Spondylolisthesis: Definition, Causes, Symptoms, and Treatment
by Dave Harrison, MD • Last updated November 26, 2022
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)

What is Spondylolisthesis?
The spine is comprised of 33 bones, called vertebra , stacked on top of each other interspaced by discs . Spondylolisthesis is a condition where one vertebra slips forward or backwards relative to the vertebra below. More specifically, retrolisthesis is when the vertebra slips posteriorly or backwards, and anterolisthesis is when the vertebra slips anteriorly or forward.
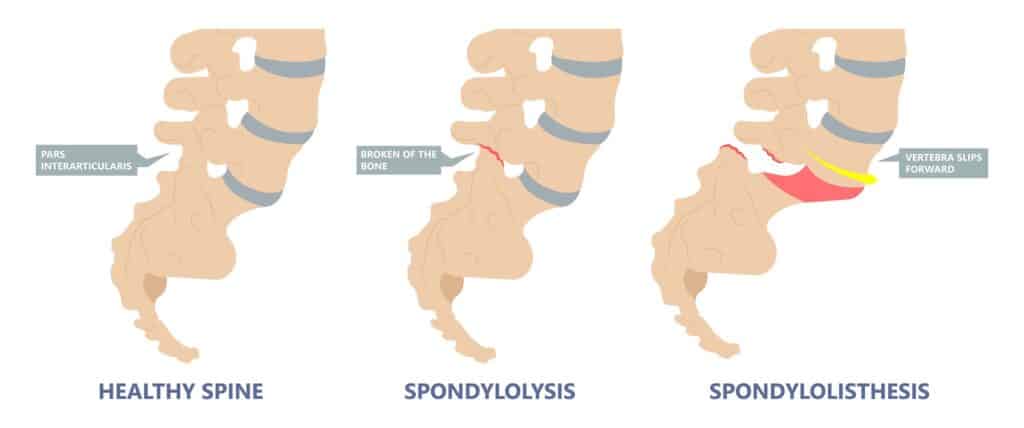
Spondylosis vs Spondylolisthesis
Spondylosis and Spondylolisthesis are different conditions. They can be related but are not the same. Spondylosis refers to a fracture of a small bone, called the pars interarticularis, which connects the facet joint of the vertebra to the one below. This may lead to instability and ultimately slippage of the vertebra. Spondylolisthesis, on the other hand, refers to slippage of the vertebra in relation to the one below.
Types and Causes of Spondylolisthesis
There are several types of spondylolisthesis, often classified by their underlying cause:
Degenerative Spondylolisthesis
Degenerative spondylolisthesis is the most common cause, and is due to general wear and tear on the spine. Overtime, the bones and ligaments which hold the spine together may become weak and unstable.
Isthmic Spondylolisthesis
Isthmic spondylolisthesis is the result of another condition, called “ spondylosis “. Spondylosis refers to a fracture of a small bone, called the pars interarticularis, which connects the facet joint of the vertebra to the one below. If this interconnecting bone is broken, it can lead to slippage of the vertebra. This can sometimes occur during childhood or adolsence but go unnoticed until adulthood when degenerative changes cause worsening slippage.
Congenital Spondylolisthesis
Congenital spondylolisthesis occurs when the bones do not form correctly during fetal development
Traumatic Spondylolisthesis
Traumatic spondylolisthesis is the result of an injury such as a motor vehicle crash
Pathologic Spondyloslisthesis
Pathologic spondylolisthesis is when other disorders weaken the points of attachment in the spine. This includes osteoporosis, tumors, or infection that affect the bones and ligaments causing them to slip.
Iatrogenic Spondylolisthesis
Iatrogenic spondylolisthesis is the result of a prior surgery. Some operations of the spine, such as a laminectomy, may lead to instability. This can cause the vertebra to slip post operatively.
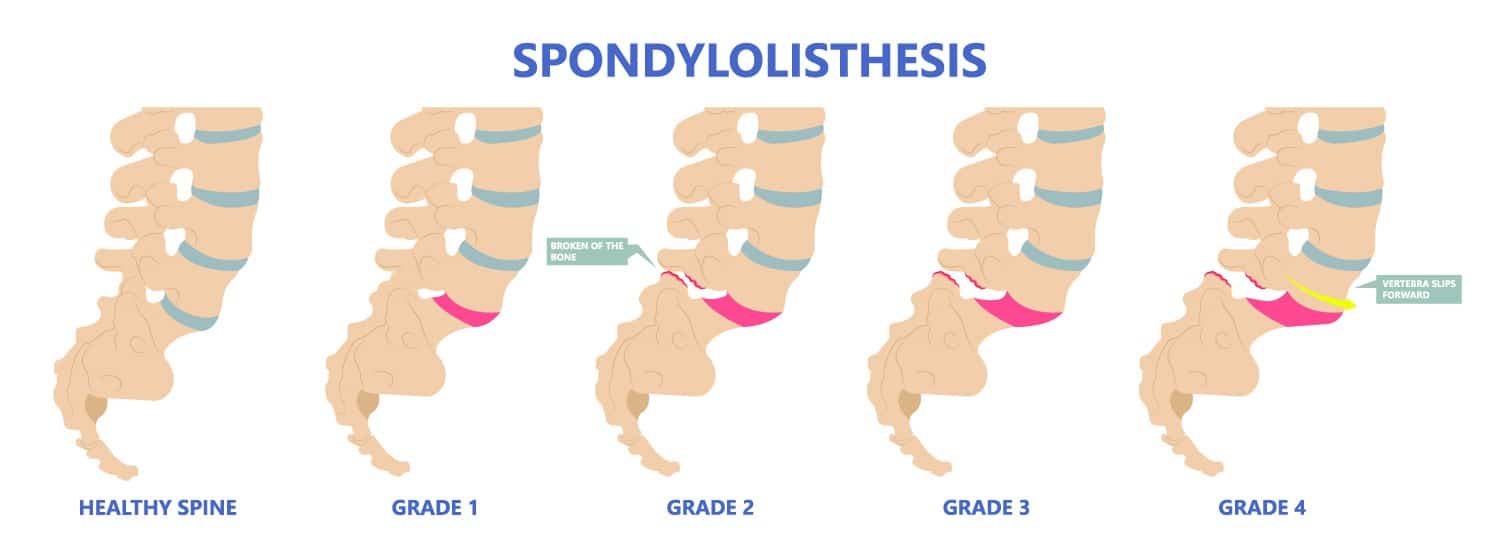
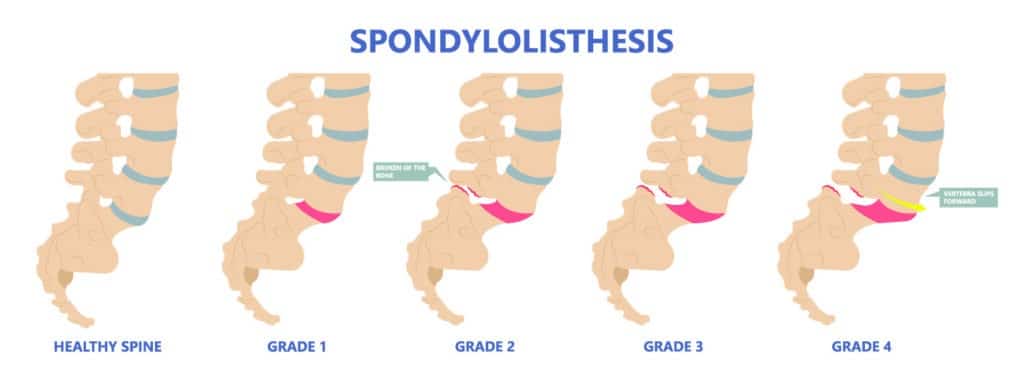
Spondylolisthesis Grades
Spondylolisthesis is classified based on the degree of slippage relative to the vertebra below
- Grade 1 : 1 – 25 % forward slip. This degree of slippage is usually asymptomatic.
- Grade 2: 26 – 50 % forward slip. May cause mild symptoms such as stiffness and pain in your lower back after physical activity, but it’s not severe enough to affect your everyday activities.
- Grade 3 : 51 – 75 % forward slip. May cause moderate symptoms such as pain after physical activity or sitting for long periods.
- Grade 4: 76 – 99% forward slip. May cause moderate to severe symptoms.
- Grade 5: Is when the vertebra has slipped completely of the spinal column. This is a severe condition known as “spondyloptysis”.
Symptoms of Spondylolisthesis
Spondylolisthesis can cause compression of spinal nerves and in severe cases, the spinal cord. The symptoms will depend on which vertebra is affected.
Cervical Spondylolisthesis (neck)
- Arm numbness or tingling
- Arm weakness
Lumbar Spondylolisthesis (low back)
- Buttock pain
- Leg numbness or tingling
- Leg weakness
Diagnosing Spondylolisthesis
Your doctor may order imaging tests to confirm the diagnosis and determine the severity of your spondylolisthesis. The most common imaging tests used include:
- X-rays : X-rays can show the alignment of the vertebrae and any signs of slippage.
- CT scan: A CT scan can provide detailed images of the bones and soft tissues in your back, allowing your doctor to see any damage or abnormalities.
- MRI: An MRI can show the spinal cord and nerves, as well as any herniated discs or other soft tissue abnormalities.
Treatments for Spondylolisthesis
Medications.
For those experiencing pain, oral medications are first line treatments. This includes non-steroidal anti-inflammatory medications (NSAIDs) such as ibuprofen, acetaminophen, or in severe cases opioids or muscle relaxants (with extreme caution). Topical medications such as lidocaine patches are also sometimes used.
Physical Therapy
Physical therapy can help improve mobility and strengthen muscles around your spine to stabilize your neck and lower back. You may also receive stretching exercises to improve flexibility and balance exercises to improve coordination.
Surgery is reserved for severe cases of spondylolisthesis in which there is a high degree of instability and symptoms of nerve compression.
In these cases a spinal fusion may be necessary. This surgery joins two or more vertebra together using rods and screws, in order to improve stability.
Reference s
- Alfieri A, Gazzeri R, Prell J, Röllinghoff M. The current management of lumbar spondylolisthesis. J Neurosurg Sci. 2013 Jun;57(2):103-13. PMID: 23676859.
- Stillerman CB, Schneider JH, Gruen JP. Evaluation and management of spondylolysis and spondylolisthesis. Clin Neurosurg. 1993;40:384-415. PMID: 8111991.
About the Author
Dave Harrison, MD
Dr. Harrison is a board certified Emergency Physician with a part time appointment at San Francisco General Medical Center and is an Assistant Clinical Professor-Volunteer at the UCSF School of Medicine. Dr. Harrison attended medical school at Tufts University and completed his Emergency Medicine residency at the University of Southern California. Dr. Harrison manages the editorial process for SpineInfo.com.

- Our Reviews
- Our Hospitals and Treatment Centers
- Interventional Pain Management
- Orthopedic Spine Surgery
- Atypical Face Pain
- Carpal Tunnel Syndrome
- Complex Regional Pain Syndrome
- Degenerative Disc Disease
- Failed Back Surgery
- Fibromyalgia
- Headaches and Migraines
- Minimally Invasive Spine Surgery
- Muscle Spasms
- Pancreatitis
- Pelvic Pain
- Peripheral Neuropathy
- Peripheral Vascular Disease
- Phantom Limb Pain
- Post-Operative Pain
- Anterior Cervical Discectomy And Fusion
- Caudal Epidural With Lysis Of Adhesions
- Cervical Fusion
- Electroencephalography
- Electromyography and Nerve Conduction Velocity Studies
- Epidural Steroid Injections
- Facet Injections
- IFuse Implant System
- Intrathecal Pump
- Kyphoplasty
- Laminectomy And Fusion
- Medial Branch Blocks and Neurotomies
- Microdiscectomy
- Pain Management
- Peripheral Field Stimulators
- Selective Nerve Root Blocks
- Small And Large Joint Injections
- Patient Portal
- Accepted Insurance
- Data Breach Notification
- Notice of Privacy Practices

Spondylolisthesis: Understanding Causes, Symptoms & Treatment
Are you experiencing lower back pain that won't go away? Have you or a loved one recently been diagnosed with spondylolisthesis? If so, you're not alone. Spondylolisthesis is a common condition that affects the spine, and understanding its causes, symptoms, and treatment is crucial for managing and improving your quality of life.
This blog post will explore everything you need about spondylolisthesis, including its various forms, underlying causes, and effective treatment options. So, whether you're dealing with this condition or simply looking to educate yourself on this joint spine issue, keep reading to understand better spondylolisthesis and how to address it effectively.

What is Spondylolisthesis?
Spondylolisthesis is a common condition that affects the spine and can cause discomfort and pain for those with it. It occurs when one vertebra (bone in the spine) slips forward over another vertebra, causing the spinal column to become misaligned. This condition can affect people of all ages, but it is most commonly seen in adults over 50 .
What is the root cause of Spondylolisthesis?
The most common cause of spondylolisthesis is a fracture or defect in the pars interarticularis , a small bony section of the vertebra. This fracture can be caused by repetitive stress due to sports or activities that pressure the spine, such as weightlifting, gymnastics, or football. It can also happen due to congenital conditions or degenerative diseases like arthritis. Sometimes, spondylolisthesis can be caused by sudden trauma, such as a car accident or a fall.
What are the signs and symptoms of Spondylolisthesis?

The symptoms of spondylolisthesis vary depending on the severity of the condition. In mild cases, there may be no noticeable symptoms, but as the condition progresses, symptoms may include:
- Lower back pain
- Muscle spasms in the back
- Stiffness in the back
- Numbness or tingling in the legs
- Difficulty standing or walking
- Decreased range of motion in the back
- Weakness in the legs
How do you stop spondylolisthesis from progressing?
How exactly do you stop spondylolisthesis from worsening? There are practical strategies for managing and halting the progression of spondylolisthesis. Get ready to take control of your spinal health and stop spondylolisthesis in its tracks.
- Exercise regularly – Regular exercise helps to strengthen the muscles in your back and abdomen, providing better support for your spine. However, if you have spondylolisthesis, some exercises may be harmful. Consult a physical therapist to create a safe, individualized exercise plan for your condition.
- Avoid high-impact activities – Jumping and landing on the feet, such as running or basketball, can put additional stress on the spine. Instead, opt for low-impact exercises like swimming or cycling.
- Practice good posture – Poor posture can contribute to spondylolisthesis. Make a conscious effort to maintain good posture throughout the day, whether sitting, standing, or bending over. Consider using a lumbar support cushion if you spend much time sitting.
- Lose weigh t – Being overweight stresses the spine, which can worsen spondylolisthesis. Maintaining a healthy weight can help ease symptoms and stop the condition from progressing.
- Avoid lifting heavy objects – Putting strain on the lower back can worsen spondylolisthesis. If you need to lift heavy objects, use proper lifting techniques, such as bending your knees and keeping your back straight.
- Consider chiropractic care – Chiropractic manipulation and adjustments can help improve joint function and decrease pain in spondylolisthesis patients.
- Seek medical treatment – If you have persistent symptoms of spondylolisthesis, it's crucial to seek medical treatment. Your doctor may recommend physical therapy, pain medication, or in severe cases, surgery.
What are the 5 stages of spondylolisthesis?
Understanding the stages of spondylolisthesis is essential to identify its severity and manage it effectively. These are the five stages of spondylolisthesis and the accompanying symptoms.
Stage 1: Grade 1 Spondylolisthesis
The first stage of spondylolisthesis is also known as mild spondylolisthesis and is characterized by the slippage of less than 25% of one vertebra over another. In this stage, the symptoms may be minimal, and most people may not experience any. However, some common symptoms of grade 1 spondylolisthesis include mild back pain, stiffness, and muscle tightness in the lower back.
Stage 2: Grade 2 Spondylolisthesis
Grade 2 spondylolisthesis is characterized by the slippage of 26% to 50% of one vertebra over another. At this stage, the symptoms can become more noticeable, including increased back pain, numbness or tingling in the legs or feet, and difficulty standing or walking for extended periods. This stage may also lead to changes in posture and decreased flexibility in the lower back.
Stage 3: Grade 3 Spondylolisthesis
In this stage, the slippage increases to 51% to 75% of one vertebra over another. At this point, the spinal deformity may become apparent. Patients may experience severe back pain that radiates to the hips and legs, making it difficult to perform daily activities. Nerve compression is also standard in this stage, leading to symptoms like weakness, numbness, and tingling in the legs.
Stage 4: Grade 4 Spondylolisthesis
Grade 4 spondylolisthesis is characterized by the slippage of more than 75% of one vertebra over another. This stage can be severely debilitating, causing extreme back pain, nerve compression, and even difficulty in controlling bladder and bowel movements. Patients may also experience weakness and numbness in the legs, making it challenging to walk or stand for extended periods.
Stage 5: Grade 5 Spondylolisthesis
The final stage of spondylolisthesis, grade 5, is also known as spondyloptosis. In this stage, the slippage is more than 100% of one vertebra over another, meaning the vertebra has completely slipped off the one below it. At this point, the spinal deformity is severe and can lead to life-altering symptoms, including severe back pain, nerve damage, and loss of motor control in the legs.
Treatment options for Spondylolisthesis
Various treatment options for spondylolisthesis can help manage and relieve its symptoms. Let’s explore these treatment options and how they can help those with spondylolisthesis.
- Physical therapy:
Physical therapy is often the first line of treatment for spondylolisthesis. A physical therapist will work with the patient to strengthen the muscles in the back and abdomen, which can help stabilize the spine and prevent further slippage. They will also teach the patient proper posture and body mechanics to reduce pressure on the affected area. Physical therapy can also include exercises to increase flexibility and range of motion, which can help alleviate pain and stiffness.
- Medications:
Over-the-counter pain relievers such as ibuprofen and acetaminophen can help manage the pain caused by spondylolisthesis. Sometimes, a doctor may prescribe more vital pain medication or muscle relaxants if the pain is severe. However, these medications should only be used under the supervision of a doctor and are not a long-term solution for managing the condition.
- Bracing:
In some cases, a back brace may be recommended to provide support and stability to the affected area. This can help alleviate pain and prevent further slippage. It is crucial to work with a physical therapist to ensure the proper fit and usage of the brace.
- Steroid injections:
If other treatment options do not provide enough relief, a doctor may recommend steroid injections. These injections can help reduce inflammation and pain in the affected area. They are generally used as a short-term solution and may need to be repeated periodically.
- Surgery:
In severe cases of spondylolisthesis, surgery may be required. The most common surgery for this condition is spinal fusion, where the affected vertebrae are fused together to prevent slippage. This surgery can help alleviate pain and prevent further damage to the spine and nerves.
Get lasting relief from Spondylolisthesis!
Ready to take control of your Spondylolisthesis and find lasting relief? Look no further than Neuro Spine & Pain Center - your top choice for comprehensive treatment and expert care for Miami pain management .
Our team of renowned spine specialists in Miami understands the complexity of Spondylolisthesis and is dedicated to creating personalized treatment plans to address its underlying causes. From advanced imaging techniques to cutting-edge therapies, we have the tools to help you overcome this condition and live your life to the fullest.
Don't let Spondylolisthesis hold you back any longer, schedule a consultation with our experts today and let us guide you towards a pain-free and active lifestyle.

The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Patient center
FAQ Notice of Privacy Practices Data Breach Notification Accepted Insurance
Usefull Links
Home Referring Providers About Us Contact Us
Copyright © 2023 Neuro Spine and Pain Center

IMAGES
VIDEO
COMMENTS
Like many other conditions, spondylolisthesiscan be measured using a grading system, where your spondylolisthesis grade is based on the degree of displacement of your vertebrae. Grades of spond…
Grade 3: 51 – 75 % forward slip. May cause moderate symptoms such as pain after physical activity or sitting for long periods. Grade 4: 76 – 99% forward slip. May cause moderate to severe symptoms. Grade 5: Is when the …
The main symptoms of spondylolisthesis include: pain in your lower back, often worse when standing or walking and relieved when sitting or bending forward. pain spreading to your …
Grade 4 spondylolisthesis is characterized by the slippage of more than 75% of one vertebra over another. This stage can be severely debilitating, causing extreme back pain, nerve compression, and even difficulty in …
Adult Spondylolisthesis in the Low Back. In spondylolisthesis, one of the bones in your spine — called a vertebra — slips forward and out of place. This may occur anywhere along the spine, but is most common in the lower back (lumbar …
Grade II: Up to 50% slippage of the vertebra; Grade III: Up to 75% slippage; Grade IV: 76%-100% slippage; Grade V: More than 100% slippage, also known as …
Spondylolisthesis patients who have severe or high-grade slips may have tingling, numbness, or weakness in one or both legs. These symptoms result from pressure on the spinal nerve root as it exits the spinal canal near the …
Spondylolisthesis is the slippage of one vertebral body with respect to the adjacent vertebral body causing mechanical or radicular symptoms or pain. It can be due to congenital, acquired, or idiopathic causes.