- About Project
- Testimonials

Business Management Ideas

Essay on Obesity
List of essays on obesity, essay on obesity – short essay (essay 1 – 150 words), essay on obesity (essay 2 – 250 words), essay on obesity – written in english (essay 3 – 300 words), essay on obesity – for school students (class 5, 6, 7, 8, 9, 10, 11 and 12 standard) (essay 4 – 400 words), essay on obesity – for college students (essay 5 – 500 words), essay on obesity – with causes and treatment (essay 6 – 600 words), essay on obesity – for science students (essay 7 – 750 words), essay on obesity – long essay for medical students (essay 8 – 1000 words).
Obesity is a chronic health condition in which the body fat reaches abnormal level. Obesity occurs when we consume much more amount of food than our body really needs on a daily basis. In other words, when the intake of calories is greater than the calories we burn out, it gives rise to obesity.
Audience: The below given essays are exclusively written for school students (Class 5, 6, 7, 8, 9, 10, 11 and 12 Standard), college, science and medical students.
Introduction:
Obesity means being excessively fat. A person would be said to be obese if his or her body mass index is beyond 30. Such a person has a body fat rate that is disproportionate to his body mass.
Obesity and the Body Mass Index:
The body mass index is calculated considering the weight and height of a person. Thus, it is a scientific way of determining the appropriate weight of any person. When the body mass index of a person indicates that he or she is obese, it exposes the person to make health risk.
Stopping Obesity:
There are two major ways to get the body mass index of a person to a moderate rate. The first is to maintain a strict diet. The second is to engage in regular physical exercise. These two approaches are aimed at reducing the amount of fat in the body.
Conclusion:
Obesity can lead to sudden death, heart attack, diabetes and may unwanted illnesses. Stop it by making healthy choices.
Obesity has become a big concern for the youth of today’s generation. Obesity is defined as a medical condition in which an individual gains excessive body fat. When the Body Mass Index (BMI) of a person is over 30, he/ she is termed as obese.
Obesity can be a genetic problem or a disorder that is caused due to unhealthy lifestyle habits of a person. Physical inactivity and the environment in which an individual lives, are also the factors that leads to obesity. It is also seen that when some individuals are in stress or depression, they start cultivating unhealthy eating habits which eventually leads to obesity. Medications like steroids is yet another reason for obesity.
Obesity has several serious health issues associated with it. Some of the impacts of obesity are diabetes, increase of cholesterol level, high blood pressure, etc. Social impacts of obesity includes loss of confidence in an individual, lowering of self-esteem, etc.
The risks of obesity needs to be prevented. This can be done by adopting healthy eating habits, doing some physical exercise regularly, avoiding stress, etc. Individuals should work on weight reduction in order to avoid obesity.
Obesity is indeed a health concern and needs to be prioritized. The management of obesity revolves around healthy eating habits and physical activity. Obesity, if not controlled in its initial stage can cause many severe health issues. So it is wiser to exercise daily and maintain a healthy lifestyle rather than being the victim of obesity.
Obesity can be defined as the clinical condition where accumulation of excessive fat takes place in the adipose tissue leading to worsening of health condition. Usually, the fat is deposited around the trunk and also the waist of the body or even around the periphery.
Obesity is actually a disease that has been spreading far and wide. It is preventable and certain measures are to be taken to curb it to a greater extend. Both in the developing and developed countries, obesity has been growing far and wide affecting the young and the old equally.
The alarming increase in obesity has resulted in stimulated death rate and health issues among the people. There are several methods adopted to lose weight and they include different diet types, physical activity and certain changes in the current lifestyle. Many of the companies are into minting money with the concept of inviting people to fight obesity.
In patients associated with increased risk factor related to obesity, there are certain drug therapies and other procedures adopted to lose weight. There are certain cost effective ways introduced by several companies to enable clinic-based weight loss programs.
Obesity can lead to premature death and even cause Type 2 Diabetes Mellitus. Cardiovascular diseases have also become the part and parcel of obese people. It includes stroke, hypertension, gall bladder disease, coronary heart disease and even cancers like breast cancer, prostate cancer, endometrial cancer and colon cancer. Other less severe arising due to obesity includes osteoarthritis, gastro-esophageal reflux disease and even infertility.
Hence, serious measures are to be taken to fight against this dreadful phenomenon that is spreading its wings far and wide. Giving proper education on benefits of staying fit and mindful eating is as important as curbing this issue. Utmost importance must be given to healthy eating habits right from the small age so that they follow the same until the end of their life.
Obesity is majorly a lifestyle disease attributed to the extra accumulation of fat in the body leading to negative health effects on a person. Ironically, although prevalent at a large scale in many countries, including India, it is one of the most neglect health problems. It is more often ignored even if told by the doctor that the person is obese. Only when people start acquiring other health issues such as heart disease, blood pressure or diabetes, they start taking the problem of obesity seriously.
Obesity Statistics in India:
As per a report, India happens to figure as the third country in the world with the most obese people. This should be a troubling fact for India. However, we are yet to see concrete measures being adopted by the people to remain fit.
Causes of Obesity:
Sedentary lifestyle, alcohol, junk food, medications and some diseases such as hypothyroidism are considered as the factors which lead to obesity. Even children seem to be glued to televisions, laptops and video games which have taken away the urge for physical activities from them. Adding to this, the consumption of junk food has further aggravated the growing problem of obesity in children.
In the case of adults, most of the professions of today make use of computers which again makes people sit for long hours in one place. Also, the hectic lifestyle of today makes it difficult for people to spare time for physical activities and people usually remain stressed most of the times. All this has contributed significantly to the rise of obesity in India.
Obesity and BMI:
Body Mass Index (BMI) is the measure which allows a person to calculate how to fit he or she is. In other words, the BMI tells you if you are obese or not. BMI is calculated by dividing the weight of a person in kg with the square of his / her height in metres. The number thus obtained is called the BMI. A BMI of less than 25 is considered optimal. However, if a person has a BMI over 30 he/she is termed as obese.
What is a matter of concern is that with growing urbanisation there has been a rapid increase of obese people in India? It is of utmost importance to consider this health issue a serious threat to the future of our country as a healthy body is important for a healthy soul. We should all be mindful of what we eat and what effect it has on our body. It is our utmost duty to educate not just ourselves but others as well about this serious health hazard.
Obesity can be defined as a condition (medical) that is the accumulation of body fat to an extent that the excess fat begins to have a lot of negative effects on the health of the individual. Obesity is determined by examining the body mass index (BMI) of the person. The BMI is gotten by dividing the weight of the person in kilogram by the height of the person squared.
When the BMI of a person is more than 30, the person is classified as being obese, when the BMI falls between 25 and 30, the person is said to be overweight. In a few countries in East Asia, lower values for the BMI are used. Obesity has been proven to influence the likelihood and risk of many conditions and disease, most especially diabetes of type 2, cardiovascular diseases, sleeplessness that is obstructive, depression, osteoarthritis and some cancer types.
In most cases, obesity is caused through a combination of genetic susceptibility, a lack of or inadequate physical activity, excessive intake of food. Some cases of obesity are primarily caused by mental disorder, medications, endocrine disorders or genes. There is no medical data to support the fact that people suffering from obesity eat very little but gain a lot of weight because of slower metabolism. It has been discovered that an obese person usually expends much more energy than other people as a result of the required energy that is needed to maintain a body mass that is increased.
It is very possible to prevent obesity with a combination of personal choices and social changes. The major treatments are exercising and a change in diet. We can improve the quality of our diet by reducing our consumption of foods that are energy-dense like those that are high in sugars or fat and by trying to increase our dietary fibre intake.
We can also accompany the appropriate diet with the use of medications to help in reducing appetite and decreasing the absorption of fat. If medication, exercise and diet are not yielding any positive results, surgery or gastric balloon can also be carried out to decrease the volume of the stomach and also reduce the intestines’ length which leads to the feel of the person get full early or a reduction in the ability to get and absorb different nutrients from a food.
Obesity is the leading cause of ill-health and death all over the world that is preventable. The rate of obesity in children and adults has drastically increased. In 2015, a whopping 12 percent of adults which is about 600 million and about 100 million children all around the world were found to be obese.
It has also been discovered that women are more obese than men. A lot of government and private institutions and bodies have stated that obesity is top of the list of the most difficult and serious problems of public health that we have in the world today. In the world we live today, there is a lot of stigmatisation of obese people.
We all know how troubling the problem of obesity truly is. It is mainly a form of a medical condition wherein the body tends to accumulate excessive fat which in turn has negative repercussions on the health of an individual.
Given the current lifestyle and dietary style, it has become more common than ever. More and more people are being diagnosed with obesity. Such is its prevalence that it has been termed as an epidemic in the USA. Those who suffer from obesity are at a much higher risk of diabetes, heart diseases and even cancer.
In order to gain a deeper understanding of obesity, it is important to learn what the key causes of obesity are. In a layman term, if your calorie consumption exceeds what you burn because of daily activities and exercises, it is likely to lead to obesity. It is caused over a prolonged period of time when your calorie intake keeps exceeding the calories burned.
Here are some of the key causes which are known to be the driving factors for obesity.
If your diet tends to be rich in fat and contains massive calorie intake, you are all set to suffer from obesity.
Sedentary Lifestyle:
With most people sticking to their desk jobs and living a sedentary lifestyle, the body tends to get obese easily.
Of course, the genetic framework has a lot to do with obesity. If your parents are obese, the chance of you being obese is quite high.
The weight which women gain during their pregnancy can be very hard to shed and this is often one of the top causes of obesity.
Sleep Cycle:
If you are not getting an adequate amount of sleep, it can have an impact on the hormones which might trigger hunger signals. Overall, these linked events tend to make you obese.
Hormonal Disorder:
There are several hormonal changes which are known to be direct causes of obesity. The imbalance of the thyroid stimulating hormone, for instance, is one of the key factors when it comes to obesity.
Now that we know the key causes, let us look at the possible ways by which you can handle it.
Treatment for Obesity:
As strange as it may sound, the treatment for obesity is really simple. All you need to do is follow the right diet and back it with an adequate amount of exercise. If you can succeed in doing so, it will give you the perfect head-start into your journey of getting in shape and bidding goodbye to obesity.
There are a lot of different kinds and styles of diet plans for obesity which are available. You can choose the one which you deem fit. We recommend not opting for crash dieting as it is known to have several repercussions and can make your body terribly weak.
The key here is to stick to a balanced diet which can help you retain the essential nutrients, minerals, and, vitamins and shed the unwanted fat and carbs.
Just like the diet, there are several workout plans for obesity which are available. It is upon you to find out which of the workout plan seems to be apt for you. Choose cardio exercises and dance routines like Zumba to shed the unwanted body weight. Yoga is yet another method to get rid of obesity.
So, follow a blend of these and you will be able to deal with the trouble of obesity in no time. We believe that following these tips will help you get rid of obesity and stay in shape.
Obesity and overweight is a top health concern in the world due to the impact it has on the lives of individuals. Obesity is defined as a condition in which an individual has excessive body fat and is measured using the body mass index (BMI) such that, when an individual’s BMI is above 30, he or she is termed obese. The BMI is calculated using body weight and height and it is different for all individuals.
Obesity has been determined as a risk factor for many diseases. It results from dietary habits, genetics, and lifestyle habits including physical inactivity. Obesity can be prevented so that individuals do not end up having serious complications and health problems. Chronic illnesses like diabetes, heart diseases and relate to obesity in terms of causes and complications.
Factors Influencing Obesity:
Obesity is not only as a result of lifestyle habits as most people put it. There are other important factors that influence obesity. Genetics is one of those factors. A person could be born with genes that predispose them to obesity and they will also have difficulty in losing weight because it is an inborn factor.
The environment also influences obesity because the diet is similar in certain environs. In certain environments, like school, the food available is fast foods and the chances of getting healthy foods is very low, leading to obesity. Also, physical inactivity is an environmental factor for obesity because some places have no fields or tracks where people can jog or maybe the place is very unsafe and people rarely go out to exercise.
Mental health affects the eating habits of individuals. There is a habit of stress eating when a person is depressed and it could result in overweight or obesity if the person remains unhealthy for long period of time.
The overall health of individuals also matter. If a person is unwell and is prescribed with steroids, they may end up being obese. Steroidal medications enable weight gain as a side effect.
Complications of Obesity:
Obesity is a health concern because its complications are severe. Significant social and health problems are experienced by obese people. Socially, they will be bullied and their self-esteem will be low as they will perceive themselves as unworthy.
Chronic illnesses like diabetes results from obesity. Diabetes type 2 has been directly linked to obesity. This condition involves the increased blood sugars in the body and body cells are not responding to insulin as they should. The insulin in the body could also be inadequate due to decreased production. High blood sugar concentrations result in symptoms like frequent hunger, thirst and urination. The symptoms of complicated stages of diabetes type 2 include loss of vision, renal failure and heart failure and eventually death. The importance of having a normal BMI is the ability of the body to control blood sugars.
Another complication is the heightened blood pressures. Obesity has been defined as excessive body fat. The body fat accumulates in blood vessels making them narrow. Narrow blood vessels cause the blood pressures to rise. Increased blood pressure causes the heart to start failing in its physiological functions. Heart failure is the end result in this condition of increased blood pressures.
There is a significant increase in cholesterol in blood of people who are obese. High blood cholesterol levels causes the deposition of fats in various parts of the body and organs. Deposition of fats in the heart and blood vessels result in heart diseases. There are other conditions that result from hypercholesterolemia.
Other chronic illnesses like cancer can also arise from obesity because inflammation of body cells and tissues occurs in order to store fats in obese people. This could result in abnormal growths and alteration of cell morphology. The abnormal growths could be cancerous.
Management of Obesity:
For the people at risk of developing obesity, prevention methods can be implemented. Prevention included a healthy diet and physical activity. The diet and physical activity patterns should be regular and realizable to avoid strains that could result in complications.
Some risk factors for obesity are non-modifiable for example genetics. When a person in genetically predisposed, the lifestyle modifications may be have help.
For the individuals who are already obese, they can work on weight reduction through healthy diets and physical exercises.
In conclusion, obesity is indeed a major health concern because the health complications are very serious. Factors influencing obesity are both modifiable and non-modifiable. The management of obesity revolves around diet and physical activity and so it is important to remain fit.
In olden days, obesity used to affect only adults. However, in the present time, obesity has become a worldwide problem that hits the kids as well. Let’s find out the most prevalent causes of obesity.
Factors Causing Obesity:
Obesity can be due to genetic factors. If a person’s family has a history of obesity, chances are high that he/ she would also be affected by obesity, sooner or later in life.
The second reason is having a poor lifestyle. Now, there are a variety of factors that fall under the category of poor lifestyle. An excessive diet, i.e., eating more than you need is a definite way to attain the stage of obesity. Needless to say, the extra calories are changed into fat and cause obesity.
Junk foods, fried foods, refined foods with high fats and sugar are also responsible for causing obesity in both adults and kids. Lack of physical activity prevents the burning of extra calories, again, leading us all to the path of obesity.
But sometimes, there may also be some indirect causes of obesity. The secondary reasons could be related to our mental and psychological health. Depression, anxiety, stress, and emotional troubles are well-known factors of obesity.
Physical ailments such as hypothyroidism, ovarian cysts, and diabetes often complicate the physical condition and play a massive role in abnormal weight gain.
Moreover, certain medications, such as steroids, antidepressants, and contraceptive pills, have been seen interfering with the metabolic activities of the body. As a result, the long-term use of such drugs can cause obesity. Adding to that, regular consumption of alcohol and smoking are also connected to the condition of obesity.
Harmful Effects of Obesity:
On the surface, obesity may look like a single problem. But, in reality, it is the mother of several major health issues. Obesity simply means excessive fat depositing into our body including the arteries. The drastic consequence of such high cholesterol levels shows up in the form of heart attacks and other life-threatening cardiac troubles.
The fat deposition also hampers the elasticity of the arteries. That means obesity can cause havoc in our body by altering the blood pressure to an abnormal range. And this is just the tip of the iceberg. Obesity is known to create an endless list of problems.
In extreme cases, this disorder gives birth to acute diseases like diabetes and cancer. The weight gain due to obesity puts a lot of pressure on the bones of the body, especially of the legs. This, in turn, makes our bones weak and disturbs their smooth movement. A person suffering from obesity also has higher chances of developing infertility issues and sleep troubles.
Many obese people are seen to be struggling with breathing problems too. In the chronic form, the condition can grow into asthma. The psychological effects of obesity are another serious topic. You can say that obesity and depression form a loop. The more a person is obese, the worse is his/ her depression stage.
How to Control and Treat Obesity:
The simplest and most effective way, to begin with, is changing our diet. There are two factors to consider in the diet plan. First is what and what not to eat. Second is how much to eat.
If you really want to get rid of obesity, include more and more green vegetables in your diet. Spinach, beans, kale, broccoli, cauliflower, asparagus, etc., have enough vitamins and minerals and quite low calories. Other healthier options are mushrooms, pumpkin, beetroots, and sweet potatoes, etc.
Opt for fresh fruits, especially citrus fruits, and berries. Oranges, grapes, pomegranate, pineapple, cherries, strawberries, lime, and cranberries are good for the body. They have low sugar content and are also helpful in strengthening our immune system. Eating the whole fruits is a more preferable way in comparison to gulping the fruit juices. Fruits, when eaten whole, have more fibers and less sugar.
Consuming a big bowl of salad is also great for dealing with the obesity problem. A salad that includes fibrous foods such as carrots, radish, lettuce, tomatoes, works better at satiating the hunger pangs without the risk of weight gain.
A high protein diet of eggs, fish, lean meats, etc., is an excellent choice to get rid of obesity. Take enough of omega fatty acids. Remember to drink plenty of water. Keeping yourself hydrated is a smart way to avoid overeating. Water also helps in removing the toxins and excess fat from the body.
As much as possible, avoid fats, sugars, refined flours, and oily foods to keep the weight in control. Control your portion size. Replace the three heavy meals with small and frequent meals during the day. Snacking on sugarless smoothies, dry fruits, etc., is much recommended.
Regular exercise plays an indispensable role in tackling the obesity problem. Whenever possible, walk to the market, take stairs instead of a lift. Physical activity can be in any other form. It could be a favorite hobby like swimming, cycling, lawn tennis, or light jogging.
Meditation and yoga are quite powerful practices to drive away the stress, depression and thus, obesity. But in more serious cases, meeting a physician is the most appropriate strategy. Sometimes, the right medicines and surgical procedures are necessary to control the health condition.
Obesity is spreading like an epidemic, haunting both the adults and the kids. Although genetic factors and other physical ailments play a role, the problem is mostly caused by a reckless lifestyle.
By changing our way of living, we can surely take control of our health. In other words, it would be possible to eliminate the condition of obesity from our lives completely by leading a healthy lifestyle.
Health , Obesity
Get FREE Work-at-Home Job Leads Delivered Weekly!

Join more than 50,000 subscribers receiving regular updates! Plus, get a FREE copy of How to Make Money Blogging!
Message from Sophia!
Like this post? Don’t forget to share it!
Here are a few recommended articles for you to read next:
- Essay on Cleanliness
- Essay on Cancer
- Essay on AIDS
- Essay on Health and Fitness
No comments yet.
Leave a reply click here to cancel reply..
You must be logged in to post a comment.
Billionaires
- Donald Trump
- Warren Buffett
- Email Address
- Free Stock Photos
- Keyword Research Tools
- URL Shortener Tools
- WordPress Theme
Book Summaries
- How To Win Friends
- Rich Dad Poor Dad
- The Code of the Extraordinary Mind
- The Luck Factor
- The Millionaire Fastlane
- The ONE Thing
- Think and Grow Rich
- 100 Million Dollar Business
- Business Ideas
Digital Marketing
- Mobile Addiction
- Social Media Addiction
- Computer Addiction
- Drug Addiction
- Internet Addiction
- TV Addiction
- Healthy Habits
- Morning Rituals
- Wake up Early
- Cholesterol
- Reducing Cholesterol
- Fat Loss Diet Plan
- Reducing Hair Fall
- Sleep Apnea
- Weight Loss
Internet Marketing
- Email Marketing
Law of Attraction
- Subconscious Mind
- Vision Board
- Visualization
Law of Vibration
- Professional Life
Motivational Speakers
- Bob Proctor
- Robert Kiyosaki
- Vivek Bindra
- Inner Peace
Productivity
- Not To-do List
- Project Management Software
- Negative Energies
Relationship
- Getting Back Your Ex
Self-help 21 and 14 Days Course
Self-improvement.
- Body Language
- Complainers
- Emotional Intelligence
- Personality
Social Media
- Project Management
- Anik Singal
- Baba Ramdev
- Dwayne Johnson
- Jackie Chan
- Leonardo DiCaprio
- Narendra Modi
- Nikola Tesla
- Sachin Tendulkar
- Sandeep Maheshwari
- Shaqir Hussyin
Website Development
Wisdom post, worlds most.
- Expensive Cars
Our Portals: Gulf Canada USA Italy Gulf UK
Privacy Overview
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
Obesity Essay
Last updated on: Feb 9, 2023
Obesity Essay: A Complete Guide and Topics
By: Nova A.
11 min read
Reviewed By: Jacklyn H.
Published on: Aug 31, 2021

Are you assigned to write an essay about obesity? The first step is to define obesity.
The obesity epidemic is a major issue facing our country right now. It's complicated- it could be genetic or due to your environment, but either way, there are ways that you can fix it!
Learn all about what causes weight gain and get tips on how you can get healthy again.

On this Page
What is Obesity
What is obesity? Obesity and BMI (body mass index) are both tools of measurement that are used by doctors to assess body fat according to the height, age, and gender of a person. If the BMI is between 25 to 29.9, that means the person has excess weight and body fat.
If the BMI exceeds 30, that means the person is obese. Obesity is a condition that increases the risk of developing cardiovascular diseases, high blood pressure, and other medical conditions like metabolic syndrome, arthritis, and even some types of cancer.
Obesity Definition
Obesity is defined by the World Health Organization as an accumulation of abnormal and excess body fat that comes with several risk factors. It is measured by the body mass index BMI, body weight (in kilograms) divided by the square of a person’s height (in meters).
Obesity in America
Obesity is on the verge of becoming an epidemic as 1 in every 3 Americans can be categorized as overweight and obese. Currently, America is an obese country, and it continues to get worse.

Paper Due? Why Suffer? That's our Job!
Causes of obesity
Do you see any obese or overweight people around you?
You likely do.
This is because fast-food chains are becoming more and more common, people are less active, and fruits and vegetables are more expensive than processed foods, thus making them less available to the majority of society. These are the primary causes of obesity.
Obesity is a disease that affects all age groups, including children and elderly people.
Now that you are familiar with the topic of obesity, writing an essay won’t be that difficult for you.
How to Write an Obesity Essay
The format of an obesity essay is similar to writing any other essay. If you need help regarding how to write an obesity essay, it is the same as writing any other essay.
Obesity Essay Introduction
The trick is to start your essay with an interesting and catchy sentence. This will help attract the reader's attention and motivate them to read further. You don’t want to lose the reader’s interest in the beginning and leave a bad impression, especially if the reader is your teacher.
A hook sentence is usually used to open the introductory paragraph of an essay in order to make it interesting. When writing an essay on obesity, the hook sentence can be in the form of an interesting fact or statistic.
Head on to this detailed article on hook examples to get a better idea.
Once you have hooked the reader, the next step is to provide them with relevant background information about the topic. Don’t give away too much at this stage or bombard them with excess information that the reader ends up getting bored with. Only share information that is necessary for the reader to understand your topic.
Next, write a strong thesis statement at the end of your essay, be sure that your thesis identifies the purpose of your essay in a clear and concise manner. Also, keep in mind that the thesis statement should be easy to justify as the body of your essay will revolve around it.
Body Paragraphs
The details related to your topic are to be included in the body paragraphs of your essay. You can use statistics, facts, and figures related to obesity to reinforce your thesis throughout your essay.
If you are writing a cause-and-effect obesity essay, you can mention different causes of obesity and how it can affect a person’s overall health. The number of body paragraphs can increase depending on the parameters of the assignment as set forth by your instructor.
Start each body paragraph with a topic sentence that is the crux of its content. It is necessary to write an engaging topic sentence as it helps grab the reader’s interest. Check out this detailed blog on writing a topic sentence to further understand it.
End your essay with a conclusion by restating your research and tying it to your thesis statement. You can also propose possible solutions to control obesity in your conclusion. Make sure that your conclusion is short yet powerful.
Obesity Essay Examples
Essay about Obesity (PDF)
Childhood Obesity Essay (PDF)
Obesity in America Essay (PDF)
Essay about Obesity Cause and Effects (PDF)
Satire Essay on Obesity (PDF)
Obesity Argumentative Essay (PDF)
Obesity Essay Topics
Choosing a topic might seem an overwhelming task as you may have many ideas for your assignment. Brainstorm different ideas and narrow them down to one, quality topic.
If you need some examples to help you with your essay topic related to obesity, dive into this article and choose from the list of obesity essay topics.
Childhood Obesity
As mentioned earlier, obesity can affect any age group, including children. Obesity can cause several future health problems as children age.
Here are a few topics you can choose from and discuss for your childhood obesity essay:
- What are the causes of increasing obesity in children?
- Obese parents may be at risk for having children with obesity.
- What is the ratio of obesity between adults and children?
- What are the possible treatments for obese children?
- Are there any social programs that can help children with combating obesity?
- Has technology boosted the rate of obesity in children?
- Are children spending more time on gadgets instead of playing outside?
- Schools should encourage regular exercises and sports for children.
- How can sports and other physical activities protect children from becoming obese?
- Can childhood abuse be a cause of obesity among children?
- What is the relationship between neglect in childhood and obesity in adulthood?
- Does obesity have any effect on the psychological condition and well-being of a child?
- Are electronic medical records effective in diagnosing obesity among children?
- Obesity can affect the academic performance of your child.
- Do you believe that children who are raised by a single parent can be vulnerable to obesity?
- You can promote interesting exercises to encourage children.
- What is the main cause of obesity, and why is it increasing with every passing day?
- Schools and colleges should work harder to develop methodologies to decrease childhood obesity.
- The government should not allow schools and colleges to include sweet or fatty snacks as a part of their lunch.
- If a mother is obese, can it affect the health of the child?
- Children who gain weight frequently can develop chronic diseases.
Obesity Argumentative Essay Topics
Do you want to write an argumentative essay on the topic of obesity?
The following list can help you with that!
Here are some examples you can choose from for your argumentative essay about obesity:
- Can vegetables and fruits decrease the chances of obesity?
- Should you go for surgery to overcome obesity?
- Are there any harmful side effects?
- Can obesity be related to the mental condition of an individual?
- Are parents responsible for controlling obesity in childhood?
- What are the most effective measures to prevent the increase in the obesity rate?
- Why is the obesity rate increasing in the United States?
- Can the lifestyle of a person be a cause of obesity?
- Does the economic situation of a country affect the obesity rate?
- How is obesity considered an international health issue?
- Can technology and gadgets affect obesity rates?
- What can be the possible reasons for obesity in a school?
- How can we address the issue of obesity?
- Is obesity a chronic disease?
- Is obesity a major cause of heart attacks?
- Are the junk food chains causing an increase in obesity?
- Do nutritional programs help in reducing the obesity rate?
- How can the right type of diet help with obesity?
- Why should we encourage sports activities in schools and colleges?
- Can obesity affect a person’s behavior?
Health Related Topics for Research Paper
If you are writing a research paper, you can explain the cause and effect of obesity.
Here are a few topics that link to the cause and effects of obesity.Review the literature of previous articles related to obesity. Describe the ideas presented in the previous papers.
- Can family history cause obesity in future generations?
- Can we predict obesity through genetic testing?
- What is the cause of the increasing obesity rate?
- Do you think the increase in fast-food restaurants is a cause of the rising obesity rate?
- Is the ratio of obese women greater than obese men?
- Why are women more prone to be obese as compared to men?
- Stress can be a cause of obesity. Mention the reasons how mental health can be related to physical health.
- Is urban life a cause of the increasing obesity rate?
- People from cities are prone to be obese as compared to people from the countryside.
- How obesity affects the life expectancy of people? What are possible solutions to decrease the obesity rate?
- Do family eating habits affect or trigger obesity?
- How do eating habits affect the health of an individual?
- How can obesity affect the future of a child?
- Obese children are more prone to get bullied in high school and college.
- Why should schools encourage more sports and exercise for children?
Tough Essay Due? Hire Tough Writers!
Topics for Essay on Obesity as a Problem
Do you think a rise in obesity rate can affect the economy of a country?
Here are some topics for your assistance regarding your economics related obesity essay.
- Does socioeconomic status affect the possibility of obesity in an individual?
- Analyze the film and write a review on “Fed Up” – an obesity epidemic.
- Share your reviews on the movie “The Weight of The Nation.”
- Should we increase the prices of fast food and decrease the prices of fruits and vegetables to decrease obesity?
- Do you think healthy food prices can be a cause of obesity?
- Describe what measures other countries have taken in order to control obesity?
- The government should play an important role in controlling obesity. What precautions should they take?
- Do you think obesity can be one of the reasons children get bullied?
- Do obese people experience any sort of discrimination or inappropriate behavior due to their weight?
- Are there any legal protections for people who suffer from discrimination due to their weight?
- Which communities have a higher percentage of obesity in the United States?
- Discuss the side effects of the fast-food industry and their advertisements on children.
- Describe how the increasing obesity rate has affected the economic condition of the United States.
- What is the current percentage of obesity all over the world? Is the obesity rate increasing with every passing day?
- Why is the obesity rate higher in the United States as compared to other countries?
- Do Asians have a greater percentage of obese people as compared to Europe?
- Does the cultural difference affect the eating habits of an individual?
- Obesity and body shaming.
- Why is a skinny body considered to be ideal? Is it an effective way to reduce the obesity rate?
Obesity Solution Essay Topics
With all the developments in medicine and technology, we still don’t have exact measures to treat obesity.
Here are some insights you can discuss in your essay:
- How do obese people suffer from metabolic complications?
- Describe the fat distribution in obese people.
- Is type 2 diabetes related to obesity?
- Are obese people more prone to suffer from diabetes in the future?
- How are cardiac diseases related to obesity?
- Can obesity affect a woman’s childbearing time phase?
- Describe the digestive diseases related to obesity.
- Obesity may be genetic.
- Obesity can cause a higher risk of suffering a heart attack.
- What are the causes of obesity? What health problems can be caused if an individual suffers from obesity?
- What are the side effects of surgery to overcome obesity?
- Which drugs are effective when it comes to the treatment of obesity?
- Is there a difference between being obese and overweight?
- Can obesity affect the sociological perspective of an individual?
- Explain how an obesity treatment works.
- How can the government help people to lose weight and improve public health?
Writing an essay is a challenging yet rewarding task. All you need is to be organized and clear when it comes to academic writing.
- Choose a topic you would like to write on.
- Organize your thoughts.
- Pen down your ideas.
- Compose a perfect essay that will help you ace your subject.
- Proofread and revise your paper.
Were the topics useful for you? We hope so!
However, if you are still struggling to write your paper, you can pick any of the topics from this list, and our essay writer will help you craft a perfect essay.
Are you struggling to write an effective essay?
If writing an essay is the actual problem and not just the topic, you can always hire an essay writing service for your help. Essay experts at 5StarEssays can help compose an impressive essay within your deadline.
All you have to do is contact us. We will get started on your paper while you can sit back and relax.
Place your order now to get an A-worthy essay.

Marketing, Thesis
As a Digital Content Strategist, Nova Allison has eight years of experience in writing both technical and scientific content. With a focus on developing online content plans that engage audiences, Nova strives to write pieces that are not only informative but captivating as well.
Was This Blog Helpful?
Keep reading.
- How to Write A Bio – Professional Tips and Examples

- Learn How to Write an Article Review with Examples

- How to Write a Poem Step-by-Step Like a Pro

- How To Write Poetry - 7 Fundamentals and Tips

- Know About Appendix Writing With the Help of Examples

- List of Social Issues Faced By the World

- How To Write A Case Study - Easy Guide

- Learn How to Avoid Plagiarism in 7 Simple Steps

- Writing Guide of Visual Analysis Essay for Beginners

- Learn How to Write a Personal Essay by Experts

- Character Analysis - A Step By Step Guide

- Thematic Statement: Writing Tips and Examples

- Expert Guide on How to Write a Summary

- How to Write an Opinion Essay - Structure, Topics & Examples

- How to Write a Synopsis - Easy Steps and Format Guide

- Learn How To Write An Editorial By Experts

- How to Get Better at Math - Easy Tips and Tricks

- How to Write a Movie Review - Steps and Examples

- Creative Writing - Easy Tips For Beginners

- Types of Plagiarism Every Student Should Know

People Also Read
- press release example
- illustration essay writing
- lab report writing
- cause and effect essay topics
- choosing essay writing service
Burdened With Assignments?
Advertisement
- Homework Services: Essay Topics Generator
© 2024 - All rights reserved
Causes and Effects of Obesity Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Laziness as the main cause of obesity, social effects of obesity, effects of obesity: health complications.
Bibliography
Maintaining good body weight is highly recommended by medical doctors as a way of promoting a healthy status of the body. This is to say that there is allowed body weight, which a person is supposed to maintain. Extreme deviations from this weight expose a person to several health complications.
While being underweight is not encouraged, cases of people who are overweight and increasing effects of this condition have raised concerns over the need of addressing the issue of obesity in the society today, where statistics are rising day and night. What is obesity? This refers to a medical condition in which a person’s body has high accumulation of body fat to the level of being fatal or a cause of serious health complications. Additionally, obesity is highly associated with one’s body mass index, abbreviated as BMI.
This denotes the value obtained when a person’s weight in kilograms is divided by the square of their height in meters (Burniat 3). According to medical experts, obesity occurs when the BMI exceeds 30kg/m 2 . While this is the case, people who have a BMI of between 25 and 29 and considered to be overweight. Obesity has a wide-range of negative effects, which may be a threat to the life of a person.
The fist effect of obesity is that it encourages laziness in the society. It is doubtless that obese people find it hard and strenuous to move from one point to the other because of accumulated fats. As a result, most of these people lead a sedentary lifestyle, which is usually characterized by minimal or no movement. In such scenarios, victims prefer being helped doing basic activities, including moving from one point to another.
Moreover, laziness makes one to be inactive and unproductive. For example, a student who is obese may find it hard to attend to his or her homework and class assignments, thus affecting performance. With regard to physical exercises, obese people perceive exercises as punishment, which is not meant for them (Korbonits 265). As a result, they do not accept simple activities like jogging because of their inability to move.
In line with this, obese people cannot participate in games like soccer, athletics, and rugby among others. Based on this sedentary lifestyle, obese people spend a lot of their time watching television, movies, and playing video games, which worsen the situation.
The main effect of obesity is health complications. Research indicates that most of the killer diseases like diabetes, heart diseases, and high blood pressure are largely associated with obesity. In the United States, obesity-related complications cost the nation approximately 150 billion USD and result into 0.3 million premature deaths annually.
When there is increase in body fat, it means that the body requires more nutrients and oxygen to support body tissues (Burniat 223). Since these elements can only be transported by the blood to various parts of the body, the workload of the heart is increased.
This increase in the workload of the heart exerts pressure on blood vessels, leading to high blood pressure. An increase in the heart rate may also be dangerous due to the inability of the body to supply required blood to various parts. Moreover, obesity causes diabetes, especially among adults as the body may become resistant to insulin. This resistance may lead to a high level of blood sugar, which is fatal.
Besides health complications, obesity causes an array of psychological effects, including inferiority complex among victims. Obese people suffer from depression, emanating from negative self-esteem and societal rejection. In some cases, people who become obese lose their friends and may get disapproval from teachers and other personalities (Korbonits 265). This is mainly based on the assumption that people become obese due to lack of self-discipline. In extreme cases, obese people may not be considered for promotion at workplaces, because of the negative perception held against them.
Due to inferiority complex, obese people avoid being in public and prefer being alone. This is because they imagine how the world sees them and may also find it hard being involved in public activities because of their sizes.
This further makes them to consider themselves unattractive based on their deviation from what is considered as the normal body size and shape. Regardless of how obese people are treated, they always believe that they are being undermined because of their body size.
In summary, obesity is a major cause of premature deaths in the United States and around the world. This health condition occurs when there is excess accumulation of body fat, caused by unhealthy lifestyles. Obesity is largely associated with several killer diseases like high blood pressure, diabetes, and diseases of the heart.
These diseases drain world economies since most of them are fatal and expensive to manage. Additionally, obesity promotes sedentary life where victims minimize movement by adopting an inactive lifestyle. Moreover, obese victims suffer psychologically because of societal rejection. In general, obesity has a wide-range of negative effects, which may be a threat to the life of a person.
Burniat, Walter. Child and Adolescent Obesity: Causes and Consequences, Prevention and Management . United Kingdom: Cambridge University Press, 2002. Print.
Korbonits, Márta. Obesity and Metabolism . Switzerland: Karger Publishers, 2008. Print.
- Childhood Obesity: Causes/Solutions
- Why are poor people more likely to be obese?
- Teachings of Hebrew Wisdom
- Recreation Hub as a Way to Combat Sedentary Lifestyle
- Parental Education on Overweight and Obese Children
- Eating Disorders: Assessment & Misconceptions
- Human Digestion
- Definitions of Obesity and Criteria for Diagnosing It
- Obesity Could Be Catching
- White Wines vs. Red Wines
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, December 11). Causes and Effects of Obesity Essay. https://ivypanda.com/essays/effects-of-obesity/
"Causes and Effects of Obesity Essay." IvyPanda , 11 Dec. 2018, ivypanda.com/essays/effects-of-obesity/.
IvyPanda . (2018) 'Causes and Effects of Obesity Essay'. 11 December.
IvyPanda . 2018. "Causes and Effects of Obesity Essay." December 11, 2018. https://ivypanda.com/essays/effects-of-obesity/.
1. IvyPanda . "Causes and Effects of Obesity Essay." December 11, 2018. https://ivypanda.com/essays/effects-of-obesity/.
IvyPanda . "Causes and Effects of Obesity Essay." December 11, 2018. https://ivypanda.com/essays/effects-of-obesity/.

Bridging the Evidence Gap in Obesity Prevention: A Framework to Inform Decision Making (2010)
Chapter: 10 conclusions and recommendations, 10 conclusions and recommendations.
D ecisions about prevention are complex, not only for the obesity problem but also for other problems with multiple types and layers of causation. Recognition of the need to emphasize population-based approaches to obesity prevention, the urgency of taking action, and the desire of many decision makers to have evidence on which actions to take have created a demand for evidence with which to answer a range of questions. In reality, the evidence approaches that apply to decision making about the treatment of obesity or other clinical problems are inadequate and sometimes inappropriate for application to decisions about public health initiatives. The need to work around evidence gaps and the limitations of using evidence hierarchies that apply to medical treatment for assessing population-based preventive interventions have been faced by the developers of several prior Institute of Medicine (IOM) reports on obesity prevention (focused on child and adolescent obesity). These evidence issues are not new and have already been the focus of many efforts in the field of public health in relation to other complex health problems. However, they are far from resolved. Considering these issues in relation to obesity prevention has the potential to advance the field of public health generally while also meeting the immediate need for clarity on evidence issues related to addressing the obesity epidemic.
The IOM’s Food and Nutrition Board formed the Committee on an Evidence Framework for Obesity Prevention Decision Making, with funding from Kaiser Permanente, the Robert Wood Johnson Foundation, and the Centers for Disease Control and Prevention. This committee was asked to develop a framework for evidence-informed decision making in obesity prevention, focused on approaches for assessing policy, environmental, and community interventions designed to influence diet and physical activity. The committee was tasked to:
provide an overview of the nature of the evidence base for obesity prevention as it is currently construed;
identify the challenges associated with integrating scientific evidence with broader influences on policy and programmatic considerations;
provide a practical and action-oriented framework of recommendations for how to select, implement, and evaluate obesity prevention efforts;
identify ways in which existing or new tools and methods can be used to build a useful and timely evidence base appropriate to the challenges presented by the epidemic, and describe ongoing attempts to meet these challenges;
develop a plan for communicating and disseminating the proposed framework and its recommendations; and
specify a plan for evaluating and refining the proposed framework in current decision-making processes.
CONCLUSIONS
Recognition is increasing that overweight and obesity are not only problems of individuals, but also societywide problems of populations. Acting on this recognition will require multifaceted, population-based changes in the socioenvironmental variables that influence energy intake and expenditure. There exist both a pressing need to act on the problem of obesity and a large gap between the type and amount of evidence needed to act and the type and amount of evidence available to meet that need. A new framework is necessary to assist researchers and a broad community of decision makers in generating, identifying, and evaluating the best evidence available and in summarizing it for use in decision making. This new framework also is important for researchers attempting to fill important evidence gaps through studies based on questions with program and policy relevance. However, the methods used and the evidence generated by traditional research designs do not yield all the types of evidence useful to inform actions aimed at addressing obesity prevention and other complex public health challenges. An expanded approach is needed that emphasizes the decision-making process and contextual considerations.
The Framework
To meet this need, the committee developed the L.E.A.D. ( L ocate Evidence, E valuate Evidence, A ssemble Evidence, and Inform D ecisions) framework, designed to facilitate a systematic approach to the identification, implementation, and evaluation of promising, reasonable actions to address obesity prevention and other complex public health challenges (see Figure 10-1 ). The framework is designed to help identify the nature of the evidence that is needed and clarify what changes in current approaches to generating and evaluating evidence will facilitate meeting those needs. This section describes the main components of the framework and issues related to these components.
Obesity prevention has not been addressed successfully by traditional study designs, which are generally linear and static. A systems approach is needed to develop more complex, interdisciplinary strategies. Accordingly, the L.E.A.D. framework
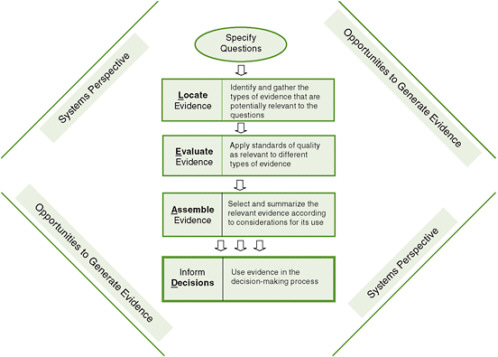
FIGURE 10-1 The L ocate Evidence, E valuate Evidence, A ssemble Evidence, Inform D ecisions (L.E.A.D.) framework for obesity prevention decision making.
recommends taking a systems perspective. In other words, it is necessary to use an approach that encompasses the whole picture, highlighting the broader context and interactions among levels, to capture the complexity of obesity prevention and other multifactorial public health challenges.
Addressing such challenges first requires specifying the question(s) being asked to guide the identification of evidence that is appropriate, inclusive, and relevant. Core to the framework is the orientation of the user. A variety of decisions have to be made to address obesity prevention. To capture the resulting mix of evidence needs, the framework adopts a typology that differentiates three broad categories of interrelated questions of potential interest to the user: Why should we do something about this problem? What specifically should we do? and How do we implement this information for our situation? This “Why,” “What,” “How” typology stresses the need for multiple types of evidence to support decisions on obesity prevention.
Once the question(s) of interest have been specified, locating useful evidence requires clear knowledge of the types of information that may be useful and an awareness of where that information can be found. The framework calls for the use of
diverse approaches to gather and synthesize information from other disciplines that address issues similar to those faced in obesity prevention and public health generally. Evidence identified and gathered to inform decision making for obesity prevention and other complex public health challenges should be assessed based on both its generalizability and level of certainty (i.e., its external and internal validity, respectively). The L.E.A.D. framework addresses these two key aspects of the evidence through the nature of the question(s) being asked, established criteria for the value of evidence, and the context in which the question(s) arise. Results of the overall evaluation of evidence should provide answers on what to do, how to do it, and how strongly the action is justified.
When decision makers are coming to a decision on obesity prevention actions, it is important for them to understand the state of the available knowledge relevant to that decision. This knowledge includes evidence on the specific problem to be addressed, the likely effectiveness and impact of proposed actions, and key considerations involved in their implementation. Successful evidence gathering, evaluation, and synthesis for use in obesity prevention usually require the involvement of a number of disciplines using a variety of methodologies and technical languages. The framework incorporates a standardized approach using a uniform language and structure for summarizing the relevant evidence in a systematic, transparent, and transdisciplinary way that is critical for communicating the process and conclusions clearly.
With an emergent problem such as obesity, decisions to act often must be made in the face of a relative absence of evidence, or evidence that is inconclusive, inconsistent, or incomplete. Evidence gathered from a particular intervention implemented in a closely controlled manner within a specific population with its own unique characteristics is often difficult to apply to a similar intervention with another population. The typical way of presenting results of obesity prevention efforts in journals often adds to the problem of incomplete evidence because useful aspects of the research related to its generalizability are not reported. If obesity prevention actions must be taken when evidence is limited, this incomplete evidence can be blended with theory, expert opinion, experience, and local wisdom to make the best decision possible. The actions taken then should undergo critical evaluation, the results of which should be used to build credible evidence for use in decision making about future efforts. Important alternatives to waiting for the funding, implementation, and publication of formal research on obesity prevention are natural experiments as sources of practice-based evidence, “evaluability assessment” of emerging innovations (defined as assessing whether a program is ready for full-scale evaluation), and continuous quality assessment of ongoing programs. The L.E.A.D. framework process leads to knowledge integration, or the incorporation of new knowledge gained through the process of applying the framework into the context of the organization or system where decisions are made.
The evidence base to support the identification of effective obesity prevention interventions is limited in many areas. Opportunities to generate evidence may occur
at any phase of the evidence review or decision-making process. The L.E.A.D. framework guides the generation of evidence related to “What,” “Why,” and “How” questions and supports the use of multiple forms of evidence and research designs from a variety of disciplines. In obesity prevention–related research, the generation of evi dence from evaluation of ongoing and emerging initiatives is a particular priority.
Researchers, decision makers, and intermediaries working on obesity prevention and other complex multifactorial public health problems are the primary audiences for communicating and disseminating the L.E.A.D. framework. With sufficient information, they can apply the framework as a guide for generating needed evidence and supporting decision making. It is important to understand the settings, communication channels, and activities of these key audiences to engage and educate them effectively on the purpose and adoption of the framework. To support the development of a communication and dissemination plan, it is critical to create partnerships, make use of existing activities and networks, and tailor the messages and approaches to each target audience.
As the target audiences begin to use the framework, assessing its use in selected settings will be essential so it can be improved and refined. Evaluation of the impact of the L.E.A.D. framework is also important for determining its relevance to current evidence-generation and decision-making processes. To this end, key outcome measures—utilization, adoption, acceptance, maintenance, and impact—should be defined and data collected on these measures. It will be important to develop or adopt data collection tools and utilize methods and existing initiatives that will best serve this purpose, as well as to systematically integrate the feedback thus obtained to sustain and improve the framework’s applicability and utilization.
RECOMMENDATIONS
The United States has made progress toward translating science into practice in the brief time since the obesity epidemic was officially recognized. But the pace of this translation has been slow relative to the scope and urgency of the problem and the associated harms and costs. As discussed above, moreover, the evidence emerging from applied research on obesity prevention can be inconclusive, incomplete, and inconsistent. A systematic process is needed to improve the use of available evidence and increase and enhance the evidence base to inform decisions on obesity prevention and other complex public health problems. Commitment to such a process is needed from both decision makers and those involved in generating evidence, including public and private policy makers and their advisors, scientific and policy think tanks, advocacy groups and stakeholders, program planners, practitioners in public health and other sectors, program evaluators, public health researchers and research scientists, journal editors, and funders. With this in mind, the committee makes the following recom-
mendations for assisting decision makers and researchers in using the current evidence base for obesity prevention and for taking a systems-oriented, transdisciplinary approach to generate more, and more useful, evidence.
Utilize the L.E.A.D. Framework
Recommendation 1: Decision makers and those involved in generating evidence, including researchers, research funders, and publishers of research, should apply the L.E.A.D. framework as a guide in their utilization and generation of evidence to support decision making for complex, multifactorial public health challenges, including obesity prevention.
Key assumptions that should guide the use of the framework include the following:
A systems perspective can help in framing and explaining complex issues.
The types of evidence that should be gathered to inform decision making are based on the nature of the questions being asked, including Why? (“Why should we do something about this problem in our situation?”), What? (“What specifically should we do about this problem?”), and How? (“How do we implement this information for our situation?”). A focus on subsets of these questions as a starting point in gathering evidence explicitly expands the evidence base that is typically identified and gathered.
The quality of the evidence should be judged according to established criteria for that type of evidence.
Both the level of certainty of the causal relationship between an intervention and the observed outcomes and the intervention’s generalizability to other individuals, settings, contexts, and time frames should be given explicit attention.
The analysis of the evidence to be used in making a decision should be summarized and communicated in a systematic, transparent, and transdisciplinary manner that uses uniform language and structure. The report on this analysis should include a summary of the question(s) asked by the decision maker; the strategy for gathering and selecting the evidence; an evidence table showing the sources, types, and quality of the evidence and the outcomes reported; and a concise summary of the synthesis of selected evidence on why an action should be taken, what that action should be, and how it should be taken.
If action must be taken when evidence is limited, this incomplete evidence can be blended carefully and transparently with theory, expert opinion, and collaboration based on professional experience and local wisdom to support making the best decision.
Sustained commitments will be needed from both the public and private sectors to achieve successful utilization of the various elements of the L.E.A.D. framework in future evidence-informed decision making and evidence generation. This respon-
sibility lies with the academic and research community, as well as with government and private funders and the leadership of journals that publish research in this area. Necessary supports will include increasing understanding of systems thinking and incorporating it into research-related activities, creating and maintaining resources to support the utilization of evidence, establishing standards of quality for different types of evidence, and supporting the generation of evidence, each of which is described in more detail below. Finally, it will be necessary to communicate, disseminate, evaluate, and refine the L.E.A.D. framework.
Incorporate Systems Thinking
Recommendation 2: Researchers, government and private funders, educators, and journal editors should incorporate systems thinking into their research-related activities.
To implement this recommendation:
Researchers should use systems thinking to guide the development of environmental and policy interventions and study designs.
Government and private funders should encourage the use of systems thinking in their requests for proposals and include systems considerations in proposal evaluations.
Universities, government agencies such as the U.S. Centers for Disease Control and Prevention, and public health organizations responsible for educating public health practitioners and related researchers should establish training capacity for the science and understanding of systems thinking and the use of systems mapping and other quantitative or qualitative systems analysis tools.
Journal editors should encourage the use of systems thinking for addressing complex problems by developing panels of peer reviewers with expertise in this area and charging them with making recommendations for how authors could use systems thinking more effectively in their manuscripts.
Build a Resource Base
Recommendation 3: Government, foundations, professional organizations, and research institutions should build a system of resources (people, compendiums of knowledge, registries of implementation experience) to support evidence-based public policy decision making and research for complex health challenges, including obesity prevention.
The Secretary of Health and Human Services, in collaboration with other public- and private-sector partners, should establish a sustainable registry of reports on evidence for environmental and policy actions for obesity prevention.
Integral to this registry should be the expanded view of evidence for decision making on obesity prevention proposed in this report and the sharing of experiences and innovative programs as the evidence evolves. A service provided by this registry should be periodic synthesis reviews based on mixed qualitative and quantitative methods.
The Secretary of Health and Human Services, in collaboration with other public- and private-sector partners, should develop and fund a resource for compiling and linking existing databases that may contain useful evidence for obesity prevention and related public health initiatives. This resource should include links to data and research from disciplines and sectors outside of obesity prevention and public health and to data from nonacademic sources that are of interest to decision makers.
Establish Standards for Evidence Quality
Recommendation 4: Government, foundations, professional organizations, and research institutions should catalyze and support the establishment of guidance on standards for evaluating the quality of evidence for which such standards are lacking.
Government and private funders should give priority to funding for the development of guidance on standards for evaluating the quality of the full range of evidence types discussed in this report that are useful in making obesity prevention decisions, especially those for which the scientific literature is limited.
Professional organizations and research institutions should encourage and bring attention to efforts by faculty, researchers, and students to establish guidance in this area.
Support the Generation of Evidence
Recommendation 5: Obesity prevention research funders, researchers, and publishers should consider, wherever appropriate, the inclusion in research studies of a focus on the generalizability of the find ings and related implementation issues at every stage, from conception through publication.
Those funding research in obesity prevention should give priority to support for studies that include an assessment of the limitations, potential utility, and applicability of the research beyond the particular population, setting, and circumstances in which the studies are conducted, including by initiating requests for applications and similar calls for proposals aimed at such studies. Additional ways in which this recommendation could be implemented include adding crite-
ria related to generalizability to proposal review procedures and training reviewers to evaluate generalizability.
Obesity prevention researchers and program evaluators should give special consideration to study designs that maximize evidence on generalizability.
Journal editors should provide guidelines and space for authors to give richer descriptions of interventions and the conditions under which they are tested to clarify their generalizability.
Recommendation 6: Research funders should increase opportunities for those carrying out obesity pre vention initiatives to measure and share their outcomes so others can learn from their experience.
Organizations funding or sponsoring obesity prevention initiatives—including national, regional, statewide, or local programs; policy changes; and environmental initiatives—should provide resources for obtaining practice-based evidence from innovative and ongoing programs and policies in a more routine, timely, and systematic manner to capture their processes, implementation, and outcomes. These funders should also encourage and support assessments of the potential for evaluating the most innovative programs in their jurisdictions and sponsor scientific evaluations where the opportunities to advance generalizable evidence are greatest.
Research funders, researchers, and journal editors should assign higher priority to studies that test obesity prevention interventions in real-world settings in which major contextual variables are identified and their influence is evaluated.
Recommendation 7: Research funders should encourage collaboration among researchers in a variety of disciplines so as to utilize a full range of research designs that may be feasible and appropriate for evaluating obesity prevention and related public health initiatives.
As part of their requests for proposals on obesity prevention research, funders should give priority to and reward transdisciplinary collaborations that include the creative use of research designs that have not been extensively used in prevention research but hold promise for expanding the evidence base on potential environmental and policy solutions.

Communicate, Disseminate, Evaluate, and Refine the L.E.A.D. Framework
Recommendation 8: A public–private consortium should bring together researchers, research funders, publishers of research, decision makers, and other stakeholders to discuss the practical uses of the
L.E.A.D. framework, and develop plans and a timeline for focused experimentation with the frame work and for its evaluation and potential refinement.
Interested funders should bring together a consortium of representatives of key stakeholders (including decision makers, government funders, private funders, academic institutions, professional organizations, researchers, and journal editors) who are committed to optimizing the use of the current obesity prevention evidence base and developing a broader and deeper base of evidence.
This consortium should develop an action-oriented plan for funding and implementing broad communication, focused experimentation, evaluation, and refinement of the L.E.A.D. framework. This plan should be based on the major purposes of the framework: to significantly improve the evidence base for obesity prevention decision making on policy and environmental solutions, and to assist decision makers in using the evidence base.
To battle the obesity epidemic in America, health care professionals and policymakers need relevant, useful data on the effectiveness of obesity prevention policies and programs. Bridging the Evidence Gap in Obesity Prevention identifies a new approach to decision making and research on obesity prevention to use a systems perspective to gain a broader understanding of the context of obesity and the many factors that influence it.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley Open Access Collection

Obesity: Risk factors, complications, and strategies for sustainable long‐term weight management
Sharon m. fruh.
1 College of Nursing, University of South Alabama, Mobile, Alabama
Background and Purpose
The aims of this article are to review the effects of obesity on health and well‐being and the evidence indicating they can be ameliorated by weight loss, and consider weight‐management strategies that may help patients achieve and maintain weight loss.
Narrative review based on literature searches of PubMed up to May 2016 with no date limits imposed. Search included terms such as “obesity,” “overweight,” “weight loss,” “comorbidity,” “diabetes,” cardiovascular,” “cancer,” “depression,” “management,” and “intervention.”
Conclusions
Over one third of U.S. adults have obesity. Obesity is associated with a range of comorbidities, including diabetes, cardiovascular disease, obstructive sleep apnea, and cancer; however, modest weight loss in the 5%–10% range, and above, can significantly improve health‐related outcomes. Many individuals struggle to maintain weight loss, although strategies such as realistic goal‐setting and increased consultation frequency can greatly improve the success of weight‐management programs. Nurse practitioners have key roles in establishing weight‐loss targets, providing motivation and support, and implementing weight‐loss programs.
Implications for Practice
With their in‐depth understanding of the research in the field of obesity and weight management, nurse practitioners are well placed to effect meaningful changes in weight‐management strategies deployed in clinical practice.
Introduction
Obesity is an increasing, global public health issue. Patients with obesity are at major risk for developing a range of comorbid conditions, including cardiovascular disease (CVD), gastrointestinal disorders, type 2 diabetes (T2D), joint and muscular disorders, respiratory problems, and psychological issues, which may significantly affect their daily lives as well as increasing mortality risks. Obesity‐associated conditions are manifold; however, even modest weight reduction may enable patients to reduce their risk for CVD, diabetes, obstructive sleep apnea (OSA), and hypertension among many other comorbidities (Cefalu et al., 2015 ). A relatively small and simple reduction in weight, for example, of around 5%, can improve patient outcomes and may act as a catalyst for further change, with sustainable weight loss achieved through a series of incremental weight loss steps. In facilitating the process of losing weight for patients, nurse practitioners play an essential role. Through assessing the patient's risk, establishing realistic weight‐loss targets, providing motivation and support, and supplying patients with the necessary knowledge and treatment tools to help achieve weight loss, followed by tools for structured lifestyle support to maintain weight lost, the nurse practitioner is ideally positioned to help patient's achieve their weight‐loss—and overall health—targets.
The obesity epidemic
The World Health Organization (WHO) defines overweight and obesity as abnormal or excessive fat accumulation that presents a risk to health (WHO, 2016a ). A body mass index (BMI) ≥25 kg/m 2 is generally considered overweight, while obesity is considered to be a BMI ≥ 30 kg/m 2 . It is well known that obesity and overweight are a growing problem globally with high rates in both developed and developing countries (Capodaglio & Liuzzi, 2013 ; WHO, 2016a , 2016b ).
In the United States in 2015, all states had an obesity prevalence more than 20%, 25 states and Guam had obesity rates >30% and four of those 25 states (Alabama, Louisiana, Mississippi, and West Virginia) had rates >35% (Centres for Disease Control and Prevention, 2016 ; Figure Figure1). 1 ). Approximately 35% and 37% of adult men and women, respectively, in the United States have obesity (Yang & Colditz, 2015 ). Adult obesity is most common in non‐Hispanic black Americans, followed by Mexican Americans, and non‐Hispanic white Americans (Yang & Colditz, 2015 ). Individuals are also getting heavier at a younger age; birth cohorts from 1966 to 1975 and 1976 to 1985 reached an obesity prevalence of ≥20% by 20–29 years of age, while the 1956–1965 cohort only reached this prevalence by age 30–39 years (Lee et al., 2010 ). Additionally, the prevalence of childhood obesity in 2‐ to 17‐year‐olds in the United States has increased from 14.6% in 1999–2000 to 17.4% in 2013–2014 (Skinner & Skelton, 2014 ). Childhood obesity is an increasing health issue because of the early onset of comorbidities that have major adverse health impacts, and the increased likelihood of children with obesity going on to become adults with obesity (50% risk vs. 10% for children without obesity; Whitaker, Wright, Pepe, Seidel, & Dietz, 1997 ).

U.S. obesity epidemic 2015.
Source . Figure adapted from Centers for Disease Control and Prevention (CDC). Retrieved from https://www.cdc.gov/obesity/data/prevalence-maps.html .
Association of obesity with mortality and comorbid disease
Obesity is associated with a significant increase in mortality, with a life expectancy decrease of 5–10 years (Berrington de Gonzalez et al., 2010 ; Kuk et al., 2011 ; Prospective Studies Collaboration et al., 2009 ). There is evidence to indicate that all‐cause, CVD‐associated, and cancer‐associated mortalities are significantly increased in individuals with obesity, specifically those at Stages 2 or 3 of the Edmonton Obesity Staging System (EOSS; Kuk et al., 2011 ; Figure Figure2). 2 ). Mortality related to cancer is, however, also increased at Stage 1, when the physical symptoms of obesity are marginal (Figure (Figure2). 2 ). Recently, a large‐scale meta‐analysis that included studies that had enrolled over 10 million individuals, indicated that, relative to the reference category of 22.5 to <25 kg/m 2 , the hazard ratio (HR) for all‐cause mortality rose sharply with increasing BMI (The Global BMI Mortality Collaboration, 2016 ). For a BMI of 25.0 to <30.0 kg/m 2 , the HR was 1.11 (95% confidence interval [CI] 1.10, 1.11), and this increased to 1.44 (1.41, 1.47), 1.92 (1.86, 1.98), and 2.71 (2.55, 2.86) for a BMI of 30.0 to <35.0, 35.0 to <40.0, and 40.0 to <60.0 kg/m 2 , respectively.

Association between EOSS stage and risk of all‐cause (A), CVD (B), cancer (C), and non‐CVD or noncancer mortality (D) in men and women. © 2011.
Source . Reproduced with permission from NRC Research Press, from Kuk et al. ( 2011 ). CVD, cardiovascular disease; NW, normal weight.
Comorbidities
Obesity is a chronic disease that is associated with a wide range of complications affecting many different aspects of physiology (Dobbins, Decorby, & Choi, 2013 ; Guh et al., 2009 ; Martin‐Rodriguez, Guillen‐Grima, Marti, & Brugos‐Larumbe, 2015 ; summarized in Table Table1). 1 ). To examine these obesity‐related morbidities in detail is beyond the scope of this review and therefore only a brief overview of some of the key pathophysiological processes is included next.
Morbidities associated with obesity (Hamdy, 2016 ; Petry, Barry, Pietrzak, & Wagner, 2008 ; Pi‐Sunyer, 2009 ; Sakai et al., 2005 ; Smith, Hulsey, & Goodnight, 2008 ; Yosipovitch, DeVore, & Dawn, 2007 )
| Class of event | Comorbidities associated with obesity |
|---|---|
| Cancer/malignancy | Postmenopausal breast, endometrial, colon and rectal, gallbladder, prostate, ovarian, endometrial renal cell, esophageal adenocarcinoma, pancreatic, and kidney cancer |
| Cardiovascular | Coronary artery disease, obesity‐associated cardiomyopathy, essential hypertension, left ventricular hypertrophy, cor pulmonale, accelerated atherosclerosis, pulmonary hypertension of obesity, dyslipidemia, chronic heart failure (CHD), left ventricular hypertrophy (LVH), cardiomyopathy, pulmonary hypertension, lymphedema (legs) |
| Gastrointestinal (GI) | Gall bladder disease (cholecystitis, cholelithiasis), gastroesophageal reflux disease (GERD), reflux esophagitis, nonalcoholic steatohepatitis (NASH), nonalcoholic fatty liver disease (NAFLD), fatty liver infiltration, acute pancreatitis |
| Genitourinary | Stress incontinence |
| Metabolic/endocrine | Type 2 diabetes mellitus, prediabetes, metabolic syndrome, insulin resistance, and dyslipidemia |
| Musculoskeletal/orthopedic | Pain in back, hips, ankles, feet and knees; osteoarthritis (especially in the knees and hips), plantar fasciitis, back pain, coxavera, slipped capital femoral epiphyses, Blount disease and Legg‐Calvé‐Perthes disease, and chronic lumbago |
| Neurological and central nervous system (CNS) | Stroke, dementia idiopathic intracranial hypertension, and meralgia paresthesia |
| Obstetric and perinatal | Pregnancy‐related hypertension, fetal macrosomia, very low birthweight, neural tube defects, preterm birth, increased cesarean delivery, increased postpartum infection and pelvic dystocia, preeclampsia, hyperglycemia, gestational diabetes (GDM) |
| Skin | Keratosis pilaris, hirsutism, acanthosis nigricans, and acrochondons, psoriasis, intertrigo (bacterial and/or fungal), and increased risk for cellulitis, venous stasis ulcers, necrotizing fasciitis, and carbuncles |
| Psychological | Depression, anxiety, personality disorder, and obesity stigmatization |
| Respiratory/pulmonary | Obstructive sleep apnea (OSA), Pickwickian syndrome (obesity hypoventilation syndrome), higher rates of respiratory infections, asthma, hypoventilation, pulmonary emboli risk |
| Surgical | Increased surgical risk and postoperative complications, deep venous thrombosis, including wound infection, pulmonary embolism, and postoperative pneumonia |
| Reproductive (Women) | Anovulation, early puberty, polycystic ovaries, infertility, hyperandrogenism, and sexual dysfunction |
| Reproductive (Men) | Hypogonadotropic hypogonadism, polycystic ovary syndrome (PCOS), decreased libido, and sexual dysfunction |
| Extremities | Venous varicosities, lower extremity venous and/or lymphatic edema |
The progression from lean state to obesity brings with it a phenotypic change in adipose tissue and the development of chronic low‐grade inflammation (Wensveen, Valentic, Sestan, Turk Wensveen, & Polic, 2015 ). This is characterized by increased levels of circulating free‐fatty acids, soluble pro‐inflammatory factors (such as interleukin [IL] 1β, IL‐6, tumor necrosis factor [TNF] α, and monocyte chemoattractant protein [MCP] 1) and the activation and infiltration of immune cells into sites of inflammation (Hursting & Dunlap, 2012 ). Obesity is also usually allied to a specific dyslipidemia profile (atherogenic dyslipidemia) that includes small, dense low‐density lipoprotein (LDL) particles, decreased levels of high‐density lipoprotein (HDL) particles, and raised triglyceride levels (Musunuru, 2010 ). This chronic, low‐grade inflammation and dyslipidemia profile leads to vascular dysfunction, including atherosclerosis formation, and impaired fibrinolysis. These, in turn, increase the risk for CVD, including stroke and venous thromboembolism (Blokhin & Lentz, 2013 ).
The metabolic and cardiovascular aspects of obesity are closely linked. The chronic inflammatory state associated with obesity is established as a major contributing factor for insulin resistance, which itself is one of the key pathophysiologies of T2D (Johnson, Milner, & Makowski, 2012 ). Furthermore, central obesity defined by waist circumference is the essential component of the International Diabetes Federation (IDF) definition of the metabolic syndrome (raised triglycerides, reduced HDL cholesterol, raised blood pressure, and raised fasting plasma glucose; International Diabetes Federation, 2006 ).
Obesity is also closely associated with OSA. To start, a number of the conditions associated with obesity such as insulin resistance (Ip et al., 2002 ), systemic inflammation, and dyslipidemia are themselves closely associated with OSA, and concurrently, the obesity‐associated deposition of fat around the upper airway and thorax may affect lumen size and reduce chest compliance that contributes to OSA (Romero‐Corral, Caples, Lopez‐Jimenez, & Somers, 2010 ).
The development of certain cancers, including colorectal, pancreatic, kidney, endometrial, postmenopausal breast, and adenocarcinoma of the esophagus to name a few, have also been shown to be related to excess levels of fat and the metabolically active nature of this excess adipose tissue (Booth, Magnuson, Fouts, & Foster, 2015 ; Eheman et al., 2012 ). Cancers have shown to be impacted by the complex interactions between obesity‐related insulin resistance, hyperinsulinemia, sustained hyperglycemia, oxidative stress, inflammation, and the production of adipokines (Booth et al., 2015 ). The wide range of morbidities associated with obesity represents a significant clinical issue for individuals with obesity. However, as significant as this array of risk factors is for patient health, the risk factors can be positively modified with weight loss.
Obesity‐related morbidities in children and adolescents
As was referred to earlier, children and adolescents are becoming increasingly affected by obesity. This is particularly concerning because of the long‐term adverse consequences of early obesity. Obesity adversely affects the metabolic health of young people and can result in impaired glucose tolerance, T2D, and early‐onset metabolic syndrome (Pulgaron, 2013 ).There is also strong support in the literature for relationships between childhood obesity and asthma, poor dental health (caries), nonalcoholic fatty liver disease (NAFLD), and gastroesophageal reflux disease (GERD; Pulgaron, 2013 ). Obesity can also affect growth and sexual development and may delay puberty in boys and advance puberty in some girls (Burt Solorzano & McCartney, 2010 ). Childhood obesity is also associated with hyperandrogenism and polycystic ovary syndrome (PCOS) in girls (Burt Solorzano & McCartney, 2010 ). Additionally, obesity is associated with psychological problems in young people including attention deficit hyperactivity disorder (ADHD), anxiety, depression, poor self‐esteem, and problems with sleeping (Pulgaron, 2013 ).
Modest weight loss and its long‐term maintenance: Benefits and risks
Guidelines endorse weight‐loss targets of 5%–10% in individuals with obesity or overweight with associated comorbidities, as this has been shown to significantly improve health‐related outcomes for many obesity‐related comorbidities (Cefalu et al., 2015 ; Figure Figure3), 3 ), including T2D prevention, and improvements in dyslipidemia, hyperglycemia, osteoarthritis, stress incontinence, GERD, hypertension, and PCOS. Further benefits may be evident with greater weight loss, particularly for dyslipidemia, hyperglycemia, and hypertension. For NAFLD and OSA, at least 10% weight loss is required to observe clinical improvements (Cefalu et al., 2015 ).

Benefits of modest weight loss. Lines demonstrate the ranges in which weight loss has been investigated and shown to have clinical benefits. Arrows indicate that additional benefits may be seen with further weight loss.
Source . Figure adapted from Cefalu et al. ( 2015 ).
Importantly, the weight‐loss benefits in terms of comorbidities are also reflected in improved all‐cause mortality. A recent meta‐analysis of 15 studies demonstrated that relatively small amounts of weight loss, on average 5.5 kg in the treatment arm versus 0.2 kg with placebo from an average baseline BMI of 35 kg/m 2 , resulted in a substantial 15% reduction in all‐cause mortality (Kritchevsky et al., 2015 ).
Cardiovascular health
Weight loss is associated with beneficial changes in several cardiovascular risk markers, including dyslipidemia, pro‐inflammatory/pro‐thrombotic mediators, arterial stiffness, and hypertension (Dattilo & Kris‐Etherton, 1992 ; Dengo et al., 2010 ; Goldberg et al., 2014 ; Haffner et al., 2005 ; Ratner et al., 2005 ). Importantly, weight loss was found to reduce the risk for CVD mortality by 41% up to 23 years after the original weight‐loss intervention (Li et al., 2014 ; Figure Figure4). 4 ). Evidence including the biological effects of obesity and weight loss, and the increased risk for stroke with obesity indicates that weight loss may be effective for primary‐ and secondary‐stroke prevention (Kernan, Inzucchi, Sawan, Macko, & Furie, 2013 ).

Reduction in cardiovascular mortality with modest weight reduction. Cumulative incidence of CVD mortality during 23 years of follow‐up in the Da Qing study (Li et al., 2014 ). Figure © 2014 Elsevier.
Source . Reproduced with permission from Li et al. ( 2014 ).
Type 2 diabetes
Three major long‐term studies, the Diabetes Prevention Program (DPP), the Diabetes Prevention Study (DPS), and the Da Qing IGT and Diabetes (Da Qing) study, have demonstrated that modest weight loss through short‐term lifestyle or pharmacologic interventions can reduce the risk for developing T2D by 58%, 58%, and 31%, respectively, in individuals with obesity and prediabetes (DPP Research Group et al., 2009 ; Pan et al., 1997 ; Tuomilehto et al., 2001 ). Long‐term benefits were maintained following the interventions; for example, in the DPP, the risk reduction of developing T2D versus placebo was 34% at 10 years and 27% at 15 years following the initial weight‐loss intervention (DPP Research Group, 2015 ; DPP Research Group et al., 2009 ). Weight loss increased the likelihood of individuals reverting from prediabetes to normoglycemia (DPP Research Group et al., 2009 ; Li et al., 2008 ; Lindstrom et al., 2003 , 2006 ; Tuomilehto et al., 2001 ), and also improved other aspects of glycemic control including fasting and postprandial glucose, and insulin sensitivity (Haufe et al., 2013 ; Li et al., 2008 ).
Sleep apnea
Data indicate that weight loss is beneficial, although not curative, in patients with obesity who experience OSA. Meta‐analyses of patients who underwent treatment with either intensive lifestyle intervention (Araghi et al., 2013 ) or bariatric surgery (Greenburg, Lettieri, & Eliasson, 2009 ) demonstrated improvements in apnea‐hypopnea index (AHI) following treatment. In the first of these meta‐analyses, in randomized controlled trials, lifestyle intervention lead to a mean reduction in BMI of 2.3 kg/m 2 , which was associated with a decrease in mean AHI of 6.0 events/h. As expected, weight loss was much higher in the second meta‐analysis that investigated the effect of bariatric surgery on measures of OSA, and this was associated with greater reductions in AHI; the mean BMI reduction of 17.9 kg/m 2 resulted in AHI events being reduced by a mean of 38.2 events/h. Once these improvements in AHI have occurred, they seem to persist for some time, irrespective of a certain degree of weight regain. In one study, an initial mean weight loss of 10.7 kg resulted in a persistent improvement in AHI over a 4‐year period despite weight regain of approximately 50% by Year 4 (Kuna et al., 2013 ).
Intentional weight loss of >9 kg reduced the risk for a range of cancers including breast, endometrium, and colon in the large‐scale Iowa Women's Health Study (Parker & Folsom, 2003 ). The overall reduction in the incidence rate of any cancer was 11% (relative risk, 0.89; 95% CI 0.79, 1.00) for participants who lost more than 9 kg compared with those who did not achieve a more than 9 kg weight loss episode. Additionally, weight loss in participants with obesity has been established to be associated with reductions in cancer biomarkers including soluble E‐selectin and IL‐6 (Linkov et al., 2012 ).
Additional health benefits
The substantial weight loss associated with bariatric surgery has been shown to improve asthma with a 48%–100% improvement in symptoms and reduction in medication use (Juel, Ali, Nilas, & Ulrik, 2012 ); however, there is a potential threshold effect so that modest weight loss of 5%–10% may lead to clinical improvement (Lv, Xiao, & Ma, 2015 ). Similarly, modest weight loss of 5%–10% improves GERD (Singh et al., 2013 ) and liver function (Haufe et al., 2013 ). A study utilizing MRI scanning to examine the effects of weight loss on NAFLD has reported a reduction in liver fat from 18.3% to 13.6% ( p = .03), a relative reduction of 25% (Patel et al., 2015 ). Taking an active role in addressing obesity through behavioral modifications or exercise can also reduce the symptoms of depression (Fabricatore et al., 2011 ), improve urinary incontinence in men and women (Breyer et al., 2014 ; Brown et al., 2006 ), and improve fertility outcomes in women (Kort, Winget, Kim, & Lathi, 2014 ). Additionally, weight loss can reduce the joint‐pain symptoms and disability caused by weight‐related osteoarthritis (Felson, Zhang, Anthony, Naimark, & Anderson, 1992 ; Foy et al., 2011 ).
Mitigating risks
Despite the array of benefits, weight loss can also be linked with certain risks that may need to be managed. One such example is the risk for gallstones with rapid weight loss, which is associated with gallstone formation in 30%–71% of individuals. Gallstone formation is particularly associated with bariatric surgery when weight loss exceeds 1.5 kg/week and occurs particularly within the first 6 weeks following surgery when weight loss is greatest. Slower rates of weight loss appear to mitigate the risk for gallstone formation compared to the general population but may not eliminate it entirely; as was noted in the year‐long, weight‐loss, SCALE trial that compared liraglutide 3.0 mg daily use to placebo and resulted in gallstone formation in 2.5% of treated subjects compared to 1% of subjects taking placebo. For this reason, the risk for cholethiasis should be considered when formulating weight‐loss programs (Weinsier & Ullmann, 1993 ).
Strategies to help individuals achieve and maintain weight loss
Rogge and Gautam have covered the biology of obesity and weight regain within another section of this supplement (Rogge & Gautam, 2017 ), so here we focus on some of the clinical strategies for delivering weight loss and weight loss maintenance lifestyle programs. Structured lifestyle support plays an important role in successful weight management. A total of 34% of participants receiving structured lifestyle support from trained‐nursing staff achieved weight loss of ≥5% over 12 weeks compared with approximately 19% with usual care (Nanchahal et al., 2009 ). This particular structured program, delivered in a primary healthcare setting, included initial assessment and goal setting, an eating plan and specific lifestyle goals, personalized activity program, and advice about managing obstacles to weight loss. Additionally, data from the National Weight Control Registry (NWCR), which is the longest prospective compilation of data from individuals who have successfully lost weight and maintained their weight loss, confirm expectations that sustained changes to both diet and activity levels are central to successful weight management (Table (Table2). 2 ). Therefore, an understanding of different clinical strategies for delivery‐structured support is essential for the nurse practitioner.
Lifestyle factors associated with achieving and maintaining weight loss
| Action | Percentage |
|---|---|
| Modified food intake | 98 |
| Increased physical activity | 94 |
| Exercised on average for 1 h each day | 90 |
| Ate breakfast every day | 78 |
| Weighed themselves weekly | 75 |
| Watched less than 10 h of television weekly | 62 |
| Lost weight with the help of a weight‐loss program | 55 |
Note . Data from (NWCR, 2016 ).
a Walking was the most common activity undertaken.
Realistic weight‐loss targets
From the outset, a patient's estimate of their achievable weight loss may be unrealistic. Setting realistic weight‐loss goals is often difficult because of misinformation from a variety of sources, including friends, media, and other healthcare professionals (Osunlana et al., 2015 ). Many individuals with obesity or overweight have unrealistic goals of 20%–30% weight loss, whereas a more realistic goal would be the loss of 5%–15% of the initial body weight (Fabricatore et al., 2007 ). Promoting realistic weight‐loss expectations for patients was identified as a key difficulty for nurse practitioners, primary care nurses, dieticians, and mental health workers (Osunlana et al., 2015 ). Visual resources showing the health and wellness benefit of modest weight loss may thus be helpful (Osunlana et al., 2015 ). Healthcare practitioners should focus on open discussion about, and re‐enforcement of, realistic weight‐loss goals and assess outcomes consistently according to those goals (Bray, Look, & Ryan, 2013 ).
Maintaining a food diary
The 2013 White Paper from the American Nurse Practitioners Foundation on the Prevention and Treatment of Obesity considers a food diary as an important evidence‐based nutritional intervention in aiding weight loss (ANPF). Consistent and regular recording in a food diary was significantly associated with long‐term weight‐loss success in a group of 220 women (Peterson et al., 2014 ). This group lost a mean of 10.4% of their initial body weight through a 6‐month group‐based weight‐management program and then regained a mean of 2.3% over a 12‐month follow‐up period, during which participants received bimonthly support in person, by telephone, or by e‐mail (Peterson et al., 2014 ). Over the 12‐month follow‐up, women who self‐monitored consistently (≥50% of the extended‐care year) had a mean weight loss of 0.98%, while those who were less consistent (<50%) gained weight (5.1%; p < .01). Therefore, frequent and consistent food monitoring should be encouraged, particularly in the weight‐maintenance phase of any program.
Motivating and supporting patients
Motivational interviewing is a technique that focuses on enhancing intrinsic motivation and behavioral changes by addressing ambivalence (Barnes & Ivezaj, 2015 ). Interviews focus on “change talk,” including the reasons for change and optimism about the intent for change in a supportive and nonconfrontational setting, and may help individuals maintain behavioral changes.
For patients that have achieved weight loss, the behavioral factors associated with maintaining weight loss include strong social support networks, limiting/avoiding disinhibited eating, avoiding binge eating, avoiding eating in response to stress or emotional issues, being accountable for one's decisions, having a strong sense of autonomy, internal motivation, and self‐efficacy (Grief & Miranda, 2010 ). Therefore, encouraging feelings of “self‐worth” or “self‐efficacy” can help individuals to view weight loss as being within their own control and achievable (Cochrane, 2008 ).
Strengthening relationships with patients with overweight or obesity to enhance trust may also improve adherence with weight‐loss programs. Patients with hypertension who reported having “complete trust” in their healthcare practitioner were more than twice as likely to engage in lifestyle changes to lose weight than those who lacked “complete trust” (Jones, Carson, Bleich, & Cooper, 2012 ). It may be prudent to ensure the healthcare staff implementing weight‐loss programs have sufficient time to foster trust with their patients.
Continued support from healthcare staff may help patients sustain the necessary motivation for lifestyle changes. A retrospective analysis of 14,256 patients in primary care identified consultation frequency as a factor that can predict the success of weight‐management programs (Lenoir, Maillot, Guilbot, & Ritz, 2015 ). Individuals who successfully maintained ≥10% weight loss over 12 months visited the healthcare provider on average 0.65 times monthly compared with an average of 0.48 visits/month in those who did not maintain ≥10% weight loss, and 0.39 visits/month in those who failed to achieve the initial ≥10% weight loss ( p < .001; Lenoir et al., 2015 ).
Educational and environmental factors
It is important to consider a patient's education and environment when formulating a weight loss strategy as environmental factors may need to be challenged to help facilitate weight loss. A family history of obesity and childhood obesity are strongly linked to adult obesity, which is likely to be because of both genetic and behavioral factors (Kral & Rauh, 2010 ). Parents create their child's early food experiences and influence their child's attitudes to eating through learned eating habits and food choices (Kral & Rauh, 2010 ). Families can also impart cultural preferences for less healthy food choices and family food choices may be affected by community factors, such as the local availability and cost of healthy food options (Castro, Shaibi, & Boehm‐Smith, 2009 ). Alongside this, genetic variation in taste sensation may influence the dietary palate and influence food choices (Loper, La Sala, Dotson, & Steinle, 2015 ). For example, sensitivity to 6‐n‐propylthiouracil (PROP) is genetically determined, and PROP‐tasting ability ranges from super taster to nontaster. When offered buffet‐style meals over 3 days, PROP nontasters consumed more energy, and a greater proportion of energy from fat compared with super tasters. So it is possible that a family's genetic profile could contribute to eating choices. To address behavioral factors, it is important to ensure that families have appropriate support and information and that any early signs of weight gain are dealt with promptly.
A healthy home food environment can help individuals improve their diet. In children, key factors are availability of fresh fruit and vegetables at home and parental influence through their own fresh fruit and vegetable intake (Wyse, Wolfenden, & Bisquera, 2015 ). In adults, unhealthy home food environment factors include less healthy food in the home and reliance on fast food ( p = .01) are all predictors of obesity (Emery et al., 2015 ).
Family mealtimes are strongly associated with better dietary intake and a randomized controlled trial to encourage healthy family meals showed a promising reduction in excess weight gain in prepubescent children (Fulkerson et al., 2015 ). Another study showed that adolescents with any level of baseline family meal frequency, 1–2, 3–4, and ≥5 family meals/week, had reduced odds of being affected by overweight or obesity 10 years later than adolescents who never ate family meals (Berge et al., 2015 ). Community health advocates have identified the failure of many families to plan meals or prepare food as a barrier to healthy family eating patterns (Fruh, Mulekar, Hall, Fulkerson et al., 2013 ). Meal planning allows healthy meals to be prepared in advance and frozen for later consumption (Fruh, Mulekar, Hall, Adams et al., 2013 ) and is associated with increased consumption of vegetables and healthier meals compared with meals prepared on impulse (Crawford, Ball, Mishra, Salmon, & Timperio, 2007 ; Hersey et al., 2001 ).
The role of the nurse practitioner
The initial and ongoing interactions between patient and nurse practitioner are keys for the determination of an effective approach and implementation of a weight loss program and subsequent weight maintenance. The initial interaction can be instigated by either the nurse practitioner or the patient and once the decision has been made to manage the patient's weight, the evaluation includes a risk assessment, a discussion about the patient's weight, and treatment goal recommendations (American Nurse Practitioner Foundation, 2013 ). Across this process, it may be advantageous to approach this using objective data and language that is motivational and/or nonjudgmental. Patients may struggle with motivation, and therefore, ongoing discussions around the health benefits and improvements to quality of life as a result of weight loss may be required (American Nurse Practitioner Foundation, 2013 ). It may be valuable to allocate personalized benefits to the weight loss such as playing with children/grandchildren (American Nurse Practitioner Foundation, 2013 ). Treatment approaches encompass nonpharmacological and pharmacological strategies; however, it is important to remember that any pharmacological agent used should be used as an adjunct to nutritional and physical activity strategies (American Nurse Practitioner Foundation, 2013 ). Pharmacotherapy options for weight management are discussed further in the article by Golden in this supplement.
Conclusions/summary
The importance of obesity management is underscored both by the serious health consequences for individuals, but also by its increasing prevalence globally, and across age groups in particular. Obesity promotes a chronic, low‐grade, inflammatory state, which is associated with vascular dysfunction, thrombotic disorders, multiple organ damage, and metabolic dysfunction. These physiological effects ultimately lead to the development of a range of morbidities, including CVD, T2D, OSA, and certain cancers along with many others, as well as causing a significant impact on mortality.
However, even modest weight loss of 5%–10% of total body weight can significantly improve health and well‐being, and further benefits are possible with greater weight loss. Weight loss can help to prevent development of T2D in individuals with obesity and prediabetes and has a positive long‐term impact on cardiovascular mortality. Beneficial, although not curative, effects have also been noted on OSA following >10% weight loss. In addition, weight loss reduces the risk for certain cancer types and has positive effects on most comorbidities including asthma, GERD, liver function, urinary incontinence, fertility, joint pain, and depression.
Weight‐loss programs that include realistic weight loss goals, frequent check‐in, and meal/activity diaries may help individuals to lose weight. Setting realistic weight‐loss goals can be difficult; however, visual resources showing the health and wellness benefit of weight loss may be helpful in discussing realistic goals, and help motivate the patient in maintaining the weight loss. Techniques such as motivational interviewing that focus on addressing resistance to behavioral change in a supportive and optimistic manner may help individuals in integrating these changes to allow them to become part of normal everyday life and thus help with maintaining the weight loss. Positive reinforcement in terms of marked early‐weight loss may also assist in improving adherence, so this should be a key goal for weight‐loss programs. Encouraging feelings of “self‐worth” or “self‐efficacy” can help individuals to view weight loss as being within their own control.
Nurse practitioners play a major role in helping patients achieve weight loss through all aspects of the process including assessment, support, motivation, goal‐setting, management, and treatment. With their in‐depth understanding of the research in the field of obesity and weight management, nurse practitioners are well placed to effect meaningful changes in the weight‐management strategies deployed in clinical practice.
List of helpful resources
| The Obesity Action Coalition (OAC): | This site has educational resources for providers and patients. It also has information on advocacy for patients. |
| Stop Obesity Alliance: | This site has many helpful resources to help prevent obesity bias and helpful educational materials for patients. It also has an excellent tool to help providers discuss the topic of obesity with patients. |
| UConn Rudd Center: | This site is an excellent resource for providers in clinical practice. This site has modules to help providers improve obesity management. |
Acknowledgments
The authors are grateful to Watermeadow Medical for writing assistance in the development of this manuscript. This assistance was funded by Novo Nordisk, who also had a role in the review of the manuscript for scientific accuracy. The author discussed the concept, drafted the outline, commented in detail on the first iteration, made critical revision of later drafts, and has revised and approved the final version for submission.
Dr. Sharon Fruh serves on the Novo Nordisk Obesity Speakers Bureau. In compliance with national ethical guidelines, the author reports no relationship with business or industry that would post a conflict of interest.
Writing and editorial support was provided by Watermeadow Medical, and funded by Novo Nordisk.
The copyright line in this article was changed on 9 August 2018 after online publication.
- American Nurse Practitioner Foundation . (2013). Nurse practitioners and the prevention and treatment of adult obesity—A White Paper of the American Nurse Practitioner Foundation (electronic version) . Summer. Retrieved from https://international.aanp.org/Content/docs/ObesityWhitePaper.pdf
- Araghi, M. H. , Chen, Y. F. , Jagielski, A. , Choudhury, S. , Banerjee, D. , Hussain, S. , … Taheri, S. , et al. (2013). Effectiveness of lifestyle interventions on obstructive sleep apnea (OSA): Systematic review and meta‐analysis . Sleep , 36 ( 10 ), 1553–1562, 1562a–1562e. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barnes, R. D. , & Ivezaj, V. (2015). A systematic review of motivational interviewing for weight loss among adults in primary care . Obesity Reviews , 16 ( 4 ), 304–318. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berge, J. M. , Wall, M. , Hsueh, T. F. , Fulkerson, J. A. , Larson, N. , & Neumark‐Sztainer, D. (2015). The protective role of family meals for youth obesity: 10‐year longitudinal associations . Journal of Pediatrics , 166 ( 2 ), 296–301. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berrington de Gonzalez, A. , Hartge, P. , Cerhan, J. R. , Flint, A. J. , Hannan, L. , MacInnis, R. J. , … Thun, M. J. , et al. (2010). Body‐mass index and mortality among 1.46 million white adults . New England Journal of Medicine , 363 ( 23 ), 2211–2219. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Blokhin, I. O. , & Lentz, S. R. (2013). Mechanisms of thrombosis in obesity . Current Opinion in Hematology , 20 ( 5 ), 437–444 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Booth, A. , Magnuson, A. , Fouts, J. , & Foster, M. (2015). Adipose tissue, obesity and adipokines: Role in cancer promotion . Hormone Molecular Biology and Clinical Investigation , 21 ( 1 ), 57–74. [ PubMed ] [ Google Scholar ]
- Bray, G. , Look, M. , & Ryan, D. (2013). Treatment of the obese patient in primary care: Targeting and meeting goals and expectations . Postgraduate Medical Journal , 125 ( 5 ), 67–77. [ PubMed ] [ Google Scholar ]
- Breyer, B. N. , Phelan, S. , Hogan, P. E. , Rosen, R. C. , Kitabchi, A. E. , Wing, R. R. , … the Look AHEAD Research Group , et al. (2014). Intensive lifestyle intervention reduces urinary incontinence in overweight/obese men with type 2 diabetes: Results from the Look AHEAD trial . Journal of Urology , 192 ( 1 ), 144–149. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brown, J. S. , Wing, R. , Barrett‐Connor, E. , Nyberg, L. M. , Kusek, J. W. , Orchard, T. J. , … Diabetes Prevention Program Research Group , et al. (2006). Lifestyle intervention is associated with lower prevalence of urinary incontinence: The Diabetes Prevention Program . Diabetes Care , 29 ( 2 ), 385–390. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Burt Solorzano, C. M. , & McCartney, C. R. (2010). Obesity and the pubertal transition in girls and boys . Reproduction , 140 ( 3 ), 399–410. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Capodaglio, P. , & Liuzzi, A. (2013). Obesity: A disabling disease or a condition favoring disability ? European Journal of Physical and Rehabilitation Medicine , 49 ( 3 ), 395–398. [ PubMed ] [ Google Scholar ]
- Castro, F. G. , Shaibi, G. Q. , & Boehm‐Smith, E. (2009). Ecodevelopmental contexts for preventing type 2 diabetes in Latino and other racial/ethnic minority populations . Journal of Behavioral Medicine , 32 ( 1 ), 89–105. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cefalu, W. T. , Bray, G. A. , Home, P. D. , Garvey, W. T. , Klein, S. , Pi‐Sunyer, F. X. , … Ryan, D. H. , et al. (2015). Advances in the science, treatment, and prevention of the disease of obesity: Reflections from a diabetes care editors' expert forum . Diabetes Care , 38 ( 8 ), 1567–1582. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Centres for Disease Control and Prevention . (2016). Overweight and obesity . Retrieved from https://www.cdc.gov/obesity/
- Cochrane, G. (2008). Role for a sense of self‐worth in weight‐loss treatments: Helping patients develop self‐efficacy . Canadian Family Physician , 54 ( 4 ), 543–547. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Crawford, D. , Ball, K. , Mishra, G. , Salmon, J. , & Timperio, A. (2007). Which food‐related behaviours are associated with healthier intakes of fruits and vegetables among women ? Public Health Nutrition , 10 ( 3 ), 256–265. [ PubMed ] [ Google Scholar ]
- Dattilo, A. M. , & Kris‐Etherton, P. M. (1992). Effects of weight reduction on blood lipids and lipoproteins: A meta‐analysis . American Journal of Clinical Nutrition , 56 ( 2 ), 320–328. [ PubMed ] [ Google Scholar ]
- Dengo, A. L. , Dennis, E. A. , Orr, J. S. , Marinik, E. L. , Ehrlich, E. , Davy, B. M. , & Davy, K. P. (2010). Arterial destiffening with weight loss in overweight and obese middle‐aged and older adults . Hypertension , 55 ( 4 ), 855–861. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Diabetes Prevention Program ( DPP) Research Group . (2015). Long‐term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15‐year follow‐up: The Diabetes Prevention Program Outcomes Study . Lancet Diabetes & Endocrinology , 3 ( 11 ), 866–875. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Diabetes Prevention Program ( DPP) Research Group , Knowler, W. C. , Fowler, S. E. , Hamman, R. F. , Christophi, C. A. , Hoffman, H. J. , … Nathan, D. M. , et al. (2009). 10‐year follow‐up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study . Lancet , 374 ( 9702 ), 1677–1686. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dobbins, M. , Decorby, K. , & Choi, B. C. (2013). The association between obesity and cancer risk: A meta‐analysis of observational studies from 1985 to 2011 . ISRN Preventive Medicine , 2013 , 680536 10.5402/2013/680536. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eheman, C. , Henley, S. J. , Ballard‐Barbash, R. , Jacobs, E. J. , Schymura, M. J. , Noone, A. M. , … Edwards, B. K. , et al. (2012). Annual Report to the Nation on the status of cancer, 1975–2008, featuring cancers associated with excess weight and lack of sufficient physical activity . Cancer , 118 ( 9 ), 2338–2366. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Emery, C. F. , Olson, K. L. , Lee, V. S. , Habash, D. L. , Nasar, J. L. , & Bodine, A. (2015). Home environment and psychosocial predictors of obesity status among community‐residing men and women . International Journal of Obesity , 39 ( 9 ), 1401–1407. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fabricatore, A. N. , Wadden, T. A. , Higginbotham, A. J. , Faulconbridge, L. F. , Nguyen, A. M. , Heymsfield, S. B. , & Faith, M. S. (2011). Intentional weight loss and changes in symptoms of depression: A systematic review and meta‐analysis . International Journal of Obesity , 35 ( 11 ), 1363–1376. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fabricatore, A. N. , Wadden, T. A. , Womble, L. G. , Sarwer, D. B. , Berkowitz, R. I. , Foster, G. D. , & Brock, J. R. (2007). The role of patients' expectations and goals in the behavioral and pharmacological treatment of obesity . International Journal of Obesity , 31 ( 11 ), 1739–1745. [ PubMed ] [ Google Scholar ]
- Felson, D. T. , Zhang, Y. , Anthony, J. M. , Naimark, A. , & Anderson, J. J. (1992). Weight loss reduces the risk for symptomatic knee osteoarthritis in women. The Framingham Study . Annals of Internal Medicine , 116 ( 7 ), 535–539. [ PubMed ] [ Google Scholar ]
- Foy, C. G. , Lewis, C. E. , Hairston, K. G. , Miller, G. D. , Lang, W. , Jakicic, J. M. , … the Look AHEAD Research Group , et al. (2011). Intensive lifestyle intervention improves physical function among obese adults with knee pain: Findings from the Look AHEAD trial . Obesity (Silver Spring) , 19 ( 1 ), 83–93. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fruh, S. M. , Mulekar, M. S. , Hall, H. R. , Adams, J. R. , Lemley, T. , Evans, B. , & Dierking, J. (2013). Meal‐planning practices with individuals in health disparity zip codes . Journal for Nurse Practitioners , 9 ( 6 ), 344–349. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fruh, S. M. , Mulekar, M. S. , Hall, H. R. , Fulkerson, J. A. , Hanks, R. S. , Lemley, T. , … Dierking, J. , et al. (2013). Perspectives of community health advocates: Barriers to healthy family eating patterns . Journal for Nurse Practitioners , 9 ( 7 ), 416–421. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fulkerson, J. A. , Friend, S. , Flattum, C. , Horning, M. , Draxten, M. , Neumark‐Sztainer, D. , … Kubik, M. , et al. (2015). Promoting healthful family meals to prevent obesity: HOME Plus, a randomized controlled trial . International Journal of Behavioral Nutrition and Physical Activity , 12 , 154. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Goldberg, R. B. , Temprosa, M. G. , Mather, K. J. , Orchard, T. J. , Kitabchi, A. E. , & Watson, K. E. , for the Diabetes Prevention Program Research Group . (2014). Lifestyle and metformin interventions have a durable effect to lower CRP and tPA levels in the diabetes prevention program except in those who develop diabetes . Diabetes Care , 37 ( 8 ), 2253–2260. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Greenburg, D. L. , Lettieri, C. J. , & Eliasson, A. H. (2009). Effects of surgical weight loss on measures of obstructive sleep apnea: A meta‐analysis . American Journal of Medicine , 122 ( 6 ), 535–542. [ PubMed ] [ Google Scholar ]
- Grief, S. N. , & Miranda, R. L. (2010). Weight loss maintenance . American Family Physician , 82 ( 6 ), 630–634. [ PubMed ] [ Google Scholar ]
- Guh, D. P. , Zhang, W. , Bansback, N. , Amarsi, Z. , Birmingham, C. L. , & Anis, A. H. (2009). The incidence of co‐morbidities related to obesity and overweight: A systematic review and meta‐analysis . BMC Public Health , 9 , 88. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Haffner, S. , Temprosa, M. , Crandall, J. , Fowler, S. , Goldberg, R. , Horton, E. , … Diabetes Prevention Program Research Group , et al. (2005). Intensive lifestyle intervention or metformin on inflammation and coagulation in participants with impaired glucose tolerance . Diabetes , 54 ( 5 ), 1566–1572. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hamdy, O. (2016). Obesity . Retrieved from https://emedicine.medscape.com/article/123702-overview
- Haufe, S. , Haas, V. , Utz, W. , Birkenfeld, A. L. , Jeran, S. , Bohnke, J. , … Engeli, S. , et al. (2013). Long‐lasting improvements in liver fat and metabolism despite body weight regain after dietary weight loss . Diabetes Care , 36 ( 11 ), 3786–3792. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hersey, J. , Anliker, J. , Miller, C. , Mullis, R. M. , Daugherty, S. , Das, S. , … Olivia, A. H. , et al. (2001). Food shopping practices are associated with dietary quality in low‐income households . Journal of Nutrition Education , 33 ( Suppl 1 ), S16–S26. [ PubMed ] [ Google Scholar ]
- Hursting, S. D. , & Dunlap, S. M. (2012). Obesity, metabolic dysregulation, and cancer: A growing concern and an inflammatory (and microenvironmental) issue . Annals of the New York Academy of Sciences , 1271 , 82–87. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- International Diabetes Federation . (2006). The IDF consensus worldwide definition of the metabolic syndrome (electronic version). Retrieved from https://www.idf.org/webdata/docs/IDF_Meta_def_final.pdf
- Ip, M. S. , Lam, B. , Ng, M. M. , Lam, W. K. , Tsang, K. W. , & Lam, K. S. (2002). Obstructive sleep apnea is independently associated with insulin resistance . American Journal of Respiratory and Critical Care Medicine , 165 ( 5 ), 670–676. [ PubMed ] [ Google Scholar ]
- Johnson, A. R. , Milner, J. J. , & Makowski, L. (2012). The inflammation highway: Metabolism accelerates inflammatory traffic in obesity . Immunological Reviews , 249 ( 1 ), 218–238. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jones, D. E. , Carson, K. A. , Bleich, S. N. , & Cooper, L. A. (2012). Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure . Patient Education and Counseling , 89 ( 1 ), 57–62. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Juel, C. T. , Ali, Z. , Nilas, L. , & Ulrik, C. S. (2012). Asthma and obesity: Does weight loss improve asthma control? A systematic review . Journal of Asthma and Allergy , 5 , 21–26. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kernan, W. N. , Inzucchi, S. E. , Sawan, C. , Macko, R. F. , & Furie, K. L. (2013). Obesity: A stubbornly obvious target for stroke prevention . Stroke , 44 ( 1 ), 278–286. [ PubMed ] [ Google Scholar ]
- Kort, J. D. , Winget, C. , Kim, S. H. , & Lathi, R. B. (2014). A retrospective cohort study to evaluate the impact of meaningful weight loss on fertility outcomes in an overweight population with infertility . Fertility and Sterility , 101 ( 5 ), 1400–1403. [ PubMed ] [ Google Scholar ]
- Kral, T. V. , & Rauh, E. M. (2010). Eating behaviors of children in the context of their family environment . Physiology & Behavior , 100 ( 5 ), 567–573. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kritchevsky, S. B. , Beavers, K. M. , Miller, M. E. , Shea, M. K. , Houston, D. K. , Kitzman, D. W. , & Nicklas, B. J. (2015). Intentional weight loss and all‐cause mortality: A meta‐analysis of randomized clinical trials . PLoS One , 10 ( 3 ), e0121993. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kuk, J. L. , Ardern, C. I. , Church, T. S. , Sharma, A. M. , Padwal, R. , Sui, X. , … Blair, S. N. , et al. (2011). Edmonton obesity staging system: Association with weight history and mortality risk . Applied Physiology, Nutrition, and Metabolism , 36 ( 4 ), 570–576. [ PubMed ] [ Google Scholar ]
- Kuna, S. T. , Reboussin, D. M. , Borradaile, K. E. , Sanders, M. H. , Millman, R. P. , Zammit, G. , … Sleep AHEAD Research Group of the Look AHEAD Research Group , et al. (2013). Long‐term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes . Sleep , 36 ( 5 ), 641–649A. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lee, J. M. , Pilli, S. , Gebremariam, A. , Keirns, C. C. , Davis, M. M. , Vijan, S. , … Gurney, J. G. , et al. (2010). Getting heavier, younger: Trajectories of obesity over the life course . International Journal of Obesity , 34 ( 4 ), 614–623. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lenoir, L. , Maillot, M. , Guilbot, A. , & Ritz, P. (2015). Primary care weight loss maintenance with behavioral nutrition: An observational study . Obesity (Silver Spring) , 23 ( 9 ), 1771–777. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li, G. , Zhang, P. , Wang, J. , An, Y. , Gong, Q. , Gregg, E. W. , … Bennett, P. H. , et al. (2014). Cardiovascular mortality, all‐cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: A 23‐year follow‐up study . Lancet Diabetes & Endocrinology , 2 ( 6 ), 474–480. [ PubMed ] [ Google Scholar ]
- Li, G. , Zhang, P. , Wang, J. , Gregg, E. W. , Yang, W. , Gong, Q. , … Bennett, P. H. , et al. (2008). The long‐term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: A 20‐year follow‐up study . Lancet , 371 ( 9626 ), 1783–1789. [ PubMed ] [ Google Scholar ]
- Lindstrom, J. , Eriksson, J. G. , Valle, T. T. , Aunola, S. , Cepaitis, Z. , Hakumaki, M. , … Tuomilehto, J. , et al. (2003). Prevention of diabetes mellitus in subjects with impaired glucose tolerance in the Finnish Diabetes Prevention Study: Results from a randomized clinical trial . Journal of the American Society of Nephrology , 14 ( 7 Suppl 2 ), S108–S113. [ PubMed ] [ Google Scholar ]
- Lindstrom, J. , Ilanne‐Parikka, P. , Peltonen, M. , Aunola, S. , Eriksson, J. G. , Hemio, K. , … Finnish Diabetes Prevention Study Group , et al. (2006). Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: Follow‐up of the Finnish Diabetes Prevention Study . Lancet , 368 ( 9548 ), 1673–1679. [ PubMed ] [ Google Scholar ]
- Linkov, F. , Maxwell, G. L. , Felix, A. S. , Lin, Y. , Lenzner, D. , Bovbjerg, D. H. , … DeLany, J. P. , et al. (2012). Longitudinal evaluation of cancer‐associated biomarkers before and after weight loss in RENEW study participants: Implications for cancer risk reduction . Gynecologic Oncology , 125 ( 1 ), 114–119. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Loper, H. B. , La Sala, M. , Dotson, C. , & Steinle, N. (2015). Taste perception, associated hormonal modulation, and nutrient intake . Nutrition Reviews , 73 ( 2 ), 83–91. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lv, N. , Xiao, L. , & Ma, J. (2015). Weight management interventions in adult and pediatric asthma populations: A systematic review . J Pulm Respir Med , 5 ( 232 ), pii: 1000232. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Martin‐Rodriguez, E. , Guillen‐Grima, F. , Marti, A. , & Brugos‐Larumbe, A. (2015). Comorbidity associated with obesity in a large population: The APNA study . Obesity Research & Clinical Practice , 9 ( 5 ), 435–447. [ PubMed ] [ Google Scholar ]
- Musunuru, K. (2010). Atherogenic dyslipidemia: Cardiovascular risk and dietary intervention . Lipids , 45 ( 10 ), 907–914. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nanchahal, K. , Townsend, J. , Letley, L. , Haslam, D. , Wellings, K. , & Haines, A. (2009). Weight‐management interventions in primary care: A pilot randomised controlled trial . British Journal of General Practice , 59 ( 562 ), e157–e166. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Osunlana, A. M. , Asselin, J. , Anderson, R. , Ogunleye, A. A. , Cave, A. , Sharma, A. M. , & Campbell‐Scherer, D. L.. (2015). 5As team obesity intervention in primary care: Development and evaluation of shared decision‐making weight management tools . Clinical Obesity , 5 ( 4 ), 219–225. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pan, X. R. , Li, G. W. , Hu, Y. H. , Wang, J. X. , Yang, W. Y. , An, Z. X. , … Howard, B. V. , et al. (1997). Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and diabetes study . Diabetes Care , 20 ( 4 ), 537–544. [ PubMed ] [ Google Scholar ]
- Parker, E. D. , & Folsom, A. R. (2003). Intentional weight loss and incidence of obesity‐related cancers: The Iowa Women's Health Study . International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity , 27 ( 12 ), 1447–1452. [ PubMed ] [ Google Scholar ]
- Patel, N. S. , Doycheva, I. , Peterson, M. R. , Hooker, J. , Kisselva, T. , Schnabl, B. , … Loomba, R. , et al. (2015). Effect of weight loss on magnetic resonance imaging estimation of liver fat and volume in patients with nonalcoholic steatohepatitis . Clinical Gastroenterology and Hepatology , 13 ( 3 ), 561–568 e561. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Peterson, N. D. , Middleton, K. R. , Nackers, L. M. , Medina, K. E. , Milsom, V. A. , & Perri, M. G. (2014). Dietary self‐monitoring and long‐term success with weight management . Obesity (Silver Spring) , 22 ( 9 ), 1962–1967. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Petry, N. M. , Barry, D. , Pietrzak, R. H. , & Wagner, J. A. (2008). Overweight and obesity are associated with psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions . 70 ( 3 ), 288–297. [ PubMed ] [ Google Scholar ]
- Pi‐Sunyer, X. (2009). The medical risks of obesity . Postgraduate Medicine , 121 ( 6 ), 21–33. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Prospective Studies Collaboration , Whitlock, G. , Lewington, S. , Sherliker, P. , Clarke, R. , Emberson, J. , … Peto, R. , et al. (2009). Body‐mass index and cause‐specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies . Lancet , 373 ( 9669 ), 1083–1096. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pulgaron, E. R. (2013). Childhood obesity: A review of increased risk for physical and psychological comorbidities . Clin Ther 35 ( 1 ), A18–A32. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ratner, R. , Goldberg, R. , Haffner, S. , Marcovina, S. , Orchard, T. , Fowler, S. , … Diabetes Prevention Program Research Group , et al. (2005). Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the diabetes prevention program . Diabetes Care , 28 ( 4 ), 888–894. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rogge, M. M. , & Gautam, B. (2017). Biology of obesity and weight regain: Implications for clinical practice . Journal of the American Association of Nurse Practitioners , 29 (Supplement 1), S15–S29. [ PubMed ] [ Google Scholar ]
- Romero‐Corral, A. , Caples, S. M. , Lopez‐Jimenez, F. , & Somers, V. K. (2010). Interactions between obesity and obstructive sleep apnea: Implications for treatment . Chest , 137 ( 3 ), 711–719. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sakai, R. , Matsui, S. , Fukushima, M. , Yasuda, H. , Miyauchi, H. , & Miyachi, Y. (2005). Prognostic factor analysis for plaque psoriasis . Dermatology , 211 ( 2 ), 103–106. [ PubMed ] [ Google Scholar ]
- Singh, M. , Lee, J. , Gupta, N. , Gaddam, S. , Smith, B. K. , Wani, S. B. , … Sharma, P. , et al. (2013). Weight loss can lead to resolution of gastroesophageal reflux disease symptoms: A prospective intervention trial . Obesity (Silver Spring) , 21 ( 2 ), 284–290. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Skinner, A. C. , & Skelton, J. A. (2014). Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012 . JAMA Pediatrics , 168 ( 6 ), 561–566. [ PubMed ] [ Google Scholar ]
- Smith, S. A. , Hulsey, T. , & Goodnight, W. (2008). Effects of obesity on pregnancy . J Obstet Gynecol Neonatal Nurs , 37 ( 2 ), 176–184. [ PubMed ] [ Google Scholar ]
- The Global BMI Mortality Collaboration . (2016). Body‐mass index and all‐cause mortality: Individual participant‐data meta‐analysis of 239 prospective studies in four continents . Lancet , 388 , 734–736. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- The National Weight Control Registry ( NWCR) . (2016). NCWR facts . Retrieved from https://www.nwcr.ws/
- Tuomilehto, J. , Lindstrom, J. , Eriksson, J. G. , Valle, T. T. , Hamalainen, H. , Ilanne‐Parikka, P. , … Finnish Diabetes Prevention Study Group , et al. (2001). Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance . New England Journal of Medicine , 344 ( 18 ), 1343–1350. [ PubMed ] [ Google Scholar ]
- Weinsier, R. L. , & Ullmann, D. O. (1993). Gallstone formation and weight loss . Obesity Research , 1 ( 1 ), 51–56. [ PubMed ] [ Google Scholar ]
- Wensveen, F. M. , Valentic, S. , Sestan, M. , Turk Wensveen, T. , & Polic, B. (2015). The "Big Bang" in obese fat: Events initiating obesity‐induced adipose tissue inflammation . European Journal of Immunology , 45 ( 9 ), 2446–2456. [ PubMed ] [ Google Scholar ]
- Whitaker, R. C. , Wright, J. A. , Pepe, M. S. , Seidel, K. D. , & Dietz, W. H. (1997). Predicting obesity in young adulthood from childhood and parental obesity . New England Journal of Medicine , 337 ( 13 ), 869–873. [ PubMed ] [ Google Scholar ]
- World Health Organization (WHO) . (2016a). 10 Facts on obesity . Retrieved from https://www.who.int/features/factfiles/obesity/facts/en/
- World Health Organization (WHO) . (2016b). Obesity . Retrieved from https://www.who.int/topics/obesity/en/
- Wyse, R. , Wolfenden, L. , & Bisquera, A. (2015). Characteristics of the home food environment that mediate immediate and sustained increases in child fruit and vegetable consumption: Mediation analysis from the Healthy Habits cluster randomised controlled trial . International Journal of Behavioral Nutrition and Physical Activity , 12 , 118. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yang, L. , & Colditz, G. A. (2015). Prevalence of overweight and obesity in the United States, 2007–2012 . JAMA Internal Medicine , 175 ( 8 ), 1412–1413. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yosipovitch, G. , DeVore, A. , & Dawn, A. (2007). Obesity and the skin: Skin physiology and skin manifestations of obesity . J Am Acad Dermatol , 56 ( 6 ), 901–916; quiz 917–920. [ PubMed ] [ Google Scholar ]
Home — Essay Samples — Nursing & Health — Public Health Issues — Obesity
Essay Examples on Obesity
Hook examples for obesity essays, "the silent epidemic among us" hook.
"Obesity silently creeps into our lives, affecting millions. Explore the hidden health crisis, its causes, and its far-reaching consequences on individuals and society."
"From Childhood to Adulthood: Battling Obesity" Hook
"Childhood obesity often follows us into adulthood. Share stories of individuals who have embarked on journeys of transformation and discuss the challenges they face."
"Obesity's Toll on Public Health" Hook
"Obesity is a public health crisis with wide-ranging effects. Investigate the strain on healthcare systems, the rise of related diseases, and the economic impact of obesity."
"The Cultural Shift: Food, Technology, and Sedentary Lifestyles" Hook
"Examine how cultural factors, including dietary habits, technology use, and sedentary lifestyles, have contributed to the obesity epidemic. What can we learn from these trends?"
"Breaking the Cycle: Strategies for Prevention" Hook
"Prevention is key to combating obesity. Discuss effective strategies for preventing obesity in children and adults, from education to policy changes."
"The Psychological Battle: Obesity and Mental Health" Hook
"Obesity often intersects with mental health challenges. Explore the complex relationship between obesity and mental well-being, as well as the stigma attached to it."
"Shifting Perspectives: Celebrating Body Positivity" Hook
"In the midst of the obesity crisis, the body positivity movement is gaining ground. Discuss the importance of promoting self-acceptance and diverse body images."
Obesity in America: a Growing Epidemic
Global obesity epidemic: causes, effects, and treatments, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
The Issue of Obesity and Way of Its Prevention
A worldwide epidemic of obesity and ways to handle it, the most common causes of obesity, the problem of obesity and the unhealthy lifestyle among the us citizens, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Obesity in America: Causes, Effects, and Ways to Combat
An increasing in obesity both in adults and children in united states, the issues of the obesity and the american problem, obesity in the united states and ways to avoid it, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
Obesity as a Stigma Or a Threat to Health
Why obesity should be classified a disease, don’t blame the eater': the issue of america’s growing weight, childhood obesity, obesity and its effects in the united kingdom, analysis of the theme of fast food and obesity in the article "don’t blame the eater", the main causes of obesity in america, careless consuming and lazy living: obesity in america, the effect of obesity on depression, analysis of the causes of obesity, the role of food companies in rising rate of obesity in america, the causes for the obesity epidemic in america, obesity as one of the most important social problems in america, the problem of obesity among college students and solutions to combat it, age and socio economic issues as risk factors of obesity, childhood obesity: prevention & treatment, the need for healthier lifestyle campaigns to prevent the issue of overweight and obesity in singapore, obesity epidemic in america and the factors contributing to it, the factors of the problem of obesity in america, actions needed to prevent childhood obesity in the usa.
Obesity is a condition in which excess body fat has accumulated to such an extent that it may have a negative effect on health. Medical organizations tend to classify people as obese based on body mass index (BMI) – a ratio of a person's weight in kilograms to the square of their height in meters.
There are three types of obesity: Class 1 (low-risk) obesity, if BMI is 30.0 to 34.9; Class 2 (moderate-risk) obesity, if BMI is 35.0 to 39.9; Class 3 (high-risk) obesity, if BMI is equal to or greater than 40.0.
The major contributors to obesity are: diet, sedentary lifestyle, genetics, other illnesses, social determinants, gut bacteria, and other factors.
Excessive body weight has a strong link to many diseases and conditions, particularly cardiovascular diseases, diabetes mellitus type 2, obstructive sleep apnea, certain types of cancer, osteoarthritis, and asthma. As a result, obesity has been found to reduce life expectancy.
Most of the world's population live in countries where overweight and obesity kills more people than underweight. 39 million children under the age of 5 were overweight or obese in 2020. Worldwide obesity has nearly tripled since 1975. From 1999-2000 through 2017-March 2020, US obesity prevalence increased from 30.5% to 41.9%.
Relevant topics
- Eating Disorders
- Drug Addiction
- Mental Health
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Bibliography
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About Journal of Molecular Cell Biology
- Society affiliations
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Obesity: causes, consequences, treatments, and challenges.
- Article contents
- Figures & tables
- Supplementary Data
Obesity: causes, consequences, treatments, and challenges, Journal of Molecular Cell Biology , Volume 13, Issue 7, July 2021, Pages 463–465, https://doi.org/10.1093/jmcb/mjab056
- Permissions Icon Permissions
Obesity has become a global epidemic and is one of today’s most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer ( Bluher, 2019 ).
Obesity is mainly caused by imbalanced energy intake and expenditure due to a sedentary lifestyle coupled with overnutrition. Excess nutrients are stored in adipose tissue (AT) in the form of triglycerides, which will be utilized as nutrients by other tissues through lipolysis under nutrient deficit conditions. There are two major types of AT, white AT (WAT) and brown AT, the latter is a specialized form of fat depot that participates in non-shivering thermogenesis through lipid oxidation-mediated heat generation. While WAT has been historically considered merely an energy reservoir, this fat depot is now well known to function as an endocrine organ that produces and secretes various hormones, cytokines, and metabolites (termed as adipokines) to control systemic energy balance. Studies over the past decade also show that WAT, especially subcutaneous WAT, could undergo ‘beiging’ remodeling in response to environmental or hormonal perturbation. In the first paper of this special issue, Cheong and Xu (2021) systematically review the recent progress on the factors, pathways, and mechanisms that regulate the intercellular and inter-organ crosstalks in the beiging of WAT. A critical but still not fully addressed issue in the adipose research field is the origin of the beige cells. Although beige adipocytes are known to have distinct cellular origins from brown and while adipocytes, it remains unclear on whether the cells are from pre-existing mature white adipocytes through a transdifferentiation process or from de novo differentiation of precursor cells. AT is a heterogeneous tissue composed of not only adipocytes but also nonadipocyte cell populations, including fibroblasts, as well as endothelial, blood, stromal, and adipocyte precursor cells ( Ruan, 2020 ). The authors examined evidence to show that heterogeneity contributes to different browning capacities among fat depots and even within the same depot. The local microenvironment in WAT, which is dynamically and coordinately controlled by inputs from the heterogeneous cell types, plays a critical role in the beige adipogenesis process. The authors also examined key regulators of the AT microenvironment, including vascularization, the sympathetic nerve system, immune cells, peptide hormones, exosomes, and gut microbiota-derived metabolites. Given that increasing beige fat function enhances energy expenditure and consequently reduces body weight gain, identification and characterization of novel regulators and understanding their mechanisms of action in the beiging process has a therapeutic potential to combat obesity and its associated diseases. However, as noticed by the authors, most of the current pre-clinical research on ‘beiging’ are done in rodent models, which may not represent the exact phenomenon in humans ( Cheong and Xu, 2021 ). Thus, further investigations will be needed to translate the findings from bench to clinic.
While both social–environmental factors and genetic preposition have been recognized to play important roles in obesity epidemic, Gao et al. (2021) present evidence showing that epigenetic changes may be a key factor to explain interindividual differences in obesity. The authors examined data on the function of DNA methylation in regulating the expression of key genes involved in metabolism. They also summarize the roles of histone modifications as well as various RNAs such as microRNAs, long noncoding RNAs, and circular RNAs in regulating metabolic gene expression in metabolic organs in response to environmental cues. Lastly, the authors discuss the effect of lifestyle modification and therapeutic agents on epigenetic regulation of energy homeostasis. Understanding the mechanisms by which lifestyles such as diet and exercise modulate the expression and function of epigenetic factors in metabolism should be essential for developing novel strategies for the prevention and treatment of obesity and its associated metabolic diseases.
A major consequence of obesity is type 2 diabetes, a chronic disease that occurs when body cannot use and produce insulin effectively. Diabetes profoundly and adversely affects the vasculature, leading to various cardiovascular-related diseases such as atherosclerosis, arteriosclerotic, and microvascular diseases, which have been recognized as the most common causes of death in people with diabetes ( Cho et al., 2018 ). Love et al. (2021) systematically review the roles and regulation of endothelial insulin resistance in diabetes complications, focusing mainly on vascular dysfunction. The authors review the vasoprotective functions and the mechanisms of action of endothelial insulin and insulin-like growth factor 1 signaling pathways. They also examined the contribution and impart of endothelial insulin resistance to diabetes complications from both biochemical and physiological perspectives and evaluated the beneficial roles of many of the medications currently used for T2D treatment in vascular management, including metformin, thiazolidinediones, glucagon-like receptor agonists, dipeptidyl peptidase-4 inhibitors, sodium-glucose cotransporter inhibitors, as well as exercise. The authors present evidence to suggest that sex differences and racial/ethnic disparities contribute significantly to vascular dysfunction in the setting of diabetes. Lastly, the authors raise a number of very important questions with regard to the role and connection of endothelial insulin resistance to metabolic dysfunction in other major metabolic organs/tissues and suggest several insightful directions in this area for future investigation.
Following on from the theme of obesity-induced metabolic dysfunction, Xia et al. (2021) review the latest progresses on the role of membrane-type I matrix metalloproteinase (MT1-MMP), a zinc-dependent endopeptidase that proteolytically cleaves extracellular matrix components and non-matrix proteins, in lipid metabolism. The authors examined data on the transcriptional and post-translational modification regulation of MT1-MMP gene expression and function. They also present evidence showing that the functions of MT1-MMP in lipid metabolism are cell specific as it may either promote or suppress inflammation and atherosclerosis depending on its presence in distinct cells. MT1-MMP appears to exert a complex role in obesity for that the molecule delays the progression of early obesity but exacerbates obesity at the advanced stage. Because inhibition of MT1-MMP can potentially lower the circulating low-density lipoprotein cholesterol levels and reduce the risk of cancer metastasis and atherosclerosis, the protein has been viewed as a very promising therapeutic target. However, challenges remain in developing MT1-MMP-based therapies due to the tissue-specific roles of MT1-MMP and the lack of specific inhibitors for this molecule. Further investigations are needed to address these questions and to develop MT1-MMP-based therapeutic interventions.
Lastly, Huang et al. (2021) present new findings on a critical role of puromycin-sensitive aminopeptidase (PSA), an integral non-transmembrane enzyme that catalyzes the cleavage of amino acids near the N-terminus of polypeptides, in NAFLD. NAFLD, ranging from simple nonalcoholic fatty liver to the more aggressive subtype nonalcoholic steatohepatitis, has now become the leading chronic liver disease worldwide ( Loomba et al., 2021 ). At present, no effective drugs are available for NAFLD management in the clinic mainly due to the lack of a complete understanding of the mechanisms underlying the disease progress, reinforcing the urgent need to identify and validate novel targets and to elucidate their mechanisms of action in NAFLD development and pathogenesis. Huang et al. (2021) found that PSA expression levels were greatly reduced in the livers of obese mouse models and that the decreased PSA expression correlated with the progression of NAFLD in humans. They also found that PSA levels were negatively correlated with triglyceride accumulation in cultured hepatocytes and in the liver of ob/ob mice. Moreover, PSA suppresses steatosis by promoting lipogenesis and attenuating fatty acid β-oxidation in hepatocytes and protects oxidative stress and lipid overload in the liver by activating the nuclear factor erythroid 2-related factor 2, the master regulator of antioxidant response. These studies identify PSA as a pivotal regulator of hepatic lipid metabolism and suggest that PSA may be a potential biomarker and therapeutic target for treating NAFLD.
In summary, papers in this issue review our current knowledge on the causes, consequences, and interventions of obesity and its associated diseases such as type 2 diabetes, NAFLD, and cardiovascular disease ( Cheong and Xu, 2021 ; Gao et al., 2021 ; Love et al., 2021 ). Potential targets for the treatment of dyslipidemia and NAFLD are also discussed, as exemplified by MT1-MMP and PSA ( Huang et al., 2021 ; Xia et al., 2021 ). It is noted that despite enormous effect, few pharmacological interventions are currently available in the clinic to effectively treat obesity. In addition, while enhancing energy expenditure by browning/beiging of WAT has been demonstrated as a promising alternative approach to alleviate obesity in rodent models, it remains to be determined on whether such WAT reprogramming is effective in combating obesity in humans ( Cheong and Xu, 2021 ). Better understanding the mechanisms by which obesity induces various medical consequences and identification and characterization of novel anti-obesity secreted factors/soluble molecules would be helpful for developing effective therapeutic treatments for obesity and its associated medical complications.
Bluher M. ( 2019 ). Obesity: global epidemiology and pathogenesis . Nat. Rev. Endocrinol . 15 , 288 – 298 .
Google Scholar
Cheong L.Y. , Xu A. ( 2021 ). Intercellular and inter-organ crosstalk in browning of white adipose tissue: molecular mechanism and therapeutic complications . J. Mol. Cell Biol . 13 , 466 – 479 .
Cho N.H. , Shaw J.E. , Karuranga S. , et al. ( 2018 ). IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045 . Diabetes Res. Clin. Pract . 138 , 271 – 281 .
Gao W. , Liu J.-L. , Lu X. , et al. ( 2021 ). Epigenetic regulation of energy metabolism in obesity . J. Mol. Cell Biol . 13 , 480 – 499 .
Huang B. , Xiong X. , Zhang L. , et al. ( 2021 ). PSA controls hepatic lipid metabolism by regulating the NRF2 signaling pathway . J. Mol. Cell Biol . 13 , 527 – 539 .
Loomba R. , Friedman S.L. , Shulman G.I. ( 2021 ). Mechanisms and disease consequences of nonalcoholic fatty liver disease . Cell 184 , 2537 – 2564 .
Love K.M. , Barrett E.J. , Malin S.K. , et al. ( 2021 ). Diabetes pathogenesis and management: the endothelium comes of age . J. Mol. Cell Biol . 13 , 500 – 512 .
Ruan H.-B. ( 2020 ). Developmental and functional heterogeneity of thermogenic adipose tissue . J. Mol. Cell Biol . 12 , 775 – 784 .
Xia X.-D. , Alabi A. , Wang M. , et al. ( 2021 ). Membrane-type I matrix metalloproteinase (MT1-MMP), lipid metabolism, and therapeutic implications . J. Mol. Cell Biol . 13 , 513 – 526 .
Author notes
Shanghai Diabetes Institute, Shanghai Key Laboratory of Diabetes Mellitus, Shanghai Clinical Center for Diabetes, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai 200233, China E-mail: [email protected]
| Month: | Total Views: |
|---|---|
| October 2021 | 130 |
| November 2021 | 124 |
| December 2021 | 74 |
| January 2022 | 81 |
| February 2022 | 149 |
| March 2022 | 125 |
| April 2022 | 146 |
| May 2022 | 128 |
| June 2022 | 123 |
| July 2022 | 115 |
| August 2022 | 101 |
| September 2022 | 123 |
| October 2022 | 183 |
| November 2022 | 199 |
| December 2022 | 151 |
| January 2023 | 191 |
| February 2023 | 298 |
| March 2023 | 466 |
| April 2023 | 545 |
| May 2023 | 632 |
| June 2023 | 831 |
| July 2023 | 388 |
| August 2023 | 559 |
| September 2023 | 495 |
| October 2023 | 515 |
| November 2023 | 477 |
| December 2023 | 394 |
| January 2024 | 444 |
| February 2024 | 504 |
| March 2024 | 525 |
| April 2024 | 661 |
| May 2024 | 664 |
| June 2024 | 464 |
| July 2024 | 329 |
| August 2024 | 288 |
Email alerts
Citing articles via, affiliations.
- Online ISSN 1759-4685
- Copyright © 2024 Chinese Academy of Sciences
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

IMAGES
VIDEO
COMMENTS
This essay aims to shed light on the conclusion for obesity, addressing its implications and potential solutions. Through careful analysis and research, we will uncover the multifaceted nature of this problem and explore the urgent need for action.
Conclusion: Obesity can lead to sudden death, heart attack, diabetes and may unwanted illnesses. Stop it by making healthy choices. Essay on Obesity (Essay 2 – 250 Words) Obesity has become a big concern for the youth of today’s generation. Obesity is defined as a medical condition in which an individual gains excessive body fat.
Obesity poses what is arguably one of the most significant threats to population health that we currently face. The data presented in this book highlight just how common obesity has become in children and in adults across the globe, and how it impacts disproportionately on the poor.
End your essay with a conclusion by restating your research and tying it to your thesis statement. You can also propose possible solutions to control obesity in your conclusion. Make sure that your conclusion is short yet powerful.
Conclusion. In summary, obesity is a major cause of premature deaths in the United States and around the world. This health condition occurs when there is excess accumulation of body fat, caused by unhealthy lifestyles. Obesity is largely associated with several killer diseases like high blood pressure, diabetes, and diseases of the heart.
Bridging the Evidence Gap in Obesity Prevention identifies a new approach to decision making and research on obesity prevention to use a systems perspective to gain a broader understanding of the context of obesity and the many factors that influence it.
Conclusions. Over one third of U.S. adults have obesity. Obesity is associated with a range of comorbidities, including diabetes, cardiovascular disease, obstructive sleep apnea, and cancer; however, modest weight loss in the 5%–10% range, and above, can significantly improve health‐related outcomes.
In conclusion, obesity is a complex issue with multiple causes and significant effects on individuals and society. Poor dietary habits, sedentary lifestyles, and genetic factors contribute to its prevalence.
Obesity, a chronic disease characterized by excessive body fat accumulation, has become a global epidemic in recent decades. This essay aims to examine the causes, effects, and treatment approaches related to obesity. It begins by discussing the primary causes of obesity, including genetic factors, sedentary... Obesity.
In summary, papers in this issue review our current knowledge on the causes, consequences, and interventions of obesity and its associated diseases such as type 2 diabetes, NAFLD, and cardiovascular disease (Cheong and Xu, 2021; Gao et al., 2021; Love et al., 2021).