
- Critical care medicine
- Dermatology
- Emergency medicine
- Endocrinology and metabolism
- Gastroenterology and hepatology
- Geriatrics and gerontology
- Haematology
- Infectious diseases and tropical medicine
- Medical ophthalmology
- Medical disorders in pregnancy
- Paediatrics
- Palliative medicine
- Pharmacology and pharmacy
- Radiology, nuclear medicine, and medical imaging
- Respiratory disorders
- Rheumatology
- Sexual and reproductive health
- Sports medicine
- Substance abuse
- Author Guidelines
- Submission Site
- Open Access
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Answer to part 1, answer to part 2, answer to part 3, answer to part 4, answer to part 5.
- < Previous
Educational Case: A 57-year-old man with chest pain
Contributed equally.
- Article contents
- Figures & tables
- Supplementary Data
Nikhil Aggarwal, Subothini Selvendran, Vassilios Vassiliou, Educational Case: A 57-year-old man with chest pain, Oxford Medical Case Reports , Volume 2016, Issue 4, April 2016, Pages 62–65, https://doi.org/10.1093/omcr/omw008
- Permissions Icon Permissions
This is an educational case report including multiple choice questions and their answers. For the best educational experience we recommend the interactive web version of the exercise which is available via the following link: http://www.oxfordjournals.org/our_journals/omcr/ec01p1.html
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by paramedics in the community. He smoked 20 cigarettes daily (38 pack years) but was not aware of any other cardiovascular risk factors. On examination he appeared comfortable and was able to complete sentences fully. There were no heart murmurs present on cardiac auscultation. Blood pressure was 180/105 mmHg, heart rate was 83 bpm and regular, oxygen saturation was 97%.
What is the most likely diagnosis?
| A | Acute coronary syndrome |
| B | Aortic dissection |
| C | Esophageal rupture |
| D | Peptic ulceration |
| E | Pneumothorax |
An ECG was requested and is shown in figure 1.
How would you manage the patient? (The patient has already received 300 mg aspirin).
| A | Atenolol 25 mg, Atorvastatin 80 mg, Clopidogrel 75 mg, GTN 500 mcg |
| B | Atenolol 25 mg, Clopidogrel 75 mg, GTN 500 mcg, Simvastatin 20 mg |
| C | Atorvastatin 80 mg, Clopidogrel 300 mcg, GTN 500 mcg, Ramipril 2.5 mg |
| D | Atorvastatin 80 mg, Clopidogrel 75 mg, Diltiazem 60 mg, Oxygen |
| E | Clopidogrel 300 mg, Morphine 5 mg, Ramipril 2.5 mg, Simvastatin 20 mg |
30 minutes later the patient's chest pain returned with greater intensity whilst waiting in the emergency department. Now, he described the pain as though “an elephant is sitting on his chest”. The nurse has already done an ECG by the time you were called to see him. This is shown in figure 2.

ECG on admission.

ECG 30 minutes after admission.
What would be the optimal management for this patient?
| A | Administer intravenous morphine |
| B | Increase GTN dose |
| C | Observe as no new significant changes |
| D | Proceed to coronary angiography |
| E | Thrombolyse with alteplase |
He was taken to the catheterization lab where the left anterior descending coronary artery (LAD) was shown to be completely occluded. Following successful percutaneous intervention and one drug eluding stent implantation in the LAD normal flow is restored (Thrombosis in myocardial infarction, TIMI = 3). 72 hours later, he is ready to be discharged home. The patient is keen to return to work and asks when he could do so.
When would you advise him that he could return to work?
| A | 1 week later |
| B | 3 weeks later |
| C | 6 weeks later |
| D | Not before repeat angiography |
| E | Not before an exercise test |
One week later, he receives a letter informing him that he is required to attend cardiac rehabilitation. The patient is confused as to what cardiac rehabilitation entails, although he does remember a nurse discussing this with him briefly before he was discharged. He phones the hospital in order to get some more information.
Which of the following can be addressed during cardiac rehabilitation?
| A | Diet |
| B | Exercise |
| C | Pharmacotherapy |
| D | Smoking cessation |
| E | All of the above |
A - Acute coronary syndrome
Although the presentation could be attributable to any of the above differential diagnoses, the most likely etiology given the clinical picture and risk factors is one of cardiac ischemia. Risk factors include gender, smoking status and age making the diagnosis of acute coronary syndrome the most likely one. The broad differential diagnosis in patients presenting with chest pain has been discussed extensively in the medical literature. An old but relevant review can be found freely available 1 as well as more recent reviews. 2 , 3
C - Atorvastatin 80 mg, Clopidogrel 300 mcg, GTN 500 mcg, Ramipril 2.5 mg,
In patients with ACS, medications can be tailored to the individual patient. Some medications have symptomatic benefit but some also have prognostic benefit. Aspirin 4 , Clopidogrel 5 , Atenolol 6 and Atorvastatin 7 have been found to improve prognosis significantly. ACE inhibitors have also been found to improve left ventricular modeling and function after an MI. 8 , 9 Furthermore, GTN 10 and morphine 11 have been found to be of only significant symptomatic benefit.
Oxygen should only to be used when saturations <95% and at the lowest concentration required to keep saturations >95%. 12
There is no evidence that diltiazem, a calcium channel blocker, is of benefit. 13
His ECG in figure 1 does not fulfil ST elevation myocardial infarction (STEMI) criteria and he should therefore be managed as a Non-STEMI. He would benefit prognostically from beta-blockade however his heart rate is only 42 bpm and therefore this is contraindicated. He should receive a loading dose of clopidogrel (300 mg) followed by daily maintenance dose (75 mg). 14 , 15 He might not require GTN if he is pain-free but out of the available answers 3 is the most correct.
D - Proceed to coronary angiography
The ECG shows ST elevation in leads V2-V6 and confirms an anterolateral STEMI, which suggests a completely occluded LAD. This ECG fulfils the criteria to initiate reperfusion therapy which traditionally require one of the three to be present: According to guidance, if the patient can undergo coronary angiography within 120 minutes from the onset of chest pain, then this represents the optimal management. If it is not possible to undergo coronary angiography and potentially percutaneous intervention within 2 hours, then thrombolysis is considered an acceptable alternative. 12 , 16
≥ 1 mm of ST change in at least two contiguous limb leads (II, III, AVF, I, AVL).
≥ 2 mm of ST change in at least two contiguous chest leads (V1-V6).
New left bundle branch block.
GTN and morphine administration can be considered in parallel but they do not have a prognostic benefit.
E - Not before an exercise test
This patient is a lorry driver and therefore has a professional heavy vehicle driving license. The regulation for driving initiation in a lorry driver following a NSTEMI/ STEMI may be different in various countries and therefore the local regulations should be followed.
In the UK, a lorry driver holds a category 2 driving license. He should therefore refrain from driving a lorry for at least 6 weeks and can only return to driving if he completes successfully an exercise evaluation. An exercise evaluation is performed on a bicycle or treadmill. Drivers should be able to complete 3 stages of the standard Bruce protocol 17 or equivalent (e.g. Myocardial perfusion scan) safely, having refrained from taking anti-anginal medication for 48 hours and should remain free from signs of cardiovascular dysfunction during the test, notably: angina pectoris, syncope, hypotension, sustained ventricular tachycardia, and/or electrocardiographic ST segment shift which is considered as being indicative of myocardial ischemia (usually >2 mm horizontal or down-sloping) during exercise or the recovery period. 18
For a standard car driving license (category 1), driving can resume one week after successful intervention providing that no other revascularization is planned within 4 weeks; left ventricular ejection fraction (LVEF) is at least 40% prior to hospital discharge and there is no other disqualifying condition.
Therefore if this patent was in the UK, he could restart driving a normal car one week later assuming an echocardiogram confirmed an EF > 40%. However, he could only continue lorry driving once he has passed the required tests. 18
E - All of the above
Cardiac rehabilitation bridges the gap between hospitals and patients' homes. The cardiac rehabilitation team consists of various healthcare professions and the programme is started during hospital admission or after diagnosis. Its aim is to educate patients about their cardiac condition in order to help them adopt a healthier lifestyle. This includes educating patients' about their diet, exercise, risk factors associated with their condition such as smoking and alcohol intake and finally, about the medication recommended. There is good evidence that adherence to cardiac rehabilitation programmes improves survival and leads to a reduction in future cardiovascular events. 19 , 20
Oille JA . Differential diagnosis of pain in the chest . Can Med Assoc J . 1937 ; 37 (3) : 209 – 216 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC536075/ .
Google Scholar
Lee TH , Goldman L . Evaluation of the patient with acute chest pain . N Engl J Med . 2000 ; 342 (16) : 1187 – 1195 . http://www.nejm.org/doi/full/10.1056/NEJM200004203421607 .
Douglas PS , Ginsburg GS . The evaluation of chest pain in women . N Engl J Med . 1996 ; 334 (20) : 1311 – 1315 . http://www.nejm.org/doi/full/10.1056/NEJM199605163342007 .
Baigent C , Collins R , Appleby P , Parish S , Sleight P , Peto R . ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. the ISIS-2 (second international study of infarct survival) collaborative group . BMJ . 1998 ; 316 (7141) : 1337 – 1343 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC28530/ .
Yusuf S , Zhao F , Mehta S , Chrolavicius S , Tognoni G , Fox K . Clopidogrel in unstable angina to prevent recurrent events trail investigators . effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation . N Engl J Med . 2001 ; 345 (7) : 494 – 502 . http://www.nejm.org/doi/full/10.1056/NEJMoa010746#t=articleTop .
Yusuf S , Peto R , Lewis J , Collins R , Sleight P . Beta blockade during and after myocardial infarction: An overview of the randomized trials . Prog Cardiovasc Dis . 1985 ; 27 (5) : 335 – 371 . http://www.sciencedirect.com/science/article/pii/S0033062085800037 .
Schwartz GG , Olsson AG , Ezekowitz MD et al. . Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: The MIRACL study: A randomized controlled trial . JAMA . 2001 ; 285 (13) : 1711 – 1718 . http://jama.jamanetwork.com/article.aspx?articleid=193709 .
Pfeffer MA , Lamas GA , Vaughan DE , Parisi AF , Braunwald E . Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction . N Engl J Med . 1988 ; 319 (2) : 80 – 86 . http://content.onlinejacc.org/article.aspx?articleid=1118054 .
Sharpe N , Smith H , Murphy J , Hannan S . Treatment of patients with symptomless left ventricular dysfunction after myocardial infarction . The Lancet . 1988 ; 331 (8580) : 255 – 259 . http://www.sciencedirect.com/science/article/pii/S0140673688903479 .
Ferreira JC , Mochly-Rosen D . Nitroglycerin use in myocardial infarction patients . Circ J . 2012 ; 76 (1) : 15 – 21 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3527093/ .
Herlitz J , Hjalmarson A , Waagstein F . Treatment of pain in acute myocardial infarction . Br Heart J . 1989 ; 61 (1) : 9 – 13 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1216614/ .
Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK, et al . ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation . Eur Heart J . 2012 ; 33 (20) : 2569 – 2619 . http://eurheartj.oxfordjournals.org/content/33/20/2569 .
The effect of diltiazem on mortality and reinfarction after myocardial infarction . the multicenter diltiazem postinfarction trial research group . N Engl J Med . 1988 ; 319 (7) : 385 – 392 . http://www.nejm.org/doi/full/10.1056/NEJM198808183190701 .
Jneid H , Anderson JL , Wright RS et al. . 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/Non–ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update) A report of the american college of cardiology foundation/american heart association task force on practice guidelines . J Am Coll Cardiol . 2012 ; 60 (7) : 645 – 681 . http://circ.ahajournals.org/content/123/18/2022.full .
Hamm CW , Bassand JP , Agewall S et al. . ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The task force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the european society of cardiology (ESC) . Eur Heart J . 2011 ; 32 (23) : 2999 – 3054 . http://eurheartj.oxfordjournals.org/content/32/23/2999.long .
O'Gara PT , Kushner FG , Ascheim DD et al. . 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: Executive summary: A report of the american college of cardiology foundation/american heart association task force on practice guidelines . J Am Coll Cardiol . 2013 ; 61 (4) : 485 – 510 . http://content.onlinejacc.org/article.aspx?articleid=1486115 .
BRUCE RA , LOVEJOY FW Jr . Normal respiratory and circulatory pathways of adaptation in exercise . J Clin Invest . 1949 ; 28 (6 Pt 2) : 1423 – 1430 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC439698/ .
DVLA . Https://Www.gov.uk/current-medical-guidelines-dvla-guidance-for-professionals-cardiovascular-chapter-appendix .
British Heart Foundation . Http://Www.bhf.org.uk/heart-health/living-with-heart-disease/cardiac-rehabilitation.aspx .
Kwan G , Balady GJ . Cardiac rehabilitation 2012: Advancing the field through emerging science . Circulation . 2012 ; 125 (7) : e369–73. http://circ.ahajournals.org/content/125/7/e369.full .
Author notes
- knowledge acquisition
| Month: | Total Views: |
|---|---|
| December 2016 | 1 |
| January 2017 | 46 |
| February 2017 | 45 |
| March 2017 | 32 |
| April 2017 | 55 |
| May 2017 | 35 |
| June 2017 | 71 |
| July 2017 | 1 |
| August 2017 | 4 |
| September 2017 | 2 |
| October 2017 | 10 |
| November 2017 | 25 |
| December 2017 | 127 |
| January 2018 | 161 |
| February 2018 | 150 |
| March 2018 | 194 |
| April 2018 | 262 |
| May 2018 | 308 |
| June 2018 | 221 |
| July 2018 | 197 |
| August 2018 | 207 |
| September 2018 | 297 |
| October 2018 | 317 |
| November 2018 | 486 |
| December 2018 | 347 |
| January 2019 | 501 |
| February 2019 | 596 |
| March 2019 | 887 |
| April 2019 | 1,123 |
| May 2019 | 1,057 |
| June 2019 | 859 |
| July 2019 | 1,045 |
| August 2019 | 1,010 |
| September 2019 | 1,290 |
| October 2019 | 1,415 |
| November 2019 | 1,238 |
| December 2019 | 996 |
| January 2020 | 1,017 |
| February 2020 | 1,649 |
| March 2020 | 1,204 |
| April 2020 | 990 |
| May 2020 | 931 |
| June 2020 | 1,247 |
| July 2020 | 1,128 |
| August 2020 | 1,021 |
| September 2020 | 1,536 |
| October 2020 | 1,454 |
| November 2020 | 1,534 |
| December 2020 | 1,488 |
| January 2021 | 1,263 |
| February 2021 | 1,232 |
| March 2021 | 1,723 |
| April 2021 | 1,685 |
| May 2021 | 1,343 |
| June 2021 | 1,477 |
| July 2021 | 1,119 |
| August 2021 | 1,469 |
| September 2021 | 2,203 |
| October 2021 | 2,429 |
| November 2021 | 2,176 |
| December 2021 | 1,900 |
| January 2022 | 1,631 |
| February 2022 | 1,755 |
| March 2022 | 2,089 |
| April 2022 | 1,825 |
| May 2022 | 1,452 |
| June 2022 | 1,045 |
| July 2022 | 749 |
| August 2022 | 944 |
| September 2022 | 1,412 |
| October 2022 | 1,677 |
| November 2022 | 1,463 |
| December 2022 | 1,134 |
| January 2023 | 1,180 |
| February 2023 | 1,474 |
| March 2023 | 1,791 |
| April 2023 | 1,389 |
| May 2023 | 1,349 |
| June 2023 | 927 |
| July 2023 | 876 |
| August 2023 | 849 |
| September 2023 | 1,204 |
| October 2023 | 1,534 |
| November 2023 | 1,524 |
| December 2023 | 1,021 |
| January 2024 | 1,247 |
| February 2024 | 1,702 |
| March 2024 | 1,971 |
| April 2024 | 1,546 |
| May 2024 | 1,786 |
| June 2024 | 250 |
Email alerts
Citing articles via, affiliations.
- Online ISSN 2053-8855
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation
Patient presentation.
Mr. Smith is a 60-year-old Caucasian male, who presents with 8/10 chest pain after working out. He just quit smoking and started a new workout and diet program after recently retiring. He has noticed some chest and shoulder discomfort with working out that usually resolves with rest, but decided to come to the emergency department because this episode was unrelenting and more severe. Mr. Smith describes his current pain as severe and sharp, and also complains of nausea and shortness of breath. Vital signs are HR: 110 BP: 150/90 RR: 30 Temp 97.6 O2 Sat: 92% on 2L nasal cannula, EKG shows ST segment elevation in leads II, III and AVf. Labs were drawn, including an elevated troponin (4.23 ng/ml), and slightly elevated white blood cell count (13.6 × 10 9 /L) .
Past Medical History
Type II diabetes (age 47), dyslipidemia (age 33), atherosclerosis (age 52), hypertension (age 49), obesity (age 33), viral pneumonia (age 29), hiatal hernia (age 28), peptic ulcer disease (age 41)
Family Medical History
Mother (deceased) – atrial fibrillation (diagnosed at age 45), died of MI (age 65)
Father (83) – obesity, type II diabetes (diagnosed at 50), COPD (diagnosed at 55)
Social History
Smoker (20 pack years), worked in an office sitting at a desk his whole career (35 years), recently began working out at his local gym since retiring this year.
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 5: 10 Real Cases on Acute Heart Failure Syndrome: Diagnosis, Management, and Follow-Up
Swathi Roy; Gayathri Kamalakkannan
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion.
- Full Chapter
- Supplementary Content
Case 1: Diagnosis and Management of New-Onset Heart Failure With Reduced Ejection Fraction
A 54-year-old woman presented to the telemetry floor with shortness of breath (SOB) for 4 months that progressed to an extent that she was unable to perform daily activities. She also used 3 pillows to sleep and often woke up from sleep due to difficulty catching her breath. Her medical history included hypertension, dyslipidemia, diabetes mellitus, and history of triple bypass surgery 4 years ago. Her current home medications included aspirin, atorvastatin, amlodipine, and metformin. No significant social or family history was noted. Her vital signs were stable. Physical examination showed bilateral diffuse crackles in lungs, elevated jugular venous pressure, and 2+ pitting lower extremity edema. ECG showed normal sinus rhythm with left ventricular hypertrophy. Chest x-ray showed vascular congestion. Laboratory results showed a pro-B-type natriuretic peptide (pro-BNP) level of 874 pg/mL and troponin level of 0.22 ng/mL. Thyroid panel was normal. An echocardiogram demonstrated systolic dysfunction, mild mitral regurgitation, a dilated left atrium, and an ejection fraction (EF) of 33%. How would you manage this case?
In this case, a patient with known history of coronary artery disease presented with worsening of shortness of breath with lower extremity edema and jugular venous distension along with crackles in the lung. The sign and symptoms along with labs and imaging findings point to diagnosis of heart failure with reduced EF (HFrEF). She should be treated with diuretics and guideline-directed medical therapy for congestive heart failure (CHF). Telemetry monitoring for arrythmia should be performed, especially with structural heart disease. Electrolyte and urine output monitoring should be continued.
In the initial evaluation of patients who present with signs and symptoms of heart failure, pro-BNP level measurement may be used as both a diagnostic and prognostic tool. Based on left ventricular EF (LVEF), heart failure is classified into heart failure with preserved EF (HFpEF) if LVEF is >50%, HFrEF if LVEF is <40%, and heart failure with mid-range EF (HFmEF) if LVEF is 40% to 50%. All patients with symptomatic heart failure should be started on an angiotensin-converting enzyme (ACE) inhibitor (or angiotensin receptor blocker if ACE inhibitor is not tolerated) and β-blocker, as appropriate. In addition, in patients with New York Heart Association functional classes II through IV, an aldosterone antagonist should be prescribed. In African American patients, hydralazine and nitrates should be added. Recent recommendations also recommend starting an angiotensin receptor-neprilysin inhibitor (ARNI) in patients who are symptomatic on ACE inhibitors.
Get Free Access Through Your Institution
Pop-up div successfully displayed.
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
To view this video please enable JavaScript, and consider upgrading to a web browser that supports HTML5 video
Case study 1: acute myocardial infarction
Published by Shanon Hunter Modified over 8 years ago
Similar presentations
Presentation on theme: "Case study 1: acute myocardial infarction"— Presentation transcript:
Cardiovascular Diseases
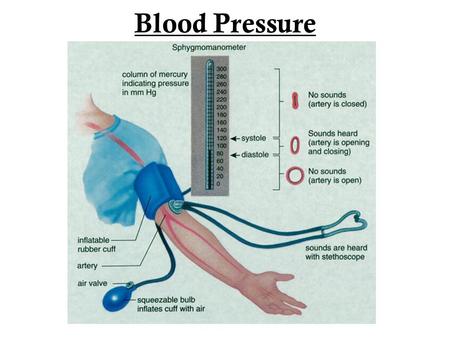
Blood Pressure.
Why is Physical Education so Important?. Benefits of Exercise Gives you more energy Reduces risk of Heart Failure Improves your Fitness Level Helps cope.
How can you prevent cardiovascular disease?. A disease that is not transmitted by another person, vector, or the environment Habits and behaviors.
The Healthy Heart Figure 14.1.
What You Will Do Identify changeable risk factors that can lead to diseases of the heart and lungs. Explain diseases that can result from certain lifestyles.
Mosby items and derived items © 2006 by Mosby, Inc. Slide 1 Chapter 19 Coronary Heart Disease and Hypertension.
By: Chelsea Eckel I’m too young to worry about heart disease. I’d know if I had high blood pressure because there are warning signs. I’ll know when I’m.
What is Diabetes? A disease in which there are high levels of sugar in the blood. Three types of Diabetes: Type 1 Type 2 Gestational Diabetes affects.
By Cyneetha Strong, MD May 19, Diseases and conditions pertaining to the heart and vascular (blood vessels) system Primarily includes heart.
Lifesaving information on Heart Attacks Presented to: Members of Virtua’s Health Systems Presented by: Rachel Zeilman.

The force of blood pushing against the walls of the arteries as the heart pumps blood High Blood Pressure is when the force of the blood against your.
What is Coronary Heart Disease? Who is at Risk for Coronary Heart Disease? Signs and Symptoms of Coronary Heart Disease. How Is Coronary Heart.
Hypertension and Nutrition Haley Aimone What Is HYPERTENSION Chronic medical condition Blood pressure in arteries are elevated Can lead to heart disease,
Transports nutrients and removes waste from the body. Supplies blood and oxygen to the body.
Risks & Prevention for Young Adults Cardiovascular Disease Kristen Hinners.

HEART HEALTH. LET’S SEE WHAT YOU KNOW ABOUT THE HUMAN HEART!
Angina and MI.
Lifestyle Diseases.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 4: 10 Real Cases on Valvular Heart Disease: Diagnosis, Management, and Follow-Up
Nikhitha Mantri; Puvanalingam Ayyadurai; Marin Nicu
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion.
- Clinical Symptoms
- Full Chapter
- Supplementary Content
Case 1: Management of Patent Foramen Ovale
A 26-year-old woman presented to the emergency department (ED) with chest pain for 1 day. The chest pain started suddenly, was nonradiating, and was associated with arm movement. She did house cleaning 1 day prior to presentation. The pain was not relieved by taking over-the-counter medication. She denied palpitations, dizziness, shortness of breath, and trauma. Her family history and social history were unremarkable. On presentation to the ED, her vital signs were stable. On physical examination, she did not have any significant findings except chest wall tenderness. Her ECG showed first-degree atrioventricular block. Initial laboratory findings were unremarkable. She was given analgesics. The patient was transferred to the telemetry floor, where an echocardiogram was performed, which showed a normal left ventricular ejection fraction with no wall motion or valvular abnormality and a small patent foramen ovale (PFO). How would you manage this case?
This patient is a young asymptomatic woman who presented with musculoskeletal chest pain. Incidentally, she was noted to have a PFO, which is asymptomatic and does not require any treatment.
PFO is an opening in the atrial wall at the location of the fossa ovalis that remains open beyond 1 year of life. After birth, when the pulmonary circulation develops, the foramen ovale closes due to the increase in left atrial pressures, which takes up to 1 year.
PFO is usually asymptomatic and is often found incidentally. However, it carries a risk of paradoxical embolism in high-risk patients. Some patients present with systemic embolism causing organ infarcts and even myocardial infarction.
The diagnostic test of choice is echocardiography. PFO can be detected using color flow Doppler, contrast echocardiography, and transmitral Doppler.
Isolated PFO does not usually require any treatment unless it is associated with an unexplained neurologic event. Such conditions are treated with antiplatelet drugs and anticoagulation therapy. Percutaneous closure of the PFO is an option when there is contraindication to medical management and anticoagulant treatment, in the setting of paradoxical embolism or cryptogenic stroke. Surgical closure is indicated when the opening is >25 mm or when there is failure of a percutaneous device.
PFO is usually asymptomatic and is often found incidentally.
Isolated PFO does not usually require any treatment unless it is associated with an unexplained neurologic event.
Case 2: Management of Aortic Stenosis
Get free access through your institution, pop-up div successfully displayed.
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Advertisement
Case presentation: a patient presenting with cardiac arrest, register for free or log in to view this content.

TAVR for Intermediate-Risk and Low-Risk Patients: Review of the Literature
Excel top line results revisited, coronary revascularization in severe heart failure: stich and beyond, we recommend.
New at TCTMD? Register today!
Forgot Password
Forgot Your Password?
Enter the email you used to register to reset your password.
Search TCTMD
Sign up for our newsletter.
Sign up to receive the most important cardiovascular news, research, and major meeting presentations.
Submit an Event
Become a premium member or log in to view exclusive content.
This content is available for meeting attendees and/or Platinum Members
- Preferences

Cardiac Case Study - PowerPoint PPT Presentation

Cardiac Case Study
For more information on ge nuclear cardiology products and the unique hawkeye ct ... the american society of nuclear cardiology and the society of nuclear medicine. ... – powerpoint ppt presentation.
- Inferior wall attenuation and correction with CT-based Attenuation Correction
- Imaging Procedure
- As part of the acquisition quality control for this data, fused SPECT-CT images were checked for proper registration of attenuation maps and emission data.
- Further quality control checks showed the acquisition to be of good quality
- The stress and rest selective linograms showed no significant motion in the vertical direction and showed no significant extra-cardiac activity that would interfere with the reconstruction.
- The stress and rest sinograms showed no significant motion in the horizontal direction
- Myocardial count density was adequate. The stress maximum pixel value was 201 rest maximal pixel value was 65. The guideline for an adequate count study for 60-64 projection images is to have a maximum pixel value of at least 50 counts within a tight circular/ elliptical ROI around the epicardial edge of the myocardium on an anterior view of the heart.
- There were no gating errors
- Thickening is the parameter most prone to error in the presence of arrhythmias. Slice appearance is maintained in the presence of arrhythmias except in very severe cases. LV ejection fraction (EF) is a robust parameter that is little affected by arrhythmias. Quantitative perfusion measures were also little affected by arrhythmias except in the case of atrial fibrillation.1
- The rotating projection images show soft tissue attenuation in the waist area which can cause increased attenuation of the inferior wall.
- What are the advantages of doing attenuation correction on cardiac studies?
- Provide images that are more uniform and easier to interpret
- Decrease acquisition time
- Increase myocardial count density
- Increase sensitivity and overall diagnostic accuracy
- Both A and D
- What are the further advantages of doing CT-based attenuation correction on cardiac studies?
- A. CT-based AC produces high quality transmission maps
- B. CT-based AC is consistent with time
- C. CT-based AC is consistent over a full range of body types
- D. All of the above
- There are significant differences in the ability of different commercial AC systems to reduce artifacts due to attenuation, hot liver / bowel activity and type of orbit. Systems that can generate high quality attenuation maps yielded the best results. A high quality attenuation map appears to be an important determinant of image quality.3
- Stress and rest images were reconstructed by filtered back projection (FBP) and iterative reconstruction with attenuation correction (IR-AC). Count deficiencies in the inferior walls of both the stress and rest FBP slices have been noticeably improved in the IR-AC slices, correcting for inferior wall attenuation.
- 1. Nichols K, Yao S, Kamran M, Faber TL, Cooke, CD, and DePuey EG. Clinical impact of arrhythmias on gated SPECT cardiac myocardial perfusion and function assessment. J Nucl Cardiol 2001 819-30.
- 2. Hendel RC, Corbett JR, Cullom SJ, DePuey EG, Garcia EV, and Bateman TM. The Value and Practice of Attenuation Correction for Myocardial Perfusion SPECT Imaging A Joint Position Statement form the American Society of Nuclear Cardiology and the Society of Nuclear Medicine. J Nucl Med 2002 43273-280
- 3. OConnor MK, Kemp B, Anstett F, Christian P, Ficaro EP, Frey E, Jacobs M, Kritzman JN, Pooley RA, and Wilk M . A multicenter evaluation of commercial attenuation compensation techniques in cardiac SPECT using phantom models. J Nucl Cardiol 2002 9361-76.
PowerShow.com is a leading presentation sharing website. It has millions of presentations already uploaded and available with 1,000s more being uploaded by its users every day. Whatever your area of interest, here you’ll be able to find and view presentations you’ll love and possibly download. And, best of all, it is completely free and easy to use.
You might even have a presentation you’d like to share with others. If so, just upload it to PowerShow.com. We’ll convert it to an HTML5 slideshow that includes all the media types you’ve already added: audio, video, music, pictures, animations and transition effects. Then you can share it with your target audience as well as PowerShow.com’s millions of monthly visitors. And, again, it’s all free.
About the Developers
PowerShow.com is brought to you by CrystalGraphics , the award-winning developer and market-leading publisher of rich-media enhancement products for presentations. Our product offerings include millions of PowerPoint templates, diagrams, animated 3D characters and more.

Cardiac Case Study
Jun 16, 2013
140 likes | 922 Views
Cardiac Case Study. Inferior wall attenuation and correction with CT-based Attenuation Correction . Linda Campbell, BS GE Applications Scientist. Type of acquisition. Time per stop. Agent. Dose. Rest . Ungated SPECT; CT. 25 seconds. 99m Tc Sestamibi. 15 mCi. Stress. Gated SPECT; CT.
Share Presentation
- vertical motion e
- correct answer
- coronary artery
- nuclear cardiology
- quantitative perfusion

Presentation Transcript
Cardiac Case Study Inferior wall attenuation and correction with CT-based Attenuation Correction Linda Campbell, BS GE Applications Scientist
Type of acquisition Time per stop Agent Dose Rest Ungated SPECT; CT 25 seconds 99m Tc Sestamibi 15 mCi Stress Gated SPECT; CT 25 seconds 99m Tc Sestamibi 30 mCi Patient History A 68 year old male was referred for myocardial perfusion imaging three months status post revascularization of the right coronary artery for evaluation of patency. Some atypical chest pain was noted. Imaging Procedure: The one day Sestamibi protocol was used, and rest imaging was performed first. SPECT imaging was done with 60 stops over 180 degrees. In addition, CT images were acquired. Acquisitions were done on a GE Hawkeye. Target heart rate (85% of maximum heartrate): 129 Maximal heart rate achieved on treadmill: 90%
Imaging Analysis As part of the acquisition quality control for this data, fused SPECT-CT images were checked for proper registration of attenuation maps and emission data. SPECT-CTsagittal fusion SPECT-CT transaxial fusion
Further quality control checks showed the acquisition to be of good quality: • The stress and rest selective linograms showed no significant motion in the vertical direction and showed no significant extra-cardiac activity that would interfere with the reconstruction. • The stress and rest sinograms showed no significant motion in the horizontal direction • Myocardial count density was adequate. The stress maximum pixel value was 201; rest maximal pixel value was 65. The guideline for an adequate count study for 60-64 projection images is to have a maximum pixel value of at least 50 counts within a tight circular/ elliptical ROI around the epicardial edge of the myocardium on an anterior view of the heart. • There were no gating errors
Question 1 – Acquisition quality controlWhich one of the following acquisition factors has the least effect on slice image quality? A. Horizontal motion B. Myocardial count density C. Gating errors D. Vertical motion E. Intense extra-cardiac activity adjacent to the heart
The correct answer is C - Gating errors Thickening is the parameter most prone to error in the presence of arrhythmias. Slice appearance is maintained in the presence of arrhythmias except in very severe cases. LV ejection fraction (EF) is a robust parameter that is little affected by arrhythmias. Quantitative perfusion measures were also little affected by arrhythmias except in the case of atrial fibrillation.1 As has been well documented in the literature, vertical and horizontal motion and myocardial count density are critical for slice image quality. Intense visceral activity close to the heart can also affect slice image quality as it results in changed slice count densities.
The rotating projection images show soft tissue attenuation in the waist area which can cause increased attenuation of the inferior wall. Click Click Stress projection images Rest projection images Soft tissue attenuation may create artifacts that mimic true perfusion abnormalities and can lead to false positive interpretation.
Question 2 – Attenuation correction What are the advantages of doing attenuation correction on cardiac studies? • Provide images that are more uniform and easier to interpret • Decrease acquisition time • Increase myocardial count density • Increase sensitivity and overall diagnostic accuracy • Both A and D
The correct answer is E – Both A and D Attenuation correction can provide images that are more uniform and easier to interpret, and increase sensitivity and overall diagnostic accuracy. The diagnostic accuracy of SPECT imaging is compromised by soft tissue attenuation artifacts. Though education, experience, and the application of gated SPECT imaging have greatly helped, there is a need for improved diagnostic accuracy. Attenuation correction SPECT techniques represent a significant advance in myocardial perfusion imaging and hold great promise for improved assessment of cardiac patients.2
Question 3 – CT-based attenuation correction What are the further advantages of doing CT-based attenuation correction on cardiac studies? A. CT-based AC produces high quality transmission maps B.CT-based AC is consistent with time C. CT-basedAC is consistent over a full range of body types D. All of the above
The correct answer is D – all of the above There are significant differences in the ability of different commercial AC systems to reduce artifacts due to attenuation, hot liver / bowel activity and type of orbit. Systems that can generate high quality attenuation maps yielded the best results.A high quality attenuation map appears to be an important determinant of image quality.3 Stress attenuation map Rest attenuation map
Stress and rest images were reconstructed by filtered back projection (FBP) and iterative reconstruction with attenuation correction (IR-AC). Count deficiencies in the inferior walls of both the stress and rest FBP slices have been noticeably improved in the IR-AC slices, correcting for inferior wall attenuation. FBP IR-AC Stress SA slices Rest SA slices FBP IR-AC Stress VLA slices Rest VLA slices
EKG Results Non-specific ECG changes were noted with no ST depression at maximal exertion. Test terminated at maximal heart rate and SOB. No chest pain was noted. Findings FBP images were interpreted as inferior wall scar with possible ischemic component. This could also be a diaphragmatic attenuation artifact. With CT-based AC the inferior wall is shown to be viable with no ischemia. The validity of the revascularization of the RCA is confirmed. For more information on GE Nuclear Cardiology products and the unique Hawkeye CT based cardiac AC, visit:GE Hawkeye Cardiac Attenuation Correction Findings and Images Courtesy of VA Medical Center, Baltimore, Maryland
References 1. Nichols K, Yao S, Kamran M, Faber TL, Cooke, CD, and DePuey EG. Clinical impact of arrhythmias on gated SPECT cardiac myocardial perfusion and function assessment. J Nucl Cardiol 2001; 8:19-30. 2. Hendel RC, Corbett JR, Cullom SJ, DePuey EG, Garcia EV, and Bateman TM. The Value and Practice of Attenuation Correction for Myocardial Perfusion SPECT Imaging: A Joint Position Statement form the American Society of Nuclear Cardiology and the Society of Nuclear Medicine. J Nucl Med 2002; 43:273-280 3. O’Connor MK, Kemp B, Anstett F, Christian P, Ficaro EP, Frey E, Jacobs M, Kritzman JN, Pooley RA, and Wilk M . A multicenter evaluation of commercial attenuation compensation techniques in cardiac SPECT using phantom models. J Nucl Cardiol 2002; 9:361-76.
- More by User
Case Study. Dominican Republic – Measures Affecting the Importation and Internal Sale of Cigarettes 蔡奉真、黃琳君、李炎蒼. Parties and measure in dispute. parties : Dominican Republic Honduras Measure in dispute : 一、多明尼加要求於該國境內銷售之香菸,不論是否進口產品,包裝上均應貼上印花,以證明已經繳稅得以合法銷售。
1.22k views • 37 slides
Cardiac Nurse Case Management HBDHB
Practice setting. Heath Care Services is the major public health provider in the region comprising Hawke's Bay Hospital on the Heretaunga Health Village site in Hastings (400 bed capacity)Rural health centres in Wairoa and Central Hawke's Bay, a city health centre in Napier and health services a
695 views • 18 slides
Case Study. Presented by. Araro Jireh Ary Andana Bambang Wijarnako. The Content. Southwest Airlines at a Glance. What makes SWA Different?. Case Analysis. Recommendation. Southwest Airlines at a Glance. Southwest Airlines at a Glance.
1.34k views • 21 slides
Haemorrhagic Fever In search of the “culprit ”. CASE STUDY. Study case presented by Daniele de Meneghi: UNITO_FMV, Italy ; Carla Rosenfeld: UACH, Chile; Ludovina Padre: UEVORA, Portugal; Carolina Pujol: UABC, Mexico , SAPUVETNET III members of group VII.
858 views • 27 slides
Case Study.
600 views • 7 slides
Case Study. By: Carla Norman. Part A: Getting to know your student. Motivation Survey Strengths: concept of print, return sweep, and word boundary Weaknesses: word formation, letter/sound association, reading comprehension
367 views • 9 slides

Case study: Complex congenital cardiac lesions…
Case study: Complex congenital cardiac lesions…. Introduction. MDCT and Cardiac MRI has stimulated the interest of radiologists in the diagnosis of congenital heart disease and encouraged the reappraisal of classifications and definitions used by cardiologists and cardiac surgeons.
1.99k views • 181 slides
Case Study. Prasun K Jalal MD Baylor College of Medicine. Case no. 1. 53/M, Caucasian Fatigue and lower extremity swelling- 6 m H/O IV drug use in 1970’s Drinks 2-3 beer a day for 20 yrs, stopped 6 m back. Examination. BMI 35 Spider angioma on chest Hepatosplenomegaly
735 views • 38 slides
CASE STUDY. Learning Objectives. To research and revise the case study for Section B of the exam. Warp Documentary.
513 views • 16 slides

Case Study . The Study of an Environmental Impact Statement for a Wind Farm Liam Dervan, EHO Galway. E.I.S. Team, Galway. Under the auspices of; Mr Brendan Lawlor, A/PEHO Team Members; Mr Gerry Leen, SEHO Mr Seamus Mitchell, SEHO Ms Niamh Kelly, EHO
661 views • 45 slides
Case Study. Deirdre Downes. My Father: My Siblings Mother, and Mom likes me best. Many Siblings One Health Care Proxy: the story of Mr. L
301 views • 7 slides
Case Study. Blood Diamonds & Human Rights in Africa. Bell Work . Finish the following words or sentences with as many words or phrases as you can. “Diamonds are …”. Blood Diamonds.
582 views • 11 slides
Case Study. The Ombudsman Perspective. What safety issues would you look for in this resident’s case?.
366 views • 11 slides
Case Study. The Financial Professional recommended that they put their retirement funds into a product such as an annuity with a guaranteed principal feature. The Financial Professional helped Dan and Sheryl purchase a conservative
528 views • 1 slides
Case Study. Integrated Metadata Driven Statistical Data Management System (IMD SDMS) CSB of Latvia [email protected] METIS 2010. Outline. The main steps for IMD SDMS creation IMD SDMS fundamental elements Costs & benefits IMD SDMS implementation strategy
470 views • 20 slides
Ted A. Bonebrake, M.D. Case Study. Initial Presentation.
945 views • 63 slides
Relevant Evidence.
271 views • 1 slides
CASE STUDY. We are going to analyze and review the zero tolerance policy but in terms of using “common sense.’ Today’s case study will take place in three different school campuses, simultaneously. Keep in mind: The definition of violence. The need for a zero tolerance policy.
926 views • 23 slides
High Risk Case Study Sudbury Regional Hospital Cardiac Rehabilitation
High Risk Case Study Sudbury Regional Hospital Cardiac Rehabilitation. High Risk Case Study. 66 year old male MI 16 years ago and 2 months ago CABG 6 years ago Cardiac Arrest during recent Angiogram. High Risk Case Study. Left Ventricle Ejection Fraction Grade 4 ( less than 20%)
352 views • 17 slides
Unfolding cardiac case study
Unfolding cardiac case study. With live role play. The patient. Mr. Smith 55 years old CC: blurry vision that started several months ago and has worsened recently
430 views • 28 slides
A CASE OF CARDIAC ASTHMA
A CASE OF CARDIAC ASTHMA. By Dr. Jawahar Shah M.D.(Hom). NOTE: To protect the patient’s identity, we have used a model’s picture or photographs for the purpose of presentation. Shri K 64 years Cardiac Asthma Last six months.
549 views • 19 slides
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

indigenous canada
8 templates
6 templates

23 templates
114 templates
11 templates
computer technology
293 templates
Sudden Cardiac Arrest Clinical Case
It seems that you like this template, sudden cardiac arrest clinical case presentation, free google slides theme, powerpoint template, and canva presentation template.
Cardiac arrest is no laughing matter: the heart stops beating all of a sudden, so you probably guess what that means. It's a medical emergency of the highest priority. Please use our template to prepare a slideshow with a clinical case about cardiac arrest. The color palette contains gray and red, the latter due to being associated with hearts, and these colors appear in the form of gradients. There are other editable resources so that your data appears on the screen in the clearest way possible.
Features of this template
- 100% editable and easy to modify
- 28 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Arq Bras Cardiol
- v.103(3); 2014 Sep

Case 4/2014 - A 66-Year-Old Man with Acute Myocardial Infarction and Death in Asystole after Primary Coronary Angioplasty
A 66-year-old man sought medical care at the hospital due to severe chest pain lasting for 24 hours. The patient was aware of being hypertensive and was a smoker. Without any prior symptom, he started to have severe chest pain and sought emergency medical care after about 24 hours, due to pain persistence.
At physical examination (August 13, 2005, 10 PM) he had a heart rate of 90 bpm and blood pressure of 110/70 mmHg. Lung examination showed no alterations. Heart assessment showed a systolic murmur in the lower left sternal border and mitral area.
The initial electrocardiogram (August 13, 2005, 22 h) showed HR of 100 bpm, sinus rhythm, 1 st -degree atrioventricular block (PR 240 ms), low-voltage QRS complexes in the frontal plane, QRS complex electrical alternans and extensive ongoing anterior wall infarction (QS V1 to V6, ST elevation in the same leads and QS in the inferior wall, II, III and aVF) ( Figure 1 ).

ECG: low QRS voltage in the frontal plane, electrical alternans of QRS complexes, electrically inactive lower wall area and extensive ongoing myocardial infarction.
Acetylsalicylic acid by oral route and 5 mg of intravenous metoprolol were administered. The patient had bradycardia and cardiorespiratory arrest in pulseless electrical activity, reversed after five minutes. He developed hypotension and peripheral hypoperfusion and was transferred to InCor (The Heart Institute).
On admission he had received heparin and continuous intravenous norepinephrine. BP was 60/30 mmHg.
The ECG (August 13, 2005, 11:36 PM) disclosed heart rate of 116 bpm, junctional escape rhythm with sinus arrest and atrial extrasystoles); low-voltage QRS complex in the frontal plane, extensive ongoing anterior acute myocardial infarction, inactive area in the inferior wall; presence of ST elevation at V1 to V5 and ST depression in leads I, II and aVF; ST elevation in aVR ( Figure 2 ).

ECG: low QRS voltage in the frontal plane, electrically inactive lower wall area and anterior myocardial infarction with increased ST elevation, still with positive T waves, "hyperacute phase of myocardial infaction".
Coronary angiography was indicated, which disclosed anterior interventricular branch occlusion and images suggestive of intracoronary thrombus, lesion of 70% in the circumflex artery, 50% in the right coronary artery and 70% in the ostium of the right posterior descending branch. Angioplasty was performed with stent implant in the anterior interventricular artery, but distal flow was not restored. This was followed by cardiac arrest in asystole, which did not respond to treatment and the patient died.
Clinical Aspects
This clinical case reports on a 66-year-old hypertensive patient, long-term smoker, who sought medical care due to acute chest pain. The main diagnostic hypothesis for this clinical case is of acute coronary syndrome.
Chest pain is one of the most common reasons for seeking emergency care and remains a challenge for the clinician, due to the difficulty in differentiating between non-emergency diagnoses and those of high morbidity and mortality, such as acute coronary syndrome (ACS), aortic dissection and pulmonary thromboembolism.
In the assessment of acute chest pain, there are three basic parameters for its management: clinical examination (clinical history and physical examination), electrocardiogram (ECG) and myocardial necrosis markers. They should be analyzed together to provide a safer approach to the patient, especially when it is necessary ruling out ACS. Chest radiography, chest Computed Tomography Angiography (CTA), echocardiography and other tests may be useful in the differential diagnosis.
Approximately 15-25% of patients presenting in the ER with chest pain are diagnosed with acute coronary syndrome, and this represents its more frequent clinical manifestation 1 . Therefore, in the first step of the evaluation, which is the clinical examination, the greater determinant of an ischemic etiology is the characteristic presence of angina.
Angina is often described as a burning or compression sensation or difficulty breathing, located in the precordial region or any other region of the chest, radiating to the neck, shoulder and left arm. It usually increases in intensity within minutes and may be accompanied by symptoms such as nausea and sweating. It can be triggered by physical or emotional stress and relieved by rest or use of nitrates. It should also be remembered that ACS can occur without obvious precipitating factors and be asymptomatic or present as ischemic equivalent, especially in the elderly and diabetic patients with autonomic dysfunction (dyspnea, syncope and pre-syncope).
On the other hand, there are characteristics of pain that make the diagnosis of ACS unlikely, such as pleuritic pain (reproduced by respiratory movements) located with the fingertip, pain in meso/hypogastrium region and reproduction of pain with local palpation or movement. These features raise the suspicion of other differential diagnoses such as pericarditis, pleuritis, gastrointestinal or musculoskeletal diseases.
In the present case report, the patient presented with prolonged chest pain, which does not rule out acute coronary syndrome (ACS), but raises the possibility of some condition associated with this coronary picture, such as pericarditis or mechanical complications.
Among the most important risk factors for atherosclerotic disease risk are dyslipidemia, diabetes mellitus, hypertension, male gender, older age, obesity/metabolic syndrome, smoking, sedentary lifestyle, chronic kidney disease, depression and stress. This patient had some risk factors that contributed to the development of coronary artery disease: age, male gender, hypertension and smoking.
Patients with chest pain and ACS often have a nonspecific physical examination, with less than 20% of them showing significant alterations in the initial evaluation 2 . This becomes important by helping in the detection of differential diagnoses (e.g., pericardial friction rub in pericarditis) or by inferring the presence of risk factors for coronary artery disease (abdominal or carotid murmur, among others).
However, when findings resulting from an ACS are present, they indicate a worse prognosis due to mechanical complications or due to a large area of myocardium at risk and ventricular dysfunction (hypotension, tachycardia, pulmonary edema and mitral regurgitation murmur secondary to ischemia).
The electrocardiogram is important in the diagnostic, prognostic and therapeutic approach and must be obtained within 10 minutes after the presentation of patients with ongoing chest pain 2 . A normal electrocardiographic tracing does not exclude the possibility of ACS and a serial ECG is indicated, which increases its sensitivity and helps differentiating between acute and chronic alterations.
The patient reported in this clinical case had, at the admission ECG performed at another service, ST-segment elevation in the anterior wall, suggesting the hypothesis of acute coronary syndrome with ST-segment elevation. However, this ECG also showed low voltage and electrical alternans of the QRS complex, which suggests large pericardial effusion or even cardiac tamponade.
The main hypothesis for this pericardial effusion is a mechanical complication of myocardial infarction: left ventricular free wall rupture. It occurs within 24 hours after infarction or between the third and fifth day, has an incidence of 0.8 to 6.2% and is more common in an extensive myocardial infarction, in the elderly, women and hypertensive patients. Its clinical course is variable 3 and may be acute and severe, leading to sudden death or subacute, with nonspecific clinical manifestations.
Other mechanical complications that may be present in myocardial infarction are papillary muscle and interventricular septum rupture. These complications do not present with significant pericardial effusion and normal pulmonary auscultation in this patient also makes the diagnosis of papillary muscle rupture less likely. This clinical condition presents with pulmonary congestion due to volume overload secondary to acute mitral regurgitation.
Another diagnostic hypothesis for this patient presenting with chest pain and pericardial effusion would be aortic dissection. Pain, in these cases, is usually of sudden onset and strong intensity since the beginning (unlike angina pain, which often increasingly escalates). It is often described as excruciating and its location reflects the site and progression of the dissection. Autonomic signs (pallor, profuse sweating) are greatly associated.
In aortic dissection, physical examination may disclose hypertensive crisis, differences between limb pulses, signs of pleural and pericardial effusion, diastolic murmur of aortic regurgitation, different from the systolic murmur detected in this clinical case. The extension of the dissection to other vessels can lead to other symptoms corresponding to ischemia of the organs irrigated by them: cerebrovascular accident, acute myocardial infarction, mesenteric ischemia, etc.
Another diagnostic hypothesis for the clinical case is pulmonary embolism. The absence of pulmonary symptoms, mainly dyspnea, makes this hypothesis less likely. It is the most common symptom of this disease, occurring in over 78% of the patients 4 . Sudden chest pain of sudden onset and very often pleuritic, affects up to 44% of patients 4 . Cough and hemoptysis may also occur. Additionally, there was no mention is made on admission at the other service, of right ventricular dysfunction manifestations, such as jugular stasis and hypotension.
The patient, an hour and 36 minutes after his admission at the Heart Institute, was submitted to coronary angiography with left anterior descending artery angioplasty. However, he developed asystole and cardiac arrest.
The main diagnoses for the final clinical picture are cardiogenic shock and/or distributive shock due to cardiac tamponade, discussed below.
The hypothesis of cardiogenic shock should be considered, as the patient had an extensive acute myocardial infarction without culprit artery reperfusion even after percutaneous revascularization attempt. However, this diagnosis cannot fully explain the patient's clinical condition, such as the absence of pulmonary congestion, which usually follows an acute myocardial failure.
Considering the patient's history, late cardiac tamponade seems to have been the main precipitating factor of the final clinical picture in this case. The electrocardiographic findings commonly observed in cardiac tamponade are low voltage and electrical alternans of the QRS complex, observed in the case. Although physical examination made no reference to clinical findings suggestive of tamponade, such as jugular stasis or muffled heart sounds, we cannot exclude this diagnostic hypothesis.
An echocardiography could have been performed to confirm this diagnosis, which is the most widely used noninvasive method for diagnostic investigation of this pathology. The ventriculography in this context would not be informative, as it was a free wall rupture with cardiac tamponade and thus, it would not allow the visualization of contrast leakage into the pericardial cavity.
This is a patient with myocardial infarction that came at the emergency room more than 24 hours after the onset of the event and who probably had a mechanical complication of myocardial infarction: ventricular free wall rupture.
Most deaths from myocardial infarction occur in the first hours of disease onset, with 40-65% occurring within the first hour and approximately 80% in the first 24 hours 5 , 6 . The recently implemented therapies for MI treatment have been proven to modify patient evolution and prognosis. However, the effectiveness of most of these measures is time-dependent and delay in seeking medical care may have been the factor that likely contributed to the clinical outcome of the patient in this case report. (Dr. Wilma Noia Ribeiro, Dr. Alice Tatsuko Yamada)
Diagnostic hypotheses: Acute myocardial infarction with mixed shock (cardiogenic - distributive) by mechanical complication - free wall rupture with tamponade (Dr. Wilma Noia Ribeiro, Dr. Alice Tatsuko Yamada)
The heart weighed 414 g. The myocardium of the left ventricular anterosseptal wall and right ventricular anterior wall was softened, slightly yellowish in color, characterizing extensive transmural acute myocardial infarction. There was an obvious narrowing of the affected anterosseptal wall, with ventricular septum rupture in the anterior region of its mid portion, with a ventricular septal defect measuring 10 mm in its longest axis. The other left ventricular walls showed to be slightly hypertrophic and there was a small area of fibrosis in the postero-inferior region of the ventricular septum. There was also moderate right ventricular dilation ( Figure 3 ).

Cross-section of the ventricles showing left ventricular transmural infarction of the anterosseptal wall (asterisks) and of the right ventricular anterior wall (arrows). The explorer shows the VSD secondary to septal rupture. Observe the ventricular wall thinning and the small area of fibrosis in the ventricular septum (arrowhead).
Histological analysis confirmed the presence of myocardial infarction, with marked neutrophil infiltration, confirming histological dating of 24-48 hours of onset. Another small ongoing microinfarction was observed in the posterior region of the ventricular septum, in addition to the previously described small area of fibrosis (healed infarction), compatible with approximately 7-10 days of evolution.
There was superficial fibrin deposition in the epicardium, with the presence of reactive inflammatory infiltrate. Examination of the initial segment of the left anterior descending artery showed fatty atherosclerotic plaques with areas of marked thinning of the fibrous cap that covered the lipid core and 80% of obstruction.
There were also areas of plaque rupture and hemorrhage, with acute thrombosis in the first and second centimeters of that artery ( Figs. 4 and and5 5 ).

Histological section of the first centimeter of the left anterior descending artery showing large lipid-core atherosclerotic plaque, with internal area of fibrin deposition and hemorrhage (asterisk). Observe the area with marked thinning of the fibrous cap of the lipid core plaque (arrow), site of potential rupture and thrombosis. Hematoxylin-eosin, 2.5×.

Histological section of the second centimeter of the anterior interventricular artery showing large lipid-core atherosclerotic plaque with ruptured area (arrows) and occlusive luminal thrombosis (asterisk). Hematoxylin-eosin, 2.5×.
The lungs weighed 1,208 g together and showed alveolar edema. The kidneys showed irregular surface and retention cysts, with hyaline arteriolosclerosis on histological examination. The aorta showed mild / moderate degree of atherosclerosis. (Dr. Luiz Alberto Benvenuti)
Anatomopathological diagnoses. Coronary atherosclerosis; acute myocardial infarction involving the left ventricular anterosseptal wall and the right ventricular anterior wall; rupture of the ventricular septum, with VSD; acute pulmonary edema (cause of death) (Dr. Luiz Alberto Benvenuti) .
This is the case report of a 66-year-old man with systemic hypertension and a chronic smoker that presented with acute severe chest pain. After medical assessment, he was diagnosed with acute myocardial infarction and the patient underwent coronary angiography, which disclosed proximal occlusion of the left anterior descending artery with images suggesting the presence of thrombi. He was submitted to balloon-angioplasty in the affected segment without restoration of distal coronary flow (unsuccessful procedure) and the patient developed irreversible cardiac arrest and died.
The autopsy confirmed acute myocardial infarction, which was very extensive, affecting the left ventricular anterosseptal wall and the right ventricular anterior wall. Histological dating was 24-48 hours of onset, consistent with the clinical history. It is noteworthy the fact that the detailed examination of the ventricular septum showed the presence of two previous microinfarctions, an old (healed) one and an ongoing one.
The presence of atherosclerosis of the coronary arteries was identified, with massive plaques in the proximal segment of the left anterior descending artery, which resulted in chronic obstruction of 80% of the lumen. The fatty plaques had extensive lipid cores and there were areas of marked thinning of the fibrous cap that covered the cores, as well as areas of rupture associated with acute thrombosis of the remaining lumen in the first two centimeters of the left anterior descending artery. It is known that acute coronary occlusions with luminal thrombosis are usually associated with large lipid-core plaques, which undergo rupture due to the instability of their thin fibrous cap 7 , as observed in this case.
Aside from the great extent of the infarcted area, the patient developed an important mechanical complication of acute myocardial infarction, the occurrence of ventricular septal rupture with the establishment of VSD 8 - which certainly aggravated his hemodynamic condition, progressing to cardiogenic shock -, acute pulmonary edema and death. It should be emphasized that the patient had two classic risk factors for atherosclerosis and myocardial infarction: systemic hypertension and chronic smoking 9 . (Dr. Luiz Alberto Benvenuti)
Section Editor: Alfredo José Mansur ( rb.psu.rocni@rusnamja )
Associated Editors: Desidério Favarato ( rb.psu.rocni@otaravaflcd )
Vera Demarchi Aiello ( rb.psu.rocni@arevpna )

IMAGES
VIDEO
COMMENTS
ED treatment. Internal STEMI Code paged at 22:55 Patient arrived at 22:57 Interventions Chest X‐Ray Assessment Repeat 12 Lead EKG. 5,000 Units IV Heparin. ED treatment. 22:05 (8 minutes after arrival) Compressions started Defibrillated at 150 J. ED treatment. 18 minutes in ED. Interventions Continued 180 mg ticagrelor Patient undressed ...
On examination, the temperature was 36.4°C, the heart rate 103 beats per minute, the blood pressure 79/51 mm Hg, the respiratory rate 30 breaths per minute, and the oxygen saturation 99% while ...
Here is a case presentation in cardiology for educational purpose for young cardiologist, emergency physicians and internists. ... Powerpoint final case study presentation. ... Case presentation heart failure.
Congestive Heart Failure Case Presentation. May 21, 2017 •. 119 likes • 44,063 views. Walaa Fahad. This is A case Study of Congestive Heart Failure, Feel free to use it and sorry for any English mistakes. Health & Medicine. 1 of 44. Congestive Heart Failure Case Presentation - Download as a PDF or view online for free.
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by ...
Free Google Slides theme and PowerPoint template. Research on cardiovascular diseases is key to improving our life expectancy. It's important to have a close look at different cardiology clinical cases to learn more about heart attacks, strokes…. Show the results of your latest case reports with this and 100% editable presentation!
Care of Patients with Cardiac Problems - Case Study. The nurse is performing an admission assessment for Mr. Glenn, a 78-year-old man with a history of cardiovascular disease and hypertension. He takes 20 mg of furosemide and 5 mg of Zestril po daily. He was seen in the physician's office today reporting swelling in his feet, shortness of ...
Patient Presentation. Mr. Smith is a 60-year-old Caucasian male, who presents with 8/10 chest pain after working out. He just quit smoking and started a new workout and diet program after recently retiring. He has noticed some chest and shoulder discomfort with working out that usually resolves with rest, but decided to come to the emergency ...
Read chapter 5 of Patient Management in the Telemetry/Cardiac Step-Down Unit: A Case-Based Approach online now, exclusively on AccessMedicine. AccessMedicine is a subscription-based resource from McGraw Hill that features trusted medical content from the best minds in medicine.
Presentation on theme: "Case study 1: acute myocardial infarction"— Presentation transcript: 1 Case study 1: ... Myocardial Infarction or Heart Attack Occurs when blood flow to part of the heart is blocked resulting in damage or death to the muscle Usually caused by a blood clot or plaque formation blocking the coronary artery, ...
Premium Google Slides theme, PowerPoint template, and Canva presentation template. Clinical cases help medical investigators and students to better understand diseases, their causes and treatments. For instance, keeping track of a patient with a heart disease can help future patients find a cure faster and more efficiently. But you need a ...
Presentation Transcript. Unfolding cardiac case study With live role play. The patient • Mr. Smith • 55 years old • CC: blurry vision that started several months ago and has worsened recently • PMH: no medical history. Has not seen a PCP in years because he feels fine and doesn't think there is a need.
Read chapter 4 of Patient Management in the Telemetry/Cardiac Step-Down Unit: A Case-Based Approach online now, exclusively on AccessCardiology. AccessCardiology is a subscription-based resource from McGraw Hill that features trusted medical content from the best minds in medicine.
AI-enhanced description. R. Ratheeshkrishnakripa. Cardiac arrest refers to the sudden cessation of cardiac activity and can lead to death if not treated. It is usually caused by conditions that disrupt the heart's electrical system such as coronary artery disease or structural heart abnormalities. Risk factors include a family history of sudden ...
The document presents a case study of a 6-year-old male child diagnosed with rheumatic heart disease. It includes details of the patient's identification, history, family history, physical examination findings, and diagnosis of mitral regurgitation resulting from rheumatic fever. The patient presented with complaints of chest pain, fatigue, and reduced activity over the past 2 years ...
Slide 1-. Congestive Heart Failure Case Study. Slide 2-. Congestive Heart Failure. Slide 3-. Congestive Heart Failure. Slide 4-. Congestive Heart Failure Impaired cardiac pumping Ventricular dysfunction Heart remodeling Reduced exercise tolerance Diminished quality of life Shortened life expectancy Associated with CAD and HTN.
Free Google Slides theme, PowerPoint template, and Canva presentation template. When presenting a clinical case, try giving a little more visual appeal to your slides, like we do in this template. The illustrations come from Stories by Freepik and the layouts are geometric. Treatment, diagnosis, recommendations, references, anything is ...
Case Presentation: A Patient Presenting With Cardiac Arrest. Presenter: Michael Mooney. October 31, 2016. REGISTER for free or LOG IN to view this content. Coronary. Presentation. TCT 2016. ACS/AMI. Up Next. Presentation TCT 2016. TAVR for Intermediate-Risk and Low-Risk Patients: Review of the Literature.
Title: Cardiac Case Study. Description: For more information on GE Nuclear Cardiology products and the unique Hawkeye CT ... the American Society of Nuclear Cardiology and the Society of Nuclear Medicine. ... - PowerPoint PPT presentation. Number of Views: 805. Avg rating:3.0/5.0. Slides: 15.
Presentation Transcript. Cardiac Case Study Inferior wall attenuation and correction with CT-based Attenuation Correction Linda Campbell, BS GE Applications Scientist. Type of acquisition Time per stop Agent Dose Rest Ungated SPECT; CT 25 seconds 99m Tc Sestamibi 15 mCi Stress Gated SPECT; CT 25 seconds 99m Tc Sestamibi 30 mCi Patient History A ...
Please use our template to prepare a slideshow with a clinical case about cardiac arrest. The color palette contains gray and red, the latter due to being associated with hearts, and these colors appear in the form of gradients. There are other editable resources so that your data appears on the screen in the clearest way possible.
The electrocardiographic findings commonly observed in cardiac tamponade are low voltage and electrical alternans of the QRS complex, observed in the case. Although physical examination made no reference to clinical findings suggestive of tamponade, such as jugular stasis or muffled heart sounds, we cannot exclude this diagnostic hypothesis.
ChefBoulder13938. 4/30/2024. Cardiac Case Presentation December 2021 Erica Erck RN BSN, Cardiac Coordinator FINANCIAL DISCLOSURE: No relevant financial relationship exists. • 43 year old male • No significant past medical history • No daily medication • No recent surgery • Does not use drugs • Nonsmoker, does use chewing tobacco 1 ...