- Research article
- Open access
- Published: 26 February 2018

The use of advanced medical technologies at home: a systematic review of the literature
- Ingrid ten Haken 1 ,
- Somaya Ben Allouch 1 &
- Wim H. van Harten 2 , 3
BMC Public Health volume 18 , Article number: 284 ( 2018 ) Cite this article
23k Accesses
41 Citations
7 Altmetric
Metrics details
The number of medical technologies used in home settings has increased substantially over the last 10–15 years. In order to manage their use and to guarantee quality and safety, data on usage trends and practical experiences are important. This paper presents a literature review on types, trends and experiences with the use of advanced medical technologies at home.
The study focused on advanced medical technologies that are part of the technical nursing process and ‘hands on’ processes by nurses, excluding information technology such as domotica. The systematic review of literature was performed by searching the databases MEDLINE, Scopus and Cinahl. We included papers from 2000 to 2015 and selected articles containing empirical material.
The review identified 87 relevant articles, 62% was published in the period 2011–2015. Of the included studies, 45% considered devices for respiratory support, 39% devices for dialysis and 29% devices for oxygen therapy. Most research has been conducted on the topic ‘user experiences’ (36%), mainly regarding patients or informal caregivers. Results show that nurses have a key role in supporting patients and family caregivers in the process of homecare with advanced medical technologies and in providing information for, and as a member of multi-disciplinary teams. However, relatively low numbers of articles were found studying nurses perspective.
Conclusions
Research on medical technologies used at home has increased considerably until 2015. Much is already known on topics, such as user experiences; safety, risks, incidents and complications; and design and technological development. We also identified a lack of research exploring the views of nurses with regard to medical technologies for homecare, such as user experiences of nurses with different technologies, training, instruction and education of nurses and human factors by nurses in risk management and patient safety.
Peer Review reports
As a result of demographic changes and the rapidly increasing number of older patients, there is a need for cost savings and health reforms, which include an increased move from inpatient to outpatient care in most industrialized countries over the last 10–15 years [ 1 , 2 ]. As a consequence, the transfer of advanced medical devices into home settings was considerable and it is expected that there will be a further increase in the near future [ 1 , 2 , 3 , 4 , 5 , 6 , 7 ].
When ‘an increase’ in the number of medical technologies used at home is mentioned, it is not clear which and how many technologies are involved. Today, there are an estimated 500,000 different kinds and types of medical devices available on the world market [ 8 , 9 ]. The European Commission (EC) publishes data regarding legislation and regulations for medical devices, but the actual figures for medical technologies in outpatient practice are not available [ 10 ]. The U.S. National Center for Health Statistics (NCHS) stated that technologies have shifted from hospitals into the home, but it too does not illustrate its findings with statistics [ 11 ]. We searched for data with regard to the actual number of medical technologies used in home settings and it proved difficult to find any systematic data sets available throughout the international landscape.
An important condition for the application of medical technology in the home setting is that quality of care and patient safety must be guaranteed [ 6 ]. From a historical perspective medical technologies were designed for hospital settings [ 12 , 13 ]. This means that specific factors regarding the implementation and use at home now need to be taken into account [ 7 , 14 , 15 ]. In general, risks with medical technologies can be classified regarding (a) environmental factors; (b) human factors and (c) technological factors [ 16 ]. Human factors, however, are very important in patient safety in both hospital and in home settings [ 1 , 6 , 12 ]. For example, a major risk factor is the number of users and handovers in the chain of care. In home settings, a sometimes impressive number of different users of medical technology, often with various levels of training, instruction or education, are involved. Although patient empowerment moves control to the patient and/or relatives, an important user group is that of professional nurses. Understanding user experiences and information about adverse events and near incidents are important aspects for developing knowledge regarding implementation and use in home care setting. Sharing this knowledge can support patients and caregivers, and especially nurses in their professional work and will also contribute to patient safety and quality of care.
Therefore, there is a need to address the question first, which types of technologies are used at home; second, how frequently are they used and third, what trends can be distinguished. Additional research questions are whether there are any scientific data regarding particular user experiences; training, instruction and education; safety and risks, and finally, what can be concluded about the role of nurses in using medical technologies in the home environment. The objective of this paper therefore is to present a systematic literature search on the international state of art concerning various aspects of the use of advanced medical technologies at home.
Definitions
First, we want to clarify some definitions. In general, ‘health technology’ refers to the application of organized knowledge and skills in the form of devices, medicines, vaccines, procedures and systems developed to solve a health problem and improve quality of life [ 17 ]. The World Health Organization [ 8 ] uses the definition of ‘medical device’ as ‘An article, instrument, apparatus or machine that is used in the prevention, diagnosis or treatment of illness or disease, or for detecting, measuring, restoring, correcting or modifying the structure or function of the body for some health purpose …….’. A specification for a home use medical device is: ‘A medical device intended for users in any environment outside of a professional healthcare facility. This includes devices intended for use in both professional healthcare facilities and homes’ [ 18 ].
The landscape of medical devices is diverse with technologies varying from relatively simple to very complex devices. Wagner et al. [ 19 ] stated that ‘high-tech dependency’ (for children) matches with ‘technology-dependency’ if it concerns ‘a medical device to compensate for the loss of a vital bodily function and substantial and ongoing nursing care to avert death or further disability’. ‘The needs of these patients may vary from the continuous assistance of a device and highly trained caretaker to less frequent treatment and intermittent nursing care’ [ 20 ]. Although patients dependent of advanced medical technologies at home are often medically stable, they sometimes have high technical needs and may be expected to need long-term recovery. They also require skilled nursing [ 21 ] and a considerable degree of advanced decision making, planning, training and oversight [ 22 ]. An overall definition of ‘advanced medical technology’ is: ‘Medical devices and software systems that are complex, provide critical patient data, or that directly implement pharmacologic or life-support processes whereby inadvertent misuse or use error could present a known probability of patient harm’ [ 23 ]. Examples of advanced medical technologies used at home include ventilators for respiratory support, systems for haemo- or peritoneal dialysis and infusion pumps to provide nutrition or medication.
In the Netherlands, the National Institute for Public Health and the Environment (RIVM) [ 24 ] uses the following definition:
Advanced medical technology or high-tech technology in the home setting is defined as technology that is part of the technical skills in nursing and meets the following conditions:
technology that is advanced or high-tech, for example equipment with a plug, an on/off switch, an alarm button and a pause button;
technology that had been applied formerly only in hospital care, but that is now also often applied in home settings;
technology that can be categorized as ‘supporting physiological functions’, ‘administration’ or ‘monitoring’.
Within the Dutch classification of advanced medical technologies 19 different devices are identified (see Table 1 ), which will be used in this review as a basis to categorize the technologies. It is a classification format in which specific advanced technologies are defined. Terms as ‘advanced medical technology’ (from now on abbreviated as AMT) will be used consistently as synonyms for ‘complex medical technology’ and ‘high-tech medical technology’. The term ‘technology’ will be used in the meaning of ‘device’ or ‘equipment’. The target is on technologies that are instrumental and ‘hands on’ use by nurses in the care for patients. This means that information technology (IT) based technologies as domotica (automation for a home) are not part of the study.
Eligibility and search strategy
The systematic review of the literature was conducted early 2016. Key concepts for the review were ‘medical technologies’ or ‘medical devices’, and ‘home settings’. The concept of ‘home settings’ is related to the terms ‘home nursing’ and ‘home care service’, of which the stem is ‘home’. Combining the key concepts provided the search string: (‘medical technology’ OR ‘medical device’). As domotica is not part of the study, the search string was extended with: AND NOT (eHealth OR telecare OR telemedicine). The exact search string is (“medical technology” OR “medical devices”) AND home AND NOT (ehealth OR telecare OR telemedicine). Online databases MEDLINE, Scopus and Cinahl were searched electronically using the search string to obtain data.
Inclusion and exclusion criteria
Criteria for selection were defined prior to the search process. General criteria for inclusion were:
Year of publication: 2000–2015.
An abstract or an article (with or without abstract) has to be available, containing reference to AMT information.
The article is published in English, German, French or Dutch/Flemish language.
If medical technology is cited, it has to conform to the definition of ‘advanced medical technology’ [ 24 ].
The abstract or the article has to contain empirical material. For the purpose of this review, ‘empirical material’ has been defined as: AMT which is designed for the home setting, or where the design or choices took into account the setting of the home, or where the medical technology has been tested for the home or if the medical technology is already on the market and being used in the home setting.
For further selection, inclusion criteria related to the key concepts for title and abstract were applied, such as ‘advanced medical technology’, ‘high-tech medical technology’, ‘home-centred health-enabling technology’ and ‘care at home’. The classification of the RIVM (see Table 1 ) has been taken as a basis to categorize technologies in this review. Domotica and telemonitoring technologies scored under ‘monitoring’, such as fetal cardiotocography, and respiratory and circulatory monitoring, were left out. If the abstract or article was about electronic health records, ‘smart home’, ambient intelligence, pervasive computing, software of devices, smartphone or surgical robots, the article was also removed from selection. Technologies as ‘VAD (ventricular assist device)’, ‘dental devices’ and ‘AED (automatic external defibrillator)’ were not seen as part of the technical nursing process and these records were left out as well. Studies conducted in the hospital, hospice or nursing home settings were also excluded. An overview of all inclusion and exclusion criteria can be found in Table 2 .
Screening process
The search in the online databases using the search string, identified a total of 1287 references. After checking for duplicates, 1070 articles remained. Those articles were reviewed by a reviewer for titles and abstracts on basis of the inclusion and exclusion criteria. A double check was performed by two reviewers, who independently screened random samples of 20% of the articles. There was an initial agreement of 88%. In case of disagreement about the inclusion of an article, the decision was based on a joint discussion by all three reviewers to an agreement of 100% and the resulting screening policy was applied to the rest of the abstracts. Based on the selected titles and/or abstracts, articles were retrieved or requested in full text and assessed for eligibility. Some articles were excluded from further study, for reasons of ‘full text not available’ or the article contained no empirical material. Finally, 87 studies remained which were included in the analysis (see Table 3 ). A graphical representation of the screening process has been included in Fig. 1 .
PRISMA flowchart
Appraisal of selected studies
To conduct the systematic literature search on the international state of art concerning various aspects of the use of advanced medical technologies at home, several sources are consulted. To guarantee a scientific standard, only articles were retrieved from academic databases. MEDLINE refers to journals for biomedical literature from around the world; Cinahl contains an index of nursing and research journals covering nursing, biomedicine, health sciences librarianship, alternative medicine, allied health and more. These databases related to discipline have been supplemented with Scopus, which is considered to be the largest abstract and citation database of peer-reviewed literature. Grey literature, such as national and international reports on regulations and safety of medical technologies, is also used to illustrate the background of the problem statement and describe definitions. The Classification of advanced medical technologies in the Netherlands according to the National Institute for Public Health and the Environment (RIVM) has been used as a framework to categorise the medical technologies in the selected articles. No methodological conditions of selected studies were applied in advance and the quality criterion we applied was that of the article had to contain empirical material, as we wanted to obtain an comprehensive overview of published studies of any design and to get insight in a variety of contents.
Categorization of included articles
The characteristics of the included articles are outlined in Table 3 . All included articles were categorized by year of publication and the type of research, like the designs, methods and used instruments in the studies. Research features were synthesized where possible into overarching categories. For example, ‘systematic review’ and ‘narrative review’ were scored as ‘review’ and instruments as ‘semi-structured interview’ and ‘in-depth individual interview’ were both assigned to the category ‘interview’.
For each study, the medical technology or technologies on which the study was based was scored. The categorization was in accordance with the classification of AMTs (see Table 1 ). For example, the devices ‘continuous positive airway pressure (CPAP)’ and ‘negative pressure ventilation (NPV) have both been categorized as ‘respiratory support’; and the devices ‘jejeunostomy tube’ and ‘gastronomy tube’ as ‘enteral nutrition’. With regard to the category ‘dialysis’, further subdivision was made by using ‘haemo dialysis’ and ‘peritoneal dialysis’. If in an article a medical technology was mentioned as an example, but was no subject of study, then the technology was not scored.
‘Medical diagnosis (or diagnoses)’ as mentioned in the studies, was included in the analysis only if it was related to the medical technology as the subject of study, not if it has been mentioned as an example. In some cases, an underlying cause of diagnosis was indicated. For example, ‘chronic respiratory failure due to congenital myopathy’, in itself a neurological disorder, has been scored as ‘neurological disorder’. Diseases or disorders have been classified as much as possible under the overarching name. For example ‘pneumonia’ and ‘cystic fibrosis’ are categorized under ‘respiratory failure’, and ‘gastroparesis’ and ‘Crohns disease’ under ‘gastrointestinal disorder’. The category ‘other’ contains diagnoses which occur only once, such as ‘chromosomal anomaly’, or which are not yet determined, like ‘chronic diseases’ or ‘congenital abnormalities’.
In relation to the research questions, articles were classified regarding one of the following categories and, where appropriate, into subcategories:
User experiences
Training, instruction and education, safety, risks, incidents and complications.
From an analysis of the articles, additional categories of content emerged:
Design and technological development
Application with regard to certain diseases or disorders, indication for and extent of use
Policy and management
Types of medical technologies used, frequency of use and trends.
In four of the 87 articles (5%) there were no specific medical technologies mentioned as a subject of study (see Table 4 ). Almost half of the studies (45%) considered medical technologies for respiratory support and 39% devices for dialysis, either haemo- ( n = 18), peritoneal- ( n = 15) or dialysis not specified ( n = 1). Of the studies, 29% reported on devices for oxygen therapy. In addition, there has been relatively more research conducted on equipment for ‘infusion therapy’ ( n = 19; 22%), parenteral nutrition and enteral nutrition with a score of 20% each ( n = 17). Relatively little research has been carried out on suction devices (8%), external electrostimulation (5%), nebulizer (5%), insulin pump therapy (3%), sleep apnea treatment (2%), patient lifting hoists (2%), vacuum assisted wound closure (1%) and continuous passive motion (1%). None of de studies considered medical technologies with regard to decubitus treatment, skeletal traction or UV (ultraviolet) therapy.
Table 4 shows that on the years 2000 and 2001 no relevant articles on the subject were found. Over the period 2000–2005, 17 articles were published, the same number over 2006–2010, and there has been a substantial increase in the number of publications to 54 over the years 2011–2015. In general, it can be concluded that more frequent investigated technologies show a fairly even distribution of publications over the years 2000–2015. Technologies, on which little research had been done, except for nebulizers, have been mainly investigated since 2010. An increase of published articles over the years 2000–2015 is apparent particularly for haemo dialysis and to a lesser extent, for devices for enteral- and parenteral nutrition. As mentioned before, several studies reported on the increase of the number of medical technologies used in home settings, but concrete data are not available. However, the number of studies and the visible trends may be indicative of the frequency of use.
In 63% of the cases ( n = 55), a medical diagnosis (or diagnoses) was mentioned in the article. Where a diagnosis has been mentioned, in almost half of the studies ( n = 26; 47%) it concerned diagnoses in the field of respiratory failure (see Fig. 2 ). This is not surprising, since ‘respiratory support’ is the medical technology most commonly found in the articles, similarly ‘oxygen therapy’ has also been considered relatively often. Diagnoses with regard to neurological disorders occurred in 42% of the studies ( n = 23). Just over a quarter of the studies (27%) considered diagnoses ‘other’, such as ‘sepsis’, ‘chromosomal anomaly’ or other not specified medical disorders, nearly a quarter (24%) considered ‘cancer’ and 22% kidney disorders ( n = 12).
Number of medical diagnoses mentioned in articles on AMTs ( n = 87, multiple answers possible)
An analysis of the used research designs identified that 64% ( n = 56) of the studies used an observational (non-experimental) design and only a small part of the studies ( n = 5; 6%) used an experimental design, such as a Randomized Control Trial (RCT). Of the included studies 19 were reviews and 8 were essays. A quantitative design ( n = 37) was used more frequently than a qualitative design ( n = 25); and only one study applied ‘mixed methods’ (quantitative and qualitative). Just over one-third of the studies (35%) used a descriptive design, and a similar number used a cross-sectional study (36%). Case series were used in 12% of the articles and a cohort-study in 9%. A phenomenological approach was applied in 16% of the records. Research instruments most frequently used were interviews (33%) and survey/questionnaires (21%). In 10% of the cases other instruments were used, including different types of assessments or tests.
With regard to the categories of content, most research has been carried out on ‘user experiences’ (see Fig. 3 ): just over one-third of the articles ( n = 31; 36%) focused on this topic. Of these articles almost all studies focused on experiences of patients or informal caregivers ( n = 29) and only a small number ( n = 2) considered the user experiences of nurses or other professionals (see Table 5 ). More than half of the studies ( n = 19) used a qualitative research design; of these 13 used a phenomenological approach. The goal of these studies was to elicit the essence of human phenomena as experienced by the users. Seven studies used a quantitative design and one an integrated mixed method. Three of the studies applied a grounded theory approach and two an experimental design (randomized controlled trial). The research instruments in this content category to collect data were interviews, either semi-structured or in-depth, and a survey. About two-thirds of the articles regarding ‘user experiences’ were published in the period 2011–2015, with an accent on the psychosocial impact of patients or informal caregivers.
Number of articles on AMTs with main content categories ( n = 87)
Relatively little research was found on ‘training, instruction, education’ ( n = 7), for the use of AMTs in home settings. It was remarkable that all the studies identified as focusing on this topic, concentrated on one category of AMT. Respiratory support was the subject of study in four instances and in the other three, the focus was on technologies for enteral nutrition, haemo dialysis and external electro-stimulation. Four of the seven articles utilized quantitative methods, among which three of them used an observational non-experimental design and one was an experimental randomized double-blind clinical trial. Another study within the initial seven articles used a qualitative observational non-experimental design, one was a review and another was in essay format.
In total, 22% of the articles discussed topics on safety, risks, incidents and complications ( n = 19). In the majority of cases ( n = 13) general aspects about the subject, for instance safe use, factors affecting safety, a safe transfer of the equipment and monitoring of assessing safety were considered. One article described technological factors with regard to safety, three articles reported on environmental factors and two explored human factors. Safety aspects were explored over a wide range of medical technologies. Five articles were reviews and one an essay. Quantitative methods were used in ten of the cases, particularly for monitoring, evaluating and assessing safety, technological and environmental factors. Only three studies used a qualitative design. Retrospective chart reviews or case series were used to collect data in some cases of unforeseen events. Table 5 shows about a doubling of published articles in the period 2011–2015 regarding this content category, compared to the previous period 2000–2010.
Approximately 20% of the selected articles considered the content category ‘design and technological development of the medical device’ ( n = 17). The studies each focused on only one type of AMT and treated a relative wide range of eight different categories, such as ‘respiratory support’, ‘oxygen therapy’, ‘haemo dialysis’, ‘infusion therapy’, ‘insulin pump therapy’ and ‘enteral nutrition’, but also ‘external electrostimulation’ and ‘patient lifting hoists’. Interestingly, in this group of articles, relatively often ( n = 6) no medical diagnosis was mentioned. Around half of the studies ( n = 8) referring to this topic were in review or essay format. All other studies used a quantitative research design and throughout the search no application of qualitative designs were found. Two studies used an experimental study design (randomized crossover trial) to obtain data and two described a prospective cohort study. The majority of papers ( n = 11) were published in the period 2011–2015 and six in the preceding period up to and including 2010.
Seven articles concerned the application of AMTs, all of them devices with regard to at least respiratory support and/or nutritional support. Five studies used a non-experimental quantitative design including the analysis of clinical data, such as record reviews or cohort studies, and two articles were reviews. Most articles on this subject ( n = 5) were published in the period 2012–2015.
Six articles described policy or management systems in different countries regarding the use of AMTs at home. The majority of the articles ( n = 4 ) were in essay or review format. The other papers concerned a qualitative cross-sectional case study analysis and an observational quantitative study in which data are collected prospectively using a database. The categories of content will now be discussed in greater detail.
Content description and trends to secondary research questions
In this category, 22 articles described the psychosocial impact on patients or informal caregivers from the use of medical technologies at home. Living at home with the assistance of medical technology needs a range of adjustments. Fex et al. [ 25 , 26 ] state that self-care is more than mastering the technology, in terms of the health-illness transition, it requires ‘…. an active learning process of accepting, managing, adjusting and improving technology’. When it comes to children, they have to learn to incorporate disability, illness and technology actively within their process of growing up [ 27 ]. It seems that the use of medical technologies in the home can have both a positive and a negative psychosocial impact on patients and their families, which in turn causes ambivalence in experiences [ 27 , 28 ]. On the one hand, patients in general gain more independence, an enhanced overall health and a better quality of life [ 29 , 30 , 31 , 32 , 33 , 34 ]. On the other hand, for some patients the experience is one of dependency on others for executing daily activities, and these circumstances, to some extent, a social restricted live and perceived stigmatization [ 29 , 30 ]. The situation in which patients need to use medical technology at home also affects family functioning and requires next of kin responsibilities [ 35 , 36 , 37 ]. As a result, next of kin caregivers are frequently faced with poor sleep quality and quantity, and/−or other significant psychosocial effects [ 38 , 39 , 40 , 41 ]. Nevertheless, family members had a positive attitude to the concept of bringing the technology into the home [ 42 ]. Knowledge of how to use the technology and permanent access to support from healthcare professionals and significant others, enabled next of kin caregivers to take responsibility for providing necessary care and to facilitate patients learning to provide self-care [ 25 , 36 , 42 , 43 , 44 ]. Bezruczko et al. [ 45 , 46 ] developed a measure of mothers’ confidence to care for children assisted with medical technologies in their homes. To provide high quality sustainable care, nurses have to recognize and understand the psychosocial dimensions for both patients and family members which arise as a result of changing role and providing care for the patients. The need to provide emotional support and support with appropriate coping strategies is a key professional role [ 25 , 26 , 47 ]. Insight into the psychosocial effects on those involved can be used to assist designers of medical devices to find strategies to better facilitate the integration of these technologies into the home [ 28 ].
Seven articles reported on the usability, barriers and accessibility experienced by patients or informal caregivers. Findings in these studies showed that several technologies were rarely perceived as user-friendly and that home medical devices inadequately met the needs of individuals with physical or sensory deficits [ 48 , 49 ]. An accessible design which meets the diversity of individual user needs, characteristics and features would be better able to help patients manage their own treatment and so could contribute to the quality of care and safety of patients and lay users [ 50 , 51 ]. Munck et al. [ 52 ] stated that restricted patients were reminded daily of the medical technology and were more dependent on assistance from healthcare professionals than masterful patients.
In contrast to the group of patients or informal caregivers, only two papers in this content category focused on the user experiences of nurses or other professional caregivers. The review demonstrates that to maintain patient safety, more education on application of medical devices for users is needed together with improved awareness and understanding of how to use the medical technology correctly in a patient-safe way [ 53 , 54 ]. More collaboration between all involved ‘actors’ in the process of care is also requisite. Continuity among carers, trust between patient and carers and supportive communication between informal and professional caregivers are important factors for the successful implementation of medical technologies in the home environment while maintaining patient safety [ 44 , 51 , 53 , 54 , 55 ].
Three articles regarding this topic focused on nurses or other professionals and four on the patients or informal caregivers. The results showed that successful use of advanced medical technologies at home requires adequate staff education and training programmes. Although many topics in educational programmes are suitable for different types of professionals in care provision, the focus for the level and application of information can vary for Registered Nurses and unregistered care staff. In addition, for overall learning experiences to be of maximum benefit there is a need for a clear focus on the specific client groups [ 56 ]. According to Sunwoo et al. [ 57 ], in the case of home non-invasive ventilation the degree of clinical support needed is extremely variable given the mixed indications for this respiratory support. A relatively simple procedure, such as the replacement of a feeding tube, can be performed by nurses, the patient and informal caregivers, provided they are trained well [ 58 ]. However, several studies revealed the complexity of the education needed by patients and informal caregivers for the use of advanced medical technologies at home [ 59 , 60 ]. Nevertheless, the studies revealed that a structured education programme, specific training, or the support of a dedicated discharge coordinator has several advantages [ 59 , 61 , 62 ]. It was evident that good preparation by patients or informal caregivers may result in a shorter length of stay in hospital, a better performance with regard to the use of the equipment or less requests by patients and/or families for assistance.
Most articles regarding this topic ( n = 13) reported on safety in general, like aspects of safe use, factors affecting safety, complications and prevention of incidents in the home. Some identified the risk factors and the complications that may arise [ 63 , 64 , 65 ], where Stieglitz et al. [ 66 ] also emphasize that human error is the main reason for critical incidents and that regular instruction for medical staff and patients is necessary. To prevent untoward and adverse events, evidence based guidelines, recommendations on the preferred methods for managing the equipment, troubleshooting techniques for potential complications and monitoring activities are necessary [ 67 , 68 ]. Faratro et al. [ 68 ] added that key performance and quality indicators are important mechanisms to ensure patient safety when using a medical device in the home. Methods to address or evaluate patient safety issues are for example, a home visit audit tool, a nationwide adverse event reporting system, programs such as the Medical Product Safety Network HomeNet, or, in the case of peripherally inserted central catheters (PICCs) a central catheter stabilization system [ 69 , 70 , 71 , 72 ]. However, a study conducted by Pourrat and Neuville [ 73 ] in France found that there are very few internal medical devices vigilance reports found within organizations that deliver devices for home parenteral nutrition and that safety management could be improved. The safe transfer of medical devices from a hospital setting to the home and vice versa, comes with several challenges regarding technological, environmental and human factors [ 14 ]. While many hospitals have developed policies to control the pathways of home-used devices in the hospitals, in case patients take them into the hospital when they are admitted for treatment [ 74 ]. Improvement of the safety of devices intended for use in home settings, implies also improvement of safety when their transfer to the hospital settings is urgently needed.
One article considered the technological factors, three the environmental and two the human factors. An example of research on the technological factors of safety related aspects of medical technologies used in home settings by Hilbers et al. [ 75 ] found that manufacturers pay insufficient attention to safety-related items in technical documentation for the use in the home setting. For instance, the environmental factor of electricity blackout leads to electrically powered medical devices failing. Studies show that this type of event causes a dramatic increase in appeal for access to emergency or hospital facilities, and that disaster preparation needs to include the specific needs of patients reliant on electrically driven devices [ 76 , 77 , 78 ]. Regarding human factors impacting on safety aspects, one article assessed the suitability of a particular theoretical framework for understanding safety-critical interactions of patients using medical devices in the home [ 79 ], while Tennankore et al. [ 80 ] described adverse events in home haemodialysis by the use of patients. It was remarkable that none of the articles focused on human factors with regard to the use of medical technologies at home by nurses or other professional caregivers.
Of those articles that focused on this topic, ten reported on the comparison between different types of medical technologies, or their advantages and disadvantages. The comparison of different devices for oxygen therapy was made by two articles [ 81 , 82 ] and one reported on the comparison of two types of enteral nutrition tubes [ 83 ]. Some studies regarding respiratory support considered the process of making a choice between different types of devices [ 84 , 85 , 86 ] while one paper considered the conditions for home-based haemo dialysis [ 87 ]. A minority, explored the individual characteristics and the clinical applications of several devices for respiratory support [ 88 , 89 ] and one considered devices for insulin pump therapy [ 90 ]. Seven papers discussed the technological development or effectiveness of medical technologies. The testing of devices for external electro-stimulation was described in two papers [ 91 , 92 ], with the testing of a new design patient lift was subject of one study [ 93 ]. Hanada and Kudou [ 94 ] explored the current status of electromagnetic interference with medical devices in the home setting, an issue of importance as more devices are considered for home use. The technological development of respiratory support for home use was part of one study [ 95 ], as were the possibilities of solar-assisted home haemo dialysis [ 96 ]. While the study by Pourtier [ 97 ] describes the advantages of analgesia pumps that can be read remotely by nurses, but also emphasizes the central position of a professional nurse in the transfer of information within a multi-disciplinary team.
Application with regard to certain diseases or disorders, indications for and extent of use
All articles described several aspects that need to be considered for use, such as clinical characteristics of the patients, indications for the use in the home setting, the technical availability of devices, the extent of their use at home or eventual complications and morbidity. It was important to note that all but one article ( n = 6) were about children or related to adults with what are usually regarded as paediatric diseases. Results show that the use of AMTs at home among children after hospital discharge is common (in 20%–60% of cases), or is standard for patients with some disorders [ 98 , 99 , 100 , 101 ]. The timely application of advanced home medical technology benefits patients and can help to reduce respiratory morbidity [ 102 ]. Nevertheless, the rate of death of patients with Möbius syndrome using the devices at home was high (30%) [ 98 ], as was that of patients with intestinal failure dependent on home parental nutrition therapy in Brazil (75% for 5 years) [ 103 ]. The average cumulative survival of children needing home ventilation was found to be between 75 and 90%, depending on the medical diagnosis [ 104 ].
Three of the papers were concerned with costs and/or reimbursement. The application of medical technologies in the home environment can be cost-effective when compared to institutionalized care [ 22 , 105 , 106 ]. Nevertheless, successful employment of medical technologies in the home necessitates medical guidelines for the indicators for use, careful identification of patients as well as careful planning and attention to details [ 105 , 106 , 107 ]. Two studies concerned the dilemma’s for implementation of the technologies in home healthcare and emphasized the importance of cooperation in the chain of key stakeholders to maximize efficiency of high-tech healthcare at home, one with regard to the purchasing policy of medical technologies [ 108 ] and one with regard to the interventions of local community service centres and hospitals supporting optimal use of these technologies in the home setting [ 5 ].
The use of medical technologies in the home setting has drawn increased attention in health care over the last 15 years, as the feasibility of this type of medical support has rapidly grown. This article systematically reviewed the international literature with regard to the state of the art on this subject, in order to provide a comprehensive overview.
Trend analysis over the period 2000–2015 shows that most research has been conducted about respiratory support, dialysis and oxygen therapy; relatively little about vacuum assisted wound closure and continuous passive motion, and no about decubitus treatment, skeletal traction and UV therapy. A substantial increase in publications was found in the period 2011–2015. Although the number of studies on technologies is indicative of the extent to which they are used in home settings, however, no firm conclusions can be drawn about this.
This review also identified that most research is conducted with regard to ‘user experiences’ of medical technologies in the home, ‘safety, risks, incidents and complications’, and ‘design and technological development of medical technologies’. There have been relatively few studies which have explored the topic of training, instruction and education. Content analysis showed that the use of AMTs in the home setting can have both a positive and a negative psychosocial impact on the patients and their families, and that it has become part of self-management and patient empowerment. Successful use of advanced equipment requires adequate education and training programmes for both patients, informal caregivers and nurses or other professionals. When trying to maximize or assure safety, technological, environmental and human factors have to be taken into account, and it is evident that human factors are the main reason for critical incidents. Studies on the design and technological development of medical technologies emphasize that research is necessary to improve its possibilities and effectiveness. The research found on the application of the technologies focused predominantly on children and the results indicate that the rate of the use of home medical devices among children after hospital discharge is common. Also that when compared to institutionalized care, the application of medical technologies in the home environment can be cost-effective. Much is known, but information on several key issues is limited or lacking.
An important finding was that in almost all the reviewed articles, the study subjects were patients or informal caregivers with very few studies focused on the role and activities of nurses or other professionals as users. This was unexpected as nurses are the main group of users of AMTs at home and they have to transfer knowledge and skills on how to use the devices to patients and other caregivers. Nurses also have a key role in setting up and maintaining collaboration between all actors involved in the process of care with regard to the use of home medical technologies and in giving support to patients and family members in this respect. There is need to initiate further in depth research on AMTs use at home focusing on the role of specifically nurses.
Another interesting result was that, despite the fact that most adverse events with AMTs at home are caused by human factors, hardly any studies conducted on this subject were found. None of the articles focused on related human factors regarding the use by nurses or other professional caregivers, although this is the main user group. Research on this area could contribute to improved patient safety and quality of care. The results also revealed the tension between the advantages and disadvantages of medical technologies as experienced by patients at home. Important aspects needed to promote the benefits include improving the user-friendliness of the devices and attuning their designs for the use in home settings. This emphasizes the importance of professionals (and patient groups) working together with the designers with regard to sharing knowledge and user experiences of the use of AMTs at home in order to improve quality of care and patient safety. This collaboration emerged as of key importance in the successful use of AMTs in the home as well.
Although all included articles were retrieved from academic databases and served our purpose, there was considerable heterogeneity of quality of the studies. Most of the studies have explicitly described their research design, albeit to a greater or lesser extent. On the other hand, there were a few studies that did not even mention their methodological approach, though it could be derived from the description. Most included reviews are of moderate quality. Although findings are almost always described clearly, the search strategy and selection criteria used are often lacking. The quantitative studies are generally well described in different methodological aspects, such as selection of respondents, research design, data collection methods and analyses. Studies of qualitative nature show more variation in the depth with which the design is described. However, almost all qualitative studies have described the research instruments very well, such as semi-structured interviews or questionnaires. Despite the varying quality of the studies, we believe that the whole of different methodological approaches and the relatively large number of included studies ( n = 87) has yielded a fairly reliable overview on the international state of art concerning various aspects of the use of advanced medical technologies at home. For future research, we recommend to emphasize the development of a more detailed methodological design, zooming in on specific technologies, using large databases or conducting large surveys, and focusing on specific groups of respondents. Both in quantitative and in qualitative studies, a good definition of the research question(s), selection of respondents, development of instruments and analysis of findings, contributes to validity, consistency and neutrality.
Some limitations do have to be taken into account with this review. Although we used the RIVM-definition of ‘advanced medical technology’, not all devices are considered as ‘complex devices’ by nurses in practice. For example, the use of an anti-decubitus mattress in the context of ‘decubitus treatment’ and ‘patient lifting hoists’ are considered by nurses as being of less or lower complexity. However, overall the RIVM-classification was found to be a good starting point, and provided a practical and useful framework from which to work to gain an insight and overview of available medical technologies. Of some of the chosen technologies defined using the RIVM-classification of AMTs, questions do have to be asked as to whether they really are part of the technical skills in nursing process. For example, ‘external electrostimulation’ and ‘continuous passive motion’ are mainly applied by physiotherapists, although with appropriate training nurses can apply them. Then too, devices regarded as only ‘monitoring’ were excluded from the review.
This systematic review study was designed to fill a gap in the current research by investigating what is known about different aspects of medical technologies used in the home. From the results it is obvious that a wide and growing range of medical technologies are used at home. Different types of technologies have been subject of study, increasingly –also in scope- over the period 2011–2015.
Professional nurses have a central role in the process of homecare which has to be recognized when considering use of AMTs at home. Nurses have to support patients and family caregivers and in consequence have a key role in providing information for, and as a member of multi-disciplinary teams. Closer collaboration by all actors involved in the process of care and feedback of user experiences to the designers is essential for the provision of high quality of care and patient safety.
This review also identified a lack of research exploring the perspectives of nurses in the processes involved in introducing and maintaining technology in homecare. Most of the research has been conducted regarding the experiences of patient experience and how informal caregivers perceive their role in using medical technologies at home. The few studies that were found, demonstrate the need for more research focused on the experiences of nurses working with advanced technologies in the home. The same applies to research on training, instruction and education to use medical technologies, as in these areas too, there was limited available research so here again there is need for further research. Despite the fact that most adverse events with medical technologies in home settings are caused by human factors, our findings also identified a lack of research in this area for nurses.
This study demonstrates that, although there is increasing attention on and recognition of the need for the use of medical technologies in the environment of the home, the research has not kept pace with the advances in care. Subjects such as user experiences of nurses with different technologies, training, instruction and education of nurses and human factors by nurses in risk management and patient safety urgently need to be investigated by further research.
Abbreviations
Automatic external defibrillator
Advanced medical technology
Continuous positive airway pressure
European Commission
Information technology
National Center for Health Statistics
Negative pressure ventilation
Peripherally inserted central catheters
Randomized Control Trial
National Institute for Public Health and the Environment
Ultraviolet
Ventricular assist device
World Health Organization
Hollestelle M, Hilbers E, van Tienhoven E, Geertsma R. Geavanceerde medische technologie in de thuissituatie: inventarisatie, gebruikersaantallen en risico’s. RIVM rapport 265011004/2005. Rijksinstituut voor Volksgezondheid en Milieu RIVM, Bilthoven; 2005.
WHO. Primary Health Care. Now more than ever. World Health Organization, Geneva; 2008.
Arno P, Bonuck K, Padgung R. The economic impact of high-technology home care. Spec. Suppl. Hast Cent Rep. 1994;24:S15–9.
Article CAS Google Scholar
Arras J, Neveloff Dubler N. Bringing the hospital home: ethical and social implications of high tech home care. Spec. Suppl. Hast Cent Rep. 1994;24:S19–28.
Lehoux P, Charland C, Richard L, Pineault R, St-Arnaud J. Technologies de pointe et soins à domicile. Où en sont les CLSC? Can Med Assoc J. 2002;166:1277–8.
Google Scholar
IGZ. Risico’s van medische technologie onderschat. Staatstoezicht op de volksgezondheid, Den Haag; 2008.
Hilbers E, de Vries C, Geertsma R. Veiligheid van medische technologie in de thuissituatie. Een analyse op basis van onderzoek van technische dossiers van fabrikanten. RIVM Rapport 360050022/2009. Rijksinstituut voor Volksgezondheid en Milieu RIVM: Bilthoven; 2009.
WHO. WHO Global model regulatory framework for medical devices including IVDS. Draft for comment. World Health Organization, Geneva; 2016.
EC. Commission welcomes new agreement for safer use of medical devices. 2016 [cited 2016 June 29]: Available from: http://ec.europa.eu/growth/tools-databases/newsroom/cf/itemdetail.cfm?item_id=8863&lang=en . 2016.
Council of the European Union. Proposal for a regulation of the European Parliament and of the council on medical devices, and amending directive 2001/83/EC, regulation (EC) no 178/2002 and regulation (EC) no 1223/2009. 2016.
NCHS. Health, United States, 2009. In Brief—Medical Technology [Internet]. National Center for Health Statistics, Hyattsville, M.D.; 2010. Available from: http://www.cdc.gov/nchs/data/hus/hus09_InBrief_MedicalTech.pdf
Weick-Brady MD, Lazerow RN. Medical devices: promoting a save migration into the home. Home Healthc Nurse. 2006;24:298–304.
Article PubMed Google Scholar
Kaufman-Rivi D, Collins-Mitchell J, Jetley R. Design considerations for medical devices in the home environment. Biomed. Instrum. Technol. 2010;Home Health:21–6.
Fu M, Weick-Brady M, Tanno E. Medical devices in the home: a unique challenge for the FDA. Work. 2012;41:361–5.
PubMed Google Scholar
Brady P. Creating home medical devices. When it comes to designing products for home healthcare, challenges are universal. Health Manag. Technol. 2011;May:32(5):17.
Verkerke GJ, ten Cate Hoedemaker HO, Drost R, Pot JWGA, Lansbergen MDI, HM BCA, et al. Medische Technologie at risk? In: Onderzoek naar risico’s bij medische technologie en mogelijkheden om deze te voorkomen of te reduceren. Onderzoeksrapportage in opdracht van het Ministerie voor Volksgezondheid, Welzijn en Sport. Onderz. Opdr. ven het Minist. voor Volksgezond. Welz. en Sport; 2011.
Sixtieth World Health Assembly. Health technologies [internet]. 2007. Available from: http://www.who.int/medical_devices/resolution_wha60_29-en1.pdf
FDA. What is a home use device? [cited 2016 June 29]: Available from: https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/HomeHealthandConsumer/HomeUseDevices/default.htm#1 .
Wagner J, Power E, Fox H. Technology dependent children: hospital versus home care. Philadelphia, PA: Office of Technology Assessment Task Force. JP; 1988.
OTA. Technology Dependent Children: Hospital v. Home Care. A Technical Memorandum (Report No. OTA-TM-H-38). US Government Printing Office Washington, DC; 1987. http://ota.fas.org/reports/8728.pdf
Hochstadt N, Yost D. In: Hochstadt N, Yost D, editors. The medically complex child: the transition to home care. Ann Arbor, Michigan: Harwood Academic Publishers, Bell & Howell; 1991.
Lewarski JS, Current GPC. Issues in home mechanical ventilation. Chest. 2007;132:671–6.
APSF. Definition and examples of advanced medical technology (AMT). [Internet]. 2016 [cited 2016 Jun 29]. Available from: http://www.apsf.org/initiatives.php
Hessels J, de Vries C, Hilbers E, de Bruijn A, Geertsma R. Risico’s bij gebruik van complexe medische technologie in de thuissituatie. Stand van zaken 2013. RIVM Rapport 2014–0061. Rijksinstituut voor Volksgezondheid en Milieu RIVM, Bilthoven; 2014.
Fex A, Ek A-C, Söderhamn O. Self-care among persons using advanced medical technology at home. J Clin Nurs. 2009;18:2809–17.
Fex A, Flensner G, Ek A-C, Söderhamn O. Health-illness transition among persons using advanced medical technology at home. Scand J Caring Sci. 2011;25:253–61.
Kirk S. How children and young people construct and negotiate living with medical technology. Soc Sci Med Elsevier Ltd. 2010;71:1796–803.
Thomson R, Martin JL, Sharples S. The psychosocial impact of home use medical devices on the lives of older people: a qualitative study. BMC Health Serv Res. 2013;13:467–75.
Article PubMed PubMed Central Google Scholar
Brooks D, King A, Tonack M, Simson H, Gould M, Goldstein R. User perspectives on issues that influence the quality of daily life of ventilator-assisted individuals with neuromuscular disorders. Can Respir J. 2004;11:547–54.
Lehoux P, Saint-Arnaud J, Richard L. The use of technology at home: what patient manuals say and sell vs. what patients face and fear. Sociol Health Illn. 2004;26:617–44.
Heaton J, Noyes J, Sloper P, Shah R. Families’ experiences of caring for technology-dependent children: a temporal perspective. Health Soc Care Community. 2005;13:441–50.
Alsaleh FM, Smith FJ, Thompson R, Al-Saleh MA, KMG T. Insulin pump therapy: impact on the lives of children/young people with diabetes mellitus and their parents. Int J Clin Pharm. 2014;36:1023–30.
Bortolussi R, Zotti P, Conte M, Marson R, Polesel J, Colussi A, et al. Quality of life, pain perception, and distress correlated to ultrasound-guided peripherally inserted central venous catheters in palliative care patients in a home or hospice setting. J Pain Symptom Manag. 2015;50:118–23.
Article Google Scholar
Gavish L, Barzilay Y, Koren C, Stern A, Weinrauch L, Novel FDJ. Continuous passive motion device for self-treatment of chronic lower back pain: a randomised controlled study. Physiotherapy. 2015;101:75–81.
Article CAS PubMed Google Scholar
Wang K-WK, Barnard A. Technology-dependent children and their families: a review. J Adv Nurs. 2004;45:36–46.
Munck B, Sandgren A, Fridlund B, Mårtensson J. Next-of-kin’s conceptions of medical technology in palliative homecare. J Clin Nurs. 2012;21:1868–77.
Toly VB, Musil CM, Carl JC. Families with children who are technology dependent: normalization and family functioning. West J Nurs Res. 2012;34:52–71.
Glader LJ, Palfrey JS. Care of the child assisted by technology. Pediatr Rev. 2009;30:439–45.
Keilty K, Cohen E, Ho M, Spalding K, Stremler R. Sleep disturbance in family caregivers of children who depend on medical technology: a systematic review. J Pediatr Rehabil Med. 2015;8:113–30.
Paddeu EM, Giganti F, Piumelli R, De Masi S, Filippi L, Viggiano MP, et al. Sleeping problems in mothers and fathers of patients suffering from congenital central hypoventilation syndrome. Sleep Breath. 2015;19:1057–64.
Toly VB, Musil CM, Zauszniewski JA. Resourcefulness training intervention: a promising approach to improve mental health of mothers with technology-dependent children. Appl Nurs Res. 2014;27:87–90.
Fex A, Flensner G, Ek A-C, Söderhamn O. Living with an adult family member using advanced medical technology at home. Nurs Inq. 2011;18:336–47.
Fex A, Flensner G, Ek A-C, Söderhamn O. Self-care agency and perceived health among people using advanced medical technology at home. J Adv Nurs. 2012;68:806–15.
Craig GM, Scambler G, Spitz L. Why parents of children with neurodevelopmental disabilities requiring gastrostomy feeding need more support. Dev Med Child Neurol. 2003;45:183–8.
Bezruczko N, Chen SPC, Hill C, Chesniak JM. Fundamental measurement of functional caregiving in rehabiliation medicine. In: 19th IMEKO world Congr; 2009. p. 2115–22.
Bezruczko N, Chen SPC, Hill CD, Chesniak JM. Measurement of mothers’ confidence to care for children assisted with tracheostomy technology in family homes. J Appl Meas. 2011;12:339–57.
Kirk S, Glendinning C, Callery P. Parent or nurse? The experience of being the parent of a technology-dependent child. J Adv Nurs. 2005;51:456–64.
Lehoux P. Patients’ perspectives on high-tech home care: a qualitative inquiry into the user-friendliness of four technologies. BMC Health Serv Res. 2004;4:1–9.
Fung CH, Igodan U, Alessi C, Martin JL, Dzierzewski JM, Josephson K, et al. Human factors/usability barriers to home medical devices among individuals with disabling conditions: in-depth interviews with positive airway pressure device users. Disabil Health J. 2015;8:86–92.
Lemke MR, Mendonca RJ. A question of accessibility: understanding lay users of medical devices. Biomed Instrum Technol 2013;Spring:201:20–5.
Rajkomar A, Farrington K, Mayer A, Walker D, Blandford A. Patients’ and carers’ experiences of interacting with home haemodialysis technology: implications for quality and safety. BMC Nephrol. 2014;15:195.
Munck B, Sandgren A, Fridlund B, Mårtensson J. Patients’ understanding of medical technology in palliative home care: a qualitative analysis. J Hosp Palliat Nurs. 2012;14:191–8.
Munck B, Fridlund B, Mårtensson J. District nurses’ conceptions of medical technology in palliative homecare. J Nurs Manag. 2011;19:845–54.
Siewers V, Holmøy T, Frich JC. Experiences with using mechanical in–exsufflation in amyotrophic lateral sclerosis. Eur J Phys. 2013;15:201–7.
Jayanti A, Wearden AJ, Morris J, Brenchley P, Abma I, Bayer S, et al. Barriers to successful implementation of care in home haemodialysis (BASIC-HHD):1. Study design, methods and rationale. BMC Nephrol. 2013;14:197.
Hewitt-Taylor J. Children who require long-term ventilation: staff education and training. Intensive Crit Care Nurs. 2004;20:93–102.
Sunwoo BY, Mulholland M, Rosen IM, Wolfe LF. The changing landscape of adult home noninvasive ventilation technology, use, and reimbursement in the united states. Chest. 2014;145:1134–40.
Fayemendy P, Sourisseau H, Jesus P, Desport JC. Changement de sonde de gastrostomie à ballonnet de l’adulte. Nutr Clin Metab. 2014;28:216–8.
Graf JM, Montagnino BA, Hueckel R, McPherson ML. Children with new tracheostomies: planning for family education and common impediments to discharge. Pediatr Pulmonol. 2008;43:788–94.
Wong J, Eakin J, Migram P, Cafazzo JA, Halifax NVD, Chan CT. Patients’ experiences with learning a complex medical device for the self-administration of nocturnal home hemodialysis. Nephrol Nurs J. 2009;36:27–32.
Tearl DK, Cox TJ, Hospital HJH. Discharge of respiratory-technology-dependent children: role of a dedicated respiratory care discharge coordinator. Respir Care. 2006;51:744–9.
dos Santos-Fontes RL, Ferreiro de Andrade KN, Sterr A. Conforto AB. Home-based nerve stimulation to enhance effects of motor training in patients in the chronic phase after stroke: a proof-of-principle study. Neurorehabil Neural Repair. 2013;27:483–90.
Buchman AL, Opilla M, Kwasny M, Diamantidis TG, Okamoto R. Risk factors for the development of catheter-related bloodstream infections in patients receiving home Parenteral nutrition. J Parenter Enter Nutr. 2014;38:744–9.
Davenport A. Complications of hemodialysis treatments due to dialysate contamination and composition errors. Hemodial Int. 2015;19(Suppl 3):S30–3.
Szeinbach SL, Pauline J, Villa KF, Commerford SR, Collins A, Seoane-Vazquez E. Evaluating catheter complications and outcomes in patients receiving home parenteral nutrition. J Eval Clin Pract. 2015;21:153–9.
Stieglitz S, George S, Priegnitz C, Hagmeyer L, Randerath W. Life-threatening events in respiratory medicine: misconnections of invasive and non-invasive ventilators and interfaces. Pneumologie. 2013;67:228–32.
McGoldrick M. Preventing infections in patients using respiratory therapy equipment in the home. Home Healthc Nurse. 2010;28:212–20.
Faratro R, Jeffries J, Nesrallah GE, MacRae JM. The care and keeping of vascular access for home hemodialysis patients. Hemodial Int. 2015;19(Suppl 1):S80–92.
François K, Faratro R, d’Gama C, Wong E, Fung S, Chan CT. Utility of baseline home visit audit in home Hemodialysis. ASAIO J. 2015;61:695–700.
Kaufman-Rivi D, Hazlett AC, Hardy MA, Smith JM, Seid HB. Provider experiences with negative-pressure wound therapy systems. Adv Skin Wound Care. 2013;26:311–8.
Kaufman D, Weick-Brady M. Homenet: ensuring patient safety with medical device use in the home. Home Healthc Nurse. 2009;27:300–7.
Egan GM, Siskin GP, Weinmann R, Galloway MM. A prospective Postmarket study to evaluate the safety and efficacy of a new peripherally inserted central catheter stabilization system. J Infus Nurs. 2013;36:181–8.
Pourrat M, Neuville S. Nutrition parentérale à domicile: prise en charge et suivi des incidents; mise en œuvre des vigilances. Enquête sur la France métropolitaine. Nutr Clin Metabolisme. 2007;21:109–14.
Tanno E. Policies and pathways of home-use medical devices through hospitals. J Clin Eng. 2010;35:215–22.
Hilbers ESM, de Vries CGJCA, Geertsma RE. Medical technology at home: safety-related items in technical documentation. Int J Technol Assess Health Care. 2013;29:20–6.
Nakayama T, Tanaka S, Uematsu M, Kikuchi A, Hino-Fukuyo N, Morimoto T, et al. Effect of a blackout in pediatric patients with home medical devices during the 2011 eastern Japan earthquake. Brain and Development. 2014;36:143–7.
Rand DA, Mener DJ, Lerner EB, DeRobertis N. The effect of an 18-hour electrical power outage on an urban emergency medical services system. Prehosp Emerg Care. 2005;9:391–7.
Greenwald PW, Rutherford AF, Green RA, Giglio J. Emergency department visits for home medical device failure during the 2003 North America blackout. Acad Emerg Med. 2004;11:786–9.
Rajkomar A, Mayer A, Blandford A. Understanding safety-critical interactions with a home medical device through distributed cognition. J Biomed Inform. 2015;56:179–94.
Tennankore KK, D’Gama C, Faratro R, Fung S, Wong E, Chan CT. Adverse technical events in home hemodialysis. Am J Kidney Dis. 2014;65(1):116–21.
Su C-L, Lee C-N, Chen H-C, Feng L-P, Lin H-W, Chiang L-L. Comparison of domiciliary oxygen using liquid oxygen and concentrator in northern Taiwan. J Formos Med Assoc. 2014;113:23–32.
Paul J, Otvos T. Comparison of nasal cannulas and the OxyArm in patients requiring chronic domiciliary oxygen therapy. Can Respir J. 2006;13:421–6.
Ao P, Sebastianski M, Selvarajah V, Gramlich L. Comparison of complication rates, types, and average tube patency between jejunostomy tubes and percutaneous gastrostomy tubes in a regional home enteral nutrition support program. Nutr Clin Pract. 2015;30:393–7.
Leger SS. Humidification des voies aériennes lors de la ventilation à domicile. Rev Mal Respir. 2005;22:1065–70.
Gregoretti C, Navalesi P, Ghannadian S, Carlucci A, Pelosi P. Choosing a ventilator for home mechanical ventilation. Breathe. 2013;9:394–409.
Chatburn RL. Which ventilators and modes can be used to deliver noninvasive ventilation? Respir Care. 2009;54:85–101.
Farrington K, Greenwood R. Home haemodialysis: trends in technology. NDT Plus. 2011;4:iii23–4.
PubMed PubMed Central Google Scholar
Scala R. Bi-level home ventilators for non invasive positive pressure ventilation. Monaldi Arch Chest Dis – Pulm Ser. 2004:213–21.
Khirani S, Louis B, Leroux K, Delord V, Fauroux B, Lofaso F. Harms of unintentional leaks during volume targeted pressure support ventilation. Respir Med. 2013;107:1021–9.
Kropff J, Del Favero S, Place J, Toffanin C, Visentin R, Monaro M, et al. 2 month evening and night closed-loop glucose control in patients with type 1 diabetes under free-living conditions: a randomised crossover trial. Lancet Diabetes Endocrinol. 2015;3:939–47.
Yik YI, Ismail KA, Hutson JM, Southwell BR. Home transcutaneous electrical stimulation to treat children with slow-transit constipation. J Pediatr Surg. 2012;47:1285–90.
Prenton S, Kenney LP, Stapleton C, Cooper G, Reeves ML, Heller BW, et al. Feasibility study of a take-home Array-based functional electrical stimulation system with automated setup for current functional electrical stimulation users with foot-drop. Arch Phys Med Rehabil. 2014;95:1870–7.
Bostelman R, Ryu J-C, Chang T, Johnson J, Agrawal SK. An advanced patient lift and transfer device for the home. J Med Device. 2010;4:11004.
Hanada E, Kudou T. Ensuring electromagnetic compatibility between medical devices and wireless communications and measures against electromagnetic noise. Trans Jpn Soc Med Biol Eng. 2014;52:OS-43–4.
Dubois P, Bérenger E. La ventilation à domicile. IRBM. 2009;30:258–61.
Agar JWM, Perkins A, Tjipto A. Solar-assisted hemodialysis. Clin J Am Soc Nephrol. 2012;7:310–4.
Pourtier J. La technologie au service d’une meilleure prise en charge de la douleur au domicile. La Rev l’infirmière. 2013;190:36–8.
Matsui K, Kataoka A, Yamamoto A, Tanoue K, Kurosawa K, Shibasaki J, et al. Clinical characteristics and outcomes of Möbius syndrome in a children’s hospital. Pediatr Neurol. 2014;51:781–9.
Feudtner C, Villareale NL, Morray B, Sharp V, Hays RM, Neff JM. Technology-dependency among patients discharged from a children’s hospital: a retrospective cohort study. BMC Pediatr. 2005;May 9;5(1):8.
Brown KA, Bertolizio G, Leone M, Dain SL. Home noninvasive ventilation: what does the anesthesiologist need to know? Anesthesiology. 2012;117:657–68.
Michihata N, Matsui H, Fushimi K, Yasunaga H. Clinical features of adult patients admitted to pediatric wards in Japan. J Adolesc Health. 2015;57:421–4.
Han YJ, Park JD, Lee B, Choi YH, Suh DI, Lim BC, et al. Home mechanical ventilation in childhood-onset hereditary neuromuscular diseases: 13 years’ experience at a single center in Korea. PLoS One. 2015;10:e0122346.
Lee ADW, Galvao FHF, Dias MCG, Cruz ME, Marin M, Pedrol CN, et al. Home parenteral nutrition program and referral of potential candidates for intestinal and multivisceral transplantation in a single Brazilian center. Transplant Proc. 2014;46:1839–41.
Amin RS, Fitton CM. Tracheostomy and home ventilation in children. Semin Neonatol. 2003;8:127–35.
Southey D, Pullinger D, Loggos S, Kumari N, Lengyel E, Morgan I, et al. Discharge of thoracic patients on portable digital suction: is it cost-effective? Asian Cardiovasc Thorac Ann. 2015;23:832–8.
Hendrickson E, Corrigan ML. Navigating reimbursement for home parenteral nutrition. Nutr Clin Pract. 2013;28:566–71.
Weiler-Ravell D. The quandary of home-care respiratory management. Isr Med Assoc J. 2002;4:459–60.
Short D, Norwood J. Why is high-tech healthcare at home purchasing underdeveloped and what could be done to improve it? Health Serv Manag Res. 2003;16:127–35.
Download references
Acknowledgements
The authors thank Ronnie van de Riet, head of the Medical Technical Care Team of the hospital ZiekenhuisGroep Twente, for his time and commitment to this project.
Not applicable.
Availability of data and materials
The dataset generated and/or analyzed during the current study are available in Table 3 .
Author information
Authors and affiliations.
Saxion University of Applied Sciences, Research Group Technology, Health & Care (TH&C), P.O. Box 70.000, 7500, KB, Enschede, The Netherlands
Ingrid ten Haken & Somaya Ben Allouch
Department Health Technology & Services Research (HTSR), University of Twente, Faculty Behavioural, Management and Social Sciences (BMS), Ravelijn 5246, P.O. Box 217, 7500, AE, Enschede, The Netherlands
Wim H. van Harten
Rijnstate General Hospital, Arnhem, The Netherlands
You can also search for this author in PubMed Google Scholar
Contributions
All authors meet the criteria for authorship and all those entitled to authorship are listed as authors. ITH made the conception and design of the study; acquisition, analysis and interpretation of data; and drafting the article. SBA and WVH have made substantial contributions to the conception and design of the study; the analysis and interpretation of data; and revising the article critically for important intellectual content. All authors have approved the final article, this submission and its publication.
Corresponding author
Correspondence to Ingrid ten Haken .
Ethics declarations
Author’s information.
Ingrid ten Haken is researcher in the research group Technology, Health & Care at Saxion University of Applied Sciences, Enschede, The Netherlands. Somaya Ben Allouch is head of the research group. Wim van Harten is professor at the University of Twente, Faculty Behavioural, Management and Social Sciences, department Health Technology & Services Research and CEO of Rijnstate general hospital, Arnhem, The Netherlands.
Ethics approval and consent to participate
Consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
ten Haken, I., Ben Allouch, S. & van Harten, W.H. The use of advanced medical technologies at home: a systematic review of the literature. BMC Public Health 18 , 284 (2018). https://doi.org/10.1186/s12889-018-5123-4
Download citation
Received : 03 October 2017
Accepted : 26 January 2018
Published : 26 February 2018
DOI : https://doi.org/10.1186/s12889-018-5123-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Home health nursing
- Medical technologies
- Patient safety
- Quality of health care
- Systematic review
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Research article
- Open access
- Published: 10 April 2021
The role of artificial intelligence in healthcare: a structured literature review
- Silvana Secinaro 1 ,
- Davide Calandra 1 ,
- Aurelio Secinaro 2 ,
- Vivek Muthurangu 3 &
- Paolo Biancone 1
BMC Medical Informatics and Decision Making volume 21 , Article number: 125 ( 2021 ) Cite this article
152k Accesses
269 Citations
25 Altmetric
Metrics details
Background/Introduction
Artificial intelligence (AI) in the healthcare sector is receiving attention from researchers and health professionals. Few previous studies have investigated this topic from a multi-disciplinary perspective, including accounting, business and management, decision sciences and health professions.
The structured literature review with its reliable and replicable research protocol allowed the researchers to extract 288 peer-reviewed papers from Scopus. The authors used qualitative and quantitative variables to analyse authors, journals, keywords, and collaboration networks among researchers. Additionally, the paper benefited from the Bibliometrix R software package.
The investigation showed that the literature in this field is emerging. It focuses on health services management, predictive medicine, patient data and diagnostics, and clinical decision-making. The United States, China, and the United Kingdom contributed the highest number of studies. Keyword analysis revealed that AI can support physicians in making a diagnosis, predicting the spread of diseases and customising treatment paths.
Conclusions
The literature reveals several AI applications for health services and a stream of research that has not fully been covered. For instance, AI projects require skills and data quality awareness for data-intensive analysis and knowledge-based management. Insights can help researchers and health professionals understand and address future research on AI in the healthcare field.
Peer Review reports
Artificial intelligence (AI) generally applies to computational technologies that emulate mechanisms assisted by human intelligence, such as thought, deep learning, adaptation, engagement, and sensory understanding [ 1 , 2 ]. Some devices can execute a role that typically involves human interpretation and decision-making [ 3 , 4 ]. These techniques have an interdisciplinary approach and can be applied to different fields, such as medicine and health. AI has been involved in medicine since as early as the 1950s, when physicians made the first attempts to improve their diagnoses using computer-aided programs [ 5 , 6 ]. Interest and advances in medical AI applications have surged in recent years due to the substantially enhanced computing power of modern computers and the vast amount of digital data available for collection and utilisation [ 7 ]. AI is gradually changing medical practice. There are several AI applications in medicine that can be used in a variety of medical fields, such as clinical, diagnostic, rehabilitative, surgical, and predictive practices. Another critical area of medicine where AI is making an impact is clinical decision-making and disease diagnosis. AI technologies can ingest, analyse, and report large volumes of data across different modalities to detect disease and guide clinical decisions [ 3 , 8 ]. AI applications can deal with the vast amount of data produced in medicine and find new information that would otherwise remain hidden in the mass of medical big data [ 9 , 10 , 11 ]. These technologies can also identify new drugs for health services management and patient care treatments [ 5 , 6 ].
Courage in the application of AI is visible through a search in the primary research databases. However, as Meskò et al. [ 7 ] find, the technology will potentially reduce care costs and repetitive operations by focusing the medical profession on critical thinking and clinical creativity. As Cho et al. and Doyle et al. [ 8 , 9 ] add, the AI perspective is exciting; however, new studies will be needed to establish the efficacy and applications of AI in the medical field [ 10 ].
Our paper will also concentrate on AI strategies for healthcare from the accounting, business, and management perspectives. The authors used the structured literature review (SLR) method for its reliable and replicable research protocol [ 11 ] and selected bibliometric variables as sources of investigation. Bibliometric usage enables the recognition of the main quantitative variables of the study stream [ 12 ]. This method facilitates the detection of the required details of a particular research subject, including field authors, number of publications, keywords for interaction between variables (policies, properties and governance) and country data [ 13 ]. It also allows the application of the science mapping technique [ 14 ]. Our paper adopted the Bibliometrix R package and the biblioshiny web interface as tools of analysis [ 14 ].
The investigation offers the following insights for future researchers and practitioners:
bibliometric information on 288 peer-reviewed English papers from the Scopus collection.
Identification of leading journals in this field, such as Journal of Medical Systems, Studies in Health Technology and Informatics, IEEE Journal of Biomedical and Health Informatics, and Decision Support Systems.
Qualitative and quantitative information on authors’ Lotka’s law, h-index, g-index, m-index, keyword, and citation data.
Research on specific countries to assess AI in the delivery and effectiveness of healthcare, quotes, and networks within each region.
A topic dendrogram study that identifies five research clusters: health services management, predictive medicine, patient data, diagnostics, and finally, clinical decision-making.
An in-depth discussion that develops theoretical and practical implications for future studies.
The paper is organised as follows. Section 2 lists the main bibliometric articles in this field. Section 3 elaborates on the methodology. Section 4 presents the findings of the bibliometric analysis. Section 5 discusses the main elements of AI in healthcare based on the study results. Section 6 concludes the article with future implications for research.
Related works and originality
As suggested by Zupic and Čater [ 15 ], a research stream can be evaluated with bibliometric methods that can introduce objectivity and mitigate researcher bias. For this reason, bibliometric methods are attracting increasing interest among researchers as a reliable and impersonal research analytical approach [ 16 , 17 ]. Recently, bibliometrics has been an essential method for analysing and predicting research trends [ 18 ]. Table 1 lists other research that has used a similar approach in the research stream investigated.
The scientific articles reported show substantial differences in keywords and research topics that have been previously studied. The bibliometric analysis of Huang et al. [ 19 ] describes rehabilitative medicine using virtual reality technology. According to the authors, the primary goal of rehabilitation is to enhance and restore functional ability and quality of life for patients with physical impairments or disabilities. In recent years, many healthcare disciplines have been privileged to access various technologies that provide tools for both research and clinical intervention.
Hao et al. [ 20 ] focus on text mining in medical research. As reported, text mining reveals new, previously unknown information by using a computer to automatically extract information from different text resources. Text mining methods can be regarded as an extension of data mining to text data. Text mining is playing an increasingly significant role in processing medical information. Similarly, the studies by dos Santos et al. [ 21 ] focus on applying data mining and machine learning (ML) techniques to public health problems. As stated in this research, public health may be defined as the art and science of preventing diseases, promoting health, and prolonging life. Using data mining and ML techniques, it is possible to discover new information that otherwise would be hidden. These two studies are related to another topic: medical big data. According to Liao et al. [ 22 ], big data is a typical “buzzword” in the business and research community, referring to a great mass of digital data collected from various sources. In the medical field, we can obtain a vast amount of data (i.e., medical big data). Data mining and ML techniques can help deal with this information and provide helpful insights for physicians and patients. More recently, Choudhury et al. [ 23 ] provide a systematic review on the use of ML to improve the care of elderly patients, demonstrating eligible studies primarily in psychological disorders and eye diseases.
Tran et al. [ 2 ] focus on the global evolution of AI research in medicine. Their bibliometric analysis highlights trends and topics related to AI applications and techniques. As stated in Connelly et al.’s [ 24 ] study, robot-assisted surgeries have rapidly increased in recent years. Their bibliometric analysis demonstrates how robotic-assisted surgery has gained acceptance in different medical fields, such as urological, colorectal, cardiothoracic, orthopaedic, maxillofacial and neurosurgery applications. Additionally, the bibliometric analysis of Guo et al. [ 25 ] provides an in-depth study of AI publications through December 2019. The paper focuses on tangible AI health applications, giving researchers an idea of how algorithms can help doctors and nurses. A new stream of research related to AI is also emerging. In this sense, Choudhury and Asan’s [ 26 ] scientific contribution provides a systematic review of the AI literature to identify health risks for patients. They report on 53 studies involving technology for clinical alerts, clinical reports, and drug safety. Considering the considerable interest within this research stream, this analysis differs from the current literature for several reasons. It aims to provide in-depth discussion, considering mainly the business, management, and accounting fields and not dealing only with medical and health profession publications.
Additionally, our analysis aims to provide a bibliometric analysis of variables such as authors, countries, citations and keywords to guide future research perspectives for researchers and practitioners, as similar analyses have done for several publications in other research streams [ 15 , 16 , 27 ]. In doing so, we use a different database, Scopus, that is typically adopted in social sciences fields. Finally, our analysis will propose and discuss a dominant framework of variables in this field, and our analysis will not be limited to AI application descriptions.
Methodology
This paper evaluated AI in healthcare research streams using the SLR method [ 11 ]. As suggested by Massaro et al. [ 11 ], an SLR enables the study of the scientific corpus of a research field, including the scientific rigour, reliability and replicability of operations carried out by researchers. As suggested by many scholars, the methodology allows qualitative and quantitative variables to highlight the best authors, journals and keywords and combine a systematic literature review and bibliometric analysis [ 27 , 28 , 29 , 30 ]. Despite its widespread use in business and management [ 16 , 31 ], the SLR is also used in the health sector based on the same philosophy through which it was originally conceived [ 32 , 33 ]. A methodological analysis of previously published articles reveals that the most frequently used steps are as follows [ 28 , 31 , 34 ]:
defining research questions;
writing the research protocol;
defining the research sample to be analysed;
developing codes for analysis; and
critically analysing, discussing, and identifying a future research agenda.
Considering the above premises, the authors believe that an SLR is the best method because it combines scientific validity, replicability of the research protocol and connection between multiple inputs.
As stated by the methodological paper, the first step is research question identification. For this purpose, we benefit from the analysis of Zupic and Čater [ 15 ], who provide several research questions for future researchers to link the study of authors, journals, keywords and citations. Therefore, RQ1 is “What are the most prominent authors, journal keywords and citations in the field of the research study?” Additionally, as suggested by Haleem et al. [ 35 ], new technologies, including AI, are changing the medical field in unexpected timeframes, requiring studies in multiple areas. Therefore, RQ2 is “How does artificial intelligence relate to healthcare, and what is the focus of the literature?” Then, as discussed by Massaro et al. [ 36 ], RQ3 is “What are the research applications of artificial intelligence for healthcare?”.
The first research question aims to define the qualitative and quantitative variables of the knowledge flow under investigation. The second research question seeks to determine the state of the art and applications of AI in healthcare. Finally, the third research question aims to help researchers identify practical and theoretical implications and future research ideas in this field.
The second fundamental step of the SLR is writing the research protocol [ 11 ]. Table 2 indicates the currently known literature elements, uniquely identifying the research focus, motivations and research strategy adopted and the results providing a link with the following points. Additionally, to strengthen the analysis, our investigation benefits from the PRISMA statement methodological article [ 37 ]. Although the SLR is a validated method for systematic reviews and meta-analyses, we believe that the workflow provided may benefit the replicability of the results [ 37 , 38 , 39 , 40 ]. Figure 1 summarises the researchers’ research steps, indicating that there are no results that can be referred to as a meta-analysis.
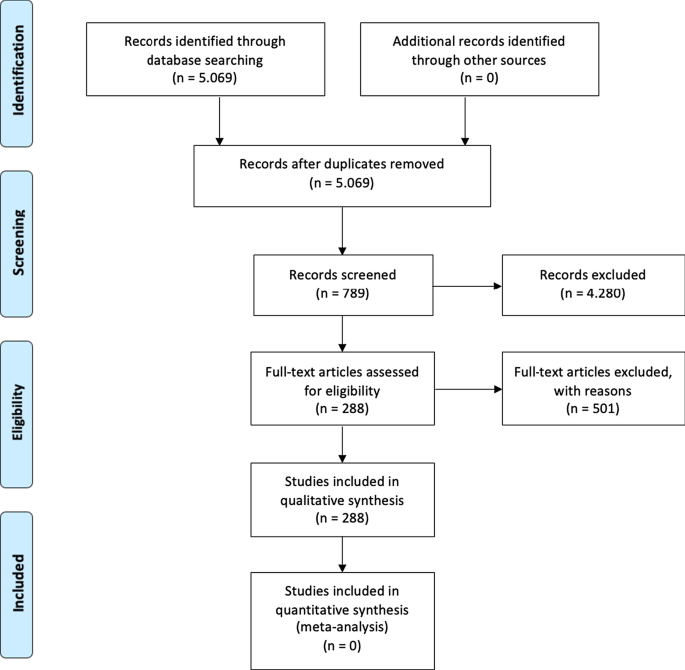
Source : Authors’ elaboration on Liberati et al. [ 37 ]
PRISMA workflow.
The third step is to specify the search strategy and search database. Our analysis is based on the search string “Artificial Intelligence” OR “AI” AND “Healthcare” with a focus on “Business, Management, and Accounting”, “Decision Sciences”, and “Health professions”. As suggested by [ 11 , 41 ] and motivated by [ 42 ], keywords can be selected through a top-down approach by identifying a large search field and then focusing on particular sub-topics. The paper uses data retrieved from the Scopus database, a multi-disciplinary database, which allowed the researchers to identify critical articles for scientific analysis [ 43 ]. Additionally, Scopus was selected based on Guo et al.’s [ 25 ] limitations, which suggest that “future studies will apply other databases, such as Scopus, to explore more potential papers” . The research focuses on articles and reviews published in peer-reviewed journals for their scientific relevance [ 11 , 16 , 17 , 29 ] and does not include the grey literature, conference proceedings or books/book chapters. Articles written in any language other than English were excluded [ 2 ]. For transparency and replicability, the analysis was conducted on 11 January 2021. Using this research strategy, the authors retrieved 288 articles. To strengthen the study's reliability, we publicly provide the full bibliometric extract on the Zenodo repository [ 44 , 45 ].
The fourth research phase is defining the code framework that initiates the analysis of the variables. The study will identify the following:
descriptive information of the research area;
source analysis [ 16 ];
author and citation analysis [ 28 ];
keywords and network analysis [ 14 ]; and
geographic distribution of the papers [ 14 ].
The final research phase is the article’s discussion and conclusion, where implications and future research trends will be identified.
At the research team level, the information is analysed with the statistical software R-Studio and the Bibliometrix package [ 15 ], which allows scientific analysis of the results obtained through the multi-disciplinary database.
The analysis of bibliometric results starts with a description of the main bibliometric statistics with the aim of answering RQ1, What are the most prominent authors, journal keywords and citations in the field of the research study?, and RQ2, How does artificial intelligence relate to healthcare, and what is the focus of the literature? Therefore, the following elements were thoroughly analysed: (1) type of document; (2) annual scientific production; (3) scientific sources; (4) source growth; (5) number of articles per author; (6) author’s dominance ranking; (7) author’s h-index, g-index, and m-index; (8) author’s productivity; (9) author’s keywords; (10) topic dendrogram; (11) a factorial map of the document with the highest contributions; (12) article citations; (13) country production; (14) country citations; (15) country collaboration map; and (16) country collaboration network.
Main information
Table 3 shows the information on 288 peer-reviewed articles published between 1992 and January 2021 extracted from the Scopus database. The number of keywords is 946 from 136 sources, and the number of keywords plus, referring to the number of keywords that frequently appear in an article’s title, was 2329. The analysis period covered 28 years and 1 month of scientific production and included an annual growth rate of 5.12%. However, the most significant increase in published articles occurred in the past three years (please see Fig. 2 ). On average, each article was written by three authors (3.56). Finally, the collaboration index (CI), which was calculated as the total number of authors of multi-authored articles/total number of multi-authored articles, was 3.97 [ 46 ].
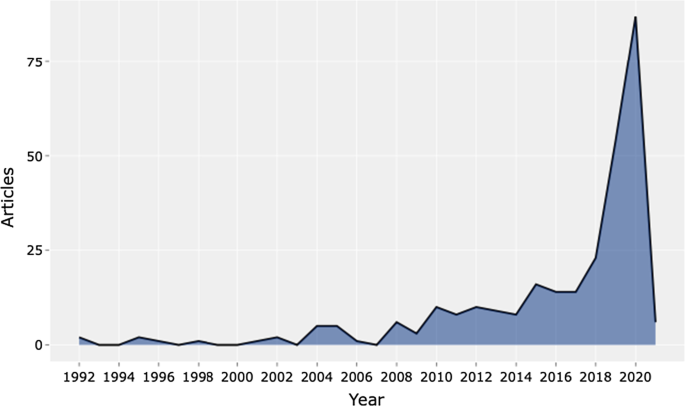
Source : Authors’ elaboration
Annual scientific production.
Table 4 shows the top 20 sources related to the topic. The Journal of Medical Systems is the most relevant source, with twenty-one of the published articles. This journal's main issues are the foundations, functionality, interfaces, implementation, impacts, and evaluation of medical technologies. Another relevant source is Studies in Health Technology and Informatics, with eleven articles. This journal aims to extend scientific knowledge related to biomedical technologies and medical informatics research. Both journals deal with cloud computing, machine learning, and AI as a disruptive healthcare paradigm based on recent publications. The IEEE Journal of Biomedical and Health Informatics investigates technologies in health care, life sciences, and biomedicine applications from a broad perspective. The next journal, Decision Support Systems, aims to analyse how these technologies support decision-making from a multi-disciplinary view, considering business and management. Therefore, the analysis of the journals revealed that we are dealing with an interdisciplinary research field. This conclusion is confirmed, for example, by the presence of purely medical journals, journals dedicated to the technological growth of healthcare, and journals with a long-term perspective such as futures.
The distribution frequency of the articles (Fig. 3 ) indicates the journals dealing with the topic and related issues. Between 2008 and 2012, a significant growth in the number of publications on the subject is noticeable. However, the graph shows the results of the Loess regression, which includes the quantity and publication time of the journal under analysis as variables. This method allows the function to assume an unlimited distribution; that is, feature can consider values below zero if the data are close to zero. It contributes to a better visual result and highlights the discontinuity in the publication periods [ 47 ].
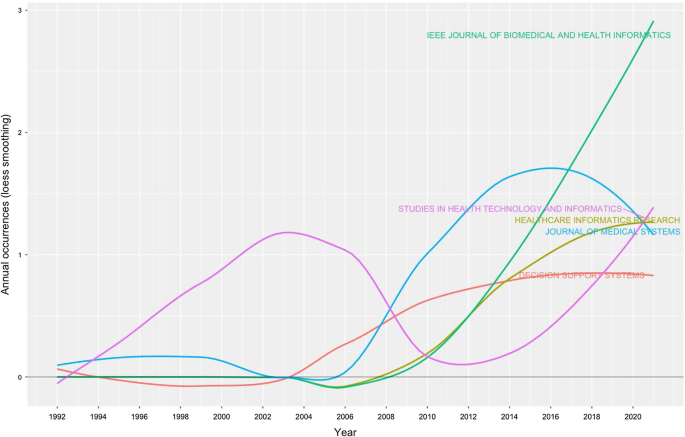
Source growth. Source : Authors’ elaboration
Finally, Fig. 4 provides an analytical perspective on factor analysis for the most cited papers. As indicated in the literature [ 48 , 49 ], using factor analysis to discover the most cited papers allows for a better understanding of the scientific world’s intellectual structure. For example, our research makes it possible to consider certain publications that effectively analyse subject specialisation. For instance, Santosh’s [ 50 ] article addresses the new paradigm of AI with ML algorithms for data analysis and decision support in the COVID-19 period, setting a benchmark in terms of citations by researchers. Moving on to the application, an article by Shickel et al. [ 51 ] begins with the belief that the healthcare world currently has much health and administrative data. In this context, AI and deep learning will support medical and administrative staff in extracting data, predicting outcomes, and learning medical representations. Finally, in the same line of research, Baig et al. [ 52 ], with a focus on wearable patient monitoring systems (WPMs), conclude that AI and deep learning may be landmarks for continuous patient monitoring and support for healthcare delivery.
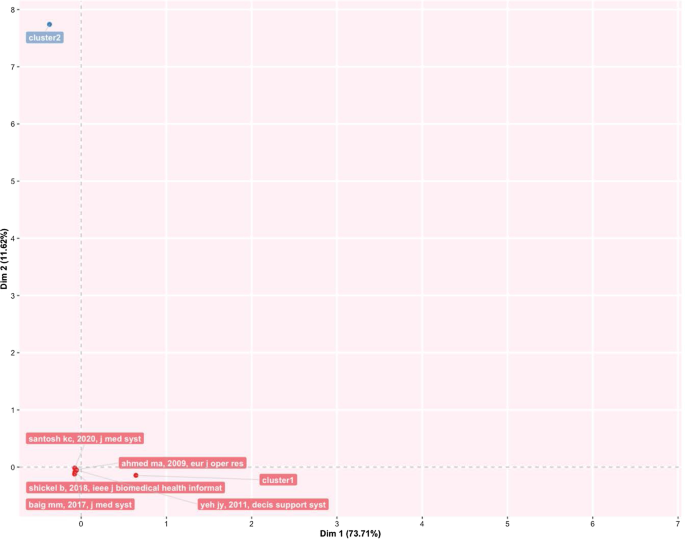
Factorial map of the most cited documents.
This section identifies the most cited authors of articles on AI in healthcare. It also identifies the authors’ keywords, dominance factor (DF) ranking, h-index, productivity, and total number of citations. Table 5 identifies the authors and their publications in the top 20 rankings. As the table shows, Bushko R.G. has the highest number of publications: four papers. He is the editor-in-chief of Future of Health Technology, a scientific journal that aims to develop a clear vision of the future of health technology. Then, several authors each wrote three papers. For instance, Liu C. is a researcher active in the topic of ML and computer vision, and Sharma A. from Emory University Atlanta in the USA is a researcher with a clear focus on imaging and translational informatics. Some other authors have two publications each. While some authors have published as primary authors, most have published as co-authors. Hence, in the next section, we measure the contributory power of each author by investigating the DF ranking through the number of elements.
Authors’ dominance ranking
The dominance factor (DF) is a ratio measuring the fraction of multi-authored articles in which an author acts as the first author [ 53 ]. Several bibliometric studies use the DF in their analyses [ 46 , 54 ]. The DF ranking calculates an author’s dominance in producing articles. The DF is calculated by dividing the number of an author’s multi-authored papers as the first author (Nmf) by the author's total number of multi-authored papers (Nmt). This is omitted in the single-author case due to the constant value of 1 for single-authored articles. This formulation could lead to some distortions in the results, especially in fields where the first author is entered by surname alphabetical order [ 55 ].
The mathematical equation for the DF is shown as:
Table 6 lists the top 20 DF rankings. The data in the table show a low level of articles per author, either for first-authored or multi-authored articles. The results demonstrate that we are dealing with an emerging topic in the literature. Additionally, as shown in the table, Fox J. and Longoni C. are the most dominant authors in the field.
Authors’ impact
Table 7 shows the impact of authors in terms of the h-index [ 56 ] (i.e., the productivity and impact of citations of a researcher), g-index [ 57 ] (i.e., the distribution of citations received by a researcher's publications), m-index [ 58 ] (i.e., the h-index value per year), total citations, total paper and years of scientific publication. The H-index was introduced in the literature as a metric for the objective comparison of scientific results and depended on the number of publications and their impact [ 59 ]. The results show that the 20 most relevant authors have an h-index between 2 and 1. For the practical interpretation of the data, the authors considered data published by the London School of Economics [ 60 ]. In the social sciences, the analysis shows values of 7.6 for economic publications by professors and researchers who had been active for several years. Therefore, the youthfulness of the research area has attracted young researchers and professors. At the same time, new indicators have emerged over the years to diversify the logic of the h-index. For example, the g-index indicates an author's impact on citations, considering that a single article can generate these. The m-index, on the other hand, shows the cumulative value over the years.
The analysis, also considering the total number of citations, the number of papers published and the year of starting to publish, thus confirms that we are facing an expanding research flow.
Authors’ productivity
Figure 5 shows Lotka’s law. This mathematical formulation originated in 1926 to describe the publication frequency by authors in a specific research field [ 61 ]. In practice, the law states that the number of authors contributing to research in a given period is a fraction of the number who make up a single contribution [ 14 , 61 ].
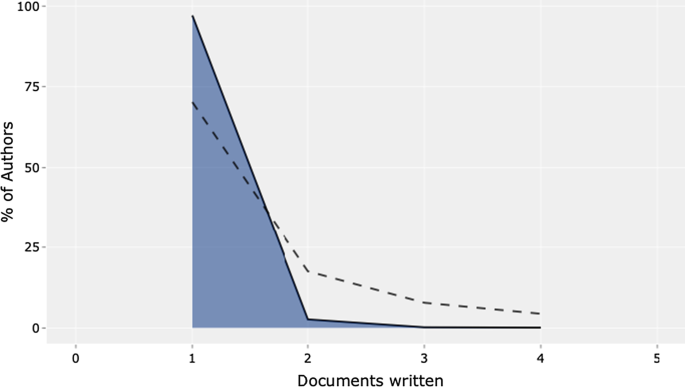
Lotka’s law.
The mathematical relationship is expressed in reverse in the following way:
where y x is equal to the number of authors producing x articles in each research field. Therefore, C and n are constants that can be estimated in the calculation.
The figure's results are in line with Lotka's results, with an average of two publications per author in a given research field. In addition, the figure shows the percentage of authors. Our results lead us to state that we are dealing with a young and growing research field, even with this analysis. Approximately 70% of the authors had published only their first research article. Only approximately 20% had published two scientific papers.
Authors’ keywords
This section provides information on the relationship between the keywords artificial intelligence and healthcare . This analysis is essential to determine the research trend, identify gaps in the discussion on AI in healthcare, and identify the fields that can be interesting as research areas [ 42 , 62 ].
Table 8 highlights the total number of keywords per author in the top 20 positions. The ranking is based on the following elements: healthcare, artificial intelligence, and clinical decision support system . Keyword analysis confirms the scientific area of reference. In particular, we deduce the definition as “Artificial intelligence is the theory and development of computer systems able to perform tasks normally requiring human intelligence, such as visual perception, speech recognition, decision-making, and translation between languages” [ 2 , 63 ]. Panch et al. [ 4 ] find that these technologies can be used in different business and management areas. After the first keyword, the analysis reveals AI applications and related research such as machine learning and deep learning.
Additionally, data mining and big data are a step forward in implementing exciting AI applications. According to our specific interest, if we applied AI in healthcare, we would achieve technological applications to help and support doctors and medical researchers in decision-making. The link between AI and decision-making is the reason why we find, in the seventh position, the keyword clinical decision support system . AI techniques can unlock clinically relevant information hidden in the massive amount of data that can assist clinical decision-making [ 64 ]. If we analyse the following keywords, we find other elements related to decision-making and support systems.
The TreeMap below (Fig. 6 ) highlights the combination of possible keywords representing AI and healthcare.
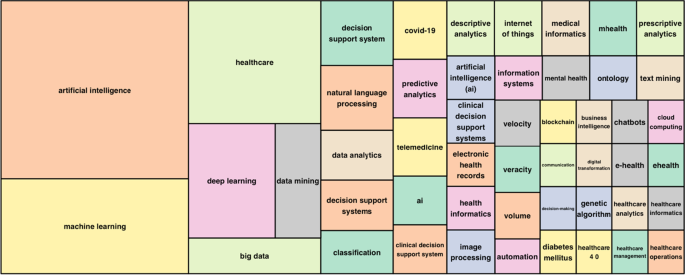
Keywords treemap.
The topic dendrogram in Fig. 7 represents the hierarchical order and the relationship between the keywords generated by hierarchical clustering [ 42 ]. The cut in the figure and the vertical lines facilitate an investigation and interpretation of the different clusters. As stated by Andrews [ 48 ], the figure is not intended to find the perfect level of associations between clusters. However, it aims to estimate the approximate number of clusters to facilitate further discussion.
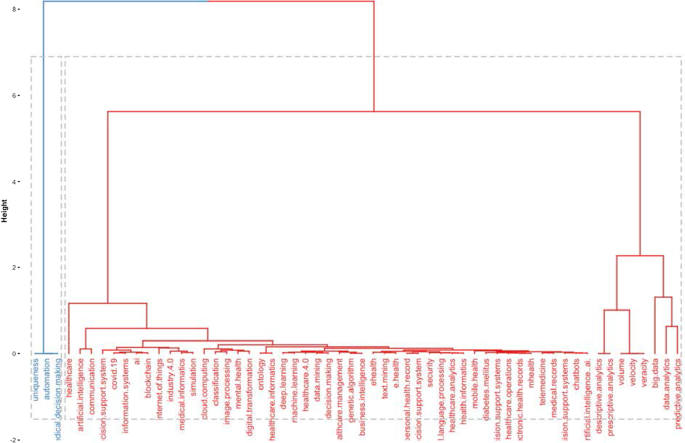
Topic dendrogram.
The research stream of AI in healthcare is divided into two main strands. The blue strand focuses on medical information systems and the internet. Some papers are related to healthcare organisations, such as the Internet of Things, meaning that healthcare organisations use AI to support health services management and data analysis. AI applications are also used to improve diagnostic and therapeutic accuracy and the overall clinical treatment process [ 2 ]. If we consider the second block, the red one, three different clusters highlight separate aspects of the topic. The first could be explained as AI and ML predictive algorithms. Through AI applications, it is possible to obtain a predictive approach that can ensure that patients are better monitored. This also allows a better understanding of risk perception for doctors and medical researchers. In the second cluster, the most frequent words are decisions , information system , and support system . This means that AI applications can support doctors and medical researchers in decision-making. Information coming from AI technologies can be used to consider difficult problems and support a more straightforward and rapid decision-making process. In the third cluster, it is vital to highlight that the ML model can deal with vast amounts of data. From those inputs, it can return outcomes that can optimise the work of healthcare organisations and scheduling of medical activities.
Furthermore, the word cloud in Fig. 8 highlights aspects of AI in healthcare, such as decision support systems, decision-making, health services management, learning systems, ML techniques and diseases. The figure depicts how AI is linked to healthcare and how it is used in medicine.
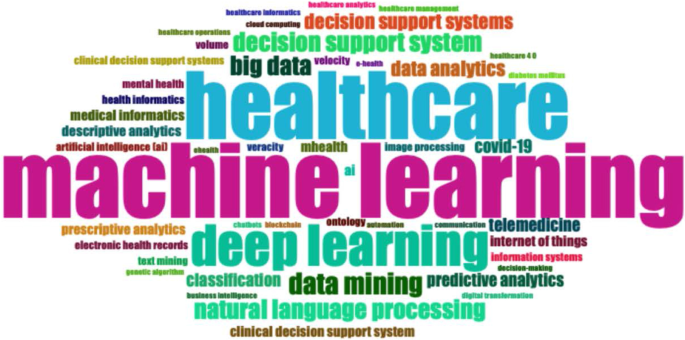
Word cloud.
Figure 9 represents the search trends based on the keywords analysed. The research started in 2012. First, it identified research topics related to clinical decision support systems. This topic was recurrent during the following years. Interestingly, in 2018, studies investigated AI and natural language processes as possible tools to manage patients and administrative elements. Finally, a new research stream considers AI's role in fighting COVID-19 [ 65 , 66 ].
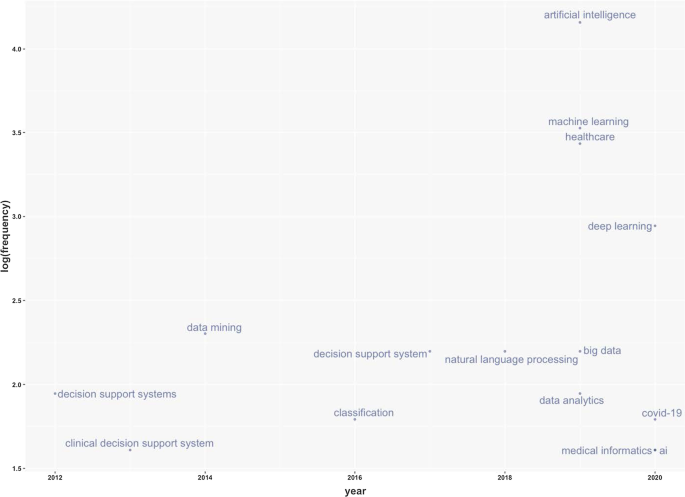
Keywords frequency.
Table 9 represents the number of citations from other articles within the top 20 rankings. The analysis allows the benchmark studies in the field to be identified [ 48 ]. For instance, Burke et al. [ 67 ] writes the most cited paper and analyses efficient nurse rostering methodologies. The paper critically evaluates tangible interdisciplinary solutions that also include AI. Immediately thereafter, Ahmed M.A.'s article proposes a data-driven optimisation methodology to determine the optimal number of healthcare staff to optimise patients' productivity [ 68 ]. Finally, the third most cited article lays the groundwork for developing deep learning by considering diverse health and administrative information [ 51 ].
This section analyses the diffusion of AI in healthcare around the world. It highlights countries to show the geographies of this research. It includes all published articles, the total number of citations, and the collaboration network. The following sub-sections start with an analysis of the total number of published articles.
Country total articles
Figure 9 and Table 10 display the countries where AI in healthcare has been considered. The USA tops the list of countries with the maximum number of articles on the topic (215). It is followed by China (83), the UK (54), India (51), Australia (54), and Canada (32). It is immediately evident that the theme has developed on different continents, highlighting a growing interest in AI in healthcare. The figure shows that many areas, such as Russia, Eastern Europe and Africa except for Algeria, Egypt, and Morocco, have still not engaged in this scientific debate.
Country publications and collaboration map
This section discusses articles on AI in healthcare in terms of single or multiple publications in each country. It also aims to observe collaboration and networking between countries. Table 11 and Fig. 10 highlight the average citations by state and show that the UK, the USA, and Kuwait have a higher average number of citations than other countries. Italy, Spain and New Zealand have the most significant number of citations.
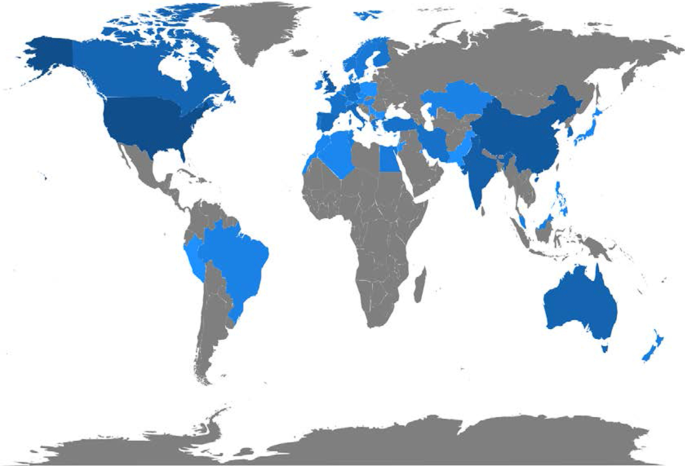
Articles per country.
Figure 11 depicts global collaborations. The blue colour on the map represents research cooperation among nations. Additionally, the pink border linking states indicates the extent of collaboration between authors. The primary cooperation between nations is between the USA and China, with two collaborative articles. Other collaborations among nations are limited to a few papers.
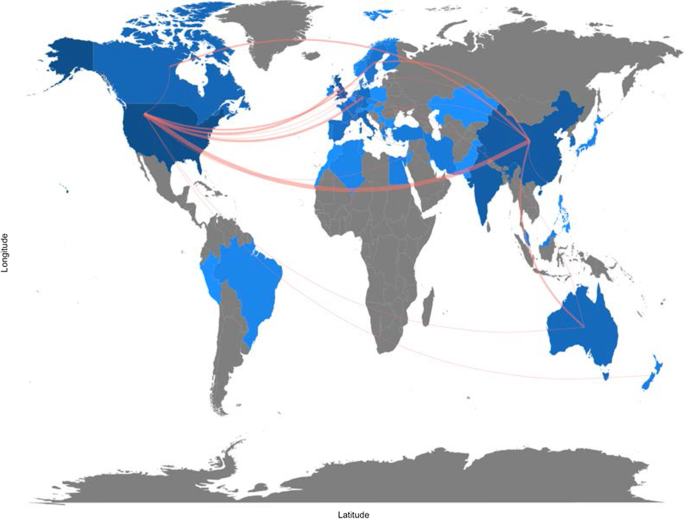
Collaboration map.
Artificial intelligence for healthcare: applications
This section aims to strengthen the research scope by answering RQ3: What are the research applications of artificial intelligence for healthcare?
Benefiting from the topical dendrogram, researchers will provide a development model based on four relevant variables [ 69 , 70 ]. AI has been a disruptive innovation in healthcare [ 4 ]. With its sophisticated algorithms and several applications, AI has assisted doctors and medical professionals in the domains of health information systems, geocoding health data, epidemic and syndromic surveillance, predictive modelling and decision support, and medical imaging [ 2 , 9 , 10 , 64 ]. Furthermore, the researchers considered the bibliometric analysis to identify four macro-variables dominant in the field and used them as authors' keywords. Therefore, the following sub-sections aim to explain the debate on applications in healthcare for AI techniques. These elements are shown in Fig. 12 .
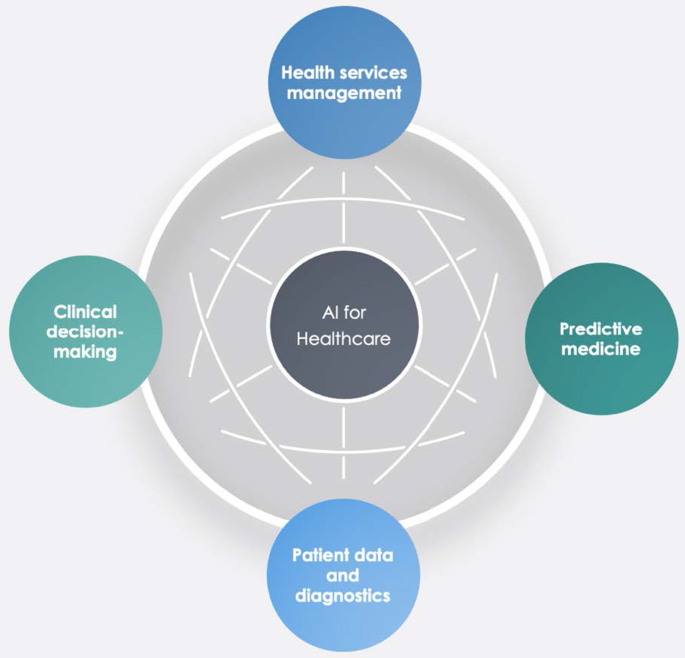
Dominant variables for AI in healthcare.
Health services management
One of the notable aspects of AI techniques is potential support for comprehensive health services management. These applications can support doctors, nurses and administrators in their work. For instance, an AI system can provide health professionals with constant, possibly real-time medical information updates from various sources, including journals, textbooks, and clinical practices [ 2 , 10 ]. These applications' strength is becoming even more critical in the COVID-19 period, during which information exchange is continually needed to properly manage the pandemic worldwide [ 71 ]. Other applications involve coordinating information tools for patients and enabling appropriate inferences for health risk alerts and health outcome prediction [ 72 ]. AI applications allow, for example, hospitals and all health services to work more efficiently for the following reasons:
Clinicians can access data immediately when they need it.
Nurses can ensure better patient safety while administering medication.
Patients can stay informed and engaged in their care by communicating with their medical teams during hospital stays.
Additionally, AI can contribute to optimising logistics processes, for instance, realising drugs and equipment in a just-in-time supply system based totally on predictive algorithms [ 73 , 74 ]. Interesting applications can also support the training of personnel working in health services. This evidence could be helpful in bridging the gap between urban and rural health services [ 75 ]. Finally, health services management could benefit from AI to leverage the multiplicity of data in electronic health records by predicting data heterogeneity across hospitals and outpatient clinics, checking for outliers, performing clinical tests on the data, unifying patient representation, improving future models that can predict diagnostic tests and analyses, and creating transparency with benchmark data for analysing services delivered [ 51 , 76 ].
Predictive medicine
Another relevant topic is AI applications for disease prediction and diagnosis treatment, outcome prediction and prognosis evaluation [ 72 , 77 ]. Because AI can identify meaningful relationships in raw data, it can support diagnostic, treatment and prediction outcomes in many medical situations [ 64 ]. It allows medical professionals to embrace the proactive management of disease onset. Additionally, predictions are possible for identifying risk factors and drivers for each patient to help target healthcare interventions for better outcomes [ 3 ]. AI techniques can also help design and develop new drugs, monitor patients and personalise patient treatment plans [ 78 ]. Doctors benefit from having more time and concise data to make better patient decisions. Automatic learning through AI could disrupt medicine, allowing prediction models to be created for drugs and exams that monitor patients over their whole lives [ 79 ].
- Clinical decision-making
One of the keyword analysis main topics is that AI applications could support doctors and medical researchers in the clinical decision-making process. According to Jiang et al. [ 64 ], AI can help physicians make better clinical decisions or even replace human judgement in healthcare-specific functional areas. According to Bennett and Hauser [ 80 ], algorithms can benefit clinical decisions by accelerating the process and the amount of care provided, positively impacting the cost of health services. Therefore, AI technologies can support medical professionals in their activities and simplify their jobs [ 4 ]. Finally, as Redondo and Sandoval [ 81 ] find, algorithmic platforms can provide virtual assistance to help doctors understand the semantics of language and learning to solve business process queries as a human being would.
Patient data and diagnostics
Another challenging topic related to AI applications is patient data and diagnostics. AI techniques can help medical researchers deal with the vast amount of data from patients (i.e., medical big data ). AI systems can manage data generated from clinical activities, such as screening, diagnosis, and treatment assignment. In this way, health personnel can learn similar subjects and associations between subject features and outcomes of interest [ 64 ].
These technologies can analyse raw data and provide helpful insights that can be used in patient treatments. They can help doctors in the diagnostic process; for example, to realise a high-speed body scan, it will be simpler to have an overall patient condition image. Then, AI technology can recreate a 3D mapping solution of a patient’s body.
In terms of data, interesting research perspectives are emerging. For instance, we observed the emergence of a stream of research on patient data management and protection related to AI applications [ 82 ].
For diagnostics, AI techniques can make a difference in rehabilitation therapy and surgery. Numerous robots have been designed to support and manage such tasks. Rehabilitation robots physically support and guide, for example, a patient’s limb during motor therapy [ 83 ]. For surgery, AI has a vast opportunity to transform surgical robotics through devices that can perform semi-automated surgical tasks with increasing efficiency. The final aim of this technology is to automate procedures to negate human error while maintaining a high level of accuracy and precision [ 84 ]. Finally, the -19 period has led to increased remote patient diagnostics through telemedicine that enables remote observation of patients and provides physicians and nurses with support tools [ 66 , 85 , 86 ].
This study aims to provide a bibliometric analysis of publications on AI in healthcare, focusing on accounting, business and management, decision sciences and health profession studies. Using the SLR method of Massaro et al. [ 11 ], we provide a reliable and replicable research protocol for future studies in this field. Additionally, we investigate the trend of scientific publications on the subject, unexplored information, future directions, and implications using the science mapping workflow. Our analysis provides interesting insights.
In terms of bibliometric variables, the four leading journals, Journal of Medical Systems , Studies in Health Technology and Informatics , IEEE Journal of Biomedical and Health Informatics , and Decision Support Systems , are optimal locations for the publication of scientific articles on this topic. These journals deal mainly with healthcare, medical information systems, and applications such as cloud computing, machine learning, and AI. Additionally, in terms of h-index, Bushko R.G. and Liu C. are the most productive and impactful authors in this research stream. Burke et al.’s [ 67 ] contribution is the most cited with an analysis of nurse rostering using new technologies such as AI. Finally, in terms of keywords, co-occurrence reveals some interesting insights. For instance, researchers have found that AI has a role in diagnostic accuracy and helps in the analysis of health data by comparing thousands of medical records, experiencing automatic learning with clinical alerts, efficient management of health services and places of care, and the possibility of reconstructing patient history using these data.
Second, this paper finds five cluster analyses in healthcare applications: health services management, predictive medicine, patient data, diagnostics, and finally, clinical decision-making. These technologies can also contribute to optimising logistics processes in health services and allowing a better allocation of resources.
Third, the authors analysing the research findings and the issues under discussion strongly support AI's role in decision support. These applications, however, are demonstrated by creating a direct link to data quality management and the technology awareness of health personnel [ 87 ].
The importance of data quality for the decision-making process
Several authors have analysed AI in the healthcare research stream, but in this case, the authors focus on other literature that includes business and decision-making processes. In this regard, the analysis of the search flow reveals a double view of the literature. On the one hand, some contributions belong to the positivist literature and embrace future applications and implications of technology for health service management, data analysis and diagnostics [ 6 , 80 , 88 ]. On the other hand, some investigations also aim to understand the darker sides of technology and its impact. For example, as Carter [ 89 ] states, the impact of AI is multi-sectoral; its development, however, calls for action to protect personal data. Similarly, Davenport and Kalakota [ 77 ] focus on the ethical implications of using AI in healthcare. According to the authors, intelligent machines raise issues of accountability, transparency, and permission, especially in automated communication with patients. Our analysis does not indicate a marked strand of the literature; therefore, we argue that the discussion of elements such as the transparency of technology for patients is essential for the development of AI applications.
A large part of our results shows that, at the application level, AI can be used to improve medical support for patients (Fig. 11 ) [ 64 , 82 ]. However, we believe that, as indicated by Kalis et al. [ 90 ] on the pages of Harvard Business Review, the management of costly back-office problems should also be addressed.
The potential of algorithms includes data analysis. There is an immense quantity of data accessible now, which carries the possibility of providing information about a wide variety of medical and healthcare activities [ 91 ]. With the advent of modern computational methods, computer learning and AI techniques, there are numerous possibilities [ 79 , 83 , 84 ]. For example, AI makes it easier to turn data into concrete and actionable observations to improve decision-making, deliver high-quality patient treatment, adapt to real-time emergencies, and save more lives on the clinical front. In addition, AI makes it easier to leverage capital to develop systems and facilities and reduce expenses at the organisational level [ 78 ]. Studying contributions to the topic, we noticed that data accuracy was included in the debate, indicating that a high standard of data will benefit decision-making practitioners [ 38 , 77 ]. AI techniques are an essential instrument for studying data and the extraction of medical insight, and they may assist medical researchers in their practices. Using computational tools, healthcare stakeholders may leverage the power of data not only to evaluate past data ( descriptive analytics ) but also to forecast potential outcomes ( predictive analytics ) and to define the best actions for the present scenario ( prescriptive analytics ) [ 78 ]. The current abundance of evidence makes it easier to provide a broad view of patient health; doctors should have access to the correct details at the right time and location to provide the proper treatment [ 92 ].
Will medical technology de-skill doctors?
Further reflection concerns the skills of doctors. Studies have shown that healthcare personnel are progressively being exposed to technology for different purposes, such as collecting patient records or diagnosis [ 71 ]. This is demonstrated by the keywords (Fig. 6 ) that focus on technology and the role of decision-making with new innovative tools. In addition, the discussion expands with Lu [ 93 ], which indicates that the excessive use of technology could hinder doctors’ skills and clinical procedures' expansion. Among the main issues arising from the literature is the possible de-skilling of healthcare staff due to reduced autonomy in decision-making concerning patients [ 94 ]. Therefore, the challenges and discussion we uncovered in Fig. 11 are expanded by also considering the ethical implications of technology and the role of skills.
Implications
Our analysis also has multiple theoretical and practical implications.
In terms of theoretical contribution, this paper extends the previous results of Connelly et al., dos Santos et al, Hao et al., Huang et al., Liao et al. and Tran et al. [ 2 , 19 , 20 , 21 , 22 , 24 ] in considering AI in terms of clinical decision-making and data management quality.
In terms of practical implications, this paper aims to create a fruitful discussion with healthcare professionals and administrative staff on how AI can be at their service to increase work quality. Furthermore, this investigation offers a broad comprehension of bibliometric variables of AI techniques in healthcare. It can contribute to advancing scientific research in this field.
Limitations
Like any other, our study has some limitations that could be addressed by more in-depth future studies. For example, using only one research database, such as Scopus, could be limiting. Further analysis could also investigate the PubMed, IEEE, and Web of Science databases individually and holistically, especially the health parts. Then, the use of search terms such as "Artificial Intelligence" OR "AI" AND "Healthcare" could be too general and exclude interesting studies. Moreover, although we analysed 288 peer-reviewed scientific papers, because the new research topic is new, the analysis of conference papers could return interesting results for future researchers. Additionally, as this is a young research area, the analysis will be subject to recurrent obsolescence as multiple new research investigations are published. Finally, although bibliometric analysis has limited the subjectivity of the analysis [ 15 ], the verification of recurring themes could lead to different results by indicating areas of significant interest not listed here.
Future research avenues
Concerning future research perspectives, researchers believe that an analysis of the overall amount that a healthcare organisation should pay for AI technologies could be helpful. If these technologies are essential for health services management and patient treatment, governments should invest and contribute to healthcare organisations' modernisation. New investment funds could be made available in the healthcare world, as in the European case with the Next Generation EU programme or national investment programmes [ 95 ]. Additionally, this should happen especially in the poorest countries around the world, where there is a lack of infrastructure and services related to health and medicine [ 96 ]. On the other hand, it might be interesting to evaluate additional profits generated by healthcare organisations with AI technologies compared to those that do not use such technologies.
Further analysis could also identify why some parts of the world have not conducted studies in this area. It would be helpful to carry out a comparative analysis between countries active in this research field and countries that are not currently involved. It would make it possible to identify variables affecting AI technologies' presence or absence in healthcare organisations. The results of collaboration between countries also present future researchers with the challenge of greater exchanges between researchers and professionals. Therefore, further research could investigate the difference in vision between professionals and academics.
In the accounting, business, and management research area, there is currently a lack of quantitative analysis of the costs and profits generated by healthcare organisations that use AI technologies. Therefore, research in this direction could further increase our understanding of the topic and the number of healthcare organisations that can access technologies based on AI. Finally, as suggested in the discussion section, more interdisciplinary studies are needed to strengthen AI links with data quality management and AI and ethics considerations in healthcare.
In pursuing the philosophy of Massaro et al.’s [ 11 ] methodological article, we have climbed on the shoulders of giants, hoping to provide a bird's-eye view of the AI literature in healthcare. We performed this study with a bibliometric analysis aimed at discovering authors, countries of publication and collaboration, and keywords and themes. We found a fast-growing, multi-disciplinary stream of research that is attracting an increasing number of authors.
The research, therefore, adopts a quantitative approach to the analysis of bibliometric variables and a qualitative approach to the study of recurring keywords, which has allowed us to demonstrate strands of literature that are not purely positive. There are currently some limitations that will affect future research potential, especially in ethics, data governance and the competencies of the health workforce.
Availability of data and materials
All the data are retrieved from public scientific platforms.
Tagliaferri SD, Angelova M, Zhao X, Owen PJ, Miller CT, Wilkin T, et al. Artificial intelligence to improve back pain outcomes and lessons learnt from clinical classification approaches: three systematic reviews. NPJ Digit Med. 2020;3(1):1–16.
Article Google Scholar
Tran BX, Vu GT, Ha GH, Vuong Q-H, Ho M-T, Vuong T-T, et al. Global evolution of research in artificial intelligence in health and medicine: a bibliometric study. J Clin Med. 2019;8(3):360.
Article PubMed Central Google Scholar
Hamid S. The opportunities and risks of artificial intelligence in medicine and healthcare [Internet]. 2016 [cited 2020 May 29]. http://www.cuspe.org/wp-content/uploads/2016/09/Hamid_2016.pdf
Panch T, Szolovits P, Atun R. Artificial intelligence, machine learning and health systems. J Glob Health. 2018;8(2):020303.
Article PubMed PubMed Central Google Scholar
Yang X, Wang Y, Byrne R, Schneider G, Yang S. Concepts of artificial intelligence for computer-assisted drug discovery | chemical reviews. Chem Rev. 2019;119(18):10520–94.
Article CAS PubMed Google Scholar
Burton RJ, Albur M, Eberl M, Cuff SM. Using artificial intelligence to reduce diagnostic workload without compromising detection of urinary tract infections. BMC Med Inform Decis Mak. 2019;19(1):171.
Meskò B, Drobni Z, Bényei E, Gergely B, Gyorffy Z. Digital health is a cultural transformation of traditional healthcare. Mhealth. 2017;3:38.
Cho B-J, Choi YJ, Lee M-J, Kim JH, Son G-H, Park S-H, et al. Classification of cervical neoplasms on colposcopic photography using deep learning. Sci Rep. 2020;10(1):13652.
Article CAS PubMed PubMed Central Google Scholar
Doyle OM, Leavitt N, Rigg JA. Finding undiagnosed patients with hepatitis C infection: an application of artificial intelligence to patient claims data. Sci Rep. 2020;10(1):10521.
Shortliffe EH, Sepúlveda MJ. Clinical decision support in the era of artificial intelligence. JAMA. 2018;320(21):2199–200.
Article PubMed Google Scholar
Massaro M, Dumay J, Guthrie J. On the shoulders of giants: undertaking a structured literature review in accounting. Account Auditing Account J. 2016;29(5):767–801.
Junquera B, Mitre M. Value of bibliometric analysis for research policy: a case study of Spanish research into innovation and technology management. Scientometrics. 2007;71(3):443–54.
Casadesus-Masanell R, Ricart JE. How to design a winning business model. Harvard Business Review [Internet]. 2011 Jan 1 [cited 2020 Jan 8]. https://hbr.org/2011/01/how-to-design-a-winning-business-model
Aria M, Cuccurullo C. bibliometrix: an R-tool for comprehensive science mapping analysis. J Informetr. 2017;11(4):959–75.
Zupic I, Čater T. Bibliometric methods in management and organization. Organ Res Methods. 2015;1(18):429–72.
Secinaro S, Calandra D. Halal food: structured literature review and research agenda. Br Food J. 2020. https://doi.org/10.1108/BFJ-03-2020-0234 .
Rialp A, Merigó JM, Cancino CA, Urbano D. Twenty-five years (1992–2016) of the international business review: a bibliometric overview. Int Bus Rev. 2019;28(6):101587.
Zhao L, Dai T, Qiao Z, Sun P, Hao J, Yang Y. Application of artificial intelligence to wastewater treatment: a bibliometric analysis and systematic review of technology, economy, management, and wastewater reuse. Process Saf Environ Prot. 2020;1(133):169–82.
Article CAS Google Scholar
Huang Y, Huang Q, Ali S, Zhai X, Bi X, Liu R. Rehabilitation using virtual reality technology: a bibliometric analysis, 1996–2015. Scientometrics. 2016;109(3):1547–59.
Hao T, Chen X, Li G, Yan J. A bibliometric analysis of text mining in medical research. Soft Comput. 2018;22(23):7875–92.
dos Santos BS, Steiner MTA, Fenerich AT, Lima RHP. Data mining and machine learning techniques applied to public health problems: a bibliometric analysis from 2009 to 2018. Comput Ind Eng. 2019;1(138):106120.
Liao H, Tang M, Luo L, Li C, Chiclana F, Zeng X-J. A bibliometric analysis and visualization of medical big data research. Sustainability. 2018;10(1):166.
Choudhury A, Renjilian E, Asan O. Use of machine learning in geriatric clinical care for chronic diseases: a systematic literature review. JAMIA Open. 2020;3(3):459–71.
Connelly TM, Malik Z, Sehgal R, Byrnes G, Coffey JC, Peirce C. The 100 most influential manuscripts in robotic surgery: a bibliometric analysis. J Robot Surg. 2020;14(1):155–65.
Guo Y, Hao Z, Zhao S, Gong J, Yang F. Artificial intelligence in health care: bibliometric analysis. J Med Internet Res. 2020;22(7):e18228.
Choudhury A, Asan O. Role of artificial intelligence in patient safety outcomes: systematic literature review. JMIR Med Inform. 2020;8(7):e18599.
Forliano C, De Bernardi P, Yahiaoui D. Entrepreneurial universities: a bibliometric analysis within the business and management domains. Technol Forecast Soc Change. 2021;1(165):120522.
Secundo G, Del Vecchio P, Mele G. Social media for entrepreneurship: myth or reality? A structured literature review and a future research agenda. Int J Entrep Behav Res. 2020;27(1):149–77.
Dal Mas F, Massaro M, Lombardi R, Garlatti A. From output to outcome measures in the public sector: a structured literature review. Int J Organ Anal. 2019;27(5):1631–56.
Google Scholar
Baima G, Forliano C, Santoro G, Vrontis D. Intellectual capital and business model: a systematic literature review to explore their linkages. J Intellect Cap. 2020. https://doi.org/10.1108/JIC-02-2020-0055 .
Dumay J, Guthrie J, Puntillo P. IC and public sector: a structured literature review. J Intellect Cap. 2015;16(2):267–84.
Dal Mas F, Garcia-Perez A, Sousa MJ, Lopes da Costa R, Cobianchi L. Knowledge translation in the healthcare sector. A structured literature review. Electron J Knowl Manag. 2020;18(3):198–211.
Mas FD, Massaro M, Lombardi R, Biancuzzi H. La performance nel settore pubblico tra misure di out-put e di outcome. Una revisione strutturata della letteratura ejvcbp. 2020;1(3):16–29.
Dumay J, Cai L. A review and critique of content analysis as a methodology for inquiring into IC disclosure. J Intellect Cap. 2014;15(2):264–90.
Haleem A, Javaid M, Khan IH. Current status and applications of Artificial Intelligence (AI) in medical field: an overview. Curr Med Res Pract. 2019;9(6):231–7.
Paul J, Criado AR. The art of writing literature review: what do we know and what do we need to know? Int Bus Rev. 2020;29(4):101717.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Biancone PP, Secinaro S, Brescia V, Calandra D. Data quality methods and applications in health care system: a systematic literature review. Int J Bus Manag. 2019;14(4):p35.
Secinaro S, Brescia V, Calandra D, Verardi GP, Bert F. The use of micafungin in neonates and children: a systematic review. ejvcbp. 2020;1(1):100–14.
Bert F, Gualano MR, Biancone P, Brescia V, Camussi E, Martorana M, et al. HIV screening in pregnant women: a systematic review of cost-effectiveness studies. Int J Health Plann Manag. 2018;33(1):31–50.
Levy Y, Ellis TJ. A systems approach to conduct an effective literature review in support of information systems research. Inf Sci Int J Emerg Transdiscipl. 2006;9:181–212.
Chen G, Xiao L. Selecting publication keywords for domain analysis in bibliometrics: a comparison of three methods. J Informet. 2016;10(1):212–23.
Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. FASEB J. 2007;22(2):338–42.
Article PubMed CAS Google Scholar
Sicilia M-A, Garcìa-Barriocanal E, Sànchez-Alonso S. Community curation in open dataset repositories: insights from zenodo. Procedia Comput Sci. 2017;1(106):54–60.
Secinaro S, Calandra D, Secinaro A, Muthurangu V, Biancone P. Artificial Intelligence for healthcare with a business, management and accounting, decision sciences, and health professions focus [Internet]. Zenodo; 2021 [cited 2021 Mar 7]. https://zenodo.org/record/4587618#.YEScpl1KiWh .
Elango B, Rajendran D. Authorship trends and collaboration pattern in the marine sciences literature: a scientometric Study. Int J Inf Dissem Technol. 2012;1(2):166–9.
Jacoby WG. Electoral inquiry section Loess: a nonparametric, graphical tool for depicting relationships between variables q. In 2000.
Andrews JE. An author co-citation analysis of medical informatics. J Med Libr Assoc. 2003;91(1):47–56.
PubMed PubMed Central Google Scholar
White HD, Griffith BC. Author cocitation: a literature measure of intellectual structure. J Am Soc Inf Sci. 1981;32(3):163–71.
Santosh KC. AI-driven tools for coronavirus outbreak: need of active learning and cross-population train/test models on multitudinal/multimodal data. J Med Syst. 2020;44(5):93.
Shickel B, Tighe PJ, Bihorac A, Rashidi P. Deep EHR: a survey of recent advances in deep learning techniques for electronic health record (EHR) analysis. IEEE J Biomed Health Inform. 2018;22(5):1589–604.
Baig MM, GholamHosseini H, Moqeem AA, Mirza F, Lindén M. A systematic review of wearable patient monitoring systems—current challenges and opportunities for clinical adoption. J Med Syst. 2017;41(7):115.
Kumar S, Kumar S. Collaboration in research productivity in oil seed research institutes of India. In: Proceedings of fourth international conference on webometrics, informetrics and scientometrics. p. 28–1; 2008.
Gatto A, Drago C. A taxonomy of energy resilience. Energy Policy. 2020;136:111007.
Levitt JM, Thelwall M. Alphabetization and the skewing of first authorship towards last names early in the alphabet. J Informet. 2013;7(3):575–82.
Saad G. Exploring the h-index at the author and journal levels using bibliometric data of productive consumer scholars and business-related journals respectively. Scientometrics. 2006;69(1):117–20.
Egghe L. Theory and practise of the g-index. Scientometrics. 2006;69(1):131–52.
Schreiber M. A modification of the h-index: the hm-index accounts for multi-authored manuscripts. J Informet. 2008;2(3):211–6.
Engqvist L, Frommen JG. The h-index and self-citations. Trends Ecol Evol. 2008;23(5):250–2.
London School of Economics. 3: key measures of academic influence [Internet]. Impact of social sciences. 2010 [cited 2021 Jan 13]. https://blogs.lse.ac.uk/impactofsocialsciences/the-handbook/chapter-3-key-measures-of-academic-influence/ .
Lotka A. The frequency distribution of scientific productivity. J Wash Acad Sci. 1926;16(12):317–24.
Khan G, Wood J. Information technology management domain: emerging themes and keyword analysis. Scientometrics. 2015;9:105.
Oxford University Press. Oxford English Dictionary [Internet]. 2020. https://www.oed.com/ .
Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2(4):230–43.
Calandra D, Favareto M. Artificial Intelligence to fight COVID-19 outbreak impact: an overview. Eur J Soc Impact Circ Econ. 2020;1(3):84–104.
Bokolo Anthony Jnr. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):132.
Burke EK, De Causmaecker P, Berghe GV, Van Landeghem H. The state of the art of nurse rostering. J Sched. 2004;7(6):441–99.
Ahmed MA, Alkhamis TM. Simulation optimization for an emergency department healthcare unit in Kuwait. Eur J Oper Res. 2009;198(3):936–42.
Forina M, Armanino C, Raggio V. Clustering with dendrograms on interpretation variables. Anal Chim Acta. 2002;454(1):13–9.
Wartena C, Brussee R. Topic detection by clustering keywords. In: 2008 19th international workshop on database and expert systems applications. 2008. p. 54–8.
Hussain AA, Bouachir O, Al-Turjman F, Aloqaily M. AI Techniques for COVID-19. IEEE Access. 2020;8:128776–95.
Agrawal A, Gans JS, Goldfarb A. Exploring the impact of artificial intelligence: prediction versus judgment. Inf Econ Policy. 2019;1(47):1–6.
Chakradhar S. Predictable response: finding optimal drugs and doses using artificial intelligence. Nat Med. 2017;23(11):1244–7.
Fleming N. How artificial intelligence is changing drug discovery. Nature. 2018;557(7707):S55–7.
Guo J, Li B. The application of medical artificial intelligence technology in rural areas of developing countries. Health Equity. 2018;2(1):174–81.
Aisyah M, Cockcroft S. A snapshot of data quality issues in Indonesian community health. Int J Netw Virtual Organ. 2014;14(3):280–97.
Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6(2):94–8.
Mehta N, Pandit A, Shukla S. Transforming healthcare with big data analytics and artificial intelligence: a systematic mapping study. J Biomed Inform. 2019;1(100):103311.
Collins GS, Moons KGM. Reporting of artificial intelligence prediction models. Lancet. 2019;393(10181):1577–9.
Bennett CC, Hauser K. Artificial intelligence framework for simulating clinical decision-making: a Markov decision process approach. Artif Intell Med. 2013;57(1):9–19.
Redondo T, Sandoval AM. Text Analytics: the convergence of big data and artificial intelligence. Int J Interact Multimed Artif Intell. 2016;3. https://www.ijimai.org/journal/bibcite/reference/2540 .
Winter JS, Davidson E. Big data governance of personal health information and challenges to contextual integrity. Inf Soc. 2019;35(1):36–51.
Novak D, Riener R. Control strategies and artificial intelligence in rehabilitation robotics. AI Mag. 2015;36(4):23–33.
Tarassoli SP. Artificial intelligence, regenerative surgery, robotics? What is realistic for the future of surgery? Ann Med Surg (Lond). 2019;17(41):53–5.
Saha SK, Fernando B, Cuadros J, Xiao D, Kanagasingam Y. Automated quality assessment of colour fundus images for diabetic retinopathy screening in telemedicine. J Digit Imaging. 2018;31(6):869–78.
Gu D, Li T, Wang X, Yang X, Yu Z. Visualizing the intellectual structure and evolution of electronic health and telemedicine research. Int J Med Inform. 2019;130:103947.
Madnick S, Wang R, Lee Y, Zhu H. Overview and framework for data and information quality research. J Data Inf Qual. 2009;1:1.
Chen X, Liu Z, Wei L, Yan J, Hao T, Ding R. A comparative quantitative study of utilizing artificial intelligence on electronic health records in the USA and China during 2008–2017. BMC Med Inform Decis Mak. 2018;18(5):117.
Carter D. How real is the impact of artificial intelligence? Bus Inf Surv. 2018;35(3):99–115.
Kalis B, Collier M, Fu R. 10 Promising AI Applications in Health Care. 2018;5.
Biancone P, Secinaro S, Brescia V, Calandra D. Management of open innovation in healthcare for cost accounting using EHR. J Open Innov Technol Market Complex. 2019;5(4):99.
Kayyali B, Knott D, Van Kuiken S. The ‘big data’ revolution in US healthcare [Internet]. McKinsey & Company. 2013 [cited 2020 Aug 14]. https://healthcare.mckinsey.com/big-data-revolution-us-healthcare/ .
Lu J. Will medical technology deskill doctors? Int Educ Stud. 2016;9(7):130–4.
Hoff T. Deskilling and adaptation among primary care physicians using two work innovations. Health Care Manag Rev. 2011;36(4):338–48.
Picek O. Spillover effects from next generation EU. Intereconomics. 2020;55(5):325–31.
Sousa MJ, Dal Mas F, Pesqueira A, Lemos C, Verde JM, Cobianchi L. The potential of AI in health higher education to increase the students’ learning outcomes. TEM J. 2021. ( In press ).
Download references
Acknowledgements
The authors are grateful to the Editor-in-Chief for the suggestions and all the reviewers who spend a part of their time ensuring constructive feedback to our research article.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Management, University of Turin, Turin, Italy
Silvana Secinaro, Davide Calandra & Paolo Biancone
Ospedale Pediatrico Bambino Gesù, Rome, Italy
Aurelio Secinaro
Institute of Child Health, University College London, London, UK
Vivek Muthurangu
You can also search for this author in PubMed Google Scholar
Contributions
SS and PB, Supervision; Validation, writing, AS and VM; Formal analysis, DC and AS; Methodology, DC; Writing; DC, SS and AS; conceptualization, VM, PB; validation, VM, PB. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Davide Calandra .
Ethics declarations
Ethical approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Secinaro, S., Calandra, D., Secinaro, A. et al. The role of artificial intelligence in healthcare: a structured literature review. BMC Med Inform Decis Mak 21 , 125 (2021). https://doi.org/10.1186/s12911-021-01488-9
Download citation
Received : 24 December 2020
Accepted : 01 April 2021
Published : 10 April 2021
DOI : https://doi.org/10.1186/s12911-021-01488-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Artificial intelligence
- Patient data
BMC Medical Informatics and Decision Making
ISSN: 1472-6947
- General enquiries: [email protected]
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Author Biographies
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
How artificial intelligence is shaping medical imaging technology: a survey of innovations and applications.

1. Introduction
2. methodology, 3. technological innovations, 3.1. transformers, 3.2. generative models, 3.3. deep learning techniques and performance optimization, 4. applications, 4.1. medical image analysis for disease detection and diagnosis, 4.2. imaging and modeling techniques for surgical planning and intervention, 4.3. image and model enhancement for improved analysis, 4.4. medical imaging datasets, 5. conclusions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Ghaffar Nia, N.; Kaplanoglu, E.; Nasab, A. Evaluation of Artificial Intelligence Techniques in Disease Diagnosis and Prediction. Discov. Artif. Intell. 2023 , 3 , 5. [ Google Scholar ] [ CrossRef ]
- Kumar, Y.; Koul, A.; Singla, R.; Ijaz, M.F. Artificial Intelligence in Disease Diagnosis: A Systematic Literature Review, Synthesizing Framework and Future Research Agenda. J. Ambient. Intell. Humaniz. Comput. 2023 , 14 , 8459–8486. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H.J.W.L. Artificial Intelligence in Radiology. Nat. Rev. Cancer 2018 , 18 , 500–510. [ Google Scholar ] [ CrossRef ]
- Waldstein, S.M.; Seeböck, P.; Donner, R.; Sadeghipour, A.; Bogunović, H.; Osborne, A.; Schmidt-Erfurth, U. Unbiased Identification of Novel Subclinical Imaging Biomarkers Using Unsupervised Deep Learning. Sci. Rep. 2020 , 10 , 12954. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Plested, J.; Gedeon, T. Deep Transfer Learning for Image Classification: A Survey. arXiv 2022 , arXiv:2205.09904. [ Google Scholar ]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing Healthcare: The Role of Artificial Intelligence in Clinical Practice. BMC Med. Educ. 2023 , 23 , 689. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sinha, A.; Dolz, J. Multi-Scale Self-Guided Attention for Medical Image Segmentation. IEEE J. Biomed. Health Inform. 2020 , 25 , 121–130. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Popescu, D.; Stanciulescu, A.; Pomohaci, M.D.; Ichim, L. Decision Support System for Liver Lesion Segmentation Based on Advanced Convolutional Neural Network Architectures. Bioengineering 2022 , 9 , 467. [ Google Scholar ] [ CrossRef ]
- Altini, N.; Brunetti, A.; Puro, E.; Taccogna, M.G.; Saponaro, C.; Zito, F.A.; De Summa, S.; Bevilacqua, V. NDG-CAM: Nuclei Detection in Histopathology Images with Semantic Segmentation Networks and Grad-CAM. Bioengineering 2022 , 9 , 475. [ Google Scholar ] [ CrossRef ]
- van de Sande, D.; Sharabiani, M.; Bluemink, H.; Kneepkens, E.; Bakx, N.; Hagelaar, E.; van der Sangen, M.; Theuws, J.; Hurkmans, C. Artificial Intelligence Based Treatment Planning of Radiotherapy for Locally Advanced Breast Cancer. Phys. Imaging Radiat Oncol. 2021 , 20 , 111–116. [ Google Scholar ] [ CrossRef ]
- Schork, N.J. Artificial Intelligence and Personalized Medicine. Cancer Treat Res. 2019 , 178 , 265–283. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Uddin, M.; Wang, Y.; Woodbury-Smith, M. Artificial Intelligence for Precision Medicine in Neurodevelopmental Disorders. npj Digit. Med. 2019 , 2 , 112. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hashimoto, D.A.; Rosman, G.; Rus, D.; Meireles, O.R. Artificial Intelligence in Surgery: Promises and Perils. Ann. Surg. 2018 , 268 , 70–76. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Literature Map Software for Lit Reviews & Research|Litmaps. Available online: https://www.litmaps.com/ (accessed on 8 December 2023).
- Iramuteq—IRaMuTeQ. Available online: http://www.iramuteq.org/ (accessed on 8 July 2023).
- Sarmet, M.; Kabani, A.; Coelho, L.; dos Reis, S.S.; Zeredo, J.L.; Mehta, A.K. The Use of Natural Language Processing in Palliative Care Research: A Scoping Review. Palliat. Med. 2023 , 37 , 275–290. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Roodschild, M.; Gotay Sardiñas, J.; Will, A. A New Approach for the Vanishing Gradient Problem on Sigmoid Activation. Prog. Artif. Intell. 2020 , 9 , 351–360. [ Google Scholar ] [ CrossRef ]
- Nair, V.; Hinton, G.E. Rectified Linear Units Improve Restricted Boltzmann Machines. In Proceedings of the 27th International Conference on International Conference on Machine Learning, Madison, WI, USA, 21 June 2010; pp. 807–814. [ Google Scholar ]
- Agarap, A.F. Deep Learning Using Rectified Linear Units (ReLU). arXiv 2018 , arXiv:1803.08375. [ Google Scholar ]
- Deng, L. The MNIST Database of Handwritten Digit Images for Machine Learning Research [Best of the Web]. IEEE Signal Process. Mag. 2012 , 29 , 141–142. [ Google Scholar ] [ CrossRef ]
- LeCun, Y.; Bengio, Y.; Hinton, G. Deep Learning. Nature 2015 , 521 , 436–444. [ Google Scholar ] [ CrossRef ]
- Gu, J.; Wang, Z.; Kuen, J.; Ma, L.; Shahroudy, A.; Shuai, B.; Liu, T.; Wang, X.; Wang, G.; Cai, J.; et al. Recent Advances in Convolutional Neural Networks. Pattern Recognit. 2018 , 77 , 354–377. [ Google Scholar ] [ CrossRef ]
- O’Shea, K.; Nash, R. An Introduction to Convolutional Neural Networks. arXiv 2015 , arXiv:1511.08458. [ Google Scholar ]
- Yandex, A.B.; Lempitsky, V. Aggregating Local Deep Features for Image Retrieval. In Proceedings of the 2015 IEEE International Conference on Computer Vision (ICCV), Santiago, Chile, 7 December 2015; pp. 1269–1277. [ Google Scholar ]
- Nwankpa, C.; Ijomah, W.; Gachagan, A.; Marshall, S. Activation Functions: Comparison of Trends in Practice and Research for Deep Learning. arXiv 2018 , arXiv:1811.03378. [ Google Scholar ]
- Szandała, T. Review and Comparison of Commonly Used Activation Functions for Deep Neural Networks. In Bio-Inspired Neurocomputing ; Bhoi, A.K., Mallick, P.K., Liu, C.-M., Balas, V.E., Eds.; Studies in Computational Intelligence; Springer: Singapore, 2021; pp. 203–224. ISBN 9789811554957. [ Google Scholar ]
- Krizhevsky, A.; Sutskever, I.; Hinton, G.E. ImageNet Classification with Deep Convolutional Neural Networks. Commun. ACM 2017 , 60 , 84–90. [ Google Scholar ] [ CrossRef ]
- Vaswani, A.; Shazeer, N.; Parmar, N.; Uszkoreit, J.; Jones, L.; Gomez, A.N.; Kaiser, Ł.; Polosukhin, I. Attention Is All You Need. In Proceedings of the 31st International Conference on Neural Information Processing Systems, Long Beach, CA, USA, 4–9 December 2017; Curran Associates Inc.: Red Hook, NY, USA, 2017; pp. 6000–6010. [ Google Scholar ]
- Dosovitskiy, A.; Beyer, L.; Kolesnikov, A.; Weissenborn, D.; Zhai, X.; Unterthiner, T.; Dehghani, M.; Minderer, M.; Heigold, G.; Gelly, S.; et al. An Image Is Worth 16 × 16 Words: Transformers for Image Recognition at Scale. arXiv 2020 , arXiv:2010.11929. [ Google Scholar ]
- Maurício, J.; Domingues, I.; Bernardino, J. Comparing Vision Transformers and Convolutional Neural Networks for Image Classification: A Literature Review. Appl. Sci. 2023 , 13 , 5521. [ Google Scholar ] [ CrossRef ]
- Shamshad, F.; Khan, S.; Zamir, S.W.; Khan, M.H.; Hayat, M.; Khan, F.S.; Fu, H. Transformers in Medical Imaging: A Survey. Med Image Anal. 2022 , 88 , 102802. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ali, H.; Mohsen, F.; Shah, Z. Improving Diagnosis and Prognosis of Lung Cancer Using Vision Transformers: A Scoping Review. BMC Med. Imaging 2023 , 23 , 129. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Al-hammuri, K.; Gebali, F.; Kanan, A.; Chelvan, I.T. Vision Transformer Architecture and Applications in Digital Health: A Tutorial and Survey. Vis. Comput. Ind. Biomed. Art 2023 , 6 , 14. [ Google Scholar ] [ CrossRef ]
- He, K.; Gan, C.; Li, Z.; Rekik, I.; Yin, Z.; Ji, W.; Gao, Y.; Wang, Q.; Zhang, J.; Shen, D. Transformers in Medical Image Analysis. Intell. Med. 2023 , 3 , 59–78. [ Google Scholar ] [ CrossRef ]
- Katar, O.; Yildirim, O. An Explainable Vision Transformer Model Based White Blood Cells Classification and Localization. Diagnostics 2023 , 13 , 2459. [ Google Scholar ] [ CrossRef ]
- Hu, J.; Shen, L.; Albanie, S.; Sun, G.; Wu, E. Squeeze-and-Excitation Networks. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Salt Lake City, UT, USA, 18–23 June 2019. [ Google Scholar ]
- Touvron, H.; Cord, M.; Sablayrolles, A.; Synnaeve, G.; Jégou, H. Going Deeper with Image Transformers. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Montreal, BC, Canada, 11–17 October 2021. [ Google Scholar ]
- Oktay, O.; Schlemper, J.; Folgoc, L.L.; Lee, M.; Heinrich, M.; Misawa, K.; Mori, K.; McDonagh, S.; Hammerla, N.Y.; Kainz, B.; et al. Attention U-Net: Learning Where to Look for the Pancreas. arXiv 2018 , arXiv:1804.03999. [ Google Scholar ]
- Nwoye, C.I.; Yu, T.; Gonzalez, C.; Seeliger, B.; Mascagni, P.; Mutter, D.; Marescaux, J.; Padoy, N. Rendezvous: Attention Mechanisms for the Recognition of Surgical Action Triplets in Endoscopic Videos. Med. Image Anal. 2022 , 78 , 102433. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rao, A.; Park, J.; Woo, S.; Lee, J.-Y.; Aalami, O. Studying the Effects of Self-Attention for Medical Image Analysis. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Montreal, BC, Canada, 11–17 October 2021. [ Google Scholar ]
- You, H.; Wang, J.; Ma, R.; Chen, Y.; Li, L.; Song, C.; Dong, Z.; Feng, S.; Zhou, X. Clinical Interpretability of Deep Learning for Predicting Microvascular Invasion in Hepatocellular Carcinoma by Using Attention Mechanism. Bioengineering 2023 , 10 , 948. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Liu, Z.; Lin, Y.; Cao, Y.; Hu, H.; Wei, Y.; Zhang, Z.; Lin, S.; Guo, B. Swin Transformer: Hierarchical Vision Transformer Using Shifted Windows. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Montreal, QC, Canada, 10–17 October 2021. [ Google Scholar ]
- Liu, Z.; Hu, H.; Lin, Y.; Yao, Z.; Xie, Z.; Wei, Y.; Ning, J.; Cao, Y.; Zhang, Z.; Dong, L.; et al. Swin Transformer V2: Scaling Up Capacity and Resolution. In Proceedings of the IEEE/CVF Conference on Computer Vision and Pattern Recognition, New Orleans, LA, USA, 18–24 June 2022. [ Google Scholar ]
- He, B.; Hofmann, T. Simplifying Transformer Blocks. arXiv 2023 , arXiv:2311.01906. [ Google Scholar ]
- Henry, E.U.; Emebob, O.; Omonhinmin, C.A. Vision Transformers in Medical Imaging: A Review. arXiv 2022 , arXiv:2211.10043. [ Google Scholar ]
- Redmon, J.; Divvala, S.; Girshick, R.; Farhadi, A. You Only Look Once: Unified, Real-Time Object Detection. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Las Vegas, NV, USA, 27–30 June 2016. [ Google Scholar ]
- Tayebi, R.M.; Mu, Y.; Dehkharghanian, T.; Ross, C.; Sur, M.; Foley, R.; Tizhoosh, H.R.; Campbell, C.J.V. Automated Bone Marrow Cytology Using Deep Learning to Generate a Histogram of Cell Types. Commun. Med. 2022 , 2 , 45. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mammeri, S.; Amroune, M.; Haouam, M.-Y.; Bendib, I.; Corrêa Silva, A. Early Detection and Diagnosis of Lung Cancer Using YOLO v7, and Transfer Learning. Multimed. Tools Appl. 2023 , 1–16. [ Google Scholar ] [ CrossRef ]
- Mortada, M.J.; Tomassini, S.; Anbar, H.; Morettini, M.; Burattini, L.; Sbrollini, A. Segmentation of Anatomical Structures of the Left Heart from Echocardiographic Images Using Deep Learning. Diagnostics 2023 , 13 , 1683. [ Google Scholar ] [ CrossRef ]
- Su, Y.; Liu, Q.; Xie, W.; Hu, P. YOLO-LOGO: A Transformer-Based YOLO Segmentation Model for Breast Mass Detection and Segmentation in Digital Mammograms. Comput. Methods Programs Biomed. 2022 , 221 , 106903. [ Google Scholar ] [ CrossRef ]
- Amiri Tehrani Zade, A.; Jalili Aziz, M.; Majedi, H.; Mirbagheri, A.; Ahmadian, A. Spatiotemporal Analysis of Speckle Dynamics to Track Invisible Needle in Ultrasound Sequences Using Convolutional Neural Networks: A Phantom Study. Int. J. CARS 2023 , 18 , 1373–1382. [ Google Scholar ] [ CrossRef ]
- Guo, S.; Sheng, S.; Lai, Z.; Chen, S. Trans-U: Transformer Enhanced U-Net for Medical Image Segmentation. In Proceedings of the 2022 3rd International Conference on Computer Vision, Image and Deep Learning & International Conference on Computer Engineering and Applications (CVIDL & ICCEA), Changchun, China, 20–22 May 2022; pp. 628–631. [ Google Scholar ]
- Zhang, Z.; Lu, X.; Cao, G.; Yang, Y.; Jiao, L.; Liu, F. ViT-YOLO:Transformer-Based YOLO for Object Detection. In Proceedings of the 2021 IEEE/CVF International Conference on Computer Vision Workshops (ICCVW), Montreal, BC, Canada, 11–17 October 2021; pp. 2799–2808. [ Google Scholar ]
- Goodfellow, I.J.; Pouget-Abadie, J.; Mirza, M.; Xu, B.; Warde-Farley, D.; Ozair, S.; Courville, A.; Bengio, Y. Generative Adversarial Networks. IEEE Signal Process. Mag. 2014 , 35 , 53–65. [ Google Scholar ] [ CrossRef ]
- Platscher, M.; Zopes, J.; Federau, C. Image Translation for Medical Image Generation: Ischemic Stroke Lesion Segmentation. Biomed. Signal Process. Control. 2022 , 72 , 103283. [ Google Scholar ] [ CrossRef ]
- Armanious, K.; Jiang, C.; Fischer, M.; Küstner, T.; Hepp, T.; Nikolaou, K.; Gatidis, S.; Yang, B. MedGAN: Medical Image Translation Using GANs. Comput. Med. Imaging Graph. 2020 , 79 , 101684. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kazeminia, S.; Baur, C.; Kuijper, A.; van Ginneken, B.; Navab, N.; Albarqouni, S.; Mukhopadhyay, A. GANs for Medical Image Analysis. Artif. Intell. Med. 2020 , 109 , 101938. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Skandarani, Y.; Jodoin, P.-M.; Lalande, A. GANs for Medical Image Synthesis: An Empirical Study. J. Imaging 2023 , 9 , 69. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wang, T.; Lei, Y.; Fu, Y.; Wynne, J.F.; Curran, W.J.; Liu, T.; Yang, X. A Review on Medical Imaging Synthesis Using Deep Learning and Its Clinical Applications. J. Appl. Clin. Med. Phys. 2021 , 22 , 11–36. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ehrhardt, J.; Wilms, M. Chapter 8-Autoencoders and Variational Autoencoders in Medical Image Analysis. In Biomedical Image Synthesis and Simulation ; Burgos, N., Svoboda, D., Eds.; The MICCAI Society Book Series; Academic Press: Cambridge, MA, USA, 2022; pp. 129–162. ISBN 978-0-12-824349-7. [ Google Scholar ]
- Kebaili, A.; Lapuyade-Lahorgue, J.; Ruan, S. Deep Learning Approaches for Data Augmentation in Medical Imaging: A Review. J. Imaging 2023 , 9 , 81. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Elbattah, M.; Loughnane, C.; Guérin, J.-L.; Carette, R.; Cilia, F.; Dequen, G. Variational Autoencoder for Image-Based Augmentation of Eye-Tracking Data. J. Imaging 2021 , 7 , 83. [ Google Scholar ] [ CrossRef ]
- Ho, J.; Jain, A.; Abbeel, P. Denoising Diffusion Probabilistic Models. Adv. Neural Inf. Process. Syst. 2020 , 33 , 6840–6851. [ Google Scholar ]
- Dhariwal, P.; Nichol, A. Diffusion Models Beat GANs on Image Synthesis. Adv. Neural Inf. Process. Syst. 2021 , 34 , 8780–8794. [ Google Scholar ]
- Kazerouni, A.; Aghdam, E.K.; Heidari, M.; Azad, R.; Fayyaz, M.; Hacihaliloglu, I.; Merhof, D. Diffusion Models in Medical Imaging: A Comprehensive Survey. Med. Image Anal. 2023 , 88 , 102846. [ Google Scholar ] [ CrossRef ]
- Yang, R.; Srivastava, P.; Mandt, S. Diffusion Probabilistic Modeling for Video Generation. Entropy 2023 , 25 , 1469. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bobrow, T.L.; Golhar, M.; Vijayan, R.; Akshintala, V.S.; Garcia, J.R.; Durr, N.J. Colonoscopy 3D Video Dataset with Paired Depth from 2D-3D Registration. Med. Image Anal. 2023 , 90 , 102956. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bond-Taylor, S.; Leach, A.; Long, Y.; Willcocks, C.G. Deep Generative Modelling: A Comparative Review of VAEs, GANs, Normalizing Flows, Energy-Based and Autoregressive Models. IEEE Trans. Pattern Anal. Mach. Intell. 2022 , 44 , 7327–7347. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rezende, D.; Mohamed, S. Variational Inference with Normalizing Flows. In Proceedings of the 32nd International Conference on Machine Learning, Lile, France, 1 June 2015; pp. 1530–1538. [ Google Scholar ]
- Ho, J.; Chen, X.; Srinivas, A.; Duan, Y.; Abbeel, P. Flow++: Improving Flow-Based Generative Models with Variational Dequantization and Architecture Design. In Proceedings of the 36th International Conference on Machine Learning, Long Beach, CA, USA, 10–15 June 2019. [ Google Scholar ]
- Sun, H.; Mehta, R.; Zhou, H.H.; Huang, Z.; Johnson, S.C.; Prabhakaran, V.; Singh, V. DUAL-GLOW: Conditional Flow-Based Generative Model for Modality Transfer. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Seoul, Korea, 27 October–2 November 2019; pp. 10611–10620. [ Google Scholar ]
- Uemura, T.; Näppi, J.J.; Ryu, Y.; Watari, C.; Kamiya, T.; Yoshida, H. A Generative Flow-Based Model for Volumetric Data Augmentation in 3D Deep Learning for Computed Tomographic Colonography. Int. J. CARS 2021 , 16 , 81–89. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yi, X.; Walia, E.; Babyn, P. Generative Adversarial Network in Medical Imaging: A Review. Med. Image Anal. 2019 , 58 , 101552. [ Google Scholar ] [ CrossRef ]
- Laptev, V.V.; Gerget, O.M.; Markova, N.A. Generative Models Based on VAE and GAN for New Medical Data Synthesis. In Society 5.0: Cyberspace for Advanced Human-Centered Society ; Kravets, A.G., Bolshakov, A.A., Shcherbakov, M., Eds.; Studies in Systems, Decision and Control; Springer International Publishing: Cham, Switzerland, 2021; pp. 217–226. ISBN 978-3-030-63563-3. [ Google Scholar ]
- Trevisan de Souza, V.L.; Marques, B.A.D.; Batagelo, H.C.; Gois, J.P. A Review on Generative Adversarial Networks for Image Generation. Comput. Graph. 2023 , 114 , 13–25. [ Google Scholar ] [ CrossRef ]
- Adeshina, S.A.; Adedigba, A.P. Bag of Tricks for Improving Deep Learning Performance on Multimodal Image Classification. Bioengineering 2022 , 9 , 312. [ Google Scholar ] [ CrossRef ]
- Saleh, G.A.; Batouty, N.M.; Haggag, S.; Elnakib, A.; Khalifa, F.; Taher, F.; Mohamed, M.A.; Farag, R.; Sandhu, H.; Sewelam, A.; et al. The Role of Medical Image Modalities and AI in the Early Detection, Diagnosis and Grading of Retinal Diseases: A Survey. Bioengineering 2022 , 9 , 366. [ Google Scholar ] [ CrossRef ]
- Han, J.-H. Artificial Intelligence in Eye Disease: Recent Developments, Applications, and Surveys. Diagnostics 2022 , 12 , 1927. [ Google Scholar ] [ CrossRef ]
- Daich Varela, M.; Sen, S.; De Guimaraes, T.A.C.; Kabiri, N.; Pontikos, N.; Balaskas, K.; Michaelides, M. Artificial Intelligence in Retinal Disease: Clinical Application, Challenges, and Future Directions. Graefes Arch. Clin. Exp. Ophthalmol. 2023 , 261 , 3283–3297. [ Google Scholar ] [ CrossRef ]
- Zain Eldin, H.; Gamel, S.A.; El-Kenawy, E.-S.M.; Alharbi, A.H.; Khafaga, D.S.; Ibrahim, A.; Talaat, F.M. Brain Tumor Detection and Classification Using Deep Learning and Sine-Cosine Fitness Grey Wolf Optimization. Bioengineering 2023 , 10 , 18. [ Google Scholar ] [ CrossRef ]
- Forte, G.C.; Altmayer, S.; Silva, R.F.; Stefani, M.T.; Libermann, L.L.; Cavion, C.C.; Youssef, A.; Forghani, R.; King, J.; Mohamed, T.-L.; et al. Deep Learning Algorithms for Diagnosis of Lung Cancer: A Systematic Review and Meta-Analysis. Cancers 2022 , 14 , 3856. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hunger, T.; Wanka-Pail, E.; Brix, G.; Griebel, J. Lung Cancer Screening with Low-Dose CT in Smokers: A Systematic Review and Meta-Analysis. Diagnostics 2021 , 11 , 1040. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lee, C.-C.; So, E.C.; Saidy, L.; Wang, M.-J. Lung Field Segmentation in Chest X-Ray Images Using Superpixel Resizing and Encoder–Decoder Segmentation Networks. Bioengineering 2022 , 9 , 351. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lee, K.W.; Chin, R.K.Y. Diverse COVID-19 CT Image-to-Image Translation with Stacked Residual Dropout. Bioengineering 2022 , 9 , 698. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Danala, G.; Maryada, S.K.; Islam, W.; Faiz, R.; Jones, M.; Qiu, Y.; Zheng, B. A Comparison of Computer-Aided Diagnosis Schemes Optimized Using Radiomics and Deep Transfer Learning Methods. Bioengineering 2022 , 9 , 256. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Adedigba, A.P.; Adeshina, S.A.; Aibinu, A.M. Performance Evaluation of Deep Learning Models on Mammogram Classification Using Small Dataset. Bioengineering 2022 , 9 , 161. [ Google Scholar ] [ CrossRef ]
- Zebari, D.A.; Ibrahim, D.A.; Zeebaree, D.Q.; Mohammed, M.A.; Haron, H.; Zebari, N.A.; Damaševičius, R.; Maskeliūnas, R. Breast Cancer Detection Using Mammogram Images with Improved Multi-Fractal Dimension Approach and Feature Fusion. Appl. Sci. 2021 , 11 , 12122. [ Google Scholar ] [ CrossRef ]
- Cè, M.; Caloro, E.; Pellegrino, M.E.; Basile, M.; Sorce, A.; Fazzini, D.; Oliva, G.; Cellina, M. Artificial Intelligence in Breast Cancer Imaging: Risk Stratification, Lesion Detection and Classification, Treatment Planning and Prognosis—A Narrative Review. Explor. Target. Antitumor. Ther. 2022 , 3 , 795–816. [ Google Scholar ] [ CrossRef ]
- Zhang, T.; Tan, T.; Samperna, R.; Li, Z.; Gao, Y.; Wang, X.; Han, L.; Yu, Q.; Beets-Tan, R.G.H.; Mann, R.M. Radiomics and Artificial Intelligence in Breast Imaging: A Survey. Artif Intell. Rev. 2023 , 56 , 857–892. [ Google Scholar ] [ CrossRef ]
- Pesapane, F.; De Marco, P.; Rapino, A.; Lombardo, E.; Nicosia, L.; Tantrige, P.; Rotili, A.; Bozzini, A.C.; Penco, S.; Dominelli, V.; et al. How Radiomics Can Improve Breast Cancer Diagnosis and Treatment. J. Clin. Med. 2023 , 12 , 1372. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Luo, C.; Zhao, S.; Peng, C.; Wang, C.; Hu, K.; Zhong, X.; Luo, T.; Huang, J.; Lu, D. Mammography Radiomics Features at Diagnosis and Progression-Free Survival among Patients with Breast Cancer. Br. J. Cancer 2022 , 127 , 1886–1892. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Granzier, R.W.Y.; Verbakel, N.M.H.; Ibrahim, A.; van Timmeren, J.E.; van Nijnatten, T.J.A.; Leijenaar, R.T.H.; Lobbes, M.B.I.; Smidt, M.L.; Woodruff, H.C. MRI-Based Radiomics in Breast Cancer: Feature Robustness with Respect to Inter-Observer Segmentation Variability. Sci. Rep. 2020 , 10 , 14163. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- World Health Organization Cancer. Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 16 June 2023).
- Bilic, P.; Christ, P.; Li, H.B.; Vorontsov, E.; Ben-Cohen, A.; Kaissis, G.; Szeskin, A.; Jacobs, C.; Mamani, G.E.H.; Chartrand, G.; et al. The Liver Tumor Segmentation Benchmark (LiTS). Med. Image Anal. 2023 , 84 , 102680. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cardobi, N.; Dal Palù, A.; Pedrini, F.; Beleù, A.; Nocini, R.; De Robertis, R.; Ruzzenente, A.; Salvia, R.; Montemezzi, S.; D’Onofrio, M. An Overview of Artificial Intelligence Applications in Liver and Pancreatic Imaging. Cancers 2021 , 13 , 2162. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Huang, X.; Wang, H.; She, C.; Feng, J.; Liu, X.; Hu, X.; Chen, L.; Tao, Y. Artificial Intelligence Promotes the Diagnosis and Screening of Diabetic Retinopathy. Front. Endocrinol. 2022 , 13 , 946915. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sheng, B.; Chen, X.; Li, T.; Ma, T.; Yang, Y.; Bi, L.; Zhang, X. An Overview of Artificial Intelligence in Diabetic Retinopathy and Other Ocular Diseases. Front. Public Health 2022 , 10 , 971943. [ Google Scholar ] [ CrossRef ]
- Li, S.; Zhao, R.; Zou, H. Artificial Intelligence for Diabetic Retinopathy. Chin. Med. J. Engl. 2022 , 135 , 253–260. [ Google Scholar ] [ CrossRef ]
- Banerjee, I.; de Sisternes, L.; Hallak, J.A.; Leng, T.; Osborne, A.; Rosenfeld, P.J.; Gregori, G.; Durbin, M.; Rubin, D. Prediction of Age-Related Macular Degeneration Disease Using a Sequential Deep Learning Approach on Longitudinal SD-OCT Imaging Biomarkers. Sci. Rep. 2020 , 10 , 15434. [ Google Scholar ] [ CrossRef ]
- Yin, C.; Moroi, S.E.; Zhang, P. Predicting Age-Related Macular Degeneration Progression with Contrastive Attention and Time-Aware LSTM. In Proceedings of the 28th ACM SIGKDD Conference on Knowledge Discovery and Data Mining, New York, NY, USA, 14 August 2022; pp. 4402–4412. [ Google Scholar ]
- Jin, K.; Ye, J. Artificial Intelligence and Deep Learning in Ophthalmology: Current Status and Future Perspectives. Adv. Ophthalmol. Pract. Res. 2022 , 2 , 100078. [ Google Scholar ] [ CrossRef ]
- Bai, J.; Wan, Z.; Li, P.; Chen, L.; Wang, J.; Fan, Y.; Chen, X.; Peng, Q.; Gao, P. Accuracy and Feasibility with AI-Assisted OCT in Retinal Disorder Community Screening. Front. Cell Dev. Biol. 2022 , 10 , 1053483. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Liu, X.; Zhao, C.; Wang, L.; Wang, G.; Lv, B.; Lv, C.; Xie, G.; Wang, F. Evaluation of an OCT-AI–Based Telemedicine Platform for Retinal Disease Screening and Referral in a Primary Care Setting. Transl. Vis. Sci. Technol. 2022 , 11 , 4. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bertolini, M.; Rossoni, M.; Colombo, G. Operative Workflow from CT to 3D Printing of the Heart: Opportunities and Challenges. Bioengineering 2021 , 8 , 130. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cappello, I.A.; Candelari, M.; Pannone, L.; Monaco, C.; Bori, E.; Talevi, G.; Ramak, R.; La Meir, M.; Gharaviri, A.; Chierchia, G.B.; et al. 3D Printed Surgical Guide for Coronary Artery Bypass Graft: Workflow from Computed Tomography to Prototype. Bioengineering 2022 , 9 , 179. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhang, Z.; Li, Y.; Shin, B.-S. Robust Medical Image Colorization with Spatial Mask-Guided Generative Adversarial Network. Bioengineering 2022 , 9 , 721. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- National Library of Medicine Visible Human Project. Available online: https://www.nlm.nih.gov/research/visible/visible_human.html (accessed on 16 June 2023).
- Bloch, B.N.; Madabhushi, A.; Huisman, H.; Freymann, J.; Kirby, J.; Grauer, M.; Enquobahrie, A.; Jaffe, C.; Clarke, L.; Farahani, K. NCI-ISBI 2013 Challenge: Automated Segmentation of Prostate Structures (ISBI-MR-Prostate-2013). 2015. Available online: https://www.cancerimagingarchive.net/analysis-result/isbi-mr-prostate-2013/ (accessed on 16 June 2023).
- Selvaraju, R.R.; Cogswell, M.; Das, A.; Vedantam, R.; Parikh, D.; Batra, D. Grad-CAM: Visual Explanations from Deep Networks via Gradient-Based Localization. Int. J. Comput. Vis. 2020 , 128 , 336–359. [ Google Scholar ] [ CrossRef ]
- Zaffino, P.; Marzullo, A.; Moccia, S.; Calimeri, F.; De Momi, E.; Bertucci, B.; Arcuri, P.P.; Spadea, M.F. An Open-Source COVID-19 CT Dataset with Automatic Lung Tissue Classification for Radiomics. Bioengineering 2021 , 8 , 26. [ Google Scholar ] [ CrossRef ]
- Ahmad, W.; Ali, H.; Shah, Z.; Azmat, S. A New Generative Adversarial Network for Medical Images Super Resolution. Sci. Rep. 2022 , 12 , 9533. [ Google Scholar ] [ CrossRef ]
- Bing, X.; Zhang, W.; Zheng, L.; Zhang, Y. Medical Image Super Resolution Using Improved Generative Adversarial Networks. IEEE Access 2019 , 7 , 145030–145038. [ Google Scholar ] [ CrossRef ]
- Zhu, J.; Yang, G.; Lio, P. A Residual Dense Vision Transformer for Medical Image Super-Resolution with Segmentation-Based Perceptual Loss Fine-Tuning. arXiv 2023 , arXiv:2302.11184. [ Google Scholar ]
- Wei, C.; Ren, S.; Guo, K.; Hu, H.; Liang, J. High-Resolution Swin Transformer for Automatic Medical Image Segmentation. Sensors 2023 , 23 , 3420. [ Google Scholar ] [ CrossRef ]
- Zhang, K.; Hu, H.; Philbrick, K.; Conte, G.M.; Sobek, J.D.; Rouzrokh, P.; Erickson, B.J. SOUP-GAN: Super-Resolution MRI Using Generative Adversarial Networks. Tomography 2022 , 8 , 905–919. [ Google Scholar ] [ CrossRef ]
- Yang, H.; Wang, Z.; Liu, X.; Li, C.; Xin, J.; Wang, Z. Deep Learning in Medical Image Super Resolution: A Review. Appl. Intell. 2023 , 53 , 20891–20916. [ Google Scholar ] [ CrossRef ]
- Chen, C.; Wang, Y.; Zhang, N.; Zhang, Y.; Zhao, Z. A Review of Hyperspectral Image Super-Resolution Based on Deep Learning. Remote Sens. 2023 , 15 , 2853. [ Google Scholar ] [ CrossRef ]
- Menze, B.H.; Jakab, A.; Bauer, S.; Kalpathy-Cramer, J.; Farahani, K.; Kirby, J.; Burren, Y.; Porz, N.; Slotboom, J.; Wiest, R.; et al. The Multimodal Brain Tumor Image Segmentation Benchmark (BRATS). IEEE Trans. Med. Imaging 2015 , 34 , 1993–2024. [ Google Scholar ] [ CrossRef ]
- The 2023 Kidney Tumor Segmentation Challenge. Available online: https://kits-challenge.org/kits23/ (accessed on 20 October 2023).
- Rajpurkar, P.; Irvin, J.; Bagul, A.; Ding, D.; Duan, T.; Mehta, H.; Yang, B.; Zhu, K.; Laird, D.; Ball, R.L.; et al. MURA: Large Dataset for Abnormality Detection in Musculoskeletal Radiographs. arXiv 2018 , arXiv:1712.06957. [ Google Scholar ]
- MedPix. Available online: https://medpix.nlm.nih.gov/home (accessed on 12 December 2023).
- NIH Chest X-rays. Available online: https://www.kaggle.com/datasets/nih-chest-xrays/data (accessed on 12 December 2023).
| Name | Description | Reference |
|---|---|---|
| BRATS | The Multimodal Brain Tumor Segmentation Benchmark (BRATS) is an annual challenge that aims to compare different algorithms for brain tumor segmentation. The dataset, which has received several enhancements over the years, consists of preoperative multimodal MRI scans of glioblastoma and lower-grade glioma with ground truth labels and survival data for participants to segment and predict the tumor. | [ ] |
| KiTS | The Kidney Tumor Segmentation Benchmark (KiTS) is a dataset used to evaluate and compare algorithms for kidney tumor segmentation. The dataset consists of CT scans of the kidneys and kidney tumors, with 300 scans in total. The data and segmentations are provided by various clinical sites around the world. | [ ] |
| LiTS | The Liver Tumor Segmentation Benchmark (LiTS) is a dataset used to evaluate and compare liver tumor segmentation algorithms. The dataset consists of CT scans of the liver and liver tumors, with 130 scans in the training set and 70 scans in the test set. The data and segmentations are provided by various clinical sites around the world. | [ ] |
| MURA | The Musculoskeletal Radiographs (MURA) dataset is a large dataset of musculoskeletal radiographs containing 40,561 images from 14,863 studies. Each study is manually labeled by radiologists as either normal or abnormal. | [ ] |
| MedPix | A free online medical image database with over 59,000 indexed and curated images from over 12,000 patients. | [ ] |
| NIH Chest X-rays | A large dataset of chest X-ray images containing over 112,000 images from more than 30,000 unique patients. The images are labeled with 14 common disease labels. | [ ] |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Pinto-Coelho, L. How Artificial Intelligence Is Shaping Medical Imaging Technology: A Survey of Innovations and Applications. Bioengineering 2023 , 10 , 1435. https://doi.org/10.3390/bioengineering10121435
Pinto-Coelho L. How Artificial Intelligence Is Shaping Medical Imaging Technology: A Survey of Innovations and Applications. Bioengineering . 2023; 10(12):1435. https://doi.org/10.3390/bioengineering10121435
Pinto-Coelho, Luís. 2023. "How Artificial Intelligence Is Shaping Medical Imaging Technology: A Survey of Innovations and Applications" Bioengineering 10, no. 12: 1435. https://doi.org/10.3390/bioengineering10121435
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

IEEE Account
- Change Username/Password
- Update Address
Purchase Details
- Payment Options
- Order History
- View Purchased Documents
Profile Information
- Communications Preferences
- Profession and Education
- Technical Interests
- US & Canada: +1 800 678 4333
- Worldwide: +1 732 981 0060
- Contact & Support
- About IEEE Xplore
- Accessibility
- Terms of Use
- Nondiscrimination Policy
- Privacy & Opting Out of Cookies
A not-for-profit organization, IEEE is the world's largest technical professional organization dedicated to advancing technology for the benefit of humanity. © Copyright 2024 IEEE - All rights reserved. Use of this web site signifies your agreement to the terms and conditions.
Appointments at Mayo Clinic
- Consumer health
Telehealth: Technology meets health care
See how technology can improve your health care.
How many times have you heard it said that the internet has changed modern life? Indeed, it's likely changed how you stay in touch with family and friends and buy goods and services. And it's probably even changed how you search for information about health problems.
Several telehealth tools are offered to help you manage your health care and receive the services you need. During the coronavirus disease 2019 (COVID-19) pandemic, many people used telehealth. People often still use it. Find out more about telehealth.
What is telehealth?
Telehealth is the use of digital information and communication technologies to access health care services remotely and manage your health care. Technologies can include computers and mobile devices, such as tablets and smartphones. This may be technology you use from home. Or a nurse or other health care professional may provide telehealth from a medical office or mobile van, such as in rural areas. Telehealth can also be technology that your health care provider uses to improve or support health care services.
The goals of telehealth, sometimes called e-health or m-health (mobile health), include the following:
- Make health care easier to get for people who live in communities that are remote or in the country.
- Keep you and others safe if you have an infectious disease such as COVID-19.
- Offer primary care for many conditions.
- Make services more easily offered or handy for people who have limited ability to move, time or transportation.
- Offer access to medical specialists.
- Improve communication and coordination of care among health care team members and a person getting care.
- Offer advice for self-management of health care.
Many people found telehealth helpful during the COVID-19 pandemic and still use it. Telehealth is being used more often.
Here are many examples of telehealth services that may be helpful for your health care.
Virtual visits
Some clinics may use telemedicine to offer remote care. For example, clinics may offer virtual visits. These can allow you to see a health care provider, mental health counselor or a nurse via online video or phone chats.
Virtual visits can offer care in many conditions such as migraines, skin conditions, diabetes, depression, anxiety, colds, coughs and COVID-19. These visits allow you to get care from a provider when you don't need or can't get an in-person visit.
Before your visit, your health care team may send you information or forms to fill out online and return to them. They may also make sure you have the technology you need. They'll check to see if you need to update or install any software or apps too. And they can tell you how to sign on and join the video chat for your visit. Also, the health care team can explain how to use the microphone, camera and text chat. If needed, ask a family member to help you set up the technology you need.
You only need a smartphone, tablet or computer with internet access to join the virtual visit. You can find a comfortable, quiet, private spot to sit during your visit. Your provider also meets from a private place.
Other options
Some people may use web or phone-based services for medical care or advice. When you log into a web-based service or call a service that offers primary or urgent care, you're guided through many questions. The provider or nurse practitioner can prescribe drugs. Or they may suggest home care tips or more medical care.
While these services are handy, they have drawbacks:
- Treatment may not be coordinated with your regular provider.
- Important details from your medical history may not be considered.
- The computer-driven model used to make decisions may not be right for you if you have a complex medical history.
- The service doesn't easily allow for you to make decisions with your provider about treatments.
Remote monitoring
Many technologies allow your provider or health care team to check your health remotely. These technologies include:
- Web-based or mobile apps for uploading data to your provider or health care team. For example, if you have diabetes, you may upload food logs, blood sugar levels and drugs that a nurse checks.
- Devices that measure and wirelessly send data, such as blood pressure, blood sugar and oxygen levels.
- Wearable devices that automatically record and send data. For example, the devices may record data such as heart rate, blood sugar, how you walk, your posture, tremors, physical activity or your sleep.
- Home monitoring devices for older people or people with dementia that can find changes in daily activities such as falls.
- Devices that send notifications to remind you to do exercises or take drugs.
Providers talking to providers
Providers can also use technology to give people better care. For example, in a virtual consultation, primary care providers can get input from specialists in other locations when they have questions about your diagnosis or treatment.
The primary care provider sends exam notes, history, test results, X-rays or other images to the specialist to review. The specialist may answer by email. Or they may do a virtual visit with you at your provider's office. They may also ask for a face-to-face meeting.
In some cases, a nurse or other health care professional may use technology to provide care from a medical office, clinic or mobile van in a rural area. They may call a specialist or provider at a medical clinic to do a remote consult.
These virtual consultations may prevent unnecessary in-person referrals to a specialist. They may also cut wait times for you to see a specialist. And they may remove the need for you to travel to a specialist.
Patient portal
Your primary care clinic may have an online patient portal. These portals offer a safer way of contacting your provider instead of email. A portal provides a safe online tool to do the following:
- Message your provider or a nurse.
- Ask for prescription refills.
- Review test results and summaries of earlier visits.
- Schedule visits or ask for appointment reminders for preventive care.
If your provider is in a large health care system, the portal may also provide one point of contact for any specialists you may see.
Personal health apps
Many apps have been made to help people better organize their medical information in one secure place. These digital tools may help you:
- Store personal health information.
- Record vital signs.
- Calculate and track your calories.
- Schedule reminders for taking drugs.
- Record physical activity such as your daily step count.
- Personal health records
An electronic personal health record system (PHR system) is a collection of information about your health that you control and maintain. A PHR app is easy for you to see anytime via a web-enabled device, such as your computer, laptop, tablet or smartphone. A PHR also allows you to review your lab results, X-rays and notes from your provider. Your provider may give this to other providers with permission.
In an emergency, a personal health record can quickly give emergency staff vital information. For example, it can show your current conditions, drugs, drug allergies and your provider's contact details.
The potential of telehealth
Technology has the potential to improve the quality of health care. And technology can make it easier for more people to get health care.
Telehealth may offer ways to make health care more efficient, better coordinated and closer to home. You can go to a virtual visit anywhere — such as at home or in your car. And you don't need to travel to go to a virtual visit.
Telehealth can be useful so you can stay home if you're sick or if it's hard for you to travel. And you can use telehealth if you live far from a medical center. And many people have been able to keep distance from others at home and still receive care during the COVID-19 pandemic. And providers can diagnose and treat COVID-19 remotely.
Virtual visits can also provide you with the choice to meet with specialists who don't live where you do.
The limitations of telehealth
Telehealth has potential for better coordinated care. But it also runs the risk of gaps in care, overuse of medical care, inappropriate drug use or unnecessary care. Providers can't do a physical exam in-person, which can affect a diagnosis.
The potential benefits of telehealth services may be limited by other factors, such as costs. Insurance reimbursement for telehealth can vary by state and type of insurance in the U.S. But insurance keeps expanding for telehealth services in the U.S. And during the COVID-19 pandemic, insurance restrictions changed for a period of time. Check with your insurance company to see which providers have virtual visits covered by insurance.
Also, some people who need improved access to care may be limited because of not having internet access or a mobile device. People without internet access may be able to access telehealth services by using wireless internet offered at public places. For example, libraries or community centers may offer wireless internet for virtual visits that can take place in private rooms.
Sometimes technology doesn't work well. It's important to have a plan with your provider to call them by phone if there is an issue with the virtual visit.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Telehealth. National Institute of Biomedical Imaging and Bioengineering. https://www.nibib.nih.gov/science-education/science-topics/telehealth. Accessed May 6, 2022.
- What is telehealth? Telehealth.HHS.gov. https://telehealth.hhs.gov/patients/understanding-telehealth/. Accessed May 6, 2022.
- Ong MK, et al. Telemedicine for adults. https://www.uptodate.com/contents/search. Accessed May 5, 2022.
- Doraiswamy S, et al. Use of telehealth during the COVID-19 pandemic: Scoping review. Journal of Medical Internet Research. 2020; doi:10.2196/24087.
- Brotman JJ, et al. Providing outpatient telehealth services in the United States: Before and during coronavirus disease 2019. Chest Reviews. 2021; doi:10.1016/j.chest.2020.11.020.
- Telehealth: Defining 21st century care. The American Telemedicine Association. https://www.americantelemed.org/resource/why-telemedicine/. Accessed May 6, 2022.
- Mahtta D, et al. Promises and perils of telehealth in the current era. Current Cardiology Reports. 2021; doi:10.1007/s11886-021-01544-w.
- AskMayoExpert. COVID-19: Outpatient management. Mayo Clinic; 2021.
- Tapuria A, et al. Impact of patient access to their electronic health record: Systematic review. 2021; doi:10.1080/17538157.2021.1879810.
- Takahashi PY (expert opinion). Mayo Clinic. May 9, 2022.
Products and Services
- The Mayo Clinic Diet Online
- A Book: Live Younger Longer
- Assortment of Health Products from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Guide to Home Remedies
- A Book: Mayo Clinic Family Health Book, 5th Edition
- A Book: The Mayo Clinic Diet Bundle
- A Book: Mayo Clinic on Digestive Health
- Myths about cancer causes
- Emergency essentials: Putting together a survival kit
- Emergency health information
- Kidney donation: Are there long-term risks?
- Living wills
- Organ donation: Don't let these myths confuse you
- Osteopathic medicine
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Telehealth Technology meets health care
We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Clinicoecon Outcomes Res
Medical technology as a key driver of rising health expenditure: disentangling the relationship
Corinna sorenson.
1 LSE Health, London School of Economics and Political Science, London, UK;
2 European Health Technology Institute for Socioeconomic Research, Brussels, Belgium;
Michael Drummond
3 Centre for Health Economics, University of York, York, UK
Beena Bhuiyan Khan
Health care spending has risen steadily in most countries, becoming a concern for decision-makers worldwide. Commentators often point to new medical technology as the key driver for burgeoning expenditures. This paper critically appraises this conjecture, based on an analysis of the existing literature, with the aim of offering a more detailed and considered analysis of this relationship. Several databases were searched to identify relevant literature. Various categories of studies (eg, multivariate and cost-effectiveness analyses) were included to cover different perspectives, methodological approaches, and issues regarding the link between medical technology and costs. Selected articles were reviewed and relevant information was extracted into a standardized template and analyzed for key cross-cutting themes, ie, impact of technology on costs, factors influencing this relationship, and methodological challenges in measuring such linkages. A total of 86 studies were reviewed. The analysis suggests that the relationship between medical technology and spending is complex and often conflicting. Findings were frequently contingent on varying factors, such as the availability of other interventions, patient population, and the methodological approach employed. Moreover, the impact of technology on costs differed across technologies, in that some (eg, cancer drugs, invasive medical devices) had significant financial implications, while others were cost-neutral or cost-saving. In light of these issues, we argue that decision-makers and other commentators should extend their focus beyond costs solely to include consideration of whether medical technology results in better value in health care and broader socioeconomic benefits.
Introduction
Health care spending has risen at rates greater than gross domestic product in most OECD countries. In 2009, average health spending reached 9.5% of gross domestic product, up from 8.8% in 2008 1 ( Figure 1 ). During the same time period, average per capita spending increased by an average of 3.8% in 2008 and 3.5% in 2009, with public spending on health growing at an even faster rate of 4.8% and 4.1%, respectively. 1 For most countries, rising health expenditure is considered an enduring challenge and one that requires a complex balancing act between cost control, affordable and equitable access to beneficial treatments, and support for innovation.

Total expenditure on health as a percentage of gross domestic product (GDP) (1980–2009).
Notes: *All data from 1980 except for Czech Republic (1990), Hungary (1991), Italy (1998), Poland (1990), and Slovenia (1995); **all data from 2009, except for Portugal (2008).
OECD Health Data 2011. 1
A number of factors have been identified as contributors to spending growth, including the ageing of populations, increased public demand and expectations, personal income growth, rising prices of physician and hospital services (eg, labor costs), and inefficiencies in the organization and payment of care. For example, the growth in life expectancy has had an obvious yet gradual impact on the demand for health care. Although the use of care depends ultimately on the health status of a person and not necessarily on their age cohort(s), elderly people use health care more often and more intensively than younger populations, with a high proportion of costs garnered at the end of life. 2 Longer life spans, in concert with an increase in unhealthy lifestyles, have also contributed to an increased prevalence of disease, particularly chronic conditions such as obesity, diabetes, and cancer. Greater prevalence of chronic conditions are likely to increase spending both through an increase in treated prevalence (ie, number of cases treated) and the cost of treatment (ie, spending per case).
However, analysts often point to advances in medical technology and their diffusion across health systems as the principal driver for burgeoning expenditures. 3 – 10 This paper critically examines this conjecture, based on an analysis of a broad range of existing evidence on the relationship between medical technology diffusion and health expenditure. We strive to focus on medical devices, given the gap in the literature on their role in health expenditures, which has predominantly centered on pharmaceuticals, and because the sector has grown considerably in recent years. Not only are there substantially more medical technologies on the market, but they have grown increasingly sophisticated.
The paper is structured as follows. We first outline the methods used to review the literature, followed by a summary of the available evidence. The paper then discusses the complexities inherent to ascertaining the impact of technology on spending, including some of the methodological challenges associated with demonstrating and quantifying this link. Based on the analysis, we close by arguing that while the impact of medical technology on rising costs is an important concern and area of inquiry, attention should also be focused on exploring whether investments in medical technology result in better value, as measured by therapeutic benefit, cost-effectiveness, and other important outcomes (eg, quality of life, improved productivity) in health care, and under which conditions technologies allow for the most effective and efficient use of available health care resources. We offer some general suggestions for what might be done to support this end.
Materials and methods
A literature review was conducted to explore the current evidence base on the relationship between medical technology and health care expenditures. Unlike previous studies in this area, we considered a wide range of literature to ensure adequate coverage of different methodological approaches and ideological perspectives for assessing this relationship. The categories of literature included in the search and review included general and descriptive analyses, policy analyses, literature reviews, multivariate analyses, cost-effectiveness analyses, and cost impact studies of specific technologies. Table 1 presents and describes the various study types included in the review.
Types of studies included in the review
| General and descriptive analyses | Generally provide an in depth analysis of the main variables or factors affecting health expenditures. Some of these studies take a broad approach examining a range of variables, while others focus on a particular issue, such as medical technology, on spending. Furthermore, studies vary in whether they examine national-level expenditures or take a narrower approach by assessing hospital spending. Most of these studies are qualitative. |
| Policy analyses | Evaluate the impact of different policy interventions (eg, managed care, changes to hospital organization or services) and their impact on health expenditures, as well as on mediating factors, such as technology diffusion. Other policy studies consider the implications of high expenditures associated with a particular cost driver (eg, aging, technological advancement). Analyses can be either qualitative or quantitative in nature. |
| Literature reviews | Assess the current literature on the impact of a particular factor or a broad array of factors on health expenditures. This category includes systematic reviews and general literature reviews. |
| Econometric analyses | Typically entails multivariate studies, which examine multiple variables and their effects (and interrelationships) on health expenditures. These studies employ three methodological approaches most frequently, including the “residual” approach, the “proxy” approach, and case studies of specific technologies. The residual approach measures the impact of certain demographic and economic factors (eg, population aging) known to affect health expenditures and then attributes the unexplained portion of spending growth to medical technology. The proxy approach is an indirect method, which employs a measurable proxy indicator for technological change (eg, spending on research and development, time, patents) to explain health care spending trends. The case study approach examines how a specific technology and the associated changes in clinical practice affect spending on specific types of patients, conditions, or settings. |
| Cost-effectiveness analyses | Assess the cost and clinical benefits of a given technology. Such studies seek to ascertain the value for money of a particular intervention. This approach often entails combining clinical benefit with quality of life in a single generic measure of health gain, the quality-adjusted life year, in a cost-utility analysis. |
| Cost impact studies | Evaluate the impact of specific technologies or policies on costs, either at one point in time or over time. |
Key databases, including PubMed, EMBASE, MEDLINE, and EconLit, were searched to identify relevant literature. The search terms employed to identify relevant literature included “technolog* AND (expenditure OR cost) AND (health OR healthcare)”, and “medical AND technolog* AND (expenditure OR cost)”.
To identify relevant cost-effectiveness analyses across all medical technologies would be a considerable task. Therefore, we took advantage of two previously completed systematic reviews of economic evaluations of medical devices in the cardiology and orthopedic sectors, the two most significant markets for therapeutic devices. 11 In these reviews, we used the National Health Service Economic Evaluation Database 12 for the searches, which contains structured reviews (abstracts) of full economic evaluations of health care treatments and programs. In these two previously conducted studies, we employed the following search terms “cardiology”, “cardiac rhythm management”, “cardiovascular”, “coronary stents”, “cardiac resychronization”, “implantable cardioverter defibrillators”, “orthopaedic”, “hip”, “knee”, “shoulder”, “ankle”, “elbow”, “arthroplasty”, and “joint”.
All the relevant abstracts were reviewed, from both the general literature review and the review of National Health Service Economic Evaluation Database. Duplicate and irrelevant abstracts were identified and eliminated. Selected articles were reviewed according to a data extraction form, developed in Microsoft Excel, to standardize the review and facilitate subsequent analysis of the collated information. The categories of information extraction included: basic bibliographic information; publication year; literature type (eg, descriptive analysis); study aims; technologies studied; study setting; methods employed; outcomes across health, costs/expenditures, and cost-effectiveness; and, stated conclusions and implications of the study. The information extracted was then analyzed for key themes across the domains interest (ie, impact of medical technology on costs or spending and factors influencing this relationship, and the methodological challenges noted in measuring such linkages).
A total of 86 studies were included in the review ( Appendix 1 ). Table 2 provides a summary of general study details. The majority (52%) of studies were more qualitative in nature (eg, descriptive and policy analyses, literature reviews), followed by cost-effectiveness (40%) and multivariate (24%) analyses. In addition, the bulk of studies were published within the last ten years (77%) and focused on the US (52%). With the exception of cost-effectiveness and cost impact studies examining specific medical devices, most studies (52%) examined medical technology in general, which in some cases included some combination of drugs, devices, diagnostics, or procedures.
Characteristics of the reviewed literature
| General/descriptive analysis | 12 | 1980–1985 | 1 |
| Policy analysis | 8 | 1986–1990 | 2 |
| Literature review | 4 | 1991–1995 | 5 |
| Multivariate analysis | 21 | 1996–2000 | 12 |
| Cost-effectiveness analysis | 34 | 2001–2005 | 37 |
| Cost impact study | 7 | 2006–2010 | 29 |
| General health technology | 27 | US | 45 |
| Specific medical devices | 41 | Europe | 21 |
| Specific drugs | 3 | OECD | 5 |
| Combination of specific drugs, devices, and/or services | 7 | Canada | 5 |
| Other | 8 | Other | 10 |
Although technological innovation is of great significance in health care 13 , 14 and has been claimed to be a key driver of health spending, the review highlighted that research measuring the potential contributions of medical technology to rising health care costs has been relatively sparse. One possible reason for this neglect, and the predominant reliance on more descriptive or qualitative analyses among available studies, is that technology itself and its possible implications on health expenditures are insufficiently understood. Other reasons center on the often limited data available to explore this relationship and the complexities of measuring such associations, which we discuss further below.
The available evidence that does exist suggests that, in general, new medical technology is an important determinant in rising health care expenditures. Of the studies reviewed that attempted to quantify this relationship, mainly econometric studies, the overall impact (ie, proportion of the cost increase) ranges from approximately 25% to 75%, averaging at about 50% 7 , 9 , 10 , 14 – 19 ( Table 3 ).
Contributions of selected factors to growth in health care spending
| Life expectancy/aging | ∼9% | 15% | 2% | 6%–7% | 2% | 2% | |
| Administrative costs | 15% | 3%–10% | 13% | ||||
| Changes in financing | 10% | 4%–5% | 10% | 10% | |||
| Personal income growth | 9%–20% | 11%–18% | 14%–18% | 5% | <23% | ||
| Health care prices | 18% | 11%–22% | 19% | ||||
| Technology | ∼65% | 50%–75% | 25% | 38%–62% | 70%–75% | 49% | >65% |
While much of the quantitative evidence indeed substantiated the cost-increasing effect of new technology overall, the broader spectrum of evidence (eg, cost-effectiveness studies, descriptive analyses) suggests that the relationship between technological advances and health care expenditure is not straightforward or static. Rather, it should be understood as being complex, with a wide range of potential intervening factors that change and shift the dynamic of the association, depending on the particular circumstances.
For example, this relationship often differed across technologies, with some exerting more upward pressure on health care expenditure than others. Of 16 diseases (and subgroups) studied by Scitovski 20 in a case study, new technology decreased costs in eight cases, increased costs in seven, and in one case had neutral effects. The use of “low-tech” technologies such as electrocardiography, laboratory tests, and x-rays stabilized or increased costs at a moderate pace, while the use of complex or sophisticated technologies and procedures such as cesarean section, new treatment modalities for breast cancer, and coronary bypass surgery substantially increased costs. In another case study, Bryan et al 21 found that technology that introduces computer-based information networks for imaging archiving increased annual hospital costs by 1.8%. A Congressional Budget Office 6 review of the available economic literature highlighted particular areas of technology advancement that has been accompanied by more spending, including revascularization for coronary artery disease, diagnostic imaging, and joint replacement.
Whether a particular technology increases or decreases costs depends on whether a given technology: substitutes for an existing service; expands the number of treatable conditions, in that it allows providers to treat conditions they previously could not treat or could not treat effectively or aggressively; intensifies level of use of the technology for the same condition; impacts the delivery of care (eg, improves the capacity of the system to treat more patients); broadens the definition of diseases; and extends life, for which each patient bears (or induces) additional years of health care consumption. 6 , 17 , 22 – 25
For instance, with regards to increasing the indications and applications of the innovations, the initial use of imaging diagnostics (eg, x-rays, computed tomography, magnetic resonance) was initially targeted to specific organs and functions, but their application has extended to almost every part of the human body, resulting in increased spending. 26 Further, some new technologies may allow lower unit costs (ie, treatment becomes cheaper) or cause less discomfort or complications, thereby offering the potential for cost savings. However, these benefits may lead to increased provision of services to persons who, without the new technology, may not have undergone a particular treatment. Therefore, when the cost savings per case are offset by the increased number of procedures, these technologies will result in increased costs in the aggregate, but will almost certainly also increase the total benefits from the care provided. Chernew et al 27 found this was the case with regard to introduction of laparoscopic techniques at the beginning of the 1990s in the US. Of course, new technology can also help extend life (in patients with life-threatening or chronic conditions), which may result in higher spending due to extended years of health care utilization. However, in parallel, a given technology may also allow individuals to live those additional years with greater quality of life or in an improved health state, which could bring potential cost-savings and/or broader social benefits.
In contrast, those technologies that have a substitutive effect, thereby reducing treatment with older technology, eg, use of percutaneous transluminal coronary angioplasty (PTCA) and coronary artery bypass grafting (CABG), may facilitate reductions in spending, even if treatment expansion follows. 25 , 26 For example, PTCA outcomes improved through the introduction of coronary stents, leading to reduced occurrence of restenosis, heart attacks, emergency CABG, and mortality. Consequently, the procedures had become highly substitutable with CABG and for patients with severe coronary artery disease. While the growth of PTCA resulted in higher costs, this has been offset over time by the substitution of PTCA for CABG. Therefore, by metrics of costs, the diffusion of some new technologies can increase spending rapidly at first as it treats those who went without, and less rapidly over time as technology substitutes for more expensive existing treatments. 28 , 29
Moreover, the impact of technology on costs varies depending on the circumstances (eg, patient population, placement in treatment pathway) within which a given therapy is used. For example, several cost-effectiveness analyses on drug-eluting stents have demonstrated that use of these devices increased per patient treatment costs compared with standard balloon angioplasty. 30 – 32 However, if used in medium-risk to high-risk patients, drug-eluting stents could be cost-neutral 31 , 32 or even cost-saving. 30
There are also organizational, economic, and social considerations that influence the link between new technology and spending and arguably interplay with the aforementioned factors. For example, impacts on costs may be affected by how the technology is administered or impacts the delivery of care, because some innovations may lead to an increased use of medical personnel, material supplies, or training, particularly if they employ a new technique or procedure, while others may reduce staff or time requirements or shift care to less costly settings of care (eg, inpatient to outpatient). 33 , 34 In particular, some technologies may improve the efficiency of care delivery by reducing procedure time, length of stay, or number of hospitalizations, thereby increasing the capacity of the hospital to treat additional patients. Overall costs may rise as a result, but such outlays will likely result in improved health outcomes for a greater number of patients.
Finally, technological advancements may generate consumer demand for care (and, perhaps more intense, costly services, even if not cost-effective), as well as the demand for insurance. 17 , 27 , 35 , 36 At the same time, expanding insurance provides increased incentives to develop new technologies. 22 Some analysts maintain that such incentives contribute to long-term growth in expenditure, because the development costs of these products must be recouped by industry (leading to higher prices). 6 Although much of this evidence originates from the US, Barros and Martinez-Giralt 37 also found that payment systems affect the rate of technology adoption and utilization in European systems. National procurement policies and practices may also influence their diffusion into the health system and the costs associated with adoption. For example, use of more centralized purchasing strategies (eg, local or regional procurement consortiums) or value-based purchasing in Europe and elsewhere, where payment is directly linked to the quality and efficiency of a new technology, may reduce spending. 38 , 39
In relation to this point, there are important differences between countries and their respective health systems that influence the adoption and diffusion of new technologies. For instance, technological change often results from incentives in the health care system. Given that incentive structures differ across countries, technology influences spending differently across jurisdictions. 40 Lambooij et al 41 assert that lower resourced countries encourage diffusion of innovations that enhance efficiency, whereas better resourced jurisdictions encourage diffusion of complex, expensive technologies.
The results of our review suggest that medical technology does have a significant role in health care expenditures, albeit a dynamic and complex one. However, there are limitations to the methodological approaches used in the available published literature, which introduce challenges to arriving at a clear assessment of such dynamics. For example, in terms of quantifying this link, the residual approach 4 , 10 , 17 can yield a reasonable indirect approximation of how medical technology relates to long-term growth in total health expenditure, but it can be sensitive to assumptions regarding the effects of other related factors (eg, personal income, health insurance coverage, technology development) and the dynamics between them. 6 , 18 This frequently leads to an overestimation of the effect of technology on spending. Another common method, ie, the proxy approach, 14 , 15 is only as good as the proxy indicator used to assimilate the impact of technology on spending. The use of time as a proxy measure for technological change, for example, not only captures such changes, but may also encapsulate variations in policy, patient experiences, preference, and expenditures. 15
Another method, ie, the case study approach, 25 , 26 is useful to explain the impact of certain medical technologies on health care costs, but there are problems of sampling and it is difficult to generalize to an aggregate or national level. 6 , 19 Consequently, most analysts using this approach have focused on the most significant conditions (eg, prevalent, contributing to high levels of mortality or disability), such as heart disease. These technical issues also characterize cost-effectiveness and cost impact analyses. 42 – 45
In addition to the limitations noted with individual approaches, there are technical issues shared across the various methods. Firstly, the results are frequently based on aggregate level data that are often subject to potential endogeneity and omit variable bias. 46 Secondly, as intimated above, several of these methods can depend on relatively simplified models dealing with highly complicated and interrelated parameters 16 and can only arrive at conclusions about the collective effect of technology on health care spending, not on the contributions of specific technologies. Different types of technologies (eg, drugs versus medical devices) arguably impact health spending differently, particularly in terms of the associated changes in clinical practice that follow their adoption. For example, a recent study 47 estimated that medical devices account for a relatively small share of national health expenditures (3%–5%), which have risen only slightly over the last 20 years, ie, a trend different from that of pharmaceuticals. Thirdly, across both quantitative and qualitative approaches, capturing the economic (and social) complexities surrounding the use of technology can be challenging, because it generally necessitates a complete understanding of the manner and magnitude of change in the clinical management pathway associated with treatment and follow-up. This process can occur over extended periods of time, and can have varying resource costs that can be both easy and difficult to measure. 48
Available studies are often focused on a narrow time window and the specific duration of the life cycle for a technology. Therefore, results from studies with longer or different time periods could vary. For instance, the price of medical technologies generally decreases over time, which would not be captured in shorter-term studies or those that happen to examine a given technology(s) close to initial launch. similarly, technological advances occur simultaneously with changes in other factors that affect health care spending, such as personal income and health financing systems, which make it difficult to identify causality reliably, and exactly how technology itself affects spending growth. Finally, current methods cannot effectively demonstrate the cost impact that would result if availability of technology were reduced or eliminated. In the short-term, cost-savings may be achieved, while limited access to technology may result in higher costs in the long term due to the presence of disease that was not adequately treated owing to reliance on older, less-effective technologies or a complete lack of viable treatment alternatives.
Therefore, while examining the role of medical technology in rising health expenditures is indeed an important area of inquiry, it is largely an incomplete exercise, due to some of the noted methodological issues, and also because most new technological innovations are cost-increasing. Even if a given technology increases costs, it may increase benefits by an even greater amount. In addition, the same technology, applied in different settings, or in different groups of patients, could be cost-effective in some instances and not in others. Consequently, alongside simply examining costs, it is perhaps more productive to assess whether the additional benefits resulting from the use of the technology justify any increase in costs and under which circumstances technologies deliver greater value in health care. That is, are the resulting spending levels reflected in more effective, cost-effective, and higher quality health care?
Several studies from the review indicate that, on average, increases in spending as a result of technological advances have provided reasonable value. For example, Cutler et al 49 found that from 1960 to 2000, average life expectancy increased by 7 years, 3.5 years of which were attributable to improvements in health care. Comparing the value of a year of life (anywhere from $50,000 to $200,000) with the finding that each year of increased life expectancy cost about $19,900 in health spending, they conclude that the increased spending, on average, had been a worthwhile investment. similar conclusions were arrived at by Cutler and McClellan 25 and Skinner et al 50 in examining technological innovation in cardiac care. The former, for example, demonstrated that the use of new technology helped to increase the average coronary patient’s life expectancy by one year (valued at $70,000 per case), while treatment costs increased $10,000 per case (4.2% per year), for a net benefit of $60,000 per case. In addition, as previously discussed, cost-effectiveness analyses of particular medical devices demonstrate value for money (as measured by cost per quality-adjusted life year) and in some limited cases, cost savings. 30 , 31 , 42 , 51 – 53 On a broader level, Fuchs and Sox 54 surveyed physician perceptions of the importance of and value brought by various areas of technological innovation, with magnetic resonance imaging and computed tomographic scanning, angiotensin-converting enzyme inhibitors, balloon angioplasty, statins, and mammography all rated highly.
Before concluding, it is important to note a few limitations to this study. Firstly, while we strove to select and review only studies focused on medical technology, some studies, particularly certain types of econometric studies, looked at technology collectively. Therefore, for those studies, we were unable to distinguish the relative contribution of different types of technology (eg, drugs versus devices) to the proportion of spending attributed to technological innovation. Secondly, we focused our review of cost-effectiveness studies only on selected cardiology and orthopedic devices. Nevertheless, these particular sectors are arguably important markets and those most likely to have a cost impact.
Major technological advances in medical science have allowed health care providers to diagnose and treat illnesses in ways that were previously impossible. In general, such developments have tended to increase health care spending, which has been seen as an important policy concern, especially considering ever-limited health care budgets.
However, examining the link between medical technology and health expenditures is only one part of the picture. In order to understand better the dynamics between innovation and spending, it is important to assess whether and under what circumstances do investments in medical technology result in better value in health care. As Cutler and McClellan 25 assert, “it does not necessarily follow that technology change is therefore bad … costs of technology need to be compared with benefits before welfare statements can be made”. Given the current global economic situation, it is ever more important to ensure that we are attaining good value for money from the technologies developed.
To be sure, the question of whether medical technologies result in added value to the health care system is, of course, also difficult to answer. It depends on our ability to determine the value of output from the health services sector, and placing a value on longer or better quality of life is difficult to appraise. As a starting point, much more comparative research is needed to understand better which technologies work best and are most cost-effective, and under what circumstances. Indeed, as previously discussed, some of the cost-increasing effects of technology arise from inappropriate use, where new treatments are offered to patients for whom there is none to little clinical benefit. Current efforts to support comparative effectiveness research in the US and health technology assessment in Europe and elsewhere may help to foster these aims. However, it is important to note that medical technologies introduce unique technical challenges to health technology assessment or comparative effectiveness research, so assessment methods should adequately account for or be developed to accommodate such aspects. 55 Moreover, in addressing questions of value, such research should strive, where possible, to assess a broad range of potential benefits beyond clinical or therapeutic benefit, including value for money, higher quality of care, improved quality of life, greater efficiency in care delivery (eg, reduced length of stay, shifting care from inpatient to outpatient settings), and enhanced ability to work or return to work.
If the evidence generated from such research is to have an impact on health care spending, it should be used to inform policy and practice. As such, comparative effectiveness research and health technology assessment should be used to help reward and support the introduction of technologies into practice that confer therapeutic benefit and reasonable value for money, either through use in coverage and payment policies, insurance benefit design, or practice guidelines. Conversely, use of low-value interventions should be disincentivized through disinvestment or limitation on their use. Such strategies should be coupled with a greater emphasis on evidence-based delivery of care (eg, aligning appropriate financial incentives for providers and consumers), which might further reduce expenditure levels if such incentives support greater use of cost-effective services. 6 However, in parallel, it will be important to monitor carefully the impact of such policy levers in order to ascertain the best way to control costs without denying the benefits of new innovation. In addition, such measures need to be coupled with other policies and practices to address some of the other drivers of health spending, including initiatives to support healthy aging and improve coordination of care for the chronically ill. Finally, given our ever-limited health care resources, it would be prudent to debate the opportunity costs of funding new (and increasingly expensive) technologies. Even in cases where medical technologies are cost-effective, available resources may be better allocated to other equally or more cost-effective investments outside of the health care sector, such as the environment or education.
Studies reviewed
- Aidelsburger P, Grabein K, Klauss V, Wasem J. Cost-effectiveness of cardiac resynchronization therapy in combination with an implantable cardioverter defibrillator (CRT-D) for the treatment of chronic heart failure from a German health care system perspective. Clin Res Cardiol. 2002; 97 :89–97. [ PubMed ] [ Google Scholar ]
- Baker L, Spetz J. Managed Care and Medical Technology Growth. 1999 National Bureau of Economic Research Working Paper Series, No 6894. Available from: http://www.nber.org/chapters/c9845.pdf . Accessed March 17, 2013. [ Google Scholar ]
- Baker LC. Managed care and technology adoption in health care: evidence from magnetic resonance imaging. J Health Econ. 2001; 20 :395–421. [ PubMed ] [ Google Scholar ]
- Baker L, Birnbaum H, Geppert J, Mishol D, Moyneur E. The relationship between technology availability and health care spending. Health Aff (Millwood) 2003;(Suppl Web Exclusives):W3-537–51. [ PubMed ] [ Google Scholar ]
- Bakhai A, Stone GW, Grines CL, et al. Cost-effectiveness of coronary stenting and abciximab for patients with acute myocardial infarction: results from the CADILLAC (Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications) Trial. Circulation. 2003; 108 :2857–2863. [ PubMed ] [ Google Scholar ]
- Banz K. Cardiac resynchronization therapy (CRT) in heart failure: a model to assess the economic value of this new medical technology. Value Health. 2005; 8 :128–139. [ PubMed ] [ Google Scholar ]
- Bagust A, Grayson AD, Palmer ND, Perry RA, Walley T. Cost-effectiveness of drug eluting coronary artery stenting in a UK setting: cost-utility study. Heart. 2006; 92 :68–74. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barros P, Martinez-Giralt X. Technological Adoption in Health Care. CEPR Discussion Papers 7558, CEPR. Discussion Papers; 2009. Available from: http://ideas.repec.org/p/unl/unlfep/wp545.html . Accessed March 17, 2013.
- Bentkover JD, Stewert EJ, Ignaszewski A, Lepage S, Liu P, Cooper J. New technologies and potential cost savings related to morbidity and mortality reduction in Class III/IV heart failure patients in Canada. Int J Cardiol. 2003; 88 :33–41. [ PubMed ] [ Google Scholar ]
- Bodenheimer T. High and rising health care costs. Part 2: technologic innovation. Ann Intern Med. 2005; 142 :932–937. [ PubMed ] [ Google Scholar ]
- Bozic KJ, Morshed S, Silverstein MD, Rubash HE, Kahn JG. Use of cost-effectiveness analysis to evaluate new technologies in orthopaedics: the case of alternative bearing surfaces in total hip arthroplasty. J Bone Joint Surg Am. 2006; 88 :706–714. [ PubMed ] [ Google Scholar ]
- Brunner-La Rocca HP, Kaiser C, Berheim A, et al. Cost-effectiveness of drug-eluting stents in patients at high or low risk of major cardiac events in the Basel Stent KostenEffektivitäts Trial (BASKET): an 18-month analysis. Lancet. 2007; 370 :155–159. [ PubMed ] [ Google Scholar ]
- Bryan S, Buxton M, Brenna E. Estimating the impact of a diffuse technology on the running costs of a hospital. Int J Technol Assess. 2000; 16 :787–798. [ PubMed ] [ Google Scholar ]
- Busse R. Expenditure on health care in the EU: making projections for the future based on the past. Eur J Health Econ. 2001; 2 :158–161. [ Google Scholar ]
- Calvert MJ, Freemantle N, Yao G, et al. Cost-effectiveness of cardiac resynchronization therapy: results from the CARE-HF trial. Eur Heart J. 2005; 26 :2681–2688. [ PubMed ] [ Google Scholar ]
- Caro J, Ward A, Moller J. Modelling the health benefits and economic implications of implanting dual-chamber vs single-chamber ventricular pacemakers in the UK. Europace. 2006; 8 :449–455. [ PubMed ] [ Google Scholar ]
- Chen L, Hay JW. Cost-effectiveness of primary implanted cardioverter defibrillator for sudden death prevention in congestive heart failure. Cardiovasc Drugs Ther. 2004; 18 :161–170. [ PubMed ] [ Google Scholar ]
- Chernew M, Hirth RA, Sonnad SS, Ermann R, Fenrick AM. Managed care, medical technology, and health care cost growth: A review of the evidence. Med Care Res Rev. 1998; 55 :259–288. [ PubMed ] [ Google Scholar ]
- Chernew M, Fenrick AM, Hirth RA. Managed care and medical technology: implications for cost growth. Health Aff (Millwood) 1997; 16 :196–206. [ PubMed ] [ Google Scholar ]
- Clemente J, Marcuello C, Montanes A, Pueyo F. On the international stability of health care expenditure functions: are government and private functions similar? J Health Econ. 2004; 23 :589–613. [ PubMed ] [ Google Scholar ]
- Cohen DJ, Murphy SA, Baim DS, et al. Cost-effectiveness of distal embolic protection for patients undergoing percutaneous intervention of saphenous vein bypass graft (results from the SAFER trial) J Am Coll Cardiol. 2004; 44 :1801–1808. [ PubMed ] [ Google Scholar ]
- Cowie MR, Marshall D, Drummond M. Lifetime cost-effectiveness of prophylactic implantation of a cardioverter defibrillator in patients with reduced left ventricular systolic function: results of Markov modelling in a European population. Europace. 2009; 11 :716–726. [ PubMed ] [ Google Scholar ]
- Cutler DM, Huckman RS. Technological development and medical productivity: the diffusion of angioplasty in New York state. J Health Econ. 2003; 22 :187–217. [ PubMed ] [ Google Scholar ]
- Cutler DM, McClellan M. Is technological change in medicine worth it? Health Aff (Millwood) 2001; 20 :11–29. [ PubMed ] [ Google Scholar ]
- Cutler DM, McClellan M. The Determinants of Technological Change in Heart Attack Treatment. NBER Working Paper No 5751; 1996. Available from: http://ideas.repec.org/p/nbr/nberwo/5751.html . Accessed March 17, 2013.
- Cutler DM. The lifetime costs and benefits of medical technology. J Health Econ. 2007; 26 :1081–1100. [ PubMed ] [ Google Scholar ]
- Cutler DM. Technology, Health Costs, and the NIH, Harvard University and the National Bureau of Economic Research. Paper prepared for the National Institutes of Health Economics Roundtable on Biomedical Research; September 1995. [ Google Scholar ]
- Di Matteo L. What drives provincial health expenditure? Canadian Tax Journal. 2004; 52 :1102. [ Google Scholar ]
- Di Matteo L. The macro determinants of health expenditure in the United States and Canada: assessing the impact of income, age distribution and time. Health Policy. 2005; 71 :23–42. [ PubMed ] [ Google Scholar ]
- Dybczak K, Przywara B. The Role of Technology on Health Care Expenditure on the EU European Economy – Economic Paper 400. Brussels, Belgium: Directorate General for Economic and Monetary Affairs, European Commission; 2010. Available from: http://ec.europa.eu/economy_finance/publications/economic_paper/2010/ecp400_en.htm . [ Google Scholar ]
- Ekman M, Sjogren I, James S. Cost-effectiveness of the Taxus paclitaxel-eluting stent in the Swedish healthcare system. Scand Cardiovasc J. 2006; 40 :17–24. [ PubMed ] [ Google Scholar ]
- Filion KB, Roy AM, Baboushkin ET, Rinfret S, Eisenberg MJ. Cost-effectiveness of drug-eluting stents including the economic impact of late stent thrombosis. Am J Cardiol. 2006; 103 :338–344. [ PubMed ] [ Google Scholar ]
- Fuchs VR. Health care for the elderly: how much? Who will pay for it? Health Aff (Millwood) 1999; 18 :11–21. [ PubMed ] [ Google Scholar ]
- Fuchs VR, Sox HR. Physicians’ views of the relative importance of thirty medical innovations. Health Aff (Millwood) 2001; 20 :30–42. [ PubMed ] [ Google Scholar ]
- Gandjour A, Weylan EJ. Cost-effectiveness of preventing fractures by hip protectors in elderly institutionalized patients in Germany. Value Health. 2008; 11 :1088–1095. [ PubMed ] [ Google Scholar ]
- Givon U, Ginsberg GM, Horoszowski H, Shemer J. Cost-utility analysis of total hip anthroplasties. Technology assessment of surgical procedures by mailed questionnaires. Int J Technol Assess. 1998; 14 :735–742. [ PubMed ] [ Google Scholar ]
- Goetghebeur MM, Forrest S, Hay JW. Understanding the underlying drivers of inpatient cost growth: a literature review. Am J Manag Care. 2003; 9 (Spec No 1):SP3–SP12. [ PubMed ] [ Google Scholar ]
- Goyen M, Debatin J. Healthcare costs for new technologies. Eur J Nucl Med Mol Imaging. 2009; 36 :139–143. [ PubMed ] [ Google Scholar ]
- Greenberg D, Rosenfield K, Garcia LA, et al. In-hospital costs of self-expanding Nitinol Stent Implantation vs. Balloon Angioplasty in the Femoropopliteal Artery (The VascuCoil Trial) J Vasc Interv Radiol. 2004; 15 :1065–1069. [ PubMed ] [ Google Scholar ]
- Grignon M. McMaster University; 2005. Aging, Health and Aggregate Medical Care Spending in France. Department of Economics Working Papers 2005–05. Available from: http://www.econbiz.de/en/search/detailed-view/doc/all/Aging,%20Health%20and%20Aggregate%20Medical%20Care%20Spending%20in%20France/10005635244/?no_cache=1 . Accessed March 17, 2013. [ Google Scholar ]
- Hall RE, Jones CI. The Value of Life and the Rise in Health Spending. 2004 National Bureau of Economic Research Working Paper Series, No 10737. Available from: http://qje.oxfordjournals.org/content/122/1/39.short . Accessed March 17, 2013. [ Google Scholar ]
- Hay JW. Hospital cost drivers: an evaluation of 1998–2001 state-level data. Am J Manag Care. 2003; 9 :SP13–SP24. [ PubMed ] [ Google Scholar ]
- Hillman BJ. Government health policy and the diffusion of new medical devices. Health Serv Res. 1986; 21 :681–711. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Holahan J, Dor A, Zuckerman S. Understanding the recent growth in Medicare physician expenditures. JAMA. 1990; 263 :1658–1661. [ PubMed ] [ Google Scholar ]
- Honkanen LA, Mushlin AI, Lachs M, Schackman BR. Can hip protector use cost effectively prevent fractures in community-dwelling geriatric populations? J Am Geriatr Soc. 2006; 54 :1658–1665. [ PubMed ] [ Google Scholar ]
- Huber M, Orosze E. Health expenditure trends in OECD countries, 1990–2001. Health Care Financ Rev. 2003; 25 :1–22. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jones CI. Why have Health Expenditures as a Share of GDP Risen So Much? National Bureau of Economic Research Working Paper Series, No 9325; 2002. Available from: http://www.stanford.edu/~chadj/health300.pdf . Accessed March 17, 2013. [ Google Scholar ]
- Kaiser C, Brunner-La Rocca HP, Buser PT, et al. Incremental cost-effectiveness of drug-eluting stents compared with a third-generation bare-metal stent in a real-world setting: randomised Basel Stent Kosten Effekivitats Trial (BASKET) Lancet. 2005; 366 :921–929. [ PubMed ] [ Google Scholar ]
- Koenig L, Siegel JM, Dobson A, Hearle K, Ho S, Rudowitz R. Drivers of healthcare expenditures associated with physician services. Am J Manag Care. 2003; 9 (Spec No 1):SP34–SP42. [ PubMed ] [ Google Scholar ]
- Kuukasjarvi P, Rasanen P, Malmivaara A, Aronen P, Sintonen H. Economic evaluation of drug-eluting stents: a systematic literature review and model-based cost-utility analysis. Int J Technol Assess. 2007; 23 :473–479. [ PubMed ] [ Google Scholar ]
- Lord SJ, Howard K, Allen F, et al. A systematic review and economic analysis of drug-eluting coronary stents available in Australia. Med J Aust. 2005; 183 :464–471. [ PubMed ] [ Google Scholar ]
- March LM, Barcinilla AL, Cross MJ, et al. Costs and outcomes of total hip and knee joint replacement for rheumatoid arthritis. Clin Rheumatol. 2008; 27 :1235–1242. [ PubMed ] [ Google Scholar ]
- Marinelli M, Soccetti A, Panfoli N, de Palma L. Cost-effectiveness of cemented versus cementless total hip anthroplasty. A Markov decision analysis based on implant cost. J Orthop Traumatol. 2008; 9 :23–28. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Martin S, Rice N, Smith PC. Does health care spending improve health outcomes? Evidence from English programme budgeting data. J Health Econ. 2008; 27 :826–842. [ PubMed ] [ Google Scholar ]
- Mas N, Seinfield J. Is managed care restraining the adoption of technology by hospitals? J Health Econ. 2008; 27 :1026–1045. [ PubMed ] [ Google Scholar ]
- Mattijs S, Lambooji PE, Westert GP. Diffusion of innovations in health care: does the structural context determine its direction? Int J Technol Assess. 2010; 26 :415–420. [ PubMed ] [ Google Scholar ]
- McClellan M, Newhouse JP. The marginal cost-effectiveness of medical technology: a panel instrumental-variables approach. J Econom. 1997; 77 :39–64. [ Google Scholar ]
- McKenzie L, Vale L, Stearns S. Metal on metal hip resurfacing arthroplasty. An economic analysis. Eur J Health Econ. 2003; 4 :122–129. [ PubMed ] [ Google Scholar ]
- Mitton CR, Rose MS, Kohman ML, Sheldon RS. Cost-utility analysis of pacemakers for the treatment of vasovagal syncope. Am J Cardiol. 1999; 84 :1356–1359. [ PubMed ] [ Google Scholar ]
- Nichol G, Kaul P, Huszti E, et al. Cost-effectiveness of cardiac resynchronization therapy in patients with symptomatic heart failure. Ann Intern Med. 2004; 141 :343–351. [ PubMed ] [ Google Scholar ]
- Newhouse J. Medical care costs: how much welfare loss? J Econ Perspect. 1992; 6 :3–21. [ PubMed ] [ Google Scholar ]
- Neyt M, Thiry N, Rameekers D, Van Brabandt H. Cost-effectiveness of implantable cardioverter defibrillators for primary prevention in a Belgian context. Appl Health Econ Health Policy. 2008; 6 :67–80. [ PubMed ] [ Google Scholar ]
- Okunade AA, Murthy VNR. Technology as a major driver of health care costs: a cointegration analysis of the Newhouse conjecture. J Health Econ. 2002; 21 :147–159. [ PubMed ] [ Google Scholar ]
- Oliveira Martins J, De La Maisonneuve C. The Drivers of Public Expenditure on Health and Long-Term Care: An Integrated Approach. 2006 Available from: http://ssrn.com/abstract=917782 . Accessed March 17, 2013. [ Google Scholar ]
- Owens DK, Sanders GD, Harris RA, et al. Cost-effectiveness of implantable cardioverter defibrillators relative to amiodarone for prevention of sudden cardiac death. Ann Intern Med. 1997; 126 :1–12. [ PubMed ] [ Google Scholar ]
- Packer C, Simpson S, Stevens A. International diffusion of new health technologies: a ten-country analysis of six health technologies. Int J Technol Assess. 2006; 22 :419–428. [ PubMed ] [ Google Scholar ]
- Pammolli F, Riccaboni M, Oglialoro C, et al. Medical Devices Competitiveness and Impact on Public Health Expenditure. Bruxelles, Belgium: Enterprise Directorate-General, European Commission; 2005. Available from: http://ideas.repec.org/p/pra/mprapa/16021.html . [ Google Scholar ]
- Peden EA, Freeland MS. A historical analysis of medical spending growth, 1960–1993. Health Aff (Millwood) 1995; 14 :235–247. [ PubMed ] [ Google Scholar ]
- Peden EA, Freeland MS. Insurance effects on US medical spending (1960–1993) Health Econ. 1998; 7 :671–687. [ PubMed ] [ Google Scholar ]
- PricewaterhouseCoopers The Factors Fueling Risking Healthcare Costs. 2002 Report prepared for the American Association of Health Plans. Available from: http://heartland.org/sites/all/modules/custom/heartland_migration/files/pdfs/14621.pdf . Accessed March 15, 2013. [ Google Scholar ]
- Rettig RA. Medical innovation duels cost containment. Health Aff (Millwood) 1994; 13 :7–27. [ PubMed ] [ Google Scholar ]
- Sanders GD, Hlatky MA, Owens DK. Cost-effectiveness of implantable cardioverter defibrillators. N Engl J Med. 2005; 353 :1471–1480. [ PubMed ] [ Google Scholar ]
- Sanders GD, Hlatky MA, Every NR, et al. Potential cost-effectiveness of prophylactic use of the implantable cardiovascular defibrillator or amiodarone after myocardial infarction. Ann Intern Med. 2001; 135 :870–883. [ PubMed ] [ Google Scholar ]
- Sanders GD, Hlatky MA, Owens DK. Special report: cost-effectiveness of implantable cardioverter defibrillators in a MADIT-II population. Technology Evaluation Center Assessment Program Report. 2004; 19 (3) [ PubMed ] [ Google Scholar ]
- Sharples LD, Dryer M, Cafferty F, et al. Cost-effectiveness of ventricular assist device use in the United Kingdom: Results from the evaluation of Ventricular Assist Device Programme in the UK (EVAD-UK) J Heart Lung Transplant. 2006; 25 :1336–1343. [ PubMed ] [ Google Scholar ]
- Schreyogg J, Baumler M, Busse R. Balancing adoption and affordability of medical devices in Europe. Health Policy. 2009; 92 :218–224. [ PubMed ] [ Google Scholar ]
- Segui-Gomez M, Keuffel E, Frick KD. Cost and effectiveness of hip protectors among the elderly. Int J Technol Assess. 2002; 18 :55–66. [ PubMed ] [ Google Scholar ]
- Shrive FM, Manns BJ, Galbraith PD, et al. Economic evaluation of sirolimus-eluting stents. Can Med Assoc J. 2005; 172 :345–351. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Singh S, Sun H, Anis AH. Cost-effectiveness of hip protectors in the prevention of osteoporosis related hip fractures in elderly nursing home residents. J Rheumatol. 2004; 31 :1607–1613. [ PubMed ] [ Google Scholar ]
- Skinner J, Staiger D. Technology Diffusion and Productivity Growth in Health Care. National Bureau of Economic Research Working Paper Series, No 14865; 2009. Available from: http://www.dartmouth.edu/~jskinner/documents/SkinnerStaigerw14865_000.pdf . Accessed March 17, 2013. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smith SD, Heffler SK, Freeland MS. The Impact of Technological Change on Health Care Cost Increases: An Evaluation of the Literature. Health Care Financing Administration Working Paper; 2000. Available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/tech_2000_0810.pdf . [ Google Scholar ]
- Von Hout BA, Serruys PW, Lemos PA, et al. One-year cost-effectiveness of sirolimus eluting stents compared with bare metal stents in the treatment of single native de novo coronary lesions: an analysis from the Ravel trial. Heart. 2005; 91 :507–512. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Weisbrod BA. The health care quadrilemma: an essay on technological change, insurance, quality of care and cost containment. J Econ Lit. 1991; 29 :523–532. [ Google Scholar ]
- Yao G, Freemantle N, Calvert MJ, et al. The long-term cost-effectiveness of cardiac resynchronization therapy with or without an implantable cardioverter defibrillator. Eur Heart J. 2007; 28 :42–51. [ PubMed ] [ Google Scholar ]
- Yock CA, Boothroyd DB, Owens DK, Garber AM, Hlatky MA. Cost-effectiveness of bypass surgery vs stenting in patients with multivessel coronary artery disease. Am J Med. 2003; 115 :382–389. [ PubMed ] [ Google Scholar ]
- You JJ, Woo A, Dennis TK, et al. Life expectancy gains and cost-effectiveness of implantable cardioverter defibrillators for the primary prevention of sudden cardiac death in patients with hypertrophic cardiomyopathy. Am Heart J. 2007; 145 :899–907. [ PubMed ] [ Google Scholar ]
The authors report no conflicts of interest in this work.
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
Study models how ketamine’s molecular action leads to its effects on the brain
Press contact :.

Previous image Next image
Ketamine, a World Health Organization Essential Medicine, is widely used at varying doses for sedation, pain control, general anesthesia, and as a therapy for treatment-resistant depression. While scientists know its target in brain cells and have observed how it affects brain-wide activity, they haven’t known entirely how the two are connected. A new study by a research team spanning four Boston-area institutions uses computational modeling of previously unappreciated physiological details to fill that gap and offer new insights into how ketamine works.
“This modeling work has helped decipher likely mechanisms through which ketamine produces altered arousal states as well as its therapeutic benefits for treating depression,” says co-senior author Emery N. Brown , the Edward Hood Taplin Professor of Computational Neuroscience and Medical Engineering at The Picower Institute for Learning and Memory at MIT, as well as an anesthesiologist at Massachusetts General Hospital and a professor at Harvard Medical School.
The researchers from MIT, Boston University (BU), MGH, and Harvard University say the predictions of their model, published May 20 in Proceedings of the National Academy of Sciences , could help physicians make better use of the drug.
“When physicians understand what's mechanistically happening when they administer a drug, they can possibly leverage that mechanism and manipulate it,” says study lead author Elie Adam , a research scientist at MIT who will soon join the Harvard Medical School faculty and launch a lab at MGH. “They gain a sense of how to enhance the good effects of the drug and how to mitigate the bad ones.”
Blocking the door
The core advance of the study involved biophysically modeling what happens when ketamine blocks the “NMDA” receptors in the brain’s cortex — the outer layer where key functions such as sensory processing and cognition take place. Blocking the NMDA receptors modulates the release of excitatory neurotransmitter glutamate.
When the neuronal channels (or doorways) regulated by the NMDA receptors open, they typically close slowly (like a doorway with a hydraulic closer that keeps it from slamming), allowing ions to go in and out of neurons, thereby regulating their electrical properties, Adam says. But, the channels of the receptor can be blocked by a molecule. Blocking by magnesium helps to naturally regulate ion flow. Ketamine, however, is an especially effective blocker.
Blocking slows the voltage build-up across the neuron’s membrane that eventually leads a neuron to “spike,” or send an electrochemical message to other neurons. The NMDA doorway becomes unblocked when the voltage gets high. This interdependence between voltage, spiking, and blocking can equip NMDA receptors with faster activity than its slow closing speed might suggest. The team’s model goes further than ones before by representing how ketamine’s blocking and unblocking affect neural activity.
“Physiological details that are usually ignored can sometimes be central to understanding cognitive phenomena,” says co-corresponding author Nancy Kopell , a professor of mathematics at BU. “The dynamics of NMDA receptors have more impact on network dynamics than has previously been appreciated.”
With their model, the scientists simulated how different doses of ketamine affecting NMDA receptors would alter the activity of a model brain network. The simulated network included key neuron types found in the cortex: one excitatory type and two inhibitory types. It distinguishes between “tonic” interneurons that tamp down network activity and “phasic” interneurons that react more to excitatory neurons.
The team’s simulations successfully recapitulated the real brain waves that have been measured via EEG electrodes on the scalp of a human volunteer who received various ketamine doses and the neural spiking that has been measured in similarly treated animals that had implanted electrode arrays. At low doses, ketamine increased brain wave power in the fast gamma frequency range (30-40 Hz). At the higher doses that cause unconsciousness, those gamma waves became periodically interrupted by “down” states where only very slow frequency delta waves occur. This repeated disruption of the higher frequency waves is what can disrupt communication across the cortex enough to disrupt consciousness.
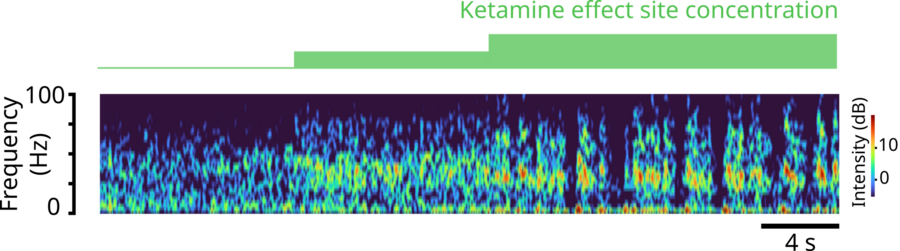
Previous item Next item
But how? Key findings
Importantly, through simulations, they explained several key mechanisms in the network that would produce exactly these dynamics.
The first prediction is that ketamine can disinhibit network activity by shutting down certain inhibitory interneurons. The modeling shows that natural blocking and unblocking kinetics of NMDA-receptors can let in a small current when neurons are not spiking. Many neurons in the network that are at the right level of excitation would rely on this current to spontaneously spike. But when ketamine impairs the kinetics of the NMDA receptors, it quenches that current, leaving these neurons suppressed. In the model, while ketamine equally impairs all neurons, it is the tonic inhibitory neurons that get shut down because they happen to be at that level of excitation. This releases other neurons, excitatory or inhibitory, from their inhibition allowing them to spike vigorously and leading to ketamine’s excited brain state. The network’s increased excitation can then enable quick unblocking (and reblocking) of the neurons’ NMDA receptors, causing bursts of spiking.
Another prediction is that these bursts become synchronized into the gamma frequency waves seen with ketamine. How? The team found that the phasic inhibitory interneurons become stimulated by lots of input of the neurotransmitter glutamate from the excitatory neurons and vigorously spike, or fire. When they do, they send an inhibitory signal of the neurotransmitter GABA to the excitatory neurons that squelches the excitatory firing, almost like a kindergarten teacher calming down a whole classroom of excited children. That stop signal, which reaches all the excitatory neurons simultaneously, only lasts so long, ends up synchronizing their activity, producing a coordinated gamma brain wave.
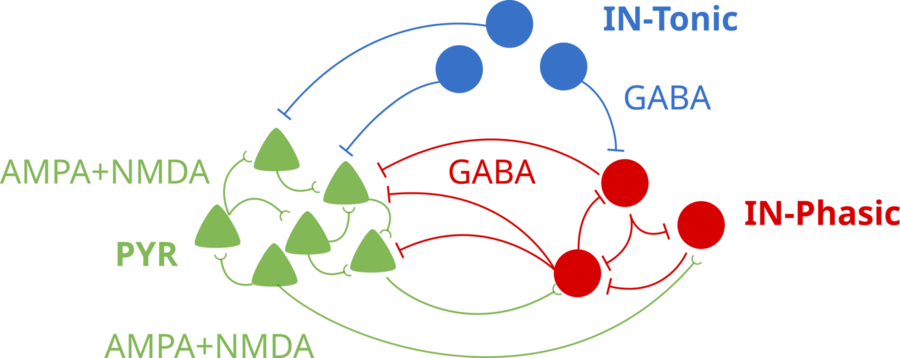
“The finding that an individual synaptic receptor (NMDA) can produce gamma oscillations and that these gamma oscillations can influence network-level gamma was unexpected,” says co-corresponding author Michelle McCarthy , a research assistant professor of math at BU. “This was found only by using a detailed physiological model of the NMDA receptor. This level of physiological detail revealed a gamma time scale not usually associated with an NMDA receptor.”
So what about the periodic down states that emerge at higher, unconsciousness-inducing ketamine doses? In the simulation, the gamma-frequency activity of the excitatory neurons can’t be sustained for too long by the impaired NMDA-receptor kinetics. The excitatory neurons essentially become exhausted under GABA inhibition from the phasic interneurons. That produces the down state. But then, after they have stopped sending glutamate to the phasic interneurons, those cells stop producing their inhibitory GABA signals. That enables the excitatory neurons to recover, starting a cycle anew.
Antidepressant connection?
The model makes another prediction that might help explain how ketamine exerts its antidepressant effects. It suggests that the increased gamma activity of ketamine could entrain gamma activity among neurons expressing a peptide called VIP. This peptide has been found to have health-promoting effects, such as reducing inflammation, that last much longer than ketamine’s effects on NMDA receptors. The research team proposes that the entrainment of these neurons under ketamine could increase the release of the beneficial peptide, as observed when these cells are stimulated in experiments. This also hints at therapeutic features of ketamine that may go beyond antidepressant effects. The research team acknowledges, however, that this connection is speculative and awaits specific experimental validation.
“The understanding that the subcellular details of the NMDA receptor can lead to increased gamma oscillations was the basis for a new theory about how ketamine may work for treating depression,” Kopell says.
Additional co-authors of the study are Marek Kowalski, Oluwaseun Akeju, and Earl K. Miller.
The work was supported by the JPB Foundation; The Picower Institute for Learning and Memory; The Simons Center for The Social Brain; the National Institutes of Health; George J. Elbaum ’59, SM ’63, PhD ’67; Mimi Jensen; Diane B. Greene SM ’78; Mendel Rosenblum; Bill Swanson; and annual donors to the Anesthesia Initiative Fund.
Share this news article on:
Related links.
- Institute for Medical Engineering and Science
- The Picower Institute for Learning and Memory
- Department of Brain and Cognitive Sciences
Related Topics
- Pharmaceuticals
- Neuroscience
- Brain and cognitive sciences
- Health sciences and technology
- Health care
- Picower Institute
- Institute for Medical Engineering and Science (IMES)
Related Articles

Anesthesia technology precisely controls unconsciousness in animal tests

Study finds tracking brain waves could reduce post-op complications
3 Questions: Emery Brown on improving anesthesia with neuroscience

Statistical model defines ketamine anesthesia’s effects on the brain
More mit news.
Students research pathways for MIT to reach decarbonization goals
Read full story →

Improving working environments amid environmental distress

A data-driven approach to making better choices

Paying it forward
John Fucillo: Laying foundations for MIT’s Department of Biology

Researchers demonstrate the first chip-based 3D printer
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Medical research articles from across Nature Portfolio
Medical research involves research in a wide range of fields, such as biology, chemistry, pharmacology and toxicology with the goal of developing new medicines or medical procedures or improving the application of those already available. It can be viewed as encompassing preclinical research (for example, in cellular systems and animal models) and clinical research (for example, clinical trials).
Shaping new paths in clinical trial design to address alcohol use disorders and alcohol-associated liver disease
An expert panel has proposed 28 recommendations for the design and conduct of clinical trials for alcohol use disorders and alcohol-associated liver disease. This field has a scarcity of clinical trials, despite alcohol abuse and alcohol-related liver disease being one of the greatest causes of morbidity and mortality worldwide.
- Juliana Serrazina
- Helena Cortez-Pinto
Gene therapy for hereditary deafness
Bilateral administration of human OTOF gene therapy appears safe, and preliminary data suggest that it could effectively treat a rare form of hereditary hearing loss by enhancing speech perception, sound source localization and overall auditory experience.
- Carson Smith
- Mohammad Faraz Zafeer
- Mustafa Tekin

Brain fluid probed by ultrasound using squishy cubes
Soft solids that swell with shifts in pressure, temperature and pH provide a way of detecting such changes in the fluid around the brain. The method could be used to determine other properties of fluids elsewhere in the body.
- Jules J. Magda
Related Subjects
- Drug development
- Epidemiology
- Experimental models of disease
- Genetics research
- Outcomes research
- Paediatric research
- Preclinical research
- Stem-cell research
- Clinical trial design
- Translational research
Latest Research and Reviews
Three-dimensional finite element analysis of the optimal mechanical design for maximum inward movement of the anterior teeth with clear aligners
- Jingcheng Chen
Effect of the COVID-19 pandemic on Vogt–Koyanagi–Harada disease
- Tetsuya Muto
- Masaaki Sakamoto
- Tetsuju Sekiryu

Penile prosthesis implantation: a bibliometric-based visualization study
- Degui Chang
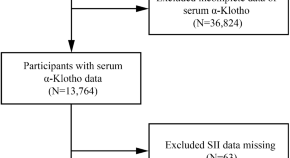
L-shaped association of systemic immune-inflammation index (SII) with serum soluble α-Klotho in the prospective cohort study from the NHANES database
- Tingting Zhang

Association between the cardiometabolic index and NAFLD and fibrosis
- Shunying Zhao
Assessing the oral and suprahyoid muscles in healthy adults using muscle ultrasound to inform the swallowing process: a proof-of-concept study
- Eileen Kelly
- Saira Nazeer
- Zudin Puthucheary
News and Comment
Trimming down with semaglutide improves cardiac health in non-diabetic patients.
- Andrea Tavosanis
This injectable gel can help to diagnose brain injury — then it disappears
The squishy sensors could be used to monitor the brain for tumours or injury, before eventually degrading.
- Gemma Conroy

MDMA therapy for PTSD rejected by FDA panel
Scientific advisers to the US Food and Drug Administration vote overwhelmingly that the risks of MDMA treatment for post-traumatic stress disorder outweigh the benefits.
- Sara Reardon
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
More From Forbes
Leveraging technology for patient safety: the role of knowledge management in healthcare.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
CEO of KMS Lighthouse . Leading the company's vision to disrupt the knowledge management market.
In the rapidly evolving landscape of healthcare technology, ensuring patient safety remains a paramount concern. By harnessing innovative technologies such as AI, data analytics and digital health platforms, healthcare providers can implement robust knowledge management (KM) systems to capture, disseminate and apply critical insights. I'll explore how technology-enabled initiatives empower healthcare teams to identify adverse events, implement evidence-based practices and foster a culture of continuous learning.
At a time when healthcare providers must thoroughly serve their patients' needs while protecting their personal information, technologies like electronic health records (EHRs), clinical decision support systems (CDSS) and telemedicine are enhancing patient safety practices.
Knowledge management is critical in making these technologies effective by streamlining access to up-to-date medical knowledge, evidence-based guidelines and patient data, enabling healthcare professionals to make informed decisions, reduce errors and improve outcomes.
Hospitals, clinics and doctors' offices owe it to their patients and themselves to leverage every available tool to uphold the highest standards of care. I'll explore the dynamic relationship between KM and healthcare technologies, delving into the transformative impact their integration is having on creating cultures of continuous learning and quality improvement while safeguarding patient well-being in the digital age.
Best High-Yield Savings Accounts Of 2024
Best 5% interest savings accounts of 2024.
Knowledge management’s role in healthcare technology improves the creation, sharing and application of knowledge to support patient safety and improve healthcare outcomes. Over the years, it has evolved to include the following.
Electronic Health Records
Before: Patient records were primarily paper-based, making it challenging to share information across different healthcare providers and settings and increasing the risk of medical errors due to incomplete or unavailable patient information.
Today: EHRs have digitized patient records, allowing healthcare professionals to access comprehensive patient information, including medical histories, test results and prescribed medications, from any authorized location. Communication, coordination and decision-making are improved , and the likelihood of medical errors is reduced.
Clinical Decision Support Systems
Before: Healthcare professionals relied heavily on individual knowledge and experience, which could result in clinical practice variations and potential oversights.
Today: CDSS integrates evidence-based guidelines, best practices and patient-specific data to provide real-time alerts, reminders and recommendations to healthcare professionals, ensuring they adhere to standardized protocols while reducing the risk of medication errors, adverse drug interactions and other preventable mistakes.
Knowledge Repositories And Expert Systems
Before: Medical knowledge was primarily stored in textbooks, journals and the collective experience of healthcare professionals, making it more challenging to consistently access and apply the latest research and best practices.
Today: Healthcare organizations use knowledge repositories and expert systems to consolidate and disseminate up-to-date medical knowledge, clinical guidelines and best practices. This means that healthcare professionals have easier access to the latest evidence-based information to enhance treatment effectiveness.
Telemedicine And Remote Monitoring
Before: Patients in remote or underserved areas had limited access to specialized healthcare services, increasing the risk of delayed diagnoses and suboptimal treatment.
Today: Telemedicine and remote monitoring technologies enable healthcare professionals to monitor and provide care to patients remotely, leveraging the knowledge and expertise of specialists across geographical borders. Access to high-quality care is improved , bridging the gap between remote and centralized healthcare and reducing the risk of complications due to delayed interventions.
Continuing Medical Education (CME) And E-Learning
Before: Healthcare professionals relied heavily on in-person training and seminars to stay current with the latest medical knowledge and best practices—an often time-consuming and logistically challenging endeavor.
Today: Online CME platforms and e-learning resources provide convenient access to educational materials, allowing providers to continuously enhance their knowledge and skills. This, in turn, helps ensure they’re equipped with the latest knowledge when making decisions on a patient’s healthcare options.
By using an integrated knowledge approach, healthcare providers can create, share and apply institutional knowledge to promote evidence-based practices, standardize care protocols and empower medical professionals with the information they need to optimize patient care outcomes.
Three Ways Technology Is Improving Patient Safety
Many researchers claim that medical error is the third-leading cause of death in the U.S., often due to poor communication, a lack of access to comprehensive patient data and best practice deviations. Healthcare providers can improve patient care by investing in innovative technologies and implementing a robust knowledge management system.
1. Artificial Intelligence: AI’s predictive capabilities enable providers to offer proactive, preventative care that improves outcomes and reduces costs. In hospitals, AI-powered clinical decision support systems integrate evidence-based guidelines, best practices and patient-specific data to provide healthcare professionals with real-time reminders and recommendations.
For instance, AI systems can analyze a patient's medical history, current medications and lab results and then alert physicians to potential adverse drug interactions or contraindications , reducing the risk of medication errors.
2. Data Analytics: Advanced healthcare analytics can potentially revolutionize the medical sector . Clinics can use data analytics tools to identify patterns and trends in patient data, enabling them to make data-driven decisions and improve care processes. For example, by analyzing patient outcomes data, a clinic can identify risk factors for certain conditions and tailor preventive care strategies accordingly.
3. Digital Healthcare Platforms: These online services moved to the forefront during the pandemic. Today, doctors' offices can use telemedicine and remote monitoring technologies to leverage knowledge management systems and provide patients with access to specialized care and expertise, regardless of geographic location.
For instance, a rural-based primary care physician might consult with a major medical center specialist, sharing patient data and medical records through a secure digital platform, ensuring timely and accurate diagnosis and treatment for a patient.
Every patient deserves a healthcare provider they can trust to keep them safe. When finding the right information at the right time can literally save lives, it’s crucial for the healthcare sector to implement solutions that facilitate timely access to accurate medical knowledge, evidence-based guidelines and patient data.
Knowledge is capital for the healthcare industry, and information technology can have a significant impact on patient safety. Healthcare-focused knowledge management systems align people, data and technologies to provide patients with secure environments where informed decisions can be made to prevent errors and improve the quality of care—a win-win for patients and providers.
Forbes Technology Council is an invitation-only community for world-class CIOs, CTOs and technology executives. Do I qualify?
- Editorial Standards
- Reprints & Permissions

IMAGES
VIDEO
COMMENTS
Then, the articles were categorised according to their content. The concepts discussed in the papers are related to information technology in health, the educational impact of e-health, the acceptance of e-health, telemedicine, and e-health security. For this purpose, the following table was created, called the concept matrix table.
The number of medical technologies used in home settings has increased substantially over the last 10-15 years. In order to manage their use and to guarantee quality and safety, data on usage trends and practical experiences are important. This paper presents a literature review on types, trends and experiences with the use of advanced medical technologies at home.
The World Health Organization (WHO) defines health technology as the application of organised knowledge and skills in the form of medicines, medical devices, vaccines, procedures and systems developed to solve a health problem and improve quality of life (World Health Organization, Health technology assessment).The Organisation for Economic Co-operation and Development (OECD) defines health ...
Medical Technology encompasses a wide range of healthcare products and is used to diagnose, monitor or treat diseases or medical conditions... | Explore the latest full-text research PDFs ...
Abstract. Technology has revolutionized the healthcare industry, impacting various aspects of patient care, clinical practice, and healthcare systems. This paper provides a comprehensive review of ...
Recent research has exploited the availability of large medical text datasets for healthcare-related natural language processing tasks, taking advantage of technical advances like transformers and ...
The research stream of AI in healthcare is divided into two main strands. The blue strand focuses on medical information systems and the internet. Some papers are related to healthcare organisations, such as the Internet of Things, meaning that healthcare organisations use AI to support health services management and data analysis.
Table 1 shows the important challenges and issues for medical AI introduction and the application of medical AI, which can cause mistrust in AI technologies. Solutions to these issues are mostly related to working with users by promoting a better understanding of AI operations, making AI work more transparent, destroying negative myths, and improving the image of AI via education.
Artificial intelligence-powered medical technologies are rapidly evolving into applicable solutions for clinical practice. Deep learning algorithms can deal with increasing amounts of data provided by wearables, smartphones, and other mobile monitoring sensors in different areas of medicine. Currently, only very specific settings in clinical practice benefit from the application of artificial ...
The Internet of Medical Things (IoMT) is the blend of medical devices with the Internet of Things (IoT). IoMTs are the future of current healthcare systems where every medical device will be connected and monitored over the Internet via healthcare professionals. This offers a faster and lower cost of health care as it evolves.
Nanomaterials and Small Molecule-Enabled Precision Therapeutics, Biosensor and Diagnostics. Bijayananda Panigrahi. Dindyal Mandal. Dr. Nidhi Verma. ROHIT KUMAR SINGH. 684 views. An innovative journal that explores technologies which can maintain healthy lives and contribute to the global bioeconomy by addressing key medical and healthcare needs.
In this paper, we survey the opportunities, risks and progress made in the use of electronic medical record (real-world) data for psychiatric research. Similar content being viewed by others
The integration of artificial intelligence (AI) into medical imaging has guided in an era of transformation in healthcare. This literature review explores the latest innovations and applications of AI in the field, highlighting its profound impact on medical diagnosis and patient care. The innovation segment explores cutting-edge developments in AI, such as deep learning algorithms ...
Biotechnology articles from across Nature Portfolio. Atom. RSS Feed. Biotechnology is a broad discipline in which biological processes, organisms, cells or cellular components are exploited to ...
SUBMIT PAPER. Hong Kong Journal of Emergency Medicine. Impact Factor: 0.6 / 5-Year Impact Factor: 0.6 . ... and quality of research methods. Three dimensions of clinical efficacy assessment applied to magnetic resonance imaging. Invest Radiol 1992; 27(3): 245-54 ... A Glimpse of Medical Technology: [First Place Winner — WFS High School ...
Healthcare is an enormous industry based on legacy systems, which can lead to inefficiencies. While governments and medical companies have long been the main investors, major tech companies including Google, Microsoft have started investing more into digital health. Moreover, with the global pandemic of COVID-19 around the world, discussions about digital healthcare are once again emerging ...
The new gene editing technology, CRISPR, is really going to transform research. It's important to point out that the major advances in health care have been based on basic scientific findings. DNA technology and the structure of DNA were basic science findings that now drive clinical genetics.
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on MEDICAL LABORATORY TECHNOLOGY. Find methods information, sources, references or conduct a literature ...
1. Establish the sociodemographic profile of respondents enrolled in the B.S. Medical Technology program. 2. Determine the level of motivation of Medical Technology students in a designated university in Manila towards pursuing a path in the healthcare sector. 3. Evaluate the level of knowledge of Medical Technology students in a designated
Technology has the potential to improve the quality of health care. And technology can make it easier for more people to get health care. ... Journal of Medical Internet Research. 2020; doi:10.2196/24087. Brotman JJ, et al. Providing outpatient telehealth services in the United States: Before and during coronavirus disease 2019. Chest Reviews ...
MIT graduate student Jason Hou and MIT postdoc Md Osman Goni Nayeem are the lead authors of the paper, along with collaborators from MIT's McGovern Institute for Brain Research, Boston University, and Caltech. The study appears today in Nature Communications. Deep in the brain
Browse Calls for Papers beta. Browse 5,060 journals and 35,600 books. A; A Review on Diverse Neurological Disorders. ... The Nuclear Research Foundation School Certificate Integrated, Volume 1. Book ... Academic Libraries and Public Engagement with Science and Technology. Book • 2019. Academic Libraries and Toxic Leadership. Book
However, analysts often point to advances in medical technology and their diffusion across health systems as the principal driver for burgeoning expenditures. 3 - 10 This paper critically examines this conjecture, based on an analysis of a broad range of existing evidence on the relationship between medical technology diffusion and health ...
"The finding that an individual synaptic receptor (NMDA) can produce gamma oscillations and that these gamma oscillations can influence network-level gamma was unexpected," says co-corresponding author Michelle McCarthy, a research assistant professor of math at BU."This was found only by using a detailed physiological model of the NMDA receptor.
High-Impact, Evidence-Based Education for Health Care ProfessionalsTo successfully train the next generation of health care professionals, medical educators must utilize innovative teaching strategies and techniques in both classroom and clinical settings. Training to Teach in Medicine is a six-month online certificate program taught by distinguished Harvard Medical School faculty for ...
Medical research involves research in a wide range of fields, such as biology, chemistry, pharmacology and toxicology with the goal of developing new medicines or medical procedures or improving ...
Before: Patient records were primarily paper-based, making it challenging to share information across different healthcare providers and settings and increasing the risk of medical errors due to ...
Official Publication of the Brazilian Metallurgical, Materials and Mining Association. The Journal of Materials Research and Technology provides an international medium for the publication of theoretical and experimental studies related to processing, properties, and performance of materials.The complex relationship between processing and properties of materials is being revealed by advanced ...