- Share full article
Advertisement
Supported by

Racial Inequities Persist in Health Care Despite Expanded Insurance
A series of studies in an influential medical journal takes a close look at longstanding gaps in medical care.

By Roni Caryn Rabin
Two decades ago, only 9 percent of white Americans rated their health as fair or poor. But 14 percent of Hispanic Americans characterized their health in those terms, as did nearly 18 percent of Black Americans.
In recent years, access to care has improved in the wake of the Affordable Care Act, which reduced the number of uninsured Americans across all racial and ethnic groups. But the racial health gap has remained , according to a series of studies published on Tuesday in the journal JAMA.
A dismal picture of persistent health disparities in America was described in an issue devoted entirely to inequities in medicine. The wide-ranging issue included research on spending and patterns of care, comparative rates of gestational diabetes and the proportion of Black physicians at medical schools.
The journal’s editors committed to a sharper focus on racism in medicine after a controversy in June, in which a staff member seemed to suggest that racism was not a problem in health care. The ensuing criticism led to the resignation of the top editor and culminated with a pledge to increase staff diversity and publish a more inclusive array of papers.
“The topics of racial and ethnic disparities and inequities in medicine and health care are of critical importance,” Dr. Phil B. Fontanarosa, interim editor in chief of JAMA, said in a statement. He noted that more than 850 articles on racial and ethnic disparities and inequities have been published in JAMA and associated journals in the past five years.
The new issue offers studies on disparities in the utilization of health care services and in overall health spending. Together, the findings paint a portrait of a nation still plagued by medical haves and have-nots whose ability to benefit from scientific advances varies by race and ethnicity, despite the fact that the A.C.A. greatly expanded insurance.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Glob Health Action
Inequalities in health: definitions, concepts, and theories
Mariana c. arcaya.
1 Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, University in Boston, MA, USA
Alyssa L. Arcaya
2 Region 2, United States Environmental Protection Agency, New York, NY, USA
S. V. Subramanian
Individuals from different backgrounds, social groups, and countries enjoy different levels of health. This article defines and distinguishes between unavoidable health inequalities and unjust and preventable health inequities. We describe the dimensions along which health inequalities are commonly examined, including across the global population, between countries or states, and within geographies, by socially relevant groupings such as race/ethnicity, gender, education, caste, income, occupation, and more. Different theories attempt to explain group-level differences in health, including psychosocial, material deprivation, health behavior, environmental, and selection explanations. Concepts of relative versus absolute; dose–response versus threshold; composition versus context; place versus space; the life course perspective on health; causal pathways to health; conditional health effects; and group-level versus individual differences are vital in understanding health inequalities. We close by reflecting on what conditions make health inequalities unjust, and to consider the merits of policies that prioritize the elimination of health disparities versus those that focus on raising the overall standard of health in a population.
Policymakers, researchers, and public health practitioners have long sought not only to improve overall population health but also to reduce or eliminate differences in health based on geography, race/ethnicity, socioeconomic status (SES), and other social factors (e.g. 1 , 2 ). This paper aims to create a centralized resource for understanding methodological, theoretical, and philosophical aspects of health inequalities research in order to help advance health inequalities research. It synthesizes and expands upon previously published work that addresses concepts relevant to the study of health inequalities and inequities ( 3 – 7 ). The article begins by clarifying vocabulary needed to describe differences in health, whether they are observed across places and social groups, or among individuals in a single population. Next, it introduces key concepts for gathering and interpreting information on health inequalities. It considers the ways in which researchers and policymakers explore health inequalities, including by social groups, or by geographic area. The article then provides an overview of theories commonly employed to explain health differences. Finally, we conclude by considering ethical questions raised by health disparities and questions policymakers might consider when structuring programs and policies to address health disparities.
Motivation for studying health inequalities
Despite considerable attention to the problem of health inequalities since the 1980s ( 8 ), striking differences in health still exist among and within countries today ( 9 ). In 2010, for example, Haitian men had a healthy life expectancy ( 10 ) of 27.8 years, while men in Japan could expect 70.6 years, over twice as long, in full health ( 11 ). Social group differences within countries are also often substantial. In India, for example, individuals from the poorest quintile of families are 86% more likely to die than are those from the wealthiest fifth of families, even after accounting for the influence of age, gender, and other factors likely to influence the risk of death ( 12 ). When health differences such as these are observed, a primary question of interest is whether the inequality in question is also inequitable.
Health inequalities versus health inequities
The term health inequality generically refers to differences in the health of individuals or groups ( 3 ). Any measurable aspect of health that varies across individuals or according to socially relevant groupings can be called a health inequality. Absent from the definition of health inequality is any moral judgment on whether observed differences are fair or just.
In contrast, a health inequity , or health disparity, is a specific type of health inequality that denotes an unjust difference in health. By one common definition, when health differences are preventable and unnecessary, allowing them to persist is unjust ( 13 ). In this sense, health inequities are systematic differences in health that could be avoided by reasonable means ( 14 ). In general, social group differences in health, such as those based on race or religion, are considered health inequities because they reflect an unfair distribution of health risks and resources ( 3 ). The key distinction between the terms inequality and inequity is that the former is simply a dimensional description employed whenever quantities are unequal, while the latter requires passing a moral judgment that the inequality is wrong.
The term health inequality can describe racial/ethnic disparities in US infant mortality rates, which are nearly three times higher for non-Hispanic blacks versus whites ( 15 ), as well as the fact that people in their 20s enjoy better health than those in their 60s ( 3 ). Of these two examples, only the difference in infant mortality would also be considered a health inequity. Health differences between those in their 20s versus 60s can be considered health inequalities but not health inequities. Health differences based on age are largely unavoidable, and it is difficult to argue that the health differences between younger and older people are unjust, since older people were once younger people and younger people, with some luck, will someday become old.
On the other hand, differences in infant mortality rates among racial/ethnic groups in the United States are partially attributable to preventable differences in education and access to health and prenatal care ( 15 ). Unlike the example of age-related health differences, disparities in health outcomes across racial/ethnic groups could be aggressively prevented. Policies and programs that improve access to health and prenatal care for underserved US racial/ethnic groups, for example, could reduce unjust differences in infant health outcomes.
While the existence of health disparities is a near universal problem, the extent to which social factors matter for health has been shown to vary by country. For example, a comparative study of 22 European nations showed that differences in mortality among those with the least versus the most education varied substantially across counties. For example, the authors found less than a twofold difference in mortality between those of high and low education in Spain, and more than a fourfold difference between the two education groups in the Czech Republic ( 16 ). Recent evidence suggests that socially patterned health disparities may be widening ( 17 – 19 ), calling for consistent attention to the issues of health inequalities.
There are compelling reasons to worry about, and address, such health differences. The persistence of health differences based on nationality, race/ethnicity, or other social factors raises moral concerns, offending many people's basic notion of fairness and justice ( 13 , 20 ). Although myriad resources and outcomes are unevenly distributed across nations and social groups, health differences can be viewed as particularly objectionable from a human rights perspective ( 21 , 22 ). The concept of health as a human right was enshrined in the United Nations General Assembly's Universal Declaration of Human Rights in 1948 ( 23 ) and has since been reflected in national constitutions, treaties and domestic laws, policies, and programs in countries around the world ( 22 ), emphasizing the unique value societies place on health. Increasingly, health equity itself is also valued. For example, the World Health Organization recognizes health equity as a priority, reflected in part by its formation of the Commission on Social Determinants of Health in 2005. This commission gathers and synthesizes global evidence on social determinants of health and recommends actions that address health inequities ( 24 ). Similarly, the United Nations (UN) has also placed an explicit value on equity. The UN's Millennium Development Goals (MDGs), which expire at the end of 2015, have focused on average-based targets that obscure inequalities. In the post-MDG era, the UN has included equity in its post-2015 sustainable development agenda. One of the six ‘essential elements’ that form the core of the post-2015 negotiations focuses on fighting inequality, in part by addressing gender-related health disparities and inequitable access to health care ( 25 ).
From a strictly utilitarian standpoint, the cost of health inequalities is staggering. Between 2003 and 2006 alone, the direct economic cost of health inequalities based on race or ethnicity in the United States was estimated at $230 billion. Researchers calculated that medical costs faced by African Americans, Asian Americans, and Hispanics were in excess by 30% due to racial and ethnic health inequalities, including premature death and preventable illnesses which reduced worker productivity. When indirect costs were factored into the calculations, the economic burden was estimated as $1.24 trillion ( 26 ). In addition to the costs that could be avoided if socially disadvantaged groups enjoyed equitable health outcomes, inequality itself may be harmful to health. A review of 155 papers that explored income inequality and population health found that health tends to be poorer in less equal societies, especially when inequality is measured at large geographic scales ( 27 ).
Whether motivated by economic or moral considerations, the study of, and fight against, health inequalities requires a familiarity with relevant definitions, concepts, and theories of health differences.
Concepts for operationalizing the study of health inequality
Group-level differences versus overall health distribution.
There are two main approaches to studying inequalities within and between populations. Most commonly, we examine differences in health outcomes at the group level to understand social inequalities in health. For example, we might ask how mean body mass index (BMI) of the poor compares to that of the rich. Because recognizing social group differences in health is necessary for targeting investments to the worst off groups, a group-level approach can support the creation of laws and programs that seek to eliminate social group differences. Because social inequities in health are shaped by unfair distributions of the social determinants of health, tracking social group differences in health is important for monitoring the state of equity in a society. The World Health Organization, for example, recommends that health indicators be reported by groups, or ‘equity stratifiers’ for the purposes of monitoring health inequities ( 5 ). Also, focusing on social groups allows us to understand current health inequalities in a historical and cultural context, which provides insights into how health differences may have arisen. For example, considering the history of slavery and segregation in the United States sheds light on current racial/ethnic health disparities. Similarly, understanding the political and religious history of the caste system in India helps us understand how it affects social status, occupation, education levels, and health outcomes for individuals today. In short, viewing health disparities through the lens of social groups can help guide interventions, enable surveillance of important equity issues, and advance our understanding of health by helping us make connections that may have not been initially obvious ( 3 , 6 ).
Alternatively, it is possible to focus on health differences across individuals, for example, describing the range or variance of a given measure across an entire population. This method is agnostic to social groupings, effectively collapsing all people into one distribution ( 8 ). Researchers studying global income inequality have used this approach to highlight the relative wealth of poor individuals in rich countries compared to well-off individuals in poor countries, for example, ( 28 ). In contrast to focusing on how people from similar backgrounds compare to one another, exploring the income distribution across one global population has yielded important insights into just how unequally resources are currently distributed, as well as what factors drive these differences.
It can also be useful to compare outcomes across individuals within a single country. For example, applying this approach to the study of inequalities in BMI in India might yield data on the difference in BMI from the fattest to thinnest person. While examining inequalities across individuals provides important information on how outcomes are distributed, it does not allow us to understand who fares better or worse, and whether the gap between the healthy and sick is preventable or unjust. Despite this limitation, some researchers have argued that considering the overall health distribution of a population is especially useful for comparing health in different places because social groups are defined differently, and carry different meanings, across the world ( 8 ). For example, race is defined differently in the United States than it is in other countries, while social grouping according to caste is relevant for just a handful of countries, including India, Nepal, Pakistan, and Sri Lanka. Considering the overall health distribution of a population may also avoid making incorrect assumptions about what social groupings matter in a particular place. Despite the challenges associated with measuring and interpreting social inequalities in health, the remainder of this article focuses on health inequalities across social groups rather than individuals.
A critical step in examining group-level health inequalities is defining the relevant social groups themselves. The World Health Organization highlights place of residence, race/ethnicity, occupation, gender, religion, education, SES, and social capital or resources as particularly relevant stratifiers that can be used to define social groups ( 5 ). Below we introduce considerations for studying health inequalities that operate across social groups. This section is followed by a discussion on exploring social group differences in health within geographies. With cross-country comparisons of health outcomes regularly reported by international bodies such as the World Health Organization (e.g. 10 ) and growing interest in within country analyses (e.g. 29 ), understanding how to approach geographic health inequalities is fundamental for researchers and practitioners.
Social group health inequalities: defining groups
Health disparities along racial, ethnic, and socioeconomic lines are observed in both low- and high-income countries, and may be widening ( 9 ), underscoring the importance of studying of group-level health differences. Understanding socially patterned health disparities requires constructing meaningful groups of individuals. Each society has its own unique ways of stratifying and dividing people into social groups. In Australia, the distinction between white Australians and aboriginal people is meaningful, while in India, caste is important. Race/ethnicity is a particularly meaningful distinction in the United States, while the level of schooling achieved contributes to social divisions in the United Kingdom. We discuss considerations for constructing and interpreting measures of social group health inequalities below.
Researchers and consumers of information on health differences should carefully consider how social groups are constructed, as health inequality data can only be interpreted with respect to group composition. Some social groupings are based on categories of membership, as is in the case with religion or race, while others are created according to ordered or continuous levels of a given variable, such as education or income. Clearly defined membership categories grounded in theory and backed by a priori contextual knowledge can facilitate the study of health inequalities, though researchers will have to make decisions about when to collapse or further differentiate groups. For example, should Catholics and Protestants be broadly categorized under the umbrella Christian, or are denominational differences important? Is it meaningful to compare non-Hispanic whites to minorities in general, or does each racial/ethnic group require its own category? Increasingly complex considerations, including, for example, how race and ethnicity are defined, differentiated, and conceptualized ( 30 , 31 ), add to the challenge of meaningfully comparing social groups. Such questions can only be answered with respect to the specific hypotheses being tested, or the disparities monitored, and should be grounded in context and theory. In general, however, it is important to be aware that group construction will drive the interpretation of health inequality data.
Alternatively, health differences can be patterned with respect to an ordered or continuous quantity such as education or income. Two key questions should be considered in these cases. First, do we believe that health outcomes hinge on meeting some benchmark with regard to the social resource (i.e. a threshold model), or do we predict a social gradient in health that exhibits more of a dose–response relationship? Secondly, do we believe that an individual's response to the social variable depends only on his own level of that variable, or does it matter where he ranks with respect to others?
A ‘social gradient’ in health ( 32 , 33 ) exists where increasing quantities of social resources such as education, social class, or income correspond with increasing levels of health in a dose–response relationship (see Table 1 for examples). As an example, consider education, which is well known to positively impact health ( 35 ). The relationship between education and health is such that even at very high and low ends of the education distribution, additional years of school correspond with marginally better health. If instead of a functioning as social gradient, education had a threshold effect on health, we might observe that not having a secondary school education was associated with worse health but that education and health were not linked for those who had completed secondary school or a higher degree. For example, under this threshold model, we would not expect those with a graduate school education to be healthier than those with a college education. Policy responses to dose–response versus threshold effects of social resources would be quite distinct, and so researchers should be sure to differentiate between the two. Whether a dose–response curve or threshold effect better represents the relationship, studying effects at high and low levels of education is critical. Plotting the relationship between health and education, with education on the x-axis and health on the y-axis, for example, would reveal the shape of a curve describing how additional schooling impacts health. That shape describes how health responds to schooling across the educational spectrum, including whether a threshold exists beyond which education impacts health very little, and the extent to which additional school matters for high and low education individuals.
Indicators of socioeconomic position used in health research measured at the individual level
| Education | Usually used as categorical measuring the levels achieved; also as a continuous variable measuring the total number of years of education |
| Income | Indicator that, jointly with wealth, directly measures the material resources component of SEP. Usually measured as household gross income per number of persons dependable on this income |
| Wealth | Includes income and all accumulated material resources |
| Occupation-based indicators | |
| The Registrar General's Social Classes | Groupings of occupation based on prestige in six hierarchical groups: I (highest), II, III non-manual, III-manual, IV, V (lowest). Often regrouped as manual versus non-manual |
| Erikson and Goldthorpe Class Schema | Groupings of occupations based on specific characteristics of employment relations such as type of contractual agreement, independence of work, authority delegation, etc. Not a hierarchical classification |
| UK National Statistics Socio-Economic Classification | Based on the same principles as the Erikson and Goldthorpe scheme. Creates non-hierarchical groups |
| Wright's Social Class Scheme | Based on Marxist principle of relation to the means of production. Not a hierarchical classification |
| Cambridge Social Interaction and Stratification scale | Based on patterns of social interaction in relation to occupational groups |
| Occupational-based census classification | For example, US census classification, country-specific socioeconomic classifications |
| Other indicators | |
| Unemployment | Lack of employment |
| Housing | Housing tenure, household amenities, housing characteristics, broken window index, social standing of the habitat |
| Overcrowding | Calculated as the number of persons living in the household per number of rooms available in the house (usually excluding kitchen and bathrooms) |
| Composite indicators | At individual (usually measured as a score that adds up the presence or absence of several SEP indicators) or at area level |
| Proxy indicators | These are not strictly indicators of SEP but they can be strongly correlated with SEP and when more appropriate information is not available they may be useful in describing social patterning. Some cases may provide insight into the mechanism that explains the underlying association of SEP and a particular health outcome. However, they may be associated with the health outcome through independent mechanisms not related to their correlation with SEP |
Source: Taken directly from Galobardes et al. ( 34 ).
Absolute versus relative social position
The second, related question deals with whether absolute or relative ( 36 ) position matters for health. This is particularly important when considering poverty, which can be defined in an absolute sense by comparing a given income to a static benchmark, or in a relative sense by comparing a given income to the overall distribution of incomes in a population ( 37 ). Absolute poverty definitions rely on a fixed monetary threshold called a poverty line, though this threshold in generally specific to year, country, and household size. Those with incomes falling below the threshold are considered impoverished. On the other hand, relative poverty is defined by comparing a given income to the distribution of income in a population. For example, those earning less than 30% of the national per capita income might be considered relatively impoverished, meaning that the poverty definition changes as average income increases. Among other distinctions between the two ways of defining poverty, it is important to note that a relative poverty definition may classify a greater proportion of a population as impoverished, especially in countries with high levels of income inequality ( 3 ).
Notions of absolute versus relative poverty highlight that measures of income can be both objective and subjective. The amount of money in one's bank account is an objective measure of wealth. Whether someone feels wealthy or poor in relation to his neighbors is a subjective measure of wealth. Absolute poverty, which is an objective measure of wealth, is a useful measure for testing the absolute income hypothesis , which posits that an individual's health depends only on his own income and not on what others in a population earn ( 3 ). By this logic, the health of an individual whose income stays constant should remain unchanged as those around him become wealthier. Similarly, it would predict that earning $50,000 per year had the same effect on health regardless of whether one's neighbors earned an average of $30,000 or $1 million annually. The absolute income hypothesis ignores the fact that as society becomes wealthier, the material goods needed to fully participate in society can change. Goods such as cars, phones, and computers are now more important than ever to accomplish tasks such as getting to work or accessing health care. As a result, those with static incomes in a changing society may fall behind, potentially suffering psychological distress and stress-related health effects from being unable to keep up with average standards of consumption ( 3 ). The relative income hypothesis, which considers subjective measures of wealth, has the advantage of considering psychosocial pathways linking income to health; though testing the hypothesis requires making assumptions about how individuals compare themselves to others. For example, do low-income families feel socially excluded only when other low-income families begin earning more, or do the rising income of celebrities matter as well ( 3 )? It is also possible that relative income matters through other mechanisms as well, with income distribution affecting the ways in which businesses and governments invest in serving the poor ( 38 ). Studies that focus on overall income distribution as a determinant of health often use a statistic called the Gini coefficient ( 39 ), which summarizes income inequality, to help predict outcomes.
As noted briefly earlier, while the differentiation of relative versus absolute position is particularly relevant when social groups are defined by income, this concept extends to other ordered stratification variables that measure the extent to which individuals are falling behind others around them. These variables may be alternative constructs for measuring access to resources in the place of income, poverty, or wealth measures. For example, Townsend created an index that took account of diet, clothing, housing, work, recreation, and education, among other factors, to measure deprivation in the UK ( 40 ). This approach to creating a multidimensional poverty measure has also been utilized to better understand deprivation in the developing country context ( 41 ). The distinction between absolute and relative position also matters outside the realm of material or economic deprivation. For example, researchers have examined the impact of winning an Academy Award on all-cause mortality among nominated movie stars in order to investigate whether relative differences in social status mattered for the health of individuals who all uniformly enjoyed high absolute levels of prestige and social status ( 42 ). Interest in relative measures of SES, broadly speaking, has grown alongside research arguing that inequality itself harms health ( 43 ). Multilevel modeling techniques ( 44 ) that allow us to disentangle the influence of individual characteristics from those of higher level structures have also been instrumental in advancing this stream of research into inequality as an independent health risk factor.
Geographic health inequalities: place versus space
Geographic setting, not just social group, plays an important role in shaping health ( 45 – 47 ). Differentiating the concepts of space and place helps us to better understand the different ways in which geography can affect health ( 48 ). S pace deals with measures of distance and proximity such that exposure to spatially distributed health risks and protective factors will change according to an individual's precise location. For example, air pollution that exacerbates asthma symptoms would be an example of a health risk that is distributed across space. Proximity to landfills, crime clusters, and health clinics are other examples of spatially patterned health risks and protective factors. In contrast, place refers to membership in political or administrative units, such as school districts, cities, or states. Many government run programs and policies that affect health, such as food assistance programs or tax policies, are specific to administrative units and operate uniformly within their boundaries. As a result, the health impacts of a wide range of programs and policies do not depend on residents’ precise physical location, but rather on membership in a given political or administrative unit.
Concepts of space and place are often treated as exchangeable, and it is easy to see why. Political and administrative units are geographically defined such that people in the same place are often also very close together in space. However, if we imagine an example in which individuals are simultaneously exposed to health risks from a polluting local factory and to health benefits from a village aid program, the conceptual differences become clear. In this example, moving farther from a point source of pollution could improve health, regardless of whether the move were to a location inside or outside the village boundaries. In contrast, maintaining aid would be contingent on residing within village boundaries regardless of where within the village a person lived. Observed geographic health disparities may be driven by processes that are rooted in space, place, or both. From a research standpoint, the studies one might propose to understand geographic health inequalities should account for whether hypothesized health risks are spatial versus place-based. From a policy perspective, programs and interventions could more effectively target geographic health disparities if space and place were both explicitly considered.
Tracking health inequalities over time
Regardless of how researchers operationalize the study of health inequalities, they also must decide how to report observed differences. Inequalities between groups can be expressed as absolute differences or as relative differences ( 49 , 50 ). Computing absolute differences involves subtracting one quantity from another, while expressing relative difference requires dividing one quantity by another to produce a ratio. As health differences are tracked over time, absolute differences between groups can increase while relative differences increase, or vice versa. For instance, if 10 people per 100,000 are hospitalized for asthma each year in State A while 20 per 100,000 are hospitalized for asthma in State B, the absolute difference in asthma hospitalizations is 10 per 100,000. There are a few points to note in this example. First, both villages enjoy very low asthma hospitalization rates, though this fact is lost when only reporting on the magnitude of the inequality. Secondly, while a difference of 10 hospitalizations per 100,000 is relatively small, the villages appear to have vastly asthma hospitalization rates when the difference is expressed as a ratio.
As inequalities are tracked over time, decisions about how to express health differences become even more complex. Imagine that we follow our two hypothetical villages for 10 years and find that asthma hospitalization rates have increased in each. Now, 45 per 100,000 are hospitalized in State A while 60 per 100,000 are hospitalized in State B. The new absolute difference has risen to 15 per 100,000, but the relative difference has actually fallen such that State B has only 33% more hospitalizations than State A. In 10 years, asthma hospitalization rates in both states have increased, as has the absolute difference between states. At the same time, relative health inequalities have narrowed. Selective reporting of absolute or relative differences makes it difficult to understand if populations are faring better or worse over time, and by how much. In general, providing baseline information, as well as data on absolute and relative differences, presents a fuller picture of trends in health inequalities.
Framework for understanding health inequalities
Previous sections of this article dealt with practical issues of how health inequalities can be measured, including whether health differences are studied across individuals or groups, how inequalities may be measured across geographies and social groups, and how observed differences can be reported cross-sectionally and over time. We now move to concepts that are useful in considering how inequalities arise, and for exploring causal mechanisms that link geographic or social group membership to health. These are generic concepts that can apply both to the study of social inequalities in health and to understanding health inequalities across individuals.
Causal pathways and conditional health effects
When studying the relationship between an exposure, such as occupation, and an outcome, such as blood pressure, it often becomes clear that a third variable matters as well. Variables that lie on the causal pathway between exposure and outcome, called mediators , are those that explain how a given exposure leads to an outcome of interest ( 51 ). For instance, in a study of occupation and its effects on blood pressure, we might learn that income is the link that explains how a person's job influences their blood pressure. In this example, occupation could determine income, which then might affect blood pressure by influencing whether a person can buy healthy food, receive adequate medical care, or experiences stress over financial matters. When designing policies or programs to influence an outcome like blood pressure, it may be effective to consider ways that income could be used as a policy tool. For example, if income is responsible for the link between occupation and blood pressure, cash transfers or public assistance for low-income workers could improve blood pressure without changing working conditions. However, we might find that, even after increasing income, occupation still has an impact on blood pressure. If this were the case, we would conclude that income only partially mediates the occupation–blood pressure relationship. Knowing that occupation has an effect on blood pressure independent of income might spur researchers to ask whether job stress or working conditions affect health. Studies of health disparities should try to identify these pathways whenever possible because doing so helps us to better understand the mechanisms by which health differences arise and provides more options for designing policy solutions to real-world problems.
Mediator: A variable that lies on the causal pathway between exposure and outcome, helping to explain the association between them.
Effect modifier: A variable that does not lay on the casual pathway between exposure and outcome, but whose presence helps explain when and how an exposure and outcome are related. The relationship between exposure and outcome may vary according to the level of the effect modifier.
In other cases, we may discover that a third variable, often called a modifier or moderator, helps explain the conditions under which an exposure and outcome are related ( 51 ). Returning to the example of occupation and blood pressure, we can consider the role of race in the workplace. In many contexts, racial discrimination persists in the workplace. Within such a context, white employees who receive promotions might experience a decrease in blood pressure, perhaps due to increased job control and workplace status. On the other hand, black employees might not reap any health benefit from promotions because discrimination persists at all occupational levels, preventing them from feeling a sense of increased status or control at work. In this example, we might observe that better occupations improve blood pressure for white, but not for black, employees. Unlike our first example, in which income had a clear, directional impact on blood pressure, our second example shows how race modifies the relationship between occupation and blood pressure in different ways. This example also reminds us that social groups are not simply of interest as exposures, but may also explain the relationship between other exposures and outcomes.
Selection is another fundamental concept for understanding health inequalities ( 52 ). Selection refers to the fact that people have a tendency to sort themselves into neighborhoods, social groups, and other clusters. For example, people who value physical activity may be more likely to move to walkable areas, while sedentary individuals might choose to live in auto-dependent suburbs. When we see data suggesting that neighborhood walkability affects whether residents are physically active, therefore, we have to ask to what extent the observed relationship is causal, and to what extent it simply reflects self-selection into neighborhoods.
Selection is also sometimes proposed as an explanation for educational, occupational, and even racial/ethnic differences in health. For example, some might attempt to explain the relationship between SES and health as a product of selection by arguing that genetically superior individuals are more likely to have good health and high IQ, therefore explaining why highly educated, high income individuals are generally healthier. Research studies designed to estimate the causal effects of social factors on health generally reject such explanations, however, showing that exposures such as occupation, income, discrimination, and neighborhood poverty, for example, do influence health ( 35 ).
Context versus composition
When selection may be a source of geographic health inequalities, researchers generally want to distinguish contextual from compositional effects ( 53 ). Contextual effects refer to the influence a neighborhood or other type of higher level unit has on people, while compositional effects are simply reflective of the characteristics of individuals comprised by the neighborhood or other setting. Classrooms, schools, neighborhoods, states, hospitals, and other units of organization can all exert contextual effects. Contextual factors that affect health include policies, infrastructural resources, and public support programs ( 3 ) and are, therefore, potential targets of intervention for reducing health inequalities.
Compositional effects refer to variations in health attributable to the health status of the individuals who are members in a given context. If the construction of a specialized healthcare facility suddenly attracted large numbers of chronically ill residents to a given neighborhood, the poor health status of residents in that neighborhood compared to surrounding areas would be compositional.
Differentiating compositional versus contextual effects is of primary importance for making causal inferences about how settings impact health. Knowing that health inequalities exist across contexts does not tell us anything about why differences exist: Does living in high poverty neighborhoods increase the risk of getting sick? After taking individual-level risk factors into account, are there still variations in health outcomes across high and low poverty neighborhoods? Furthermore, does neighborhood poverty have the same health impact on all social groups, or are some at particular risk? Concentrated poverty and many other contextual characteristics may not just impact the average health of a community, but also health disparities between social groups ( 3 ).
Life course perspective
The impact of geography and social group membership on health is not only powerful but also persistent. Differences in early life and in utero circumstances can impact later health regardless of subsequent life events, generating health inequalities between social groups. ( 54 , 55 ). There are critical or sensitive developmental periods during which health is affected in ways that cannot be completely reversed. For example, poor nutrition in adolescence, when bones develop, could put individuals at risk for bone fracture in later life, regardless of attempts to slow bone loss in adulthood. Habits that develop early in life may influence the trajectory of one's health choices. Poor exercise habits in childhood may influence the choices that people later make as adults. Although adults can choose to exercise more later in life, childhood habits may serve as predictors of adult choices that continue to impact health. Finally, long-term exposure to conditions over the course of a lifetime also affects health. Earning a low income may have a greater effect on individuals who grew up poor than for those who grew up rich, for example. This prolonged deprivation could amplify the health effects of poverty.
Key Terms ( 56 ):
Life course perspective: A consideration of health inequalities that acknowledges that one's health status reflects both prior and contemporary conditions, including in utero and childhood effects. The life course perspective recognizes the impact of latent, pathway, and cumulative effects on later health.
Latent effects: Health effects caused by prior conditions that impact later health, regardless of subsequent life events. Examples include lack of adequate prenatal care or poor nutrition in childhood.
Pathway effects: Health effects resulting from early life conditions, which continue to impact future behavior. Examples include poor exercise habits in childhood that continue into adulthood. Although these habits can be changed in adulthood, they can be predictors of adult choices that themselves have health effects.
Cumulative effects: Health effects resulting from long-term exposure to conditions that affect health. Examples include prolonged exposure to environmental toxins or long-term poverty.
When social mobility is low and socially marginalized groups have historically limited options about where to live, early life conditions may be especially powerful in explaining current health inequalities. For example, in societies that struggle with the intergenerational transfer of poverty, or have a long history of ghettoizing marginalized groups, it is likely that individuals currently exposed to socially patterned health risks were previously exposed to socially patterned health risks as well, see Fig. 1 ( 57 ). Researchers should be aware that lagged exposures, even those as distant as parental occupation or childhood neighborhood, may be useful in explaining current health outcomes. Subject matter expertise in human development should inform studies or projects that explore prior life conditions to explain current health differences between groups. Longitudinal data, in addition to allowing for the exploration of lagged or cumulative effects, are also crucial for understanding the direction of causal relationships driving associations between health and social conditions. For example, recent evidence suggests that neighborhood poverty may indeed increase health risks ( 58 ), but that poor health may also systematically sort individuals into poorer neighborhoods ( 59 ). Only longitudinal study designs can help to clarify whether and the extent to which challenging social conditions and poor health outcomes reinforce each other over time.

The impact of socioeconomic status on health across the life course. Source: Taken directly from Adler et al. ( 57 ).
Explaining health inequalities
Social epidemiologists apply the concepts presented above to help measure and understand health inequalities. Several broad categories of explanations ( 3 , 54 , 60 , 61 ) are generally tested when trying to explain health differences across geographies and social groups but may also drive health differences across individuals in a population.
One type of explanation points to material factors in the creation of health disparities. Material factors include food, shelter, pollution, and other physical risks and resources that influence health outcomes. Measures of absolute resources, such as absolute income, are useful in testing the role of material deprivation in creating health differences, as are objective measures of physical health risk factors such as air quality. An unequal distribution of physical health risks and resources across geographies and social groups contributes to social inequalities in health via material pathways.
A second class of explanation points to psychosocial ( 62 ) factors as driving health inequalities and social group differences in health in particular. Psychosocial health impacts stem from feelings of social exclusion, discrimination, stress, low social support, and other psychological reactions to social experiences. Negative psychological states affect physical health by activating the biological stress response, which can lead to increased inflammation, elevated heart rates, and blood pressure, among other outcomes ( 63 , 64 ). Measures of relative position, perceived versus objectively measured variables, and instruments that capture different experiences of stress are all useful in studies of psychosocial risk factors. To the extent that certain social groups are systematically more likely to have stressful, demoralizing, and otherwise emotionally negative experiences, psychosocial factors can help explain health inequities.
Behavioral differences are also commonly cited as contributing to health inequalities. For example, a behavioral explanation might attribute health inequalities to differences in eating habits, smoking prevalence, or cancer screening rates across social groups or across individuals in a population. While health behaviors often do vary across groups, ecosocial ( 65 , 66 ) and social–ecological ( 67 ) frameworks prompt us to ask what upstream factors might be responsible for these variations. For example, if differences in smoking rates are caused by unequal educational opportunities, an inequitable distribution of psychosocial risk factors, and targeted marketing, attributing health disparities to behaviors may be of limited usefulness.
A fourth type of explanation points to differences in biological health risk factors that are patterned across social groups or contexts ( 60 , 68 ), or vary across individuals in a population. Biomedical explanations can suffer the same weaknesses as behavioral explanations for social inequalities in health when they focus on the downstream effects of social context without acknowledging why levels of biological risk factors vary across populations. Genetic and gene-by-environment interactions explanations are also, in part, biomedical in their nature. This class of explanation may be more useful for understanding variations in health observed across individuals in a population where social group differences are not the focus of investigation.
Applying a life course perspective to the consideration of all four types of explanations while considering that factors from each category may be main exposures, mediators, or moderators creates useful complexity in thinking about how health inequalities arise.
Conclusions
This article has introduced definitions and concepts that may be combined and applied in a wide range of settings. Previous work on health inequalities has introduced critical concepts and explored defining questions ( 3 ), evaluated relevant theories and considered resulting policy implications ( 4 ), discussed measuring and monitoring disparities ( 5 , 7 , 69 ), among other contributions. Building on these and other valuable resources, this paper has sought to unite salient theories, concepts, and methods into a single article, and to highlight previously under-discussed aspects of disparities research, such as the distinctions between space and place. When considering differences in health, it is important to determine whether inequalities were measured across individuals in a single population, or describe group-level differences. Group definitions will vary by historic and social context, and establishing meaningful groupings will be specific to those contexts. Social group health inequalities may be generated early or late in life by differences in access to material resources, social circumstances that generate stress, or health behaviors. Understanding causal pathways linking social factors to health, as well as conditional health, can aid in intervention planning. Geographic health disparities are also common and often reflect unjust social structures. Differentiating the concepts of place and space can help uncover what generates geographic health differences.
Even more difficult than executing well-designed studies of health inequalities is deciding what to study and how to use findings to narrow gaps between groups. A central task is deciding when a health inequality is inequitable, and why. Setting a policy agenda around health inequities is also fraught with difficult questions and decisions, including whether it is better to reduce absolute or relative health differences between groups; whether to focus on improving health for the worst-off groups or for the largest groups; and how to set benchmarks for health outcomes for various groups. For example, should we set the target life expectancy for black Americans to that of whites, or should we be aiming for both groups to live even longer? Are certain social groups or health outcomes more deserving of attention than others? If so, why? Do particularly unjust health differences deserve attention, or should we focus on health outcomes that are especially expensive or prevalent? What are the merits of investing resources into improving overall population health, and what are arguments for focusing on the elimination of health disparities instead?
There are no clear cut answers to any of these questions, though they are among the central factors shaping how health inequalities are studied and discussed. Criteria for prioritizing scarce resources may by economic, political, moral, or practical. These and other factors must be weighed in crafting research and policy agendas to track and understand health inequalities.
Authors' contributions
MCA and SVS conceptualized the article. MCA ALA and SVS wrote the manuscript. SVS provided overall supervision and critical edits.
Conflict of interest and funding
The authors have no conflicts of interest to report. Nothing in this manuscript is intended to represent the official policy or position of the US. Environmental Protection Agency.
- Search Menu
Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- Ethnic Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Politics of Development
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

Social Inequalities in Health: New evidence and policy implications
Author Webpage
- Cite Icon Cite
- Permissions Icon Permissions
Health inequalities according to people's social standing are persisting, or even growing, in modern societies. Recent decades have revealed evidence of strong variations in life expectancy, both between countries and within them. This widening of social inequalities has developed despite considerable progress in medical science and an increase in health care spending. The reasons behind this are complex, and the implications considerable. This book provides a summary of the major achievements of a five-year European Science Foundation (ESF) Programme on ‘Social Variations in Health Expectancy in Europe’. The contributors to this book are major figures in their subjects, and combine state of the art reviews with the latest results from interdisciplinary research in epidemiology, sociology, psychology, and biomedicine. Three conceptual frameworks of life course influences, health effects of stressful environments, and macro social determinants of health, are unified, while each chapter addresses the policy implications and recommendations derived from currently available evidence. The major topics covered include the role of family in early life, social integration and health, work stress and job security, successful ways of facing adversity, and the impact of the larger environment on health.
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
| Month: | Total Views: |
|---|---|
| October 2022 | 2 |
| October 2022 | 3 |
| October 2022 | 1 |
| October 2022 | 3 |
| October 2022 | 3 |
| October 2022 | 10 |
| October 2022 | 3 |
| October 2022 | 4 |
| October 2022 | 6 |
| October 2022 | 6 |
| October 2022 | 1 |
| November 2022 | 2 |
| November 2022 | 8 |
| November 2022 | 11 |
| November 2022 | 6 |
| November 2022 | 3 |
| November 2022 | 2 |
| November 2022 | 9 |
| November 2022 | 15 |
| November 2022 | 1 |
| November 2022 | 6 |
| November 2022 | 9 |
| November 2022 | 5 |
| November 2022 | 3 |
| December 2022 | 9 |
| December 2022 | 7 |
| December 2022 | 8 |
| December 2022 | 4 |
| December 2022 | 1 |
| December 2022 | 3 |
| December 2022 | 5 |
| December 2022 | 5 |
| December 2022 | 11 |
| December 2022 | 8 |
| January 2023 | 1 |
| January 2023 | 25 |
| January 2023 | 38 |
| January 2023 | 1 |
| January 2023 | 1 |
| January 2023 | 2 |
| January 2023 | 6 |
| January 2023 | 11 |
| January 2023 | 9 |
| January 2023 | 25 |
| January 2023 | 9 |
| January 2023 | 55 |
| January 2023 | 39 |
| February 2023 | 16 |
| February 2023 | 2 |
| February 2023 | 11 |
| February 2023 | 11 |
| February 2023 | 4 |
| February 2023 | 5 |
| February 2023 | 3 |
| February 2023 | 6 |
| February 2023 | 10 |
| February 2023 | 6 |
| February 2023 | 5 |
| March 2023 | 1 |
| March 2023 | 5 |
| March 2023 | 3 |
| March 2023 | 9 |
| March 2023 | 5 |
| March 2023 | 1 |
| March 2023 | 4 |
| April 2023 | 14 |
| April 2023 | 6 |
| April 2023 | 1 |
| April 2023 | 2 |
| April 2023 | 2 |
| April 2023 | 1 |
| April 2023 | 7 |
| May 2023 | 10 |
| May 2023 | 1 |
| May 2023 | 7 |
| May 2023 | 7 |
| May 2023 | 2 |
| May 2023 | 3 |
| May 2023 | 4 |
| May 2023 | 2 |
| May 2023 | 6 |
| May 2023 | 3 |
| June 2023 | 2 |
| June 2023 | 1 |
| June 2023 | 1 |
| July 2023 | 6 |
| July 2023 | 2 |
| July 2023 | 3 |
| July 2023 | 4 |
| July 2023 | 1 |
| July 2023 | 2 |
| July 2023 | 2 |
| July 2023 | 3 |
| July 2023 | 2 |
| July 2023 | 2 |
| July 2023 | 2 |
| July 2023 | 2 |
| July 2023 | 4 |
| July 2023 | 3 |
| August 2023 | 4 |
| August 2023 | 1 |
| August 2023 | 1 |
| August 2023 | 1 |
| August 2023 | 4 |
| September 2023 | 5 |
| September 2023 | 6 |
| September 2023 | 3 |
| September 2023 | 3 |
| September 2023 | 3 |
| September 2023 | 3 |
| September 2023 | 3 |
| September 2023 | 4 |
| September 2023 | 4 |
| October 2023 | 5 |
| October 2023 | 4 |
| October 2023 | 6 |
| October 2023 | 1 |
| October 2023 | 2 |
| October 2023 | 2 |
| October 2023 | 4 |
| November 2023 | 1 |
| November 2023 | 14 |
| November 2023 | 5 |
| November 2023 | 1 |
| November 2023 | 1 |
| November 2023 | 1 |
| November 2023 | 3 |
| November 2023 | 2 |
| November 2023 | 1 |
| November 2023 | 15 |
| November 2023 | 6 |
| December 2023 | 1 |
| December 2023 | 7 |
| December 2023 | 4 |
| December 2023 | 6 |
| December 2023 | 1 |
| December 2023 | 2 |
| December 2023 | 1 |
| December 2023 | 1 |
| December 2023 | 3 |
| January 2024 | 1 |
| January 2024 | 2 |
| January 2024 | 1 |
| January 2024 | 2 |
| February 2024 | 1 |
| February 2024 | 12 |
| February 2024 | 5 |
| February 2024 | 1 |
| February 2024 | 1 |
| February 2024 | 2 |
| February 2024 | 10 |
| February 2024 | 4 |
| March 2024 | 1 |
| March 2024 | 6 |
| March 2024 | 3 |
| March 2024 | 4 |
| March 2024 | 3 |
| March 2024 | 3 |
| March 2024 | 4 |
| April 2024 | 5 |
| April 2024 | 2 |
| April 2024 | 10 |
| April 2024 | 10 |
| April 2024 | 2 |
| April 2024 | 1 |
| April 2024 | 2 |
| April 2024 | 2 |
| April 2024 | 2 |
| April 2024 | 3 |
| April 2024 | 3 |
| April 2024 | 3 |
| April 2024 | 8 |
| April 2024 | 9 |
| May 2024 | 4 |
| May 2024 | 7 |
| May 2024 | 2 |
| May 2024 | 4 |
| May 2024 | 1 |
| June 2024 | 2 |
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 25 April 2023
Social inequality, social networks, and health: a scoping review of research on health inequalities from a social network perspective
- Sylvia Keim-Klärner 1 ,
- Philip Adebahr 2 ,
- Stefan Brandt 3 ,
- Markus Gamper 4 ,
- Andreas Klärner 1 ,
- André Knabe 5 ,
- Annett Kupfer 6 ,
- Britta Müller 7 ,
- Olaf Reis 8 ,
- Nico Vonneilich 9 ,
- Maxi A. Ganser 10 ,
- Charlotte de Bruyn 11 &
- Holger von der Lippe 10
International Journal for Equity in Health volume 22 , Article number: 74 ( 2023 ) Cite this article
5212 Accesses
3 Citations
4 Altmetric
Metrics details
This review summarises the present state of research on health inequalities using a social network perspective, and it explores the available studies examining the interrelations of social inequality, social networks, and health.
Using the strategy of a scoping review, as outlined by Arksey and O’Malley (Int J Sci Res Methodol 8:19–32, 2005), our team performed two searches across eight scientific, bibliographic databases including papers published until October 2021. Studies meeting pre-defined eligibility criteria were selected. The data were charted in a table, and then collated, summarised, and reported in this paper.
Our search provided a total of 15,237 initial hits. After deduplication ( n = 6,168 studies) and the removal of hits that did not meet our baseline criteria ( n = 8,767 studies), the remaining 302 full text articles were examined. This resulted in 25 articles being included in the present review, many of which focused on moderating or mediating network effects. Such effects were found in the majority of these studies, but not in all. Social networks were found to buffer the harsher effects of poverty on health, while specific network characteristics were shown to intensify or attenuate the health effects of social inequalities.
Conclusions
Our review showed that the variables used for measuring health and social networks differed considerably across the selected studies. Thus, our attempt to establish a consensus of opinion across the included studies was not successful. Nevertheless, the usefulness of social network analysis in researching health inequalities and the employment of health-promoting interventions focusing on social relations was generally acknowledged in the studies. We close by suggesting ways to advance the research methodology, and argue for a greater orientation on theoretical models. We also call for the increased use of structural measures; the inclusion of measures on negative ties and interactions; and the use of more complex study designs, such as mixed-methods and longitudinal studies.
Introduction
This scoping review departs from two meta-analytically substantiated insights into the sociological and psychological determinants of people’s health and health behaviour. First, there is broad evidence that social inequality engenders health inequality : the fewer economic and educational resources individuals possess, the less healthy they typically are, and the fewer – or less effective – health behaviours they exhibit [ 34 , 50 ].
Second, the literature also indicates that networks of personal relationships are important for individuals’ health and health behaviour [ 3 , 44 ]. Analyses of social networks take the structural and compositional features of people’s networks into account. These networks impact people’s health and health behaviour, with the effects ranging from helpful to harmful. For instance, networks that provide individuals with a high degree of social integration typically foster their well-being and promote social learning from their network members [ 44 ]. While these network relationships might lead people to adopt healthy behaviours, they might also push or entice people to engage in unhealthy risk behaviours. Thus, recent studies have examined all three aspects and their interrelationships,that is, they have addressed both social inequality and social networks in the context of research on health differences and inequalities.
In recent years, a large and growing number of empirical studies have examined the interrelationships between social networks and health. Although these findings are promising, research gaps have been pointed out [ 35 , 38 , 41 ]. What has so far been missing in this strand of research is a systematic exploration of how the social network perspective contributes to our understanding of the correlation between social and health inequalities.
From a theoretical point of view, the social network perspective has been identified as having the potential to improve our understanding of health inequalities [ 23 ]. This perspective may be particularly valuable when it focuses on the structures and the mechanisms that influence health outcomes, while also analysing how individual differences are multiplied by social networks, and how social inequalities are reproduced.
Therefore, this paper is guided by two leading questions:
To what extent have existing studies examined social inequality, social networks, and health inequality using a single empirical approach?
What have the findings of these studies revealed about the effects of the structural and the compositional characteristics of social networks on the association between social inequalities and health?
The topic: social networks, health, and social inequalities
Today, the term “social network” is widely used, often in reference to online networks. However, our focus is on the research perspective of social network analysis that defines social networks broadly as “webs of social relationships that surround an individual and the characteristics of those ties” ([ 3 ], p. 145). Such relationships and their interconnections are not volatile,instead, they are arranged in “lasting structures” that are constantly produced and reproduced by interactions ([ 6 ], p. 6). It is this “overall configuration or pattern of relationships” ([ 44 ], p. 6) that is of interest in network research. This configuration may, for example, be captured by:
homogeneity and homophily measures of one’s network members (indices of, respectively, the similarity of one’s network partners and their resemblance to oneself);
measures of the density or redundancy of one’s network (indices that show to what extent a network is or is not loosely knit); or
the presence and the number of bonding ties (the core network of close contacts) or bridging ties (which provide access to resources and information not available within the core network).
While these measures describe specific structural features, network indices form composite measures of different types of relations. An index that is often applied in this context is the Berkman-Syme Social Network Index (SNI), which focuses on the isolation/integration of a person, and collects information on the individual’s marital status, number and frequency of contacts with children, close relatives and close friends, church group membership, and membership in other community organisations. By means of such indices, subjects can be categorised into different network types, which are often characterised as having high to low levels of social integration [ 4 ].
An assumption that underlies many network approaches is that social networks “have emergent properties not explained by the constituent parts and not present in the parts” ([ 41 ], p. 407). Thus, network research combines an interest in the specific contacts individuals have in different areas of life (e.g., relatives, friends, colleagues,plus their characteristics) with a focus on their interactions and the functional aspects of these relationships (e.g., social support). Moreover, network research is interested in the larger structure that emerges based on these single ties. Drawing on this perspective, network research goes beyond other measures and concepts of social contacts and interpersonal influences by collecting information not only on the characteristics of the individuals in the network, but also on their relationships and their interconnections.
Social capital research from Bourdieu [ 8 ] to Coleman [ 13 ] or Putnam [ 36 ] has often referred to social networks in defining social capital. However, social capital studies have used structural network measures and network theory to varying degrees, from “building a network theory of social capital” [ 27 ], to focusing exclusively on the aggregate level, by, for example, measuring involvement in organisations and associations (yes/no) and general norms of trust [ 36 ]. These aggregate measures were often based on network theoretical thinking, with the aim of measuring network variables efficiently. For example, involvement in organisations can be used as an indicator of bridging ties without the need to collect complex network data.
Given the inconsistent and often metaphorical use of the term “social networks”, we have provided a definition of social networks that guides us in this review in Table 1 . It specifies that social networks are characterised by relationship characteristics (focusing on different types of relations), by information on the function of relationships (e.g., support), and by structural information on the patterns the relationships form (e.g., density).
In health research, network studies examine the direct impacts of networks on people’s behaviour, as well as the diffusion of ideas, diseases, and behaviours within these structures [ 3 , 44 ].
Unlike in health research, social network studies are not very common in inequality research [ 16 ], even though their concepts have much to offer in investigations of inequality [ 28 ]. Network characteristics such as homophily (“birds of a feather flock together”) or transitivity (“my friend’s friend is also my friend”) can lead to segregated networks of individuals who have either high or low resources, and can therefore not just reproduce social affiliations, but also foster social inequality and inhibit social mobility. People’s social status can affect their opportunities for engaging in beneficial social contacts. For example, an individual with higher social status has access to places (e.g., clubs, business meetings, societal events) where other people in higher social positions meet, and the person can use this access to social resources to advance his/her own career. In contrast, the homogenous network of an individual with lower social status cannot provide him/her with access to such resources [ 7 ]. These dynamics can be directly connected to an individual’s health and health behaviour, as people with higher social status are known to adopt healthier behaviours, and to form relationships with similar individuals, which may also have a positive impact on their health. This pattern can lead to the widening of health disparities [ 33 ]. However, the interrelations of social networks and social inequality are complex. Social networks can also help to reduce social inequality, by, for example, buffering individuals from the detrimental effects of financial deprivation [ 18 ]. The mechanisms involved in how social networks impact individual health or buffer or foster health inequalities are complex and manifold [ 24 ]. It is therefore far beyond the scope of this paper to go into all these possible mechanisms in more detail. In what follows, we focus on moderator and mediator effects of social networks on health inequalities.
Figure 1 illustrates the most commonly identified types of interconnections between social networks and social and health inequalities. Part A of the figure displays a so-called moderator model. In this model, social networks do not have direct correlations with social or with health inequalities, but they can influence the correlations between these inequalities, by, for instance, having a buffer effect, as was mentioned above. Part B of the figure shows a so-called mediation model. Here, the baseline correlation between social and health inequalities is – fully or partially – altered (“mediated”) by the characteristics of a person’s social networks. In this model, the empirical question of whether the baseline correlation is attenuated (“statistical mediation”) or increased (“statistical suppression”) when social networks are included as a mediating variable remains open.
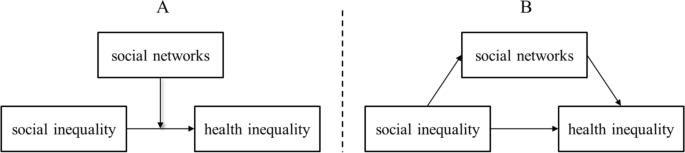
Schematic representation of moderator ( A ) and mediator ( B ) effects of social networks on health inequality. Source: own display
In the present scoping review, we examine to what extent existing studies have analysed the interconnections of social inequality, social networks, and health inequality using a single empirical approach. We also intend to summarise what the findings of these existing studies have revealed about the effects of the structural and the compositional characteristics of social networks on the association between social inequalities and health.
Methods: reviewing studies using a social network perspective on health inequalities
The literature reviewing process was conducted by the members of a research network on social networks and health inequalities “Soziale Netzwerke und gesundheitliche Ungleichheiten (SoNegU)” funded by the German Research Foundation. The 25 members of this group discussed, scrutinised, and critically assessed the methodological approach and the proceedings of the review on several occasions, a total of 18 members were involved in the article screening. Although we did not strictly follow the PRESS strategy [ 30 ], we employed a third party review of our search strategy by two renowned experts in the field. Given the broad nature of our research questions and the heterogeneity of the studies in the field, we used the method of a scoping review. This method is especially applicable in contexts in which concepts are blurry or heterogeneously understood (as is the case for social networks, social support, social capital), and in which there are a variety of definitions, operationalisation approaches, and research designs that are difficult to compare systematically [ 1 ].
This scoping review strategy follows the method created and outlined by Arksey and O’Malley [ 1 ]. Their methodological framework describes five steps that must be taken to adequately perform a scoping review: 1. Identifying the research question; 2. Identifying relevant studies; 3. Selecting studies; 4. Charting the data; and 5. Collating, summarising, and reporting the results.
Identifying relevant studies: data sources and search terms
The initial literature search was limited to peer-reviewed journal articles in English or German language, using the following international and German medical and social science data bases: Pubmed; PsycINFO and MEDLINE via Ovid; Solis (until 2017), SA (Sociological Abstracts, from 2017), SSA (Social Services Abstracts), ASSIA (Applied Social Sciences Index and Abstracts), and Scopus. The restriction to peer-reviewed articles was made for qualitative and time-efficiency reasons. Because the term "social networks" was often used metaphorically, we had to screen a large number of articles. A restriction to peer-reviewed articles ensured both a high-quality standard and a manageable number of hits. The search was conducted until October 2021. Articles were deemed eligible for inclusion only if they contained at least one search term from each of the following three topics: health, social inequality, and social network analysis. Table 2 displays the search terms that were applied to titles , abstracts, keyword, or MeSH terms of empirical studies . Additional information on how we translated these search terms into MeSH terms is provided in Appendix 1 .
Selecting studies: article screening and eligibility criteria
Eligibility criteria were consensually determined by the research group. Various preparatory steps (including a pilot trial) were taken to homogenise the evaluation of the literature in the research group (a two-stage pretest, discussion sessions for dissent, etc.). Through this process, a final eligibility list was generated.
Due to the large number of resulting findings, we needed to limit the scope of research to specific contexts. Given our interest in population health, studies focusing on health service use, on specific health issues (e.g., AIDS), or on specific groups (such as homeless individuals, or men who have sex with men) were excluded, as these works may require a separate review. A clear regional focus on OECD countries was also included in the criteria. Table 3 displays all of the study exclusion criteria.
While we began the initial selection process by reviewing titles and abstracts, we then proceeded to review full texts (see Fig. 2 ). We recorded the selected texts, using a spreadsheet, indicating included or excluded texts as well as the reasons for exclusion. After reviewing full texts, it became obvious that some articles used the term “social network” in a rather metaphorical way, and often as a synonym for one-item measurements of social relations or support. We decided to exclude the studies that did not report on more advanced relational, functional, or structural indicators (see the aforementioned social network perspective). Additionally, the empirical connections the studies made between social inequality and social networks were evaluated. Papers that did not relate social inequalities to social networks, but instead treated them as independent controls, were excluded. Figure 2 displays the full sequence of the selection process.
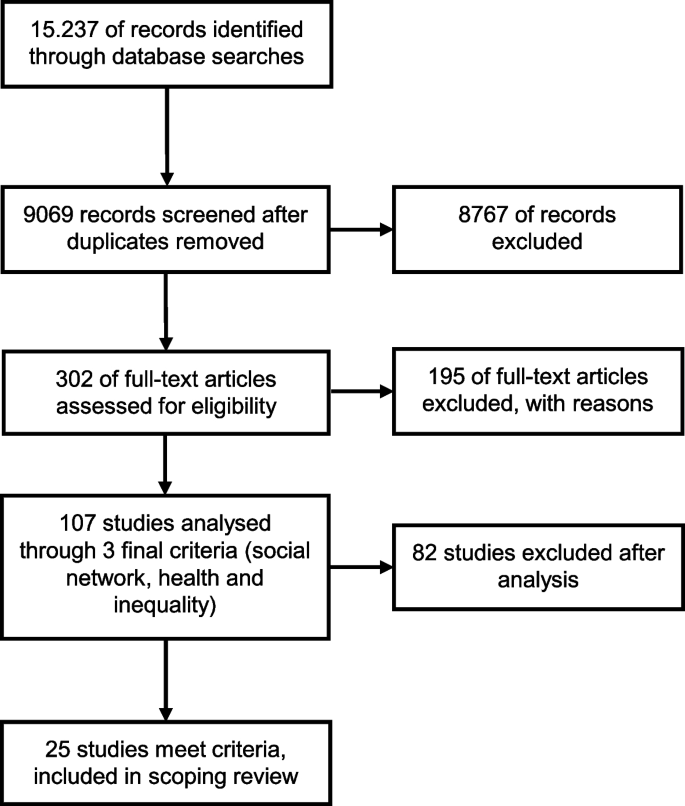
Flowchart of paper selection process (adapted from [ 1 ]). Source: own display
Data charting and final extraction
A resulting and refined 17-column spreadsheet indicated the relevant variables for extraction. This spreadsheet was pilot-tested with 20 papers, discussed in the working group and then provided to all involved in data charting along with examples and an explanatory text. The selected studies were evaluated with regard to characteristics such as research questions, study designs, methods and variables used, and central findings. Appendix 2 illustrates this procedure using the final study selection of this review.
Results: characteristics and main findings of the eligible studies
General characteristics of the final body of studies.
The resulting 25 studies were conducted between 1999 and 2021. Of those, more than half were performed after 2010. Thus, a steady increase in the publication of relevant articles can be observed over the years, with only four of the studies being published before 2005. Of the selected studies, 15 were conducted in Europe, five were conducted in the US, two were conducted in Canada, two were conducted in Australia, and one was conducted in New Zealand.
Given our selection criteria, all 25 studies stem from academic journals, typically from health sector journals such as “Social Science and Medicine” (e.g., [ 9 *, 45 *]) and “Health & Place” (e.g., [ 2 *, 15 *, 46 *]). None of the selected articles had been published in a journal on social network research. Although network journals publish various articles on health issues, these articles did not deal with social inequalities.
Methodological characteristics of the final body of studies
Study design and methodology.
Of the 25 included studies, 24 used quantitative data and performed one or more types of regression analyses. The studies were predominantly cross-sectional, and only seven papers used longitudinal data sets. One study used a mixed-methods design [ 2 *] that began by collecting quantitative data through a postal questionnaire, followed by face-to-face interviews with participants from the questionnaire part. Cattell [ 9 *] was the only purely qualitative study included in this review. Adopting a Grounded Theory approach, this study focused on in-depth face-to-face interviews in two impoverished London neighbourhoods, and developed a typology of social networks in relation to social and health inequalities.
Types of health measurements
The numbers and the types of variables collected in order to quantitatively depict health differentials varied between the studies (cf. also Appendix 2 ). A measure for self-rated, self-reported, subjective, or perceived health was most commonly used, appearing in 11 studies. Nine studies combined three or more health measures; e.g., on physical functioning, mental health, well-being, or vitality. Other studies focused on single measures of general interest, such as BMI (two studies) or resting heart rate (one study). Measures of health behaviour, such as smoking, alcohol consumption, or physical activity, were used as dependent variables in five studies.
Types of social inequality measurements
The included studies showed less variation in their approaches to measuring vertical social inequality. Most common were measures of education and income. Among the other measures used were wealth, perceived income adequacy, employment, occupation, social class, and economic living standard.
Types of social network measurements
The studies included in this review utilised a wide array of variables measuring social networks, including relational, functional, and structural measures (see Appendix 2 ). The relationship characteristics they collected were diverse, and most commonly referred to partnerships, family and friends, and contact frequency. In contrast, one functional characteristic, social support, was used in 15 of the studies. However, these studies varied considerably in the types of support they measured (e.g., emotional, instrumental), and in whether they assumed that the support was needed, perceived, received, or provided. Structural network measures were used in 15 studies, with the variable of network size being the most frequently used (11 studies). In contrast, the use of other structural network measures was rare, and those that were included were diverse. Network density was measured in three studies, and the homogeneity of networks was also measured in three studies. One study focused on homogeneity in terms of ethnicity and gender [ 20 *], while another study focused on homogeneity of belonging to a small number of membership groups [ 9 *], and a third study measured homogeneity of income, age, race, education, being employed, living in the local area, and being family members [ 26 *]. Verhaeghe and colleagues [ 46 *] studied the occupational composition of social networks. Homophily was measured in one study using the I-E Index, which indicated the similarity of alters with ego regarding smoking, age, and education [ 31 *]. The structural constructs of bridging or bonding social relations were applied in three studies. In addition to network measures, 13 studies also used aggregate social capital measures such as trust, neighbourhood cohesion, or community activities.
Most studies covered two of the three named network characteristics: i.e., either relational and functional measures or relational and structural measures. Nine studies were more complex and used variables on multiple types of relationships, network functions, and structural information. For example, Nemeth and colleagues [ 31 *] collected information on the persons the respondent spends the most time with and the persons whom the respondent asks for advice, including information on the characteristics of these persons (e.g., age, smoking status). They also used measures of perceived support (by partner, family, and friends), network size, and density. Four studies reduced complexity by using the Social Network Index (SNI) by Berkman and Syme [ 4 ] and the Social Integration Index (SII), a modified version of the SNI [ 5 ]. These indices captured different types of relations, and they were enriched with additional support or loneliness measures [ 25 *, 29 *, 47 *, 48 *, 49 *].
Main findings of included studies on the interconnections between social inequality, social networks, and health inequality
The interconnections between the crucial three constructs of interest were predominantly analysed using statistical moderator analyses (11 studies) and mediator analyses (nine studies), but multivariate regressions were also applied (six studies). Footnote 1
Social networks as moderators of health inequalities (moderator analysis “type 1”)
Regarding the moderating effect of social networks on the correlation of social inequalities and health inequalities (here termed “type 1”; see Fig. 1 A in the introductory section), the results of four out of five studies showed the relevance of different kinds of social network measures. Richards [ 37 *] and Gele and Harsløff [ 20 *] described moderator effects. Both focused on strong and weak network ties: on close ties, activities in organisations, and having a doctor as a friend [ 20 *], and on friends, support, activities in organisations, and their frequency [ 37 *]. Gele and Harsløff [ 20 *] showed that in their sample, social networks were significant brokers of social resources. For example, they found that being linked to higher educated network partners was beneficial for the respondents’ health, particularly for those with low education. Richards [ 37 *] observed that a high level of social integration acted as a buffer for the negative correlation of well-being and financial strains. Specifically, they found that financial problems impacted a person’s happiness less severely when the person had strong and supportive informal ties as well as extensive weak ties. In the studies by Baum et al. [ 2 *] and Craveiro [ 15 *], neither the relational, structural, nor functional network characteristics under study (e.g., contact frequency, support, network size) were shown to be relevant,but aggregate measures, such as perceived neighbourhood cohesion and safety, social participation, and general network satisfaction, were found to have a moderating effect on health inequalities. However, Craveiro [ 15 *] observed these effects in central and southern Europe only. By contrast, Chappell and Funk [ 10 *] found no similar moderator effects for network size, group membership, community activities, service use, or trust. Emotional support was only used as a control variable in this study.
SES as moderators of network impact on health (moderator analysis “type 2”)
In contrast to the model displayed in Fig. 1 A, and somewhat surprisingly, six studies of the review sample also examined whether social inequality moderated the relationship between social networks and health (here termed “type 2” moderation). Four of these six studies found such moderating effects.
Schöllgen and colleagues [ 40 *] reported that SES had a moderator effect on the relationship between social resources and health. Specifically, they found that network support was more beneficial for the subjective health of individuals with lower than with higher income levels. In a similar vein, Vonneilich et al. [ 47 *] reported that the health risks associated with the lack of emotional and instrumental support were higher for subjects with lower than with higher SES. Focusing and bonding social capital, Kim et al. [ 22 *] showed that the association between social capital and health was moderated by income, with higher bonding social capital being linked with better health for low-income households only. However, the measure of network density, in combination with the health measure BMI, was found to be associated with higher health risks for persons with lower levels of education [ 12 *]. The authors explained this finding by noting that lower educated individuals tend to have less resourceful/supportive and more homophilic social networks. Unfortunately, measures of network homophily or support were not included in this study.
While Unger and colleagues [ 43 *] and Weyers and colleagues [ 49 *] did not find any “type 2” moderator effects in their data, they do no reject the relevance of social networks. The former authors assumed that it could be a mediator effect, and the latter authors stated that having a lower socio-economic position strengthens the influence of social networks on adverse health behaviour.
Social networks as mediators of health inequalities
Regarding the mediating effect of social networks on the correlation of social inequalities with health inequalities (see Fig. 1 B), seven out of nine studies reported such findings. This mediating effect was found in cross-sectional studies as well as in longitudinal studies. The study by Li [ 26 *] found that people of a higher social class were more likely to mobilise their social resources and networks for their own well-being than people of a lower social class. The authors noted, however, that these partial mediation effects of network size and diversity on health and well-being were numerically small compared to the effects of social class. In addition, Verhaeghe et al. [ 46 *] found a prevalent class effect as well as a mediator effect of social networks, with lower levels of social support contributing to a reduction in self-rated health. In a longitudinal study, Klein and colleagues [ 25 *] found that social networks mediated up to 35% of the social inequality effect on self-rated health. They showed that low SES was associated with lower levels of social integration and poorer social support, which in turn led to adverse effects on health. In their longitudinal study, Vonneilich et al. and colleagues [ 48 *] also found a considerable mediating effect, stating that “social relationships substantially contribute to the explanation of SES differences in subjective health” ([ 48 *]: 1/11).
In her qualitative study, Cattell [ 9 *] described how being financially restricted or living in a poor area impeded social participation, which in turn led to a higher risk of social exclusion (smaller networks, less support) and poor health. She also showed that structural social network features (such as density and reciprocity) and functional characteristics (such as support) reduced the harsher effects of poverty on health.
While the mediation studies discussed so far dealt with some indicator of perceived or self-rated health, [ 29 *] demonstrated that social isolation mediated the relationship between SES and resting heart rate by increasing the latter when subjects felt socially isolated and had smaller networks. Looking at different welfare regimes, Craveiro [ 14 *] found that social networks mediated the effects of SES on health, but also that the mediating variables varied across different welfare regimes. However, social support and network satisfaction were found to be consistent mediators in all regions under study.
Two studies did not find any mediating effects. Chappell and Funk [ 10 *] analysed the effects of network size, emotional support, group membership, and community activities on the perceived mental and physical health of individuals with different levels of education and income, while Sabbah and colleagues [ 39 *] researched the mediating effects of support and network size on dental health. However, while the latter authors did not reject the idea that social networks could play a role in inequality in dental health in general, they critically evaluated their applied support measures. Among other measures, they used the subjects’ “need for emotional support”, instead of the more commonly used receipt of support.
Social networks in multivariate models of health inequalities
Another strand of studies refrained from formulating explicit moderator or mediator models. Instead, these six studies investigated social and health inequalities together with social networks in multivariate models without statistical interaction terms. All of these studies showed the relevance of social networks for health inequalities. Stephens and colleagues [ 42 *] found that having a lower income was associated with having less social support, having a more restricted social network, and being less socially integrated, which in turn had detrimental health effects. Moreover, they found these social factors led to a higher risk of loneliness, which was strongly related to several adverse health effects. Similarly, Chavez et al. [ 11 *] demonstrated that people who reported having trust and feelings of reciprocity in their social context had better self-reported health. Although Veenstra [ 45 *] found that income and education were the strongest predictors for health, this author also showed that being socially integrated at work contributed to better self-reported health.
Two of these studies focused on health behaviours. Nemeth and colleagues [ 31 *] showed that when strong neighbourhood cohesion was combined with the belief in the general acceptability of smoking in a deprived neighbourhood, and when social networks contained many smokers, it was more difficult for smokers to quit, as doing so would jeopardise their social acceptance. Kamphuis and colleagues [ 21 *] showed that social networks played an important role in differences in sports participation, as people with lower SES, smaller networks, and less network cohesion had lower levels of sports participation.
The longitudinal study by Novak and colleagues [ 32 *] introduced network characteristics from past study waves as “parental control in school” and “not being popular in school”. They showed that people who had low education as well as these social network characteristics during their school years were more likely to be obese in adulthood.
Discussion and conclusion
Health inequalities have been investigated and discussed in research for many decades, and form an established research topic. Social network analysis, by contrast, is a novel research approach, but one that is gaining in popularity. Thus, the present scoping review was guided by two main questions: to what extent have existing studies examined social inequality, social networks, and health inequality using a joint empirical approach; and what have the findings of these studies revealed about the effects of the structural and the compositional characteristics of social networks on the association between social and health inequalities?
Despite the large number of initial hits in the literature research (9,064), after we reviewed the papers’ contents in more detail, we found a comparatively small number of publications (25) that fitted the aim of this review. A typical phenomenon that occurred during the selection process was that at first glance, many articles seemed suitable based on the term “social networks” in their abstract. At second glance, however, we found that the authors often used this term rather metaphorically for some unspecified kind of social relations or support. In these articles, which we excluded from this review, the authors neither made connections to the theoretical concepts or to methods of social network analysis; nor explored different types of relationships, analysed network functions, or measured structural network characteristics. Thus, despite the recent prominence of the term “social network”, there are only a few studies on health inequalities that can clearly be identified as social network analyses.
Among the studies considered for this review, the majority were published less than 10 years ago, and this set of studies exemplifies the growing popularity of network studies in research on health inequalities. From a theoretical and a statistical point of view, analyses of mediator, moderator, and multivariate models were the most common. Table 4 summarises the central results of this scoping review, which we will discuss in the following sections.
The empirical basis of statements 1 and 2 in Table 4 is provided by Table 5 . When summarising the studies that applied statistical mediation or “type 1 moderation” models, we observed that 11 out of 14 empirical studies successfully located social networks conceptually between social and health inequalities. From our perspective, this approach also appears to be particularly valid, because networks temporally arise more frequently from a person's social class than vice versa. The models we termed “moderation type 2” models appeared to be less plausible to us for that reason. The 11 studies mentioned above showed that social networks are a relevant explanatory tool for improving our understanding of the complex relationships between socially unequal industrialised societies and health outcomes.
Another finding that we deem particularly interesting – including for future research – is that social networks appeared to be particularly relevant for attenuating the detrimental effects on health of deprived social contexts or statuses (statements 3 and 4 in Table 4 ). When the structure, function, or composition of social networks provide health-related resources to people, the health of deprived individuals typically benefits. However, we also found evidence of the often overlooked “dark side” of networks: studies that focused their research on behavioural variables to describe health (e.g., BMI, smoking, and alcohol consumption) often found a negative correlation between these behaviours and social inequality due to the power and influence of social networks . For instance, the study by Child et al. [ 12 *] demonstrated that social networks could have reinforcing effects on the behaviour of people with both low and high incomes, resulting in higher predicted BMI for people in low-income communities and lower BMI for people in high-income communities. These results were echoed by Nemeth et al. [ 31 *] in their study of smoking cessation and by Weyers et al. [ 49 *] in their study of social relations’ overall impact on behaviour. In other words, depending on the variables used to describe health and networks, the intervening effects of networks on health changed, but the value of social network analysis within this research framework did not.
Methodological discussion and future research directions
If the reported level of interest in the role of social networks in health research continues as was previously described, within the next few decades, more studies will be conducted using social network analysis as a mediator and moderator between health and social inequalities. This projected growth in the literature will provide a broader set of precedents and more consistency in both the variables collected and the results produced in this research field. While the 25 studies included in this scoping review provide an illuminating introduction to this topic, they should ultimately represent only the beginning of research into what we hope will become a very useful explanatory tool for studying these complex relationships in the years to come. Many of the studies in this review started out by stating that the body of knowledge on the role of social networks in health inequalities is small (e.g., [ 15 *, 25 *, 47 *]), indeed, it appears that the authors of these studies were often unaware of other research on this topic, as the studies seldom cite each other in the text or in the references. This could reflect the strength of disciplinary boundaries; the centredness of the authors on specific health topics, populations, or specific countries; or the authors’ reading habits, which led them to focus on a small number of journals in the large landscape of health-related journals. This review can help scholars overcome these boundaries by bringing together evidence from various research streams.
Looking more closely at the methodological approaches and the network measures used in the presented studies provides us with valuable insights for formulating future directions for researching the role of social networks in health inequalities.
A first critical issue is the large amount of heterogeneity that the selected studies displayed, and especially the diversity of their network measures. Even a comparatively simple network variable such as size was measured in many different ways (number of close ties, number of supportive ties, etc.), and the studies often combined very different relational, functional, structural, and even aggregate measures into one empirical approach. This heterogeneity currently impedes quantitative meta-analyses in terms of systematic reviews. In future research on social and health inequalities, all network analyses could benefit by orienting empirical measures on theoretical models, such as the notions of supportive, integrating, influencing (norming), or contagious network ties. The current literature is still far from having reached a consensus on these issues. For instance, studies grounded in the theoretical considerations of social capital did not automatically enter this review because their network-related variables were typically too broad and too aggregate. While many of the included studies found that social networks could partially explain the association between socio-economic position and health, the researchers often did not observe the expected interrelations of social networks, social inequality, and health. These authors suggested [ 10 *, 39 *], or even insisted, that better measures should be used to clarify these interrelations [ 11 *]. Apart from orienting measures on theoretical models in general, using structural network indicators may be one step in this direction, as the studies using multiple network variables indicated. The best examples of this approach were provided in the studies by Li [ 26 *], who found mediating effects of network size and diversity, by [ 12 *], who found a moderating effect of network density, and by [ 31 *], who showed the relevance of homophily for smoking behaviour. One way of dealing with the complexities of collecting and analysing network measures is the development of tools such as the Social Network Index (SNI), which was created and developed by Berkman and Syme [ 4 ], or its successor, the Social Integration Index (SII) [ 5 ]. These tools were included in four of the studies presented here. They provide important precedents that constitute essential tools for increasing the consistency of studies in this field. In the future, the use of more standardised research tools would enhance the reliability and consistency of social network analysis within this research field. The benefits of using these tools would be compounded by the establishment of a set of baseline variables collected through precedent and testing.
Second, as social network research builds on a rich tradition of quantitative studies, it is not surprising that quantitative social network analysis emerges so strongly in the articles we reviewed. However, the single qualitative study included in the present study shows the valuable contributions qualitative methods can make in identifying the pathways through which social networks affect health, and the role of social inequality in this association. An especially interesting approach for future network research on social and health inequalities could be to conduct mixed-methods studies, which have received increased attention in recent years [ 17 , 19 ]. Only one mixed-methods study entered this review, and the qualitative aspect of this study did not, unfortunately, focus on social networks.
Third, the studies we reviewed were mostly cross-sectional, and several of the authors explicitly asked for the use of more longitudinal data (e.g., [ 10 *, 12 *, 22 *]). Fourth, another limitation of these studies that became apparent is the focus on the social gradient and the decision not to include certain socially excluded groups such as the homeless. Future studies could examine whether exploring the social networks of such groups would lead to similar conclusions.
Lastly, this research, which demonstrated how networks can buffer the detrimental health effects of having lower socio-economic status, or how networks pertain to the reproduction of health inequalities, can inform health policies in general, and health interventions more specifically. Many of the authors suggested focusing on social networks and on interventions aimed at helping socially disadvantaged individuals increase their contact with others. However, other researchers insisted that if we want to reduce health inequalities, we need to start by reducing social inequalities, given the evidence that accumulating ties that have detrimental effects on health (e.g., getting acquainted with other smokers) will not reduce health inequalities. Thus, when examining the effects of social networks on health inequalities, the role of negative ties and the negative effects of social relations on health inequalities should be considered more often.
Availability of data and materials
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Numbers sum up to more than 25 or 100 percent, respectively, because one study presented more than one analytical approach.
* Studies are part of the final selection of this scoping review
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Science Research Methodology. 2005;8:19–32. https://doi.org/10.1080/1364557032000119616 .
Article Google Scholar
*Baum FE, Ziersch AM, Zhang G, Osborne K. Do perceived neighbourhood cohesion and safety contribute to neighbourhood differences in health? Health Place. 2009;15:925–34. https://doi.org/10.1016/j.healthplace.2009.02.013 .
Berkman LF, Glass T. Social integration, social networks, social support, and health. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2000. p. 137–73.
Google Scholar
Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. https://doi.org/10.1093/oxfordjournals.aje.a112674 .
Article CAS PubMed Google Scholar
Berkman LF, Melchior M, Chastang J-F, Niedhammer I, Leclerc A, Goldberg M. Social integration and mortality: A prospective study on French employees of electricity of France-Gas of France. The GAZEL Cohort Am J Epidemiol. 2004;159:167–74. https://doi.org/10.1093/aje/kwh020 .
Article PubMed Google Scholar
Bidart C, Degenne A, Grossetti M. Living in networks. The dynamics of social relations (Structural analysis in the social sciences, Bd. 49). Cambridge: Cambridge University Press; 2020.
Böhnke P, Link S. Poverty and the dynamics of social networks. An analysis of german panel data. Eur Sociol Rev. 2017;33(4):615–32. https://doi.org/10.1093/esr/jcx063 .
Bourdieu P. The forms of capital. In: Richardson JG, editor. The Handbook of Theory: Research for the Sociology of Education. New York: Greenwood Press; 1986. p. 241–58.
*Cattell V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Sc Sci Med. 2001;52:1501–16. https://doi.org/10.1016/S0277-9536(00)00259-8 .
*Chappell NL, Funk LM. Social capital: does it add to the health inequalities debate? Soc Indic Res. 2010;99:357–73. https://doi.org/10.1007/s11205-010-9597-4 .
*Chavez R, Kemp L, Harris E. The social capital: health relationship in two disadvantaged neighbourhoods. J Health Serv Res Policy. 2004;9:29–34. https://doi.org/10.1258/1355819042349871 .
*Child ST, Walsemann KM, Kaczynski AT, Fleischer NL, Mclain AC, Moore S. Personal network characteristics and body mass index: the role of education among Black Americans. J Public Health. 2018;41:130–7. https://doi.org/10.1093/pubmed/fdy020 .
Coleman JS. Social capital in the creation of human capital. Am J Sociol. 1998;94:S95-120.
*Craveiro D. Ties and inequalities in later life: welfare state regime and the role of social networks in health inequalities in later life in Europe. Eur Soc. 2016;19:268–91. https://doi.org/10.1080/14616696.2016.1258084 .
*Craveiro D. The role of personal social networks on health inequalities across European regions. Health Place. 2017;45:24–31. https://doi.org/10.1016/j.healthplace.2017.02.007 .
DiMaggio P, Garip F. Network Effects and Social Inequality. Ann Rev Sociol. 2012;38:93–118. https://doi.org/10.1146/annurev.soc.012809.102545 .
Dominguez S, Hollstein B. Mixed Methods Social Networks Research. Cambridge University Press, Cambridge. 2014. https://doi.org/10.1017/CBO9781139227193 .
Domínguez S, Watkins C. Creating networks for survival and mobility: social capital among African-American and Latin-American low-income mothers. Soc Probl. 2003;50(1):111–35. https://doi.org/10.1525/sp.2003.50.1.111 .
Gamper M, Schoenhuth M. Visual network research (VNR)–a theoretical and methodological appraisal of an evolving field. Vis Stud. 2020;35(4):374–93. https://doi.org/10.1080/1472586X.2020.1808524 .
*Gele AA, Harsløff I. Types of social capital resources and self-rated health among the Norwegian adult population. Int J Equity Health. 2010;9. https://doi.org/10.1186/1475-9276-9-8 .
*Kamphuis CBM, Van Lenthe FJ, Giske K, Huisman M, Brug J, Mackenbach JP. Socioeconomic status, environmental and individual factors, and sports participation. Med Sci Sports Ecers. 2008;40:71–81. https://doi.org/10.1249/mss.0b013e318158e467 .
*Kim Y, Schneider T, Faß E, Lochbaum M. Personal social capital and self-rated health among middle-aged and older adults: a cross-sectional study exploring the roles of leisure-time physical activity and socioeconomic status. BMC Public Health. 2021;21:48. https://doi.org/10.1186/s12889-020-10043-6 .
Klärner A, Gamper M, Keim-Klärner S, Moor I, von der Lippe H, Vonneilich N. Social Networks and Health Inequalities. Cham: Springer International Publishing; 2022. https://doi.org/10.1007/978-3-030-97722-1 .
Book Google Scholar
Klärner A, von der Lippe H. Social Network Mechanisms. In: Klärner A, Gamper M, Keim-Klärner S, Moor I, von der Lippe H, Vonneilich N, editors. Social Networks and Health Inequalities. Cham: Springer International Publishing; 2022. p. 49–56. https://doi.org/10.1007/978-3-030-97722-1_4 .
Chapter Google Scholar
*Klein J, Vonneilich N, Baumeister SE, Kohlmann T, von dem Knesebeck O. Do social relations explain health inequalities? Evidence from a longitudinal survey in a changing eastern German region. Int J Public Health. 2012;57:619–27. https://doi.org/10.1007/s00038-012-0356-y .
*Li Y. Social mobility, social network and subjective well-being in the UK. Contemp Soc Sci. 2016;11:222–37. https://doi.org/10.1080/21582041.2016.1190860 .
Lin N. Building a Network Theory of Social Capital. Connections. 1999;22(1):28–51 http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.96.3792&rep=rep1&type=pdf .
Martin JL, Murphy JP. Networks, status, and inequality. In: Light R, Moody J, editors. The Oxford handbook of social networks (Oxford handbooks. New York NY: Oxford University Press; 2020. p. 98–115.
*McCrory C, Finuacane C, OHare C, Frewn J, Nolan H, Layte R, Kearney PM, Kenny RA. Social Disadvantage and Social Isolation Are Associated With a Higher Resting Heart Rate: Evidence From The Irish Longitudinal Study on Ageing. J Gerontol B Psychol Sci Soc Sci. 2016;71:463–73. https://doi.org/10.1093/geronb/gbu163 .
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6. https://doi.org/10.1016/j.jclinepi.2016.01.021 .
*Nemeth JM, Thomson TL, Peng J, Krebs V, Doogan NJ, Ferketich AK, Post DM, Browning CR, Paskett ED, Wewers ME. A social -contextual investigation of smoking among rural women: multilevel factors associated with smoking status and considerations for cessation. Rural Remote Health. 2018;18:4338. https://doi.org/10.22605/RRH4338 .
*Novak M, Ahlgren C, Hammarström A. A life-course approach in explaining social inequity in obesity among young adult men and women. International J Obes. 2006;30:191–200. https://doi.org/10.1038/sj.ijo.0803104 .
Pampel FC, Krueger PM, Denney JT. Socioeconomic Disparities in Health Behaviors. Ann Rev Sociol. 2010;36:349–70. https://doi.org/10.1146/annurev.soc.012809.102529 .
Pathirana TI, Jackson CA. Socioeconomic status and multimorbidity: a systematic review and meta-analysis. Aust N Z J Public Health. 2018;42:186–94. https://doi.org/10.1111/1753-6405.12762 .
Perkins JM, Subramanian SV, Christakis NA. Social networks and health: a systematic review of sociocentric network studies in low- and middle-income countries. Soc Sci Med. 2015;1982(125):60–78. https://doi.org/10.1016/j.socscimed.2014.08.019 .
Putnam R. Bowling Alone: The Collapse and Revival of American Community. New York: Simon & Schuster; 2000.
*Richards L. For Whom Money Matters Less: Social Connectedness as a Resilience Resource in the UK. Soc Indic Res. 2016;125:509–35. https://doi.org/10.1007/s11205-014-0858-5 .
Roth AR. Social networks and health in later life: a state of the literature. Sociol Health Illn. 2020;42(7):1642–56. https://doi.org/10.1111/1467-9566.13155 .
*Sabbah W, Tsakos G, Chandola T, Newton T, Kawachi I, Sheiham A, Marmot MG, Watt RG. The relationship between social network, social support and periodontal disease among older Americans. J Clin Periodontol. 2011;38:547–525. https://doi.org/10.1111/j.1600-051X.2011.01713.x .
*Schöllgen I, Huxhold O, Schüz B, Tesch-Römer C. Resources for health: differential effects of optimistic self-beliefs and social support according to socioeconomic status. Health Psychol. 2011;30:326–35. https://doi.org/10.1037/a0022514 .
Smith KP, Christakis NA. Social Networks and Health. Ann Rev Sociol. 2008;34:405–29. https://doi.org/10.1146/annurev.soc.34.040507.134601 .
*Stephens C, Alpass F, Towers A, Stevenson B. The effects of types of social networks, perceived Social Support, and loneliness on the health of older people: accounting for the social context. J Aging Health. 2011;23:887–911. https://doi.org/10.1177/0898264311400189 .
*Unger JB, McAvay G, Bruce ML, Berkmann L, Seeman T. Variation in the impact of social network characteristics on physical functioning in elderly persons: MacArthur studies of successful aging. J Gerontol B Psychol Sci Soc Sci. 1999;54:245–51. https://doi.org/10.1093/geronb/54B.5.S245 .
Valente TW. Social Networks and Health: Models, Methods, and Applications. New York: Oxford University Press; 2010.
*Veenstra G. Social capital, SES and health: an individual-level analysis. Soc Sci Med. 2000;50:619–29. https://doi.org/10.1016/S0277-9536(99)00307-X .
*Verhaeghe P, Pattyn E, Bracke P, Verhaeghe M, Van De Putte B. The association between network social capital and self-rated health: Pouring old wine in new bottles? Health & Place. 2012;18:358–65. https://doi.org/10.1016/j.healthplace.2011.11.005 .
*Vonneilich N, Jöckel KH, Erbel R, Klein J, Dragano N, Weyers S, Moebus S, Siegrist J, von dem Knesebeck O. Does socioeconomic status affect the association of social relationships and health? A moderator analysis. Int J Equity Health. 2011;10:43. https://doi.org/10.1186/1475-9276-10-43 .
*Vonneilich N, Jöckel KH, Erbel R, Klein J, Dragano N, Siegrist J, von dem Knesebeck O. The mediating effect of social relationships on the association between socioeconomic status and subjective health - results from the Heinz Nixdorf Recall cohort study. BMC Public Health. 2012;12:285. https://doi.org/10.1186/1471-2458-12-285 .
*Weyers S, Dragano N, Möbus S, Beck E, Stang A, Möhlenkamp S, Jöckel KH, Erbel R, Siegrist J. Poor social relations and adverse health behavior: stronger associations in low socioeconomic groups? Int J Public Health. 2010;55:17–23. https://doi.org/10.1007/s00038-009-0070-6 .
Zell E, Strickhouser JE, Krizan Z. Subjective social status and health: A meta-analysis of community and society ladders. Health Psychol. 2018;37:979–87. https://doi.org/10.1037/hea0000667 .
Download references
Acknowledgements
The authors would like to thank all members of the DFG research network “SoNegU” for the inspiring meetings and discussions. Special thanks are extended to Lea Ellwardt, Irene Moor, Eike Quilling, Nancy Reims and Katharina Seebaß for their contributions to reviewing articles for this paper. Emily LeCouvie Nantel was very helpful in the final polishing of the paper.
Open Access funding enabled and organized by Projekt DEAL. This publication emerged from meetings of the research network on “Social Networks and Health Inequalities”, funded by the German Research Foundation (DFG), Project number 280679966. This foundation was not involved in the preparation of this research article. We acknowledge institutional and financial support for this research by the Thuenen Institute of Rural Studies and the Medical School Berlin.
Author information
Authors and affiliations.
Thünen Institute of Rural Studies, Bundesallee 64, Brunswick, Germany
Sylvia Keim-Klärner & Andreas Klärner
Institute of Sociology, University of Technology Chemnitz, Chemnitz, Germany
Philip Adebahr
Landesfrauenrat Mecklenburg-Vorpommern e.V., Rostock, Germany
Stefan Brandt
Institut für vergleichende Bildungsforschung und Sozialwissenschaften, University of Cologne, Cologne, Germany
Markus Gamper
Rostocker Institut für Sozialforschung und gesellschaftliche Praxis e.V., Rostock, Germany
André Knabe
Institute of Social Pedagogy, Social Work and Welfare Studies, Technische Universität Dresden, Dresden, Germany
Annett Kupfer
Institute of Medical Psychology and Medical Sociology, Rostock University Medical Center, Rostock, Germany
Britta Müller
Klinik für Psychiatrie, Neurologie, Psychosomatik und Psychotherapie im Kindes- und Jugendalter, Rostock University Medical Center, Rostock, Germany
Institute of Medical Sociology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
Nico Vonneilich
MSB Medical School Berlin, Berlin, Germany
Maxi A. Ganser & Holger von der Lippe
Alumna of MSB Medical School Berlin, Berlin, Germany
Charlotte de Bruyn
You can also search for this author in PubMed Google Scholar
Contributions
All authors were involved in the reviewing process, they discussed eligibility criteria, reviewed literature regarding their eligibility and summarized the contents of the eligible studies. This work forms the basis of the results section. All authors drafted and reviewed the full manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Sylvia Keim-Klärner .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Table 6 Translating search terms into mesh terms
|
|
|---|---|
| |
health, well-being | health |
life satisfaction | no MeSH term |
illness | disease attributes |
disease, disorder | disease |
health status | health status |
health behavior | health behavior |
risk behavior | risk-taking |
coping | adaptation, psychological |
mortality | mortality |
morbidity | morbidity |
life expectancy | life expectancy |
quality of life | quality of life |
| |
social status, socioeconomic status, SES, social class, income, education, occupation, poverty, low-income, deprivation | socioeconomic factors |
prestige | social class |
wealth | - no MeSH term |
financial strain | - no MeSH term |
inequalities | socioeconomic factors, healthcare disparities |
disparities | healthcare disparities, health status disparities |
| |
social network, support network, informal network | social support |
personal network, egocentered, egonet, friendship network, egocentric network, whole network, network chart, sociogram | - no MeSH term |
|
|
- Comment: For our interest in Social Network Analysis (SNA), the MeSH terms social support and family are not sufficiently specific, therefore we did not use MeSH terms for the third topic SNA and rather performed our search with the search terms indicated above within titles and abstracts
Table 7 Data charting sheet: the 25 selected studies: study design and measurements
|
|
|
|
|
|
|
| |
|---|---|---|---|---|---|---|---|---|
1 | Baum | 2009 | cross-sectional mixed methods | 3: smoking, exercise, self-reported health | 2: education, income | 1) contact frequency 2) support 4)associational membership, reciprocity and 3 more | moderator analysis (type 1) | of aggregate measures (neighbourhood cohesion, neighbourhood safety) |
2 | Cattell | 2001 | cross-sectional, qualitative | qualitative accounts on health and wellbeing | qualitative accounts on poverty | 1) tie characteristics, contact frequency/duration 2) support given/ received 3) size, subgroups, density, homo/heterogeneity | qualitative mediator analysis | (size, density, homogeneity, reciprocity, support) |
3 | Chappell | 2010 | cross-sectional, quantitative | 3: perceived and mental health, physical function | 2: education, income | 3) size 4) trust, group membership, community activities, service use | moderator (type 1), mediator analysis | no moderating effect no mediating effect |
4 | Chavez | 2004 | cross-sectional, quantitative | 1: self-reported health | 3: housing, education, employment status | 1) family/friends in neighbourhood (bonding ties) 2) support 4) trust, local participation/ membership and 8 more | multivariate analysis | trust is of relevance for health in disadvantaged neighbourhoods |
5 | Child | 2018 | cross-sectional, quantitative | 1: BMI | 2: education, income | 1) up to three close ties, their educational level and residence 3) density | moderator analysis (type 2) | of education on the association between network (density) and health |
6 | Craveiro | 2016 | cross-sectional, quantitative | 3: chronic disease, perceived health, ADL limitation | 4: education, income, wealth, perceived income adequacy | 1) close ties, daily contact 2) support 3) size 4) social participation, network satisfaction | mediator analysis | (participation, daily contact, support); mediator effects of size only in eastern countries |
7 | Craveiro | 2017 | cross-sectional, quantitative | 3: chronic disease, perceived health, ADL limitation | 4: education, income, wealth, perceived income adequacy | 1) partner, children, daily contacts, closeness 2) support 3) size 4) participation in activities, network satisfaction | moderator analysis (type 1) | in central and southern Europe for aggregate measures (mainly: social participation, network satisfaction), not in northern Europe |
8 | Gele | 2010 | cross-sectional, quantitative | 1: self-rated health | 3: occupation, income group and education | 1)strong and weak ties, contact frequency w/ family and friends, nurses/medical doctors as friends 3)size, ethnic/gender diversity, bonding/bridging ties 4)activities in organisations | moderator analysis (type 1) | (strong ties, activities in organisations, one friend is a doctor) |
9 | Kamphuis | 2008 | cross-sectional, quantitative | 3: sports frequency, duration, intensity | 2: education, income | 3) neighbourhood network (small, medium, large) 4) social cohesion, opinion of neighbourhood, disorganisation, frequency of social gathering | mediator analysis | (network size, neighbourhood attractiveness and neighbourhood safety, social cohesion) |
10 | Kim | 2021 | cross-sectional, quantitative | 2: Self-rated health, physical activities | 2: education, income | 3) bonding and bridging ties (Personal Social Capital Scale) | moderator analysis (type 2) | of income on the association of network (bridging and bonding ties) and health |
11 | Klein | 2012 | longitudinal, quantitative | 1: self-rated health | 3: income, education, profession | 1 + 4) Social Integration Index: living with a partner, number of close ties, affiliation in associations 2) support | mediator analysis | (SII and support) |
12 | Li | 2016 | longitudinal, quantitative | 3: perceived health, happiness, satisfaction | 3: degree and employment, parents’ class | 3) size, diversity (income, age, race, education, employment, place of living, family member) 4) civic engagement, neighbourhood cohesion | mediator analysis | significant but small (size, diversity, neighbourhood cohesion, civic engagement) |
13 | McCrory | 2014 | cross-sectional, quantitative | 1: resting heartrate, | 1: household income | 1 + 4) Social Network Index: marital status, number of children, contact frequency, close relatives/friends, church group/ organisational membership 4) loneliness | mediator analysis | (SNI, loneliness) |
14 | Nemeth | 2018 | cross-sectional, quantitative | 2: smoking, depression | 3: education, income, employment status | 1) partner, persons spending time with/asking for advice, their characteristics (e.g., smoking status) 2) perceived support, social influence scale, 3) size, density, E/I index (similarity of Ego and Alter in smoking, age and education) 4) participation, neighbourhood cohesion and 3 more | multivariate analysis | perception of social acceptability of smoking, homophily on smoking and neighbourhood cohesion are associated with current smoking in a disadvantaged population, cessation interventions need to acknowledge the social context |
15 | Novak | 2006 | longitudinal, quantitative | 1: BMI | 2: occupation (parents’ and own) and education | 1) marital status, number of children, social network index, contact with parents; 2) social support index, parental support in adolescence 4) participation in associations; popularity in school | multivariate analysis | educational gradient in BMI at middle age is explained by support (men), popularity (women) in adolescence and nonparticipation in associations in young adulthood (men) |
16 | Richards | 2015 | longitudinal study, quantitative | 2: long-term illness, subjective well being | 2: financial situation, employment status | 1) friends (strong ties) 2) support in 5 dimensions (strong ties) 4) activities in organisations, their frequency (weak ties) | moderator analysis (type 1) | (weak ties, supportive strong ties) |
17 | Sabbah | 2011 | cross-sectional study, quantitative | 2: damaged teeth, paradontose | 2: education, income | 1) close friends, marital status 2) support 3) size | mediator analysis | no mediating effect |
18 | Schöllgen | 2011 | cross-sectional study, quantitative | 3: physical, functional, subjective health | 2: education, income | 2) emotional support, informational support 3) size | moderator analysis (type 2) | (supportive network) |
19 | Stephens | 2011 | cross-sectional, qualitative | 8: physical function, mental health, pain and more | 2: economic living standard, education | 1) living distance from relatives, contact frequency to family, neighbours, friends 2) support, 4) involvement in community, loneliness | multivariate analysis | social network and social support explain 33% of mental health and 15% of physical health, social gradients in health can be partially explained by social networks |
20 | Unger | 1999 | longitudinal, quantitative | 1: physical functioning | 2: education, income | 1) marital status 2) emotional and instrumental support by spouse, children, friends and relatives 3) size | moderator analysis (type 2) | no moderating effect of income on the association of networks/support and functional decline |
21 | Veenstra: | 2000 | cross-sectional, quantitative | 1: self reported health | 2: income, education | 1) contact frequency (family, workmates, neighbours…) 4) trust, religious attendance, civic participation | multivariate analysis | income and education were strongest predictors for health, social integration at work and attending religious services additionally contributed to better health |
22 | Verhaeghe | 2012 | cross-sectional, quantitative | 1: self-rated health | 3: education, occupation, social class | 1) friends, family, acquaintances w/ different occupations 2) perceived support 3) volume of social capital, occupational composition | mediator analysis | positive associations between network social capital and health beyond the influence of social class. Support only partially mediated the association of network social capital and health |
23 | Vonneilich | 2011 | longitudinal, quantitative | 2: self-rated health, depressive symptoms | 2: income, education | 1 + 4) Social Integration index: living with a partner, number of close ties, affiliation in associations 2) emotional/instrumental, perceived/received support | moderator analysis (type 2) | of SES on the association between networks (SII, support) and health |
24 | Vonneilich | 2012 | longitudinal, quantitative | 1: General subjective Health | 3: income, education | 1 + 4) Social Integration index: living with a partner, number of close ties, affiliation in associations ( 2) emotional/instrumental, perceived/received support | mediator analysis | (SII, support)—> network interventions fostering relationships can help lower SES groups to enhance health and buffer health inequalities |
25 | Weyers | 2010 | cross-sectional, quantitative | 3: smoking, nutrition, physical exercise | 2 income, education | 1) Social Integration index: living with a partner, number of close ties, affiliation in associations 2) emotional/instrumental, perceived/received support | moderator analysis (type 2) | no moderating effect; additive effect (SII, support) |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Keim-Klärner, S., Adebahr, P., Brandt, S. et al. Social inequality, social networks, and health: a scoping review of research on health inequalities from a social network perspective. Int J Equity Health 22 , 74 (2023). https://doi.org/10.1186/s12939-023-01876-9
Download citation
Received : 17 October 2022
Accepted : 28 March 2023
Published : 25 April 2023
DOI : https://doi.org/10.1186/s12939-023-01876-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social network
- Socioeconomic status
- Social support
- Scoping review
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
By continuing on our website, you agree to our use of the cookie for statistical and personalization purpose. Learn More
- Tools and Data Resources
Advanced Search
Filter your query, publication types.
Our Scorecard ranks every state’s health care system based on how well it provides high-quality, accessible, and equitable health care. Read the report to see health care rankings by state .
Area of Focus
Fund Reports
April 18, 2024
Advancing Racial Equity in U.S. Health Care

Dr. Reshma Chugani checks 7-year-old Zoe Oliver’s ears during a medical visit at Atlanta Children’s Clinical Center on September 29, 2023. Health care system performance varies widely by race and ethnicity, both within states and between states. Photo: Alyssa Pointer for the Washington Post via Getty Images
Deep-seated racial and ethnic health disparities persist across the United States, even in states with otherwise high-performing health systems
American Indians and Black Americans die at significantly higher rates from preventable and treatable causes than members of other racial and ethnic groups
- Equity Profiles by Race/Ethnicity (zip) ↓
- State Profiles (zip) ↓
- Appendices ↓
- Chartpack (pdf) ↓
- Chartpack (ppt) ↓
- News Release ↓
- Revealing Disparities: Health Care Workers’ Observations of Discrimination Against Patients
- Inequities in Health and Health Care in Black and Latinx/Hispanic Communities: 23 Charts
- Inequities in Health Insurance Coverage and Access for Black and Hispanic Adults: The Impact of Medicaid Expansion and the Pandemic
- Achieving Racial and Ethnic Equity in U.S. Health Care
- Racial and Ethnic Inequities in Health Care Coverage and Access, 2013–2019
- Gap Closed: The Affordable Care Act’s Impact on Asian Americans’ Health Coverage
- Paying for It: How Health Care Costs and Medical Debt Are Making Americans Sicker and Poorer
- The State of U.S. Health Insurance in 2022: Findings from the Commonwealth Fund Biennial Health Insurance Survey
- Six Policy Imperatives to Improve Quality, Advance Equity, and Increase Affordability
Introduction
For nearly two decades, the Commonwealth Fund has tracked health and health care in each state, seeking both to understand how the policy choices we make affect people’s health outcomes and to motivate the change needed to improve the health of all communities across the United States. But assessing how well a state performs on average can mask the profound inequities that many people experience.
This report evaluates disparities in health and health care across racial and ethnic groups, both within states and between U.S. states. We collected data for 25 indicators of health system performance, specifically focusing on health outcomes, access to health care, and quality and use of health care services for Black, white, Hispanic, American Indian and Alaska Native (AIAN), and Asian American, Native Hawaiian, and Pacific Islander (AANHPI) populations. We then produced a health system performance “score” for each of the five racial and ethnic groups in every state where we were able to make direct comparisons between those groups and between groups in other states. (For complete details on our methods, see How We Measure Performance of States’ Health Care Systems for Racial and Ethnic Groups .)
Our hope is that policymakers, health system leaders, and community stakeholders will use this tool to investigate the impact of current and past health policies on different racial and ethnic groups and to take steps to ensure an equitable health care system for the future.

Overview of Health Disparities in the United States
Profound racial and ethnic disparities in health, well-being, and life expectancy have long been the norm in the United States. These disparities are especially stark for Black and AIAN people, who live fewer years, on average, than white and Hispanic people 1 and are more likely to die from treatable conditions, more likely to die during or after pregnancy and suffer serious pregnancy-related complications, more likely to lose children in infancy, 2 and are at higher risk for many chronic health conditions, from diabetes to hypertension. 3
The COVID-19 pandemic only made things worse. Its disproportionate impact on Black, Hispanic, and AIAN people caused a sharper decline in average life expectancy since 2020 for these groups compared to white people. 4
Factors contributing to health disparities . Deep racial and ethnic disparities in health are driven by factors inside and outside state health care systems. For example, in many communities where people of color live, poverty rates are higher than average, levels of pollution and crime are elevated, and green spaces are few — all key contributors to health disparities. 5 A lack of affordable, quality health care options, meanwhile, can make it difficult to get timely treatment — a barrier that people of color disproportionately face. Black, Hispanic, and AIAN people are also less likely than other groups to have health insurance, more likely to delay care because of costs, and more likely to incur medical debt. 6 And they are less likely to have a usual source of care or to regularly receive timely preventive services like vaccinations. 7
Studies show as well that many people of color contend with interpersonal racism and discrimination in health care settings and more often receive worse medical care than white patients. 8 According to an assessment by the federal Agency for Healthcare Research and Quality (AHRQ), Black patients received worse care than white patients on 52 percent of quality measures in 2023. 9 The study also found marked disparities in quality of care and patient safety with respect to heart disease, cancer, stroke, 10 maternal health outcomes, 11 pain management, 12 and surgery. 13
The policy choices that federal, state, and local leaders have made over many decades have led to economic suppression, unequal educational access, and widespread housing segregation, all of which have contributed in their own ways to worse health outcomes for people of color. 14 While the nation’s steady and slow progress toward universal, comprehensive coverage has narrowed racial and ethnic disparities in coverage and access to care, it has not eliminated them. In particular, the 10 states that have yet to expand eligibility for Medicaid under the Affordable Care Act (ACA), have the largest coverage gaps by race and ethnicity.
A Note on the Racial and Ethnic Categories Used in This Report
None of the five racial and ethnic groups discussed in this report are homogeneous: each encompasses distinct communities with a range of cultures, experiences, socioeconomic levels, and immigration challenges. Such groupings thus conceal substantial differences, as evidenced by the great variation seen in health insurance coverage rates among Asian Americans. 15
Aggregation of these categories was necessary to obtain sufficient sample sizes for our analysis of state health system performance, but state and local stakeholders should interpret the findings within the context of their communities. Our report should be considered only as a starting point for more targeted research exploration and policy development.
Racial and ethnic disparities are pervasive across all states.
Health care system performance varies widely by race and ethnicity, both within states and between states (Exhibit 1). Mirroring national patterns, substantial health and health care disparities exist between white and Black, Hispanic, and American Indian and Alaska Native (AIAN) communities in nearly all states.
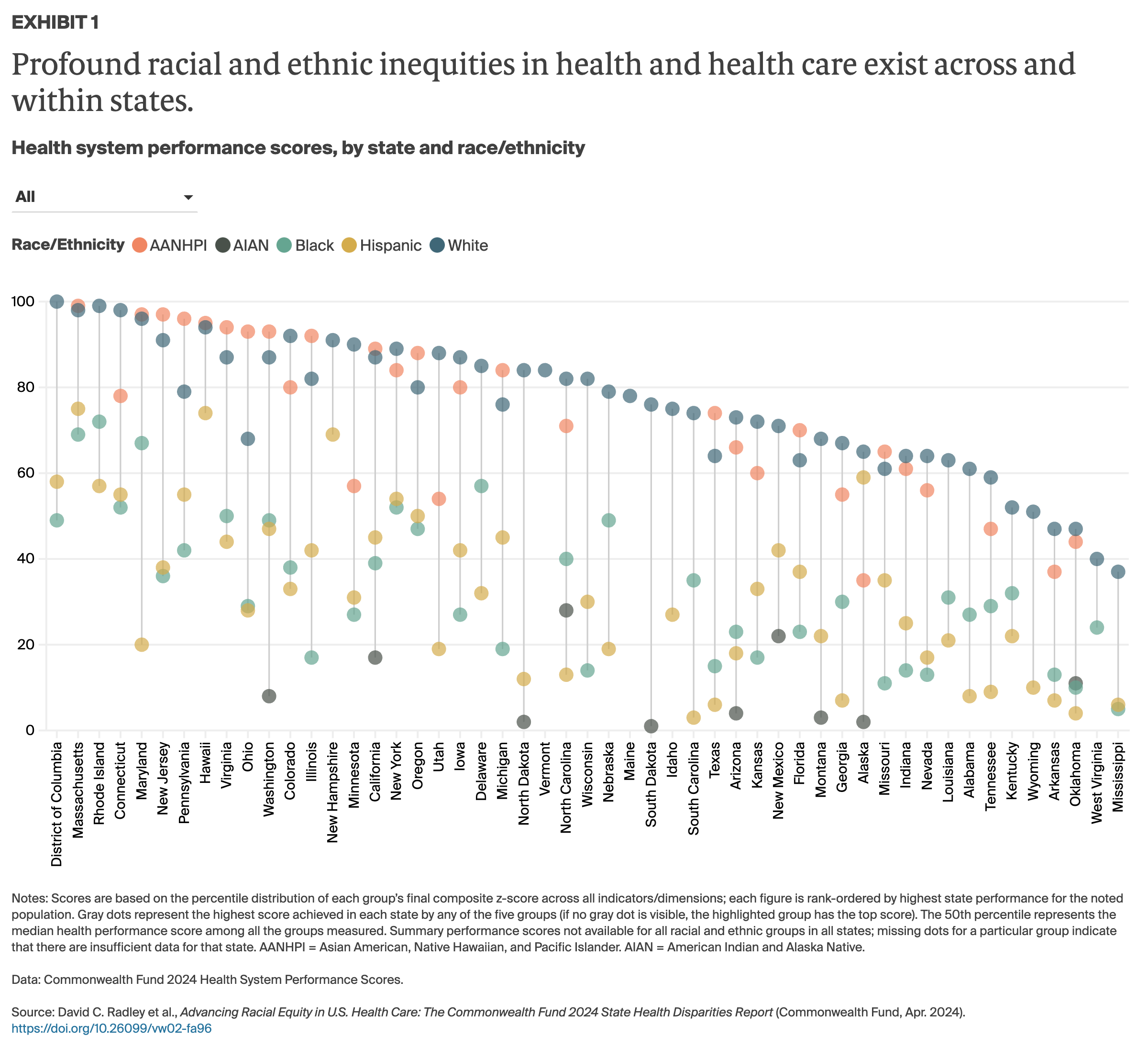
Massachusetts, Rhode Island, and Connecticut stand out for their relatively high performance for all racial and ethnic groups, 16 yet, even so, these states have considerable disparities in access to care, the quality of care people receive, and health outcomes. Health care systems in certain states, including Oklahoma, West Virginia, and Mississippi, perform poorly for all groups for which we were able to calculate overall performance scores.
Our overall health system score for each group within a state represents aggregate performance across three domains: health outcomes; health care access; and quality and use of health care services. Below we discuss findings for each of these aspects of health system performance.
Health Outcomes
Death rates and prevalence of health problems vary significantly by race and ethnicity in every state..
Health outcomes, as measured primarily by death rates and the presence of health problems, differ significantly by race and ethnicity. Historically, Black and AIAN people have had lower life expectancies compared to other groups in the U.S. They also experienced greater loss of life from COVID-19 infections. 17
We tracked deaths before age 75 from health conditions considered preventable and treatable — a measure known as “premature avoidable mortality.” This measure is highly correlated with life expectancy. 18 On average, Black people are more likely than Asian American, Native Hawaiian, and Pacific Islander (AANHPI), Hispanic, and white people to die early from avoidable causes (Exhibit 2). AIAN residents of South Dakota, Wyoming, Montana, and North Dakota had among the highest rates of any group in any state. Average premature mortality rates were lowest for AANHPI communities.
Nationally, Hispanic people generally have lower premature mortality rates compared to Black and white people, despite having higher uninsured rates and worse access to health care than these groups. It is important to note that the U.S. Hispanic population is highly diverse, and health care access and outcomes for groups within this population vary, particularly by immigration status. 19 Lower rates of premature mortality could also stem from the relative youth of U.S. Hispanic populations and their lower rates of risky health behaviors, such as smoking. 20 Nevertheless, recent research shows rising mortality and prevalence of chronic conditions over time within Hispanic populations. 21
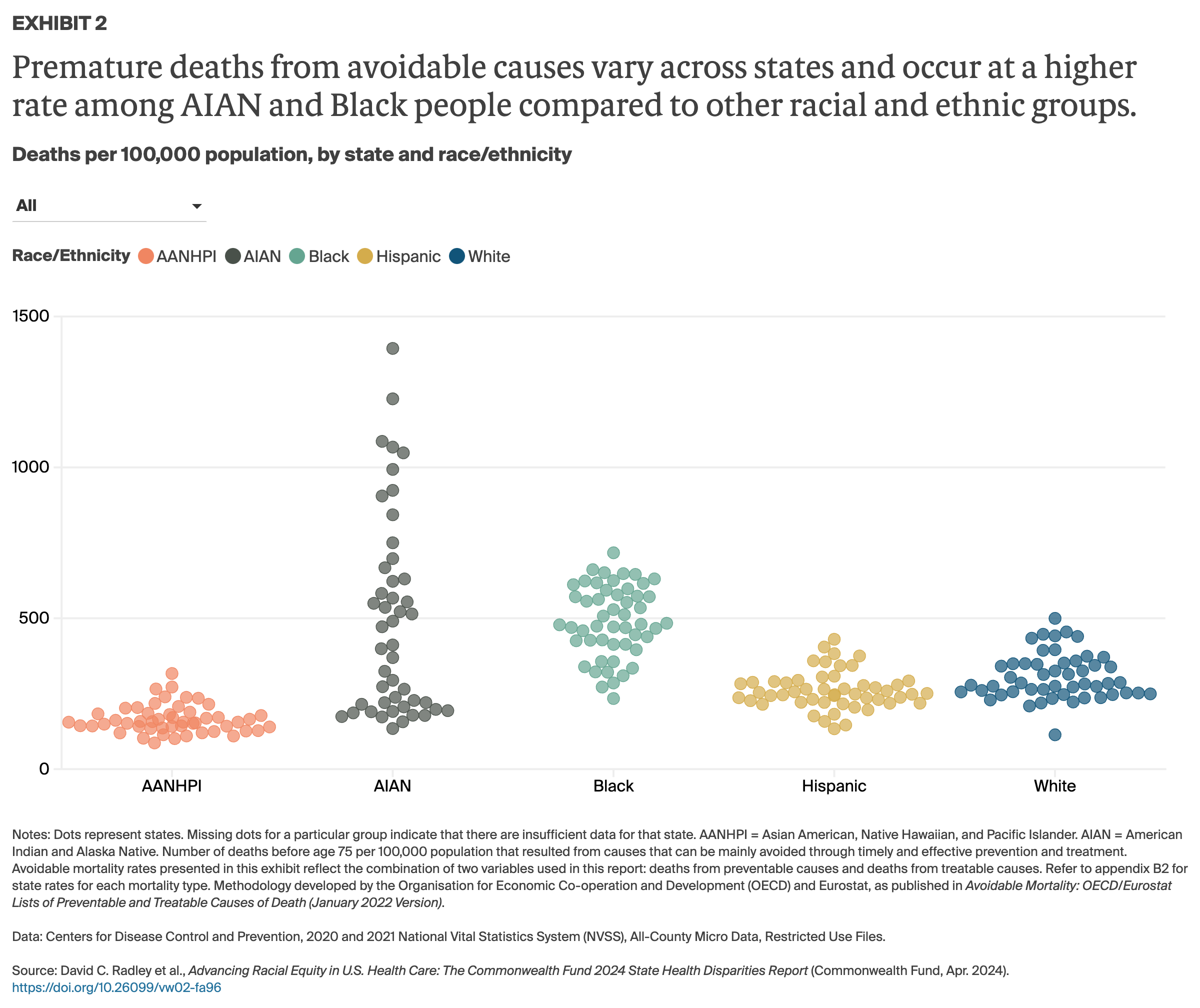
We found distinct regional patterns in premature avoidable mortality. For example:
- Preventable mortality rates are higher for both Black and white residents in several southern and south-central states — Arkansas, Mississippi, Louisiana, Tennessee, Kentucky, and Missouri — compared to most other parts of the country ( Appendix B2 ).
- For AIAN people, rates are highest in the northern plains and southwestern states ( Appendix B2 ).
- In several southwestern and mountain states, including New Mexico, Arizona, Colorado, Oklahoma, Texas, and Wyoming, premature mortality rates for Hispanic residents are higher than the low rates for that group found elsewhere in the U.S., where they align more closely with rates for white residents.
There are also sizeable disparities in mortality rates for conditions that are considered treatable. ( Appendix B2 ). Breast cancer is considered treatable when detected early but is more likely to be diagnosed at later stages among Black women, who have much higher age-adjusted death rates for the disease than other women in most states. 22 And in most areas of the U.S., infant and maternal mortality rates are highest for Black and AIAN residents, a pattern that has been documented by other studies. 23
Health Care Access
Racial and ethnic health disparities are perpetuated by less insurance coverage and unequal access to high-quality care..
Large disparities in health care access between white people and members of most other racial and ethnic groups are apparent across states. Hispanic people have the highest uninsured rates and cost-related problems in getting care.
Lack of comprehensive insurance coverage is a key contributor to disparities in access . Health insurance is essential for accessing health care. Since the Affordable Care Act (ACA) became law, the number of people with insurance has climbed steadily. The law created a federal standard for comprehensive insurance and made subsidized coverage available through marketplace plans as well as expanded Medicaid eligibility. Policy changes enacted during the COVID-19 pandemic and extended by Congress in 2022 further boosted coverage. In 2024, a record 21.3 million people enrolled in ACA marketplace plans. 24
Still, 25 million people remain uninsured, and the unwinding of the pandemic-era policy keeping people continuously enrolled in Medicaid will likely lead to an increase in that number this year as people lose their coverage. 25 Moreover, surveys indicate that a large percentage of U.S. residents with any kind of health insurance — including employer plans, which cover the majority of Americans — face high deductibles and other cost sharing that often lead to delays in care. Many people suffer negative health effects from delayed treatment. 26 Research has also found that millions of Americans who do get care struggle later to pay off medical debt.
While the ACA’s insurance expansions led to coverage gains across all racial and ethnic groups, coverage disparities remain (Exhibit 3). 27 In nearly all states, uninsured rates continue to be higher for Black, Hispanic, and AIAN residents than they are for white and AANHPI residents ( Appendix B3 ). In 2024, Hispanic and Black Americans remain disproportionally represented in the 10 states that have not taken up the ACA’s Medicaid expansion, which elsewhere has significantly reduced disparities in coverage and access.
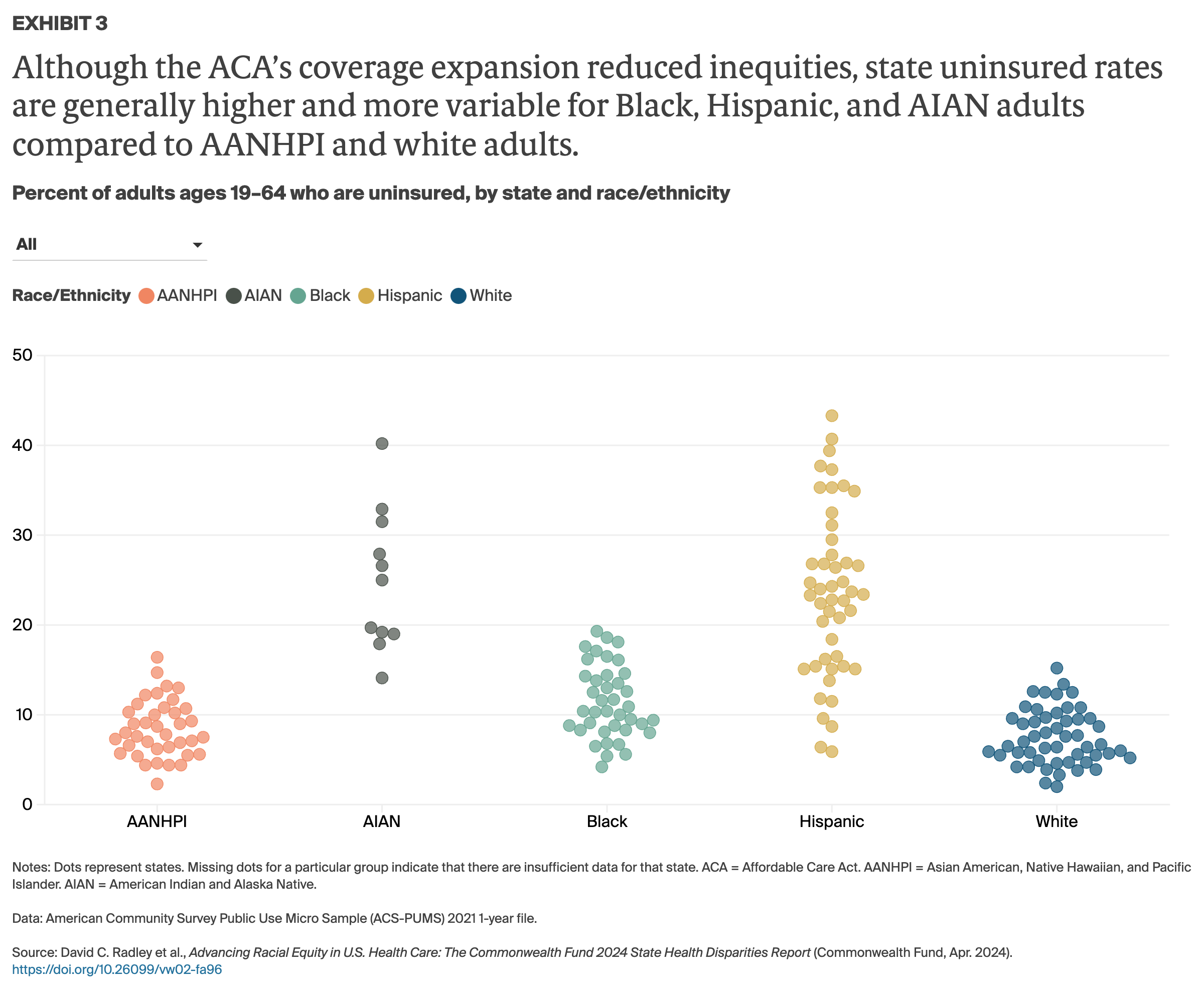
Some Hispanic and AANHPI populations continue to face immigration-related barriers to getting subsidized coverage through Medicaid or the ACA marketplaces. AIAN people also face unique access concerns related to the underfunding and limited availability of Indian Health Service (IHS) facilities as well as to socioeconomic factors and geographic barriers. 28
Being uninsured or underinsured has consequences . When people are uninsured, have gaps in coverage, or are in plans that don’t provide comprehensive coverage, they are unable to get care when they need it or have to pay high out-of-pocket costs for their care. 29 With comparatively lower incomes and fewer savings, Black, Hispanic, and AIAN people are more likely to report experiencing delays in their care or financial distress. 30
Many people of color in the U.S. are also less likely to have a usual source of care, a crucial point of first contact with the health system that helps ensure people get treatment when they need it ( Appendix B3 ). Lack of a regular care provider is associated with a lack of coverage as well as with Medicaid’s low payment rates, which limit the network of participating providers and hospitals in neighborhoods where people of color live. 31
Quality and Use of Health Care Services
Racial and ethnic disparities in care quality are driven by unequal access to and use of primary care..
Racial and ethnic disparities in quality of care and use of services have been extensively documented. 32 Across and within most states, white people overall receive better quality of care than Black, Hispanic, AIAN, and, often, AANHPI people.
Primary care clinicians play an especially critical role in providing people with high-value services, including preventive care like cancer screenings and vaccines as well as chronic disease management. In fact, when people of color have access to clinicians of the same racial background as themselves, they tend to have better health care experiences, more efficient health care utilization, and better health outcomes. 33 When there are barriers to obtaining primary care, such as costs or a lack of providers, people are more likely to get care in more intense and costly care settings, particularly an emergency department (ED). 34 For example, Black Medicare beneficiaries are more likely than white beneficiaries to be hospitalized for acute exacerbations of chronic conditions that are treatable and manageable with appropriate primary care, and they are more likely to seek and receive care in an ED for conditions that are nonurgent or can otherwise be treated in a primary care setting (Exhibit 4).
For all Medicare beneficiaries, greater use of primary care services is associated with less use of EDs for treatable conditions and fewer hospital admissions. 35
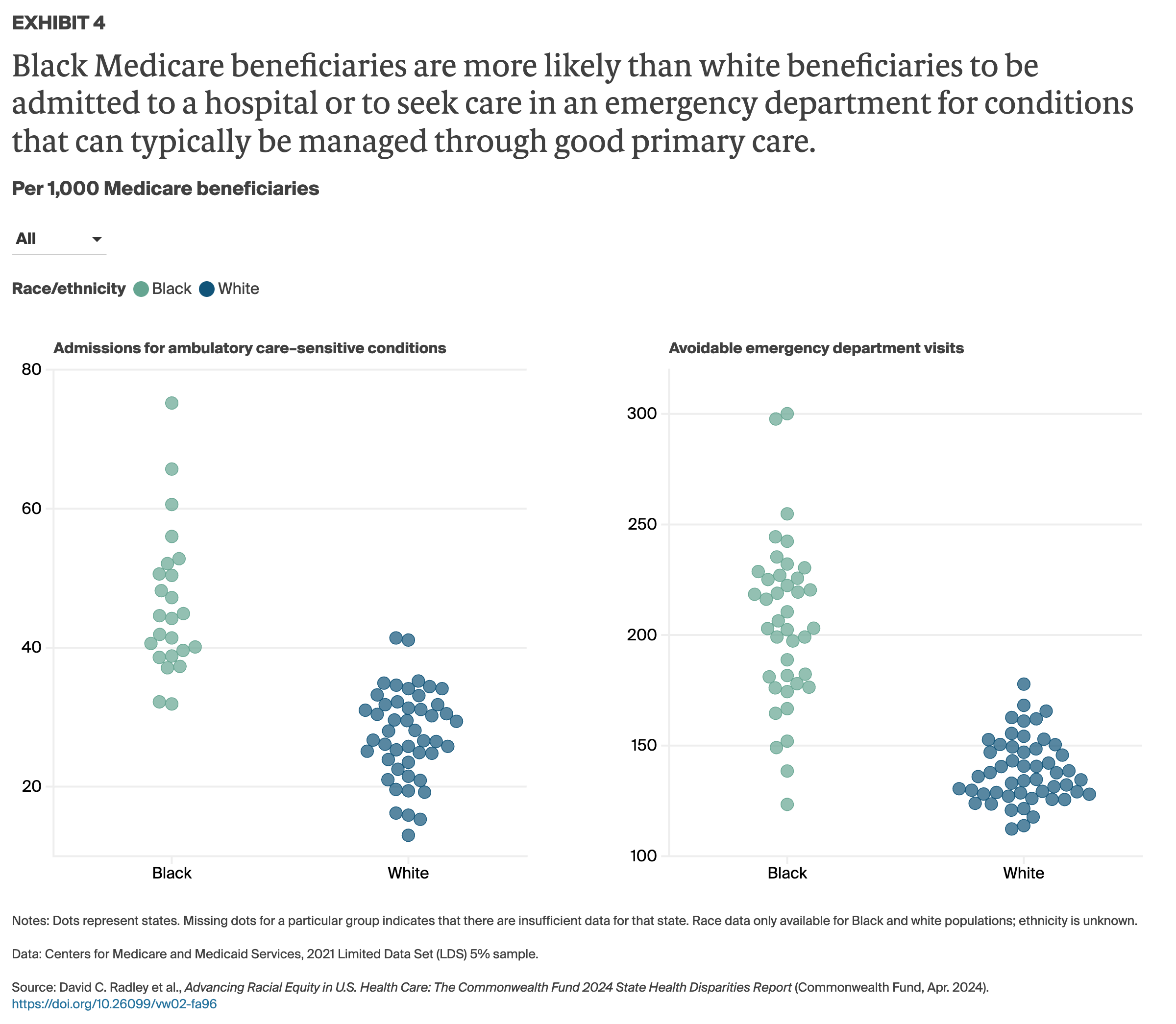
This report highlights persistent racial and ethnic disparities in health care across the United States. These disparities are fueled by inequities in access to high-quality care that affect health outcomes.
Advancing equity in health and health care should be a top priority of health care leaders and policymakers. A good start would be to identify policies that impede progress toward this goal. Leaders at the federal, state, and local levels could consider evaluating existing and emerging laws and regulations for their implications for the health of people of color. And they could pursue reforms to remedy the longstanding disparities described in this report.
To monitor trends in disparities and promote accountability, policymakers and health system leaders can support the ongoing development and use of standardized, equity-focused measures across all regulatory and performance-reporting agencies and institutions. 36 Such metrics can be used to track whether states, health systems, and health plans are reducing racial disparities in clinical outcomes, insurance coverage, access to clinicians, and other areas.
What Policy Changes Can Bridge the Gap?
Policymakers at every level of government, along with leaders in the health care sector, have many tools to make U.S. health care more equitable and to narrow persistent racial and ethnic disparities in health outcomes. Following are some options for them to consider.
Ensuring universal, affordable, and equitable health coverage . Twenty-five million people in the U.S. are still uninsured, and they are disproportionately people of color. About one-quarter of U.S. working-age adults are underinsured, facing high out-of-pocket costs and deductibles relative to their income. 37 To address these coverage gaps:
- Congress could permanently extend the enhanced marketplace premium subsidies set to expire in 2025.
- The 10 states that have yet to expand their Medicaid programs could do so. As a fallback, Congress could allow Medicaid-eligible people in the coverage gap in these states to enroll in zero-premium marketplace plans. 38
- Congress could reduce deductibles and out-of-pocket costs for marketplace insurance plans. Two options are to extend cost-sharing reduction subsidies further up the income scale and change the benchmark plan that determines the size of premium subsidies from silver to gold.
- Congress could lower immigration-related barriers to coverage. An estimated 3 million uninsured adults cannot enroll in Medicaid or subsidized marketplace plans because of their immigration status. 39 Lawmakers could allow certain groups of undocumented, low-income immigrant adults and children to enroll in Medicaid or other affordable coverage, as several states already have done. 40
- The federal government could promote more equitable treatment of enrollees in commercial insurance plans. Policymakers could require insurers to collect and report information on race and ethnicity during enrollment and make it linkable to claims data; 41 meet ACA requirements for including essential community providers in their networks; 42 and obtain health equity accreditation.
Strengthening primary care and improving the delivery of services . Predominantly Black and Hispanic communities tend to have fewer primary care providers and lower-quality health care facilities than mostly white communities. 43 To reverse these disparities, federal and state policymakers could:
- Reimburse primary care providers based on the value of care they deliver to patients. Doing so would encourage investment in health promotion, disease prevention, and chronic disease management. 44 For example, North Carolina’s Medicaid program uses a prospective payment model that emphasizes primary care–based population health management. Oregon and Washington are linking Medicaid provider payments to performance on equity measures. 45
- Offer financial incentives, such as higher reimbursement rates and/or loan repayment, to providers who serve in medically underserved communities.
- Expand training for community health workers and incorporate them in multidisciplinary care teams. As residents of the communities they serve, these individuals can help people navigate the health system to get the care they need. They can help arrange for interpretation and translation services, provide culturally appropriate health education and information, and lend other assistance. 46 Evidence shows that a community-based workforce can help improve patient-reported quality of care as well as reduce hospitalizations and 30-day readmissions. 47
- Diversify the health workforce by strengthening pipelines into the health professions for people of color and monitoring and chronicling the impact of policies on diversity in health care. 48
- Modernize medical licensing to allow health care professionals to practice across state lines. 49
Reducing inequitable administrative burdens affecting patients and providers . Americans seeking to enroll in health insurance or get health care face far higher administrative hurdles than residents of other high-income nations. 50 Recent research points to the negative impact these barriers have on access to care for lower-income individuals, including many people of color. 51 To reduce such barriers:
- Congress could create a longer period of continuous Medicaid eligibility. Disruption in Medicaid coverage because of eligibility changes, administrative errors, and other factors can leave people uninsured and unable to get care. These disruptions particularly affect people of color, given their disproportionate enrollment in Medicaid. Lawmakers could apply the lessons of the pandemic and give states the option — without having to apply for a waiver — to maintain continuous enrollment eligibility for adults for 12 months.
- Congress could create an auto-enrollment mechanism. Research shows that many uninsured people are eligible for Medicaid or subsidized marketplace coverage. By allowing auto-enrollment in comprehensive coverage, Congress could move the nation closer to universal coverage. 52
- Public and private insurers could simplify rules for quality reporting, care management, utilization review, and prior authorization programs. These programs can create unnecessary red tape, and even financial penalties, for underresourced providers of care to communities of color. Administrators could audit oversight and accountability programs for their disproportionate impact on these providers.
Investing in social services . The U.S. spends less on economic and social supports for children and working-age adults than most other high-income countries. Given the socioeconomic disadvantages these groups face, this relative lack of investment is likely contributing significantly to racial and ethnic disparities in health outcomes. 53 To remedy this inequity, federal and state policymakers could:
- Expand economic support for lower-income families, such as by expanding unemployment compensation, the Earned Income Tax Credit and child tax credit programs, and childcare, food security, and targeted wealth-building programs. 54
- Increase investment in affordable housing, public transportation, early childhood development, and affordable higher education. 55
Our measurement strategy was designed to produce a state health system performance score for each of five racial and ethnic groups in every state where direct comparisons are possible among those groups and among groups in other states. The five groups are: Black, white, Hispanic, American Indian and Alaska Native (AIAN), and Asian American, Native Hawaiian, and Pacific Islander (AANHPI).
We started by collecting data for 25 performance indicators, stratified by state and by race and ethnicity. Indicators were grouped into three domains: health outcomes, health care access, and quality and use of health care services.
Scoring method . For each of the 25 indicators, we calculate a standardized score for each state or population group with sufficient data. As an example, for adult uninsured rates, we calculate standardized scores using point estimates for 211 state racial and ethnic group pairs (e.g., 51 white, 48 Hispanic, 41 Black, 40 AANHPI, 31 AIAN) with sufficient data.
Within each performance domain, we combined indicator values to create a summary score. We then combined the domain summary scores in each state to create a composite state health system performance score for each racial and ethnic group — Black, white, AIAN, and AANHPI (non-Hispanic), and Hispanic (any race). The ability to generate these scores is dependent on having a sufficient population sample size for each indicator.
Based on the totality of composite scores, each racial or ethnic group within each state received a percentile score providing both national and state-level context on the performance of a state health system for that population. The percentile scoring, from 1 (worst) to 100 (best), reflects the observed distribution of health system performance for all groups measured in this report and enables comparisons within and across states. It is important to note that because scores are set relative to one another rather than to a predefined benchmark, there is still room for improvement in health system performance at or near the 100th percentile.
Use of racial/ethnic data categories . The five racial and ethnic data categories often group together populations with different experiences, cultures, immigration barriers, and other socioeconomic factors. This includes a wide range of culturally distinct Hispanic communities and Asian American communities. Such groupings are imperfect, as they mask significant differences. For example, past research has shown variability in health insurance coverage rates among Asian American subpopulations and between Asian Americans and Native Hawaiians or Pacific Islanders. 56
These categories are necessary, however, because they reflect the ways that populations are grouped in the data sources we drew upon for this report, and because our analysis required sufficient sample sizes. States and localities should interpret the findings within the context of their own communities, using them as a starting point to help guide more targeted research and policy solutions.
Refer to the appendices for complete study methods, list of indicators, and health system performance scores for each state and racial and ethnic population.
We owe our sincere appreciation to the researchers who developed indicators and conducted data analyses for this report. These include: Sherry Glied and Dong Ding, New York University Robert F. Wagner Graduate School of Public Service; and Caitlin Burbank, Gulcan Cil, and Shreya Roy from the Center for Evidence-Based Policy at Oregon Health & Science University. In addition, we would like to thank the four-member advisory panel who provided crucial feedback and review throughout development of the methods used in this report: Cara James, Ph.D. (Grantmakers In Health); Zinzi Bailey, Sc.D., M.S.P.H. (University of Miami Miller School of Medicine); Dolores Acevedo-Garcia, Ph.D., M.P.A.-U.R.P. (Brandeis University); and Marc Elliott, Ph.D., M.A. (RAND Corporation).
We would like to thank the following Commonwealth Fund staff members: Joseph Betancourt, Sarah Christie (health equity fellow), Melinda Abrams, and Rachel Nuzum for providing constructive feedback and guidance; and the Fund’s communications and support teams, including Chris Hollander, Bethanne Fox, Jen Wilson, Paul Frame, Sam Chase, Josh Tallman, Barry Scholl, Relebohile Masitha, Celli Horstman, Avni Gupta, Alexandra Bryan, Sara Federman, and Evan Gumas for their guidance, editorial and production support, and public dissemination efforts.
Finally, we wish to acknowledge Maya Brod of Burness for her assistance with media outreach, and the Center for Evidence-Based Policy at Oregon Health & Science University for its support of the research unit, which enabled the analysis and development of the report.
- Elizabeth Arias et al., Provisional Life Expectancy Estimates for 2020 (NVSS Vital Statistics Rapid Release no. 15, National Center for Health Statistics, July 2021); and Indian Health Service, “ Disparities Fact Sheet ,” Oct. 2019. ↩
- “ Mortality amenable to health care, deaths per 100,000 population ,” Commonwealth Fund Health Systems Data Center, n.d., and calculations from 2018–19 CDC National Vital Statistics System; Eugene Declercq and Laurie C. Zephyrin, Maternal Mortality in the United States: A Primer (Commonwealth Fund, Dec. 2020); “ Infant mortality per 1,000 live births ,” Commonwealth Fund Health Systems Data Center, n.d.; and Centers for Disease Control and Prevention, “ Infant Mortality ,” last updated Sept. 13, 2023. ↩
- Jesse C. Baumgartner et al., Inequities in Health and Health Care in Black and Latinx/Hispanic Communities: 23 Charts (Commonwealth Fund, June 2021); and IHS, “ Disparities Fact Sheet ,” 2019. ↩
- Arias et al., Provisional Life Expectancy , 2021; and Jessica Arrazola et al., “ COVID-19 Mortality Among American Indian and Alaska Native Persons — 14 States, January–June 2020 ,” Morbidity and Mortality Weekly Report 69, no. 49 (Dec. 2020): 1853–56. ↩
- Gina Kolata, “ Social Inequities Explain Racial Gaps in Pandemic, Studies Find ,” New York Times , Dec. 9, 2020; Samrachana Adhikari et al., “ Assessment of Community-Level Disparities in Coronavirus Disease 2019 (COVID-19) Infections and Deaths in Large U.S. Metropolitan Areas ,” JAMA Network Open 3, no. 7 (July 28, 2020): e2016938; and Nancy Krieger, Pamela D. Waterman, and Jarvis T. Chen, “ COVID-19 and Overall Mortality Inequities in the Surge in Death Rates by Zip Code Characteristics: Massachusetts, January 1 to May 19, 2020 ,” American Journal of Public Health 110, no. 12 (Dec. 2020): 1850–52. ↩
- Shiwani Mahajan et al., “ Trends in Differences in Health Status and Health Care Access and Affordability by Race and Ethnicity in the United States, 1999–2018 ,” JAMA 326, no. 7 (Aug. 17, 2021): 637–48; Health Insurance Coverage and Access to Care for American Indians and Alaska Natives: Current Trends and Key Challenges (ASPE, July 2021); and Jesse C. Baumgartner, Sara R. Collins, and David C. Radley, Inequities in Health Insurance Coverage and Access for Black and Hispanic Adults: The Impact of Medicaid Expansion and the Pandemic (Commonwealth Fund, Mar. 2023). ↩
- Mahajan et al., “ Trends in Differences ,” 2021; Jesse C. Baumgartner, Sara R. Collins, and David C. Radley, Racial and Ethnic Inequities in Health Care Coverage and Access, 2013–2019 (Commonwealth Fund, June 2021); and Jesse C. Baumgartner et al., How Prepared Are States to Vaccinate the Public Against COVID-19? Learning from Influenza and H1N1 Vaccination Programs (Commonwealth Fund, Dec. 2020). ↩
- Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, eds., Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (Institute of Medicine, 2003); Kiran Clair et al., “ Disparities by Race, Socioeconomic Status, and Insurance Type in the Receipt of NCCN Guideline-Concordant Care for Select Cancer Types in California ,” Journal of Clinical Oncology 38, no. 15 suppl. (May 2020): 7031; and William L. Schpero et al., “ For Selected Services, Blacks and Hispanics More Likely to Receive Low-Value Care Than Whites ,” Health Affairs 36, no. 6 (June 2017): 1065–69. ↩
- Agency for Healthcare Research and Quality, 2023 National Healthcare Quality and Disparities Report Appendixes , AHRQ Pub. No. 23(24)-0091-EF (AHRQ, Dec. 2023). ↩
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, eds., Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (National Academies Press, 2003). ↩
- Madeline Y. Sutton et al., “ Racial and Ethnic Disparities in Reproductive Health Services and Outcomes, 2020 ,” Obstetrics and Gynecology 137, no. 2 (Feb. 2021): 225–33. ↩
- Kelly M. Hoffman et al., “ Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs About Biological Differences Between Blacks and Whites ,” Proceedings of the National Academy of Sciences 113, no. 16 (Apr. 19, 2016): 4296–301. ↩
- Matthew J. Best et al., “ Racial Disparities in the Use of Surgical Procedures in the U.S. ,” JAMA Surgery 156, no. 3 (Mar. 2021): 274–81. ↩
- Zinzi D. Bailey, Justin M. Feldman, and Mary T. Bassett, “ How Structural Racism Works — Racist Policies as a Root Cause of U.S. Racial Health Inequities ,” New England Journal of Medicine 384, no. 8 (Feb. 25, 2021): 768–73; and Jamila Taylor, Racism, Inequality, and Health Care for African Americans (Century Foundation, Dec. 2019). ↩
- Munira Z. Gunja et al., Gap Closed: The Affordable Care Act’s Impact on Asian Americans’ Health Coverage (Commonwealth Fund, July 2020). ↩
- These states performed comparatively well for all race and ethnicity groups for which there were sufficient data to support the calculation of performance scores; for AIAN residents in Connecticut, Massachusetts, and Rhode Island, we were not able to calculate a performance score, nor were we able to calculate one for AANHPI residents in Rhode Island. ↩
- Elizabeth Arias et al., Mortality Profile of the Non-Hispanic American Indian or Alaska Native Population, 2019 (National Vital Statistics Reports, vol. 70, no. 12, Nov. 2021); GBD U.S. Health Disparities Collaborators, “ Life Expectancy by County, Race, and Ethnicity in the USA, 2000–19: A Systematic Analysis of Health Disparities ,” The Lancet 400, no. 10345 (July 2, 2022): 25–38; and Elizabeth Arias et al., Provisional Life Expectancy Estimates for 2021 (NVSS Vital Statistics Rapid Release no. 23, National Center for Health Statistics, Aug. 2022). ↩
- The correlation between mortality amenable to health care and life expectancy holds for all racial and ethnic groups analyzed in this report. Commonwealth Fund analysis using 2018 and 2019 data from the Centers for Disease Control and Prevention’s National Vital Statistics System (NVSS); and 2021 County Health Rankings: Data and Documentation (University of Wisconsin Population Health Institute). See also: Stephen C. Schoenbaum et al., “ Mortality Amenable to Health Care in the United States: The Roles of Demographics and Health Systems Performance ,” Journal of Public Health Policy 32, no. 4 (Nov. 2011): 407–29; and Margaret E. Kruk et al., “ Mortality Due to Low-Quality Health Systems in the Universal Health Coverage Era: A Systematic Analysis of Amenable Deaths in 137 Countries ,” The Lancet 392, no. 10160 (Nov. 17, 2018): 2203–12. ↩
- Luisa N. Borrell, “ Hispanic Health Is Not Homogenous ,” podcast, season 7, episode 4, National Patient Advocate Foundation; Kimberly D. Miller et al., “ Cancer Statistics for Hispanics/Latinos, 2018 ,” CA: A Cancer Journal for Clinicians 68, no. 6 (Nov./Dec. 2018): 425–45; and Eduardo Velasco-Mondragon et al., “ Hispanic Health in the USA: A Scoping Review of the Literature ,” Public Health Reviews 37 (Dec. 2016): 31. ↩
- Velasco-Mondragon et al., “ Hispanic Health ,” 2016; and Lourdes Medrano, “ The ‘Hispanic Paradox’: Does a Decades-Old Finding Still Hold Up? ,” American Heart Association News , May 10, 2023. ↩
- Steven H. Woolf et al., “ Changes in Midlife Death Rates Across Racial and Ethnic Groups in the United States: Systematic Analysis of Vital Statistics ,” BMJ 362 (Aug. 2018): k3096. ↩
- Clement G. Yedjou et al., “ Health and Racial Disparity in Breast Cancer ,” in Breast Cancer Metastasis and Drug Resistance. Advances in Experimental Medicine and Biology (Springer, 2019). ↩
- Declercq and Zephyrin, Maternal Mortality Primer , 2020; “ Infant mortality per 1,000 live births ,” Commonwealth Fund Health Systems Data Center, n.d.; Danielle M. Ely and Anne K. Driscoll, Infant Mortality in the United States, 2018: Data from the Period Linked Birth/Infant Death File (National Vital Statistics Reports, vol. 69, no. 7, July 2020); and Gopal K. Singh and Stella M. Yu, “ Infant Mortality in the United States, 1915–2017: Large Social Inequalities Have Persisted for Over a Century ,” International Journal of Maternal and Child Health and AIDS 8, no. 1 (2019): 19–31. ↩
- “ Historic 21.3 Million People Choose ACA Marketplace Coverage ,” press release, Centers for Medicare and Medicaid Services, Jan. 24, 2024. ↩
- Brian Tsai, “ U.S. Uninsured Rate Hits Record Low in First Quarter of 2023 ,” NCHS: A Blog of the National Center for Health Statistics , Aug. 3, 2023; Sara Rosenbaum and MaryBeth Musumeci, “ The Broader Policy Implications of the Medicaid Unwinding Crisis ,” To the Point (blog), Commonwealth Fund, Nov. 28, 2023; and KFF, “ Medicaid Enrollment and Unwinding Tracker ,” Feb. 2024. ↩
- Sara R. Collins, Shreya Roy, and Relebohile Masitha, Paying for It: How Health Care Costs and Medical Debt Are Making Americans Sicker and Poorer — Findings from the Commonwealth Fund 2023 Health Care Affordability Survey (Commonwealth Fund, Oct. 2023). ↩
- Baumgartner, Collins, and Radley, Inequities in Health Insurance Coverage , 2023. ↩
- Mark Walker, “ For Tribal Members in Oklahoma, Medicaid Expansion Improves Access to Specialty Care ,” New York Times, Sept. 22, 2021; Eric Whitney, “ Native Americans Feel Invisible In U.S. Health Care System ,” NPR, Dec. 12, 2017; Medicaid and CHIP Payment and Access Commission, Medicaid’s Role in Health Care for American Indians and Alaska Natives (MACPAC, Feb. 2021); and Office of Minority Health, “ American Indian/Alaska Native Health ,” U.S. Department of Health and Human Services, n.d. ↩
- Sara R. Collins, Munira Z. Gunja, and Gabriella N. Aboulafia, U.S. Health Insurance Coverage in 2020: A Looming Crisis in Affordability — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2020 (Commonwealth Fund, Aug. 2020). ↩
- William Darity Jr. et al., What We Get Wrong About Closing the Racial Wealth Gap (Duke University, Samuel Dubois Cook Center on Social Equity, Apr. 2018); “ Individuals with high out-of-pocket medical spending ,” Commonwealth Fund Health Systems Data Center, n.d.; and Sara R. Collins, Gabriella N. Aboulafia, and Munira Z. Gunja, As the Pandemic Eases, What Is the State of Health Care Coverage and Affordability in the U.S.? — Findings from the Commonwealth Fund Health Care Coverage and COVID-19 Survey, March–June 2021 (Commonwealth Fund, July 2021). ↩
- Cindy Mann and Adam Striar, “ How Differences in Medicaid, Medicare, and Commercial Health Insurance Payment Rates Impact Access, Health Equity, and Cost ,” To the Point (blog), Commonwealth Fund, Aug. 17, 2022; Roosa S. Tikkanen et al., “ Hospital Payer and Racial/Ethnic Mix at Private Academic Medical Centers in Boston and New York City ,” International Journal of Health Services 47, no. 3 (July 2017): 460–76; Elizabeth J. Brown et al., “ Racial Disparities in Geographic Access to Primary Care in Philadelphia ,” Health Affairs 35, no. 8 (Aug. 2016): 1374–81; Darrell J. Gaskin et al., “ Residential Segregation and the Availability of Primary Care Physicians ,” Health Services Research 47, no. 6 (Dec. 2012): 2353–76; and Emily P. Terlizzi et al., “ Reported Importance and Access to Health Care Providers Who Understand or Share Cultural Characteristics with Their Patients Among Adults, by Race and Ethnicity ,” HHS National Health Statistics Reports 130 (Oct. 8, 2019). ↩
- Agency for Healthcare Research and Quality, 2022 National Healthcare Quality and Disparities Report (AHRQ, 2022). ↩
- John E. Snyder et al., “ Black Representation in the Primary Care Physician Workforce and Its Association with Population Life Expectancy and Mortality Rates in the U.S. ,” JAMA Network Open 6, no. 4 (Apr. 14, 2023): e236687. ↩
- Jody A. Vogel et al., “ Reasons Patients Choose the Emergency Department over Primary Care: A Qualitative Metasynthesis ,” Journal of General Internal Medicine 34, no. 11 (Nov. 2019): 2610–19. ↩
- Correlation between primary care spending, expressed as a share of total per beneficiary spending, and hospital admissions for primary care–sensitive conditions was stronger among Black beneficiaries (r = –0.49) than among white beneficiaries (r = –0.22). Similarly, higher levels of primary care spending were associated with lower levels of emergency department use for nonemergent conditions, with a stronger correlation among Black beneficiaries (r = –0.40) than white beneficiaries (r = –0.24). ↩
- Sherita Hill Golden and Neil R. Powe, “ Hospital Equity Rating Metrics — Promise, Pitfalls, and Perils ,” JAMA Health Forum 4, no. 10 (Oct. 13, 2023): e233188. ↩
- Sara R. Collins, Lauren A. Haynes, and Relebohile Masitha, The State of U.S. Health Insurance in 2022: Findings from the Commonwealth Fund Biennial Health Insurance Survey (Commonwealth Fund, Sept. 2022). ↩
- Collins, Roy, and Masitha, Paying for It , 2023. ↩
- Sara R. Collins and Gabriella N. Aboulafia, “ Will the American Rescue Plan Reduce the Number of Uninsured Americans? ,” To the Point (blog), Commonwealth Fund, Mar. 22, 2021. ↩
- Katherine Rizzolo et al., “ Access to Kidney Care for Undocumented Immigrants Across the United States ,” Annals of Internal Medicine 176, no. 6 (June 2023): 877–79; Melody Gutierrez, “ California Expands Medi-Cal, Offering Relief to Older Immigrants Without Legal Status ,” Los Angeles Times , July 27, 2021; and Justin Giovannelli and Rachel Schwab, “ States Expand Access to Affordable Private Coverage for Immigrant Populations ,” To the Point (blog), Commonwealth Fund, Feb. 8, 2024. ↩
- Kevin McAvey and Alisha Reginal, Unlocking Race and Ethnicity Data to Promote Health Equity in California: Proposals for State Action (Manatt Health, Apr. 2021). ↩
- Katie Keith, “ How Insurers Can Advance Health Equity Under the Affordable Care Act ,” To the Point (blog), Commonwealth Fund, Aug. 10, 2021. ↩
- Brown et al., “ Racial Disparities ,” 2016; Gaskin et al., “ Residential Segregation ,” 2012; and Elizabeth A. Howell et al., “ Black–White Differences in Severe Maternal Morbidity and Site of Care ,” American Journal of Obstetrics and Gynecology 214, no. 1 (Jan. 2016): 122. e1–122.e7. ↩
- Diane Alexander and Molly Schnell, The Impacts of Physician Payments on Patient Access, Use, and Health , Working Paper 26095 (National Bureau of Economic Research, July 2019, revised Aug. 2020); and Commonwealth Fund Task Force on Payment and Delivery System Reform, Six Policy Imperatives to Improve Quality, Advance Equity, and Increase Affordability (Commonwealth Fund, Nov. 2020). ↩
- Mandy Cohen et al., “ Buying Health, Not Just Health Care: North Carolina’s Pilot Effort ,” To the Point (blog), Commonwealth Fund, Jan. 27, 2020; and Sophia Tripoli et al., “ To Advance Health Equity, Federal Policy Makers Should Build on Lessons from State Medicaid Experiments ,” Health Affairs Forefront (blog), Apr. 14, 2021. ↩
- National Heart, Lung, and Blood Institute, “ Role of Community Health Workers ,” National Institutes of Health, last updated June 2014. ↩
- Shreya Kangovi et al., “ Effect of Community Health Worker Support on Clinical Outcomes of Low-Income Patients Across Primary Care Facilities: A Randomized Clinical Trial ,” JAMA Internal Medicine 178, no. 12 (Dec. 2018): 1635–43. ↩
- Laurie C. Zephyrin, Josemiguel Rodriguez, and Sara Rosenbaum, “ The Case for Diversity in the Health Professions Remains Powerful ,” To the Point (blog), Commonwealth Fund, July 20, 2023. ↩
- Commonwealth Fund, Six Policy Imperatives , 2020; Donnie L. Bell and Mitchell H. Katz, “ Modernize Medical Licensing, and Credentialing, Too — Lessons From the COVID-19 Pandemic ,” JAMA Internal Medicine 181, no. 3 (Jan. 13, 2021): 312–15. ↩
- Eric C. Schneider et al., Mirror, Mirror 2021 — Reflecting Poorly: Health Care in the U.S. Compared to Other High-Income Countries (Commonwealth Fund, Aug. 2021). ↩
- Michael Anne Kyle and Austin B. Frakt, “ Patient Administrative Burden in the U.S. Health Care System ,” Health Services Research 56, no. 5 (Oct. 2021): 755–65. ↩
- Linda J. Blumberg, John Holahan, and Jason Levitis, How Auto-Enrollment Can Achieve Near-Universal Coverage: Policy and Implementation Issues (Commonwealth Fund, June 2021) . ↩
- Roosa S. Tikkanen and Eric C. Schneider, “ Social Spending to Improve Population Health — Does the United States Spend as Wisely as Other Countries? ,” New England Journal of Medicine 382, no. 10 (Mar. 5, 2020): 885–87. ↩
- Oxfam America, The Best and Worst States to Work in America – During COVID-19 (Oxfam, Aug. 2020); Erica Williams, Samantha Waxman and Julian Legendre, States Can Adopt or Expand Earned Income Tax Credits to Build a Stronger Future Economy (Center on Budget and Policy Priorities, Mar. 2020); and Shera Avi-Yonah and Danielle Moran, “ NYC, Connecticut Start ‘Baby Bond’ Programs to Shrink Inequality ,” Bloomberg , July 8, 2021. ↩
- Schneider et al., Mirror, Mirror , 2021. ↩
- Gunja et al., Gap Closed , 2020. ↩
Publication Details
David C. Radley, Senior Scientist, Tracking Health System Performance, The Commonwealth Fund
David C. Radley et al., Advancing Racial Equity in U.S. Health Care: The Commonwealth Fund 2024 State Health Disparities Report (Commonwealth Fund, Apr. 2024). https://doi.org/10.26099/vw02-fa96
- Advancing Health Equity
Race Based Disparities , State Health Policy , Health Equity
Related Content

Stressors Stack Up on Essential Maternity Providers — Community Health Centers Need Support in a Post-Dobbs World
blog / Jun 11, 2024

A Community-Led Approach to Transforming Maternity Care
publication / Jun 07, 2024

Insights into the U.S. Maternal Mortality Crisis: An International Comparison
Issue Briefs / Jun 04, 2024
The independent source for health policy research, polling, and news.
Disparities in Health and Health Care: 5 Key Questions and Answers
Nambi Ndugga and Samantha Artiga Published: Apr 21, 2023
Introduction
The COVID-19 pandemic and nationwide racial justice movement over the past several years have heightened the focus on health disparities and their underlying causes and contributed to the increased prioritization of health equity. These disparities are not new and reflect longstanding structural and systemic inequities rooted in racism and discrimination. Although growing efforts have focused recently on addressing disparities, the ending of some policies implemented during the COVID-19 pandemic, including continuous enrollment for Medicaid and the Children’s Health Insurance Program (CHIP), may reverse progress and widen disparities. Addressing health disparities is not only important from an equity standpoint, but also for improving the nation’s overall health and economic prosperity. This brief provides an introduction to what health and health care disparities are, why it is important to address disparities, what the status of disparities is today, recent federal actions to address disparities, and key issues related to addressing disparities looking ahead.
What are health and health care disparities?
Health and health care disparities refer to differences in health and health care between groups that stem from broader inequities . There are multiple definitions of health disparities. Healthy People 2030 defines a health disparity, as “a particular type of health difference that is linked with social, economic, and/or environmental disadvantage,” and that adversely affects groups of people who have systematically experienced greater obstacles to health. The Centers for Disease Control and Prevention (CDC) defines health disparities as, “preventable differences in the burden, disease, injury, violence, or in opportunities to achieve optimal health experienced by socially disadvantaged racial, ethnic, and other population groups and communities.” A health care disparity typically refers to differences between groups in health insurance coverage, affordability, access to and use of care, and quality of care. The terms “health inequality” and “inequity” are also sometimes used to describe unjust differences. Racism, which the CDC defines as the structures, policies, practices, and norms that assign value and determine opportunities based on the way people look or the color of their skin, results in conditions that unfairly advantage some and disadvantage others, placing people of color at greater risk for poor health outcomes.
Health equity generally refers to individuals achieving their highest level of health through the elimination of disparities in health and health care. Healthy People 2030 defines health equity as the attainment of the highest level of health for all people and notes that it requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and health and health care disparities. The CDC describes health equity as when everyone has the opportunity to be as healthy as possible.
A broad array of factors within and beyond the health care system drive disparities in health and health care (Figure 1) . Though health care is essential to health, research shows that health outcomes are driven by multiple factors, including underlying genetics, health behaviors, social and environmental factors, and access to health care. While there is currently no consensus in the research on the magnitude of the relative contributions of each of these factors to health, studies suggest that health behaviors and social and economic factors, often referred to as social determinants of health , are the primary drivers of health outcomes and that social and economic factors shape individuals’ health behaviors. Moreover, racism negatively affects mental and physical health both directly and by creating inequities across the social determinants of health.
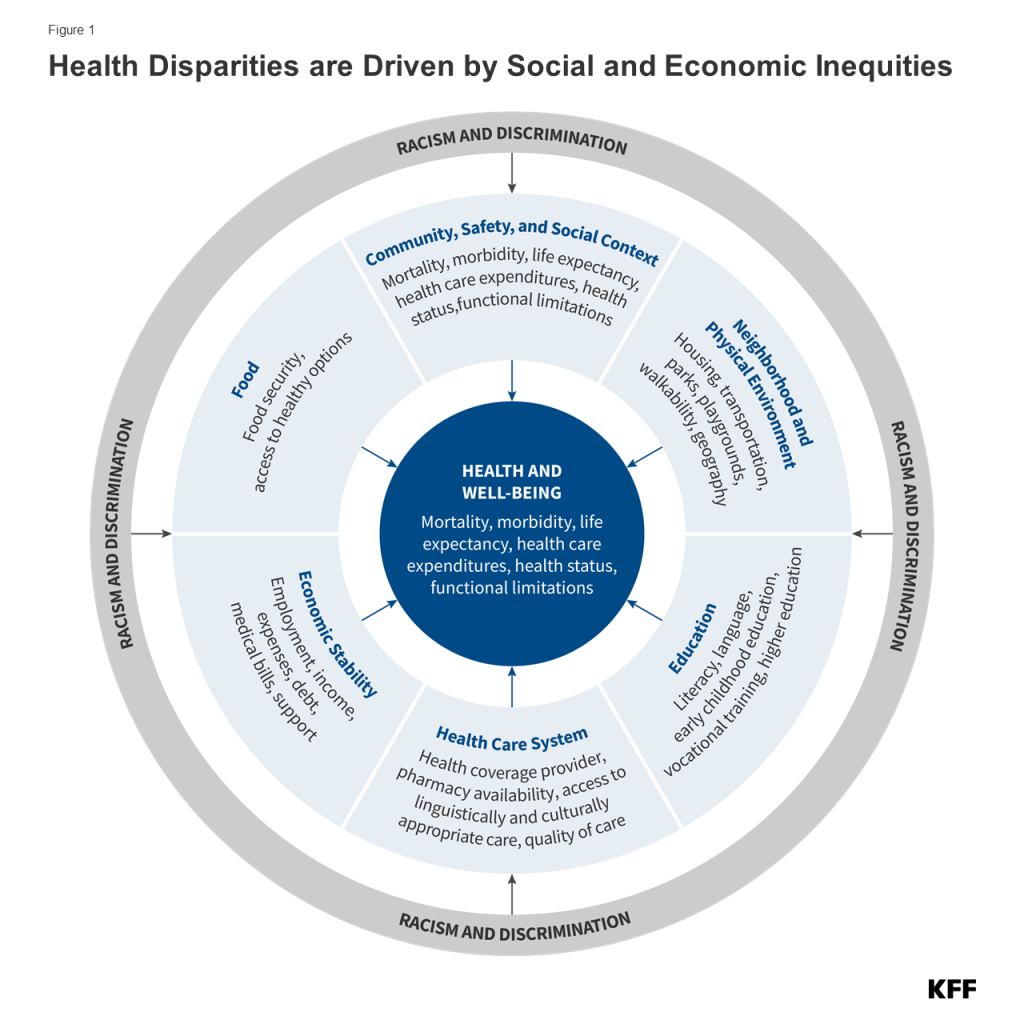
Health and health care disparities are often viewed through the lens of race and ethnicity, but they occur across a broad range of dimensions. For example, disparities occur across socioeconomic status, age, geography, language, gender, disability status, citizenship status, and sexual identity and orientation. Research also suggests that disparities occur across the life course, from birth, through mid-life, and among older adults. Federal efforts to reduce disparities focus on designated priority populations , including, “members of underserved communities: Black, Latino, and Indigenous and Native American persons, Asian Americans and Pacific Islanders and other persons of color; members of religious minorities; lesbian, gay, bisexual, transgender, and queer (LGBT+) persons; persons with disabilities; persons who live in rural areas; and persons otherwise adversely affected by persistent poverty or inequality.” These groups are not mutually exclusive and often intersect in meaningful ways. Disparities also occur within subgroups of populations. For example, there are differences among Hispanic people in health and health care based on length of time in the country, primary language, and immigration status . Data often also mask underlying disparities among subgroups within the Asian population.
Why is it important to address disparities?
Addressing disparities in health and health care is important not only from an equity standpoint but also for improving the nation’s overall health and economic prosperity . People of color and other underserved groups experience higher rates of illness and death across a wide range of health conditions, limiting the overall health of the nation. Research further finds that health disparities are costly, resulting in excess medical care costs and lost productivity as well as additional economic losses due to premature deaths each year.
What is the status of disparities today?
Disparities in health and health care are persistent and prevalent. Major recognition of health disparities began more than three decades ago with the Report of the Secretary’s Task Force on Black and Minority Health (Heckler Report) in 1985, which documented persistent health disparities that accounted for 60,000 excess deaths each year and synthesized ways to advance health equity. The Heckler Report led to the creation of the U.S. Department of Health and Human Services Office of Minority Health and influenced federal recognition of and investment in many aspects of health equity. In 2003, the Institute of Medicine’s Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care released the report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care , which identified systemic racism as a major cause of health disparities in the United States. Despite the recognition and documentation of disparities for decades and overall improvements in population health over time, many disparities have persisted, and, in some cases, widened over time.
Beyond coverage, people of color and other marginalized and underserved groups continue to experience many disparities in accessing and receiving care . For example, people in rural areas face barriers to accessing care due to low density of providers and longer travel times to care, as well as more limited access to health coverage. There also are inequities in experiences receiving health care across groups. For example, the KFF/The Undefeated 2020 Survey on Race and Health , found that one in five Black adults and one in five Hispanic adults report being treated unfairly treatment due to their race or ethnicity while getting health care for themselves or a family member in the past year. Nearly one-quarter (24%) of Hispanic adults and over one in three (34%) potentially undocumented Hispanic adults reported that it was very or somewhat difficult to find a doctor who explains this in a way that is easy to understand in a 2021 KFF survey. Other KFF survey data from 2022 found that nearly one in ten (9%) of nonelderly adult women who visited a health care provider in the past two years said they experienced discrimination because of their age, gender, race, sexual orientation, religion, or some other personal characteristic during a health care visit. KFF data also showed that LGBT+ people were more likely than their non-LGBT+ counterparts to report certain negative experiences while getting health care, including a doctor not believing they were telling the truth, suggesting they are personally to blame for a health problem, assuming something about them without asking, and/or dismissing their concerns. The 2023 KFF/The Washington Post Trans Survey found that trans adults were more likely to report having difficulty finding affordable health care or a provider who treated them with dignity and respect compared to cisgender adults.
The COVID-19 pandemic has taken a disproportionate toll on the health and well-being of people of color and other underserved groups. Cumulative age-adjusted data showed that AIAN and Hispanic people have had a higher risk for COVID-19 infection and AIAN, Hispanic, and Black people have had a higher risk for hospitalization and death due to COVID-19. Beyond these direct health impacts, the pandemic has negatively impacted the mental health, well-being, and social and economic factors that drive health for people of color and other underserved groups, including LGBT+ people . As such, the pandemic may contribute to worsening health disparities going forward.
Concerns about mental health and substance use have increased since the onset of the pandemic, particularly among some groups. According to a 2022 KFF/CNN survey , 90% of the public think there is a mental health crisis in the U.S. today. Over the course of the pandemic, many adults reported symptoms consistent with anxiety and depression. Additionally, drug overdose deaths have sharply increased – largely due to fentanyl – and after a brief period of decline, suicide deaths are once again on the rise. These negative mental health and substance use outcomes have disproportionately affected some populations, particularly communities of color and youth. Drug overdose death rates were highest among AIAN and Black people as of 2021. Alcohol-induced death rates increased substantially during the pandemic, with rates increasing the fastest among people of color and people living in rural areas. From 2019 to 2021, many people of color experienced a larger growth in suicide death rates compared to their White counterparts. Additionally, self-harm and suicidal ideation has increased faster among adolescent females compared to their male peers. Findings from a 2023 KFF/The Washington Post survey found that more trans adults reported struggling with serious mental health issues compared to cisgender adults and were six times as likely as cisgender adults to have engaged in self-harm in the previous year (17% vs. 3%). There are also substantial disparities in mental health, including suicidality, among LGBT+ youth compared to their non-LGBT+ peers.
What are recent federal actions to address disparities?
In the wake of the COVID-19 pandemic, there has been a heightened awareness of and focus on addressing health disparities. The disparate impacts of COVID-19 and coinciding racial reckoning following the police killing of George Floyd contributed to a growing awareness of racial disparities in health and their underlying causes, including racism. Early in his presidency, President Biden issued a series of executive orders focused on advancing health equity, including orders that outlined equity as a priority for the federal government broadly and as part of the pandemic response and recovery efforts . Federal agencies were directed with developing Equity Action Plans that outlined concrete strategies and commitments to addressing systemic barriers across the federal government. In its Health Equity Plan, the Department of Health and Human Services (HHS) outlined a series of new strategies, including addressing increased pregnancy and postpartum morbidity and mortality among Black and AIAN women; addressing barriers that individuals with limited English proficiency face in obtaining information, services, and benefits from HHS programs; leveraging grants to incorporate equity consideration into funding opportunities, implementing equity assessments across its major policies and programs; investing in resources to advance civil rights; and expanding contracting opportunities for small, disadvantaged businesses. The plan builds on earlier efforts that included increasing stakeholder engagement, establishing the Office of Climate Change and Health Equity , and establishing the National Institutes of Health UNITE Initiative to address structural racism and racial inequities in biomedical research. Since the release of its Equity Action Plan, HHS has taken actions to extend postpartum coverage through Medicaid and CHIP; issued rules to strengthen patient protections, including nondiscrimination protections; and issued nondiscrimination guidance to ensure that telehealth services are accessible to people with disabilities and those with limited English proficiency.
The Centers for Medicare and Medicaid Services (CMS) released an updated framework to advance health equity, expand health coverage, and improve health outcomes for people covered by Medicare, Medicaid, CHIP, and the Health Insurance Marketplaces. The framework outlined five priorities including expanding the collecting, reporting, and analysis of standardized data on demographics and social determinants of health; assessing the causes of disparities within CMS programs and addressing inequities in policies and operations; building capacity of health care organizations and the workforce to reduce disparities; advancing language access, health literacy, and the provision of culturally tailored services; and increasing all forms of accessibility to health services and coverage. The Administration has also identified advancing health equity and addressing social determinants of health as key priorities within Medicaid and has encouraged states to propose Section 1115 Medicaid waivers that expand coverage, reduce health disparities, and/or advance “whole-person care.” States have increasingly requested and/or received approval for waivers that aim to advance equity . Further, a growing number of states have approved or pending waivers with provisions related to addressing health-related social needs , such as food and housing, often focused on specific populations with high needs or risks.
The Administration and Congress have taken a range of actions to stabilize and increase access to health coverage amid the pandemic. Early in the pandemic, Congress passed the Families First Coronavirus Response Act (FFCRA), which included a temporary requirement that Medicaid programs keep people continuously enrolled during the COVID-19 Public Health Emergency in exchange for enhanced federal funds. Primarily due to the continuous enrollment provision, Medicaid enrollment has grown substantially compared to before the pandemic, and the uninsured rate has dropped with differences in uninsured rates between people of color and White people narrowing. Coverage gains also likely reflected enhanced ACA Marketplace subsidies made available by the American Rescue Plan Act (ARPA) of 2021 and renewed for another three years in the Inflation Reduction Act of 2022, boosted outreach and enrollment efforts, a Special Enrollment Period for the Marketplaces provided in response to the pandemic, and low Marketplace attrition . Additionally, in 2019, the Biden Administration reversed changes the Trump Administration had previously made to public charge immigration policies that increased reluctance among some immigrant families to enroll in public programs, including health coverage. Most recently, the Consolidated Appropriations Act of 2023 included a requirement for all states to implement 12 months of continuous coverage for children, supporting their coverage stability. However, it also set the end of the broader Medicaid continuous enrollment provision for March 31, 2023, which could lead to coverage losses for millions of people, reversing recent coverage gains.
There have been growing federal efforts to address disparities in maternal health. Over the past few years, the Administration launched several initiatives focused on addressing inequities in maternal health. In April 2021, President Biden issued a proclamation to recognize the importance of addressing the high rates of maternal mortality and morbidity among Black people. At the end of 2021, the White House hosted its inaugural White House Maternal Health Day of Action during which areas of concern in maternal health outcomes were identified and the Administration announced actions aimed at solving the maternal health crisis. In June 2022, the Biden Administration released the Blueprint for Addressing the Maternal Health Crisis . The Blueprint outlines priorities and actions across federal agencies to improve access to coverage and care, expand and enhance data collection and research, grow and diversify the perinatal workforce, strengthen social and economic support, and increase trainings and incentives to support women being active participants in their care before, during and after pregnancy. In July 2022, CMS announced a Maternity Care Action Plan to support the implementation of the Biden-Harris Administration’s Blueprint for Addressing the Maternal Health Crisis. The action plan takes a holistic and coordinated approach across CMS to improve health outcomes and reduce inequities for people during pregnancy, childbirth, and the postpartum period. ARPA included an option, made permanent in the Consolidated Appropriations Act , to allow states to extend Medicaid postpartum coverage from 60 days to 12 months. As of April 2023, the majority of states have taken steps to extend postpartum coverage. The Human Resources and Services Administration also announced $12 million in awards for the Rural Maternal and Obstetrics Management Strategies Program (RMOMS), which is designed to develop models and implement strategies to improve maternal health in rural communities.
The Administration has also taken steps to address health disparities and discrimination experienced among LGBT+ people. On his first day in office, President Biden signed an Executive Order on “Preventing and Combating Discrimination on the Basis of Gender Identity or Sexual Orientation.” Since then, the Administration has taken multiple actions to address discrimination within health care specifically. In May 2021, the Biden Administration announced that the HHS Office for Civil Rights (OCR) would include gender identity and sexual orientation as it interprets and enforces the ACA’s prohibition against sex discrimination (Section 1557), reversing the approach taken by the Trump Administration. Additionally, the Administration has spoken out against state actions aimed at curtailing access to gender affirming care for transgender and gender nonconforming people, particularly policies targeting youth. In January 2023, the Administration released its Federal Evidence Agenda on LGBTQI+ Equity , a “roadmap for federal agencies as they work to create their own data-driven and measurable SOGI Data,” which the Administration views as central to understanding disparities and discrimination facing this community.
What are key issues related to health disparities looking ahead?
The end of the Medicaid continuous enrollment provision may lead to coverage losses and widening disparities. Following the ending of the Medicaid continuous enrollment provision on March 31, 2023, states resumed Medicaid redeterminations. KFF estimates that between 5 and 14 million people could lose Medicaid coverage, including many who newly gained coverage during the pandemic. Other research shows that Hispanic and Black people are likely to be disproportionately impacted by the expiration of the continuous enrollment provision. Moreover, some groups, such as individuals with limited English proficiency and people with disabilities may face increased challenges in completing the Medicaid renewal process increasing their risk of coverage loss even if they remain eligible for coverage. OCR has reminded states of their obligations under federal civil rights laws to take reasonable steps to provide meaningful language access for individuals with limited English proficiency and ensure effective communication with individuals with disabilities to prevent lapses in coverage amid the unwinding of the continuous enrollment provision. CMS issued guidance that provides a roadmap for states to streamline processes and implement strategies to reduce the number of people who lose coverage even though they remain eligible. The extent to which states simplify processes to renew or transition to other coverage and provide outreach and assistance to individuals more likely to face challenges completing renewal processes will impact coverage losses and potential impacts on coverage disparities.
The end of the COVID-19 Public Health Emergency (PHE) and the potential depletion of the federally purchased supply of COVID-19 vaccines, treatments, and tests may curtail access to these supplies for some individuals, particularly those who are uninsured. In response to the COVID-19 pandemic, the federal government spent billions of dollars in emergency funds to purchase COVID-19 vaccines, including boosters, treatments, and tests to provide free of charge to the public. In addition, Congress enacted legislation that included special requirements for their coverage by both public and private insurers, and the Administration issued guidance and regulations to protect patient access and promote equitable distribution. The upcoming end to the PHE on May 11, 2023, as well as the potential depletion of federally purchased supplies in the absence of any additional funding, could result in new or higher cost-sharing and/or reduced access to these products although these impacts may vary by product and the type of health coverage an individual has. People who are uninsured or underinsured face the greatest risk of access challenges, including limited access to free vaccines and no coverage for treatment or tests. Since people of color and people with lower incomes are more likely to be uninsured, they may be at a disproportionate risk of facing barriers to accessing COVID-19 vaccines, tests, and treatments once the PHE ends and the federal supply is depleted.
The overturning of Roe v. Wade may exacerbate the already large racial disparities in maternal and infant health. The decision to overturn the longstanding Constitutional right to abortion and elimination of federal standards on abortion access has resulted in growing variation across states in laws protecting or restricting abortion. These changes may disproportionately impact women of color, as they are more likely to obtain abortions, have more limited access to health care, and face underlying inequities that would make it more difficult to travel out of state for an abortion compared to their White counterparts. Restricted access to abortions may widen the already stark racial disparities in maternal and infant health, as some groups of color are at higher risk of dying from pregnancy-related reasons and during infancy and are more likely to experience birth risks and adverse birth outcomes compared to White people. It may also have negative economic consequences associated with the direct costs of raising children and impacts on educational and employment opportunities. Further, women from underserved communities may be at increased risk for criminalization in a post-Roe environment, as prior to the ruling, there were already cases of women being criminalized for their miscarriages, stillbirths, or infant death, many of whom were low-income or women of color.
Many states have implemented policies banning or limiting access to gender affirming care, especially for youth, as well as other legal actions that threaten access to care for LGBT+ people . Policies aimed at limiting access to gender affirming care may have significant negative implications for the health of trans and nonconforming people, particularly young people, including negative mental health impacts, and an increased risk of suicidality . Additionally, the recent Braidwood case on preventive care access directly affects LGBT+ people in its treatment of Pre-Exposure Prophylaxis (PrEP). It relies, in part, on religious protections arguments to limit access to the drug based on the plaintiff’s claim that it “facilitate[s] and encourage[s] homosexual behavior, prostitution, sexual promiscuity, and intravenous drug use.” If PrEP use declines as a result of the Braidwood decision, HIV incidence could increase , likely disproportionally impacting people of color and LGBT+ people. Efforts to curtail access to gender affirming care and the Braidwood decision are at odds with the Administration’s stated approach to health equity for LGBT+ people. How such policies play out in the longer term will be determined largely by the courts.
Evolving immigration policies may impact the health and well-being of immigrant families. When the PHE ends on May 11, 2023, Title 42 restrictions that suspended the entry of individuals at the U.S. border to protect public health during the COVID-19 emergency are expected to terminate. It is anticipated that when the authority ends, there will be an increase in immigrant activity at the U.S. border. The Biden Administration has announced plans to increase security and enforcement at the border to reduce unlawful crossings, expand “legal pathways for orderly migration”, invest additional resources in the border region, and partner with Mexico to implement the aforementioned plans. However, it remains to be seen how shifting policies will impact trends at the border and health and health care in that region. The future of the Deferred Action for Childhood Arrivals (DACA) program remains uncertain, and its implementation is currently limited subject to court orders . If the DACA program is found to be unlawful in pending court rulings, individuals would lose their DACA status and subsequently their work authorizations. The loss of status and work authorization may result in loss of employer-based health coverage, leaving people uninsured and unable to qualify for Medicaid, CHIP, or to purchase coverage through the Marketplaces. Additionally, although the Biden Administration reversed public charge regulations implemented by the Trump Administration as part of an effort to address immigration-related fears that limited immigrant families’ participation in government assistance programs, including Medicaid and CHIP, many families continue to have fears and concerns about enrolling in these programs, contributing to ongoing gaps in coverage for immigrants and children of immigrants.
Growing mental health and substance use concerns and ongoing racism, discrimination, and violence may contribute to health disparities. As previously noted, mental health and substance use concerns have increased since the onset of the pandemic, with some groups particularly affected. These trends may lead to new and widening disparities. For example, people of color have experienced larger increases in drug overdose death rates than White people, resulting in the death rate for Black people newly surpassing that of White people by 2020. Further, Black and Asian people have reported negative mental health impacts due to heightened anti-Black and anti-Asian racism and violence in recent years. Research has documented the negative health impacts, including negative impacts on mental health and well-being, of exposure to violence, including police and violence. Research shows African American and AIAN men and women, and Latino men are at increased risk of being killed by police compared to their White peers. Black and Hispanic adults also are more likely than White adults to worry about gun violence according to 2023 KFF survey data . Other KFF analysis shows that firearm death rates increased sharply among Black and Hispanic youth during the pandemic driven primarily by gun assaults and suicide by firearm. Research further shows that repeated and chronic exposure to racism and discrimination is associated with negative physical and mental health outcomes , including premature aging and associated health risks, referred to as “ weathering ,” as well as higher mortality .
Despite growing mental health concerns, people of color continue to face disproportionate barriers to accessing mental health care. Research suggests that structural inequities may contribute to disparities in use of mental health care, including lack of health insurance coverage and financial and logistical barriers to accessing care, stemming from broader inequities in social and economic factors . Lack of a diverse mental health care workforce, the absence of culturally informed treatment options, and stereotypes and discrimination associated with poor mental health may also contribute to limited mental health treatment among people of color. Amid the pandemic, many states implemented telehealth behavioral health services to expand access to behavioral health care, and most states intend to keep these services. States are also adopting strategies to address workforce shortages in behavioral health. As states seek to expand access to behavioral health care, it will be important to ensure that services address the cultural and linguistic needs of diverse populations. Further, in 2022, the federal government mandated the suicide and crisis lifeline number that provides a single three-digit number (988) to access a network of over 200 local and state-funded crisis centers. The 988 number is expected to improve the delivery of mental health crisis care; however, it is unknown how well it will address the needs of people of color and other underserved populations.
In sum, disparities in health and health care for people of color and other underserved groups are longstanding challenges, many of which are driven by underlying structural and economic disparities rooted in racism. Addressing disparities is key not only from an equity standpoint but for improving the nation’s overall health and economic prosperity. Amid the COVID-19 pandemic, the federal government identified health equity as a priority and has since launched initiatives to address disparities wrought by the COVID-19 pandemic and more broadly. Alongside the federal government, states, local communities, private organizations, and providers have engaged in efforts to reduce health disparities. Moving forward, a broad range of efforts both within and beyond the health care system will be instrumental in reducing disparities and advancing equity.
- Racial Equity and Health Policy
- Coronavirus (COVID-19)
- Women's Health Policy
- Access to Care
- American Indian/Alaska Native
- Race/Ethnicity
Also of Interest
- How History Has Shaped Racial and Ethnic Health Disparities: A Timeline of Policies and Events
- Key Data on Health and Health Care by Race and Ethnicity
- Health Coverage by Race and Ethnicity, 2010-2022
- Public Health
- Health Outcomes
Relationship of social disadvantage and inequalities with health outcomes Shrawasti
- August 2023

- Tribhuvan University
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Thomas E Cox

- Geoffrey R Swain
- M S Pradhan
- Umesh Ghimire
- Jyoti Manandhar
- Arun Gautam
- Yogendra Sabi Shouta Tuladhar
- Tesfayi Prasai
- Gebreselassie
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Open access
- Published: 14 June 2024
Inequalities in patients’ experiences with cancer care: the role of economic and health literacy determinants
- Vladimir Jolidon 1 ,
- Manuela Eicher 2 , 3 ,
- Isabelle Peytremann-Bridevaux 1 &
- Chantal Arditi 1
BMC Health Services Research volume 24 , Article number: 733 ( 2024 ) Cite this article
Metrics details
Patients with fewer socioeconomic and health literacy resources are disadvantaged in their access and use of healthcare, which may give rise to worse experiences with care and thus inequalities in patient experiences. However, only a limited number of studies have examined how socioeconomic and health literacy factors shape inequalities in patients’ experiences with cancer care.
To examine whether patients’ experiences with cancer care differ according to their economic status and health literacy.
Secondary analysis of data on 2789 adult patients diagnosed with cancer from the Swiss Cancer Patient Experiences-2 (SCAPE-2) study, a cross-sectional survey conducted in eight hospitals across Switzerland from September 2021 to February 2022. Regression analysis was applied to examine the independent effect of patients’ economic status and health literacy on various outcomes of experiences with cancer care, covering eight different dimensions of patient-centred care, controlling for confounding factors.
Adjusted regression analysis showed that patients with lower economic status reported significantly worse experiences with cancer care in 12 out of 29 specific care experiences, especially in the dimensions of ‘respect for patients’ preferences’ and ‘physical comfort’ where all items of experiences were associated with economic status. Additionally, lower health literacy was associated with worse patient experiences in 23 specific care experiences. All items in the dimensions of ‘respect for patients’ preferences’, ‘physical comfort’ and ‘emotional support’ were associated with health literacy.
This study revealed significant inequalities in experiences with cancer care shaped by the economic status and health literacy of patients across different dimensions of patient-centred care. It is essential to address the needs of more disadvantaged patients who face obstacles in their access and use of the healthcare system, not only to mitigate inequalities in cancer care but also to avoid inequalities in health outcomes.
Peer Review reports
Introduction
Patient experience of care is acknowledged as a key element of the quality of healthcare and relates to safety of care and clinical effectiveness [ 1 , 2 ]. Hence, it is included in performance frameworks evaluating the quality of healthcare. Patient experience is typically assessed with patient-reported experience measures (PREMs), which collect information on the care received by patients, their interactions with health professionals and the outcomes of those interactions [ 3 , 4 , 5 , 6 , 7 ]. PREMs were developed to capture the experiences of patients with various care events and to provide specific and practical information that may be acted upon to improve patient care. They differ from patient satisfaction measures, which cover a limited area of patient experience with care and provide a narrower perspective compared to the multiple facets of patient experiences [ 8 , 9 ]. Importantly, PREMs have been regarded as an accurate indicator of patient-centredness in healthcare. Patient-centredness is a dimension of quality of care that is defined as care provision responsive to and respectful of patient needs, preferences, and values [ 10 , 11 ].
Most commonly, overall levels of patient experience with care (i.e. the proportion of patients reporting a positive experience with care) are reported to assess healthcare services, with little examination of possible variations between subgroups of patients. That is, patients’ experiences may be shaped by their sociodemographic profiles and access to resources, which can result in inequalities in care experiences when more disadvantaged patients consistently report poorer experiences. The perception and experience of vulnerable patients with care are critically important yet poorly understood dimension of healthcare delivery. Indeed, limited attention has been paid to how individuals’ socioeconomic status may give rise to inequalities in care experiences, although health equity is a central goal for healthcare improvement in the “quintuple aim” framework [ 12 ]. This is particularly important since patient experiences may affect healthcare access and health outcomes [ 13 , 14 ], and inequalities in patient experience may thus exacerbate disparities in health and quality of life.
Previous research has shown that factors such as age, gender, ethnicity, cancer prognosis and health status may influence patients’ experiences with care [ 15 , 16 , 17 ]. Nevertheless, there has been a relative lack of attention given to the effect of socioeconomic status and particularly health literacy on patient experiences, despite recent studies suggesting that these factors may affect care experiences [ 18 , 19 , 20 ]. In sum, it is essential to investigate social inequalities in PREMs as a key element of quality of care. Results of such research can contribute to a better understanding of specific groups of patients who require further attention, in order to address their needs and enhance their care experience, and in turn, their health outcomes.
Socioeconomic status and patient experiences in cancer care
Past studies have shown socioeconomic inequalities in patient satisfaction and care experiences. Lower income patients and those from deprived neighbourhoods tend to report lower satisfaction and worse experiences with healthcare services compared to more affluent patients [ 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 ]. In the field of cancer care, previous studies have revealed sociodemographic differences in patient care experiences, such as age, ethnicity and gender differences [ 15 , 16 , 29 , 30 , 31 ]. However, these studies were mostly conducted in the United Kingdom and the United States of America [ 17 ] and research on socioeconomic inequalities in cancer patients’ experiences remains limited.
Inequalities in patient experience may be explained from the standpoint of the fundamental cause theory [ 32 ]. According to this framework, social conditions act as fundamental causes of individual health since the resources available to individuals, such as knowledge, power, money and social networks, determine their ability to avoid diseases and protect their health [ 32 ]. While this theory does not directly address healthcare use and experience, its authors asserted that fundamental social conditions “directly shape individual health behaviours by influencing whether people know about, have access to, can afford and are motivated to engage in health-enhancing behaviours” [ 32 ]. Hence, socioeconomically disadvantaged patients may face more barriers in healthcare use compared to their more advantaged counterparts, and may experience unmet healthcare needs stemming from the (direct and indirect) costs of healthcare [ 33 , 34 , 35 ]. In sum, a vulnerable condition defined by lower socioeconomic status and limited financial resources may negatively affect patients’ experiences of healthcare services.
The role of health literacy
In addition to socioeconomic resources, patient’s cultural skills and competencies may influence their experience with care. Thus, the fundamental cause theory is complemented by the “cultural health capital” framework, which stresses that patients’ encounters with healthcare services are defined by their cultural resources [ 36 ]. That is, patients who have an “enterprising and proactive disposition, a fluency in biomedical concepts and language, bureaucratic know-how, and an interactional agility with authoritative experts” [ 36 ] are better equipped to navigate the complexities of the healthcare system. Such individual characteristics also facilitate their interactions and exchange of informations with healthcare professionals. Consequently, inequalities in care experiences may stem from differences in patients’ cultural abilities, and the dynamics of unequal treatment that these engender in the healthcare context [ 37 ].
In this framework, health literacy is a key characteristic that determines patients’ ability to communicate and function in the healthcare environment. It is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” [ 38 ]. Individuals with lower health literacy may experience difficulty obtaining, understanding, and retaining health information, which is associated with the under-utilisation of (preventive) healthcare services [ 18 , 39 ], more frequent hospitalisations and emergency care utilisation [ 40 , 41 ], worse health outcomes and increased mortality [ 42 , 43 ]. These associations were also found among patients with cancer [ 44 , 45 , 46 , 47 ]. Moreover, lower health literacy was shown to relate to the inefficiency of consultations and dissatisfaction with healthcare [ 18 , 19 , 48 , 49 ], as well as lower health-related quality of life among patients with cancer [ 50 , 51 ].
Although health literacy has been studied in different areas of cancer care [ 52 ], no study has examined health literacy-related inequalities across a range of PREMs encompassing diverse dimensions of patient care experiences. Thus, it is important to elucidate the association of health literacy with various care experiences, especially since research has evidenced its independent association with various health outcomes, health-related behaviours, and health service use [ 53 ]. While health literacy levels may indeed relate to people’s socioeconomic conditions, this relationship can be more complex and influenced by further factors, such as family and social support networks. Hence, health literacy should not solely be considered as a mediator, and its potential direct effect on care experiences warrant analysis.
Finally, health literacy directly relates to a patient-centred care approach that places patients’ perspectives, values, needs and preferences as the starting point and the importance of communication and information [ 10 , 19 ]. Indeed, for patients to be empowered to understand health information and make decisions about their own care, they should have the necessary education, information, and support [ 19 , 53 , 54 ]. However, if health literacy is unequally distributed, as well as support for patients, inequalities in patients’ experiences and health outcomes may persist.
In that context, the present study aims to investigate inequalities in cancer care experiences shaped by patients’ economic and health literacy resources. This is particularly relevant since a limited number of studies have focused on such inequalities in patients’ experiences, especially in the field of cancer care and in countries other than the UK and USA.
Study design, population, and data
The present study is a secondary analysis of data from the second wave of the Swiss Cancer Patient Experiences-2 (SCAPE-2) study. This cross-sectional and multicentre survey collected data from patients diagnosed with cancer in eight Swiss hospitals between September 2021 and February 2022. The survey inclusion criteria were adult patients (18 years of age or older) who had a cancer diagnosis, at least one cancer-related hospitalisation or outpatient visit at one of the recruiting hospitals between January 1 and June 30, 2021, and a home address in Switzerland. The patient selection procedure was carried out by local hospital teams, manually reviewing patient lists or using electronic databases. The hospitals were recruited by sending invitation letters to the oncology departments of 13 hospitals, including all five university hospitals as well as those with large oncology departments. Eight hospitals agreed to participate in the study, achieving a broad representation of Swiss hospitals. Notably, four were located in the French-speaking region and four in the German-speaking region, each situated in a different canton. Among them were three university hospitals and five cantonal (regional) hospitals, with two located in major Swiss cities (Geneva and Zurich), four in medium-sized cities (Lausanne, Lucerne, Zug, and Fribourg), and two in smaller cities (Chur and Sion) situated in more rural cantons. The hospitals varied in size, with four having between 7,000 and 12,000 employees and four having between 1,000 and 6,000 employees.
The data was collected using the SCAPE-2 questionnaire, a self-administered questionnaire based on the NHS Cancer Patients Experience Survey [ 55 ]. The questionnaire, translated and culturally adapted from the original version developed in the United Kingdom, contained 130 questions in total, including patient experience, health, and socio-demographic questions. Respondents had the option to fill it out on paper and return it by post, or to complete it online. The questionnaire was sent to patients’ homes by each hospital in September 2021, and reminders were sent to non-respondents in November 2021. Patients who returned the questionnaire by the end of February 2022 were included in the study. Out of 6873 patients who were invited to take part in the survey, 3220 completed it (crude participation rate 46.8%).
Outcome variables
Of the 71 patient experience questions, we selected 29 questions pertaining to experiences regarding cancer care in general that applied to all patients as outcomes in this study. These questions covered the cancer care pathway, from pre-diagnostic care to home care, and assessed the eight dimensions of patient-centred care. Building upon the work of Gerteis and colleagues [ 56 ], the Picker Institute developed these dimensions, capturing the essential components of care quality [ 57 , 58 ]:
Access to care: waiting time before seeing a specialist (before_wait).
Information and education: understood diagnostic explanations (dx_explanation), received written diagnostic information (dx_information), treatment options were explained (ttt_opt), treatment side effects explained in understandable way (ttt_sidefx_expl), told about long-term side effects (ttt_sidefx_future), received information on impact of cancer on daily activities (info_impact), received information on support groups (info_support_gp), received information on getting financial help (info_support_fin), receiving a care plan (careplan).
Coordination and integration of care: professionals working well together (collaboration), test results or medical records available (test_avail), receiving clear and consistent information (info_consist), Test not repeated (test_repet).
Continuity and transition: support and equipment available at home (home_support), care from health or social services during (home_service_during) or after (home_serv_after) treatment, GP receiving information (gp_info).
Involvement of family and friends: told that could be accompanied (dx_accompanied), family involved in treatment decisions (ttt_dec_fam), family was given information for care at home (home_info_fam).
Respect for patients’ preferences: involved in treatment decisions (ttt_involve), situation and habits taken into account (ttt_dec_hab).
Physical comfort: information/support to deal with symptoms (ttt_support_symp), information/support to deal with long-term effects (support_ltsidefx).
Emotional support: told in a sensitive manner (dx_tactful), offered to see health professional to discuss worries (support_worries), GP support (gp_support), received information on support to handle emotions (info_support_emo).
Most experience questions had 5-point Likert-type scale response options to measure positive experiences (i.e. ‘yes, completely’; ‘yes, to some extent’; ‘no’; ‘not applicable’; and ‘don’t know/can’t remember’). We computed binary variables for each question to capture patients’ positive experiences (response ‘yes, absolutely’) versus non-positive experiences (responses ‘yes, to some extent’ and ‘no’), while neutral (‘don’t know/can’t remember’) and not applicable answers were excluded, following the methodology of the NHS Cancer Patients Experience Survey [ 55 ] and previous similar studies [ 16 , 59 ]. The dichotomisation of outcome variables facilitates clearer presentation, interpretation, and comparison across the numerous outcome measures assessed.
Independent variables
The first independent variable of interest, ‘economic status’, was computed using the following three questions: ‘In the past 12 months, have you had difficulty paying for your bills (taxes, insurances, telephone, electricity, credit card, etc.)?’, ‘In the past 12 months, have you skipped any medical care because of the cost?’ and ‘Have you or your family had to make financial sacrifices because of treatment or the long term effects of cancer?’. These variables were dichotomised (yes = 1, no = 0) and summed into a score from 0 to 3. A higher score entailed more economic hardship and thus a lower economic status, that is, patients who answered that they faced economic hardships in the three questions obtained a score of 3. The second independent variable of interest, ‘health literacy’, was obtained from a question assessing patients’ difficulty in understanding written medical information, which has shown to have good sensitivity and specificity in capturing individuals’ health literacy limitations [ 60 ]: ‘When you receive written information concerning a medical treatment or your health, do you have problems understanding it?’ to which respondents could respond ‘always’, ‘often’, ‘sometimes’, ‘occasionally’, or ‘never’. Answers were recoded into a binary variable with the categories ‘low health literacy’ (always, often) and ‘high health literacy’ (sometimes, occasionally, never). Finally, other independent variables of our study were patients’ age (continuous variable), sex (woman, man) and self-rated health (5-point scale: 0 ‘bad’, 25 ‘average’, 50 ‘good’, 75 ‘very good’, 100 ‘excellent’).
Statistical analyses
After the exclusion of patients with missing information for the independent variables ( n = 431; 13.4%), the study sample contained 2789 individuals. As the 29 outcomes, analysed in separate models, had different amounts of missing information, the final sample size for each of these outcomes is reported in Table 1 . First, we performed univariate analysis to describe the independent (patient sociodemographic and health characteristics) and dependent (patient care experiences) variables of the study. Then, we conducted multiple logistic regression analyses to examine the association between economic status and health literacy and 29 outcomes of patient experiences with care, in separate models. Model 1 only included the independent variable of interest – economic status or health literacy - and hospital fixed effects (one dummy variable for each hospital except one) to control for between-hospital heterogeneity. Model 2 was adjusted for age, sex, self-rated health, health literacy, economic status and hospital fixed effects. Odds ratios (ORs) with 95% confidence intervals were graphically presented, for ease of interpretation of the results.
In sensitivity analyses, we replicated Models 2 using economic status as a categorical variable (instead of a continuous score variable) with four categories from 0 (no economic hardship reported by the patient) to 3 (economic hardship were reported in all three questions), zero (0) being the reference category. We also conducted sensitivity analyses for multiple testing using Benjamini and Hochberg False Discovery Rate [ 61 ] to correct p-values, which is a method to ensure that we do not over-interpret a few significant results that may occur (by chance) when multiple tests are performed. As all statistically significant associations remained significant after applying the multiple testing correction, we did not present the corrected p-values in our figures (available on request). An additional sensitivity analysis was performed on the adjusted models (Models 2) where the type of cancer was added as a control variable to ensure that it did not confound the association between health literacy/economic status and patients’ care experiences.
Multicollinearity between independent variables was tested with variance inflation factors and no potential issues of collinearity were detected. All analyses were performed using Stata BE 17.0.
Patient involvement
Patient involvement in research ensures that the research is relevant for patients and the larger public, that the research objectives are acceptable and feasible, and that the research and its documents are appropriate and comprehensive [ 62 ]. Two patients, trained and experienced in patient involvement in research, contributed to the development and implementation of the SCAPE-2 survey. They were recruited via the patient advisory board of the Swiss clinical cancer research organisation and involved in all steps of the research process. That is, they contributed to developing and pre-testing the questionnaire, preparing the materials sent to patients along with the questionnaire, replying to patients’ queries during the recruitment period, analysing questionnaires’ free-text comments, writing lay summaries of results shared with participating patients, and disseminating results on social media and to the scientific community.
Table 2 presents a summary of respondents’ characteristics. On average, they were 64 years old and 51% of them were women. The mean self-reported health was 54 on a scale from 0 to 100. Around one-fourth of the respondents reported a low level of health literacy (problems understanding written health information), and the mean score for economic status was 0.5 on a scale from 0 to 3.
Patients’ experiences with cancer care across eight dimensions of patient-centred care are presented in Table 1 . In the dimensions of ‘access to care’ and ‘coordination and integration’, more than 80% of patients reported positive experiences in all items. More than 80% of patients also reported positive experiences in other dimensions for specific items such as ‘treatment options were explained’, ‘received information on impact of cancer on daily activities’, ‘received information on support groups’, ‘GP receiving information’, ‘told in a sensitive manner’, ‘offered to see health professional to discuss worries’ and ‘received information on support to handle emotions’. In the dimensions of ‘involvement of family and friends’ and ‘respect for patients’ preferences’, about 60–75% of the patients reported positive experiences with cancer care. Finally, in the dimension ‘information and education’, 4 out of 9 items had proportions of positive experience lower than 60%, and this was also the case for specific items such as ‘care from health/social services after treatment’ and ‘information/support to deal with long-term effects’, falling under the dimensions ‘continuity and transition’ and ‘physical comfort’, respectively.
The effect of patients’ economic status on their experiences with cancer care is shown in Fig. 1 . In the unadjusted models (M1), a lower economic status was significantly associated with a lower probability of reporting positive care experiences in 25 out of 29 specific cancer care experiences. In the adjusted models (M2), economic status remained associated with 12 out of 29 cancer care experiences. Specifically, all items in the dimensions ‘respect for patients’ preferences’ (ttt_involve, ttt_dec_hab) and ‘physical comfort’ (ttt_support_sympt, support_ltsidefx) were associated with economic status in Models 2. The other dimensions had either one or two items associated with economic status (info_impact, info_support_fin, collaboration, home_support, home_service_during, ttt_dec_fam, home_info_fam, gp_support) except for ‘access to care’ (before_wait), in which the single item ‘waiting time before seeing a specialist was adequate’ was not found to be associated.

Effect of economic status on patients’ experiences with cancer care, odds ratio and 95% confidence intervals, unadjusted (M1) and adjusted models (M2). Note: M1 only included the independent variable ‘economic status’ and hospital fixed effects, and M2 added sex, age, self-rated health, and health literacy as control variables
Concerning the effect of patients’ health literacy on their experiences with cancer care (Fig. 2 ), unadjusted models (M1) showed that patients’ lower health literacy was significantly associated with a lower probability of reporting positive care experiences in 27 out of 29 specific cancer care experiences. In the adjusted models (M2), health literacy remained associated with 23 out of 29 specific cancer care experiences. In particular, all items in the dimensions ‘respect for patients’ preferences’ (ttt_involve, ttt_dec_hab), ‘physical comfort’ (ttt_support_sympt, support_ltsidefx), ‘coordination and integration’ (collaboration, test_avail, info_consist, test_repet) and ‘emotional support’ (dx_tactful, support_worries, gp_support, info_support_emo) were associated with health literacy in Models 2, as well as all items except one in the ‘information and education’ (dx_explanation, dx_information, ttt_opt, ttt_sidefx_expl, ttt_sidefx_future, info_impact, info_support_gp, info_support_fin) dimensions. The dimensions of ‘continuity and transition’ and ‘involvement of family and friends’ had two (home_service_during, home_serv_after) and one item (home_info_fam) associated with health literacy, respectively, and the single item in ‘access to care’ (before_wait) was not found to be associated with health literacy.

Effect of health literacy on patients’ experiences with cancer care, odds ratio and 95% confidence intervals, unadjusted (M1) and adjusted models (M2). Note: M1 only included the independent variable ‘health literacy’ and hospital fixed effects, and M2 added sex, age, self-rated health, and economic status as control variables
When comparing the adjusted models (Model 2) of economic status and health literacy in Figs. 1 and 2, we observe that these two predictors were associated with ten common cancer care experiences (info_impact, info_support_fin, collaboration, home_service_during, home_info_fam, ttt_involve, ttt_dec_hab, ttt_support_symp, support_ltsidefx, gp_support). Health literacy alone was significantly associated with 13 additional care experiences (dx_explanation, dx_information, ttt_opt, ttt_sidefx_expl, ttt_sidefx_future, info_support_gp, test_avail, info_consist, test_repet, home_serv_after, dx_tactful, support_worries, info_support_emo).
In sensitivity analyses, Model 2 was replicated using economic status as a categorical variable. Out of the 12 cancer care experiences that were found to be significantly associated with economic status as a continuous (score) variable, six were associated with all three categories of economic status, showing clear gradients throughout the ORs of the categories (info_impact, info_support_fin, ttt_involve, ttt_dec_hab, support_ltsidefx, gp_support). The remaining six care experiences (home_info_fam, home_support, home_service_during, collaboration, ttt_support_symp, ttt_dec_fam) were associated with only one or two categories and showed relatively clear gradients throughout the categories (tables available upon request to the authors). In the sensitivity analysis where type of cancer was added to Models 2 (adjusted models), the results remained robust, with no substantial changes in the ORs of health literacy and economic status variables, and their statistical significance (results available upon request to the authors). Given that type of cancer did not affect the results, it was not included in the final models to avoid overfitting.
This study showed substantial inequalities in patient experiences, related to economic and health literacy factors, among patients with cancer treated in eight hospitals located in Switzerland. In adjusted models, lower economic status and lower health literacy were associated with worse care experiences in 12 and 23 out of 29 specific care experiences, respectively. Economic status affected all experience outcomes within the patient-centred care dimensions related to ‘respect for patients’ preferences’ and ‘physical comfort’, and health literacy affected all items in the dimensions of ‘respect for patients’ preferences’, ‘physical comfort’ and ‘emotional support’. Importantly, the effect of economic status and health literacy on the different experience outcomes remained significant after applying the multiple testing correction, pointing out that these findings are unlikely to have occurred by chance.
The results of our study are concordant with previous research that found that socioeconomically disadvantaged patients report worse experiences with healthcare [ 17 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 ]. Our results add to the literature on socioeconomic inequalities in patient experience specific to patients with cancer, which has been limited. Individuals with fewer financial resources reported worse experiences with ‘received information on getting financial help’, ‘support at home from health/social services’ and ‘care from health/social services during treatment’. This might indicate that the current Swiss health system is not responding enough to the needs of socioeconomically disadvantaged people, especially in supporting them with healthcare costs that are not covered under the basic health insurance. Compared to other European countries with universal health insurance coverage, the Swiss health system involves relatively high health insurance premiums and out-of-pocket expenditures. This context may contribute to lower income individuals forgoing healthcare due to cost, which has been evidenced in Switzerland [ 34 , 63 , 64 , 65 ], as well as to socioeconomic inequalities in healthcare, including cancer screening use [ 66 , 67 , 68 , 69 ]. These inequalities seem to persist despite the provision of health insurance subsidies to eligible low-income individuals in Switzerland, as previous research has shown that receiving a premium subsidy is associated with forgoing healthcare [ 34 , 63 , 65 , 66 , 70 ]. It is possible that financially vulnerable individuals and families tend to prioritise expenses other than healthcare, given their economic constraints. In sum, our results suggest that cancer care experiences are affected by the healthcare costs borne by patients in Switzerland. Healthcare professionals and policy-makers should consider this issue since healthcare forgoing and poor patient experience may lead to worse health outcomes in disadvantaged populations.
Our findings are also in line with past research that showed that lower health literacy is associated with inadequate healthcare services use and poor experiences with care [ 18 , 19 , 20 , 48 ]. Our study significantly adds to this literature since few studies have examined health literacy in relation to comprehensive measures of patient experiences, such as the patient-centred care dimensions [ 20 ]. Following the cultural health capital framework [ 36 ], several assumptions could be made to explain how health literacy influences patient experience with care in our results. Indeed, patients with lower health literacy may face difficulties in understanding and engaging with medical information and navigating a complex healthcare system. Limited health literacy may hinder patients’ capacity to understand the risks and benefits associated with cancer treatment, and to follow instructions from providers [ 18 , 40 , 71 , 72 ]. Moreover, previous studies also showed that lower health literacy can affect the information exchange process during doctor visits, potentially limiting individuals’ ability to engage in effective and meaningful patient-doctor communication [ 49 , 73 , 74 ]. Health practitioners should pay attention to patients with lower health literacy to ensure that they understand the provided information and strive to improve the quality of their communication. This is crucial to guarantee equal opportunities to receive adequate care and support. In clinical settings, various interventions have aimed at improving communication with patients with low health literacy to facilitate their comprehension of health information and instructions [ 53 , 75 , 76 , 77 ]. These interventions often include strategies such as simplifying written materials, employing different communication formats (e.g. visual aids, illustrated text, spoken animations), and implementing techniques like “teach-back” (i.e. patients rephrasing important information in their own words) to ensure patients’ understanding and enhance face-to-face communication [ 75 , 77 ]. Other interventions have aimed at improving the education and training of frontline healthcare professionals to improve their ability to address health literacy needs [ 78 , 79 ].
Notably, in adjusted models, patients’ health literacy was more consistently related to cancer care experience items than economic status. This substantiates the claim that health literacy bears an independent and direct relation to care experiences. Indeed, while material factors such as economic resources are key determinants of disparities in health and healthcare, as put forward by the fundamental cause theory, underlying mechanisms affecting the experience of patients with the healthcare system might be found in immaterial factors, such as cultural resources and abilities. This interpretation is in line with Shim’s “cultural health capital” theory [ 36 ], which stresses the role of patients’ cultural competencies, and patient-provider interaction and exchange of information, in producing inequalities in care.
In several studies, patients with higher education levels reported more negative evaluations of healthcare, although results were not always consistent [ 24 , 80 , 81 ]. One may expect that these patients experience better care due to their higher health literacy resources. However, a higher education level may also increase expectations, leading patients to underrate their care experiences. A potential response bias might also stem from the different response patterns of individuals of lower and higher socioeconomic status when answering patient experience questions [ 80 , 82 ]. Additionally, education level may be a proxy for both health literacy and socioeconomic status, potentially conflating distinct effects and yielding contradictory results. Hence, our study adopted a more direct measurement of health literacy, rather than relying on a proxy such as education level, by simultaneously controlling models for both individuals’ economic status and health literacy, thereby providing a better assessment of these variables and disentangling their effect in our analyses.
The findings of this study carry significant implications for practitioners, policy-makers and researchers, as they show that economic status and health literacy level are associated with patient experiences with care. Given the influence of economic status and health literacy, ‘one-size-fits-all’ approaches in cancer care are likely inadequate for improving patient experience equally. Indeed, the diversity in patient experiences and their distinct characteristics needs to be taken into account. Patient-centred cancer care should not only be tailored to address patient needs and preferences, but also to tackle persistent social and structural inequalities among them. Patients with low health literacy and low income will require more attention and targeted interventions to ensure that care delivery responds to their specific conditions. They may benefit from tailored information and enhanced patient navigation to ensure that care is provided and explained in accessible ways. For example, a study found that the presence of care coordinators strongly improved care coordination, particularly benefiting patients with low health literacy [ 83 ]. This suggests that having care coordinators in the healthcare team providing tailored information may facilitate navigation within the healthcare system for disadvantaged patients with low health literacy and improve their experiences with care [ 84 ]. Additionally, research showed that clinical nurse specialists played an important role in improving experiences of care coordination, participation in treatment decisions, and feeling treated with respect and dignity [ 85 , 86 ]. As Nutbeam and Lloyd [ 53 ] highlighted, there is a need to shift focus from individual-level interventions to organisational- and community-level interventions, such as efforts aiming at reducing organisational complexity within healthcare systems to improve accessibility and understanding of health information. Known as organisational health literacy (OHL), these initiatives strive to create health-literate environments that facilitate patient navigation and comprehension [ 78 , 87 ]. However, research evaluating the effectiveness of such interventions in mitigating inequalities in patient experiences has been limited [ 53 ].
Furthermore, in light of the increasing prevalence of virtual care modalities like e-health and telemedicine – further accelerated by the global COVID-19 pandemic and its consequent limitations on healthcare access [ 88 ] – the significance of factoring in patients’ health literacy levels becomes even more pronounced. Indeed, recent studies have pointed out inequalities in the use of virtual care and electronic patient communication, e.g. email communication [ 89 , 90 ]. Given the persistence of digital divides, understanding how health literacy is related to the experiences of patients with remote consultations and supports is essential [ 91 , 92 ]. Research should further examine how such changes in care delivery, including e-health and telemedicine, may have affected inequalities in patient experiences, and how care experiences may be effectively and equally improved in this context.
The following strengths of our study are worth underscoring. First, we conducted a comprehensive analysis of specific patient experiences using a PREM cancer-specific validated questionnaire that encompasses the eight key dimensions of patient-centred care, as well as key aspects of the cancer care pathway – from diagnosis to treatment and follow-up. Second, this is the first study to assess inequalities in cancer patient experiences across multiple hospitals located throughout Switzerland and in a large sample of patients. Only one study has examined such inequalities in four hospitals located in the French-speaking region of Switzerland [ 93 ]. Third, our study contributes to the limited literature on socioeconomic and health literacy inequalities in care experiences among patients with cancer by using PREMs rather than satisfaction measures. This is important since research has usually examined inequalities in patient satisfaction (Batbaatar et al., 2017), while satisfaction is only one facet of patient experience, influenced by various factors that may be unrelated to the direct experience of care services.
Our study also has limitations that need to be considered when interpreting the results. This study is based on a cross-sectional survey data, which does not allow for inferring causal relationhips. We could only consider a limited number of control variables measured in the survey, leaving room for potential unmeasured confounding effects. Our findings reflect care experiences as reported by patients who participated in the survey and were cared for in the participating hospitals. Given the focus of our study on hospitals, future research may assess the care experiences of patients in ambulatory/outpatient centres and private practices. Even in a survey with a relatively high response rate, there is always potential for non-response bias. That is, past research showed that survey participants tend to be younger and more advantaged socioeconomically [ 94 , 95 ] compared to non-responders, which may affect both the survey’s representativeness and the rating of patient experiences. Unfortunately, information on non-responders was not accessible for the SCAPE-2 survey. Time since diagnosis could potentially influence the recall of care experiences in different ways. However, previous research found marginal differences in patterns of care experience when analyses were restricted to patients diagnosed within the past year [ 96 ]. Some outcome variables had a smaller sample size due to the exclusion of ‘not applicable’ responses, potentially affecting statistical power and increasing the likelihood of Type II errors by reducing the ability to detect true associations for these outcomes. Additionally, cancer patient surveys inherently focus on survivors, which excludes patients with shorter survival periods [ 96 , 97 ]. Finally, our study focused on economic status and health literacy, while further patients’ characteristics may influence their experience with cancer care. For example, we did not examine the potential effect of family and social support on patient experience, as these aspects were not included in the SCAPE-2 survey. A recent systematic review stressed the role of patients’ health status, cancer type, prognosis and stage of disease, as well as survey collection methods, in influencing patient-reported experiences [ 17 ]. In this review, being from a lower socioeconomic status or an ethnic minority group, or having a poorer mental health status, were also found to relate to worse cancer care experiences. Future research should pay attention to these determinants, and their potential interaction effects on different cancer care experience outcomes.
To conclude, PREMs have been developed both as a quality indicator for healthcare organisations and systems and as a research topic across different care settings, including cancer care. The present study evidenced inequalities in cancer care as patients with less economic and health literacy resources reported worse experiences with cancer care across eight dimensions of patient-centred care. Such insights into the disparity of experiences between more advantaged and disadvantaged patients may support healthcare professionals and policy-makers in prioritising initiatives to enhance cancer patients’ encounters with the healthcare system. Our findings highlight that cancer care efforts are not yet effectively meeting the needs of disadvantaged patients, implying that a ‘one-size-fits-all’ approach to care may not equally enhance patient experience. Thus, care systems may need to be redesigned considering patients’ socioeconomic and health literacy resources, along with the dimensions of patient-centred care and the patients’ care pathway.
Data availability
While the dataset generated and analysed in this study is not publicly available, it can be accessed upon reasonable request from the data.unisante.ch repository (DOI: https://doi.org/10.16909/DATASET/38 ).
Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open, 2013. 3(1).
Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–69.
Article PubMed Google Scholar
Miller D, et al. Patient-centered care and patient-reported measures: Let’s look before we Leap. Patient. 2015;8(4):293–9.
Jamieson Gilmore K, et al. The uses of patient reported experience measures in health systems: a systematic narrative review. Health Policy. 2023;128:1–10.
Arditi C, Peytremann I, Bridevaux. Giving patients a voice about cancer care: should Switzerland do more to collect patients’ experiences of cancer care? In policy brief . Swiss Learning Health System; 2021.
Bull C, et al. A systematic review of the validity and reliability of patient-reported experience measures. Health Serv Res. 2019;54(5):1023–35.
Article PubMed PubMed Central Google Scholar
Ahmed F, Burt J, Roland M. Measuring patient experience: concepts and methods. Patient. 2014;7(3):235–41.
Bull C. Patient satisfaction and patient experience are not interchangeable concepts. Int J Qual Health Care, 2021. 33(1).
Friedel AL et al. Measuring Patient Experience and Patient Satisfaction-How Are We Doing It and Why Does It Matter? A Comparison of European and U.S. American Approaches Healthcare (Basel), 2023. 11(6).
Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–110.
Article CAS PubMed Google Scholar
Tzelepis F, et al. Measuring the quality of patient-centered care: why patient-reported measures are critical to reliable assessment. Patient Prefer Adherence. 2015;9:831–5.
Nundy S, Cooper LA, Mate KS. The Quintuple Aim for Health Care Improvement: a new imperative to Advance Health Equity. JAMA. 2022;327(6):521–2.
Llanwarne NR, et al. Relationship between clinical quality and patient experience: analysis of data from the English quality and outcomes framework and the National GP Patient Survey. Ann Fam Med. 2013;11(5):467–72.
Black N, Varaganum M, Hutchings A. Relationship between patient reported experience (PREMs) and patient reported outcomes (PROMs) in elective surgery. BMJ Qual Saf. 2014;23(7):534–42.
Weech-Maldonado R, et al. Race/ethnicity, language, and patients’ assessments of care in Medicaid managed care. Health Serv Res. 2003;38(3):789–808.
Saunders CL, Abel GA, Lyratzopoulos G. Inequalities in reported cancer patient experience by socio-demographic characteristic and cancer site: evidence from respondents to the English Cancer Patient Experience Survey. Eur J Cancer Care (Engl). 2015;24(1):85–98.
Alessy SA, et al. Factors influencing cancer patients’ experiences of care in the USA, United Kingdom, and Canada: a systematic review. EClinicalMedicine. 2022;47:101405.
MacLeod S, et al. The impact of inadequate health literacy on patient satisfaction, healthcare utilization, and expenditures among older adults. Geriatr Nurs. 2017;38(4):334–41.
Altin SV, Stock S. The impact of health literacy, patient-centered communication and shared decision-making on patients’ satisfaction with care received in German primary care practices. BMC Health Serv Res. 2016;16(1):450.
Aoki T, Inoue M. Association between health literacy and patient experience of primary care attributes: a cross-sectional study in Japan. PLoS ONE. 2017;12(9):e0184565.
Batbaatar E, et al. Determinants of patient satisfaction: a systematic review. Perspect Public Health. 2017;137(2):89–101.
Okunrintemi V, et al. Association of Income Disparities with patient-reported Healthcare Experience. J Gen Intern Med. 2019;34(6):884–92.
DeVoe JE, Wallace LS, Fryer GE Jr. Measuring patients’ perceptions of communication with healthcare providers: do differences in demographic and socioeconomic characteristics matter? Health Expect. 2009;12(1):70–80.
Nuno-Solinis R et al. Inequalities in Health Care experience of patients with chronic conditions: results from a Population-based study. Healthc (Basel), 2021. 9(8).
Saunders CL, et al. Sociodemographic inequalities in patients’ experiences of primary care: an analysis of the General Practice Patient Survey in England between 2011 and 2017. J Health Serv Res Policy. 2021;26(3):198–207.
Zhong A, et al. Understanding disparities in primary care patient experience. Can Fam Physician. 2021;67(7):e178–87.
Campbell JL, Ramsay J, Green J. Age, gender, socioeconomic, and ethnic differences in patients’ assessments of primary health care. Qual Health Care. 2001;10(2):90–5.
Article CAS PubMed PubMed Central Google Scholar
Glenngard AH. Is patient satisfaction in primary care dependent on structural and organizational characteristics among providers? Findings based on data from the national patient survey in Sweden. Health Econ Policy Law. 2013;8(3):317–33.
El Turabi A, et al. Variation in reported experience of involvement in cancer treatment decision making: evidence from the National Cancer Patient Experience Survey. Br J Cancer. 2013;109(3):780–7.
Bone A, et al. Inequalities in the care experiences of patients with cancer: analysis of data from the National Cancer Patient Experience Survey 2011–2012. BMJ Open. 2014;4(2):e004567.
Ayanian JZ, et al. Patients’ experiences with care for lung cancer and colorectal cancer: findings from the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2010;28(27):4154–61.
Phelan JC, et al. Fundamental causes of social inequalities in mortality: a test of the theory. J Health Soc Behav. 2004;45(3):265–85.
Mielck A, et al. Association between forgone care and household income among the elderly in five western European countries - analyses based on survey data from the SHARE-study. BMC Health Serv Res. 2009;9:p52.
Article Google Scholar
Guessous I, et al. High prevalence of forgoing healthcare for economic reasons in Switzerland: a population-based study in a region with universal health insurance coverage. Prev Med. 2012;55(5):521–7.
van Doorslaer E, et al. Inequalities in access to medical care by income in developed countries. CMAJ. 2006;174(2):177–83.
Shim JK. Cultural health capital: a theoretical approach to understanding health care interactions and the dynamics of unequal treatment. J Health Soc Behav. 2010;51(1):1–15.
Dubbin LA, Chang JS, Shim JK. Cultural health capital and the interactional dynamics of patient-centered care. Soc Sci Med. 2013;93:113–20.
Ratzan SC, et al. National library of medicine current bibliographies in medicine: health literacy. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services; 2000. pp. 331–7.
Google Scholar
Bennett IM, et al. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med. 2009;7(3):204–11.
Berkman ND, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107.
Herndon JB, Chaney M, Carden D. Health literacy and emergency department outcomes: a systematic review. Ann Emerg Med. 2011;57(4):334–45.
Dewalt DA, et al. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19(12):1228–39.
Baker DW, et al. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167(14):1503–9.
Baccolini V, et al. The association between adherence to cancer screening programs and health literacy: a systematic review and meta-analysis. Prev Med. 2022;155:106927.
Amalraj S, et al. Health Literacy, communication, and treatment decision-making in Older Cancer patients Health literacy: improving patient understanding. Oncology-New York. 2009;23(4):369–75.
Bostock S, Steptoe A. Association between low functional health literacy and mortality in older adults: longitudinal cohort study. BMJ. 2012;344:e1602.
Cartwright LA, et al. Health literacy is an independent predictor of cancer patients’ hospitalizations. HLRP: Health Lit Res Pract. 2017;1(4):e153–62.
Shea JA, et al. Health literacy weakly but consistently predicts primary care patient dissatisfaction. Int J Qual Health Care. 2007;19(1):45–9.
Ishikawa H, et al. Patient health literacy and patient-physician information exchange during a visit. Fam Pract. 2009;26(6):517–23.
Halverson JL, et al. Health literacy and health-related quality of Life among a Population-based sample of Cancer patients. J Health Commun. 2015;20(11):1320–9.
Song L, et al. How does health literacy affect quality of life among men with newly diagnosed clinically localized prostate cancer? Findings from the North Carolina-Louisiana prostate Cancer Project (PCaP). Cancer. 2012;118(15):3842–51.
Holden CE, et al. The role of health literacy in cancer care: a mixed studies systematic review. PLoS ONE. 2021;16(11):e0259815.
Nutbeam D, Lloyd JE. Understanding and responding to Health Literacy as a Social Determinant of Health. Annu Rev Public Health. 2021;42:159–73.
Toro N. Who global strategy on integrated people-centred health services (IPCHS). Int J Integr Care, 2015. 15.
NHS England. National Cancer Patient Experience Survey. 2021; https://www.ncpes.co.uk/ .
Gerteis M, et al. Through the patient’s eyes: understanding and promoting patient-centered care. Wiley; 2002.
Jenkinson C, Coulter A, Bruster S. The picker patient experience questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care. 2002;14(5):353–8.
Handley SC, Bell S, Nembhard IM. A systematic review of surveys for measuring patient-centered care in the hospital setting. Med Care. 2021;59(3):228–37.
Abel GA, Saunders CL, Lyratzopoulos G. Cancer patient experience, hospital performance and case mix: evidence from England. Future Oncol. 2014;10(9):1589–98.
Chew LD, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–6.
Benjamini Y, Hochberg Y. Controlling the false Discovery Rate - a practical and powerful Approach to multiple testing. J Royal Stat Soc Ser B-Statistical Methodol. 1995;57(1):289–300.
Colomer-Lahiguera S, et al. Patient and public involvement in cancer research: a scoping review. Cancer Med. 2023;12(14):15530–43.
Petrovic D, et al. The determinants and consequences of forgoing healthcare. Eur J Pub Health. 2020;30:V641–641.
Bodenmann P, et al. Screening primary-care patients forgoing health care for economic reasons. PLoS ONE. 2014;9(4):e94006.
Rosselet PC, et al. Impact of forgoing care because of costs on the quality of diabetes care: a three-year cohort study. Eur J Intern Med. 2017;41:e35–7.
Guessous I, et al. Forgoing dental care for economic reasons in Switzerland: a six-year cross-sectional population-based study. BMC Oral Health. 2014;14:121.
Jolidon V, et al. Revisiting the effects of Organized Mammography Programs on inequalities in breast screening uptake: a multilevel analysis of Nationwide Data from 1997 to 2017. Front Public Health. 2022;10:812776.
Jolidon V, et al. Never and under cervical cancer screening in Switzerland and Belgium: trends and inequalities. BMC Public Health. 2020;20(1):1517.
Fedewa SA, et al. Colorectal Cancer screening in Switzerland: cross-sectional trends (2007–2012) in socioeconomic disparities. PLoS ONE. 2015;10(7):e0131205.
de Mestral C, et al. Forgoing healthcare in Switzerland. Prevalence, determinants, and consequences. Report commissioned by the Federal Office of Public Health. FOPH Bern; 2022.
Davis TC, et al. Health literacy and cancer communication. CA Cancer J Clin. 2002;52(3):134–49.
Koay K, Schofield P, Jefford M. Importance of health literacy in oncology. Asia Pac J Clin Oncol. 2012;8(1):14–23.
Wynia MK, Osborn CY. Health literacy and communication quality in health care organizations. J Health Commun. 2010;15(Suppl 2):102–15.
Williams MV, et al. The role of health literacy in patient-physician communication. Fam Med. 2002;34(5):383–9.
PubMed Google Scholar
Ha Dinh TT, et al. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: a systematic review. JBI Database Syst Rev Implement Rep. 2016;14(1):210–47.
Sheridan SL, et al. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011;16(Suppl 3):30–54.
Visscher BB, et al. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health. 2018;18(1):1414.
Coleman C. Teaching health care professionals about health literacy: a review of the literature. Nurs Outlook. 2011;59(2):70–8.
Kaper MS, et al. Developing and pilot testing a comprehensive health literacy communication training for health professionals in three European countries. Patient Educ Couns. 2018;101(1):152–8.
Elliott MN, et al. Adjusting for subgroup differences in extreme response tendency in ratings of health care: impact on disparity estimates. Health Serv Res. 2009;44(2 Pt 1):542–61.
Rademakers J, et al. Educational inequalities in patient-centred care: patients’ preferences and experiences. BMC Health Serv Res. 2012;12:261.
Roberts BW, et al. Income disparities and Nonresponse Bias in surveys of patient experience. J Gen Intern Med. 2020;35(7):2217–8.
Mora-Pinzon MC, et al. Variation in coordination of care reported by breast cancer patients according to health literacy. Support Care Cancer. 2019;27(3):857–65.
Del Vecchio NJ, et al. Relationships between health literacy, having a cancer care coordinator, and long-term health-related quality of life among cancer survivors. Support Care Cancer. 2021;29(12):7913–24.
Prue G, et al. Exploring patient experiences of cancer care in Northern Ireland: a thematic analysis of free-text responses to the 2018 Northern Ireland Patient Experience Survey (NICPES). BMC Health Serv Res. 2021;21(1):564.
Alessy SA, et al. Being assigned a clinical nurse specialist is associated with better experiences of cancer care: English population-based study using the linked National Cancer Patient Experience Survey and Cancer Registration dataset. Eur J Cancer Care (Engl). 2021;30(6):e13490.
Trezona A, Dodson S, Osborne RH. Development of the organisational health literacy responsiveness (Org-HLR) framework in collaboration with health and social services professionals. BMC Health Serv Res. 2017;17(1):513.
Royce TJ, Sanoff HK, Rewari A. Telemedicine for Cancer Care in the time of COVID-19. JAMA Oncol. 2020;6(11):1698–9.
Safavi AH, et al. Virtual care and electronic patient communication during COVID-19: cross-sectional study of inequities across a Canadian Tertiary Cancer Center. J Med Internet Res. 2022;24(11):e39728.
Katz AJ, et al. Evaluation of Telemedicine Use among US patients with newly diagnosed Cancer by Socioeconomic Status. JAMA Oncol. 2022;8(1):161–3.
Richards T. Can you do what I’m asking you to do? BMJ. 2021;375:n3014.
Kim H, et al. Mobile Health application and e-Health literacy: opportunities and concerns for Cancer patients and caregivers. J Cancer Educ. 2019;34(1):3–8.
Arditi C, et al. Socio-demographic and health-related determinants of patients’ overall rating and experiences of cancer care. BMC Cancer. 2023;23(1):918.
Abel GA, Saunders CL, Lyratzopoulos G. Post-sampling mortality and non-response patterns in the English Cancer Patient Experience Survey: implications for epidemiological studies based on surveys of cancer patients. Cancer Epidemiol. 2016;41:34–41.
Alessy SA, et al. How representative are colorectal, lung, breast and prostate cancer patients responding to the National Cancer Patient Experience Survey (CPES) of the cancer registry population in England? A population-based case control study. BMJ Open. 2019;9(12):e034344.
Lyratzopoulos G, et al. Variation in number of general practitioner consultations before hospital referral for cancer: findings from the 2010 National Cancer Patient Experience Survey in England. Lancet Oncol. 2012;13(4):353–65.
Nartey Y, et al. Who is assessed by a lung cancer nurse specialist in the English Cancer Patient Experience Survey? Lung Cancer. 2022;165:S40–1.
Download references
Acknowledgements
We thank all the patients who took part in the SCAPE-2 survey and made this study possible. We thank the directors of the oncology and haematology departments of the participating hospitals: Prof Solange Peters and Prof Michel Duchosal, Centre hospitalier universitaire vaudois; Dr Sandro Anchisi, Centre Hospitalier du Valais Romand; Dr Adrienne Bettini, Hôpital Fribourgeois; Prof Pierre-Yves Dietrich and Prof Yves Chalandon, Hôpitaux Universitaires de Genève; Prof Dr Roger von Moos, Kantonsspital Graubünden; Prof Dr Stefan Aebi, Luzerner Kantonsspital; Prof Dr Andreas Wicki, Universitätsspital Zürich; and Dr Donat Dürr, Zuger Kantonsspital. We also thank the oncological teams of the participating hospitals for their help in selecting eligible patients, as well as our local administrative team who managed the reception and processing of paper questionnaires. Finally, we thank the Fondation ISREC for their financial support.
Open access funding provided by University of Lausanne. The study was supported by the Swiss Cancer Research foundation (grant number: HSR-4946-11-2019).
Open access funding provided by University of Lausanne
Author information
Authors and affiliations.
Unisanté, University Center for Primary Care and Public Health, Department of Epidemiology and Health Systems, University of Lausanne, CH-1011 Lausanne, Switzerland
Vladimir Jolidon, Isabelle Peytremann-Bridevaux & Chantal Arditi
Institute of Higher Education and Research in Healthcare (IUFRS), Faculty of Biology and Medicine, University of Lausanne, Lausanne, Switzerland
Manuela Eicher
Department of Oncology, Lausanne University Hospital (CHUV), Lausanne, Switzerland
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: VJ, CA, IPB, ME; Formal analysis: VJ; Investigation: CA, IPB, ME; Funding acquisition: CA, IPB, ME; Methodology: VJ, CA, IPB, ME; Project administration: CA, IPB, ME; Supervision: CA, IPB, ME; Visualization: VJ; Writing - original draft: VJ; Writing - review & editing: VJ, CA, IPB, ME; All authors read and approved the final manuscript.
Corresponding author
Correspondence to Chantal Arditi .
Ethics declarations
Ethics approval and consent to participate.
Study methods and analyses were implemented in accordance with the relevant guidelines and regulations. The Ethics Committee on Research involving Humans of Canton of Vaud (CER-VD), which grants authorisations for conducting research within the scope of the Swiss Law on Human Research, reviewed and approved the present study (authorisation number 2021 − 00986). All study participants provided written informed consent.
Consent for publication
Not applicable (personally identifiable information was destroyed and therefore it is not possible to identify participants).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jolidon, V., Eicher, M., Peytremann-Bridevaux, I. et al. Inequalities in patients’ experiences with cancer care: the role of economic and health literacy determinants. BMC Health Serv Res 24 , 733 (2024). https://doi.org/10.1186/s12913-024-11174-x
Download citation
Received : 25 October 2023
Accepted : 05 June 2024
Published : 14 June 2024
DOI : https://doi.org/10.1186/s12913-024-11174-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient experience
- Patient survey
- Patient satisfaction
- Health literacy
- Socioeconomic status
- Information
- Coordination
- Communication
- Quality of care
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
What is Health Equity?
Factors affecting health equity (social determinants of health), ohe’s role in cdc’s core commitment to health equity.
- Optimize Interventions
What You Can Do to Promote Health Equity
Health equity is the state in which everyone has a fair and just opportunity to attain their highest level of health. Achieving this requires ongoing societal efforts to:
- Address historical and contemporary injustices;
- Overcome economic, social, and other obstacles to health and health care; and
- Eliminate preventable health disparities. [1,2]
To achieve health equity, we must change the systems and policies that have resulted in the generational injustices that give rise to racial and ethnic health disparities. Through its CORE strategy , CDC is leading this effort, both in the work we do on behalf of the nation’s health and the work we do internally as an organization.

Health disparities are preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by populations that have been disadvantaged by their social or economic status, geographic location, and environment. [1] Many populations experience health disparities, including people from some racial and ethnic minority groups, people with disabilities, women, people who are LGBTQI+ (lesbian, gay, bisexual, transgender, queer, intersex, or other), people with limited English proficiency, and other groups.
Across the country, people in some racial and ethnic minority groups experience higher rates of poor health and disease for a range of health conditions, including diabetes, hypertension, obesity, asthma, heart disease, cancer, and preterm birth, when compared to their White counterparts. For example, the average life expectancy among Black or African American people in the United States is four years lower than that of White people. [3] These disparities sometimes persist even when accounting for other demographic and socioeconomic factors, such as age or income.
Communities can prevent health disparities when community- and faith-based organizations, employers, healthcare systems and providers, public health agencies, and policymakers work together to develop policies, programs, and systems based on a health equity framework and community needs.
Social determinants of health are the conditions in the places where people live, learn, work, play, and worship that affect a wide range of health risks and outcomes. Long-standing inequities in six key areas of social determinants of health are interrelated and influence a wide range of health and quality-of-life risks and outcomes. Examining these layered health and social inequities can help us better understand how to promote health equity and improve health outcomes.

A person’s social and community context includes their interactions with the places they live, work, learn, play, and worship and their relationships with family, friends, co-workers, community members, and institutions. [4] Interventions are critical to protecting the health and well-being of people who do not get the level of support they need to thrive from their social and community context. For example, children of incarcerated or detained parents may gain from their parents’ participation in reentry programs that assist with job placement or offer parenting support, [5] and lesbian, gay or bi-sexual high school students who are bullied would benefit from school-based programs to reduce violence and prevent bullying. [6]
Social and community context also includes discrimination – or the unfair treatment of people or groups based on characteristics such as race, gender, age, or sexual orientation. Discrimination exists in many systems in society including those meant to protect well-being or health such as health care, housing, education, criminal justice, and finance. [7] Discrimination often has a negative effect on the people and groups who experience it and some people who belong to groups that historically have experienced discrimination, such as people with disabilities, people experiencing homelessness, and people who are incarcerated or detained. As a result, people who have experienced discrimination may be affected by layered health and social inequities.
A growing body of research shows that racism has occurred for centuries at many levels in society in the United States and has had a negative impact on communities of color. [8] Racism is a system, supported and maintained through institutional structures and policies, cultural norms and values, and individual behaviors. [9] There are various forms of racism that—for more than 400 years—have defined and created most of the inequitable structures that exist in our society and lead to health inequities today. The three types of racism include:
- Structural, Institutional, or Systemic Racism : Differential access to the goods, services, and opportunities of society by race
- Personally-mediated or Interpersonal Racism : Prejudice (differential assumptions) and discrimination (differential actions) by individuals towards others
- Internalized Racism : Acceptance by members of the stigmatized races of negative messages about their own abilities and intrinsic worth [10]
Racism determines opportunity based on the way people look or the color of their skin. It also shapes social and economic factors that put some people from racial and ethnic minority groups at increased risk for negative mental health outcomes and health-related behaviors, as well as chronic and toxic stress or inflammation. [11],[12] Racism prevents millions of people from attaining their highest level of health, and consequently, affects the health of our nation.
People with disabilities and people from some racial and ethnic minority groups, rural areas, and White populations with lower incomes are more likely to face multiple barriers to accessing health care. [13][14] For example, structural barriers related to socioeconomic status, such as lack of insurance, [15] transportation, childcare, or ability to take time off work, can make it hard to go to the doctor. Cultural differences between patients and providers as well as language barriers affect patient-provider interactions and health care quality. [16] Inequities in treatment [17] and historical events, like the Tuskegee Study of Untreated Syphilis in the African American Male and sterilization of American Indian women without their permission , might also explain why some people from racial and ethnic minority groups do not trust health care systems and the government’s health-related guidance. [18],[19],[20],[21]
People from racial and ethnic minority groups are disproportionately affected by difficulties finding affordable and quality housing. The practice of redlining or denying mortgages among people of color – and as a result, access to public transportation, supermarkets, and health care – has contributed to segregation of cities in the United States. Although the U.S. Federal Government has enacted legislation since the 1970’s to reduce the segregation of cities, [22] this historical discriminatory practice has limited housing options among racial and ethnic minority groups to neighborhoods and residences that have school districts with inadequate funding, higher crime rates, and poorly resourced infrastructure. These conditions may make illnesses, diseases, and injuries more common and more severe among these groups. In addition, access to nutritious, affordable foods may be limited for these groups, and they may experience more environmental pollution within their neighborhoods. [23],24]
Not all workers have the same risk of experiencing a work-related health problem, even when they have the same job. Occupational health inequities are avoidable differences in work-related disease incidence, mental illness, or morbidity and mortality that are closely linked with social, economic, and/or environmental disadvantage, such as temporary work arrangements, socio-demographic characteristics (e.g., age, sex, gender identity, race, or class), and organizational factors (e.g., lack of worker safety measures, limited or no health insurance benefits).
People who have been historically marginalized, such as people from racial and ethnic minority groups, people with disabilities, and people with lower incomes, are disproportionately affected by inequities in access to high-quality education. [13][14] Policies that link public school funding to the tax base of a neighborhood limit the resources available in schools of lower income neighborhoods. This results in lower-quality education for residents of lower income neighborhoods, which can lead to lower literacy and numeracy levels , lower high school completion rates, and barriers to college entrance. In addition to educational barriers, limited access to quality job training or programs tailored to the language needs of some racial and ethnic minority groups may limit future job options and lead to lower paying or less stable jobs.
People from some racial and ethnic minority groups and other historically marginalized groups also face greater challenges in getting higher paying jobs with good benefits due to less access to high-quality education, [25] geographic location, language differences, discrimination, and transportation barriers. People with limited job options often have lower incomes, experience barriers to wealth accumulation, and carry greater debt. The historical practice of redlining and denying mortgages to people of color has also created a lack of opportunity for home ownership, and thus wealth accumulation, due to the inability to pass down property and build wealth. Such financial challenges may make it difficult to manage expenses, pay medical bills, and access affordable quality housing, education, nutritious food, and reliable childcare.

CDC is transforming its public health research, surveillance, and implementation science efforts to expand beyond listing the markers of health inequities to identifying and addressing the drivers of these disparities. Through the CORE strategy , CDC is integrating health equity as a foundational element across our work – from science and research, to programs, partnerships, and workforce. As part of the initiative, OHE has adopted four CORE goals.

Cultivate comprehensive health equity science
OHE will facilitate and accelerate health equity principles’ adoption across CDC programs, policies, data systems, and funding structures.
OHE is working to:
- Standardize health equity language and principles.
- Establish standards in health equity data collection.
- Provide guidance on analyzing and using data to assess health equity and manage public health programs.
- Incorporate health equity principles and data collection standards into Notice of Funding Opportunities that support research and non-research public health programs at the state and local level.
Potential Impact: National, state, local, tribal, and territorial public health staff will have a better understanding of health equity, the increased capacity to use data to integrate health equity into public health systems and interventions, and ultimately eliminate health disparities in the communities they serve.
Goal in Action: CDC’s CORE Commitment to Health Equity Science and Intervention Strategy

Optimize interventions
OHE/Office of Women’s Health will collaborate with partners to address and reduce the impact of gender discrimination and gendered racism in the workplace.
OHE is collaborating with internal and external partners to:
- Provide input to a national survey to assess the status and impact of gender discrimination and gendered racism in the U.S. population.
- Compile and communicate strategies, policies, and best practices intended to reduce gender discrimination and gendered racism in the workplace.
- Develop and implement strategies for strengthening organizational capacity to achieve and sustain systems changes that promote health equity in the workplace.
Potential Impact: Systems changes will occur in the workplace, including workplaces that set the standard for gender equity best practices, that decrease experiences of gender discrimination and gendered racism, and ultimately, improve mental and physical health among people of all gender identities.
Goal in Action: Evaluation of data on perceptions and experiences of gender discrimination and gendered racism in the workplace.

Reinforce and expand robust partnerships
OHE will mobilize partners to develop and implement strategies addressing health disparities and long-standing inequities including social determinants of health.
OHE is providing guidance and support to partners who respond to public health needs to:
- Develop partners’ capacity to work with CDC to address health inequities, health disparities, and structural and social determinants of health in response to public health crises.
- Design new, or evaluate and refine existing, evidence-based strategies that address health equity and long-standing health disparities and inequities; and develop guidance for implementation of these strategies in diverse communities.
Potential Impact: CDC partners will be engaged and ready to respond to public health emergencies and address long-standing health inequities, health disparities, and structural and social determinants of health.
Goal in Action: National Initiative to Address COVID-19 Health Disparities Among Populations at High-Risk and Underserved, Including Racial and Ethnic Minority Populations and Rural Communities

Enhance capacity and workforce engagement
OHE will transform the public health workforce to ensure diversity and health equity competencies in existing and future staff.
OHE collaborates with internal and external partners to:
- Expand access to undergraduate student internships by linking CDC Undergraduate Public Health Scholars (CUPS) grantees with state, local, and community partners interested in hosting students or establishing pipeline programs.
- Integrate competencies of health equity as well as racism and health into the CDC and public health workforce.
Potential Impact: National, state, local, tribal, and territorial public health agencies will have increased opportunity to support underserved undergraduate students and the current public health workforce with learning how to integrate health equity competencies into public health work. Ultimately, we will create a public health workforce that reflects the communities we serve and is responsive to the country’s changing demographics.
Goal in Action: CDC OHE Student Programs

You—as a community member or member of an organization—can join the effort to ensure that all people have equitable access to resources to maintain and manage their physical and mental health, including easy access to important information, goods and services, and affordable medical and mental health care. Community- and faith-based organizations, employers, healthcare systems and providers, public health agencies, policy makers, and others play a key part in promoting fair access to health, improving opportunity, and ensuring all communities can thrive.
Communities can promote health equity by adopting policies, programs, and practices that:
- Support equitable access to quality and affordable health and other social services (e.g., education, housing, transportation, child care) and accessibility within these services.
- Recognize, respect, and support the diversity of the community they serve.
- Partner with trusted messengers and community health workers/ promotores de salud to share clear and accurate information tailored to a community’s languages, literacy levels, and cultures.
- Include community engagement efforts that can help strengthen partnerships between community members and public health entities, build trust, and promote social connection.
- Engage trusted leaders known by the community and who share the same race and ethnicity, sexual orientation, and cultural or religious beliefs as the community to share information, collect input, or conduct outreach. [24]
- Use clear, easy-to-read, accurate, transparent, and consistent information from a reputable source that is locally and culturally relevant in terms of language, messaging, tone, images, and format. [24] Information should be suitable for diverse audiences, including people with disabilities, limited English proficiency, low literacy, or people who face other challenges accessing health information.
Below are examples of additional actions that organizations and agencies can take to support health equity.
Community and faith-based organizations can:
- Help connect people with healthcare providers, goods (e.g., healthy foods, temporary housing), and services to meet their physical, spiritual, and mental health needs.
- Work with others to address misinformation, myths, and lack of access to appropriate resources. This might include working with trusted local media, local public health departments, or community members to share information or community insights that help connect individuals to resources and free or low-cost services.
Employers can:
- Train employees at all levels of the organization to identify and interrupt all forms of discrimination; provide them with training in implicit bias .
- Establish and maintain equitable leave policies that are fair and flexible to meet the needs of all employees.
Healthcare delivery systems can:
- Deliver all health-related services in a culturally appropriate way and according to the needs of patients. This may include providing the necessary patient supports (e.g., translator, patient navigators).
- Ensure providers show awareness of and respect for culture when providing care.
- Collect and report race and ethnicity data on all patients and educate staff and patients on why this information is an important part of making sure populations are receiving equitable access to care.
Public health agencies can:
- Build partnerships with different sectors (e.g., community- and faith-based organizations, racial and ethnic minority-serving organizations, tribal communities, school and transportation systems, scientific researchers, professional organizations) and community members to share information and collaborate to advance health equity in communities.
- Address misunderstandings about why people are being asked for personal information, including race and ethnicity, and why this information is important to allocate resources and information sharing to people who need them most.

State, tribal, local, and territorial governments can:
- Explore options to provide free or low-cost broadband Internet access so people can use telehealth and get information on health care and social services.
- Reassess policies that create barriers for healthcare providers to collect and report data on race and ethnicity and social determinants of health.
- Partner with public health agencies to evaluate current and proposed policies in transportation, housing, community development, and more for their impacts on health, using a Health in All Policies framework. Prioritize health for communities experiencing health disparities in all policy change.
- Explore options to protect renters from evictions.
- Work to expand childcare service options.
- Increase public transportation services (e.g., free access to city bike programs).
[1] Office of Disease Prevention and Health Promotion. (2021, August 11). Healthy People 2020: Disparities. U.S. Department of Health and Human Services. Retrieved August 13, 2021, from https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities . [2] Braveman P, Arkin E, Orleans T, Proctor D, & Plough A. (2017, May 17). What is health equity? And what difference does a definition make? Robert Wood Johnson Foundation. https://www.rwjf.org/en/library/research/2017/05/what-is-health-equity-.html . [3] Centers for Disease Control and Prevention. Impact of Racism on our Nation’s Health. 2021 [cited 2021 Nov 12]. available from https://www.cdc.gov/healthequity/racism-disparities/impact-of-racism.html . [ 4] DHHS Office of Disease Prevention and Health Promotion. Healthy People 2030: Social and Community Context . Retrieved April 21, 2022 from https://health.gov/healthypeople/objectives-and-data/browse-objectives/social-and-community-context . [5] DHHS Office of Disease Prevention and Health Promotion. Healthy People 2030: Reduce bullying of lesbian, gay, or bisexual high school students — LGBT05 . Retrieved April 27, 2022 from https://health.gov/healthypeople/objectives-and-data/browse-objectives/lgbt/reduce-bullying-lesbian-gay-or-bisexual-high-school-students-lgbt-05 . [6] DHHS Office of Disease Prevention and Health Promotion. Healthy People 2030: Reduce the proportion of children with a parent or guardian who has served time in jail — SDOH05 . Retrieved April 27, 2022 from https://health.gov/healthypeople/objectives-and-data/browse-objectives/social-and-community-context/reduce-proportion-children-parent-or-guardian-who-has-served-time-jail-sdoh-05 . [7] American Psychological Association (2019, October 31). Discrimination: What it is, and how to cope . Retrieved March 21, 2022 from https://www.apa.org/topics/racism-bias-discrimination/types-stress . [8] DHHS Office of Disease Prevention and Health Promotion. Discrimination | Healthy People 2020 . Retrieved March 21, 2022 from https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/discrimination . [9] Center for the Study of Social Policy. (2019, September). Key equity terms and concepts: A glossary for shared understanding. Retrieved July 29, 2021, from https://cssp.org/resource/key-equity-terms-and-concepts-a-glossary-for-shared-understanding . [10] Jones CP. Levels of Racism: A Theoretic Framework and a Gardener’s Tale. Am J Public Health. 2000;90: 1212-1215. https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.90.8.1212 . [11] Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006; 35(4):888–901. DOI: https://doi.org/10.1093/ije/dyl056 . [12 ] Simons RL, Lei MK, Beach SRH, et al. Discrimination, segregation, and chronic inflammation: Testing the weathering explanation for the poor health of Black Americans. Dev Psychol. 2018;54(10):1993-2006. DOI: https://doi.org/10.1037/dev0000511 . [13] Krahn GL, Walker DK, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public Health . 2015;105 Suppl 2(Suppl 2 ):S 198-S206. doi:10.2105/AJPH.2014.302182 [14] Baah FO, Teitelman AM, Riegel B. Marginalization: Conceptualizing patient vulnerabilities in the framework of social determinants of health-An integrative review. Nurs Inq . 2019;26(1 ):e 12268. doi:10.1111/nin.12268 [15] Berchick ER, Barnett JC, and Upton RD. Current Population Reports, P60-267(RV), Health Insurance Coverage in the United States: 2018, U.S. Government Printing Office, Washington, DC, 2019. [16] Institute of Medicine (US) Committee on the Consequences of Uninsurance. Care Without Coverage: Too Little, Too Late. Washington (DC): National Academies Press (US); 2002. DOI: https://doi.org/10.17226/10367 . [17] Institute of Medicine. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press. DOI: https://doi.org/10.17226/10260 . [18] U.S. National Library of Medicine. Native Voices: Timeline: Government admits forced sterilization of Indian Women [online]. 2011 [cited 2020 Jun 24]. Available from: https://www.nlm.nih.gov/nativevoices/timeline/543.html . [19] Novak NL, Lira N, O’Connor KE, Harlow SD, Kardia SLR, Stern AM. Disproportionate Sterilization of Latinos Under California’s Eugenic Sterilization Program, 1920-1945. Am J Public Health. 2018;108(5):611-613. DOI: https://dx.doi.org/10.2105%2FAJPH.2018.304369 . [20] Stern AM. Sterilized in the name of public health: race, immigration, and reproductive control in modern California. Am J Public Health. 2005 Jul;95(7):1128-38. DOI: https://dx.doi.org/10.2105%2FAJPH.2004.041608 . [21] Prather C, Fuller TR, Jeffries WL 4th, et al. Racism, African American Women, and Their Sexual and Reproductive Health: A Review of Historical and Contemporary Evidence and Implications for Health Equity. Health Equity. 2018;2(1):249-259. DOI: https://dx.doi.org/10.1089%2Fheq.2017.0045 . [ 22] Njoku, A., Joseph, M., & Felix, R. (2021). Changing the Narrative: Structural Barriers and Racial and Ethnic Inequities in COVID-19 Vaccination. International journal of environmental research and public health, 18(18), 9904. DOI: https://doi.org/10.3390/ijerph18189904 . [23] Krieger, J., & Higgins, D. L. (2002). Housing and health: time again for public health action. American journal of public health, 92(5), 758–768. DOI: https://doi.org/10.2105/ajph.92.5.758 . [24] Swope, C. B., & Hernández, D. (2019). Housing as a determinant of health equity: A conceptual model. Social science & medicine (1982), 243, 112571. DOI: https://doi.org/10.1016/j.socscimed.2019.112571 . [25] The Annie E. Casey Foundation. Unequal Opportunities in Education [online]. 2006 [cited 2020 Jun 24]. Available from: https://www.aecf.org/m/resourcedoc/aecf-racemattersEDUCATION-2006.pdf . [26] Centers for Disease Control and Prevention. A Guide for Community Partners-Increasing COVID-19 Vaccine Uptake Among Racial and Ethnic Minority Communities [online]. 2021 [cited 2021 Nov 12]. Available from: https://www.cdc.gov/vaccines/covid-19/downloads/guide-community-partners.pdf .
To receive email updates about this page, enter your email address:
- Follow us on Twitter
- Connect on LinkedIn
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Home — Essay Samples — Social Issues — Jim Crow Laws — The Pernicious Legacy of Jim Crow Laws
The Pernicious Legacy of Jim Crow Laws
- Categories: Contract Law Jim Crow Laws
About this sample

Words: 700 |
Published: Jun 13, 2024
Words: 700 | Pages: 2 | 4 min read
Table of contents
Introduction, origins and implementation of jim crow laws, the socio-economic impact of jim crow laws, the political and cultural ramifications of jim crow laws.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr Jacklynne
Verified writer
- Expert in: Law, Crime & Punishment Social Issues

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 875 words
4 pages / 1749 words
3 pages / 1420 words
2 pages / 851 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Jim Crow Laws
The Jim Crow laws were put into place for white people to feel superior to black people, and created even more segregation and racism for African Americans throughout the 1930s. The Jim Crow laws were created to reinforce the [...]
Racial discrimination against blacks circulated the nowadays American society. This type of marginalization took many forms throughout American history. While civil rights movement has addressed the decades-long struggle of [...]
Upon reading a story in the Guardian, the long read titled; "Black Lives Matter: birth of a movement" by Wesley Lowery, one recognizes the theme of police brutality on the black people. Death of Michael Brown generated black [...]
Creating symbolism in literature adds depth and meaning to any story. Alex Haley’s The Autobiography of Malcolm X displays an abundance of symbols that offer insight into the life of Malcolm X himself. Often, the symbols [...]
This study primarily examines the experiences of LGBT workers of color in the workplace. It provides statistics on a wide range of subjects within the overall topic, including unemployment and poverty rates. The report provides [...]
On August 28,1963, Dr. Martin Luther King Jr. delivered a public speech on the steps of the Lincoln Memorial in Washington D.C. This speech would go on to be known as the most famous speech in history, the “I Have a Dream” [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Goal 5: Achieve gender equality and empower all women and girls
Gender equality is not only a fundamental human right, but a necessary foundation for a peaceful, prosperous and sustainable world. There has been progress over the last decades, but the world is not on track to achieve gender equality by 2030.
Women and girls represent half of the world’s population and therefore also half of its potential. But gender inequality persists everywhere and stagnates social progress. On average, women in the labor market still earn 23 percent less than men globally and women spend about three times as many hours in unpaid domestic and care work as men.
Sexual violence and exploitation, the unequal division of unpaid care and domestic work, and discrimination in public office, all remain huge barriers. All these areas of inequality have been exacerbated by the COVID-19 pandemic: there has been a surge in reports of sexual violence, women have taken on more care work due to school closures, and 70% of health and social workers globally are women.
At the current rate, it will take an estimated 300 years to end child marriage, 286 years to close gaps in legal protection and remove discriminatory laws, 140 years for women to be represented equally in positions of power and leadership in the workplace, and 47 years to achieve equal representation in national parliaments.
Political leadership, investments and comprehensive policy reforms are needed to dismantle systemic barriers to achieving Goal 5 Gender equality is a cross-cutting objective and must be a key focus of national policies, budgets and institutions.
How much progress have we made?
International commitments to advance gender equality have brought about improvements in some areas: child marriage and female genital mutilation (FGM) have declined in recent years, and women’s representation in the political arena is higher than ever before. But the promise of a world in which every woman and girl enjoys full gender equality, and where all legal, social and economic barriers to their empowerment have been removed, remains unfulfilled. In fact, that goal is probably even more distant than before, since women and girls are being hit hard by the COVID-19 pandemic.
Are they any other gender-related challenges?
Yes. Worldwide, nearly half of married women lack decision-making power over their sexual and reproductive health and rights. 35 per cent of women between 15-49 years of age have experienced physical and/ or sexual intimate partner violence or non-partner sexual violence.1 in 3 girls aged 15-19 have experienced some form of female genital mutilation/cutting in the 30 countries in Africa and the Middle East, where the harmful practice is most common with a high risk of prolonged bleeding, infection (including HIV), childbirth complications, infertility and death.
This type of violence doesn’t just harm individual women and girls; it also undermines their overall quality of life and hinders their active involvement in society.
Why should gender equality matter to me?
Regardless of where you live in, gender equality is a fundamental human right. Advancing gender equality is critical to all areas of a healthy society, from reducing poverty to promoting the health, education, protection and the well-being of girls and boys.
What can we do?
If you are a girl, you can stay in school, help empower your female classmates to do the same and fight for your right to access sexual and reproductive health services. If you are a woman, you can address unconscious biases and implicit associations that form an unintended and often an invisible barrier to equal opportunity.
If you are a man or a boy, you can work alongside women and girls to achieve gender equality and embrace healthy, respectful relationships.
You can fund education campaigns to curb cultural practices like female genital mutilation and change harmful laws that limit the rights of women and girls and prevent them from achieving their full potential.
The Spotlight Initiative is an EU/UN partnership, and a global, multi-year initiative focused on eliminating all forms of violence against women and girls – the world’s largest targeted effort to end all forms of violence against women and girls.

Facts and figures
Goal 5 targets.
- With only seven years remaining, a mere 15.4 per cent of Goal 5 indicators with data are “on track”, 61.5 per cent are at a moderate distance and 23.1 per cent are far or very far off track from 2030 targets.
- In many areas, progress has been too slow. At the current rate, it will take an estimated 300 years to end child marriage, 286 years to close gaps in legal protection and remove discriminatory laws, 140 years for women to be represented equally in positions of power and leadership in the workplace, and 47 years to achieve equal representation in national parliaments.
- Political leadership, investments and comprehensive policy reforms are needed to dismantle systemic barriers to achieving Goal 5. Gender equality is a cross-cutting objective and must be a key focus of national policies, budgets and institutions.
- Around 2.4 billion women of working age are not afforded equal economic opportunity. Nearly 2.4 Billion Women Globally Don’t Have Same Economic Rights as Men
- 178 countries maintain legal barriers that prevent women’s full economic participation. Nearly 2.4 Billion Women Globally Don’t Have Same Economic Rights as Men
- In 2019, one in five women, aged 20-24 years, were married before the age of 18. Girls | UN Special Representative of the Secretary-General on Violence Against Children
Source: The Sustainable Development Goals Report 2023
5.1 End all forms of discrimination against all women and girls everywhere
5.2 Eliminate all forms of violence against all women and girls in the public and private spheres, including trafficking and sexual and other types of exploitation
5.3 Eliminate all harmful practices, such as child, early and forced marriage and female genital mutilation
5.4 Recognize and value unpaid care and domestic work through the provision of public services, infrastructure and social protection policies and the promotion of shared responsibility within the household and the family as nationally appropriate
5.5 Ensure women’s full and effective participation and equal opportunities for leadership at all levels of decisionmaking in political, economic and public life
5.6 Ensure universal access to sexual and reproductive health and reproductive rights as agreed in accordance with the Programme of Action of the International Conference on Population and Development and the Beijing Platform for Action and the outcome documents of their review conferences
5.A Undertake reforms to give women equal rights to economic resources, as well as access to ownership and control over land and other forms of property, financial services, inheritance and natural resources, in accordance with national laws
5.B Enhance the use of enabling technology, in particular information and communications technology, to promote the empowerment of women
5.C Adopt and strengthen sound policies and enforceable legislation for the promotion of gender equality and the empowerment of all women and girls at all levels
He for She campaign
United Secretary-General Campaign UNiTE to End Violence Against Women
Every Woman Every Child Initiative
Spotlight Initiative
United Nations Children’s Fund (UNICEF)
UN Population Fund: Gender equality
UN Population Fund: Female genital mutilation
UN Population Fund: Child marriage
UN Population Fund: Engaging men & boys
UN Population Fund: Gender-based violence
World Health Organization (WHO)
UN Office of the High Commissioner for Human Rights
UN High Commissioner for Refugees (UNHCR)
UN Education, Scientific and Cultural Organisation (UNESCO)
UN Department of Economic and Social Affairs, Gender Statistics
Fast Facts: Gender Equality

Infographic: Gender Equality
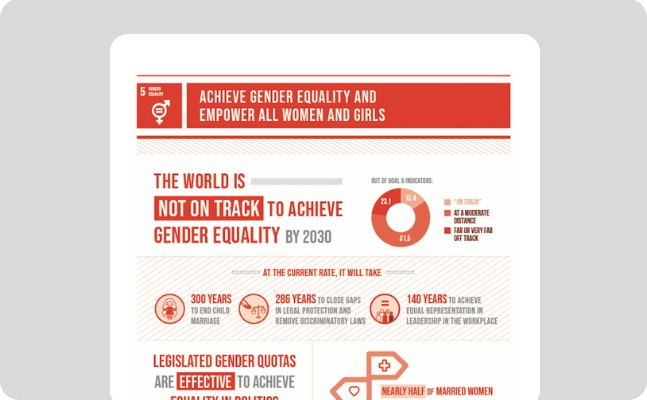
The Initiative is so named as it brings focused attention to this issue, moving it into the spotlight and placing it at the centre of efforts to achieve gender equality and women’s empowerment, in line with the 2030 Agenda for Sustainable Development.
An initial investment in the order of EUR 500 million will be made, with the EU as the main contributor. Other donors and partners will be invited to join the Initiative to broaden its reach and scope. The modality for the delivery will be a UN multi- stakeholder trust fund, administered by the Multi-Partner Trust Fund Office, with the support of core agencies UNDP, UNFPA and UN Women, and overseen by the Executive Office of the UN Secretary-General.
Related news
Press release| the world is failing girls and women, according to new un report.
Yinuo 2023-09-06T19:30:02-04:00 07 Sep 2023 |
The world is failing girls and women, according to new UN report New figure points to the need of an additional $360 billion in investment per year to achieve genderequality and women’s empowerment by 2030. [...]
Liberia, Mexico, Niger, Senegal and Sierra Leone to tackle barriers to the deployment of women in peace operations with the support of the UN Elsie Initiative Fund
Vesna Blazhevska 2021-04-28T13:20:09-04:00 28 Apr 2021 |
PRESS RELEASE 28 APRIL 2021 MEDIA ENQUIRIES [email protected] Liberia, Mexico, Niger, Senegal and Sierra Leone to tackle barriers to the deployment of women in peace operations with the support of the UN Elsie Initiative [...]
Women’s job market participation stagnating at less than 50% for the past 25 years, finds UN report
Vesna Blazhevska 2020-10-20T15:06:56-04:00 20 Oct 2020 |
New York, 20 October – Less than 50% of working-age women are in the labour market, a figure that has barely changed over the last quarter of a century, according to a new UN report launched today. Unpaid domestic and care work falls disproportionately on women, restraining their economic potential as the COVID-19 pandemic additionally affects women’s jobs and livelihoods, the report warns.
Related videos
Press release | progress on basic energy access reverses for first time in a decade.
Global energy access gap worsens as population growth outpaces new connections: 685 million people living without electricity access in 2022, 2.1 billion people continue to rely on damaging cooking fuels globally 12 June 2024 | [...]
Guterres hails 60 years of UN trade and development action
The right to development is inextricably linked with trade which the world’s poorest countries - now “mired in debt” through no fault of their own - have every right to pursue on much fairer terms, UN chief António Guterres insisted on Wednesday.
Ukraine Recovery Conference: UN sounds alarm over humanitarian funding
The UN is becoming increasingly concerned over falling levels of humanitarian funding for civilians across war-torn Ukraine, the head of the UN Development Programme (UNDP) told delegates to the Ukraine Recovery Conference in Berlin on Wednesday.

COMMENTS
The February issue of 2018 addressed the role of theory in health inequality research, the relationship between socio-political context and health [], and it also highlighted the recent turn in social epidemiology towards studying the impact of institutional arrangements, social policy and political context on population health [].Moreover, the issue suggested that moving forward from where we ...
In this essay, we focus on the potential and promise that intersectionality holds as a lens for studying the social determinants of health, reducing health disparities, and promoting health equity and social justice. Research that engages intersectionality as a guiding conceptual, methodological, and praxis-oriented framework is focused on power dynamics, specifically the relationships between ...
Leveraging Community Health Workers and Social Determinants of Health for Predicting Emergency Department Readmissions, 2023 Fifth International Conference on Transdisciplinary AI (TransAI), (42 ...
"The topics of racial and ethnic disparities and inequities in medicine and health care are of critical importance," Dr. Phil B. Fontanarosa, interim editor in chief of JAMA, said in a statement.
INTRODUCTION. Social determinants of health (SDoH) as defined by the US Centers for Disease Control and Prevention (CDC) are the conditions in which people live, learn, work, and play that are determined by the distribution of money, power, and resources and that affect a wide range of health and quality-of-life risks and outcomes. 1 Influenced by the social construct of race, SDoH exert ...
This study aimed to review the role of health-related social factors in overcoming health disparities. We conducted a search of English-language literature, including studies published on health and health equalities or inequalities. Most reports show that social determinants of health have a higher effect on health.
2.1. Health inequality. Dictionaries define inequality as the "quality of being unequal or uneven" (Merriam-Webster, n.d.).The term, health inequality, used in most countries other than the U.S., is based on the seminal work of Margaret Whitehead in the United Kingdom (Whitehead, 2007), and refers not only to the quality of being unequal or uneven in health outcomes between groups but also ...
A review of 155 papers that explored income inequality and population health found that health tends to be poorer in less equal societies, ... Social group health inequalities may be generated early or late in life by differences in access to material resources, social circumstances that generate stress, or health behaviors. ...
Abstract. Health inequalities according to people's social standing are persisting, or even growing, in modern societies. Recent decades have revealed evidence of strong variations in life expectancy, both between countries and within them. This widening of social inequalities has developed despite considerable progress in medical science and ...
In the United States, racial/ethnic minority, rural, and low-income populations continue to experience suboptimal access to and quality of health care despite decades of recognition of health dispa...
This review summarises the present state of research on health inequalities using a social network perspective, and it explores the available studies examining the interrelations of social inequality, social networks, and health. Using the strategy of a scoping review, as outlined by Arksey and O'Malley (Int J Sci Res Methodol 8:19-32, 2005), our team performed two searches across eight ...
Essays on Health Care and Inequality Abstract This dissertation consists of three chapters analyzing the role of institutional factors in observed health inequities. In the first chapter, I measure how differences in neighborhood environments contribute to Black-white disparities in primary care outcomes. I study this question in the context
The social determinants of health that typically make up this field of study are social class, sex, age, race, and ethnicity. In this essay I focus mainly on social class but note that there is a ...
A September 2019 report from the National Academies of Sciences, Engineering, and Medicine suggests that integrating social care into the delivery of health care for groups experiencing health disparities requires a careful approach with a range of specific activities. "Many programs and commitments are in the early stages — awareness of ...
investigate three areas of interest to social sc ientists studying health: (1) economic. inequality and financial crises, (2) socioeco nomic inequality and health behaviors, and. (3) cohort ...
Health-care systems worldwide are fraught with inequalities that have a disproportionate impact on minoritised ethnic and racial groups. These inequalities may lead to reduced access to appropriate health care services, and consequently, poorer health outcomes. Furthermore, research focusing on health outcomes of racial minorities is vastly lacking. In an effort to address the need for ...
This report evaluates disparities in health and health care across racial and ethnic groups, ... July 2020); and Gopal K. Singh and Stella M. Yu, "Infant Mortality in the United States, 1915-2017: Large Social Inequalities Have Persisted for Over a Century," International Journal of Maternal and Child Health and AIDS 8, ...
Inequalities in Health and Illness. An Essay by Emma Bushnell. ... Social inequalities reported to influence the health were income, education, housing, diet, employment, and conditions of work and, thus, the report recommended social policy measures should be introduced to combat these inequalities. Gray, (1982).
A health care disparity typically refers to differences between groups in health insurance coverage, affordability, access to and use of care, and quality of care. The terms "health inequality ...
Relationship between social disadva ntage and inequalities in health outcom es. Karmacharya, Shrawasti. 2022. Introduction. World Health Organization defines the health as a state of complete ph ...
Background Patients with fewer socioeconomic and health literacy resources are disadvantaged in their access and use of healthcare, which may give rise to worse experiences with care and thus inequalities in patient experiences. However, only a limited number of studies have examined how socioeconomic and health literacy factors shape inequalities in patients' experiences with cancer care ...
Health equity is the state in which everyone has a fair and just opportunity to attain their highest level of health. Achieving this requires ongoing societal efforts to: Address historical and contemporary injustices; Overcome economic, social, and other obstacles to health and health care; and. Eliminate preventable health disparities. [1,2]
As health inequality researchers have been keen to point out, the very term inequality implies a difference which is unfair, harmful and avoidable [9]. First and fore-most, health inequalities are a problem of injustice, because they unfairly deprive people of life-chances based on their position in society. Secondly, health inequalities are a ...
I feel like I'm being a social worker again, at the hospice': Using interpretative phenomenological analysis to explore social workers' experiences of hospice work
Overall, these findings cast doubt on the claim that intraracial inequalities based on skin color gradients equate or exceed categorical inequalities between ethnoracial groups. Although such assertions might be valid in certain areas, such as health ( Monk 2015 ), this is not the case for educational and labor market outcomes.
The International Agency for Research on Cancer (IARC) classifies tobacco smoke as a Group 1 carcinogen, meaning it is a confirmed cause of cancer in humans. Smoking is linked to cancers of the lung, mouth, throat, esophagus, pancreas, bladder, and cervix, among others. Lung cancer, in particular, is the leading cause of cancer-related deaths ...
embedded within systems of inequality. Intersectionality also is attentive to the need to link individual, institutional, and structural levels of power in a given sociohistori-cal context for advancing health equity and social justice. DISCUSSION PAPER Perspectives Expert Voices in Health & Health Care Health Disparities, Inequity, and Social
Gregory Mantsios' essay "Class in America" brings to light the stark realities of social inequality in the United States. Through a combination of statistical evidence and insightful commentary, Mantsios challenges the pervasive myth of a classless society and underscores the significant disparities that exist between different social strata.
Jim Crow laws, a system of institutionalized racial segregation and discrimination, emerged in the United States during the late 19th and early 20th centuries. These laws, named after a black minstrel show character, effectively relegated African Americans to a status of second-class citizenship. The ramifications of Jim Crow laws were profound ...
But gender inequality persists everywhere and stagnates social progress. On average, women in the labor market still earn 23 percent less than men globally and women spend about three times as ...