- Research article
- Open access
- Published: 25 September 2011

Awareness and knowledge of sexually transmitted diseases (STDs) among school-going adolescents in Europe: a systematic review of published literature
- Florence N Samkange-Zeeb 1 ,
- Lena Spallek 1 &
- Hajo Zeeb 1
BMC Public Health volume 11 , Article number: 727 ( 2011 ) Cite this article
140k Accesses
92 Citations
19 Altmetric
Metrics details
Sexually transmitted diseases (STDs) are a major health problem affecting mostly young people, not only in developing, but also in developed countries.
We conducted this systematic review to determine awareness and knowledge of school-going male and female adolescents in Europe of STDs and if possible, how they perceive their own risk of contracting an STD. Results of this review can help point out areas where STD risk communication for adolescents needs to be improved.
Using various combinations of the terms "STD", "HIV", "HPV", "Chlamydia", "Syphilis", "Gonorrhoea", "herpes", "hepatitis B", "knowledge", "awareness", and "adolescents", we searched for literature published in the PubMed database from 01.01.1990 up to 31.12.2010. Studies were selected if they reported on the awareness and/or knowledge of one or more STD among school-attending adolescents in a European country and were published in English or German. Reference lists of selected publications were screened for further publications of interest. Information from included studies was systematically extracted and evaluated.
A total of 15 studies were included in the review. All were cross-sectional surveys conducted among school-attending adolescents aged 13 to 20 years. Generally, awareness and knowledge varied among the adolescents depending on gender.
Six STDs were focussed on in the studies included in the review, with awareness and knowledge being assessed in depth mainly for HIV/AIDS and HPV, and to some extent for chlamydia. For syphilis, gonorrhoea and herpes only awareness was assessed. Awareness was generally high for HIV/AIDS (above 90%) and low for HPV (range 5.4%-66%). Despite knowing that use of condoms helps protect against contracting an STD, some adolescents still regard condoms primarily as an interim method of contraception before using the pill.
In general, the studies reported low levels of awareness and knowledge of sexually transmitted diseases, with the exception of HIV/AIDS. Although, as shown by some of the findings on condom use, knowledge does not always translate into behaviour change, adolescents' sex education is important for STD prevention, and the school setting plays an important role. Beyond HIV/AIDS, attention should be paid to infections such as chlamydia, gonorrhoea and syphilis.
Peer Review reports
Over the period 1985-1996, a general decrease of gonorrhoea, syphilis and chlamydia infections was noted in developed countries, both in the general population and among adolescents [ 1 ]. From the mid-1990s however, increases in the diagnoses of sexually transmitted diseases, in particular syphilis, gonorrhoea and chlamydia have been reported in several European countries, especially among teenagers 16-19 years old [ 2 – 7 ].
The problem with most STDs is that they can occur symptom-free and can thus be passed on unaware during unprotected sexual intercourse. On an individual level, complications can include pelvic inflammatory diseases and possibly lead to ectopic pregnancies and infertility [ 8 – 11 ]. Female adolescents are likely to have a higher risk of contracting an STD than their male counterparts as their partners are generally older and hence more likely to be infected [ 2 , 12 ].
The declining age of first sexual intercourse has been proffered as one possible explanation for the increase in numbers of STDs [ 7 ]. According to data from different European countries, the average age of first sexual intercourse has decreased over the last three decades, with increasing proportions of adolescents reporting sexual activity before the age of 16 years [ 13 – 18 ]. An early onset of sexual activity not only increases the probability of having various sexual partners, it also increases the chances of contracting a sexually transmitted infection [ 19 ]. The risk is higher for female adolescents as their cervical anatomic development is incomplete and especially vulnerable to infection by certain sexually transmitted pathogens [ 20 – 23 ].
The reluctance of adolescents to use condoms is another possible explanation for the increase in STDs. Some surveys of adolescents have reported that condoms were found to be difficult to use for sexually inexperienced, detract from sensual pleasure and also embarrassing to suggest [ 24 – 26 ]. Condoms have also been reported to be used primarily as a protection against pregnancy, not STD, with their use becoming irregular when other contraceptives are used [ 15 , 27 ]. Furthermore, many adolescents do not perceive themselves to be at risk of contracting an STD [ 27 ].
We conducted this systematic review in order to determine awareness and knowledge of school-going adolescents in Europe of sexually transmitted diseases, not only concerning HIV/AIDS, but also other STDs such as chlamydia, gonorrhoea, syphilis and human papillomavirus (HPV). Where possible we will identify differences in awareness and knowledge by key demographic variables such as age and gender, and how awareness has changed over time.
Although knowledge and awareness have been reported to have a limited effect on changing attitudes and behaviour, [ 16 , 28 – 30 ] they are important components of sex education which help promote informed, healthy choices [ 31 – 33 ]. As schooling in Europe is generally compulsory at least up to the age of 15 years [ 34 ] and sex education is part of the school curriculum in almost all European countries, school-going adolescents should be well informed on the health risks associated with sexual activity and on how to protect themselves and others. In view of the decreasing age of sexual debut and the reported increasing numbers of diagnosed STDs among young people, results of our review can help point out areas where STD risk communication for school-attending adolescents needs to be improved.
Search strategy
We performed literature searches in PubMed using various combinations of the search terms "STD", "HIV", "HPV", "chlamydia", "syphilis", "gonorrhoea", "herpes", "hepatitis B", "knowledge", "awareness", and "adolescents". The reference lists of selected publications were perused for further publications of interest. The search was done to include articles published from 01.01.1990 up to 31.12.2010. Inclusion and exclusion criteria were specified in advance and documented in a protocol (Additional File 1 ).
Inclusion criteria
Studies were selected if they reported on awareness and/or knowledge of one or more sexually transmitted disease(s) among school-attending adolescents in a European country, or in Europe as a whole, and were published in English or German.
Exclusion criteria
Case reports, reviews, editorials, letters to the editor, expert opinions, studies on sexual activity/behaviour only, studies evaluating intervention programmes and studies not specifically on school-attending adolescents were excluded.
Methodological assessment of reviewed studies
We used a modified version of the Critical Appraisal Form from the Stanford School of Medicine to assess the methodology of the studies included in the review [ 35 ]. The studies were classified according to whether or not they fulfilled given criteria such as 'Were the study outcomes to be measured clearly defined?', 'Was the study sample clearly defined?', or 'Is it clear how data were collected?' (Table 1 ). No points were allocated. Instead, the following categorisations could be selected for each assessment statement: 'Yes', 'Substandard', 'No', 'Not Clear', 'Not Reported', 'Partially Reported', 'Not Applicable', 'Not Possible to Assess', 'Partly'. The assessment was done independently by two of the authors (FSZ, LS) who then discussed their findings.
Definition of awareness and knowledge
For the purpose of this review studies were said to have assessed awareness if participants were merely required to identify an STD from a given list or name an STD in response to an open question. Knowledge assessment was when further questions such as on modes of transmission and protection were posed.
Overall, 465 titles and abstracts were obtained from the searches conducted. Three hundred and ninety-three articles were excluded as they did not report on studies conducted in Europe (Figure 1 ). A further 47 were excluded as they did not focus on knowledge and awareness of adolescents. Of the 25 identified articles dealing with knowledge on STDs among adolescents in Europe, 8 were excluded as they either did not specifically address the question of knowledge and/or awareness, or focused more on sexual behaviour/beliefs. A further seven articles were excluded because the study population was not clearly stated to be school-attending.
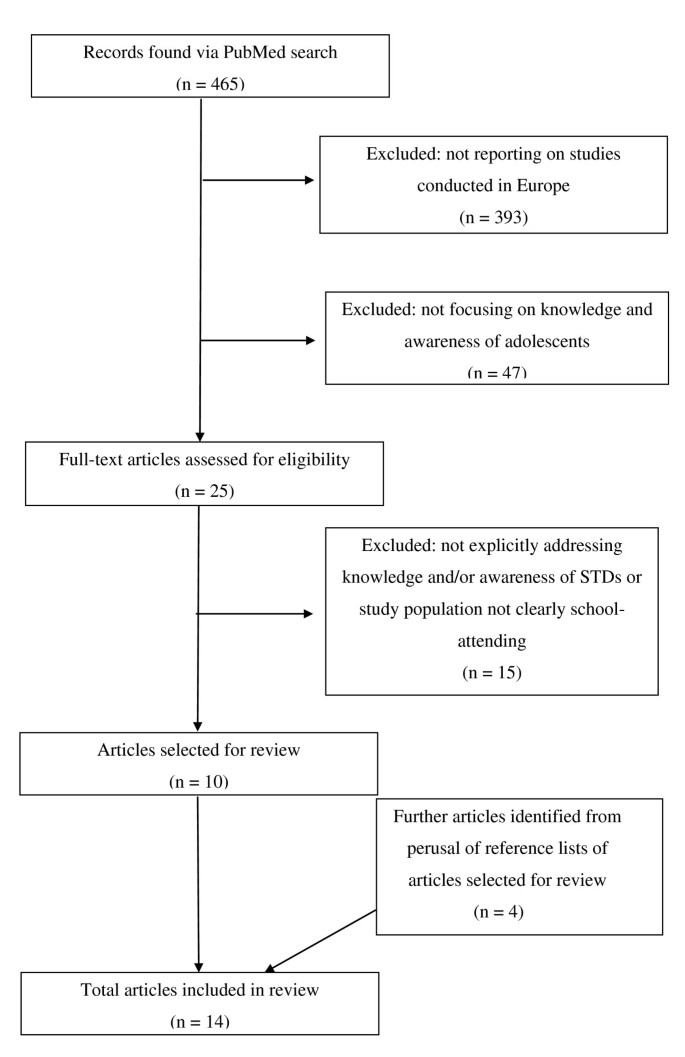
Flow diagram showing selection process of articles included in the review .
A review of the references listed in the 10 articles meeting inclusion criteria yielded four additional relevant articles. One article reported on two studies, hence a total of 15 studies published from 1990-2000 were included in the systematic review.
Six of the articles were published before the year 2000 [ 36 – 41 ], and nine after 2000 [ 42 – 49 ]. The studies report on surveys conducted from as early as 1986 to 2005 (Table 2 ).
The majority of the 15 studies specifically focused on HIV/AIDS only (7 studies) [ 36 , 39 , 41 , 43 , 44 , 49 ], four on STDs in general [ 37 , 38 , 40 , 42 ], one on STDs in general with focus on HPV [ 47 ], and three on HPV only [ 45 , 46 , 48 ]. All the HPV studies were published after the approval and market introduction of the HPV vaccine in 2006.
Generally the studies were conducted in particular regions/towns in different countries, with only one being conducted across three towns in three different countries (Russia, Georgia and the Ukraine) [ 43 ]. Six of the studies were conducted in Sweden [ 37 , 38 , 40 , 41 , 46 , 47 ] two in Russia [ 39 , 43 ] and one each in Ireland, [ 36 ] England, [ 42 ] Croatia, [ 44 ] Finland, [ 45 ] Italy [ 48 ] and Germany [ 49 ] (Table 2 ).
In the studies, generally both male and female adolescents varying in age from 13-20 years were surveyed. One study surveyed females only [ 40 ] and adolescents 11-12 years old were included in only one study [ 49 ] (Table 2 ). Whereas most of the studies included assessed awareness and knowledge among boys and girls separately, only one study [ 48 ] specifically assessed the association between age and awareness/knowledge.
Methodological summary of studies included in the review
All studies included in the review were cross-sectional in design. Apart from one study which recruited pupils by mailing the questionnaire to all households with adolescents in the 9 th grade, [ 45 ] pupils were recruited via schools. For 8 of the 15 studies it could not be deduced from the methods section how the participating schools were selected and in 4 studies it was not clear how the participating pupils were selected. The pupils completed questionnaires in school in 10 studies, and in two the questionnaires were completed at home [ 45 , 48 ]. Face-to-face interviews were used only in the surveys by Andersson-Ellström et al. [ 40 ] and by Goodwin et al. [ 43 ] (Table 2 ).
The study outcomes were clearly defined in all studies and the topics on which questions were posed were clearly described in all but one study. The majority of the studies also reported the individual questions posed to assess the given outcomes. In six studies the authors did not mention whether the instruments used for data collection had been pre-tested, validated, or whether the questions posed had been used in previous surveys (Table 1 ). Of the 9 studies which clearly reported participation rates, 7 had participation rates ranging from 79% to 100%. The remaining two studies had participation rates of 21.5% and 58% (Table 2 ).
Six STDs were focussed on in the studies included in the review, with awareness and knowledge being assessed in depth mainly for HIV/AIDS and HPV,[ 36 , 41 – 43 , 46 – 49 ] and to some extent for chlamydia [ 37 , 38 , 42 , 47 ]. For syphilis, gonorrhoea and herpes, only awareness was assessed in four studies [ 37 , 38 , 42 , 47 ].
Awareness and knowledge of HPV
The reported awareness of HPV among the surveyed adolescents was generally low (identification from given list), ranging from 5.4% in the study by Höglund et al. [ 47 ] to 66% in the study by Pelucchi et al. [ 48 ]. In the two studies which also reported results for females and males separately, awareness was observed to be statistically significantly higher among females than among males: 16.4% vs. 9.6% in the Swedish study by Gottvall et al. [ 46 ] and 71.6% vs. 51.2% in the Italian study by Pelucchi et al. [ 48 ]. In the study by Höglund et al., only one of the participating 459 adolescents mentioned HPV (in response to an open question on known STDs) [ 47 ].
Awareness of the HPV vaccine was also very low, with 5.8% and 1.1% of adolescents surveyed in the studies by Gottvall et al. and Höglund et al. respectively, reporting being aware of the vaccine [ 46 , 47 ]. Whereas only 2.9% and 9.2% of adolescents in these two Swedish studies were aware that HPV is sexually transmitted, the proportion was 60.6% in the Italian study [ 48 ]. A minority of adolescents knew that HPV is a risk factor for cervical cancer: 1.2% in the study by Höglund et al. [ 47 ] and 8.1% in the study by Gottvall et al. [ 46 ]. Among the adolescents who participated in the survey by Pelucchi et al., 48.6% were aware that the aim of the HPV vaccine is to prevent cervical cancer [ 48 ]. Among female adolescents who participated in the study by Gottvall et al., 11.8% did not believe they would be infected with HPV [ 46 ]. The proportion was 55% among female participants in the study by Pelucchi et al. [ 48 ]. The latter study surveyed pupils aged 14-20 years but did not report on age differences in awareness.
Three studies reported on awareness of condylomata, genital warts which are caused by the human papilloma virus. Two of the studies reported awareness of 35% [ 38 ] and 43% [ 37 ]. The third study mentioned that awareness of condylomata was lower than that for chlamydia without stating the corresponding figures [ 40 ].
Awareness and knowledge of HIV/AIDS
Knowledge and awareness was quite high in all studies reporting on HIV/AIDS, with more than 90% of adolescents being able to identify the disease as an STD from a given list or in response to the direct question "Have you ever heard of HIV/AIDS?" [ 36 , 38 , 42 ]. In one study where the open question "Which STDs do you know or have you heard of?" was used, 88% of respondents mentioned HIV/AIDS [ 47 ] (Table 3 ).
In the studies where this was asked, a large majority of the adolescents knew that HIV is caused by a virus, [ 36 , 41 ] is sexually transmitted,[ 36 , 41 , 43 , 47 , 49 ] and that sharing a needle with an infected person may lead to infection with the virus [ 36 , 41 , 43 , 49 ]. Statistically significant age specific differences in knowledge on mode of HIV-transmission were reported in the study conducted in Germany [ 49 ]. Compared to 13 and 15 year old pupils, a higher proportion of 14 year old pupils correctly identified the level of risk of HIV-transmission associated with bleeding wounds, intravenous drug use and sexual contact. For the latter mode of transmission, the lowest proportion of correct answers was observed among 16 year old pupils. Generally the proportion of respondents correctly reporting that use of condoms helps protect against contraction of HIV was above 90%. The only exception was in the Russian study conducted by Lunin et al. in 1993, in which only 42% of females and 60% of males were aware of this fact [ 39 ]. In the same study, only 15% of the adolescents perceived themselves 'not at risk' of contracting HIV (Table 3 ).
Only one study reported asking the adolescents if one can tell by looking at someone if they have HIV, to which 47% responded affirmatively [ 43 ].
Awareness and knowledge of chlamydia
The proportion of adolescents able to identify chlamydia as an STD from a list of diseases ranged from 34% in the study conducted in England by Garside et al. [ 42 ] to 96% in the Swedish study by Andersson-Ellström et al. [ 22 ]. In the Garside study, the proportion was higher among year 9 than among year 11 pupils (p < 0.05). In another Swedish study by Höglund et al. 86% of the surveyed adolescents mentioned chlamydia as one of the STDs known to them in response to an open question [ 47 ]. In the two studies which reported on awareness among boys and girls separately, girls were observed to have higher awareness proportions than boys [ 38 , 42 ]. While the observation was not statistically significant in one of the studies, [ 27 ] this was not reported on in the other study [ 38 ].
Not many adolescents knew that chlamydia can be symptom-free: 40% and 56% in the 1986 and 1988 surveys by Andersson-Ellström et al. [ 37 ] and 46% in the study by Höglund et al. [ 47 ]. In one Swedish study where the level of knowledge in the same study population was assessed at age 16 and 18, a statistically significant increase in knowledge was observed over time [ 40 ]. Only the Finish study reported on the subjective rating of risk of contracting chlamydia. 55% of the adolescents surveyed reported 'low perceived susceptibility' [ 45 ] (Table 3 ).
Awareness and knowledge of gonorrhoea
Gonorrhoea was identified as an STD from a given list by 84% of adolescents in the survey by Tyden et al.,[ 38 ] by 98% in the survey by Andersson-Ellström et al.,[ 37 ] and by 53% in the survey by Garside et al. [ 42 ]. In the latter, the difference between year 9 and year 11 pupils was more pronounced among boys: 53% among year 9 and 60% among year 11 (p > 0.05). A statistically significant increase in knowledge over time was observed in a group of girls surveyed at age 16 and 18 [ 40 ]. Only 50% of the adolescents surveyed in the study by Höglund et al. mentioned gonorrhoea in response to an open question on known STDs [ 47 ] (Table 3 ).
Awareness of syphilis and herpes
Awareness of syphilis was surveyed only in the study conducted in England where 45% of the participating adolescents correctly identified the disease from a given list as an STD. The proportion was slightly higher among year 11 compared to year 9 pupils and awareness was slightly higher among girls than among boys (p > 0.05) [ 42 ] (Table 3 ).
In the Tyden et al. study, [ 38 ] 56% of the surveyed adolescents identified herpes as an STD from a given list. The proportion was 90% in the survey by Andersson-Ellström et al. [ 37 ] and 59% in the Garside et al. study [ 42 ]. In the latter, considerable differences were observed between year 9 and year 11 pupils (p < 0.05), but not between girls and boys in the same school year. Herpes was mentioned as an STD by 64% of the adolescents surveyed in the study by Höglund et al. [ 47 ] (Table 3 ).
Awareness of STDs in general
Five of the studies reviewed assessed the knowledge of participating adolescents on STDs in general. In the England study, all in all 59.7% of the participants knew that STDs in general can be symptom-free [ 42 ]. Among girls, knowledge was higher among year 11 than year 9 pupils, while the opposite was true for boys. The proportion of boys in year 9 who knew this fact (64.2%) was considerably higher than that of year 9 girls (53.8%) (Table 3 ). In two Swedish studies by Tyden et al. and by Andersson-Ellström et al., all surveyed adolescents knew that the use of condoms can protect against the contraction of STDs in general [ 38 , 40 ]. In an earlier study by Andersson-Ellström et al., 20% of sexually active pupils surveyed in 1986 were aware that condoms protect against infection. The figure significantly went up to 43% in 1988, with boys having significantly higher awareness than girls in both years [ 22 ] (Table 3 ). In the same study, the proportion of girls who felt themselves to be at risk of contracting an STD in general went down from 32% in the 1986 survey to 24% in the 1988 survey. Among boys, the proportion increased from 16% in 1986 to 24% in 1988. These changes were not statistically significant [ 37 ]. In the Finish study, 55% of the surveyed adolescents perceived themselves to be at low risk of contracting an STD [ 45 ].
Reported use of condoms
Use of condoms by sexually active participants was assessed in three studies, all conducted in Sweden [ 38 , 46 , 47 ]. Reported use at sexual debut was lowest in the study published in 1991 (31%), [ 38 ] and higher in the other studies both published in 2009: 61% [ 47 ] and 65% [ 46 ] respectively (Table 3 ). In the earlier study, the proportion of girls reporting condom use was, at 50%, considerably higher than that of boys (40%) [ 38 ]. In the study by Gottvall et al., no difference in condom use was observed between girls and boys [ 46 ]. Condom use at recent coitus was reported on only in the earlier study [ 38 ]. It was observed that the decrease in the proportion of girls reporting using condoms was more pronounced than that of boys (26% vs. 40%) (Table 3 ).
The highest awareness and knowledge were reported for HIV/AIDS. This is certainly linked to the fact that since the mid 1980s, extensive awareness campaigns on this topic have been conducted globally. The lowest proportions were reported for HPV, with awareness as low as 5.4% in one study [ 47 ]. With only about 1 in 8 respondents knowing that HPV is an STD, awareness was still very low in one of the two studies conducted after the introduction of the HPV vaccine [ 46 ]. A higher awareness (66.6% of respondents aware), measured in a different population, was observed in the second recent study on HPV [ 48 ].
Two factors appeared to have influenced awareness. The first was of a methodological nature and related to the fact whether an open or closed question was posed. Of the studies included in the review which assessed awareness, all but one used closed-form questions only. The adolescents either had to identify sexually transmitted diseases from a given list of diseases, or the question was in a yes/no format. Initially, Höglund et al. asked participating adolescents to list all STDs known to them and then later on, if they had ever heard of HPV. Only one participant (0.2%) mentioned HPV as one of the STDs known to them, but later, 24 (5.4%) reported to have heard of HPV [ 47 ]. In comparison to open-form questions, closed questions are not only more practical and easier to respond to, but also easier to code and analyse. One of the arguments raised against closed questions, especially where a list of possible answers is given, is the risk of guesswork. It can not be ruled out that some participants, unable to answer the question, will select answers at random [ 50 , 51 ]. In the study by Garside et al. for example, among year 9 pupils, 14.5% incorrectly identified plasmodium, and 20.6% filariasis from a given list as STDs [ 42 ]. Open questions have been recommended for surveying participants with unknown or varying knowledge/awareness [ 50 ] as these questions provide a more valid picture of the state of knowledge [ 51 ].
To a lesser extent, gender also appears to have influenced knowledge and awareness, especially for HPV [ 46 , 48 ]. Significant gender differences were observed, with females having better awareness and knowledge than males. Although the data are limited as not all studies reported results separately for males and females, these findings, could be reflective of the way awareness campaigns, for example on HPV, have been targeted more at females than at males.
The studies on HIV included in our review generally reported high awareness of the protective effect of condoms among adolescents [ 36 , 41 , 43 , 47 , 49 ]. One study included in the review however observed that adolescents seem to regard condoms primarily as a method of contraception and not as a means of protection against sexually transmitted diseases (40). In this study, 19 out of 20 female adolescents who reported more than 4 sexual partners at the age of 18 reported intercourse without a condom in relationships of less than 6 months' duration. The majority of them were, however, convinced that they had neither acquired (96%) nor transmitted (93%) an STD at last unprotected intercourse [ 40 ]. Other studies also indicate that consistent condom use is generally low among adolescents [ 27 , 52 – 55 ].
Where reported, participation rates were generally high, probably due to the fact that the adolescents were recruited in schools. In some instances however, the number of participants was low even though the participation rate was reported as high. In the study by Tyden et al. for example, the study sample consisted of 213 pupils, 12% of the 1830 students in the first form of upper secondary school in Uppsala [ 38 ]. The authors base the participation rate of their study (98%) on the 12%, without explaining how it came about that only 213 pupils were considered for participation. The one study which recruited participants per post had a very low participation rate of 21.5% [ 45 ]. Nevertheless, the study had more participants than others with comparatively higher participation rates. Bias related to selective participation is an issue that needs to be considered on a study by study basis, and reporting on response proportions should be considered essential for all studies.
Study strengths and limitations
To our knowledge no systematic reviews of published literature on knowledge and awareness of sexually transmitted diseases among school-attending adolescents in Europe have been conducted to date. The current review confirms that there are considerable gaps in knowledge and awareness on major STDs in European adolescents. Our results underline the importance of the objectives set for adolescents' sexual and reproductive health in Europe, the first of which foresees that adolescents be informed and educated on all aspects of sexuality and reproduction [ 31 ].
We could not identify many studies on knowledge and awareness of sexually transmitted diseases among school-attending adolescents in Europe. This could be due to the fact that knowledge has been shown to have little impact on behaviour change, and prevention interventions have generally moved away from a focus on knowledge and awareness as key mediators. Another possible reason is that schools are not always willing to participate in such studies due to competing demands of other school activities or because of the subject content [ 16 , 28 – 30 ].
One limitation of our review is that the 15 studies included did not all focus on the same sexually transmitted diseases. The four studies conducted in Eastern Europe were all on HIV/AIDS knowledge and awareness only, whereas Western European studies were on STDs in general or on HPV. Furthermore, the formulation of the questions used to assess awareness and knowledge varied between studies, making it difficult to directly compare the findings of individual studies. Another potential limiting factor is the age variation of participants in the studies included in the review, especially as all but one study did not clearly investigate the association between age and awareness or knowledge. Due to the afore-mentioned factors and the small number of studies available, it was not possible to perform a meta-analysis of the study findings.
The representativeness of study participants in some studies could not be assessed as it was not mentioned how the schools were selected [ 37 , 40 – 44 , 49 ]. Different socioeconomic environments of individual schools are likely to affect results, but there is currently not sufficient information to assess this.
The school setting offers an effective way to access adolescent populations universally, comprehensively and uniformly [ 56 ]. It plays an important role for sex education, especially for those adolescents with no other information sources. Furthermore, some parents are not comfortable discussing sexual issues with their children. It therefore comes as no surprise that many young people cite the school as an important source of information about sexually transmitted diseases [ 26 , 27 ]. Although sex education is part of the school curriculum in many European countries, there are differences in the issues focused on. In some countries sex education is integrated in life skills approach, whilst biological issues are predominant in others and at times the focus is on HIV/AIDS prevention [ 57 ]. Generally it seems that education schedules offer a range of opportunities to raise knowledge and awareness of STD among adolescents.
In general, the studies reported similar low levels of knowledge and awareness of sexually transmitted diseases, with the exception of HIV/AIDS. Although, as shown by some of the findings on condom use, knowledge does not always translate into behaviour change, adolescents' sex education is important for STD prevention, and the school setting plays an important role. Beyond HIV/AIDS, attention should be paid to infections such as chlamydia, gonorrhoea and syphilis.
World Health Organisation: Global prevalence and incidence of selected curable sexually transmitted infections. 2001, WHO, Geneva
Google Scholar
Panchaud C, Singh S, Feivelson D, Darroch JE: Sexually transmitted diseases among adolescents in developed countries. Fam Plan Persp. 2000, 32: 24-32 &45. 10.2307/2648145.
Article CAS Google Scholar
Berglund T, Fredlund H, Giesecke J: Epidemiology of the re-emergence of gonorrhoea in Sweden. Sex Transm Dis. 2001, 111-114.
Health protection Surveillance Centre.: Surveillance of STI. A report by the Sexually Transmitted Infections subcommittee for the Scientific Advisory committee of the health Protection Surveillance Centre. December 2005,
Nicoll A, Hamers FF: Are trends in HIV, gonorrhoea and syphilis worsening in Western Europe?. BMJ. 2002, 324: 1324-1327. 10.1136/bmj.324.7349.1324.
Article PubMed PubMed Central Google Scholar
Twisselmann B: Rising trends of HIV, gonorrhoea, and syphilis in Europe make case for introducing European surveillance systems. Euro Surveill. 2002, 6 (23): pii = 1952-Last accessed 30.11.2010, [ http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=1952 ]
Adler MW: Sexually transmitted infections in Europe. Eurohealth. 2006, 12: 3-6.
PHLS, DHSS & PS and the Scottish ISD(D)5 Collaborative Group: Trends in Sexually Transmitted Infections in the United Kingdom 1990-1999. 2000, Public Health Laboratory Service London
Stamm W, Guinan M, Johnson C: Effect of treatment regiments for Neisserie gonorrhoea on simultaneous infections with Chlamydia trachomatis. New Eng J Med. 1984, 310: 545-559. 10.1056/NEJM198403013100901.
Article CAS PubMed Google Scholar
MacDonald NE, Brunham R: The Effects of Undetected and Untreated Sexually Transmitted Diseases: Pelvic Inflammatory Disease and Ectopic Pregnancy in Canada. The Canadian Journal of Human Sexuality. 1997, 6 (2): Special Issue: STDs and Sexual/Reproductive Health-
Simms I, Stephenson JM: Pelvic inflammatory disease epidemiology; What do we know and what do we need to know?. Sex Trans Inf. 2000, 76: 80-87. 10.1136/sti.76.2.80.
Bozon M, Kontula O: Sexual initiation and gender in Europe. Sexual behavior and HIV/AIDS in Europe. Edited by: M Hubert, N Bajos, and T Sandfort. 1998, London: UCL Press, 37-67.
Kangas I, Andersen B, McGarrigle CA, Ostergaad L: A comparison of sexual behaviour and attitudes of healthy adolescents in a Danish high school in 1982, 1996 and 2001. Pop Health Metr. 2004, online publication: last accessed 03.12.2010, [ http://www.pophealthmetrics.com/content/2/1/5 ]
Ross J, Godeau E, Dias S: Sexual health. Young people's health in context. Health Behaviour in School-aged Children (HSBC) study: International report from the 2001/2002 survey. Edited by: Currie C, Roberts C, Morgan A, et al. 2004, Copenhagen: WHO
Bundeszentrale für gesundheitliche Aufklärung: Jugendsexualität. Repräsentative Wiederholungsbefragung von 14- bis 17-Jährigen Jugendlichen und ihren Eltern. 2006, BZgA
Tucker JS, Fitzmaurice AE, Imamura M, Penfold S, Penney GC, van Teijlingen E, Schucksmith J, Philip KL: The effect of the national demonstration project Healthy Respect on teenage sexual health behaviour. Eur J Public Health. 2006, 17 (1): 33-41. 10.1093/eurpub/ckl044.
Article PubMed Google Scholar
Godeau E, Gabhainn SN, Vignes C, Ross J, Boyce W, Todd J: Contraceptive use by 15-year-old students at their last sexual intercourse: Results from 24 countries. Arch Paediatr Adolesc Med. 2008, 162: 66-73. 10.1001/archpediatrics.2007.8.
Article Google Scholar
Bundeszentrale für gesundheitliche Aufklärung: Sexualität und Migration: Milieuspezifische Zugangswege für die Sexualaufklärung Jugendlicher. Ergebnisse einer repräsentativen Untersuchung der Lebenswelten von 14- bis 17-Jährigen Jugendlichen mit Migrationshintergrund. 2010, BZgA,
Heinz M: Sexuell übertragbare Krankheiten bei Jugendlichen: Epidemiologische Veränderungen und neue diagnostische Methoden. 2001, Arbeitsgemeinschaft Kinder-und Jugendgynäkologie e.V, last accessed 03.12.2010, [ http://www.kindergynaekologie.de/html/kora22.html ]
Berrington de González A, Sweetland S, Green J: Comparisons of risk factors for squamous cell and adenocarcinomas of the cervix: a meta-analysis. Br J Cancer. 2004, 90: 1787-1791.
PubMed PubMed Central Google Scholar
Reich O: Is early first intercourse a risk factor for cervical cancer?. Gynäkol Geburtshilfliche Rundsch. 2005, 45: 251-256. 10.1159/000087143.
Gille G, Klapp C: Chlamydia trachomatis infections in teenagers. Der Hautarzt. 2007, 58: 31-37. 10.1007/s00105-006-1265-x.
Hwang LY, Ma Y, Miller Benningfield S, Clayton L, Hanson EN, Jay J, Jonte J, Godwin de Medina C, Moscicki AB: Factors that influence the rate of epithelial maturation in the cervix of healthy young women. J Adolesc Health. 2009, 44 (2): 103-110. 10.1016/j.jadohealth.2008.10.006.
Kegeles SM, Adler NE, Irwin CE: Adolescents and condoms. Am J Dis Child. 1989, 143: 911-915.
Ford N: The AIDS awareness and sexual behaviour of young people in the South-west of England. J Adolesc. 1992, 15: 393-413. 10.1016/0140-1971(92)90071-C.
Persson E, Sandströäm B, Jarlbro G: Sources of information, experiences and opinions on sexuality, contraception and STD protection among young Swedish students. Advances in Contraception. 1992, 8: 41-49. 10.1007/BF01849347.
Editorial team: Young people's knowledge of sexually transmitted infections and condom use surveyed in England. Euro Surveill. 2005, 10 (31): pii = 2766- Last accessed 30.11.2010
Lister-Sharpe D, Chapman S, Stewart-Brown S, Sowden A: Health promoting schools amd health promotion in schools: two systematic reviews. Health Technol Assess. 1999, 3 (22): 1-207.
Wight D, Raab G, Henderson M, Abraham C, Buston K, Hart G, Scott S: Limits of teacher delivered sex education: interim behavioural outcomes from randomised trial. BMJ. 2002, 324: 1-6.
Stephenson J, Strange V, Forrest S, Oakley A, Copas A, Allen E, Babiker A, Black S, Ali M, Monteiro H, Johnson AM: Pupil-led sex education in England (RIPPLE study): cluster randomised intervention trial. Lancet. 2004, 364 (9431): 338-346. 10.1016/S0140-6736(04)16722-6.
WHO Regional Office for Europe: Who Regional Strategy on Sexual and Reproductive Health. 2001, pdf last accessed 17.03.2011, [ http://www.euro.who.int/__data/assets/pdf_file/0004/69529/e74558.pdf ]
Bundeszentrale für gesundheitliche Aufklärung: Country papers on youth sexuality in Europe - Synopsis. 2006, BZgA,
Bobrova N, Sergeev O, Grechukhina T, Kapiga S: Social-cognitive predictors of consistent condom use among young people in Moscow. Perspect Sex Reprod Health. 2005, 37 (4): 174-178. 10.1363/3717405.
European Commission: Compulsory education in Europe 2010/2011. pdf last accessed 10.05.2011, [ http://eacea.ec.europa.eu/education/eurydice/documents/compulsory_education/compulsory_education.pdf ]
Assessing scientific admissibility and merit of published articles: Critical appraisal form. last accessed 08.03.2011, [ http://peds.stanford.edu/Tools/documents/Critical_Appraisal_Form_CGP.pdf ]
Fogarty J: Knowledge about AIDS among leaving certificate students. Irish Med Journal. 1990, 83: 19-21.
CAS Google Scholar
Andersson-Ellström A, Forssman L: Sexually transmitted diseases - knowledge and attitudes among young people. J Adolesc Health. 1991, 12: 72-76. 10.1016/0197-0070(91)90446-S.
Tyden T, Norden L, Ruusuvaara L: Swedish students' knowledge of sexually transmitted diseases and their attitudes to the condom. Midwifery. 1991, 7: 25-30. 10.1016/S0266-6138(05)80131-7.
Lunin I, Hall TL, Mandel JS: Adolescent sexuality in Saint Petersburg, Russia. AIDS. 1995, 9 (suppl 1): S53-S60.
PubMed Google Scholar
Andersson-Ellström A, Forssman L, Milsom I: The relationship between knowledge about sexually transmitted diseases and actual sexual behaviour in a group of teenage girls. Genitourin Med. 1996, 72: 32-36.
Eriksson T, Sonesson A, Isacsson A: HIV/AIDS - information and knowledge: a comparative stud of Kenyan and Swedish teenagers. Scand J Soc Med. 1997, 25: 111-118.
CAS PubMed Google Scholar
Garside R, Ayres R, Owen M, Pearson VAH, Roizen J: 'They never tell you about the consequences': young people's awareness of sexually transmitted infections. Int J STD & AIDS. 2001, 12: 582-588. 10.1258/0956462011923750.
Goodwin R, Kozlova A, Nizharadze G, Polyakove G: HIV/AIDS among adolescents in Eastern Euorpe: knowledge of HIV/AIDS, social representations of risk and sexual activity among school children and homeless adolescents in Russia, Georgia and the Ukraine. J Health Psych. 2004, 9: 381-396.
Macek M, Matkovic V: Attitudes of school environment towards integration of HIV-positive pupils into regular classes and knowledge about HIV/AIDS: cross-sectional study. Croat Med J. 2005, 26: 320-325.
Woodhall Sc, Lehtinen M, Verho T, Huhtala H, Hokkanen M, Kosunen E: Anticipated acceptance of HPV vaccination at the baseline of implementation: a survey of parental and adolescent knowledge and attitudes in Finland. J Adolesc Health. 2007, 40: 466-469. 10.1016/j.jadohealth.2007.01.005.
Gottvall M, Larsson M, Högkund AT, Tydén T: High HPV vaccine acceptance despite low awareness among Swqedish upper secondary school students. Eur J Contr Repr Health Care. 2009, 14: 399-405. 10.3109/13625180903229605.
Höglund AT, Tydén T, Hannerfors AK, Larsson M: Knowledge of human papillomavirus and attitudes to vaccination among Swedish high school students. Int J STD & AIDS. 2009, 20: 102-107. 10.1258/ijsa.2008.008200.
Pelucchi C, Esposito S, Galeone C, Semino M, Sabatini C, Picciolli I, Consolo S, Milani G, Principi N: Knowledge of human papillomavirus infection and its prevention among adolescents and parents in the greater Milan area, Northern Italy. BMC Public Health. 2010, 10: 378-10.1186/1471-2458-10-378.
Sachsenweger M, Kundt G, Hauk G, Lafrenz M, Stoll R: Knowledge of school pupils about the HIV/AIDS topic at selected schools in Mecklenburg-Pomerania: Results of a survey of school pupils. Gesundheitswesen. 2010, online publication 2.3.2010, , [ http://dx.doi.org/10.1055/s-0029-1246199 ]
Vinten G: Open versus closed questions - an open issue?. Manag. 1995, 33: 27-31.
Krosnick JA, Presser S: Question and Questionnaire Design. Handbook of Survey research. Edited by: Wright JD, Marsden PV. 2010, Bingley: Emerald Group Publishing Ltd, 263-314. Last accessed 02.05.2011, [ http://comm.stanford.edu/faculty/krosnick/Handbook%20of%20Survey%20Research.pdf ]2
Piccinino LJ, Mosher WD: Trends in contraceptive use in the United States: 1982-1995. Family Planning Perspectives. 1998, 30: 4-10. 10.2307/2991517.
Glei DA: Measuring contraceptive use patterns among teenage and adult women. Family Planning Perspectives. 1999, 31: 73-80. 10.2307/2991642.
Everett SA, Warren CW, Santelli JS, Kann L, Collins JL, Kolbe LJ: Use of birth control pills, condoms and withdrawal among U.S. high school students. Journal of Adolescent Health. 2000, 27: 112-118. 10.1016/S1054-139X(99)00125-1.
Kaaya SF, Flisher AJ, Mbwambo JK, Schaalma H, Aaro LE, Klepp KI: A review of studies of sexual behaviour of school students in sub-Saharan Africa. Scandinavian Journal of Public Health. 2002, 30: 148-160.
Abraham C, Wight D: Developing HIV-preventive behavioural interventions for young people in Scotland. Int Journal of STD and AIDS. 1996, 7 (suppl 2): 39-42.
Helfferich C, Heidtke B: Country papers on youth sex education in Europe. 2006, BZgA
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2458/11/727/prepub
Download references
Author information
Authors and affiliations.
Bremen Institute for Prevention Research and Social Medicine, University of Bremen, Germany
Florence N Samkange-Zeeb, Lena Spallek & Hajo Zeeb
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Florence N Samkange-Zeeb .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
FSZ developed the concept for the study, conducted the literature search, assessed studies for inclusion in the review and extracted data. She also prepared drafts and undertook edits. LS was involved in the development of the study concept, conducted the literature search, assessed studies for inclusion in the review and extracted data. HZ was involved in the development of the study concept. All authors contributed to the editing of the drafts and have read and approved all versions of the manuscript.
Electronic supplementary material
12889_2011_3510_moesm1_esm.doc.
Additional file 1: Review Protocol: The preparation process for the systematic review is documented in the file. Included are the objectives of the review, inclusion and exclusion criteria, the search strategy, definition of outcomes, as well as the data abstraction table. (DOC 112 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Samkange-Zeeb, F.N., Spallek, L. & Zeeb, H. Awareness and knowledge of sexually transmitted diseases (STDs) among school-going adolescents in Europe: a systematic review of published literature. BMC Public Health 11 , 727 (2011). https://doi.org/10.1186/1471-2458-11-727
Download citation
Received : 12 May 2011
Accepted : 25 September 2011
Published : 25 September 2011
DOI : https://doi.org/10.1186/1471-2458-11-727
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cervical Cancer
- Participation Rate
- Human Papilloma Virus
- Transmitted Disease
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Loading metrics
Open Access
A Collection on the prevention, diagnosis, and treatment of sexually transmitted infections: Call for research papers
* E-mail: [email protected]
Affiliation Institute of Social and Preventive Medicine, University of Bern, Bern, Switzerland
Affiliation World Health Organization, Geneva, Switzerland
Affiliation PLOS Medicine, Public Library of Science, Cambridge, United Kingdom
- Nicola Low,
- Nathalie Broutet,
- Richard Turner

Published: June 27, 2017
- https://doi.org/10.1371/journal.pmed.1002333
- Reader Comments
Citation: Low N, Broutet N, Turner R (2017) A Collection on the prevention, diagnosis, and treatment of sexually transmitted infections: Call for research papers. PLoS Med 14(6): e1002333. https://doi.org/10.1371/journal.pmed.1002333
Copyright: © 2017 Low et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: RT is paid a salary by the Public Library of Science and contributed to this editorial during his salaried time.
Competing interests: We have read the journal's policy and have the following conflicts: NL receives a stipend as a specialty consulting editor for PLOS Medicine and serves on the journal's editorial board. RT’s individual competing interests are at http://journals.plos.org/plosmedicine/s/staff-editors . PLOS is funded partly through manuscript publication charges, but the PLOS Medicine Editors are paid a fixed salary (their salaries are not linked to the number of papers published in the journal).
Abbreviations: HPV, human papillomavirus; STI, sexually transmitted infection
Provenance: Commissioned; not externally peer-reviewed.
Sexually transmitted infections (STIs) are common, diverse, and dangerous to health—extending from bacterial diseases that may be readily treatable once diagnosed to viral infections such as HIV that can be life-threatening and, as yet, have no cure. A wide range of sexually transmissible pathogens have adverse effects on sexual and reproductive health, including infertility in women and several different types of cancer, with the global burden of cervical cancer a particular concern. Having an STI can also lead to low self-esteem, stigma, and sexual dysfunction. Moreover, some STIs are transmitted from mother to child and thereby lead to poor pregnancy, neonatal, and child health outcomes, including stillbirth. Emerging pathogens that prove to be sexually transmissible, recently exemplified by Ebola and Zika viruses, can be expected to evoke substantial and widespread concern where the risks and possible consequences of a disease outbreak are sketchily understood.
According to WHO [ 1 ], more than 30 different bacteria, viruses, and parasites lead to greater than 1 million sexually transmitted infections each day. Chlamydia (with an estimated 131 million new infections annually), gonorrhea (78 million infections), syphilis (5.6 million infections), and trichomoniasis (143 million infections) are 4 of the most common infections worldwide that can, at present, be treated with existing antibiotic regimens. However, antimicrobial resistance is a growing threat, particularly for gonorrhea and Mycoplasma genitalium . The most prevalent viral STIs are genital herpes simplex virus infection (affecting an estimated 500 million people worldwide) and human papillomavirus (HPV) infection (affecting 290 million women and leading to some 500,000 cases of cervical cancer annually). While antiviral treatment may control recurring herpes in some people, disease prevention and, where possible, vaccine development and deployment are priorities in the absence of curative interventions. Enmeshed as they are in human biology, behavior, and culture, STIs provide great challenges to those responsible for disease surveillance, planning services, and provision of treatment in all countries.
Because of the enormous burden of STIs and their wide-ranging adverse health effects, decisive action will be an essential part of efforts to meet the health component of the Sustainable Development Goals, and the targets of the global health sector strategy on sexually transmitted infections 2016–2021 [ 2 ], which were adopted by the 69th World Health Assembly in May 2016. Accompanying this Editorial are several articles forming part of a WHO-sponsored Collection addressing global policy and practice aimed at achieving control of STIs. Andrew Seale and colleagues discuss the development process for the global strategy to counter STIs [ 3 ]. Global targets for STI control specify, by 2030, achievement of a 90% reduction in syphilis incidence; a 90% reduction in gonorrhea incidence; and occurrence of 50 or fewer cases of congenital syphilis per 100,000 live births in 80% of countries, and Melanie Taylor and colleagues discuss systems for STI surveillance and monitoring of treatment resistance towards these targets [ 4 ]. Taylor and colleagues also discuss programs and criteria aimed at elimination of mother-to-child transmission of syphilis and HIV [ 5 ]. Finally, Paul Bloem and colleagues discuss HPV vaccination for control of cervical cancer and other HPV-related diseases [ 6 ] in different settings, illustrating the prospects of new interventions for STI control. Further discussion articles will appear in future issues of PLOS Medicine , and, as part of the cross-journal Collection, research papers are being published in PLOS Medicine and in other PLOS journals [ 7 ].
To accompany this Collection, we are inviting submission of reports of high-quality research studies with the potential to inform clinical practice or thinking relevant to STIs, focused on the following:
- Epidemiological studies on the incidence, prevalence, and disease burden of STIs, including emerging and re-emerging infections, mother-to-child transmission of STIs, and STIs in the context of new HIV prevention approaches;
- Molecular and genomic studies relevant to clinical advances in STI research, including antimicrobial resistance and microbiome analysis;
- Studies investigating treatment, partner notification, vaccination, behavioral, and combination interventions for STIs, with reports of randomized controlled trials particularly welcome;
- Implementation research, especially focused on interventions for STI prevention and point-of-care approaches to disease diagnosis in low- and middle-income countries, including qualitative research on issues such as stigma;
- Modelling and cost-effectiveness studies relevant to STIs, addressing prevention and treatment interventions.
Please submit your manuscript at http://journals.plos.org/plosmedicine/s/submit-now . We (NL and NB) will be the guest editors for the Collection, and successful submissions will be published, following peer review, from December 2017 onwards. Papers to be published in December should be submitted by August 11, 2017 but submissions will still be considered, and can be included in the Collection, after that date. Presubmission inquiries are not required, but we ask that you indicate your interest in this call for papers in your cover letter.
Author Contributions
- Conceptualization: NL NB RT.
- Writing – original draft: RT.
- Writing – review & editing: NL NB RT.
- 1. World Health Organization. Sexually transmitted infections factsheet. [Cited 2017 May 18]. Available from: http://www.who.int/mediacentre/factsheets/fs110/en/
- 2. World Health Organization. Global health sector strategy on sexually transmitted infections, 2016–2021. [Cited 2017 May 18]. Available from: http://www.who.int/reproductivehealth/publications/rtis/ghss-stis/en/
- View Article
- Google Scholar
- PubMed/NCBI
Sexually transmitted infection prevention behaviours: health impact, prevalence, correlates, and interventions
- Psychology and Health 38(1):1-26
- CC BY-NC-ND 4.0

- Utrecht University

- UNSW Sydney

- Maastricht University
Abstract and Figures

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- BMC PUBLIC HEALTH
- Frédérique Tremblay
- Yohann Courtemanche

- Lisa S. Pair
- William E. Somerall

- Namrah Khan
- Fawad Ali Shah

- Paul Norman
- CURR OPIN INFECT DIS

- Zhixian Chen

- Martin Fishbein
- Paige A. Muellerleile
- Jayleen K. L. Gunn

- Darrel H. Higa

- Silke David
- Birgit H B van Benthem
- AM J HEALTH PROMOT

- AIDS Res Ther

- Light Tsegay
- Sarah Wiatrek
- Maria Zlotorzynska
- Travis Sanchez
- Christine M. Khosropour

- Laura Nyblade
- Pia Mingkwan
- Melissa A. Stockton

- Hillard Weinstock

- Ian H. Spicknall

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Sex Transm Dis AIDS
- v.38(1); Jan-Jun 2017
Knowledge and attitude about sexually transmitted infections other than HIV among college students
Nagesh tumkur subbarao.
Department of Dermatology, STD and Leprosy, Sapthagiri Institute of Medical Sciences and Research Center, Bengaluru, Karnataka, India
Background:
Sexually transmitted infections (STIs) are the infections which are mainly transmitted through sexual intercourse. Young individuals in the age group of 16 to 24 years are considered to be at more risk for STIs compared to older adults. Young individuals are more likely to practice unprotected sex and have multiple sexual partners. If the STIs are not treated adequately, it can lead to various complications.Most of the people may be aware about HIV/AIDs because of the awareness created by media and the government programs, however knowledge about STIs other than HIV/AIDS is low in the developing countries.
Materials and Methods:
This study was a descriptive cross sectional study to assess the knowledge, awareness and attitude of college students about STIs other than HIV. A total of 350 engineering students from various semesters were included in the study. They were asked to fill up an anonymous questionnaire.
Two hundred and fifty six (73%) males and 94 (27%) females participated in the study. 313 (90%) students had heard about sexually transmitted infections (STIs) and 223 (64%) students had heard about STIs other than HIV. 99% of students knew about HIV where as less than 50% of students knew about other STIs. Teachers, internet and media were the source of information for most of the participants. Almost 75% of the students knew about the modes of transmission of STIs. Less than 50% of the participants knew about the symptoms of STIs and complications. Also attitude of the students towards sexual health and prevention of STIs was variable.
Conclusion:
The findings of our study shows that it is important to orient the students about sexual health and safe sexual practices as it will go a long way in prevention and control of STIs. Also the morbidities and complications associated with STIs can be prevented.
INTRODUCTION
Sexually transmitted infections (STIs) are the infections which are mainly transmitted through sexual intercourse. The common STIs which we come across in daily practice are gonorrhea, chancroid, syphilis, and chlamydial infections which can be cured and others such as HIV, genital herpes, HPV, and hepatitis B infection which cannot be cured but can be modified with the available treatments.[ 1 ]
Young individuals in the age group of 16–24 years are considered to be at more risk for STIs compared to older adults. The World Health Organization estimates that 20% of persons living with HIV/AIDS are in their 20s and one out of twenty adolescents contract an STI each year.[ 1 ]
Many young individuals stay away from families for a long time when they take up higher education. They either stay in hostels or in paying guest accommodations and come in contact with people from different sociocultural background.
Young individuals are more likely to practice unprotected sex and have multiple sexual partners. In addition, they may not have access to the required information and services to avoid STIs. Furthermore, they may feel hesitant to approach the facilities where information is available.[ 2 ]
If the STIs are not treated adequately, it can lead to various complications such as infertility, urethral stricture, abortions, malignancies, perinatal, and neonatal morbidities.[ 3 , 4 ] Both ulcerative and nonulcerative STIs enhance the transmission of HIV/AIDS.[ 5 ]
Knowledge of STI and their complications and attitude of the young generation toward sexual health are important in planning preventive and treatment strategies.[ 6 ] Most of the people may be aware about HIV/AIDs because of the awareness created by media and government programs; however, knowledge about STIs other than HIV/AIDS is low in the developing countries.[ 7 ]
This study was a descriptive cross-sectional study to assess the knowledge, awareness, and attitude of college students about STIs other than HIV.

MATERIALS AND METHODS
This cross-sectional study was conducted among college students in the age group of 18–22 years. A total of 350 engineering students from various semesters were included in the study. A questionnaire was administered to all the students where they had to mention only their age and place. We tried to assess from the questionnaire, knowledge, and attitude of the students regarding the STIs and also their awareness about STIs other than HIV/AIDS. The questions tried to assess their knowledge about symptoms of STI, predisposing/causative factors, preventive measures, complications of STIs, and attitude toward sexual health.
A total of 350 students were administered the questionnaire, 256 (73%) males and 94 (27%) females. One hundred and seventeen students were from Bengaluru and 213 students were from different parts of the country and twenty students were from other countries such as Africa and New Guinea.
One hundred and eighty-six (53%) students were staying with their parents or family and 164 (47%) students were staying with their friends or alone in hostels or paying guest accommodations.
Around 90% (313) of students had heard about STIs and 223 (64%) students had heard about STIs other than HIV. One hundred and eight (30%) students knew that STI can be present in a person even without symptoms, 214 (61%) students did not know if it was possible to have STI without symptoms and 28 (8%) students mentioned that it was not possible to have STI without symptoms.
Tuberculosis, leprosy, and vitiligo were considered as STI by 17 (4.8%), 17 (4.8%), and 20 (5.7%) students, respectively. HIV was known as an STI by 347 (99.2%) students. One hundred and fourteen (32.5%) students knew genital herpes, 95 (27%) syphilis, 108 (30.8%) hepatitis B, 107 (30.5%) genital warts, 92 (26.2%) gonorrhea, 26 (7.4%) lymphogranuloma venereum (LGV), and 13 (3.7%) chancroid as STI [ Table 1 ].
Knowledge about various sexually transmitted diseases ( n =350)

Source of information
Teachers were the source of information about STIs in 203 (58%) students followed by internet 181 (51.7%), newspaper/magazines 162 (46.2%), TV/radio 158 (45.1%), friends 142 (40.5%), doctor/clinics 96 (27.4%, parents 28 (8%), and relatives 11 (3.1%) [ Table 2 ].
Source of information about sexually transmitted infections ( n =350)

Predisposing/causative factor
Virus was known to be a causative factor for STI by 169 (48.2%) students followed by bacteria (49, 14%) and fungi (27, 7.7%). Multiple sexual partners and unprotected sex were considered as predisposing factors for STI by 252 (71.7%) and 236 (67.4%), respectively. Other factors considered were sex outside marriage (60, 17.1%), premarital sex (43, 12.2%), alcohol and drug abuse (39, 11.1%), and sex during menstruation (44, 12.5%).
Modes of transmission
The main modes of transmission of STIs known by students include sex with prostitutes/multiple partners (279, 79.7%), infected needles/drugs (256, 73.1%), blood transfusion (252, 72%), not using condoms (242, 69.1%), and mother to child transmission during childbirth (193, 55.1%). Other factors considered by students were poor hygiene 50 (14.2%), kissing 48 (13.7%), using public toilet (31, 8.8%), mosquitoes (35, 10%), shaking hands (13, 13.7%), and sharing towels 14 (4%) [ Table 3 ].
Knowledge about transmission of sexually transmitted infections ( n =350)

Symptoms of sexually transmitted infections
Fever on and off, vaginal/urethral discharge, genital ulcer, abdominal pain, swelling in the groin, and pain while passing urine were the options given to students to assess their knowledge about symptoms of STIs. Vaginal/urethral discharge was considered as a symptom of STI by 136 (38.8%) students followed by genital ulcer 120 (34.2%), fever on and off 118 (33.7%), pain while passing urine 108 (30.8%), swelling in the groin 90 (25.7%), and abdominal pain 104 (29.7%). All the options were considered as symptoms of STI by 41 (11.7%) students. Around 165 students did not know about the symptoms [ Chart 1 ].

Knowledge about symptoms of sexually transmitted infections ( n =350)
Complications of sexually transmitted infections
More than 50% (234) of students did not know about the complications of STI. Cervical cancer was answered by 94 (26.8%) students, infertility by 90 (25.7%), and abortion by 62 (17.7%). Forty (11.4%) students thought all the options to be complication of STIs [ Table 4 ].
Knowledge about complications of sexually transmitted infections ( n =350)

Only 59 (16.8%) students felt masturbation to be harmful to health whereas 138 (39.4%) students disagreed and 151 (43.1%) participants did not know its effect on health [ Table 5 ].
Attitude toward sexually transmitted infections and sexual health ( n =350)

Majority of the students (330, 94.2%) agreed that sex education should be mandatory for young people. However, 13 (3.7%) students were unsure and 7 (2%) students disagreed about the need for sex education.
One hundred and sixty-two (46.2%) participants felt that one should wait until marriage to have sex, whereas 103 (29.4%) students thought it was okay to have premarital sex. Moreover, 85 (24.2%) students did not have any opinion about premarital sex.
One hundred and nine (31.1%) participants did not mind marrying a person who had sex before marriage, whereas 153 (43.7%) students were against such an idea and 88 (25.1%) students could not opine about the issue.
Isolating patients of STI for the safety of others was considered an appropriate measure by 147 (42%) students; however, 120 (34.2%) students did not agree with such measures and 83 (23.7%) students did not know if it was right to do so.
The idea of banning prostitution to control the spread of STIs was agreed upon by 177 (50.5%) students and disagreed by 65 (18.5%) students. One hundred and eight (30.8%) students did not know if this could help control the spread of STI.
Emergency contraceptive pill was considered as a preventive measure for STI by 119 (34%) students, whereas 70 (20%) students disagreed with this measure and 161 (46%) students did not know if emergency contraceptive pills prevented acquiring STI.
Only 107 (30.5%) students agreed that there was no cure for HIV at present whereas 110 (31.4%) students thought HIV/AIDS can be cured and 108 (30.8%) students did not know if HIV can be cured.
The main objective of the study was to assess the knowledge, awareness, and attitude of the engineering college students about STIs, other than HIV and AIDS.
Our study shows that most of the students had heard about STIs, but they knew mostly about HIV/AIDS. STIs other than HIV were known by only around 64% (223) of students. Conditions such as LGV and chancroid were known only to 3%–7% of students. Furthermore, there were students who thought tuberculosis, leprosy, and vitiligo to be sexually transmitted. The findings are similar to a study conducted by Andersson-Ellström and Milsom[ 8 ] and Lal et al .[ 9 ]
Most of the participants in our study had known about these infections through teachers, internet, and newspaper/magazines. Information provided in internet and newspaper/magazines might not be complete and also mislead the student as not all content on internet is scrutinized by qualified health professional. Although many students knew about the STIs, they did not have in-depth knowledge about the diseases and their presentations. A similar finding has been published by Amu and Adegun in their study among secondary school adolescents.[ 10 ]
Most of the respondents had a good knowledge about prevention and transmission of STIs; however, not many were aware of the clinical features and complications of STIs. Only around 40% of students knew about the symptoms of STIs. Our review of literature shows a similar finding in many studies conducted at different geographic locations.[ 5 , 9 , 10 , 11 , 12 , 13 ]
The attitude of the students about sexual health was variable. Only about 16% students felt masturbation to be harmful to health and another 43% did not know about its effect on health. Whereas 39.4% felt it is not deleterious to health. One-third of students thought it was okay to have premarital sex and 24.2% students did not opine. Almost 46% students answered that they would wait till marriage to have sex. As mentioned in earlier studies, staying away from families and mingling with people from different sociocultural background might change their attitude toward premarital sex and safe sexual practices.[ 9 , 10 ]
When asked about prevention and containment of STI, more than 50% of the participants felt isolation of patient with STI and banning prostitution as an option to prevent spread of STI. Furthermore, almost one-third of the students thought emergency contraceptive pills can prevent STI and one-third did not know if it could prevent STI. Although most of the students knew about the mode of spread of STIs, many of them still had misconceptions about the prevention of spread of STIs. The main problem we felt was almost one-third of students felt emergency contraceptive pills can prevent STI. This point has not been discussed much in earlier studies.[ 8 , 14 ]
Most importantly, only 30% of the students knew that there was no cure for HIV/AIDS, 31.4% thought HIV infection can be cured, and 30% did not know if it can be cured.
Almost 90% of the students agreed about the need for sex education to be included in the curriculum. Probably, they felt they would have had a better knowledge if they had been educated about the issues at a younger age. Similar findings have been reported in other studies.[ 14 ]
On review of literature, not many studies have been done in India, to assess the knowledge and attitude of college students about STIs. Most of the times, sexual health is not discussed by parents/relatives with children as it is still considered a taboo by many people. Even in our study, parents/relatives as a source of information about STIs are very less (11%).[ 9 ] Our study shows that teachers, internet, and media are the main source of information for students.
The studies which have been done earlier are mainly among school students. Although few studies have been done in general population[ 15 , 16 , 17 ] and among university students,[ 4 , 5 ] it is from a different sociocultural background. Hence, our study has aimed at assessing knowledge and attitude of students from professional course (engineering) about STI and AIDS. The findings of our study show that it is important to orient the students about sexual health and safe sexual practices as it will go a long way in prevention and control of STIs. Furthermore, the morbidities and complications associated with STIs can be prevented.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Acknowledgment
We acknowledge the help and support provided by Dr. Jayanthi V, Dr. Savitha AS, Dr. Priyadarshini M, and Dr. Reshma Abraham in the conduct of the study and preparation of the manuscript.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Journal Proposal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Awareness, knowledge and risky behaviors of sexually transmitted diseases among young people in greece.

1. Introduction
2. materials and methods, 2.1. study design and participants, ethics approval, 2.2. data collection and processing, 2.3. evaluation of knowledge score, 2.4. data management, 2.5. statistical analysis, 3.1. socio-demographic characteristics of respondents, 3.2. sexual-risk associated knowledge, 3.3. evaluation of sexual behavior-associated risk, 3.4. assessment of std knowledge score, 3.5. unifactorial associations of knowledge score with socio-demographic characteristics, 3.6. multifactorial associations of knowledge score with socio-demographic characteristics, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest.
- Newman, L.; Rowley, J.; Hoorn, S.v.; Wijesooriya, N.S.; Unemo, M.; Low, N.; Stevens, G.; Gottlieb, S.; Kiarie, J.; Temmerman, M. Global Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2012 Based on Systematic Review and Global Reporting. PLoS ONE 2015 , 10 , e0143304. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Rowley, J.; Hoorn, S.V.; Korenromp, E.; Low, N.; Unemo, M.; AbuRaddad, L.J.; Chico, R.M.; Smolak, A.; Newman, L.; Gottlieb, S.; et al. Chlamydia, Gonorrhoea, Trichomoniasis and Syphilis: Global Prevalence and Incidence Estimates. 2016. Available online: https://www.who.int/bulletin/volumes/97/8/18-228486.pdf (accessed on 7 August 2021).
- Sexually Transmitted Infections (STIs). Available online: https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) (accessed on 7 August 2021).
- Korenromp, E.L.; Rowley, J.; Alonso, M.; Mello, M.B.; Wijesooriya, N.S.; Mahiané, S.G.; Ishikawa, N.; Le, L.-V.; Newman-Owiredu, M.; Nagelkerke, N.; et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes—Estimates for 2016 and progress since 2012. PLoS ONE 2019 , 14 , e0211720. [ Google Scholar ] [ CrossRef ]
- WHO|Global Health Sector Strategy on Sexually Transmitted Infections, 2016–2021. Available online: https://www.who.int/reproductivehealth/publications/rtis/ghss-stis/en/ (accessed on 7 August 2021).
- Juliana, N.C.A.; Omar, A.M.; Pleijster, J.; Aftab, F.; Uijldert, N.B.; Ali, S.M.; Ouburg, S.; Sazawal, S.; Morré, S.A.; Deb, S.; et al. The Natural Course of Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, and Mycoplasma genitalium in Pregnant and Post-Delivery Women in Pemba Island, Tanzania. Microorganisms 2021 , 9 , 1180. [ Google Scholar ] [ CrossRef ]
- World Health Organization. Department of Child and Adolescent Health and Development. World Health Organization, Child and Adolescent Health and Development Progress Report 2009 ; WHO: Geneva, Switzerland, 2010. [ Google Scholar ]
- Bekker, L.-G.; Johnson, L.; Wallace, M.; Hosek, S. Building our youth for the future. J. Int. AIDS Soc. 2015 , 18 , 20027. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Vanable, P.A.; Carey, M.P.; Brown, J.L.; DiClemente, R.J.; Salazar, L.F.; Brown, L.K.; Romer, D.; Valois, R.F.; Hennessy, M.; Stanton, B.F. Test–Retest Reliability of Self-Reported HIV/STD-Related Measures Among African-American Adolescents in Four U.S. Cities. J. Adolesc. Health 2009 , 44 , 214–221. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Siracusano, S.; Silvestri, T.; Casotto, D. Sexually Transmitted Diseases: Epidemiological and Clinical Aspects in Adults. Urol. J. 2014 , 81 , 200–208. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sieving, R.E.; O’Brien, J.R.G.; Saftner, M.A.; Argo, T.A. Sexually Transmitted Diseases Among US Adolescents and Young Adults: Patterns, Clinical Considerations, and Prevention. Nurs. Clin. N. Am. 2019 , 54 , 207–225. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Downing-Matibag, T.M.; Geisinger, B. Hooking Up and Sexual Risk Taking Among College Students: A Health Belief Model Perspective. APA PsycNet 2009 , 19 , 1196–1209. [ Google Scholar ] [ CrossRef ]
- Visalli, G.; Cosenza, B.; Mazzu, F.; Bertuccio, M.; Spataro, P.; Pellicanò, G.F.; di Pietro, A.; Picerno, I.; Facciolà, A. Knowledge of sexually transmitted infections and risky behaviours: A survey among high school and university students. J. Prev. Med. Hyg. 2019 , 60 , E84. [ Google Scholar ] [ CrossRef ]
- Xenaki, D.; Plotas, P.; Michail, G.; Poulas, K.; Jelastopulu, E. Knowledge, behaviours and attitudes for human papillomavirus (HPV) prevention among educators and health professionals in Greece. Eur. Rev. Med. Pharmacol. Sci. 2020 , 24 , 7745–7752. [ Google Scholar ] [ CrossRef ]
- Nikolopoulos, G.K.; Chanos, S.; Tsioptsias, E.; Hodges-Mameletzis, I.; Paraskeva, D.; Dedes, N. HIV incidence among men who have sex with men at a community-based facility in Greece. Cent. Eur. J. Public Health 2019 , 27 , 54–57. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Pavlopoulou, I.D.; Dikalioti, S.K.; Gountas, I.; Sypsa, V.; Malliori, M.; Pantavou, K.; Jarlais, D.D.; Nikolopoulos, G.K.; Hatzakis, A. High-risk behaviors and their association with awareness of HIV status among participants of a large-scale prevention intervention in Athens, Greece. BMC Public Health 2020 , 20 , 105. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Loumpardia, P.; Bourmpos, K.; Loumpardias, G.A.; Kalampoki, V.; Valasoulis, G.; Valari, O.; Vythoulkasl, D.; Deligeoroglou, E.; Koliopoulos, G. Epidemiological, Clinical, and Virological Characteristics of Women with Genital Warts in Greece—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/26054116/ (accessed on 17 September 2021).
- Folasayo, A.T.; Oluwasegun, A.J.; Samsudin, S.; Saudi, S.N.S.; Osman, M.; Hamat, R.A. Assessing the Knowledge Level, Attitudes, Risky Behaviors and Preventive Practices on Sexually Transmitted Diseases among University Students as Future Healthcare Providers in the Central Zone of Malaysia: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2017 , 14 , 159. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Gökengin, D.; Yamazhan, T.; Özkaya, D.; Aytuǧ, S.; Ertem, E.; Arda, B.; Serter, D. Sexual Knowledge, Attitudes, and Risk Behaviors of Students in Turkey. J. Sch. Health 2003 , 73 , 258–263. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ekşi, Z.; Kömürcü, N. Knowledge Level of University Students about Sexually Transmitted Diseases. Procedia Soc. Behav. Sci. 2014 , 122 , 465–472. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Carvalho, R.X.D.; Evangelista, T.M.; Ii, A.; Xavier, R.; Carvalho, C. Knowledge, attitudes and practices of university adolescents about syphilis: A cross-sectional study in the Northeast. Rev. Saúde Pública 2020 . [ Google Scholar ] [ CrossRef ]
- Caetano, M.E.; Linhares, I.M.; Pinotti, J.A.; da Fonseca, A.M.; Wojitani, M.D.; Giraldo, P.C. Sexual behavior and knowledge of sexually transmitted infections among university students in Sao Paulo, Brazil. Int. J. Gynecol. Obstet. 2010 , 110 , 43–46. [ Google Scholar ] [ CrossRef ]
- Samkange-Zeeb, F.N.; Spallek, L.; Zeeb, H. Awareness and knowledge of sexually transmitted diseases (STDs) among school-going adolescents in Europe: A systematic review of published literature. BMC Public Health 2011 , 11 , 1–12. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Huppert, J.S. Trichomoniasis in teens: An update. Curr. Opin. Obstet. Gynecol. 2009 , 21 , 371–378. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lo, Y.I.; Ji, D.A.; Hung, C.H. Prevalent and Incident HIV Diagnoses among Entamoeba histolytica-Infected Adult Males: A Changing Epidemiology Associated with Sexual Transmission—Taiwan, 2006–2013. PLoS Negl. Trop. Dis. 2014 , 8 , e3222. [ Google Scholar ] [ CrossRef ]
- Trichomoniasis—STI Treatment Guidelines. Available online: https://www.cdc.gov/std/treatment-guidelines/trichomoniasis.htm (accessed on 17 September 2021).
- Goundry, A.L.R.; Finlay, E.R.; Llewellyn, C.D. Talking about links between sexually transmitted infections and infertility with college and university students from SE England, UK: A qualitative study. Reprod. Health 2013 , 10 , 1–7. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Duru, O.E.; Yama, D.; Duro, A.A.; Odetola, T.; Danboyi, O.M.; Avidime, K.A. Mohammed, Correlates of socio-demographic variables and attitude to condom use in HIV/AIDS prevention among students in some selected Nigerian Universities. Niger. Med. J. 2020 , 61 , 316. [ Google Scholar ] [ CrossRef ]
- Almeida-Santos, M.A. Condom use and vulnerabilities to sexually transmitted infections in quilombola communities: A descriptive study Condom use in quilombola communities. Epidemiol. Serv. Saudes 2021 , 30 . [ Google Scholar ] [ CrossRef ]
- Zizza, A.; Guido, M.; Recchia, V.; Grima, P.; Banchelli, F.; Tinelli, A. Knowledge, Information Needs and Risk Perception about HIV and Sexually Transmitted Diseases after an Education Intervention on Italian High School and University Students. Int. J. Environ. Res. Public Health 2021 , 18 , 2069. [ Google Scholar ] [ CrossRef ]
- Kanda, L.; Mash, R. Reasons for inconsistent condom use by young adults in Mahalapye, Botswana. Afr. J. Prim. Health Care Fam. Med. 2018 , 10 , 7. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Milic, M.; Gazibara, T.; Stevanovic, J.; Parlic, M.; Nicholson, D.; Mitic, K.; Lazic, D.; Dotlic, J. Patterns of condom use in a university student population residing in a high-risk area for HIV infection. Eur. J. Contracept. Rep. Health Care 2020 , 25 , 269–278. [ Google Scholar ] [ CrossRef ]
- Fasciana, T.; Capra, G.; di Carlo, P.; Calà, C.; Vella, M.; Pistone, G.; Colomba, C.; Giammanco, A. Socio-Demographic Characteristics and Sexual Behavioral Factors of Patients with Sexually Transmitted Infections Attending a Hospital in Southern Italy. Int. J. Environ. Res. Public Health 2021 , 18 , 4722. [ Google Scholar ] [ CrossRef ]
- Samkange-Zeeb, F.; Mikolajczyk, R.T.; Zeeb, H. Awareness and Knowledge of Sexually Transmitted Diseases Among Secondary School Students in Two German Cities. J. Community Health 2012 , 38 , 293–300. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jahanfar, S.; Lye, M.S.; Rampal, L. A randomised controlled trial of peer-adult-led intervention on improvement of knowledge, attitudes and behaviour of university students regarding HIV/AIDS in Malaysia. Orig. Artic. Singap. Med J. 2009 , 50 , 173. [ Google Scholar ]
- Vaidakis, D.; Moustaki, I.; Zervas, I.; Barbouni, A.; Merakou, K.; Chrysi, M.S.; Creatsa, G.; Panoskaltsis, T. Knowledge of Greek adolescents on human papilloma virus (HPV) and vaccination, Medicine (United States). Medicine 2017 , 96 , e5287. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Okoboi, S.; Castelnuovo, B.; Moore, D.M.; Musaazi, J.; Kambugu, A.; Birungi, J.; Nanfuka, M.; van Rie, A. Incidence rate of sexually transmitted infections among HIV infected patients on long-term ART in an urban and a rural clinic in Uganda. BMC Public Health 2019 , 19 , 1–8. [ Google Scholar ] [ CrossRef ]
- Warner, C.; Carlson, S.; Crichlow, R.; Ross, M.W. Sexual Health Knowledge of U.S. Medical Students: A National Survey. J. Sex. Med. 2018 , 15 , 1093–1102. [ Google Scholar ] [ CrossRef ]
- Bjekic, M.D.; Sipetic-Grujicic, S.B.; Vlajinac, H.D.; Nikolic, A.M. Oral sex related knowledge and oral sex behavior among homosexual and heterosexual men in Belgrade: A cross-sectional study, Indian Journal of Dermatology. Venereol. Leprol. 2018 , 84 , 563–568. [ Google Scholar ] [ CrossRef ]
- Hendry, N.A.; Brown, G.; Dowsett, G.W.; Carman, M. Association between sexually transmissible infection testing, numbers of partners and talking to partners and friends about sexual health: Survey of young adults. Sex. Health 2017 , 14 , 378–382. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Masaro, C.L.; Dahinten, V.S.; Johnson, J.; Ogilvie, G.; Patrick, D.M. Perceptions of sexual partner safety, Sexually Transmitted Diseases. Sex Transm. Dis. 2008 , 35 , 566–571. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Vardavas, C.I.; Kondilis, B.K.; Patelarou, E.; Akrivos, P.D.; Falagas, M.E. Health literacy and sources of health education among adolescents in Greece. Int. J. Adolesc. Med. Health 2009 , 21 , 179–186. [ Google Scholar ] [ CrossRef ] [ PubMed ]
Click here to enlarge figure
| Age: Mean ± SD (Min–Max) | 21.48 ± 2.88(18–30) |
|---|---|
| : male/female/other n (%) | 449(24.5)/1377(75.10/7(0.4) |
| Primary/High School/University, n (%) | 16(0.9)/88(4.8)/1729(94.3) |
| : Full-time/Part-time/Unemployed, n (%) | 281(15.3)/417(22.7)/1135(61.9) |
| : City/Town/Village, n (%) | 1572(85.8)/157(8.6)/104(5.7) |
| : no/yes, n (%) | 848(46.3)/985(53.7) |
| : Heterosexual/Homosexual/Bisexual, n (%) | 1530(83.5)/86(4.7)/217(11.8) |
| : Mean ± SD (min–max) | 5.37 ± 10.32(0–250) |
| = 1322): Mean ± SD (min–max) | 17.41 ± 1.92(10–29) |
| Diseases Classified as STDs | Diseases Causing Genital Cancer | Diseases Causing Infertility | Diseases Transmitted by Oral Contact | |
|---|---|---|---|---|
| WartsHuman papilloma virus (HPV) | 467 (25.5) | |||
| Trichomoniasis | 31 (1.7) | 87 (4.8) | ||
| Hepatitis C | 147 (8.0) | 169 (9.2) | 264 (14.4) | |
| Hepatitis B | 124 (6.8) | 161 (8.8) | 265 (14.5) | |
| Hepatitis A | 575 (31.4) | 54 (2.9) | 75 (4.1) | |
| Genital Herpes | ||||
| Infectious mononucleosis | 292 (15.9) | 20 (1.1) | 57 (3.1) | 235 (12.8) |
| COVID-19 | 57 (3.1) | 5 (0.3) | 7 (0.4) | 100 (5.5) |
| Malaria | 20 (1.1) | 2 (0.1) | 12 (0.7) | 18 (1.0) |
| AIDS (HIV) | 620 (33.8) | |||
| Mycoplasmosis | 24 (1.3) | 58 (3.2) | ||
| Syphilis | 145 (7.9) | 317 (17.3) | ||
| Gonorrhea | 93 (5.1) | |||
| Amoebiasis | 14 (0.8) | 35 (1.9) | 44 (2.4) | |
| Echinococcosis | 135 (7.4) | 15 (0.8) | 40 (2.2) | 32 (1.8) |
| Molluscum contagiosum | 16 (0.9) | 31 (1.7) | 83 (4.5) | |
| Chlamydia | 182 (10.0) | |||
| Pubic lice | 25 (1.4) | 61 (3.3) | 38 (2.1) | |
| Do not know | 792 (43.2) | 953 (52.0) | 553 (30.2) |
| Way of Transmission | The Use of Condoms Protects Against STDs | The Use of Contraceptive Pills Protects Against STDs | |||
|---|---|---|---|---|---|
| 1198 (65.4) | Correct | 86 (4.7) | |||
| 1578 (86.1) | Yes | 545 (29.7) | 1544 (84.2) | ||
| 1406 (76.7) | Do not know | 90 (5.0) | Do not know | 203 (11.1) | |
| 1249 (68.1) | |||||
| 166 (9.1) | |||||
| Common utensils | 156 (8.5) | ||||
| 518 (28.3) | |||||
| Do not know | 19 (1.0) | ||||
| Never | 14 (0.8) |
| Only if partner prefers it | 23 (1.3) |
| In permanent sexual relationships | 512 (27.9) |
| In permanent sexual relationships following testing of a partner for STDs | 499 (27.2) |
| In case of HIV non-detectable seropositive partner | 39 (2.1) |
| In case my partner or I am receiving PrEP treatment | 5 (0.3) |
| Always | 741 (40.4) |
| At regular intervals following physical and blood examinations | 194 (10.6) |
| At regular intervals following blood examination | 422 (23.0) |
| Following suspicious sexual activity | 105 (5.7) |
| Following suspicion of STDs due to associated symptoms | 221 (12.1) |
| Never | 891 (48.6) |
| Yes (I always notify my partners): | 112 (6.1) |
| Yes (I notify only my permanent partner but not my occasional partners): | 56 (3.1) |
| Yes, without notifying my partners: | 16 (1.0) |
| No | 1.649 (90%) |
| STD Knowledge Score | |||
|---|---|---|---|
| Mean ± SD (%) | p Value | ||
| Gender | Male | 41.09 ± 12.16 | <0.001 |
| Female | 45.84 ± 12.36 | ||
| Education | Primary or High School | 42.33 ± 12.08 | 0.051 |
| University | 44.80 ± 12.52 | ||
| Employment | Unemployed | 44.37 ±12.52 | <0.001 |
| Part-time | 43.50 ±11.99 | ||
| Full-time | 47.51 ± 12.81 | ||
| Residence | Town or Village | 43.13 ± 12.92 | 0.039 |
| City | 44.91 ± 12.42 | ||
| Do you have a permanent partner | No | 43.44 ± 12.85 | <0.001 |
| Yes | 45.70 ± 12.12 | ||
| Sexual preference | Heterosexual | 44.32 ± 12.59 | 0.065 |
| Homosexual | 46.64 ± 12.66 | ||
| Bisexual | 46.21 ± 11.71 | ||
| Age | Pearson’s r | r = 0.177 | <0.001 |
| Number of sexual partners to date | r = 0.105 | <0.001 | |
| Reference Category | R | Beta ± SE | p-Value | |
|---|---|---|---|---|
| Age | --- | 0.031 | 0.62 ± 0.11 | <0.001 |
| Gender (female) | Male | 0.027 | 4.62 ± 0.66 | <0.001 |
| Education (university) | Primary or High School | 0.002 | 2.39 ± 1.22 | 0.050 |
| Employment (Unemployed, -Part time) | Full time | 0.000 | 0.80 ± 0.87 | 0.420 |
| Residence (town-village) | City | 0.001 | 1.01 ± 0.81 | 0.215 |
| Do you have a permanent partner | No | 0.002 | 1.23 ± 0.58 | 0.035 |
| Sexual preference(Homosexual-Bisexual) | Heterosexual | 0.003 | 1.90 ± 0.77 | 0.014 |
| Number of sexual partners to date | --- | 0.006 | 0.08 ± 0.03 | 0.003 |
| MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
Share and Cite
Voyiatzaki, C.; Venetikou, M.S.; Papageorgiou, E.; Anthouli-Anagnostopoulou, F.; Simitzis, P.; Chaniotis, D.I.; Adamopoulou, M. Awareness, Knowledge and Risky Behaviors of Sexually Transmitted Diseases among Young People in Greece. Int. J. Environ. Res. Public Health 2021 , 18 , 10022. https://doi.org/10.3390/ijerph181910022
Voyiatzaki C, Venetikou MS, Papageorgiou E, Anthouli-Anagnostopoulou F, Simitzis P, Chaniotis DI, Adamopoulou M. Awareness, Knowledge and Risky Behaviors of Sexually Transmitted Diseases among Young People in Greece. International Journal of Environmental Research and Public Health . 2021; 18(19):10022. https://doi.org/10.3390/ijerph181910022
Voyiatzaki, Chrysa, Maria S. Venetikou, Effie Papageorgiou, Fragiski Anthouli-Anagnostopoulou, Panagiotis Simitzis, Dimitrios I. Chaniotis, and Maria Adamopoulou. 2021. "Awareness, Knowledge and Risky Behaviors of Sexually Transmitted Diseases among Young People in Greece" International Journal of Environmental Research and Public Health 18, no. 19: 10022. https://doi.org/10.3390/ijerph181910022
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 02 August 2022
Sexually transmitted infections and female reproductive health
- Olivia T. Van Gerwen ORCID: orcid.org/0000-0002-9362-6234 1 ,
- Christina A. Muzny ORCID: orcid.org/0000-0002-4005-3858 1 &
- Jeanne M. Marrazzo 1
Nature Microbiology volume 7 , pages 1116–1126 ( 2022 ) Cite this article
26k Accesses
58 Citations
459 Altmetric
Metrics details
- Applied microbiology
- Bacterial infection
- Microbiology
Women are disproportionately affected by sexually transmitted infections (STIs) throughout life. In addition to their high prevalence in women, STIs have debilitating effects on female reproductive health due to female urogenital anatomy, socio-cultural and economic factors. In this Review, we discuss the prevalence and impact of non-HIV bacterial, viral and parasitic STIs on the reproductive and sexual health of cisgender women worldwide. We analyse factors affecting STI prevalence among transgender women and women in low-income settings, and describe the specific challenges and barriers to improved sexual health faced by these population groups. We also synthesize the latest advances in diagnosis, treatment and prevention of STIs.
Similar content being viewed by others
Prevalence of STIs, sexual practices and substance use among 2083 sexually active unmarried women in Lebanon
Hormonal contraceptive use and the risk of sexually transmitted infections: a systematic review and meta-analysis
Antimicrobial treatment and resistance in sexually transmitted bacterial infections
Sexually transmitted infections (STIs) cause reproductive morbidity worldwide. In 2019, the World Health Organization (WHO) estimated that there were 376 million new episodes of chlamydia, gonorrhoea, syphilis and trichomoniasis (Fig. 1 ) 1 . In 2019, the United States Centers for Disease Control and Prevention (CDC) reported a nearly 30% increase in chlamydia, gonorrhoea and syphilis between 2015–2019 and a rising incidence of all STIs for the sixth consecutive year 2 . In the United States in 2018, several STIs were estimated to be more prevalent among women than men, including gonorrhoea, chlamydia and trichomoniasis 3 . Women often experience complications from STIs, including infertility and chronic pelvic pain, that can have lifelong impact 4 . STIs can increase peripartum morbidity and mortality in both industrialized areas and in rural and underserved areas of developed countries.
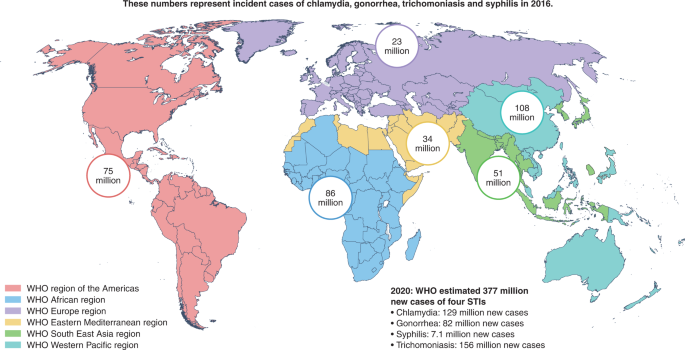
WHO global regions and the incident cases of four STIs (chlamydia, gonorrhoea, trichomoniasis and syphilis) from 2016 estimates. The WHO estimates of new cases of these four STIs worldwide in 2020 are shown at the bottom right of the figure.
The larger impact of STIs in women compared with men is in part due to the female anatomy (Fig. 2 ). A woman’s urogenital anatomy is more exposed and vulnerable to STIs compared with the male urogenital anatomy, particularly because the vaginal mucosa is thin, delicate and easily penetrated by infectious agents 5 . The cervix at the distal end of the vagina leads to the upper genital tract including the uterus, endometrium, fallopian tubes and ovaries. STIs can produce a variety of symptoms and effects at different parts of the female reproductive tract, including genital ulcer disease, vaginitis, pelvic inflammatory disease (PID) and infertility 6 .
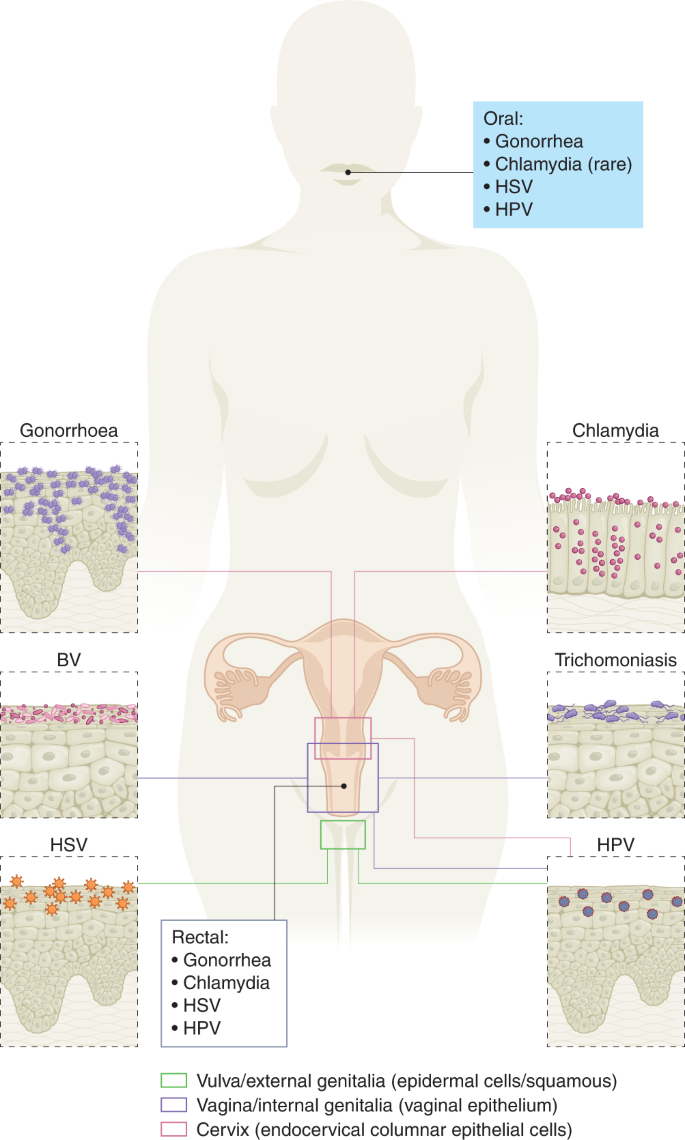
STIs can affect genital and extragenital sites in women. Gonorrhoea and chlamydia typically present as cervicitis. Bacterial vaginosis (BV) and trichomoniasis can also cause cervicitis, but more commonly manifest as vaginitis. HSV and HPV most typically affect the vulva or external genitalia of women.
In this Review, we focus on the impact of non-HIV bacterial, viral and parasitic STIs on the sexual and reproductive health of cisgender women (Table 1 ). We discuss adverse outcomes of STIs, treatment and prevention, including vaccine development. STIs in transgender women (TGW) are discussed in brief because an exhaustive review of STIs in this population has recently been published 7 , 8 . We do not review developments in HIV prevention or treatments in women and refer readers to reviews published elsewhere 9 , 10 , 11 , 12 , 13 . Hepatitis B was also excluded as it would merit its own dedicated review.
Human papilloma virus (HPV) is a small circular double-stranded DNA papilloma virus that infects cutaneous or mucosal epithelial tissues in humans 14 . More than 200 genotypes of HPV have been identified, including at least 40 that affect the genitals, and are grouped into high- or low-risk 15 . Although HPV infection is often asymptomatic and self-limiting, symptoms can include anogenital warts, respiratory papillomatosis, and precancerous or cancerous cervical, penile, vulvar, vaginal, anal and oropharyngeal lesions 16 . HPV is the most common STI worldwide, with most sexually active people exposed to it during their lifetime 17 . Among women, HPV prevalence is highest among those in low- and middle-income countries (LMICs), peaking at <25 years old 18 . While most women clear HPV spontaneously, persistent infection can cause cervical, anal, or head and neck cancer 19 . Cervical cancer has been a leading cause of mortality among women for decades; in 2012, there were 266,000 HPV-related cervical cancer deaths worldwide, accounting for 8% of all female cancer deaths that year 20 . Cervical cancer also causes substantial genitourinary morbidity, including radiation treatment-related infertility and urinary or faecal incontinence 21 . Persistent infection with high-risk HPV types is responsible for 99.7% of cervical squamous cell cancer cases 22 .
In women with HPV, one factor that increases the risk of progression to cervical cancer is co-infection with a different STI 23 . HIV, for example, increased the oncogenic potential of HPV, especially in immunosuppressed women 24 . Women adherent to antiretroviral therapy are less likely to acquire high-risk HPV types, and progression to pre-malignant or malignant lesions is reduced 25 . In HIV-negative women, persistent HPV increases the risk of acquiring HIV, but the underlying mechanism is unclear 23 . Persistent HPV and Chlamydia trachomatis co-infection has also been proposed as a cofactor in the progression of cervical malignancy in women, with chronic inflammation as a mediating factor 26 . For these reasons, primary prevention using HPV vaccination is essential.
HPV vaccine development is one the most important medical achievements of the twenty-first century. Universal HPV vaccination has the potential to prevent between 70% to 90% of HPV-related disease, including anogenital warts and HPV-associated cancers 27 . The global strategy of the WHO is to vaccinate 90% of females by age 15, in addition to screening and treating older females, with the goal of eliminating cervical cancer in the next century 28 . There are four available HPV vaccines: Gardasil (Merck, 2006), Ceravrix (GlaxoSmithKline, 2007), Gardasil 9 (Merck, 2014) and Cecolin (Xiamen Innovax Biotech Co., 2021) 27 . All offer protection against HPV16 and HPV18 high-risk genotypes, which account for 66% of all cervical cancers (Table 2 ). Gardasil 9 targets 5 additional oncogenic HPV types (HPV31, 33, 45, 52, 58) that account for another 15% of cervical cancers. Gardasil products also offer protection against HPV6 and HPV11, which cause >90% of genital warts 16 . Cervarix and Cecolin offer protection only against HPV16 and HPV18 29 .
HPV vaccination programmes have resulted in a profound reduction in pre-malignant and malignant cancers in women 30 . In England since 2008, HPV immunization has been routinely recommended for girls aged 12–13 years, with a catch-up programme at 14–18 years. A 2019 observational study of this population reported that for those vaccinated at ages 12–13, there was an estimated 87% relative reduction in cervical cancer rates and a 97% risk reduction for cervical intraepithelial neoplasia 3 compared with a reference unvaccinated cohort. Among vaccinated cohorts in the same study, since 2008, investigators estimated 448 fewer cervical cancers and 17,235 fewer cervical intraepithelial neoplasia 3 cases than expected by 2019 31 . The study authors concluded that the immunization programme in England has almost eliminated cervical cancer in women born since 1995. Programmes in Denmark and Sweden have reported similar levels of success 30 .
These findings show that elimination of cervical cancer in the short term is possible with primary prevention programmes, at least in adequately resourced countries. In other settings, infrastructural and cultural challenges can make establishment of such programmes difficult. Efforts to implement HPV vaccination programmes in all areas are essential, especially to vaccinate girls before sexual debut and complete all doses in the vaccination series 32 .
HPV-related anal cancer is also of concern for women, especially those with HIV 33 . HPV has been linked to 80% of anal cancer cases in the United States 34 . Women living with HIV have a 7.8-fold higher risk of anal carcinoma in situ and a 10-fold higher risk of anal squamous cell carcinoma compared with women without HIV 35 , 36 . In contrast to cervical cancer, it is less clear whether screening for HPV-associated precancerous lesions will impact the incidence of anal cancers. The Anal Cancer HSIL Outcomes Research (ANCHOR) study is an ongoing trial investigating whether treatment of precancerous high-grade squamous intraepithelial lesions (HSIL) is effective in reducing the incidence of anal cancer in people with HIV, including women ( NCT02135419 ). Preliminary results in 4,446 participants demonstrated that removal of HSILs identified on screening anal Papanicolaou smears notably reduced the risk of progression to anal cancer 37 . Currently, there are no routine screening recommendations for anal cancer for women 16 .
Detection of high-risk HPV based on cytology screening of precancerous anal lesions is challenging because sensitivity is limited and diagnosis requires the provision of adequate follow-up infrastructure (for example, high-resolution anoscopy). Molecular assays might reduce the number of unnecessary high-resolution anoscopies performed 38 , 39 .
Genital herpes is caused by herpes simplex virus type 1 (HSV-1) or type 2 (HSV-2), which are members of the Herpesviridae family. In 2016, the WHO estimated that up to 192 million people were affected by genital HSV-1 and 491 million people by HSV-2 40 . Although HSV-1 is more commonly associated with oral disease (‘cold sores’), the proportion of sexually transmitted anogenital herpes attributed to HSV-1 has increased over time, especially among women aged 18–30 years old 41 . HSV-2 is the primary causative agent of genital herpes infections globally 42 . Although HSV infection is chronic and lifelong, many women experience few or no symptoms. When present, symptoms range from painful genital sores to discomfort that is sometimes misdiagnosed as recurrent vulvovaginal candidiasis. HSV infections can be managed with oral antivirals including suppressive therapy, such as valacylovir (Table 3 ) 16 .
One devasting consequence of HSV infection in pregnant women is neonatal herpes. In the U.S., the incidence of neonatal HSV has increased, with 5.3/10,000 infants affected in 2015, up from 3.75/10,000 births in the early 2000s 43 , 44 . Neonatal herpes manifests when neonates are infected with HSV during vaginal birth. Neonatal infection can affect the skin, eyes or mouth, but the central nervous system or multiple organs can also become infected; incidence of central nervous system manifestations of neonatal herpes is estimated to be between 1 in 3,000 and 1 in 20,000 live births. Mortality in such cases without treatment is as high as 85%, with a high likelihood of long-term neurological sequalae in those infants who do survive 45 . Mother-to-child transmission is preventable by elective Caesarian-section delivery in mothers with active herpetic lesions.
HSV-2 infection in women is associated with a threefold increased risk of HIV acquisition and horizontal transmission 46 , 47 . One analysis concluded that an estimated 420,000/1.4 million HIV infections (population attributable fraction 29.6% (22.9–37.1)) were attributed to HSV-2 infections worldwide 48 .
Diagnosis of genital herpes is challenging because characteristic lesions often resolve by the time patients present to care. A presumptive diagnosis can be made by physical examination but should be confirmed with type-specific nucleic acid amplification testing (NAAT) or culture 16 . The use of HSV serologies is discussed in detail elsewhere 16 , 49 .
Episodic and suppressive treatments for HSV do not prevent recurrence. Even if indefinite suppressive antivirals are administered, HSV shedding can still occur 50 . Lifelong antivirals are not cost effective and perfect adherence can be challenging for patients 16 . Therefore, there is continued interest in developing vaccines for HSV-2 (Table 2 ). Despite extensive investigation of many candidate HSV vaccines, none have performed well enough in clinical trials to be brought to the market. In the 1990s, initial studies investigated subunit vaccines, which aimed to select targets that induce immune responses against HSV-2 51 . One such vaccine candidate, Simplirix (GSK), targeted the glycoprotein D subunit (gD), which facilitates host cell entry by HSV. Initial trials demonstrated 74% efficacy in HSV-1/HSV-2 seronegative women with seropositive partners, but these results were not replicated in seronegative men 52 . Given the promising initial efficacy findings among seronegative women, additional trials were performed in women; however, they largely failed to meet primary endpoints. Most notably, efficacy of the same GSK gD subunit vaccine in the Herpevac trial was only 58% and 20% against HSV-1 and HSV-2, respectively 53 . The discrepancy in results between these two studies is puzzling, but given that gD is known to elicit a strong immune response, it has been a component in several additional vaccine candidates 51 , 54 . A major concern with HSV subunit vaccines is cost, so research and development strategies have pivoted towards cheaper nucleic acid-based vaccine platforms and the potential of live-attenuated vaccines 55 , 56 , 57 . Given the complex immunology of HSV, there is interest in understanding the role of mucosal immunity in the genital tract to aid the development of a successful vaccine against HSV-2 58 .
Bacterial STIs
Syphilis is caused by the spirochaete Treponema pallidum subspecies pallidum . Main symptoms of syphilis include anogenital or oral painless chancres in primary syphilis, diffuse rash in secondary syphilis, aseptic meningitis and pan uveitis 59 . The impact of syphilis on women has intensified over the past decade. In the United States between 2014 and 2018, rates of primary and secondary syphilis among women doubled and similar trends have been noted globally 1 , 60 . Rates of primary and secondary syphilis are lower among US women compared with men who have sex with men (MSM), but cases among heterosexual women increased by 178.6% between 2015 and 2019, suggesting an epidemic mediated by heterosexual transmission 60 . Increasing primary and secondary syphilis cases among women are also predominant among those of childbearing age 60 . Therefore, the rising rates of congenital syphilis are not surprising; in 2013, congenital syphilis occurred in 9.2 cases per 100,000 live births and in 2020 increased to 57.3 cases per 100,000 live births 60 . Tragically, this trajectory has resulted in increasing numbers of syphilitic stillbirths and congenital syphilis-related infant deaths 60 . Syphilis in pregnancy is the second leading cause of stillbirth globally and has been associated with low birth weight, neonatal infections and preterm delivery 61 . Congenital syphilis is preventable with early detection and prompt treatment of maternal infection; however, many women lack access to adequate syphilis treatment, even with early diagnosis 62 . Limited prenatal care and timely syphilis testing are barriers to preventing congenital syphilis, especially in LMICs where prenatal care and syphilis screening resources are limited 63 . Currently, the CDC and WHO recommend routine serologic screening of pregnant women at their initial prenatal visit, at 28 weeks’ gestation and at the time of delivery in high-prevalence settings, although recommendations vary geographically 16 , 64 .
Consequences of untreated syphilis in pregnancy are dire for both mother and neonate. Options for effective treatment are straightforward because syphilis is treatable with penicillin G and antimicrobial resistance is essentially non-existent 16 . Depending on the stage and site of infection, treatment regimens differ in terms of penicillin dose frequency and route of administration, as discussed elsewhere 16 . Doxycycline can be given in certain situations to non-pregnant women (that is, in cases of true penicillin allergy) to effectively treat primary, secondary or latent syphilis; however, penicillin G is the only antimicrobial agent that has demonstrated efficacy in preventing congenital syphilis 65 . Thus, treatment of women with a true penicillin allergy and those who are unable to access penicillin G is challenging. The ideal dosing regimen of penicillin G for syphilis treatment during pregnancy is not clear, but evidence suggests that an additional injection of benzathine penicillin G after the initial dose reduces the risk of congenital syphilis 65 , 66 , 67 .
Chlamydia trachomatis is an obligate intracellular Gram-negative bacterium that can replicate only inside a host cell 68 . Although usually asymptomatic in women, C. trachomatis infection can result in reproductive damage, and when untreated, it can be associated with PID, ectopic pregnancy, chronic pelvic pain and tubal infertility. In the U.S., women <25 years account for most infections, so annual screening in this age group is recommended to reduce the frequency of PID and other adverse health outcomes 16 , 60 , 69 . Perinatal maternal Chlamydia infection is associated with preterm birth, stillbirth, low birth weight and neonatal infections such as pneumonia and conjunctivitis 69 , 70 , 71 .
The composition of the vaginal microbiome probably has a role in host defence against chlamydial infection. An optimal vaginal microbiota is dominated by Lactobacillus crispatus , which produces lactic acid that has antimicrobial properties and can inactivate C. trachomatis , decreasing the likelihood of ascension of this pathogen into the upper genital tract 72 . Women with bacterial vaginosis, defined by a paucity of L. crispatus and other favourable vaginal lactobacilli, and an increased abundance of facultative and strict anaerobes, may have reduced immune defence against C. trachomatis , leading to increased risk of acquiring this pathogen as well as Neisseria gonorrhoeae and Trichomonas vaginalis 73 .
Prompt diagnosis and treatment are the best approaches to preventing the reproductive morbidity and sequelae associated with chlamydia (Table 3 ). For decades, single-dose oral azithromycin (2 g) was a first-line treatment option for C. trachomatis , offering the option of directly observed therapy. Recent data suggest that this regimen is inferior to oral doxycycline given twice daily for 7 days, specifically for women and men with urogenital and rectal infection 74 . Thus, the only currently recommended first-line agent for uncomplicated urogenital or rectal chlamydia is multidose doxycycline 16 . This change in guidance in 2021 was driven by data related to men with chlamydia; more efficacy studies are needed in women 75 . However, rectal chlamydial infection has been found to occur in women more frequently than previously thought. In addition to receptive anal sex, auto-inoculation from cervicovaginal chlamydial infection may yield rectal infection 76 , 77 . While single-dose azithromycin is efficacious for urogenital C. trachomatis in women, the possibility that concomitant rectal infection that may not be adequately treated with this regimen is concerning 78 . Single-dose azithromycin is also recommended for the treatment of chlamydia in pregnant women as doxycycline is not safe in pregnancy 16 .
Currently, no vaccines are available for C. trachomatis 79 . Given the high rates of re-infection, especially among young women 80 , vaccines offer the promise of both protecting from disease and reducing antibiotic use, treatment burden, preventing development of antimicrobial resistance in other infections (for example, gonorrhoea) and decreasing reproductive morbidity 81 , 82 . A major challenge in C. trachomatis vaccine research has been targeting both humoral and cell-mediated immune responses in infected individuals; complete protection requires activity in both pathways 83 , 84 . Comprehensive monitoring of this complicated immune response is difficult. Despite approximately 220 chlamydial vaccine trials having been conducted from 1946 until the present—over seven decades—an effective vaccine remains elusive (Table 2 ).
Gonorrhoea is caused by N. gonorrhoeae , a Gram-negative diplococcal bacterium. N. gonorrhoeae can yield mucosal infections in epithelia of the urogenital tract and the ectocervix 85 . Gonorrhoea is extremely common worldwide, with an estimated global annual incidence of 86.9 million adults and a prevalence among women of 0.9%, with the greatest burden among women in LMICs 1 . Genitourinary gonorrhoea can present in women as cervicitis or urethritis but is mostly asymptomatic 86 . If untreated, gonococcal infections can result in serious complications such as PID, tubal infertility, ectopic pregnancy and disseminated gonococcal infection 87 , 88 , 89 . Gonorrhoea also facilitates transmission of HIV and other STIs 86 . Similar to other bacterial STIs, untreated gonorrhoea has been associated with adverse birth outcomes such as preterm birth, low birth weight and premature rupture of membranes 90 , 91 . Perinatal exposure to an infected cervix puts neonates at risk for serious complications such as gonococcal sepsis and ophthalmia neonatorum, the latter of which can lead to blindness if untreated 92 .
When detected in a timely manner, gonorrhoea can be treated and its negative sequelae can be avoided. The landscape of gonorrhoea treatment, however, has been in flux over the past several decades due to the emergence of resistance to multiple antimicrobials among gonococcal isolates worldwide 60 , 93 . The Gonococcal Isolate Surveillance Program (GISP) was established in the United States in 1986 to monitor trends in antimicrobial resistance among urethral N. gonorrhoeae isolates. This programme is integral in generating clinical guidance on gonococcal therapy 94 . Since the generation of GISP, notable gonococcal resistance has emerged to several antimicrobial drug classes, including fluoroquinolones (for example, ciprofloxacin) and macrolides (for example, azithromycin); use of these agents is no longer recommended in national treatment guidelines 16 , 95 . The 2021 CDC STI treatment guidelines currently recommend cephalosporins for first-line gonorrhoea treatment, specifically 500 mg intramuscular ceftriaxone for people weighing less than 150 kg 16 . Oral cephalosporins, such as cefixime, are not recommended as first-line treatment, given many instances of treatment failure and limited efficacy in treating pharyngeal gonococcal infection 96 , 97 , 98 , 99 , 100 . While ceftriaxone remains a reliable choice in most situations, there is growing concern for widespread ceftriaxone-resistant gonococcal isolates. Such strains have been reported in Denmark, France, Japan, Thailand and the United Kingdom; alternative treatment options are limited 101 , 102 , 103 , 104 .
In the past 10 years, several novel anti-gonococcal antimicrobials have been conceptualized and developed 105 , 106 , 107 . One example is zoliflodacin, a single-dose spiropyrimidinetrione antimicrobial that works by inhibiting DNA biosynthesis through blocking gyrase complex cleavage 108 . In a multicentre Phase 2 trial in the United States, most patients who received zoliflodacin for uncomplicated urogenital and rectal gonococcal infection were successfully treated. Efficacy for treating pharyngeal infections was less impressive, with only 50% and 82% of those who received 2 g and 3 g of zoliflodacin, respectively, achieving cure. Regardless, several studies have shown that zoliflodacin continues to have excellent in vitro activity against multidrug-resistant gonococcal isolates, including those with resistance to extended-spectrum cephalosporins 109 , 110 .
Given global increases in antimicrobial resistance, vaccines preventing acquisition of gonorrhoea are urgently needed. Modelling studies have demonstrated that a gonococcal vaccine of moderate efficacy and duration would have a substantial impact on disease prevalence and prevention of adverse reproductive sequelae 111 . The WHO has named N. gonorrhoeae as a global priority, hence increasing interest and funding have been funnelled into development of candidate gonorrhoea vaccines ( Table 2 ) . Fortunately, available tools for other gonococcal species may offer opportunity for N. gonorrhoeae prevention, an approach currently under study. The rMenB+OMV NZ vaccine (Bexsero) was first licensed in the European Union in 2013 and in the United States in 2015 for prevention of meningococcal disease caused by N. meningitidis serogroup B 112 . An earlier version of a vaccine aimed at a meningococcal B outbreak (MeNZB) was introduced in New Zealand in the early 2000s. A retrospective case-control study revealed that this vaccine programme not only led to a decrease in meningococcal disease, as expected, but had an estimated reduction of future gonorrhoea acquisition of 31% (95% CI: 21–39) in those who received 3 doses of vaccine 113 . Clinical trials are ongoing to assess the efficacy of Bexsero in preventing urogenital and/or rectal gonorrhoea (NCT 04350138).
Parasitic STIs
Trichomoniasis.
Globally, trichomoniasis has an enormous impact on women as the most common non-viral STI 1 . It is caused by the parasitic protozoan Trichomonas vaginalis , and results in vaginal discharge and dysuria when symptomatic 114 . T. vaginalis has also been associated with adverse birth outcomes (for example, preterm birth, low birth weight, preterm rupture of membranes) 115 and an increased risk of HIV acquisition and transmission, PID and cervical cancer related to HPV infection 116 , 117 , 118 , 119 . Despite these significant health impacts, has been viewed as a nuisance infection and investigation has been limited until recent years. Globally, trichomoniasis is not currently reportable 120 , 121 . Marked racial and geographic disparities have also been described in relation to T. vaginalis infection. In the United States, according to the most recent National Health and Nutrition Examination Survey data, the overall prevalence of T. vaginalis in women in the United States is 1.8% 122 , being 6.8% among black women compared with 0.4% among women of other racial/ethnic backgrounds 122 . The global epidemiology of trichomoniasis is less well-defined, but one systematic review including men and women noted a prevalence range of 3.9%–24.6% in LMICs from Latin America and Southern Africa 123 .
Diagnosis of T. vaginalis has greatly improved in women (and men) over the past decade with the use of highly sensitive and specific NAAT tests 124 , 125 , 126 , 127 . Treatment recommendations for women with T. vaginalis have been largely unchanged for decades, with 5-nitroimidazoles such as metronidazole (MTZ) and tinidazole (TDZ) remaining mainstays of therapy (Table 3 ). Guidelines published by the WHO in June 2021 recommend treatment with either a single dose of MTZ (2 g orally) or twice-daily dose of MTZ (500 mg orally) for 7 days 128 . In LMIC and other resource-limited settings where adherence to a multidose MTZ regimen may be difficult, a single-dose treatment option may be advantageous. Accumulating data suggest, however, that single-dose treatment with MTZ for women may not be optimal 129 , 130 . A recent multicentre randomized controlled trial in the United States compared the multidose oral MTZ regimen to the single-dose regimen among HIV-negative women. Participants who received the multidose regimen were significantly less likely to re-test positive for T. vaginalis at 1 month compared with women in the single-dose group; adherence among both groups were similar 130 . Thus, the multidose oral MTZ regimen is now the recommended regimen for all women; this update may influence future global guidelines moving forward 16 . Notably, MTZ is safe for pregnant women at all stages of pregnancy 131 . Therefore, to prevent adverse birth outcomes associated with this infection, prompt treatment is essential 115 , 131 .
Due to limited clinical trial data in men, the single 2 g dose of oral MTZ remains the recommended treatment regimen for T. vaginalis in men 16 . This is the first time there has been a discrepancy in the treatment of an STI based on gender. Such a situation could lead to complicated public health logistics in partner treatment of infected women and additional studies are needed to discover the optimal treatment regimen for men 132 . Women are re-infected by their male sex partners if they are either not treated or are inadequately treated for trichomoniasis 133 .
Oral secnidazole (SEC) was recently approved by the US Food and Drug Administration (FDA) for treatment of T. vaginalis in both men and women. Given its microbiologic cure rate of 92.2% in a randomized double-blind placebo-controlled delayed-treatment study, SEC offers a promising new single-dose treatment option for trichomoniasis 134 .
STI prevention challenges and disparities in minority populations
Gender minority women.
STI prevention poses challenges for women in general, but some populations face additional barriers to sexual healthcare (Table 4 ). Gender minority women, including transgender women (TGW), or people who were assigned male sex at birth but whose gender identity is female, are at high risk of acquiring STIs through engagement in sexual behaviours such as commercial sex work and condomless anal receptive intercourse 135 . Consequently, STIs disproportionally affect TGW; an estimated 14% of TGW in the United States are living with HIV 136 , and global bacterial STI prevalence has been reported to be as high as 50%, 19% and 25% for syphilis, gonorrhoea and chlamydia, respectively 8 , 135 , 136 . These high rates may be related to the limited engagement of TGW with effective sexual health services—for example, regular HIV/STI screening—and underutilization of pre-exposure prophylaxis 137 , 138 . This lack of engagement arises from a suite of factors, including stigma, mistrust of the healthcare system, limited trans-affirming clinical services, previous sexual trauma or competing healthcare priorities such as hormone replacement therapy for gender-affirming therapy 139 , 140 .
Given the combination of this population’s unique sexual health needs and mistrust of the medical establishment, community-driven patient-centred prevention efforts are necessary. One qualitative study assessing attitudes related to HIV prevention among TGW in the Southeastern United States found that limited trans-affirming sexual health resources are a major barrier to engaging in care 141 . In addition, an individualized approach to affirming sexual history-taking should be employed by providers when caring for TGW. More broadly, another driver of sexual health disparities among TGW is their limited representations in research studies and clinical trials in the field. Data for TGW are often aggregated together with those of cisgender MSM and thus difficult to interpret. Study design and trial recruitment planning efforts must be made to appropriately report data on TGW.
Women in LMICs
Women living in LMICs face additional STI prevention challenges largely due to limited healthcare infrastructure, availability of sexual health resources and misogynistic cultural attitudes towards sexuality 142 . African countries have been particularly impacted, with the most recent WHO STI global prevalence estimates reporting the highest rates worldwide for gonorrhoea, trichomoniasis and syphilis among women in the region 1 . In addition, until very recently, distribution of HPV vaccines has been largely limited to European and North American nations, with LMICs receiving little support until approximately 2019. Even when HPV vaccines were introduced in many LMICs, uptake of the full series has been limited due to logistical challenges, highlighting an enormous, missed opportunity to curtail the rates of cervical cancer worldwide 32 .
Affordable STI testing that can be performed at the point-of-care is an important tool that needs to be made available to women in LMICs. Concurrent availability and accessibility of appropriate treatment for STIs are also essential. Clinics or other community settings need to provide confidential diagnostics and treatment to mitigate restricted access owing to stigma and the potential for gender-based violence that sometimes occurs when male sexual partners find out about sexual health diagnoses. Vaccines against STIs such as C. trachomatis and HSV-2 also hold great promise for women of LMICs, offering both disease prevention and a reduction in the need for diagnosis and treatment. Continued pursuit of safe and effective STI vaccines should be prioritized.
Women are disproportionately affected by STIs throughout their lives compared with men. This is mainly owing to the higher efficiency of male-to-female transmission of STIs and the biology of the female reproductive tract. In addition, the social and structural barriers to women realizing full sexual health include limited availability of HPV immunization in many parts of the world, barriers to contraception access, lack of confidential evaluation and counselling services, and lack of STI diagnostics. Finally, women are generally less well-resourced, both financially and socially, than men. This restricts their access to the resources required for sexual safety such as comprehensive sexual healthcare and HIV/STI prevention services, and the financial security that is fundamental to sexual health. Ensuring access to diagnostics and therapies on its own will not address the yawning gap in sexual health between men and women but would be a good start.
Rowley, J. et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull. World Health Organ. 97 , 548–562 (2019).
Article PubMed PubMed Central Google Scholar
Reported STDs reach all-time high for 6th consecutive year. CDC (3 April 2021); https://www.cdc.gov/nchhstp/newsroom/2021/2019-std-surveillance-report-press-release.html
Kreisel, K. M. et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2018. Sex. Transm. Dis . https://doi.org/10.1097/OLQ.0000000000001355 (2021).
Rietmeijer, C. A. et al. Report from the national academies of sciences, engineering and medicine–STI: adopting a sexual health paradigm–a synopsis for sti practitioners, clinicians, and researchers. Sex. Transm. Dis . https://doi.org/10.1097/olq.0000000000001552 (2021).
CDC Fact Sheet: 10 Ways STDs Impact Women Differently from Men (Centers for Disease Control and Prevention, 2011); https://www.cdc.gov/std/health-disparities/stds-women-042011.pdf
Smolarczyk, K. et al. The impact of selected bacterial sexually transmitted diseases on pregnancy and female fertility. Int. J. Mol. Sci. 22 , 2170 (2021).
Van Gerwen, O. T., Aryanpour, Z., Selph, J. P. & Muzny, C. A. Anatomical and sexual health considerations among transfeminine individuals who have undergone vaginoplasty: a review. Int. J. STD AIDS 33 , 106–113 (2022).
Article PubMed Google Scholar
Van Gerwen, O. T. et al. Prevalence of sexually transmitted infections and human immunodeficiency virus in transgender persons: a systematic review. Transgend. Health 5 , 90–103 (2020).
Deese, J. et al. Recent advances and new challenges in cisgender women’s gynecologic and obstetric health in the context of HIV. Clin. Obstet. Gynecol. 64 , 475–490 (2021).
Hodges-Mameletzis, I. et al. Pre-exposure prophylaxis for HIV prevention in women: current status and future directions. Drugs 79 , 1263–1276 (2019).
Article CAS PubMed Google Scholar
O’Leary, A. Women and HIV in the twenty-first century: how can we reach the UN 2030 goal? AIDS Educ. Prev. 30 , 213–224 (2018).
Heumann, C. L. Biomedical approaches to HIV prevention in women. Curr. Infect. Dis. Rep. 20 , 11 (2018).
Kharsany, A. B. & Karim, Q. A. HIV infection and AIDS in Sub-Saharan Africa: current status, challenges and opportunities. Open AIDS J. 10 , 34–48 (2016).
Article CAS PubMed PubMed Central Google Scholar
Burk, R. D., Harari, A. & Chen, Z. Human papillomavirus genome variants. Virology 445 , 232–243 (2013).
Burd, E. M. Human papillomavirus and cervical cancer. Clin. Microbiol. Rev. 16 , 1–17 (2003).
Workowski, K. A. et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm. Rep. 70 , 1–187 (2021).
Human Papilloma Virus Statistics (Centers for Disease Control and Prevention, 2021); https://www.cdc.gov/std/hpv/stats.htm
Bruni, L. et al. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J. Infect. Dis. 202 , 1789–1799 (2010).
Brianti, P., De Flammineis, E. & Mercuri, S. R. Review of HPV-related diseases and cancers. New Microbiol . 40 , 80–85 (2017).
CAS PubMed Google Scholar
de Martel, C., Plummer, M., Vignat, J. & Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 141 , 664–670 (2017).
Article PubMed PubMed Central CAS Google Scholar
Serrano, B., Brotons, M., Bosch, F. X. & Bruni, L. Epidemiology and burden of HPV-related disease. Best Pract. Res. Clin. Obstet. Gynaecol. 47 , 14–26 (2018).
Walboomers, J. M. et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J. Pathol. 189 , 12–19 (1999).
Liu, G. et al. Prevalent HPV infection increases the risk of HIV acquisition in African women: advancing the argument for HPV immunization. AIDS https://doi.org/10.1097/qad.0000000000003004 (2021).
Liu, G., Sharma, M., Tan, N. & Barnabas, R. V. HIV-positive women have higher risk of human papilloma virus infection, precancerous lesions, and cervical cancer. AIDS 32 , 795–808 (2018).
Kelly, H., Weiss, H. A., Benavente, Y., de Sanjose, S. & Mayaud, P. Association of antiretroviral therapy with high-risk human papillomavirus, cervical intraepithelial neoplasia, and invasive cervical cancer in women living with HIV: a systematic review and meta-analysis. Lancet HIV 5 , e45–e58 (2018).
Smith, J. S. et al. Evidence for Chlamydia trachomatis as a human papillomavirus cofactor in the etiology of invasive cervical cancer in Brazil and the Philippines. J. Infect. Dis. 185 , 324–331 (2002).
Wang, R. et al. Human papillomavirus vaccine against cervical cancer: opportunity and challenge. Cancer Lett. 471 , 88–102 (2020).
Cervical Cancer Elimination Initiative (WHO, 2022); https://www.who.int/initiatives/cervical-cancer-elimination-initiative
Monie, A., Hung, C.-F., Roden, R. & Wu, T. C. Cervarix: a vaccine for the prevention of HPV 16, 18-associated cervical cancer. Biologics 2 , 97–105 (2008).
PubMed Google Scholar
Lei, J. et al. HP V vaccination and the risk of invasive cervical cancer. N. Eng. J. Med. 383 , 1340–1348 (2020).
Article CAS Google Scholar
Falcaro, M. et al. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study. Lancet https://doi.org/10.1016/s0140-6736(21)02178-4 (2021).
Bruni, L. et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010-2019. Prev. Med . 144 , 106399 (2021).
Clifford, G. M. et al. Toward a unified anal cancer risk scale. Int. J. Cancer 148 , 38–47 (2021). A meta-analysis of anal cancer incidence by risk group .
Chin-Hong, P. V. & Palefsky, J. M. Human papillomavirus anogenital disease in HIV-infected individuals. Dermatol. Ther. 18 , 67–76 (2005).
Frisch, M., Biggar, R. J. & Goedert, J. J. Human papillomavirus-associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. J. Natl Cancer Inst. 92 , 1500–1510 (2000).
Silverberg, M. J. et al. Risk of anal cancer in HIV-infected and HIV-uninfected individuals in North America. Clin. Infect. Dis. 54 , 1026–1034 (2012).
Palefsky, J. et al. Treatment of anal high-grade squamous intraepithelial lesions to prevent anal cancer. N. Engl. J. Med. 386 , 2273–2282 (2022).
Ellsworth, G. B. et al. Xpert HPV as a screening tool for anal histologic high-grade squamous intraepithelial lesions in women living with HIV. J. Acquir. Immune Defic. Syndr. 87 , 978–984 (2021).
Chiao, E. Y. et al. Screening strategies for the detection of anal high-grade squamous intraepithelial lesions in women living with HIV. AIDS 34 , 2249–2258 (2020).
Herpes Simplex Virus (WHO, 2022); https://www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus
Bernstein, D. I. et al. Epidemiology, clinical presentation, and antibody response to primary infection with herpes simplex virus type 1 and type 2 in young women. Clin. Infect. Dis. 56 , 344–351 (2012).
James, C. et al. Herpes simplex virus: global infection prevalence and incidence estimates, 2016. Bull. World Health Organ. 98 , 315–329 (2020).
Mahant, S. et al. Neonatal herpes simplex virus infection among medicaid-enrolled children: 2009–2015. Pediatrics https://doi.org/10.1542/peds.2018-3233 (2019).
Kimberlin, D. W. Neonatal herpes simplex infection. Clin. Microbiol. Rev. 17 , 1–13 (2004).
Kimberlin, D. Herpes simplex virus, meningitis and encephalitis in neonates. Herpes 11 , 65a–76a (2004).
Masese, L. et al. Changes in the contribution of genital tract infections to HIV acquisition among Kenyan high-risk women from 1993 to 2012. AIDS 29 , 1077–1085 (2015).
Freeman, E. E. et al. Herpes simplex virus 2 infection increases HIV acquisition in men and women: systematic review and meta-analysis of longitudinal studies. AIDS 20 , 73–83 (2006).
Looker, K. J. et al. Global and regional estimates of the contribution of herpes simplex virus type 2 infection to HIV incidence: a population attributable fraction analysis using published epidemiological data. Lancet Infect. Dis. 20 , 240–249 (2020).
Feltner, C. et al. Serologic screening for genital herpes: an updated evidence report and systematic review for the US preventive services task force. JAMA 316 , 2531–2543 (2016).
Venturino, E., Shoukat, A. & Moghadas, S. M. Dynamics of HSV-2 infection with a therapeutic vaccine. Heliyon 6 , e04368 (2020).
Kim, H. C. & Lee, H. K. Vaccines against genital herpes: where are we? Vaccines https://doi.org/10.3390/vaccines8030420 (2020).
Stanberry, L. R. et al. Glycoprotein-D–adjuvant vaccine to prevent genital herpes. N. Engl. J. Med. 347 , 1652–1661 (2002).
Belshe, R. B. et al. Efficacy results of a trial of a herpes simplex vaccine. N. Engl. J. Med. 366 , 34–43 (2012).
Bernstein, D. I. et al. Therapeutic vaccine for genital herpes simplex virus-2 infection: findings from a randomized trial. J. Infect. Dis. 215 , 856–864 (2017).
Dropulic, L. K. et al. A randomized, double-blinded, placebo-controlled, phase 1 study of a replication-defective herpes simplex virus (HSV) type 2 vaccine, HSV529, in adults with or without HSV infection. J. Infect. Dis. 220 , 990–1000 (2019).
Chandra, J. et al. Immune responses to a HSV-2 polynucleotide immunotherapy COR-1 in HSV-2 positive subjects: a randomized double blinded phase I/IIa trial. PLoS ONE 14 , e0226320 (2019).
Veselenak, R. L. et al. A Vaxfectin(®)-adjuvanted HSV-2 plasmid DNA vaccine is effective for prophylactic and therapeutic use in the guinea pig model of genital herpes. Vaccine 30 , 7046–7051 (2012).
Roth, K., Ferreira, V. H. & Kaushic, C. HSV-2 vaccine: current state and insights into development of a vaccine that targets genital mucosal protection. Microb. Pathog. 58 , 45–54 (2013).
Peeling, R. W. et al. Syphilis. Nat. Rev. Dis. Primers 3 , 17073 (2017).
Sexually Transmitted Disease Surveillance 2019 (Centers for Disease Control and Prevention, accessed 1 December 2021); https://www.cdc.gov/std/statistics/2019/default.htm
Data on Syphilis (WHO, 2021); https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/data-on-syphilis
Wu, M. X. et al. Congenital syphilis on the rise: the importance of testing and recognition. Med. J. Aust. 215 , 345–346.e1 (2021).
Hopkins, A. O. et al. Evaluation of the WHO/CDC Syphilis Serology Proficiency Programme to support the global elimination of mother-to-child transmission of syphilis: an observational cross-sectional study, 2008–2015. BMJ Open 10 , e029434 (2020).
WHO Guideline on Syphilis Screening and Treatment for Pregnant Women (WHO, 2017).
Wendel, G. D. Jr. et al. Treatment of syphilis in pregnancy and prevention of congenital syphilis. Clin. Infect. Dis. 35 , S200–S209 (2002).
Walker, G. J. Antibiotics for syphilis diagnosed during pregnancy. Cochrane Database Syst. Rev. 2001 , Cd001143 (2001).
PubMed Central Google Scholar
Alexander, J. M., Sheffield, J. S., Sanchez, P. J., Mayfield, J. & Wendel, G. D. Jr. Efficacy of treatment for syphilis in pregnancy. Obstet. Gynecol. 93 , 5–8 (1999).
Witkin, S. S. et al. Chlamydia trachomatis: the persistent pathogen. Clin. Vaccine Immunol. 24 , e00203-17 (2017).
He, W., Jin, Y., Zhu, H., Zheng, Y. & Qian, J. Effect of Chlamydia trachomatis on adverse pregnancy outcomes: a meta-analysis. Arch. Gynecol. Obstet. 302 , 553–567 (2020).
Article PubMed CAS Google Scholar
Hammerschlag, M. R. Chlamydial and gonococcal infections in infants and children. Clin. Infect. Dis. 53 , S99–S102 (2011).
Hammerschlag, M. R., Chandler, J. W., Alexander, E. R., English, M. & Koutsky, L. Longitudinal studies on chlamydial infections in the first year of life. Pediatr. Infect. Dis. 1 (1982).
Gong, Z., Luna, Y., Yu, P. & Fan, H. Lactobacilli inactivate Chlamydia trachomatis through lactic acid but not H2O2. PLoS ONE 9 , e107758 (2014).
Brotman, R. M. et al. Bacterial vaginosis assessed by gram stain and diminished colonization resistance to incident gonococcal, chlamydial, and trichomonal genital infection. J. Infect. Dis. 202 , 1907–1915 (2010).
Dukers-Muijrers, N. et al. Treatment effectiveness of azithromycin and doxycycline in uncomplicated rectal and vaginal Chlamydia trachomatis infections in women: a multicenter observational study (FemCure). Clin. Infect. Dis. 69 , 1946–1954 (2019).
Kissinger, P. J. et al. Azithromycin treatment failure for Chlamydia trachomatis among heterosexual men with nongonococcal urethritis. Sex. Transm. Dis. 43 , 599–602 (2016).
Gratrix, J. et al. Evidence for increased Chlamydia case finding after the introduction of rectal screening among women attending 2 Canadian sexually transmitted infection clinics. Clin. Infect. Dis. 60 , 398–404 (2015).
Rank, R. G. & Yeruva, L. An alternative scenario to explain rectal positivity in Chlamydia -infected individuals. Clin. Infect. Dis. 60 , 1585–1586 (2015).
Lazenby, G. B., Korte, J. E., Tillman, S., Brown, F. K. & Soper, D. E. A recommendation for timing of repeat Chlamydia trachomatis test following infection and treatment in pregnant and nonpregnant women. Int. J. STD AIDS 28 , 902–909 (2017).
Phillips, S., Quigley, B. L. & Timms, P. Seventy years of Chlamydia vaccine research – limitations of the past and directions for the future. Front. Microbiol. https://doi.org/10.3389/fmicb.2019.00070 (2019).
Whittington, W. L. et al. Determinants of persistent and recurrent Chlamydia trachomatis infection in young women: results of a multicenter cohort study. Sex. Transm. Dis. 28 , 117–123 (2001).
Owusu-Edusei, K. Jr. et al. The estimated direct medical cost of selected sexually transmitted infections in the United States, 2008. Sex. Transm. Dis. 40 , 197–201 (2013).
Unemo, M. et al. Sexually transmitted infections: challenges ahead. Lancet Infect. Dis. 17 , e235–e279 (2017).
Williams, D. M., Grubbs, B. & Schachter, J. Primary murine Chlamydia trachomatis pneumonia in B-cell-deficient mice. Infect. Immun. 55 , 2387–2390 (1987).
Ramsey, K. H., Soderberg, L. & Rank, R. G. Resolution of chlamydial genital infection in B-cell-deficient mice and immunity to reinfection. Infect. Immun. 56 , 1320–1325 (1988).
Quillin, S. J. & Seifert, H. S. Neisseria gonorrhoeae host adaptation and pathogenesis. Nat. Rev. Microbiol. 16 , 226–240 (2018).
Hook, E. W. in Sexu a lly Transmitted Diseases (eds Sparling, P. F. et al.) 451–466 (McGraw-Hill, 1999).
Brunham, R. C., Gottlieb, S. L. & Paavonen, J. Pelvic inflammatory disease. N. Engl. J. Med. 372 , 2039–2048 (2015).
Reekie, J. et al. Risk of pelvic inflammatory disease in relation to chlamydia and gonorrhea testing, repeat testing, and positivity: a population-based cohort study. Clin. Infect. Dis. 66 , 437–443 (2017).
Article Google Scholar
Farley, T. A., Cohen, D. A. & Elkins, W. Asymptomatic sexually transmitted diseases: the case for screening. Prev. Med. 36 , 502–509 (2003).
Gao, R. et al. Association of maternal sexually transmitted infections with risk of preterm birth in the United States. JAMA Netw. Open 4 , e2133413 (2021).
Vallely, L. M. et al. Adverse pregnancy and neonatal outcomes associated with Neisseria gonorrhoeae : systematic review and meta-analysis. Sex. Transm. Infect. 97 , 104–111 (2021).
Unemo, M. et al. Gonorrhoea. Nat. Rev. Dis. Primers 5 , 79 (2019).
Multi-Drug Resistant Gonorrhoea (WHO, 2021); https://www.who.int/news-room/fact-sheets/detail/multi-drug-resistant-gonorrhoea
Schwarcz, S. K. et al. National surveillance of antimicrobial resistance in Neisseria gonorrhoeae . The Gonococcal Isolate Surveillance Project. JAMA 264 , 1413–1417 (1990).
Update to CDC’s sexually transmitted diseases treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal infections. MMWR Morb. Mortal. Wkly Rep. 56 , 332–336 (2007).
Allen, V. G. et al. Neisseria gonorrhoeae treatment failure and susceptibility to cefixime in Toronto, Canada. JAMA 309 , 163–170 (2013).
Unemo, M., Golparian, D., Potočnik, M. & Jeverica, S. Treatment failure of pharyngeal gonorrhoea with internationally recommended first-line ceftriaxone verified in Slovenia, September 2011. Euro Surveill. 17 (2012).
Unemo, M., Golparian, D. & Hestner, A. Ceftriaxone treatment failure of pharyngeal gonorrhoea verified by international recommendations, Sweden, July 2010. Euro Surveill . 16 , 19792 (2011).
van Dam, A. P. et al. Verified clinical failure with cefotaxime 1g for treatment of gonorrhoea in the Netherlands: a case report. Sex. Transm. Infect. 90 , 513–514 (2014).
Lewis, D. A. et al. Phenotypic and genetic characterization of the first two cases of extended-spectrum-cephalosporin-resistant Neisseria gonorrhoeae infection in South Africa and association with cefixime treatment failure. J. Antimicrob. Chemother. 68 , 1267–1270 (2013).
Kueakulpattana, N. et al. Multidrug-resistant Neisseria gonorrhoeae infection in heterosexual men with reduced susceptibility to ceftriaxone, first report in Thailand. Sci. Rep. 11 , 21659 (2021).
Lee, K. et al. Clonal expansion and spread of the ceftriaxone-resistant Neisseria gonorrhoeae strain FC428, identified in Japan in 2015, and closely related isolates. J. Antimicrob. Chemother. 74 , 1812–1819 (2019).
Terkelsen, D. et al. Multidrug-resistant Neisseria gonorrhoeae infection with ceftriaxone resistance and intermediate resistance to azithromycin, Denmark, 2017. Euro Surveill. 22 , 17–00659 (2017).
Article PubMed Central Google Scholar
de Curraize, C. et al. Ceftriaxone-resistant Neisseria gonorrhoeae isolates (2010 to 2014) in France characterized by using whole-genome sequencing. Antimicrob. Agents Chemother. 60 , 6962–6964 (2016).
Jacobsson, S. et al. In vitro activity of the novel triazaacenaphthylene gepotidacin (GSK2140944) against MDR Neisseria gonorrhoeae . J. Antimicrobial. Chemother. 73 , 2072–2077 (2018).
Jacobsson, S. et al. In vitro activity of the novel Pleuromutilin lefamulin (BC-3781) and effect of efflux pump inactivation on multidrug-resistant and extensively drug-resistant Neisseria gonorrhoeae . Antimicrob. Agents Chemother. 61 , 11 (2017).
Jacobsson, S. et al. In vitro activity of the novel oral antimicrobial SMT-571, with a new mechanism of action, against MDR and XDR Neisseria gonorrhoeae : future treatment option for gonorrhoea? J. Antimicrobial. Chemother. 74 , 1591–1594 (2019).
Taylor, S. N. et al. Single-dose zoliflodacin (ETX0914) for treatment of urogenital gonorrhea. N. Engl. J. Med. 379 , 1835–1845 (2018).
Le, W. et al. Susceptibility trends of zoliflodacin against multidrug-resistant Neisseria gonorrhoeae clinical isolates in Nanjing, China, 2014 to 2018. Antimicrob. Agents Chemother. https://doi.org/10.1128/aac.00863-20 (2021).
Unemo, M. et al. High susceptibility to zoliflodacin and conserved target (GyrB) for zoliflodacin among 1209 consecutive clinical Neisseria gonorrhoeae isolates from 25 European countries, 2018. J. Antimicrob. Chemother. 76 , 1221–1228 (2021).
Craig, A. P. et al. The potential impact of vaccination on the prevalence of gonorrhea. Vaccine 33 , 4520–4525 (2015).
Ruiz García, Y. et al. Looking beyond meningococcal B with the 4CMenB vaccine: the Neisseria effect. NPJ Vaccines 6 , 130–130 (2021).
Petousis-Harris, H. et al. Effectiveness of a group B outer membrane vesicle meningococcal vaccine against gonorrhoea in New Zealand: a retrospective case-control study. Lancet 390 , 1603–1610 (2017).
Meites, E. et al. A review of evidence-based care of symptomatic Trichomoniasis and asymptomatic Trichomonas vaginalis Infections. Clin. Infect. Dis. 61 , S837–S848 (2015).
Van Gerwen, O. T. et al. Trichomoniasis and adverse birth outcomes: a systematic review and meta-analysis. BJOG 128 , 1907–1915 (2021).
Kissinger, P. & Adamski, A. Trichomoniasis and HIV interactions: a review. Sex. Trans. Infect. 89 , 426–433 (2013).
Yang, M. et al. Co-infection with Trichomonas vaginalis increases the risk of cervical intraepithelial neoplasia grade 2-3 among HPV16 positive female: a large population-based study. BMC Infect. Dis. 20 , 642 (2020).
Yang, S. et al. Trichomonas vaginalis infection-associated risk of cervical cancer: a meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 228 , 166–173 (2018).
Moodley, P. et al. Trichomonas vaginalis is associated with pelvic inflammatory disease in women infected with human immunodeficiency virus. Clin. Infect. Dis. 34 , 519–522 (2002).
Muzny, C. A. Why does Trichomonas vaginalis continue to be a "neglected" sexually transmitted infection? Clin. Infect. Dis. 67 , 218–220 (2018).
Hoots, B. E. et al. A trich-y question: should Trichomonas vaginalis infection be reportable? Sex Transm. Dis. 40 , 113–116 (2013).
Patel, E. U. et al. Prevalence and correlates of Trichomonas vaginalis infection among men and women in the United States. Clin. Infect. Dis. 67 , 211–217 (2018).
Joseph Davey, D. L. et al. Prevalence of curable sexually transmitted infections in pregnant women in low- and middle-income countries from 2010 to 2015: a systematic review. Sex. Trans. Dis. 43 , 450–458(2016).
Schwebke, J. R. et al. Molecular testing for Trichomonas vaginalis in women: results from a prospective U.S. clinical trial. J. Clin. Microbiol. 49 , 4106–4111 (2011).
Van Der Pol, B. et al. Detection of Trichomonas vaginalis DNA by use of self-obtained vaginal swabs with the BD ProbeTec Qx assay on the BD Viper system. J. Clin. Microbiol. 52 , 885–889 (2014).
Van Der Pol, B. et al. Clinical performance of the BD CTGCTV2 assay for the BD MAX System for detection of Chlamydia trachomatis , Neisseria gonorrhoeae , and Trichomonas vaginalis infections. Sex. Trans. Dis. 48 , 134–140 (2021).
Van Der Pol, B. A profile of the cobas® TV/ MG test for the detection of Trichomonas vaginalis and Mycoplasma genitalium . Exp. Rev. Molec. Diag. 20 , 381–386 (2020).
Guidelines for the Management of Symptomatic Sexually Transmitted Infections (World Health Organization, 2021).
Howe, K. & Kissinger, P. J. Single-dose compared with multidose metronidazole for the treatment of trichomoniasis in women: a meta-analysis. Sex. Trans. Dis. 44 , 29–34 (2017).
Kissinger, P. et al. Single-dose versus 7-day-dose metronidazole for the treatment of trichomoniasis in women: an open-label, randomised controlled trial. Lancet Infect. Dis. 18 , 1251–1259 (2018).
Mann, J. R. et al. Treatment of trichomoniasis in pregnancy and preterm birth: an observational study. J. Womens Health 18 , 493–497 (2009).
Muzny, C. A., Richter, S. & Kissinger, P. Is It time to stop using single-dose oral metronidazole for the treatment of trichomoniasis in women? Sex. Trans. Dis. 46 , e57–e59 (2019).
Van Gerwen, O. T. et al. Epidemiology, natural history, diagnosis, and treatment of Trichomonas vaginalis in men. Clin. Infect. Dis. 73 , 1119–1124 (2021).
Muzny, C. A. et al. Efficacy and safety of single oral dosing of secnidazole for trichomoniasis in women: results of a phase 3, randomized, double-blind, placebo-controlled, delayed-treatment study. Clin. Infect. Dis. 73 , e1282–e1289 (2021).
Herbst, J. H. et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 12 , 1–17 (2008).
HIV Infection Risk, Prevention, and Testing Behaviors Among Men Who Have Sex With Men—National HIV Behavioral Surveillance, 23 U.S. Cities, 2017 (CDC, 2019).
Sullivan, P. S. et al. Trends in the use of oral emtricitabine/tenofovir disoproxil fumarate for pre-exposure prophylaxis against HIV infection, United States, 2012-2017. Ann. Epidemiol. 28 , 833–840 (2018).
Pitasi, M. A. et al. HIV testing among transgender women and men - 27 states and guam, 2014-2015. MMWR Morb. Mortal. Wkly Rep. 66 , 883–887 (2017).
Phillips, G. II et al. Utilization and avoidance of sexual health services and providers by YMSM and transgender youth assigned male at birth in Chicago. AIDS Care 31 , 1282–1289 (2019).
Fisher, C. B. et al. Perceived barriers to HIV prevention services for transgender youth. LGBT Health 5 , 350–358 (2018).
Van Gerwen, O. T. et al. ‘It's behaviors, not identity’: attitudes and beliefs related to HIV risk and pre-exposure prophylaxis among transgender women in the Southeastern United States. PLoS ONE 17 , e0262205 (2022).
van der Ham, M. et al. Gender inequality and the double burden of disease in low-income and middle-income countries: an ecological study. BMJ Open 11 , e047388 (2021).
Petca, A. et al. Non-sexual HPV transmission and role of vaccination for a better future (Review). Exp. Ther. Med. 20 , 186–186 (2020).
Sun-Kuie, T., Tew-Hongw, H. & Soo-Kim, L.-T. Is genital human papillomavirus infection always sexually transmitted? Aust. N. Z. J. Obstet. Gynaecol. 30 , 240–242 (1990).
Hong, Y., Li, S.-Q., Hu, Y.-L. & Wang, Z.-Q. Survey of human papillomavirus types and their vertical transmission in pregnant women. BMC. Infect. Dis. 13 , 109 (2013).
Graham, S. V. The human papillomavirus replication cycle, and its links to cancer progression: a comprehensive review. Clin. Sci. 131 , 2201–2221 (2017).
Schiffer, J. T. et al. Herpes simplex virus-2 transmission probability estimates based on quantity of viral shedding. J. R. Soc. Interface 11 , 20140160 (2014).
Kriebs, J. M. Understanding herpes simplex virus: transmission, diagnosis, and considerations in pregnancy management. J. Midwifery Womens Health 53 , 202–208 (2008).
Ribes, J. A. et al. Six-year study of the incidence of herpes in genital and nongenital cultures in a central Kentucky medical center patient population. J. Clin. Microbiol. 39 , 3321–3325 (2001).
Cliffe, A. R. & Wilson, A. C. Restarting lytic gene transcription at the onset of herpes simplex virus reactivation. J. Virol. 91 , 2 (2017).
Stoltey, J. E. & Cohen, S. E. Syphilis transmission: a review of the current evidence. Sex. Health 12 , 103–109 (2015).
Ko, W. J. et al. Successful prevention of syphilis transmission from a multiple organ donor with serological evidence of syphilis. Transplant. Proc. 30 , 3667–3668 (1998).
Raguse, J. D. et al. Occupational syphilis following scalpel injury. Ann. Intern. Med. 156 , 475–476 (2012).
Chlamydia CDC Fact Sheet (CDC, accessed 7 Feb 2022); https://www.cdc.gov/std/chlamydia/stdfact-chlamydia.htm
Elwell, C., Mirrashidi, K. & Engel, J. Chlamydia cell biology and pathogenesis. Nat. Rev. Microbiol. 14 , 385–400 (2016).
Gonorrhea CDC Fact Sheet (CDC, accessed 7 February 2022); https://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea-detailed.htm
Burch, T. A., Rees, C. W. & Reardon, L. V. Epidemiological studies on human trichomoniasis. Am. J. Trop. Med. Hyg. 8 , 312–318 (1959).
Crucitti, T. et al. Non-sexual transmission of Trichomonas vaginalis in adolescent girls attending school in Ndola, Zambia. PLoS ONE 6 , e16310 (2011).
Peterson, K. & Drame, D. Iatrogenic transmission of Trichomonas vaginalis by a traditional healer. Sex. Trans. Infect. 86 , 353–354 (2010).
Edwards, T. et al. Trichomonas vaginalis : clinical relevance, pathogenicity and diagnosis. Crit. Rev. Microbiol. 42 , 406–417 (2016).
Download references
Acknowledgements
We thank N. J. Van Wagoner for advice on the HSV vaccinology section of this paper and M. Kawai from the UAB Center of Clinical and Translational Sciences for assistance in creating figures. O.T.V.G. acknowledges the Doris Duke Charitable Foundation COVID-19 Fund to Retain Clinician Scientists (Grant No. 2021255) and the UAB COVID-19 CARES Retention Program (CARES at UAB).
Author information
Authors and affiliations.
Division of Infectious Diseases, University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL, USA
Olivia T. Van Gerwen, Christina A. Muzny & Jeanne M. Marrazzo
You can also search for this author in PubMed Google Scholar
Contributions
O.T.V.G. led efforts in the literature review and writing of this manuscript. C.A.M. and J.M.M. contributed to the final version of the manuscript. All authors conceived the main conceptual ideas for the manuscript together.
Corresponding author
Correspondence to Olivia T. Van Gerwen .
Ethics declarations
Competing interests.
O.T.V.G. has received research grant support from Gilead Sciences, Inc. and Abbott Molecular, and serves on the scientific advisory board for Scynexis. C.A.M. has received research grant support from Lupin Pharmaceuticals, Gilead Sciences, Inc. and Abbott Molecular, is a consultant for Cepheid, Scynexis, Lupin Pharmaceuticals, PhagoMed and BioFire Diagnostics, and has received honoraria from Elsevier, Abbott Molecular, Cepheid, Becton Dickinson, Roche Diagnostics and Lupin. J.M. serves on scientific advisory committees for Merck and Gilead, has received research grant support from Becton Dickinson and GlaxoSmithKline, and serves as a scientific advisor for OSEL.
Peer review
Peer review information.
Nature Microbiology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Van Gerwen, O.T., Muzny, C.A. & Marrazzo, J.M. Sexually transmitted infections and female reproductive health. Nat Microbiol 7 , 1116–1126 (2022). https://doi.org/10.1038/s41564-022-01177-x
Download citation
Received : 21 October 2021
Accepted : 20 June 2022
Published : 02 August 2022
Issue Date : August 2022
DOI : https://doi.org/10.1038/s41564-022-01177-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Microbiology newsletter — what matters in microbiology research, free to your inbox weekly.

COMMENTS
In the following, the diagnosis, symptoms, treatment, and prevention of a selection of sexually transmitted diseases are presented. In addition, a case report is included in this review to provide a more clinical context.
In this paper, we examine the epidemiology, screening, management, and prevention of STIs in adolescents. STI rates in adolescents have been rising since 2014, with young women and men who have sex with men at particularly high risk. Barriers to STI screening for adolescents include confidentiality concerns and lack of access to health services.
We conducted this systematic review in order to determine awareness and knowledge of school-going adolescents in Europe of sexually transmitted diseases, not only concerning HIV/AIDS, but also other STDs such as chlamydia, gonorrhoea, syphilis and human papillomavirus (HPV).
Sexually transmitted infections (STIs) are common, diverse, and dangerous to health—extending from bacterial diseases that may be readily treatable once diagnosed to viral infections such as HIV that can be life-threatening and, as yet, have no cure.
Research on STI prevention behaviour has extended from a focus on abstinence, partner reduction and condom use, to also include novel preventive behaviours, notably...
Sexually transmitted infections (STIs) are the infections which are mainly transmitted through sexual intercourse. Young individuals in the age group of 16 to 24 years are considered to be at more risk for STIs compared to older adults.
Adolescents and young adults are at high risk for sexually transmitted infections (STIs). Providers have the responsibility to accurately manage these infections to prevent medical complications and the spread of STIs. This article will review the epidemiology, screening recommendations, diagnostic tests, and treatment guidelines for STIs most ...
Sexually transmitted diseases (STDs) affect mainly young individuals and cause health, social, and economic problems worldwide. The present study used a web questionnaire to assess the awareness, knowledge, sexual behaviors, and common practices regarding STDs in young Greek adults.
This peer-reviewed journal provides a forum for investigating and treating sexually transmissible infections, HIV and AIDS. Contributors from around the world promote activities aimed at research, prevention and control of these infections. The journal contains original research, in-depth reviews, short papers, case reports, audits and CPD papers.
Sexually transmitted infections (STIs) cause reproductive morbidity worldwide. In 2019, the World Health Organization (WHO) estimated that there were 376 million new episodes of chlamydia,...