- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
- Open Access Articles
- Research Collections
- Review Collections
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About Health Policy and Planning
- About the London School of Hygiene and Tropical Medicine
- HPP at a glance
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
Introduction, scoping review methodology, an iterative approach, acknowledgements.
- < Previous
Using WhatsApp messenger for health systems research: a scoping review of available literature
- Article contents
- Figures & tables
- Supplementary Data
Karima Manji, Johanna Hanefeld, Jo Vearey, Helen Walls, Thea de Gruchy, Using WhatsApp messenger for health systems research: a scoping review of available literature, Health Policy and Planning , Volume 36, Issue 5, June 2021, Pages 774–789, https://doi.org/10.1093/heapol/czab024
- Permissions Icon Permissions
Globally, the use of mobile phones for improving access to healthcare and conducting health research has gained traction in recent years as rates of ownership increase, particularly in low- and middle-income countries (LMICs). Mobile instant messaging applications, including WhatsApp Messenger, provide new and affordable opportunities for health research across time and place, potentially addressing the challenges of maintaining contact and participation involved in research with migrant and mobile populations, for example. However, little is known about the opportunities and challenges associated with the use of WhatsApp as a tool for health research. To inform our study, we conducted a scoping review of published health research that uses WhatsApp as a data collection tool. A key reason for focusing on WhatsApp is the ability to retain contact with participants when they cross international borders. Five key public health databases were searched for articles containing the words ‘WhatsApp’ and ‘health research’ in their titles and abstracts. We identified 69 articles, 16 of which met our inclusion criteria for review. We extracted data pertaining to the characteristics of the research. Across the 16 studies—11 of which were based in LMICs—WhatsApp was primarily used in one of two ways. In the eight quantitative studies identified, seven used WhatsApp to send hyperlinks to online surveys. With one exception, the eight studies that employed a qualitative ( n  = 6) or mixed-method ( n  = 2) design analysed the WhatsApp content generated through a WhatsApp-based programmatic intervention. We found a lack of attention paid to research ethics across the studies, which is concerning given the controversies WhatsApp has faced with regard to data protection in relation to end-to-end encryption. We provide recommendations to address these issues for researchers considering using WhatsApp as a data collection tool over time and place.
WhatsApp Messenger provides new and affordable opportunities for health research across time and place, potentially addressing the challenges of maintaining contact and participation involved in research with migrant and mobile populations, for example.
However, little is known about the opportunities and challenges associated with the use of WhatsApp as a tool for health research.
Reviewing the literature reveals that most of the studies using WhatsApp as a data collection tool for health research have been undertaken in low-and-middle-income countries and that WhatsApp was primarily used either to send hyperlinks to online surveys or to analyse the WhatsApp content generated through a WhatsApp-based intervention.
These studies pay little to no attention to research ethics, which is concerning given the controversies WhatsApp has faced with regard to data protection in relation to end-to-end encryption.
We provide recommendations to address these issues for researchers considering using WhatsApp as a data collection tool over time and place.
A growing body of literature addresses the role that increased ownership and use of mobile phones can play in improving both access to healthcare and health systems research in low-and middle-income countries (LMICs), specifically in sub-Saharan Africa ( Bloomfield et al. , 2014 ; Hampshire et al. , 2015 ; Lee et al. , 2017 ). The sub-Saharan African region is characterized by mixed migration flows and multiple health challenges, including HIV and tuberculosis, that, due to the inequalities experienced in access to healthcare disproportionately affect many groups—including migrants and mobile populations ( Vearey et al., 2017 ; Vearey, 2018 ). Given the existing structural factors impeding access to healthcare, coupled with high rates of mobile telephone use across the sub-Saharan African region, ‘mobile health’ or ‘mHealth’—broadly defined as the use of mobile phones in health systems ( Noordam et al. , 2011 )—is consistently recognized as having great potential for improving access to healthcare in this context ( Bloomfield et al. , 2014 ; Hampshire et al. , 2015 ; Lee et al. , 2017 ). Its application ranges from the use of mobile phones to improve point-of-care data collection, delivery and communication to real-time medication monitoring and adherence support ( Bervell and Al-Samarraie, 2019 ). Such mobile technologies also offer opportunities for health systems research.
The Migration, Gender and Health Systems (MiGHS) project—a collaboration between the Universities of Cape Town and the Witwatersrand, the London School of Hygiene and Tropical Medicine, and the South African National Department of Health (NDoH)—is researching the impact of migration and mobility on the South African public healthcare system. We identified a gap in methodologies that are able to capture ‘real-time’ data about the healthcare-seeking experiences and interactions with healthcare systems that migrant and mobile populations have over time and place.
To this end, we are exploring the use of WhatsApp Messenger (‘WhatsApp’), a Mobile Instant Messaging (MIM) platform, as a tool for conducting longitudinal research on health systems use by migrant and mobile communities in South Africa. We focus on WhatsApp due to the specific opportunities it presents for undertaking health systems research across both time and place with migrant and mobile populations, including those moving within South Africa (internal migrants) and those crossing borders (international migrants, including refugees and asylum seekers). Our decision to focus on WhatsApp is informed by several key observations, including those drawn from existing literature.
Firstly, mobile phones play important and diverse roles in the lives of migrants, both in the Global North and South ( Bacishoga et al. , 2016 ; DA Silva Braga, 2016 ; Frouws et al. , 2016 ; Lim and Pham, 2016 ; Alencar et al. , 2019 ; Mancini et al. , 2019 ; Mattelart, 2019 ; Alencar, 2020 ; Godin and Donà, 2020 ; Greene, 2020 ), including in South Africa ( Marchetti-Mercer and Swartz, 2020 ). WhatsApp is a prevalent and affordable platform in South and Southern Africa ( Shambare, 2014 ; Pindayi, 2017 ; Dahir, 2018 ).
Secondly, WhatsApp facilitates the collection of ‘real-time’ data over both time and place. This is achieved through two key functions; participants are able to share their location via WhatsApp, capturing experiences as they are happening and WhatsApp enables users to keep the same mobile phone number and/or account should they cross international borders. The ability to retain the same number has long been a feature of WhatsApp, but recent updates mean that if the number associated with a WhatsApp account is changed, contacts are notified of the change. As such, if a research participant changes their number, they would remain contactable by a research team.
Finally, WhatsApp can also interface with online platforms that allow for the automatic administration of surveys through WhatsApp. The latter function, which is unique to WhatsApp, warrants an independent review of the use of WhatsApp as a data collection tool, given its potential for conducting health research.
Whilst WhatsApp has been successfully used in research with migrant and mobile groups ( Almenara-Niebla and Ascanio-Sánchez, 2020 ; Khoso et al. , 2020 ), little is known about the use of WhatsApp in health systems research. To address this gap, we have undertaken a scoping review exploring the use of WhatsApp in health systems research. In doing so, we hope to glean lessons learned on how best to design and implement research using WhatsApp with migrant and mobile communities in South Africa. Given the well-documented sensitivities that can emerge when conducting research with migrant and mobile groups ( Duvell et al. , 2008 ; Ahmed et al. , 2019 ), we pay particular attention in our review to the approaches taken to protect participants’ privacy.
After providing an overview of MIM approaches and WhatsApp more specifically, we present the methodology for our scoping review, followed by our findings. We then discuss the implications for health systems research and conclude with recommendations for researchers interested in exploring the use of WhatsApp as a research tool.
Mobile Instant Messaging and the use of WhatsApp Messenger for health systems research
Many mHealth interventions make use of Mobile Instant Messaging (MIM), a feature which allows smartphone users to connect to the internet to send real-time text messages to individuals or groups at little or no cost ( Church and De Oliveira, 2013 ). The real-time text message feature of MIM provides an easy-to-use tool for data collection: it enables immediate communication between researcher and participant; and offers flexibility regarding place and time of use as participants and investigators do not have to share a geographic location ( Kaufmann, 2018b ; Kaufmann and Peil, 2019 ). As a result, research using MIM can be carried out wherever there is internet connectivity, via cell phone networks or Wi-Fi, thus providing new opportunities for research. This is particularly relevant when working with communities, including migrant and mobile populations, that are difficult to reach and/or to maintain contact with over time when using more traditional research methods such as face-to-face interviews and administered surveys ( Kaufmann and Peil, 2019 ).
Globally, WhatsApp Messenger (‘WhatsApp’) has emerged as one of the world’s fastest-growing MIM applications ( Endeley, 2018 ; Fiesler and Hallinan, 2018 ), and, by February 2020 had 2 billion users in >100 countries ( WHATSAPP, 2020 ). The WhatsApp software offers a plethora of health-related uses, including for optimizing communication and the delivery of health education ( Araújo et al. , 2019 ; Lima et al. , 2019 ). It has particularly high penetration rates in India, Indonesia, Malaysia, Brazil and South Africa ( Dahir, 2018 ; Fiesler and Hallinan, 2018 ). Most recently, WhatsApp has formed part of both South Africa and the World Health Organization’s (WHO) responses to the SARS-CoV-2 pandemic ( DEPARTMENT OF HEALTH, S. A., 2020 ; Farai, 2020 ). In March 2020, Health Connect was created for the South African National Department of Health (NDoH) by Praekelt.org, building on Praekelt.org’s experience with national mHealth programmes, including the established MomConnect application ( Seebregts et al. , 2018 ). The Health Connect software has since been used by the WHO to create their own WHO HealthAlert Covid19 chat service, indicating the opportunities and reach provided by WhatsApp globally ( Farai, 2020 ).
Methodological and ethical concerns
The use of WhatsApp necessitates consideration of key methodological, practical and ethical questions ( Boase, 2013 ; Tagg et al. , 2017 ; Barbosa and Milan, 2019 ). For example, there is a need for adequate infrastructure, including reliable access to electricity and the internet, and ownership of smartphones capable of running WhatsApp ( Tagg et al. , 2017 ). Gender and other equity-related differences in the use of mobile technology must also be carefully considered ( Noordam et al. , 2011 ). For example, for many people in Southern Africa, access to a WhatsApp compatible phone remains restrictively expensive. There is also a growing body of literature, particularly from developing countries, on the significant gender divide in access to mobile phones, with men being far more likely to have access to a device than women ( Blumenstock and Eagle, 2010 ; Zainudeen et al., 2010 ; Murphy and Priebe, 2011 ). Some studies reveal the nuanced intersections of mobile phone usage with gender, poverty and other social strata: findings from a study in Rwanda ( Blumenstock and Eagle, 2010 ) indicate that phone owners are wealthier, better educated and predominantly men when compared to the general population. Research using WhatsApp thus has the potential to exacerbate existing inequities, if such considerations are not thoughtfully addressed beforehand.
Ensuring the privacy and confidentiality of participants and data are also critical when engaging with WhatsApp as a research tool, due to ongoing concerns with the application’s security ( Kimmel and Kestenbaum, 2014 ; Kaufmann and Peil, 2019 ). Although communication on WhatsApp has been encrypted since 2016, allowing data between communicating parties to be secure, this does not stop Facebook—who purchased WhatsApp in 2014—from accessing and using data collected from subscribers, without their affirmative consent ( Kimmel and Kestenbaum, 2014 ). Nor does the encryption technology guarantee privacy from government surveillance for national security purposes ( Endeley, 2018 ). Further, Ganguly (2017) has reported a design feature in WhatsApp that could potentially allow some encrypted messages to be read by unintended recipients, compounding the possible breaches of WhatsApp data. Ethical considerations relating to confidentiality and anonymity of human participants are thus central when collecting data via WhatsApp. This issue is especially pertinent when working with individuals in potentially precarious positions ( Barbosa and Milan, 2019 ), as is often the case, for example, with migrant and mobile communities, who may not hold the documents required to be in a country legally.
The purpose of a scoping review is to identify, retrieve and synthesize literature relevant to a particular topic for the purpose of assessing the main concepts underscoring a research area and the key sources and types of available evidence ( Weeks and Strudsholm, 2008b ). This scoping review thus endeavours to provide not only a clearer picture of the ways in which WhatsApp is currently being used for health research but also of the opportunities and challenges that the MIM service creates.
The main stages of this scoping review were: (1) searching for relevant studies; (2) selecting studies based on pre-defined inclusion and exclusion criteria; (3) extracting data and (4) characterizing, summarizing and reporting the results. However, this process was iterative, incorporating flexibility in the movement between stages and with some repetition of steps as required to ensure a comprehensive review of the literature ( Weeks and Strudsholm, 2008b ).
Scoping review methodology observes many of the same steps as systematic reviews: the use of rigorous and transparent methods for data collection, analysis and synthesis remains crucial to enhance the reliability of results and the potential for replication ( Weeks and Strudsholm, 2008b ; Pham et al. , 2014 ; Munn et al. , 2018 ). A key difference between scoping and systematic reviews, however, is that whilst the study design as well as study findings are important considerations for both, scoping reviews do not typically include a process of quality assessment ( Weeks and Strudsholm, 2008a ; Grant and Booth, 2009 ). Thus, we did not use study quality as a criterion for selecting studies for the review.
Search strategy
Two study investigators (K.M. and T.d.G.) simultaneously conducted a search of article titles and abstracts in five key public health electronic databases—Scopus, PubMed, SAGE Journals Online, ScienceDirect and JSTOR. The keywords ‘WhatsApp’ and ‘health research’ were combined using the Boolean operator ‘AND’, limiting the publication date from 2009 (the year when WhatsApp was first launched) to November 2019 (the time at which the search was undertaken). Sixty-nine articles were identified through the search—see Table 1 for an overview of the results. We searched both titles and abstracts, as searching and screening titles alone might miss studies using WhatsApp for data collection that did not reflect on this in the study title. Due to time and cost considerations, we limited our search to English language publications.
Study selection
We used the inclusion/exclusion criteria outlined in Table 2 to assign a value of ‘include’, ‘exclude’ or ‘maybe’ to the 69 identified articles in order to ascertain whether the article should be included in the review. In cases where it was not possible to decide based on the abstract alone, the full article was reviewed. Inter-rater reliability of the study selection was high with only five discrepancies, representing 6.3% of the total selected studies. Each discrepancy was a case of one reviewer coding an article as ‘maybe’ with the other coding it as ‘include’ or ‘exclude’. In all cases, the full article was retrieved and read by both investigators (K.M. and T.d.G.) to resolve the discrepancy. Following the full-paper review and exclusion of 5 additional articles, 16 articles were included in the subsequent analysis.
Inclusion/exclusion criteria for selecting studies for review
In order to be as inclusive as possible, given the small amount of evidence currently in this area, inclusion and exclusion criteria were deliberately kept broad. For example, no exclusion criteria were defined based on study design or publication type, and we did not use study quality as an inclusion criteria ( Weeks and Strudsholm, 2008a) .
Data extraction
Following the selection of the articles for review, two study investigators (K.M. and J.H.) developed a standard coding template, which was discussed with all co-investigators, to extract data from each original research article. The template was designed to include a description of the amount, focus and nature (i.e. the scope) of research related to the use of WhatsApp for health research data collection, and to support the summarizing of findings. Whilst the framework was initially developed a priori, we also followed an iterative approach, further expanding on the initial framework to comprehensively cover the findings identified in the data extraction process, in line with our iterative approach ( Lavallee et al. , 2014 ).
Two study investigators (K.M. and T.d.G.) independently extracted the data from each article and entered them into the coding template, developed in Excel. One additional study investigator (J.H.) extracted data from randomly selected articles as an additional cross-check of the findings. With regards to these random checks, we achieved inter-rater reliability of the descriptive data extraction process of 100% agreement.
To describe the overall quantity of research in this field over time, we recorded the year of publication of each article. To describe the focus of the research, we extracted data on the study setting and on, broadly defined, the research participants—healthcare workers or users. To describe the nature of the research, we extracted data on the disciplinary perspective underpinning the study, characterized iteratively (elaborated below) and the study design—whether quantitative, qualitative or mixed-methods, how WhatsApp was being applied to collect data and reflections on the choice of WhatsApp for data collection. In addition, if the information was available, we included the following methodological considerations of using WhatsApp: (1) how the participants interacted with the WhatsApp interface—the opportunities and challenges, and an assessment of any social stratification implications of using the application, including gender and/or socio-economic factors, such as those discussed earlier, that can shape certain groups’ access to mobile technology; (2) the impact of WhatsApp, which refers to the researchers’ evaluation of implementing WhatsApp for health research, including technical insights and (3) the ethical implications of using WhatsApp in health research.
Whilst our coding framework was developed a priori, our categories evolved, guided by the data. For example, we expanded the category of research participants to include (in addition to healthcare users and workers) the general public, which we identified as a new code in the data. Further, we distinguished ‘health systems’ from ‘health services’, although the two disciplines are often used interchangeably. In our reading of the studies reviewed, we observed clusters that either: (1) explored the perspectives of health care providers within the health system, for the purpose of health systems strengthening or (2) involved research with healthcare users, to capture aspects of service delivery in the target population. Given these distinctions, we classified the prior studies under ‘health systems’ and the latter under the ‘health services’ umbrella.
Collating, summarizing and reporting results
We used a qualitative descriptive approach ( Weeks and Strudsholm, 2008a) to characterize the evidence on the use of WhatsApp for health research data collection. Figure 1 summarizes the search strategy and study selection processes of the scoping review.

Results of search strategy and process of selecting articles on the use of WhatsApp for health research data collection.
Our results are presented in three main categories: (1) the number of articles published per year (the amount) and focus of research; (2) discipline and study design and (3) methodological implications—a brief overview of which can be found in Table 3. As such, the first section provides a summary of the trends observed in the literature, including the number of studies published according to year, the study settings and a classification of the study subjects (health providers and/or users and/or general public). The second section distinguishes between the different disciplines that cut across the literature and the various study designs that use WhatsApp for health researchas linked to these disciplines. It further examines the study designs, including approaches to data collection and analysis, according to three classifications: (1) quantitative studies; (2) qualitative studies and (3) mixed-methods studies. In the final section, the methodological implications of using WhatsApp are elaborated according to the study designs identified in the previous section.
Amount and focus of research employing WhatsApp as a data collection tool
We identified 16 articles that employed WhatsApp for health research in the defined time period (2009–19). All articles were published in 2016 or later, with nine articles (over half of the total) published in 2019. The articles identified covered research from a variety of contexts. Five of the studies present work undertaken in HICs; the United Kingdom (UK) ( Raiman et al. , 2017 ; Rathbone et al. , 2020 ), the United Arab Emirates (UAE) ( Hazzam and Lahrech, 2018 ), Saudi Arabia ( Alsohibani et al. , 2019 ) and Israel ( Gesser-Edelsburg et al. , 2019 ). The remaining 11 articles focused on research from LMICs; three present work from India ( Rasidi and Varma, 2017 ; Karim et al. , 2019 ; Tyagi et al. , 2019 ), two from Nigeria ( Khalid et al. , 2019 ; Shitu et al. , 2019 ) and one each from Kenya ( Henry et al. , 2016 ); Malawi ( Pimmer et al. , 2017 ); Mozambique ( Arroz et al. , 2019 ); Peru ( Bayona et al. , 2017 ); Syria ( Fardousi et al. , 2019 ) and Zimbabwe ( Madziyire et al. , 2017 ). The majority of the studies (11 out of 16) collected data on the perspective of healthcare providers, including interns (apprentices or trainees). Two studies collected data from healthcare users, one from the general public, one from the general public and healthcare providers and one from medical students.
Nature of research employing WhatsApp as a data collection tool
Discipline and study design.
The 16 studies identified were from a variety of disciplinary backgrounds, most commonly health systems ( Henry et al. , 2016 ; Pimmer et al. , 2017 ; Hazzam and Lahrech, 2018 ; Arroz et al. , 2019 ; Fardousi et al. , 2019 ; Rathbone et al. , 2020 ). Additional disciplines include health services ( Bayona et al. , 2017 ; Tyagi et al. , 2019 ), public health ( Alsohibani et al. , 2019 ; Gesser-Edelsburg et al. , 2019 ), medical education ( Raiman et al. , 2017 ) and various clinical science disciplines, including dentistry ( Rasidi and Varma, 2017 ), medicine ( Madziyire et al. , 2017 ; Karim et al. , 2019 ) and pharmacy ( Khalid et al. , 2019 ; Shitu et al. , 2019 ).
Half of the studies included in the review are quantitative in nature ( Madziyire et al. , 2017 ; Rasidi and Varma, 2017 ; Hazzam and Lahrech, 2018 ; Alsohibani et al. , 2019 ; Gesser-Edelsburg et al. , 2019 ; Karim et al. , 2019 ; Khalid et al. , 2019 ; Shitu et al. , 2019 ) of which the majority ( n  = 5) are from the clinical science disciplines (as listed above). None of the quantitative studies includes a statement on their decision to use WhatsApp for data collection, such as the opportunities it provides for the research in question, either generally, or compared to other online data collection approaches. In seven of the eight quantitative studies identified, WhatsApp was used—either exclusively ( n  = 2), or in combination with other social media channels ( n  = 5)—to send hyperlinks to online surveys, thereby functioning as an intermediary platform for data collection. One study ( Gesser-Edelsburg et al. , 2019 ), however, used a web-based platform to build an interactive survey that was distributed via multiple social media channels, including WhatsApp. As described earlier, WhatsApp can interface with such web-based platforms that allow for the automatic administration of surveys through WhatsApp, such that participants can receive and respond to questions one at a time in the chat box. Although the above study in question does imply that the survey was administered—via several online channels—on a question-by-question basis, rather than simply distributed at one go, the authors did not elaborate on the exact process of data collection.
Across the quantitative studies, the recruitment strategies used were poorly described. Two studies ( Madziyire et al. , 2017 ; Khalid et al. , 2019 ) indicate that recruitment of participants occurred before sending them the survey link via WhatsApp, without elaborating any further. In five of the studies, WhatsApp was used as the recruitment tool; authors either directly sent the survey link to pre-identified target groups, at large, as a means of recruiting potential individuals ( Hazzam and Lahrech, 2018 ; Karim et al. , 2019 ; Shitu et al. , 2019 ); or they sent the link to a sub-set of known individuals in the target group, who then, through a snowball approach identified and forwarded the link to additional eligible participants ( Alsohibani et al. , 2019 , Gesser-Edelsburg et al. , 2019 ). The process of recruitment across these five studies, however, is vague. It appears there was no explicit strategy, and that recruitment happened passively, through simply forwarding the survey link to potential participants (and in some cases requesting them to re-forward the link further). In one study ( Rasidi and Varma, 2017 ), there is no indication given at all as to how the participants were recruited.
Six of the studies employed a qualitative design ( Henry et al. , 2016 ; Bayona et al. , 2017 ; Raiman et al. , 2017 , ; Arroz et al. , 2019 ; Fardousi et al. , 2019 ; Rathbone et al. , 2020 ) and were undertaken with either a health systems or health services disciplinary focus. Of these, three studies analysed data sourced from (written) text messages sent over WhatsApp ( Henry et al. , 2016 ; Bayona et al. , 2017 ; Rathbone et al. , 2020 ); one study analysed WhatsApp text messages and images ( Arroz et al. , 2019 ); another one analysed text messages, images and webpage links shared via WhatsApp ( Raiman et al. , 2017 ); and the final study analysed voice calls recorded over WhatsApp ( Fardousi et al. , 2019 ). The data from the studies were analysed using either thematic analysis ( n  = 4) or content analysis ( n  = 2).
With one exception ( Fardousi et al. , 2019 ), the qualitative studies and two mixed-methods studies (discussed below), all used WhatsApp in a tethered approach—to deliver an intervention, either for mentoring or improving access to care, with the success of the intervention subsequently evaluated through analysing the WhatsApp content that was generated as part of the intervention (as specified above and below). As exemplified in these studies, WhatsApp was used for data collection, beyond just delivering the intervention in question.
To elaborate further, two-thirds of the qualitative studies ( Henry et al. , 2016 ; Raiman et al. , 2017 ; Arroz et al. , 2019 ; Rathbone et al. , 2020 ) used WhatsApp to facilitate communication between junior and senior workers for mentoring and/or educational purposes. Given the nature of these studies, since the mentoring and/or educational intervention that was delivered via WhatsApp also formed the data source, the participants in the intervention were simultaneously recruited as the subjects for the data collection component of the study.
Of these, three studies ( Henry et al. , 2016 ; Raiman et al. , 2017 ; Arroz et al. , 2019 ) explicitly discuss the choice of WhatsApp for data collection, based on its popularity as a social communication tool. The other two qualitative studies included in the review employed WhatsApp (in combination with other approaches) to collect data amongst groups facing vulnerability. One study ( Bayona et al. , 2017 ) describes how WhatsApp (and SMS) text messages were employed to elicit barriers and facilitators to accessing HIV health services amongst men who have sex with men (MSM) in Peru. The authors make a general observation regarding the acceptability of mHealth interventions amongst this group of individuals, without specifically justifying their choice of WhatsApp, either generally—as an instant messaging platform—or over other digital platforms. In the other study ( Fardousi et al. , 2019 ), the authors describe how they selected WhatsApp (and Skype) to conduct interviews remotely, in areas where physical access was a barrier, to understand challenges experienced by healthcare providers in besieged areas in Syria. The authors indicate that they used purposive sampling to recruit healthcare providers, who were then snowballed, with each recommending two-to-three additional potential participants.
The two remaining studies included in the review employed mixed-methods approaches. Pimmer et al. (2017) used WhatsApp as a communication tool between healthcare workers—with a similar design and recruitment approach as the four qualitative studies described earlier—to explicitly understand its application to support healthcare work. They subsequently analysed the WhatsApp text messages, both thematically and statistically. In the other mixed-methods study ( Tyagi et al. , 2019 ), rehabilitated participants with spinal cord injury sent video clips of their daily activities via email, text or WhatsApp (pre-intervention) that were then used by therapists to highlight images of wrong movements captured in these videos (as part of the intervention). The patients were recruited through a spinal rehabilitation centre. To analyse the functional status of patients pre- and post-intervention, patients completed the spinal cord independence measure (SCIM). The authors broadly infer the opportunities of telehealth to overcome barriers to continuity of care, without specific reference to the choice of WhatsApp in the study.
Methodological implications of using WhatsApp
Opportunities, challenges and impact.
Of the eight quantitative studies included in the review, none discuss the experiences of the research participants (positive or otherwise) while interacting with the WhatsApp interface, and neither do they evaluate the impact nor provide technical insights of implementing WhatsApp in the study. A limitation noted in three of the quantitative studies ( Hazzam and Lahrech, 2018 ; Khalid et al. , 2019 ; Shitu et al. , 2019 ), all of which focus on health care providers, is the exclusion of participants who do not use social media platforms. Three studies, also amongst providers, describe challenges that also link to the technological nature of the research: (1) low response rates ( Khalid et al. , 2019 ); (2) difficulties in determining response rates as the number of eligible participants who received the survey link were unknown ( Shitu et al. , 2019 ) and (3) the inability of respondents to seek clarity on questions ( Madziyire et al. , 2017 ).
With regards to the qualitative and mixed-methods study designs, the most commonly identified opportunities, as extracted from the data collected via WhatsApp (described earlier) suggest that WhatsApp is mobilized to share information ( Henry et al. , 2016 , ; Bayona et al. , 2017 ; Raiman et al. , 2017 ; Pimmer et al. , 2017 ; Arroz et al. , 2019 ; Rathbone et al. , 2020 ), raise questions ( Henry et al. , 2016 , ; Bayona et al. , 2017 ; Pimmer et al. , 2017 ; Arroz et al. , 2019 ) and support the professional development of junior-level staff ( Henry et al. , 2016 ; Raiman et al. , 2017 ; Rathbone et al. , 2020 ). In addition, two studies ( Pimmer et al. , 2017 ; Arroz et al. , 2019 ) cite the participatory communication function of the application as an advantage in the context of collecting group information. All the studies that used WhatsApp to facilitate communication between health professionals ( Henry et al. , 2016 ; Pimmer et al. , 2017 ; Raiman et al. , 2017 ; Arroz et al. , 2019 ; Rathbone et al. , 2020 ) report improved communication as a result of using the application. Two studies ( Bayona et al. , 2017 ; Tyagi et al. , 2019 ) report the usefulness of WhatsApp in overcoming barriers to continuity of care, with Bayona et al. (2017) further emphasizing the opportunity of employing WhatsApp as a means to provide patient perspectives that are missing in provider-defined care models. Fardousi et al. (2019) describe how using WhatsApp for health research in hard to access humanitarian settings can help others similarly situated to mitigate health systems challenges and raise awareness to mobilize the international community. Across several studies, authors cited the potential for discrimination or bias resulting from inadequate infrastructure, technological competency ( Bayona et al. , 2017 ; Pimmer et al. , 2017 ; Arroz et al. , 2019 , Fardousi et al. , 2019 ; Tyagi et al. , 2019 ) and gender discrepancies in access to technology ( Henry et al. , 2016 ; Fardousi et al. , 2019 ) as challenges linked to using WhatsApp. Additional challenges in two studies that use WhatsApp to facilitate communication between health workers ( Pimmer et al. , 2017 ; Rathbone et al. , 2020 ) point to the sharing of unrelated and/or inappropriate content, difficulties maintaining work-life balance (due to the timing of messages) and delays in responses. Several studies ( Pimmer et al. , 2017 ; Raiman et al. , 2017 ; Arroz et al. , 2019 ) also point to the lack of face-to-face interaction as being problematic in the context of facilitating supervision.
Ethical considerations
We found little consistency between the studies with regards to efforts taken to ensure privacy, confidentiality and anonymity when using WhatsApp as a data collection tool, even in studies of a similar design.
None of the quantitative studies discussed the ethical implications of using WhatsApp for health research. Two of the studies point to some ethical measures taken to inform and protect participants in the research. Khalid et al. (2019) state that their online questionnaire conveyed the study information and emphasized the voluntary nature of participation. Alsohibani et al. (2019) cite that participants’ consent was obtained before administering the online questionnaire, but they do not elaborate on the consent process.
Across the qualitative studies, discussion of research ethics was largely missing with one notable exception. Fardousi et al. (2019) reported taking the following measures for obtaining informed consent and to protect the privacy of healthcare workers in besieged areas of Syria: (1) participants used mobile phones to photograph and send signed consent forms; (2) interviews were recorded anonymously using identification codes and (3) interviewers did not ask for participant names.
In four of the qualitative studies, patient data were shared between health care professionals ( Henry et al. , 2016 ; Pimmer et al. , 2017 ; Raiman et al. , 2017 ; Rathbone et al. , 2020 ). However, only one of them ( Pimmer et al. , 2017 ) discusses explicit training measures undertaken to prevent sharing of patient-identifying information on WhatsApp. Rathbone et al. (2020) highlight concerns of patient privacy, pointing to a lack of training regarding a safe way to discuss patients on the platform. On the other hand, Raiman et al. (2017) maintain that WhatsApp’s end-to-end encryption enables safe referral to and discussion of patients, thereby eliminating the need to anonymise the data. Similarly, Henry et al. (2016) indicate that the WhatsApp content that was shared between health workers was not anonymized; rather, health workers were instructed to obtain verbal consent before posting photos of patients, and personal identifiers were removed from chat logs to ensure patient confidentiality in the reporting of results. Both the study on patients with spinal cord injury ( Tyagi et al. , 2019 ) and the study of health access experiences of MSM ( Bayona et al. , 2017 ) report using patient data directly transmitted by the patients via the WhatsApp platform. However, neither detail how issues of patient confidentiality were handled. This finding is particularly surprising in the case of the latter, as MSM are a population group that are in many contexts marginalized and considered particularly vulnerable ( Cáceres et al. , 2008 ).
The rapid increase in the number of studies using WhatsApp as a tool for health research published per year indicates the growing interest in this area—and reflects developments in mobile technology and the increase in WhatsApp’s user base. That most of the articles we identified describe research conducted in LMICs, with six of those in sub-Saharan Africa, is unsurprising, given that WhatsApp has particularly high penetration rates in these contexts, with India, Indonesia, Malaysia, Brazil and South Africa topping the list ( Dahir, 2018 ; Fiesler and Hallinan, 2018 ). Within these studies, WhatsApp was largely used in one of two ways for health research—to send hyperlinks to online surveys, or to deliver and evaluate, either an intervention designed for healthcare users or a communication programme for healthcare providers.
Our review is limited to studies in health research databases. Using different and/or additional search terms beyond ‘health research’ (e.g. ‘health studies’ or ‘health investigations’) may have yielded more results. We reason, however, that using supplemental search terms would have produced studies similar in nature to those we identified and included in our review. Given that we observed distinct patterns across the wide range of study types and disciplines included in this review, we are confident in the interpretation of our results, including our analysis of the current (limited and nascent) state of literature using WhatsApp for health research. Indeed, the most noteworthy finding of our review is the lack of discussion on how and why WhatsApp was used by the researchers and on the potential limitations or implications of this, including, and especially with regards to ethical concerns. There is a clear need to report on these issues for digital studies, given the known challenges regarding confidentiality and data breaches. We subsequently focus on issues of research ethics in this discussion, in light of the urgent need for researchers to systematically document their use of WhatsApp and engage with its ethical issues.
In almost half of the studies we identified ( n  = 7), WhatsApp was used to facilitate data collection via online surveys. These studies offered little in the way of ethical insights for online research. In most of the surveys we located, the nature of the data collected appeared not to be sensitive, nor were vulnerable populations being surveyed. Nonetheless, the electronic and online nature of survey data add new methodological complexities surrounding data storage and security ( Buchanan and Hvizdak, 2009 ). Given in particular that the mobile app industry is largely unregulated and cybercrime is prevalent, it would have been pertinent for authors to inform the study participants about the potential risks involved and what precautions were being taken to support the privacy and security of the participants’ data ( O’Connor et al. , 2016 ).
In addition, whether individuals consider their data to be safe, secure and used appropriately by those who control it can be a key consideration in a participant’s choice to enrol in a study ( O’Connor et al. , 2016 ). The perception of a survey invitation as spam or containing viruses, and the level of data security can have a possible negative impact on data quality and response rates ( Scriven and Smith-Ferrier, 2003 ). The latter was indeed cited as an issue in several of the studies identified, without the authors providing any explanations regarding participants’ poor engagement. As we reported earlier, the recruitment approaches across the quantitative studies were poorly described and many appeared not to involve an explicit or active strategy for engaging participants. One of the main findings in a systematic review of the factors affecting engagement in digital health studies ( O’Connor et al. , 2016 ) suggests that an active recruitment approach that engages with issues around privacy and security is key to overcoming barriers preventing people from participating in studies of this nature. The process of informed consent prior to the study allows researchers to establish trust with the respondents and provide an explanation of the purpose of the study, the selection criteria, how data will be employed and who will have access to it ( Buchanan and Hvizdak, 2009 ). Obtaining informed consent and assuring that data are carefully handled is essential in academic research and imperative in digital studies ( Kaufmann and Peil, 2019 ), given concerns with confidentiality and data breaches. However, only one of the identified survey designs cites that informed consent was obtained from the research participants. That the remaining studies failed to describe if and how they obtained participants’ consent prior to recruiting them suggests that research ethics is not foregrounded in these studies.
In the remaining half of the studies identified, WhatsApp functioned as both research field site and as a data collection tool, often involving the exchange of sensitive information. These approaches necessitate a systematic discussion of the methodological and ethical implications of the platform’s use for health research. Except for two of the studies identified ( Pimmer et al. , 2017 ; Fardousi et al. , 2019 ), ethical procedures outlined were generally limited to obtaining approval from research ethics committees. With regards to digital data in qualitative research, ethical decision-making is compounded in this case by the fact that ethical review boards and respondents themselves may not understand the nuances of software-based data collection tools, including issues associated with the assumed end-to-end encryption of WhatsApp, which is often presumed to be secure ( Markham and Buchanan, 2012 ; Boase, 2013 ). This resonates with data protection concerns within the mHealth field, including the observation that few African countries have comprehensive mHealth data protection legislation in place to begin with, compounding concerns about data security and privacy in LMICs ( Hackett et al. , 2018 ).
The recent introduction of end-to-end encryption to WhatsApp also risks giving users a false sense of security and encourages individuals to use it also for sensitive exchanges, exposing participants to potential risks that researchers may indirectly amplify ( Barbosa and Milan, 2019 ). In fact, the authors in one of the studies ( Raiman et al. , 2017 ) explicitly discuss how the end-to-end encryption offered by WhatsApp provides a safe and secure platform to discuss patients, thereby eliminating the need to anonymize the data. However, as Kaufman and Peil (2019) explain, researchers are in fact unable to guarantee data security on the part of the platform provider as participants are also subject to WhatsApp’s terms of usage and pass over their data rights to Facebook when initially setting up their accounts. In general, we observed a lack of documentation of efforts taken, if any, to anonymize third-party data in the identified studies whereby health professionals exchanged patient data on the platform. With the exception of one of the studies ( Pimmer et al. , 2017 ), the remaining four did not report any formal training on ways to safely share patient data.
Two of the studies identified in our review ( Bayona et al. , 2017 ; Fardousi et al. , 2019 ) dealt with research subjects facing specific vulnerabilities that could result in serious ramifications if the data linked to them were exposed. In one study of MSM in Peru, although the authors, like others before them ( Cáceres et al. , 2008 ) recognized the participants as being from a group facing marginalization and stigma in the country, they did not report taking measures to protect the subjects’ identity through anonymization of the digital data. Such measures, if taken, should be made clear in the manuscript. In the second such study, participants comprised frontline health workers in opposition-controlled areas in Syria. In this case, the authors took a systematic approach to implement full anonymisation (described earlier) in order to protect the research participants from any harm that could result from exposure of their political affiliations.
The purpose of this review was to inform our approach for exploring the use of WhatsApp for data collection among migrant and mobile healthcare users in South Africa. Given our specific interest in capturing ‘real-time’ data about healthcare users’ experiences over time and place, through the administration of a survey methodology, and the unique opportunity that WhatsApp provides in this regard, we hoped to glean insights from other similar studies that may have implemented WhatsApp in this way. However, understanding the methodological opportunities, barriers and impact of using WhatsApp for health research was constrained by the limited ways in which WhatsApp has been used, and how its use has been reported, to date.
Seven out of the eight studies administering surveys used WhatsApp to send hyperlinks to online surveys, with WhatsApp functioning as a ‘static’ platform to facilitate data collection. Such use may not have warranted a discussion of the practical and logistical applications of using the software for health research. However, as described earlier, WhatsApp can also be used to administer surveys directly and ‘actively’ on the platform, an approach that appears to have been considered in one study located in our review ( Gesser-Edelsburg et al. , 2019 ). The authors of this study developed a WhatsApp compatible web-based survey that has the potential to contribute to innovation regarding the nature of digital survey administration. To name a few features, these surveys can be automatically broadcasted to participants, one question at a time, with the receipt of each question being dependent on the completion of the previous one. Further, automated reminders can be sent to participants if, for example, they fail to start the survey after a certain amount of time has lapsed. Such features can enhance response rates in digital surveys, which, as cited earlier, was identified as a common challenge across several studies included in our review. The authors, however, failed to describe their method, which is a lost opportunity for future research.
Indeed with a few exceptions, most of the studies reviewed did not clearly document and describe their use of WhatsApp to collect health-related data, which makes it difficult to identify emerging best practice in this field. Given the use and acceptability of WhatsApp among hard-to-reach and often precarious communities, including asylum seekers and undocumented migrants ( Kaufmann, 2018a ), significant opportunities exist for the use of WhatsApp in research with these populations. However, specific methodological and ethical issues arise when working with these communities, including the uncompromising need to safeguard participant privacy ( Barbosa and Milan, 2019 ). As such, we identify three key imperatives for researchers using WhatsApp in health research.
Primarily, given WhatsApp’s novelty as a research tool, researchers need to systematically and clearly document and discuss their use of the application when presenting their research. Current research tends to gloss over how WhatsApp is used as a research tool obfuscating understanding of best practice moving forward. Improving the state of knowledge in this regard, by documenting the challenges associated with and opportunities provided by WhatsApp, will allow for its improved use.
Secondly, given the ethical concerns regarding the use of WhatsApp, researchers must give consideration to selecting and recording only that information which is necessary to the project, encrypting the recorded data so that it is only available to the researchers, removing identifying information from the data and saving the data on secure servers ( Boase, 2013 ). Although we do recognize that the latter recommendation poses its own challenges, as currently most universities no longer run their own servers and service, preferring to rely on commercial alternatives such as Google and Microsoft ( Barbosa and Milan, 2019 ).
As such, when using WhatsApp as a data collection tool, researchers should endeavour to systematically and clearly document research and ethical considerations. Whereas the WHO guidelines for reporting on mHealth interventions ( Agarwal et al. , 2016 ) are specific to digital programmes aimed at improving access to and use of health services—which is beyond the scope of this study—certain aspects of the guidelines are applicable to research using WhatsApp as a data collection tool. For example, the guidelines advocate the reporting of various important aspects of research design and implementation, to enhance the transparency in reporting, promote the critical assessment of digital research evidence, and improve the rigour of future reporting of research findings. In particular, item 14 of the 16-item checklist explicitly focuses on data security, entrusting researchers using mHealth to describe their data security and confidentiality protocols, including all the steps taken to secure personally identifiable information. This dimension cannot be overstated in our study, given that we have identified critical gaps in protecting the privacy and confidentiality of participant identity and health information in the current state of health research employing WhatsApp.
In addition, addressing barriers to infrastructure must be understood beyond simplified notions of the internet and/or smartphone access. As face-to-face interactions between researchers and participants are limited, additional efforts must be made to ensure that participants understand the terms of the research and are provided with information, relating to the specifics of the research project, regarding how they can seek and access support should it be required. Being able to judge whether study participants require health and/or psychological services and referring them accordingly may be difficult via WhatsApp, which raises additional ethical questions when using WhatsApp to conduct research with groups facing vulnerability. Researchers must accordingly document how they plan to overcome such challenges.
This scoping review highlights the opportunities that WhatsApp provides as a tool for health systems research, specifically with migrant and mobile communities in LMIC settings. WhatsApp is low-cost and convenient to operate, has high penetration globally, and, importantly, enables migrant and mobile users to share their location and retain their mobile phone number or WhatsApp account as they cross borders. This offers multiple opportunities for developing new approaches to health systems research in the future. However, the field of health systems research applying WhatsApp as a tool is in its infancy, and real ethical concerns exist. We urge researchers to be cognizant of the risks associated with the use of WhatsApp, to systematically document their use of the application, and to share how they address ethical challenges and concerns around data security.
The authors would like to thank Langa Mlotshwa for her input to the manuscript. We would also like to thank Lenore Longwe and Kwanda Ndaba from the African Centre for Migration & Society, University of the Witwatersrand, and, Faizah Rahshid, Tambu Agere, Hannah Miyanji and Michael Naranjo from the LSHTM, for their administrative support.
This work was supported through the Health Systems Research Initiative (HSRI) in the UK, and is jointly funding by the Department of International Development (DFID), the Economic and Social Research Council (ESRC), the Medical Research Council (MRC) and the Wellcome Trust. Grant number: MR/S013601/1.
Conflict of Interest
The author(s) have declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical considerations No ethical approval was required for this study.
Agarwal S , Lefevre AE , Lee J , WHO mHealth Technical Evidence Review Group et al. 2016 . Guidelines for reporting of health interventions using mobile phones: mobile health (mHealth) evidence reporting and assessment (mERA) checklist . BMJ (Clinical Research ed.) 352 : i1174 .
Google Scholar
Ahmed A , Vandrevala T , Hendy J , Kelly C , Ala A. 2019 . An examination of how to engage migrants in the research process: building trust through an ‘insider’ perspective . Ethnicity & Health 1 – 20 .
Alencar A. 2020 . Mobile communication and refugees: an analytical review of academic literature . Sociology Compass 14 : e12802 .
Alencar A , Kondova K , Ribbens W. 2019 . The smartphone as a lifeline: an exploration of refugees’ use of mobile communication technologies during their flight . Media, Culture & Society 41 : 828 – 44 .
Almenara-Niebla S , Ascanio-Sánchez C. 2020 . Connected Sahrawi refugee diaspora in Spain: gender, social media and digital transnational gossip . European Journal of Cultural Studies 23 : 768 – 83 .
Alsohibani A , Alkheder R , Alharbi M et al. 2019 . Public awareness, knowledge, and attitudes regarding epilepsy in the Qassim region, Saudi Arabia . Epilepsy & Behavior 92 : 260 – 4 .
Araújo ETH , Almeida CAPL , Vaz JR et al. 2019 . Use of social networks for data collection in scientific productions in the health area: integrative literature review . Aquichan 19 : 1 – 12 .
Arroz JA , Candrinho BN , Mussambala F et al. 2019 . WhatsApp: a supplementary tool for improving bed nets universal coverage campaign in Mozambique . BMC Health Services Research 19 : 86 .
Bacishoga KB , Hooper VA , Johnston KA. 2016 . The role of mobile phones in the development of social capital among refugees in South Africa . The Electronic Journal of Information Systems in Developing Countries 72 : 1 – 21 .
Barbosa S , Milan S. 2019 . Do not harm in private chat apps: ethical issues for research on and with WhatsApp . Westminster Papers in Communication and Culture 14 : 49 – 65 .
Bayona E , Menacho L , Segura ER et al. 2017 . The experiences of newly diagnosed men who have sex with men entering the HIV Care Cascade in Lima, Peru, 2015–2016: a qualitative analysis of counselor–participant text message exchanges . Cyberpsychology, Behavior, and Social Networking , 20 , 389 – 396 .
Google Preview
Bervell B , Al-Samarraie H. 2019 . A comparative review of mobile health and electronic health utilization in sub-Saharan African countries . Social Science & Medicine 232 : 1 – 16 .
Bloomfield GS , Vedanthan R , Vasudevan L et al. 2014 . Mobile health for non-communicable diseases in Sub-Saharan Africa: a systematic review of the literature and strategic framework for research . Globalization and Health 10 : 49 .
Blumenstock JE , Eagle N. 2010 . Mobile divides: gender, socioeconomic status, and mobile phone use in Rwanda. In: Proceedings of the 4th ACM/IEEE International Conference on Information and Communication Technologies and Development . pp. 1-10. http://www.gg.rhul.ac.uk/ict4d/ictd2010/papers/ICTD2010%20Blumenstock%20et%20al.pdf , last accessed 22 February 2021.
Boase J. 2013 . Implications of software-based mobile media for social research . Mobile Media & Communication 1 : 57 – 62 .
Buchanan EA , Hvizdak EE. 2009 . Online survey tools: ethical and methodological concerns of human research ethics committees . Journal of Empirical Research on Human Research Ethics 4 : 37 – 48 .
Cáceres C , Cueto M , Palomino N. 2008 . Policies around sexual and reproductive health and rights in Peru: conflict, biases and silence . Global Public Health 3 : 39 – 57 .
Church K , DE Oliveira R. 2013 . What's up with WhatsApp? Comparing mobile instant messaging behaviors with traditional SMS. In: Proceedings of the 15th International Conference on Human-Computer Interaction with Mobile Devices and Services . pp. 352 – 361 .
DA Silva Braga R. 2016 . Technologies as a means, meetings as an end: urban interactions of a migrant community in Rio de Janeiro, Brazil, mobilized through WhatsApp. In: Abdelnour-Nocera J, Strano M., Ess C, Van der Velden M, Hrachovec H. (eds) Culture, Technology, Communication. Common World, Different Futures. CaTaC 2016. IFIP Advances in Information and Communication Technology, vol 490 . Springer, Cham. pp. 68 – 81 .
Dahir AL. 2018 . WhatsApp is the most popular messaging app in Africa. Quartz Africa , 745 https://qz.com/africa/1206935/whatsapp-is-the-most-popular-messaging-app-in-africa/ , last accessed 22 February 2021.
DEPARTMENT OF HEALTH, S. A . 2020 . COVID-19 Connect South Africa [Online]. Praekelt Foundation. https://www.praekelt.org/covid-19-response-in-sa , last accessed 23 June 2020.
Duvell F , Triandafyllidou A , Vollmer B. 2008 . Ethical issues in irregular migration research. In: Prepared for Work Package of Two of the Research Project CLANDESTINO, Undocumented Migration: Counting the Uncountable, Data and Trends Across the Europe, European Commission, Brussels.
Endeley RE. 2018 . End-to-end encryption in messaging services and national security—case of WhatsApp messenger . Journal of Information Security 09 : 95 – 9 .
Farai SF. 2020 . WHO is raising coronavirus awareness globally using a WhatsApp bot developed in South Africa. https://qz.com/africa/1826415/coronavirus-who-adopts-south-african-whatsapp-health-alert/ , last accessed 17 June 2020.
Fardousi N , Douedari Y , Howard N. 2019 . Healthcare under siege: a qualitative study of health-worker responses to targeting and besiegement in Syria . BMJ Open 9 : e029651 .
Fiesler C , Hallinan B. 2018 . “We are the product” public reactions to online data sharing and privacy controversies in the media. In: Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems(CHI ’18), Montreal, QC, Canada, pp. 1 – 13 .
Frouws B , Phillips M , Hassan A , Twigt M. 2016 . Getting to Europe the WhatsApp way: the use of ICT in contemporary mixed migration flows to Europe. In: Regional Mixed Migration Secretariat Briefing Paper . Nairobi, Kenya: Regional Mixed Migration Secretariat.
Ganguly M. 2017 . WhatsApp design feature means some encrypted messages could be read by third party. In: The Guardian . https://www.theguardian.com/technology/2017/jan/13/whatsapp-design-feature-encrypted-messages , last accessed 22 February 2021.
Gesser-Edelsburg A , Shahbari NAE , Cohen R et al. 2019 . Differences in perceptions of health information between the public and health care professionals: nonprobability sampling questionnaire survey . Journal of Medical Internet Research 21 : e14105 .
Godin M , Donà G. 2020 . Rethinking transit zones: migrant trajectories and transnational networks in Techno-Borderscapes . Journal of Ethnic and Migration Studies 1 – 17 .
Grant MJ , Booth A. 2009 . A typology of reviews: an analysis of 14 review types and associated methodologies . Health Information & Libraries Journal 26 : 91 – 108 .
Greene A. 2020 . Mobiles and ‘making do’: Exploring the affective, digital practices of refugee women waiting in Greece . European Journal of Cultural Studies 23 : 731 – 48 .
Hackett KM , Kazemi M , Sellen DW. 2018 . Keeping secrets in the cloud: mobile phones, data security and privacy within the context of pregnancy and childbirth in Tanzania . Social Science & Medicine 211 : 190 – 7 .
Hampshire K , Porter G , Owusu SA et al. 2015 . Informal m-health: how are young people using mobile phones to bridge healthcare gaps in Sub-Saharan Africa? Social Science & Medicine 142 : 90 – 9 .
Hazzam J , Lahrech A. 2018 . Health care professionals’ social media behavior and the underlying factors of social media adoption and use: quantitative study . Journal of Medical Internet Research 20 : e12035 .
Henry JV , Winters N , Lakati A et al. 2016 . Enhancing the supervision of community health workers with WhatsApp mobile messaging: qualitative findings from 2 low-resource settings in Kenya . Global Health: Science and Practice 4 : 311 – 25 .
Karim HMR , Sinha M , Kumar M , Khetrapal M , Dubey R. 2019 . An observation from an online survey: is fresh gas flow used for sevoflurane and desflurane different from isoflurane based anesthesia? Medical Gas Research 9 : 13 .
Kaufmann K. 2018a . Navigating a new life: Syrian refugees and their smartphones in Vienna . Information, Communication & Society 21 : 882 – 98 .
Kaufmann K. 2018b . The smartphone as a snapshot of its use: mobile media elicitation in qualitative interviews . Mobile Media & Communication 6 : 233 – 46 .
Kaufmann K , Peil C. 2019 . The Mobile Instant Messaging Interview (MIMI): Using WhatsApp to Enhance Self-Reporting and Explore Media Usage in Situ. Mobile Media & Communication , Vol. 8(2), pp. 229 – 246 .
Khalid GM , Jatau AI , Ibrahim UI et al. 2019 . Antibiotics self-medication among undergraduate pharmacy students in Northern Nigeria . Medicine Access @ Point of Care 3 : 239920261984684 .
Khoso A , Thambiah S , Hussin H. 2020 . Social practices of Pakistani migrant workers in Malaysia: conserving and transforming transnational affect . Emotion, Space and Society 37 : 100742 .
Kimmel L , Kestenbaum J. 2014 . What's up with WhatsApp: a transatlantic view on privacy and merger enforcement in digital markets . Antitrust 29 : 48 .
Lavallee M , Robillard P-N , Mirsalari R. 2014 . Performing systematic literature reviews with novices: an iterative approach . IEEE Transactions on Education 57 : 175 – 81 .
Lee S , Cho Y-M , Kim S-Y. 2017 . Mapping mHealth (mobile health) and mobile penetrations in sub-Saharan Africa for strategic regional collaboration in mHealth scale-up: an application of exploratory spatial data analysis . Globalization and Health 13 : 63 .
Lim SS , Pham B. 2016 . ‘If you are a foreigner in a foreign country, you stick together’: technologically mediated communication and acculturation of migrant students . New Media & Society 18 : 2171 – 88 .
Lima ICVD , Galvão MTG , Pedrosa SC et al. 2019 . Instant messaging application for the care of people living with HIV/aids . Revista Brasileira de Enfermagem 72 : 1161 – 6 .
Madziyire M , Mateveke B , Gidiri M. 2017 . Beliefs and practices in using misoprostol for induction of labour among obstetricians in Zimbabwe . South African Journal of Obstetrics and Gynaecology 23 : 24 – 7 .
Mancini T , Sibilla F , Argiropoulos D , Rossi M , Everri M. 2019 . The opportunities and risks of mobile phones for refugees’ experience: a scoping review . PLoS One 14 : e0225684 .
Marchetti-Mercer MC , Swartz L. 2020 . Familiarity and separation in the use of communication technologies in South African migrant families . Journal of Family Issues 41 : 1859 – 84 .
Markham A , Buchanan E. 2012 . Ethical decision-making and internet research: Version 2.0. Recommendations from the AoIR ethics working committee. https://aoir.org/reports/ethics2.pdf , last accessed 22 February 2021.
Mattelart T. 2019 . Media, communication technologies and forced migration: promises and pitfalls of an emerging research field . European Journal of Communication 34 : 582 – 93 .
Munn Z , Peters MD , Stern C et al. 2018 . Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach . BMC Medical Research Methodology 18 : 143 .
Murphy LL , Priebe AE. 2011 . “My co-wife can borrow my mobile phone!” Gendered geographies of cell phone usage and significance for Rural Kenyans . Gender, Technology and Development 15 : 1 – 23 .
Noordam AC , Kuepper BM , Stekelenburg J , Milen A. 2011 . Improvement of maternal health services through the use of mobile phones . Tropical Medicine & International Health 16 : 622 – 6 .
O’Connor S , Hanlon P , O’Donnell CA et al. 2016 . Understanding factors affecting patient and public engagement and recruitment to digital health interventions: a systematic review of qualitative studies . BMC Medical Informatics and Decision Making 16 : 120 .
Pham MT , Rajić A , Greig JD et al. 2014 . A scoping review of scoping reviews: advancing the approach and enhancing the consistency . Research Synthesis Methods 5 : 371 – 85 .
Pimmer C , Mhango S , Mzumara A , Mbvundula F. 2017 . Mobile instant messaging for rural community health workers: a case from Malawi . Global Health Action 10 : 1368236 .
Pindayi B. 2017 . Social media uses and effects: the case of Whatsapp in Africa. In: Nelson O, Oyebuyi BR and Salawu A (eds) Impacts of the Media on African Socio-economic Development. Hershey, PA: IGI Global.
Raiman L , Antbring R , Mahmood A. 2017 . WhatsApp messenger as a tool to supplement medical education for medical students on clinical attachment . BMC Medical Education 17 : 7 .
Rasidi MQZBM , Varma MA. 2017 . Knowledge, attitude and practice on hyposalivation in complete denture patients among dental interns in Chennai, India . Journal of Pharmaceutical Sciences and Research 9 : 225 .
Rathbone AP , Norris R , Parker P et al. 2020 . Exploring the use of WhatsApp in out-of-hours pharmacy services: a multi-site qualitative study . Research in Social and Administrative Pharmacy 16 : 503 – 10 .
Scriven A , Smith-Ferrier S. 2003 . The application of online surveys for workplace health research . Journal of the Royal Society for the Promotion of Health 123 : 95 – 101 .
Seebregts C , Dane P , Parsons AN et al. 2018 . Designing for scale: optimising the health information system architecture for mobile maternal health messaging in South Africa (MomConnect) . BMJ Global Health 3 : e000563 .
Shambare R. 2014 . The adoption of WhatsApp: breaking the vicious cycle of technological poverty in South Africa . Journal of Economics and Behavioral Studies 6 : 542 – 50 .
Shitu Z , Jatau A , Mustapha M et al. 2019 . Factors associated with an interest in practice-based research among pharmacists in Nigeria . Journal of Pharmacy Technology 35 : 98 – 104 .
Tagg C , Lyons A , Hu R , Rock F. 2017 . The ethics of digital ethnography in a team project . Applied Linguistics Review 8 : 271 – 92 .
Tyagi N , Goel SA , Alexander M. 2019 . Improving quality of life after spinal cord injury in India with telehealth . Spinal Cord Series and Cases 5 : 1 – 5 .
Vearey J. 2018 . Moving forward: why responding to migration, mobility and HIV in South (ern) Africa is a public health priority . Journal of the International AIDS Society 21 : e25137 .
Vearey J , Modisenyane M , Hunter-Adams J. 2017 . Towards a migration-aware health system in South Africa: a strategic opportunity to address health inequity . South African Health Review 2017 : 89 – 98 .
Weeks LC , Strudsholm T. 2008a . A scoping review of research on complementary and alternative medicine (CAM) and the mass media: looking back, moving forward . BMC Complementary and Alternative Medicine 8 : 1 – 9 .
Weeks LC , Strudsholm T. 2008b . A scoping review of research on complementary and alternative medicine (CAM) and the mass media: looking back, moving forward . BMC Complementary and Alternative Medicine 8 : 43 .
WHATSAPP . 2020 . Two Billion Users – Connecting the World Privately . https://blog.whatsapp.com/two-billion-users-connecting-the-world-privately , last accessed 17 June 2020.
Zainudeen A , Iqbal T , Samarajiva R. 2010 . Who’s got the phone? Gender and the use of the telephone at the bottom of the pyramid . New Media & Society 12 : 549 – 66 .
- africa south of the sahara
- developing countries
- public health medicine
- research ethics
- health care systems
- quantitative research
- cell phone use
Email alerts
Citing articles via.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1460-2237
- Copyright © 2024 The London School of Hygiene and Tropical Medicine and Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- CAREER FEATURE
- 09 May 2023
- Correction 06 June 2023
How scientists are using WhatsApp for research and communication
- Christine Ro 0
Christine Ro is a science writer in London.
You can also search for this author in PubMed Google Scholar
In March, Holly Bik and Virginia Schutte were a few weeks late departing for East Antarctica, where they would collect sea-floor mud to better understand tiny deep-sea invertebrates. The delay was due to a combination of COVID-19 protocols and port congestion.But their time quarantining in a New Zealand hotel as a COVID-19 precaution was productive.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
doi: https://doi.org/10.1038/d41586-023-01575-z
Updates & Corrections
Correction 06 June 2023 : An earlier version of this story erroneously stated that the scoping review Thea de Gruchy was involved in was part of the LGBT+ study. They were separate studies.
Ndashimye, F., Hebie, O. & Tjaden, J. Soc. Sci. Comput. Rev . https://doi.org/10.1177/08944393221111340 (2022).
Article Google Scholar
Manji, K., Hanefeld, J., Vearey, J., Walls, H. & de Gruchy, T. Health Policy Plan. 36 , 774–789 (2021).
Download references
Related Articles

Training: Narrative tools for researchers
Training: Networking for researchers

I’m worried I’ve been contacted by a predatory publisher — how do I find out?
Career Feature 15 MAY 24

How I fled bombed Aleppo to continue my career in science
Career Feature 08 MAY 24

Illuminating ‘the ugly side of science’: fresh incentives for reporting negative results

Neglecting sex and gender in research is a public-health risk
Comment 15 MAY 24
Interpersonal therapy can be an effective tool against the devastating effects of loneliness
Correspondence 14 MAY 24
Inequality is bad — but that doesn’t mean the rich are

Hunger on campus: why US PhD students are fighting over food
Career Feature 03 MAY 24
Faculty Positions& Postdoctoral Research Fellow, School of Optical and Electronic Information, HUST
Job Opportunities: Leading talents, young talents, overseas outstanding young scholars, postdoctoral researchers.
Wuhan, Hubei, China
School of Optical and Electronic Information, Huazhong University of Science and Technology
Postdoc in CRISPR Meta-Analytics and AI for Therapeutic Target Discovery and Priotisation (OT Grant)
APPLICATION CLOSING DATE: 14/06/2024 Human Technopole (HT) is a new interdisciplinary life science research institute created and supported by the...
Human Technopole
Research Associate - Metabolism
Houston, Texas (US)
Baylor College of Medicine (BCM)
Postdoc Fellowships
Train with world-renowned cancer researchers at NIH? Consider joining the Center for Cancer Research (CCR) at the National Cancer Institute
Bethesda, Maryland
NIH National Cancer Institute (NCI)
Faculty Recruitment, Westlake University School of Medicine
Faculty positions are open at four distinct ranks: Assistant Professor, Associate Professor, Full Professor, and Chair Professor.
Hangzhou, Zhejiang, China
Westlake University
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Advertisement
WhatsApp and other messaging apps in medicine: opportunities and risks
- IM-Point of view
- Published: 15 February 2020
- Volume 15 , pages 171–173, ( 2020 )
Cite this article

- Marco Masoni ORCID: orcid.org/0000-0001-5943-8689 1 &
- Maria Renza Guelfi ORCID: orcid.org/0000-0003-0073-5288 1
14k Accesses
40 Citations
10 Altmetric
Explore all metrics
WhatsApp is a popular messaging application frequently used by physicians and healthcare organizations that can improve the continuity of care and facilitate effective health services provision, especially in acute settings. However WhatsApp does not comply with the rules of the European GDPR and the US HIPA Act. So it is inappropriate to share clinical information via WhatsApp.
For this reason alternatives to Whatsapp are considered. In particular, the features that must have secure messaging apps to be in compliance with GDPR and HIPAA and to protect patient data will be discussed. The aim is to encourage healthcare organizations and physicians to abandon WhatsApp and to adopt one of the many secure messaging apps now available, some of them at no cost.
Avoid common mistakes on your manuscript.
WhatsApp: use and regulatory concerns
WhatsApp is an instant messaging application created in 2009 and acquired by the Facebook family of companies in 2014. Mainly used with mobile devices, it also runs on desktop computers. Although asynchronous as e-mail, most users perceive WhatsApp as a synchronous communication tool.
The WhatsApp installation involves the transmission of the contacts list on Facebook Servers and it is possible to select manually the storage of messages. Communication through end-to-end encryption allows the maintainance of data confidentiality because only the sender and the receiver can decipher the message.
Physicians frequently use WhatsApp to communicate with peers. The clinical utility of this communication tool is now emerging, especially in acute settings [ 1 , 2 ]. Other more general benefits are reported: communication improvement and streamline workflows, reduction of phone tags, decreased consultation time, promotion of a collaborative environment to improve the level of healthcare provided to patients [ 3 ].
As far as the European Community is concerned, the use of WhatsApp must comply with the General Data Protection Regulation (GDPR), which came into force in May 2018, a complex set of rules that allows EU citizens greater control over personal data.
The GDPR does not allow the storage of sensitive data of EU citizens on servers located outside the geographic area of the European Community. Furthermore, faced with a request for access to personal data (Subject Access Request—SAR), organizations are obliged to provide information and to correct or delete it. It is therefore mandatory that hospitals and healthcare centers know where and how the data are stored [ 4 ].
The GDPR rules apply to all EU countries without the intervention of national parliaments and they are mainly directed at organizations, which can suffer fines of up to €20 million or 4% of annual turnover. This will encourage hospitals and health organizations to closely monitor their employees so that GDPR rules are respected.
Since the installation of WhatsApp uploads contacts list and storages messages on servers outside the EU area, Facebook is not able to meet the rules of the GDPR and it is therefore inappropriate to share clinical information via WhatsApp [ 5 ].
The same considerations also apply to other apps, such as online calendars, Dropbox and Google Drive, which store data in servers worldwide, making it extremely difficult to comply with the GDPR rules and to respond to SARs.
Obviously, these issues are known by the massive organizations that manage Internet services. WhatsApp has recently tried to tackle the problem by interrupting data sharing for EU users, but has failed to find a longer term solution that allows data sharing in line with the GDPR rules [ 4 ].
With regard to the United States, patients' right to data confidentiality is governed by the Health Insurance Portability and Accoutability Act (HIPAA). According to this law, no communication platform completely complies with its rules as this does not depend on how the software is made, but rather on how it is managed by users [ 6 ].
The lack of access control with an account, other than the one on the device, is the first obstacle to the use of WhatsApp for keeping patient data confidential. Any person who uses a smartphone can read WhatsApp messages and, if the screen is not locked, can see notifications to messages.
The possibility of deleting messages received and the inability of WhatsApp to keep a record of those sent is contrary to the HIPAA rules as it prevents the possibility of any audit. Furthermore, the replacement of the smartphone determines the impossibility to recover the messages, unless they have been backed up. Finally, if the employee leaves the organization, complete deletion of sensitive data is required. This can be complex and it cannot be performed remotely. The best solution would be to delete the account, an action that the user would probably reject [ 6 ].
Given the non compliance of WhatsApp with GDPR and HIPAA, its use puts the physician at risk to make errors in the management of patient data. Some suggestions that can be useful to use WhatsApp in an appropriate way to avoid regulatory investigation for not having taken the necessary steps to keep patient confidentiality are discussed below [ 7 ].
Firstly, when sending a message one of the most important precautions is always to make sure that the recipient is the right person. This is particularly true when there is a long list of contacts and there is no different group between contacts linked to the exercise of the profession and the ones that belongs to family and friends.
Secondly, when communicating it is good practice to avoid entering information that could lead to the recognition of the patient such as his name and surname, an identifier, the date of birth or home location. Sometimes a vague phrase like "the patient with autoimmune disease we saw yesterday morning" may suffice to break this rule. To this it should be added that the attempt to anonymize clinical images acquired via smartphone through editing and clipping, it may not be sufficient for the presence of accompanying metadata such as date, time, geographical coordinates together with the model of the mobile device [ 8 ].
The limitations of WhatsApp force us to explore alternative software that can be used in the healthcare environment.
Alternatives to WhatsApp
One ot the main limit in the development of messaging apps is that, unlike most internet services, there are no standards and Request For Comments that define a set of communication rules that these applications must respect to communicate. This results in a poor ability to share data between different applications.
Similar to Whatsapp, many other messaging apps exist [ 8 ]. Some are linked to Social Networking Sites (for example Facebook Messenger), while others (for example Telegram, and Vibes) are stand alone applications that do not need other software for their operation.
The main problem of these commercial messaging apps is that they are owned by companies whose main aim is to collect data from their users. For this reason it is difficult to imagine a future where these applications can satisfy the requests concerning the processing of personal health data both at european and US level. So WhatsApp, Messenger and Telegram seems only workarounds [ 9 ].
What healthcare systems need are Secure Messagging Apps (SMA) specifically dedicated to keep confidentiality of patient data. Beyond encrypting data within a private communication network, SMA must prevent data being sent outside the healthcare organization’s network. Saving of sensitive data to external hard-drives or outside the organization’s network must be avoided and administrative control must be available, deleting messages if the smartphone is stolen or lost (remote wipe) or after a predetermined period of time [ 10 ].
Siilo is an interesting SMA for the healthcare area. It is GDPR compliant and freely available from Apple and Google Play stores. It can save images, ECGs and other sensitive patient data in an encrypted manner on the personal mobile device, overcoming the restriction of storing information on remote servers. For this and other functionalities, many organizations are adopting Siilo as a tool for communication between employees. Hospify is another free SMA GDPR compliant, available from Apple and Google Play Store.
As far as HIPAA compliant messaging apps are concerned, an interesting Web site that compare features of different software is available at the URL: https://www.g2.com/categories/hipaa-compliant-messaging .
To date SMA are poorly interoperable with EHR systems. This makes difficult the simple transfer of messages containing diagnostic and therapeutic information to the digital medical record. For this reason the communication left in the smartphone remains compartmentalized and in any case cannot be used formally. Some HIPAA compliant SMA come bundled with Clinical Communication and Collaboration Platforms that allow the integration of documents, images and messages with EHR systems [ 8 ]. Examples of this type of platforms are Trillian, SimplePractice, Tiger Connect and OnCall Health. Table 1 summarizes the main features of SMA discussed before.
As we see, many companies and start-ups are involved on implementing SMA, but their adoption among healthcare organizations is still scarce. Despite the uncertainties that accompany the use of WhatsApp, it continues to spread among physicians and healthcare workers [ 6 ]. Perhaps this seems tolerated due to the low occurrence of related adverse events to this date. Convenience seems to overcome mantainance of confidentiality of personal health data [ 9 ].
The use of SMA integrated with EHR could be an important step forward in the management of patient data. Healthcare organizations should implement policies related to the use of mobile devices and communications via messaging apps to be followed by physicians and other professionals. The switch to the use of these types of SMA should not be difficult because they are all user-friendly and work in a way similar to WhatsApp.
Compliance with the legislative provision related to the exchange of sensitive data must be considered equally important compared with the sharing of information that can improve the delivery of effective care. So WhatsApp is not an adequate tool to share clinical information due to its non compliance with the GDPR and HIPAA rules. Consequently healthcare organizations and physicians should abandon WhatsApp moving towards SMA able to keep confidentiality and security of patient data.
Johnston MJ, King D, Arora S, Behar N, Athanasiou T, Sevdalis N, Darzi A (2015) Smartphones let surgeons know WhatsApp: an analysis of communication in emergency surgical teams. Am J Surg 209(1):45–51
Article Google Scholar
Astarcioglu MA, Sen T, Kilit C, Durmus HI, Gozubuyuk G, Kalcik M et al (2015) Time-to reperfusion in STEMI undergoing inter hospital transfer using smartphone and WhatsApp messenger. Am J Emerg Med 33(10):1382–1384
De Benedictis A, Lettieri E, Masella C, Gastaldi L, Macchini G, Santu C et al (2019) WhatsApp in hospital? An empirical investigation of individual and organizational determinants to use. PLoS ONEne 14(1):e0209873
John B (2018) Are you ready for General Data Protection Regulation? BMJ 360:k941
Hawkes N (2018) Sixty seconds on … Whatsapp. BMJ 360:K1041
Calleja-Castillo JM, Gonzalez-Calderon G (2018) WhatsApp in stroke systems: current use and regulatory concerns. Front Neurol 9:388
Mistry K (2018) Information governance considerations for staff on the use of instant messaging software in acute clinical settings. NHS. https://digital.nhs.uk/binaries/content/assets/website-assets/data-and-information/ig-resources/information-governance-considerations-for-individuals-on-the-use-of-instant-messaging-software-in-acute-clinical-settings.pdf. Accessed 20 Jan 2020
Thomas K (2018) Wanted: a WhatsApp alternative for clinicians. BMJ 360:k622
Bergeron D, Iorio-Morin C (2019) In reply to the letter to the editor "other apps beyond WhatsApp". World Neurosurg 130:568
HIPAA Journal. Secure messaging app. https://www.hipaajournal.com/healthcare-messaging-app/. Accessed 20 Jan 2020
Download references
Author information
Authors and affiliations.
Department of Experimental and Clinical Medicine, University of Firenze, Largo Brambilla 3, 50134, Florence, Italy
Marco Masoni & Maria Renza Guelfi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Marco Masoni .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any study with human and animals by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Masoni, M., Guelfi, M.R. WhatsApp and other messaging apps in medicine: opportunities and risks. Intern Emerg Med 15 , 171–173 (2020). https://doi.org/10.1007/s11739-020-02292-5
Download citation
Received : 17 December 2019
Accepted : 03 February 2020
Published : 15 February 2020
Issue Date : March 2020
DOI : https://doi.org/10.1007/s11739-020-02292-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Secure messaging apps
- Data confidentiality
- Find a journal
- Publish with us
- Track your research
- Help & FAQ
Impact of the COVID-19 Pandemic on a Physician Group’s WhatsApp Chat: Qualitative Content Analysis
Research output : Contribution to journal › Article › peer-review
Background: Social media has emerged as an effective means of information sharing and community building among health professionals. The utility of these platforms is likely heightened during times of health system crises and global uncertainty. Studies have demonstrated that physicians’ social media platforms serve to bridge the gap of information between on-the-ground experiences of health care workers and emerging knowledge. Objective: The primary aim of this study was to characterize the use of a physician WhatsApp (WhatsApp LLC) group chat during the early months of the COVID-19 pandemic. Methods: Through the lens of the social network theory, we performed a qualitative content analysis of the posts of a women physician WhatsApp group located in the United Arab Emirates between February 1, 2020, and May 31, 2020, that is, during the initial surge of COVID-19 cases. Results: There were 6101 posts during the study period, which reflected a 2.6-fold increase in platform use when compared with platform use in the year prior. A total of 8 themes and 9 subthemes were described. The top 3 uses of the platform were requests for information (posts: 2818/6101, 46.2%), member support and promotion (posts: 988/6101, 16.2%), and information sharing (posts: 896/6101, 14.7%). A substantial proportion of posts were related to COVID-19 (2653/6101, 43.5%), with the most popular theme being requests for logistical (nonmedical) information. Among posts containing COVID-19–related medical information, it was notable that two-thirds (571/868, 65.8%) of these posts were from public mass media or unverified sources. Conclusions: Health crises can potentiate the use of social media platforms among physicians. This reflects physicians’ tendency to turn to these platforms for information sharing and community building purposes. However, important questions remain regarding the accuracy and credibility of the information shared. Our findings suggest that the training of physicians in social media practices and information dissemination may be needed.
- Communication
- Content analysis
- Information seeking
- Information sharing
- Information-seeking behavior
- Misinformation
- Qualitative
- Social media
ASJC Scopus subject areas
- Medicine (miscellaneous)
- Health Informatics
Access to Document
- 10.2196/31791
Other files and links
- Link to publication in Scopus
- Link to the citations in Scopus
Fingerprint
- Social Media Medicine & Life Sciences 92%
- Information Dissemination Medicine & Life Sciences 88%
- Physicians Medicine & Life Sciences 59%
- Health Medicine & Life Sciences 27%
- United Arab Emirates Medicine & Life Sciences 26%
- Social Theory Medicine & Life Sciences 24%
- Mass Media Medicine & Life Sciences 24%
- Social Networking Medicine & Life Sciences 21%
T1 - Impact of the COVID-19 Pandemic on a Physician Group’s WhatsApp Chat
T2 - Qualitative Content Analysis
AU - Abdel-Razig, Sawsan
AU - Anglade, Pascale
AU - Ibrahim, Halah
N1 - Publisher Copyright: © Sawsan Abdel-Razig, Pascale Anglade, Halah Ibrahim.
PY - 2021/12
Y1 - 2021/12
N2 - Background: Social media has emerged as an effective means of information sharing and community building among health professionals. The utility of these platforms is likely heightened during times of health system crises and global uncertainty. Studies have demonstrated that physicians’ social media platforms serve to bridge the gap of information between on-the-ground experiences of health care workers and emerging knowledge. Objective: The primary aim of this study was to characterize the use of a physician WhatsApp (WhatsApp LLC) group chat during the early months of the COVID-19 pandemic. Methods: Through the lens of the social network theory, we performed a qualitative content analysis of the posts of a women physician WhatsApp group located in the United Arab Emirates between February 1, 2020, and May 31, 2020, that is, during the initial surge of COVID-19 cases. Results: There were 6101 posts during the study period, which reflected a 2.6-fold increase in platform use when compared with platform use in the year prior. A total of 8 themes and 9 subthemes were described. The top 3 uses of the platform were requests for information (posts: 2818/6101, 46.2%), member support and promotion (posts: 988/6101, 16.2%), and information sharing (posts: 896/6101, 14.7%). A substantial proportion of posts were related to COVID-19 (2653/6101, 43.5%), with the most popular theme being requests for logistical (nonmedical) information. Among posts containing COVID-19–related medical information, it was notable that two-thirds (571/868, 65.8%) of these posts were from public mass media or unverified sources. Conclusions: Health crises can potentiate the use of social media platforms among physicians. This reflects physicians’ tendency to turn to these platforms for information sharing and community building purposes. However, important questions remain regarding the accuracy and credibility of the information shared. Our findings suggest that the training of physicians in social media practices and information dissemination may be needed.
AB - Background: Social media has emerged as an effective means of information sharing and community building among health professionals. The utility of these platforms is likely heightened during times of health system crises and global uncertainty. Studies have demonstrated that physicians’ social media platforms serve to bridge the gap of information between on-the-ground experiences of health care workers and emerging knowledge. Objective: The primary aim of this study was to characterize the use of a physician WhatsApp (WhatsApp LLC) group chat during the early months of the COVID-19 pandemic. Methods: Through the lens of the social network theory, we performed a qualitative content analysis of the posts of a women physician WhatsApp group located in the United Arab Emirates between February 1, 2020, and May 31, 2020, that is, during the initial surge of COVID-19 cases. Results: There were 6101 posts during the study period, which reflected a 2.6-fold increase in platform use when compared with platform use in the year prior. A total of 8 themes and 9 subthemes were described. The top 3 uses of the platform were requests for information (posts: 2818/6101, 46.2%), member support and promotion (posts: 988/6101, 16.2%), and information sharing (posts: 896/6101, 14.7%). A substantial proportion of posts were related to COVID-19 (2653/6101, 43.5%), with the most popular theme being requests for logistical (nonmedical) information. Among posts containing COVID-19–related medical information, it was notable that two-thirds (571/868, 65.8%) of these posts were from public mass media or unverified sources. Conclusions: Health crises can potentiate the use of social media platforms among physicians. This reflects physicians’ tendency to turn to these platforms for information sharing and community building purposes. However, important questions remain regarding the accuracy and credibility of the information shared. Our findings suggest that the training of physicians in social media practices and information dissemination may be needed.
KW - COVID-19
KW - Communication
KW - Community
KW - Content analysis
KW - Information seeking
KW - Information sharing
KW - Information-seeking behavior
KW - Misinformation
KW - Pandemic
KW - Physician
KW - Qualitative
KW - Social media
KW - WhatsApp
UR - http://www.scopus.com/inward/record.url?scp=85122029121&partnerID=8YFLogxK
UR - http://www.scopus.com/inward/citedby.url?scp=85122029121&partnerID=8YFLogxK
U2 - 10.2196/31791
DO - 10.2196/31791
M3 - Article
AN - SCOPUS:85122029121
SN - 2561-326X
JO - JMIR Formative Research
JF - JMIR Formative Research
M1 - e31791
WhatsApp in Clinical Practice-The Challenges of Record Keeping and Storage. A Scoping Review
Affiliations.
- 1 Department of TeleHealth, School of Nursing & Public Health, College of Health Sciences, University of KwaZulu-Natal, Durban 4041, South Africa.
- 2 Department of Community Health Sciences, Cumming School of Medicine, University of Calgary, Calgary, AB T2N 4N1, Canada.
- 3 Flinders Digital Health Research Centre, College of Nursing & Health Sciences, Flinders University, 5042 Tonsley, Australia.
- PMID: 34949033
- PMCID: PMC8708459
- DOI: 10.3390/ijerph182413426
The use of WhatsApp in health care has increased, especially since the COVID-19 pandemic, but there is a need to safeguard electronic patient information when incorporating it into a medical record, be it electronic or paper based. The aim of this study was to review the literature on how clinicians who use WhatsApp in clinical practice keep medical records of the content of WhatsApp messages and how they store WhatsApp messages and/or attachments. A scoping review of nine databases sought evidence of record keeping or data storage related to use of WhatsApp in clinical practice up to 31 December 2020. Sixteen of 346 papers met study criteria. Most clinicians were aware that they must comply with statutory reporting requirements in keeping medical records of all electronic communications. However, this study showed a general lack of awareness or concern about flaunting existing privacy and security legislation. No clear mechanisms for record keeping or data storage of WhatsApp content were provided. In the absence of clear guidelines, problematic practices and workarounds have been created, increasing legal, regulatory and ethical concerns. There is a need to raise awareness of the problems clinicians face in meeting these obligations and to urgently provide viable guidance.
Keywords: WhatsApp; data storage; medical records; record keeping.
Publication types
- Research Support, N.I.H., Extramural
- Information Storage and Retrieval
Grants and funding
- D43TW007004-13/Fogarty International Centre for the National Institutes of Health
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
A survey on the effectiveness of WhatsApp for teaching doctors preparing for a licensing exam
Roles Conceptualization, Data curation, Formal analysis, Methodology, Resources, Software, Supervision, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Faculty of Clinical Sciences, Obafemi Awolowo College of Health Sciences, Olabisi Onabanjo University, Sagamu, Ogun State, Nigeria
Roles Conceptualization, Data curation, Formal analysis, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing
Roles Data curation, Formal analysis, Investigation, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing
Affiliation Science and Technology Policy Fellow, American Association for the Advancement of Science, Washington, D.C., United States of America
- Bankole K. Oyewole,
- Victor J. Animasahun,
- Helena J. Chapman

- Published: April 2, 2020
- https://doi.org/10.1371/journal.pone.0231148
- Reader Comments
Introduction
The use of WhatsApp for health professional education is not novel and is described increasingly in literature as an affordable, familiar, and convenient tool for collaboration. Social media technologies for health practitioner education allow the use of text and audio-visual aids, peer-to-peer based learning, and problem-based learning. This study presents a survey on the effectiveness of WhatsApp in doctors’ preparation for a medical licensing exam.
A cross-sectional study was conducted among one hundred and ninety-four participants of a WhatsApp group preparing for the PLAB exam over a three-month period. A twenty-item questionnaire designed on Google Form was completed by consenting participants on the publication of exam results.
WhatsApp can be an effective tool for health professional education, using a pre-defined curriculum coupled with organizational structure. This study reported both subjective and objective measures of effectiveness and demonstrated that the use of multiple e-learning resources can lead to improved learning outcomes.
Citation: Oyewole BK, Animasahun VJ, Chapman HJ (2020) A survey on the effectiveness of WhatsApp for teaching doctors preparing for a licensing exam. PLoS ONE 15(4): e0231148. https://doi.org/10.1371/journal.pone.0231148
Editor: Elisa J. F. Houwink, Leiden University Medical Center, NETHERLANDS
Received: September 30, 2019; Accepted: March 17, 2020; Published: April 2, 2020
Copyright: © 2020 Oyewole et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
The frequency and utility of real-time social media tools (e.g., smartphone apps) in classroom and community settings has been a fundamental addition to medical education.[ 1 ] With an increase in the use of innovative technology for learning, these tools have been instrumental in providing medical students with the timely access to clinical information, such as laboratory values or pharmaceutical side effects.[ 2 ]Medical students have incorporated social media platforms (e.g., YouTube, Facebook, WhatsApp) in their e-learning, using online question banks and study aids to supplement their academic learning.[ 3 ] The evaluation of these social media tools and platforms in medical students’ preparation of formal standardized examinations (e.g., national medical board certifications) may highlight an overlooked benefit in the learning process.
WhatsApp is a free social media platform based on mobile instant messaging (MIM) that facilitates the creation of groups of participants and sharing of text messages, multimedia files, and other documents. The use of WhatsApp for health professional education is not novel and has been described in preparation of a psychiatry membership exam, academic courses in histology and ophthalmology, and primary health education activities. Social media technologies allow the use of text and audio-visual aids, peer-to-peer based learning, and problem-based learning. They provide a platform that stimulates interaction, collaboration and participation through the sharing ideas and experience, this has led participants to report positive outcomes in the use of WhatsApp as a learning aid.[ 4 – 7 ]
The Professional and Linguistics Assessments Board examination (PLAB), organised by the General Medical Council (GMC), is the test that international medical graduates (IMGs) complete to be considered for registration to the United Kingdom’s medical register and subsequently be granted a general license to practise. The examination consists of two parts. The first part is a multiple-choice question (MCQ) consisting of 180 questions, while the second part is an objectively-structured clinical examination (OSCE) made up of eighteen scenarios.[ 8 ] In 2018, 7,559 candidates completed the PLAB 1 examination in over twenty centres across the world.[ 9 ] This represented an increase of over two thousand candidates writing the exam, when compared to the previous year. Notably, unlike the United States Medical Licensing Exam (USMLE), the GMC does not offer exam preparation courses to medical graduates.
In September 2016, a WhatsApp group named “PLAB Network” was created as a forum, where doctors preparing for their PLAB 1 examination could discuss, exchange ideas, and share relevant practise materials, experience, and knowledge. Participants were added to the group based on recommendations from previous or current members and an eligible passing score on the International English Language Testing System (IELTS). This study aimed to assess the effectiveness of WhatsApp social media technology in preparing physicians to obtain a passing score on the medical licencing exam. The secondary study objective was to identify factors that were associated with physicians obtaining a passing exam score.
Methodology
Study design.
In this cross-sectional study, a twenty-item survey was administered to one hundred and ninety-four participants WhatsApp group participants during a two-week period (April 27 to May 11, 2019). Inclusion criteria are those WhatsApp participants who completed the PLAB 1 on March 14, 2019. Exclusion criteria being participation in the group for less than the two weeks.
Description of the WhatsApp platform
This gratuitous WhatsApp platform serves as a biannual forum, with an average of two hundred and forty participants and ten moderators, where questions are discussed and answered using approved references. Forum sessions are dedicated to specific clinical subjects (e.g., electrocardiogram interpretation, neurology, medical ethics) and other general topics (e.g., academic and clinical learning gaps). Due to limitations of this social media platform, only two hundred and fifty-six participants can join one WhatsApp group.
Sessions started approximately three months prior to the PLAB 1 examination date, initially lasting one hour daily and then increased to three hours daily during weekdays, between the hours of 20:00 and 23:00. Using a compiled question bank, practice questions were discussed using a problem-solving approach, with participation of a facilitator and two moderators. Moderators were unpaid volunteers who have been previous participants of the group that have shown a keen interest in teaching and had a passing score of the PLAB 1 examination. This platform allowed the sharing of references from GMC approved websites, images that helped to explain anatomical or clinical scenarios were also shared and discussed, website links to relevant guidelines and information like that of the National Institute for Health and Care Excellence (NICE) were attached to relevant explanations, PowerPoint presentations developed by moderators on topics like interpretation of electrocardiograms and ethics were provided to participants and participants were also sign posted to relevant book chapters and paragraphs that contained detailed information on scenarios. These facilitated collective discussion. After-hours posts were reviewed, and queries were answered the following weekday.
Dataset description and questionnaire design
The questionnaire was designed on the virtual Google Form, consisting of twenty questions with fourteen mandatory questions necessary for submitting the form. There were three sections: demography, exam preparation, and perception of group effectiveness. The demography section contained five questions which covered participant biodata and level of training, the section on exam preparation contained five questions assessing participants score, study materials and duration of preparation while the section on perception of group effectiveness contained ten questions assessing respondent’s perception of group organization, motivation to learn, level of intrusiveness and recommendations.
Authors BKO and VJA independently conducted comprehensive literature reviews to identify germane questions that assessed effectiveness of social media in medical education and agreed upon a final list of items included in the survey questions which was then pretested and finalized, these ensured the validity and reliability of the questionnaire. No personal information data (e.g., names, email) were collected.
Data analysis
Data on group participants was downloaded from Google Forms into Microsoft Excel and subsequently coded and transferred into the IBM Statistical Package for Social Sciences (SPSS) version 25. Data on global statistics on average pass marks and rate was extracted from the GMC website. Descriptive statistics were calculated in form of frequencies, percentages, means, and standard deviation. Inferential statistics were calculated, and the level of significance was set at 5 percent. Independent sample t-test was used to calculate the mean difference of variables. Chi-square test and Fisher’s exact test were used to determine associations between categorical variables.
Ethical considerations
The authors performed the study independently, outside of their current institutional affiliations. However, ethical standards were maintained following the applicable principles of the World Medical Association Declaration of Helsinki.[ 10 ] Informed consent was obtained by study participants, and data were anonymised. Data collection complied with WhatsApp–s terms and conditions.
General characteristics of the respondents
PLAB result of participants in the PLAB network

Factors associated with passing the PLAB exam
Of those respondents, the mean age of those who passed the PLAB exam was lower than those who did not pass the exam (30.3±4.4 vs 33.2±5.8 years) (t = 2.16; p = 0.03). Other factors had no significant association with passing the PLAB exam, including mean duration of preparation in months (t = -0.41; p = 0.68), average study hours per day (t = -0.71; p = 0.48), and number of years post-graduation (X 2 = 3.314; p = 0.19).
Passing the PLAB exam was significantly associated with using the following as the main study resource: Plabable (an online question bank) (p = 0.009) and combining PLAB network with Plabable (p = 0.001). Passing the PLAB exam was not significantly associated with using the following as main study resource: PLAB network (p = 0.23); 1700 questions (p = 0.77); pass medicine (p = 1.00); others (e.g. textbooks, internet resources, telegram groups, lecture notes (p = 1.00); combining PLAB network with 1700 questions (p = 0.42); combining PLAB network with pass medicine (an online question bank) (p = 0.33); and combining PLAB network with other resources (p = 0.19) ( Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0231148.t001
Participants’ perceptions about the PLAB network learning platform
Of the respondents, 83.3 percent reported that the platform increased their motivation to learn, 80.7 percent believed that the platform encouraged collaborative learning and participation, and 93.8 percent stated that moderators were knowledgeable. Over two-thirds (68.4 percent) mentioned that they preferred learning through this WhatsApp platform, and 72.8 percent felt that the sessions were organised and easy-to-follow. However, about half (50.9 percent) felt the level of irrelevant messages were either low or very low, 27.2 percent felt it was average, and 22 percent) felt that it was high or very high. ( Table 2 ). A total of 97.4 percent of participants said that they would recommend the PLAB network to any colleague who planned to prepare for an upcoming PLAB exam.
https://doi.org/10.1371/journal.pone.0231148.t002
WhatsApp is believed to be one of the most preferred mobile messaging applications for interaction, communication, and learning.[ 11 ] Our study uniquely assessed both qualitative and quantitative measures of effectiveness in the use of WhatsApp in healthcare professional education. The gender distribution (57.9 percent male, 42.1 percent female) was similar to that (58.4 percent male, 41.6 percent female) of IMGs writing the United States Medical Licensing Examination (USMLE) exam and that that (54 percent male, 46 percent female) of all doctors registered with the GMC.[ 12 , 13 ] The mean age (30.6 years) of respondents was also similar that (30.8 years) of IMGs taking the USMLE exam.[ 12 ]
The mean score of participants of the WhatsApp teaching in our study was higher than the general GMC average, and the majority (88.6 percent) passed the exam. There is evidence that these interactive, web chat-based social media platforms can improve learning experience and enhance knowledge acquisition, which was exemplified by neurology case-based discussions and problem-based learning among medical students in Nigeria and the United Kingdom.[ 14 , 15 ] However, one study among medical students in India reported no significant difference in knowledge among respondents when WhatsApp learning was compared with didactic lectures.[ 16 ] Notably, in this study, combining the WhatsApp learning with an independent online resource (Plabable) was most beneficial for passing the PLAB exam, rather than using the PLAB network WhatsApp learning platform as the only study resource. This was similar to findings of a quasi-experimental study design among selected secondary school teenagers, where a significant increase in post-intervention scores was observed with teenagers who had supplementary learning on WhatsApp coupled with traditional classroom learning, versus only received classroom lessons.[ 11 ] Hence, this suggests that the WhatsApp teaching coupled with secondary learning strategies have the potential to enhance an individual’s success on standard exams like PLAB exam.
Respondents’ perceived level of intrusive messages during WhatsApp teaching sessions was higher than previous studies.[ 14 , 15 ] This might reflect the peer-led nature of our study, as opposed to other studies where professional hierarchy might help ensure decorum. Although posting of irrelevant messages is a known disadvantage of WhatsApp learning platforms,[ 7 ] we believe that by setting clear ground rules and giving warnings or sanctions may maximize focus and productivity.
With increased interest in the use of WhatsApp in medical education, more than seventy-five percent of articles on this topic have been published in the last three years.[ 17 ] This reflects both the popularity of the use of convenient mobile platforms like WhatsApp for medical education among healthcare professionals and also the need for data on their effectiveness among researchers.[ 11 , 17 ]
Since its creation in 2016, the PLAB Network has remained popular WhatsApp platform among doctors writing the PLAB exam. Based on participants’ recommendations, the group has reached maximum capacity for its three-monthly biannual sessions over the last three years. An average of more than seven hundred and fifty doctors have participated in the group over this period. Participants reported positive feedback, agreeing that it fosters collaborative learning as a hub for sharing relevant study resources. The group–s effectiveness was demonstrated via a positive perception from participants and observation of higher pass rates.
This study has several limitations. First, nonresponse bias may have resulted, since participants who achieved passing or failing scores may have varying perspectives of the effectivity of the WhatsApp platform. Second, the variability of their participation, whether for partial or complete duration, may have affected their perception of the effectiveness. Third, due to the homogenous study population, cultural differences could not be explored in this study, limiting the generalization of study findings to other population groups.
Finally, teaching methods via each WhatsApp group may vary and influence the effectiveness as a teaching tool. However, a pre-defined curriculum coupled with organizational structure can harness social media technologies for medical education.
The study examined the use of social media technology among medical graduates as they prepared for a medical licensing examination. Studies among other population groups have reported positive or non-significant outcomes, which highlights the need for further research in social media applications related to medical education.
Social media technologies like WhatsApp are a convenient way for healthcare practitioners to collaboratively prepare and acquire essential information and resources to pass licensing examinations. This study reported both positive quantitative and qualitative measures of effectiveness related to the WhatsApp tool. Study findings demonstrated that the use of multiple e-learning resources, including social media technology, may lead to improvement in learning outcomes.
Supporting information
https://doi.org/10.1371/journal.pone.0231148.s001
- View Article
- Google Scholar
- PubMed/NCBI
- 8. General Medical Council. A guide to the PLAB test. https://www.gmc-uk.org/registration-and-licensing/join-the-register/plab/a-guide-to-the-plab-test . 2019 [cited 19 May 2019].
- 9. General Medical Council. Recent pass rates for PLAB 1 and PLAB 2. https://www.gmc-uk.org/registration-and-licensing/join-the-register/plab/recent-pass-rates-for-plab-1-and-plab-2 . 2019 [cited 19 May 2019].
- 13. General Medical Council. Data explorer. https://data.gmc-uk.org/gmcdata/home/#/reports/The%20Register/Stats/report . 2019 [cited 16 July 2019].
Best WhatsApp Medical Groups
- Reading time: 2 minutes, 59 seconds
- Revised on: 2020-09-07
From our own research, we have come up with the Best Whatsapp Medical Groups that once you join guarantee you high yield information and discussion.
Just click on the links below and choose an appropriate best WhatsApp medical group to join.
Medical and postgraduate group https://chat.whatsapp.com/JzIJGV6W28FICJTvlxwD6j
Medical and PG group https://chat.whatsapp.com/BS2jM3lBAp43irJp2VAHfp
M. B. B. S. Medicine 🔬💊: https://chat.whatsapp.com/invite/BV6nVlcVQ0m37v6BWnSk9V MEDICINE ONLY: https://chat.whatsapp.com/invite/D631BBqbX2P8G9Sw2GCyr8
Medical exams preparation: https://chat.whatsapp.com/invite/7frlHoeM9N42OQufPonIyL Pharmacist: https://chat.whatsapp.com/invite/0qUFf7kLtGqB9L9YLJ9inH
Medical group.🏥: https://chat.whatsapp.com/invite/4l6YddcYRO99u0drLdQCPG Medicos Aspirants: https://chat.whatsapp.com/invite/5Q3myUwa5Nq1BWScKOLfX0 Medical Group⛑️⛑️👔: https://chat.whatsapp.com/invite/BeFHCNyUfILE8RratAi81o MEDICAL 💊GROUP https://chat.whatsapp.com/invite/8UHLCZTKOXGBUDGHZe6P7p MEDICS ARENA: https://chat.whatsapp.com/invite/6Z8beirmVpkI0IpwM779kd
Medicine; Discussion Group: https://chat.whatsapp.com/invite/DpI1NjKsyNOCCQA8jUsSsC Medical group: https://chat.whatsapp.com/invite/7jVzvkLz2gEGiqbNONpS10 Medical Case Consult Members: https://chat.whatsapp.com/invite/Hb218XO77XSG4ofSqalf4E
Study of medicine: https://chat.whatsapp.com/invite/HbuuGyNDzijJZjkjEGoEAq Medical group: https://chat.whatsapp.com/invite/HbuuGyNDzijJZjkjEGoEAq
Medical Cases & Updates : https://chat.whatsapp.com/invite/0e04UOqDE4j4eWcLaxRP1d Biomedical ebook GROUP: https://chat.whatsapp.com/invite/DxVMAAi5WZ1JcATXha0jO3
International Mbbs studies: https://chat.whatsapp.com/invite/6Tl1L0wYprpFPyEmFfSiOQ Health Professionals 🎓🎓: https://chat.whatsapp.com/invite/CWScPb5EGWFAKYZ7mx3zuQ Dr. Knowledge & IQ Test: https://chat.whatsapp.com/invite/CuHqzi0WmXnHYfYIMJCkkL
NEET UG 2019 Toppers' Grp: https://chat.whatsapp.com/invite/FNXvKmROJPj12uXKcgblNg
Consultant Case DiscussiOn: https://chat.whatsapp.com/invite/EGOtwnviAulEpFuQGaUloU MCAT Quiz Qstns: https://chat.whatsapp.com/invite/Go6JPBJawcP90VSrrZWt9D Medical seat: https://chat.whatsapp.com/invite/5HDtMA5QywT4jVH9kRqS8b Exam ideas: https://chat.whatsapp.com/invite/HEk3oUItJXt3Y3PP5cspNp
Doctor's gang: https://chat.whatsapp.com/invite/D0O2lH7iiJb2y2IduGOfNp Human science: https://chat.whatsapp.com/invite/41vDozWN7eLACaEd2sokUb Education Hub: https://chat.whatsapp.com/invite/BfNq8PFDFZUBO6AgtkckkL Human bioscience: https://chat.whatsapp.com/invite/41vDozWN7eLACaEd2sokUb
Medicine rx : https://chat.whatsapp.com/invite/KjTQgEH4wb43nl0OqVMcPR Medical discussions (MCQ): https://chat.whatsapp.com/invite/KFNuXWDHLmJHvMnsg8sz91
Medical Science Group: https://chat.whatsapp.com/invite/6K46S5t0SKULxSuIqn0qrM Medical Group: https://chat.whatsapp.com/invite/LOe5eRt1H0E7IPquoMXh2O
EXTRA KNOWLEDGE📚: https://chat.whatsapp.com/invite/6c6PKu3rYjh4SMJbSr9fGT DoctorBasti: https://chat.whatsapp.com/invite/JiIpQd5AdSY1m9GUxVDE9N Medical World: https://chat.whatsapp.com/invite/A9XgPtwgQFCL8rJq9asTY2 Nielit CCC tests https://chat.whatsapp.com/invite/8VRHnvgbLWhFmBDz1psQMz
Bio, physics & chemistry📔📕: https://chat.whatsapp.com/invite/C5IXKmTJLc7L4Hc9LeOdo4 Education Hub: https://chat.whatsapp.com/invite/BfNq8PFDFZUBO6AgtkckkL World of Biology: https://chat.whatsapp.com/invite/F9POOMYq6gG6VuwWSvZNfI BIOLOGY LOVERS: https://chat.whatsapp.com/invite/27YIfgwdUoJ99z39EL5Tjk
Biology Study Group🌲: https://chat.whatsapp.com/invite/HX1cIYOhSpS6OZfuX6dXo7 BSc students: https://chat.whatsapp.com/invite/HovD7ulfksL97G071WN9m4 Study MBBS ABROAD: https://chat.whatsapp.com/invite/AClY2VB7LOTA3hq4DgQosm
We hope that this list will be of importance to you and your studies. You can promote it by sharing with your friends who may be needing to join the best whatsapp medical groups
Article Details
- 0.50 Points
About The Author

Admin Ogera
Most popular posts.

Slide Presentations

Join WhatsApp Group For Medical Students; Preclinical and Clinical
- Medical School
- September 3, 2022
It can be difficult to find a study group or other people with the same interests as you for your medical school discussions.
Facebook and other social media platforms are great ways of making connections.
But if you want a more intimate setting that helps you discuss topics that will help you scale through your medical exams and your medical career as a whole, then WhatsApp Groups for medical students are the perfect solution.
There are medical student Whatsapp group links that actually study groups you can join to connect with other medical students.
We have created WhatsApp groups for medical students, each for different stages in the life of a medical student . The following is the list of available Medical Student WhatsApp Group Links We have created
- Medarchive pre-clinical Whatsapp Group [Join Now ]
- Medarchive Clinical WhatsApp Group [ Join Now ]
- M-ECOMM Advertising WhatsApp Group [ JOIN NOW ]
Table of Contents
Other ground rules for security and privacy:, subjects of discussion include:, benefits of joining and participation, subjects of discussion include:, benefits of joining and participation, topics of discussion include:, benefits of joining, medarchive editorial whatsapp group, m-ecomm advertising whatsapp group, final words, general rules for each whatsapp group for medical students.
- These WhatsApp groups are only for medical students from medical schools all over the world and doctors. Non medics are not allowed to join.
- The language of communication is English only.
- The group is open for medical students all over the world.
- Active participation is mandatory.
- Inactivity could be as a result of any of the following;
- Not contributing questions, clinical cases and scenarios for review.
- Not taking part in providing solutions to questions and clinical cases.
- Posting of unrelated and non-medical contents or contents that will not benefit the community is not allowed.
- You will be removed from the groups after 1 month of inactivity to help create room for other active medical students.
- The group admins will be selected based on merit on a rotational fashion and judged by the most active members of the group monitored over a given period of time.
- The fact that messaging is open for all should not be abused. Only drop messages when necessary.
- No one likes being distracted or spammed by random persons messaging on a group.
- The groups are no-spam zones….they are strictly for serious medical business.
- Limit your interaction with people you don’t know on the group…there are fraudsters and scammers everywhere.
- You are mandated to help us keep the groups safe by informing any of the admins of suspicious or malicious activities from other users in the group like unsolicited private messaging, and attempts to fraud.
- We will never message you privately, send an email to request for money, payment for any premium service, financial support/assistance or any of such. If you receive any of such messages, kindly report it to the Admins.
- Again! You are expected to be fully active. Otherwise why are you joining?
- Defaulters will be banned permanently from all the groups.
We hope these medical students’ WhatsApp groups change everything for you in the positive direction as it has for so many before you.
How To Join The Various WhatsApp Groups For Medical Students
In the sections below, you will find details about each of the groups and the respective medical students’ WhatsApp group links to join each of them.
NB: Each of the WhatsApp Groups is strictly for medical students or doctors who fall under each of the categories; either premedical or medical WhatsApp Groups.
1. Preclinical Medical Student WhatsApp Group Link
The preclinical medical student WhatsApp Group is strictly for medical students who are yet to enter the clinical classes.
- Human Anatomy
- Human Physiology
- Human Biochemistry
- Medical Psychology
- Unlimited access to questions from the respective topics of discussion
- Free access to study materials from the subjects
- Access to routine quizzes from the various subjects
- Participate in quiz competitions in your region and win prizes
- Freedom to interact freely with other medical students and build meaningful connections from all over the world.
- Chances of publishing your contents, research and works on this magazine.
2. Clinical Medical Student WhatsApp Group Link
The clinical medical student Whatsapp group link is only for medical students who are currently in the clinical years of medical school and/or doctors who are interested in contributing positively to the community.
- Pharmacology
- Obstetrics and Gyneacology
- Medicine including Internal Medicine
- Constant access to questions, clinical reviews, and discussions from the respective topics of discussion
- Unlimited access to study materials from the subjects of discussion
Premium WhatsApp Group For Medical Students And Graduates

This is a special update WhatsApp group for medical students that can only be accessed via paid yearly subscriptions .
- Career opportunities for International medical school graduates
- Medical council of Canada
- Australian Medical Council
- Other Promising International Opportunities for medical school graduates
- Updates on IELTS for English speaking countries and more!
Constant information of the various career opportunities for medical graduates both in medical practice, business, and other skills of cross-sectional relevance.
Updates on the various medical licensing exams in the major countries of the world.
Access to available study materials for each of the medical licensing exams
Connect with other medical graduates all over the world who share similar interest
Link To Join This Group Is Coming Soon
Other WhatsApp groups by Medarchive you may want to join
Are you a medical student with some experience in affairs related to medical school? Are you looking for a friendly community where you can freely express yourself through writing? You can be part of our Editorial community where you can cultivate your writing skills and at the same time share your experience with other medical students who read our blog. You can do this by simply being part of our community on Whatsapp. You also have the privilege of getting published in Medarchive Magazine and your content featured on the front page of our blog if your content meets our guidelines for content publication . You can check the guideline here . Follow the link on the button below to join our Medarchive Editorial WhatsApp Group.
Are you looking for a friendly ecosystem on WhatsApp where you can promote your legitimate hustle and online businesses? The M-ECOMM free advertising group is a solution created by Medarchive Magazine to fulfill your advertising needs. To start promoting your business today, quickly join the WhatsApp group by clicking the button below. ( Make sure you read the group description for the rules and regulations of the group to avoid getting kicked out without warning ).
All the above WhatsApp groups were designed specifically to meet the various needs of medical students and medical graduates all over the world.
In as much as we try to keep these WhatsApp groups for medical students active and secure for all members, we also enjoin you to help us keep it safe by being careful and reporting suspicious activities to the admins.
Our goal is to build a community for enlightenment and growth for both medical students and medical graduates from all over the world on WhatsApp.
If you are inspired by this dream, you can share this post with your friends using any of the sharing options below.
We hope these groups help you be a better doctor!
You May Also Like:
- Medarchive TV: Biggest Medical WhatsApp TV In Nigeria
- Join Medical Discussion Forum on Discord
Medical Education Website created to enlighten, inform and inspire!
Leave a Reply Cancel Reply
Your email address will not be published. Required fields are marked *
Add Comment *
Save my name, email, and website in this browser for the next time I comment.
Post Comment
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Related Posts

15 Best Study Podcasts for Medical Students on Spotify
- November 22, 2023

10 Best Medical Billing and Coding Schools (Online and On Campus)
- July 8, 2023

Best Desk for Medical School [Top 5 Reviewed]
- July 6, 2023

Scientific Career of Dr. Tatiana Domratcheva

Tatiana Domratcheva
- November 2000: PhD in Physical Chemistry, M.V. Lomonosov Moscow State University, Chemistry Department, Moscow, Russia
- June 1995: Diploma in Chemistry, Mari State University, Faculty of Biology and Chemistry, Yoshkar-Ola, Russia
Professional Career
- 2001 - 2004: Max Planck Institute for Molecular Physiology, Dortmund, Germany. Postdoc in the Department of Prof. R. Goody. Research focused on computational studies of phosphoryl-transfer reactions and modelling of kinase inhibitors
- 2004 - 2009: Max Planck Institute for Medical Research, Germany. Research Associate (Wissenschaftliche Mitarbeiter), Department of Biomolecular Mechanisms (Prof. Ilme Schlichting). Research focused on computational studies of blue-light activated proteins
- 2009 - 2016: Max Planck Institute for Medical Research, Germany. Minerva research group in the Department of Biomolecular Mechanisms (Prof. Ilme Schlichting). Research focused on method development for computational studies of flavin-containing photosensory proteins
- 2016 - present: Max Planck Institute for Medical Research, Germany. Independent group leader position funded by the Department of Biomolecular Mechanisms (Prof. Ilme Schlichting). Research focused on computational studies of photosensory and fluorescent biomolecules.
Awards and Elected Memberships
- 2009 - 2016: W2 professor position awarded by the Minerva Program of the Max Planck Society
- 2015 - 2017: Visiting professor of the Nagoya Institute of Technology (NIT) supported by the NIT Unit Invitation program, http://frontier.web.nitech.ac.jp/en/archives/faculty/tatiana-domratcheva-assoc-prof.
- Open access
- Published: 14 May 2024
Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study
- Jocelyn Schroeder 1 ,
- Barbara Pesut 1 , 2 ,
- Lise Olsen 2 ,
- Nelly D. Oelke 2 &
- Helen Sharp 2
BMC Nursing volume 23 , Article number: 326 ( 2024 ) Cite this article
31 Accesses
Metrics details
Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Canada’s legislation is the first to permit Nurse Practitioners (NP) to serve as independent MAiD assessors and providers. Registered Nurses’ (RN) also have important roles in MAiD that include MAiD care coordination; client and family teaching and support, MAiD procedural quality; healthcare provider and public education; and bereavement care for family. Nurses have a right under the law to conscientious objection to participating in MAiD. Therefore, it is essential to prepare nurses in their entry-level education for the practice implications and moral complexities inherent in this practice. Knowing what nursing students think about MAiD is a critical first step. Therefore, the purpose of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context.
The design was a mixed-method, modified e-Delphi method that entailed item generation from the literature, item refinement through a 2 round survey of an expert faculty panel, and item validation through a cognitive focus group interview with nursing students. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
During phase 1, a 56-item survey was developed from existing literature that included demographic items and items designed to measure experience with death and dying (including MAiD), education and preparation, attitudes and beliefs, influences on those beliefs, and anticipated future involvement. During phase 2, an expert faculty panel reviewed, modified, and prioritized the items yielding 51 items. During phase 3, a sample of nursing students further evaluated and modified the language in the survey to aid readability and comprehension. The final survey consists of 45 items including 4 case studies.
Systematic evaluation of knowledge-to-date coupled with stakeholder perspectives supports robust survey design. This study yielded a survey to assess nursing students’ attitudes toward MAiD in a Canadian context.
The survey is appropriate for use in education and research to measure knowledge and attitudes about MAiD among nurse trainees and can be a helpful step in preparing nursing students for entry-level practice.
Peer Review reports
Medical Assistance in Dying (MAiD) is permitted under an amendment to Canada’s Criminal Code which was passed in 2016 [ 1 ]. MAiD is defined in the legislation as both self-administered and clinician-administered medication for the purpose of causing death. In the 2016 Bill C-14 legislation one of the eligibility criteria was that an applicant for MAiD must have a reasonably foreseeable natural death although this term was not defined. It was left to the clinical judgement of MAiD assessors and providers to determine the time frame that constitutes reasonably foreseeable [ 2 ]. However, in 2021 under Bill C-7, the eligibility criteria for MAiD were changed to allow individuals with irreversible medical conditions, declining health, and suffering, but whose natural death was not reasonably foreseeable, to receive MAiD [ 3 ]. This population of MAiD applicants are referred to as Track 2 MAiD (those whose natural death is foreseeable are referred to as Track 1). Track 2 applicants are subject to additional safeguards under the 2021 C-7 legislation.
Three additional proposed changes to the legislation have been extensively studied by Canadian Expert Panels (Council of Canadian Academics [CCA]) [ 4 , 5 , 6 ] First, under the legislation that defines Track 2, individuals with mental disease as their sole underlying medical condition may apply for MAiD, but implementation of this practice is embargoed until March 2027 [ 4 ]. Second, there is consideration of allowing MAiD to be implemented through advanced consent. This would make it possible for persons living with dementia to receive MAID after they have lost the capacity to consent to the procedure [ 5 ]. Third, there is consideration of extending MAiD to mature minors. A mature minor is defined as “a person under the age of majority…and who has the capacity to understand and appreciate the nature and consequences of a decision” ([ 6 ] p. 5). In summary, since the legalization of MAiD in 2016 the eligibility criteria and safeguards have evolved significantly with consequent implications for nurses and nursing care. Further, the number of Canadians who access MAiD shows steady increases since 2016 [ 7 ] and it is expected that these increases will continue in the foreseeable future.
Nurses have been integral to MAiD care in the Canadian context. While other countries such as Belgium and the Netherlands also permit euthanasia, Canada is the first country to allow Nurse Practitioners (Registered Nurses with additional preparation typically achieved at the graduate level) to act independently as assessors and providers of MAiD [ 1 ]. Although the role of Registered Nurses (RNs) in MAiD is not defined in federal legislation, it has been addressed at the provincial/territorial-level with variability in scope of practice by region [ 8 , 9 ]. For example, there are differences with respect to the obligation of the nurse to provide information to patients about MAiD, and to the degree that nurses are expected to ensure that patient eligibility criteria and safeguards are met prior to their participation [ 10 ]. Studies conducted in the Canadian context indicate that RNs perform essential roles in MAiD care coordination; client and family teaching and support; MAiD procedural quality; healthcare provider and public education; and bereavement care for family [ 9 , 11 ]. Nurse practitioners and RNs are integral to a robust MAiD care system in Canada and hence need to be well-prepared for their role [ 12 ].
Previous studies have found that end of life care, and MAiD specifically, raise complex moral and ethical issues for nurses [ 13 , 14 , 15 , 16 ]. The knowledge, attitudes, and beliefs of nurses are important across practice settings because nurses have consistent, ongoing, and direct contact with patients who experience chronic or life-limiting health conditions. Canadian studies exploring nurses’ moral and ethical decision-making in relation to MAiD reveal that although some nurses are clear in their support for, or opposition to, MAiD, others are unclear on what they believe to be good and right [ 14 ]. Empirical findings suggest that nurses go through a period of moral sense-making that is often informed by their family, peers, and initial experiences with MAID [ 17 , 18 ]. Canadian legislation and policy specifies that nurses are not required to participate in MAiD and may recuse themselves as conscientious objectors with appropriate steps to ensure ongoing and safe care of patients [ 1 , 19 ]. However, with so many nurses having to reflect on and make sense of their moral position, it is essential that they are given adequate time and preparation to make an informed and thoughtful decision before they participate in a MAID death [ 20 , 21 ].
It is well established that nursing students receive inconsistent exposure to end of life care issues [ 22 ] and little or no training related to MAiD [ 23 ]. Without such education and reflection time in pre-entry nursing preparation, nurses are at significant risk for moral harm. An important first step in providing this preparation is to be able to assess the knowledge, values, and beliefs of nursing students regarding MAID and end of life care. As demand for MAiD increases along with the complexities of MAiD, it is critical to understand the knowledge, attitudes, and likelihood of engagement with MAiD among nursing students as a baseline upon which to build curriculum and as a means to track these variables over time.
Aim, design, and setting
The aim of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context. We sought to explore both their willingness to be involved in the registered nursing role and in the nurse practitioner role should they chose to prepare themselves to that level of education. The design was a mixed-method, modified e-Delphi method that entailed item generation, item refinement through an expert faculty panel [ 24 , 25 , 26 ], and initial item validation through a cognitive focus group interview with nursing students [ 27 ]. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
Participants
A panel of 10 faculty from the two nursing education programs were recruited for Phase 2 of the e-Delphi. To be included, faculty were required to have a minimum of three years of experience in nurse education, be employed as nursing faculty, and self-identify as having experience with MAiD. A convenience sample of 5 fourth-year nursing students were recruited to participate in Phase 3. Students had to be in good standing in the nursing program and be willing to share their experiences of the survey in an online group interview format.
The modified e-Delphi was conducted in 3 phases: Phase 1 entailed item generation through literature and existing survey review. Phase 2 entailed item refinement through a faculty expert panel review with focus on content validity, prioritization, and revision of item wording [ 25 ]. Phase 3 entailed an assessment of face validity through focus group-based cognitive interview with nursing students.
Phase I. Item generation through literature review
The goal of phase 1 was to develop a bank of survey items that would represent the variables of interest and which could be provided to expert faculty in Phase 2. Initial survey items were generated through a literature review of similar surveys designed to assess knowledge and attitudes toward MAiD/euthanasia in healthcare providers; Canadian empirical studies on nurses’ roles and/or experiences with MAiD; and legislative and expert panel documents that outlined proposed changes to the legislative eligibility criteria and safeguards. The literature review was conducted in three online databases: CINAHL, PsycINFO, and Medline. Key words for the search included nurses , nursing students , medical students , NPs, MAiD , euthanasia , assisted death , and end-of-life care . Only articles written in English were reviewed. The legalization and legislation of MAiD is new in many countries; therefore, studies that were greater than twenty years old were excluded, no further exclusion criteria set for country.
Items from surveys designed to measure similar variables in other health care providers and geographic contexts were placed in a table and similar items were collated and revised into a single item. Then key variables were identified from the empirical literature on nurses and MAiD in Canada and checked against the items derived from the surveys to ensure that each of the key variables were represented. For example, conscientious objection has figured prominently in the Canadian literature, but there were few items that assessed knowledge of conscientious objection in other surveys and so items were added [ 15 , 21 , 28 , 29 ]. Finally, four case studies were added to the survey to address the anticipated changes to the Canadian legislation. The case studies were based upon the inclusion of mature minors, advanced consent, and mental disorder as the sole underlying medical condition. The intention was to assess nurses’ beliefs and comfort with these potential legislative changes.
Phase 2. Item refinement through expert panel review
The goal of phase 2 was to refine and prioritize the proposed survey items identified in phase 1 using a modified e-Delphi approach to achieve consensus among an expert panel [ 26 ]. Items from phase 1 were presented to an expert faculty panel using a Qualtrics (Provo, UT) online survey. Panel members were asked to review each item to determine if it should be: included, excluded or adapted for the survey. When adapted was selected faculty experts were asked to provide rationale and suggestions for adaptation through the use of an open text box. Items that reached a level of 75% consensus for either inclusion or adaptation were retained [ 25 , 26 ]. New items were categorized and added, and a revised survey was presented to the panel of experts in round 2. Panel members were again asked to review items, including new items, to determine if it should be: included, excluded, or adapted for the survey. Round 2 of the modified e-Delphi approach also included an item prioritization activity, where participants were then asked to rate the importance of each item, based on a 5-point Likert scale (low to high importance), which De Vaus [ 30 ] states is helpful for increasing the reliability of responses. Items that reached a 75% consensus on inclusion were then considered in relation to the importance it was given by the expert panel. Quantitative data were managed using SPSS (IBM Corp).
Phase 3. Face validity through cognitive interviews with nursing students
The goal of phase 3 was to obtain initial face validity of the proposed survey using a sample of nursing student informants. More specifically, student participants were asked to discuss how items were interpreted, to identify confusing wording or other problematic construction of items, and to provide feedback about the survey as a whole including readability and organization [ 31 , 32 , 33 ]. The focus group was held online and audio recorded. A semi-structured interview guide was developed for this study that focused on clarity, meaning, order and wording of questions; emotions evoked by the questions; and overall survey cohesion and length was used to obtain data (see Supplementary Material 2 for the interview guide). A prompt to “think aloud” was used to limit interviewer-imposed bias and encourage participants to describe their thoughts and response to a given item as they reviewed survey items [ 27 ]. Where needed, verbal probes such as “could you expand on that” were used to encourage participants to expand on their responses [ 27 ]. Student participants’ feedback was collated verbatim and presented to the research team where potential survey modifications were negotiated and finalized among team members. Conventional content analysis [ 34 ] of focus group data was conducted to identify key themes that emerged through discussion with students. Themes were derived from the data by grouping common responses and then using those common responses to modify survey items.
Ten nursing faculty participated in the expert panel. Eight of the 10 faculty self-identified as female. No faculty panel members reported conscientious objector status and ninety percent reported general agreement with MAiD with one respondent who indicated their view as “unsure.” Six of the 10 faculty experts had 16 years of experience or more working as a nurse educator.
Five nursing students participated in the cognitive interview focus group. The duration of the focus group was 2.5 h. All participants identified that they were born in Canada, self-identified as female (one preferred not to say) and reported having received some instruction about MAiD as part of their nursing curriculum. See Tables 1 and 2 for the demographic descriptors of the study sample. Study results will be reported in accordance with the study phases. See Fig. 1 for an overview of the results from each phase.
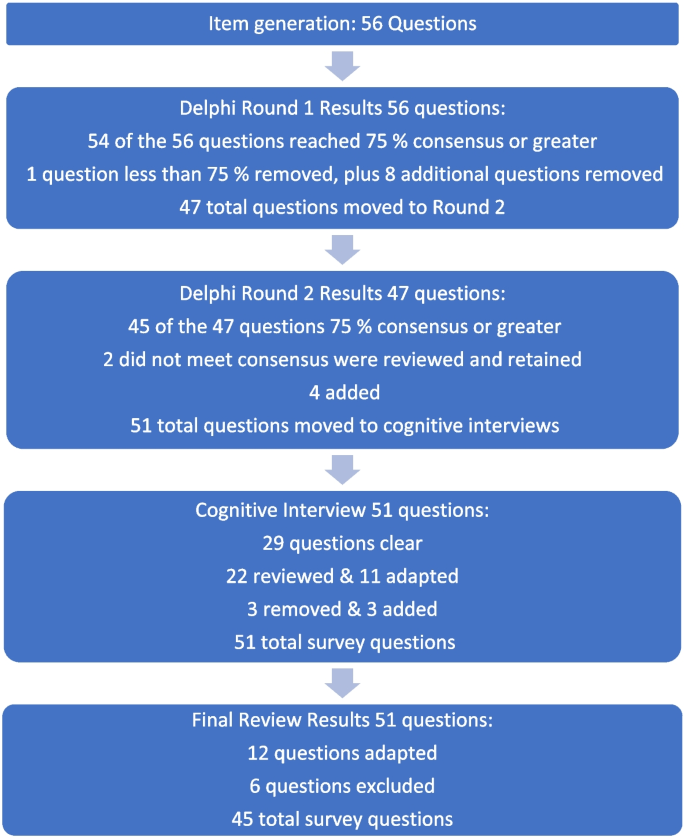
Fig. 1 Overview of survey development findings
Phase 1: survey item generation
Review of the literature identified that no existing survey was available for use with nursing students in the Canadian context. However, an analysis of themes across qualitative and quantitative studies of physicians, medical students, nurses, and nursing students provided sufficient data to develop a preliminary set of items suitable for adaptation to a population of nursing students.
Four major themes and factors that influence knowledge, attitudes, and beliefs about MAiD were evident from the literature: (i) endogenous or individual factors such as age, gender, personally held values, religion, religiosity, and/or spirituality [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ], (ii) experience with death and dying in personal and/or professional life [ 35 , 40 , 41 , 43 , 44 , 45 ], (iii) training including curricular instruction about clinical role, scope of practice, or the law [ 23 , 36 , 39 ], and (iv) exogenous or social factors such as the influence of key leaders, colleagues, friends and/or family, professional and licensure organizations, support within professional settings, and/or engagement in MAiD in an interdisciplinary team context [ 9 , 35 , 46 ].
Studies of nursing students also suggest overlap across these categories. For example, value for patient autonomy [ 23 ] and the moral complexity of decision-making [ 37 ] are important factors that contribute to attitudes about MAiD and may stem from a blend of personally held values coupled with curricular content, professional training and norms, and clinical exposure. For example, students report that participation in end of life care allows for personal growth, shifts in perception, and opportunities to build therapeutic relationships with their clients [ 44 , 47 , 48 ].
Preliminary items generated from the literature resulted in 56 questions from 11 published sources (See Table 3 ). These items were constructed across four main categories: (i) socio-demographic questions; (ii) end of life care questions; (iii) knowledge about MAiD; or (iv) comfort and willingness to participate in MAiD. Knowledge questions were refined to reflect current MAiD legislation, policies, and regulatory frameworks. Falconer [ 39 ] and Freeman [ 45 ] studies were foundational sources for item selection. Additionally, four case studies were written to reflect the most recent anticipated changes to MAiD legislation and all used the same open-ended core questions to address respondents’ perspectives about the patient’s right to make the decision, comfort in assisting a physician or NP to administer MAiD in that scenario, and hypothesized comfort about serving as a primary provider if qualified as an NP in future. Response options for the survey were also constructed during this stage and included: open text, categorical, yes/no , and Likert scales.
Phase 2: faculty expert panel review
Of the 56 items presented to the faculty panel, 54 questions reached 75% consensus. However, based upon the qualitative responses 9 items were removed largely because they were felt to be repetitive. Items that generated the most controversy were related to measuring religion and spirituality in the Canadian context, defining end of life care when there is no agreed upon time frames (e.g., last days, months, or years), and predicting willingness to be involved in a future events – thus predicting their future selves. Phase 2, round 1 resulted in an initial set of 47 items which were then presented back to the faculty panel in round 2.
Of the 47 initial questions presented to the panel in round 2, 45 reached a level of consensus of 75% or greater, and 34 of these questions reached a level of 100% consensus [ 27 ] of which all participants chose to include without any adaptations) For each question, level of importance was determined based on a 5-point Likert scale (1 = very unimportant, 2 = somewhat unimportant, 3 = neutral, 4 = somewhat important, and 5 = very important). Figure 2 provides an overview of the level of importance assigned to each item.
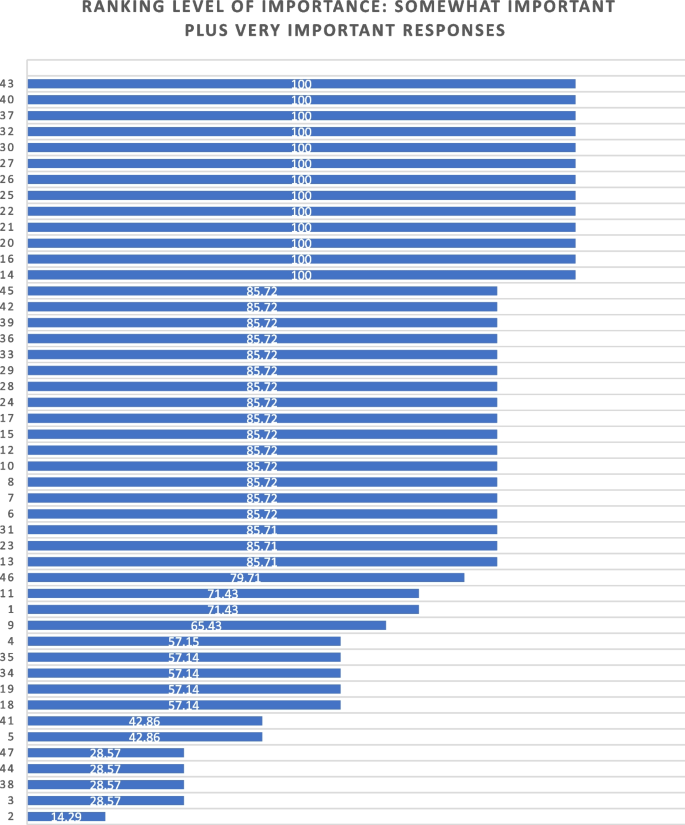
Ranking level of importance for survey items
After round 2, a careful analysis of participant comments and level of importance was completed by the research team. While the main method of survey item development came from participants’ response to the first round of Delphi consensus ratings, level of importance was used to assist in the decision of whether to keep or modify questions that created controversy, or that rated lower in the include/exclude/adapt portion of the Delphi. Survey items that rated low in level of importance included questions about future roles, sex and gender, and religion/spirituality. After deliberation by the research committee, these questions were retained in the survey based upon the importance of these variables in the scientific literature.
Of the 47 questions remaining from Phase 2, round 2, four were revised. In addition, the two questions that did not meet the 75% cut off level for consensus were reviewed by the research team. The first question reviewed was What is your comfort level with providing a MAiD death in the future if you were a qualified NP ? Based on a review of participant comments, it was decided to retain this question for the cognitive interviews with students in the final phase of testing. The second question asked about impacts on respondents’ views of MAiD and was changed from one item with 4 subcategories into 4 separate items, resulting in a final total of 51 items for phase 3. The revised survey was then brought forward to the cognitive interviews with student participants in Phase 3. (see Supplementary Material 1 for a complete description of item modification during round 2).
Phase 3. Outcomes of cognitive interview focus group
Of the 51 items reviewed by student participants, 29 were identified as clear with little or no discussion. Participant comments for the remaining 22 questions were noted and verified against the audio recording. Following content analysis of the comments, four key themes emerged through the student discussion: unclear or ambiguous wording; difficult to answer questions; need for additional response options; and emotional response evoked by questions. An example of unclear or ambiguous wording was a request for clarity in the use of the word “sufficient” in the context of assessing an item that read “My nursing education has provided sufficient content about the nursing role in MAiD.” “Sufficient” was viewed as subjective and “laden with…complexity that distracted me from the question.” The group recommended rewording the item to read “My nursing education has provided enough content for me to care for a patient considering or requesting MAiD.”
An example of having difficulty answering questions related to limited knowledge related to terms used in the legislation such as such as safeguards , mature minor , eligibility criteria , and conscientious objection. Students were unclear about what these words meant relative to the legislation and indicated that this lack of clarity would hamper appropriate responses to the survey. To ensure that respondents are able to answer relevant questions, student participants recommended that the final survey include explanation of key terms such as mature minor and conscientious objection and an overview of current legislation.
Response options were also a point of discussion. Participants noted a lack of distinction between response options of unsure and unable to say . Additionally, scaling of attitudes was noted as important since perspectives about MAiD are dynamic and not dichotomous “agree or disagree” responses. Although the faculty expert panel recommended the integration of the demographic variables of religious and/or spiritual remain as a single item, the student group stated a preference to have religion and spirituality appear as separate items. The student focus group also took issue with separate items for the variables of sex and gender, specifically that non-binary respondents might feel othered or “outed” particularly when asked to identify their sex. These variables had been created based upon best practices in health research but students did not feel they were appropriate in this context [ 49 ]. Finally, students agreed with the faculty expert panel in terms of the complexity of projecting their future involvement as a Nurse Practitioner. One participant stated: “I certainly had to like, whoa, whoa, whoa. Now let me finish this degree first, please.” Another stated, “I'm still imagining myself, my future career as an RN.”
Finally, student participants acknowledged the array of emotions that some of the items produced for them. For example, one student described positive feelings when interacting with the survey. “Brought me a little bit of feeling of joy. Like it reminded me that this is the last piece of independence that people grab on to.” Another participant, described the freedom that the idea of an advance request gave her. “The advance request gives the most comfort for me, just with early onset Alzheimer’s and knowing what it can do.” But other participants described less positive feelings. For example, the mature minor case study yielded a comment: “This whole scenario just made my heart hurt with the idea of a child requesting that.”
Based on the data gathered from the cognitive interview focus group of nursing students, revisions were made to 11 closed-ended questions (see Table 4 ) and 3 items were excluded. In the four case studies, the open-ended question related to a respondents’ hypothesized actions in a future role as NP were removed. The final survey consists of 45 items including 4 case studies (see Supplementary Material 3 ).
The aim of this study was to develop and validate a survey that can be used to track the growth of knowledge about MAiD among nursing students over time, inform training programs about curricular needs, and evaluate attitudes and willingness to participate in MAiD at time-points during training or across nursing programs over time.
The faculty expert panel and student participants in the cognitive interview focus group identified a need to establish core knowledge of the terminology and legislative rules related to MAiD. For example, within the cognitive interview group of student participants, several acknowledged lack of clear understanding of specific terms such as “conscientious objector” and “safeguards.” Participants acknowledged discomfort with the uncertainty of not knowing and their inclination to look up these terms to assist with answering the questions. This survey can be administered to nursing or pre-nursing students at any phase of their training within a program or across training programs. However, in doing so it is important to acknowledge that their baseline knowledge of MAiD will vary. A response option of “not sure” is important and provides a means for respondents to convey uncertainty. If this survey is used to inform curricular needs, respondents should be given explicit instructions not to conduct online searches to inform their responses, but rather to provide an honest appraisal of their current knowledge and these instructions are included in the survey (see Supplementary Material 3 ).
Some provincial regulatory bodies have established core competencies for entry-level nurses that include MAiD. For example, the BC College of Nurses and Midwives (BCCNM) requires “knowledge about ethical, legal, and regulatory implications of medical assistance in dying (MAiD) when providing nursing care.” (10 p. 6) However, across Canada curricular content and coverage related to end of life care and MAiD is variable [ 23 ]. Given the dynamic nature of the legislation that includes portions of the law that are embargoed until 2024, it is important to ensure that respondents are guided by current and accurate information. As the law changes, nursing curricula, and public attitudes continue to evolve, inclusion of core knowledge and content is essential and relevant for investigators to be able to interpret the portions of the survey focused on attitudes and beliefs about MAiD. Content knowledge portions of the survey may need to be modified over time as legislation and training change and to meet the specific purposes of the investigator.
Given the sensitive nature of the topic, it is strongly recommended that surveys be conducted anonymously and that students be provided with an opportunity to discuss their responses to the survey. A majority of feedback from both the expert panel of faculty and from student participants related to the wording and inclusion of demographic variables, in particular religion, religiosity, gender identity, and sex assigned at birth. These and other demographic variables have the potential to be highly identifying in small samples. In any instance in which the survey could be expected to yield demographic group sizes less than 5, users should eliminate the demographic variables from the survey. For example, the profession of nursing is highly dominated by females with over 90% of nurses who identify as female [ 50 ]. Thus, a survey within a single class of students or even across classes in a single institution is likely to yield a small number of male respondents and/or respondents who report a difference between sex assigned at birth and gender identity. When variables that serve to identify respondents are included, respondents are less likely to complete or submit the survey, to obscure their responses so as not to be identifiable, or to be influenced by social desirability bias in their responses rather than to convey their attitudes accurately [ 51 ]. Further, small samples do not allow for conclusive analyses or interpretation of apparent group differences. Although these variables are often included in surveys, such demographics should be included only when anonymity can be sustained. In small and/or known samples, highly identifying variables should be omitted.
There are several limitations associated with the development of this survey. The expert panel was comprised of faculty who teach nursing students and are knowledgeable about MAiD and curricular content, however none identified as a conscientious objector to MAiD. Ideally, our expert panel would have included one or more conscientious objectors to MAiD to provide a broader perspective. Review by practitioners who participate in MAiD, those who are neutral or undecided, and practitioners who are conscientious objectors would ensure broad applicability of the survey. This study included one student cognitive interview focus group with 5 self-selected participants. All student participants had held discussions about end of life care with at least one patient, 4 of 5 participants had worked with a patient who requested MAiD, and one had been present for a MAiD death. It is not clear that these participants are representative of nursing students demographically or by experience with end of life care. It is possible that the students who elected to participate hold perspectives and reflections on patient care and MAiD that differ from students with little or no exposure to end of life care and/or MAiD. However, previous studies find that most nursing students have been involved with end of life care including meaningful discussions about patients’ preferences and care needs during their education [ 40 , 44 , 47 , 48 , 52 ]. Data collection with additional student focus groups with students early in their training and drawn from other training contexts would contribute to further validation of survey items.
Future studies should incorporate pilot testing with small sample of nursing students followed by a larger cross-program sample to allow evaluation of the psychometric properties of specific items and further refinement of the survey tool. Consistent with literature about the importance of leadership in the context of MAiD [ 12 , 53 , 54 ], a study of faculty knowledge, beliefs, and attitudes toward MAiD would provide context for understanding student perspectives within and across programs. Additional research is also needed to understand the timing and content coverage of MAiD across Canadian nurse training programs’ curricula.
The implementation of MAiD is complex and requires understanding of the perspectives of multiple stakeholders. Within the field of nursing this includes clinical providers, educators, and students who will deliver clinical care. A survey to assess nursing students’ attitudes toward and willingness to participate in MAiD in the Canadian context is timely, due to the legislation enacted in 2016 and subsequent modifications to the law in 2021 with portions of the law to be enacted in 2027. Further development of this survey could be undertaken to allow for use in settings with practicing nurses or to allow longitudinal follow up with students as they enter practice. As the Canadian landscape changes, ongoing assessment of the perspectives and needs of health professionals and students in the health professions is needed to inform policy makers, leaders in practice, curricular needs, and to monitor changes in attitudes and practice patterns over time.
Availability of data and materials
The datasets used and/or analysed during the current study are not publicly available due to small sample sizes, but are available from the corresponding author on reasonable request.
Abbreviations
British Columbia College of Nurses and Midwives
Medical assistance in dying
Nurse practitioner
Registered nurse
University of British Columbia Okanagan
Nicol J, Tiedemann M. Legislative Summary: Bill C-14: An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying). Available from: https://lop.parl.ca/staticfiles/PublicWebsite/Home/ResearchPublications/LegislativeSummaries/PDF/42-1/c14-e.pdf .
Downie J, Scallion K. Foreseeably unclear. The meaning of the “reasonably foreseeable” criterion for access to medical assistance in dying in Canada. Dalhousie Law J. 2018;41(1):23–57.
Nicol J, Tiedeman M. Legislative summary of Bill C-7: an act to amend the criminal code (medical assistance in dying). Ottawa: Government of Canada; 2021.
Google Scholar
Council of Canadian Academies. The state of knowledge on medical assistance in dying where a mental disorder is the sole underlying medical condition. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-Where-a-Mental-Disorder-is-the-Sole-Underlying-Medical-Condition.pdf .
Council of Canadian Academies. The state of knowledge on advance requests for medical assistance in dying. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2019/02/The-State-of-Knowledge-on-Advance-Requests-for-Medical-Assistance-in-Dying.pdf .
Council of Canadian Academies. The state of knowledge on medical assistance in dying for mature minors. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-for-Mature-Minors.pdf .
Health Canada. Third annual report on medical assistance in dying in Canada 2021. Ottawa; 2022. [cited 2023 Oct 23]. Available from: https://www.canada.ca/en/health-canada/services/medical-assistance-dying/annual-report-2021.html .
Banner D, Schiller CJ, Freeman S. Medical assistance in dying: a political issue for nurses and nursing in Canada. Nurs Philos. 2019;20(4): e12281.
Article PubMed Google Scholar
Pesut B, Thorne S, Stager ML, Schiller CJ, Penney C, Hoffman C, et al. Medical assistance in dying: a review of Canadian nursing regulatory documents. Policy Polit Nurs Pract. 2019;20(3):113–30.
Article PubMed PubMed Central Google Scholar
College of Registered Nurses of British Columbia. Scope of practice for registered nurses [Internet]. Vancouver; 2018. Available from: https://www.bccnm.ca/Documents/standards_practice/rn/RN_ScopeofPractice.pdf .
Pesut B, Thorne S, Schiller C, Greig M, Roussel J, Tishelman C. Constructing good nursing practice for medical assistance in dying in Canada: an interpretive descriptive study. Global Qual Nurs Res. 2020;7:2333393620938686. https://doi.org/10.1177/2333393620938686 .
Article Google Scholar
Pesut B, Thorne S, Schiller CJ, Greig M, Roussel J. The rocks and hard places of MAiD: a qualitative study of nursing practice in the context of legislated assisted death. BMC Nurs. 2020;19:12. https://doi.org/10.1186/s12912-020-0404-5 .
Pesut B, Greig M, Thorne S, Burgess M, Storch JL, Tishelman C, et al. Nursing and euthanasia: a narrative review of the nursing ethics literature. Nurs Ethics. 2020;27(1):152–67.
Pesut B, Thorne S, Storch J, Chambaere K, Greig M, Burgess M. Riding an elephant: a qualitative study of nurses’ moral journeys in the context of Medical Assistance in Dying (MAiD). Journal Clin Nurs. 2020;29(19–20):3870–81.
Lamb C, Babenko-Mould Y, Evans M, Wong CA, Kirkwood KW. Conscientious objection and nurses: results of an interpretive phenomenological study. Nurs Ethics. 2018;26(5):1337–49.
Wright DK, Chan LS, Fishman JR, Macdonald ME. “Reflection and soul searching:” Negotiating nursing identity at the fault lines of palliative care and medical assistance in dying. Social Sci & Med. 2021;289: 114366.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;54(4):511–20.
Bruce A, Beuthin R. Medically assisted dying in Canada: "Beautiful Death" is transforming nurses' experiences of suffering. The Canadian J Nurs Res | Revue Canadienne de Recherche en Sci Infirmieres. 2020;52(4):268–77. https://doi.org/10.1177/0844562119856234 .
Canadian Nurses Association. Code of ethics for registered nurses. Ottawa; 2017. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-ethics .
Canadian Nurses Association. National nursing framework on Medical Assistance in Dying in Canada. Ottawa: 2017. Available from: https://www.virtualhospice.ca/Assets/cna-national-nursing-framework-on-maidEng_20170216155827.pdf .
Pesut B, Thorne S, Greig M. Shades of gray: conscientious objection in medical assistance in dying. Nursing Inq. 2020;27(1): e12308.
Durojaiye A, Ryan R, Doody O. Student nurse education and preparation for palliative care: a scoping review. PLoS ONE. 2023. https://doi.org/10.1371/journal.pone.0286678 .
McMechan C, Bruce A, Beuthin R. Canadian nursing students’ experiences with medical assistance in dying | Les expériences d’étudiantes en sciences infirmières au regard de l’aide médicale à mourir. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2019;5(1). https://doi.org/10.17483/2368-6669.1179 .
Adler M, Ziglio E. Gazing into the oracle. The Delphi method and its application to social policy and public health. London: Jessica Kingsley Publishers; 1996
Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53(2):205–12.
Keeney S, Hasson F, McKenna H. The Delphi technique in nursing and health research. 1st ed. City: Wiley; 2011.
Willis GB. Cognitive interviewing: a tool for improving questionnaire design. 1st ed. Thousand Oaks, Calif: Sage; 2005. ISBN: 9780761928041
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood EW. Conscience, conscientious objection, and nursing: a concept analysis. Nurs Ethics. 2017;26(1):37–49.
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood K. Nurses’ use of conscientious objection and the implications of conscience. J Adv Nurs. 2018;75(3):594–602.
de Vaus D. Surveys in social research. 6th ed. Abingdon, Oxon: Routledge; 2014.
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: A primer. Front Public Health. 2018;6:149. https://doi.org/10.3389/fpubh.2018.00149 .
Puchta C, Potter J. Focus group practice. 1st ed. London: Sage; 2004.
Book Google Scholar
Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. 5th ed. Oxford: Oxford University Press; 2015.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Adesina O, DeBellis A, Zannettino L. Third-year Australian nursing students’ attitudes, experiences, knowledge, and education concerning end-of-life care. Int J of Palliative Nurs. 2014;20(8):395–401.
Bator EX, Philpott B, Costa AP. This moral coil: a cross-sectional survey of Canadian medical student attitudes toward medical assistance in dying. BMC Med Ethics. 2017;18(1):58.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;53(4):511–20.
Brown J, Goodridge D, Thorpe L, Crizzle A. What is right for me, is not necessarily right for you: the endogenous factors influencing nonparticipation in medical assistance in dying. Qual Health Res. 2021;31(10):1786–1800.
Falconer J, Couture F, Demir KK, Lang M, Shefman Z, Woo M. Perceptions and intentions toward medical assistance in dying among Canadian medical students. BMC Med Ethics. 2019;20(1):22.
Green G, Reicher S, Herman M, Raspaolo A, Spero T, Blau A. Attitudes toward euthanasia—dual view: Nursing students and nurses. Death Stud. 2022;46(1):124–31.
Hosseinzadeh K, Rafiei H. Nursing student attitudes toward euthanasia: a cross-sectional study. Nurs Ethics. 2019;26(2):496–503.
Ozcelik H, Tekir O, Samancioglu S, Fadiloglu C, Ozkara E. Nursing students’ approaches toward euthanasia. Omega (Westport). 2014;69(1):93–103.
Canning SE, Drew C. Canadian nursing students’ understanding, and comfort levels related to medical assistance in dying. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2022;8(2). https://doi.org/10.17483/2368-6669.1326 .
Edo-Gual M, Tomás-Sábado J, Bardallo-Porras D, Monforte-Royo C. The impact of death and dying on nursing students: an explanatory model. J Clin Nurs. 2014;23(23–24):3501–12.
Freeman LA, Pfaff KA, Kopchek L, Liebman J. Investigating palliative care nurse attitudes towards medical assistance in dying: an exploratory cross-sectional study. J Adv Nurs. 2020;76(2):535–45.
Brown J, Goodridge D, Thorpe L, Crizzle A. “I am okay with it, but I am not going to do it:” the exogenous factors influencing non-participation in medical assistance in dying. Qual Health Res. 2021;31(12):2274–89.
Dimoula M, Kotronoulas G, Katsaragakis S, Christou M, Sgourou S, Patiraki E. Undergraduate nursing students’ knowledge about palliative care and attitudes towards end-of-life care: A three-cohort, cross-sectional survey. Nurs Educ Today. 2019;74:7–14.
Matchim Y, Raetong P. Thai nursing students’ experiences of caring for patients at the end of life: a phenomenological study. Int J Palliative Nurs. 2018;24(5):220–9.
Canadian Institute for Health Research. Sex and gender in health research [Internet]. Ottawa: CIHR; 2021 [cited 2023 Oct 23]. Available from: https://cihr-irsc.gc.ca/e/50833.html .
Canadian Nurses’ Association. Nursing statistics. Ottawa: CNA; 2023 [cited 2023 Oct 23]. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-statistics .
Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025–47. https://doi.org/10.1007/s11135-011-9640-9 .
Ferri P, Di Lorenzo R, Stifani S, Morotti E, Vagnini M, Jiménez Herrera MF, et al. Nursing student attitudes toward dying patient care: a European multicenter cross-sectional study. Acta Bio Medica Atenei Parmensis. 2021;92(S2): e2021018.
PubMed PubMed Central Google Scholar
Beuthin R, Bruce A. Medical assistance in dying (MAiD): Ten things leaders need to know. Nurs Leadership. 2018;31(4):74–81.
Thiele T, Dunsford J. Nurse leaders’ role in medical assistance in dying: a relational ethics approach. Nurs Ethics. 2019;26(4):993–9.
Download references
Acknowledgements
We would like to acknowledge the faculty and students who generously contributed their time to this work.
JS received a student traineeship through the Principal Research Chairs program at the University of British Columbia Okanagan.
Author information
Authors and affiliations.
School of Health and Human Services, Selkirk College, Castlegar, BC, Canada
Jocelyn Schroeder & Barbara Pesut
School of Nursing, University of British Columbia Okanagan, Kelowna, BC, Canada
Barbara Pesut, Lise Olsen, Nelly D. Oelke & Helen Sharp
You can also search for this author in PubMed Google Scholar
Contributions
JS made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. JS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. BP made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. BP has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. LO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. LO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. NDO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. NDO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. HS made substantial contributions to drafting and substantively revising the work. HS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Authors’ information
JS conducted this study as part of their graduate requirements in the School of Nursing, University of British Columbia Okanagan.
Corresponding author
Correspondence to Barbara Pesut .
Ethics declarations
Ethics approval and consent to participate.
The research was approved by the Selkirk College Research Ethics Board (REB) ID # 2021–011 and the University of British Columbia Behavioral Research Ethics Board ID # H21-01181.
All participants provided written and informed consent through approved consent processes. Research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schroeder, J., Pesut, B., Olsen, L. et al. Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study. BMC Nurs 23 , 326 (2024). https://doi.org/10.1186/s12912-024-01984-z
Download citation
Received : 24 October 2023
Accepted : 28 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12912-024-01984-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical assistance in dying (MAiD)
- End of life care
- Student nurses
- Nursing education
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Advertisement
Food 'addiction' should be treated like drug abuse, claim doctors
A group of doctors and scientists is getting behind the controversial idea that people can be addicted to certain trigger foods, in the same way as drugs and alcohol. The team says this addiction should be treated with abstinence, which goes against mainstream medical advice
By Clare Wilson
17 May 2024

Certain “trigger foods” may be hard for some people to avoid
Wirestock, Inc./Alamy
Is it possible to be “addicted” to eating unhealthy food? Yes, says a group of doctors and scientists who are going against mainstream medical advice to declare a provocative new way to think about overeating.
The idea isn’t entirely new, as a few researchers have been arguing for years that some people overeat so much that their relationship with food should be seen as an addiction. But because it seems different to other kinds of addictions, such as when people are dependent on alcohol or take…
Sign up to our weekly newsletter
Receive a weekly dose of discovery in your inbox! We'll also keep you up to date with New Scientist events and special offers.
To continue reading, subscribe today with our introductory offers
No commitment, cancel anytime*
Offer ends 2nd of July 2024.
*Cancel anytime within 14 days of payment to receive a refund on unserved issues.
Inclusive of applicable taxes (VAT)
Existing subscribers
More from New Scientist
Explore the latest news, articles and features
Ultra-processed foods have a bad reputation – is it backed by science?
Subscriber-only
Tackling ultra-processed food must focus on evidence and avoid stigma
How ultra-processed food harms your health and how to fix the problem, highly processed junk food consumption is rising among us adults, popular articles.
Trending New Scientist articles
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Psychiatry
- v.62(3); May-Jun 2020
Problems in using WhatsApp groups for survey research
Shahul ameen.
Department of Psychiatry, St. Thomas Hospital, Changanacherry, Kerala, India
Samir Kumar Praharaj
1 Department of Psychiatry, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India. E-mail: moc.oohay@neemaluhahs
Links to online surveys and requests to participate in them are now a common sight in WhatsApp groups. Although earlier such messages used to be apparently for small-scale studies intended for conference presentations, off late, the requests often say that the research is part of some thesis or dissertation. Following the recent outbreak of COVID-19, numerous organizations and researchers have chosen the WhatsApp route to conduct surveys exploring its psychosocial impact. However, such use of WhatsApp groups as a data collection avenue for survey research is fraught with the following problems:
- Surveys help us infer the rates in the population from the responses provided by the sample. For the findings to be generalizable, the sample has to be selected from a clearly defined population through random sampling. However, when you are forwarding the link to as many groups as possible and requesting the members to forward the same to as many other groups as possible, your population will not be clearly defined. Consequently, one cannot know the population to which the survey results would be applicable
- Such samples will be convenience ones, with their inherent problems. For example, they would not be suitable for testing hypotheses using inferential statistics. They can, at best, be used for descriptive purposes and generating hypotheses
- The response rate – the number of people who responded to the survey questions, divided by the total number of people approached to participate – is a crucial measure in survey research. A low response rate would suggest that the sample is not representative of the population. However, in these WhatsApp surveys, one can never know the response rate
- Information about the nonresponders is essential because if it is demonstrated that their sociodemographic profile matches that of the responders, then we can conclude that the responders are indeed representative of the population. This, too, is not possible in WhatsApp surveys, and hence, there is no way to assess the magnitude of selection bias. A large sample does not solve this issue
- It is unethical to study a sample larger than what is suggested by appropriate sample size calculations. However, as the links get forwarded from groups to groups, an unnecessarily large number of people may participate in the survey, with no gains from the time and effort they sacrifice
- Considering the privacy issues with open-source software, collecting sensitive data may not be ethical, even after taking consent, as most participants will not be aware of the implications – i.e., it is no longer an informed consent.
One solution would be to randomly select the sample from a list (e.g., membership directory of an organization or a list of the entire staff of a hospital), ring them up to request consent, collect basic sociodemographic information from those who refuse, and then send the link to only those who consented, with a request to not forward it further. Forwarding of the link to inappropriate groups or persons may be prevented to some extent by mentioning the inclusion and exclusion criteria in the request message.
Two other issues, not restricted to the use of WhatsApp groups, too deserve the consideration of the researchers: (i) As in any survey, sufficient attention has to be paid to the reliability and validity of the questionnaire, so as to reduce the measurement error. (ii) Using a different browser or a second SIM card, the same person may participate in a survey more than once; it may not be possible to detect this with Internet Protocol tracking.
The ethics committees that approve these surveys should include experts on data privacy. If the researchers mention, in the message accompanying the link, about such precautions in place, it may improve the response rate. Furthermore, all steps involved should be accurately described in the manuscript (e.g., what instructions were given, any reminders sent, etc.,) to increase the transparency of the findings.[ 1 ]
Conflicts of interest
There are no conflicts of interest.

IMAGES
VIDEO
COMMENTS
Qualitative WhatsApp group created as a means of improving team communication. Used and analysed WhatsApp text messages. ... (HSRI) in the UK, and is jointly funding by the Department of International Development (DFID), the Economic and Social Research Council (ESRC), the Medical Research Council (MRC) and the Wellcome Trust. Grant number: MR ...
Whilst WhatsApp has been successfully used in research with migrant and mobile groups ( Almenara-Niebla and Ascanio-Sánchez, 2020; Khoso et al., 2020 ), little is known about the use of WhatsApp in health systems research. To address this gap, we have undertaken a scoping review exploring the use of WhatsApp in health systems research.
We used WhatsApp in our research for the first time in 2018, on a very ad hoc basis. We had a larger group of research assistants to manage this time. It was becoming a challenge to ensure that all the research assistants received the same information and to coordinate their work. The WhatsApp group was a new feature and just proliferating in use.
A mix of features. It's not only aboard research vessels that WhatsApp can be useful for scientists. Because the app is convenient, popular and free to use, researchers have been using it for ...
The advent of telemedicine has allowed physicians to deliver medical treatment to patients from a distance. Mobile apps such as WhatsApp Messenger, an instant messaging service, came as a novel concept in all fields of social life, including medicine. The use of instant messaging services has been shown to improve communication within medical ...
1. Introduction. The use of instant messaging applications, and in particular WhatsApp, to share patient information between clinicians is becoming increasingly common [1,2,3].An earlier review noted that most WhatsApp use in clinical services was in the developing world [].For example, studies from Malaysia, South Africa, and Brazil show that WhatsApp use is common (with 74%, 87%, and 97% of ...
WhatsApp groups provide efficient mechanisms for clinical management advice, decision-making support and peer review. However, most HCPs do not fully understand the legal and ethical implications of sharing content in a WhatsApp group setting, which is often thought to be hosted on a secure platform and therefore removed from public scrutiny.
A key reason for focusing on WhatsApp is the ability to retain contact with participants when they cross international borders. Five key public health databases were searched for articles containing the words 'WhatsApp' and 'health research' in their titles and abstracts.
WhatsApp is a popular messaging application frequently used by physicians and healthcare organizations that can improve the continuity of care and facilitate effective health services provision, especially in acute settings. However WhatsApp does not comply with the rules of the European GDPR and the US HIPA Act. So it is inappropriate to share clinical information via WhatsApp.For this reason ...
Among posts containing COVID-19-related medical information, it was notable that two-thirds (571/868, 65.8%) of these posts were from public mass media or unverified sources. ... Dive into the research topics of 'Impact of the COVID-19 Pandemic on a Physician Group's WhatsApp Chat: Qualitative Content Analysis'. ... we performed a ...
Abstract. In everyday clinical practice, healthcare professionals (HCPs) are exposed to large quantities of confidential patient information, and many use WhatsApp groups to share this information ...
Background: Online interactions within a closed WhatsApp group can influence the attitudes and behaviors of the users in relation to health issues. Objective: This study aimed to analyze the activity of the members of a WhatsApp group initiated to raise awareness of the possible health effects of 5G mobile networks and mobilize members to sign the related petition.
WhatsApp has become a medium of communication with the potential of promoting collaborative environment with peers, patients and general population. Till date, no analysis of professional WhatsApp groups' activities exists in physiotherapy. The official WhatsApp group chats of the Association of Clinical and Academic Physiotherapists of Nigeria (ACAPN) was analyzed. A total of 20760 chats ...
A scoping review of nine databases sought evidence of record keeping or data storage related to use of WhatsApp in clinical practice up to 31 December 2020. Sixteen of 346 papers met study criteria. Most clinicians were aware that they must comply with statutory reporting requirements in keeping medical records of all electronic communications.
A total of 88.6 percent of participants passed the exam in contrast to the global average pass rate of 69 percent, while the average score among participants was 131.5 compared to a global average score of 128. Passing the exam was significantly associated with combining the WhatsApp group with the online question bank Plabable (p = 0.001).
The use of a WhatsApp group discussion was associated with short-term tobacco abstinence. WhatsApp group discussion for smoking relapse prevention: a randomised controlled trial ... HEALTH AND MEDICAL RESEARCH FUND # # µ 29 3 3 µ 2023 µ .hkmj.org 17 2023 evaluate group, time, and group-by-time interaction effects on ancillary outcomes. ...
From our own research, we have come up with the Best Whatsapp Medical Groups that once you join guarantee you high yield information and discussion. Just click on the links below and choose an appropriate best WhatsApp medical group to join.
In the sections below, you will find details about each of the groups and the respective medical students' WhatsApp group links to join each of them. NB: Each of the WhatsApp Groups is strictly for medical students or doctors who fall under each of the categories; either premedical or medical WhatsApp Groups. 1.
Weiwei Xue et al. A new technique has allowed scientists to freeze human brain tissue so that it regains normal function after thawing, potentially opening the door to improved ways of studying ...
These stages are (i) identifying research questions, (ii) identifying relevant articles, (iii) study selection, (iv) charting the data and (v) collating, summarising, and reporting the results. The purposes of the review were to define the nature of existing research into WhatsApp® for medical learning and to identify a focus for future research.
The National Medical Research Center of Endocrinology of the Ministry of Health of the Russian Federation is a unique, leading in Russia and CIS countries modern medical diagnostic, research and teaching complex. Highly professional doctors work in the laboratories and departments of the center.
Research focused on computational studies of blue-light activated proteins. 2009 - 2016: Max Planck Institute for Medical Research, Germany. Minerva research group in the Department of Biomolecular Mechanisms (Prof. Ilme Schlichting). Research focused on method development for computational studies of flavin-containing photosensory proteins.
Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Canada's legislation is the first to permit Nurse Practitioners (NP) to serve as independent MAiD assessors and providers. Registered Nurses' (RN) also have important roles in MAiD that include MAiD care coordination; client and family teaching and support, MAiD procedural quality; healthcare provider and public education ...
HHS on Wednesday also proposed a debarment, in which federal research funds are banned usually for up to three years — but which can last longer if circumstances warrant. The group has three active NIH grants totaling $2.6 million from last year, per the New York Times , funding studies on zoonotic viruses in southeast Asia and the potential ...
P. Hertsen Moscow Oncology Research Institute (MORI) - the branch of the FSBI "National Medical Research Radiological Centre" (NMRRC) of the Ministry of Health of the Russian Federation is the first oncological hospital in Russia with high-tech equipment, the latest ways and methods of diagnostics and treatment of tumors.
Health Food 'addiction' should be treated like drug abuse, claim doctors. A group of doctors and scientists is getting behind the controversial idea that people can be addicted to certain trigger ...
WASHINGTON, D.C.— Today, U.S. Senator Angus King (I-ME) is calling on the leaders of the Appropriations Committee to prioritize funding for traumatic brain injury (TBI) research in the FY2025 spending bill. In a letter to Defense Subcommittee Chairman Jon Tester (D-MT) and Ranking Member Susan Collins (R-ME), the Senator led a bipartisan group of his colleagues to urge the Appropriations ...
The Blokhin National Medical Research Center of Oncology of the Russian Ministry of Health is the largest oncological clinic in Russia and Europe, one of the largest oncological clinics in the world, which has the latest equipment and all advanced methods of diagnosis and treatment of cancer.
However, such use of WhatsApp groups as a data collection avenue for survey research is fraught with the following problems: Surveys help us infer the rates in the population from the responses provided by the sample. For the findings to be generalizable, the sample has to be selected from a clearly defined population through random sampling.
NHS managers are destroying the careers of whistleblowers who raise concerns about patient safety, a group of medics warns. More than 50 doctors and nurses have told The Telegraph they have been ...