

Gender-affirming care has a long history in the US – and not just for transgender people
Associate Professor of History, Roanoke College
Disclosure statement
G. Samantha Rosenthal is co-founder of the Southwest Virginia LGBTQ+ History Project
View all partners
In 1976, a woman from Roanoke, Virginia, named Rhoda received a prescription for two drugs: estrogen and progestin. Twelve months later, a local reporter noted Rhoda’s surprisingly soft skin and visible breasts. He wrote that the drugs had made her “so completely female.”
Indeed, that was the point. The University of Virginia Medical Center in nearby Charlottesville had a clinic specifically for women like Rhoda. In fact, doctors there had been prescribing hormones and performing surgeries – what today we would call gender-affirming care – for years.
The founder of that clinic, Dr. Milton Edgerton , had cut his teeth caring for transgender people at Johns Hopkins University in the 1960s. There, he was part of a team that established the nation’s first university-based Gender Identity Clinic in 1966.
When politicians today refer to gender-affirming care as new, “ untested ” or “ experimental ,” they ignore the long history of transgender medicine in the United States.
It’s been nearly 60 years since the first transgender medical clinic opened in the U.S. , and 47 years since Rhoda started her hormone therapy. Understanding the history of these treatments in the U.S. can be a helpful guide for citizens and legislators in a year when a record number of bills in statehouses target the rights of transgender people.

Treating gender in every population
As a trans woman and a scholar of transgender history , I have spent much of the past decade studying these issues . I also take several pills each morning to maintain the proper hormonal balance in my body: spironolactone to suppress testosterone and estradiol to increase estrogen.
When I began HRT, or hormone replacement therapy, like many Americans I wasn’t aware that this treatment had been around for generations. What I was even more surprised to learn was that HRT is often prescribed to cisgender women – women who were assigned female at birth and raised their whole lives as women. In fact, many providers in my region already had a long record of prescribing hormones to cis women , primarily women experiencing menopause.
I also learned that gender-affirming hormone therapies have been prescribed to cisgender youths for generations – despite what contemporary politicians may think. Disability scholar Eli Clare has written of the history and continued practice of prescribing hormones to boys who are too short and girls who are too tall for what is considered a “normal” range for their gender. Because of binary gender norms that celebrate height in men and smallness in women, doctors, parents and ethicists have approved the use of hormonal therapies to make children conform to these gender stereotypes since at least the 1940s .
Clare describes a severely disabled young woman whose parents – with the approval of doctors and ethicists from their local children’s hospital – administered puberty blockers so that she would never grow into an adult. They deemed her mentally incapable of becoming a “real” woman.
The history of these treatments demonstrates that hormone therapies and puberty blockers have been used on cisgender children in this country – for better or for worse – with the goal of regulating the passage from girlhood to womanhood and from boyhood to manhood. Gender stereotypes concerning the presence or absence of secondary sex characteristics – too tall, too short, too much body hair – have all led parents and doctors to perform gender-affirming care on cisgender children.
For over half a century, legal and medical authorities in the U.S. have also approved and administered surgeries and hormone therapies to force the bodies of intersex children to conform to binary gender stereotypes. I myself had genital surgery in infancy to bring my anatomy into alignment with expectations for what a “male” body should look like. In most cases, intersex surgeries are unnecessary for the health or well-being of a child.
Historians such as Jules Gill-Peterson have shown that early advances in transgender medicine in this country are deeply interwoven with the nonconsensual treatment of intersex children . Doctors at Johns Hopkins and the University of Virginia practiced reconstructing the genitalia of intersex people before applying those same treatments on transgender patients.
Given these intertwined histories, I contend that the current political focus on prohibiting gender-affirming care for transgender people is evidence that opposition to these treatments is not about the safety of any specific medications or procedures, but rather their use specifically by transgender people.
How transgender people access care
Many transgender people in the U.S. have deeply complicated feelings about gender-affirming care. This complexity is a result of over half a century of transgender medicine and patient experiences in the U.S.
In Rhoda’s time, medical gatekeeping meant that she had to live “full time” as a woman and prove her suitability for gender-affirming care to a team of primarily white, cis male doctors before they would give her treatment. She had to mimic language about being “ born in the wrong body ” – language invented by cis doctors studying trans people, not by trans people themselves. She had to affirm she would be heterosexual and seek marriage and monogamy with a man. She could not be a lesbian or bisexual or promiscuous.
Many trans people still need to jump through similar hoops today to receive gender-affirming care. For example, a diagnosis of “ gender dysphoria ,” a designated mental disorder, is sometimes required before treatment. Many trans people argue that these preconditions for access to care should be removed because being trans is an identity and a lived experience, not a disorder.
Feminist activists in the 1970s also critiqued the role of medical authority in gender-affirming care. Writer Janice Raymond decried “ the transsexual empire ,” her term for the physicians, psychologists and other professionals who practice transgender medicine. Raymond argued that cis male doctors were making an army of trans women to satisfy the male gaze: promoting iterations of womanhood that reinforced sexist gender stereotypes, ultimately ushering in the displacement and eradication of the world’s “biological” women. The origins of today’s gender-critical, or trans-exclusionary radical feminist , movement are visible in Raymond’s words. But as trans scholar Sandy Stone wrote in her famous reply to Raymond , it’s not that trans women are unwilling dupes of cis male medical authority, but rather that we have to strategically perform our womanhood in certain ways to access the care and treatments we need.
The future of gender-affirming care
In many states, especially in the South, where I live, governors and legislatures are introducing bills to ban gender-affirming care – even for adults – in ignorance of history. The consequences of hurried legislation extend beyond trans people, because access to hormones and surgeries is a basic medical service many people may need to feel better in their body.
Prohibitions on hormone therapy and gender-related surgeries for minors could mean ending the same treatment options for cisgender children . The legal implications for intersex children may directly clash with proposed legislation in several states that aims to codify “male” and “female” as discrete biological sexes with certain anatomical features.
Prohibitions on hormone replacement therapy for adults could affect access to the same treatments for menopausal women or limit access to hormonal birth control. Prohibitions of gender-affirming surgeries could affect anyone’s ability to access a hysterectomy or a mastectomy . So-called cosmetic surgeries such as breast implants or reductions, and even facial feminization procedures such as lip fillers or Botox, could also come under question.
These are all different types of gender-affirming procedures. Are most Americans willing to live with this level of government intrusion into their bodily autonomy?
Almost every major medical organization in the U.S. has come out against new government restrictions on gender-affirming care because, as doctors and professionals, they know that these treatments are time-tested and safe . These treatments have histories reaching back over 50 years.
Trans and intersex people are important voices in this debate, because our bodies are the ones politicians opposing gender-affirming care most frequently treat as objects of ridicule and disgust . Legislators are developing policies about us despite the fact that most Americans say they do not even know a trans person .
But trans and intersex people know what it is like to have to fight to access the care and treatment we need. And we know the joy of finally feeling comfortable in our own skin and being able to affirm our gender on our own terms.
- Gender stereotypes
- Transgender
- Health care
- Gender dysphoria
- History of medicine
- Hormone therapy
- Johns Hopkins University
- Transgender rights
- Transgender health
- Trans rights
- LGBTQ history
- gatekeepers
- US health care
- Gender-affirming healthcare
- Trans healthcare
- Gender disparities
- Anti-trans legislation
- University of Virginia
- trans history

Dean (Head of School), Indigenous Knowledges

Business Improvement Lead

Senior Research Fellow - Curtin Institute for Energy Transition (CIET)

Laboratory Head - RNA Biology

Head of School, School of Arts & Social Sciences, Monash University Malaysia

- Games & Quizzes
- History & Society
- Science & Tech
- Biographies
- Animals & Nature
- Geography & Travel
- Arts & Culture
- On This Day
- One Good Fact
- New Articles
- Lifestyles & Social Issues
- Philosophy & Religion
- Politics, Law & Government
- World History
- Health & Medicine
- Browse Biographies
- Birds, Reptiles & Other Vertebrates
- Bugs, Mollusks & Other Invertebrates
- Environment
- Fossils & Geologic Time
- Entertainment & Pop Culture
- Sports & Recreation
- Visual Arts
- Demystified
- Image Galleries
- Infographics
- Top Questions
- Britannica Kids
- Saving Earth
- Space Next 50
- Student Center
- Introduction
Gender-affirmation care
Development, advances in gender-affirming care.

- When did science begin?
- Where was science invented?

gender-affirming surgery
Our editors will review what you’ve submitted and determine whether to revise the article.
- Table Of Contents
Recent News
gender-affirming surgery , medical procedure in which the physical sex characteristics of an individual are modified. Gender-affirming surgery typically is undertaken when an individual chooses to align their physical appearance with their gender identity , enabling the individual to achieve a greater sense of self and helping to reduce psychological distress that may be associated with gender dysphoria .
An individual’s physical sex may not match their gender identity when the person is intersex , having been born outside the binary of male and female and thus having ambiguous genitalia, or when the person identifies as transgender . Parents of an intersex child may elect to have surgical procedures carried out in order to have the child’s anatomy conform to binary notions of gender . A person’s ascribed legal sex may not match their gender identity as they mature. However, this situation raises serious concerns regarding the appropriateness of performing unnecessary medical procedures on the bodies of minors. Intersexuality is a normal biological variation and is not considered a medical condition. Therefore, medical interventions such as surgery and hormone therapy are typically unnecessary for intersex children.

Transgender individuals may seek gender-affirming surgery to align their physical body with their perception of their gender identity. Gender identity refers to an individual’s perception of their own gender, which may or may not correspond to their designated gender at birth. Gender identity encompasses the identification as male, female, both, neither, or somewhere else on the spectrum of gender. It is distinct from biological sex, which is determined by the sex chromosomes and anatomy of an individual. While the gender identity of most individuals corresponds to their ascribed biological sex, the gender identity of some individuals differs from their ascribed sex at birth, which can result in gender dysphoria and thereby lead the individual to seek gender-affirming surgery.
Individuals assigned male at birth may undergo one or more procedures to feminize their anatomy, including facial feminization surgery, penectomy (removal of the penis ), orchidectomy (removal of the testicles ), vaginoplasty (construction of a vagina ), and a tracheal shave (reduction of the Adam’s apple). Individuals who are assigned female at birth and who desire surgical intervention to masculinize their anatomy may seek breast reduction surgery, hysterectomy (removal of the uterus ), oophorectomy (removal of the ovaries ), and phalloplasty (construction of a penis).
Gender-affirming surgeries were performed during the 1920s and ’30s, primarily in Europe. These procedures were experimental and not extensively accepted by the medical community . At the time, it was widely believed that gender identity was immutable and that surgery could not alter it. However, Magnus Hirschfeld , a German sexologist and vocal advocate for sexual and gender diversity , assisted with the care of several transgender individuals.
Dora Richter was the first transgender individual to undergo complete male-to-female genital surgery under Hirschfeld’s supervision. Richter was one of several transgender individuals under Hirschfeld’s care at the Berlin Institute for Sexual Research. In 1922 Richter underwent an orchidectomy and, in 1931, a penectomy and vaginoplasty.
In 1930 and 1931 Lili Elbe also underwent several gender-affirming surgeries. These procedures included an orchidectomy, an ovarian transplant , and a penectomy. Elbe underwent a fourth surgery in June 1931, which consisted of an experimental uterine transplant and vaginoplasty. Elbe’s body rejected the transplanted uterus, and she died of postoperative complications in 1931.
During the 1950s and ’60s, significant advancements were made in the field of gender-affirming surgery, including the establishment of several major medical centres and the refinement of surgical techniques. Christian Hamburger, a Danish endocrinologist, performed a gender-affirming surgery in 1952 on Christine Jorgensen , a transgender individual, who underwent hormone replacement therapy and surgery to remove her testicles and create a vagina. Jorgensen became a public figure advocating for transgender rights and promoting awareness about gender-affirming surgery after their case received significant media attention.
Other medical centres in Europe and the United States began conducting gender-affirming surgeries around the same time, including the Johns Hopkins Gender Identity Clinic, founded in 1966. The founder of the clinic, psychiatrist John Money, believed that gender was a social construct and that gender-affirming surgery could be an effective treatment for individuals with gender dysphoria. Money’s theories had a significant impact on the field of gender-affirming surgery and helped to change the attitudes of the medical community regarding the procedure.
During the 1960s, new surgical techniques were developed, including advances in vaginoplasty and phalloplasty. In the 1950s Belgian surgeon Georges Burou devised a technique involving the use of skin grafts from the patient’s thigh to create a vaginal canal lining. For penises, he attached the phallus to a blood supply using tissue . This technique improved tissue perfusion and decreased the risk of complications such as tissue necrosis . These procedures marked a turning point in the development of gender-affirming care because they demonstrated the potential for successful genital reconstruction in transgender patients.
- Health Tech
- Health Insurance
- Medical Devices
- Gene Therapy
- Neuroscience
- H5N1 Bird Flu
Health Disparities
- Infectious Disease
- Mental Health
- Cardiovascular Disease
- Chronic Disease
- Alzheimer's
- Coercive Care
- The Obesity Revolution
- The War on Recovery
- Adam Feuerstein
- Matthew Herper
- Jennifer Adaeze Okwerekwu
- Ed Silverman
- CRISPR Tracker
- Breakthrough Device Tracker
- Generative AI Tracker
- Obesity Drug Tracker
- 2024 STAT Summit
- Wunderkinds Nomination
- STAT Madness
- STAT Brand Studio
Don't miss out
Subscribe to STAT+ today, for the best life sciences journalism in the industry
‘History is repeating itself’: The story of the nation’s first clinic for gender-affirming surgery
By Theresa Gaffney Oct. 3, 2022

N early 60 years ago, Johns Hopkins Hospital opened a first-of-its-kind clinic to provide gender-affirming surgery. The Gender Identity Clinic blazed a new trail, with more than a dozen new clinics opening across the country in the decade that followed.
But in 1979, the clinic shut its doors. And while the institution claimed for years that the decision was made based on the evidence — which, they argued, showed such surgeries didn’t benefit patients — new research by a Johns Hopkins medical school student reveals a different story. The student, Walker Magrath, dug through years of archived correspondence and notes at both Johns Hopkins and Harvard University, and found that internal politics and pushback from hospital leadership ultimately caused the clinic to close.
advertisement
“It’s important for Johns Hopkins as an institution to reckon with its harmful history with LGBTQ patients,” said Magrath,who authored a new paper documenting the history of the center published Monday in Annals of Internal Medicine. For decades after the center closed, Johns Hopkins didn’t provide gender-affirming surgeries for trans patients — but it recently opened a center for transgender care.
In light of recent threats made to hospitals that provide gender-affirming care to trans patients and the closures of gender-affirming and reproductive health clinics across the country over the last year, Magrath felt that it was critical to make clear that this isn’t the first time gender-affirming clinics have faced backlash and closures.
Related: Harassment prompts children’s hospitals to strip websites, threatening access to gender-affirming care
“We need to be critical of mainstream medical institutions that wield a lot of power because their influence causes a [ripple] effect,” Magrath said. When the clinic at Johns Hopkins closed, others around the country began to shutter too. While there were 20 similar clinics in 1979, only two or three were still operating by the mid-1990s, according to Magrath.
“History is repeating itself,” said Alex Keuroghlian, of Massachusetts General Hospital and the Fenway Institute, who co-authored an editorial on Magrath’s paper with Asa Radix, of New York University and the Callen-Lorde Community Health Center. “We’re seeing the exact same tactics being used — defamation, sensationalist transphobia, intimidation of providers who want to offer this care,” Keuroghlian said.
Magrath found documentation that showed the clinic was met with bias and stigma from hospital leaders such as Paul McHugh, who became the hospital’s chief of psychiatry in 1975. McHugh arrived at Hopkins intending to stop gender-affirming surgery, according to Magrath. But Magrath also noted that McHugh, known for his pathologizing and homophobic statements on LGBTQ+ health, is just one of many leaders at the institution who fought against the clinic’s mission.
John Hoopes, the hospital’s chief of plastic surgery while the clinic operated, originally supported gender-affirming surgery and served as the GIC’s inaugural director, saying “there exists reasonably good evidence” that surgery could lead to positive results. But his opinions adapted as plastic surgery became a higher-profile specialty, leaving him worried that the slower progress around gender-affirming surgery would become a liability to his department. He later described transgender patients as “hysterical,” “freakish,” and “artificial.” Years before the closure, Hoopes ordered that the GIC be separated from the surgery department, depriving the clinic of valuable resources and leaving its physicians to operate under obstetrics department, which was mired in its own set of controversies that made it difficult to support the GIC’s work.
Related: Gender-affirming care should be embraced, not met with vitriol and bomb threats
When the clinic closed, the mainstream narrative was that research performed at Johns Hopkins had concluded that gender-affirmative surgery had no advantage for patients’ “social rehabilitation.” But the methods of the study were swiftly questioned by experts, who noted the conclusions may be unreasonable based on the statistics used. Magrath notes that the sample of patients included in that study were those treated in the earliest days of the clinic’s work, when surgical techniques were new and evolving. The clinic’s co-founder, psychologist John Money, admitted that some of those early cases were not successful, but was never given funding to do his own follow-up research.
In their accompanying editorial, Keuroghlian and Radix also point out that the metrics that researchers used to define rehabilitation focused more on fitting trans people into a limited, traditional model of success, rather than measuring their actual well-being.
“Studies are often used to fuel political agendas,” Magrath said. “Science often can be manipulated, and you can see that in our modern society.” It happened decades ago when the GIC was closed, he noted, and it’s happening now as pressure builds on facilities that provide gender-affirming care.
Historically, marginalized communities like trans and nonbinary people haven’t been included in providing care for their own communities, said Keuroghlian, who helps to train physicians across the country to provide gender-affirming care as part of their work at the Fenway Institute. This was part of the problem with the GIC, they said.
Related: ‘Critically important work’: Adm. Rachel Levine on efforts to combat gender-based discrimination in health care
“There was a real paternalism to how decisions were made by leadership, which is how a lot of medicine is characterized,” Keuroghlian said.
The health system still has a service in the Department of Plastic Surgery at Johns Hopkins named after Hoopes, and McHugh is still listed as a University Distinguished Service Professor on the institution’s website.
Liz Vandendriessche, a spokesperson for Johns Hopkins, said that while the institution supports its community members sharing their perspectives, the paper represents only Magrath’s personal opinion. She added that the hospital’s Center for Transgender Health provides care in line with the standards from the World Professional Association for Transgender Health.
To Keuroghlian and Magrath, there’s a need for more accountability from leading institutions like Johns Hopkins, which help to set the standard for health care.
“If our major, well-resourced academic teaching hospitals don’t set the example of providing care for the most marginalized in our communities, and don’t lead with health equity and social justice as organizing principles, then nobody else is going to do it,” Keuroghlian said.
This story has been updated to include a statement from a Johns Hopkins Medicine spokesperson.
About the Author Reprints
Theresa gaffney.
Morning Rounds Writer and Podcast Producer
Theresa Gaffney is the lead Morning Rounds writer and a podcast producer at STAT.
STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect
To submit a correction request, please visit our Contact Us page .

Recommended

Recommended Stories

Telling new stories can help people see the value of vaccines

Walgreens executive says it is ‘doubling down’ on recruiting customers into clinical trials

STAT Plus: The inside story of how Lykos’ MDMA research went awry

STAT Plus: Google’s Verily to offer GLP-1 drugs through Lightpath, its retooled chronic care app

STAT Plus: At BIO, signs Congress’ tough stance on China is chilling biotech relationships
- Nation & World
Key dates for transgender rights in the US
Share story.
Some important events in the history of transgender rights in the United States:
1952: Christine Jorgensen completes sex-reassignment surgery in Denmark; she was the first American known for undergoing such a transition.
1969: Transgender people are in the forefront of the Stonewall Inn riots in New York City, which helped spark the U.S. gay-rights movement.
1977: The New York Supreme Court rules in favor of transgender physician/athlete Renee Richards in her bid to play pro tennis as a woman.
Most Read Nation & World Stories
- Oprah Winfrey hospitalized, Gayle King (over)shares
- Concerns about Princess Kate ramping up again
- Jimmy Carter not awake every day, 15 months into hospice
- Large whale group spotted off New England includes orca eating a tuna, dozens of endangered species VIEW
- Nevada man accused of interfering with crew on flight from Seattle to Anchorage is arrested
1993: Transgender man Brandon Teena is raped and murdered in Nebraska; his story is later made into the film “Boys Don’t Cry.” Minnesota becomes the first state to ban anti-transgender discrimination in employment, housing and public accommodations.
1999: Observance of the first international Day or Remembrance, an annual event honoring victims of anti-transgender violence.
2005: A pioneering California law bars health insurance companies from discriminating against transgender people.
2008: Isis King becomes first transgender model featured in the reality TV show “America’s Next Top Model.”
2009: President Obama signs a federal hate-crimes law that covers crimes motivated by anti-transgender bias.
2010: In response to a lawsuit, players of the Ladies Professional Golf Association vote to allow transgender players to compete on tour.
2012: Miss Universe opens its competition to transgender contestants. The Equal Employment Opportunity Commission rules that discrimination based on transgender status is sex discrimination in violation of the Civil Rights Act.
2013: The American Psychiatric Association updates its diagnostic manual to stipulate that being transgender is no longer considered a mental disorder.
2014: Actress Laverne Cox becomes first transgender person featured on the cover of Time magazine. Maine’s highest court rules that a transgender fifth-grader should have been allowed to use the girls’ bathroom at her school.
2015: Caitlyn Jenner completes her gender transition, appears on the cover of Vanity Fair. Voters in Houston defeat an ordinance that would have extended nondiscrimination protections to transgender people.
2016: The U.S. military lifts its ban on transgender service members. The U.S. Supreme Court agrees to hear a Virginia case involving Gavin Grimm, a transgender boy seeking the right to use the boys’ restroom at his high school. The Obama administration advises public schools that transgender students should be allowed to use restrooms and locker rooms of their choice.
2017: The Trump administration revokes the Obama-era directive, saying policies for transgender students’ bathroom access should be set at the state and local level.
- Search Menu
Sign in through your institution
- Advance articles
- Author Guidelines
- Open Access
- Submission Site
- Book Reviews
- Why Submit?
- About American Journal of Legal History
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

- < Previous
The Lawfulness of Gender Reassignment Surgery
- Article contents
- Figures & tables
- Supplementary Data
Penney Lewis, The Lawfulness of Gender Reassignment Surgery, American Journal of Legal History , Volume 58, Issue 1, March 2018, Pages 56–85, https://doi.org/10.1093/ajlh/njx032
- Permissions Icon Permissions
In the common law world, both the medical and legal professions initially considered gender reassignment surgery to be unlawful when first practised and discussed in the first half of the twentieth century. While most medical procedures are covered by the medical exception to the law governing serious offences against the person, many doctors and the lawyers they consulted doubted that this exception applied to gender reassignment surgery. In this article I trace the differing and changing interpretations of the medical exception as applied to gender reassignment surgery, and the shift towards legal acceptance in the two common law jurisdictions that led the way in both performing gender reassignment surgery and debating its legality, the United States and the United Kingdom. Although this shift occurred without formal legal intervention either through legislation or judicial decision (for example on a test case), inferences of legality drawn from related civil-law decisions bolstered the legal acceptance of gender reassignment surgery.
By increasing the suffering of patients and potential patients, the criminal law played both an important and primarily malign role prior to the eventual public, professional and legal acceptance of GRS. A real threat of criminal prosecution inhibited doctors from proceeding, distorted diagnoses and affected the kinds of procedures performed. After-care was expanded and manipulated to avoid the risk of prosecution or the appearance of unlawful surgery. By contrast, civil and administrative law played a more positive, albeit indirect, role in interpreting the medical exception and its application to gender reassignment surgery.
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Short-term Access
To purchase short-term access, please sign in to your personal account above.
Don't already have a personal account? Register
| Month: | Total Views: |
|---|---|
| December 2017 | 19 |
| January 2018 | 18 |
| February 2018 | 19 |
| March 2018 | 20 |
| April 2018 | 17 |
| May 2018 | 13 |
| June 2018 | 6 |
| July 2018 | 2 |
| August 2018 | 17 |
| September 2018 | 9 |
| October 2018 | 9 |
| November 2018 | 14 |
| December 2018 | 25 |
| January 2019 | 6 |
| February 2019 | 10 |
| March 2019 | 23 |
| April 2019 | 9 |
| May 2019 | 5 |
| June 2019 | 4 |
| July 2019 | 6 |
| August 2019 | 1 |
| September 2019 | 8 |
| October 2019 | 5 |
| November 2019 | 16 |
| December 2019 | 6 |
| January 2020 | 6 |
| February 2020 | 15 |
| March 2020 | 10 |
| April 2020 | 11 |
| May 2020 | 5 |
| June 2020 | 11 |
| July 2020 | 8 |
| August 2020 | 2 |
| September 2020 | 3 |
| October 2020 | 4 |
| November 2020 | 3 |
| December 2020 | 4 |
| January 2021 | 10 |
| February 2021 | 5 |
| March 2021 | 8 |
| April 2021 | 4 |
| May 2021 | 6 |
| June 2021 | 2 |
| July 2021 | 1 |
| August 2021 | 1 |
| September 2021 | 6 |
| October 2021 | 10 |
| November 2021 | 29 |
| December 2021 | 29 |
| January 2022 | 8 |
| February 2022 | 9 |
| March 2022 | 5 |
| April 2022 | 7 |
| May 2022 | 10 |
| June 2022 | 1 |
| July 2022 | 1 |
| August 2022 | 3 |
| September 2022 | 1 |
| October 2022 | 7 |
| November 2022 | 5 |
| December 2022 | 7 |
| January 2023 | 3 |
| February 2023 | 2 |
| March 2023 | 4 |
| April 2023 | 5 |
| May 2023 | 11 |
| June 2023 | 3 |
| July 2023 | 2 |
| August 2023 | 2 |
| September 2023 | 3 |
| November 2023 | 3 |
| December 2023 | 1 |
| January 2024 | 1 |
| February 2024 | 7 |
| March 2024 | 2 |
| April 2024 | 17 |
| May 2024 | 4 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 2161-797X
- Print ISSN 0002-9319
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Origins of Gender Affirmation Surgery: The History of the First Gender Identity Clinic in the United States at Johns Hopkins
Affiliation.
- 1 Office of Diversity and Inclusion, Johns Hopkins Medical Institutions, Baltimore, MD.
- PMID: 30557186
- DOI: 10.1097/SAP.0000000000001684
Background: Gender-affirming care, including surgery, has gained more attention recently as third-party payers increasingly recognize that care to address gender dysphoria is medically necessary. As more patients are covered by insurance, they become able to access care, and transgender cultural competence is becoming recognized as a consideration for health care providers. A growing number of academic medical institutions are beginning to offer focused gender-affirming medical and surgical care. In 2017, Johns Hopkins Medicine launched its new Center for Transgender Health. In this context, history and its lessons are important to consider. We sought to evaluate the operation of the first multidisciplinary Gender Identity Clinic in the United States at the Johns Hopkins Hospital, which helped pioneer what was then called "sex reassignment surgery."
Methods: We evaluated the records of the medical archives of the Johns Hopkins University.
Results: We report data on the beginning, aim, process, outcomes of the clinic, and the reasons behind its closure. This work reveals the function of, and the successes and challenges faced by, this pioneering clinic based on the official records of the hospital and mail correspondence among the founders of the clinic.
Conclusion: This is the first study that highlights the role of the Gender Identity Clinic in establishing gender affirmation surgery and reveals the reasons of its closure.
PubMed Disclaimer
- The Legacy of Gender-Affirming Surgical Care Is Complex. Edmiston EK. Edmiston EK. Ann Plast Surg. 2019 Oct;83(4):371. doi: 10.1097/SAP.0000000000002008. Ann Plast Surg. 2019. PMID: 31524723 No abstract available.
- Reply to: The Legacy of Gender-Affirming Surgical Care Is Complex. Neira PM, Siotos C, Coon D. Neira PM, et al. Ann Plast Surg. 2019 Oct;83(4):372. doi: 10.1097/SAP.0000000000002009. Ann Plast Surg. 2019. PMID: 31524724 No abstract available.
Similar articles
- A History of Gender-Affirming Surgery at the University of Michigan: Lessons for Today. Roblee C, Keyes O, Blasdel G, Haley C, Lane M, Marquette L, Hsu J, Kuzon WM Jr. Roblee C, et al. Semin Plast Surg. 2024 Jan 19;38(1):53-60. doi: 10.1055/s-0043-1778042. eCollection 2024 Feb. Semin Plast Surg. 2024. PMID: 38495068 Review.
- Age at First Experience of Gender Dysphoria Among Transgender Adults Seeking Gender-Affirming Surgery. Zaliznyak M, Bresee C, Garcia MM. Zaliznyak M, et al. JAMA Netw Open. 2020 Mar 2;3(3):e201236. doi: 10.1001/jamanetworkopen.2020.1236. JAMA Netw Open. 2020. PMID: 32176303 Free PMC article.
- Gender-Affirming Surgery in Persons with Gender Dysphoria. Weissler JM, Chang BL, Carney MJ, Rengifo D, Messa CA 4th, Sarwer DB, Percec I. Weissler JM, et al. Plast Reconstr Surg. 2018 Mar;141(3):388e-396e. doi: 10.1097/PRS.0000000000004123. Plast Reconstr Surg. 2018. PMID: 29481407
- The Amsterdam Cohort of Gender Dysphoria Study (1972-2015): Trends in Prevalence, Treatment, and Regrets. Wiepjes CM, Nota NM, de Blok CJM, Klaver M, de Vries ALC, Wensing-Kruger SA, de Jongh RT, Bouman MB, Steensma TD, Cohen-Kettenis P, Gooren LJG, Kreukels BPC, den Heijer M. Wiepjes CM, et al. J Sex Med. 2018 Apr;15(4):582-590. doi: 10.1016/j.jsxm.2018.01.016. Epub 2018 Feb 17. J Sex Med. 2018. PMID: 29463477
- A Historical Review of Gender-Affirming Medicine: Focus on Genital Reconstruction Surgery. Frey JD, Poudrier G, Thomson JE, Hazen A. Frey JD, et al. J Sex Med. 2017 Aug;14(8):991-1002. doi: 10.1016/j.jsxm.2017.06.007. J Sex Med. 2017. PMID: 28760257 Review.
- Decoding the Misinformation-Legislation Pipeline: an analysis of Florida Medicaid and the current state of transgender healthcare. Lockmiller C. Lockmiller C. J Med Libr Assoc. 2023 Oct 2;111(4):750-761. doi: 10.5195/jmla.2023.1724. J Med Libr Assoc. 2023. PMID: 37928129 Free PMC article. Review.
- Journeying Through the Hurdles of Gender-Affirming Care Insurance: A Literature Analysis. Patel H, Camacho JM, Salehi N, Garakani R, Friedman L, Reid CM. Patel H, et al. Cureus. 2023 Mar 29;15(3):e36849. doi: 10.7759/cureus.36849. eCollection 2023 Mar. Cureus. 2023. PMID: 37123806 Free PMC article. Review.
- On, With, By-Advancing Transgender Health Research and Clinical Practice. Streed CG Jr, Perlson JE, Abrams MP, Lett E. Streed CG Jr, et al. Health Equity. 2023 Mar 3;7(1):161-165. doi: 10.1089/heq.2022.0146. eCollection 2023. Health Equity. 2023. PMID: 36895704 Free PMC article.
- Classification of Transgender Man's Breast for Optimizing Chest Masculinizing Gender-affirming Surgery. Wolf Y, Kwartin S. Wolf Y, et al. Plast Reconstr Surg Glob Open. 2021 Jan 25;9(1):e3363. doi: 10.1097/GOX.0000000000003363. eCollection 2021 Jan. Plast Reconstr Surg Glob Open. 2021. PMID: 33564589 Free PMC article.
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Ovid Technologies, Inc.
- Wolters Kluwer
- MedlinePlus Health Information
Research Materials
- NCI CPTC Antibody Characterization Program

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Transgender Legal Battles: A Timeline
New laws regarding transgender youth are based on the assumption that the gender binary is natural.

In 1952, Christine Jorgensen stepped off of a plane from Denmark, where she had received groundbreaking medical care and had grown into herself as a “blonde beauty,” as the New York Daily News declared upon her return to the United States. By most accounts, she was accepted whole-heartedly into mainstream society and fawned upon as an ideal feminine figure, a somewhat unexpected response to the first well-known transgender woman in the country. In a 2011 article in Feminist Studies , historian Emily Skidmore argues that Christine Jorgensen’s success stemmed from her ability to uphold cultural norms of whiteness and femininity , both by playing the part expected of her, and rejecting any associations with “sex deviates” such as gay men, or transgender women without access to sex reassignment surgeries. Ironically, the first key congressional mention of gender identity came almost sixteen years later in 1968, during a hearing of the House of Representatives Committee on Appropriations in which Dr. Stanley F. Yolles, director of the National Institute of Mental Health, described the use of federal funds to study and treat these same “sex deviates” .

The contrast between the experience of Christine Jorgensen and other lesbian, gay, bisexual, and transgender (LGBT) people in the 1950s and 60s—who were routinely discriminated against, harassed, and arrested—emphasizes the way that legislation is designed to enforce heteronormative gender roles and expectations. At the time, legislation was still focused on the criminalization of homosexuality through “gay behavior” in the bedroom and otherwise, with violent police harassment in private and public settings. Political campaigns at the time depicted gay people as dangerous and harmful , and enforcement of laws designed to control and oppress them disproportionately affected gender non-conforming people over those who “passed” as straight. Arrests of effeminate gay men, butch lesbians, low-income transgender women, “street queens,” and other gender non-conforming people were commonplace under laws that criminalized dressing or behaving in a way that the police officers deemed inappropriate for someone of a certain sex.
Both public opinion at the time and anti-LGBT legislation hinged upon the the belief that people could verify another’s gender identity through real or hypothetical cues, or “determine gender,” as researchers Laurel Westbrook and Kristen Schilt term it in their 2014 Gender and Society article. During this process, individuals use visual cues such as facial hair and clothing as proxies for biological validation of one’s sex , and when such cues conflict or become ambiguous, it may “create an interactional breakdown, generating anxiety, concern, and even anger.” This provides an incentive for cisgender people, whose own internal concept of their gender identity (as a man or woman) aligns with the sex they were assigned by a doctor at birth (male or female), to maintain and enforce a system in which “heterosexuality is positioned as the only natural and desirable sexual form.” On the other side of the same coin that allowed Christine Jorgensen to be accepted, there are implied and explicit forms of violence against people who do not fit neatly into heteronormative gender and sexuality boxes, with a harsher consequences for non-white or lower income communities.
In June 1969, patrons at a dodgy New York City gay bar called the Stonewall Inn began to fight back, creating a scene during a routine police raid of the premises. An event that purportedly started with a butch resisting arrest soon drew a crowd and turned into a six-day rebellion that would become a catalyst for gay rights movements around the country. Notably, the Stonewall Uprising was only one of a series of backlashes against inhumane police treatment of gay bar clientele at the time, including raids of Compton’s Cafeteria in San Francisco and the Black Cat Tavern in Los Angeles, but the context around the Stonewall Uprising in particular situated it as notable and memorable , allowing it to live on in historical accounts as the spark for gay liberation . On the first anniversary of Stonewall, the first gay liberation marches were held in New York City, San Francisco, and Los Angeles, to commemorate the event. Those annual celebrations were the foundation for today’s pride parades and festivals, held across the country in the summer months.
Despite these instances of protest and growing resistance, legislative progress lagged for nearly three more decades. While arrests for “cross-dressing” tapered off, police found new ways to use “sodomy laws,” which outlawed certain types of sexual conduct, to harass and arrest gay people. Although many of these laws applied to straight–and even married–couples, they were focusing on LGBT circles, as a way to continue policing proper gender roles and identities. In 1982, 27-year-old bartender Michael Hardwick was arrested in Georgia for consensual sex in his own bedroom, after a police officer entered his house on a false warrant. The district attorney chose not to prosecute the case, but Hardwick and the American Civil Liberties Union (ACLU) took the Bowers v. Hardwick case to the federal courts, until ultimately, the Supreme Court ruled that the sodomy law in question was constitutional and allowed to stand, along with existing sodomy laws in 24 other states. These laws slowly toppled over time, but 14 states still criminalized sodomy when Bowers v. Hardwick was overturned by Lawrence v. Texas in 2003 , after police entered John Lawrence’s apartment on a false report of a weapon on the premises and found him engaged in so-called “homosexual conduct” with Tyron Garner.
Other legislation in the 1990s and early 2000s restricted financial means and support of the LGBT community, allowing discrimination against “transvestites” in housing and disability coverage, and criticizing use of funds toward LGBT art and film . In 1996, Bill Clinton signed the Defense of Marriage Act (DOMA), invalidating any marriage between individuals of the same sex and enacting officially for the purposes of federal law, definitions of both “marriage” and “spouse” to avoid any interpretive gray area. Simultaneously, and in contrast to restrictive laws being created, the plight and suffering of LGBT people began to enter the public and legislative arena. In 1998, Representative Tom Lantos of California, Holocaust survivor and human rights champion, stood before Congress and urged them to fight for the fair treatment of LGBT people globally . He argued, eloquently, in his opening statement,
Whatever our views on our own domestic laws, Mr. Speaker, the Caucus and all Members of Congress should be standing together in decrying the persecution of individuals and the denial of human rights for any reason, including sexual orientation. … Gay, lesbian, bisexual, and transgendered people in communities all around the world have been brutally punished both physically and mentally for exercising their fundamental human rights to freedom of speech, freedom of association, and freedom of belief. Mr. Speaker, these violations fall squarely within the scope of international human rights laws.
Just two months after Tom Lantos called attention to the suffering of LGBT people in other areas of the world, the disfigured, nearly lifeless body of Matthew Shepard, a gay college student, was discovered by a kid in Laramie, Wyoming. Matthew Shepard passed away in the hospital six days later, without waking from an injury-induced coma, and his death triggered a large-scale change in the public opinion of gay people and hate crime legislation. Awareness of the unfair treatment of LGBT individuals continued to grow in the 2000s, and in 2009, forty years after the original Stonewall Uprising, President Barack Obama designated June as LGBT Pride Month . That same year, the Matthew Shepard and James Byrd Jr. Hate Crimes Prevention Act amended the wording of the Federal Hate Crimes Law to include crimes based on real or perceived sexual orientation, gender, gender identity, or disability.
As the legislative landscape moved toward prohibiting explicit discrimination against LGBT people in the bedroom, the workforce, the military, and the nation’s schools, the social and legal system maintaining the heterosexual status quo of sex, gender, and sexuality began to lose control. The Obama Administration (2009-2017) was marked by the push and pull of progressive laws allowing more freedoms for LGBT Americans alongside restrictive laws with a new focus on controlling the lives of gender non-conforming youth. In stark juxtaposition, laws benefiting transgender adults passed as waves of attacks on transgender kids were introduced. The passing of the School Success and Opportunity Act in California, allowing students to participate in programs and use facilities consistent with their gender identity , regardless of sex assigned at birth, was quickly followed by the first proposed “bathroom bill” in Arizona, criminalizing use of facilities that did not align with one’s sex assigned at birth . Although this bill in Arizona ultimately failed, it set the precedent for a series of similar bills in other states.
In 2018, the first bills were introduced in New Hampshire explicitly prohibiting insurance coverage and performance of gender-affirming healthcare –such as hormone replacement treatment (HRT), puberty blockers, and “sex reassignment surgeries”–for transgender youth. Simultaneously, the world-wide discussion around sex enforcement in women’s sports , which had previously focused on testing endogenous testosterone levels in cisgender women, refocused onto banning transgender women and girls from participation. In 2019, Georgia introduced the first bill designed to limit the participation of athletes , specifically youth, in sports based on biological sex. In the following years, attempted legal restrictions on gender-affirming healthcare and participation in sports would soar, reaching highs of 34 and 67 introduced bills, respectively, in 2021. So far in 2022, bills have been introduced in Florida and passed the House in Idaho that would criminally prosecute any medical providers who provide gender-affirming care. Texas has gone so far as to introduce a bill that classifies the acceptance and affirmation of transgender children as child abuse and criminalizes parents who support a child’s.
With the focus on controlling the ability of transgender youth to express or affirm their identities through healthcare, participation in activities, or acceptance from adults in their lives, the pertinent question becomes: why do these issues warrant such strict restrictions on the affirmation and validation of transgender children and youth? Is it truly harmful or dangerous to do so, either for the transgender youth or their cisgender peers?
Proponents of laws restricting gender-affirming care access generally cite concerns that children are too young to understand their own gender and the implications of taking hormones or undergoing surgery, or that they will come to accept their gender identity as aligning with their sex assigned at birth and will regret transitioning. For example, in a 2017 article in The New Atlantis , a journal funded by a conservative advocacy group and not peer reviewed, lead author Paul Hruz and colleagues argue that the disruption of puberty, even when temporary, may be harmful , because “gender identity is shaped during puberty and adolescence as young people’s bodies become more sexually differentiated and mature”. The authors find this especially relevant in the context of scientific unknowns and conflicting findings on the outcomes of gender non-conforming children; although most adolescents that experience gender dysphoria continue to report these feelings through adulthood, the same finding does not hold up for young children under 12 who express discomfort with their assigned sex or gender role.
On the contrary, S Giordano argues that failing to delay puberty for transgender children has the potential to harm children equally , or more. Blocking puberty allows children to alleviate the distress of gender dysphoria while allowing them the time to consider whether they want to continue with a medical transition. In his 2008 article in the Journal for Medical Ethics , he describes, “if the child does not wish to transition, puberty suppressant drugs can be withheld and development restarts as normal. If the child decides to change sex, transition is much smoother if puberty has been arrested.” Giordano further concludes,
If allowing puberty to progress appears likely to harm the child, puberty should be suspended. There is nothing unethical with interfering with spontaneous development, when spontaneous development causes great harm to the child. Indeed, it is unethical to let children suffer, when their suffering can be alleviated.
Although they ultimately disagree on the path forward, both authors acknowledge that transgender populations are particularly vulnerable to anxiety, depression, and suicidal ideation–making improved care an important public health issue. The most recent, large-scale survey of transgender adults in the United States found that 81.7 percent of respondents had seriously considered suicide in their lifetimes , and the surveyed population had a past-year prevalence of suicide attempts 18 times higher than the general US population. In addition, the study identified unique risk factors for transgender populations, concluding,
It’s clear that minority stress experiences, such as family rejection, discrimination experiences, and lack of access to gender affirming health care, create added risks for transgender people. Furthermore, the cumulative effect of experiencing multiple minority stressors is associated with dramatically higher prevalence of suicidality.
Notably, this 2019 research report by the Williams Institute also emphasized factors that were associated with a lower risk of suicidal ideation and attempt for respondents, including supportive family, access to hormone therapy and/or surgical care, and the presence of gender identity nondiscrimination statutes. A more recent research report published by the same group indicated that gender-affirming medical care, including pubertal suppression treatment, is recommended and supported as evidence-based patient care for transgender youth by several large-scale pediatric and psychiatric organizations, as it improves overall mental and physical health. Similarly, the World Professional Association for Transgender Health (WPATH) guidelines for providing the highest standards of care, which are “based on the best available science and expert professional consensus,” ultimately stress that “ withholding puberty suppression and subsequent feminizing or masculinizing hormone therapy is not a neutral option for adolescents. ” These reports arrive at an understanding that recognizes knowledge gaps in current scientific evidence and the potential risks of treatments, while accounting for the known risks of denying or delaying care to transgender youth and adults.
Research in the Human Diversity Lab led by Kristina Olson, currently at Princeton University, has shown that the development of transgender children and their understanding of their gender matches cisgender children with the same gender identity, rather than sex assigned at birth. In a 2015 paper published in Psychological Science , they conclude, “ transgender children show responses that look largely indistinguishable from those of cisgender children, who match transgender children’s gender expression on both more- and less-controllable measures. ” The group further found in a 2019 study, published in PNAS, that gender identity of transgender children is “self-socialized” based on observations in all facets of their lives , rather than socialized based on how they are treated at home. They note,
Transgender children’s gender development does not appear to show lingering impact of early sex-assignment or sex-specific socialization. That is, a 10-y-old transgender girl who was labeled a boy at birth and raised for 9 y as a boy, a 10-y-old transgender girl who was labeled a boy at birth and raised for 5 y as a boy, and a 10-y-old cisgender girl … who was labeled a girl at birth and was raised for 10 y as a girl did not significantly differ in their identification and preferences…. These findings therefore provide preliminary evidence that neither sex assignment at birth nor direct or indirect sex-specific socialization and expectations … necessarily define how a child later identifies or expresses their gender.
In light of these findings and the many unanswered questions about gender development and outcomes of care in youth, researchers have developed the “gender affirmative model” of care, which advocates for “ listen[ing] to the child and decipher[ing] with the help of parents or caregivers what the child is communicating about both gender identity and gender expressions .” In this model, children are supported through the process of exploring their gender expression as they mature, and ultimately, making informed decisions about their care at appropriate ages.
Weekly Newsletter
Get your fix of JSTOR Daily’s best stories in your inbox each Thursday.
Privacy Policy Contact Us You may unsubscribe at any time by clicking on the provided link on any marketing message.
Overall, research relating to physical and mental health outcomes in transgender youth indicates that rejection by family and community predicts negative outcomes, and that positive support from family, friends, and community protects youth and predicts positive outcomes . Current legislation restricting access of transgender youth to activities and facilities consistent with their gender identity, prohibiting gender-affirming care, and criminalizing family support functionally confines them in all aspects of their lives. Together, these sets of legislation would prohibit both social and medical transition for transgender youth to live and express themselves in a way that is consistent with their gender identity. As Laurel Westbrook and Kristen Schilt described, attempts to police participation in sex-segregated spaces and deny support to transgender people are designed to “uphold the logic of gender segregation” and “reassert the naturalness of a male-female binary”, which averts and subdues any panic or uncertainty around determining where transgender and gender non-conforming people fit into this system.
Through this lens, new waves of laws allowing discrimination and controlling access to social support for transgender youth may be reinventions of the cross-dressing and sodomy laws that enforced heterosexual and cisgender norms of behavior. As society struggles to reinforce a rigid gender binary in the face of growing dissent, the battle lines are formed by the lives, bodies, and health of transgender youth–all while their voices often go unheard.
Support JSTOR Daily! Join our new membership program on Patreon today.

JSTOR is a digital library for scholars, researchers, and students. JSTOR Daily readers can access the original research behind our articles for free on JSTOR.
Get Our Newsletter
More stories.

- Biobanking the Victims of Nuclear War

The Olive Trees of Palestine

The Race to Be the Tallest Building in the World

Eleutheria: A Lost Utopia in the Caribbean
Recent posts.
- Sex (No!), Drugs (No!), and Rock and Roll (Yes!)
- Revolutionary Writing in Carlos Bulosan’s America
- Saturn’s Ocean Moon Enceladus Is Able to Support Life
- Pas de Deux With Cancel Culture

Support JSTOR Daily
Sign up for our weekly newsletter.
- Name Search
- Browse Legal Issues
- Browse Law Firms
State Laws on Gender-Affirming Care
By Vaishali Gaur, Esq. | Legally reviewed by Laura Temme, Esq. | Last reviewed June 14, 2023
Legally Reviewed
This article has been written and reviewed for legal accuracy, clarity, and style by FindLaw’s team of legal writers and attorneys and in accordance with our editorial standards .
Fact-Checked
The last updated date refers to the last time this article was reviewed by FindLaw or one of our contributing authors . We make every effort to keep our articles updated. For information regarding a specific legal issue affecting you, please contact an attorney in your area .
Gender-affirming medical care helps nonbinary or transgender people with their physical transition. But many states have restricted access to this type of medical care for minors. Some states have even criminalized providing minors with gender-affirming care.
Gender-affirming care is crucial for the well-being of many transgender and nonbinary people. However, access to gender-affirming care has become inconsistent across the United States. This is especially true for minors.
Almost half of the state legislatures in the country recently passed laws restricting or banning such care. Some states have even criminalized providing minors with gender-affirming care.
This article provides an overview of what gender-affirming care is and which states have restricted access.
What is Gender-Affirming Care?
Gender-affirming care refers to many types of treatment for gender transitions and gender dysphoria. It can focus on psychiatric care, physical medical care, or multidisciplinary treatment. Gender dysphoria is the feeling of distress or discomfort a person feels when their gender identity does not align with the sex they were assigned at birth. It negatively impacts a person's mental health, often leading to depression and other issues.
Gender transitions can involve:
- Social transition (dressing according to gender identity, using a different name or pronouns)
- Medical transition (any combination of hormone therapy, surgical medical procedures, and nonsurgical medical procedures)
- Legal transition (legally changing name and gender marker )
Gender-affirming medical care helps nonbinary or transgender people with their physical transition. It can include hormone replacement therapy, gender-affirming surgery, or both. Gender-affirming surgery might involve:
- “Top" surgery (reconstructive surgery for the chest area)
- “Bottom" surgery (reconstructive surgery for the genital area, also known as gender confirmation, sex reassignment, or gender reassignment surgery)
- Facial feminization or masculinization procedures
- Voice surgery procedures
For many, gender-affirming care is a life-saving course of treatment. A transgender or nonbinary person's gender identity is still valid even if they have not pursued this type of care.
Gender-Affirming Care for Transgender Minors
For children and adolescents, gender-affirming care often focuses on social transition. However, in some cases, transgender children will be prescribed puberty blockers . These medications temporarily halt the changes young people experience during puberty.
For someone identified as male at birth, puberty blockers can prevent the deepening of their voice and the growth of facial and body hair. For those identified at birth as female, puberty blockers stop menstruation and breast development. But if young people stop taking the medication, puberty resumes, and they will go through the expected physical changes.
Puberty blockers are also used to treat precocious puberty . This condition, unrelated to gender dysphoria, causes a child to go through puberty too early.
Many major medical organizations support gender-affirming health care for minors, including:
- American Academy of Pediatrics
- American Medical Association
- American Academy of Child and Adolescent Psychiatry
- American Psychological Association
- American Psychiatric Association
- Endocrine Society
These organizations view gender-affirming care as appropriate “evidence-based" transgender health care. This describes an approach where doctors and medical providers rely on the best available scientific evidence from clinical research to decide what is best for their patients. Still, lawmakers in some states have passed laws in recent legislative sessions that limit or even ban gender-affirming care.

Types of Laws on Gender-Affirming Care
The map above depicts the level of restrictions on gender-affirming care in different states (as of the date of this article). States that appear in light blue currently restrict access to gender-affirming care for minors. Those states are:
Mississippi
North carolina, north dakota.
- South Carolina*
South Dakota
West virginia.
States in this list with an asterisk (*) have legislation pending that restricts access for minors.
States Without Restrictions on Gender-Affirming Care
States that appear in medium blue currently have no restrictions on gender-affirming care. Those states are:
District of Columbia
New hampshire, pennsylvania, rhode island.
The only state that appears in white is Missouri, which has restricted gender-affirming care for both minors and adults. A dark blue dot near the border of Missouri and Kansas indicates that Kansas City, Missouri, has declared itself a sanctuary city.
Some of these states are currently considering competing legislation. In New Hampshire, Republican-sponsored bills aim to ban gender-affirming care for minors and would even define it as child abuse. Meanwhile, Democrats in the state proposed a bill to make New Hampshire a sanctuary state (discussed below).
Sanctuary States
State legislation banning gender-affirming care for minors has caused worry for many. Families of nonbinary and transgender youth might feel displaced or unsafe. In response, a handful of states have designated themselves as safe harbors or "sanctuary states." These states appear in dark blue on the map above.
Sanctuary states protect access to gender-affirming care for residents of that state. Plus, they are a safe haven for trans and nonbinary people from other states. These states will not enforce penalties from another state relating to gender-affirming care:
Connecticut
Massachusetts.
Below, we provide a detailed look at the laws currently in effect in each state.
Access to Gender-Affirming Care by State
Note: The laws surrounding gender-affirming care are changing quickly. While we aim to provide the most up-to-date information on this topic, it's best to check your state legislature's website for the most recent information if you or a loved one wish to pursue gender-affirming care.
Alabama banned gender-affirming care for minors in April 2022. The law criminalizes giving puberty blockers and other gender-affirming treatments to anyone under 19. A charge under this law could result in up to 10 years in prison.
Alaska has no ban on gender-affirming care for minors or adults.
In 2022, Arizona prohibited minors from obtaining gender-affirming care ( SB 1138 ). The bill allows exceptions in the case of physical injury or illness that places the individual in imminent danger of death or for intersex individuals. The state does not have any laws prohibiting adults from receiving gender-affirming care.
Arkansas was the first state to pass a law outlawing gender-affirming care for minors ( HB 1570 ). In 2021, the state legislature passed a bill banning gender surgery and hormone therapy for minors. The law was challenged in federal court and barred by a preliminary injunction. The state's appellate court upheld the injunction . This means the ban will not take effect until the district court makes its final determination. The state does not have any laws prohibiting adults from receiving gender-affirming care.
California is a sanctuary state. In 2023, a state law providing protections for trans youth and their families went into effect (SB 107). Some states are removing minors from their parent's care if they allow the child to receive gender-affirming care. But California will not enforce another state's order to remove a minor from their parent or guardian's care.
Colorado is a sanctuary state. In 2023, a bill defining gender-affirming care as a “legally protected health-care activity" was signed into law . Under this law, state courts will not issue subpoenas connected to another state's lawsuit against a doctor who provides gender-affirming care.
Connecticut is a sanctuary state. In 2022, the state passed a law protecting individuals against out-of-state judgments based on gender-affirming care they receive in Connecticut. The state has no ban on gender-affirming care for minors or adults.
Delaware has no ban on gender-affirming care for minors or adults.
The District of Columbia has no ban on gender-affirming care for minors or adults.
Florida bans minors from receiving gender-affirming care . The Florida Board of Medicine also prohibited health care providers from performing gender-affirming care for minors unless the minor has already undergone surgery.
Georgia bans minors from receiving gender-affirming care. In 2023, a bill prohibiting medical professionals from providing gender-affirming care to minors was signed into law . The law provides exceptions for:
- Intersex individuals
- Situations where the treatment is deemed medically necessary
- Cases where minors are being treated with irreversible hormone replacement therapy
Hawai'i does not ban gender-affirming care for minors or adults.
Idaho passed a law in 2023 that makes it a felony for a medical professional to provide gender-affirming care to minors. The law includes exceptions for intersex individuals and the treatment of any infection or injury caused by prior gender-affirming care. The state does not have any laws prohibiting adults from receiving gender-affirming care.
Illinois is a sanctuary state and passed a law in 2023 that increased protections for medical professionals providing and individuals receiving gender-affirming care. The law defines gender-affirming care as “lawful health care." It prohibits the enforcement of subpoenas related to the enforcement of another state's gender-affirming care laws.
An Indiana law restricted minors from accessing gender-affirming care in 2023 and mandated any minors currently taking gender-affirming medications to cease doing so by the end of 2023.
The law provides exceptions for intersex minors, procedures necessary to treat an injury or illness caused by prior gender-affirming care, and the imminent threat of death.
The state does not have any laws prohibiting adults from receiving gender-affirming care.
In 2023, Iowa passed a law prohibiting medical professionals from providing gender-affirming care to minors.
Kansas does not ban gender-affirming care for minors or adults. However, the governor recently vetoed a proposed state law that would have required the state's medical board to revoke the medical licenses of physicians providing gender-affirming care to minors.
Kentucky recently passed a law prohibiting minors from accessing gender-affirming care and requiring medical professionals to end any gender-affirming care for minors. Although the bill was originally vetoed by the governor, the veto was ultimately overridden by the legislature. The state does not ban adults from seeking gender-affirming care.
A bill was recently introduced in Louisiana aimed at banning gender-affirming care for minors. In addition to banning hormone replacement therapy and gender-affirming surgery, the bill would also ban minors from undergoing cosmetic procedures, such as hair transplants and liposuction, if the goal of the procedures is to “promote the development of feminizing or masculinizing features in the opposite sex." Lawmakers in Louisiana's House of Representatives passed the bill. However, it was rejected by a state Senate committee in May 2023 . The state does not ban adults from accessing gender-affirming care.
Maine does not ban gender-affirming care for minors or adults.
Maryland does not ban gender-affirming care for minors or adults.
Massachusetts is a sanctuary state. It passed a law in 2022 , expanding protections for individuals seeking gender-affirming care. Among other things, the law defined gender-affirming care as “legally protected health care" and protected individuals from out-of-state legal action for seeking gender-affirming care.
In October 2022, a bill was introduced in Michigan that could make it a first-degree felony of child abuse for a parent or guardian to allow minor children to access gender-affirming care. However, that measure was unsuccessful. In March 2023, the state's House of Representatives passed an amendment to the Eliot-Larsen Civil Rights Act . This bill expands the state's protections against discrimination to include gender identity and sexual orientation. Governor Gretchen Whitmer signed the bill into law on March 16, 2023.
Minnesota is a sanctuary state. Recently, the state governor signed a bill protecting gender-affirming care . Among other things, the law prohibits the use of subpoenas to gather information about individuals that are related to out-of-state laws banning gender-affirming care. It also provides custody protections to parents or guardians who assist their minor children in accessing gender-affirming care.
Mississippi recently banned health care professionals from providing gender-affirming care to minors .
In April 2023, Missouri's Attorney General issued an emergency regulation to ban gender-affirming care for minors and adults. The rule was temporarily blocked by a state judge after being challenged in court .
In 2023, state lawmakers passed a bill banning gender-affirming care for minors. It also restricts access to care for adults who rely on Medicare for their health care costs. Governor Mike Parson signed the bill into law, and it will take effect on August 28, 2023.
However, officials in Kansas City declared the state's largest city as a sanctuary for gender-affirming care . For more details on how this affects access to care, it's best to consult with a local civil rights or health care attorney .
Montana recently passed a law prohibiting minors from receiving gender-affirming care. It also puts health care professionals at risk of having their licenses suspended if they provide minors with access to gender-affirming care. There are currently no state laws prohibiting adults from accessing gender-affirming care.
In May 2023, Nebraska Governor Jim Pillen signed a bill restricting gender-affirming care for those under the age of 19. The bill is known as the "Let Them Grow Act" (LB 574). It bans gender transition surgeries, puberty blockers, and hormone treatments for patients under 19.
There are currently no state laws in Nevada prohibiting adults or minors from accessing gender-affirming care. But the Nevada legislature is currently considering two bills that could protect access. One bill proposes requiring health insurance companies to cover gender-affirming care . Another would protect healthcare providers from having their licenses revoked and facing other penalties for providing gender-affirming care.
Two bills involving gender-affirming care have been introduced in the New Hampshire legislature this year. One would prohibit gender-affirming care for minors . The other aims to provide sanctuary protections for the families of minors seeking gender-affirming care . There are currently no state laws prohibiting adults from accessing gender-affirming care.
New Jersey is a sanctuary state, and its governor recently signed Executive Order No. 326 , which provided protections for healthcare professionals giving gender-affirming care to out-of-state residents seeking gender-affirming care.
New Mexico is a sanctuary state. It recently passed a law prohibiting the release of information regarding gender-affirming care for an out-of-state “investigation or proceeding that seeks to impose civil or criminal liability or professional disciplinary action." The law designates gender-affirming care as a “protected health care activity." The state also passed a law protecting access to gender-affirming care by ensuring that local governments cannot bar access to gender-affirming care.
New York is a sanctuary state and is currently seeking to pass a bill that would provide various protections for:
- Minors seeking gender-affirming care
- Families permitting gender-affirming care to minors
- Health care providers giving gender-affirming care to minors
Among other things, the bill would prohibit:
- Law enforcement agencies from providing information regarding gender-affirming care to out-of-state agencies
- The issuance of subpoenas in connection with out-of-state proceedings involving people traveling to New York to receive gender-affirming care
- The arrest of a person for performing or assisting in gender-affirming care
- Insurers from taking action against health care providers who provide gender-affirming care
The North Carolina House of Representatives recently passed a bill that would ban minors from getting gender-affirming surgery. It would also prevent state funds (such as Medicaid) from being used for any gender-affirming procedures provided to a person under 18. If the bill passes in the Senate and is signed by the governor, it will take effect on October 1, 2023.
North Dakota has banned gender-affirming care for minors . There are currently no state laws prohibiting adults from accessing gender-affirming care.
The Ohio legislature is currently reviewing a bill that would prohibit gender-affirming care for minors and ban health care providers from giving gender-affirming care to minors.
Oklahoma Governor Kevin Stitt recently signed a bill making it a felony for physicians to provide access to gender-affirming care to patients under 18 years old. This includes hormone treatments.
There are currently no state laws in Oregon prohibiting minors or adults from accessing gender-affirming care. Lawmakers are currently considering a bill that would:
- Provide protections to out-of-state individuals seeking gender-affirming care in Oregon
- Provide protections for health care professionals giving gender-affirming care to patients
- Expand the definition of “medically necessary" gender-affirming care, such as cosmetic procedures.
There are currently no state laws in Pennsylvania prohibiting minors or adults from accessing gender-affirming care.
There are currently no state laws in Rhode Island prohibiting minors or adults from accessing gender-affirming care.
South Carolina
There are three bills regarding gender-affirming care circulating in the South Carolina legislature. If passed, S0274 could ban transgender or nonbinary people under 21 years old from receiving gender-affirming care. This bill would also require school employees to notify a minor's parents or guardians if the minor identifies as transgender or struggles with their gender identity. S0243 seeks to block physicians from providing gender-affirming care to minors. S0276 would amend the state constitution to define “gender" as one's sex assigned at birth.
South Dakota passed a law banning gender-affirming care for minors. Health care providers risk losing their medical licenses and could face civil action if they do not comply. There are currently no state laws prohibiting adults from accessing gender-affirming care.
Tennessee recently passed a law that prohibits health care providers from giving gender-affirming care to minors.
In June 2023, Texas Governor Greg Abbott signed a bill banning gender-affirming care for most minors . The law will take effect September 1, 2023, and prohibits access to hormone treatments and puberty blockers for those under 18.
Two other bills have been introduced in the Texas legislature regarding gender-affirming care. HB42 would criminalize gender-affirming care for minors by defining it as child abuse. HB41 would take away liability insurance from providers that provide gender-affirming care to minors.
Utah recently signed a bill that bans gender-affirming care for minors and prohibits health care providers from giving gender-affirming care to minors.
In May 2023, Vermont Governor Phil Scott signed two bills into law protecting gender-affirming health care. House Bill 89 states that gender-affirming health care is now protected by state law. It also shields out-of-state patients (and their doctors) from penalties against gender-affirming care in their home state. Senate Bill 37 requires health insurance companies in Vermont to cover gender-affirming care.
A bill introduced in the Virginia legislature would prohibit health care providers from providing gender-affirming care to minors if passed.
A bill signed in May 2023 will provide shelter to minors seeking gender-affirming care. Until now, licensed youth shelters were required to notify a minor's parents within 72 hours of their arrival. Under the new law, these facilities can instead contact Washington's Department of Children, Youth and Families. These minors will also be able to stay with volunteer host families without parental consent.
West Virginia recently banned gender-affirming care for minors . There are currently no state laws prohibiting adults from accessing gender-affirming care.
There are currently no state laws in Wisconsin prohibiting adults or minors from accessing gender-affirming care. In 2022, Representative Scott Allen introduced legislation that would have prohibited doctors from performing gender-confirming surgery on patients under 18. However, the bill did not pass.
In 2023, Dane County, Wisconsin (which includes the city of Madison) is considering a resolution making the county a sanctuary for gender-affirming care.
There are currently no state laws in Wyoming prohibiting adults from accessing gender-affirming care. Two bills were introduced by GOP senators but ultimately did not pass in the House. One bill would have made providing minors with gender-affirming care a felony of child abuse. The other bill would have revoked the licenses of health care professionals if they gave minors gender-affirming care as well as prohibited coverage of gender-affirming care under insurance.
Are There Federal Laws On Gender-Affirming Care?
There is currently no federal law protecting access to gender-affirming care. However, the Biden administration has taken steps to make health care more accessible for the LGBTQ+ community. Furthermore, the Affordable Care Act prohibits health care discrimination based on sex. Sex discrimination includes discrimination based on gender identity. The Supreme Court's decision in Bostock v. Clayton County supports this interpretation of the ACA.
Getting Legal Help
If you need guidance in navigating these laws or your state's laws, an attorney can help. A civil rights lawyer or health care lawyer can explain the protections provided above, along with any additional protections your state may provide.

Visit Our LGBTQ+ Hub
Up-to-date legal information focused on your rights.
Read more >
You May Also Like
- How to Access Gender-Affirming Healthcare for Transgender Youth
- Aging With Dignity While Living With HIV
- Hiring an Attorney in the LGBTQ+ Community
You Don’t Have To Solve This on Your Own – Get a Lawyer’s Help
Meeting with a lawyer can help you understand your options and how to best protect your rights. Visit our attorney directory to find a lawyer near you who can help.
Contact a qualified attorney for legal services focused on LGBTQ+ rights.
Enter information. (Required)
Get Help for a Criminal Case
- Criminal Law Basics
- Hate Crimes
- Domestic Violence
Thank you for subscribing!
FindLaw Newsletters Stay up-to-date with how the law affects your life
The email address cannot be subscribed. Please try again.
Learn more about FindLaw’s newsletters, including our terms of use and privacy policy.
Find a Lawyer
- Search Legal Resources
- Find Cases and Laws
- Introduction
- Conclusions
- Article Information
Error bars represent 95% CIs. GAS indicates gender-affirming surgery.
Percentages are based on the number of procedures divided by number of patients; thus, as some patients underwent multiple procedures the total may be greater than 100%. Error bars represent 95% CIs.
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Wright JD , Chen L , Suzuki Y , Matsuo K , Hershman DL. National Estimates of Gender-Affirming Surgery in the US. JAMA Netw Open. 2023;6(8):e2330348. doi:10.1001/jamanetworkopen.2023.30348
Manage citations:
© 2024
- Permissions
National Estimates of Gender-Affirming Surgery in the US
- 1 Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, New York, New York
- 2 Department of Obstetrics and Gynecology, University of Southern California, Los Angeles
Question What are the temporal trends in gender-affirming surgery (GAS) in the US?
Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Meaning These findings suggest that there will be a greater need for clinicians knowledgeable in the care of transgender individuals with the requisite expertise to perform gender-affirming procedures.
Importance While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, Setting, and Participants This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main Outcome Measures Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and Relevance Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
Gender dysphoria is characterized as an incongruence between an individual’s experienced or expressed gender and the gender that was assigned at birth. 1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS). 2 GAS encompasses a variety of procedures that align an individual patient’s gender identity with their physical appearance. 2 - 4
While numerous surgical interventions can be considered GAS, the procedures have been broadly classified as breast and chest surgical procedures, facial and cosmetic interventions, and genital reconstructive surgery. 2 , 4 Prior studies 2 - 7 have shown that GAS is associated with improved quality of life, high rates of satisfaction, and a reduction in gender dysphoria. Furthermore, some studies have reported that GAS is associated with decreased depression and anxiety. 8 Lastly, the procedures appear to be associated with acceptable morbidity and reasonable rates of perioperative complications. 2 , 4
Given the benefits of GAS, the performance of GAS in the US has increased over time. 9 The increase in GAS is likely due in part to federal and state laws requiring coverage of transition-related care, although actual insurance coverage of specific procedures is variable. 10 , 11 While prior work has shown that the use of inpatient GAS has increased, national estimates of inpatient and outpatient GAS are lacking. 9 This is important as many GAS procedures occur in ambulatory settings. We performed a population-based analysis to examine trends in GAS in the US and explored the temporal trends in the types of GAS performed across age groups.
To capture both inpatient and outpatient surgical procedures, we used data from the Nationwide Ambulatory Surgery Sample (NASS) and the National Inpatient Sample (NIS). NASS is an ambulatory surgery database and captures major ambulatory surgical procedures at nearly 2800 hospital-owned facilities from up to 35 states, approximating a 63% to 67% stratified sample of hospital-owned facilities. NIS comprehensively captures approximately 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP), covering more than 97% of the US population. Both NIS and NASS contain weights that can be used to produce US population estimates. 12 , 13 Informed consent was waived because data sources contain deidentified data, and the study was deemed exempt by the Columbia University institutional review board. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We selected patients of all ages with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) diagnosis codes for gender identity disorder or transsexualism ( ICD-10 F64) or a personal history of sex reassignment ( ICD-10 Z87.890) from 2016 to 2020 (eTable in Supplement 1 ). We first examined all hospital (NIS) and ambulatory surgical (NASS) encounters for patients with these codes and then analyzed encounters for GAS within this cohort. GAS was identified using ICD-10 procedure codes and Common Procedural Terminology codes and classified as breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures. 2 , 4 Breast and chest surgical procedures encompassed breast reconstruction, mammoplasty and mastopexy, or nipple reconstruction. Genital reconstructive procedures included any surgical intervention of the male or female genital tract. Other facial and cosmetic procedures included cosmetic facial procedures and other cosmetic procedures including hair removal or transplantation, liposuction, and collagen injections (eTable in Supplement 1 ). Patients might have undergone procedures from multiple different surgical groups. We measured the total number of procedures and the distribution of procedures within each procedural group.
Within the data sets, sex was based on patient self-report. The sex of patients in NIS who underwent inpatient surgery was classified as either male, female, missing, or inconsistent. The inconsistent classification denoted patients who underwent a procedure that was not consistent with the sex recorded on their medical record. Similar to prior analyses, patients in NIS with a sex variable not compatible with the procedure performed were classified as having undergone genital reconstructive surgery (GAS not otherwise specified). 9
Clinical variables in the analysis included patient clinical and demographic factors and hospital characteristics. Demographic characteristics included age at the time of surgery (12 to 18 years, 19 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, 61 to 70 years, and older than 70 years), year of the procedure (2016-2020), and primary insurance coverage (private, Medicare, Medicaid, self-pay, and other). Race and ethnicity were only reported in NIS and were classified as White, Black, Hispanic and other. Race and ethnicity were considered in this study because prior studies have shown an association between race and GAS. The income status captured national quartiles of median household income based of a patient’s zip code and was recorded as less than 25% (low), 26% to 50% (medium-low), 51% to 75% (medium-high), and 76% or more (high). The Elixhauser Comorbidity Index was estimated for each patient based on the codes for common medical comorbidities and weighted for a final score. 14 Patients were classified as 0, 1, 2, or 3 or more. We separately reported coding for HIV and AIDS; substance abuse, including alcohol and drug abuse; and recorded mental health diagnoses, including depression and psychoses. Hospital characteristics included a composite of teaching status and location (rural, urban teaching, and urban nonteaching) and hospital region (Northeast, Midwest, South, and West). Hospital bed sizes were classified as small, medium, and large. The cutoffs were less than 100 (small), 100 to 299 (medium), and 300 or more (large) short-term acute care beds of the facilities from NASS and were varied based on region, urban-rural designation, and teaching status of the hospital from NIS. 8 Patients with missing data were classified as the unknown group and were included in the analysis.
National estimates of the number of GAS procedures among all hospital encounters for patients with gender identity disorder were derived using discharge or encounter weight provided by the databases. 15 The clinical and demographic characteristics of the patients undergoing GAS were reported descriptively. The number of encounters for gender identity disorder, the percentage of GAS procedures among those encounters, and the absolute number of each procedure performed over time were estimated. The difference by age group was examined and tested using Rao-Scott χ 2 test. All hypothesis tests were 2-sided, and P < .05 was considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
A total of 48 019 patients who underwent GAS were identified ( Table 1 ). Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged 12 to 18 years. Private insurance coverage was most common in 29 064 patients (60.5%), while 12 127 (25.3%) were Medicaid recipients. Depression was reported in 7192 patients (15.0%). Most patients (42 467 [88.4%]) were treated at urban, teaching hospitals, and there was a disproportionate number of patients in the West (22 037 [45.9%]) and Northeast (12 396 [25.8%]). Within the cohort, 31 668 patients (65.9%) underwent 1 procedure while 13 415 (27.9%) underwent 2 procedures, and the remainder underwent multiple procedures concurrently ( Table 1 ).
The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. Among encounters with a billing code for gender identity disorder, there was a consistent rise in the percentage that were for GAS from 4552 (32.9%) in 2016 to 13 011 (37.1%) in 2019, followed by a decline to 12 818 (33.3%) in 2020 ( Figure 1 and eFigure in Supplement 1 ). Among patients undergoing ambulatory surgical procedures, 37 394 (80.3%) of the surgical procedures included gender-affirming surgical procedures. For those with hospital admissions with gender identity disorder, 10 625 (11.8%) of admissions were for GAS.
Breast and chest procedures were most common and were performed for 27 187 patients (56.6%). Genital reconstruction was performed for 16 872 patients (35.1%), and other facial and cosmetic procedures for 6669 patients (13.9%) ( Table 2 ). The most common individual procedure was breast reconstruction in 21 244 (44.2%), while the most common genital reconstructive procedure was hysterectomy (4489 [9.3%]), followed by orchiectomy (3425 [7.1%]), and vaginoplasty (3381 [7.0%]). Among patients who underwent other facial and cosmetic procedures, liposuction (2945 [6.1%]) was most common, followed by rhinoplasty (2446 [5.1%]) and facial feminizing surgery and chin augmentation (1874 [3.9%]).
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020 ( Figure 1 ). Similar trends were noted for breast and chest surgical procedures as well as genital surgery, while the rate of other facial and cosmetic procedures increased consistently from 2016 to 2020. The distribution of the individual procedures performed in each class were largely similar across the years of analysis ( Table 3 ).
When stratified by age, patients 19 to 30 years had the greatest number of procedures, 25 099 ( Figure 2 ). There were 10 476 procedures performed in those aged 31 to 40 years and 4359 in those aged 41 to 50 years. Among patients younger than 19 years, 3678 GAS procedures were performed. GAS was less common in those cohorts older than 50 years. Overall, the greatest number of breast and chest surgical procedures, genital surgical procedures, and facial and other cosmetic surgical procedures were performed in patients aged 19 to 30 years.
When stratified by the type of procedure performed, breast and chest procedures made up the greatest percentage of the surgical interventions in younger patients while genital surgical procedures were greater in older patients ( Figure 2 ). Additionally, 3215 patients (87.4%) aged 12 to 18 years underwent GAS and had breast or chest procedures. This decreased to 16 067 patients (64.0%) in those aged 19 to 30 years, 4918 (46.9%) in those aged 31 to 40 years, and 1650 (37.9%) in patients aged 41 to 50 years ( P < .001). In contrast, 405 patients (11.0%) aged 12 to 18 years underwent genital surgery. The percentage of patients who underwent genital surgery rose sequentially to 4423 (42.2%) in those aged 31 to 40 years, 1546 (52.3%) in those aged 51 to 60 years, and 742 (58.4%) in those aged 61 to 70 years ( P < .001). The percentage of patients who underwent facial and other cosmetic surgical procedures rose with age from 9.5% in those aged 12 to 18 years to 20.6% in those aged 51 to 60 years, then gradually declined ( P < .001). Figure 2 displays the absolute number of procedure classes performed by year stratified by age. The greatest magnitude of the decline in 2020 was in younger patients and for breast and chest procedures.
These findings suggest that the number of GAS procedures performed in the US has increased dramatically, nearly tripling from 2016 to 2019. Breast and chest surgery is the most common class of procedure performed while patients are most likely to undergo surgery between the ages of 19 and 30 years. The number of genital surgical procedures performed increased with increasing age.
Consistent with prior studies, we identified a remarkable increase in the number of GAS procedures performed over time. 9 , 16 A prior study examining national estimates of inpatient GAS procedures noted that the absolute number of procedures performed nearly doubled between 2000 to 2005 and from 2006 to 2011. In our analysis, the number of GAS procedures nearly tripled from 2016 to 2020. 9 , 17 Not unexpectedly, a large number of the procedures we captured were performed in the ambulatory setting, highlighting the need to capture both inpatient and outpatient procedures when analyzing data on trends. Like many prior studies, we noted a decrease in the number of procedures performed in 2020, likely reflective of the COVID-19 pandemic. 18 However, the decline in the number of procedures performed between 2019 and 2020 was relatively modest, particularly as these procedures are largely elective.
Analysis of procedure-specific trends by age revealed a number of important findings. First, GAS procedures were most common in patients aged 19 to 30 years. This is in line with prior work that demonstrated that most patients first experience gender dysphoria at a young age, with approximately three-quarters of patients reporting gender dysphoria by age 7 years. These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments. 19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent GAS, even in the highest volume years. GAS in adolescents has been the focus of intense debate and led to legislative initiatives to limit access to these procedures in adolescents in several states. 20 , 21
Second, there was a marked difference in the distribution of procedures in the different age groups. Breast and chest procedures were more common in younger patients, while genital surgery was more frequent in older individuals. In our cohort of individuals aged 19 to 30 years, breast and chest procedures were twice as common as genital procedures. Genital surgery gradually increased with advancing age, and these procedures became the most common in patients older than 40 years. A prior study of patients with commercial insurance who underwent GAS noted that the mean age for mastectomy was 28 years, significantly lower than for hysterectomy at age 31 years, vaginoplasty at age 40 years, and orchiectomy at age 37 years. 16 These trends likely reflect the increased complexity of genital surgery compared with breast and chest surgery as well as the definitive nature of removal of the reproductive organs.
This study has limitations. First, there may be under-capture of both transgender individuals and GAS procedures. In both data sets analyzed, gender is based on self-report. NIS specifically makes notation of procedures that are considered inconsistent with a patient’s reported gender (eg, a male patient who underwent oophorectomy). Similar to prior work, we assumed that patients with a code for gender identity disorder or transsexualism along with a surgical procedure classified as inconsistent underwent GAS. 9 Second, we captured procedures commonly reported as GAS procedures; however, it is possible that some of these procedures were performed for other underlying indications or diseases rather than solely for gender affirmation. Third, our trends showed a significant increase in procedures through 2019, with a decline in 2020. The decline in services in 2020 is likely related to COVID-19 service alterations. Additionally, while we comprehensively captured inpatient and ambulatory surgical procedures in large, nationwide data sets, undoubtedly, a small number of procedures were performed in other settings; thus, our estimates may underrepresent the actual number of procedures performed each year in the US.
These data have important implications in providing an understanding of the use of services that can help inform care for transgender populations. The rapid rise in the performance of GAS suggests that there will be a greater need for clinicians knowledgeable in the care of transgender individuals and with the requisite expertise to perform GAS procedures. However, numerous reports have described the political considerations and challenges in the delivery of transgender care. 22 Despite many medical societies recognizing the necessity of gender-affirming care, several states have enacted legislation or policies that restrict gender-affirming care and services, particularly in adolescence. 20 , 21 These regulations are barriers for patients who seek gender-affirming care and provide legal and ethical challenges for clinicians. As the use of GAS increases, delivering equitable gender-affirming care in this complex landscape will remain a public health challenge.
Accepted for Publication: July 15, 2023.
Published: August 23, 2023. doi:10.1001/jamanetworkopen.2023.30348
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Wright JD et al. JAMA Network Open .
Corresponding Author: Jason D. Wright, MD, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, 161 Fort Washington Ave, 4th Floor, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Wright had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Wright, Chen.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Wright.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Wright, Chen.
Administrative, technical, or material support: Wright, Suzuki.
Conflict of Interest Disclosures: Dr Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- The rise and fall of gende...
The rise and fall of gender identity clinics in the 1960s and 1970s
Editor’s note: this article is based on the second-place poster in the american college of surgeons history of surgery poster contest at the virtual clinical congress 2020. the authors note that as the field of medicine and society have evolved to better understand the experiences of transgender individuals, terminology has changed significantly. the authors have […].
Melanie Fritz, Nat Mulkey
April 1, 2021
Editor’s note: This article is based on the second-place poster in the American College of Surgeons History of Surgery poster contest at the virtual Clinical Congress 2020. The authors note that as the field of medicine and society have evolved to better understand the experiences of transgender individuals, terminology has changed significantly. The authors have kept the original wording of direct quotes, but elsewhere in the article terminology is used that is consistent with present-day standards; that is, “transgender” or “transgender and gender nonbinary.”
HIGHLIGHTS Summarizes early pioneering work in the GAS field in the U.S. and Europe Describes the effects of clinic closures in the 1970s Outlines the resurgence of multidisciplinary clinics for TGNB patients at academic centers and in private practice Identifies ongoing barriers related to GAS, including financial concerns and access to reliable information
Transgender and gender nonbinary (TGNB) individuals have existed for thousands of years and in cultures throughout the world. In Western medicine, however, the modern era of gender-affirming surgery (GAS) began at the Institute of Sexual Research in Berlin, Germany, under the leadership of Magnus Hirschfeld, MD. Surgeons at the institute performed the earliest vaginal constructions in the 1930s. Early patients included an employee of the facility, known by the last name of Dorchen, and the Danish painter Lili Elbe, whose story was depicted in the 2015 film The Danish Girl . 1
Around the same time that Dr. Hirschfeld’s institute began performing vaginoplasties, the father of plastic surgery, Sir Harold Gillies, OBE, FRCS, had been refining techniques for genital construction in Britain. He did so primarily by operating on British men who had sustained genital injuries during wartime and subsequently presented to him for assistance. In the 1940s, he performed the first known phalloplasty for a transgender patient on Michael Dillon, MD, a British physician. Dr. Gillies later performed a vaginoplasty on patient Roberta Cowell, who gained some renown in Britain. 2
In the 1950s, Georges Burou, MD, began performing vaginoplasty operations in Casablanca, Morocco, and is widely credited with inventing the anteriorly pedicled penile skin flap inversion vaginoplasty. 3
Increased awareness in the U.S.
One of the earliest known GAS procedures performed in the U.S. was for patient Alan Hart, MD, a transgender man and physician, who underwent a hysterectomy in 1910. 1
The field of GAS subsequently remained dormant in the U.S. until the 1950s, when pioneers like Elmer Belt, MD, University of California Los Angeles, and Milton Edgerton, MD, Johns Hopkins University (JHU) began performing GAS. 4,5
The work of sexologist and endocrinologist Harry Benjamin, MD, in the 1950s and 1960s provided additional momentum to the field within the medical community. At the time, many psychiatrists and physicians believed that the correct approach to treating transgender patients was exclusively through psychoanalytic therapy aimed at altering the desire to live as a different gender. Dr. Benjamin is attributed with being one of the first physicians to challenge this notion.
In 1966, he published The Transsexual Phenomenon , which detailed the era’s approach to GAS. 4 Notably, this text includes far more detail about male-to-female (MTF) surgical operations, such as vaginoplasty, than female-to-male (FTM) operations, such as phalloplasty or metoidioplasty. At the time, transgender men were incorrectly believed to be less common than transgender women, and surgeons were reluctant to perform FTM GAS procedures. Based on writings from the era, some of this reluctance stemmed from uncertainty as to whether surgical techniques were capable of constructing a neophallus that would be satisfactory to the patient. 6
A boom of awareness of GAS within both the field of medicine and the larger U.S. public can primarily be attributed to one individual: Christine Jorgensen. Ms. Jorgensen was a transgender woman who captured the attention and interest of the general public after undergoing a series of operations for GAS in Denmark from 1951 to 1952. 4 Her coming out story and transition were covered extensively in popular media, appearing in the New York Daily News under the eye-catching headline “Ex-GI Becomes Blonde Beauty.” 7
Wave of clinics providing GAS
Publication of Dr. Benjamin’s book coincided with the public announcement of JHU Gender Identity Clinic in November 1966. 8 While several major academic centers had internally discussed the formation of research institutes to study the treatment of transgender patients since the early 1960s, the opening of the JHU clinic marked a transition from quiet deliberation to public recruitment for research on GAS. Initiatives quickly sprung up at many major universities and hospitals, marked by interdisciplinary collaboration between psychiatrists, urologists, plastic surgeons, gynecologists, and social workers. While estimates vary, the increase in U.S. patients who underwent GAS was dramatic, growing to more than 1,000 by the end of the 1970s from approximately 100 patients in 1969. 5,9
Producing positive results in a stigmatized field
Whereas GAS was a new endeavor for U.S. physicians, these clinics primarily operated as research programs. As a new field of practice, the physicians involved in the clinics faced significant skepticism from colleagues, such as psychiatrist Joost Meerloo, MD, who outlined his concerns in the American Journal of Psychiatry in 1967. Dr. Meerloo wrote, “Unwittingly, many a physician does not treat the disease as such but treats, rather, the fantasy a patient develops about his disease…I believe the surgical treatment of transsexual yearnings easily falls into this trap…. What about our medical responsibility and ethics? Do we have to collaborate with the sexual delusions of our patients?” 10
Understandably, physicians involved in these gender identity clinics described feeling pressure to demonstrate successful postoperative outcomes in order to justify their work. In the introduction to a published case series on GAS, Norman Fisk, MD, a psychiatrist at Stanford University, CA, wrote, “In our efforts we were preoccupied with obtaining good results. This preoccupation, we believed, would enable us to continue our work in an area where many professional colleagues had, and retain, serious doubts as to the validity of gender reorientation.” 11
In an attempt to obtain good results, these clinics often maintained rigorous selection criteria that excluded a number of patients. The evaluation process required that patients undergo hormone treatment and live for a set period of time as the gender to which they intended to transition. This period of time could extend up to five years depending on the clinic, imposing a significant burden on patients. As one patient, transgender man Mario Martino, stated, “One talks of a period of two to five years. I agree that people should be tested. I think that they should be tested in every way possible before being accepted as a candidate for treatment. However, one of the problems that people tend to forget is that a female with a 48-inch bust cannot pass as a male for one day, much less for one year or five years, no matter how much he tries.” 12
Individuals who were considered traditionally attractive and were expected to be easily perceived as a member of the other sex, as well as individuals who were heterosexual per their gender identity, were considered better surgical candidates. To demonstrate the scale of this selectivity, out of 2,000 applications sent to JHU within two years of opening, only 24 patients underwent an operation. 5,11,13
Though early studies were small, many did, in fact, demonstrate successful psychiatric outcomes. A report from Edgerton and colleagues in 1970 found that at one to two years postoperatively, of nine patients who underwent GAS, all were glad to have undergone surgery, had greater self-confidence, and held “a brighter outlook for their future.” 5 When considering the competing demands of producing positive outcomes and providing GAS to patients in need, it’s clear how physicians working in these clinics were confronted with challenges in their roles. They were advocates for a marginalized population, and yet they also functioned as gatekeepers for thousands of transgender patients desperate for surgery and who faced reinforced gender-based stereotypes as described earlier in the eligibility criteria.
Timeline and clinic closure
Toward the end of the 1970s, many centers closed their doors to new patients. These closures often were kept out of the public eye, making it difficult to discern precise timing or causes. There were, however, two notable exceptions to the pattern of patient enrollment quietly declining and ceasing.
At JHU, a new chair of psychiatry, Paul McHugh, MD, was hired in 1975. Dr. McHugh disapproved of offering GAS to transgender patients and acknowledged that from the moment he was hired, he intended to stop this practice at the clinic. Under his leadership, JHU psychiatrist Jon Meyer, MD, published a study of 50 surgical patients from the JHU clinic, which concluded that GAS offered “no objective benefit” for transgender people. Although this claim directly contradicted a growing body of evidence that found significant benefit for transgender patients, the publication sparked the rapid closure of the JHU clinic in 1979. 14
FIGURE 1. GENDER IDENTITY CLINIC TIMELINE
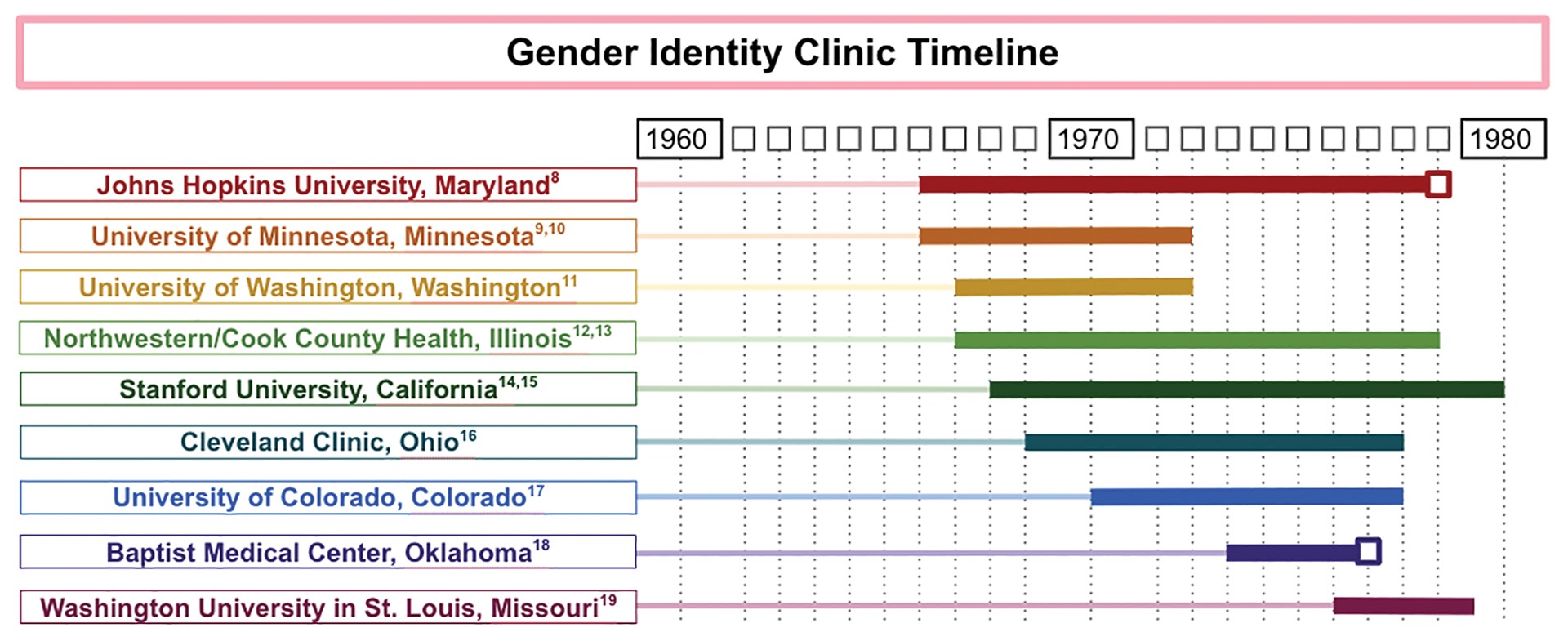
Another gender identity clinic where operations were abruptly terminated was the Baptist Medical Center in Oklahoma City. The Gender Identity Foundation at the center had offered a variety of services for transgender patients, including GAS, since 1973, under the radar of local religious leaders. In 1977, however, the issue of GAS was brought to the attention of the board of directors of the Baptist General Convention of Oklahoma. The physicians involved fervently advocated to be allowed to continue their practice, including surgeons Charles L. Reynolds, Jr., MD, FACS, and David W. Foerster, MD, FACS, who issued a joint statement that said, “[I]f Jesus Christ were alive today, undoubtedly he would render help and comfort to the transsexual.” Despite these appeals, the board of directors voted 54–2 to ban GAS at the Baptist Medical Center. 15
Given the known timing of when these two clinics closed, they are marked with a box in a timeline constructed by the authors (see Figure 1). The remaining end dates are estimates derived from the latest reported operations in the medical literature and news articles, which likely underestimate the length of time the clinics were in operation. The reasons for closure of the remaining clinics appear to be multifactorial.
The publicity around the Meyer paper that led to JHU’s clinic closure may have played a role in the decision to close other clinics. 16 In addition, some clinics described financial challenges during this time, as patients often were unable to afford the expensive operations, and insurance companies refused to cover them. For example, at the University of Minnesota, Minneapolis, clinic, the first two dozen operations were funded by a research grant at the expense of the state, but a news article from 1972 suggests that funding difficulties were exacerbated when the state no longer wanted to fund the project. 9 Institutional pushback, such as that experienced at JHU, and the retirement of leading surgeons also may have played a role in the closure of gender identity clinics across the nation.
Even though many clinics’ GAS-related research was winding down in the late 1970s, the last 15 years of academic interest motivated the 1979 establishment of the Harry Benjamin International Gender Dysphoria Association. This organization, formed with the goal of organizing professionals who were “interested in the study and care of transexualism and gender dysphoria,” has since been renamed the World Professional Association for Transgender Health (WPATH) and has grown into an international interdisciplinary organization. 17 WPATH has established internationally accepted guidelines for treating individuals with gender dysphoria, which are periodically updated. The most recent of these guidelines is the Standards of Care Version 7 (SOC7). 18 Today, insurance companies, national payors, and treatment teams in both the U.S. and Europe use the WPATH SOC7 guidelines for establishing surgical eligibility.
Present day significance
The contemporaneous evolution of the first wave of gender identity clinics generated a rich field for refinement of surgical technique, as well as the assessment of postoperative outcomes, and produced a foundation of scientific literature demonstrating successful psychiatric outcomes for transgender people undergoing GAS. These milestones foreshadowed a resurgence of multidisciplinary clinics for TGNB individuals in academic centers and paved the way for private practitioners to specialize in GAS. For example, Stanley Biber, MD, a private practice surgeon in Colorado, performed more than 5,000 GAS operations during his 35 years in practice. 19
Many centers for transgender medicine and surgery now exist across the U.S., and the number of GAS operations being performed in the U.S. has increased substantially, along with expanded insurance coverage. In 2015, the U.S. Transgender Survey found that 25 percent of TGNB individuals had one or more gender-affirming operations. 20 Similar to the earlier wave of clinics, present-day clinics still are frequently composed of an interdisciplinary team of primary care, surgical, and mental health professionals.
Although the number of GAS continues to increase, the current discourse echoes earlier concerns about how to limit barriers for this marginalized population while prioritizing positive surgical outcomes. The WPATH standards of care often function as guides to assist health care centers in creating TGNB health programs. 21 The WPATH SOCs have evolved since their establishment and presently tend to include fewer preoperative requirements for TGNB patients than in the 1970s and 1980s.
However, TGNB patients continue to face significant barriers to accessing GAS. A 2018 survey of TGNB patients found that the most commonly cited barriers to gender-affirming care are financial concerns, access to physicians who are knowledgeable about GAS, and access to reliable information. 22 These financial concerns can be exacerbated by the cost of obtaining the mental health evaluations recommended by WPATH SOC7, and challenges associated with insurance coverage. 23 To address these barriers, institutions are considering preoperative models besides the WPATH SOC7 to potentially reduce challenges.
Moreover, general medical education initiatives are under way to increase provider knowledge about this population. 24,25 As the field of GAS continues to evolve in the present day, we look forward to seeing how the surgical and medical community partners with patients to minimize these barriers and promote access to these essential surgical treatments.
- Denny D. Gender reassignment surgeries in the XXth century. Workshop at 9th Transgender Lives: The Intersection of Health and Law Conference, Farmington, CT. May 10, 2015. Available at: http://dallasdenny.com/Writing/2015/05/10/gender-reassignment-surgeries-in-the-xxth-century-2015/ . Accessed February 11, 2021.
- Kennedy P. The First Man-Made Man: The Story of Two Sex Changes, One Love Affair, and a Twentieth-Century Medical Revolution . New York: Bloomsbury USA; 2007.
- Hage JJ, Kareem RB, Laub DR. On the origin of pedicled skin inversion vaginoplasty: Life and work of Dr. Georges Burou of Casablanca. Ann Plast Surg . 2007;59(6):723-729.
- Benjamin H. The Transsexual Phenomenon . New York, New York: Warner Books Incorporated; 1966.
- Edgerton MT, Knorr NJ, Callison JR. The surgical treatment of transsexual patients. Limitations and indications. Plast Reconstr Surg . 1970;45(1):38-46.
- Williams G. An approach to transsexual surgery. Nurs Times . 1973;69(25):787.
- Ex-GI becomes blonde beauty: Operations transform Bronx youth. New York Daily News . December 1, 1952:75. Available at: www.newspapers.com/clip/25375703/ex-gi-becomes-blonde-beauty/ . Accessed March 22, 2021.
- Buckley T. A changing of sex by surgery begun at Johns Hopkins. The New York Times . November 21, 1966. Available at: www.nytimes.com/1966/11/21/archives/a-changing-of-sex-by-surgery-begun-at-johns-hopkins-johns-hopkins.html . Accessed March 22, 2021.
- Brody J. 500 in the U.S. change sex in six years with surgery. The New York Times . Nov 20, 1972. Available at: www.nytimes.com/1972/11/20/archives/500-in-the-u-s-change-sex-in-six-years-with-surgery-500-change-sex.html . Accessed February 11, 2021.
- Meerloo JA. Change of sex and collaboration with the psychosis. Am J Psychiatry . 1967;124(2):263-264.
- Fisk NM. Five spectacular results. Arch Sex Behav . 1978;7(4):351-369.
- Money J. Transsexualism: Open forum. Arch Sex Behav . 1978;7(4):387-415.
- Hastings D, Markland C. Post-surgical adjustment of 25 transsexuals at University of Minnesota. Arch Sex Behav . 1978;7(4):327-336.
- Siotos C, Neira PM, Lau BD, et al. Origins of gender affirmation surgery: The history of the first gender identity clinic in the United States at Johns Hopkins. Ann Plast Surg . 2019;83(2):132-136.
- Baptists vote to ban sex change operations. Sarasota Herald-Tribune . October 15, 1977.
- Nutt AE. Long shadow cast by psychiatrist on transgender issues finally recedes at Johns Hopkins. Washington Post . April 5, 2017. Available at: www.washingtonpost.com/national/health-science/long-shadow-cast-by-psychiatrist-on-transgender-issues-finally-recedes-at-johns-hopkins/2017/04/05/e851e56e-0d85-11e7-ab07-07d9f521f6b5_story.html . Accessed February 11, 2021.
- Walker PA. The University of Texas Medical Branch. Memo to persons interested in the Harry Benjamin International Gender Dysphoria Association. April 17, 1979. Available at: www.wpath.org/media/cms/Documents/History/Harry%20Benjamin/First%20HBIGDA%20Membership%20Request%20Letter%201979.pdf . Accessed February 11, 2021.
- Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend . 2012;13(4):165-232.
- Arrillaga P. Onetime coal mining town bolstered by changing economy. Los Angeles Times . June 4, 2000. Available at: www.latimes.com/archives/la-xpm-2000-jun-04-me-37512-story.html . Accessed February 11, 2021.
- James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The Report of the 2015 Transgender Survey. Washington, DC: National Center for Healthcare Equality, 2016. Available at: www.transequality.org/sites/default/files/docs/USTS-Full-Report-FINAL.PDF . Accessed February 11, 2021.
- National LGBT Health Education Center. Creating a transgender health program at your health center: Planning to implementation. September 2018. Available at: www.lgbtqiahealtheducation.org/wp-content/uploads/2018/10/Creating-a-Transgender-Health-Program.pdf . Accessed February 11, 2021.
- El-Hadi H, Stone J, Temple-Oberle C, Harrop AR. Gender-affirming surgery for transgender individuals: Perceived satisfaction and barriers to care. Plast Surg . 2018;26(4):263-268.
- Puckett JA, Cleary P, Rossman K, Newcomb ME, Mustanski B. Barriers to gender-affirming care for transgender and gender nonconforming individuals. Sex Res Social Policy . 2018;15(1):48-59.
- Lichtenstein M, Stein L, Connolly E, et al. The Mount Sinai patient-centered preoperative criteria meant to optimize outcomes are less of a barrier to care than WPATH SOC 7 criteria before transgender-specific surgery. Transgend Health . 2020;5(3):166-172.
- Streed CG, Davis JA. Improving clinical education and training on sexual and gender minority health. Curr Sex Health Rep . 2018;10:273-280.
- Lone Star Politics
- Politifact Texas
- Austin History
Fact-check: What does the law say about children and sex reassignment surgery?
During an Oct. 31 press conference, leaders from conservative advocacy organizations in Texas urged Gov. Greg Abbott to call a special legislative session to elect a new House speaker.
Earlier that month, embattled House Speaker Dennis Bonnen, R-Lake Jackson, announced that he would not seek reelection to his seat in the House.
The activists also outlined policy proposals that they want lawmakers to address during a special session, proposals they say Republican leaders failed to pursue during the regular session earlier this year.
Cindi Castilla, president of the Dallas Eagle Forum, said lawmakers need to take steps to limit what gender transition treatments are available to children, in light of an ongoing legal battle in Dallas over the gender identity of a 7-year-old.
“During our last session, our legislators decided to pass a law protecting Texans from e-cigarettes until they reach the age of 21,” she said. “They left children able to be sterilized and mutilated at any point in their life. This was a failing, and we need a remedy.
“Texas Eagle Forum asked lawmakers to carry a very common-sense bill that would protect young Texans. That bill would have protected (the child), no matter what the verdict was going to be from the courts.”
Before we dive into this check, it should be noted that medical or surgical treatments used by doctors for transitioning must meet the same safety requirements of other medications or surgeries. To suggest that any child might be mutilated by doctors is inaccurate.
“Children in Texas are already robustly protected by the Texas Family Code and medical rules of ethics,” Brian Klosterboer, an attorney at the American Civil Liberties Union of Texas, said in a statement. “No one in Texas may harm a child, including parents and medical professionals.”
When reached via email, Castilla said that she is unaware of any state laws that “protect children from being given treatments that can lead to sterilization and no law prohibiting surgeries that would seek to make a child appear to be a gender different than the gender they were born.”
“Thus far, it appears very young children have been protected from this only because of the good sense of the medical community,” she said. “As we see this protection waning among a small portion of the medical community we would like to make sure that the most vulnerable Texans are protected.”
Castilla said the bill she mentioned at the press conference would have “protected children from these procedures,” but the group could not find a lawmaker to carry the legislation.
Dallas custody case
The legal battle in Dallas that Castilla mentioned in her remarks is a custody dispute between a mother and father that centers on the gender identity of their 7-year-old child.
The child’s mother says the 7-year-old is a transgender girl and wants to dress as a girl and be identified by female pronouns — a process referred to as a social transition . The child’s father disagrees and insists that the child is a boy.
The case has spurred a national debate about children and their gender identities, with some Texas Republicans pledging to pursue legislation to prevent minors in Texas from transitioning by medical means.
Gillian Branstetter, spokeswoman for the National Center for Transgender Equality, said an important point to consider in this case is the child’s age.
“This child is 7 years old,” she said, noting that “no one is talking about” pursuing a medical or surgical transition. “We’re talking about gender affirming parenting and letting the child explore who they are.”
Looking at the law
Under federal law, transition-related medical care is considered the same as any other medically-necessary care and carries the same requirements when it comes to minors, according to Branstetter and attorneys with ACLU of Texas.
Generally speaking, Texas law dictates that parents have a “duty” to provide medical and dental care to their children and they have the “right” to consent to that care.
But pursuing gender transition treatment is an individualized process for transgender and gender non-binary people and can take many forms, according to multiple resources on gender identity and gender dysphoria.
People with gender dysphoria — when a person feels a conflict between the gender they were assigned at birth and the gender with which they identify — choose to act on this in different ways.
This can include wearing clothes and using pronouns associated with their gender identity; changing their gender and name on legal documents; pursuing hormone treatment or surgical options available for transitioning.
Not every person who has gender dysphoria and is transgender will pursue medical or surgical transition treatment.
People can be diagnosed with gender dysphoria at any age, even as children.
“While some children express feelings and behaviors relating to gender dysphoria at 4 years old or younger, many may not express feelings and behaviors until puberty or much later,” reads an article on the subject from the American Psychiatric Association. “For some children, when they experience puberty, they suddenly find themselves unable to identify with their own body.
Medical treatment standards prioritize affirmation
When it comes to caring for children who might be exhibiting signs of gender dysphoria, the American Academy of Pediatrics recommends the “gender-affirmative care model” that prioritizes validating a child’s gender identity and supporting their exploration and expression of that identity.
“There are absolutely no medical interventions or surgical interventions on any prepubertal child,” said Colt Keo-Meier, a Texas-based psychologist and author who specializes in gender and sexual health. “That is not happening.”
The widely accepted “Standards of Care” maintained by the World Professional Association for Transgender Health also emphasize this point.
“Before any physical interventions are considered for adolescents, extensive exploration of psychological, family, and social issues should be undertaken,” the standards read. “The duration of this exploration may vary considerably depending on the complexity of the situation.”
Once a child starts puberty, other options emerge. Keo-Meier said the most common treatment — medication to delay the onset of puberty — is fully reversible.
“That is literally just hitting pause,” he said.
The World Professional Association for Transgender Health outline minimum criteria that must be met before a child can receive puberty-suppressing medication, including that the child has demonstrated a “long-lasting and intense pattern of gender nonconformity or gender dysphoria” and that it “emerged or worsened with the onset of puberty.”
Other interventions like hormone therapy (partially reversible) or surgery (irreversible) won’t be considered until a patient reaches adolescence.
Even then, the Standards of Care stress that certain procedures should not be performed until a patient is old enough to consent on their own (typically 16-18 years old) and others should occur only once a person has received other treatments for a specific time period.
Castilla said state lawmakers “left children able to be sterilized and mutilated at any point in their life” by failing to adopt a law prohibiting minors from undergoing medical or surgical gender transitions.
Castilla is right that there is no law regulating transition-related treatment separately from other medically-necessary care and the same age regulations apply — minors need parental consent.
Widely accepted guidelines for transition care emphasize gender-affirming care and therapy as primary tools for children. More intensive options, like surgery or hormone treatment, are typically reserved for older adolescents (with parental consent) and adults.
We rate this claim Mostly False.
Austin American-Statesman, Conservative groups call for special legislative session, Oct. 30, 2019 Dallas Morning News, Could transgender kids’ care be next ‘bathroom bill’ for Texas Republicans?, Oct. 25, 2019 Dallas Morning News, Mother in Dallas 7-year-old transgender child custody case calls for judge’s recusal, Nov. 5, 2019 GLAAD, Media Reference Guide — Transgender, accessed Nov. 1, 2019 University of California-San Francisco, Transition Roadmap, accessed Nov. 1, 2019 The World Professional Association for Transgender Health, Standards of Care Version 7, 2012 Texas Health Steps, Teen Consent and Confidentiality, Nov. 7, 2019 Phone interview with Gillian Branstetter, spokesperson for the National Center for Transgender Equality, Nov. 6, 2019 Email interview with Branstetter, Nov. 6, 2019 Centers for Disease Control and Prevention, Transgender Identity and Experiences of Violence Victimization, Substance Use, Suicide Risk, and Sexual Risk Behaviors Among High School Students, Jan. 25, 2019 Endocrine News, Endocrine Society Urges Policy Makers to Follow Science on Transgender Health, October 2019 American Academy of Pediatrics, AAP Policy Statement Urges Support and Care of Transgender and Gender-Diverse CHildren and Adolescents, Sept. 17, 2018 American Academy of Pediatrics, Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents, Oct. 2018 The Arizona Republic, Judges can overrule parents on treatment for transgender children, Arizona Supreme Court rules, April 26, 2019 American Psychiatric Association, What is Gender Dysphoria?, accessed Nov. 1, 2019 U.S. Department of Health and Human Services, Access to Healthcare: Non-discrimination, accessed Nov. 5, 2019 Email interview with Imelda Mejia, spokesperson for the American Civil Liberties Union of Texas, Nov. 7, 2019 Phone interview with Colt Keo-Meier, psychologist who specializes in gender and sexual health, Nov. 7, 2019 Email interview with Keo-Meier, Nov. 9, 2019
States are banning gender-affirming care for minors. What does that mean for patients and providers?
More than 20 u.s. states have banned or severely limited treatment to align a young person’s body with their gender identity. that leaves some doctors caught between breaking the law and providing what they say can be lifesaving medical care..

In this excellent post , my colleague Steven Petrow advised that if you're wondering whether someone you know is transitioning from one gender to the other, it's best to "check your curiosity and hold your tongue." But we all have questions about a subject that is increasingly mainstream. Aside from the recent coverage of Bruce Jenner 's apparent transition , Laverne Cox last year became the first trans person on the cover of Time magazine, and Amazon debuted “Transparent,” a show about a father who is transitioning.
[UPDATE: Bruce Jenner: ‘Call me Caitlyn’ ]
Here are answers to some of the questions surrounding this issue.
How many people are transgender?
The Williams Institute, a think tank at the UCLA School of Law dedicated to research on sexual orientation law and public policy, estimates that 700,000 Americans are transgender . But a good piece last year on fivethirtyeight.com noted that there are no national surveys. And if there were, there is no agreement on what "trangender" means.
How many people have sex reassignment surgery?
It's very difficult to know. The Encyclopedia of Surgery says that "the number of gender reassignment procedures conducted in the United States each year is estimated at between 100 and 500. The number worldwide is estimated to be two to five times larger." At least one other researcher says there are many more. Marci Bowers, a transgender obstetrician and gynecologist in Burlingame, Calif., who performs the surgeries, said in an interview that she does about 200 per year herself, about three quarters of them male to female.
Fred Ettner, a physician in Evanston, Ill., who works with people going through transition, estimated that only about 25 percent to 30 percent of transgender people have any kind of surgery.
How does one begin the process of changing one's sex?
Under the standards of care adopted by the World Professional Association for Transgender Health (WPATH), the first step usually is meeting with a mental health professional for a diagnosis and psychotherapy. A diagnosis of gender identity disorder or gender dysphoria and a letter of recommendation from the therapist allows a person to begin hormone therapy with a doctor. That is usually followed by a period of living publicly as a member of the opposite sex and, finally, surgery to alter the genitalia and other body parts.
What do hormones do?
Androgens are given to women to help them develop secondary male sex characteristics such as a beard and body hair. Estrogen and anti-androgens are given to men to help change their musculature, skin and fat distribution, all of which will make them appear more feminine. Body hair also diminishes.
But Ettner said the hormones' most important contribution is to reduce the dysphoria transgender people have been struggling with all their lives. After a month or two, their bodies and brains begin aligning.
"It's very obvious to the individuals," Ettner said, adding, "Their brain finally is getting this hormone. They feel differently. They behave differently.
"The first effect is the brain effect," he said.
What is the Real-Life Experience (also known as the Real-Life Test)
Surgeons who follow the WPATH standards of care (which some patients and experts consider too strict) usually require candidates for surgery to live for as long as a year in their preferred gender role. They must work or go to school; do volunteer work; change their first names and prove to the surgeon that people other than their therapists know they are successfully living this way.
What happens during surgery?
Male to female genital surgery is easier, less expensive and generally more successful than female to male surgery. That's one reason why fewer women choose to have surgery on their genitals, Bowers said. (Another is cost.)
In male to female surgery , the testicles and most of the penis are removed and the urethra is cut shorter. Some of the skin is used to fashion a largely functional vagina. A "neoclitoris" that allows sensation can be created from parts of the penis. Men retain their prostates.
In female to male surgery, the breasts, uterus and ovaries are removed (in two separate procedures). A "neophallus" can be constructed using tissue from the forearm or other parts of the body that allows sexual sensation, an expensive procedure. Extending the urethra to allow standing urination has proved to be perhaps the most difficult part of the process, Bowers said.
What other kinds of surgery are performed?
Women wishing to live as men often have mastectomies. Men transitioning to women can have plastic surgery to "feminize" their appearance, including work on their eyes, noses, brows, chins and hairlines. They also can have their Adam's apple shaved down so it is less prominent.
Sounds expensive. Is it covered by insurance?
Bowers and Ettner said a woman who chooses the full range of surgical procedures available would spend $75,000 or more to transition to a male. Switching from male to female might cost in the $40,000 to $50,000 range. Some people have the work done in Thailand, which is well known for the surgery and where the cost is much lower.
Insurance is just beginning to cover some of the costs. Last year, Medicare lifted a 33-year ban on coverage for gender reassignment surgery , and the surgery was performed on 74-year-old Army veteran .
Do many people regret having the surgery?
Anecdotal accounts of regret abound, but overall it appears to be rare. Bowers said that only two of the 1,300 people she has operated on have wanted to go back to their old bodies.
But that doesn't mean that surgery is a miracle cure for the difficulties of gender dysphoria. People who make the transition often lose spouses, families, friends and jobs. They may find themselves completely alone if they relocate to start new lives. Johns Hopkins University, which in the 1960s was one of the first medical institutions to perform sex reassignment surgery, halted the practice when officials concluded that it was not helping the transgendered overall.
A 2o11 study of 324 Swedish transsexuals by the Karolinska Institute showed that "after sex reassignment, [they] have considerably higher risks for mortality, suicidal behaviour, and psychiatric morbidity than the general population. Our findings suggest that sex reassignment, although alleviating gender dysphoria, may not suffice as treatment for transsexualism, and should inspire improved psychiatric and somatic care after sex reassignment for this patient group."
The forgotten history of Bruce Jenner
Transgender etiquette 101
Transgender at 7: Tyler gets a legal name change

Gender Confirmation Surgery Is on the Rise in the U.S.

T he number of gender confirmation surgeries has risen in the United States, according to new data from the American Society of Plastic Surgeons (ASPS). The organization reported that in 2016 there were 3,200 gender confirmation surgeries—nearly a 20% increase from 2015.
“In the past, U.S. citizens had to go abroad to get this care,” says report author Dr. Loren Schechter, a board-certified plastic surgeon based in Chicago. “The medical community now recognizes the importance of these procedures and the impact they can have on people’s lives.”
The surgeries tracked in the report include a variety of procedures, including facial conturing and gender reassignment surgeries. This is the first time the organization has reported these surgeries.
Access to transgender-related surgeries has increased in recent years. The Affordable Care Act (ACA) included inclusive language about the treatment of gender-nonconforming people in the medical setting and prohibited a person’s gender identity from being classified as a pre-existing condition . Under ACA, insurance companies cannot discriminate based on a person’s gender. In 2014, Medicare removed a decades-long ban on coverage for gender reassignment surgery.
“Two decades ago, it was difficult to find a hospital that would allow us to do these surgeries,” says Schechter. “I think education is critical. We need to make people in society aware that this is a community that has needs that need to be serviced.”
Since the ASPS has only recently started tracking these surgeries, the group cannot say precisely how much they have risen, but anecdotally, Schechter calls the rise “dramatic”. “There is no question there has been an increase,” he says, which he attributes both to increased access to these surgeries and greater education about the surgeries among the medical community and the public.
Whether that increase in surgeries will continue remains unknown, Schechter says. Doctors may actually be doing fewer in the future, since more young people may begin taking medication that can suppress puberty, which could cut down on the need for some surgeries.
More Must-Reads from TIME
- How Joe Biden Leads
- Lai Ching-te Is Standing His Ground
- Do Less. It’s Good for You
- There's Something Different About Will Smith
- What Animal Studies Are Revealing About Their Minds—and Ours
- What a Hospice Nurse Wants You to Know About Death
- 15 LGBTQ+ Books to Read for Pride
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
- New Hampshire
- North Carolina
- Pennsylvania
- West Virginia
- Online hoaxes
- Coronavirus
- Health Care
- Immigration
- Environment
- Foreign Policy
- Kamala Harris
- Donald Trump
- Mitch McConnell
- Hakeem Jeffries
- Ron DeSantis
- Tucker Carlson
- Sean Hannity
- Rachel Maddow
- PolitiFact Videos
- 2024 Elections
- Mostly True
- Mostly False
- Pants on Fire
- Biden Promise Tracker
- Trump-O-Meter
- Latest Promises
- Our Process
- Who pays for PolitiFact?
- Advertise with Us
- Suggest a Fact-check
- Corrections and Updates
- Newsletters
Stand up for the facts!
Our only agenda is to publish the truth so you can be an informed participant in democracy. We need your help.
I would like to contribute

- Public Health
- Cindi Castilla
Cindi Castilla, president of the Dallas Eagle Forum, listens to U.S. Sen. Ted Cruz, R-Texas, speak in Austin in August 2018 (Stephen Spillman / for American-Statesman).

What does the law say about children and sex reassignment surgery?
During an Oct. 31 press conference, leaders from conservative advocacy organizations in Texas urged Gov. Greg Abbott to call a special legislative session to elect a new House speaker.
Earlier that month, embattled House Speaker Dennis Bonnen announced that he would not seek re-election to his seat in the House.
The activists also outlined policy proposals that they want lawmakers to address during a special session, proposals they say Republican leaders failed to pursue during the regular session earlier this year.
Cindi Castilla, president of the Dallas Eagle Forum, said lawmakers need to take steps to limit what gender transition treatments are available to children, in light of an ongoing legal battle in Dallas over the gender identity of a 7-year-old.
"During our last session, our legislators decided to pass a law protecting Texans from e-cigarettes until they reach the age of 21," she said. "They left children able to be sterilized and mutilated at any point in their life. This was a failing, and we need a remedy.
"Texas Eagle Forum asked lawmakers to carry a very common-sense bill that would protect young Texans. That bill would have protected (the child), no matter what the verdict was going to be from the courts."
Before we dive into this check, it should be noted that medical or surgical treatments used by doctors for transitioning must meet the same safety requirements of other medications or surgeries. To suggest that any child might be mutilated by doctors is inaccurate.
"Children in Texas are already robustly protected by the Texas Family Code and medical rules of ethics," said Brian Klosterboer, an attorney at the American Civil Liberties Union of Texas, in a statement. "No one in Texas may harm a child, including parents and medical professionals."
When reached via email, Castilla said that she is unaware of any state laws that "protect children from being given treatments that can lead to sterilization and no law prohibiting surgeries that would seek to make a child appear to be a gender different than the gender they were born."
"Thus far, it appears very young children have been protected from this only because of the good sense of the medical community," she said. "As we see this protection waning among a small portion of the medical community we would like to make sure that the most vulnerable Texans are protected."
Castilla said the bill she mentioned at the press conference would have "protected children from these procedures," but the group could not find a lawmaker to carry the legislation.
Dallas custody case
The legal battle in Dallas that Castilla mentioned in her remarks is a custody dispute between a mother and father that centers on the gender identity of their 7-year-old child.
The child’s mother says the 7-year-old is a transgender girl and wants to dress as a girl and be identified by female pronouns — a process referred to as a social transition . The child’s father disagrees and insists that the child is a boy.
The case has spurred a national debate about children and their gender identities, with some Texas Republicans pledging to pursue legislation to prevent minors in Texas from transitioning by medical means.
Gillian Branstetter, spokeswoman for the National Center for Transgender Equality, said an important point to consider in this case is the child’s age.
"This child is 7 years old," she said, noting that "no one is talking about" pursuing a medical or surgical transition. "We’re talking about gender affirming parenting and letting the child explore who they are."
Looking at the law
Under federal law, transition-related medical care is considered the same as any other medically-necessary care and carries the same requirements when it comes to minors, according to Branstetter and attorneys with ACLU of Texas.
Featured Fact-check

Generally speaking , Texas law dictates that parents have a "duty" to provide medical and dental care to their children and they have the "right" to consent to that care.
But pursuing gender transition treatment is an individualized process for transgender and gender non-binary people and can take many forms, according to multiple resources on gender identity and gender dysphoria.
People with gender dysphoria — when a person feels a conflict between the gender they were assigned at birth and the gender with which they identify — choose to act on this in different ways.
This can include wearing clothes and using pronouns associated with their gender identity; changing their gender and name on legal documents; pursuing hormone treatment or surgical options available for transitioning.
Not every person who has gender dysphoria and is transgender will pursue medical or surgical transition treatment.
People can be diagnosed with gender dysphoria at any age, even as children.
"While some children express feelings and behaviors relating to gender dysphoria at 4 years old or younger, many may not express feelings and behaviors until puberty or much later," reads an article on the subject from the American Psychiatric Association. "For some children, when they experience puberty, they suddenly find themselves unable to identify with their own body.
Medical treatment standards prioritize affirmation
When it comes to caring for children who might be exhibiting signs of gender dysphoria, the American Academy of Pediatrics recommends the "gender-affirmative care model" that prioritizes validating a child’s gender identity and supporting their exploration and expression of that identity.
"There are absolutely no medical interventions or surgical interventions on any prepubertal child," said Colt Keo-Meier, a Texas-based psychologist and author who specializes in gender and sexual health. "That is not happening."
The widely accepted "Standards of Care" maintained by the World Professional Association for Transgender Health also emphasize this point.
"Before any physical interventions are considered for adolescents, extensive exploration of psychological, family, and social issues should be undertaken," the standards read. "The duration of this exploration may vary considerably depending on the complexity of the situation."
Once a child starts puberty, other options emerge. Keo-Meier said the most common treatment — medication to delay the onset of puberty — is fully reversible.
"That is literally just hitting pause," he said.
The World Professional Association for Transgender Health outline minimum criteria that must be met before a child can receive puberty-suppressing medication, including that the child has demonstrated a "long-lasting and intense pattern of gender nonconformity or gender dysphoria" and that it "emerged or worsened with the onset of puberty."
Other, interventions like hormone therapy (partially reversible) or surgery (irreversible) won’t be considered until a patient reaches adolescence.
Even then, the Standards of Care stress that certain procedures should not be performed until a patient is old enough to consent on their own (typically 16-18 years old) and others should occur only once a person has received other treatments for a specific time period.
Castilla said state lawmakers "left children able to be sterilized and mutilated at any point in their life" by failing to adopt a law prohibiting minors from undergoing medical or surgical gender transitions.
Castilla is right that there is no law regulating transition-related treatment separately from other medically-necessary care and the same age regulations apply — minors need parental consent.
Widely accepted guidelines for transition care emphasize gender-affirming care and therapy as primary tools for children. More intensive options, like surgery or hormone treatment, are typically reserved for older adolescents (with parental consent) and adults.
We rate this claim Mostly False.
Read About Our Process
The Principles of the Truth-O-Meter
Our Sources
Austin American-Statesman, Conservative groups call for special legislative session , Oct. 30, 2019
Dallas Morning News, Could transgender kids’ care be next ‘bathroom bill’ for Texas Republicans? , Oct. 25, 2019
Dallas Morning News, Mother in Dallas 7-year-old transgender child custody case calls for judge’s recusal, Nov. 5, 2019
GLAAD, Media Reference Guide — Transgender , accessed Nov. 1, 2019
University of California-San Francisco, Transition Roadmap , accessed Nov. 1, 2019
The World Professional Association for Transgender Health, Standards of Care Version 7 , 2012
Texas Health Steps, Teen Consent and Confidentiality , Nov. 7, 2019
Phone interview with Gillian Branstetter, spokesperson for the National Center for Transgender Equality, Nov. 6, 2019
Email interview with Branstetter, Nov. 6, 2019
Centers for Disease Control and Prevention, Transgender Identity and Experiences of Violence Victimization, Substance Use, Suicide Risk, and Sexual Risk Behaviors Among High School Students, Jan. 25, 2019
Endocrine News, Endocrine Society Urges Policy Makers to Follow Science on Transgender Health , October 2019
American Academy of Pediatrics, AAP Policy Statement Urges Support and Care of Transgender and Gender-Diverse CHildren and Adolescents , Sept. 17, 2018
American Academy of Pediatrics, Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents , Oct. 2018
The Arizona Republic, Judges can overrule parents on treatment for transgender children, Arizona Supreme Court rules , April 26, 2019
American Psychiatric Association, What is Gender Dysphoria? , accessed Nov. 1, 2019
U.S. Department of Health and Human Services, Access to Healthcare: Non-discrimination, accessed Nov. 4, 2019
Browse the Truth-O-Meter
More by madlin mekelburg.

Support independent fact-checking. Become a member!
- My View My View
- Following Following
- Saved Saved
US judge strikes down Florida ban on gender-affirming healthcare
- Medium Text

Sign up here.
Reporting by Jonathan Allen in New York; Editing by Bill Berkrot
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab
Read Next / Editor's Picks

Industry Insight Chevron

David Thomas
Mike Scarcella, David Thomas

Karen Sloan

Henry Engler
- Share full article
For more audio journalism and storytelling, download New York Times Audio , a new iOS app available for news subscribers.

- Apple Podcasts
- Google Podcasts
Real Teenagers, Fake Nudes: The Rise of Deepfakes in American Schools
Students are using artificial intelligence to create sexually explicit images of their classmates..

Hosted by Sabrina Tavernise
Featuring Natasha Singer
Produced by Sydney Harper and Shannon M. Lin
Edited by Marc Georges
Original music by Marion Lozano , Elisheba Ittoop and Dan Powell
Engineered by Chris Wood
Listen and follow The Daily Apple Podcasts | Spotify | Amazon Music | YouTube
Warning: this episode contains strong language, descriptions of explicit content and sexual harassment
A disturbing new problem is sweeping American schools: Students are using artificial intelligence to create sexually explicit images of their classmates and then share them without the person depicted even knowing.
Natasha Singer, who covers technology, business and society for The Times, discusses the rise of deepfake nudes and one girl’s fight to stop them.
On today’s episode
Natasha Singer , a reporter covering technology, business and society for The New York Times.

Background reading
Using artificial intelligence, middle and high school students have fabricated explicit images of female classmates and shared the doctored pictures.
Spurred by teenage girls, states have moved to ban deepfake nudes .
There are a lot of ways to listen to The Daily. Here’s how.
We aim to make transcripts available the next workday after an episode’s publication. You can find them at the top of the page.
The Daily is made by Rachel Quester, Lynsea Garrison, Clare Toeniskoetter, Paige Cowett, Michael Simon Johnson, Brad Fisher, Chris Wood, Jessica Cheung, Stella Tan, Alexandra Leigh Young, Lisa Chow, Eric Krupke, Marc Georges, Luke Vander Ploeg, M.J. Davis Lin, Dan Powell, Sydney Harper, Mike Benoist, Liz O. Baylen, Asthaa Chaturvedi, Rachelle Bonja, Diana Nguyen, Marion Lozano, Corey Schreppel, Rob Szypko, Elisheba Ittoop, Mooj Zadie, Patricia Willens, Rowan Niemisto, Jody Becker, Rikki Novetsky, John Ketchum, Nina Feldman, Will Reid, Carlos Prieto, Ben Calhoun, Susan Lee, Lexie Diao, Mary Wilson, Alex Stern, Sophia Lanman, Shannon Lin, Diane Wong, Devon Taylor, Alyssa Moxley, Summer Thomad, Olivia Natt, Daniel Ramirez and Brendan Klinkenberg.
Our theme music is by Jim Brunberg and Ben Landsverk of Wonderly. Special thanks to Sam Dolnick, Paula Szuchman, Lisa Tobin, Larissa Anderson, Julia Simon, Sofia Milan, Mahima Chablani, Elizabeth Davis-Moorer, Jeffrey Miranda, Maddy Masiello, Isabella Anderson, Nina Lassam and Nick Pitman.
Natasha Singer writes about technology, business and society. She is currently reporting on the far-reaching ways that tech companies and their tools are reshaping public schools, higher education and job opportunities. More about Natasha Singer
Advertisement

IMAGES
VIDEO
COMMENTS
e. The legal and regulatory history of transgender and transsexual people in the United States begins in the 1960s. Such legislation covers federal, state, municipal, and local levels, as well as military justice. It reflects broader societal attitudes which have shifted significantly over time and have impacted legislative and judicial outcomes.
care has a long history in the US - and not just for transgender people. In 1976, a woman from Roanoke, Virginia, named Rhoda received a prescription for two drugs: estrogen and progestin ...
The legal status of gender-affirming surgery and gender-affirming hormone therapy varies by jurisdiction, often interacting with other facets of the legal status of transgender people.Key considerations include whether people are allowed to get such surgeries, at what ages they are allowed to if so, and whether surgeries are required in order for a gender transition to be legally recognized.
In the United States, the rights of transgender people vary considerably by jurisdiction. In recent decades, there has been an expansion of federal, state, and local laws and rulings to protect transgender Americans; however, many rights remain unprotected, and some rights are being eroded. Since 2020, there has been a national movement by ...
Jorgensen became a public figure advocating for transgender rights and promoting awareness about gender-affirming surgery after their case received significant media attention. Other medical centres in Europe and the United States began conducting gender-affirming surgeries around the same time, including the Johns Hopkins Gender Identity ...
Nicolas AsfouriAFP/Getty Images. N early 60 years ago, Johns Hopkins Hospital opened a first-of-its-kind clinic to provide gender-affirming surgery. The Gender Identity Clinic blazed a new trail ...
The Associated Press. Some important events in the history of transgender rights in the United States: 1952: Christine Jorgensen completes sex-reassignment surgery in Denmark; she was the first ...
In the common law world, both the medical and legal professions initially considered gender reassignment surgery to be unlawful when first practised and discussed in the first half of the twentieth century. While most medical procedures are covered by the medical exception to the law governing serious offences against the person, many doctors ...
This is the first study that highlights the role of the Gender Identity Clinic in establishing gender affirmation surgery and reveals the reasons of its closure. Ann Plast Surg . 2019 Aug;83(2):132-136. doi: 10.1097/SAP.0000000000001684.
The most recent, large-scale survey of transgender adults in the United States found that 81.7 percent of respondents had seriously considered suicide in their lifetimes, and the surveyed population had a past-year prevalence of suicide attempts 18 times higher than the general US population. In addition, the study identified unique risk ...
The law will take effect September 1, 2023, and prohibits access to hormone treatments and puberty blockers for those under 18. Two other bills have been introduced in the Texas legislature regarding gender-affirming care. HB42 would criminalize gender-affirming care for minors by defining it as child abuse.
The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020.
Siotos C, Neira PM, Lau BD, et al. Origins of gender affirmation surgery: The history of the first gender identity clinic in the United States at Johns Hopkins. Ann Plast Surg. 2019;83(2):132-136. Baptists vote to ban sex change operations. Sarasota Herald-Tribune. October 15, 1977. Nutt AE.
Republican Gov. Jim Pillen signed into law on May 22, 2023, a bill that limits gender-affirming medical care for minors, which covers people under the age of 19 in Nebraska. The law, which also ...
The first physician to perform sex reassignment surgery in the United States was Los Angeles-based urologist Elmer Belt, who quietly performed operations from the early 1950s until 1968. [citation needed] In 1966, Johns Hopkins University opened the first sex reassignment surgery clinic in America. The Hopkins Gender Identity Clinic was made up ...
Credit Brandon Thibodeaux for The New York Times. Oct. 17, 2010. First Openly Transgender Judge. Phyllis R. Frye, a lawyer since 1981, was sworn in as a judge in Houston, becoming the nation's ...
The legal battle in Dallas that Castilla mentioned in her remarks is a custody dispute between a mother and father that centers on the gender identity of their 7-year-old child.
It was not until 1952 that gender affirmation surgery would become internationally recognized following the well-publicized sex reassignment surgery of World War II American veteran Christine Jorgensen, previously known as George Jorgensen Jr, in Denmark. 3 Following this event, gender affirmation surgery demand spiked in Denmark, with ...
Across the United States, 23 states have adopted laws or policies that ban or severely limit gender-affirming care (GAC) for minors, and several others are eyeing the possibility. Experts estimate that the efforts could ultimately affect more than 144,000 young people .
It's very difficult to know. The Encyclopedia of Surgery says that "the number of gender reassignment procedures conducted in the United States each year is estimated at between 100 and 500. The ...
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
May 22, 2017 9:43 AM EDT. T he number of gender confirmation surgeries has risen in the United States, according to new data from the American Society of Plastic Surgeons (ASPS). The organization ...
stated on April 21, 2024 in a post on X. By Louis Jacobson • April 23, 2024. Generally speaking, Texas law dictates that parents have a "duty" to provide medical and dental care to their ...
A person holds up a flag during rally to protest the Trump administration's reported transgender proposal to narrow the definition of gender to male or female at birth, at City Hall in New York ...
Reporting from Miami. June 11, 2024. Key parts of a Florida law that bans gender transition care for minors and imposes hurdles on adults seeking such care are unconstitutional, a federal judge ...
Russian lawmakers vote to ban gender reassignment surgery 06/14/2023 June 14, 2023. A new bill prohibiting gender reassignment has passed its first reading in the Russian lower house.
Real Teenagers, Fake Nudes: The Rise of Deepfakes in American Schools Students are using artificial intelligence to create sexually explicit images of their classmates.