- Help & FAQ

Psychological safety: A systematic review of the literature
- Department of Management
Research output : Contribution to journal › Article › Research › peer-review
Since the concept of psychological safety was introduced, empirical research on its antecedents, outcomes, and moderators at different levels of analysis has proliferated. Given a burgeoning body of empirical evidence, a systematic review of the psychological safety literature is warranted. As well as reviewing empirical work on psychological safety, the present article highlights gaps in the literature and provides direction for future work. In doing so, it highlights the need to advance our understanding of psychological safety through the integration of key theoretical perspectives to explain how psychological safety develops and influences work outcomes at different levels of analysis. Suggestions for future empirical research to advance our understanding of psychological safety are also provided.
| Original language | English |
|---|---|
| Pages (from-to) | 521-535 |
| Number of pages | 15 |
| Journal | |
| Volume | 27 |
| Issue number | 3 |
| DOIs | |
| Publication status | Published - 1 Sept 2017 |
- Measurement issues
- Psychological safety
- Work outcomes
Access to Document
- 10.1016/j.hrmr.2017.01.001
Other files and links
- Link to publication in Scopus
Press/Media
Employee wellbeing: building a psychologically safe place for all.
30/11/18 → 11/11/19
2 items of Media coverage
Press/Media : Article/Feature
Human Resource Management Review Scholarly Impact Award Winner (2017-2022)
Newman, Alex (Recipient), Donohue, Ross (Recipient) & Eva, Nathan (Recipient), 2022
Prize : Other distinction
T1 - Psychological safety
T2 - A systematic review of the literature
AU - Newman, Alexander
AU - Donohue, Ross
AU - Eva, Nathan
PY - 2017/9/1
Y1 - 2017/9/1
N2 - Since the concept of psychological safety was introduced, empirical research on its antecedents, outcomes, and moderators at different levels of analysis has proliferated. Given a burgeoning body of empirical evidence, a systematic review of the psychological safety literature is warranted. As well as reviewing empirical work on psychological safety, the present article highlights gaps in the literature and provides direction for future work. In doing so, it highlights the need to advance our understanding of psychological safety through the integration of key theoretical perspectives to explain how psychological safety develops and influences work outcomes at different levels of analysis. Suggestions for future empirical research to advance our understanding of psychological safety are also provided.
AB - Since the concept of psychological safety was introduced, empirical research on its antecedents, outcomes, and moderators at different levels of analysis has proliferated. Given a burgeoning body of empirical evidence, a systematic review of the psychological safety literature is warranted. As well as reviewing empirical work on psychological safety, the present article highlights gaps in the literature and provides direction for future work. In doing so, it highlights the need to advance our understanding of psychological safety through the integration of key theoretical perspectives to explain how psychological safety develops and influences work outcomes at different levels of analysis. Suggestions for future empirical research to advance our understanding of psychological safety are also provided.
KW - Learning
KW - Measurement issues
KW - Psychological safety
KW - Work outcomes
UR - http://www.scopus.com/inward/record.url?scp=85009816141&partnerID=8YFLogxK
U2 - 10.1016/j.hrmr.2017.01.001
DO - 10.1016/j.hrmr.2017.01.001
M3 - Article
AN - SCOPUS:85009816141
SN - 1053-4822
JO - Human Resource Management Review
JF - Human Resource Management Review
- Access through your organization
- Purchase PDF
- Patient Access
- Other access options
Article preview
Section snippets, references (40), cited by (2), education and clinical practice: special features psychological safety : what it is, why teams need it, and how to make it flourish, psychological safety: an overview, psychological safety in pccm: safety and quality, psychological safety for the administrator: strategies to foster psychological safety on teams, conclusions, financial/nonfinancial disclosures, psychological safety: a systematic review of the literature, hum res manag rev, psychological safety and infection prevention practices: results from a national survey, am j infect control, resilience vs. vulnerability: psychological safety and reporting of near misses with varying proximity to harm in radiation oncology, jt comm j qual patient saf, patient safety: break the silence, the fearless organization: creating psychological safety in the work place for learning, innovation, and growth, psychological safety: the history, renaissance, and future of an interpersonal construct, annu rev organ psychol organ behav, managing the risk of learning: psychological safety in work teams, what google learned from its quest to build the perfect team, the clinician as leader: why, how, and when, ann am thorac soc, understanding psychological safety in health care and education organizations: a comparative perspective, res hum dev, psychological conditions of personal engagement and disengagement at work, acad manage j, to err is human: building a safer health system, speaking up for patient safety by hospital-based health care professionals: a literature review, bmc health serv res, dissecting communication barriers in healthcare: a path to enhancing communication resiliency, reliability, and patient safety, j patient saf, psychological safety on the healthcare team, nurs manage, the presence and potential impact of psychological safety in the healthcare setting: an evidence synthesis, behavioral integrity for safety, priority of safety, psychological safety, and patient safety: a team-level study, j appl psychol, making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams, j organ behav, the role of continuous quality improvement and psychological safety in predicting work-arounds, health care manage rev, managing routine exceptions: a model of nurse problem solving behavior, mistakes are not an option: aggression from peers and other correlates of anxiety and depression in pediatricians in training, second victim experience: a dynamic process conditioned by the environment. a qualitative research.
- Social Perception
- Developmental Psychology
- Psychological Safety
Psychological safety: A systematic review of the literature
- January 2017
- Human Resource Management Review 27(3)

- Deakin University
- This person is not on ResearchGate, or hasn't claimed this research yet.

- Monash University (Australia)
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
Article Contents
Introduction, methodology.
- < Previous
A systematic review of factors that enable psychological safety in healthcare teams
- Article contents
- Figures & tables
- Supplementary Data
Róisín O’donovan, Eilish Mcauliffe, A systematic review of factors that enable psychological safety in healthcare teams, International Journal for Quality in Health Care , Volume 32, Issue 4, May 2020, Pages 240–250, https://doi.org/10.1093/intqhc/mzaa025
- Permissions Icon Permissions
The current systematic review will identify enablers of psychological safety within the literature in order to produce a comprehensive list of factors that enable psychological safety specific to healthcare teams.
A keyword search strategy was developed and used to search the following electronic databases PsycINFO, ABI/INFORM, Academic search complete and PubMed and grey literature databases OpenGrey, OCLC WorldCAT and Espace.
Peer-reviewed studies relevant to enablers of psychological safety in healthcare setting that were published between 1999 and 2019 were eligible for inclusion. Covidence, an online specialized systematic review website, was used to screen records. Data extraction, quality appraisal and narrative synthesis were conducted on identified papers.
Thirty-six relevant studies were identified for full review and data extraction. A data extraction template was developed and included sections for the study methodology and the specific enablers identified within each study.
Identified studies were reviewed using a narrative synthesis. Within the 36 articles reviewed, 13 enablers from across organizational, team and individual levels were identified. These enablers were grouped according to five broader themes: priority for patient safety, improvement or learning orientation, support, familiarity with colleagues, status, hierarchy and inclusiveness and individual differences.
This systematic review of psychological safety literature identifies a list of enablers of psychological safety within healthcare teams. This list can be used as a first step in developing observational measures and interventions to improve psychological safety in healthcare teams.
When teams are psychologically safe, they have a shared belief that they can take interpersonal risks, such as speaking up, asking questions and sharing ideas [ 1 ]. Psychological safety is associated with improved team learning [ 1 , 2 ], workplace creativity [ 3 , 4 ] and team performance [ 5–7 ]. These outcomes make psychological safety particularly important within high stakes work environments, such as healthcare organizations. Healthcare professionals must work interdependently, within a highly complex and dynamic work environment, to provide safe care for patients [ 3 , 8 ]. This makes psychological safety particularly vital within healthcare settings.
Despite the importance of psychological safety in healthcare teams, it is often lacking. Healthcare professionals are reluctant to speak up about concerns due to fear of retribution, not being listened to or not wanting to cause trouble [ 9–12 ]. There is an absence of interventions to improve psychological safety within healthcare teams and a lack of clear objective measures to understand when psychological safety is low and to track changes over time [ 13 ]. Previous research has established the benefits of improving psychological safety in healthcare teams, and it is now time to shift our focus to building interventions to do so. Identifying practical enablers of psychological safety within healthcare teams is an important first step in developing interventions to improve and maintain psychological safety.
Previous research has established that inclusive leadership behaviours, good interpersonal relationships and supportive organizational practices can promote psychological safety [ 5 , 6 , 14 , 15 ]. Previous systematic reviews have explored antecedents of psychological safety in a variety of workplace contexts [ 6 , 7 ]. Most recently, Newman and colleagues [ 5 ] examined antecedents of psychological safety, including, supportive leadership, organizational practices, relationship networks, team characteristics and individual differences. However, only 6 (13%) of these studies were conducted in a healthcare environment [ 2 , 8 , 16–19 ]. Aranzamendez et al. [ 15 ] identified leaders’ behaviour as a major antecedent to psychological safety in healthcare settings. While leadership plays an important role in psychological safety, it is but one dimension of a complex system of organizational-, team- and individual-level factors that may influence an individual’s sense of psychological safety. This study seeks to advance our understanding of the concept of psychological safety by taking a systems approach to identify the practical enablers of psychological safety in the healthcare environment. This list of practical enablers can inform the development of observational measures of psychological safety and interventions to improve psychological safety, which are tailored for use within healthcare teams.
The protocol for this review has been published on PROSPERO (registration number: CRD42018107650).
Inclusion and exclusion criteria
Peer-reviewed studies that identified enablers of psychological safety, speaking up or voice behaviour, within healthcare teams were included in this review. Included studies were experimental or observational research from any country carried between 1999 and 2019. The relevant studies were extracted from systematic literature reviews, and the reviews were excluded to avoid duplication of data. Studies were excluded if they were not available in English or if they were not conducted within a healthcare setting.
Search strategy
Keywords were identified through a scoping review of the literature and were grouped together using the OR Boolean term. The search strategy was reviewed by a researcher with extensive systematic review experience. The final search is presented in Table 1 .
Search strategies used
| Database . | Search string . |
|---|---|
| PsychInfo and ABI/INFORM | AB,TI(“Psychological safe ” OR “speak up” OR voic OR silen ) |
| PubMed | (((“Psychological safe ”[Title/Abstract] OR “speak up”[Title/Abstract] OR voic [Title/Abstract] OR silen [Title/Abstract])) AND (“1999/01/01”[PDat]: “2018/12/31”[PDat])) |
| Academic search complete search string | AB “Psychological safe ” OR “speak up” OR voic OR silen |
| Database . | Search string . |
|---|---|
| PsychInfo and ABI/INFORM | AB,TI(“Psychological safe ” OR “speak up” OR voic OR silen ) |
| PubMed | (((“Psychological safe ”[Title/Abstract] OR “speak up”[Title/Abstract] OR voic [Title/Abstract] OR silen [Title/Abstract])) AND (“1999/01/01”[PDat]: “2018/12/31”[PDat])) |
| Academic search complete search string | AB “Psychological safe ” OR “speak up” OR voic OR silen |
Information sources
Electronic databases were searched between 19 March 2018 and 8 June 2018 and were then updated between 10 July 2019 and 19 August 2019. The electronic databases searched were PsycINFO, ABI/INFORM, Academic search complete and PubMed. The grey literature databases searched were OpenGrey, OCLC WorldCAT and Espace (Curtin’s institutional repository). The authors also hand-searched the reference lists of included studies and contacted experts in the field to identify any further eligible studies.
Study screening
Covidence, an online specialized systematic review website, was used to screen studies. One reviewer screened record titles and abstracts based on the eligibility criteria. Two reviewers then independently reviewed the identified full-text studies. If there was any disagreement or ambiguity, a third reviewer assessed the relevant records, and consensus was reached on eligibility through discussion.
Data extraction process
A data extraction template was developed based on the guidelines produced by the Cochrane Public Health Group (see Table 2 ).
Data extraction template
| Review title or ID | |||||
| Author(s) | |||||
| Date published | |||||
| Date extraction completed | |||||
| Publication type | |||||
| Notes | |||||
| Methods | |||||
| Descriptions as stated in report/paper | Location in text | ||||
| Aim of study | |||||
| Design | |||||
| Participants | |||||
| Data collection | |||||
| Variables of interest | |||||
| Key findings | |||||
| Ethical approval needed/obtained for study | □ | □ | □ | ||
| Yes | No | Unclear | |||
| Notes: | |||||
| Enabler 1 | |||||
| Description | Location in text | ||||
| Description/definition | |||||
| Relationship to other enablers | |||||
| Other evidence | |||||
| Notes: | |||||
| Review title or ID | |||||
| Author(s) | |||||
| Date published | |||||
| Date extraction completed | |||||
| Publication type | |||||
| Notes | |||||
| Methods | |||||
| Descriptions as stated in report/paper | Location in text | ||||
| Aim of study | |||||
| Design | |||||
| Participants | |||||
| Data collection | |||||
| Variables of interest | |||||
| Key findings | |||||
| Ethical approval needed/obtained for study | □ | □ | □ | ||
| Yes | No | Unclear | |||
| Notes: | |||||
| Enabler 1 | |||||
| Description | Location in text | ||||
| Description/definition | |||||
| Relationship to other enablers | |||||
| Other evidence | |||||
| Notes: | |||||
Quality assessment
Depending on the study design, the Critical Appraisal Skills Programme (CASP) Qualitative Checklist, the CASP Cohort Study Checklist, the Joanna Briggs Institute Critical Appraisal Checklist for Analytical Cross-Sectional Studies or the Mixed Methods Appraisal Tool was used to assess the quality of included studies.
Study synthesis
Identified studies were reviewed using a narrative synthesis [ 20 ]. The iterative steps outlined in Popay et al. [ 20 ] were followed: familiarization with studies and organizing then into logical categories, comparing and synthesizing studies, exploring relationships within and between the studies and synthesizing data under the relevant themes.
Thirty-six relevant studies were included for full review and data extraction. The PRISMA diagram included in Fig. 1 illustrates the full screening process. A summary of each article can be found in Table 3 . Table 4 presents the 13 enablers identified.

PRISMA flow diagram illustrating the inclusion and exclusion of identified studies.
The key themes identified in the literature are reported below.
Priority for patient safety
Thirteen studies suggested that a priority for patient safety can support psychological safety.
Safety culture . At the organizational level, studies identified safety culture as an enabler of psychological safety. Nurses’ with higher perceptions of safety climate also had higher psychological safety [ 21 ]. When hospitals have a safety culture, staff can speak up and discuss concerns openly [ 22–24 ]. Cultivating a safety culture among all healthcare professionals can help to make safe public spaces which can encourage newly graduated registered nurses to speak up [ 25 ].
Leader behavioural integrity for safety . Behavioural integrity is when leaders’ words and deeds relating to safety are in alignment. This signals to team members that their concern for safety is genuine and that it is safe to report errors. Leroy et al. [ 17 ] found that team psychological safety moderated the indirect relationship between leader behavioural integrity for safety and reported treatment error.
Professional responsibility . When healthcare professionals know that speaking up will result in meaningful change to patient safety, they are more likely to speak up [ 26 ]. Nursing staff have reported that their sense of responsibility and accountability for their patients motivated them to speak up to protect them, even when doing so was difficult or uncomfortable [ 10 , 24 , 27–31 ].
Summary of reviewed studies, sorted by year of publication
| Author . | Aims . | Participants . | Setting . | Enablers identified . | Methods of Evaluation . |
|---|---|---|---|---|---|
| Edmondson (2003) | Explore the impact of leader behaviours on speaking up within teams | 16 operating room teams | Hospital | Boundary spanning coaching leadership | Interviews: qualitative and quantitative data |
| Atwal and Caldwell (2005) | Record interactions of the team members using the Bales’ interaction process analysis | Healthcare professionals in two older persons multidisciplinary team meetings | Large acute NHS Trust | Hierarchy/status | Observations of meetings |
| Maxfield (2005) | Exploring concerns about communication that may contribute to avoidable errors and other problems in healthcare | 1700 nurses, physicians, clinical care and administrative staff | Urban, suburban and rural hospitals in the USA | Culture of safety | Focus groups, interviews, workplace observations and survey |
| Nembhard and Edmondson (2006) | Examine the relationship between status and psychological safety | 1440 healthcare professionals (physicians, nurses, respiratory therapists, social workers, dieticians) | 23 neonatal intensive care units in the USA and Canada | Status Leader inclusiveness | Survey |
| Attree (2007) | Explore factors influencing nurses’ decisions to raise concerns | 142 nurses | Acute National Health Service (NHS) Trust in England | Professional responsibility Positive leadership | Survey |
| Dufresne (2007) | Explore the relationship between debriefing leaders, psychological safety and learning behaviours after critical incidents | 40 teams (227 resident anaesthesiologists) | Center for Medical Simulation in Cambridge | Positive leadership behaviours | Videotaped team debriefing |
| Halbesleben and Rathert (2008) | Examine continuous quality improvement and psychological safety in workarounds | 83 cancer registrars | Acute care hospitals in the USA | Continuous improvement | Survey |
| Tangirala and Ramanujam (2008) | Examine the cross-level effects of procedural justice climate on silence | 606 frontline hospital nurses from 30 workgroups | A large Midwestern hospital | Personal control | Survey |
| Carmeli and Zisu (2009) | Examine a three-pronged model of organizational trust, perceived organizational support and psychological safety | Employees who work in medical clinics and provide daily medical services | Large healthcare organization in Israel | Perceived organizational support | Survey |
| Rathert (2009) | Explore model linking the work environment to work engagement, organizational commitment, patient safety and psychological safety | 252 respondents: nurses (87%), allied health professionals (7%) and healthcare support personnel (6%) | Large metropolitan acute care hospital | Quality improvement and patient centred climate | Survey |
| Churchman and Doherty (2010) | Explore the extent to which nurses are willing to challenge doctors’ practice | 12 nurses | Acute NHS hospital in England | Supportive organization Status and hierarchy | Interviews |
| Adelman (2012) | Understanding CEO behaviours and actions that promote employee voice and upward communication in healthcare organizations | In each hospital, interviews took place with: the CEO, the Baldridge lead, a director and supervisor of a clinical service area and a frontline nurse | Four healthcare organizations who had received a performance award in the past 7 years | Leader: visibility, approachability, focus on continuous improvement, communication strategies | Document review and semi-structured interviews |
| Garon (2012) | Explore nurses’ perceptions of their own ability to speak up and be heard in the workplace | Staff registered nurses and managers | Magnet and non-magnet hospitals in California, USA | Experience and education organizational administration | Focus groups |
| Hirak (2012) | Investigate relationship between leader inclusiveness and psychological safety | 55 work unit leaders and a total of 224 unit members | Clinical units in a large hospital in Israel | Leader inclusiveness | Survey |
| Leroy (2012) | Explore how behavioural integrity for safety helps followers speak up | 54 nursing departments. An average of 11 nurses per department | Four Belgian hospitals | Leader behavioural integrity | Survey |
| Lyndon (2012) | Explore factors effecting whether clinicians to speak up about safety concerns | 125 obstetricians and registered nurses | Two moderately sized US labour and delivery units | Professional responsibility | Survey |
| Sayre (2012) | Evaluate intervention to develop speaking up behaviours among nurses | 58 (53 post-test) registered nurses in the intervention 87 (51 at post-test) in control group | Two acute care hospitals | Familiarity with leader | Survey list of individual nurse behaviours |
| Raes (2013) | Investigates when and how team engage in team learning behaviours | 28 divisional nursing teams | University hospital in Belgium | Transformational and laissez-faire leadership | Questionnaire |
| Ortega (2014) | Examine role of change-oriented leadership in learning process | 107 nursing teams ( = 689) from different hospital areas | 37 public hospitals in Spain | Change-oriented leadership | Survey |
| Schwappach and Gehring (2014) | Explore factors influencing voice or silence in oncology staff | 32 doctors and nurses from 7 oncology units | Six Swedish hospitals (seven oncology departments) | Professional responsibility Hierarchy/status | Interviews |
| Sundqvist and Carlsson (2014) | Describe advocacy in anaesthesia care during the perioperative phase | 112 registered nurse anaesthetists | Two hospitals in Sweden | Professional responsibility Experience | Interviews |
| Yanchus (2014) | Explore perceptions of communication in psychologically safe and unsafe environments | Clinical providers | USA veterans’ Health Administration | Communication Hierarchy/status Speaking up culture | Interviews and survey |
| Law and Chan (2015) | To explore the process of learning to speak up | Newly graduated registered nurses | Public hospital in Hong Kong | Speaking up training Mentoring Safety culture | Interviews Email conversation |
| Aydon (2016) | Identify factors influencing nurse’s decisions to question medication administration | 103 nurses | Neonatal care units in two public hospitals in Western Australia | Organizational support Professional responsibility Knowledge | Interviews |
| Jain (2016) | Examine psychological safety through a patient case study | Single case study and discussion | Cancer care teams | Hierarchy/status Familiarity Boundary spanning Inclusive leadership | Case study |
| O’Leary (2016) | Examine effective communication, shared decision-making and knowledge sharing | Teams of care providers ( = 24) and one client | Two private facilities for older people in Ireland | Leadership behaviour | Field notes Interviews Group discussion |
| Reese (2016) | Understand barriers facilitating factors of assertion communication | 6 focus group with 36 nurses, residents and attending physicians | 373 beds in academic children’s hospital | Hierarchy Familiarity | Focus group |
| Etchegaray (2017) | Examine association between willingness to speak up and perception teamwork and safety organizational cultures | Healthcare professionals with direct patient care responsibility | Large healthcare system in the USA | Leadership and cultural enablers | Survey: qualitative and quantitative |
| Martinez (2017) | Compare factors related to interns’ and residents’ speaking up about traditional versus professionalism safety threats | 1800 medical and surgical interns and residents (47% responded) | Across 6 US academic medical centres | Professional responsibility Leadership behaviour Peer support | Survey |
| Munn (2016) | Examine effect of safety climate, leader inclusiveness and psychological safety on nurses’ error reporting | Nurses ( = 814) Nurse manager ( = 43) | Large academic medical centre in the USA | Leadership Safety climate | Self-administrated surveys |
| Ng (2017) | Explore perceptions of communication openness communication issues and speaking up | 80 ICU staff members | Large public hospital in Hong Kong | Familiarity Hierarchy/status | Questionnaire and interviews |
| Weiss (2017) | Test the effects of inclusive leader language on voice | 40 anaesthesia nurses, 16 recovery room nurses, 52 resident anaesthesiologists and 18 attending anaesthesiologists ( = 126) | Hospital setting | Leader inclusiveness | Participants completed simulation exercise and questionnaire Behavioural coding and leader language analyses |
| Farh & Chen (2018) | Assess effect of leader behaviours and familiarity on voice | 118 surgical team performance episodes (or cases) randomly sampled | Five hospitals within a large hospital system | Coaching leadership Familiarity | Observer ratings Survey data |
| Omura (2018) | Explore nurses’ perceptions of assertive communication and identify facilitating or impeding factors | 23 Japanese registered nurses | Workplace or university in Japan | Supportive environment Positive relationships Effective role models Experience and knowledge Professional responsibility | Interviews |
| Albritton (2019) | Explore effectiveness of new quality improvement (QI) teams | 122 hospital-based QI teams | Hospitals in Ghana | Team leadership | Survey observer-rated measures |
| Alingh (2019) | Explore relationships between control-based and commitment-based safety management, safety climate, psychological safety and speaking up | 302 nurse managers and 2627 nurses from 334 clinical wards in Dutch hospitals | 84 Dutch hospitals | Leadership behaviour: commitment-based management | Survey |
| Author . | Aims . | Participants . | Setting . | Enablers identified . | Methods of Evaluation . |
|---|---|---|---|---|---|
| Edmondson (2003) | Explore the impact of leader behaviours on speaking up within teams | 16 operating room teams | Hospital | Boundary spanning coaching leadership | Interviews: qualitative and quantitative data |
| Atwal and Caldwell (2005) | Record interactions of the team members using the Bales’ interaction process analysis | Healthcare professionals in two older persons multidisciplinary team meetings | Large acute NHS Trust | Hierarchy/status | Observations of meetings |
| Maxfield (2005) | Exploring concerns about communication that may contribute to avoidable errors and other problems in healthcare | 1700 nurses, physicians, clinical care and administrative staff | Urban, suburban and rural hospitals in the USA | Culture of safety | Focus groups, interviews, workplace observations and survey |
| Nembhard and Edmondson (2006) | Examine the relationship between status and psychological safety | 1440 healthcare professionals (physicians, nurses, respiratory therapists, social workers, dieticians) | 23 neonatal intensive care units in the USA and Canada | Status Leader inclusiveness | Survey |
| Attree (2007) | Explore factors influencing nurses’ decisions to raise concerns | 142 nurses | Acute National Health Service (NHS) Trust in England | Professional responsibility Positive leadership | Survey |
| Dufresne (2007) | Explore the relationship between debriefing leaders, psychological safety and learning behaviours after critical incidents | 40 teams (227 resident anaesthesiologists) | Center for Medical Simulation in Cambridge | Positive leadership behaviours | Videotaped team debriefing |
| Halbesleben and Rathert (2008) | Examine continuous quality improvement and psychological safety in workarounds | 83 cancer registrars | Acute care hospitals in the USA | Continuous improvement | Survey |
| Tangirala and Ramanujam (2008) | Examine the cross-level effects of procedural justice climate on silence | 606 frontline hospital nurses from 30 workgroups | A large Midwestern hospital | Personal control | Survey |
| Carmeli and Zisu (2009) | Examine a three-pronged model of organizational trust, perceived organizational support and psychological safety | Employees who work in medical clinics and provide daily medical services | Large healthcare organization in Israel | Perceived organizational support | Survey |
| Rathert (2009) | Explore model linking the work environment to work engagement, organizational commitment, patient safety and psychological safety | 252 respondents: nurses (87%), allied health professionals (7%) and healthcare support personnel (6%) | Large metropolitan acute care hospital | Quality improvement and patient centred climate | Survey |
| Churchman and Doherty (2010) | Explore the extent to which nurses are willing to challenge doctors’ practice | 12 nurses | Acute NHS hospital in England | Supportive organization Status and hierarchy | Interviews |
| Adelman (2012) | Understanding CEO behaviours and actions that promote employee voice and upward communication in healthcare organizations | In each hospital, interviews took place with: the CEO, the Baldridge lead, a director and supervisor of a clinical service area and a frontline nurse | Four healthcare organizations who had received a performance award in the past 7 years | Leader: visibility, approachability, focus on continuous improvement, communication strategies | Document review and semi-structured interviews |
| Garon (2012) | Explore nurses’ perceptions of their own ability to speak up and be heard in the workplace | Staff registered nurses and managers | Magnet and non-magnet hospitals in California, USA | Experience and education organizational administration | Focus groups |
| Hirak (2012) | Investigate relationship between leader inclusiveness and psychological safety | 55 work unit leaders and a total of 224 unit members | Clinical units in a large hospital in Israel | Leader inclusiveness | Survey |
| Leroy (2012) | Explore how behavioural integrity for safety helps followers speak up | 54 nursing departments. An average of 11 nurses per department | Four Belgian hospitals | Leader behavioural integrity | Survey |
| Lyndon (2012) | Explore factors effecting whether clinicians to speak up about safety concerns | 125 obstetricians and registered nurses | Two moderately sized US labour and delivery units | Professional responsibility | Survey |
| Sayre (2012) | Evaluate intervention to develop speaking up behaviours among nurses | 58 (53 post-test) registered nurses in the intervention 87 (51 at post-test) in control group | Two acute care hospitals | Familiarity with leader | Survey list of individual nurse behaviours |
| Raes (2013) | Investigates when and how team engage in team learning behaviours | 28 divisional nursing teams | University hospital in Belgium | Transformational and laissez-faire leadership | Questionnaire |
| Ortega (2014) | Examine role of change-oriented leadership in learning process | 107 nursing teams ( = 689) from different hospital areas | 37 public hospitals in Spain | Change-oriented leadership | Survey |
| Schwappach and Gehring (2014) | Explore factors influencing voice or silence in oncology staff | 32 doctors and nurses from 7 oncology units | Six Swedish hospitals (seven oncology departments) | Professional responsibility Hierarchy/status | Interviews |
| Sundqvist and Carlsson (2014) | Describe advocacy in anaesthesia care during the perioperative phase | 112 registered nurse anaesthetists | Two hospitals in Sweden | Professional responsibility Experience | Interviews |
| Yanchus (2014) | Explore perceptions of communication in psychologically safe and unsafe environments | Clinical providers | USA veterans’ Health Administration | Communication Hierarchy/status Speaking up culture | Interviews and survey |
| Law and Chan (2015) | To explore the process of learning to speak up | Newly graduated registered nurses | Public hospital in Hong Kong | Speaking up training Mentoring Safety culture | Interviews Email conversation |
| Aydon (2016) | Identify factors influencing nurse’s decisions to question medication administration | 103 nurses | Neonatal care units in two public hospitals in Western Australia | Organizational support Professional responsibility Knowledge | Interviews |
| Jain (2016) | Examine psychological safety through a patient case study | Single case study and discussion | Cancer care teams | Hierarchy/status Familiarity Boundary spanning Inclusive leadership | Case study |
| O’Leary (2016) | Examine effective communication, shared decision-making and knowledge sharing | Teams of care providers ( = 24) and one client | Two private facilities for older people in Ireland | Leadership behaviour | Field notes Interviews Group discussion |
| Reese (2016) | Understand barriers facilitating factors of assertion communication | 6 focus group with 36 nurses, residents and attending physicians | 373 beds in academic children’s hospital | Hierarchy Familiarity | Focus group |
| Etchegaray (2017) | Examine association between willingness to speak up and perception teamwork and safety organizational cultures | Healthcare professionals with direct patient care responsibility | Large healthcare system in the USA | Leadership and cultural enablers | Survey: qualitative and quantitative |
| Martinez (2017) | Compare factors related to interns’ and residents’ speaking up about traditional versus professionalism safety threats | 1800 medical and surgical interns and residents (47% responded) | Across 6 US academic medical centres | Professional responsibility Leadership behaviour Peer support | Survey |
| Munn (2016) | Examine effect of safety climate, leader inclusiveness and psychological safety on nurses’ error reporting | Nurses ( = 814) Nurse manager ( = 43) | Large academic medical centre in the USA | Leadership Safety climate | Self-administrated surveys |
| Ng (2017) | Explore perceptions of communication openness communication issues and speaking up | 80 ICU staff members | Large public hospital in Hong Kong | Familiarity Hierarchy/status | Questionnaire and interviews |
| Weiss (2017) | Test the effects of inclusive leader language on voice | 40 anaesthesia nurses, 16 recovery room nurses, 52 resident anaesthesiologists and 18 attending anaesthesiologists ( = 126) | Hospital setting | Leader inclusiveness | Participants completed simulation exercise and questionnaire Behavioural coding and leader language analyses |
| Farh & Chen (2018) | Assess effect of leader behaviours and familiarity on voice | 118 surgical team performance episodes (or cases) randomly sampled | Five hospitals within a large hospital system | Coaching leadership Familiarity | Observer ratings Survey data |
| Omura (2018) | Explore nurses’ perceptions of assertive communication and identify facilitating or impeding factors | 23 Japanese registered nurses | Workplace or university in Japan | Supportive environment Positive relationships Effective role models Experience and knowledge Professional responsibility | Interviews |
| Albritton (2019) | Explore effectiveness of new quality improvement (QI) teams | 122 hospital-based QI teams | Hospitals in Ghana | Team leadership | Survey observer-rated measures |
| Alingh (2019) | Explore relationships between control-based and commitment-based safety management, safety climate, psychological safety and speaking up | 302 nurse managers and 2627 nurses from 334 clinical wards in Dutch hospitals | 84 Dutch hospitals | Leadership behaviour: commitment-based management | Survey |
Enablers identified across levels of healthcare organizations
| Organizational . | Team . | Individual . |
|---|---|---|
| Safety culture | Leader behavioural integrity | Professional responsibility |
| Continuous improvement culture | Status, hierarchy and inclusiveness | Individual differences |
| Organizational support | Change-oriented leadership | |
| Familiarity across teams | Leader support | |
| Peer support | ||
| Familiarity leader | ||
| Familiarity team members |
| Organizational . | Team . | Individual . |
|---|---|---|
| Safety culture | Leader behavioural integrity | Professional responsibility |
| Continuous improvement culture | Status, hierarchy and inclusiveness | Individual differences |
| Organizational support | Change-oriented leadership | |
| Familiarity across teams | Leader support | |
| Peer support | ||
| Familiarity leader | ||
| Familiarity team members |
Improvement or learning orientation
Four studies highlighted the positive impact of a learning orientation on psychological safety.
A culture of continuous improvement . Care providers who reported greater continuous quality improvement environments also reported greater psychological safety [ 2 ]. Halbesleben and Rathert [ 19 ] found that psychological safety mediated the relationship between a climate for continuous quality improvement and staff engaging in experimentation and suggesting improvements to work processes.
Change-orientated leadership . Leaders play an important role in encouraging continuous quality improvement and psychological safety [ 19 , 32 ]. Change-oriented leaders enable psychological safety by encouraging innovative thinking, envisioning change, taking personal risks and facilitating open discussion of errors and solutions [ 19 ].
Seventeen studies explored the role of support in creating psychological safety.
Organizational support . Supportive healthcare environments have an open and respectful culture; raising concerns is a professional duty that is received positively and supported by administration and policies [ 10 , 27 , 28 , 33 ]. This promotes speaking up and assertive communication [ 24 , 27 ]. Healthcare professionals, who believe that their organization values their contribution and cares about their wellbeing, experience a higher level of psychological safety [ 34 ].
Support from leader . Predicted level of support from manager influences nurses’ decisions to raise concerns [ 10 ]. Transformational and commitment-based leaders, who are positive role models and prioritize patient safety, facilitate psychological safety and assertiveness [ 24 , 35 , 36 ]. Laissez-faire leadership encourages psychological safety by giving team members shared authority to make decisions and resolve problems [ 35 ]. However, more directive leadership, such as coaching, also facilitates psychological safety [ 37 , 38 ]. Leaders, who listen and provide feedback, facilitate open communication across healthcare organizations [ 28 , 32 , 39 ]. To foster psychological safety, leaders can use more advocacy statements and less negative evaluative statement [ 40 ] and recognize the impact they have on psychological safety within their team [ 41 ].
Support from peers . In psychologically safe teams, shared co-worker norms and values about speaking up influence team members’ willingness to speak up [ 39 ]. Having positive relationships, effective role models [ 24 ] and higher teamwork climates [ 23 , 26 ] can encourage assertive communication and speaking up for safety. Stronger workgroup identification reduces silence in nursing teams, once the procedural justice climate, the perception of organisational authorities as making fair decisions, was high [ 42 ].
Familiarity with colleagues
Familiarity with colleagues as an enabler of psychological safety was mentioned by six studies.
Familiarity between team members . Familiarity and face-to-face communication between team members facilitates psychological safety [ 43 ]. To leverage the expertise of specialists who work in different areas, geographically dispersed teams are often required in healthcare. This reduces the direct communication needed to develop psychological safety [ 44 ]. Similarly, when new members are constantly joining the team, building and maintaining psychological safety becomes challenging [ 45 ]. Having a stable core team membership facilitates the development of trusting interpersonal relations and team psychological safety [ 45 ].
Familiarity across teams . Due to the complex and interdependent nature of healthcare teams, there is a growing need to communicate and collaborate across different teams. Boundary spanners are members of the team who integrate the work of other teams in order to facilitate communication and information sharing [ 38 ]. Both Edmondson [ 38 ] and Jain et al. [ 44 ] found a positive association between boundary spanning and team psychological safety.
Familiarity with team leaders . Hospital leaders who are visible and present on a regular basis promote employee voice [ 32 ]. This visibility creates familiarity between employees and their leader allowing trusting relationships to develop. Sayre et al. [ 46 ] created more leader visibility in order to improve speaking up behaviours among registered nurses.
Status, hierarchy and inclusiveness
Healthcare professionals find it easier to challenge those who have less experience than them [ 24 , 27 , 29 , 33 , 47 , 31 ]. Those with higher status report higher levels of psychological safety [ 29 , 43 , 44 , 48 ], while those lower in the hierarchy perceive a knowledge gap between themselves and their superiors and are less likely to assert themselves [ 29 , 43 , 48 ].
Inclusive leadership behaviours help to overcome the negative effects of low status on psychological safety by flattening hierarchical differences [ 8 , 16 , 21 , 32 , 23 , 45 , 49 ]. Inclusive leadership is when leaders’ words and deeds invite and appreciate their contributions and feedback from all team members [ 8 ]. In interventions to improve psychological safety, implicit inclusive leader language, such as ‘we’, ‘us’ or ‘our’, improved voice behaviour [ 49 ] and inclusive leadership behaviours helped to develop team psychological safety [ 45 ].
Individual differences . Individual differences can also enable psychological safety in healthcare teams. Three studies found that gender influences psychological safety. Females have a lower rate per minute of asking and giving opinions [ 48 ], while males are more likely to speak up about professionalism safety issues [ 26 ]. Personality also influences healthcare professionals’ likelihood of speaking up. Registered nurses and obstetricians were more inclined to speak up when they had higher bravery and assertiveness scores [ 30 ]. Courage was associated with speaking up among medical and surgical interns and residents [ 26 ]. Similarly, nurses perceive speaking up as a behaviour requiring bravery and courage [ 25 , 29 ].
Tangirala and Ramanujam [ 42 ] found that personal control positively affected the speaking up behaviour of nurses. This relationship was U-shaped meaning that when personal control was either high or low, there were higher levels of voice behaviour. This relationship was moderated by organisational identification, with those who had high levels of personal control and stronger identification having higher use of voice.
This review identified 13 enablers of psychological safety within healthcare contexts. Four were at the organizational level, seven were at the team level and two were at the individual level (see Table 4 ). These findings concur with previous research [ 5 , 6 , 14 , 15 ]. While this review has not identified any novel enablers of psychological safety, it adds value to previous research by adopting a systems lens to identify a comprehensive list of factors at organization, team and individual levels that enable psychological safety within healthcare teams. The review was driven by a desire to shift the focus from understanding the antecedents of psychological safety, to thinking more about how to enable and improve psychological safety in teams. We grouped our findings into five broad categories: priority for patient safety, improvement or learning orientation, support, familiarity with colleagues and status, hierarchy and inclusiveness and individual differences.
The category ‘priority for patient safety’ reflects this reviews’ specific focus on the healthcare environment. There is an important bidirectional relationship between psychological safety and safety culture, while a safety culture improves psychological safety in healthcare teams, psychologically safe healthcare professionals also become more engaged in behaviours that improve safety cultures [ 6 , 8 , 14 ]. Leader’s behavioural integrity for safety promotes psychological safety in healthcare teams, as well as improves overall safety culture within these teams [ 2 , 8 ]. These findings highlight that having a priority for safety can cultivate both a safe environment for patients and high psychological safety among staff.
When healthcare organizations have a climate of continuous improvement, it supports the development of psychological safety and encourages staff to become more engaged in improving team or organizational practices. At the team level, change-oriented leaders play a key role in enabling psychological safety by role modelling innovative thinking, taking interpersonal risks and discussing errors.
Support from organizations, leaders and peers all encourage psychological safety within healthcare settings. This can also be seen outside of the healthcare context [ 5 , 50 ]. Leader visibility can promote familiarity with their team members and is also an opportunity for leaders to role model supportive behaviours which cultivate psychological safety. While the familiarity that results from face-to-face contact and stable team membership facilitates psychological safety, creating these circumstances can be challenging within a complex and rapidly changing healthcare environment [ 3 , 8 , 44 ]. Healthcare teams need to engage in the active process of ‘teaming’, which occurs when diverse employees are brought together as needs demand and are then disbanded once the need has been addressed [ 51 ]. While teaming allows organizations to adapt to chaotic environments, it reduces the time teams have to develop familiarity and psychological safety. It is necessary to develop psychological safety alongside teaming in order for healthcare professionals to adapt to the demands of increasingly complex patient care [ 52 ]. The other enablers of psychological safety identified in this review, such as priority for safety, may be used in order to compensate for any lack of familiarity within and across healthcare teams.
Similar to the aviation industry [ 53 ], team members with high status, and more knowledge and experience, are more likely to feel psychologically safe. When staff are less experienced and have a lower status, inclusive leadership can support them to feel more psychologically safe. Although, psychological safety has been defined as a group level phenomenon [ 1 ], it is influenced by healthcare professionals’ individual differences such as gender, personality traits and individuals’ perceptions of personal control.
Strengths and limitations
This systematic review presents factors which enable psychological safety within healthcare teams. While the enablers identified are not novel, this review takes a systems approach to develop a comprehensive list of practical enablers of psychological safety in the healthcare environment. This list can be applied to the development of more objective measures of psychological safety and interventions targeted at improving psychological safety in healthcare teams. To minimize the risk of publication bias, searches were conducted on academic and grey literature databases as well as through contacting experts.
Practical implications and future research
The list of practical enablers presented in this review aid the future development of objective measures of psychological safety and interventions to improve psychological safety within healthcare teams. Despite the important role played by psychologically safe healthcare teams, a culture of fear still exists [ 11 , 12 , 14 , 38 ]. There is a lack of guidance on how healthcare teams can improve and maintain psychological safety and, therefore, a need to develop and implement interventions to improve psychological safety within these teams [ 13 ]. The enablers of psychological safety presented in this review are a useful starting point for developing the necessary components of these interventions. It is recommended that future research draw on the enablers outlined by this review in order to develop effective interventions to improve psychological safety. Ensuring that future interventions focus on developing a priority for safety may be of particular importance to improving psychological safety in healthcare organizations. By incorporating intervention components that target the development of enablers of psychological safety, future interventions are more likely to be successful.
In order to understand whether an intervention is successful in improving psychological safety, there is a need for objective outcome measures. To date, most studies have relied on self-report survey measures which can be limited by self-report bias and response fatigue [ 5 , 54 ]. Therefore, there is a need for reliable objective measures of psychological safety, such as observational measures, which can offer a more holistic understanding of changes in psychological safety over time [ 5 , 13 ]. Understanding the enablers of psychological safety is necessary in order to develop these observational measures. Future research is needed in order to incorporate enablers of psychological safety into objective measures of psychological safety. By building on this review, future research can identify observable behaviours associated with the enablers of psychological safety in healthcare teams and include them as part of an observational measure of psychological safety.
The current systematic review identifies a list of enablers of psychological safety within healthcare teams. These findings provide a starting point for future research to develop objective measures and interventions to improve psychological safety within healthcare teams.
This work was supported by the Irish Research Council.
Edmondson A . Psychological safety and learning behavior in work teams Amy Edmondson . Adm Sci Q 1999 ; 44 : 350 – 83 .
Google Scholar
Rathert C , Ishqaidef G , May DR . Improving work environments in health care: test of a theoretical framework . Health Care Manag Rev 2009 ; 34 : 334 – 43 .
Kessel M , Kratzer J , Schultz C . Psychological safety, knowledge sharing, and creative performance in healthcare teams . Creat Innov Manag 2012 ; 21 : 147 – 57 .
Lee YSH . Fostering creativity to improve health care quality. Unpublished doctoral dissertation . New Haven, Connecticut : Yale University 2017 .
Google Preview
Newman A , Donohue R , Eva N . Psychological safety: a systematic review of the literature . Hum Resour Manag Rev 2017 ; 27 : 521 – 35 .
Edmondson AC , Lei Z . Psychological safety: the history, renaissance, and future of an interpersonal construct . Annu Rev Organ Psych Organ Behav 2014 ; 1 : 23 – 43 .
Singer S , Edmondson A . Confronting the tension between learning and performance . Refl: Syst Think 2012 ; 11 : 34 – 43 .
Nembhard IM , Edmondson AC . Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams . J Organ Behav 2006 ; 27 : 941 – 66 .
Maxfield D , Grenny J , Lavandero R et al. The Silent Treatment: Why Safety Tools and Checklists Aren’t Enough . Patient Safety & Quality Healthcare , 2011 . Available at: https://faculty.medicine.umich.edu/sites/default/files/resources/silent_treatment.pdf .
Attree M . Factors influencing nurses’ decisions to raise concerns about care quality . J Nurs Manag 2007 ; 15 : 392 – 402 .
Moore L , McAuliffe E . Is inadequate response to whistleblowing perpetuating a culture of silence in hospitals? Clin Govern Int J 2010 ; 15 : 166 – 78 .
Moore L , McAuliffe E . To report or not to report? Why some nurses are reluctant to whistleblow . Clin Govern Int J 2012 ; 17 : 332 – 42 .
O’Donovan R , McAuliffe E . A systematic review exploring the content and outcomes of interventions to improve psychological safety, speaking up and voice behaviour . BMC Health Serv Res 2020 ; 20 : 1 – 11 .
Appelbaum NP , Dow A , Mazmanian PE et al. The effects of power, leadership and psychological safety on resident event reporting . Med Educ 2016 ; 50 : 343 – 50 .
Aranzamendez G , James D , Toms R . Finding antecedents of psychological safety: a step toward quality improvement . Nurs Forum 2015 ; 50 : 171 – 8 .
Hirak R , Peng AC , Carmeli A et al. Linking leader inclusiveness to work unit performance: the importance of psychological safety and learning from failures . Leadersh Q 2012 ; 23 : 107 – 17 .
Leroy H , Dierynck B , Anseel F et al. Behavioral integrity for safety, priority of safety, psychological safety, and patient safety: a team-level study . J Appl Psychol 2012 ; 97 : 1273 – 81 .
Ortega A , Van den Bossche P , Sánchez-Manzanares M et al. The influence of change-oriented leadership and psychological safety on team learning in healthcare teams . J Bus Psychol 2014 ; 29 : 311 – 21 .
Halbesleben JR , Rathert C . The role of continuous quality improvement and psychological safety in predicting work-arounds . Health Care Manag Rev 2008 ; 33 : 134 – 44 .
Popay J , Roberts H , Sowden A et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme, Version 1 , 2006 , b92 .
Munn LT . Team dynamics and learning behavior in hospitals: a study of error reporting by nurses . Unpublished Doctoral dissertation . Chapel Hill : The University of North Carolina 2016 .
Maxfield D . Silence Kills: The Seven Crucial Conversations for Healthcare . Provo, UT : VitalSmarts , 2005 .
Etchegaray JM , Ottosen MJ , Dancsak T et al. Barriers to speaking up about patient safety concerns . J Patient Saf 2017 , doi: 10.1097/PTS.0000000000000334 .
Omura M , Stone TE , Maguire J et al. Exploring Japanese nurses' perceptions of the relevance and use of assertive communication in healthcare: a qualitative study informed by the theory of planned behaviour . Nurse Educ Today 2018 ; 67 : 100 – 7 .
Law BYS , Chan EA . The experience of learning to speak up: a narrative inquiry on newly graduated registered nurses . J Clin Nurs 2015 ; 24 : 1837 – 48 .
Martinez W , Etchegaray JM , Thomas EJ et al. Speaking up about patient safety concerns and unprofessional behaviour among residents: validation of two scales . BMJ Qual Saf 2015 ; 24 : 671 – 80 .
Aydon L , Hauck Y , Zimmer M et al. Factors influencing a nurse's decision to question medication administration in a neonatal clinical care unit . J Clin Nurs 2016 ; 25 : 2468 – 77 .
Garon M . Speaking up, being heard: registered nurses’ perceptions of workplace communication . J Nurs Manag 2012 ; 20 : 361 – 71 .
Schwappach DL , Gehring K . Trade-offs between voice and silence: a qualitative exploration of oncology staff’s decisions to speak up about safety concerns . BMC Health Serv Res 2014 ; 14 : 303 .
Lyndon A , Sexton JB , Simpson KR et al. Predictors of likelihood of speaking up about safety concerns in labour and delivery . BMJ Qual Saf 2012 ; 21 : 791 – 9 .
Sundqvist AS , Carlsson AA . Holding the patient's life in my hands: Swedish registered nurse anaesthetists' perspective of advocacy . Scand J Caring Sci 2014 ; 28 : 281 – 8 .
Adelman K . Promoting employee voice and upward communication in healthcare: the CEO’s influence . J Healthc Manag 2012 ; 57 : 133 – 48 .
Churchman JJ , Doherty C . Nurses’ views on challenging doctors’ practice in an acute hospital . Nurs Stand 2010 ; 24 : 42 – 8 .
Carmeli A , Zisu M . The relational underpinnings of quality internal auditing in medical clinics in Israel . Soc Sci Med 2009 ; 68 : 894 – 902 .
Raes E , Decuyper S , Lismont B et al. Facilitating team learning through transformational leadership . Instr Sci 2013 ; 41 : 287 – 305 .
Alingh CW , van Wijngaarden JD , van de Voorde K et al. Speaking up about patient safety concerns: the influence of safety management approaches and climate on nurses’ willingness to speak up . BMJ Qual Saf 2019 ; 28 : 39 – 48 .
Farh CI , Chen G . Leadership and member voice in action teams: test of a dynamic phase model . J Appl Psychol 2018 ; 103 : 97 – 110 .
Edmondson AC , Woolley AW . Understanding outcomes of organizational learning interventions. In: International Handbook of Organizational Learning and Knowledge Management . London : Blackwell , 2003 , 185 – 211 .
Yanchus NJ , Derickson R , Moore SC et al. Communication and psychological safety in veterans health administration work environments . J Health Organ Manag 2014 ; 28 : 754 – 76 .
Dufresne RL . Learning from critical incidents by ad hoc teams: The impacts of team debriefing leader behaviors and psychological safety . Dissertations and Theses . Boston College 2007 .
Albritton JA , Fried B , Singh K et al. The role of psychological safety and learning behavior in the development of effective quality improvement teams in Ghana: an observational study . BMC Health Serv Res 2019 ; 19 : 385 .
Tangirala S , Ramanujam R . Exploring nonlinearity in employee voice: the effects of personal control and organizational identification . Acad Manag J 2008 ; 51 : 1189 – 203 .
Reese J , Simmons R , Barnard J . Assertion practices and beliefs among nurses and physicians on an inpatient pediatric medical unit . Hosp Pediatr 2016 ; 6 : 275 – 81 .
Jain AK , Fennell ML , Chagpar AB et al. Moving toward improved teamwork in cancer care: the role of psychological safety in team communication . J Oncol Pract 2016 ; 12 : 1000 – 11 .
O’Leary DF . Exploring the importance of team psychological safety in the development of two interprofessional teams . J Interprof Care 2016 ; 30 : 29 – 34 .
Sayre MM , McNeese-Smith D , Leach LS et al. An educational intervention to increase “speaking-up” behaviors in nurses and improve patient safety . J Nurs Care Qual 2012 ; 27 : 154 – 60 .
Ng GWY , Pun JKH , So EHK et al. Speak-up culture in an intensive care unit in Hong Kong: a cross-sectional survey exploring the communication openness perceptions of Chinese doctors and nurses . BMJ Open 2017 ; 7 : e015721 .
Atwal A , Caldwell K . Do all health and social care professionals interact equally: a study of interactions in multidisciplinary teams in the United Kingdom . Scand J Caring Sci 2005 ; 19 : 268 – 73 .
Weiss M , Kolbe M , Grote G et al. We can do it! Inclusive leader language promotes voice behavior in multi-professional teams . Leadersh Q 2018 ; 29 : 389 – 402 .
May DR , Gilson RL , Harter LM . The psychological conditions of meaningfulness, safety and availability and the engagement of the human spirit at work . J Occup Organ Psychol 2004 ; 77 : 11 – 37 .
Edmondson AC . Teaming: How Organizations Learn, Innovate, and Compete in the Knowledge Economy . San Francisco : John Wiley & Sons , 2012 .
Nawaz H , Edmondson AC , Tzeng TH et al. Teaming: an approach to the growing complexities in health care AOA critical issues . J Bone Joint Surg 2014 ; 96 : 1 – 7 .
Bienefeld N , Grote G . Speaking up in ad hoc multiteam systems: individual-level effects of psychological safety, status, and leadership within and across teams . Eur J Work Organ Psy 2014 ; 23 : 930 – 45 .
Donaldson SI , Grant-Vallone EJ . Understanding self-report bias in organizational behavior research . J Bus Psychol 2002 ; 17 : 245 – 60 .
- patient care team
- patient safety
- health care safety
| Month: | Total Views: |
|---|---|
| March 2020 | 3 |
| April 2020 | 116 |
| May 2020 | 59 |
| June 2020 | 197 |
| July 2020 | 168 |
| August 2020 | 195 |
| September 2020 | 830 |
| October 2020 | 199 |
| November 2020 | 89 |
| December 2020 | 78 |
| January 2021 | 171 |
| February 2021 | 328 |
| March 2021 | 394 |
| April 2021 | 506 |
| May 2021 | 358 |
| June 2021 | 389 |
| July 2021 | 268 |
| August 2021 | 170 |
| September 2021 | 156 |
| October 2021 | 365 |
| November 2021 | 584 |
| December 2021 | 496 |
| January 2022 | 604 |
| February 2022 | 601 |
| March 2022 | 659 |
| April 2022 | 658 |
| May 2022 | 651 |
| June 2022 | 637 |
| July 2022 | 519 |
| August 2022 | 651 |
| September 2022 | 671 |
| October 2022 | 850 |
| November 2022 | 823 |
| December 2022 | 754 |
| January 2023 | 805 |
| February 2023 | 912 |
| March 2023 | 1,262 |
| April 2023 | 1,026 |
| May 2023 | 900 |
| June 2023 | 700 |
| July 2023 | 983 |
| August 2023 | 774 |
| September 2023 | 909 |
| October 2023 | 1,258 |
| November 2023 | 1,026 |
| December 2023 | 836 |
| January 2024 | 1,125 |
| February 2024 | 1,273 |
| March 2024 | 1,341 |
| April 2024 | 1,385 |
| May 2024 | 1,456 |
| June 2024 | 1,096 |
| July 2024 | 1,252 |
| August 2024 | 896 |
| September 2024 | 938 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1464-3677
- Print ISSN 1353-4505
- Copyright © 2024 International Society for Quality in Health Care and Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- A-Z Publications
Annual Review of Organizational Psychology and Organizational Behavior
Volume 1, 2014, review article, psychological safety: the history, renaissance, and future of an interpersonal construct.
- Amy C. Edmondson 1 , and Zhike Lei 2
- View Affiliations Hide Affiliations Affiliations: 1 Harvard Business School, Boston, Massachusetts 02163; email: [email protected] 2 European School of Management and Technology (ESMT), 10178 Berlin, Germany
- Vol. 1:23-43 (Volume publication date March 2014) https://doi.org/10.1146/annurev-orgpsych-031413-091305
- First published as a Review in Advance on January 10, 2014
- © Annual Reviews
Psychological safety describes people’s perceptions of the consequences of taking interpersonal risks in a particular context such as a workplace. First explored by pioneering organizational scholars in the 1960s, psychological safety experienced a renaissance starting in the 1990s and continuing to the present. Organizational research has identified psychological safety as a critical factor in understanding phenomena such as voice, teamwork, team learning, and organizational learning. A growing body of conceptual and empirical work has focused on understanding the nature of psychological safety, identifying factors that contribute to it, and examining its implications for individuals, teams, and organizations. In this article, we review and integrate this literature and suggest directions for future research. We first briefly review the early history of psychological safety research and then examine contemporary research at the individual, group, and organizational levels of analysis. We assess what has been learned and discuss suggestions for future theoretical development and methodological approaches for organizational behavior research on this important interpersonal construct.
Article metrics loading...
Full text loading...
Data & Media loading...
- Article Type: Review Article
Most Read This Month
Most cited most cited rss feed, conservation of resources in the organizational context: the reality of resources and their consequences, self-determination theory in work organizations: the state of a science, burnout and work engagement: the jd–r approach, employee voice and silence, psychological capital: an evidence-based positive approach, how technology is changing work and organizations, research on workplace creativity: a review and redirection, abusive supervision, alternative work arrangements: two images of the new world of work.
Publication Date: 21 Mar 2014
Online Option
Sign in to access your institutional or personal subscription or get immediate access to your online copy - available in PDF and ePub formats
Psychological Safety Comes of Age: Observed Themes in an Established Literature
Annual Review of Organizational Psychology & Organizational Behavior, Vol. 10, Issue 1, pp. 55-78, 2023
Posted: 2 Feb 2023
Amy C. Edmondson
Harvard University
Derrick P. Bransby
Date Written: January 2023
Since its renaissance in the 1990s, psychological safety research has flourished—a boom motivated by recognition of the challenge of navigating uncertainty and change. Today, its theoretical and practical significance is amplified by the increasingly complex and interdependent nature of the work in organizations. Conceptual and empirical research on psychological safety—a state of reduced interpersonal risk—is thus timely, relevant, and extensive. In this article, we review contemporary psychological safety research by describing its various content areas, assessing what has been learned in recent years, and suggesting directions for future research. We identify four dominant themes relating to psychological safety: getting things done, learning behaviors, improving the work experience, and leadership. Overall, psychological safety plays important roles in enabling organizations to learn and perform in dynamic environments, becoming particularly relevant in a world altered by a global pandemic.
Suggested Citation: Suggested Citation
Amy C. Edmondson (Contact Author)
Harvard university ( email ), do you have a job opening that you would like to promote on ssrn, paper statistics, related ejournals, annual review of organizational psychology & organizational behavior.
Subscribe to this free journal for more curated articles on this topic
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
A systematic review of factors that enable psychological safety in healthcare teams
Affiliation.
- 1 School of Nursing, Midwifery & Health Systems, Health Sciences Centre, University College Dublin, Dublin 4, Ireland.
- PMID: 32232323
- DOI: 10.1093/intqhc/mzaa025
Purpose: The current systematic review will identify enablers of psychological safety within the literature in order to produce a comprehensive list of factors that enable psychological safety specific to healthcare teams.
Data sources: A keyword search strategy was developed and used to search the following electronic databases PsycINFO, ABI/INFORM, Academic search complete and PubMed and grey literature databases OpenGrey, OCLC WorldCAT and Espace.
Study selection: Peer-reviewed studies relevant to enablers of psychological safety in healthcare setting that were published between 1999 and 2019 were eligible for inclusion. Covidence, an online specialized systematic review website, was used to screen records. Data extraction, quality appraisal and narrative synthesis were conducted on identified papers.
Data extraction: Thirty-six relevant studies were identified for full review and data extraction. A data extraction template was developed and included sections for the study methodology and the specific enablers identified within each study.
Results of data synthesis: Identified studies were reviewed using a narrative synthesis. Within the 36 articles reviewed, 13 enablers from across organizational, team and individual levels were identified. These enablers were grouped according to five broader themes: priority for patient safety, improvement or learning orientation, support, familiarity with colleagues, status, hierarchy and inclusiveness and individual differences.
Conclusion: This systematic review of psychological safety literature identifies a list of enablers of psychological safety within healthcare teams. This list can be used as a first step in developing observational measures and interventions to improve psychological safety in healthcare teams.
Keywords: Enablers; Healthcare teams; Psychological safety.
© The Author(s) 2020. Published by Oxford University Press in association with the International Society for Quality in Health Care. All rights reserved. For permissions, please e-mail: [email protected].
PubMed Disclaimer
Similar articles
- A systematic review exploring the content and outcomes of interventions to improve psychological safety, speaking up and voice behaviour. O'Donovan R, McAuliffe E. O'Donovan R, et al. BMC Health Serv Res. 2020 Feb 10;20(1):101. doi: 10.1186/s12913-020-4931-2. BMC Health Serv Res. 2020. PMID: 32041595 Free PMC article.
- Health professionals' experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. Eddy K, Jordan Z, Stephenson M. Eddy K, et al. JBI Database System Rev Implement Rep. 2016 Apr;14(4):96-137. doi: 10.11124/JBISRIR-2016-1843. JBI Database System Rev Implement Rep. 2016. PMID: 27532314 Review.
- The measurement of collaboration within healthcare settings: a systematic review of measurement properties of instruments. Walters SJ, Stern C, Robertson-Malt S. Walters SJ, et al. JBI Database System Rev Implement Rep. 2016 Apr;14(4):138-97. doi: 10.11124/JBISRIR-2016-2159. JBI Database System Rev Implement Rep. 2016. PMID: 27532315 Review.
- Measuring psychological safety in healthcare teams: developing an observational measure to complement survey methods. O'Donovan R, Van Dun D, McAuliffe E. O'Donovan R, et al. BMC Med Res Methodol. 2020 Jul 29;20(1):203. doi: 10.1186/s12874-020-01066-z. BMC Med Res Methodol. 2020. PMID: 32727374 Free PMC article.
- Team interventions in acute hospital contexts: a systematic search of the literature using realist synthesis. Cunningham U, Ward ME, De Brún A, McAuliffe E. Cunningham U, et al. BMC Health Serv Res. 2018 Jul 11;18(1):536. doi: 10.1186/s12913-018-3331-3. BMC Health Serv Res. 2018. PMID: 29996820 Free PMC article. Review.
- Motivation for patient engagement in patient safety: a multi-perspective, explorative survey. Raab C, Gambashidze N, Brust L, Weigl M, Koch A. Raab C, et al. BMC Health Serv Res. 2024 Sep 11;24(1):1052. doi: 10.1186/s12913-024-11495-x. BMC Health Serv Res. 2024. PMID: 39261814 Free PMC article.
- Medical Professionals' Responses to a Patient Safety Incident in Healthcare. Kupkovicova L, Skoumalova I, Madarasova Geckova A, Dankulincova Veselska Z. Kupkovicova L, et al. Int J Public Health. 2024 Jul 26;69:1607273. doi: 10.3389/ijph.2024.1607273. eCollection 2024. Int J Public Health. 2024. PMID: 39132384 Free PMC article.
- Psychological safety is associated with better work environment and lower levels of clinician burnout. de Lisser R, Dietrich MS, Spetz J, Ramanujam R, Lauderdale J, Stolldorf DP. de Lisser R, et al. Health Aff Sch. 2024 Jul 17;2(7):qxae091. doi: 10.1093/haschl/qxae091. eCollection 2024 Jul. Health Aff Sch. 2024. PMID: 39081721 Free PMC article.
- Improving departmental psychological safety through a medical school-wide initiative. Porter-Stransky KA, Horneffer-Ginter KJ, Bauler LD, Gibson KM, Haymaker CM, Rothney M. Porter-Stransky KA, et al. BMC Med Educ. 2024 Jul 25;24(1):800. doi: 10.1186/s12909-024-05794-4. BMC Med Educ. 2024. PMID: 39061019 Free PMC article.
- Cultivating a psychological health and safety culture for interprofessional primary care teams through a co-created evidence-informed toolkit. Atanackovic J, Corrente M, Myles S, Eddine Ben-Ahmed H, Urdaneta K, Tello K, Baczkowska M, Bourgeault IL. Atanackovic J, et al. Healthc Manage Forum. 2024 Sep;37(5):334-339. doi: 10.1177/08404704241263918. Epub 2024 Jul 23. Healthc Manage Forum. 2024. PMID: 39042941 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Silverchair Information Systems
- MedlinePlus Health Information
Research Materials
- NCI CPTC Antibody Characterization Program

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Harvard Business School →
- Faculty & Research →
- January 2023
- Annual Review of Organizational Psychology and Organizational Behavior
Psychological Safety Comes of Age: Observed Themes in an Established Literature
- Format: Print
- | Pages: 24
- Find it at Harvard
About The Author
Amy C. Edmondson
More from the authors.
- September 2024
- Faculty Research
Leading Culture Change at SEB
- September–October 2024
- Harvard Business Review
Where Data-Driven Decision-Making Can Go Wrong
- July 11, 2024
- Harvard Business Review Digital Articles
Research: New Hires’ Psychological Safety Erodes Quickly
- Leading Culture Change at SEB By: Amy C. Edmondson and Cat Huang
- Where Data-Driven Decision-Making Can Go Wrong By: Michael Luca and Amy C. Edmondson
- Research: New Hires’ Psychological Safety Erodes Quickly By: Derrick P. Bransby, Michael J. Kerrissey and Amy C. Edmondson
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Download Free PDF
Psychological safety: A systematic review of the literature

2017, Human Resource Management Review
Free related PDFs Related papers
Psychological safety [PS] was introduced in the 90s, and is a term popularized by Harvard Business School professor Amy Edmonson in a study conducted among medical teams in hospitals. PS is an environment of being able to express one’s self without fear of negative consequences such as embarrassment, and ridicule on self image, status or even career (Kahn 1990 as cited in Edmonson 2003). PS enhances sense of self-worth because it overpowers feelings of rejection and negative impacts on self-image whenever self-expression is exercised in the workplace. PS increases morale and self-confidence of members of a team, without having to be personally close to one another. Subsequent researches concluded that greater trust and respect were developed among teams in workplaces of varied settings. This paper is a literature review on various studies and applications of psychological safety. Using literatures published in scholarly journals from 2009 to 2010, the review revealed that many indus...
Academy of Management Discoveries, 2020

BMC Public Health, 2023

Journal of Applied Psychology, 2009

Asia Pacific Journal of Human Resources, 2012

Journal of Occupational and Organizational Psychology, 2010

Safety Science, 2020

Importance: Various psychological concepts have been proposed over time as potential solutions to improving patient safety and quality of care. Psychological safety has been identified as a crucial mechanism of learning and development, and one that can facilitate optimal patient safety in healthcare. Objective: We investigated the quantitative evidence on the relationship between psychological safety and objective patient safety outcomes.Evidence review: We searched 8 databases and conducted manual scoping to identify peer reviewed quantitative studies published up to November 2023. Objective patient safety outcomes of any type were eligible. The findings were analysed descriptively and discussed in a narrative synthesis.Findings: Nine papers were selected for inclusion which reported on heterogeneous patient safety outcomes. Five studies showed a significant relationship between psychological safety and patient safety. The majority of studies reported on the experiences of nurses working in healthcare from the USA. Conclusion: No clear conclusions can be extracted regarding the relationship between psychological safety and patient safety. Patient safety may be contradictory to elements of psychological safety and a more nuanced approach is needed. 2Systematic review registration This systematic review is registered with the International Prospective Register of Systematic Reviews (PROSPERO CRD4202347829)

Work & Stress, 2012

The aim of this article was to investigate the psychosocial risk environment influencing employee behaviour, and subsequently the trust relationship between employer and employee. The unique nature and commonness of negative acts, such as unsafe behaviour, human errors, poor performance and negligence (also referred to as unsafe practices) are explored in this article. Pertinent literatures were reviewed on the nature of negative acts or unsafe behaviour. The findings of this study were used to draw comparisons between unsafe behaviour/misconduct and accidents in the workplace and finally recommendations were made on how the problem can be addressed from a labour relations perspective. The results indicate that a relationship between unsafe practice/misconduct and occupational injuries and accidents exist, owing to system flaws, human error or psychosocial risk.

Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
BMC Health Services Research, 2022

2007 IEEE 8th Human Factors and Power Plants and HPRCT 13th Annual Meeting, 2007

Papeles del Psicologo

The Journal of applied psychology, 2017

Journal of Safety Research, 2003

Journal of Management Sciences

Journal of Safety Research, 2004

International Journal of Applied …, 2008

International Journal of Stress Management, 2010

Scientific Papers Of Silesian University Of Technology – Organization And Management Series – Issue 2023, No 181, 203-216, 2023

Journal of Vocational Behavior, 1998

XIII International Symposium Engineering Management and Competitiveness 2023 (EMC 2023), 2023

Asian Social Science, 2015

Psihologia resurselor umane, 2023

Journal of Applied …, 2011

NICE research journal, 2022

Research in Personnel and Human Resources Management, 2010

WORK ACCIDENTS: WHAT PSYCHOLOGY DOES IN THE FACE OF THIS PROBLEM (Atena Editora), 2022

Journal of Occupational and Organizational Psychology, 2014

HealthcarePapers

International Journal of Stress Management, 2011

Related topics
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Research article
- Open access
- Published: 10 February 2020
A systematic review exploring the content and outcomes of interventions to improve psychological safety, speaking up and voice behaviour
- Róisín O’Donovan ORCID: orcid.org/0000-0003-1993-5319 1 &
- Eilish McAuliffe 1
BMC Health Services Research volume 20 , Article number: 101 ( 2020 ) Cite this article
33k Accesses
74 Citations
50 Altmetric
Metrics details
Having psychologically safe teams can improve learning, creativity and performance within organisations. Within a healthcare context, psychological safety supports patient safety by enabling engagement in quality improvement and encouraging staff to speak up about errors. Despite the low levels of psychological safety in healthcare teams and the important role it plays in supporting patient safety, there is a dearth of research on interventions that can be used to improve psychological safety or its related constructs. This review synthesises the content, theoretical underpinnings and outcomes of interventions which have targeted psychological safety, speaking up, and voice behaviour within a healthcare setting. It aims to identify successful interventions and inform the development of more effective interventions.
A key word search strategy was developed and used to search electronic databases (PsycINFO, ABI/Inform, Academic search complete and PubMed) and grey literature databases (OpenGrey, OCLC WorldCat, Espace). Covidence, an online specialised systematic review website, was used to screen records. Data extraction, quality appraisal and narrative synthesis were conducted on identified papers.
Fourteen interventions were reviewed. These interventions fell into five categories. Educational interventions used simulation, video presentations, case studies and workshops while interventions which did not include an educational component used holistic facilitation, forum play and action research meetings. Mixed results were found for the efficacy or effectiveness of these interventions. While some interventions showed improvement in outcomes related to psychological safety, speaking up and voice, this was not consistently demonstrated across interventions. Included interventions’ ability to demonstrate improvements in these outcomes were limited by a lack of objective outcome measures and the ability of educational interventions alone to change deeply rooted speaking up behaviours.
To improve our understanding of the efficacy or effectiveness of interventions targeting psychological safety, speaking up and voice behaviour, longitudinal and multifaceted interventions are needed. In order to understand whether these interventions are successful, more objective measures should be developed. It is recommended that future research involves end users in the design phase of interventions, target both group and organisational levels, ensure visible leader support and work across and within interdisciplinary teams.
Prospero registration number
CRD42018100659.
Peer Review reports
When teams are psychologically safe, there is a shared belief that members are safe to take interpersonal risks, such as speaking up and engaging in voice behaviour. This definition of psychological safety was proposed by Amy Edmondson [ 1 ] in 1999 and began research on psychological safety as a phenomenon that exists at a group level and is built through workplace interactions. Psychological safety is a key determinant of high-quality communication, trust and decision making which improves team performance and, therefore, plays an important role within workplace teams [ 2 , 3 , 4 ]. Psychological safety plays a particularly vital role in high-risk work contexts, such as healthcare [ 3 ]. When healthcare teams are psychologically safe they are more likely to engage in quality improvement and team learning initiatives [ 5 , 6 ]. This engagement allows healthcare teams to deal with the increased knowledge they need to absorb, the specialisation of healthcare professionals and the resulting interdependence between these professionals [ 5 ]. Therefore, having psychologically safe teams is critical to the delivery of safe and effective care within a complex, dynamic and high stakes work environment. However, a culture of fear and low psychological safety still exists within healthcare organisations [ 7 , 8 , 9 ]. Given the important outcomes associated with psychological safety, there is a need to develop and implement interventions to improve psychological safety within healthcare teams. This article will build on previous reviews of psychological safety literature [ 2 , 3 ] by examining interventions which specifically aimed to improve psychological safety, or its related constructs, speaking up and voice behaviour. It is hoped that the findings of this synthesis will inform the development of future interventions.
Although research to date has illustrated the beneficial outcomes of psychological safety, there is little guidance on how teams can introduce, improve and maintain psychological safety. In their cross-industry comparison study examining psychological safety in both healthcare and educational contexts, Edmondson and colleagues [ 10 ] acknowledge that there is limited research on interventions to promote psychological safety. They argue that psychological safety would be a useful focus for interventions and provide suggestive avenues for research into such interventions. However, given the dearth of interventions targeting psychological safety, this review will take a broader view by including interventions targeting speaking up and voice behaviour, which are closely related to psychological safety.
Speaking up and voice are interpersonally risky behaviours which are facilitated by psychological safety [ 5 , 11 , 12 , 13 ]. Lack of psychological safety has been associated with silence [ 14 ]. Even when employees believe they have something useful to say, lack of psychological safety often leads them to choose silence over voice [ 9 , 15 , 16 , 17 ]. It is necessary to encourage an organisational climate where it is safe to speak up and voice ideas or concerns, as this enables organisational learning and organisational safety [ 9 , 17 , 18 ].
This review aims to identify team building interventions which have focused on psychological safety and its related components, speaking up, voice and silence behaviours. Team development interventions have been broadly defined as intentional actions which attempt to improve or support teams that may be struggling or adequately performing or maximise the capacities of teams ready to advance to a higher level of performance [ 19 ]. These interventions are relevant to this review, because they are suited to targeting psychological safety, speaking up and voice behaviours. They focus on interpersonal relations in order to increase teamwork process and emergent states such as mutual support and communication [ 20 ]. Team development interventions can also focus on problem solving which promotes synergy through encouraging team members to practice setting goals, developing interpersonal relations, clarifying team roles and working to improve organisational characteristics through participating in problem solving tasks. These types of team development interventions have the strongest and most consistent effects on affectively driven states that are critical to teams, such as psychological safety [ 20 ].
This systematic review of the literature will synthesise the content, theoretical underpinnings and outcomes of interventions which have been conducted to date to improve psychological safety and its related components, speaking up and voice behaviour, within a healthcare setting. Both efficacy and effectiveness outcomes will be considered. This review aims to answer the research questions: What interventions have been conducted to improve psychological safety, speaking up and voice behaviour within a healthcare setting? What are the underlying theoretical approaches in these interventions? How have these interventions been evaluated? Which interventions have been most effective for encouraging a climate of psychological safety? This will enable future research to build on what has been done before to create a reliable intervention for improving psychological safety in workplace teams.
A systematic review was used to explore the above research questions. Systematic reviews are an essential tool for synthesising the evidence from available studies to answer a specific research questions [ 21 , 22 , 23 , 24 ]. The Cochrane and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 23 , 24 , 25 ] have been followed in this review.
The protocol for this review has been published on Prospero (registration number: CRD42018100659). Since publishing this protocol, the following changes were made to the reivew:
The terms Speaking Up and Voice Behaviour were added to the title of the review in order to accurately capture the interventions reviewed. Originally, this review intended to examine interventions targeting psychological safety alone. However, given the limited number of interventions targeting psychological safety, the inclusion criteria were widened to include interventions targeting speaking up and voice behaviour.
After conducting the search, a large number of interventions conducted within a healthcare setting were identified. In addition, the literature highlighted the import role played by psychological safety, speaking up and voice in a healthcare setting. Therefore, the inclusion criteria for the setting of the interventions was narrowed from “no defined setting” to “within a healthcare setting”. As well as reflecting the body of literature found by this review, narrowing the setting allowed the review to explore the identified interventions in more detail and to consider their impact within a specific work setting.
The research question “how have these interventions been evaluated?” was added to the final version of this review in order to explore the ways in which each study assessed the impact of the intervention on psychological safety, speaking up and voice.
The inclusion criteria of the final review were updated to reflect the above changes.
Inclusion and exclusion criteria
Studies eligible for inclusion were peer reviewed, from any country, published between 1999 and 2018 and explored the development, implementation and/or evaluation of interventions relevant to psychological safety in healthcare settings. Given the limited number of interventions targeting psychological safety, the inclusion criteria were widened to include interventions targeting speaking up and voice behaviour.
Studies were excluded if they were not available in English or if they reported on interventions conducted outside healthcare settings.
Search strategy
The search strategy used key words identified through a scoping review of the literature. They were grouped together using the OR Boolean term. The resulting search strategy was reviewed by a researcher with extensive systematic review experience. The final search strategy was: “Psychological* safe*” OR “Speak* up” OR voic* OR silen*. The term “intervention” had been included in an earlier iteration but was excluded because it narrowed the search too much. A full search strategy can be found in Additional file 1 .
Information sources
Electronic databases were searched between the 19th of March 2018 and the 8th of June 2018 to find relevant studies (See search strings in online supplementary material). Electronic databases searched were: PsycINFO, ABI/Inform, Academic search complete and PubMed.
A grey literature search was conducted to supplement the above searches. Grey literature was identified by searching electronic databases which had a broad scope and the ability to conduct specific searches [ 26 , 27 ]. The databases searched were; OpenGrey, OCLC WorldCAT, Espace (Curtin’s institutional repository). In addition, the authors hand-searched the reference lists of included studies and contacted experts in the field to identify any eligible studies.
Study screening
Covidence, an online specialised systematic review website, was used to screen records. One reviewer screened titles and abstracts based on the eligibility criteria. When the eligible papers were identified, two reviewers independently reviewed each text. The reviewers met to discuss and resolve any conflicts or disagreements. An option to involve a third reviewer if agreement could not be reached was put in place but proved unnecessary, as following discussion, the original two reviewers reached agreement on all papers for inclusion.
Data extraction process
A data extraction template was developed to capture the relevant information from included studies. This template was based on the third version of guidelines produced by Cochrane in 2014 for data collection for intervention reviews of randomised control trials and non-randomised control trials and recommendations from Hoffmann and colleagues [ 28 ]. Information was collected for: aims, design, theoretical underpinnings, details of the intervention, participant information and outcomes. The final template can be seen in Additional file 2 .
Quality assessment
Depending on the study design, the Critical Appraisal Skills Programme [ 29 ] Qualitative Checklist, Cohort Study Checklist, or the Mixed Methods Appraisal Tool [ 30 ] were used to assess the quality of included studies.
Study synthesis
Given the heterogeneity in interventions and measures used in this review, a narrative approach to synthesis was deemed most appropriate [ 31 ]. Narrative synthesis relies on words and text to ‘tell the story’ of the included studies [ 31 ]. Based on guideline from Popay and colleagues [ 31 ], the narrative synthesis followed three iterative steps: organising studies into logical categories by becoming familiar with them, comparing them to one another and synthesising their findings; analysing the findings within each category by exploring relationships within and between the studies and synthesising data under the relevant themes.
Search result
The database search yielded 8947 studies and 11 grey literature studies were identified. After 5614 duplicates were removed, 3344 were screened. Three thousand one hundred forty-eight studies were excluded based on title and abstract screening, leaving 196 studies for full text screening. One hundred eighty-two full text articles were excluded, leaving 14 studies included in the review.
Figure 1 shows the PRISMA flow chart which summarises the screening stage of this review.
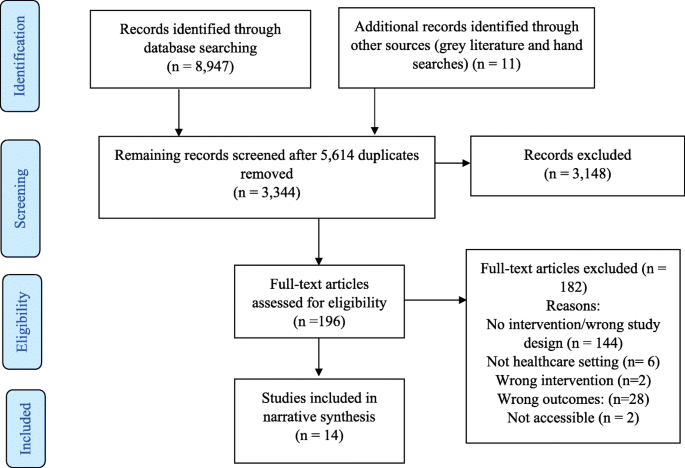
PRISMA flow diagram. This PRISMA flow diagram illustrates the inclusion and exclusion of identified studies
No study was excluded from the review based on quality assessment (see Additional file 3 ).
Included studies
A summary of included studies can be found in Additional file 4 : Tables S1, S2, S3, S4 and S5. They were divided into interventions using education and simulation ( n = 5), interventions using education and leadership videos ( n = 2), interventions using education and case studies ( n = 3), interventions using educational workshops alone ( n = 1) and non-educational interventions ( n = 3). All interventions are synthesised below.
Narrative synthesis
Interventions conducted to improve psychological safety or its related components.
Educational interventions and simulation exercises
Simulation exercises offer opportunities for developing skills without endangering the health of patients through placing them in situations that replicate real clinical practice [ 32 , 33 , 34 ]. The simulation exercises included in five educational interventions presented participants with opportunities to practice speaking up behaviour and were followed by group reflection and debriefing.
Both Pian-Smith and colleagues [ 35 ] and Raemer and colleagues [ 36 ] used simulation-based scenarios to present anaesthesiologists with opportunities to speak up to healthcare professionals (nurses, surgeons and anaesthesiologists). Both conducted educational workshops which introduced participants to tools for speaking-up (see Additional file 4 : Table S1). Pian-Smith and colleagues [ 35 ] found improvements in anaesthesiologists speaking up behaviours, however, Raemer and colleagues [ 36 ] found no statistically significant changes. Given that Pian-Smith and colleagues [ 35 ] explicitly told participants that there would be opportunities to practice speaking up, they had expected their scores to be much higher. Participants in both studies were less likely to speak up to a circulating nurse, suggesting a lack of appreciation of the role of circulating nurses. However, low levels of speaking up were also identified within the anaesthesiologist discipline, with only 25% of participants speaking up to their anaesthesiologist colleague [ 36 ].
Dufresne [ 37 ] simulated a critical incident for anaesthesia teams. They found that the debriefing leaders’ behaviour had a significant impact on the development of psychological safety. Specifically, when leaders balanced advocacy and inquiry language in the first 10 minutes of the debriefing, the team had lower psychological safety. There were also lower levels of psychological safety when the leader used negative evaluative statements. This suggests that, to cultivate psychological safety, leaders should avoid making early evaluative statements about team or individual performance. Further analysis also suggested when leaders showed they were willing to share their own insights, the team felt more psychologically safe. However, this finding did not reach significance.
Ginsburg and Bain [ 38 ] used simulation as part of their multifaceted intervention to promote speaking up behaviour and teamwork in an emergency department (ED). This intervention took place within the context of the hospital’s new Accountability Framework, which holds staff accountable to speak up in the face of unsafe or unprofessional behaviour. Participants were given the opportunity to practice speaking up techniques during role playing simulations and to take part in debriefing sessions, staff huddles and one to one meetings. While there was no significant difference between the ED and Intensive Care Unit (control group) at baseline, the teamwork climate score in the ED was significantly higher post intervention. This score included measures of “speaking up”, but these results were not reported separately.
Thomas and colleagues [ 39 ] used simulation to assess changes in team behaviours following an educational intervention. While the intervention focused on a variety of team behaviours, speaking up and voice inquiry, information sharing, and assertion were most relevant to this review. Participants completed a simulated resuscitation where they could use the behaviours they had been taught. Compared to the control group, the intervention group showed more incidents of inquiry, information sharing and assertion.
Leaders video presentations
Two educational interventions used video presentations to communicate leaders support for speaking up. O’Connor et al. [ 40 ] presented videos of attending physicians discussing situations they faced as interns where their communication and assertiveness skills were challenged. While their intervention had no significant effect on interns’ attitudes towards speaking up about stress or to seniors, the post-training group had significantly more positive attitudes towards speaking up to seniors than the pre-training group. Participants’ speaking behaviour was measured using standardised patient exercises, which showed no significant improvement.
Sayre and colleagues [ 41 ] used videos of senior staff expressing their expectation and support for nurses to speak up to remove any implicit sanctions against nurses speaking up. After the videos, participants discussed barriers to speaking up and developed action plans. The intervention group showed a significant improvement in speaking up survey scores and individual lists of nurse behaviours (see Additional file 4 : Table S2). There was no difference found in the control group.
Video presentations and case studies
Johnson & Kimsey [ 42 ] used video presentations of scenarios where there was a risk or an error to spark discussion. Like Pian-Smith [ 35 ] and Raemer [ 36 ] they introduced tools for speaking up. After the course, the majority (78%) of participants reported believing that they were better able to question decisions or actions of those in authority and were no longer afraid to ask questions (75%). As an objective measure, they found a marked decrease in the number of near misses or sentinel events requiring root cause analysis post training.
Coyle et al. [ 43 ] used video dramatization of a medical event and case studies of medical events that occurred in the study clinic to improve attitudes and behaviour related to medical event reporting. They also conducted educational conferences (see Additional file 4 : Table S3). According to questionnaires completed post intervention, there was no significant change in participants’ attitude and behaviour towards medical event reporting. However, those who participated in more conferences showed a more positive change in medical event reporting attitudes and behaviour.
Shapiro et al. [ 44 ] used video vignettes to encourage clinicians to discuss professional behaviour and the responsibility of bystanders to speak up. Participants were taught specific strategies for managing conflict and speaking up to colleagues who have behaved unprofessionally (see Additional file 4 : Table S3). Following this intervention, the number of reported concerns regarding professional behaviour increased across 3 years. Participants also reported that they were aware of their personal role in ensuring a culture of professionalism.
Educational workshops
Cave et al. [ 45 ] was the only intervention to educational workshops alone. They introduced the CENTRE tool to teams by providing education on the use of the guidelines. CENTRE is a tool which establishes guidelines to promote psychological safety by focusing on confidentiality, equal airtime and non-judgemental listening (see Additional file 4 : Table S4). While 17 health care group leaders have said that they found using CENTRE helpful, no formal assessment of this tool has been published to date. Further research is needed to test the effectiveness of this tool in promoting psychological safety.

Interventions without educational component
The studies which did not include an educational component all used different interventions and are discussed separately below.
Swahnberg and Wijma [ 46 ] used an intervention based on “forum play” (see Additional file 4 : Table S5) to understand staffs perceptions of Abuse in Health Care (AHC). Findings were particularly relevant to psychological safety as the intervention created an open climate where all staff felt comfortable discussing AHC. Staff shifted from being detached to having an emotional engagement with AHC. They saw acting against or speaking up about AHC as their responsibility and emphasised the critical role played by bystanders.
Brown and McCormack [ 47 ] used holistic facilitation to create psychologically safe spaces where nurses could explore their oppressed behaviours, helping them to discuss differences in opinions more openly within a multidisciplinary team. The facilitation sessions made ward leaders more aware of the role they played in creating a culture of psychological safety in their unit. This enabled the leaders to build trusting partnerships that permitted information and knowledge sharing which could help solve problems.
O’Leary [ 48 ] conducted action research meetings with two newly-formed interprofessional project teams. The supportive leadership style used by the author encouraged psychological safety within team meetings. However, psychological safety developed differently in each team. In the first team, a psychologically safe space developed, allowing them to share power and to co-generate knowledge. In the other team, psychological safety did not fully develop. The differences between the teams in this study were explained by the impact of organisational norms and stability in team membership, with organisational norms of shared decision making and a stable core group of team members supporting the development of psychological safety.
Interventions most effective at improving psychological safety and its related components
The diagram presented in Fig. 2 maps the relationships between the five categories of interventions and outcomes which are relevant to psychological safety.

Map of interventions categories, individual interventions review and relevant outcomes. This diagram maps the intervention categories, the studies grouped within them and the relationship between each intervention and key outcomes
As can be seen in Fig. 2 , mixed results were found for the impact of the interventions on outcomes related to psychological safety, speaking up and voice. Five studies [ 38 , 39 , 41 , 43 , 44 ] reported improved and three studies [ 35 , 40 , 43 ] found mixed results for “questioning, challenging, reporting or speaking up”. One further study [ 36 ] found no significant relationship. Three studies [ 39 , 46 , 47 ] reported improved and one study [ 48 ] found mixed results for “communication and collaboration” following interventions. Five studies [ 38 , 40 , 42 , 44 , 45 ] reported positive evaluations by participants post-interventions. Three studies had “Psychological safety” as an outcome, with one of these reporting mixed results for the impact of the intervention on psychological safety [ 48 ] and the other two reporting improvement [ 37 , 47 ]. Mixed results were found for the impact of one intervention on “power sharing” [ 48 ]. Lastly, one study [ 46 ] showed a positive impact of the intervention on creating an “open climate” and another showed improvement in “trusting relationships” [ 47 ].
This review examined educational and non-educational interventions which targeted psychological safety, speaking up and voice behaviour. The outcomes from these studies were mixed. These mixed results limit our ability to accurately answer the research question: “Which interventions have been most effective for encouraging a climate of psychological safety?”. However, the results of this review highlight areas where further research is needed to improve our understanding of the efficacy or effectiveness of interventions targeting psychological safety, speaking up and voice.
Emerging themes and issues for future research
Limitations of educational interventions.
Educational interventions identified challenges related to changing deeply rooted speaking up behaviours and questioned whether education alone is sufficient [ 35 , 36 ]. Implementation science literature suggests that education alone is insufficient for changing behaviour and that it is necessary to have a context which is receptive to change and appropriate facilitation [ 47 , 49 ]. The limitations associated with educational interventions may explain the mixed outcomes from studies in this review. Some educational studies suggested that there would have been more improvement if interventions had been conducted over a longer period of time [ 38 , 41 ] and O’Leary [ 48 ] highlights how having core team members who are meeting regularly supported the development of psychological safety. These findings suggest that educational interventions may benefit from more regular, longitudinal and multifaceted interventions for improving psychological safety, speaking up and voice.
Measuring outcomes
This review identified issues with outcome measurement. Although the simulated scenarios used were as close as possible to reality, they are limited by participants’ awareness that they are not in a real clinical environment. This perception of scenarios realism may affect participants’ behaviour particularly within a healthcare context, when issues of patient safety arise. However, the results from the simulated scenarios made an important contribution to the evidence in this review by providing behavioural evidence of changes relevant to psychological safety, speaking up and voice. This evidence was missing from studies which used questionnaire and survey measures, which were limited by the potential for self-report bias.
According to Shuffler et al. [ 19 ] team building interventions, such as the ones reviewed here, are often judged subjectively by collecting data on participants perceptions of the interventions value. However, in order to fully understand if interventions are successful, more objective measures are needed. This is particularly true for interventions targeting psychological safety. Only three interventions reviewed here evaluated psychological safety as an outcome. While other interventions may have been effective in improving psychological safety, no measure was taken to verify this. There is a need to develop more objective ways of assessing the effectiveness of interventions targeting psychological safety. For example, the observational scheme developed by Hoenderdos et al. [ 50 ] provides a more objective measure of psychological safety. However, this measure has not yet been adapted for a healthcare context and further validation is needed. Future research should focus on developing more objective measures for assessing changes in psychological safety and its related behaviours in order to fully understand the effects of interventions.
Levels of intervention
Many of the interventions reviewed here were team level interventions, however, O’Leary [ 48 ] demonstrated the impact of factors at the organisational level by showing that it is difficult to develop psychological safety within organisations where shared decision making is not an organisational norm. In order for future research to develop effective interventions, they should target the organisational level, as well as the team level.
Who should participate in the intervention?
Studies in this review highlighted the importance and relevance of psychological safety, speaking up and voice behaviour within interdisciplinary teams [ 35 , 36 , 44 , 47 , 48 ]. This highlights the need for future interventions to address psychological safety, speaking up and voice behaviour across and between all disciplines. Studies also illustrated the need to involve team members in the development of interventions. Effective team building interventions ensure that team members contribute their knowledge of the team’s needs to inform the design of the intervention [ 19 ]. Four interventions in this review engaged with participants as part of the development stage of their intervention to ensure the intervention was grounded in reality of the participants work environment [ 43 , 46 , 47 , 48 ]. However, other studies delivered pre-designed interventions that were not based on the needs of the participants. Adopting a co-design approach, where researchers and end-users collaborate in designing the intervention, can ensure that future interventions are tailored to teams needs. A study protocol published by Ward et al. outlines plans to work with key stakeholders, staff and patient representatives to co-design an intervention to create a culture of medical professionalism in relation to patient safety. Future research should ensure that participants are involved in the development stages on interventions, to ensure that the intervention is grounded in the team’s needs.
Lastly, team leaders play a key role in creating psychologically safe teams and should be involved in interventions [ 1 ]. In line with this, key stakeholders and leaders were involved in many of the studies reviewed here, either as a participant in the study or in facilitating the interventions. Leaders were involved in interventions through their behaviour facilitating psychological safety [ 37 , 48 ] or through showing their support and commitment to the intervention [ 38 , 40 , 41 , 47 ]. Since the search for this systematic review was conducted, a case study intervention focused on understanding voice and improving the response to disruptive behaviours has been published by Dixon-Woods et al. Leaders played a key role within this case study by becoming more open and willing to listen and to take staff concerns on board and by completing training in skills for encouraging voice and having difficult conversations. The interventions reviewed here, along with the recent paper by Dixon-Woods et al., highlight the important role leaders play in the success of interventions. This suggests that future research should ensure that key stakeholders and leaders are engaged with interventions in order to create a supportive environment that facilitates change.
Strengths and limitations
In order to minimise the risk of publication bias, searches were conducted on academic and grey literature databases as well as through contacting experts. In addition, the eligibility of the included papers were independently screened by two reviewers.
Given the lack of interventions focused on psychological safety, the scope of this review was widened to included speaking up and voice behaviour. This allowed the review to gain a broader view of how interventions could be used to improve behaviours related to psychological safety. While these behaviours are strongly associated with psychological safety, the phenomenon of psychological safety is also associated with a variety of other concepts, including communication, decision making, team performance, team learning and divergent thinking. However, examining interventions which targeted each of these related concepts was beyond the scope of this review.
This review is the first systematic review to examine interventions to improve psychological safety, speaking up and voice behaviour in healthcare teams. The mixed results found suggest a need to improve the effectiveness or efficacy, and measurement of these interventions. Longitudinal and multifaceted interventions may allow future studies to further investigate the efficacy or effectiveness of these interventions. In addition, the development and use of more objective measures may allow future studies to understand whether interventions are successful in improving psychological safety. Based on the identification of the successful elements of the interventions reviewed here, it is suggested that future intervention studies test the impact of these elements by involving end users in the design phase, target both group and organisational levels, ensure visible leader support and work across and within interdisciplinary teams.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
Abuse in Health Care
Audience Response System
Confidentiality, Equal airtime, Non-Judgemental (respectful) listening, Timeliness, Right to pass, Engaged
Chief Nursing Officer
Centre for Professionalism and Peer Support
Crew Resource Model
Concerned, Uncomfortable, Stop
Describe, Express, Suggest, Consequences
Emergency Department
Neonatal Resuscitation Program
Obstetrics/gynocology
Online Computer Library Center
Promoting Action of Research Implementation in Health Service
Preferred Reporting of Items for Systematic Reviews and Meta-Analysis
Situation, Background, Assessment, Recommendation
Team Strategies and Tools to Enhance Performance and Patient Safety
World Health Organisation
Edmondson A. Psychological safety and learning behavior in work teams. Adm Sci Q. 1999;44(2):350–83.
Article Google Scholar
Edmondson AC, Lei Z. Psychological safety: The history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav. 2014;1(1):23–43.
Newman A, Donohue R, Eva N. Psychological safety: A systematic review of the literature. Hum Res Manag Rev. 2017;27(3):521–35.
Google Scholar
Singer S, Edmondson A. Confronting the tension between learning and performance. Reflect The SoL J. 2012;11(4):34–43.
Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav. 2006;27(7):941–66.
Rathert C, Ishqaidef G, May DR. Improving work environments in health care: test of a theoretical framework. Health Care Manag Rev. 2009;34(4):334–43.
Moore L, McAuliffe E. To report or not to report? Why some nurses are reluctant to whistleblow. Clin Gov. 2012;17(4):332–42.
Moore L, McAuliffe E. Is inadequate response to whistleblowing perpetuating a culture of silence in hospitals? Clin Gov. 2010;15(3):166–78.
Edmondson AC. Speaking up in the operating room: how team leaders promote learning in interdisciplinary action teams. J Manag Stud. 2003;40(6):1419–52.
Edmondson AC, Higgins M, Singer S, et al. Understanding psychological safety in health care and education organizations: a comparative perspective. Res Hum Dev. 2016;13(1):65–83.
Pearsall MJ, Ellis AP. Thick as thieves: the effects of ethical orientation and psychological safety on unethical team behavior. J Appl Psychol. 2011;96(2):401.
Article PubMed Google Scholar
Bienefeld N, Grote G. Speaking up in ad hoc multiteam systems: Individual-level effects of psychological safety, status, and leadership within and across teams. Eur J Work Organ Psychol. 2014;23(6):930–45.
Leroy H, Dierynck B, Anseel F, et al. Behavioral integrity for safety, priority of safety, psychological safety, and patient safety: a team-level study. J Appl Psychol. 2012;97(6):1273.
Brinsfield CT. Employee silence motives: investigation of dimensionality and development of measures. J Organ Behav. 2013;34(5):671–97.
Detert JR, Edmondson AC. Implicit voice theories: taken-for-granted rules of self censorship at work. Acad Manag J. 2011;54:461–88.
Kish-Gephart JJ, Detert JR, Treviño LK, et al. Silenced by fear: The nature, sources, and consequences of fear at work. Res Organ Behav. 2009;29:163–93.
Morrison EW, Milliken FJ. Organizational silence: a barrier to change and development in a pluralistic world. Acad Manag Rev. 2000;25(4):706–25.
Beer M, Eisenstat RA. The silent killers of strategy implementation and learning. Sloan Manage Rev. 2000;41(4):29.
Shuffler ML, Diazgranados D, Maynard MT, et al. Developing, sustaining, and maximizing team effectiveness: an integrative, dynamic perspective of team development interventions. Acad Manag Ann. 2018;12(2):688–724.
Article PubMed PubMed Central Google Scholar
Tannenbaum SI, Beard RL, Salas E. Team building and its influence on team effectiveness: an examination of conceptual and empirical developments. North Holland Adv Psychol. 1992;82:117–53.
Khan K, Kunz R, Kleijnen J., et al. Systematic reviews to support evidence-based medicine: Crc press 2011.
Kitchenham B. Procedures for performing systematic reviews, vol. 33. Keele: Keele University; 2004. p. 1–26.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Moher D, Liberati A, Tetzlaff J, et al. Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Wiley Online Library; 2008.
Book Google Scholar
Godin K, Stapleton J, Kirkpatrick SI, et al. Applying systematic review search methods to the grey literature: a case study examining guidelines for school-based breakfast programs in Canada. Syst Rev. 2015;4(1):138.
Oliver KB, Swain R. Directories of institutional repositories: research results & recommendations. 72nd IFLA general conference and council; 2006. p. 20–4.
Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
Critical Appraisal Skills Programme. CASP Qualitative, Cohort Study and Randomised Controlled trial Checklist. 2018. Available at: https://casp uk.net/casptools-checklists/ Accessed: 20/03/2018.
Pluye P, Robert E, Cargo M, Bartlett G, O’Cathain A, Griffiths F, Boardman F, Gagnon MP, & Rousseau MC. Proposal: A mixed methods appraisal tool for systematic mixed studies reviews. 2011. Retrieved on [20/03/2018] from http://mixedmethodsappraisaltoolpublic.pbworks.com . Archived by WebCite ® at http://www.webcitation.org/5tTRTc9yJ
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version, vol. 1; 2006. p. b92.
Hovancsek MT. Using simulation in nursing education. Simulation in nursing education: From conceptualization to evaluation; 2007. p. 1–9.
Murray DJ, Boulet JR, Kras JF, Woodhouse JA, Cox T, McAllister JD. Acute care skills in anesthesia PracticeA simulation-based resident performance assessment. Anesthesiology. 2004;101(5):1084–95.
Issenberg SB, McGaghie WC, Hart IR, Mayer JW, Felner JM, Petrusa ER, Waugh RA, Brown DD, Safford RR, Gessner IH, Gordon DL. Simulation technology for health care professional skills training and assessment. JAMA. 1999;282(9):861–6.
Article CAS PubMed Google Scholar
Pian-Smith MC, Simon R, Minehart RD, Podraza M, Rudolph J, Walzer T, Raemer D. Teaching residents the two-challenge rule: a simulation-based approach to improve education and patient safety. Simul Healthc. 2009;4(2):84–91.
Raemer DB, Kolbe M, Minehart RD, et al. Improving anesthesiologists’ ability to speak up in the operating room: a randomized controlled experiment of a simulation based intervention and a qualitative analysis of hurdles and enablers. Acad Med. 2016;91(4):530–9.
Dufresne RL. Learning from critical incidents by ad hoc teams: the impacts of team debriefing leader behaviors and psychological safety: Unpublished dissertation. Boston: Boston College; 2007.
Ginsburg L, Bain L. The evaluation of a multifaceted intervention to promote “speaking up” and strengthen interprofessional teamwork climate perceptions. J Interprof Care. 2017;31(2):207–17.
Thomas EJ, Taggart B, Crandell S, et al. Teaching teamwork during the Neonatal Resuscitation Program: a randomized trial. J Perinatol. 2007;27(7):409.
O’Connor P, Byrne D, O’Dea A, et al. “Excuse me:” teaching interns to speak up. Jt Comm J Qual Patient Saf. 2013;39(9):426–31.
Sayre MM, McNeese-Smith D, Leach LS, et al. An educational intervention to increase “speaking-up” behaviors in nurses and improve patient safety. J Nurs Care Qual. 2012;27(2):154–60.
Johnson HL, Kimsey D. Patient safety: break the silence. AORN J. 2012;95(5):591–601.
Coyle YM, Mercer SQ, Murphy-Cullen CL, et al. Effectiveness of a graduate medical education program for improving medical event reporting attitude and behavior. BMJ Qual Saf. 2005;14(5):83–8.
Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual Patient Saf. 2014;40(4):168–AP1.
Cave D, Pearson H, Whitehead P, Rahim-Jamal S. CENTRE: creating psychological safety in groups. Clin Teach. 2016;13(6):427–31.
Swahnberg K, Wijma B. Staff’s perception of abuse in healthcare: a Swedish qualitative study. BMJ Open. 2012;2(5):e001111.
Brown D, McCormack B. Exploring psychological safety as a component of facilitation within the promoting action on research implementation in health services framework. J Clin Nurs. 2016;25(19–20):2921–32.
O’Leary DF. Exploring the importance of team psychological safety in the development of two interprofessional teams. J Interprof Care. 2016;30(1):29–34.
Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–5.
Hoenderdos JW. Towards an observational measure for team psychological safety: Unpublished thesis. Enschede: University of Twente; 2013.
Download references
Acknowledgements
Not applicable.
This research is funded by the Irish Research Council and the Ireland East Hospital Group under the Employment Based Partnership Scholarship. The funding body did not play a role in the study design, data collection, analysis and interpretation of data or in the writing of the manuscript.
Author information
Authors and affiliations.
UCD School of Nursing, Midwifery & Health Systems, UCD Health Sciences Centre, University College Dublin, Dublin 4, Ireland
Róisín O’Donovan & Eilish McAuliffe
You can also search for this author in PubMed Google Scholar
Contributions
Both authors were involved in the design and planning of this systematic review. ROD completed title and abstract screening. Both authors completed full text screening. ROD completed data extraction. ROD drafted the manuscript and EMcA contributed to writing and revising the paper. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Róisín O’Donovan .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Search Strategy. Search strategies presented for each database searched.
Additional file 2.
Data Extraction Template. The categories by which data was extracted from excluded studies are presented in the final template.
Additional file 3.
Quality Assessment. The results of the quality assessment conducted are presented according to study design. The Critical Appraisal Skills Programme Qualitative Checklist, Cohort Study Checklist, or the Mixed Methods Appraisal Tool are presented.
Additional file 4.
Summaries of included studies. Each table includes summary details of all interventions included in the review. Details are listed under the following titles: Author, Aims, Participants, Intervention Duration, Intervention Content, Methods of Evaluation, Key Findings.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
O’Donovan, R., McAuliffe, E. A systematic review exploring the content and outcomes of interventions to improve psychological safety, speaking up and voice behaviour. BMC Health Serv Res 20 , 101 (2020). https://doi.org/10.1186/s12913-020-4931-2
Download citation
Received : 02 May 2019
Accepted : 27 January 2020
Published : 10 February 2020
DOI : https://doi.org/10.1186/s12913-020-4931-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychological safety
- Speaking up
- Voice behaviour
- Interventions
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.9(1); 2022 Jan
A concept analysis of psychological safety: Further understanding for application to health care
1 Department of Gerontological Nursing and Healthcare Systems Management, Graduate School of Health Care Sciences, Tokyo Medical and Dental University (TMDU), Tokyo Japan
Yoshie Yumoto
Miki sasaki, yasuko ogata, associated data.
The data that support the findings of this study are available in the Appendix of this article.
To clarify the concept of psychological safety in a healthcare context and to provide the first theoretical framework for improving interpersonal relationships in the workplace to better patient care.
A Rodgers’ concept analysis.
The concept analysis was conducted using a systematic search strategy on PubMed, CINAHL, PsycINFO and Ichushi‐Web.
An analysis of 88 articles studying psychological safety in health care identified five attributes: perceptions of the consequences of taking interpersonal risks, strong interpersonal relationships, group‐level phenomenon, safe work environment for taking interpersonal risks and non‐punitive culture. The antecedents included structure/system factors, interpersonal factors and individual factors. The four consequences included performance outcomes, organizational culture outcomes, and psychological and behavioural outcomes.
1. INTRODUCTION
Improving patient safety is a top priority in health care around the world (WHO, 2019). According to the World Health Organization ( 2019 ), providing an open and blame‐free safety culture around incident reporting is crucial for maintaining patient safety. Meanwhile, the Organisation for Economic Co‐operation and Development ( 2017 ) advises that a focus on collective improvement and teamwork is also crucial for patient safety. Establishing a sense of psychological safety in the clinical environment fosters these elements, allowing nurses to more effectively ensure patient safety.
2. BACKGROUND
The concept of psychological safety has been discussed across various disciplines and industries such as aviation, education and manufacturing. Common definitions of psychological safety include ‘feeling able to show and employ one's self without fear of negative consequences to self‐image, status, or career’ (Kahn, 1990 , p. 708) and ‘a shared belief that the team is safe for interpersonal risk‐taking’ (Edmondson, 1999 , p. 354). This concept's application has spread to the healthcare discipline since it is known to yield positive healthcare outcomes. Recent studies in health care have demonstrated that psychological safety influences patient safety, interprofessional collaboration, engagement in quality improvement work, learning from failures and reporting adverse events (Arnetz, Sudan, Goetz, Counts, & Arnetzet al., 2019 ; Greene et al., 2020 ; Hirak et al., 2012 ; O'Leary, 2016 ; Tucker et al., 2007 ). Thus, psychological safety is considered a critical factor to account for in projects that seek to better health care, including those interested in high‐quality nursing, effective teamwork and patient safety.
Although research on psychological safety has increased in the healthcare field, its definition in this context remains unclear. A concept taken from other domains should be critically considered about its utility and importance in a new domain (Meleis, 2017 ). However, little research has discussed psychological safety in a theoretical sense. For example, one study has described psychological safety using the same concept as trust (Kang et al., 2020 ); others have described psychological safety as a speaking‐up‐related climate, part of justice culture, or feeling of safety around innovation (Appelbaum et al., 2018 ; Schwappach et al., 2018 ; Zuber & Moody, 2018 ). The lack of theoretical underpinning may hinder the advancement in healthcare management in terms of ensuring a conducive environment for high‐quality care. Furthermore, few specific tools measure psychological safety in a healthcare context (O’Donovan et al., 2020 ). For example, Edmondson ( 1999 ) developed a scale to measure psychological safety in a general context including health care; meanwhile, Richard et al. ( 2017 ) developed a questionnaire measuring aspects such as psychological safety that influence speaking‐up behaviour among healthcare staff about patient safety concerns. Nonetheless, the lack of statistically rigorous measurements of psychological safety, specifically in the context of health care (O’Donovan et al., 2020 ), prevents the exploration of its antecedents and implications for healthcare management.
2.1. Research question
A concept analysis can clarify the structures of a concept and its relationships to other concepts. It also highlights implications for future scale development and clinical practices. Rodgers ( 2000 ) developed a concept analysis approach to describe a concept that changes in a context, allowing for its development and further research. Thus, this study aimed to identify the concept of psychological safety in a healthcare context through a Rodgers’ concept analysis and provide the first theoretical foundations for how such an understanding may better interpersonal relationships and patient care. Therefore, our research question was What are the attributes, antecedents and consequences of psychological safety in the context of health care?
3. THE STUDY
3.1. design.
This study used Rodgers’ evolutionary approach. Rodgers’ approach aims to capture changing and evolving concepts over time and develop a concept for further research and clinical practice. It includes the following six steps to analyse a concept: (1) identifying the concept of interest and associated expressions; (2) identifying and selecting an appropriate realm (setting and sample) for data collection; (3) collecting data relevant to identify the attributes of the concept, the antecedents, consequences and related concepts; (4) analysing the data in terms of the above characteristics of the concept; (5) identifying an exemplar of the concept, if appropriate; and (6) identifying implications, hypotheses and implications for further development of the concept (Rodgers, 2000 , p.85).
3.2. Method
This concept analysis was conducted using a systematic search strategy on PubMed, CINAHL, PsycINFO and Ichushi‐Web, with no publication date limitation. Keywords used were as follows: “psychological safety [AB]” was used in PubMed, CINAHL and Ichushi‐Web; “psychological safety [AB]” AND (health care OR doctor OR physician OR nurs* OR hospital OR medic*) were used in PsycINFO. This study was undertaken in April 2020.
The search yielded 300 articles after removing duplicates. Articles that met the following inclusion criteria were selected: (1) focused on concepts of psychological safety, (2) conducted in health care, (3) employees completed a survey, (4) were not literature review articles, (5) was an empirical study, (6) not duplicated among databases and (7) other reasons, such as written in English and Japanese and availability of the full text. Two reviewers scanned the titles and abstracts of the articles. As shown in Figure 1 , this procedure excluded 134 articles. Additionally, 78 articles were excluded through the full‐text scanning by the reviewers. Finally, this systematic strategy led to 88 articles. The PRISMA guideline was used for this concept analysis.

Flowchart of article selection
3.3. Analysis
As described by Rodgers ( 2000 ), a thematic analysis was conducted to identify the concept, and descriptions of attributes, antecedents and consequences were selected from each article. According to Rodgers’ approach, attributes constitute a real definition, an antecedent is a phenomenon before an instance of the concept, and a consequence is a result of the concept (Rodgers, 2000 ). The findings from the articles were put into the matrix sheet. Subsequently, they were categorized and organized the descriptions according to their similarities and trends. Finally, we again grouped the categories made to increase the level of abstraction. This analysis process was repeated until four researchers agreed on the whole process of categorizations and abstractions.
3.4. Ethics
We declare no conflicts of interest associated with this manuscript. This work was supported by JSPS KAKENHI, Grant Number JP19H03920. Furthermore, this concept analysis was not needed the Research Ethics Committee approval and the patient consent because our study analysed only published articles.
4.1. Overview of contexts and results
Table A1 in the Appendix lists the 88 articles analysed in this study. Of these 88 articles, 60 were published between 2016 and 2020. Fifty‐one articles cited definitions of psychological safety by Edmondson ( 1999 ). Fifty‐eight articles used instruments to measure psychological safety, of which 35 (60.3%) used self‐report measurements developed by Edmondson ( 1999 ). Additionally, 47 of the included articles were studies conducted in Northern America (United States: n = 47; Canada: n = 1), 26 in Europe (Western: n = 16; Northern: n = 9; Southern: n = 1) and 8 in Asia (Western: n = 4; Eastern: n = 2; Southeastern: n = 1; and Southern: n = 1).
This concept analysis identified five attributes, three antecedents and four consequences. Figure 2 illustrates the conceptual model of psychological safety in the healthcare context based on the findings of this analysis.

Conceptual model of psychological safety in the health care context
4.2. Attributes
4.2.1. perceptions of the consequences of taking interpersonal risks.
The concept analysis found that psychological safety captured perceptions of the consequences of interpersonal risk behaviours in the work environment. Interpersonal risk behaviour has often caused team members to be labelled ignorant, incompetent and disturbers in work environments, including behaviours such as asking questions, reporting errors and bringing up concerns (Edmondson, 2019 ). For example, MacCurtain et al. ( 2018 ) described psychological safety as when employees feel safe voicing concerns and reporting problems and can trust their supervisor.
4.2.2. Strong interpersonal relationships
This attribute included a description of strong interpersonal relationships, such as trust and respect. For example, Albritton et al. ( 2019 ) described that a high level of psychological safety reflected a team climate of interpersonal trust and mutual respect.
4.2.3. Group‐level phenomenon
This attribute suggested that psychological safety was a group‐level phenomenon, although the first and second themes described psychological safety as an individual‐level concept, including individuals’ perceptions and feelings. Lee, Yang, and Chen ( 2016 ) described psychological safety as a shared belief among groups that facilitated the acceptability of behavioural risks.
4.2.4. Safe work environment for taking interpersonal risks
The concept analysis found that psychological safety concerns in the work environment were linked to interpersonal risk behaviours. Noah and Steve ( 2012 ) stated that the organizational work environment includes systems, procedures, practices, values and philosophies. Singer et al. ( 2015 ) identified psychological safety as a cultivated environment safe for interpersonal risk‐taking. Based on the definition of the work environment, the concept of psychological safety concerns the structure dimension in an organization that facilitates interpersonal risk.
4.2.5. Non‐punitive culture
Psychological safety was recognized as an organizational culture where team members were not punished or blamed even if they took interpersonal risks. According to previous studies, organizational culture is a wider concept than that of the work environment described in the previous category in this paper. Allaire and Firsirotu ( 1984 ) argued that organizational culture comprises three components: the structure of an organization; a cultural system including an organization's myths, ideology and values; and individual factors including employees’ experiences, personalities and cognitions. Lee et al. ( 2016 ) stated that teams possessed a common belief and a non‐punitive culture that accepted the risk of reporting behaviours when team members perceived psychological safety.
4.3. Antecedents
4.3.1. the structure/system factor.
This theme included policy and procedures, fairness, organizational support and a specific management style. As an example of management style, Halbesleben and Rathert ( 2008 ) reported that an improvement orientation management style was a predictor of psychological safety.
4.3.2. Interpersonal factors
Interpersonal factors were identified as antecedents of psychological safety, including trust, respect, effective relationships, support, high‐quality communication and leader behaviour. Effective relationships involved interpersonal relationships among work teams, such as collegial teamwork and familiarity in the team. This analysis distinguishes support in this theme from organizational support described in the previous category. Support in this theme is particularly concerned with interpersonal support among team members in a work environment. Examples include support from leaders, team members and peers.
Additionally, high‐quality communication fosters psychological safety. High‐quality communication for psychological safety has the following features: frequent, open and honest communication.
Furthermore, this analysis found that leader behaviour was a prerequisite for psychological safety. Leader behaviour as an antecedent comprises leadership, inclusiveness, behavioural integrity and acknowledging employees’ fallibility. Various types of leadership were positively related to psychological safety, although there were mixed results among the selected articles. For instance, transformational leadership predicted psychological safety (Raes et al., 2013 ). A leader's inclusiveness, described as a leader's words and deeds that invite and appreciate others’ contributions (Nembhard & Edmondson, 2006 ), facilitated psychological safety. Furthermore, behavioural integrity, defined as the perception of alignment between a leader's words and deeds (Simons, 2002 ), promoted psychological safety.
4.3.3. Individual factors
Individual factors included demographic characteristics, status differences and employees’ behaviours and skills.
Demographic characteristics were associated with psychological safety. For example, age was negatively related to psychological safety (Buljac‐Samardžić et al., 2018 ). Moreover, minorities perceive lower psychological safety than that of white employees (Derickson et al., 2015 ). Differences in status levels also influenced psychological safety. This analysis identified two types of status differences as antecedents. First, there were status differences in disciplines; for example, residents generally had lower status than physicians. Residents’ perceptions of power distance were related to psychological safety (Appelbaum et al., 2016 ). Second, status differences among disciplines were also antecedents. For instance, about psychological safety, physicians felt more than nurses, and nurses felt more than respiratory therapists in a neonatal intensive care unit (Nembhard & Edmondson, 2006 ).
Finally, employee behaviours and skills were identified as antecedents. Less incivility and more self‐forgiveness skills were associated with greater feelings of psychological safety.
4.4. Consequences
4.4.1. performance outcomes.
Psychological safety influenced safety culture in a team and quality of care, including patient safety, effective rescue, patient‐centred care, patient satisfaction and transition to professional practice.
4.4.2. Organizational culture outcomes
This theme of consequences included dimensions of interpersonal relationships and the culture/work environment. The analysis revealed that psychological safety facilitated interpersonal relationships such as interprofessional collaboration, teamwork and trust. Additionally, psychological safety influenced the dimensions of culture and work environment in a healthcare organization. Creativity, transparency and innovation appeared in work environments with high psychological safety. Furthermore, psychological safety created a climate of organizational learning.
4.4.3. Psychological outcomes
Psychological safety influenced healthcare providers’ psychological outcomes. Specifically, psychological safety enhanced job satisfaction, work engagement, organizational commitment and empowerment and led to less emotional exhaustion and stress. Additionally, psychological safety encouraged healthcare providers to engage in quality improvement work.
4.4.4. Behavioural outcomes
Finally, this analysis identified the dimensions of healthcare workers’ behavioural outcomes as consequences of psychological safety.
A high level of psychological safety allows healthcare workers to engage in interpersonal risk behaviours. Interpersonal risk behaviours include learning behaviour, speaking‐up behaviour, giving and seeking feedback, error‐seeking behaviour, extra‐role behaviour and implementation of new practices. Learning behaviour allows a team to obtain and process data that facilitates a team to adapt and improve (Edmondson, 1999 ). Furthermore, psychological safety engendered speaking‐up behaviour. Speaking‐up behaviour was referred to as an open statement of views or opinions about workplace matters (Premeaux & Bedeian, 2003 ). Specifically, reporting errors, suggesting ideas, bringing up concerns, asking questions, asking for help and sharing knowledge were identified as positive outcomes of psychological safety in health care.
Furthermore, high‐quality communication was built when healthcare providers felt psychological safety. In contrast, lack of psychological safety was associated with negative behaviours. For instance, the absence of psychological safety increased oppressive behaviour, disruptive behaviour, workarounds and bullying.
4.5. Model case
A new graduate nurse makes a mistake. At first, she/he is afraid to report the mistake, but the fear eventually disappears.
The psychologically safe unit allows the graduate nurse to report the mistake to the nurse manager. The unit has a policy of fostering a culture that does not punish others for reporting errors. The manager in the unit has implemented this policy by her/his words and deeds to keep her/his integrity. Moreover, the new graduate nurses have received support from other nurses in the unit. The policy and supportive relationships help the new nurses feel safe in reporting errors in the unit. In addition, the unit with high psychological safety influences their psychological and performance dimension. The new graduate nurses could engage in their work in the psychologically safe unit and transition successfully into professional practice.
This exemplar demonstrates the attributes, antecedents and consequences of psychological safety in a healthcare team, with a high level of it identified in this concept analysis. It can help nurse managers and researchers understand the concept of psychological safety in a clinical situation.
5. DISCUSSION
Our concept analysis identified the attributes, antecedents and consequences of psychological safety in a healthcare context. The concept of psychological safety is a multilevel phenomenon related to a unit culture that facilitates interpersonal risk behaviour. This study demonstrated that psychological safety in a healthcare work environment influenced proactive behaviours, such as asking questions, reporting errors and communicating openly. Additionally, psychological safety proved to be associated with strong interpersonal relationships and an effective culture that includes collaboration, trust and innovation, which ensure patient safety.
Many of the included articles were published in the past five years, suggesting that the concept of psychological safety in health care is still developing. More than half of the articles cited the definition or measurement developed by Edmondson ( 1999 ). This finding suggests that Edmondson's work has been instrumental in stimulating research on psychological safety in the healthcare field. Mounting research has yielded attributes of psychological safety that are unique to health care and demonstrated that antecedents and consequences reflect the context (in this case, health care).
We found five themes related to attributes. The theme of a group‐level phenomenon was considered an attribute specific to health care. This is in line with a previous study comparing the characteristics of healthcare and educational settings (Edmondson et al., 2016 ), which concluded that psychological safety as a group phenomenon was unique to the healthcare environment. In the educational context, differences in the perception of psychological safety existed between elementary and high schools. Centrally, in the healthcare context, differences in perception exist in a hospital; that is, there were differences between units, such as between surgical and medical units.
However, this analysis identified psychological safety as an individual‐level phenomenon, including themes of the perception of interpersonal risk and strong interpersonal relationships. Therefore, our findings suggest that psychological safety has both group and individual dimensions. We considered this finding to be complementary rather than contradictory. The theory of organizational culture (Allaire & Firsirotu, 1984 ) explains this complex characteristic of psychological safety. According to this theory, organizational culture consists of interpretations of what members experience in the group; in other words, a feeling of psychological safety among members is a prerequisite for building a culture of psychological safety in teams.
We also identified three antecedent themes (structure/system factors, interpersonal factors and individual factors). Specifically, the findings suggest that the theme of status differences was a unique antecedent in the healthcare context. A systematic review (Newman et al., 2017 ) analysing articles without limitations on disciplines had similarly identified status differences as an antecedent. Notably, this study found two types of status differences in the context of health care—in a discipline and among disciplines. Moreover, our findings indicated that, to establish psychological safety in healthcare organizations, it is necessary to reduce status gaps both in and among disciplines.
Four themes were identified as consequences of psychological safety. The theme of implementing new practices reflected the contextual characteristics of health care. As diseases and evidence‐based care evolve and new equipment and skills are periodically developed, healthcare providers must constantly try to implement new practices. Therefore, our results suggested that additional studies to examine the relationship between psychological safety and implementation of new practices are necessary to promote high performance in the healthcare environment. Furthermore, we found complex themes that were identified as both antecedents and consequences, including trust, interpersonal support and high‐quality communication. This finding implied that some of the antecedents and consequences of psychological safety influenced each other.
Our concept analysis has implications for further research. First, we recommend that further research develop a measurement including specific items that reflect the context of health care. Many of the selected articles used the measurement developed by Edmondson ( 1999 ). This measurement captures psychological safety in the general context and is composed of a single factor. An additional measurement that captures psychological safety in the context of health care reflecting the attributes found in this study is needed to obtain detailed suggestions for nursing managers. Therefore, the themes of attributes, antecedents and consequences in this analysis may help develop a new measurement tool. New measurements could also facilitate empirical studies that would establish a team culture of psychological safety.
Second, we recommend examining whether psychological safety is affected by national culture. Only a few articles conducted in Eastern cultures were selected, although this analysis used both English and Japanese databases. Newman et al. ( 2017 ) stated that national culture influences psychological safety. For instance, team members in a work environment in Western cultures perceive more psychological safety than those in Eastern cultures, as Western cultures are generally characterized by a low level of collectivism; thus, speaking‐up behaviour is considered to have minimal social cost. However, previous studies concluded that little is known about how psychological safety is influenced by differences in culture (Newman et al., 2017 ). Therefore, additional research in the healthcare field needs to be conducted in various countries to clarify cultural influences.
5.1. Limitations
Two limitations to this concept analysis were identified. First, the inclusion criteria for articles may have resulted in bias: This analysis included articles that referred to ‘psychological safety’ in the abstract; moreover, we excluded grey literature or articles written in languages other than English and Japanese. Therefore, we could have missed relevant articles. Second, this analysis used the search term “psychological safety,” which may have caused us to miss articles that expressed “psychological safety” using different terms. However, to minimize bias, we checked the surrogate terms of psychological safety and discussed the validity of the search term before conducting the search strategy.
5.2. Conclusion
This study demonstrated that psychological safety in a healthcare work environment influences proactive behaviours such as asking questions, reporting errors and open communication. Additionally, psychological safety is associated with strong interpersonal relationships and an effective culture that includes collaboration, trust and innovation, which ensure patient safety.
In clinical environments, nurse managers serve an important role in cultivating a constructive work environment. Nurse managers’ roles include improving quality and performance and encouraging collaboration among interprofessional staff and nurses. Our findings offer insights to help nurse managers enhance psychological safety in the workplace. First, nurse managers can build a unit with psychological safety through a set of procedures while adopting consistency, bias‐suppression, accuracy, correctability, representativeness and ethicality rules (Leventhal, 1980 ). Nurse managers consider these rules when making decisions, which allows them to achieve high‐quality care through psychological safety.
Second, nurse managers can build interpersonal relationships with high psychological safety through leadership behaviours consisting of inclusiveness and/or high‐quality communication. Specially, we recommend that nurse managers encourage staff nurses’ contributions to their unit and openly and frequently communicate with nurses and interprofessional staff. Nurse managers can use these behaviours to establish psychologically safe relationships that allow staff nurses to ask questions and provide better care with interprofessional collaboration.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest associated with this manuscript.
AUTHOR CONTRIBUTIONS
Ayano Ito involved in design, data collection, analysis and interpretation of data, and drafting the manuscript. Kana Sato involved in design, data collection and drafting the manuscript. Yoshie Yumoto and Miki Sasaki involved in interpretation of data and drafting the manuscript. Yasuko Ogata involved in design, interpretation of data and drafting the manuscript.
ACKNOWLEDGEMENT
We would like to thank the support of Japan Society for Promotion Science (JSPS).
List of included articles
| No. | Authors | Purposes of study | Attribute | Antecedent | Consequence |
|---|---|---|---|---|---|
| 1 | Agius et al. ( ), United Kingdom | To explore primary educators’ perceptions on modern process consultants at hospitals and the impacts of modernization on their roles | ‐ | ‐ | Organizational culture outcome— Effective work environment Psychological outcome— Engagement in improvement work |
| 2 | Albritton et al. ( ), Ghana | To analyse the relationships between psychological safety, learning behaviour and quality improvement implementation | Strong interpersonal relationship | ‐ | Organizational culture outcome— Support, creativity Psychological outcome— Engagement in improvement work Behavioural outcome— Learning behaviour |
| 3 | Alingh et al. ( ), Netherlands | To explore the relationships between specific management styles, safety climate, psychological safety and speaking‐up behaviour | ‐ | Structure/system factor— Commitment‐based safety management Interpersonal factor— Leader behaviour | Behavioural outcome— Speaking‐up behaviour, bringing up concerns, high‐quality communication, learning behaviour |
| 4 | Appelbaum et al. ( ), United States | To establish the validity of two instruments that assess the learning environment perceptions in the clinical environment | ‐ | ‐ | Psychological outcome— Job satisfaction Behavioural outcome— Learning behaviour |
| 5 | Appelbaum et al. ( ), United States | To explore relationships between power distance and inclusiveness on psychological safety and reporting behaviour | ‐ | Structure/system factor— Policy, Procedure Interpersonal factor— Inclusiveness Individual factor— Status differences, less fear of being ignorant, incompetent, disruptive | Performance outcome— High patient safety Behavioural outcome— Reporting errors, intention to report adverse events |
| 6 | Arnetz et al. ( ), United States | To identify organizational determinants of bullying and the resulting work disengagement among nurses | Strong interpersonal relationship | ‐ | Psychological outcome— Work engagement Behavioural outcome— Reporting adverse events, less bullying |
| 7 | Arnetz et al. ( ), United States | To examine associations between work environment, specific stress biomarkers and patient outcomes about the quality of nurse care | ‐ | ‐ | Organizational culture outcome— Effective work environment Psychological outcome— Work engagement, less stress Behavioural outcome— Learning behaviour, reporting errors, less bullying |
| 8 | Baik and Zierler ( ), United States | To explore experiences and perceptions about team intervention, including the Team Strategies and Tool to Enhance Performance and Patient Safety (STEPPS)® training and the structured interdisciplinary bedside rounds (SIBR) process | ‐ | ‐ | Behavioural outcome— Bringing up concerns, asking questions, sharing information |
| 9 | Barling et al. ( ), Canada | To examine the effects of various leadership behaviours by surgeons on team performance | ‐ | Interpersonal factor — Transformational leadership, coaching, less abusive supervision | Behavioural outcome— Implementation of new practices, bullying |
| 10 | Basit ( ), Malaysia | To examine the mediator roles of psychological safety and feelings of obligation between trust in supervisors and job engagement | Perceptions of the consequences of taking interpersonal risks | Interpersonal factor — Effective relationship, support from leader, trust (leader–member) | Psychological outcome— Work engagement, obligation feeling Behavioural outcome— Interpersonal risk behaviour, asking questions |
| 11 | Bindels et al. ( ), Netherlands | To explore how physicians conceptualize and experience reflection in their professional practice | ‐ | ‐ | Performance outcome— high patient safety Psychological outcome— Engagement in improvement work Behavioural outcome— Speaking‐up behaviour |
| 12 | Bradley et al. ( ), United States | To develop a scale for assessing organizational culture about efforts to reduce mortality in hospitals and assess the validity and reliability of the scale | Group‐level phenomenon | ‐ | ‐ |
| 13 | Brown and McCormack ( ), Northern Ireland | To explore the factors that enhanced pain management practices for older people | ‐ | ‐ | Performance outcome — Person‐centred care |
| 14 | Brown and McCormack ( ), Northern Ireland | To explore the facilitators that allowed the healthcare team to analyse their practice and enhance quality of care | ‐ | Interpersonal factor – Effective relationship, leadership, support, respect | Organizational culture outcome— Effective work environment Behavioural outcome— Interpersonal risk behaviour, less oppressive behaviour |
| 15 | Buljac‐Samardžić et al. ( ), Netherlands | To analyse the relationship between psychological safety, psychological detachment and patient safety | ‐ | Individual factor— Gender, age | Organizational culture outcome— Support Psychological outcome— Work engagement, more psychological detachment Behavioural outcome— Interpersonal risk behaviour, learning behaviour, speaking‐up behaviour, sharing knowledge, reporting errors, feedback behaviour, extra‐role behaviour |
| 16 | Carmeli and Zisu ( ), Israel | To explore the relationships between organizational trust, perceived organizational support, psychological safety and internal auditing | Group‐level phenomenon | Structure/system factor— Support from organization Interpersonal factor— Trust | Psychological outcome— Engagement in improvement work Behavioural outcome— Learning behaviour, reporting errors, feedback behaviour |
| 17 | Clark et al. ( ), United States | To investigate the influence of role definition as moderator between safety climate and organizational citizenship behaviour among nurses | ‐ | ‐ | ‐ |
| 18 | Colet et al. ( ), Saudi Arabia | To investigate nurses’ perceptions of climate for preventing infections and explore its predictors | ‐ | Individual factor— Nationality, clinical experience | ‐ |
| 19 | Cuellar et al. ( ), United States | To investigate the influence of various practice ownerships on work environment, culture of learning behaviour, psychological safety and burnout | ‐ | ‐ | ‐ |
| 20 | Curry et al. ( ), EU countries | To explore the influence of organizational culture and improve hospital performance on care by implementing an intervention | ‐ | ‐ | Organizational culture outcome— Effective work environment, supportive relationships, power‐sharing Behavioural outcome— Speaking‐up behaviour |
| 21 | Curşeu ( ), Netherlands | To explore the relationships between diversity in team, communication, trust, psychological safety and learning behaviour | ‐ | Interpersonal factor— Frequency of communication | Behavioural outcome— Learning behaviour, speaking‐up behaviour |
| 22 | De Brún and McAuliffe ( ), Ireland | To theoretically understand the contextual conditions and mechanisms to promote collective leadership and the outcomes | ‐ | Interpersonal factor— Frequency of communication, open communication | Performance outcome— Patient satisfaction, safety culture Organizational culture outcome— Effective teamwork, power‐sharing, conflict management Psychological outcome— Job satisfaction, engagement in improvement work Behavioural outcome— Sharing knowledge |
| 23 | Derickson et al. ( ), United States | To explore the relationship between psychological safety and the willingness to report errors | ‐ | Interpersonal factor— Inclusiveness Individual factor— Race, status difference | Behavioural outcome—s Interpersonal risk behaviour, learning behaviour, reporting errors |
| 24 | Edmondson et al. ( ), United States | To examine the relationship between psychological safety, collective learning and implementation of new routines | ‐ | Interpersonal factor— Leader behaviour | Organizational culture outcome— Coordination Behavioural outcome— Interpersonal risk behaviour, learning behaviour, implementation of new practices |
| 25 | Edmondson et al. ( ), United States | To compare and understand the characteristics of psychological safety in 26 healthcare and education organizations | Group‐level phenomenon | Interpersonal factor— Inclusiveness, acknowledgement of mistakes and fallibility, acceptance, support from leader, respect Individual factor— Status difference | Psychological outcome— Engagement in improvement work Behavioural outcome— Learning behaviour, asking for help |
| 26 | Erichsen Andersson et al. ( ), Sweden | To examine the process of a knowledge translation intervention to improve hand hygiene and aseptic techniques | ‐ | ‐ | Psychological outcome – Engagement in improvement work Behavioural outcome – Learning behaviour, implementation of new practices, less disruptive behaviours |
| 27 | George, Elwy et al. ( ), United States | To explore the relationship between the perceptions of organizational culture and adverse events | ‐ | ‐ | Performance outcome— Safety culture Psychological outcome— Work engagement Behavioural outcome— Bringing up concerns |
| 28 | George, Parker et al. ( ), United States | To describe and compare the approaches used to select safety priorities | ‐ | ‐ | Organizational culture outcome— Effective work environment Behavioural outcome— Bringing up concerns |
| 29 | Gilmartin et al. ( ), United States | To describe the intervention for quality improvement experience and evaluate the effectiveness | ‐ | ‐ | Behavioural outcome— Speaking‐up behaviour, suggesting ideas |
| 30 | Gilmartin et al. ( ), United States | To explore the relationship between perceptions of psychological safety and reports of non‐adherence to the central line insertion checklist at the unit level | ‐ | ‐ | Behavioural outcome— Learning behaviour, reporting errors, suggesting ideas |
| 31 | Gong et al. ( ), China | To explore the relationships between psychological safety, ethical leadership, feedback seeking and the effect of power distance | ‐ | Interpersonal factor— Ethical leadership Individual factor— Power distance | Behavioural outcome— Feedback behaviour |
| 32 | Grant et al. ( ), Unites States | To measure emotional exhaustion, self‐verification, psychological safety and external rapport in surveys before and after the interventions | ‐ | Individual factor— Self‐reflective titles | Psychological outcome— Less emotional exhaustion Behavioural outcome— Asking for help, expressing oneself |
| 33 | Greene et al. ( ), United States | To examine relationships between psychological safety and practices to prevent specific infections | ‐ | ‐ | Performance outcome— Patient safety, safety culture Behavioural outcome— Learning behaviour |
| 34 | Halbesleben and Rathert ( ), United States | To examine the relationship between climate for continuous quality improvement, psychological safety and workarounds | Group‐level phenomenon | Structure/system factor— Organizational/team structure, improvement orientation management, support from organization Interpersonal factor— High‐quality communication, behavioural integrity, support from leader, trust (leader–member, member–member), respect | Performance outcome— Patient safety Behavioural outcome— Fewer workarounds |
| 35 | Halbesleben et al. ( ), United States | To examine the relationships between psychological safety, behavioural integrity, safety compliance and occupational injuries | ‐ | Interpersonal factor — Trust | Performance outcome — Safety culture Behavioural outcome— Learning behaviour, reporting behaviours |
| 36 | Hesselgreaves and MacVicar ( ), Scotland | To explore trainees’ perspectives to understand the impact of practice‐based small‐group learning on curriculum needs, preparation for independent practice and facilitator learning | ‐ | ‐ | Behavioural outcome— Learning behaviour |
| 37 | Hirak et al. ( ), Israel | To analyse the relationship between leader inclusiveness, members’ perceptions of psychological safety, learning from failures and unit performance | ‐ | Structure/system factor— Support from organization Interpersonal factor — Inclusiveness, acknowledgement of mistakes and fallibility, accessibility to leader, openness | Behavioural outcome— Learning behaviour, suggesting ideas, bringing up concerns, expressing oneself |
| 38 | Huddleston and Gray ( ), United States | To explore nurses’ perceptions of a healthy Work environment setting and define the characteristics of a healthy work environment | ‐ | ‐ | Behavioural outcome— Speaking‐up behaviour |
| 39 | Jain et al. ( ), United States | To explore the role of psychological safety as a key factor to improve team communication | ‐ | Structure/system factor— Geographic dispersion Interpersonal factor— Familiarity, leader behaviour, status difference | Organizational culture outcome— Collaboration, effective teamwork Behavioural outcome— Suggesting ideas, sharing knowledge, open communication |
| 40 | Kang et al. ( ), Unites States | To examine the relationships between employee engagement, patient satisfaction and various organizational culture characteristics, including psychological safety, fairness and innovation | Group‐level phenomenon | Structure/system factor— Fairness | Performance outcome— Patient satisfaction Psychological outcome— Work engagement, positive emotion, empowerment |
| 41 | Keitz et al. ( ), United States | To examine the influence of clinical learning experiences on career choices and considerations about future employment | ‐ | ‐ | Psychological outcome— Job satisfaction, engagement in improvement work, less turnover intention Behavioural outcome Reporting errors |
| 42 | Kessel et al. ( ), German | To examine the impact of psychological safety on the process of sharing knowledge and creative performance in teams | Group‐level phenomenon, strong interpersonal relationships | ‐ | Psychological outcome— Engagement in improvement work Behavioural outcome— Interpersonal risk behaviour, learning behaviour, sharing knowledge, frequent communication |
| 43 | Klingberg et al. ( ), Switzerland | To estimate the influence of incivility on psychological safety among physicians in an emergency department | ‐ | Interpersonal factor— Less incivility | Organizational culture outcome— Innovation Behavioural outcome— Learning behaviour |
| 44 | Kolbe et al. ( ), Switzerland | To develop a debriefing approach for simulation training and demonstrate its effectiveness | ‐ | ‐ | ‐ |
| 45 | Lazzara et al. ( ), United States | To examine the effect of telemedicine on team attitudes, behaviours, cognitions and climates | ‐ | ‐ | ‐ |
| 46 | Lee et al. ( ), United Kingdom, Taiwan | To examine the factors that allowed nurses to report incidents | Non‐punitive culture, group‐level phenomenon | ‐ | Organizational culture outcome— Effective work environment Behavioural outcome— Interpersonal risk behaviour, reporting incidents, intention to report incidents, suggesting ideas, intention to ask questions, intention to discuss incidents |
| 47 | Leroy et al. ( ), Belgium | To understand the influence of leader integrity on safety climate and patient safety outcomes | ‐ | ‐ | Behavioural outcome— Reporting errors |
| 48 | Lyman, Ethington et al. ( ), United States | To describe the process to reach excellent clinical performance in a team and examine the relationship between psychological safety and organizational learning | ‐ | ‐ | Organizational culture outcome— Support Psychological outcome — Engagement in improvement work Behavioural outcome— Interpersonal risk behaviour, reporting hazardous situations |
| 49 | Lyman, Shaw et al. ( ), United States | To discover new insights about organizational learning in hospital units | ‐ | Interpersonal factor— Ethical leadership, change‐oriented leadership, inclusiveness, trust (leader–member) | Psychological outcome — Engagement in improvement work Behavioural outcome— Learning behaviour |
| 50 | Lyman et al. ( ), United States | To describe the experiences on psychological safety perceived by new graduate Registered Nurses | Group‐level phenomenon | Structure/system factor— Spending time, supportive system Interpersonal factor— Effective relationship, support from leader, support from members, trust | Performance outcome— Transition to professional practice Organizational culture outcome— Effective work environment Psychological outcome — Work environment, commitment to patient safety Behavioural outcome— Speaking up about problems, sharing ideas |
| 51 | MacCurtain et al. ( ), Ireland | To examine the relationships between a bystander's perception of psychological safety and their response to witnessing bullying | Perceptions of the consequences of taking interpersonal risks, group‐level phenomenon, strong interpersonal relationships | ‐ | Behavioural outcome— Reporting problems, bringing up concerns, less bullying |
| 52 | Martland, et al. ( ), Australia | To explore the communication process between clinicians that facilitated the activation of rapid response teams | ‐ | Behavioural outcome— Learning behaviour, speaking‐up behaviour | |
| 53 | MacCurtain et al. ( ), United States | To describe the experiences of psychological safety and explore the factors to build a psychological safety climate | ‐ | ‐ | ‐ |
| 54 | Nembhard and Edmondson ( ), United States | To examine the relationship between professional status, leader inclusiveness, psychological safety in teams and engagement in quality improvement | Group‐level phenomenon | Interpersonal factor — Leadership, inclusiveness Individual factor— Status differences among disciplines, experience year | Psychological outcome— Engagement in improvement work Behavioural outcome— Interpersonal risk behaviour, implementation of new practices |
| 55 | O'Leary ( )Ireland | To explore the influence of psychological safety on the development of interdisciplinary teams | Non‐punitive culture | Interpersonal factor — Inclusiveness, acknowledgement of mistakes and fallibility, empowerment, respect | Organizational culture outcome— Collaboration, effective teamwork Behavioural outcome— Interpersonal risk behaviour, asking questions, sharing knowledge, effective discussion |
| 56 | Ortega et al. ( ), Spain | To examine the relationship between team learning and performance and team beliefs about the interpersonal context, including psychological safety, task interdependence and potency | Group‐level phenomenon | ‐ | Behavioural outcome— Learning behaviour, reporting errors |
| 57 | Pannick et al. ( ), United Kingdom | To examine the impact of an intervention for identifying clinical challenges and planning to resolve them | Perceptions of the consequences of taking interpersonal risks | ‐ | Behavioural outcome— Speaking‐up behaviour |
| 58 | Pogorzelska‐Maziarz et al. ( ), United States | To examine the validity of a psychometric tool to measure the organizational climate and prevent infections | ‐ | ‐ | ‐ |
| 59 | Prestia et al. ( ), United States | To describe nurses’ experiences with moral distress | ‐ | ‐ | Behavioural outcome– Interpersonal risk behaviour, speaking‐up behaviour |
| 60 | Prottas and Nummelin ( ), United Status | To explore the relationships between the perceptions of a manager's belief in Theory X or Y, psychological safety, organizational citizenship behaviour, quality of care, patient satisfaction and the employing entity | ‐ | ‐ | Organizational culture outcome– Creativity Behavioural outcome– Learning behaviour, sharing knowledge, organizational citizenship behaviour |
| 61 | Raes et al. ( ), Belgium | To explore when and how teams engage in team learning behaviours | ‐ | Interpersonal factor— Leader behaviour, transformational leadership | Organizational culture outcome— Conflict management Behavioural outcome— Interpersonal risk behaviour, learning behaviour |
| 62 | Rahmati and Poormirzaei ( ), Iran | To predict nurses’ psychological safety by considering forgiveness dimensions | Perceptions of the consequences of taking interpersonal risks | Individual factor— Self‐forgiveness | Psychological outcome— Forgiveness Behavioural outcome— Reporting errors, suggesting ideas |
| 63 | Ramana Feeser et al. ( ), United States | To examine the relationship between organizational support and psychological safety and explore the factors associated with the perception of the learning environment | Group‐level phenomenon | Individual factor— Status difference | Organizational culture outcome— Collaboration, creativity Psychological outcome— Engagement in improvement work, commitment, positive emotion Behavioural outcome— Suggesting ideas, asking for help. Feedback behaviour, admitting mistakes |
| 64 | Rathert et al. ( ), United States | To explore a theoretical framework of the work environment for continuous quality improvement and examine the relationships between the work environment, psychological safety, organizational commitment, engagement and patient safety | ‐ | ‐ | Performance outcome— Patient safety, patient‐centred care Psychological outcome— Satisfaction, work engagement, engagement in improvement work, organizational commitment Behavioural outcome— Learning behaviour, fewer workarounds |
| 65 | Richard et al. ( ), Switzerland | To develop a questionnaire to assess speaking‐up behaviour about patient safety | ‐ | ‐ | Psychological outcome— Engagement in learning Behavioural outcome— Speaking‐up behaviour, bringing up concerns, feedback behaviour |
| 66 | Scheepers, et al. ( ), Netherlands | To investigate the relationship between perceptions of psychological safety and the feedback on performance received from peers | ‐ | Interpersonal factor— Peer support, trust | Performance outcome— Safety culture Organizational culture outcome— Trust Psychological outcome— Job satisfaction, engagement in improvement work Behavioural outcome— Learning behaviour, reporting adverse events, bringing up concerns, sharing knowledge, feedback behaviour |
| 67 | Schulze et al. ( ), Switzerland | To develop and evaluate a training programme including an airway algorithm for pulmonologists using non‐anaesthesiologist administered propofol sedation | Perceptions of the consequences of taking interpersonal risks | ‐ | Behavioural outcome— Learning behaviour |
| 68 | Schwappach and Gehring ( ), United States | To examine the impact of practice ownership on the work environment, a climate of learning, psychological safety and burnout | ‐ | ‐ | ‐ |
| 69 | Schwappach and Niederhauser ( ), Switzerland | To examine speaking‐up‐related behaviour and climate for the first time in psychiatric hospitals | ‐ | ‐ | Behavioural outcome— Speaking‐up behaviour |
| 70 | Schwappach and Richard ( ), Switzerland | To examine the frequencies of speaking‐up behaviours and the relationship between safety climate and speaking‐up behaviours and withholding voice behaviours | ‐ | ‐ | Organizational culture outcome— Effective teamwork Behavioural outcome— Speaking‐up behaviour |
| 71 | Schwappach et al. ( ), Austria | To examine the speaking‐up behaviour and psychological safety as a safety climate | ‐ | Individual factor— Status differences among disciplines | Behavioural outcome— Speaking‐up behaviour |
| 72 | Shea et al. ( ), Australia | To examine the associations with workplace type, strategies for occupational violence and aggression, and support after incidents | ‐ | ‐ | Organizational culture outcome— Support |
| 73 | Sholomovich and Magnezi ( ), Israel | To examine the correlation between the psychological safety of an organization's nursing staff and its sense of personal responsibility for avoiding transmission of infections | ‐ | Structure/system factor Support from organization Individual factor— Status differences among disciplines | Performance outcome— Safety culture Behavioural outcome— Interpersonal risk behaviour, learning behaviour, implementation of new practices |
| 74 | Singer et al. ( ), United States | To examine the relationships between learning‐oriented behaviours by managers and quality and safety performance in the interdisciplinary teams | Safe work environment for taking interpersonal risks | ‐ | Organizational culture outcome— Effective work environment Behavioural outcome— Learning behaviour |
| 75 | Smith et al. ( ), United States | To explore the impact of interpersonal and organizational factors on failure to rescue | ‐ | ‐ | Performance outcome— Effective rescue Behavioural outcome— Bringing up concerns e – |
| 76 | Stühlinger et al. ( ), Switzerland | To investigate the mechanisms between shared professional language, quality of care, and job satisfaction and examine the role of psychological safety and relational coordination as mediators | ‐ | Interpersonal factor—Effective relationship, high‐quality communication | Organizational culture outcome— Open atmosphere, conflict management Psychological outcome— Job satisfaction Behavioural outcome— Learning behaviour, speaking‐up behaviour |
| 77 | Swendiman et al. ( ), United States | To describe the personal qualities and teaching methods practised by effective surgical educators | Group‐level phenomenon | ‐ | Performance outcome— Patient safety Psychological outcome— Job satisfaction |
| 78 | Torralba et al. ( ), United States | To explore the facilitators of psychological safety and the impact of psychological safety on satisfaction with the clinical learning environment | ‐ | ‐ | Psychological outcome— Job satisfaction |
| 79 | True et al. ( ), United States | To explore teamwork support factors and their impact on team‐based task delegation | ‐ | ‐ | Behavioural outcome— High‐quality communication |
| 80 | Tucker et al. ( ), United States | To examine the influence of best practice transfer, team learning and process change on the implementation of new practices | ‐ | ‐ | Psychological outcome— Job satisfaction, engagement in improvement work Behavioural outcome— Learning behaviour, less disruptive behaviours |
| 81 | Wakatsuki et al. ( ), United States | To describe residents’ perceptions of behaviours by the best teachers | ‐ | Behavioural outcome— Learning behaviour, asking questions | |
| 82 | Wakeam et al. ( ), United States | To explore the influence of organizational factors, including psychological safety about failure to rescue | ‐ | Structure/system factor— Constant team structure | Performance outcome— Effective rescue Behavioural outcome— High‐quality communication |
| 83 | Wholey et al. ( ), United States | To examine the effect of leadership on interdependence, constructive climate, coordination and improvement initiatives | ‐ | Interpersonal factor— Leadership, inclusiveness | Organizational culture outcome — Coordination Behavioural outcome— Learning behaviour |
| 84 | Wilkens and London ( ), United States | To examine relationships between group climate (learning orientation, psychological safety and self‐disclosure), process (feedback and conflict) and performance | Perceptions of the consequences of taking interpersonal risks, group‐level phenomenon | ‐ | Behavioural outcome— Learning behaviour, speaking‐up behaviour, bringing up concerns, asking for help |
| 85 | Yanchus et al. ( ), United States | To explore employee's perceptions of communication and experiences of psychological safety in the clinical environment | Perceptions of the consequences of taking interpersonal risks | Interpersonal factor— Open communication, honest communication, trust (leader–member) | Behavioural outcome— Speaking‐up behaviour, high‐quality communication |
| 86 | Yanchus et al. ( ), United States | To examine the workplace antecedents of engagement and disengagement and clarify the concepts of engagement and disengagement | ‐ | Interpersonal factor— Effective relationship, teamwork | Organizational culture outcome— Effective interprofessional relationship Psychological outcome— Work engagement |
| 87 | Zhou et al. ( ), China | To explore the differences in perception of safety climate among different departments and job types | ‐ | ‐ | Behavioural outcome— Speaking‐up behaviour |
| 88 | Zuber and Moody ( ), United States | To identify the conditions that allowed nurses to consider behaviours for innovation and change | ‐ | ‐ | Organizational culture outcome— Innovation Behavioural outcome— Interpersonal risk behaviour, speaking‐up behaviour |
Ito, A. , Sato, K. , Yumoto, Y. , Sasaki, M. , & Ogata, Y. (2022). A concept analysis of psychological safety: Further understanding for application to health care . Nursing Open , 9 , 467–489. 10.1002/nop2.1086 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
This work was supported by JSPS KAKENHI, Grant Number JP19H03920
DATA AVAILABILITY STATEMENT
- Agius, S. J. , Willis, S. C. , McArdle, P. J. , & O’Neill, P. A. (2008). Managing change in postgraduate medical education: Still unfreezing? Medical Teacher , 30 ( 4 ), e87–e94. 10.1080/01421590801929976 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Albritton, J. A. , Fried, B. , Singh, K. , Weiner, B. J. , Reeve, B. , & Edwards, J. R. (2019). The role of psychological safety and learning behavior in the development of effective quality improvement teams in Ghana: An observational study . BMC Health Services Research , 19 , 385. 10.1186/s12913-019-4234-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alingh, C. W. , van Wijngaarden, J. D. H. , van de Voorde, K. , Paauwe, J. , & Huijsman, R. (2019). Speaking up about patient safety concerns: The influence of safety management approaches and climate on nurses’ willingness to speak up . BMJ Quality & Safety , 28 ( 1 ), 39–48. 10.1136/bmjqs-2017-007163 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Allaire, Y. , & Firsirotu, M. E. (1984). Theories of organizational culture . Organization Studies , 5 , 193–226. 10.1177/017084068400500301 [ CrossRef ] [ Google Scholar ]
- Appelbaum, N. P. , Dow, A. , Mazmanian, P. E. , Jundt, D. K. , & Appelbaum, E. N. (2016). The effects of power, leadership and psychological safety on resident event reporting . Medical Education , 50 , 343–350. 10.1111/medu.12947 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Appelbaum, N. P. , Santen, S. A. , Aboff, B. M. , Vega, R. , Munoz, J. L. , & Hemphill, R. R. (2018). Psychological safety and support: Assessing resident perceptions of the clinical learning environment . Journal of Graduate Medical Education , 10 ( 6 ), 651–656. 10.4300/JGME-D-18-00286.1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Arnetz, J. , Sudan, S. , Goetz, C. , Counts, S. , & Arnetz, B. (2019). Nurse work environment and stress biomarkers: Possible implications for patient outcomes . Journal of Occupational and Environmental Medicine , 61 , 676–681. 10.1097/JOM.0000000000001642 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baik, D. , & Zierler, B. (2019). Clinical nurses’ experiences and perceptions after the implementation of an interprofessional team intervention: A qualitative study . Journal of Clinical Nursing , 28 ( 3–4 ), 430–443. 10.1111/jocn.14605 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barling, J. , Akers, A. , & Beiko, D. (2018). The impact of positive and negative intraoperative surgeons’ leadership behaviors on surgical team performance . American Journal of Surgery , 215 ( 1 ), 14–18. 10.1016/j.amjsurg.2017.07.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Basit, A. A. (2017). Trust in supervisor and job engagement: Mediating effects of psychological safety and felt obligation . Journal of Psychology , 151 ( 8 ), 701–721. 10.1080/00223980.2017.1372350 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bindels, E. , Verberg, C. , Scherpbier, A. , Heeneman, S. , & Lombarts, K. (2018). Reflection revisited: How physicians conceptualize and experience reflection in professional practice – A qualitative study . BMC Medical Education , 18 ( 1 ), 105. 10.1186/s12909-018-1218-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradley, E. H. , Brewster, A. L. , Fosburgh, H. , Cherlin, E. J. , & Curry, L. A. (2017). Development and psychometric properties of a scale to measure hospital organizational culture for cardiovascular care . Circulation: Cardiovascular Quality and Outcomes , 10 ( 3 ). 10.1161/CIRCOUTCOMES.116.003422 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown, D. , & McCormack, B. G. (2011). Developing the practice context to enable more effective pain management with older people: An action research approach . Implementation Science , 6 , 9. 10.1186/1748-5908-6-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown, D. , & McCormack, B. (2016). Exploring psychological safety as a component of facilitation within the promoting action on research implementation in health services framework . Journal of Clinical Nursing , 25 ( 19–20 ), 2921–2932. 10.1111/jocn.13348 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buljac‐Samardžić, M. , Dekker‐van Doorn, C. , & Van Wijngaarden, J. (2018). Detach yourself: The positive effect of psychological detachment on patient safety in long‐term care . Journal of Patient Safety , 14 , e45‐e46. do: 10.1097/PTS.0000000000000479 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carmeli, A. , & Zisu, M. (2009). The relational underpinnings of quality internal auditing in medical clinics in Israel . Social Science and Medicine , 68 ( 5 ), 894–902. 10.1016/j.socscimed.2008.12.031 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Clark, O. L. , Zickar, M. J. , & Jex, S. M. (2014). Role definition as a moderator of the relationship between safety climate and organizational citizenship behavior among hospital nurses . Journal of Business and Psychology , 29 ( 1 ), 101–110. 10.1007/s10869-013-9302-0 [ CrossRef ] [ Google Scholar ]
- Colet, P. C. , Cruz, J. P. , Cacho, G. , Al‐Qubeilat, H. , Soriano, S. S. , & Cruz, C. P. (2018). Perceived infection prevention climate and its predictors among nurses in Saudi Arabia . Journal of Nursing Scholarship , 50 ( 2 ), 134–142. 10.1111/jnu.12360 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cuellar, A. , Krist, A. H. , Nichols, L. M. , & Kuzel, A. J. (2018). Effect of practice ownership on work environment, learning culture, psychological safety, and burnout . The Annals of Family Medicine , 16 ( Suppl 1 ), S44–S51. 10.1370/afm.2198 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Curry, L. A. , Brault, M. A. , Linnander, E. L. , McNatt, Z. , Brewster, A. L. , Cherlin, E. , Flieger, S. P. , Ting, H. H. , & Bradley, E. H. (2018). Influencing organisational culture to improve hospital performance in care of patients with acute myocardial infarction: A mixed‐methods intervention study . BMJ Quality & Safety , 27 ( 3 ), 207–217. 10.1136/bmjqs-2017-006989 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Curşeu, P. L. (2013). Demographic diversity, communication and learning behaviour in healthcare groups . The International Journal of Health Planning and Management , 28 ( 3 ), 238–247. 10.1002/hpm.2130 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- De Brún, A. , & McAuliffe, E. (2020). Identifying the context, mechanisms and outcomes underlying collective leadership in teams: Building a realist programme theory . BMC Health Services Research , 20 ( 1 ), 261. 10.1186/s12913-020-05129-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Derickson, R. , Fishman, J. , Osatuke, K. , Teclaw, R. , & Ramsel, D. (2015). Psychological safety and error reporting within veterans health administration hospitals . Journal of Patient Safety , 11 , 60–66. 10.1097/PTS.0000000000000082 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Edmondson, A. (1999). Psychological safety and learning behavior in work teams . Administrative Science Quarterly , 44 , 350–383. 10.2307/2666999 [ CrossRef ] [ Google Scholar ]
- Edmondson, A. C. (2019). The fearless organization: Creating psychological safety in the workplace for learning, innovation, and growth . Wiley. [ Google Scholar ]
- Edmondson, A. C. , Bohmer, R. M. , & Pisano, G. P. (2001). Disrupted routines: Team learning and new technology implementation in hospitals . Administrative Science Quarterly , 46 ( 4 ), 685–716. 10.2307/3094828 [ CrossRef ] [ Google Scholar ]
- Edmondson, A. C. , Higgins, M. , Singer, S. , & Weiner, J. (2016). Understanding psychological safety in health care and education organizations: A comparative perspective . Research in Human Development , 13 , 65–83. 10.1080/15427609.2016.1141280 [ CrossRef ] [ Google Scholar ]
- Erichsen Andersson, A. , Frödin, M. , Dellenborg, L. , Wallin, L. , Hök, J. , Gillespie, B. M. , & Wikström, E. (2018). Iterative co‐creation for improved hand hygiene and aseptic techniques in the operating room: Experiences from the safe hands study . BMC Health Services Research , 18 ( 1 ), 2. 10.1186/s12913-017-2783-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- George, J. , Elwy, A. R. , Charns, M. P. , Maguire, E. M. , Baker, E. , Burgess, J. F. Jr , & Meterko, M. (2020). Exploring the association between organizational culture and large‐scale adverse events: Evidence from the Veterans Health Administration . The Joint Commission Journal on Quality and Patient Safety , 46 ( 5 ), 270–281. 10.1016/j.jcjq.2020.02.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- George, J. , Parker, V. A. , Sullivan, J. L. , Greenan, M. A. , Chan, J. , Shin, M. H. , Chen, Q. , Shwartz, M. , & Rosen, A. K. (2020). How hospitals select their patient safety priorities: An exploratory study of four Veterans Health Administration hospitals . Health Care Management Review , 45 ( 4 ), E56–E67. 10.1097/HMR.0000000000000260 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gilmartin, H. , Lawrence, E. , Leonard, C. , McCreight, M. , Kelley, L. , Lippmann, B. , Coy, A. , & Burke, R. E. (2019). Brainwriting premortem: A novel focus group method to engage stakeholders and identify preimplementation barriers . Journal of Nursing Care Quality , 34 ( 2 ), 94–100. 10.1097/NCQ.0000000000000360 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gilmartin, H. M. , Langner, P. , Gokhale, M. , Osatuke, K. , Hasselbeck, R. , Maddox, T. M. , & Battaglia, C. (2018). Relationship between psychological safety and reporting nonadherence to a safety checklist . Journal of Nursing Care Quality , 33 ( 1 ), 53–60. 10.1097/NCQ.0000000000000265 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gong, Z. , Van Swol, L. , Xu, Z. , Yin, K. , Zhang, N. , Gul Gilal, F. , & Li, X. (2019). High‐power distance is not always bad: Ethical leadership results in feedback seeking . Frontiers in Psychology , 10 , 2137. 10.3389/fpsyg.2019.02137 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Grant, A. M. , Berg, J. M. , & Cable, D. M. (2014). Job titles as identity badges: How self‐reflective titles can reduce emotional exhaustion . Academy of Management Journal , 57 ( 4 ), 1201–1225. 10.5465/amj.2012.0338 [ CrossRef ] [ Google Scholar ]
- Greene, M. T. , Gilmartin, H. M. , & Saint, S. (2020). Psychological safety and infection prevention practices: Results from a national survey . American Journal of Infection Control , 48 , 2–6. 10.1111/j.1365-2648.2011.05619.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Halbesleben, J. R. B. , Leroy, H. , Dierynck, B. , Simons, T. , Savage, G. T. , McCaughey, D. , & Leon, M. R. (2013). Living up to safety values in health care: The effect of leader behavioral integrity on occupational safety . Journal of Occupational Health Psychology , 18 ( 4 ), 395–405. 10.1037/a0034086 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Halbesleben, J. R. , & Rathert, C. (2008). The role of continuous quality improvement and psychological safety in predicting work‐arounds . Health Care Management Review , 33 , 134–144. 10.1097/01.HMR.0000304505.04932.62 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hesselgreaves, H. , & MacVicar, R. (2012). Practice‐based small group learning in GP specialty training . Education for Primary Care , 23 ( 1 ), 27–33. 10.1080/14739879.2012.11494067 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hirak, R. , Peng, A. C. , Carmeli, A. , & Schaubroeck, J. M. (2012). Linking leader inclusiveness to work unit performance: The importance of psychological safety and learning from failures . Leadership Quarterly , 23 , 107–117. 10.1016/j.leaqua.2011.11.009 [ CrossRef ] [ Google Scholar ]
- Huddleston, P. , & Gray, J. (2016). Describing nurse leaders’ and direct care nurses’ perceptions of a healthy work environment in acute care settings, Part 2 . JONA: The Journal of Nursing Administration , 46 ( 9 ), 462–467. 10.1097/NNA.0000000000000376 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jain, A. K. , Fennell, M. L. , Chagpar, A. B. , Connolly, H. K. , & Nembhard, I. M. (2016). Moving toward improved teamwork in cancer care: The role of psychological safety in team communication . Journal of Oncology Practice , 12 ( 11 ), 1000–1011. [ PubMed ] [ Google Scholar ]
- Kahn, W. A. (1990). Psychological conditions of personal engagement and disengagement at work . Academy of Management Journal , 33 , 692–724. 10.2307/256287 [ CrossRef ] [ Google Scholar ]
- Kang, J. Y. , Lee, M. K. , Fairchild, E. M. , Caubet, S. L. , Peters, D. E. , Beliles, G. R. , & Matti, L. K. (2020). Relationships among organizational values, employee engagement, and patient satisfaction in an Academic Medical Center . Mayo Clinic Proceedings: Innovations, Quality & Outcomes , 4 ( 1 ), 8–20. 10.1016/j.mayocpiqo.2019.08.001 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Keitz, S. A. , Aron, D. C. , Brannen, J. L. , Byrne, J. M. , Cannon, G. W. , Clarke, C. T. , Gilman, S. C. , Hettler, D. L. , Kaminetzky, C. P. , Zeiss, R. A. , Bernett, D. S. , Wicker, A. B. , & Kashner, T. M. (2019). Impact of clinical training on recruiting graduating health professionals . The American Journal of Managed Care , 25 ( 4 ), e111–e118. [ PubMed ] [ Google Scholar ]
- Kessel, M. , Kratzer, J. , & Schultz, C. (2012). Psychological safety, knowledge sharing, and creative performance in healthcare teams . Creativity and Innovation Management , 21 ( 2 ), 147–157. 10.1111/j.1467-8691.2012.00635.x [ CrossRef ] [ Google Scholar ]
- Klingberg, K. , Gadelhak, K. , Jegerlehner, S. N. , Brown, A. D. , Exadaktylos, A. K. , & Srivastava, D. S. (2018). Bad manners in the Emergency Department: Incivility among doctors . PLoS One , 13 ( 3 ), e0194933. 10.1371/journal.pone.0194933 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kolbe, M. , Weiss, M. , Grote, G. , Knauth, A. , Dambach, M. , Spahn, D. R. , & Grande, B. (2013). TeamGAINS: A tool for structured debriefings for simulation‐based team trainings . BMJ Quality & Safety , 22 ( 7 ), 541–553. 10.1136/bmjqs-2012-000917 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lazzara, E. H. , Benishek, L. E. , Patzer, B. , Gregory, M. E. , Hughes, A. M. , Heyne, K. , Salas, E. , Kuchkarian, F. , Marttos, A. , & Schulman, C. (2015). Utilizing telemedicine in the trauma Intensive Care Unit: Does it impact teamwork? Telemedicine and e‐Health , 21 ( 8 ), 670–676. 10.1089/tmj.2014.0074 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee, Y.‐H. , Yang, C.‐C. , & Chen, T.‐T. (2016). Barriers to incident‐reporting behavior among nursing staff: A study based on the theory of planned behavior . Journal of Management and Organization , 22 , 1–18. 10.1017/jmo.2015.8 [ CrossRef ] [ Google Scholar ]
- Leroy, H. , Dierynck, B. , Anseel, F. , Simons, T. , Halbesleben, J. R. , McCaughey, D. , Savage, G. T. , & Sels, L. (2012). Behavioral integrity for safety, priority of safety, psychological safety, and patient safety: A team‐level study . Journal of Applied Psychology , 97 ( 6 ), 1273–1281. 10.1037/a0030076 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leventhal, G. S. (1980). What should be done with equity theory? New approaches to the study of fairness in social relationships. In Gergen K., & Willis R. (Eds.), Social exchange: Advances in theory and research (pp. 167–218). Plenum Press. 10.1007/978-1-4613-3087-5_2 [ CrossRef ] [ Google Scholar ]
- Lyman, B. , Ethington, K. M. , King, C. , Jacobs, J. D. , & Lundeen, H. (2017). Organizational learning in a cardiac intensive care unit: A learning history . Dimensions of Critical Care Nursing , 36 ( 2 ), 78–86. 10.1097/DCC.0000000000000233 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lyman, B. , Shaw, L. , & Moore, C. (2017). Organizational learning in an orthopaedic unit: A learning history . Orthopaedic Nursing , 36 ( 6 ), 424–431. 10.1097/NOR.0000000000000403 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lyman, B. , Gunn, M. M. , & Mendon, C. R. (2020). New graduate registered nurses’ experiences with psychological safety . Journal of Nursing Management , 28 ( 4 ), 831–839. 10.1111/jonm.13006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- MacCurtain, S. , Murphy, C. , O’Sullivan, M. , MacMahon, J. , & Turner, T. (2018). To stand back or step in? Exploring the responses of employees who observe workplace bullying . Nursing Inquiry , 25 , e12207. 10.1111/nin.12207 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Martland, J. , Chamberlain, D. , Hutton, A. , & Smigielski, M. (2016). Communication and general concern criterion prior to activation of the rapid response team: A grounded theory . Australian Health Review , 40 ( 5 ), 477–483. 10.1071/AH15123 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Meleis, A. I. (2017). Theoretical nursing: Development and progress , 6th ed. Lippincott Williams & Wilkins. [ Google Scholar ]
- Nembhard, I. M. , & Edmondson, A. C. (2006). Making it safe: The effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams . Journal of Organizational Behavior , 27 , 941–966. 10.1002/job.413 [ CrossRef ] [ Google Scholar ]
- Newman, A. , Donohue, R. , & Eva, N. (2017). Psychological safety: A systematic review of the literature . Human Resource Management Review , 27 , 521–535. 10.1016/j.hrmr.2017.01.001 [ CrossRef ] [ Google Scholar ]
- Noah, Y. , & Steve, M. (2012). Work environment and job attitude among employees in a Nigerian work organization . Journal of Sustainable Society , 1 , 36–43. 10.11634/21682585140398 [ CrossRef ] [ Google Scholar ]
- O’Donovan, R. , Van Dun, D. , & McAuliffe, E. (2020). Measuring psychological safety in healthcare teams: Developing an observational measure to complement survey methods . BMC Medical Research Methodology , 20 , 203. 10.1186/s12874-020-01066-z [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O'Leary, D. F. (2016). Exploring the importance of team psychological safety in the development of two interprofessional teams . Journal of Interprofessional Care , 30 , 29–34. 10.3109/13561820.2015.1072142 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Organisation for Economic Co‐operation and Development (2017). The economics of patient safety in primary and ambulatory care: Flying blind. Retrieved from The‐Economics‐of‐Patient‐Safety‐in‐Primary‐and‐Ambulatory‐Care‐April2018.pdf (oecd.org).
- Ortega, A. , Sánchez‐Manzanares, M. , Gil, F. , & Rico, R. (2013). Enhancing team learning in nursing teams through beliefs about interpersonal context . Journal of Advanced Nursing , 69 ( 1 ), 102–111. 10.1111/j.1365-2648.2012.05996.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pannick, S. , Archer, S. , Johnston, M. J. , Beveridge, I. , Long, S. J. , Athanasiou, T. , & Sevdalis, N. (2017). Translating concerns into action: A detailed qualitative evaluation of an interdisciplinary intervention on medical wards . British Medical Journal Open , 7 ( 4 ), e014401. 10.1136/bmjopen-2016-014401 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pogorzelska‐Maziarz, M. , Nembhard, I. M. , Schnall, R. , Nelson, S. , & Stone, P. W. (2016). Psychometric evaluation of an instrument for measuring organizational climate for quality: Evidence from a national sample of infection preventionists . American Journal of Medical Quality , 31 ( 5 ), 441–447. 10.1177/1062860615587322 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Premeaux, S. F. , & Bedeian, A. G. (2003). Breaking the silence: The moderating effects of self‐monitoring in predicting speaking up in the workplace . Journal of Management Studies , 40 , 1537–1562. 10.1111/1467-6486.00390 [ CrossRef ] [ Google Scholar ]
- Prestia, A. S. , Sherman, R. O. , & Demezier, C. (2017). Chief nursing officers’ experiences with moral distress . JONA: The Journal of Nursing Administration , 47 ( 2 ), 101–107. 10.1097/NNA.0000000000000447 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prottas, D. J. , & Nummelin, M. R. (2018). Theory X/Y in the health care setting: Employee perceptions, attitudes, and behaviors . The Health Care Manager , 37 ( 2 ), 109–117. 10.1097/HCM.0000000000000210 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Raes, E. , Decuyper, S. , Lismont, B. , Van den Bossche, P. , Kyndt, E. , Demeyere, S. , & Dochy, F. (2013). Facilitating team learning through transformational leadership . Instructional Science , 41 , 287–305. 10.1007/s11251-012-9228-3 [ CrossRef ] [ Google Scholar ]
- Rahmati, A. , & Poormirzaei, M. (2018). Predicting nurses’ psychological safety based on the forgiveness skill . Iranian Journal of Nursing and Midwifery Research , 23 ( 1 ), 40–44. 10.4103/ijnmr.IJNMR_240_16 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ramana Feeser, V. , Zemore, Z. , Appelbaum, N. , Santen, S. A. , Moll, J. , Aboff, B. , & Hemphill, R. R. (2019). Analysis of the emergency medicine clinical learning environment . AEM Education and Training , 3 ( 3 ), 286–290. 10.1002/aet2.10356 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rathert, C. , Ishqaidef, G. , & May, D. R. (2009). Improving work environments in health care: Test of a theoretical framework . Health Care Management Review , 34 , 334–343. 10.1097/HMR.0b013e3181abce2b [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Richard, A. , Pfeiffer, Y. , & Schwappach, D. (2017). Development and psychometric evaluation of the speaking up about patient safety questionnaire . Journal of Patient Safety. Advance Online Publication , 10.1097/PTS.0000000000000415 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rodgers, B. L. (2000). Concept analysis: An evolutionary view. In Rodgers B. L., & Knafl K. A. (Eds.), Concept development in nursing: Foundations, techniques, and applications , 2nd ed. (pp. 77–102). W. B. Saunders. [ Google Scholar ]
- Scheepers, R. A. , van den Goor, M. , Arah, O. A. , Heineman, M. J. , & Lombarts, K. M. J. M. H. (2018). Physicians’ perceptions of psychological safety and peer performance feedback . Journal of Continuing Education in the Health Professions , 38 ( 4 ), 250–254. 10.1097/CEH.0000000000000225 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwappach, D. L. B. , & Gehring, K. (2015). Frequency of and predictors for withholding patient safety concerns among oncology staff: A survey study . European Journal of Cancer Care , 24 ( 3 ), 395–403. 10.1111/ecc.12255 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwappach, D. L. B. , & Niederhauser, A. (2019). Speaking up about patient safety in psychiatric hospitals – A cross‐sectional survey study among healthcare staff . International Journal of Mental Health Nursing , 28 ( 6 ), 1363–1373. 10.1111/inm.12664 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwappach, D. , & Richard, A. (2018). Speak up‐related climate and its association with healthcare workers’ speaking up and withholding voice behaviours: A cross‐sectional survey in Switzerland . BMJ Quality & Safety , 27 ( 10 ), 827–835. 10.1136/bmjqs-2017-007388 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwappach, D. , Sendlhofer, G. , Häsler, L. , Gombotz, V. , Leitgeb, K. , Hoffmann, M. , Jantscher, L. , & Brunner, G. (2018). Speaking up behaviors and safety climate in an Austrian university hospital . International Journal for Quality in Health Care , 30 ( 9 ), 701–707. 10.1093/intqhc/mzy089 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schulze, M. , Grande, B. , Kolbe, M. , Kriech, S. , Nöthiger, C. B. , Kohler, M. , Spahn, D. R. , & Franzen, D. (2016). SafAIRway: An airway training for pulmonologists performing a flexible bronchoscopy with nonanesthesiologist administered propofol sedation: A prospective evaluation . Medicine , 95 ( 23 ), e3849. 10.1097/MD.0000000000003849 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shea, T. , Cooper, B. , De Cieri, H. , Sheehan, C. , Donohue, R. , & Lindsay, S. (2018). Postincident support for healthcare workers experiencing occupational violence and aggression . Journal of Nursing Scholarship , 50 ( 4 ), 344–352. 10.1111/jnu.12391 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sholomovich, L. , & Magnezi, R. (2017). Tell me how pleased you are with your workplace, and I will tell you how often you wash your hands . American Journal of Infection Control , 45 ( 6 ), 677–681. 10.1016/j.ajic.2016.12.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Simons, T. (2002). Behavioral integrity: The perceived alignment between managers’ words and deeds as a research focus . Organization Science , 13 , 18–35. 10.1287/orsc.13.1.18.543 [ CrossRef ] [ Google Scholar ]
- Singer, S. J. , Hayes, J. E. , Gray, G. C. , & Kiang, M. V. (2015). Making time for learning‐oriented leadership in multidisciplinary hospital management groups . Health Care Management Review , 40 , 300–312. 10.1097/HMR.0000000000000037 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith, M. E. , Wells, E. E. , Friese, C. R. , Krein, S. L. , & Ghaferi, A. A. (2018). Interpersonal and organizational dynamics are key drivers of failure to rescue . Health Affairs , 37 ( 11 ), 1870–1876. 10.1377/hlthaff.2018.0704 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stühlinger, M. , Schmutz, J. B. , & Grote, G. (2019). I hear you, but do I understand? The relationship of a shared professional language with quality of care and job satisfaction . Frontiers in Psychology , 10 , 1310. 10.3389/fpsyg.2019.01310 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Swendiman, R. A. , Hoffman, D. I. , Bruce, A. N. , Blinman, T. A. , Nance, M. L. , & Chou, C. M. (2019). Qualities and methods of highly effective surgical educators: A grounded theory model . Journal of Surgical Education , 76 ( 5 ), 1293–1302. 10.1016/j.jsurg.2019.02.011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Torralba, K. D. , Loo, L. K. , Byrne, J. M. , Baz, S. , Cannon, G. W. , Keitz, S. A. , Wicker, A. B. , Henley, S. S. , & Kashner, T. M. (2016). Does psychological safety impact the clinical learning environment for resident physicians? Results from the VA’s learners’ perceptions survey . Journal of Graduate Medical Education , 8 ( 5 ), 699–707. 10.4300/JGME-D-15-00719.1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- True, G. , Stewart, G. L. , Lampman, M. , Pelak, M. , & Solimeo, S. L. (2014). Teamwork and delegation in medical homes: Primary care staff perspectives in the Veterans Health Administration . Journal of General Internal Medicine , 29 ( Suppl 2 ), S632–S639. 10.1007/s11606-013-2666-z [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tucker, A. L. , Nembhard, I. M. , & Edmondson, A. C. (2007). Implementing new practices: An empirical study of organizational learning in hospital intensive care units . Management Science , 53 , 894–907. 10.1287/mnsc.1060.0692 [ CrossRef ] [ Google Scholar ]
- Wakatsuki, S. , Tanaka, P. , Vinagre, R. , Marty, A. , Thomsen, J. L. D. L. , & Macario, A. (2018). What makes for good anesthesia teaching by faculty in the operating room? The Perspective of Anesthesiology Residents . Cureus , 10 ( 5 ), e2563. 10.7759/cureus.2563 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wakeam, E. , Hyder, J. A. , Ashley, S. W. , & Weissman, J. S. (2014). Barriers and strategies for effective patient rescue: A qualitative study of outliers . The Joint Commission Journal on Quality and Patient Safety , 40 ( 11 ), 503–506. [ PubMed ] [ Google Scholar ]
- Wholey, D. R. , Disch, J. , White, K. M. , Powell, A. , Rector, T. S. , Sahay, A. , & Heidenreich, P. A. (2014). Differential effects of professional leaders on health care teams in chronic disease management groups . Health Care Management Review , 39 ( 3 ), 186–197. 10.1097/HMR.0b013e3182993b7f [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wilkens, R. , & London, M. (2006). Relationships between climate, process, and performance in continuous quality improvement groups . Journal of Vocational Behavior , 69 ( 3 ), 510–523. 10.1016/j.jvb.2006.05.005 [ CrossRef ] [ Google Scholar ]
- World Health Organization (2019). Patient safety: Global action on patient safety. Retrieved from https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_26‐en.pdf
- Yanchus, N. J. , Derickson, R. , Moore, S. C. , Bologna, D. , & Osatuke, K. (2014). Communication and psychological safety in veterans health administration work environments . Journal of Health Organization and Management , 28 ( 6 ), 754–776. 10.1108/JHOM-12-2012-0241 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yanchus, N. J. , Carameli, K. A. , Ramsel, D. , & Osatuke, K. (2020). How to make a job more than just a paycheck: Understanding physician disengagement . Health Care Management Review , 45 ( 3 ), 245–254. 10.1097/HMR.0000000000000218 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhou, P. , Bai, F. , Tang, H. Q. , Bai, J. , Li, M. Q. , & Xue, D. (2018). Patient safety climate in general public hospitals in China: Differences associated with department and job type based on a cross‐sectional survey . British Medical Journal Open , 8 ( 4 ), e015604. 10.1136/bmjopen-2016-015604 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zuber, C. D. , & Moody, L. (2018). Creativity and innovation in health care . Nursing Administration Quarterly , 42 ( 1 ), 62–75. 10.1097/NAQ.0000000000000267 [ PubMed ] [ CrossRef ] [ Google Scholar ]

What is psychological safety at work? Here’s how to start creating it
The term refers to your ability to freely express your opinions at work without fear
- Healthy Workplaces
- Managing Human Capital
- Mental Health

Have you ever questioned your boss’s decisions in your own mind, but felt it was safer to just not say anything out loud? Unfortunately, far too many workplaces have a culture where that sentiment is common. It can result in mistakes that should have been prevented, lost opportunities, and an overall lack of new and original ideas. The antidote is to build a psychologically safe workplace, which can make an incredible impact on teams reaching their goals (Edmondson & Bransby, 2023).
“Psychological safety” has become a catchphrase. Those unfamiliar with the term often think about protecting workers’ mental health or protecting workers from psychological harm to ensure a psychologically healthy workplace, just as “physical safety” means protecting workers’ bodily health. But psychological safety is one component of a psychologically healthy workplace. It is a specific, targeted concept critical for innovation and success.
What this looks like
Psychological safety develops over time. When it exists, members of a team can be themselves, and they share the belief they can take appropriate risks, and they can and should:
- admit and discuss mistakes,
- openly address problems and tough issues,
- seek help and feedback,
- trust that no one on the team is out to get them, and
- trust that they are a valued member of the team.
For example, when an employee makes the decision to pose difficult questions to their boss about a tough issue, there is a risk the questions may be misperceived as a personal attack or as unproductive, which depending on the leader and the team could put the worker’s job or reputation in jeopardy.
Amy Edmondson, PhD, the Novartis professor of leadership and management at the Harvard Business School and author of The Fearless Organization: Creating Psychological Safety in the Workplace for Learning, Innovation, and Growth , says, “Leaders must prioritize a culture of learning and innovation for team members to be comfortable speaking up, taking risks, and sharing information. This does not happen by default. It emerges with effort and curiosity and care. When achieved, the result is a more creative, innovative, and successful team and organization.”
Is your workplace psychologically safe?
You can measure where your team stands by asking them the following questions in an anonymous survey:
- If you make a mistake on this team, will it be held against you?
- Are the members of this team able to bring up problems and tough issues?
- Do members on this team sometimes reject other members for being different?
- Is it safe to take a risk on this team?
- Is it difficult to ask other members of this team for help?
- Would anyone on the team deliberately act in a way that undermines efforts?
- Working with members of this team, are unique skills and talents valued and utilized?
Robert Sutton, PhD Stanford professor, organizational psychologist, and co-author of The Friction Project: How Smart Leaders Make the Right Things Easier and the Wrong Things Harder , says “A good test is, who are the stars in your workplace? Are they the people who stifle, frighten, and blame their colleagues? Or do they promote learning and drive out fear by talking openly about their own mistakes and gently but candidly pointing out others’ failures and mistakes, and talking about what we can all learn together from such troubles? When people talk about their own mistakes, rather than point out others' missteps, that suggests your workplace is psychologically safe."
What you can do to build psychological safety
Here are some great examples to begin building this culture:
Leaders can
- Celebrate learning from mistakes and build “lessons learned” debriefing sessions into every project.
- Lead by example to show how to raise problems and tough issues for discussion in a constructive, nonjudgmental manner.
- Encourage all team members to raise problems or tough issues that may be on their minds.
- Applaud thoughtful risk taking and demonstrate it yourself.
- Publicly recognize and celebrate the unique skills and talents brought by each member of the teams you lead.
Organizations can
- Train leaders and managers on concrete steps for fostering psychological safety.
- Examine the organization to see if there are unnecessary hierarchies, chains-of-command, or professional boundaries that discourage communication from front-line workers to upper management.
- Provide ways to recognize and celebrate employees’ unique skills and talents in organization-wide communications.
- Repeatedly emphasize that the organization will not tolerate any employee deliberately undermining the efforts of another employee.
Employees can
- Focus on finding solutions with questions like “what can we all do to help solve this problem?”
- Ask others for their opinions—with questions like “I’d love to get your feedback on that idea.”
- Actively listen to the ideas shared by your colleagues and ask respectful questions.
- Extend kindness and respect when team members share ideas even if you disagree with them.
- Provide feedback in a respectful, thoughtful way.
Beth M. Schwartz, PhD, associate director in the Office of Applied Psychology at APA, noted “Through psychological safety we can find out what each member of a team has to offer. It allows us to learn what smart and talented team members really bring to the table, and ultimately, leads to more productive organizations.”
Much more can be found in Edmondson’s many publications, including her two books The Fearless Organization and Right Kind of Wrong .
Edmondson, A. C. (2023). Right kind of wrong: The science of failing well. Atria Books.
Edmondson, A. C., & Bransby, D. P. (2023). Psychological safety comes of age: Observed themes in an established literature. Annual Review of Organizational Psychology and Organizational Behavior , 10(1), 55–78. https://doi.org/10.1146/annurev-orgpsych-120920-055217
Edmondson, A. C. (2018). The fearless organization: Creating psychological safety in the workplace for learning, innovation, and growth . John Wiley & Sons.
Ferrère, A., Rider, C., Renerte, B., & Edmondson, A. C. (2022). Fostering ethical conduct through psychological safety. MIT Sloan Management Review , 63 (4), 39-43.
Newman, A., Donohue, R., & Eva, N. (2017). Psychological safety: A systematic review of the literature. Human Resource Management Review , 27 (3), 521-535. https://doi.org/10.1016/j.hrmr.2017.01.001
Stomski, L., & Jensen, K. (2021). Building learning agility through psychological safety. In V. S. Harvey & K. P. De Meuse (Eds.), The age of agility: Building learning agile leaders and organizations (pp. 365–381). Society for Industrial and Organizational Psychology; Oxford University Press. https://doi.org/10.1093/oso/9780190085353.003.0015
Sutton, R. I., & Rao, H. (2024). The fiction project: How smart leaders make the right things easier and the wrong things harder . St. Martine’s Press.
Recommended Reading
Related topics.
- Healthy workplaces
- These organizations make mental health a priority
- 5 ways to improve employee mental health
- How to combat toxic workplaces
You may also like
What Is Psychological Safety?
by Amy Gallo

Summary .
What exactly is psychological safety? It’s a term that’s used a lot but is often misunderstood. In this piece, the author answers the following questions with input from Harvard Business School professor Amy Edmondson, who coined the phrase “team psychological safety”: 1) What is psychological safety? 2) Why is psychological safety important? 3) How has the idea evolved? 4) How do you know if your team has it? 5) How do you create psychological safety? 6) What are common misconceptions?
No one likes to deliver bad news to their boss. But that’s exactly what I had to do when a project I’d been working on wasn’t delivering the results we expected. I’d been a big advocate for our team taking on the initiative and, personally, I’d invested a lot of time into it — and convinced others to do the same.
Partner Center

IMAGES
VIDEO
COMMENTS
Our review of the literature led to a number of key observations. As can be seen in Fig. 1, although psychological safety is a multilevel construct, our review suggests that it is likely to be more potent and meaningful at the team level, as opposed to the organizational level, unless the organization is small.This may be the reason why few studies have been conducted at the organizational level.
Since the concept of psychological safety was introduced, empirical research on its antecedents, outcomes, and moderators at different levels of analysis has proliferated. Given a burgeoning body of empirical evidence, a systematic review of the psychological safety literature is warranted. As well as reviewing empirical work on psychological safety, the present article highlights gaps in the ...
Since its renaissance in the 1990s, psychological safety research has flourished—a boom motivated by recognition of the challenge of navigating uncertainty and change. Today, its theoretical and practical significance is amplified by the increasingly complex and interdependent nature of the work in organizations. Conceptual and empirical research on psychological safety—a state of reduced ...
To conclude, we believe that psychological safety is important given it is a key cognitive state that allows learning processes to occur, and contributes to improved work outcomes at different levels of analysis (Edmondson, 1999, Edmondson et al., 2007). From a practical perspective, this review has highlighted the myriad of positive workplace ...
Given a burgeoning body of empirical evidence, a systematic review of the psychological safety literature is warranted. As well as reviewing empirical work on psychological safety, the present article highlights gaps in the literature and provides direction for future work. In doing so, it highlights the need to advance our understanding of ...
Psychological safety has emerged as a critical feature of high-performing teams across many industries, including health care. It facilitates patient safety, quality improvement, learning, and innovation. This review presents an overview of psychological safety in medicine, describing its impact on learning, patient safety, and quality improvement.
Since high psychological safety is a promotor of good communication within teams (allowing those with differing aims and working practices to communicate and work together successfully ), the benefit of this review lies in its potential to further understand how psychological safety has been explored within the clinical literature, looking at ...
First, we compare effect sizes to determine the relative effectiveness of antecedents to psychological safety. Second, we examine the extent to which psychological safety influences both task performance and organizational citizenship behaviors over and beyond related concepts such as positive leader relations and work engagement.
Newman et al. (2017) who systematically reviewed the psychological safety literature argue that it is often determined based on the assessment of external factors, such as social environment ...
Although psychological safety research has flourished in recent years, and despite the empirical support for the important role of psychological safety in the workplace, several critical questions remain. In order to address these questions, we aggregate theoretical and empirical works, and draw on 136 independent samples representing over 22,000 individuals and nearly 5,000 groups, to conduct ...
This systematic review of psychological safety literature identifies a list of enablers of psychological safety within healthcare teams. This list can be used as a first step in developing observational measures and interventions to improve psychological safety in healthcare teams. Psychological safety, Enablers, Healthcare teams.
The findings of the study present important contributions to the present knowledge in the domain. First, the research contributes to psychological safety literature by unfolding its little-known relationship with TE, answering the theoretical call from Abror (2017) to examine the relationship between the two constructs. As discussed, we found a ...
Psychological safety has emerged as a critical feature of high-performing teams across many industries, including health care. It facilitates patient safety, quality improvement, learning, and innovation. This review presents an overview of psychological safety in medicine, describing its impact on learning, patient safety, and quality improvement.
Psychological safety describes people's perceptions of the consequences of taking interpersonal risks in a particular context such as a workplace. First explored by pioneering organizational scholars in the 1960s, psychological safety experienced a renaissance starting in the 1990s and continuing to the present. Organizational research has identified psychological safety as a critical factor ...
However, the seven-item measure reflecting a narrow definition of psychological safety may not capture the entire content domain and may not represent more recent developments in the psychological safety research literature (Liu et al., n.d.). Assessments of psychological safety as a unidimensional construct may also limit potential ...
Conceptual and empirical research on psychological safety—a state of reduced interpersonal risk—is thus timely, relevant, and extensive. In this article, we review contemporary psychological safety research by describing its various content areas, assessing what has been learned in recent years, and suggesting directions for future research.
Purpose: The current systematic review will identify enablers of psychological safety within the literature in order to produce a comprehensive list of factors that enable psychological safety specific to healthcare teams. Data sources: A keyword search strategy was developed and used to search the following electronic databases PsycINFO, ABI/INFORM, Academic search complete and PubMed and ...
Psychological safety (PS) is defined as a team-level belief that members will not be punished or humiliated for speaking up with new ideas, ... Literature review and research aims Psychological safety and interdisciplinary learning. For interdisciplinary teams working on complex problems, PS is vital to the productive exchange of knowledge ...
Conceptual and empirical research on psychological safety—a state of reduced interpersonal risk—is thus timely, relevant, and extensive. In this article, we review contemporary psychological safety research by describing its various content areas, assessing what has been learned in recent years, and suggesting directions for future research.
This led to the identification of 83 articles for inclusion in our review, 78 of which were empirical studies. 3. A review of the psychological safety literature 3.1. Defining and measuring psychological safety The construct of psychological safety is grounded in the seminal work conducted by Schein and Bennis (1965) on organizational change. ...
Background Having psychologically safe teams can improve learning, creativity and performance within organisations. Within a healthcare context, psychological safety supports patient safety by enabling engagement in quality improvement and encouraging staff to speak up about errors. Despite the low levels of psychological safety in healthcare teams and the important role it plays in supporting ...
Articles that met the following inclusion criteria were selected: (1) focused on concepts of psychological safety, (2) conducted in health care, (3) employees completed a survey, (4) were not literature review articles, (5) was an empirical study, (6) not duplicated among databases and (7) other reasons, such as written in English and Japanese ...
Introduction While the concept of psychological safety has been gaining momentum, research concerning psychological safety in inpatient mental health wards is lacking. ... both researchers felt that data saturation was reached at this point. All authors contributed to the final review of themes. Where a finding was supported by two quotations ...
What this looks like. Psychological safety develops over time. When it exists, members of a team can be themselves, and they share the belief they can take appropriate risks, and they can and should: admit and discuss mistakes, openly address problems and tough issues, seek help and feedback, trust that no one on the team is out to get them, and.
A culture of trust and belonging doesn't just happen. Here's how you make one. Summary. What exactly is psychological safety? It's a term that's used a lot but is often misunderstood. In ...
Psychology has traditionally neglected the specific needs of rural communities. This chapter reviews the situation of psychology in rural areas and discusses the need for a rural psychology. An open Internet review using Google search engine and "rural psychology" as key word was conducted, as well as an academic literature review. Results show that psychology tends to be framed in urban ...