- Open access
- Published: 24 March 2022

Health care workers’ experiences during the COVID-19 pandemic: a scoping review
- Souaad Chemali 1 ,
- Almudena Mari-Sáez 1 ,
- Charbel El Bcheraoui 2 &
- Heide Weishaar ORCID: orcid.org/0000-0003-1150-0265 2
Human Resources for Health volume 20 , Article number: 27 ( 2022 ) Cite this article
25k Accesses
92 Citations
18 Altmetric
Metrics details
COVID-19 has challenged health systems worldwide, especially the health workforce, a pillar crucial for health systems resilience. Therefore, strengthening health system resilience can be informed by analyzing health care workers’ (HCWs) experiences and needs during pandemics. This review synthesizes qualitative studies published during the first year of the COVID-19 pandemic to identify factors affecting HCWs’ experiences and their support needs during the pandemic. This review was conducted using the Joanna Briggs Institute methodology for scoping reviews. A systematic search on PubMed was applied using controlled vocabularies. Only original studies presenting primary qualitative data were included.
161 papers that were published from the beginning of COVID-19 pandemic up until 28th March 2021 were included in the review. Findings were presented using the socio-ecological model as an analytical framework. At the individual level, the impact of the pandemic manifested on HCWs’ well-being, daily routine, professional and personal identity. At the interpersonal level, HCWs’ personal and professional relationships were identified as crucial. At the institutional level, decision-making processes, organizational aspects and availability of support emerged as important factors affecting HCWs’ experiences. At community level, community morale, norms, and public knowledge were of importance. Finally, at policy level, governmental support and response measures shaped HCWs’ experiences. The review identified a lack of studies which investigate other HCWs than doctors and nurses, HCWs in non-hospital settings, and HCWs in low- and lower middle income countries.
This review shows that the COVID-19 pandemic has challenged HCWs, with multiple contextual factors impacting their experiences and needs. To better understand HCWs’ experiences, comparative investigations are needed which analyze differences across as well as within countries, including differences at institutional, community, interpersonal and individual levels. Similarly, interventions aimed at supporting HCWs prior to, during and after pandemics need to consider HCWs’ circumstances.
Conclusions
Following a context-sensitive approach to empowering HCWs that accounts for the multitude of aspects which influence their experiences could contribute to building a sustainable health workforce and strengthening health systems for future pandemics.
Peer Review reports
Introduction
The COVID-19 pandemic has put health systems worldwide under pressure and tested their resilience. The World Health Organization (WHO) acknowledges health workforce as one of the six building blocks of health systems [ 1 ]. Health care workers (HCWs) are key to a health system’s ability to respond to external shocks such as outbreaks and as first responders are often the hardest hit by these shocks [ 2 ]. Therefore, interventions supporting HCWs are key to strengthening health systems resilience (ibid). To develop effective interventions to support this group, a detailed understanding of how pandemics affect HCWs is needed.
Several recent reviews [ 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 ] focus on HCWs’ experiences during COVID-19 and the impact of the pandemic on HCWs’ well-being, including their mental health [ 3 , 7 , 8 , 11 , 12 , 13 , 14 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 ]. Most of these reviews refer to psychological scales measurements to provide quantifiable information on HCWs’ well-being and mental health [ 8 , 13 , 14 , 19 , 21 , 22 , 23 , 24 , 25 , 28 ]. While useful in assessing the scale of the problem, such quantitative measures are insufficient in capturing the breadth of HCWs’ experiences and the factors that impact such experiences. The added value of qualitative studies is in understanding the complex experiences of HCWs during COVID-19 and the contextual factors that influence them [ 29 ].
This paper reviews qualitative studies published during the first year of the pandemic to investigate what is known about HCWs’ experiences during COVID-19 and the factors and support needs associated with those experiences. By presenting HCWs’ perspectives on the pandemic, the scoping review provides the much-needed evidence base for interventions that can help strengthen HCWs and alleviate the pressures they experience during pandemics.
The review follows the Joanna Briggs Institute (JBI) process and guideline on conducting scoping reviews [ 30 ]. JBI updated guidelines identify scoping reviews as the most suitable choice to explore the breadth of literature on a topic, by mapping and summarizing available evidence [ 30 ]. Scoping reviews are also suitable to address knowledge gaps and provide insightful input for decision-making [ 30 ]. The review also applies the PRISMA checklist guidance on reporting literature reviews [ 31 ].
Information sources
A systematic search was conducted on PubMed database between the 9th and 28th of March 2021.
Search strategy
Drawing on Shaw et al. [ 32 ] and WHO [ 33 ], the search strategy used a controlled vocabulary of index terms including Medical Subject Headings (Mesh) of the keywords and synonyms “COVID-19”, “HCWs”, and “qualitative”. Keywords were combined using the Boolean operator “AND” (see Additional file 1 ).
Eligibility criteria
The population of interest included all types of HCWs, independent of geography and settings. Only original studies were included in the review. Papers further had to (1) report primary qualitative data, (2) report on HCWs’ experiences and perceptions during COVID-19, and (3) be available as full texts in English, German, French, Spanish or Arabic, i.e., in a language that could be reviewed by one or several of the authors. Studies focusing solely on HCWs’ assessment of newly introduced modes of telemedicine during COVID-19 were excluded from the review as their clear emphasis on coping with technical challenges deviated from the review’s focus on HCWs’ personal and professional experiences during the pandemic.
Selection process
The initial search yielded 3976 papers. All papers were screened and assessed against the eligibility criteria by one researcher (SC) to identify relevant studies. A random 25% sample of all papers was additionally screened by a second researcher (HW). Any uncertainty or inconsistency regarding inclusion were resolved by discussing the respective articles ( n = 76) among the authors.
Data collection process
Based on the research question, an initial data extraction form was developed, independently piloted on ten papers by SC and HW and finalised to include information on: (1) author(s), (2) year of publication, (3) type of HCW, (5) study design, (6) sample size, (7) topic of investigation, (8) data collection tool(s), (9) analytical approach, (10) period of data collection, (11) country, (12) income level according to World Bank [ 34 ], (13) context, and (14) main findings related to experiences, factors and support needs. Using the final extraction form, all articles were extracted by SC, with the exception of four German articles (which were extracted by HW), one Spanish and one French article (which were extracted by AMS). As far as applicable, the quality of the included articles was appraised using the JBI critical appraisal tool for qualitative research [ 35 ].
Synthesis methods
The socio-ecological model originally developed by Brofenbrenner was adapted as a framework to analyze and present the findings [ 36 , 37 , 38 ]. The model aims to understand the interconnectedness and dynamics between personal and contextual factors in shaping human development and experiences [ 36 , 38 ]. The model was chosen, because it accounts for the multifaceted interactions between individuals and their environment and is thus suited to capture the different dimensions of HCWs’ experiences, the factors associated with those experiences as well as the sources of support identified. The five socio-ecological levels (individual, interpersonal, institutional, community and policy) of the model served as a framework for analysis and were used to categorise the main themes that were identified in the scoping review as relevant to HCWs’ experiences. The process of identifying the sub-themes was conducted by SC using an excel extraction sheet, in which the main findings were captured and mapped against the socio-ecological framework.
Study selection
The selection process and the number of papers found, screened and included are illustrated in a PRISMA flow diagram (Fig. 1 ). A total of 161 papers were included in the review (see Additional file 2 ). Table 1 lists the included studies based on study characteristics, including type of HCW, healthcare setting, income level of countries studied and data collection tools.
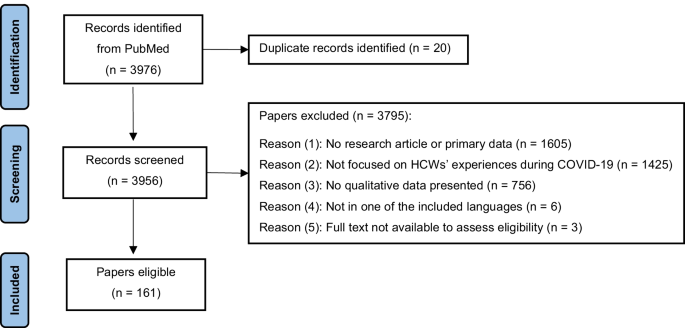
PRISMA flow diagram
Study characteristics
Included papers investigated various types of HCWs. The most investigated type were nurses, followed by doctors/physicians. Medical and nursing students were also studied frequently, while only a small number of studies focused on other professions, e.g., community health workers, therapists and managerial staff. A third of all studies studied multiple HCWs, rather than targeting single professions. The majority of papers investigated so-called “frontline staff”, i.e., HCWs who engaged directly with patients who were suspected or confirmed to be infected with COVID-19. Fewer studies focused on non-frontline staff, and some explored both frontline and non-frontline staff.
Around two-thirds of all papers studied HCWs’ experiences in high-income countries, notably the USA, followed by the UK. Many papers also focused on HCWs in upper-middle income countries, with almost half of them conducted in China. Few papers investigated HCWs in lower-middle income countries, including India, Zimbabwe, Pakistan, Nigeria, and Senegal. Finally, one paper focused on HCWs in Ethiopia, a low-income country. A couple of studies presented data from multiple countries of different income levels, and one study investigating HCWs in Palestine could not be categorised. Overall, the USA was the most studied and China the second most studied geographical location (see Additional file 3 ). Hospitals were by far the most investigated healthcare settings, whereas outpatient settings, including primary care, pharmacies, homes care, nursing homes, healthcare facilities in prisons and schools as well as clinics, were investigated to a considerably lesser extent. Several studies covered more than one setting.
All studies applied a cross-sectional study design, with 54% published in 2020, and the remainder in 2021. A range of qualitative data collection methods were applied, with interviews being by far the most prominent one, followed by open-ended questionnaires. Focus groups and a few other methods including social media, online platforms or recording systems submissions, observations and open reflections were used with rare frequencies. The sample size in studies using interviews ranged between 6 and 450 interviewees. The sample size in studies using Focus Group Discussions (FGDs) ranged between 7 and 40 participants. Further information on the composition and context of the FGDs can be found in additional file 4 . Several studies used multiple data collection tools. The majority of studies applied common analysis methods, including thematic and content analysis, with few using other specific approaches.
Results of syntheses
An overview of the findings based on the socio-ecological framework is summarised in Table 2 , which lists the main sub-themes identified under each socio-ecological level.
Individual level
At the individual level, HCWs’ experiences related to their well-being, professional and personal identity as well as daily work–life routine. In terms of well-being, HCWs reported negative impacts on their physical health (e.g., tiredness, discomfort, skin damage, sleep disorders) [ 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 ] and compromised mental health. The reported negative impact on mental health included increased levels of self-reported stress, depression, anxiety, fear, grief, guilt, anger, isolation, uncertainty and helplessness [ 39 , 41 , 43 , 44 , 45 , 46 , 47 , 49 , 50 , 51 , 52 , 53 , 54 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 ]. The reported reasons for HCWs’ reduced well-being included work-related factors, such as having to adhere to new requirements in the workplace, the lack and/or burden of using Personal Protective Equipment (PPE) [ 41 , 44 , 52 , 63 , 64 , 78 , 93 , 124 , 125 ], increased workload, lack of specialised knowledge and experience, concerns over delivering low quality of care [ 42 , 44 , 49 , 52 , 53 , 63 , 69 , 70 , 73 , 74 , 76 , 78 , 79 , 83 , 84 , 85 , 86 , 89 , 90 , 93 , 94 , 101 , 103 , 109 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 ] and being confronted with ethical dilemmas [ 43 , 72 , 76 , 78 , 136 , 141 , 142 , 143 , 144 , 145 ]. HCWs’ compromised psychological well-being was also triggered by extensive exposure to concerning information via the media and by the pressure that was experienced due to society and the media assigning HCWs hero status [ 53 , 72 , 81 , 92 , 97 , 107 , 139 , 146 ]. Factors that were reported by HCWs as helping them cope with pressure comprised diverse self-care practices and personal activities, including but not limited to psychological techniques and lifestyle adjustments [ 47 , 56 , 64 , 71 , 72 , 78 , 90 , 139 , 147 , 148 ] as well as religious practices [ 81 , 112 , 149 ].
Self-reported well-being differed across occupations, roles in the pandemic response and work settings. One study reported that HCWs working in respiratory, infection and emergency departments expressed more worries compared to HCWs who worked in other hospital wards [ 64 ]. Similarly, frontline HCWs seemed more likely to experience feelings of helplessness and guilt as they witnessed the worsening situation of COVID-19 patients, whereas non-frontline HCWs seemed to experience feelings of guilt due to not supporting their frontline colleagues [ 98 ]. HCWs with managerial responsibility reported heightened concern for their staff’s health [ 75 , 110 , 150 ]. HCWs working in nursing homes and home care reported feelings of being abandoned and not sufficiently recognised [ 75 , 123 , 144 ], while one study investigating HCWs responding to the pandemic in a slums-setting reported fear of violence [ 56 ].
HCWs reported that the pandemic impacted both positively and negatively on their professional and personal identity. While negative emotions were more dominant at the beginning of the pandemic, positive effects were reported to gradually develop after the initial pandemic phase and included an increased sense of motivation, purpose, meaningfulness, pride, resilience, problem-solving attitude, as well as professional and personal growth [ 43 , 44 , 47 , 49 , 50 , 51 , 63 , 67 , 68 , 69 , 71 , 73 , 74 , 75 , 76 , 78 , 79 , 87 , 90 , 91 , 92 , 93 , 98 , 102 , 104 , 112 , 114 , 117 , 118 , 119 , 122 , 124 , 131 , 132 , 143 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 ]. Frontline staff reported particularly strong positive effects related to feelings of making a difference [ 69 , 92 ]. On the other hand, some HCWs reported doubts with regard to their career choices and job dissatisfaction [ 40 , 46 , 59 , 130 ]. Junior staff, assistant doctors and students often reported feelings of exclusion and concerns about the negative effects of the pandemic on their training [ 40 , 162 , 163 ]. Challenges with regard to their professional identity and a sense of failing their colleagues on the frontline were particularly reported by HCWs who had acquired COVID-19 themselves and experienced long COVID-19 [ 121 , 160 , 164 ]. HCWs who reached out to well-being support services expressed concern at being stigmatised [ 97 ].
HCWs reported a work–life imbalance [ 57 , 97 ] as they had to adapt to the disruption of their usual work routine [ 59 , 62 , 131 ]. This disruption manifested in taking on different roles and responsibilities [ 39 , 49 , 67 , 73 , 83 , 89 , 94 , 97 , 110 , 137 , 139 , 144 , 151 ], increased or decreased workload pressure [ 85 , 128 , 130 , 133 ] and sometimes redeployment [ 57 , 155 , 165 ]. HCWs also reported negative financial effects [ 59 , 86 , 166 ].
Interpersonal level
The findings presented in this section relate to HCWs’ perceptions of their relationships in the private and professional environment during the pandemic and to the impact these relationships had on them. With regard to the home environment, HCWs’ concerns over being infected with COVID-19 and transmitting the virus to family members were identified in almost all studies [ 41 , 44 , 48 , 51 , 54 , 56 , 61 , 68 , 75 , 77 , 80 , 85 , 90 , 128 , 139 , 160 , 167 , 168 , 169 , 170 , 171 ]. HCWs living with children or elderly family members were particularly concerned [ 47 , 65 , 95 , 97 , 163 , 172 ]. In some cases, HCWs reported that they had introduced changes to their living situation to protect their loved ones, with some deciding to move out to ensure physical distance and minimise the risk of transmission [ 39 , 43 , 44 , 89 , 105 , 161 ]. Some HCWs reported sharing limited details about their COVID-19-related duties to decrease the anxiety and fear of their significant others [ 81 ]. While in several studies, interpersonal relationships were reported to cause concerns and worries, some study also identified interpersonal relationships and the subsequent emotional connectedness as a helpful resource [ 47 , 173 , 174 ] that could, for example, alleviate anxiety [ 64 ] or provide encouragement for working on the frontline [ 49 , 106 ]. However, interpersonal relationships did not always have a supportive function, with some HCWs reporting being shunned by family and friends [ 66 , 111 , 175 ].
With regard to the work environment, relationships with colleagues were mainly described as supportive and empowering, with various studies reporting the value of teamwork during the pandemic [ 47 , 51 , 52 , 67 , 71 , 77 , 83 , 91 , 97 , 98 , 108 , 134 , 148 , 151 , 161 ]. Challenges with regard to collegial relationships included social distancing (which hindered HCWs’ interaction in the work place) [ 176 ] and working with colleagues one had never worked with before (causing a lack of familiarity with the work environment and difficulties to adapt) [ 79 ]. HCWs who worked in prisons reported interpersonal conflicts due to perceived increased authoritarian behaviour by security personnel that was perceived to manifest in arrogance and non-compliance with hygiene practices [ 88 ].
In terms of HCWs’ relationships with patients, many studies reported challenges in communicating with patients [ 50 , 55 , 126 , 132 , 133 , 172 ]. This was attributed to the use of PPE during medical examinations and care and the reduction of face-to-face visits or a complete switch to telehealth [ 128 , 139 ]. The changes in the relationships with patients varied according to the nature of work. Frontline HCWs, for example, reported challenges in caring for isolated patients [ 41 , 43 , 52 , 148 ], whereas HCWs working in specific settings and occupational roles that required specific interpersonal skills faced other challenges. This was, for example, the case for HCWs working with people with intellectual disabilities, who found it challenging to explain COVID-19 measures to this group and also had to mitigate physical contact that was considered a significant part of their work [ 71 ]. For palliative care staff, the use of PPE and measures of social distancing were challenging to apply with regard to patients and family members [ 177 ]. Building relationships and providing appropriate emotional support was reported to be particularly challenging for mental health and palliative care professionals supporting vulnerable adults or children [ 117 ]. Challenges for health and social care professionals were associated with virtual consultations and more difficult conversations [ 117 ]. Physicians reported particular frustration with remote monitoring of chronic diseases when caring for low-income, rural, and/or elderly patients [ 169 ]. Having to adjust, and compromise on, the relationships with patients caused concerns about the quality of care, which in turn, was reported to impact negatively on HCWs’ professional identity and emotional well-being.
Institutional level
This section presents HCWs’ perceptions of decision-making processes in the work setting, organizational factors and availability of institutional support.
With regard to decision-making, a small number of studies reported HCWs’ trust in the institutions they worked in [ 143 , 172 ], while the majority of studies revealed discontent about institutional leadership and feelings of exclusion from decision-making processes [ 65 , 178 ]. More specifically, HCWs reported a lack of clear communication and coordination [ 41 , 70 , 144 , 148 , 179 ] and a wish to be provided with the rationales behind management decisions and to be included in recovery phase planning [ 48 ]. They perceived centralised decision-making processes as unfamiliar and restrictive [ 150 ]. Instead, HCWs endorsed de-centralised and participatory approaches to communication and decision-making [ 56 ]. Emergency and critical care physicians suggested to include bioethicists as part of the decision-making on triaging scarce critical resources [ 126 ]. Studies of both hospital and primary care settings reported perceived disconnectedness and poor collaboration between managerial, administrative and clinical staff, which was a contributing factor to burnout among HCWs [ 60 , 83 , 149 , 169 , 180 , 181 , 182 ]. Dissatisfaction with communication also related to constantly changing protocols, which were perceived as highly burdening and frustrating, creating ambiguity and negatively affecting HCWs’ work performance [ 44 , 55 , 59 , 78 , 112 , 183 ].
In terms of organizational factors, many HCWs reported a perceived lack of organizational preparedness and poor organization of care [ 60 , 65 , 120 , 179 ]. Changes in the organization of care were perceived as chaotic, especially at the beginning of the pandemic, and changes in roles and responsibilities and role allocation were perceived as unfair and unsatisfying [ 72 , 97 ]. Only in one study, changes in work organisation were perceived positively, with nurses reporting satisfaction with an improved nurse–patient ratio resulting from organisational changes [ 52 ]. Overall, frontline HCWs advocated for more stability in team structure to ensure familiarity and consistency at work [ 47 , 66 , 72 , 114 , 116 ]. HCWs appreciated multidisciplinary teams, despite challenges with regard to achieving rapid and efficient collaboration between members from different departments [ 41 , 143 , 152 ].
Regarding institutional support, in some instances, psychological, managerial, material and technical support was positively acknowledged, while the majority of studies reported HCWs’ dissatisfaction with the support provided by the institution they worked in [ 46 , 48 , 73 , 84 , 92 , 97 , 114 , 139 , 144 , 174 , 184 ]. Across studies, a lack of equipment, including the unavailability of suitable PPEs, was one of the most prominent critiques, especially in the initial phase the pandemic [ 41 , 46 , 54 , 55 , 61 , 69 , 70 , 72 , 73 , 81 , 84 , 85 , 96 , 97 , 111 , 118 , 144 , 147 , 168 ]. In one study of a rural nursing home, HCWs reported being illegally required to treat COVID-19 patients without adequate PPE [ 39 ]. Specialised physicians, such as radiologists, for example, reported that PPE were prioritised for COVID-19 ward workers [ 65 ]. In another instance, HCWs reported that they had taken care of their own mask supply [ 113 ]. Insufficient equipment and the subsequent lack of protection induced fear and anxiety regarding one’s personal safety [ 64 , 87 ]. HCWs also reported inadequate human resources, which had consequences on increased workload [ 44 , 46 , 54 , 69 , 75 , 85 ]. Dissatisfaction with limited infrastructure was reported overall and across settings, but specific limitations were particularly relevant in certain contexts [ 116 ]. HCWs in low resource settings, including Pakistan, Zimbabwe and India, reported worsening conditions regarding infrastructure, characterised by a lack of water supply and ventilation, poor conditions of isolation wards and lack of quality rest areas for staff [ 41 , 58 , 84 ]. Despite adaptive interventions aimed at shifting service delivery to outdoors, procedures such as patient registration and laboratory work took place in poorly ventilated rooms [ 56 ]. Technical support such as the accessibility to specialised knowledge and availability of training were identified by HCWs as an important resource that required strengthening. They advocated for better “tailor-made” trainings in emergency preparedness and response, crisis management, PPE use and infection control [ 41 , 52 , 61 , 68 , 73 , 127 , 144 ]. HCWs argued that the availability of such training would improve their sense of control in health emergencies, while a lack of training compromised their confidence in their ability to provide quality healthcare [ 47 , 134 ].
Structural factors such as power hierarchies and inequalities played a role in HCWs’ perceived sense of institutional support amidst the quick changes in their institutions. Such factors were particularly mentioned in studies investigating nurses who reported dissatisfaction over doctors’ dominance and discrimination in obtaining PPE [ 54 ] as well as unfairness in work allocation [ 72 , 184 ]. They also perceived ambiguity in roles and responsibilities between nurses and doctors [ 101 ]. A low sense of institutional support was also reported by other HCWs. Junior medical staff and administrative staff reported feeling exposed to unacceptable risks of infection and a lack of recognition by their institution [ 139 ]. Staff in non‐clinical roles, non-frontline staff, staff working from home, acute physicians and those on short time contracts felt less supported and less recognised compared to colleagues on the frontline [ 48 , 139 ].
Community level
This level entails how morale and norms, as well as public knowledge relate to HCWs’ experiences in the pandemic. On the positive side, societal morale and norms were perceived as enhancing supportive attitudes among the public toward HCWs and triggering community initiatives that supported HCWs in both emotional and material ways [ 47 , 78 , 92 , 108 , 140 , 147 ]. This supportive element was especially experienced by frontline HCWs, who felt valued, appreciated and empowered by their communities. HCWs’ reaction to the hero status that was assigned to them was ambivalent [ 146 , 185 ]. In response to this status attribution, HCWs reported a sense of pressure to be on the frontline and to work beyond their regular work schedule [ 51 ]. With community support being perceived as clearly focusing on hospital frontline staff, HCWs working from home, in nursing homes, home care and non-frontline facilities and wards perceived less public support [ 139 ] and appreciation [ 85 , 144 ]. One study highlighted that HCWs did not benefit from this form of public praise but preferred an appreciation in the form of tangible and financial resources instead [ 160 ].
A clear negative aspect of social norms manifested in the stigmatisation and negative judgment by community members [ 72 , 100 , 106 , 186 , 187 ], who avoided contact with HCWs based on the perceptions that they were virus carriers and spreaders [ 43 , 68 , 92 , 111 ]. Such discrimination had negative consequences with regard to HCWs’ personal lives, including lack of access to public transportation, supermarkets, childcare and other public services [ 65 , 80 , 107 ]. Chinese HCWs working abroad reported bullying due to others perceiving and labeling COVID-19 as the ‘Chinese virus’ [ 77 ]. Negative judgment was mainly reported in studies on nurses . In a study of a COVID-19-designated hospital, frontline nurses reported unusually strict social standards directed solely at them [ 122 ]. In a comparative study of nursing homes in four countries, geriatric nurses reported social stigma toward their profession, which the society perceive not worth of respect [ 75 ].
Beyond social norms, studies identified the level of public awareness, knowledge and compliance as important determinants of HCWs’ experiences and emotional well-being [ 147 ]. For example, a lack of compliance with social distancing and other preventive measures was reported to induce feelings of betrayal, anger and anxiety among HCWs [ 41 , 80 , 81 , 111 , 188 ]. The dissemination of false information and rumors and their negative influence on knowledge and compliance was also reported with anger by HCWs in general [ 58 ], an in particular by those who worked closely with local communities [ 129 ]. Online resources and voluntary groups facilitated information exchange and knowledge transfer, factors which were valued by HCWs as an important source of information and support [ 131 , 189 ].
Policy level
Findings presented here include HCWs’ perceptions of governmental responses, governmental support and the impact of governmental measures on their professional and private situation. In a small number of studies, HCWs expressed confidence in their government’s ability to respond to the pandemic and satisfaction with governmental compensation [ 45 , 47 ]. In most cases, however, HCWs expressed dissatisfactions with the governmental response, particularly with the lack of health system organisation, the lack of a coordinated, unified response and the failure to follow an evidence-based approach to policy making. HCWs also perceived governmental guidelines as chaotic, confusing and even contradicting [ 61 , 85 , 86 , 115 , 117 , 118 , 120 , 123 , 147 , 160 , 182 , 190 ]. In one study, inadequate staffing was directly attributed to inadequate governmental funding decisions [ 191 ]. Many studies reported that HCWs had a sense of being failed by their governments [ 60 , 100 , 191 ], with non-frontline staff, notably HCWs working with the disabled [ 71 , 181 ], the elderly [ 39 , 75 , 123 , 151 ] or in home-based care [ 58 ], being particularly likely to voice feelings of being forgotten, deprioritised, invisible, less recognised and less valued by their governments. Care home staff perceived governmental support to be unequally distributed across health facilities and as being focused solely on public institutions, which prevented them from receiving state benefits [ 149 ].
Measures and regulations imposed at the governmental level had a considerable impact on HCWs’ professional as well as personal experiences. In nursing homes, HCWs perceived governmental regulations such as visiting restrictions as particularly challenging and complained that rules had not been designed or implemented with consideration to individual cases [ 62 ]. The imposed rules burdened them with additional administrative tasks and forced them to compromise on the quality of care, resulting in moral distress [ 62 ]. In abortion clinics, HCWs expressed concerns about their services being classed as non-essential services during the early stages of the pandemic [ 190 ]. Governmental policies also had impacts on HCWs personally. For example, the closure of childcare negatively impacted HCWs’ ability to balance personal and private roles and commitments. National lockdowns which restricted travel made it harder for HCWs to get to work or to see their families, especially in places with low political stability [ 95 ]. The de-escalation of measures, notably the opening of airports, was perceived as betrayal by HCWs who felt they bore the burden of increased COVID-19 incidences resulting from de-escalation strategies [ 111 ].
HCWs identified clear and consistent governmental crisis communication [ 97 , 126 ], better employees’ rights and salaries, and tailored pandemic preparedness and crisis management policies that considered different healthcare settings and HCWs’ needs [ 43 , 64 , 81 , 101 , 124 , 160 , 167 , 169 , 188 , 192 , 193 ] as important areas for improvement. HCWs in primary care advocated for strengthened primary health care, improved public health education [ 45 , 130 ] and a multi-sectoral approach in pandemic management [ 129 ].
Our scoping review of HCWs’ experiences, support needs and factors that influence these experiences during COVID-19 shows that HCWs were affected at individual, interpersonal, institutional, community and policy levels. It also highlights that certain experiences can have disruptive effects on HCWs’ personal and professional lives, and thus identifies problems which need to be addressed and areas that could be strengthened to support HCWs during pandemics.
To the best of our knowledge, our review is the first to provide a comprehensive account of HCWs’ experiences during COVID-19 across contexts. By applying an exploratory angle and focusing on existing qualitative studies, the review does not only provide a rich description of the situation of HCWs but also develops an in-depth analysis of the contextual multilevel factors which impact on HCWs’ experiences.
Our scoping review shows that, while studies on HCWs’ experiences in low resource settings are scarce, the few studies that exist and the comparison with other studies point towards setting-specific experiences and challenges. We thus argue that understanding HCWs’ experiences requires comparative investigations, which not only take countries’ income levels into account but also other contextual differences. For example, in our analysis, we identify particular challenges experienced by HCWs working in urban slums and places with limited infrastructure and low political stability. Similarly, in a recent short communication in Social Science & Medicine, Smith [ 194 ] presents a case study on the particular challenges of midwives in resource-poor rural Indonesia at the start of the pandemic, highlighting increased risks and intra-country health system inequalities. Contextual intra-country differences in HCWs’ experiences also manifest at institutional level. For example, the review suggests that HCWs who work in non-hospital settings, such as primary care services, nursing homes, home based care or disability services, experienced particular challenges and felt less recognized in relation to hospital-based HCWs. In a similar vein, HCWs working in care homes felt that as state support was not equally distributed, those working in public institutions had better chances to benefit from state support.
The review highlights that occupational hierarchies play a crucial role in HCWs’ work-related experiences. Our analysis suggests that existing occupational hierarchies seem to increase or be exposed during pandemics and that occupation is a structural factor in shaping HCWs’ experiences. The review thus highlights the important role that institutions and employers play in pandemics and is in line with the growing body of evidence that associates HCWs’ well-being during COVID-19 with their occupational role [ 195 ] and the availability of institutional support [ 195 , 196 ]. The findings suggest that to address institutional differences and ensure the provision of needs-based support to all groups of HCWs, non-hierarchical and participative processes of decision-making are crucial.
Another contextual factor affecting HCWs’ experiences are their communities. While the majority of HCWs experience emotional and material support from their community, some also feel pressure by the expectations they are confronted with. The most prominent example of such perceived pressure is the ambivalence that was reported with regard to the assignment of a hero status to HCWs. On the one hand, this attribution meant that HCWs felt recognized and appreciated by their communities. On the other hand, it led to HCWs feeling pressured to work without respecting their own limits and taking care of themselves.
This scoping review points towards a number of research gaps, which, if addressed, could help to hone interventions to support HCWs and improve health system performance and resilience.
First, the majority of existing qualitative studies investigate nurses’ and doctors’ experiences during COVID-19. Given that other types of HCWs play an equally important role in pandemic responses, future research on HCWs’ experiences in pandemics should aim for more diversity and help to tease out the specific challenges and needs of different types of HCWs. Investigating different types of HCWs could inform and facilitate the development of tailored solutions and provide need-based support.
Second, the majority of studies on HCWs’ experiences focus on hospital settings. This is not surprising considering that the bulk of societal and political attention during COVID-19 has been on the provision of acute, hospital-based care. The review thus highlights a gap with regard to research on HCWs in settings which might be considered less affected and neglected but which might, in fact, be severely collaterally affected during pandemics, such as primary health centers, care homes and home-based care. It also indicates that research which compares HCWs’ experiences across levels of care can help to tease out differences and identify specific challenges and needs.
Third, the review highlights the predominance of cross-sectional studies. In fact, we were unable to identify any longitudinal studies of HCWs’ experiences during COVID-19. A possible reason for the lack of longitudinal research is the relatively short time that has passed since the start of the pandemic which might have made it difficult to complete longitudinal qualitative studies. Yet, given the dynamics and extended duration of the pandemic, and knowledge about the impact of persistent stress on an individual’s health and well-being [ 197 , 198 , 199 , 200 ], longitudinal studies on HCWs’ experiences during COVID-19 would provide added value and allow an analysis across different stages of the pandemic as well as post-pandemic times. In our review, three differences in HCWs’ experiences across the phases of the pandemic were observed. The first one is on the individual level, reflecting the dominance of the negative emotions at the initial phase of the pandemic, which was gradually followed by increased reporting of the positive impact on HCWs’ personal and professional identity. The two other differences were on the institutional level, referring to the dissatisfaction over the lack of equipment and organization of care, mainly observed at the initial pandemic phase. Further comparative analysis of changes in HCWs’ experiences over the course of a pandemic is an interesting and important topic for future research, which could also map HCWs’ experiences against hospital capacities, availability of vaccines and tests as well as changes in pandemic restrictions. Such comparative analysis can inform the development of suitable policy level interventions accounting for HCWs’ experiences at different pandemic stages, from preparedness to initial response and recovery.
Finally, the majority of studies included in the review were conducted in the Northern hemisphere, revealing a gap in understanding the reality of HCWs in low- and lower middle income countries. Ensuring diversity in geographies and including resource-poor settings in research on HCWs would help gain a better contextual understanding, contribute to strengthening pandemic preparedness in settings, where the need is greatest, and facilitate knowledge transfer between the global North and South. While further research can help to increase our understanding of HCWs’ experiences during pandemics, this scoping review establishes a first basis for the evaluation and improvement of interventions aimed at supporting HCWs prior to, during and after COVID-19. A key finding of our analysis to strengthen HCWs’ resilience are the interdependencies of factors across the five levels of the socio-ecological model. For example, institutional, community or policy level factors (such as dissatisfaction with decision-making processes, public non-compliance or failures in pandemic management) can have a negative impact on HCWs at interpersonal and individual levels by impacting on their professional relationships, mental health or work performance. Similarly, policy, community or institutional level factors (such as adequate policy measures, appreciation within the community and the provision of PPE and other equipment) can act as protective factors for HCWs’ well-being. In line with the social support literature [ 201 ], interpersonal relationships were identified as a key factor in shaping HCWs’ experiences. The identification of the inter-dependencies between factors affecting HCWs during pandemics further highlights that health systems are severely impacted by factors outside the health systems’ control. Previous scholars have recognized the embeddedness of health systems within, and their constant interaction with, their socio-economic and political environment [ 202 ]. Previous literature, however, also shows that interventions tackling distress of HCWs have largely focused on individual level factors, e.g., on interventions aimed at relieving psychological symptoms, rather than on contextual factors [ 16 ]. To strengthen HCWs and empower them to deal with pandemics, the contextual factors that affect their situation during pandemics need to be acknowledged and interventions need to follow a multi-component approach, taking the multitude of aspects and circumstances into account which impact on HCWs’ experiences.
Limitations and strengths
Our scoping review comes with a number of limitations. First, due to resource constraints, the search was conducted using only one database. The authors acknowledge that running the search strategy on other search engines could have resulted in additional interesting studies to be reviewed. To mitigate any weaknesses, extensive efforts were made to build a strong search string by reviewing previous peer-reviewed publications as well as available resources from recognized public health institutions. Considering the high numbers of studies identified, it can be, however, assumed that the search strategy and review led to valid conclusions. Second, the review excluded non-original publications. While other types of publications could have provided additional data and perspectives on HCWs’ experiences, we decided to limit our review to original, peer-reviewed research articles to ensure quality. Third, the review excluded studies on other pandemics, which could have provided further insights into HCWs’ experiences during health crises. Given the limited resources available to the research project, it was decided to focus only on COVID-19 to accommodate a larger target group of all types of HCWs and a variety of geographical locations and healthcare settings. Furthermore, it can be argued that previous pandemics did not reach the magnitude of COVID-19 and did not lead to similar responses. With the review looking at the burden of COVID-19 as a stressor, it can be assumed that the more important the stressor, the more interesting the results. Therefore, the burdens and the way in which HCWs dealt with these burdens would be particularly augmented with regard to COVID-19, making it a suitable focus example to investigate HCWs’ experiences in health crises. The authors acknowledge that during other pandemics HCWs’ experiences might differ and be less pronounced, yet this review has addressed stressors and ways of supporting HCWs that could also inform future health crises. In our view, a major strength of the review is that is does not apply any limitation in terms of the types of HCWs, the geographical locations or the healthcare settings included. This approach did not only allow us to review a wide range of literature on an expanding area of knowledge [ 30 ], but to appropriately investigate HCWs’ experiences during a public health emergency of international concern that affects countries across the globe. Providing detailed information about the contexts in which HCWs were studied, allowed us to shed light on the contextual factors affecting HCWs’ experiences.
Implications for policy and practice
Areas of future interventions that improve HCWs’ resilience at individual level could aim towards alleviating stress and responding to their specific needs during pandemics, in line with encouraging self-care activities that can foster personal psychological resilience. Beyond that, accounting for the context when designing and implementing interventions is crucial. This can be done by addressing the circumstances HCWs live and work in, referred to in German-speaking countries as “Verhältnisprävention”, i.e., prevention through tackling living and working conditions. Respective interventions should tackle all levels outlined in the socio-ecological model, applying a systems approach. At the interpersonal level, creating a positive work environment in times of crises that is supportive of uninterrupted and efficient communication among HCWs and between HCWs and patients is important. In addition, interpersonal support, e.g., by family and friends could be facilitated. At institutional level, organizational change should consider transparent and participatory decision making and responsible planning of resources availability and allocation. At community level, tracing rumors and misinformation during health emergencies is crucial, as well as advocating for accountable journalism and community initiatives that support HCWs in times of crisis. At policy level, pandemic regulations need to account for their consequences on HCWs’ work situations and personal lives. Governmental policies and guidelines should build on scientific evidence and take into account the situations and lived experiences of HCWs across all levels of care.
This scoping review of existing qualitative research on HCWs’ experiences during COVID-19 sheds light on the impact of a major pandemic on the health workforce, a key pillar of health systems. By identifying key drawbacks, strengths that can be built upon, and crucial entry-points for interventions, the review can inform strategies towards strengthening HCWs and improving their experiences. Following a systems approach which takes the five socio-ecological levels into account is crucial for the development of context-sensitive strategies to support HCWs prior to, during and after pandemics. This in turn can contribute to building a sustainable health workforce and to strengthening and better preparing health systems for future pandemics.
Availability of data and materials
All data generated during this study are included in this published article and its supplementary information files, except for a detailed extraction sheet for all studies included, which is available from the corresponding author upon request.
Abbreviations
- Health care workers
Joanna Briggs Institute
Focus Groups Discussions
Personal Protective Equipment
World Health Organization
World Health Organization. Strengthening health systems to improve health outcomes—WHO framework for action 2007. https://www.who.int/healthsystems/strategy/everybodys_business.pdf?ua=1 . Accessed 29 July 2020.
Hanefeld J, Mayhew S, Legido-Quigley H, Martineau F, Karanikolos M, Blanchet K. Towards an understanding of resilience: responding to health systems shocks. Health Policy Plan. 2018;33(3):355–67.
PubMed PubMed Central Google Scholar
Schwartz R, Sinskey JL, Anand U, Margolis RD. Addressing postpandemic clinician mental health: a narrative review and conceptual framework. Ann Intern Med. 2020;173(12):981–8.
PubMed Google Scholar
Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A, et al. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4(4):CD013582.
Bhaumik S, Moola S, Tyagi J, Nambiar D, Kakoti M. Community health workers for pandemic response: a rapid evidence synthesis. BMJ Glob Health. 2020;5(6): e002769.
Chersich MF, Gray G, Fairlie L, Eichbaum Q, Mayhew S, Allwood B, et al. COVID-19 in Africa: care and protection for frontline healthcare workers. Glob Health. 2020;16(1):46.
Google Scholar
Giorgi G, Lecca LI, Alessio F, Finstad GL, Bondanini G, Lulli LG, et al. COVID-19-related mental health effects in the workplace: a narrative review. Int J Environ Res Public Health. 2020;17(21):7857.
CAS PubMed Central Google Scholar
De Brier N, Stroobants S, Vandekerckhove P, De Buck E. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): a rapid systematic review. PLoS ONE. 2020;15(12): e0244052.
Rieckert A, Schuit E, Bleijenberg N, Ten Cate D, de Lange W, de Man-van Ginkel JM, et al. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open. 2021;11(1): e043718.
Kuek JTY, Ngiam LXL, Kamal NHA, Chia JL, Chan NPX, Abdurrahman A, et al. The impact of caring for dying patients in intensive care units on a physician’s personhood: a systematic scoping review. Philos Ethics Humanit Med. 2020;15(1):12.
Salazar de Pablo G, Vaquerizo-Serrano J, Catalan A, Arango C, Moreno C, Ferre F, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J Affect Disord. 2020;275:48–57.
CAS PubMed PubMed Central Google Scholar
Shreffler J, Petrey J, Huecker M. The impact of COVID-19 on healthcare worker wellness: a scoping review. West J Emerg Med. 2020;21(5):1059–66.
Sanghera J, Pattani N, Hashmi Y, Varley KF, Cheruvu MS, Bradley A, et al. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—a systematic review. J Occup Health. 2020;62(1): e12175.
Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA, Pastor-Moreno G, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. 2020;277:347–57.
Fernandez R, Lord H, Halcomb E, Moxham L, Middleton R, Alananzeh I, et al. Implications for COVID-19: a systematic review of nurses’ experiences of working in acute care hospital settings during a respiratory pandemic. Int J Nurs Stud. 2020;111: 103637.
Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland S, et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res. 2020;293: 113441.
Paiano M, Jaques AE, Nacamura PAB, Salci MA, Radovanovic CAT, Carreira L. Mental health of healthcare professionals in China during the new coronavirus pandemic: an integrative review. Rev Bras Enferm. 2020;73(suppl 2): e20200338.
Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—a review. Asian J Psychiatry. 2020;51: 102119.
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–7.
Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. 2020;18(1):100.
Cénat JM, Blais-Rochette C, Kokou-Kpolou CK, Noorishad PG, Mukunzi JN, McIntee SE, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295: 113599.
da Silva FCT, Neto MLR. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: a systematic review with meta-analysis. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021;104: 110057.
Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—a systematic review and meta-analysis. Psychiatry Res. 2020;291: 113190.
da Silva FCT, Neto MLR. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Progr Neuro-psychopharmacol Biol Psychiatry. 2021;104: 110062.
Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. 2020;22(8):43.
Carmassi C, Foghi C, Dell’Oste V, Cordone A, Bertelloni CA, Bui E, et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 2020;292: 113312.
Chow KM, Law BMH, Ng MSN, Chan DNS, So WKW, Wong CL, et al. A Review of psychological issues among patients and healthcare staff during two major coronavirus disease outbreaks in China: contributory factors and management strategies. Int J Environ Res Public Health. 2020;17(18):6673.
Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293: 113382.
Xiong Y, Peng L. Focusing on health-care providers’ experiences in the COVID-19 crisis. Lancet Glob Health. 2020;8(6):e740–1.
Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–26.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Shaw RL, Booth A, Sutton AJ, Miller T, Smith JA, Young B, et al. Finding qualitative research: an evaluation of search strategies. BMC Med Res Methodol. 2004;4:5.
World Health Organization. Finding public health information: WHO library PubMed cochrane library 2016. https://www.gfmer.ch/SRH-Course-2019/research-methodology/pdf/WHOLibPubMedCochrane-Allen-2019.pdf . Accessed 21 Jan 2021.
World Bank. World development indicators (WDI) 2021. https://databank.worldbank.org/source/world-development-indicators . Accessed 21 July 2021.
Joanna Briggs Institute. Checklist for qualitative research critical appraisal tools for use in JBI systematic reviews 2020. https://jbi.global/sites/default/files/2020-08/Checklist_for_Qualitative_Research.pdf . Accessed 19 May 2021.
Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–31.
Bronfenbrenner U. The Ecology of human development. Cambridge: Harvard University Press; 1979.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77.
CAS PubMed Google Scholar
Leskovic L, Erjavec K, Leskovar R, Vukovič G. Burnout and job satisfaction of healthcare workers in Slovenian nursing homes in rural areas during the COVID-19 pandemic. Ann Agric Environ Med. 2020;27(4):664–71.
Whelehan DF, Connelly TM, Ridgway PF. COVID-19 and surgery: a thematic analysis of unintended consequences on performance, practice and surgical training. Surgeon. 2021;19(1):e20–7.
Haq W, Said F, Batool S, Awais HM. Experience of physicians during COVID-19 in a developing country: a qualitative study of Pakistan. J Infect Dev Ctries. 2021;15(2):191–7.
Okediran JO, Ilesanmi OS, Fetuga AA, Onoh I, Afolabi AA, Ogunbode O, et al. The experiences of healthcare workers during the COVID-19 crisis in Lagos, Nigeria: a qualitative study. Germs. 2020;10(4):356–66.
Muz G, Erdoğan YG. Experiences of nurses caring for patients with COVID-19 in Turkey: a phenomenological enquiry. J Nurs Manag. 2021;29(5):1026–35.
Ardebili ME, Naserbakht M, Bernstein C, Alazmani-Noodeh F, Hakimi H, Ranjbar H. Healthcare providers experience of working during the COVID-19 pandemic: a qualitative study. Am J Infect Control. 2021;49(5):547–54.
Xu Z, Ye Y, Wang Y, Qian Y, Pan J, Lu Y, et al. Primary care practitioners’ barriers to and experience of COVID-19 epidemic control in China: a qualitative study. J Gen Intern Med. 2020;35(11):3278–84.
Yıldırım N, Aydoğan A, Bulut M. A qualitative study on the experiences of the first nurses assigned to COVID-19 units in Turkey. J Nurs Manag. 2021;29(6):1366–74.
Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. 2020;48(6):592–8.
Cubitt LJ, Im YR, Scott CJ, Jeynes LC, Molyneux PD. Beyond PPE: a mixed qualitative–quantitative study capturing the wider issues affecting doctors’ well-being during the COVID-19 pandemic. BMJ Open. 2021;11(3): e050223.
Cui S, Zhang L, Yan H, Shi Q, Jiang Y, Wang Q, et al. Experiences and psychological adjustments of nurses who voluntarily supported COVID-19 patients in Hubei Province, China. Psychol Res Behav Manag. 2020;13:1135–45.
Aksoy H, Ayhan Başer D, Fidancı İ, Arsava EY, Cankurtaran M. Family medicine research assistants’ experiences during COVID-19 pandemic: a qualitative study. Int J Clin Pract. 2020;75: e13975.
Gómez-Ibáñez R, Watson C, Leyva-Moral JM, Aguayo-González M, Granel N. Final-year nursing students called to work: experiences of a rushed labour insertion during the COVID-19 pandemic. Nurse Educ Pract. 2020;49: 102920.
Fernández-Castillo RJ, González-Caro MD, Fernández-García E, Porcel-Gálvez AM, Garnacho-Montero J. Intensive care nurses’ experiences during the COVID-19 pandemic: a qualitative study. Nurs Crit Care. 2021;26(5):397–406.
Alizadeh A, Khankeh HR, Barati M, Ahmadi Y, Hadian A, Azizi M. Psychological distress among Iranian health-care providers exposed to coronavirus disease 2019 (COVID-19): a qualitative study. BMC Psychiatry. 2020;20(1):494.
Moradi Y, Baghaei R, Hosseingholipour K, Mollazadeh F. Challenges experienced by ICU nurses throughout the provision of care for COVID-19 patients: a qualitative study. J Nurs Manag. 2021;29(5):1159–68.
Hoernke K, Djellouli N, Andrews L, Lewis-Jackson S, Manby L, Martin S, et al. Frontline healthcare workers’ experiences with personal protective equipment during the COVID-19 pandemic in the UK: a rapid qualitative appraisal. BMJ Open. 2021;11(1): e046199.
George CE, Inbaraj LR, Rajukutty S, de Witte LP. Challenges, experience and coping of health professionals in delivering healthcare in an urban slum in India during the first 40 days of COVID-19 crisis: a mixed method study. BMJ Open. 2020;10(11): e042171.
Yu JC, McIntyre M, Dow H, Robinson L, Winston P. Changes to rehabilitation service delivery and the associated physician perspectives during the COVID-19 pandemic: a mixed-methods needs assessment study. Am J Phys Med Rehabil. 2020;99(9):775–82.
Mackworth-Young CR, Chingono R, Mavodza C, McHugh G, Tembo M, Chikwari CD, et al. Community perspectives on the COVID-19 response, Zimbabwe. Bull World Health Organ. 2021;99(2):85–91.
Szabo RA, Wilson AN, Homer C, Vasilevski V, Sweet L, Wynter K, et al. Covid-19 changes to maternity care: experiences of Australian doctors. Aust N Z J Obstet Gynaecol. 2021;61(3):408–15.
Bennett P, Noble S, Johnston S, Jones D, Hunter R. COVID-19 confessions: a qualitative exploration of healthcare workers experiences of working with COVID-19. BMJ Open. 2020;10(12): e043949.
Collado-Boira EJ, Ruiz-Palomino E, Salas-Media P, Folch-Ayora A, Muriach M, Baliño P. “The COVID-19 outbreak”—an empirical phenomenological study on perceptions and psychosocial considerations surrounding the immediate incorporation of final-year Spanish nursing and medical students into the health system. Nurse Educ Today. 2020;92: 104504.
Sizoo EM, Monnier AA, Bloemen M, Hertogh C, Smalbrugge M. Dilemmas with restrictive visiting policies in dutch nursing homes during the COVID-19 pandemic: a qualitative analysis of an open-ended questionnaire with elderly care physicians. J Am Med Dir Assoc. 2020;21(12):1774-81.e2.
Chen F, Zang Y, Liu Y, Wang X, Lin X. Dispatched nurses’ experience of wearing full gear personal protective equipment to care for COVID-19 patients in China—a descriptive qualitative study. J Clin Nurs. 2021;30(13–14):2001–14.
Fang M, Xia B, Tian T, Hao Y, Wu Z. Drivers and mediators of healthcare workers’ anxiety in one of the most affected hospitals by COVID-19: a qualitative analysis. BMJ Open. 2021;11(3): e045048.
Foley SJ, O’Loughlin A, Creedon J. Early experiences of radiographers in Ireland during the COVID-19 crisis. Insights Imaging. 2020;11(1):104.
Crowe S, Howard AF, Vanderspank-Wright B, Gillis P, McLeod F, Penner C, et al. The effect of COVID-19 pandemic on the mental health of Canadian critical care nurses providing patient care during the early phase pandemic: a mixed method study. Intensive Crit Care Nurs. 2020;63: 102999.
Palacios-Ceña D, Fernández-de-Las-Peñas C, Florencio LL, de-la-Llave-Rincón AI, Palacios-Ceña M. Emotional experience and feelings during first COVID-19 outbreak perceived by physical therapists: a qualitative study in Madrid, Spain. Int J Environ Res Public Health. 2020;18(1):127.
PubMed Central Google Scholar
Urooj U, Ansari A, Siraj A, Khan S, Tariq H. Expectations, fears and perceptions of doctors during Covid-19 pandemic. Pak J Med Sci. 2020;36(Covid19-s4):S37–42.
Kaur R, Kaur A, Kumar P. An experience of otorhinolaryngologists as frontline worker with novel coronavirus: a qualitative analysis. Indian J Otolaryngol Head Neck Surg. 2021. https://doi.org/10.1007/s12070-021-02369-3 .
Article PubMed Google Scholar
González-Timoneda A, Hernández Hernández V, Pardo Moya S, Alfaro Blazquez R. Experiences and attitudes of midwives during the birth of a pregnant woman with COVID-19 infection: a qualitative study. Women Birth. 2020;34(5):465–72.
Embregts P, Tournier T, Frielink N. Experiences and needs of direct support staff working with people with intellectual disabilities during the COVID-19 pandemic: a thematic analysis. J Appl Res Intell Disabil. 2021;34(2):480–90.
Kackin O, Ciydem E, Aci OS, Kutlu FY. Experiences and psychosocial problems of nurses caring for patients diagnosed with COVID-19 in Turkey: a qualitative study. Int J Soc Psychiatry. 2020;67(2):158–67.
Tan R, Yu T, Luo K, Teng F, Liu Y, Luo J, et al. Experiences of clinical first-line nurses treating patients with COVID-19: a qualitative study. J Nurs Manag. 2020;28(6):1381–90.
Liu YE, Zhai ZC, Han YH, Liu YL, Liu FP, Hu DY. Experiences of front-line nurses combating coronavirus disease-2019 in China: a qualitative analysis. Public Health Nurs. 2020;37(5):757–63.
Sarabia-Cobo C, Pérez V, de Lorena P, Hermosilla-Grijalbo C, Sáenz-Jalón M, Fernández-Rodríguez A, et al. Experiences of geriatric nurses in nursing home settings across four countries in the face of the COVID-19 pandemic. J Adv Nurs. 2021;77(2):869–78.
Billings J, Biggs C, Ching BCF, Gkofa V, Singleton D, Bloomfield M, et al. Experiences of mental health professionals supporting front-line health and social care workers during COVID-19: qualitative study. BJPsych Open. 2021;7(2): e70.
Song J, McDonald C. Experiences of New Zealand registered nurses of Chinese ethnicity during the COVID-19 pandemic. J Clin Nurs. 2020;30(5–6):757–64.
LoGiudice JA, Bartos S. Experiences of nurses during the COVID-19 pandemic: a mixed-methods study. AACN Adv Crit Care. 2021;32(1):e1–13.
CoşkunŞimşek D, Günay U. Experiences of nurses who have children when caring for COVID-19 patients. Int Nurs Rev. 2021;68(2):219–27.
Galehdar N, Kamran A, Toulabi T, Heydari H. Exploring nurses’ experiences of psychological distress during care of patients with COVID-19: a qualitative study. BMC Psychiatry. 2020;20(1):489.
Munawar K, Choudhry FR. Exploring stress coping strategies of frontline emergency health workers dealing Covid-19 in Pakistan: a qualitative inquiry. Am J Infect Control. 2021;49(3):286–92.
Nyashanu M, Pfende F, Ekpenyong M. Exploring the challenges faced by frontline workers in health and social care amid the COVID-19 pandemic: experiences of frontline workers in the English Midlands region. UK J Interprof Care. 2020;34(5):655–61.
Gemine R, Davies GR, Tarrant S, Davies RM, James M, Lewis K. Factors associated with work-related burnout in NHS staff during COVID-19: a cross-sectional mixed methods study. BMJ Open. 2021;11(1): e042591.
Raza A, Matloob S, Abdul Rahim NF, Abdul Halim H, Khattak A, Ahmed NH, et al. Factors impeding health-care professionals to effectively treat coronavirus disease 2019 patients in Pakistan: a qualitative investigation. Front Psychol. 2020;11: 572450.
White EM, Wetle TF, Reddy A, Baier RR. Front-line nursing home staff experiences during the COVID-19 pandemic. J Am Med Dir Assoc. 2021;22(1):199–203.
Shalhub S, Mouawad NJ, Malgor RD, Johnson AP, Wohlauer MV, Coogan SM, et al. Global vascular surgeons’ experience, stressors, and coping during the coronavirus disease 2019 pandemic. J Vasc Surg. 2021;73(3):762-771.e4.
Lapum J, Nguyen M, Fredericks S, Lai S, McShane J. “Goodbye … through a glass door”: emotional experiences of working in COVID-19 acute care hospital environments. Can J Nurs Res = Revue canadienne de recherche en sciences infirmieres. 2020;53(1):5–15.
Testoni I, Francioli G, Biancalani G, Libianchi S, Orkibi H. Hardships in Italian prisons during the COVID-19 emergency: the experience of healthcare personnel. Front Psychol. 2021;12: 619687.
Ness MM, Saylor J, Di Fusco LA, Evans K. Healthcare providers’ challenges during the coronavirus disease (COVID-19) pandemic: a qualitative approach. Nurs Health Sci. 2021;23(2):389–97.
Mayfield-Johnson S, Smith DO, Crosby SA, Haywood CG, Castillo J, Bryant-Williams D, et al. Insights on COVID-19 from community health worker state leaders. J Ambul Care Manag. 2020;43(4):268–77.
He Q, Li T, Su Y, Luan Y. Instructive messages and lessons from Chinese countermarching nurses of caring for COVID-19 patients: a qualitative study. J Transcult Nurs. 2021;32(2):96–102.
DeliktasDemirci A, Oruc M, Kabukcuoglu K. ‘It was difficult, but our struggle to touch lives gave us strength’: the experience of nurses working on COVID-19 wards. J Clin Nurs. 2020;30(5–6):732–41.
Fontanini R, Visintini E, Rossettini G, Caruzzo D, Longhini J, Palese A. Italian nurses’ experiences during the COVID-19 pandemic: a qualitative analysis of internet posts. Int Nurs Rev. 2021;68(2):238–47.
Comfort AB, Krezanoski PJ, Rao L, El Ayadi A, Tsai AC, Goodman S, et al. Mental health among outpatient reproductive health care providers during the US COVID-19 epidemic. Reprod Health. 2021;18(1):49.
Maraqa B, Nazzal Z, Zink T. Mixed method study to explore ethical dilemmas and health care workers’ willingness to work amid COVID-19 pandemic in Palestine. Front Med. 2020;7: 576820.
Gesser-Edelsburg A, Cohen R, Shahbari NAE, Hijazi R. A mixed-methods sequential explanatory design comparison between COVID-19 infection control guidelines’ applicability and their protective value as perceived by Israeli healthcare workers, and healthcare executives’ response. Antimicrob Resist Infect Control. 2020;9(1):148.
Feeley T, Ffrench-O’Carroll R, Tan MH, Magner C, L’Estrange K, O’Rathallaigh E, et al. A model for occupational stress amongst paediatric and adult critical care staff during COVID-19 pandemic. Int Arch Occup Environ Health. 2021;94(7):1–17.
Shaw C, Gallagher K, Petty J, Mancini A, Boyle B. Neonatal nursing during the COVID-19 global pandemic: a thematic analysis of personal reflections. J Neonatal Nurs. 2021;27(3):165–71.
García-Martín M, Roman P, Rodriguez-Arrastia M, Diaz-Cortes MDM, Soriano-Martin PJ, Ropero-Padilla C. Novice nurse”s transitioning to emergency nurse during COVID-19 pandemic: a qualitative study. J Nurs Manag. 2021;29(2):258–67.
Arnetz JE, Goetz CM, Arnetz BB, Arble E. Nurse reports of stressful situations during the COVID-19 pandemic: qualitative analysis of survey responses. Int J Environ Res Public Health. 2020;17(21):8126.
Jia Y, Chen O, Xiao Z, Xiao J, Bian J, Jia H. Nurses’ ethical challenges caring for people with COVID-19: a qualitative study. Nurs Ethics. 2021;28(1):33–45.
Danielis M, Peressoni L, Piani T, Colaetta T, Mesaglio M, Mattiussi E, et al. Nurses’ experiences of being recruited and transferred to a new sub-intensive care unit devoted to COVID-19 patients. J Nurs Manag. 2021;29(5):1149–58.
Gao X, Jiang L, Hu Y, Li L, Hou L. Nurses’ experiences regarding shift patterns in isolation wards during the COVID-19 pandemic in China: a qualitative study. J Clin Nurs. 2020;29(21–22):4270–80.
Zhang MM, Niu N, Zhi XX, Zhu P, Wu B, Wu BN, et al. Nurses’ psychological changes and coping strategies during home isolation for the 2019 novel coronavirus in China: a qualitative study. J Adv Nurs. 2021;77(1):308–17.
Arcadi P, Simonetti V, Ambrosca R, Cicolini G, Simeone S, Pucciarelli G, et al. Nursing during the COVID-19 outbreak: a phenomenological study. J Nurs Manag. 2021;29(5):1111–9.
KalatehSadati A, Zarei L, Shahabi S, Heydari ST, Taheri V, Jiriaei R, et al. Nursing experiences of COVID-19 outbreak in Iran: a qualitative study. Nurs Open. 2020;8(1):72–9.
Ohta R, Matsuzaki Y, Itamochi S. Overcoming the challenge of COVID-19: a grounded theory approach to rural nurses’ experiences. J Gen Fam Med. 2020;22(3):134–40.
Vindrola-Padros C, Andrews L, Dowrick A, Djellouli N, Fillmore H, Bautista Gonzalez E, et al. Perceptions and experiences of healthcare workers during the COVID-19 pandemic in the UK. BMJ Open. 2020;10(11): e040503.
Banerjee D, Vajawat B, Varshney P, Rao TS. Perceptions, experiences, and challenges of physicians involved in dementia care during the COVID-19 lockdown in India: a qualitative study. Front Psychiatry. 2020;11: 615758.
White JH. A phenomenological study of nurse managers’ and assistant nurse managers’ experiences during the COVID-19 pandemic in the United States. J Nurs Manag. 2021;29(6):1525–34.
Gunawan J, Aungsuroch Y, Marzilli C, Fisher ML, Nazliansyah, Sukarna A. A phenomenological study of the lived experience of nurses in the battle of COVID-19. Nurs Outlook. 2021;69(4):652–9.
Norful AA, Rosenfeld A, Schroeder K, Travers JL, Aliyu S. Primary drivers and psychological manifestations of stress in frontline healthcare workforce during the initial COVID-19 outbreak in the United States. Gen Hosp Psychiatry. 2021;69:20–6.
Moradi Y, Baghaei R, Hosseingholipour K, Mollazadeh F. Protective reactions of ICU nurses providing care for patients with COVID-19: a qualitative study. BMC Nurs. 2021;20(1):45.
Zhang Y, Wei L, Li H, Pan Y, Wang J, Li Q, et al. The psychological change process of frontline nurses caring for patients with COVID-19 during its outbreak. Issues Ment Health Nurs. 2020;41(6):525–30.
Fawaz M, Itani M. The psychological experiences of Lebanese ground zero front-line nurses during the most recent COVID-19 outbreak post Beirut blast: a qualitative study. Int J Soc Psychiatry. 2021. https://doi.org/10.1177/00207640211004989 .
Zerbini G, Ebigbo A, Reicherts P, Kunz M, Messman H. Psychosocial burden of healthcare professionals in times of COVID-19—a survey conducted at the University Hospital Augsburg. German Med Sci. 2020;18:Doc05.
Aughterson H, McKinlay AR, Fancourt D, Burton A. Psychosocial impact on frontline health and social care professionals in the UK during the COVID-19 pandemic: a qualitative interview study. BMJ Open. 2021;11(2): e047353.
Lee RLT, West S, Tang ACY, Cheng HY, Chong CYY, Chien WT, et al. A qualitative exploration of the experiences of school nurses during COVID-19 pandemic as the frontline primary health care professionals. Nurs Outlook. 2020;69(3):399–408.
Paula ACR, Carletto AGD, Lopes D, Ferreira JC, Tonini NS, Trecossi SPC. Reactions and feelings of health professionals in the care of hospitalized patients with suspected covid-19. Revista gaucha de enfermagem. 2021;42(spe): e20200160.
Iheduru-Anderson K. Reflections on the lived experience of working with limited personal protective equipment during the COVID-19 crisis. Nurs Inquiry. 2021;28(1): e12382.
Taylor AK, Kingstone T, Briggs TA, O’Donnell CA, Atherton H, Blane DN, et al. ‘Reluctant pioneer’: a qualitative study of doctors’ experiences as patients with long COVID. Health Expect. 2021;24(3):833–42.
Lee N, Lee HJ. South Korean nurses’ experiences with patient care at a COVID-19-designated hospital: growth after the frontline battle against an infectious disease pandemic. Int J Environ Res Public Health. 2020;17(23):9015.
Nyashanu M, Pfende F, Ekpenyong MS. Triggers of mental health problems among frontline healthcare workers during the COVID-19 pandemic in private care homes and domiciliary care agencies: lived experiences of care workers in the Midlands region, UK. Health Soc Care Community. 2020;30(2):e370–6.
Galehdar N, Toulabi T, Kamran A, Heydari H. Exploring nurses’ perception of taking care of patients with coronavirus disease (COVID-19): a qualitative study. Nurs Open. 2021;8(1):171–9.
Arasli H, Furunes T, Jafari K, Saydam MB, Degirmencioglu Z. Hearing the voices of wingless angels: a critical content analysis of nurses’ COVID-19 experiences. Int J Environ Res Public Health. 2020;17(22):8484.
Mulla A, Bigham BL, Frolic A, Christian MD. Canadian emergency medicine and critical care physician perspectives on pandemic triage in COVID-19. J Emerg Manag. 2020;18(7):31–5.
Ortiz Z, Antonietti L, Capriati A, Ramos S, Romero M, Mariani J, et al. Concerns and demands regarding COVID-19. Survey of health personnel. Medicina. 2020;80(Suppl 3):16–24.
Monzani A, Ragazzoni L, Della Corte F, Rabbone I, Franc JM. COVID-19 pandemic: perspective from italian pediatric emergency physicians. Disaster Med Public Health Prep. 2020;14(5):648–51.
Al Ghafri T, Al Ajmi F, Anwar H, Al Balushi L, Al Balushi Z, Al Fahdi F, et al. The experiences and perceptions of health-care workers during the COVID-19 pandemic in Muscat, Oman: a qualitative study. J Prim Care Community Health. 2020;11:2150132720967514.
Yin Y, Chu X, Han X, Cao Y, Di H, Zhang Y, et al. General practitioner trainees’ career perspectives after COVID-19: a qualitative study in China. BMC Fam Pract. 2021;22(1):18.
Foye U, Dalton-Locke C, Harju-Seppänen J, Lane R, Beames L, Vera San Juan N, et al. How has Covid-19 affected mental health nurses and the delivery of mental health nursing care in the UK? Results of a mixed methods study. J Psychiatr Ment Health Nurs. 2021;28(2):126–37.
Goh YS, Ow Yong QYJ, Chen TH, Ho SHC, Chee YIC, Chee TT. The impact of COVID-19 on nurses working in a University Health System in Singapore: a qualitative descriptive study. Int J Ment Health Nurs. 2020;30(3):643–52.
Verhoeven V, Tsakitzidis G, Philips H, Van Royen P. Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open. 2020;10(6): e039674.
Travers JL, Schroeder K, Norful AA, Aliyu S. The influence of empowered work environments on the psychological experiences of nursing assistants during COVID-19: a qualitative study. BMC Nurs. 2020;19:98.
Semaan A, Audet C, Huysmans E, Afolabi B, Assarag B, Banke-Thomas A, et al. Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Glob Health. 2020;5(6): e002967.
Begerow A, Michaelis U, Gaidys U. Wahrnehmungen von Pflegenden im Bereich der Intensivpflege während der COVID-19-Pandemie. Pflege. 2020;33(4):229–36.
Santos J, Balsanelli AP, Freitas EO, Menegon FHA, Carneiro IA, Lazzari DD, et al. Work environment of hospital nurses during the COVID-19 pandemic in Brazil. Int Nurs Rev. 2021;68(2):228–37.
Fan J, Jiang Y, Hu K, Chen X, Xu Q, Qi Y, et al. Barriers to using personal protective equipment by healthcare staff during the COVID-19 outbreak in China. Medicine. 2020;99(48): e23310.
Digby R, Winton-Brown T, Finlayson F, Dobson H, Bucknall T. Hospital staff well-being during the first wave of COVID-19: staff perspectives. Int J Ment Health Nurs. 2020;30(2):440–50.
Nelson H, Hubbard Murdoch N, Norman K. The role of uncertainty in the experiences of nurses during the Covid-19 pandemic: a phenomenological study. Can J Nurs Res = Revue canadienne de recherche en sciences infirmieres. 2021;53(2):124–33.
Patterson JE, Edwards TM, Griffith JL, Wright S. Moral distress of medical family therapists and their physician colleagues during the transition to COVID-19. J Marital Fam Ther. 2021;47(2):289–303.
Palinkas LA, Whiteside L, Nehra D, Engstrom A, Taylor M, Moloney K, et al. Rapid ethnographic assessment of the COVID-19 pandemic April 2020 ‘surge’ and its impact on service delivery in an Acute Care Medical Emergency Department and Trauma Center. BMJ Open. 2020;10(10): e041772.
Hou Y, Zhou Q, Li D, Guo Y, Fan J, Wang J. Preparedness of our emergency department during the coronavirus disease outbreak from the nurses’ perspectives: a qualitative research study. J Emerg Nurs. 2020;46(6):848-861.e1.
Sterling MR, Tseng E, Poon A, Cho J, Avgar AC, Kern LM, et al. Experiences of home health care workers in New York City during the coronavirus disease 2019 pandemic: a qualitative analysis. JAMA Intern Med. 2020;180(11):1453–9.
Butler CR, Wong SPY, Wightman AG, O’Hare AM. US clinicians’ experiences and perspectives on resource limitation and patient care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(11): e2027315.
Halberg N, Jensen PS, Larsen TS. We are not heroes—the flipside of the hero narrative amidst the COVID19-pandemic: a Danish hospital ethnography. J Adv Nurs. 2021;77(5):2429–36.
Hennein R, Lowe S. A hybrid inductive-abductive analysis of health workers’ experiences and wellbeing during the COVID-19 pandemic in the United States. PLoS ONE. 2020;15(10): e0240646.
Casafont C, Fabrellas N, Rivera P, Olivé-Ferrer MC, Querol E, Venturas M, et al. Experiences of nursing students as healthcare aid during the COVID-19 pandemic in Spain: a phemonenological research study. Nurse Educ Today. 2021;97: 104711.
Bilal A, Saeed MA, Yousafzai T. Elderly care in the time of coronavirus: perceptions and experiences of care home staff in Pakistan. Int J Geriatr Psychiatry. 2020;35(12):1442–8.
Butler CR, Wong SPY, Vig EK, Neely CS, O’Hare AM. Professional roles and relationships during the COVID-19 pandemic: a qualitative study among US clinicians. BMJ Open. 2021;11(3): e047782.
Williams CM, Couch A, Haines T, Menz HB. Experiences of Australian podiatrists working through the 2020 coronavirus (COVID-19) pandemic: an online survey. J Foot Ankle Res. 2021;14(1):11.
Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health. 2020;8(6):e790–8.
Härter M, Bremer D, Scherer M, von dem Knesebeck O, Koch-Gromus U. Impact of COVID-19-pandemic on clinical care, work flows and staff at a University Hospital: results of an interview-study at the UKE. Gesundheitswesen (Bundesverband der Arzte des Offentlichen Gesundheitsdienstes (Germany)). 2020;82(8–09):676–81.
Sheng Q, Zhang X, Wang X, Cai C. The influence of experiences of involvement in the COVID-19 rescue task on the professional identity among Chinese nurses: a qualitative study. J Nurs Manag. 2020;28(7):1662–9.
Donnelly C, Ashcroft R, Bobbette N, Mills C, Mofina A, Tran T, et al. Interprofessional primary care during COVID-19: a survey of the provider perspective. BMC Fam Pract. 2021;22(1):31.
Losty LS, Bailey KD. Leading through chaos: perspectives from nurse executives. Nurs Adm Q. 2021;45(2):118–25.
Catania G, Zanini M, Hayter M, Timmins F, Dasso N, Ottonello G, et al. Lessons from Italian front-line nurses’ experiences during the COVID-19 pandemic: a qualitative descriptive study. J Nurs Manag. 2020;29(3):404–11.
Daphna-Tekoah S, MegadasiBrikman T, Scheier E, Balla U. Listening to hospital personnel’s narratives during the COVID-19 outbreak. Int J Environ Res Public Health. 2020;17(17):6413.
Fan J, Hu K, Li X, Jiang Y, Zhou X, Gou X, et al. A qualitative study of the vocational and psychological perceptions and issues of transdisciplinary nurses during the COVID-19 outbreak. Aging. 2020;12(13):12479–92.
Missel M, Bernild C, Dagyaran I, Christensen SW, Berg SK. A stoic and altruistic orientation towards their work: a qualitative study of healthcare professionals’ experiences of awaiting a COVID-19 test result. BMC Health Serv Res. 2020;20(1):1031.
Pravder HD, Langdon-Embry L, Hernandez RJ, Berbari N, Shelov SP, Kinzler WL. Experiences of early graduate medical students working in New York hospitals during the COVID-19 pandemic: a mixed methods study. BMC Med Educ. 2021;21(1):118.
de Wit K, Mercuri M, Wallner C, Clayton N, Archambault P, Ritchie K, et al. Canadian emergency physician psychological distress and burnout during the first 10 weeks of COVID-19: a mixed-methods study. J Am College Emerg Physicians Open. 2020;1(5):1030–8.
Kuliukas L, Hauck Y, Sweet L, Vasilevski V, Homer C, Wynter K, et al. A cross sectional study of midwifery students’ experiences of COVID-19: uncertainty and expendability. Nurse Educ Pract. 2021;51: 102988.
Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, et al. Developing services for long COVID: lessons from a study of wounded healers. Clin Med. 2021;21(1):59–65.
Searby A, Burr D. The impact of COVID-19 on alcohol and other drug nurses’ provision of care: a qualitative descriptive study. J Clin Nurs. 2021;30(11–12):1730–41.
Hower KI, Pfaff H, Pförtner TK. Pflege in Zeiten von COVID-19: onlinebefragung von Leitungskräften zu Herausforderungen. Belastungen und Bewältigungsstrategien Pflege. 2020;33(4):207–18.
He K, Stolarski A, Whang E, Kristo G. Addressing general surgery residents’ concerns in the early phase of the COVID-19 pandemic. J Surg Educ. 2020;77(4):735–8.
Góes FGB, Silva A, Santos A, Pereira-Ávila FMV, Silva LJD, Silva LFD, et al. Challenges faced by pediatric nursing workers in the face of the COVID-19 pandemic. Rev Lat Am Enfermagem. 2020;28: e3367.
Halley MC, Mathews KS, Diamond LC, Linos E, Sarkar U, Mangurian C, et al. The intersection of work and home challenges faced by physician mothers during the coronavirus disease 2019 pandemic: a mixed-methods analysis. J Women’s Health. 2021;30(4):514–24.
Algunmeeyn A, El-Dahiyat F, Altakhineh MM, Azab M, Babar ZU. Understanding the factors influencing healthcare providers’ burnout during the outbreak of COVID-19 in Jordanian hospitals. J Pharm Policy Pract. 2020;13:53.
Sougou NM, Diouf JB, Diallo AA, Seck I. Risk perception of COVID-19 pandemic among health care providers: qualitative study conducted at the King Baudoin Hospital in Guédiawaye, the first hospital faced with managing a community-acquired COVID-19 case in Senegal. Pan Afr Med J. 2020;37(Suppl 1):23.
Conlon C, McDonnell T, Barrett M, Cummins F, Deasy C, Hensey C, et al. The impact of the COVID-19 pandemic on child health and the provision of care in paediatric emergency departments: a qualitative study of frontline emergency care staff. BMC Health Serv Res. 2021;21(1):279.
Bender AE, Berg KA, Miller EK, Evans KE, Holmes MR. “Making sure we are all okay”: healthcare workers’ strategies for emotional connectedness during the COVID-19 pandemic. Clin Soc Work J. 2021;49(4):1–11.
Yin X, Zeng L. A study on the psychological needs of nurses caring for patients with coronavirus disease 2019 from the perspective of the existence, relatedness, and growth theory. Int J Nurs Sci. 2020;7(2):157–60.
Creese J, Byrne JP, Conway E, Barrett E, Prihodova L, Humphries N. “We all really need to just take a breath”: composite narratives of hospital doctors’ well-being during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(4):2051.
Silies K, Schley A, Sill J, Fleischer S, Müller M, Balzer K. Die COVID-19-Pandemie im akutstationären Setting aus Sicht von Führungspersonen und Hygienefachkräften in der Pflege - Eine qualitative Studie. Pflege. 2020;33(5):289–98.
Tremblay-Huet S, McMorrow T, Wiebe E, Kelly M, Hennawy M, Sum B. The impact of the COVID-19 pandemic on medical assistance in dying in Canada and the relationship of public health laws to private understandings of the legal order. J Law Biosci. 2020;7(1): lsaa087.
Geremia DS, Vendruscolo C, Celuppi IC, Adamy EK, Toso B, Souza JB. 200 years of Florence and the challenges of nursing practices management in the COVID-19 pandemic. Rev Lat Am Enfermagem. 2020;28: e3358.
Kurotschka PK, Serafini A, Demontis M, Serafini A, Mereu A, Moro MF, et al. General practitioners’ experiences during the first phase of the COVID-19 pandemic in Italy: a critical incident technique study. Front Public Health. 2021;9: 623904.
Renaa T, Brekke M. Restructuring in a GP practice during the COVID-19 pandemic—a focus-group study. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke. 2021. https://doi.org/10.4045/tidsskr.20.0713 .
Article Google Scholar
Desroches ML, Ailey S, Fisher K, Stych J. Impact of COVID-19: nursing challenges to meeting the care needs of people with developmental disabilities. Disabil Health J. 2021;14(1): 101015.
Damian AJ, Gonzalez M, Oo M, Anderson D. A national study of community health centers’ readiness to address COVID-19. J Am Board Fam Med. 2021;34(Suppl):S85–94.
Schroeder K, Norful AA, Travers J, Aliyu S. Nursing perspectives on care delivery during the early stages of the covid-19 pandemic: a qualitative study. Int J Nurs Stud Adv. 2020;2: 100006.
Cho H, Sagherian K, Steege LM. Hospital nursing staff perceptions of resources provided by their organizations during the COVID-19 pandemic. Workplace Health Saf. 2021;69(4):174–81.
Hennekam S, Ladge J, Shymko Y. From zero to hero: an exploratory study examining sudden hero status among nonphysician health care workers during the COVID-19 pandemic. J Appl Psychol. 2020;105(10):1088–100.
He J, Liu L, Chen X, Qi B, Liu Y, Zhang Y, et al. The experiences of nurses infected with COVID-19 in Wuhan, China: a qualitative study. J Nurs Manag. 2021;29(5):1180–8.
Fawaz M, Samaha A. The psychosocial effects of being quarantined following exposure to COVID-19: a qualitative study of Lebanese health care workers. Int J Soc Psychiatry. 2020;66(6):560–5.
Mersha A, Shibiru S, Girma M, Ayele G, Bante A, Kassa M, et al. Perceived barriers to the practice of preventive measures for COVID-19 pandemic among health professionals in public health facilities of the Gamo zone, southern Ethiopia: a phenomenological study. BMC Public Health. 2021;21(1):199.
Austin Z, Gregory P. Resilience in the time of pandemic: the experience of community pharmacists during COVID-19. Res Soc Adm Pharm. 2021;17(1):1867–75.
Roberts SCM, Schroeder R, Joffe C. COVID-19 and independent abortion providers: findings from a rapid-response survey. Perspect Sex Reprod Health. 2020;52(4):217–25.
Brophy JT, Keith MM, Hurley M, McArthur JE. Sacrificed: Ontario healthcare workers in the time of COVID-19. New Solut. 2021;30(4):267–81.
Ilesanmi OS, Afolabi AA, Akande A, Raji T, Mohammed A. Infection prevention and control during COVID-19 pandemic: realities from health care workers in a north central state in Nigeria. Epidemiol Infect. 2021;149: e15.
Halcomb E, Williams A, Ashley C, McInnes S, Stephen C, Calma K, et al. The support needs of Australian primary health care nurses during the COVID-19 pandemic. J Nurs Manag. 2020;28(7):1553–60.
Smith C. The structural vulnerability of healthcare workers during COVID-19: observations on the social context of risk and the equitable distribution of resources. Soc Sci Med. 2020;258: 113119.
Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Glob Health. 2020;16(1):89.
Labrague LJ, De Los Santos JAA. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag. 2020;28(7):1653–61.
Abdallah CG, Geha P. Chronic pain and chronic stress: two sides of the same coin? Chronic Stress. 2017. https://doi.org/10.1177/2470547017704763 .
Article PubMed PubMed Central Google Scholar
Vachon-Presseau E. Effects of stress on the corticolimbic system: implications for chronic pain. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):216–23.
Salvagioni DAJ, Melanda FN, Mesas AE, González AD, Gabani FL, Andrade SM. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS ONE. 2017;12(10): e0185781.
Hapke U, Maske UE, Scheidt-Nave C, Bode L, Schlack R, Busch MA. Chronic stress among adults in Germany: results of the German health interview and examination survey for adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56(5–6):749–54.
Killgore WDS, Taylor EC, Cloonan SA, Dailey NS. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020;291: 113216.
Karl B, Sara LN, Ben R, Francisco P-M. Governance and capacity to manage resilience of health systems: towards a new conceptual framework. Int J Health Policy Manag. 2017;6(8):431–5.
Download references
Acknowledgements
Not applicable.
Open Access funding enabled and organized by Projekt DEAL. The study was funded by the German Federal Ministry of Health (Bundesministerium für Gesundheit, BMG).
Author information
Authors and affiliations.
Centre for International Health Protection, Robert Koch Institute, Nordufer 20, 13353, Berlin, Germany
Souaad Chemali & Almudena Mari-Sáez
Evidence-Based Public Health, Centre for International Health Protection, Robert Koch Institute, Nordufer 20, 13353, Berlin, Germany
Charbel El Bcheraoui & Heide Weishaar
You can also search for this author in PubMed Google Scholar
Contributions
HW and AMS conceived and designed the scoping review. SC extracted, analyzed and conceptualized the data as well as drafted the initial version of this manuscript. HW and AMS provided quality checks for the methodology and analysis. HW, AMS and CEB substantively revised each version of the manuscript and provided substantial inputs. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Heide Weishaar .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
: Table S1. Search strategy. The document includes the search strings for the review.
Additional file 2
: Table S2. List of included papers. The file lists the 161 included papers, detailing the title, authors, publication year and DOI link.
Additional file 3
: Table S3. List of countries studied. The file includes a table listing the countries in which the included studies were conducted according to frequency.
Additional file 4
: Table S4. Detailed information on FGDs. This document provides information extracted from studies that used FGDs as a qualitative data collection tool. The table lists the overall number of focus group discussion’s participants in each of those studies, the number of FGDs per study, whether FGDs were conducted online or offline, the type of study participants, and any other information on the methods that could be extracted.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chemali, S., Mari-Sáez, A., El Bcheraoui, C. et al. Health care workers’ experiences during the COVID-19 pandemic: a scoping review. Hum Resour Health 20 , 27 (2022). https://doi.org/10.1186/s12960-022-00724-1
Download citation
Received : 23 September 2021
Accepted : 09 March 2022
Published : 24 March 2022
DOI : https://doi.org/10.1186/s12960-022-00724-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Experiences
- Health systems
Human Resources for Health
ISSN: 1478-4491
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 21 June 2024
Professional quality of life and job satisfaction among nurses working at tertiary hospitals in central Ethiopia
- Sentayehu Admasu Saliya 1 ,
- Taye Mezgebu Ashine 1 ,
- Asnakech Zekiwos Heliso 1 ,
- Getachew Ossabo Babore 1 ,
- Bethelhem Birhanu 1 &
- Awoke Girma Hailu 1
BMC Nursing volume 23 , Article number: 417 ( 2024 ) Cite this article
199 Accesses
Metrics details
Professional quality of life is a crucial aspect of healthcare professionals’ well-being and job satisfaction. Job satisfaction, on the other hand, encompasses fulfillment of desired needs within the work environment, happiness or gratifying emotional response towards working conditions, and job values or equity. Existing literature tends to address job satisfaction and professional quality of life separately, overlooking their interconnectedness, especially within the unique context of Ethiopia. This study aimed to assess nurses’ professional quality of life and job satisfaction.
A descriptive cross-sectional study was conducted from September 1–30 2023 among 420 nurses using a structured questionnaire. The study participants were recruited by simple random sampling. Multiple linear regressions were used to identify factors associated with outcome variables.
The study involved 420 nurses, with 407 completing the questionnaire, yielding a 96.68% response rate. The findings revealed varying levels of professional quality of life. Specifically, 258 participants (63.4%) exhibited low compassion satisfaction, while 271 (66.6%) and 266 (65.4%) experienced average levels of burnout and secondary traumatic stress, respectively. Job satisfaction was moderate to high for 55% of the participants. As the finding of this study indicates, there is a positive correlation between compassion satisfaction and job satisfaction in nursing. The study also identified predictors for job satisfaction, compassion satisfaction, and compassion fatigue, such as marital status, education, and experience.
The majority of participants reported a medium level of compassion satisfaction, with a significant proportion experiencing moderate to high levels of compassion fatigue. Although more than half of the participants had moderate to high job satisfaction, there were still low levels of satisfaction. The study recommends developing targeted training programs, implementing workplace policies, and designing initiatives to enhance education, experience, and compassion satisfaction.
Peer Review reports
Introduction
The standard of patient care and the well-being of healthcare professionals are significantly impacted by professional quality of life and job satisfaction in the nursing profession [ 1 ].
A nurse’s job-related satisfaction is impacted by both their favorable and detrimental daily work experiences [ 2 ]. Compassion Satisfaction is a positive aspect of professional quality of life, whereas Compassion Fatigue is a negative aspect. Two factors contribute to compassion fatigue. Burnout, which includes tiredness, frustration, rage, and despair that are usually connected to one’s job, is the first element. The second element is secondary trauma stress, which is an uncomfortable feeling brought on by fear and trauma at work [ 3 ].
In the nursing field, job satisfaction was characterized by three aspects: the ability to meet needs in the workplace, happiness or a positive emotional reaction to working conditions, and employment equity or values [ 4 ].
In the nursing context, these two elements are intricately interrelated, as the emotional demands and stressors inherent in the profession directly impact the overall job satisfaction of nurses [ 5 ]. The emotional toll of empathetic caregiving can have a significant impact on a nurse’s general well-being. Excessive compassion fatigue can have negative effects on one’s physical and mental health, while high levels of compassion satisfaction are linked to job satisfaction and general well-being [ 6 ].
Burnout, compassion fatigue, and workload pressures are among the key contributors to diminished professional quality of life and job satisfaction in nursing [ 7 ]. The study from the United States indicates compassion satisfaction is positively correlated with job satisfaction [ 8 ]. Studies have indicated that individuals who provide support to others who have had traumatic stressors may be more susceptible to negative symptoms of depression, burnout, and post-traumatic stress disorder [ 9 , 10 , 11 , 12 ]. On the other hand high level of job satisfaction has a positive effect on a high level of professional quality [ 13 ]. Job satisfaction is crucial to prevent burnout. It is defined as a “syndrome resulting from chronic workplace stress that was not properly addressed” [ 14 ].
In Ethiopia, the national pooled prevalence of job satisfaction among health professionals is 46.17% [ 15 ], However, there is a significant variation in job satisfaction levels across different regions of the country. For instance, the study conducted in the Amhara region reported a high level of job satisfaction among health professionals, with a mean score of 57.5 [ 16 ] On the other hand, a cross-sectional study in the Oromia region found that only 16.5% of health professionals were satisfied with their jobs.
In contrast, studies have reported moderate levels of compassion fatigue among health professionals in Ethiopia [ 17 ]. Similarly, a study conducted in South Africa, Turkey Saudi Arabia, and the United States reported moderate levels of compassion fatigue among healthcare providers [ 10 , 11 , 18 , 19 ]. Studies from Latvia indicate there was a positive correlation between compassion fatigue and secondary traumatic stress [ 20 ].
Achieving the best possible patient outcomes depends on nursing practitioners who feel satisfied with their work [ 1 ]. A significant positive relationship was observed between compassion satisfaction and clinical competence [ 21 ]. Nurses with higher levels of compassion satisfaction and lower levels of compassion fatigue and secondary traumatic stress tend to have higher levels of clinical competencies [ 22 ].
Altruism and the satisfaction that comes from being able to help others might be seen as the positive sides of helping. The degree of the painful content that the caregiver is exposed to such as direct contact with victims exacerbates the negative impacts of caregiving, especially when the exposure is ugly and explicit. Burnout, depression, increased substance use, and symptoms of posttraumatic stress disorder are possible effects [ 9 ].
Despite the abundance of individual studies on job satisfaction [ 15 , 16 , 23 , 24 ] and professional quality of life [ 17 , 25 ] in various occupational sectors in Ethiopia, there is a lack of comprehensive exploration that consolidates these two critical dimensions into a single study.
The existing body of literature tends to address job satisfaction and professional quality of life separately, overlooking the interconnectedness between these facets, especially within the unique context of Ethiopia, especially in nursing. This gap highlights the need for a comprehensive investigation that not only identifies the distinct contributors to job satisfaction and professional quality of life but also explores their synergies and interdependencies within the Ethiopian work environment. A study was conducted to assess professional quality of life and job satisfaction among nurses working in tertiary hospitals in central Ethiopia.
Objective To assess nurses’ professional quality of life and level of job satisfaction among nurses working at tertiary hospitals in central Ethiopia in 2023.
Study design and period
The institution-based cross-sectional was conducted from September 1–30, 2023.
The study was carried out in tertiary-level hospitals in central, Ethiopia. The region is organized into 6 zones and three special woredas on an administrative level. In the region, there are 3 tertiary-level hospitals; Wolikite University Hospital, Wachemo University Hospital, and Worabe Hospital. About 539 nurses were working in those hospitals. Worabe Hospital is located 172 km south of Ethiopia’s capital city, Addis Ababa, in Worabe, a town. There are 112 nurses in the hospital at Worabe Hospital. Wachemo University Hospital Referral is in Hossaena town, 232 km south of Addis Ababa, Ethiopia’s capital city. There are 287 nurses in total at the Wachemo University Hospital. Wolikite University Hospital is located 158 km from Addis Ababa, Ethiopia’s capital. There are 140 nurses in total at the Wolikite University Hospital.
The source population was all nurses working at tertiary level hospitals of central Ethiopia and the study population was all sampled nurses who were working at tertiary level hospitals in central Ethiopia, 2023.
Eligibility criteria
All nurses who were working at tertiary-level hospitals in central Ethiopia, in 2023 were included in the study and nurses who were sick, unable to respond, and on annual leave were excluded from the study.
Sample size determination
The sample size was calculated using a single population proportion calculation that takes into account the following factors: 95% confidence interval, 46.68% proportion [ 26 ], and a margin of error of 5%.
\(N = (1.96)2 * \frac{{0.4801(1 - .0.4801)}}{{0.05 * 0.05}}\) = 382 a total of 420 is obtained by adding a 10% non-response rate.
Sampling technique
The total sample size was proportionally distributed based on the number of nurses working in each academic tertiary hospital as shown in the figure below (Fig. 1 ).
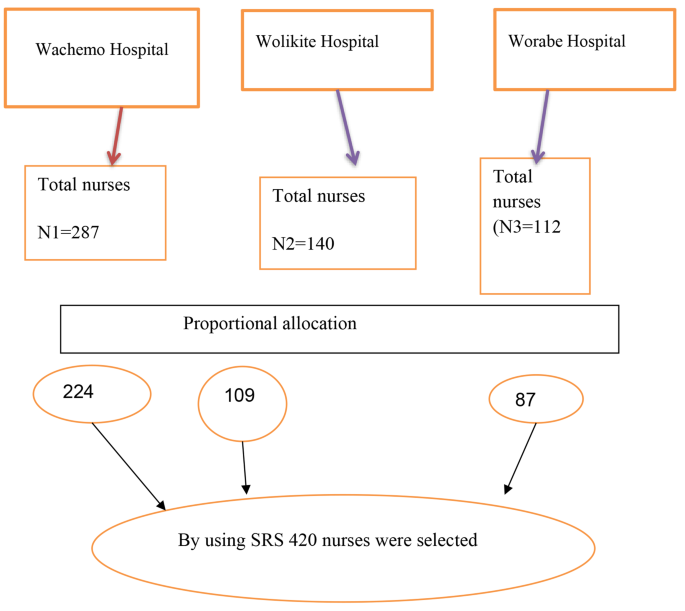
Sampling procedure to select study participants from tertiary level Hospitals in central, Ethiopia 2023
Ni = proportional sample size for each hospital.
Nh = total number of nurses in each hospital.
Nt = overall number of nurses in the hospital.
N = estimated sample size.
Then, the sampling frame was prepared for each hospital by having lists of nurses from the hospital’s human resource management. Finally, nurses of each hospital were selected by a simple random sampling technique using a computer-generated random number from the sampling frame.
Data collection tool and procedure
Data were collected using pre-tested, structured, and self-administered questionnaires which were adopted from previous Ethiopian studies [ 24 , 27 , 28 ]. The questionnaire was written in English and then translated into Amharic, with questions retranslated back into English for consistency. The questionnaire was divided into socio-demographic, Minnesota Satisfaction scale, and professional quality of life scale.
A pre-test was conducted in Hawassa University’s Comprehensive Specialized Hospital two weeks before the actual data collection time on 10%(42 nurses) of the sample size.
The Minnesota Satisfaction Questionnaire (MSQ) short form was used to assess job satisfaction [ 29 , 30 , 31 ]. Twenty questions were rated on a 5-point Likert scale, with 1 signifying severely dissatisfied and 5 denoting very satisfied. Negative items were reversed to positive before summing. The measuring items on nurses’ job satisfaction were achievement, advancement, work itself, recognition, growth at work, organization policy, relationship with colleagues and supervisor, payment, and working conditions. The overall score of the questionnaire ranges from 20 to 100 so the score ranges of 20–47, 48–76, and 77–100 indicate a low, moderate, and high level of job satisfaction, respectively [ 32 ].
The reliability test in the previous study revealed that the tool for the subscale was reliable, with a Cronbach’s alpha score of 0.83 [ 14 ], in this study reliability test value was acceptable with Cronbach’s alpha of 0.891. The mean score was calculated after checking the normality of the distribution.
The professional quality of life scale contains 30 items and the scale has 3 sub-scales [ 33 ]: Compassion satisfaction, secondary traumatic stress, and burnout scale. The secondary traumatic stress subscale and burnout subscale measure compassion fatigue. The scale was measured using a point Likert scale (5 = very often to 1 = never) [ 34 ]. The higher the score of compassion satisfaction, the higher the compassion satisfaction, the higher the score of compassion fatigue, and the higher the risk of compassion fatigue.
Dependent and independent variables of the study
Dependent variable.
Job Satisfaction.
Professional quality of life.
Independent variables
Socio-demographic factors.
Educational level
marital status
work experience
Operational definition
- Job satisfaction
The questionnaire’s total score ranges from 20 to 100, with scores in the three categories of 20–47, 48–76, and 77–100, representing low, moderate, and high levels of job satisfaction, respectively [ 32 ].
A score of 22 or less indicated a low degree of burnout, a score between 23 and 41 indicated an intermediate level of burnout, and a score of 42 or above indicated a severe level of burnout [ 35 ].
Secondary traumatic stress
A score of 22 or a low level; a score between 23 and 41 an average level, and a score of 42 or more indicated a high level of Secondary traumatic stress [ 35 ].
- Compassion satisfaction
A score of 22 or less low level, a between 22 and 41 is an average level, and a score of 42 or more indicates a high level of Compassion satisfaction [ 35 ].
Data management and analysis
After the data were checked for consistency and completeness, data were entered into EpiData version 4.6 and exported to SPSS (Statistical Package for Social Sciences) version 26 for analysis. Tables, graphs, and charts were used to interpret and show the results. Those that were associated with outcome variables in bivariate analysis at P values of 0.25 or lower were included in the multivariable linear regression model. We then performed tests for multicollinearity, including variance inflation factor reports and condition number tests because of the potentially high overlap between the explanatory variables; for example, age and work experience, and gender and profession. Age and years of work experience variables were highly collinear and age was removed from explanatory variables. We report regression coefficients for these models. Variables with estimated coefficients that had P values ≤ 0.05 were considered statistically significant associated factors in this study.
Ethical consideration
Ethical clearance was obtained from the Wachemo University College of Medicine and Health Science, with reference number IRB/172/16. Written informed consent was approved by the Wachemo University College of Medicine and Health Science Institutional Review Board. Written informed consent was obtained from all study participants. To protect participants from risks, the study did not record participants’ names, identification numbers, and names of health facilities where he or she worked.
Socio-demographic data
The questionnaires were distributed to the 420 sampled nurses working in tertiary-level hospitals. Four hundred-seven (407) nurses returned the questionnaires, indicating a 96.9% response rate. The participants were between 20 and 41 years old, with a mean age of 30.85 and an SD of 6.39. The respondents predominantly were between the ages of 25 to 29 years. The majority of 220 (54.1%) respondents were female. In terms of marital status, 204 (50.1%) study participants were single. Most respondents, 298 (73.2%), had a BSc degree in nursing. The majority of study participants 248 (60.9%) had less than five years of work experience. The average monthly income of respondents was 888.43, with a minimum of 5000 and a maximum income of 13,000 Ethiopian Birr (Table 1 ).
- Professional quality of life
The mean compassion satisfaction score among study participants was found to be 26.34 ± 9.38, with a minimum score of 10.00 and a maximum score of 47.00 [ 1 ]. On the other hand, the mean compassion fatigue score was significantly higher at 55.26 ± 18.80, with a minimum score of 20.00 and a maximum score of 93.00.
The results suggest that the average mean score of compassion satisfaction was lower than the mean score of compassion fatigue, indicating that most of the study participants experienced lower compassion satisfaction. This finding is concerning, as compassion satisfaction is an essential factor in maintaining the well-being and mental health of healthcare providers see (Table 2 ).
The findings of our study indicate that 258 (63.4%%) of the participants were found to have low levels of compassion satisfaction. Our study finding indicates the level of burnout and secondary traumatic stress is mainly average with 271(66.6%) and 266(65.4) respectively as shown in Table 3 .
The statement “I am pleased with how I can keep up with helping techniques and protocols” had the highest agreement level in the study, with 153 responses (37.6%) indicating often and 127 responses (31.2%) indicating sometimes. The statement “I get satisfaction from being able to help people” has the lowest agreement level in the study, with 116 responses (28.5%) indicating Sometimes and 98 responses (24.1%) indicating Often. The statement “I feel invigorated after working with those I help” has the highest disagreement level in the study, with 153 responses (37.6%) indicating often and 71 responses (17.4%) indicating “never.” The statement “I believe I can make a difference through my work” had the lowest disagreement level in the study, with 85 responses (20.9%) indicating often and 2 responses (0.5%) indicating always as shown in (Table 4 ).
- Compassion fatigue
The statement “I avoid certain activities or situations because they remind me of frightening experiences of the people I help” had the highest agreement level in the study, with 114 responses (28.0%) indicating often and 122 responses (30.0%) indicating sometimes. The statement “I feel as though I am experiencing the trauma of someone I have helped” has the lowest agreement level in the study, with 136 responses (33.4%) indicating often and 70 responses (17.2%) indicating never. The highest level of disagreement in the study was The statement “I feel depressed because of the traumatic experiences of the people” has the highest disagreement level, with 152 responses (37.3%) indicating Sometimes and 56 responses (13.8%) indicating Often. “The statement with the lowest agreement levels in the study was, “I think that I might have been affected by the traumatic stress of those I help.” has the lowest disagreement level, with 53 responses (13.0%) indicating often and 2 responses (0.5%) indicating always as shown in (Table 5 ).
The statement “I feel trapped by my job as a helper” has the highest agreement level in the study, with 132 responses (32.4%) indicating “Sometimes” and 98 responses (24.1%) indicating Often. The statement “I am the person I always wanted to be” had the lowest agreement level, with 152 responses (37.3%) indicating often and 43 responses (10.6%) indicating always. The highest disagreement levels in the study were The statement “I feel overwhelmed because my case workload seems endless” has the highest disagreement level, with 127 responses (31.2%) indicating often and 1 response (0.2%) indicating always. lowest disagreement levels, the statement “I feel happy” has the lowest disagreement level, with 152 responses (37.3%) indicating Sometimes and 56 responses (13.8%) indicating Often as shown in (Table 6 ).
The study found that the overall mean score for job satisfaction among healthcare providers was 27.46 ± 9.86. This score falls within the moderate range of job satisfaction, indicating that healthcare providers in the study reported a moderate level of satisfaction with their jobs.
Furthermore, the study found that 55% of healthcare providers reported a moderate to high level of job satisfaction. There is still room for improvement, as the overall mean score for job satisfaction falls within the moderate range.
as shown in (Fig. 2 ).
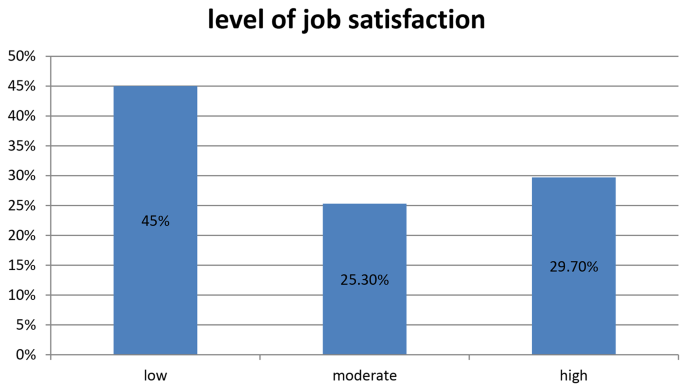
level of job satisfaction of nurses working at tertiary level hospitals in central Ethiopia, 2023
Job satisfaction various conditions revealed that the nurses working in academic tertiary hospitals were satisfied with five factors: satisfaction in achievement (0.73449), advancement (1.4263 (0.69797), autonomy (1.6454 (0.69723), the recognition they get for good work (2.7232 (1.06691), leadership and organizational policy (2.2973 (0.96494), salary and working conditions (2.0511 (0.75966) and relationship (3.2973 (0.98667)) (Table 2 ). According to the mean score of each, the nurses working in academic tertiary hospitals were dissatisfied with the remaining fifteen factors. The highest level of dissatisfaction was reported for the opportunity for training or education at 1.36 (0.503). This was followed by a house allowance of 1.53 (0.749), hazard allowance for nurses of 1.93 (0.259), availability of resources and supplies of 2.17 (0.800), feeling about the job itself of 2.85 (1.319), and Salary (3.20 ± 1.535), respectively as shown in the (Table 7 ).
Correlation between compassion fatigue and job satisfaction
The finding of our study indicates compassion satisfaction and job satisfaction are strongly correlated, with a Pearson’s correlation coefficient of 0.762 and a p -value of 0.001. This indicates that there is a significant relationship between compassion satisfaction and job satisfaction among the nurses in the study. This strong correlation signifies a meaningful and significant relationship between compassion satisfaction and job satisfaction within the study cohort. This finding underscores the interconnectedness of these two factors and highlights the importance of addressing both compassion satisfaction and job satisfaction to enhance the overall well-being and job performance of nurses. as shown in the (Table 8 ).
Multiple linear regression analysis for compassion satisfaction and compassion fatigue
For Compassion fatigue, the results showed that marital status had a negative relationship with the outcome variable, with a standardized beta coefficient of − 0.127, indicating that participants who were not married had higher levels of compassion fatigue. The educational level also had a negative relationship with the outcome variable, with a standardized beta coefficient of − 0.269, indicating that participants with lower levels of education had higher levels of compassion fatigue. For compassion satisfaction, the results showed that marital status had a negative relationship with the outcome variable, with a standardized beta coefficient of − 0.132, indicating that participants who were not married had lower levels of compassion satisfaction. educational level also had a negative relationship with the outcome variable, with a standardized beta coefficient of − 0.244 and a, indicating that participants with lower levels of education had lower levels of compassion satisfaction as shown in (Table 9 ).
Multiple linear regression analysis job satisfaction
The results showed that educational level had a positive relationship with the outcome variable, with a standardized beta coefficient of 0.088 and a t-value of 2.712, indicating that participants with higher levels of education had higher levels of job satisfaction. Experience in a year had a negative relationship with the outcome variable, with a standardized beta coefficient of − 0.094 and a t-value of -2.740, indicating that participants with more years of experience had lower levels of job satisfaction as shown in (Table 10 ).
This study was conducted to assess levels of professional quality of life and job satisfaction among nurses working at tertiary hospitals in central Ethiopia.
The finding of our study indicates that 64.1%% of the participants were found to have moderate to high levels of compassion satisfaction. Only 0.7% of the study participants have a high level of compassion satisfaction. This is lower than the study from China oncology nurses [ 36 ], 668, Guangzhou, Guangdong, China, 78% [ 37 ], a study from Nepal [ 38 ] with, a moderate level of compassion satisfaction is 71.3%, and a high-level compassion satisfaction 28.3%, Saudi Arabia, in which high of compassion satisfaction is 17.7% [ 35 ], a study from Thailand 75.3% [ 39 ], Northwest Ethiopia especially those on the high level of compassion satisfaction aspect in this study is 32.7% [ 27 ].
The discrepancies in studies can be attributed to various factors, including differences in sample size, for example, sample size from China oncology nurses [ 36 ], sample size 668, Guangzhou, Guangdong, China, its sample size 337 [ 37 ], and the specific population of nurses being studied.
This study indicated level of compassion fatigue is 124(30.5%), 275(67.6%), 5(0.5%) low, moderate and high level satisfaction respectively. Concerning components like burnout and secondary traumatic stress those who have moderate to high levels of burnout and secondary traumatic stress are 67%0.2,66.9% respectively.
The finding is consistent with a study from China on component burnout 63% and lower on secondary traumatic stress 76% component [ 37 ]. A similar study from a China frontline nurse in Wuhan [ 40 ] was higher than a study from Saud Arabia [ 35 ] in which the compassion fatigue level was 18% and burnout level 15%. Lower than the study from Nepal in which the level of compassion fatigue was moderate at 77% high level of 3.5% [ 38 ], a study from Uganda reported 49.11% high levels, 29.62% reported average levels, and 21.27% low levels of compassion fatigue [ 41 ]. Studies from oncology nurses also reported a high level of compassion fatigue and a low level of compassion satisfaction [ 34 ].
In our study, nurses working in central Ethiopia, have a moderate to high level of job satisfaction is 55%. This finding is consistent with other studies in Ethiopia like; a study from Jimma Ethiopia, with overall job satisfaction of [ 28 ], Bahir Dar Ethiopia [ 24 ], Ethiopia [ 42 ], and Ethiopian national pooled prevalence of job satisfaction [ 43 ], and lower than study from USA 2018 national sample survey of registered nurses, which 88.7% either extremely or moderately satisfied. Reasons for low level could be poor job conditions and limited resources [ 44 ], limited opportunities for career development, a combination of financial and non-financial incentives, and lack of motivation through incentives such as bonuses, house allowances, and salary increments [ 45 ].
The finding of our study indicates compassion satisfaction and job satisfaction are strongly correlated, with a Pearson’s correlation coefficient of 0.762 and a p -value of 0.001. This indicates that there is a significant relationship between compassion satisfaction and job satisfaction among nurses. This finding is in line with a study from the USA [ 8 ]. High levels of compassion satisfaction and job satisfaction can contribute to the overall well-being of nurses. Nurses’ satisfaction directly impacts the quality of care they provide to patients.
In this study, marital status had a negative relationship with the outcome variable, with a standardized beta coefficient of − 0.127 and a t-value of -2.779, indicating that participants who were not married had higher levels of compassion fatigue. The educational level also had a negative relationship with the outcome variable, with a standardized beta coefficient of − 0.269 and a t-value of -5.573, indicating that participants with lower levels of education had higher levels of compassion fatigue. This finding is consistent with a study from Turkey that found that being single or divorced and not having children were related to the highest levels of burnout in nurses [ 46 ].
The finding of our study indicates; that marital status and educational level were predictor variables for both compassion satisfaction and compassion fatigue.
This finding suggests that being married may serve as a protective factor against the development of compassion fatigue. This could be due to various reasons. For example, married individuals may have access to emotional support from their partners, which can help them cope with the emotional demands of their work. They may also have a stronger support system in general, including family and friends, which can contribute to their overall well-being and resilience. On the other hand, the negative relationship between educational level and compassion fatigue suggests that individuals with lower levels of education may be more susceptible to experiencing compassion fatigue. This could be attributed to several factors. For instance, individuals with lower levels of education may have limited access to resources and support systems that can help them cope with the emotional demands of their work. They may also have fewer opportunities for professional development and self-care, which can contribute to higher levels of emotional exhaustion.
For Compassion satisfaction, the results showed that marital status had a negative relationship with the outcome variable, with a standardized beta coefficient of − 0.132 and a t-value of -2.887, indicating that participants who were not married had lower levels of compassion satisfaction. educational level also had a negative relationship with the outcome variable, with a standardized beta coefficient of − 0.244 and a t-value of -5.043, indicating that participants with lower levels of education had lower levels of compassion satisfaction. This finding is consistent with systematic review and meta-analysis of oncology nurses [ 34 ].
The finding from our study indicates; that educational level has a positive relationship with nurses’ job satisfaction, with a standardized beta coefficient of 0.88. which indicates that participants with a higher level of education status had increased satisfaction with their jobs. On the other hand; experience in a year has a negative relationship with job satisfaction, with a standardized coefficient of -0.094 and a a t-value of -2.74. the finding was in line with study from Ethiopia [ 47 ] and Slovenia [ 34 ].
A study on the impact of broadcasting mistake management culture found that organizations that prioritize the quality of work life (QWL) of their personnel, which can include factors like educational opportunities, tend to have higher job satisfaction levels [ 48 ]. Another study on nursing home residents found that having more choice and control over relocation was associated with higher psychological well-being, which can be related to job satisfaction [ 49 ].
Conclusion and recommendations
The study aimed to assess the levels of professional quality of life and job satisfaction among nurses working at tertiary hospitals in central Ethiopia. The majority of participants reported a medium level of compassion satisfaction, with a significant proportion experiencing moderate to high levels of compassion fatigue. Although more than half of the participants had moderate to high job satisfaction, there were still low levels of satisfaction. The study also identified predictors for compassion satisfaction and compassion fatigue, such as marital status, education, and experience, providing valuable insights into factors influencing professionals’ well-being. The strong correlation between compassion satisfaction and job satisfaction underscores the interconnectedness of these factors in nursing. Addressing the factors that contribute to satisfaction is essential for promoting the well-being of nurses and ensuring high-quality patient care. The study recommends developing targeted training programs, implementing workplace policies, and designing initiatives to enhance education, experience, and compassion satisfaction.
Strength and limitation
The results of this study provide fresh knowledge and reflect the state of nurse professional quality of life and job satisfaction in tertiary hospitals of central Ethiopia. The sample was taken randomly, which nearly represented the population under the study. However, this study employed a cross-sectional study design and it was not possible to ascertain the temporal relationships between the outcome and explanatory variables.
Data availability
The dataset used and analyzed during the current study will be available from the corresponding author upon reasonable request.
Abbreviations
Compassion Satisfaction
Compassion Fatigue
Professional Quality of Life
Adjusted OD Ratio
Confidence Interval
Alshammari MH, Alenezi A. Nursing workforce competencies and job satisfaction: the role of technology integration, self-efficacy, social support, and prior experience. BMC Nurs. 2023;22(1):308.
Article PubMed PubMed Central Google Scholar
Sodeke-Gregson EA, Holttum S, Billings J. Compassion satisfaction, burnout, and secondary traumatic stress in UK therapists who work with adult trauma clients. Eur J Psychotraumatology. 2013;4(1):21869.
Article Google Scholar
Serra N, Botti S, Guillari A, Simeone S, Latina R, Iacorossi L, et al. Workload, job satisfaction and quality of Nursing Care in Italy: a systematic review of native Language Articles. Healthc (Basel). 2023;11:18.
Google Scholar
Liu Y, Aungsuroch Y, Yunibhand J. Job satisfaction in nursing: a concept analysis study. Int Nurs Rev. 2016;63(1):84–910020.
Article CAS PubMed Google Scholar
Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Satele DV et al. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2017. (1942–5546 (Electronic)).
Van Puyvelde M, Van Herck J, Van den Bossche J, Goethals F, Gijbels D, Detaille F et al. Walk the line: a systemic perspective on stress experienced by emergency medical personnel by comparing military and civilian prehospital settings. (2296–565 (Electronic)).
Taylor CA-O, Scott EJ, Owen K. Physical activity, burnout and quality of life in medical students: a systematic review. (1743-498X (Electronic)).
Sessions LC, Ness M, Mark H, Yang BK. Nursing Faculty Job satisfaction during COVID-19: a mixed-methods study. Nurs Educ Perspect. 2023;44(6):353–8.
Article PubMed Google Scholar
Stamm B. The concise manual for the professional quality of life scale. 2010.
DeVaul D, Reulet B, Daniels J, Zhu X, Wilkins R, Gordy XZ. Compassion satisfaction, Burnout, and secondary traumatic stress among respiratory therapists in Mississippi: a cross-sectional study. J Respiration. 2023;3(4):191–92673.
Wentzel DL, Brysiewicz P. A survey of compassion satisfaction, burnout and compassion fatigue in nurses practicing in three oncology departments in Durban, South Africa. Int J Afr Nurs Sci. 2018;8:82–6.
Cetrano G, Tedeschi F, Rabbi L, Gosetti G, Lora A, Lamonaca D et al. How are compassion fatigue, burnout, and compassion satisfaction affected by quality of working life? Findings from a survey of mental health staff in Italy. (1472–6963 (Electronic)).
Duarte J, Pinto-Gouveia J. The role of psychological factors in oncology nurses’ burnout and compassion fatigue symptoms. Eur J Oncol Nurs. 2017;28:114–211462.
Marín-Tejeda M. Prevention of burnout and compassion fatigue: evaluation of a group intervention. J Behav Heal Soc. 2017;2017:9.
Habtamu AA, Animut A, Luel D. Job satisfaction among Ethiopian nurses: a systematic review. Front Nurs.8(1):75–82.
Admasu B, Temamen T, Dagmawit B, Abdela AD. Job satisfaction and associated factors among nurses working in the operation theater at government hospitals of Eastern Ethiopia, 2017. Palliat Med Care. 2018;5(2):1–7.
Mirutse A, Mengistu Z, Bizuwork K. Prevalence of compassion fatigue, burnout, compassion satisfaction, and associated factors among nurses working in cancer treatment centers in Ethiopia, 2020. BMC Nurs. 2023;22(1):373.
Bahari G, Asiri K, Nouh N, Alqahtani N. Professional Quality of Life among nurses: Compassion satisfaction, Burnout, and secondary traumatic stress: a Multisite Study. SAGE Open Nurs. 2022;8:23779608221112329.
PubMed PubMed Central Google Scholar
Yalaza M, Keskinkılıç Yağız B. Compassion satisfaction and Compassion fatigue among General surgeons: a nationwide cross-sectional study. Indian J Surg. 2023;85(2):329–36.
Circenis K, Millere I, Deklava L. Measuring the Professional Quality of Life among Latvian nurses. Procedia - Social Behav Sci. 2013;84:1625–9.
Zakeri MA, Bazmandegan G, Ganjeh H, Zakeri M, Mollaahmadi S, Anbariyan A, et al. Is nurses’ clinical competence associated with their compassion satisfaction, burnout and secondary traumatic stress? A cross-sectional study. Nurs Open. 2021;8(1):354–. – 63%@ 2054 – 1058.
Kim K, Han Y, Kwak Y, Kim J-s. Professional Quality of Life and clinical competencies among Korean nurses. Asian Nurs Res. 2015;9(3):200–6.
Temesgen K, Aycheh MW, Leshargie CT. Job satisfaction and associated factors among health professionals working at Western Amhara Region, Ethiopia. Health Qual Life Outcomes. 2018;16(1):65.
Ayalew E, Workineh Y. Job satisfaction and associated factors among nurses in Bahir Dar City administrative, North West Ethiopia, 2017. BMC Res Notes. 2019;12(1):319.
Abate M, Tadesse N, Mitiku K. Level of compassionate health care service provision and its associated factors among health professionals working in public hospitals of Addis Ababa: health professionals’ perspective. Heliyon. 2022;8(3):2405–8440.
Tenaw Z, Siyoum M, Tsegaye B, Werba TB, Bitew ZW. Health professionals Job satisfaction and Associated Factors in Ethiopia: a systematic review and Meta-analysis. Health Serv Res Managerial Epidemiol. 2021;8:23333928211046484.
Adem M, Birhanu Y, Tigabu M, Bahiru J, Endris A. Level of compassion fatigue and associated factors among nurses working at comprehensive specialized hospitals in northwest Amhara region, Ethiopia 20222023.
Yami A, Hamza L, Fau - Hassen A, Hassen A, Fau - Jira C, Jira C, Fau - Sudhakar M, Sudhakar M. Job satisfaction and its determinants among health workers in jimma university specialized hospital, southwest Ethiopia. (2413–7170 (Electronic)).
Girma BA-O, Nigussie J, Molla A, Mareg M. Health professional’s job satisfaction and its determinants in Ethiopia: a systematic review and meta-analysis. (0778–7367 (Print)).
Buitendach JH, Rothmann S. The validation of the Minnesota job satisfaction questionnaire in selected organisations in South Africa. SA J Hum Resource Manage. 2009;7(1):1–8.
Weiss DJ, Dawis RV, England GW. Manual for the Minnesota satisfaction questionnaire. Minnesota studies in vocational rehabilitation. 1967.
Heidari S, Parizad N, Goli R, Mam-Qaderi M, Hassanpour A. Job satisfaction and its relationship with burnout among nurses working in COVID-19 wards: a descriptive correlational study. Annals Med Surg. 2022;82:104591.
Stamm BH. Professional quality of life scale. Psychological Trauma: Theory, Research, Practice, and Policy. 2005.
Ortega-Campos E, Vargas-Román K, Velando-Soriano A, Suleiman-Martos N, Cañadas-de la Fuente GA, Albendín-García L et al. Compassion fatigue, Compassion satisfaction, and Burnout in Oncology nurses: a systematic review and Meta-analysis. Sustainability. 2019;12(1).
Alharbi I, Alyamani N, Zafer D, Munshi S, Jawa H. Compassion fatigue, burnout and compassion satisfaction among physicians in Makkah region, Saudi Arabia: a cross sectional study. Med Sci. 2023;27:1–12.
Yu H, Jiang A, Shen J. Prevalence and predictors of compassion fatigue, burnout and compassion satisfaction among oncology nurses: a cross-sectional survey. Int J Nurs Stud. 2016;57:28–380020.
Zhang B, Li H, Jin X, Peng W, Wong CL, Qiu D. Prevalence and factors associated with compassion satisfaction and compassion fatigue among Chinese oncology healthcare professionals: a cross-sectional survey. Asia-Pacific J Oncol Nurs. 2021;9.
Poudyal S, Sharma K, Ghimire S, COMPASSION FATIGUE, BURNOUT AND COMPASSION SATISFACTION AMONG NURSES, WORKING IN A TERTIARY CARE HOSPITAL OF NEPAL DURING COVID-19 PANDEMIC. J Chitwan Med Coll. 2022;12:19–22.
Unjai S, Forster EM, Mitchell AE, Creedy DK. Predictors of compassion satisfaction among healthcare professionals working in intensive care units: a cross-sectional study. Intensive Crit Care Nurs. 2023;79:103509.
Xia WA-O, Defang W, Xiaoli G, Jinrui C, Weidi WA-O, Junya L et al. Compassion satisfaction and compassion fatigue in frontline nurses during the COVID-19 pandemic in Wuhan. China. (1365–2834 (Electronic)).
Kabunga A, Anyayo LG, Okalo P, Apili B, Nalwoga V, Udho S. Prevalence and contextual factors associated with compassion fatigue among nurses in northern Uganda. PLoS ONE. 2021;16(9):e0257833.
Article CAS PubMed PubMed Central Google Scholar
Woldekiros AN, Getye E, Abdo ZA. Magnitude of job satisfaction and intention to leave their present job among nurses in selected federal hospitals in Addis Ababa, Ethiopia. PLoS ONE. 2022;17(6):e0269540.
Tenaw Z, Siyoum M, Tsegaye B, Werba TB, Bitew ZW. Health professionals job satisfaction and associated factors in Ethiopia: a systematic review and meta-analysis. Health Serv Res Managerial Epidemiol. 2021;8:233339282110464842333–3928.
Ayalew F, Kibwana S, Shawula S, Misganaw E, Abosse Z, van Roosmalen J, et al. Understanding job satisfaction and motivation among nurses in public health facilities of Ethiopia: a cross-sectional study. BMC Nurs. 2019;18(1):46.
Hailay AA-O, Aberhe W, Mebrahtom GA-O, Zereabruk K, Gebreayezgi GA-OX, Haile T. Burnout among Nurses Working Ethiopia. (1875–8584 (Electronic)).
Cañadas-De la Fuente GA-O, Ortega E, Ramirez-Baena LA-O, De la Fuente-Solana EI, Vargas C, Gómez-Urquiza JA-O, Gender. Marital status, and children as risk factors for Burnout in nurses: a Meta-Analytic Study. LID – 10.3390/ijerph15102102 [doi] LID – 2102. (1660–4601 (Electronic)).
Basazin Mingude A, Negese B, Emiru M, Bekele Gonitie G. Magnitude of missed nursing care and associated factors in case of North Shewa Zone public hospitals, Amhara regional state, Ethiopia. Int J Afr Nurs Sci. 2022;17:100497.
Amini A, Mortazavi S. The impact of the broadcasting mistake management culture in a healthy organization on the quality of the personnel work life. (2249-782X (Print)).
Solomon BC, Nikolaev BN, Shepherd DA. Does educational attainment promote job satisfaction? The bittersweet trade-offs between job resources, demands, and stress. J Appl Psychol. 2022;107(7):1227–41.
Download references
Acknowledgements
We would like to say thanks to the supervisors, data collectors, and our study participants for their valuable input. We also would like to give our greatest thanks to Wachemo University, College of Medicine and Health Science, School of Nursing, for providing an opportunity to carry out this study.
No funding agency.
Author information
Authors and affiliations.
College of Medicine and Health Science, School of Nursing, Wachemo University, Hosanna, Ethiopia
Sentayehu Admasu Saliya, Taye Mezgebu Ashine, Asnakech Zekiwos Heliso, Getachew Ossabo Babore, Bethelhem Birhanu & Awoke Girma Hailu
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: Sentayehu Admasu SaliyaData curation: Sentayehu Admasu Saliya, and Taye Mezgebu Ashine Formal analysis: Sentayehu Admasu Saliya, Taye Mezgebu Ashine, and Asnakech Zekiwos HelisoFunding acquisition: Getachew Ossabo Babore, Bethelhem Birhanu, and Awoke Girma HailuInvestigation: Sentayehu Admasu SaliyaMethodology: Sentayehu Admasu Saliya, Taye Mezgebu Ashine, Asnakech Zekiwos Heliso, Getachew Ossabo Babore, Bethelhem Birhanu, and Awoke Girma HailuValidation: Sentayehu Admasu Saliya, Taye Mezgebu Ashine, Asnakech Zekiwos Heliso, Getachew Ossabo Babore, Bethelhem Birhanu, and Awoke Girma Hailu Visualization Sentayehu Admasu Saliya, Taye Mezgebu Ashine, Asnakech Zekiwos Heliso, Getachew Ossabo Babore, Bethelhem Birhanu, and Awoke Girma HailuWriting – original draft: Sentayehu Admasu SaliyaWriting – review & editing: Sentayehu Admasu Saliya, Taye Mezgebu Ashine, Asnakech Zekiwos Heliso, Getachew Ossabo Babore, Bethelhem Birhanu, and Awoke Girma Hailu.
Corresponding author
Correspondence to Sentayehu Admasu Saliya .
Ethics declarations
Ethical consideration and consent to participate.
Ethical clearance was obtained from the Wachemo University College of Medicine and Health Science, with reference number IRB/172/16. In Ethiopia, we did not ask the National Research Ethics Review Committee (NRERC) to obtain ethical approval/waiver for the following two reasons: (a) This study had no significant risks on study participants as approved by Wachemo University College of Medicine and Health Science, with reference number IRB/172/16; (b) NRERC is primarily focused on providing ethical decisions for clinical trials involving new drugs, experimental research, and studies that require human biological specimens/samples. Instead of NRERC ethical approval, the human resources for health experts at Wachemo.
The University Institutional Review Board (IRB) of the College of Medicine and Health Science reviewed the study protocol and granted permission to conduct the study. Written informed consent was approved by the Wachemo University College of Medicine and Health Science Institutional Review Board. Written informed consent was obtained from all study participants.
To protect participants from risks, the study did not record participants’ names, identification numbers, and names of health facilities where he or she worked. Data were also entered into a computer with unique randomly generated ID numbers given for each study participant. All methods were carried out following relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Saliya, S.A., Ashine, T.M., Heliso, A.Z. et al. Professional quality of life and job satisfaction among nurses working at tertiary hospitals in central Ethiopia. BMC Nurs 23 , 417 (2024). https://doi.org/10.1186/s12912-024-02101-w
Download citation
Received : 27 November 2023
Accepted : 17 June 2024
Published : 21 June 2024
DOI : https://doi.org/10.1186/s12912-024-02101-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 21 June 2024
Community health worker perspectives: examining current responsibilities and strategies for success
- Monica Kowalczyk 1 ,
- Nicole Yao 1 ,
- LaToya Gregory 1 ,
- Jeannine Cheatham 2 ,
- Tarrah DeClemente 3 ,
- Kenneth Fox 3 ,
- Stacy Ignoffo 4 &
- Anna Volerman 1 , 2
Archives of Public Health volume 82 , Article number: 94 ( 2024 ) Cite this article
161 Accesses
Metrics details
Community health worker (CHW) interventions have demonstrated positive impacts globally, with the COVID-19 pandemic further highlighting the potential of CHWs at the frontline to support prevention, outreach, and healthcare delivery. As the workforce expands, understanding the work and capabilities of CHWs is key to design successful interventions. This study examines the perspectives of experienced CHWs in Chicago about their current work and strategies for success.
As part of a community-academic partnership in Chicago, semi-structured interviews were completed with individuals who held positions aligned with CHW. Interviews were conducted between January and April 2022. Questions focused on participants’ work and factors contributing to their effectiveness to gain insights into workforce strategies for success to be applied in healthcare and community settings. De-identified transcripts were analyzed using inductive reasoning with codes organized into themes and subthemes under two domains identified a priori. The themes informed a logic model focused on the early stages to support the success of CHWs in their role.
Fourteen individuals participated in the study. The two predetermined domains in this study were: current work of CHWs and strategies for CHWs to be successful.
Five themes were identified about CHWs’ current work: providing services, building alliances with clients, establishing and maintaining collaborations, collecting data, and experiencing challenges in role. From their perspectives, all these responsibilities enhance client care and support workforce sustainability efforts.
Five themes emerged about strategies for the success of CHWs: background of CHWs, champions to support work of CHWs, materials to perform work of CHWs, preparation for CHW role, and characteristics of CHWs. Participants described key traits CHWs should possess to be hired, individuals who can champion and advocate for their work, and specific materials needed to fulfill responsibilities. They reported that training and familiarity with the community were integral to developing and refining the qualities and skills necessary to be effective in their role.
CHWs play an increasingly important role in enhancing healthcare delivery and improving health outcomes. This study offers a framework for policymakers, communities, and organizations to utilize for preparing CHWs to succeed in their roles.
Peer Review reports
Text box 1. Contributions to literature |
|---|
• This study adds to existing literature that focuses on community health worker (CHW) practices in enhancing client care. |
• This study brings attention to CHW efforts in workforce sustainability, which is overlooked in existing literature. |
• Our study presents a logic model, informed by experienced CHWs, on early strategies for success in CHW roles that highlights relevant trainings, materials, and support systems. |
• Our research was conducted in Chicago, bringing unique insights with the city’s distinct population, healthcare systems, and communities. |
Introduction
The community health worker (CHW) workforce in the United States has grown substantially since it was established in the 1960s, with the goal of effectively linking underserved communities to vital health services [ 1 ]. CHWs—also known as promotores/as de salud, peer health educators, and lay health advocates—are frontline public health workers who help community members overcome barriers to better health and support health systems to enhance care delivery. Typically, CHWs are members of and/or have a thorough understanding of the community, improving the quality and cultural competence of services provided to individuals [ 2 ]. They provide services to both adults and children most often in community and medical settings,[ 3 ] including health education, linkages to health and social resources, system navigation, and motivation to achieve health goals [ 4 , 5 ]. The potential of CHWs as key members of health care teams has been recently underscored by the COVID-19 pandemic, which uncovered and deepened health inequities. CHWs have been recognized as powerful forces for addressing the pandemic by supporting testing, contact tracing, and vaccination [ 6 , 7 ].
The successes of CHW interventions worldwide are well-documented. Studies demonstrate that CHWs support individuals in managing chronic health conditions, [ 8 , 9 , 10 , 11 ] provide social support through screenings and referrals, [ 12 , 13 ] and promote healthy behaviors [ 14 , 15 ]. Such interventions are often completed via home visits and/or phone calls, through which CHWs can assess social risk factors, provide education, and support resource navigation [ 8 , 11 , 13 , 14 ]. Additionally, CHW interventions have proven to be highly cost-effective, especially for high-risk populations [ 16 , 17 , 18 ].
As the CHW workforce is expanding [ 19 ] and evolving, [ 3 ] it is important to understand the current roles and capabilities of CHWs and consider factors that contribute to their success, which is critical for implementation of programs and sustainability of the workforce. While broader-scale efforts exist to understand newly acquired competencies and responsibilities of CHWs, [ 20 ] the local context may introduce unique qualities, skills, and tasks. Thus, this study aims to describe current responsibilities of CHWs and identify early strategies for CHWs to succeed in their roles from the perspectives of CHWs in Chicago in context of their unique population, healthcare systems, and communities.
Study design
This qualitative study was conducted as part of an academic-community partnership between an academic institution (University of Chicago), public school district (Chicago Public Schools), and community-engaged research (Sinai Urban Health Institute) in Chicago [ 21 ]. The study focused on Chicago, an urban city with several regions, including the Northwest Side with a predominantly White population, South Side with a majority Black population, and West Side with a largely Hispanic/Latino population [ 22 , 23 , 24 ]. This study was deemed exempt by the Institutional Review Board.
The study included individuals from the Chicago area who held positions that aligned with a CHW role, including working in and/or with a community to promote better health. Participants were recruited using email advertisements distributed by the community-engaged research institute and their partners, including various local and state listservs for community health worker organizations and resources. Interested participants then contacted the study team directly to participate. This study utilized snowball sampling with participants asked at the end of the interview to identify additional CHWs who may provide relevant insights.
Data collection
Semi-structured interviews ( n =14) were conducted via Zoom between January and April 2022. All interviews were conducted by a research project coordinator with a master’s degree in public health training and four years of experience in qualitative methods. Verbal consent was obtained from each participant prior to the start of the interview.
An interview guide was utilized for the discussion. Participants were asked about current work responsibilities, essential relationships, challenges faced, and methods for effectiveness in their role. This manuscript reports results from a group of questions focused on the CHW role overall; a subsequent group of questions asked about the integration of CHWs in schools and these results are reported elsewhere [ 25 ]. Each interview lasted 60-120 minutes. Participants received a $50 e-gift card. Interviews were continued until thematic saturation was reached.
Data analysis
Interviews were recorded, transcribed, and de-identified prior to analysis. Thematic analysis was conducted based on grounded theory principles with an inductive reasoning approach applied [ 26 , 27 ]. Four researchers (AV, LG, MK, NY) independently read and coded the first five interviews based on two pre-determined domains: current work of CHWs and strategies for success in CHW role. Researchers met after coding each interview to compare codes, resolve discrepancies, and develop a coding framework with themes and subthemes. Once the framework was finalized, it was applied by three researchers (LG, MK, NY) to the remaining interviews. Any new codes, themes, subthemes, and discrepancies were discussed and resolved. All transcripts were re-coded by two researchers (LG, MK) using the final thematic framework. Discrepancies were discussed until a consensus was reached. Dedoose Version 9.0.46 was utilized for analysis. To ensure validity of the results, the framework was shared with a diverse group of experienced CHWs as well as CHW program leaders, designers, and evaluators from the community-based research institute for review and feedback, which was incorporated into the final framework.
Development of logic model
The themes from the domain about strategies for CHW success were applied to develop a logic model, a visual representation of the resources and actions needed to achieve long-lasting outcomes. This model depicts the considerations for hiring and onboarding as well as types of supports and activities needed for a CHW to be successful in their role.
Fourteen individuals participated in the study (Table 1 ). Their years of experience in the field ranged from 0.5 to 22 years. Some participants’ current role titles included “community health workers” and “COVID-19 response workers,” with the latter group responsible for providing resources and COVID-19 education during the pandemic. Certain participants had advanced to the roles of “CHW supervisor” and “CHW coordinator”, overseeing CHWs and programs. One participant transitioned to the role of “communicable disease investigator,” surveying infectious diseases within local communities. The majority were affiliated with health systems ( n =11, 78.5%) and served Chicago’s West side ( n =8, 57.1%) and South side ( n =8, 57.1%), with some participants working in more than one region of Chicago.
Domain 1: Current work of CHWs
Five themes emerged from participants about the current responsibilities of CHWs: providing services to clients, building alliances with clients to improve health outcomes, establishing and maintaining collaborations, collecting data to support work, and navigating challenges in their work (Table 2 ).
Theme 1: Providing services
Participants emphasized their primary role is to provide services to clients seeking care for their needs. Examples of services included navigation of the health care system and linkage to health and social resources. Participants reported additional services for clients included educating about health topics, delivering materials (e.g., green cleaning kits, medications), and troubleshooting issues negatively affecting care – all of which are addressing “what the patient [client] needs.”
Participants also shared their contributions to the development and implementation of CHW programs, including supporting design of programs and materials. CHWs applied their unique expertise to developing projects. For example, one participant shared, “Sometimes, especially when it’s a new program, it’s rare [to have] things come in translated; or when you’re getting trained, you don’t get trained in Spanish. You have to do your own translation.” Participants described additional responsibilities including conducting recruitment, data collection, and trainings. One participant described that they ensured continuing education was available, “I’m trying to get courses or presentations to be available to CHWs as we move into different roles or things they want to get a refresher on.”
In specific settings, participants described CHWs providing more tailored services. They discussed conducting health outreach and education at community events, such as health fairs. Although the COVID-19 pandemic paused direct outreach, some participants still conducted community outreach including canvassing schools to provide COVID-19 information: “ if they wanted some information on the vaccination for their kids, for their parents, you let them [schools] know what you’re doing.” In clinical settings, CHWs can uniquely connect with clients to further learn about their health status and factors influencing their health to inform clinicians as one participant explained, “ a lot of times our clients [are] not comfortable speaking and being open with their physicians… It’s our job to listen to them and then relay the message back to the doctor’s office.”
Theme 2: Building alliances with clients to improve health outcomes
Participants described that, for CHWs to effectively provide services, a significant part of their work is establishing trust with clients. They emphasized the importance of CHWs utilizing their communication and interpersonal skills by being attentive to clients’ needs, connecting with clients through shared experiences, being transparent with clients, and assuring clients of their support. One participant shared how they first interact with clients, “I introduced them myself or even let them ask me question… Things like that have also been very helpful in building that rapport with the participants.”
Additionally, the various ways that CHWs interact with clients can help establish alliances. Participants expressed that in-person contacts through door-to-door canvassing and home visits effectively built trust with clients. While the COVID-19 pandemic resulted in limited in-person interactions with clients, one participant emphasized the importance of continuing meaningful engagement with clients in virtual environments, “Having that time to talk with them and to ask those opening questions to see what’s the root cause of what’s going on and then try to address that so it can change some of the other outcomes.”
Theme 3: Establishing and maintaining collaborations
Participants also described how their current work leverages their various relationships with partners: collaborators within health systems, CHW teams, community organizations, and community members.
Participants affiliated with a health system described working across departments and collaborating with various personnel to support patients. They indicated the integration of CHWs into health teams has become an easier process with health systems becoming more familiar with CHWs as one participant shared. “When I first started as a CHW, a lot of people weren’t aware of us. Right now, we are popular.” Further, some participants explained that they worked directly with clinicians in the health system to coordinate care for clients. One participant emphasized the importance of consistent communication in this partnership, “Sometimes it can happen that they [clinic staff] make the same appointment, or they forget to make the appointment so it’s [important] to keep them updated about what resources you [CHWs] are providing.” CHWs also relied on collaborations within the health system to acquire knowledge and resources. One participant shared about their partnership with social workers, “[Social workers] know a lot. If they don’t know or if I don’t know, they’re finding the best way to figure it out.”
Beyond the health system, participants shared that it was essential to collaborate within their CHW teams. Participants expressed these partnerships have helped them be effective and stay motivated in their roles, especially during a public health crisis. Some participants shared that, even with limited in-person interactions, they made time to meet with their coworkers to share successes and challenges as one participant explained, “If it is something I don’t feel that I’m dealing with correctly, our CHWs are so open to assist you [me].” Additionally, through these partnerships, CHWs were able to share their expertise to support each other’s clients. One participant described, “We work on different projects… ‘I have an asthma patient. Could you talk to them? Could you do education?’ I’ll just call them and then they’ll come do the education.”
In addition to working with health systems and CHWs teams, CHWs discussed their collaborations with community organizations, community members, and other partners (e.g., CHW associations and groups) to gather and expand resources. CHWs worked to develop partnerships with local organizations and external networks to link clients to resources (e.g., food pantries, housing assistance) as well as to provide health education to community members. One participant shared the benefits of having such local partnerships to minimize gaps in resources, “If there’s one [service] that we don’t offer, then [we are] reaching out to organizations that offer [the service].” Participants described that these partnerships can be bidirectional with CHW providing trainings to these organizations. Also, participants stated CHWs worked closely with community members to tailor their services to community needs. For instance, CHW programs have organized community advisory boards to obtain suggestions to enhance the programs. One participant shared how they leverage their community advisory board to enhance a CHW program, “We do have a community advisory board. Whenever we want to do changes to our programs, we try to connect with them to see what they say and one of those is an example of our name . We’re trying to be more inclusive and more gender neutral…so we went to our advisory board.” Additionally, participants have worked with CHW networks to build knowledge and expertise as one participant shared, “Joining the national CHW organization – that’s a must because you’re getting information.”
Theme 4: Collecting data to support work
Some participants described significant involvement in data collection as a part of their roles. They stated that CHWs collect health and social-related data to identify factors influencing health outcomes as well as to monitor client’s progress in working with a CHW. Additionally, participants shared the importance of data collection for CHWs to track their own work progress. This data may be related to the reach and impact of their work, including the number of client interactions each day and number of clients who accepted or rejected services, resources, or referrals. Participants also talked about the importance of tracking outcomes of resources provided to clients to screen for the quality of services provided. One participant described the information they provide, “We enter the resources they need and if we provide it… and I enter notes because sometimes you have bad experiences.”
Participants indicated the data collected by CHWs are utilized for evaluation, maintenance, expansion, and dissemination of programs. Data on the outcomes of CHW services can highlight the successes of CHW programs as well as areas for improvement. For example, one participant shared how the data collected led to not only refining the program but also expanding it, “I was in a diabetes program. Before I started, it was called [program 1]. Once they collected that information, they saw some fine-tuning they needed to do and so they did it. Then, they created a second one, which was called [program 2]. That’s when they hired new CHWs. They brought in more because they realized they needed more CHWs to roll out this program.” Additionally, this data can bring to light the needs of vulnerable communities and impacts of CHWs through dissemination: “We use [data] to improve our programs. Use it to help tell the story of these community concerns we were addressing or identified through this programming. Data is our support and validation.”
Theme 5: Navigating challenges in role
Participants highlighted various challenges encountered in their community health work. One challenge was related to the different relationships within their roles. CHWs shared difficulties in their client relationships. Some participants discussed working on overwhelming client cases and coping by learning to create healthy boundaries and rely on other CHWs. CHWs also spoke about barriers in interacting with clients, especially virtually, which can limit communication. Participants shared that some clients may be heavily reliant on CHWs, while some may distrust them: “In the past, it was a struggle to get that trust from the community. The health care system has been very harsh towards Black and Brown individuals.” Beyond client relationships, some participants described challenges with integrating into clinical teams. Some experienced being unwelcomed by clinicians and other staff due to limited understanding about CHW role. One participant cited the insufficient recognition given to the work of CHWs, “ The world doesn’t see a CHW like they would a CNA [certified nursing assistant] or another kind of assistant... it’s been verified and documented that having a CHW attached to a person within their health challenges makes a difference.”
Another challenge described by participants was related to gaps in resources for clients and materials needed to complete their work. Participants highlighted the limited funding to support clients and CHW programs. One participant described the struggles of overcoming financial barriers for clients to receive health care, “ With COVID-19, a lot of people lost their employment… If there’s no resources, then it’s hard for people to commit to having a [medical] procedure.” Additionally, there are limited funds to provide as incentives to foster success in CHW programs.
Additional challenges raised by participants included fluctuations in work. They indicated the pandemic led to drastic changes with the transition to remote work, which affected how CHWs interacted with clients. One participant shared, “Now, it’s more difficult to get them [clients] virtually and actually show you [their] home... You would think it’s easier virtually because you’re not going in, but they don’t want to do it.” With remote work also comes the challenge of maintaining a work-life balance that participants reported, as one shared, “ Some patients really do need support and they want to stay with you on the phone for hours and we can’t do that.” Lastly, participants discussed how the nature of home visits and community outreach posed a challenge due to increases in crime in the communities served: “Most of the neighborhoods that we work in are high crime areas… We could make our appointments for early in the morning and it’s usually safe in the morning, but now it’s just as bad early in the morning as it is in late evening.”
Domain 2: Strategies for CHWs to be successful in their roles
Five themes emerged from participants about strategies for CHWs to be successful in their roles: background, champions to support work, materials to perform work, preparation for role, and acquired characteristics (Table 3 ). These strategies aligned with a logic model, including inputs, activities, and outputs with the outcome of an effective CHW (Fig. 1 ).

Logic model describing strategies for community health workers to succeed in role, as informed by interviews with experienced community health workers in Chicago, Illinois (2022)
Theme 1: Background of CHWs
Participants highlighted innate attributes to consider when hiring CHWs. One characteristic considered important was being a member of the community served. Participants shared this quality was valuable for navigating local resources and building trust with clients. Participants emphasized the importance of having shared backgrounds (e.g., demographics, experiences) and language with clients to build trusting relationships. One participant shared that having the same adversities as clients prepared them to join the workforce, “I was the mother waiting in a room to get the service, and nobody gave the service because [there was] nobody who speaks Spanish... I'm not the first, but I'm not the last one. That gave me that responsibility.” Along with shared backgrounds as clients, participants reported certain past experiences that transferred to their roles, including education in psychology or sociology as well as previous roles in health or helping others.
Theme 2: Champions to support the work of CHWs
Participants listed key players who have supported their role as CHWs. An essential entity identified by participants as a champion was their own internal organization. They expressed appreciation that their organization’s culture encourages collaborations and nurtures professional growth by providing education and materials. One participant shared about their organization, “I think one of the reasons that I really like to do what I do is because I feel supported and because, like [organization’s] philosophy, if we’re okay emotionally, we can better perform our job.”
Internal to their organizations, participants reported their CHW teams were champions for their work. Their team members were especially helpful by providing guidance and emotional support, particularly when starting in their roles. One participant described their team member’s lasting impact when beginning their role, “Something came up...I’m like, ‘I can’t do this. I’ve got to find something else to do.’ My [team member] was like, ‘Okay, see you tomorrow’… When people new come to me, I’m like, ‘Okay, let’s take a deep breath. Go home and do some self-care. I’ll see you tomorrow. Tomorrow, let’s talk about what happened yesterday.’” In addition to serving as champions at the start, participants emphasized that team members helped enhance their performance by sharing expertise and resources as well as creating space to debrief on difficult cases. Lastly, participants stated the leaders within their teams are champions for their work, providing support and resources for CHWs to be effective in their role. One participant shared the importance of having a leader who respects them, “Having that type of support with your supervisor does make that type of work a lot easier...it makes [me] happy to be working in that field.”
Outside of their organizations, some participants recognized external organizations as champions for their work. Participants shared that they relied on other CHW-focused organizations for topic expertise and client referrals. Participants who have been integrated in clinical settings emphasized the importance of having a clinician who trusts the CHW and serves as a champion. One participant shared their experience, “I have this one champion...she is a doctor still. She is the one that was, ‘go ahead and talk [to] them,’ ‘go ahead and do this,’ ‘go ahead and tell them.’”
Theme 3: Materials to perform work of CHW
Participants highlighted the various materials needed in their line of work. A key material was readily available resources with information and referrals for clients, such as community referral programs like “Purple Binder” and “NowPow”. One participant described how they use such resources with clients, “I have physical resources. I can get copies and highlight numbers they’ve got to call, addresses, appointments.” Participants also shared that CHWs need materials for client care, including medications, medical supplies, and cleaning products to support chronic condition management at home. During the COVID-19 pandemic, they also provided personal protective equipment and at-home tests. Further, participants discussed that communication tools were important for working with clients and their teams, including phones, social media, and translated materials for non-English speaking clients. For their data collection responsibilities, CHWs typically used laptops or tablets to record their work and as appropriate database software. Participants also suggested CHWs should have paper versions of documents in times without Wi-Fi access. To support client education, participants recommend CHWs should have presentations as well as visual tools like anatomical models and practical materials (e.g., diabetes and asthma devices) to demonstrate aspects of disease management. As for continued education, participants largely relied on online tools like Coursera and YouTube.
Theme 4: Preparation for CHW role
Participants reported training and continuing education were essential to be prepared for the CHW field. Specifically, participants highlighted the various lessons from CHW core skills training, which focuses on relevant competencies and skills that were applicable when working closely with diverse clients. One participant shared they felt prepared for the CHW role after completing such training, “I had to understand culture humility...how to communicate with physicians...how to document... Once the expectation had been set and the knowledge has been layered on that, then it gets you ready to do the work in hand.” In addition, participants reported trainings on various health topics prepared them to support condition-specific programs. Some participants were cross-trained on multiple health topics, including chronic health conditions (e.g., asthma, diabetes, breast cancer), mental health, and COVID-19. These trainings ensured that CHWs attained knowledge on health topics to share with clients, as described by one participant, “ We can all jump in different interventions and educate a person. If I’m seeing somebody for breast health and I know that person has asthma, I can interject some of my asthma knowledge. ” Along with CHW core skills and health topic trainings, participants emphasized the importance of having practical experience through role-playing, shadowing experienced CHWs, and learning on the job. One participant shared, “ If you don’t have experience from doing home visits with the educators…having face-to-face contact with people… you're never going to have that connection with people [clients]. ” Also, participants emphasized the importance of continuing education to provide quality services to clients. Participants described they have requested subject-specific training on health topics and skills from their internal organization as well as conducted their own research or completed online trainings to ensure up-to-date knowledge.
Along with trainings, participants shared it is vital for individuals to complete other preparation for their role, including developing familiarity with the people and needs of communities they are serving. In addition, some participants emphasized the importance of knowing the community for their safety, as one participant shared, “You can’t help anyone if you’re not around to help anyone.” Finally, some participants highlighted additional preparations related to programming, such as reviewing materials and understanding responsibilities.
Theme 5: Characteristics of CHW
Participants listed qualities and skills that individuals should have to work in the CHW field, some of which are gained or refined through external experiences and preparation for their CHW role. They commented that key qualities of a CHW include being respectful, flexible, and compassionate. Participants emphasized the importance of being comfortable working with others when taking on the role of CHW, as one participant stated, “People can sense when you’re genuine and when you actually want to help them.” In addition, participants commented that it is important to be empathetic, especially when working with various clients with different backgrounds. One participant stated, “You’ve got to be open to work with all kinds--homeless, intoxicated people, people in a bad mood. You need to be empathetic... It is still your duty to help them.”
Regarding skills necessary to be an effective CHW, participants highlighted resourcefulness, interpersonal skills, problem solving, and time management. They emphasized the importance of having strong communication skills to work with various parties – clients and individuals within both internal and external organizations. One individual stressed the importance of tailoring communication style for clients with various backgrounds, “You have to be able to speak to anyone on any level - street level, education level...You’ve got to be able to deal with any type of person.” In addition, participants commented that it is important for CHWs to be mindful of their limitations and create healthy boundaries in their role, “At the beginning, I wanted to do it all. I thought, ‘I could do this, I could do that.’ And then, it was causing burnout…saying no as well was something that just made me more efficient [and] successful.”
As CHWs serve increasingly important roles in connecting health care, social care, and community, this study provides insights into the current work of CHWs from the perspective of experienced workforce members who are set within Chicago’s unique environment. Further, this study is the first to utilize such perspectives to develop a logic model that delineates key early strategies for CHWs to succeed in their role and how organizations can support these early stages.
Participants highlighted that current CHW responsibilities focus on two areas: client care and workforce sustainability. For client care, they described various roles in which CHWs support community and individual needs, in alignment with current literature. Examples include conducting health assessments, providing local health and social resources, and educating about health [ 3 , 9 , 28 ]. To effectively deliver these services, CHWs must build trusting relationships with clients, coworkers, and community members. This study’s findings corroborate existing literature that describes the critical roles of CHWs in healthcare and community settings, including establishing unique connections with patients to inform clinical teams on tailoring care for unique needs and gaining trust of community members to deliver tailored interventions within intimate settings (e.g., home visits) [ 5 , 20 , 29 , 30 , 31 ]. These capabilities and strengths of CHWs should be considered when designing CHW interventions within clinical, community, and broader settings to maximize the impact of CHWs on patient, community, and workforce outcomes. Programming should also take into account the challenges raised by participants related to building trust with clients and the community, including the mistrust of health providers and healthcare systems as well as limited resources [ 32 , 33 ]. These barriers can contribute to distress or demoralization among CHWs [ 32 , 33 ]. As such, along with programmatic efforts to alleviate these barriers, a range of approaches should be adopted to support the wellbeing of CHWs. Participants’ recommendations and prior research suggest CHW support systems, self-management trainings, and coaching on strengthening engagement, while also establishing and maintaining healthy boundaries to avoid burnout in the role, are critical to success and sustainability [ 32 , 34 ].
While CHW responsibilities related to client care are well-established in the literature, their roles in promoting workforce sustainability have been underexplored. In this study, CHWs described their roles in programming, including developing materials and training for CHWs. These activities play a significant role in sustainability and are not traditionally recognized as core responsibilities for CHWs [ 20 ]. With unique insights from their on-the-job experiences, senior CHWs have contributed to improving training standards by updating training curricula as well as leading training sessions [ 35 ]. Further, this study also highlighted CHWs’ involvement in program evaluation and quality assurance, which has been described in literature [ 20 , 36 , 37 ]. CHWs are often responsible for collecting data on client interactions and outcomes, which is utilized to evaluate and improve programs as well as to secure funding [ 38 ]. Beyond data collection, involving CHWs in all stages of evaluation and research, from identifying research questions to disseminating findings, has been recommended [ 38 ]. In addition to material development, training, and program evaluation, a few CHWs in our study cited involvement in program design. Such opportunities can be foundational to developing successful programs for clients and further building the workforce [ 39 ]. Existing programs can consider expanding CHWs’ involvement in program development and evaluation to incorporate their valuable perspectives into such efforts.
Based on the multiple CHW responsibilities described, this study’s findings informed a new logic model that outlines key resources and activities essential for the early success of CHWs (Fig. 1 ). While some aspects of this logic model align with existing research, this model moves beyond to examine resources and activities across various levels. Existing frameworks in the literature focus primarily on CHW workforce readiness, including trainings, evaluation, and broader program support [ 35 , 40 , 41 ]. For instance, a pre-existing logic model for CHWs describes programmatic and systematic factors that enhance CHW performance in low and middle-income countries; however it does not incorporate factors at the individual level [ 41 ]. This study’s logic model incorporates factors across individual, interpersonal, program, and systems levels that are critical for the effectiveness of CHWs in the early stages of their roles. Organizations that are developing CHW programs can reference this logic model to understand the necessary infrastructure and resources required to set a CHW for success in their role. Additionally, this model can be utilized for established programs to identify gaps and implement strategies to effectively support CHWs in their programs.
Informed by participants, the inputs of this model are the background of CHWs, champions to support CHWs, and materials to perform the work—key factors at the individual level. Participants in our study noted it is important to select CHWs from the communities being served who share experiences with community members. This finding corresponds with systematic literature reviews showing that CHWs residing in local communities understand community culture and language(s) in unique ways, which enable them to establish and build trust and respect among clients [ 28 , 30 ]. While participants reported that educational background in certain subjects prepared them for the CHW workforce, there is no existing consensus on criteria for level of education. Qualifications for the CHW role in current literature have varied widely, from high school to secondary education, in addition to relevant training courses [ 3 , 30 ]. In terms of prior work experiences, this study mirrors prior research which has documented the importance of experiences in the health or social welfare sectors, such as a caregiver or community organizer [ 28 ]. The considerations outlined can be valuable for organizations initiating or expanding CHW programs, particularly when hiring qualified candidates for CHW positions.
In addition to the background of CHWs, additional inputs of the model are ensuring there are champions to support CHWs as they begin and carry out their work as well as materials to perform the work. Opportunities to support CHWs include providing essential materials for fulfilling their responsibilities as well as creating systems to ensure mentorship in their work [ 42 , 43 ]. Beyond the opportunities mentioned in this study, literature has described that job aids (e.g., checklists, pictorial instructions) and transportation options are useful to support CHW activities [ 44 , 45 ]. Additionally, prior research has identified that access to electronic health records is helpful in identifying clients, scheduling appointments, and facilitating communication between clients and care teams [ 42 ]. Lastly, collaborations between CHWs and their CHW teams can be a source of valuable support, a finding consistent with previous studies that highlight the benefits of CHW supervision and peer support [ 42 , 43 ]. While adopting strategies for supportive supervision for CHW programs, such as supervisors coaching and mentoring CHWs, is not strongly recommended, [ 46 ] organizations that integrate CHWs should ensure to hire and train supervisors to offer comprehensive support to CHWs. This recommendation stems from participants’ emphasis on the impact of their CHW team leader’s feedback and advocacy. These considerations can help organizations implement an infrastructure of support for CHWs to succeed in their work with the necessary equipment and robust support system.
Building upon the inputs in the logic model, participants highlighted key activities for CHW success, including completing trainings as well as deepening insights and connections within communities. Suggested training topics include core competencies (e.g., cultural humility, advocacy) and health topics (e.g., mental health), which corresponds with topics described in the literature [ 35 , 47 ]. Along with trainings, CHWs should gain practical experience and community familiarity to succeed in their roles through activities like role-playing as well as conducting research to identify health or social issues within communities and develop plans to address them [ 35 , 48 ]. While the training and experience can support preparedness for the role, CHWs’ knowledge and skill proficiencies can also be evaluated using observation, examination, and self-assessment [ 35 , 40 , 49 ]. Such strategies can equip CHWs with the qualities and skills identified as crucial for success, such as emotional intelligence, cultural competence, interpersonal skills, and problem-solving abilities–the outputs of our logic model. These qualities and skills are frequently discussed in existing literature as key competencies for CHWs, along with characteristics such as an open-minded personality and respect for diversity [ 50 ]. Other attributes in research that were not emphasized by this study’s participants include intrinsic motivation and soft skills like leadership [ 28 , 30 , 50 ]. It is critical for CHW organizations to provide such learning opportunities for newly hired CHWs to acquire the necessary skills and knowledge to be effective in their role as well as to offer continuous professional development as the role and field evolve.
Strengths of this study include the rich, comprehensive data from one-on-one interviews with participants and the prioritization of the perspectives of CHWs, who possess unique insights into their role. The generalizability of the findings may be limited as all participants were from the Chicago area, and experiences may differ in non-urban or rural areas, US states, and countries with different policies about community health work. Most participants worked within healthcare systems, providing insights relevant to a sizeable proportion of CHWs; however, these experiences may not be shared by CHWs without such affiliations [ 3 , 51 ]. Also, interviews may have been affected by social desirability bias or recall bias. The researchers attempted to minimize bias by ensuring the interviewer was not affiliated with the participants’ organizations, asking participants questions about various experiences, and de-identifying transcripts prior to analysis. Future steps include gathering more experiences from CHWs with different backgrounds, roles, and/or programs to validate the framework.
It is also important to recognize this study’s findings focus on preparing a CHW and early strategies for success. It does not contemplate the longer-term support needed as the work of CHWs evolves over time. Experiences show that effective supervision, consistent upskilling opportunities, peer support and learning, and intentional career ladders are all important to the longer-term success of CHWs [ 52 ].
This study sheds light on the role of CHWs in improving the health of vulnerable communities and sustaining the workforce in Chicago. Current responsibilities that contribute to such efforts include providing services to clients and collaborators along with building relationships, collecting data, and overcoming challenges related to their role. In addition, this study provides a framework for community-based organizations and policymakers to apply to future CHW programming to ensure that qualified CHWs are supported and equipped to be successful in their role with the necessary trainings, materials, and support systems. As the CHW workforce is expanding, it is essential to recognize and leverage CHWs’ current abilities and enhance their effectiveness to achieve health equity among vulnerable populations.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
Community health worker
Pérez LM, Martinez J. Community Health Workers: Social Justice and Policy Advocates for Community Health and Well-Being. Am J Public Health. 2008;98(1):11–4.
Article PubMed PubMed Central Google Scholar
American Public Health Association. Community Health Workers. [cited 2023 Feb 21]. Available from: https://www.apha.org/apha-communities/member-sections/community-health-workers/ .
Malcarney MB, Pittman P, Quigley L, Horton K, Seiler N. The Changing Roles of Community Health Workers. Health Serv Res. 2017;52(S1):360–82.
National Heart, Lung, and Blood Institute. Role of Community Health Workers. 2014 [cited 2022 Jul 31]. Available from: https://www.nhlbi.nih.gov/health/educational/healthdisp/role-of-community-health-workers.htm .
Hartzler AL, Tuzzio L, Hsu C, Wagner EH. Roles and Functions of Community Health Workers in Primary Care. Ann Family Med. 2018;16(3):240–5.
Article Google Scholar
Ballard M, Bancroft E, Nesbit J, Johnson A, Holeman I, Foth J, et al. Prioritising the role of community health workers in the COVID-19 response. BMJ Global Health. 2020;5(6):e002550.
Article PubMed Google Scholar
Goldfield NI, Crittenden R, Fox D, McDonough J, Nichols L, Lee Rosenthal E. COVID-19 Crisis Creates Opportunities for Community-Centered Population Health: Community Health Workers at the Center. J Ambul Care Manage. 2020;43(3):184–90.
Hughes MM, Yang E, Ramanathan D, Benjamins MR. Community-Based Diabetes Community Health Worker Intervention in an Underserved Chicago Population. J Community Health. 2016;41(6):1249–56.
Ingram M, Doubleday K, Bell ML, Lohr A, Murrieta L, Velasco M, et al. Community Health Worker Impact on Chronic Disease Outcomes Within Primary Care Examined Using Electronic Health Records. Am J Public Health. 2017;107(10):1668–74.
Ye W, Kuo S, Kieffer EC, Piatt G, Sinco B, Palmisano G, et al. Cost-Effectiveness of a Diabetes Self-Management Education and Support Intervention Led by Community Health Workers and Peer Leaders: Projections From the Racial and Ethnic Approaches to Community Health Detroit Trial. Diabetes Care. 2021;44(5):1108–15.
Article CAS PubMed Google Scholar
Martin MA, Pugach O, Mosnaim G, Weinstein S, Rosales G, Roy A, et al. Community Health Worker Asthma Interventions for Children: Results From a Clinically Integrated Randomized Comparative Effectiveness Trial (2016–2019). Am J Public Health. 2021;111(7):1328–37.
Fiori KP, Rehm CD, Sanderson D, Braganza S, Parsons A, Chodon T, et al. Integrating Social Needs Screening and Community Health Workers in Primary Care: The Community Linkage to Care Program. Clin Pediatr (Phila). 2020;59(6):547–56.
Schechter SB, Lakhaney D, Peretz PJ, Matiz LA. Community Health Worker Intervention to Address Social Determinants of Health for Children Hospitalized With Asthma. Hosp Pediatr. 2021;11(12):1370–6.
Guerra PH, Silvestre R, de Mello THT, Carvalho ALBS, da Costa FF, Florindo AA. Effects of community health worker-based interventions on physical activity levels in children: a systematic review. Rev Paul Pediatr. 2021;40:e2020232.
Hejjaji V, Khetan A, Hughes JW, Gupta P, Jones PG, Ahmed A, et al. A combined community health worker and text messagingbased intervention for smoking cessation in India: Project MUKTI - A mixed methods study. Tob Prev Cessat. 2021;7:23.
Huang SJ, Galárraga O, Smith KA, Fuimaono S, McGarvey ST. Cost-effectiveness analysis of a cluster-randomized, culturally tailored, community health worker home-visiting diabetes intervention versus standard care in American Samoa. Hum Resour Health. 2019;17(1):17.
Smith L, Atherly A, Campbell J, Flattery N, Coronel S, Krantz M. Cost-effectiveness of a statewide public health intervention to reduce cardiovascular disease risk. BMC Public Health. 2019;19(1):1234.
Jacob V, Chattopadhyay SK, Hopkins DP, Reynolds JA, Xiong KZ, Jones CD, et al. Economics of Community Health Workers for Chronic Disease: Findings From Community Guide Systematic Reviews. Am J Prev Med. 2019;56(3):e95–106.
U.S Department of Health and Human Services. HHS.gov. 2022 [cited 2022 Sep 15]. HHS Announces $226.5 Million to Launch Community Health Worker Training Program. Available from: https://www.hhs.gov/about/news/2022/04/15/hhs-announces-226-million-launch-community-health-worker-training-program.html .
The Community Health Worker Core Consensus Project TTUHSC El Paso. 2022 [cited 2023 May 9]. CHW Core Consensus Project. Available from: https://www.c3project.org/ .
Vaughn S, Kowalczyk M, DeClemente T, Ignoffo S, Fox K, Cheatham J, et al. A model of community health worker integration into schools: Community-based participatory research in action. Progress in Community Health Partnerships: Research, Education, and Action. 2023 May 16;Forthcoming.
Chicago Health Atlas. [cited 2024 May 13]. Northwest. Available from: https://chicagohealthatlas.org/region/northwest?tab=data .
Chicago Health Atlas. [cited 2024 May 13]. Near South. Available from: https://chicagohealthatlas.org/region/near-south .
West. [cited 2024 May 13]. Available from: https://chicagohealthatlas.org/region/west .
Yao N, Kowalczyk M, Cheatham J, DeClemente T, Fox K, Ignoffo S, et al. Community Health Workers’ Perspectives on Integrating into School Settings to Support Student Health. Front Public Health. 2023;21:23.
Google Scholar
Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 4th ed. Los Angeles, CA: SAGE Publications, Inc; 2014. p. 456.
Glaser B, Strauss A. The discovery of grounded theory: strategies for qualitative research. Chicago: Aldine; 1967. p. 271.
Hill J, Peer N, Oldenburg B, Kengne AP. Roles, responsibilities and characteristics of lay community health workers involved in diabetes prevention programmes: A systematic review. PLOS ONE. 2017;12(12):e0189069.
Collinsworth AW, Vulimiri M, Schmidt KL, Snead CA. Effectiveness of a Community Health Worker–led Diabetes Self-Management Education Program and Implications for CHW Involvement in Care Coordination Strategies. Diabetes Educ. 2013;39(6):792–9.
Olaniran A, Smith H, Unkels R, Bar-Zeev S, van den Broek N. Who is a community health worker? – a systematic review of definitions. Glob Health Action. 2017;10(1):1272223.
Schroeder K, McCormick R, Perez A, Lipman TH. The role and impact of community health workers in childhood obesity interventions: a systematic review and meta-analysis. Obes Rev. 2018;19(10):1371–84.
Article CAS PubMed PubMed Central Google Scholar
Garcini LM, Kanzler KE, Daly R, Abraham C, Hernandez L, Romero R, et al. Mind the gap: Identifying training needs of community health workers to address mental health in U.S. Latino communities during and beyond the COVID-19 pandemic. Front Public Health. 2022;10:928575.
Lapidos A, Kieffer EC, Guzmán R, Hess K, Flanders T, Heisler M. Barriers and Facilitators to Community Health Worker Outreach and Engagement in Detroit, Michigan: A Qualitative Study. Health Promotion Practice. 2022;23(6):1094–104.
Johnson LJ, Schopp LH, Waggie F, Frantz JM. Challenges experienced by community health workers and their motivation to attend a self-management programme. Afr J Prim Health Care Fam Med. 2022;14(1):2911.
Lee LK, Ruano E, Fernández P, Ortega S, Lucas C, Joachim-Célestin M. Workforce Readiness Training: A Comprehensive Training Model That Equips Community Health Workers to Work at the Top of Their Practice and Profession. Front Public Health. 2021;8(9):673208.
Peacock N, Issel LM, Townsell SJ, Chapple-McGruder T, Handler A. An Innovative Method to Involve Community Health Workers as Partners in Evaluation Research. Am J Public Health. 2011;101(12):2275–80.
Moses K, Benyo A, Nuamah A. Community Health Workers & Promotores in the Future of Medi-Cal: Resource Package #3: The CHW/P Role in Data Collection and Outcome Measurement. 2021. Available from: https://www.chcf.org/wp-content/uploads/2021/04/CHWPsMediCalRsrcPkg3DataCollectionOutcomeMgmtDRAFT.pdf .
Rodela K, Wiggins N, Maes K, Campos-Dominguez T, Adewumi V, Jewell P, et al. The Community Health Worker (CHW) Common Indicators Project: Engaging CHWs in Measurement to Sustain the Profession. Front Public Health. 2021;22(9):674858.
Musoke D, Atusingwize E, Ndejjo R, Ssemugabo C, Siebert P, Gibson L. Enhancing Performance and Sustainability of Community Health Worker Programs in Uganda: Lessons and Experiences From Stakeholders. Glob Health Sci Pract. 2021;9(4):855–68.
Allen CG, Brownstein JN, Cole M, Hirsch G, Williamson S, Rosenthal EL. Building a Framework for Community Health Worker Skills Proficiency Assessment to Support Ongoing Professional Development. J Ambul Care Manage. 2018;41(4):298.
Naimoli JF, Frymus DE, Wuliji T, Franco LM, Newsome MH. A Community Health Worker “logic model”: towards a theory of enhanced performance in low- and middle-income countries. Hum Resour Health. 2014;2(12):56.
Mehra R, Boyd LM, Lewis JB, Cunningham SD. Considerations for Building Sustainable Community Health Worker Programs to Improve Maternal Health. J Prim Care Community Health. 2020;10(11):2150132720953673.
Celletti F, Wright A, Palen J, Frehywot S, Markus A, Greenberg A, et al. Can the deployment of community health workers for the delivery of HIV services represent an effective and sustainable response to health workforce shortages? Results of a multicountry study. AIDS. 2010;24:S45.
Kok MC, Dieleman M, Taegtmeyer M, Broerse JE, Kane SS, Ormel H, et al. Which intervention design factors influence performance of community health workers in low- and middle-income countries? A systematic review. Health Policy Plan. 2015;30(9):1207–27.
Scott K, Beckham SW, Gross M, Pariyo G, Rao KD, Cometto G, et al. What do we know about community-based health worker programs? A systematic review of existing reviews on community health workers. Hum Resour Health. 2018;16(16):39.
World Health Organization. WHO guidelines on health policy and system support to optimize community health worker programmes. World Health Organization; 2018. Available from: https://iris.who.int/bitstream/handle/10665/275474/9789241550369-eng.pdf?ua=1&ua=1 .
Wiggins N, Kaan S, Rios-Campos T, Gaonkar R, Morgan ER, Robinson J. Preparing Community Health Workers for Their Role as Agents of Social Change: Experience of the Community Capacitation Center. J Comm Practice. 2013;21(3):186–202.
Shahidi H, Sickora C, Clancy S, Nagurka R. Community health workers recruitment from within: an inner-city neighborhood-driven framework. BMC Res Notes. 2015;24(8):715.
Taylor C, Nhlema B, Wroe E, Aron M, Makungwa H, Dunbar EL. Determining whether Community Health Workers are ‘Deployment Ready’ Using Standard Setting. Ann Glob Health. 2018;84(4):630–9.
Surjaningrum ER, Jorm AF, Minas H, Kakuma R. Personal attributes and competencies required by community health workers for a role in integrated mental health care for perinatal depression: voices of primary health care stakeholders from Surabaya, Indonesia. Int J Ment Health Syst. 2018;14(12):46.
Jones TM, Schulte A, Ramanathan S, Assefa M, Rebala S, Maddox PJ. Evaluating the association of state regulation of community health workers on adoption of standard roles, skills, and qualities by employers in select states: a mixed methods study. Hum Resour Health. 2021;4(19):148.
Ignoffo S, Margellos-Anast H, Banks M, Morris R, Jay K. Clinical Integration of Community Health Workers to Reduce Health Inequities in Overburdened and Under-Resourced Populations. Popul Health Manag. 2022;25(2):280–3.
Download references
This project was supported by the Robert Wood Johnson Foundation Clinical Scholars Program. Anna Volerman was also supported by the National Heart, Lung, and Blood Institute (K23 HL143128).
Author information
Authors and affiliations.
Department of Medicine, University of Chicago Biological Sciences Division, 5841 S. Maryland Ave, Chicago, IL, USA
Monica Kowalczyk, Nicole Yao, LaToya Gregory & Anna Volerman
Department of Pediatrics, University of Chicago Biological Sciences Division, 5841 S. Maryland Ave, Chicago, IL, USA
Jeannine Cheatham & Anna Volerman
Chicago Public Schools Office of Student Health and Wellness, 42 W. Madison St, Chicago, IL, USA
Tarrah DeClemente & Kenneth Fox
Sinai Urban Health Institute, 1500 S. Fairfield Ave, Chicago, IL, #1782, USA
Stacy Ignoffo
You can also search for this author in PubMed Google Scholar
Contributions
JC, TD, KF, SI, and AV acquired funding for study. JC, TD, KF, MK, SI, and AV conceptualized study. MK and AV designed study and collected data. LG, MK, AV, and NY analyzed and interpreted data. MK and NY drafted manuscript. All authors critically revised manuscript.
Corresponding author
Correspondence to Anna Volerman .
Ethics declarations
Ethics approval and consent to participate.
This study was deemed exempt by the University of Chicago’s Institutional Review Board. Participants provided verbal informed consent prior to participating in this study.
Consent for publication
This study did not include an identifying information of participants, thus consent for publication was not required.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kowalczyk, M., Yao, N., Gregory, L. et al. Community health worker perspectives: examining current responsibilities and strategies for success. Arch Public Health 82 , 94 (2024). https://doi.org/10.1186/s13690-024-01313-5
Download citation
Received : 18 January 2024
Accepted : 02 June 2024
Published : 21 June 2024
DOI : https://doi.org/10.1186/s13690-024-01313-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Community health workers
- Workforce sustainability
- Logic model
- Health equity
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]

Healthcare PPE Selection Guidance Research Gaps Identified Through Literature Review
Degree grantor, degree level, degree name, committee member, thesis type, usage metrics.
- Open access
- Published: 26 June 2024
Health care workers’ self-perceived meaning of residential care work
- Sui Yu Yau 1 ,
- Yin King Linda Lee 1 ,
- Siu Yin Becky Li 1 ,
- Sin Ping Susan Law 1 ,
- Sze Ki Veronica Lai 1 &
- Shixin Huang 2
BMC Health Services Research volume 24 , Article number: 766 ( 2024 ) Cite this article
137 Accesses
Metrics details
Attracting and supporting a sustainable long-term care (LTC) workforce has been a persistent social policy challenge across the globe. To better attract and retain a sustainable LTC workforce, it is necessary to adopt a unified concept of worker well-being. Meaning of work is an important psychological resource that buffers the negative impacts of adverse working conditions on workers’ motivation, satisfaction, and turnover intention. The aim of this study was to explore the positive meaning of care work with older people and its implications for health care workers’ job satisfaction and motivation to work in the LTC sector.
This study adopted a qualitative descriptive design that pays particular attention to health care workers; such as nurses, personal care workers; as active agents of the meaning making and reframing of care work in LTC communities in a East Asia city. In-depth semi-structured interviews were conducted with thirty health care workers in LTC communities in Hong Kong. Thematic analysis was employed for data analysis.
The research findings indicate that while health care workers perform demanding care work and experience external constraints, they actively construct positive meanings of care work with older people as a helping career that enables them to facilitate the comfortable aging of older people, build affectional relationships, achieve professional identity, and gain job security.
Conclusions
This qualitative study explores how health care workers negotiate the positive meaning of older people care work and the implications of meaningful work for workers’ job satisfaction and motivation to work in the LTC sector. The importance of a culturally sensitive perspective in researching and developing social policy intervention are suggested.
Peer Review reports
Introduction
Recruiting and retaining health care workers (HCWs) in the long-term care (LTC) sector is a persistent worldwide social policy challenge [ 1 ]. Across the globe, population aging will create significantly higher demands for LTC services for older people. These demands include residential care services, especially among older people with complex care needs due to age-related disabilities and chronic diseases [ 2 ]. Comprised mainly of nurses and personal care workers, HCWs in LTC communities perform a variety of tasks that are essential to maintain the functional ability of older people, including helping with activities of daily living (ADL) (such as bathing, toileting and eating), instrumental activities of daily living (IADL) (such as taking medication), monitoring and coordinating care, and communicating with older people and their families [ 3 ]. Despite the growing demand and significance of LTC services, health care work in LTC communities is often devalued as “dirty work” and characterized by low wages, precarious working conditions, limited career development opportunities, understaffing, and work overload [ 4 ].
In the context of LTC communities, while the research to date has extensively evaluated the demanding working conditions that lead to negative well-being outcomes for HCWs [ 1 ], relatively little is known about the positive meaning that HCWs experience in, and attribute to, their care work in LTC communities [ 5 ]. Further exploration of how HCWs engage in meaningful work is helpful to the development of strategies that improve worker well-being and other work outcomes in LTC communities, especially job satisfaction and worker retention. In addition, cultural and social contexts exert a heavy influence on the meaning of care [ 6 ]. Most of the current literature on older people care work has been produced and addressed in Anglo-American contexts; there are limited evaluations of the meanings and experiences of older people care work from the perspectives of HCWs in East Asia, a region that is characterized by a large, rapidly aging population and unique socio-cultural meanings of older people care. A culturally sensitive understanding of what contributes to meaningful work in the LTC setting is thus needed to attract and support the LTC workforce beyond the Western contexts. Thus, this qualitative study aims to examine how HCWs in LTC communities construct positive meanings of older people care and also the implications of meaningful work for their job satisfaction and intention to stay in the LTC sector in Hong Kong, in the People’s Republic of China. This study is produced as part of a larger research project examining the social construction of stigma attached to older people care work in Hong Kong’s LTC communities [ 7 ] and pays particular attention to HCWs’ meaning construction in relation to the policy, organizational, and socio-cultural contexts to inform LTC workforce development policy.
Constructing meaning of work in LTC communities
Meaning of work (MOW) is an important psychological resource that buffers the negative impacts of adverse working conditions on workers’ motivation, satisfaction, and turnover intention [ 8 , 9 ]. Across different occupational contexts, organizational scholars have consistently found that MOW is a significant aspect of workers’ subjective well-being and is associated with positive worker and organizational outcomes, including higher work engagement, organizational commitment, worker retention, and productivity [ 10 ]. MOW refers to “employees’ understandings of what they do at work as well as the significance of what they do” [ 11 ]. It captures how employees make sense of their experiences at work, as well as the role of work in the context of life [ 12 ]. MOW consists of three primary facets: positive meaning in work, meaning making through work, and greater good motivation [ 13 ]. Meaning in work concerns individuals’ subjective interpretations of experiences and interactions at work in terms of the values, attitudes, and beliefs that they see as intrinsic to the nature of their work and working relationships [ 10 ]. Meaning making through work involves the idea that work could serve as a critical avenue for meaning making in life, such as facilitating personal growth, deepening self-understanding, and attaining personal and professional identity [ 14 ]. Lastly, greater good motivation implies the perception that one’s work has positive impacts on the greater good, ranging from generating positive contributions to others to responding to the meaning of work [ 15 ].
Although MOW is experienced by individual employees as feelings and cognitions, a sociological perspective of MOW suggests that the meaning individuals ascribe to their work is constructed within an array of socially influenced worldviews regarding the value of their work activities [ 16 ]. Individuals’ meaning making of their jobs, roles, and selves at work is a dynamic process that is influenced by the social and interpersonal valuation and devaluation of their work [ 11 ]. Work in the LTC sector is often socially constructed as “dirty work” that is physically, socially, and morally tainted [ 17 , 18 ]. The social discourses on “dirty work” are further reinforced by the emotionally and physically demanding nature of care work, as well as the poor job quality in the LTC sector [ 19 ]. Work in LTC communities is typically characterized by poor compensation, heavy workloads, precarious part-time employment, limited career development prospects, limited training and supervision, and low occupational status compared to other healthcare fields [ 20 ].
Given these external constraints, it is not surprising that HCWs in LTC communities feel disempowered to make positive sense of their care work [ 21 ], which in turn negatively influences their job satisfaction and intention to work in the LTC sector [ 17 ]. Despite the social devaluation and demanding nature of older people care work, HCWs in LTC communities could actively engage in negotiating the meaning of their work and construct positive career identities to overcome the taint of dirty work, a research theme that to date remains underdeveloped [ 22 ]. These positive meanings might include forming caring relationships with older people [ 5 ].
Residential care services and LTC workforce in Hong Kong
Health care workers in LTC communities negotiate the meaning of care work within particular social policy, organizational, and socio-cultural contexts [ 7 ]. Given the drastically increasing demand for residential care among older people, the chronic workforce crisis in the LTC sector, and the transforming socio-cultural meaning of care for older people [ 4 ], it has never been timelier to explore the meaning of work in Hong Kong’s LTC communities.
Hong Kong is an economically advanced metropolis located in the Southern part of China. With increasing life expectancy, Hong Kong’s aging population is projected to increase from 1.12 million (or 15% of total population) in 2015 to 1.51 million (or 30.6% of total population) in 2043, significantly higher than the OECD (Organisation for Economic Co-operation and Development) average percentage (25% in 2043) [ 23 ]. As a result, the demand for LTC services, including residential care services, will also increase drastically. The limited residential spaces, the transformation of family structure, and the imbalanced public investment in community and residential care have turned the number of older people who require residential care in Hong Kong into one of the highest among developed economies [ 24 ].
Hong Kong adopts a hybrid model in the financing and provision of its residential care services. In 2022, there were about 76,200 older people require residential care in Hong Kong, among which 46% (or a total number of 35,040) were subsidized by the government and 54% (or a total number of 41,160) were non-subsidized [ 25 ]. While residential care services in general are provided by non-governmental organizations (NGOs) (31%) and the private sector (69%), the majority of subsidized residential services are provided by NGOs, although the government also purchases subsidized places and services from private facilities [ 26 ]. Like many developed economies, Hong Kong has experienced an acute shortage of HCWs in LTC communities [ 26 ]. Even though the Hong Kong government has initiated many measures over the past few years to tackle the issues of the care workforce crisis, such as increasing salaries, launching different schemes to train young people and encouraging migrant workers to join the LTC communities, 20% of HCW positions in LTC communities remain vacant [ 27 ].
HCWs’ well-being is indeed connected to workforce attraction and retention. Despite the Hong Kong government initiating various ongoing measures to increase the number of workforce in LTC sector, there will be a shortfall of 4,500 HCWs in the next three year [ 28 ]. To better attract and retain a sustainable LTC workforce, it is necessary to adopt a unified concept of worker well-being that not only addresses the structural factors, such as economic and physical working conditions, but also the subjective factors that attract and motivate workers to join and remain in the LTC sector, including promoting meaningful, valued work [ 29 , 30 ]. Caring for older people entails unique socio-cultural meanings in Hong Kong and East Asian societies. Although sociodemographic changes have transformed the patterns of social care for older people, most noticeably exemplified by the rising demand for residential care, such cultural norms still exert significant influences on the meaning of care work [ 31 ]. The aim of this study was to explore the positive meaning of care work with older people and its implications for health care workers’ job satisfaction and motivation to work in the LTC sector.
This study adopted a qualitative descriptive design that focuses on HCWs as active agents of the meaning making and reframing of care work in LTC communities. The use of qualitative descriptive design is common in health care research because of its simplicity and flexibility in diverse healthcare environment. Qualitative research is appropriate to explore experiences and perceptions on subjective nature of a phenomenon. It is especially suitable for nursing and healthcare studies that interested in individual’s experience [ 32 ]. Thus, this design is particularly relevant to this study which aimed to explore the positive meaning of care work with older people and its implications for health care workers’ job satisfaction and motivation to work in the LTC sector.
In the context of Hong Kong, HCWs in LTC communities include personal care workers (PCWs) who take care of residents’ ADL and IADL, health workers (HWs, largely equivalent to “certified nursing assistants” in the United States) who monitor the work of PCWs and are responsible for the delivery of basic nursing care, and enrolled nurses (ENs) and registered nurses (RNs) who provide nursing care and oversee the work of PCWs and HWs.
Recruitment sample
Purposive sampling was used to recruit HCWs from LTC communities as research participants. To meet the inclusion criteria, participants had to (1) be serving in the role of a PCW, HW, EN, or RN; (2) have at least 6 months of experience working in an LTC community; and (3) be providing frontline services to older people. The exclusion criteria were as follows: (1) LTC workers who had only a managerial role and did not provide frontline care; (2) LTC workers working in other roles (e.g., social workers, occupational therapists, physical therapists). In the process of participant recruitment, the maximum variation sampling method was used to ensure the heterogeneity of participants in terms of participants’ characteristics. The use of maximum variation sampling method aimed to recruit information-rich participants and to capture the widest range of possible perspectives [ 33 ]. Thus, in order to ensure maximum variation, this study recruited participants based on a variety of nature such as gender, age, role and rank, years of work experience, and types of LTC communities worked for including publicly subsidized and private communities.
Six LTC communities were approached by the researchers. The managerial staff of each LTC community was invited to refer potential participants to the researchers after briefed for the purpose of the study, as well as the inclusion and exclusion criteria of the sample. The researcher (S. Huang) liaised with the managerial staff to schedule the logistics. Participants were fully informed of the purpose and procedures of the study. Informed consents were obtained before data collection commenced. Pseudonyms were used in the study in order to protect participants’ identities.
Data were collected between February 2021 and December 2021. Thirty participants were recruited in the study. The average age of the participants was 37 years old, and their mean years of tenure in the care sector were 7 years. Reflecting the gender ratio of the overall population of the care workforce, 5 participants were male and 25 were female. Thirteen of the participants worked as nurses (five RNs and eight ENs), eight worked as HWs, and nine were PCWs. Sixteen participants had attained a post-secondary education and 13 had earned secondary education, with only one participant having received primary or below education (see Table 1 for demographic data of the participants) [see Additional file 1].
Data collection
Semi-structured in-depth interviews were conducted. Interviewers were trained in qualitative study methods and came from a variety of healthcare research backgrounds of nursing and social work. Interviews were conducted in private meeting rooms in LTC communities. Interview sessions lasted from 30 to 80 min (mean = 55 min). Cantonese was adopted in the interviews. An interview guide was developed for this study [see Additional file 2]. Each interview began with general questions revolving around the nature of the participant’s work and daily work routines, followed by exploratory questions that unraveled the meanings the participant made from her/his work. With the written informed consent of participants, all interviews were audio-recorded and transcribed verbatim.
Data analysis
Thematic analysis [ 34 ] was used to analyze the interview data. Adopting an inductive approach to analysis, this study followed the six-phase approach to thematic analysis that includes (1) data familiarization, (2) coding, (3) initial theme generation, (4) theme development and review, (5) refining, defining and naming themes, and (6) writing up [ 35 ]. Two experienced qualitative researchers (V. Lai and S. Huang) coded each interview transcript independently. Transcripts were coded with the facilitation of the qualitative research data analysis software NVivo 12. All the authors met regularly to review interview transcripts, compare coding, and generate initial analytical themes together. Disagreements regarding coding were raised and discussed in team meetings until agreements were reached. Two authors then finalized the processes by developing, reviewing, refining, defining, and naming themes.
The trustworthiness and rigor of the study was ensured by credibility, dependability, confirmability and transferability [ 36 ]. In order to enhance the credibility, two researchers read the transcripts and conduct coding independently for comparison. They discussed the emergent themes and codes until a consensus was researched. Dependability was achieved by using an audit trail that detailed the description of the research process to reduce bias. Peer debriefing with an expertise was used for confirmability. Transferability of findings was attained by describing the participant characteristics and the methodology of the study transparently and comprehensively in order to allow readers understood the strengths and limitations of the study.
Engaging in care for others can be highly rewarding work as reflected from the participants. Five themes identified from the data that articulated the positive meaning that HCWs ascribed to their work in LTC communities, including (1) “My work makes their lives more comfortable”: Helping older people to age comfortably; (2) “Everyday our affections increase”: Building meaningful relationships; (3) “These are all skills”: Forming a professional identity of older people care; (4) “I want to find a job that ensures I will never be unemployed”: Ensuring job security; and (5) “They are extra work”: Barriers to attaining the positive meaning of work.

“My work makes their lives more comfortable”: Helping older people to age comfortably
When making meaning of their work, the HCWs most frequently evoked the notion of helping older people to “age comfortably” in LTC communities. The idea of comfortable aging, as suggested by HCWs in this study, referred to both physical well-being (i.e., having desirable health outcomes and being free of pain) and psychosocial well-being. The physical and psychosocial well-being entailed the traditional socio-cultural values in Chinese society.
The HCWs suggested that their care activities supported older people’s comfortable aging by maintaining and even improving their physical health. The HCWs in LTC communities engaged in a variety of caregiving tasks in their everyday work. The daily work routine of the HWs, ENs, and RNs revolved around addressing the health needs of older residents through clinical and medical activities such as wound dressing, medication administration, peritoneal dialysis, tube feeding, etc. The care activities of the PCWs included personal care such as assisting with bathing, dressing, eating, toileting, transferring, grooming, etc., depending on the frailty level of the older residents. The HCWs suggested that they found their work meaningful because their care activities were helpful to older residents achieving desirable health outcomes.
I feel happy because my work makes their lives more comfortable. For example, a resident’s wound was quite severe and was at stage one or stage two before intervention. Then, we had multiple interventions and dressed the wound one shift after another until it finally healed. I gained a sense of fulfillment in the process. This process made me feel that our care was effective. (EN2)
As demonstrated by a participant, in the process of helping older people maintain their physical health, HCWs gain a strong sense of self efficacy and job satisfaction. Even though the HCWs pointed out that their care did not always lead to full recovery as many older people in LTC communities are physically frail and experiencing health deterioration, they deemed their work to be meaningful because it helped older people maintain the highest level of physical comfort possible.
Not everyone recovers. Some are not in a good condition, but at least my care helps to ensure they are not too bad. Even though they cannot recover fully, their wounds might get smaller or not deteriorate any more. They don’t feel so much pain… They can feel more comfortable. (HW3)
In addition, the HCWs suggested that their everyday care conveys companionship and psychological support to older people in LTC communities, which is also essential to their comfortable aging.
Actually, the meaning of taking care of them is about being part of their last journey of life. In other words, I can create a happy and comfortable later life for them before they pass away. There is someone who can talk with them and provide good care to them. For me, that is what nursing care is about. (EN4)
The idea of facilitating comfortable aging espoused by HCWs has socio-cultural relevance in Chinese society, where providing care to older people to enable their comfortable aging is seen as a moral virtue. Several HCWs, including those in younger ages, framed their care as rewarding and meaningful work as they believed that taking good care of older people would “accumulate good karma” for themselves and their family.
I quite like taking care of older people. It is like some sort of traditional thought… I think taking care of older people is accumulating good karma. I believe that this is beneficial to my family and myself. (EN1) I think it is accumulating good karma. When taking care of older people, I am thinking that if I take good care of them now, I will be treated well by others when I get old and need care from others in the future. I do my work with this mindset. Therefore, I do not see my work as hard or dirty. (HW4)
“Every day our affections increase”: Building meaningful relationships
The second theme that the HCWs ascribed to their work concerned the valuable long-term relationships they built with older residents in their daily work, through which they found joy and personal growth.
HCWs, especially the nurses, constantly drew comparisons between LTC communities and other health care settings, such as hospitals, when discussing the meaning of their work. They suggested that working in a LTC facility allowed them to form long-term, genuine bonds with the older people they cared for, something they argued was rarely possible elsewhere. According to a participant, residential homes allow “the cultivation of human relationships and affection that is absent in hospitals” (RN3). A participant further elaborated:
I like talking with people. Working in a hospital is like fighting a war. I had no time to know the backgrounds of my patients. I couldn’t even remember their names when they were discharged from the hospital. Then, I will never see them again… However, LTC communities are very different. The conditions of the older people we serve are more stable. I have more time to get along with them. (EN6)
The cultivation of relationship involves human interaction and emotional exchange as reflected from the participants. The HCWs believed that they were the ones who provided “close, personal care” to the residents. In the process of performing everyday care activities, they had frequent interactions and developed close relationships with older people. Many participants suggested that being able to communicate and interact with older people was the most enjoyable part of their work. Despite the challenges of caregiving work, participants found their relationships with older residents “joyful”, “satisfying”, and “rewarding”.
When I perform my work and provide care to them, I gain joy and fun out of it. I feel happy to interact with people. [The happiness] is very personal. It might be chatting with a resident and receiving an unexpected response. Some residents with dementia are very funny. They always come up with something unexpected and make me feel happy. (HW4) The sense of satisfaction comes from my interactions with older people. Every day, our affections increase. They treat me like their granddaughter. I think acknowledgement from the boss does not matter a lot; I feel the biggest sense of satisfaction by getting the acknowledgement of the older people. They personally experience how well I deliver care. (EN5)
Moreover, some HCWs reported that their relationships with older residents were “reciprocal”, not only because they constantly received appreciation from the residents but also, more importantly, because they were able to learn “old wisdom” and achieve personal growth from the lived experiences of the older residents.
It is not only about providing a service to them; sometimes when I talk with them, they offer me their perspectives, from which I can learn something. This is more like a reciprocal relationship…Sometimes, the older people have old wisdom and special perspectives. (RN4) I think I learn a lot from the older people because I meet a lot of people here and learn about their lived experiences from our conversations. They like sharing with me and I can reflect upon myself… (HW5)
“These are all skills”: Forming a professional identity of older people care
HCWs proposed that older people care is highly skillful and professional, requiring communication, coordination, and chronic illness care skills. Being able to form a professional identity as a HCW for the older people thus constituted a salient MOW for the participants.
Participants in this study reported that they constantly experienced devaluation of their work by their family, friends, and health care professional allies, who regarded care work in LTC communities as “dirty, less skilled, and unprofessional”.
People imagine that this work is about changing diapers and dealing with shit and piss… My aunt used to say to me that she’d rather beg than work in a residential home. People are not willing to join this sector because they think older people care is dirty work and cannot accept dealing with human excreta. (PCW4) They think that we work here because our nursing skills are not competent enough to work as hospital nurses. But when they hear that I am working in an LTC community, they doubt that my work is different from that in hospitals. They doubt that we work here because our nursing skills are not competent enough to work as hospital nurses. (EN6)
Contrary to the negative evaluations of their work, the HCWs evoked positive meanings of care work in LTC communities. One participant described that care in LTC communities and care in hospitals were “both part of the continuum of care that tackles the different health needs of older people, ranging from acute disease to long-term chronic illness” (RN5). More importantly, their care work in LTC communities allowed them to reimagine the nature of health care from delivering physical care tasks to providing holistic care that included psychological support, health education, human communication, resource coordination, and organizational management.
It is wrong to assume that nurses working with older people are not professional. Instead, we are differently professional in our specialties. For hospital nurses, their professional expertise lies in emergency treatment. But working in LTC is professional in terms of mastering the daily operation of a facility, governmental ordinances, and communication with family members. (RN2)
While the HCWs framed their work as valuable and professional, the HCWs described how performing personal care for older residents, such as positioning, lifting, transferring, feeding, and bathing, requires specialized knowledge, training, and experience.
Everything, every machine here requires specialized knowledge and training to handle. It is not that straightforward and simple. So, working as a PCW is not only about changing diapers. We need to grasp health and medical knowledge to monitor older peoples’ vital signs. We must also monitor whether the older people have bruises or wounds. We must be very careful to know whether the older people are doing ok. These are all skills. (PCW2)
Participants indicated that there were many other aspects that distinguished them as “professional” that further produced meanings and values in their personal life. One participant, a HW, indicated that working in LTC communities enabled her to work with interdisciplinary professionals such as doctors, nurses, nutritionists, social workers, physical therapists, and occupational therapists and thus allowed her to gain health knowledge. Many HCWs mentioned that the older people care knowledge and skills they learned from work could be useful in their personal life, particularly in terms of taking care of their older parents and grandparents at home.
“I want to find a job that ensures I will never be unemployed”: Ensuring job security
HCWs, especially PCW and HW working in government-subsidized facilities, perceived that the LTC sector offers relatively promising job opportunities and security, a stable income, and a career development pathway. These instrumental values made the LTC sector attractive for the participants.
Across the globe, the LTC sector has long been suffering from the challenge of workforce shortage. For participants in this study, however, this challenge was perceived as a positive opportunity that added value to their jobs. Many proposed that they found older people care as meaningful work because with the trend of population aging, there would always be increasing workforce demands in the job market which could provide them with promising job opportunities and security. Some HCWs also mentioned that the job offered them income stability, which they deemed as valuable compared to other work in the service industry.
The availability of job stability and opportunities in older people care work was particularly salient for participants during the COVID-19 pandemic, when the unemployment rate was high due to economic recession. Several participants described that they joined the LTC sector during the COVID-19 pandemic for the stability it offered. For example, a participant described, “I was working in the hotel industry…Then I lost my job and couldn’t find a new one. I wanted to find a job that will ensure I will never be unemployed.” (PCW5).
In addition, participants suggested that they found their work meaningful because of the relatively promising career development opportunities. The LTC sector in Hong Kong provides HCWs with a career pathway and ladder to pursue career development. Although promotion and degree admission opportunities are highly competitive, some participants saw the career ladder that moves up from PCW, HW, and EN to RN as a promising pathway for them to gain better income and work benefits.
“They are extra work”: Barriers to attaining meaning of work
Despite the HCWs ascribing a variety of positive meanings to their work, they admitted that it was not always possible to attain these meanings in their everyday work. They identified several barriers to attaining MOW, including the lack of organizational support for relational care, heavy workloads and workforce shortages, as well as emotional burnout.
As described above, HCWs found that the relational components of their work, particularly the helping relationships and affectional interactions with older residents, made the work highly meaningful. However, participants reported that although the LTC sector had long placed emphasis on person-centered care, they received little organizational support to develop meaningful relationships in their everyday work. Given that their daily work routines and timetables were predominantly organized around the delivery of physical caregiving tasks, many HCWs described an important and meaningful part of care work – relationship building and psychological support – as “extra” work that received little organizational recognition.
Of course, a lot of my work with the residents is extra work. I prefer to deliver holistic care that goes beyond physical care. Physical care tasks are those that appear on the timetable. But for the other parts, I must address them for the residents at other times by myself. (RN1)
Moreover, the heavy workloads and the chronic lack of workers in LTC communities impose further strains on HCWs in fulfilling their daily work routines, making it even more difficult for them to provide relational care. Despite these organizational constraints, the HCWs reported that they creatively made time and space in and between their work routines to build relationships and address older residents’ psychosocial well-being needs.
When I distribute medications, I usually have casual chats with the residents by greeting them and asking how their sleep and meals went. Just chatting. But it depends on the situation. When accidents happen, I would be too busy to handle this. (HW2) Sometimes I am very busy and do not have time to interact with the residents at all… I usually use meal times when I am more or less available. Residents are usually sitting and waiting for meals before we distribute them. I will use the ten minutes or so to chat with them. (HW1)
Relationship building and affectional interaction can be satisfying and exhausting simultaneously. The HCWs described the high emotional demands from older people and their family members they had to bear in their everyday work, which frequently put them in a situation of emotional burnout which can detract from building meaning. In addition, some HCWs reported that it took a lot of emotional labor (i.e. to manage feeling as to fulfill job requirement) to care for older residents with difficult behaviors or personalities, especially those with declining mental health and dementia. They said that they constantly experienced distrust, blaming, and rejection from older residents when they performed caregiving tasks such as feeding, which added a considerable amount of strain to their work. Similarly, the HCWs had to deal with constant distrust and misunderstanding from residents’ family members, which caused some of them frustration and stress.
This is work that cannot get understanding from everyone. Some [family members of the residents] would not notice my efforts to care for the residents. However, if I make a minor mistake, they will blame me. Human beings make mistakes and are not perfect. I am also sincerely concerned for the older people, but they don’t understand and blame me for my mistake. (PCW7)
This study examines HCWs’ engagement in meaningful work in LTC communities in the context of an economically developed Chinese society in Hong Kong. It is found that HCWs deemed their work to be a meaningful helping career that facilitated comfortable aging for older people and connoted positive socio-cultural values. They further attributed their MOW to the valuable relationships developed in their daily work and to the positive professional identity and relatively promising job security in their work, although the attainment of positive MOW was hindered by a number of barriers. In this discussion, we describe how these findings can support social policy initiatives to attract, retain, and support the LTC workforce.
To date, research and social policy interventions on LTC workforce development have largely focused on structural factors that influence the retention of HCWs and their job satisfaction [ 37 ]. Studies informed by this line of inquiry have identified the importance of working conditions, especially pay and compensation, workload and staffing level, teamwork, and supervision, in shaping work-related outcomes [ 29 , 38 , 39 ]. Even though the positive organizational scholarship has long argued the beneficial impacts of positive psychological states, including perceptions of meaningful work, on workforce functioning and productivity [ 40 ], relatively little attention has been paid to positive working experiences in the LTC sector. Our study moves a step forward from the current literature by shedding light on the subjective meaning making of work as an important, yet often overlooked, aspect of direct care work in LTC communities. While the structural factors of working conditions are pivotal to the job quality in LTC communities, MOW can serve as a psychological resource that engenders positive emotions and motivates HCWs to engage in direct care work in LTC communities. The findings of this study thus provide nuanced evidence about promoting meaningful work as a promising intervention for LTC workforce development. This could be done by addressing structural factors such as promoting job security, improving time and resource constrains, enhancing organizational support in LTC communities. Also, this could be done by supporting relationship building and better integrating psychosocial care into older people care work and exploring socio-cultural resources that contribute to positive meaning making of older people care work. In addition, as an extension of this qualitative study, quantitative research that examines the impacts of MOW on workers’ turnover intention and job satisfaction, as well as MOW as a mediating mechanism in explaining the impacts of working conditions on worker outcomes in the LTC sector, will be an important area for future exploration.
The findings of this study also imply that the meaning construction of older people care should be further understood and supported in the broader contexts, including the LTC policy, organizational support, and the socio-cultural meaning of older people care. As indicated by our research findings, the professional identity and job security in the LTC sector are important parts of HCWs’ MOW. While research to date has stressed the lack of job security and professional status in the LTC sector [ 41 ], our study has provided somewhat contradictory findings. Participants in the present study has relatively positive perceptions about career prospects in the LTC sector, proposing that the growing demand for LTC in the face of population aging entails job opportunities and job security, both of which make a career in LTC attractive. The nurses highlighted that their work was different to but equally as professional, skilled, and challenging as acute hospital care. Some indicated that their nursing care experiences in LTC communities allowed them to develop specialties in chronic disease management to maintain the wellness and quality of life of older people. This positive perception of LTC work is partly shaped by the preliminary, yet far from finished, social policy attempts to professionalize the LTC workforce in the local context. In Hong Kong, LTC policy has laid out the foundation of a relatively promising career development pathway in the nursing profession for HCWs in the LTC sector, most noticeably through the establishment of the Vocational Qualifications Pathway (VQP) for the LTC service industry and professional training programs [ 42 ]. Our findings thus call for research and social policy interventions to address the professionalization of the LTC sector and enable HCWs to gain public recognition, rewarding pay, job security, and career development.
Additionally, the findings of this study add to the existing studies on working conditions in LTC communities by highlighting the lack of organizational support for relational care as an organizational barrier to attaining meaningful work. Our study echoes existing research findings that HCWs deem affectional interactions and long-term relationships with older people as meaningful and valuable [ 29 ]. Yet HCWs’ yearning for meaningful relationships with older people is constantly constrained by the organizational structures of LTC communities, particularly the traditional institutional model of care centered around measurable and functional caregiving tasks [ 43 , 44 ]. The culture change movement that calls for humanizing care practice by transforming the institutional form of care in LTC communities to person-centered and relational care [ 45 , 46 ]. This culture change movement is thus particularly relevant to promoting the meaningful work of HCWs. Facilitating positive, meaningful working experiences for the LTC workforce would require changes in the organizational cultures of LTC communities to enable flexible caregiving routines, professional training opportunities that address relationship and rapport building, and a humanizing working environment.
Lastly, the meaning of older people care is constructed under an array of socio-cultural values. Even though increasing scholarly attention is being paid to revealing a culturally sensitive approach to older people care [ 47 ], very few studies have examined the socio-cultural meanings and values attached to older people care work from HCWs’ perspectives in the international contexts. As illustrated in this study, the notion of facilitating comfortable aging was seen as “accumulating good karma” and contained socio-cultural meaning towards older people care within the Chinese society. While engaging in older people care work is socially constructed as a “dirty work” [ 17 ], it could entail cultural salience and be regarded as a rewarding career in a society that values the life experience and moral authority of older people. This finding thus reveals the importance of a culturally sensitive perspective in researching and developing social policy interventions for LTC workforce development, including promoting a culturally resonant positive image of work in the LTC sector. This policy implication is not only resonant to other Asian societies, but also to the international contexts as Asian migrant workers represent a considerable proportion of the LTC workforce in developed countries such as Australia, US, UK and other European countries [ 48 , 49 ].
Limitations
Although this study adopted the maximum variation sampling method to increase the variety of HCWs’ perspectives and experiences, its use of purposive sampling is limited in representativeness. Additionally, this research intended to explore the MOW for all types of HCWs (eg, EN, RN, HW, PCW). However, these HCWs have quite different working experiences and work meaning because of different job quality and professional status. As non-nurses are particularly vulnerable to the deprivation of subjective well-being in work because of the poor job quality of their work [ 5 ], future studies would benefit from examining the subjective meaning making of work among this specific group of workers.
This qualitative study explores how HCWs negotiate the positive meaning of older people care work and the implications of meaningful work for workers’ job satisfaction and motivation to work in the LTC sector in Hong Kong’s LTC communities. While HCWs perform physically and emotionally demanding care work, they actively construct a subjective meaning of older people care as a helping career that enables them to facilitate comfortable aging of older people, build affectionate relationships, achieve professional identity, and gain job security. Their construction of meaningful work is further discussed in an array of social policy, organizational, and socio-cultural factors that all entail future research and social policy implications of LTC workforce development.
Availability of data and materials
The datasets generated and analysed during this study are not publicly available to protect the participant' confidentiality. However, they are available from the corresponding author upon reasonable request.
Abbreviations
Activities of daily living
Enrolled nurses
Health care workers
Health workers
Instrumental activities of daily living
Long-term care
Meaning of works
Personal care workers
Registered nurses
Llena-Nozal A, Rocard E, Sillitti. Providing long-term care: options for a better workforce. Int Soc Sec Rev. 2022;75:121–44. https://doi.org/10.1111/issr.12310 .
Article Google Scholar
United Nations. Growing need for long-term care: assumptions and realities. 2016. https://www.un.org/esa/socdev/ageing/documents/un-ageing_briefing-paper_Long-term-care.pdf .
OECD. Who cares? attracting and retaining elderly care workers. 2020. https://doi.org/10.1787/92c0ef68-en .
Scales K. It is time to resolve the direct care workforce crisis in long-term care. Gerontologist. 2021;61:497–504. https://doi.org/10.1093/geront/gnaa116.PMID:32853357;PMCID:PMC7499598 .
Article PubMed Google Scholar
Vassbø TK, Kirkevold M, Edvardsson D, et al. The meaning of working in a person-centred way in nursing homes: a phenomenological-hermeneutical study. BMC Nurs. 2019;18:45. https://doi.org/10.1186/s12912-019-0372-9.PMID:31632193;PMCID:PMC6790040 .
Article PubMed PubMed Central Google Scholar
Leininger M. Special Research Report: Dominant culture care (EMIC) meanings and practice findings from Leininger’s Theory. J Transcult Nurs. 1998;8(2):45–48. https://doi.org/10.1177/104365969800900207 .
Lai VS, Yau SY, Lee LY, et al. Caring for older people during and beyond the COVID-19 pandemic: experiences of residential health care workers. Int J Environ Res Public Health. 2022;19(22):15287. https://doi.org/10.3390/ijerph192215287.PMID:36430006;PMCID:PMC9692584 .
Arnoux-Nicolas C, Sovet L, Lhotellier L, et al. Perceived work conditions and turnover intentions: the mediating role of meaning of work. Front Psychol. 2016;7:704. https://doi.org/10.3389/fpsyg.2016.00704.PMID:27242616;PMCID:PMC4863887 .
Humphrey SE, Nahrgang JD, Morgeson FP. Integrating motivational, social, and contextual work design features: a meta-analytic summary and theoretical extension of the work design literature. J Appl Psychol. 2007;92:1332–56. https://doi.org/10.1037/0021-9010.92.5.1332 . PMID: 17845089.
Steger MF, Dik BJ. Work as meaning: individual and organizational benefits of engaging in meaningful Work. Oxf Handbook Pos Psy Work. 2009. https://doi.org/10.1093/oxfordhb/9780195335446.013.0011 .
Wrzesniewski A, Dutton JE, Debebe G. Interpersonal sensemaking and the meaning of work. Res Org Behavior. 2003;25(03):93–135. https://doi.org/10.1016/S0191-3085(03)25003-6 .
Rosso BD, Dekas KH, Wrzesniewski A. On the meaning of work: a theoretical integration and review. Res Organ Behav. 2010;30:91–127. https://doi.org/10.1016/j.riob.2010.09.001 .
Steger MF, Dik BJ, Duffy RD. Measuring meaningful work: the Work and Meaning Inventory (WAMI). J Car Ass. 2012;20:322–37. https://doi.org/10.1177/1069072711436160 .
Westwood R, Lok P. The meaning of work in chinese contexts. Int J of Cross Cultural Mgt. 2003;3(2):139–65. https://doi.org/10.1177/14705958030032001 .
Dik BJ, Duffy RD. Calling and vocation at work. Couns Psychol. 2009;37:424–50. https://doi.org/10.1177/0011000008316430 .
Dutton JE, Debebe G, Wrzesniewski A. Being valued and devalued at work: a social valuing perspective. In B. A. Bechky & K. D. Elsbach (Eds.), Qualitative organizational research: best papers from the davis conference on qualitative research 2006, 9–51. https://psycnet.apa.org/record/2016-25892-002 .
Manchha AV, Way KA, Tann K, et al. The social construction of stigma in aged-care work: implications for health professionals’ work intentions. Gerontologist. 2022;12(62):994–1005. https://doi.org/10.1093/geront/gnac002.PMID:35018434;PMCID:PMC9372892 .
Yau SY, Lee YK, Li SY, et al. The social construction of “Dirty Work” for working in residential care homes for the elderly In: Law, V.T.S., Fong, B.Y.F. (eds) Ageing with dignity in Hong Kong and Asia. Quality of life in Asia, vol 16. Springer, Singapore. https://doi.org/10.1007/978-981-19-3061-4_5
Scales K. Transforming direct care jobs, reimagining long-term services and supports. J Am Med Dir Assoc. 2022;23(2):207–13. https://doi.org/10.1016/j.jamda.2021.12.005 . Epub 2021 Dec 29 PMID: 34973168.
Yeatts DE, Seckin G, Shen Y, et al. Burnout among direct-care workers in nursing homes: Influences of organisational, workplace, interpersonal and personal characteristics. J Clin Nurs. 2018;27:3652–65. https://doi.org/10.1111/jocn.14267 . Epub 2018 Jul 17 PMID: 29322572.
Scales K, Bailey S, Middleton J, et al. Power, empowerment, and person-centred care: using ethnography to examine the everyday practice of unregistered dementia care staff. Sociol Health Illn. 2017;39:227–43. https://doi.org/10.1111/1467-9566.12524 . PMID: 27891628.
Clarke M, Ravenswood K. Constructing a career identity in the aged care sector: overcoming the “taint” of dirty work. Pers Rev. 2019;48(1):76–97. https://doi.org/10.1108/PR-08-2017-0244 .
Working Group on Elderly Services Programme Plan. Elderly services programme plan. 2017. https://www.elderlycommission.gov.hk/en/download/library/ESPP_Final_Report_Eng.pdf .
Chui EW. Long-term care policy in Hong Kong: challenges and future directions. Home Health Care Serv Q. 2011;30(3):119–32. https://doi.org/10.1080/01621424.2011.592413 . PMID: 21846226.
The Government of the Hong Kong Special Administrative Region. Hong Kong Yearbook 2022. 2022. https://www.yearbook.gov.hk/2022/en/pdf/E14.pdf .
Lum T, Shi C, Wong G, et al. COVID-19 and long-term care policy for older people in Hong Kong. J Aging Soc Policy. 2020;32(4–5):373–9. https://doi.org/10.1080/08959420.2020.1773192 . Epub 2020 May 31 PMID: 32476597.
Social Welfare Department. Navigation scheme for young persons in care services. 2023. https://www.swd.gov.hk/en/pubsvc/elderly/cat_ms_ita/nsypcc/ .
Labour and Welfare Bureau. Measure to increase and enhance manpower resources for the sector of residential care homes for the elderly. 2023. https://www.legco.gov.hk/yr2023/english/panels/ws/ws_rcp/papers/ws_rcp20230214cb2-98-1-e.pdf .
Franzosa E, Tsui EK, Baron S. “Who’s Caring for Us?”: understanding and addressing the effects of emotional labor on home health aides’ well-being. Gerontologist. 2019;59(6):1055–64. https://doi.org/10.1093/geront/gny099 . PMID: 30124808.
Schulte PA, Guerin RJ, Schill AL, et al. Considerations for incorporating “Well-Being” in public policy for workers and workplaces. Am J Public Health. 2015;105:e31-44. https://doi.org/10.2105/AJPH.2015.302616 . Epub 2015 Jun 11. PMID: 26066933; PMCID: PMC4504308.
Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893–907. https://doi.org/10.1007/s11135-017-0574-8 . Epub 2017 Sep 14. PMID: 29937585; PMCID: PMC5993836.
Doyle L, McCabe C, Keogh B, et al. An overview of the qualitative descriptive design within nursing research. J Res Nurs. 2022;25(5):443–55. https://doi.org/10.1177/1744987119880234 .
Elena L, Luminita V, Aurelia M. Multi-stage maximum variation sampling in health promotion programs’ evaluation. J Prev Med. 2007;15:5–18.
Google Scholar
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. https://doi.org/10.1191/1478088706qp063oa .
Braun V, Clarke V. Thematic analysis. In E. Lyons & A. Coyle (Eds.), Analysing qualitative data in psychology 2021. https://doi.org/10.1037/13620-004 .
Lincoln Y, Guba E. Naturalistic inquiry. USA: Sage Publications; 1985.
Book Google Scholar
White EM, Aiken LH, Sloane DM, et al. Nursing home work environment, care quality, registered nurse burnout and job dissatisfaction. Geriatr Nurs. 2020;41(2):158–64. https://doi.org/10.1016/j.gerinurse.2019.08.007 . Epub 2019 Sep 3. PMID: 31488333; PMCID: PMC7051884.
Kemper P, Heier B, Barry T, et al. What do direct care workers say would improve their jobs? Differences across settings. Gerontologist. 2008;48 Spec 1:17–25. https://doi.org/10.1093/geront/48.supplement_1.17 . PMID: 18694983.
Matthews M, Carsten MK, Ayers DJ, et al. Determinants of turnover among low wage earners in long term care: the role of manager-employee relationships. Geriatr Nurs. 2018;39:407–13. https://doi.org/10.1016/j.gerinurse.2017.12.004 . Epub 2018 Feb 27 PMID: 29499899.
Simone SD. Conceptualizing wellbeing in the workplace. Int J Bus Soc Sci. 2014;5:118–22 https://ijbssnet.com/journals/vol_5_no_12_november_2014/14.pdf .
Scales K, Lepore MJ. Always essential: valuing direct care workers in long-term care. Pub Pol Aging Report. 2020;30:173–7. https://doi.org/10.1093/ppar/praa022 .
HKQF. Vocational qualifications pathway. 2019. https://www.hkqf.gov.hk/ecs/en/pathways/index.html .
Rockwell J. From person-centered to relational care: expanding the focus in residential care facilities. J Ger Soc Work. 2012;55:233–48. https://doi.org/10.1080/01634372.2011.639438 .
Ronch JL. Changing institutional culture: Can we Re-Value the nursing home?. J Ger Soc Work. 2004;43:61–82. https://doi.org/10.1300/J083v43n01_06 .
Kartupelis J. Relational care: improving lives for older people, carers and families. In making relational care work for older people. London: Routledge; 2020. p. 1–32.
Koren MJ. Person-centered care for nursing home residents: the culture-change movement. Health Aff (Millwood). 2010;29:312–7. https://doi.org/10.1377/hlthaff.2009.0966 . Epub 2010 Jan 7 PMID: 20056692.
Claeys A, Berdai-Chaouni S, Tricas-Sauras S, et al. Culturally Sensitive care: definitions, perceptions, and practices of health care professionals. J Transcult Nurs. 2021;32:484–92. https://doi.org/10.1177/1043659620970625 . Epub 2020 Nov 5 PMID: 33150857.
Negin J, Coffman J, Connell J, et al. Foreign-born aged care workers in Australia: a growing trend. Australas J Ageing. 2016;35:E13–7. https://doi.org/10.1111/ajag.12321 . Epub 2016 Jun 1 PMID: 27245976.
Willis E, Xiao LD, Morey W, et al. New migrants in residential aged care: managing diversity in not-for-profit organisations. J Int Mig Int. 2018;19(3):683–700. https://doi.org/10.1007/s12134-018-0564-2 .
Download references
Acknowledgements
We should like to thank the health care workers for participating in the study and the superintendents of the residential care homes for the older people to recruit the participants.
The work described in this paper was fully supported by a grant from the Research Grants Council of the Hong Kong Special Administrative Region, China (UGC/FDS16/M12/20).
Author information
Authors and affiliations.
Hong Kong Metropolitan University, Jockey Club Institute of Healthcare, 1 Sheung Shing Street, Homantin, Hong Kong
Sui Yu Yau, Yin King Linda Lee, Siu Yin Becky Li, Sin Ping Susan Law & Sze Ki Veronica Lai
The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong
Shixin Huang
You can also search for this author in PubMed Google Scholar
Contributions
Y.S.Y., L.Y.K.L., L.S.Y.B., L.S.P.S. and L.S.K.V. conceived the ideas for the research. H.S., L.S.Y.B., L.S.P.S. and L.S.K.V. collected the data. Y.S.Y. and H.S. analysed the data. H.S. led the writing with the help of Y.S.Y. All authors critically revised the manuscript for important intellectual content. All authors have approved the final version of the article.
Corresponding author
Correspondence to Shixin Huang .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Research Ethics Committee (REC) at Hong Kong Metropolitan University (HE-RGC2020/NHS04). All the participants provided written informed consent and consent to participate.
Consent for publication
The participants gave their consent to participate in the study. The names of the participants have been anonymized. Informed consent was obtained from all participants for the publication of images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yau, S.Y., Lee, Y.K.L., Li, S.Y.B. et al. Health care workers’ self-perceived meaning of residential care work. BMC Health Serv Res 24 , 766 (2024). https://doi.org/10.1186/s12913-024-11218-2
Download citation
Received : 30 January 2024
Accepted : 19 June 2024
Published : 26 June 2024
DOI : https://doi.org/10.1186/s12913-024-11218-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health care work
- Long-term care workforce
- Meaning of work
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Instructions for Authors
- BMJ Journals
You are here
- Online First
- Homecare workers needs and experiences in end of life care: rapid review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Catherine Forward 1 ,
- http://orcid.org/0000-0001-7890-8682 Zana Bayley 2 ,
- Liz Walker 3 ,
- Justine Krygier 4 ,
- Caroline White 3 ,
- Kasonde Mwaba 4 ,
- Helene Elliott-button 4 ,
- Paul Taylor 5 and
- http://orcid.org/0000-0001-6204-9158 Miriam J Johnson 4
- 1 Health and Social Care Workforce Research Unit , King's College London , London , UK
- 2 University of Hull , Hull , UK
- 3 Faculty of Health Sciences , University of Hull , Hull , Kingston Upon Hull , UK
- 4 Wolfson Palliative Care Research Centre, Hull York Medical School , University of Hull , Hull , Kingston Upon Hull , UK
- 5 Sheffield Centre for Health and Related Research , The University of Sheffield , Sheffield , UK
- Correspondence to Professor Miriam J Johnson, Wolfson Palliative Care Research Centre, University of Hull, Kingston Upon Hull, UK; miriam.johnson{at}hyms.ac.uk
Background Social homecare workers provide essential care to those living at home at the end of life. In the context of a service experiencing difficulties in attracting and retaining staff, we have limited knowledge about the training, support needs and experiences of this group.
Aim To gain a timely understanding from the international literature of the experience, training and support needs of homecare workers providing end-of-life care.
Methods We conducted a rapid review and narrative synthesis using the recommendations of the Cochrane Rapid Reviews Methods Group. Building on a previous review, social homecare worker and end-of-life search terms were used to identify studies. Quality appraisal was conducted using a multimethods tool.
Data sources CINAHL and Medline databases (2011–2023; English language).
Results 19 papers were included representing 2510 participants (91% women) providing new and deeper insights. Four themes were generated: (1) emotional support; homecare workers need to manage complex and distressing situations, navigating their own, their clients’ and clients’ family, emotions; (2) interaction with other social and healthcare workers; homecare workers are isolated from, and undervalued and poorly understood by the wider healthcare team; (3) training and support; recognising the deteriorating client, symptom management, practicalities around death, communications skills and supervision; (4) recognising good practice; examples of good practice exist but data regarding effectiveness or implementation of interventions are scant.
Conclusions Social homecare workers are essential for end-of-life care at home but are inadequately trained, often isolated and underappreciated. Our findings are important for policy-makers addressing this crucial challenge, and service providers in social and healthcare.
- Home Care Services
- Social care
- Terminal care
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/spcare-2023-004737
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Social homecare workers form part of an essential care network and workforce that enables people to remain at home during the last months of life.
Compared with other professionals delivering care in this context, they receive less training, support for career development or remuneration.
WHAT THIS STUDY ADDS
Some training exists for homecare workers, but the most beneficial and acceptable content, delivery and implementation of training remains unknown.
Homecare workers are often isolated from their own teams, and usually from the wider health and social care teams.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Community-based healthcare and social care workers include social homecare workers in training, interdisciplinary communication and support regarding end-of-life care.
The development and evaluation of widely available training content and guidelines for supportive practice are indicated to support this vital workforce.
Introduction
People living with advanced illnesses, approaching the end of life, often express a wish to remain at home as long as possible. 1–3 Homecare provision is an essential part of the network of care, which can support them in this preference 4–6 and is reflected in UK policy. 7 With policy and practice changes, alongside an ageing population, there is likely to be an increasing demand for homecare services alongside an increasingly complex client base with comorbidities requiring end-of-life care. 8
Social homecare workers not only support people at home with activities of daily living, but also provide emotional support and can help avoid unnecessary hospital admissions or unwanted transfer to institutional care. 4–6 Despite their essential role, homecare workers remain poorly paid, often lacking the support and training they need to fulfil a range of caring roles when clients have such complex needs. 9 Homecare agencies in the UK and elsewhere are struggling to recruit and retain care staff; a chronic problem exacerbated in the UK by the departure from the European Union and the effects of the COVID-19 pandemic. 10–12 Concerns around the difficulties of attracting people to the care workforce have focused attention on aspects of their working environment such as training and support.
The evidence around the experiences and training needs of homecare workers is limited. A review conducted in 2013 showed only nine papers examining the role of support workers in providing end-of-life care, eight of which studied assistant healthcare workers and only one examined social homecare workers. 13 However, the available literature confirms challenges regarding a lack of training about the specific needs of this client group, the emotional labour involved in this care and a lack of support for the homecare worker as health and care needs of their clients change. 13–16 Given the ongoing difficulties in recruiting and retaining care staff, 8 17 a more comprehensive understanding is required of the specific training and support needs of homecare workers when providing end-of-life care.
With a better understanding of the needs and experiences of homecare workers, more effective training and support can be developed to improve working conditions and care delivery. This review provides an update of the 2013 review 13 and focusses on the experience of homecare workers, as distinct from healthcare practitioners, given their different role, training background and working environment.
Given the focused nature of this topic and the current crisis in social care provision in many countries, a rapid scoping review was considered the most suitable to gain an insight into the current availability, content and quality of evidence. 17 18 Rapid reviews are commonly used when an understanding of the current evidence regarding a topic is required and resources, such as time, are limited. Quality searching and reporting standards still apply to ensure that the results remain relevant and reflect an accurate representation of the evidence. 18 We conducted this narrative rapid review guided by the recommendations of the Cochrane Rapid Reviews Methods Group. 19 We report it in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 20 The review was not registered, and a protocol was not prepared.
Search strategy and study selection
To build on the work by Herber and Johnston, 13 we used the same search terms for homecare workers, but excluded any related to healthcare workers (see table 1 ). The journal databases Medline and CINAHL were searched from May 2011 (the end date of the original search) to March 2023, restricted to English language texts and peer-reviewed papers. Given the topic and paucity of the literature, there was no restriction on the type of studies. The search was updated on 5 December 2023
- View inline
Search terms
Retrieved titles and abstracts were screened initially by one researcher (CF) against a priori eligibility criteria (see table 2 ) and checked independently by at least one other researcher (KM, ZB or JK). An additional reviewer (MJJ) was available in the event of persistent disagreement. In cases where it was unclear if a paper was suitable for inclusion, full papers were retrieved for further assessment for inclusion. Rationale for excluding papers included the population (eg, not end-of-life clients or patients) and the setting (eg, not homecare). The full process and reasons for exclusions are detailed in figure 1 .
Inclusion and exclusion criteria
- Download figure
- Open in new tab
- Download powerpoint
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
Data extraction
Data from included studies were extracted using a customised extraction form to record the study setting, focus and aims, study design, methodology, country of origin, client group and summary of findings. Data were extracted by author CF and independently checked by ZB and KM.
Quality appraisal was conducted using a tool (Hawker et al designed to apply to different study designs 21 ) used in the original Herber et al review 13 by CF. Papers were independently checked by one other researcher (ZB or JK) with any discrepancies being resolved by an additional researcher (MJJ).
Data analysis
A narrative synthesis 22 of the characteristics and key findings of the studies was undertaken. The key findings from each included study were initially summarised by CF and patterns observed to form a preliminary synthesis. This allowed a textual overview of the key issues. Relationships within and between studies were then explored, including possible explanation, which were discussed by all authors and revised iteratively to agree finalised themes.
Selected studies
The first database search identified 1506 papers; 1243 following deduplication. The process of selection is shown in the PRISMA flow chart ( figure 1 ). Following screening, 19 papers were included (see 1 online supplemental table 1 ). Two papers tested the same training evaluation; however, they focus on different aspects and therefore both are included in the review. No studies were identified from the updated search.
Supplemental material
Characteristics of selected studies, study design.
Eight qualitative, 5 23–29 six quantitative papers 30–35 and five mixed methods studies 15 36–39 were included. Qualitative data collection was primarily collected through interviews, 5 23 26 29 39 focus groups 15 24 27 36 38 or a mixture of interviews and focus groups. 24 28
The quantitative studies were observational, with data collected using questionnaires or surveys 15 30 33–35 38 and two reports from one randomised controlled trial. 31 32
Three papers evaluated training delivered to either homecare workers 15 or multidisciplinary teams that included homecare workers. 31 32 These latter two papers reported on the same training evaluation; however, they focused on different aspects of the training and therefore are both included in the review.
Seven of the papers sought to explore the experiences of homecare workers working with clients at the end of life. 5 23–28 30 This included considering their challenges, potential training and support needs as well as reflections on good practice of homecare workers when working with those with life-limiting illnesses. Three studies had built on earlier work to develop training materials for homecare workers. Several papers reported findings from the impact or evaluation of these materials and training programmes. 15 31 32 38 In addition to training, there were other studies that aimed to improve support for homecare workers. One such paper included a symptom assessment solution, which aimed to help staff assess changes in symptoms and any associated decision-making, aiming to increase skills and confidence. 25 This study used focus groups to plan such a programme but was not evaluated. Another study explored the nature and importance of effective communication on the relationships established between non-clinical workers and service users. 39
Included papers came from predominantly ‘Western’ nations and Japan (see online supplemental table 1 ). Five papers were from the UK, 5 15 24 26 29 four from the USA, 25 27 28 36 two from Canada, 23 37 one from Australia, 38 one from Sweden, 30 and five from Japan 31–35 and one from Hong Kong and Australia. 39
Participants
In total, 2510 participants are represented. In those studies which reported data on gender, 91% of participants were women.
1261 research participants were homecare workers and managers, while 1249 were other stakeholders such as nurses, doctors, clients, family carers or other professionals, although the level of data reported means that the percentages of each group are not calculable. Some studies were a mix of homecare workers and health and social care professionals such as District Nurses or Local Authority managers (n=6 24 25 31 32 35 39 ), or gathered data from the homecare agencies more generally (n=2 33 37 ). Two studies included families of those receiving homecare, although recruitment from this group was understandably difficult and limited. 26 38
While the focus of this review was on homecare provision around the end of life, the papers varied in terms of their patient group focus. 12 papers considered end-of-life care for people with a range of conditions. 15 26 28 30–35 37–39 Seven of the papers focused on specific conditions (dementia, n=5 5 23 24 27 29 ; heart failure, n=2 27 36 ), while another focused on symptom management such as shortness of breath or pain in a range of illnesses. 25
The narrative analysis is presented in four themes that are evident across the literature: emotional support; interactions with other practitioners; training and support needs; and recognising good practice.
Emotional support
While the commissioned role undertaken by homecare workers for end-of-life care is usually practical provision of personal hygiene or medication support, much of the described support to people with advanced conditions towards the end of life can be more complex, involving supporting the client and their family with more intangible emotional support:
They [clients, families] don’t know what’s going on, they don’t know what to ask you, they don’t know what to expect of you […] you walk into this environment of … it can be chaotic and other dynamics are … you can sense it as soon as you walk in. There’s a small degree of panic, […] but they are, I have to say overall, very, very, very grateful of anything that you do. (community care worker 8) [38, p275]
There is significant and nuanced emotional labour in supporting a client and their family through this period of life. 24 25 27 28 This is aggravated by the isolating and isolated nature of homecare work leading to staff feeling undersupported and underprepared. Unlike healthcare workers, social homecare workers rarely have explicit and structured support such as an equivalent to clinical supervision. Support is required to reduce the impact of the emotional and cognitive stresses of working so closely with those at end of life, and the associated grief, to reduce the impact of these on staff and to limit stress and burnout. 27–29 Both peer and manager support were suggested as useful resources to help reduce such stresses, but can often be unstructured and not embedded in formal processes:
“It’s quite ad hoc if I am honest. We do not have like a, you know, a person, we do not have like a, what do you call them, a therapist or a counsellor or anything for people to go to. I think any of the office staff here would always listen and lend an ear to the care workers.” (male homecare worker, aged between 25–40). [29 p357].
The widespread impact of the COVID-19 pandemic brought the need for additional support, and key areas of practice which require improvement such as communication skills—both verbal and non-verbal—into sharp focus. 30 However, there was limited detail on what this should look like and how the effects of grief and loss might be mitigated or how such support would be implemented in practice in the context of understaffing and limited financial resources.
Interaction with other practitioners
The changing nature of providing care for clients with progressive, advanced conditions and their families is a particular challenge in the context of end-of-life care. 5 35 Given the complex and changing situation, the wide team of practitioners, family and friends involved in the client’s care, communication between other care providers (both professional and informal) and homecare workers was difficult and aggravated by the lack of systematic communication between them. 34 38 Homecare workers reported a lack of clarity regarding their role:
“The agency doesn’t make clear to anyone who we are or what we do. You know, we’re not just the help!” [27 p4]
The lack of clarity, particularly among the wider healthcare team, left homecare workers feeling poorly understood and valued and led to them being left out of wider support and communications:
‘Because you’re a carer you get pushed to the side and people don’t listen to what you’re saying but when we come to [the hospice] nobody does that, and people can ask the things that they’ve been afraid to ask. And having the professionals the other side has helped to answer some of the questions that we’ve not always been able to get the answer for’. [15 p26]. “We’re with the clients all day, more than anyone else. So why aren’t we included in the conversation?” [38 p5].
An evaluation of an educational booklet used as a basis for focus group discussions aiming to address poor interdisciplinary understanding and working in the wider social and healthcare team notably improved mutual respect and appreciation. 30
In contrast to the isolated homecare worker, community palliative and primary care teams are well established and multidisciplinary in nature. Unqualified healthcare workers practice in an environment which has a comparatively well-established training and support system and often work closely with qualified healthcare professionals. Homecare workers report working with less support and training than their healthcare colleagues. Homecare workers practice outside of the healthcare structure and yet are expected to work with an increasingly complex client group, often outside of ‘normal’ working hours (with little access to advice from other service workers) and alongside the additional support services which accompany this:
“You’re calling and calling. You’re by yourself and no one picks up at the agency. You’re stranded with the client, and you don’t know what to do and you need help. It’s a huge problem.” [38, p5].
Training and support needs
The need for specific training support in the end-of-life context was clearly recognised alongside the current gap in provision for homecare workers. Four papers presented findings from training programme evaluations for homecare workers. 30 31 37 The findings identified that the content and delivery of training for homecare workers, including communication skills training (verbal and non-verbal) requires further work to establish the optimum training content and to evaluate the outcomes in staff learning, confidence and practice. There was an indication that homecare workers would benefit from increased knowledge to help them access support for their client when they deteriorate:
You see a change, but you can't go on the phone and say to the doctor, ‘Well she’s changed,’ because there isn't a word for it […] it’s like a gut feeling for me. [Staff focus group, manager] [24, p5].
Condition-specific literature also highlighted the need for focused training around challenging symptoms associated with dementia or heart failure, 5 35 and the importance of understanding policies and procedures for after a death has occurred for staff confidence:
You need to know that these are the steps that you have to follow, like reporting death policy that you would have in place, so you know what to follow. (female homecare worker, aged between 18 and 24). {5 p1988].
While many examples of good practice were described, the homecare workforce is often underprepared for the complexity of caring for those who are approaching the last months of life, despite being a key service provider in this situation. Some evaluations of training initiatives reflected increased confidence at work although this did not translate to increased job satisfaction; further development and testing of training programmes is needed to evaluate changes in practice and client experience and outcomes. 15 30 31
A suggestion that less experienced staff would benefit most from training reflected an assumption that staff learn skills and confidence ‘on the job’, further emphasising both a gap in current practice and the nature of the knowledge required. 29 While training provision was clearly a positive aspect, barriers to training were found regarding consistent attendance at training sessions, 15 suggesting that while the establishment of a training programme is laudable, the implementation of this must consider the challenges of working with a busy, community-based workforce and the costs of provision and/or access. Condition-specific training was also identified as a need, 22 35 as the presentation and symptoms of different conditions require different management.
Recognising good practice
Examples of good practice included recognition of, and communication that, a client may be approaching the last months of life; something which can be difficult in chronic conditions with which clients have lived for many years. 23 Other good practices included regular scheduled supervision-type processes:
There is good sides, but there is often especially if you look after someone with dementia, there is also a lot of stress. And so, what we have done to help reduce that stress is every month we have one of the directors who has (a faith-based background). This person does reflective supervision with the staff (P25, male homecare manager, aged between 25–40). [29, p 357].
Homecare workers may have provided care for clients with long-term conditions who are now reaching the end-stage of disease, but the homecare worker is unaware of this change. Good communication between homecare and health professionals, clients and their informal carers is a consistently recognised factor in good practice, although, with limited evidence as to how this might be operationalised. A good understanding, and appreciation, of the role of each professional was noted to improve collaboration, with interprofessional communication helping to provide better quality care for clients. 34 The changing nature of end-of-life care was reflected in several of the papers, as conditions, symptoms and function can fluctuate unpredictably, creating stress for the client, their family and the homecare worker. The findings suggest that this is approached with flexibility on the part of the homecare worker, however, having the confidence and skillset to be able to do this is something which requires experience and training. 5
Summary findings
There are significant support and training needs regarding end-of-life care provision in domestic settings such as the need for communication and mutual role clarification and respect within the wider multidisciplinary team, and further training on managing changing function or symptoms, and what to do after a death. Condition-specific literature highlighted the need for more focused training, especially around challenging symptoms and behaviours associated with common diagnoses such as dementia or heart failure. Also indicated is a need for training homecare workers who may require additional support around both verbal and non-verbal communication skills. Finally, increased support is required around the emotional and cognitive stresses of working so closely with those at end of life, and the grief and loss associated with this.
Quality appraisal
The quality appraisal found a generally high level of quality, including in the observational studies where there were robust sampling methods and confounders were addressed in the analysis. Online supplemental table 2 shows the scoring for each of the papers included in the review. The most common omissions were a lack of reporting on bias 24 25 37 38 and limited samples such as from one organisation 15 or homecare workers from a particular union. 26 Other omissions were reporting ethnicity or other demographic information, 23 36 which might have helped indicate the generalisability of the findings.
Homecare workers caring for those at end of life provide care in the context of complex, changing and often emotionally charged situations. They care for clients with advanced and progressing disease, with little to no specific training on managing changing physical function and symptoms, client and family distress, or on verbal and non-verbal communication. Navigating the personal–professional boundaries which may become blurred with a dying client requires skills and good supervision and support which is commonly lacking. Working alongside, but employed outside of, a network of healthcare practitioners and family and friends, means that there is a need for clear and reliable communication within the wider multidisciplinary team. Failure to do so aggravates the emotional burden experienced by homecare workers if; (1) their role is not clear to themselves or others, (2) their role is unappreciated by the extended team and (3) they are unaware of other practitioners’ input, support or clinical care plans relating to deteriorating health. Being faced with unmet need of a client with whom the homecare worker may have developed a strong relationship, homecare workers may ‘self-extend’ their duties beyond their skills, training, responsibilities and capabilities. Homecare workers remain isolated and expected to learn through experience. The need for better training and support is recognised, but there is little information as to the content, the effectiveness or implementation of these important interventions in practice.
Our review highlights the emotional and psychological impact of caring for those approaching the last months of life. It indicated the need for additional support to reduce the impact on staff and limit stress and burnout 27–29 but provided little detail about what this should include, or how it should be provided. The isolating nature of homecare work was seen particularly through the COVID-19 pandemic with calls for additional support. 32 The emotional support needs of homecare workers working within end-of-life care are recognised in the wider literature. 39 40 The distress experienced by care workers likely contribute to the issues around staff retention and staff absence in this service industry. 28 Both healthcare and social care services include workers with no formal qualifications, in addition to registered professions such as nurses or therapists or social workers. In some publications, these unqualified groups are treated as synonymous, 13 but in practice they have different training and support networks. Within the context of end-of-life healthcare, it is recognised that caring for those at end of life requires specialist skills and knowledge. Community palliative care and primary care teams are well established and are multidisciplinary in nature, with each profession having specified training and supervision requirements, and unqualified and qualified healthcare staff often work closely together. By contrast, homecare workers appear to work with less support. 9 10 Of note, a similar experience can also affect healthworkers—particularly the unqualified healthcare assistants—who, although being part of the multidisciplinary healthcare team, in practice work alone. 41 42
In healthcare settings, there is an evidence base regarding staff well-being, for example, in palliative care settings, acknowledging the level of emotional labour in this staff group and increased risk of burnout compared with other settings. 39 42 43 Interventions include meditation, arts-based supervision practice and improving communication skills all with the aim of addressing the emotional support needs of those working in palliative care. 43 Other examples of addressing this element of emotional labour include Acceptance and Commitment Therapy, 43 orientation or induction programmes, access to bereavement advisors, team debriefs and peer support. 44 An emerging literature shows that clinical supervision for healthcare workers in general is associated with better well-being, 45 lower rates of burnout and better staff retention. 46 However, the recognition that supervision is often the first aspect of work to be lost under increased work pressures, such as during the pandemic 46 means that implementing this into the already pressured world of homecare would be challenging.
Our review highlighted the importance of communication with the wider team involved in the care of clients at the end of life. They are present in the home with the client and their families and face difficult conversations and potentially increased risk if they are not fully included in healthcare communications. 47 48 However, not only does the homecare worker need to be informed by the healthcare team of advance care plans and changes in care goals, but they also know their clients well and may be the first to recognise deterioration or a change in need. Effective three-way communication (written and verbal) among the client, carers and healthcare professionals could improve appropriate escalation and avoid unnecessary hospital admissions. 48–51 In addition to recommending increased training in communication for homecare workers, this review indicates that healthcare workers would also benefit from training about social homecare worker roles and skills and the importance of including homecare workers in communications and what a homecare worker’s role entails. A fundamental shift in the respect and appreciation between the whole social and healthcare team would foster better teamworking and homecare worker confidence and support. The shift in the UK to electronic documentation for homecare workers may help support more effective communication if utilised effectively, but further evidence on this is required. 3 There is a current drive in the UK to integrate health and social care services, 52 citing the community multidisciplinary team as a potential mechanism to improve care. 53 However, while social workers may be members of such teams, homecare workers and their managers are not.
We identified a current gap in training and support for homecare workers in respect of end-of-life care. While many examples of good practice were described, the homecare workforce is underprepared for the complexity of caring for those who are approaching the last months of life, despite being one of the central professions involved. The training initiative evaluations included in our review showed an increase in confidence in their work but not in job satisfaction indicating the need for further development and testing to show changes in practice. 30 The suggestion that less experienced staff would benefit from training reflected the tendency for staff to learn skills and confidence ‘on the job,’ highlighting both a gap in current practice and the nature of the knowledge required. 29 The assumption that less educated workers need little formal training and that ‘on the job’ experience over time is sufficient, is a pervasive problem recognised across many fields of employment, and a persistent training gap lies with a lack of supply of training by the employer rather than a low demand by employees. 54
While training provision was seen as positive, barriers to training were highlighted particularly in terms of ability to attend. 15 The implementation of a training programme must take the challenges of working with a busy, time-poor community-based workforce into account. We found some evidence of good practice but there does not appear to be a national or international standards for homecare at the end of life. A rapid scoping review of systematic reviews, focussing on service delivery models to maximise quality of life for older people at end of life, found limited reference to social care. 55 A King’s Fund report on homecare in England made no reference to palliative or end-of-life care, 56 similarly for the 2020 Skills for Care annual review of adult social care. 57 Further, in England, the Government policy vision for adult social care makes minimal reference to the need for/provision of support at end of life. 58
Strengths and limitations of the review
A rapid review method inevitably limits depth and rigour compared with a systematic review. For example, no grey literature or non-English publications were included which may have yielded further insights into the needs and experiences of homecare workers. However, we followed standard guidance for rapid reviews. 19 The inclusion and exclusion criteria and search terms were agreed a priori and the data extraction was carried out systematically and in discussion with the research team. However, we acknowledge that there are a number of terms used to describe social homecare workers, some of which are hard to distinguish from healthcare; therefore, we may have excluded some relevant papers. A formal quality appraisal of the papers was carried out using objective and transparent processes, 21 showing the papers to be of good quality, enabling us to have confidence in the findings.
Compared with Herber and Johnston, 13 we found significantly more published literature about social homecare workers (a further 19 papers, vs 1). This indicates a growing interest in this issue, but still highlights a lack of work evaluating solutions to the challenges; most were qualitative or observational in nature. We were able to confirm previous findings including applicable findings from the healthcare assistant population. 13 We gained new and deeper understanding particularly regarding the isolation from the wider multidisciplinary team involved in the care of the dying person, lack of role clarity, lack role respect and understanding by the wider team and potential benefits from educational and team-working interventions. However, despite the increased literature, there were no studies from countries other than ‘Western’ nations or Japan. The focused nature of our review question means that other models of homecare provision, for example, the community volunteer service in Kerala, India, 59 is out of scope.
Implications for policy, practice and research
Social care needs of older adults are expected to double in England by 2040 and those requiring 24-hour care will rise by over a third by 2035. 60 Homecare services, provided mainly by private agencies, are increasing in the UK, although with considerable turnover, with the adult social care workforce making up 5.3% of the English workforce (1.47 million employees). 4 57 A large excess in home deaths was seen throughout the COVID-19 pandemic. 61 District nurses and homecare workers provide the backbone of homecare. The lack of integration and strain on both services leaves end-of-life care at risk in face of a projected 42% increase in demand by 2040. 62 This provides context to a wider need to consider structural factors such as the socioeconomic position of homecare workers, the recognised need for the increased professionalisation of this sector and the value of care labour more generally. 9
Our findings are widely applicable in a ‘Western’ context and highlight several key areas for consideration for future policy, research and practice including training and support needs, emotional support and recognising good practice. 18
An understanding of homecare workers’ education and support needs and how they integrate with the wider healthcare workforce is vital for the White Paper call for integrated care systems. 56 In addition, a Health Foundation briefing document 63 described how ‘social care issues are under the radar and underappreciated. The longstanding political neglect of social care in England has been laid bare for all to see. Continued neglect would leave the system vulnerable to future shocks’. Despite social care reform being a stated UK top priority with the COVID-19 pandemic pushing it ‘up the political agenda and on to the front pages’, 64 to date, successive governments have failed to materially address these failings in policy change supported with necessary funding.
Caring for those approaching the end of life in a home environment requires practices which cannot only improve the quality of care for the client but also the experience of those caring for them—both paid and unpaid. Notable features of good practice include a recognition and communication that a client may be approaching the last months of life, something which can be difficult to establish with confidence in chronic conditions which clients have lived with for many years. 23 Good communication between care and health professionals, and with the client and their unpaid carers, is a consistent factor in good practice, although, there is limited evidence as to how this might be operationalised, demonstrating that flexibility is something which requires experience and training. 5
Training needs are identified across a range of topics such as communication skills, multidisciplinary working, symptom management and managing the emotional labour involved in caring in this context. However, further evidence is required to inform the content and nature of this training to make it effective and accessible. This review indicates that the role of the homecare worker providing care to those approaching the end of life is one which requires flexibility and effective communication. In practice this means that both homecare workers and their colleagues in the wider multidisciplinary team should be aware of the need for good communication by discussing changes in care needs, function or advanced care planning. Those responsible for supporting homecare workers should be aware of the complexity of caring in this context and provide both practical and emotional support within the limits of the existing evidence.
With regard to future research, a knowledge of the overall priorities within the sector, and careful consideration of the effectiveness, delivery and implementation of training or other interventions are priorities. Training within work time or paid attendance needs to be considered otherwise the uptake will be limited especially as there is no current career progression attached to such training. A better understanding is required of what would make future training relevant and accessible to improve uptake, including a focus on content (such as communication skills, legal aspects of end of life, managing emotions and accessing support, working with the wider team) and the optimal forms of delivery (such as face to face or online). Training resources built on examples of good practice, codesigned with homecare workers and informed by their stated needs, are required. Training for those working alongside homecare workers, such as community palliative care teams, should include content about the role of homecare workers to promote good quality interprofessional communication across health and social care boundaries. Lastly, we found no studies regarding paid homecare support at the end of life in low-middle-income countries and non-‘Westernised’ cultures. This is important as the ageing population in many Asian countries, and changing culture with more women in paid employment, will lead to challenging practical implications on the provision of homecare by family at the end-of-life. 65
Homecare workers provide essential care to enable end-of-life care at home, but need further training and support, and recognition by and inclusion with the wider healthcare team. While some training has been developed, there is little evidence of widespread adoption of end-of-life training and effectiveness, and implementation evidence is scant. Our findings are important reading for policy-makers attempting to address this current and crucial challenge, and service providers in both social and healthcare.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- Calanzani N ,
- Gysels M , et al
- Higginson IJ ,
- Sarmento VP ,
- Calanzani N , et al
- Konlan KD ,
- Care Quality Commission (CQC)
- Vandrevala T ,
- Samsi K , et al
- Miyawaki A ,
- Kobayashi Y , et al
- Department of Health
- Timonen V ,
- Donnellan WJ ,
- Clarke K , et al
- Cannings-John R ,
- Schoenbuchner S ,
- Jones H , et al
- Turnpenny A ,
- Herber OR ,
- Johnston BM
- Franzosa E , et al
- Ghasemi L ,
- Westerdale E , et al
- Moriarty J ,
- Manthorpe J ,
- Khangura S ,
- Cushman R , et al
- Garritty C ,
- Gartlehner G ,
- Nussbaumer-Streit B , et al
- McKenzie JE ,
- Bossuyt PM , et al
- Kerr C , et al
- Centre for reviews and dissemination
- Savundranayagam MY ,
- Orange JB , et al
- Bamford C ,
- Poole M , et al
- Odierna DH ,
- Feuz MA , et al
- Percival J ,
- Lasseter G ,
- Purdy S , et al
- Sterling MR ,
- Leung PB , et al
- Wladkowski SP ,
- Kusmaul N ,
- Vandrevala T , et al
- Craftman ÅG ,
- Pakpour AH ,
- Calderon H , et al
- Ikezaki S , et al
- Igarashi A ,
- Kurinobu T ,
- Ko A , et al
- Watanabe M ,
- Yamamoto-Mitani N ,
- Nishigaki M , et al
- Noguchi-Watanabe M , et al
- Sterling MR , et al
- McPherson CJ ,
- Ta VC-Y , et al
- Poulos RG ,
- Poulos CJ , et al
- Turnbull M ,
- Brighton LJ ,
- Selman LE ,
- Bristowe K , et al
- Patynowska KA ,
- McConnell T ,
- McAtamney C , et al
- Dijxhoorn A-FQ ,
- van der Linden YM , et al
- Medisauskaite A ,
- Carton ER ,
- Saarinen PI ,
- Lizarondo L ,
- Kumar S , et al
- McIlfatrick S
- Silverglow A ,
- Johansson L ,
- Lidén E , et al
- Wilson DM ,
- Maetens A ,
- Beernaert K ,
- De Schreye R , et al
- Department of Health and Social Care
- Wolters A , et al
- Ellis-Smith C , et al
- The King’s Fund
- Price R , et al
- Philip RR ,
- Tripathy JP , et al
- Kingston A ,
- Comas-Herrera A ,
- Jagger C , et al
- Etkind SN ,
- Gomes B , et al
- Alarilla A , et al
- Majmundar M , National Research Council
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
X @Zaunders_OU, @carolinannwhite, @MJJohnson_HYMS
Correction notice This article has been corrected since it was published online. There is an error in referencing in this review by the first author of reference 42 (Patynowska et al) in the discussion. Her paper has been attributed to the incorrect sentence. The correct reading should be as follows: "Of note, a similar experience can also affect healthworkers – particularly the unqualified healthcare assistants – who, although being part of the multi-disciplinary healthcare team, in practice work alone.[41, 42] In healthcare settings, there is an evidence base regarding staff wellbeing, for example, in palliative care settings, acknowledging the level of emotional labour in this staff group and increased risk of burnout compared with other settings.[39, 42, 43] Interventions include meditation, arts-based supervision practice and improving communication skills all with the aim of addressing the emotional support needs of those working in palliative care.[43]"
Contributors Concept and design: MJJ, CF and LW. Search: CF and HE-B. Screening and data extraction: CF, ZB, JK, KM and MJJ. Preliminary analysis: CF and MJJ. Quality appraisal: CF, ZB and MJJ. First draft manuscript: CF. Manuscript revisions: all authors. Approval of final manuscript: all authors. Guarantor: MJJ.
Funding This study/project is funded by the NIHR HSDR Programme (project reference NIHR135128). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Open access
- Published: 26 June 2024
Climate change and heat stress resilient outdoor workers: findings from systematic literature review
- Peymaneh Habibi 1 ,
- Jaleh Razmjouei 2 ,
- Amirhossein Moradi 3 ,
- Farank Mahdavi 1 ,
- Saeed Fallah-Aliabadi 4 , 5 &
- Ahad Heydari 6
BMC Public Health volume 24 , Article number: 1711 ( 2024 ) Cite this article
74 Accesses
1 Altmetric
Metrics details
Global warming has led to an increase in the number and intensity of extreme heat events, posing a significant threat to the health and safety of workers, especially those working outdoors, as they often have limited access to cooling strategies. The present systematic literature review (a) summarizes the current knowledge on the impacts of climate change on outdoor workers, (b) provides historical background on this issue, (c) explores factors that reduce and increase thermal stress resilience, (d) discusses the heat mitigation strategies, and (e) provides an overview of existing policy and legal frameworks on occupational heat exposure among outdoor workers.
Materials and methods
In this systematic review, we searched scientific databases including Scopus ( N = 855), Web of Science ( N = 828), and PubMed ( N = 202). Additionally, we identified relevant studies on climate change and heat-stress control measures through Google Scholar ( N = 116) using specific search terms. In total, we monitored 2001 articles pertaining to worker populations (men = 2921; women = 627) in various outdoor climate conditions across 14 countries. After full-text assessment, 55 studies were selected for inclusion, and finally, 29 eligible papers were included for data extraction.
Failure to implement effective control strategies for outdoor workers will result in decreased resilience to thermal stress. The findings underscore a lack of awareness regarding certain adaptation strategies and interventions aimed at preventing and enhancing resilience to the impact of climate change on heat stress prevalence among workers in outdoor tropical and subtropical environments. However, attractive alternative solutions from the aspects of economic and ecological sustainability in the overall assessment of heat stress resilience can be referred to acclimatization, shading, optimized clothing properties and planned breaks.
The integration of climate change adaptation strategies into occupational health programs can enhance occupational heat resilience among outdoor workers. Conducting cost-benefit evaluations of health and safety measures for thermal stress adaptation strategies among outdoor workers is crucial for professionals and policymakers in low- and middle-income tropical and subtropical countries. In this respect, complementary measures targeting hydration, work-rest regimes, ventilated garments, self-pacing, and mechanization can be adopted to protect outdoor workers. Risk management strategies, adaptive measures, heat risk awareness, practical interventions, training programs, and protective policies should be implemented in hot-dry and hot-humid climates to boost the tolerance and resilience of outdoor workers.
Peer Review reports
Introduction
Extreme weather events and severe heat pose significant hazards to the safety and health of workers, leading to increased accidents, mortality, and morbidity during hot climate conditions [ 1 , 2 , 3 ]. Global warming presents a new and formidable challenge for most countries [ 4 , 5 ]. Global climate change substantially affects physiological and perceptual responses through both direct and indirect effects on core body temperature [ 6 ], heart rate, skin temperature, and thermal comfort [ 7 , 8 , 9 ]. Working in hot and humid environments during long shifts with high physical activity can jeopardize the safety and health of worker populations [ 7 , 10 ]. Increased exposure to thermal stress among workers in outdoor environments has been documented in tropical and subtropical countries with hot seasons [ 11 ]. Exposure to hot working environments, and the resulting elevated physiological and perceptual responses, can lead to occupational heat stress, reducing safety, health, and work capacity [ 12 ], and increasing the risk of heat-related illnesses (HRI) [ 13 ]. The increment in the levels of ambient temperature, radiation and shifts in the distribution of daily peak temperature can cause indirect and direct effects on outdoor workers [ 14 , 15 ]. High temperatures and high humidity can exacerbate the effects of physical workload on individuals working outdoors during long shifts in developing and tropical countries [ 16 ]. Working in high-temperature and high-humidity environments can have adverse health effects on workers, particularly agricultural workers, construction workers, drivers, sellers, brick-making workers, and daily wage workers [ 17 , 18 ]. High hot-humid and hot-dry temperatures can lead to occupational heat strain when core body temperature rises above 38 °C [ 19 ]. Exposure to heat radiation, either when working outdoors with exposure to the sun or around hot machinery, can greatly increase physiological pressure and lead to reduced work capacity [ 20 ].These physiological mechanisms worsen under high climate conditions and climate change, emphasizing the need to identify strategies to increase occupational heat stress resilience and develop solutions and policies to protect the health and safety of outdoor workers [ 21 , 22 ]. Projected future global warming conditions will dangerously affect the anticipated occupational heat stress resilience of outdoor workers worldwide. There is insufficient knowledge regarding strategies to increase occupational heat stress resilience, necessitating protective measures against heat stress and climate change to reduce health risks and fatalities for future outdoor workers in hot and humid work environments. The findings of this study can inform planning for increasing occupational heat stress resilience, developing heat acclimation strategies, and identifying risk factors to mitigate heat stress caused by global warming, particularly in middle- and low-income communities.
Search strategy
This systematic literature review was conducted following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [ 23 ]. We searched scientific databases, including PubMed, Scopus, and Web of Science, and identified additional records through Google Scholar. We used Mesh terms in PubMed to identify synonyms for ‘climate change’ and ‘thermal resistance.’ We also consulted specialists to identify relevant keywords. Our search syntax was developed and applied to title, abstract, or keyword queries in selected databases. To ensure the specificity and accuracy of our search strategy, we tested the number needed to read (NNR) in the Web of Science database. We also investigated the references of included studies and searched key journals via Scopus to identify potentially relevant articles. The full search strategy in three main databases has been mentioned in Appendix 1. Our search syntax was as follows:
PubMed: (“heat wave”[tiab] OR “heat stress”[tiab] OR “climate change*”[tiab] OR (climate[tiab] AND change[tiab]) OR “extreme weather”[tiab] OR “extreme heat”[tiab] OR “global warming”[tiab] OR “hot day*”[tiab] OR “warm day*”[tiab]) AND (“heat tolerance“[tiab] OR “heat resilien*“[tiab] OR (heat[tiab] AND resilien*[tiab]) OR (heat[tiab] AND tolera*[tiab]) OR “Heat resistan*”[tiab] OR thermotolerance[tiab] OR “heat endurance”[tiab] OR (heat[tiab] AND endur*[tiab])) AND (worker*[tiab] OR Firefighter*[tiab] OR “fire fighter*”[tiab] OR firem*[tiab] OR “fire m*”[tiab] OR nurs*[tiab] OR operator*[tiab] OR driver*[tiab] OR farmer[tiab]* OR welder*[tiab] OR miner*[tiab] OR employee[tiab] OR laborer*[tiab] OR labour*[tiab]).
Inclusion criteria
The research question components (PECO) were as follows: P (workers), E (Exposure), C (heat stress), and O (increase occupational heat stress resilience). We included studies that (a) measured physiological and perceptual responses in workplaces and resting environments of workers; (b) studied working populations, including both males and females (healthy and unhealthy populations); (c) assessed the impact of climate change on occupational heat strain, as well as the health, safety, and well-being of workers including work-related variables (income, work type, time), environmental variables (wet-bulb globe temperature (WBGT), relative humidity), physiological variables (heart rate, respiratory, rate of perceived exertion (RPE)), and demographic variables (age, sex, body mass index (kg/m 2 ); (d) focused on air temperature, relative humidity (RH), heat waves, solar radiation, climate change, UV radiation, and thermal stress; (e) considered local and international contexts, countries, and workplaces; and (f) investigated workers’ perceptions of climate change, occupational heat strain, and their knowledge and attitudes toward adaptation strategies.
Exclusion criteria
Studies were excluded if they (a) studied climate change-related phenomena such as storms, cyclones, rainfall, rising sea levels, and drought; (b) evaluated the impact of climate change on plants, crop yields, pest dynamics, soil processes, water availability, and animals; (c) had inaccessible full-texts; or (d) focused on indoor workplaces.
Screening and selection
We entered all identified studies into EndNote and removed duplicates. One team member (PH) screened studies based on their titles and abstracts, and two members of the research team (AH and PH) independently selected relevant studies by reviewing the full texts. Disagreements regarding study inclusion were resolved through team discussion. We also conducted searches in three key journals: environmental research, urban climate, and global environmental change, but did not identify any additional studies.
Data extraction and quality assessment
Two team members (AH and PH) independently assessed the eligibility of included studies based on our inclusion and exclusion criteria. They also evaluated the methodological quality of selected studies using the quality assessment tool for studies with diverse designs (QATSDD), which consists of 16 items and is a reliable and valid tool for assessing the methodological quality of various types of studies [ 24 ]. Any disagreements regarding study inclusion were resolved through team discussion.
Search results
The numbers of identified studies and the studies reviewed during the screening and selection stages are presented in Fig. 1 . The initial search yielded 2001 articles including the additional articles sourced from Scholar Google. After full-text assessment, 55 studies were selected for inclusion, and finally, 29 eligible papers were included for data extraction. No additional studies meeting our eligibility criteria were identified after the full-text investigation. Similarly, no studies were identified through searches of key journals and the references of included studies. Table 1 provides details on the selected studies, including author/year, study location, document type, population/sample size, climate conditions, assessment of physical, perceptual, and physiological factors, authors’ conclusions, and quality ratings. Table 2 presents suggestions for increasing and decreasing occupational heat stress resilience among outdoor workers.

Flow diagram of the screening process of included studies the strategies to increase occupational heat stress resilience among outdoor workers
Descriptive analysis
Out of the 29 selected studies, 18 addressed global warming’s impact on occupational heat stress resilience, risk management strategies, and adaptation strategies for warming conditions. Most of these studies emphasized that climate change will exacerbate the health impacts of extreme heat. The prevalence of negative effects due to climate change will intensify workers’ health risks in future work scenarios, particularly in regions with hot and humid climates and poor economic conditions. As of our selection period until 2023, 20 studies (68.96%) were published between 2016 and 2023. Of the 29 assessed papers, 18 (62.06%) directly investigated the effects of climate change and adaptation strategies for outdoor workers in various countries, including Australia, the USA, China, Japan, Africa, Korea, Slovenia, Taiwan, Indonesia, Ghana, Korea, India, Iran, and Pakistan. The predominant themes identified in these papers revolved around strategies to increase occupational heat stress resilience. In conclusion, the study’s findings were categorized into main themes, including risk factors that decrease occupational heat stress resilience and suggestions for increasing occupational heat stress resilience among outdoor workers.
Thematic content analysis
This systematic review provides a summary of evidence published to date regarding strategies to enhance occupational heat stress resilience, especially in hot outdoor workplaces. Despite variations in study design and analytical approaches, the evidence presented in this systematic review consistently highlights a strong association between thermal stress resulting from global warming and occupational heat stress. Broad findings from these studies indicate that exposure to heatwaves and global warming is linked to adverse health impacts on workers.
Furthermore, several studies underscore the need for sentinel effects and leading indicators to facilitate surveillance of climate-related occupational heat stress effects, as well as strategies and interventions for preventing the impact of climate change on outdoor workers. Finally, the review identifies interventions and adaptation strategies for outdoor workers, including the provision of accessible cool drinking water [ 13 , 26 , 41 , 44 , 47 ], optimized work-rest schedules [ 12 , 13 , 16 , 26 , 36 , 43 , 44 , 47 ], the availability of proper resting shade [ 16 , 47 , 49 ], training and awareness programs [ 20 , 38 , 40 ], self-paced work [ 13 , 38 , 40 , 44 , 47 ], and the use of supportive protective equipment [ 41 ].
Factors that reduce resilience to climate change among outdoor workers
Resilience to climate change among outdoor workers can be reduced by various factors, categorized into personal risk factors, environmental risk factors, and occupational-related heat exposure risk factors during work.
Individual-related heat exposure risk factors
Personal factors associated with reduced resilience to climate change, identifiable from outdoor workers’ data, include dehydration [ 20 , 25 , 28 , 32 , 34 , 37 , 40 , 46 , 47 , 48 ], unique medical characteristics [ 41 , 47 ], pregnancy [ 38 , 40 , 47 ], BMI [ 29 , 30 , 37 , 40 , 47 , 49 ], obesity and body fat [ 29 , 30 , 32 , 34 , 47 ], overall health status [ 33 , 34 , 37 , 47 ], lack of sleep [ 33 , 34 , 40 , 47 ], experience of a previous HRI [ 32 , 34 , 44 , 45 , 46 , 47 ], presence of certain concurrent diseases and chronic disease [ 35 , 47 ], kidney disease [ 20 , 26 , 38 , 43 , 46 , 47 ], consumption of caffeine and alcohol [ 26 , 28 , 30 , 34 , 37 , 40 , 41 , 46 , 47 ], smoking [ 30 ], use of drugs [ 26 , 37 , 40 , 41 , 47 ], age [ 16 , 33 , 35 , 38 , 39 , 40 , 41 , 46 , 47 ], older workers with low education [ 38 , 40 , 43 , 44 , 46 , 47 ], physical fitness [ 26 , 32 , 40 , 47 ], metabolism rate [ 40 , 47 ], type of clothing [ 40 , 47 ], prior heat injury [ 40 , 46 , 47 ], physical activity and heavy workload [ 16 , 27 , 31 , 34 , 38 , 39 , 40 , 46 , 47 , 48 ], gender [ 16 , 33 , 35 , 38 , 39 , 40 , 41 , 46 , 47 ], education level [ 16 , 39 , 41 , 44 , 46 , 47 ], wearing PPE [ 16 , 26 , 27 , 31 , 38 , 39 , 44 , 46 , 47 ], and non-acclimatization [ 29 , 32 , 37 , 40 , 41 , 43 , 44 , 47 ]. Physiological risk factors most frequently expressed by outdoor workers included excessive heart rate [ 30 , 45 , 47 , 49 ], oral [ 47 , 49 ], skin [ 45 , 46 , 47 , 49 ], core temperature [ 26 , 27 , 29 , 31 , 32 , 34 , 45 , 46 , 47 , 48 , 49 ], sweating [ 39 , 47 ], and blood pressure [ 45 , 46 , 47 , 49 ]. This is often followed by heat exhaustion [ 47 , 48 ] or tiredness [ 47 ], headaches [ 47 ], heat rash [ 47 ], and fainting [ 47 ]. Older adults are more vulnerable to chronic dehydration [ 28 , 45 ], especially those living with multiple chronic diseases [ 43 , 47 ]. Aging is also associated with reductions in sweat production [ 8 ]. Consequently, studies have generally reported greater elevations in body heat storage and core temperature in older compared to younger adults during environmental heat exposure [ 26 , 37 , 46 , 47 ]. Additionally, personal factors correlated with occupational heat strain include the adequacy of water intake [ 41 , 47 ].
Environmental-related heat exposure risk factors
The environmental factors contributing to thermal stress include high air temperature [ 12 , 16 , 26 , 27 , 31 , 34 , 40 , 45 , 46 , 47 , 48 , 49 ], heat wave [ 43 , 47 , 48 ], airspeed and movement around the workplace [ 16 , 43 , 45 , 47 , 48 , 49 ], high levels of heat exposure (WBGT = 37.5–49 ℃) [ 38 , 46 , 47 ], tropical nights [ 48 ], working in sun- exposed conditions [ 16 , 38 , 39 , 47 ], solar radiation [ 26 , 40 , 43 , 46 , 47 , 48 ], high humidity [ 16 , 27 , 31 , 34 , 40 , 43 , 45 , 47 , 48 , 49 ], UV radiation [ 26 , 47 , 48 , 49 ], the moisture content of the outdoor settings or workplaces [ 16 , 39 ], radiant heat [ 16 , 26 , 31 , 36 , 45 , 47 , 48 ], and the air-pollution index [ 30 ].
Occupational-related heat exposure risk factors
However, workers encounter various barriers, such as inadequate cool housing designs for rest [ 38 ], a lack of management and engineering commitment [ 41 , 42 , 47 ], heavy physical workloads for long hours [ 16 , 47 ] or physically demanding jobs [ 44 , 46 ], insufficient awareness and prevention training [ 38 , 40 , 41 , 43 , 47 ], a lack of knowledge regarding adaptive behavior [ 41 , 43 ], the absence of occupational heat stress guidelines and adaptation strategies [ 38 , 41 , 46 , 47 ], a lack of regular training on adaptation measures [ 41 ], limited management commitment [ 41 ], the nature of the physical workload [ 16 , 40 , 41 , 46 , 47 ], the absence of specific thermal stress-related policy regulations [ 41 ], working in proximity to heat sources [ 16 , 44 , 47 ], the type of protective clothing [ 16 , 40 , 47 ], limited access to innovative technology and equipment [ 41 ], the nature of the work [ 40 , 41 , 46 , 47 ], inadequate management commitment, work-break regimes [ 43 , 47 ] and cooling systems [ 26 , 28 , 40 , 41 , 47 , 48 ]. Additionally, workers face challenges such as inadequate knowledge of adaptive behavior [ 41 , 46 ], a lack of regular training on thermal stress risk, adaptation, and safety measures [ 41 , 47 ], a deficiency in specific heat-related policies and regulations [ 41 ], limited management commitment to heat-related health and safety measures [ 41 ], restricted access to innovative equipment and technology [ 41 ], insufficient regular breaks and work-rest time [ 35 , 39 , 41 , 46 , 47 ], limited access to shade [ 38 , 43 , 47 ], inadequate financial resources [ 38 , 41 ], the absence of an acclimatization program [ 41 , 43 , 47 ], suboptimal water management [ 47 ], and insufficient medical attention when implementing adaptation strategies for climate change and occupational heat stress.
Factors that enhance resilience to climate change among outdoor workers
Enhanced resilience to climate change can be achieved through various means, including personal, managerial, and engineering protective factors.
Personal protective factors
Outdoor workers can take several measures to protect themselves. They should consider adjusting their work schedule [ 35 , 47 ], maintaining adequate hydration [ 28 , 33 , 35 , 37 , 38 , 39 , 40 , 47 ], adjusting their clothing [ 31 , 35 , 47 ], drinking more water [ 35 ] or drinking plenty of cool water frequently before feeling thirsty [ 13 , 26 , 41 , 44 , 47 ]. It’s important to take more frequent planned breaks [ 35 , 38 , 44 ], wear broad-brimmed hats [ 35 , 39 , 41 , 47 ] and ventilated helmets [ 28 ], understand how to self-pace [ 13 , 38 , 40 , 44 , 47 ], wear sun-protective gear [ 38 , 49 ], including sunglasses and gloves during hot weather conditions [ 41 ], and take work breaks and rest in cooler or shaded areas [ 13 , 28 , 33 , 35 , 38 , 39 , 40 , 41 , 43 , 44 , 47 ]. Using sunblock [ 38 , 39 , 44 ], and having a higher education level [ 39 , 44 , 47 ], are also beneficial. Workers should consider wearing loose and light-colored clothing [ 28 , 34 , 35 , 38 , 39 , 41 , 44 ] and opting for short-sleeved shirts and shorts when possible [ 13 ]. Using cooling vests [ 27 , 47 ], implementing a ‘Buddy system’ [ 47 ], acclimatization [ 26 , 29 , 30 , 31 , 32 , 33 , 34 , 36 , 37 , 40 , 47 ], maintaining normal anthropometric measures [ 29 ], and changing clothing ensembles to more breathable single-layer garments [ 43 ] can further enhance personal protection.
Managerial protective factors
Maintaining good quality working conditions and a suitable climate can significantly improve worker performance, productivity, and company profits [ 37 ]. Workplace management and training programs [ 16 , 35 , 38 , 40 , 41 , 47 , 49 ] are crucial for worker well-being. Developing prevention strategies [ 12 , 13 , 38 , 48 ], improving guidelines for worker safety, health, and productivity, and adhering to occupational health standards [ 12 , 38 , 47 ] are essential. Scheduling heavy routine outdoor work during the early morning [ 47 ] or evening hours or in shaded areas [ 13 , 41 , 44 , 49 ] can help mitigate heat stress. Providing access to cooling systems, such as air conditioning and fans [ 13 , 16 , 26 , 38 , 39 , 40 , 41 , 44 , 47 ], and offering climate change adaptation strategies [ 13 , 48 , 49 ] are beneficial. Adjusting the duration of breaks/rest periods [ 12 , 13 , 16 , 26 , 36 , 43 , 44 , 47 ], ensuring access to shade [ 16 , 47 , 49 ], and providing access to drinking water or implementing programs to improve hydration status [ 13 , 16 , 20 , 25 , 44 , 47 , 49 ] are important managerial measures. Training workers in heat-related illness prevention [ 20 , 38 , 40 ], providing access to medical attention [ 20 ], sharing heavier jobs and rotating job assignments on shift schedules [ 13 , 41 , 47 , 49 ], offering air-conditioned vehicles [ 13 , 38 , 47 ], promoting climate change awareness to support healthy lives and decent jobs [ 39 ], implementing work stoppages if the daily maximum temperature exceeds 40 °C [ 13 , 44 , 47 ], raising worker awareness about heat risks [ 47 ] modifying work habits [ 49 ], considering the TWL [ 30 ], and promoting the understanding of the need for workers to self-pace during hot weather [ 13 , 38 , 47 ] are all valuable managerial protective factors.
Engineering protective factors
Providing and designing regular breaks in shaded areas [ 38 , 47 ], implementing strategies to eliminate or replace thermal stress risks [ 37 , 44 ], installing a central cooling system [ 13 , 44 , 47 ], halting work during periods of high thermal stress and supplying mechanical equipment [ 41 , 47 ], initiating heat-shield projects [ 47 ], and enhancing ventilation [ 38 , 39 , 44 , 47 ].
Our systematic review’s outcomes help us understand strategies for increasing occupational heat stress resilience and assessing the effects of global warming on outdoor workers’ adaptation strategies. This is particularly crucial in numerous warm workplaces, especially in low- and middle-income countries. The implementation of strategies to ensure adequate hydration, including access to drinking water and programs to improve hydration status [ 13 , 16 , 20 , 25 , 44 , 47 , 49 ], is one of the most critical interventions for managing warm workplaces. Hydrated workers [ 28 , 33 , 35 , 37 , 38 , 39 , 40 , 47 ] are more likely to maintain an acceptable work rate and physical activity without health risks in various hot-dry and hot-humid weather conditions [ 25 ]. Employers bear the responsibility of providing a safe work environment, conducting training and awareness programs [ 16 , 35 , 38 , 40 , 41 , 47 , 49 ], supervision [ 50 ], and providing suitable protective equipment to mitigate the negative effects of thermal stress due to global warming on safety and health [ 26 , 49 ]. Cooling the core body temperature through wearable liquid cooling garments (SCG) [ 27 ], evaporative cooling garments (ECGs) [ 15 ], fluid cooling garments (FCGs) [ 51 ], hybrid cooling (HBCGs) [ 52 ], and phase change materials (PCMs) [ 53 ] worn by individuals who require personal protective equipment [ 47 , 54 ], including firefighters and construction workers, significantly reduces occupational heat strain and enhances thermal comfort and performance [ 32 ]. Chan et al. recommend implementing appropriate protective measures, such as work-rest schedules and heat tolerance guidelines, to ensure the safety and health of personnel exposed to hot weather conditions [ 28 ]. Therefore, it’s advisable to conduct further research on work-rest schedule optimization models for workers, particularly in the context of construction workers [ 28 ]. It is recommended that safe work durations should be modified based on expected type of clothing and work intensity [ 55 ]. Our review’s results indicate that personal risk factors such as dehydration [ 20 , 25 , 28 , 32 , 34 , 37 , 40 , 46 , 47 , 48 ], smoking [ 30 ] and alcohol-drinking habits [ 26 , 28 , 30 , 34 , 37 , 40 , 41 , 46 , 47 ], age [ 16 , 33 , 35 , 38 , 39 , 40 , 41 , 46 , 47 ], BMI [ 29 , 30 , 37 , 40 , 47 , 49 ], and non-acclimatization [ 29 , 32 , 37 , 40 , 41 , 43 , 44 , 47 ]; as well as work-related factors like work-rest cycles [ 35 , 39 , 41 , 46 , 47 ] and environmental risk factors such as air temperature [ 12 , 16 , 26 , 27 , 31 , 34 , 40 , 45 , 46 , 47 , 48 , 49 ], relative humidity (RH) [ 16 , 27 , 31 , 34 , 40 , 43 , 45 , 47 , 48 , 49 ], heat radiant [ 16 , 26 , 31 , 36 , 45 , 47 , 48 ], and Thermal Work Limit (TWL) [ 30 ], are significant predictors for determining the physiological responses to HRI among outdoor workers [ 30 ]. More efforts should be made to educate workers and employers about the effects of occupational heat stress on safety, health and performance, and appropriate screening protocols (pre-employment and periodic examinations) should be included in health and safety legislation [ 56 ].
Educating outdoor workers about physiological and perceptual responses to HRI [ 20 , 38 , 40 ] and heat acclimation under uncompensated thermal stress [ 26 , 29 , 30 , 31 , 32 , 33 , 34 , 36 , 37 , 40 , 47 ], as well as emphasizing cooling techniques and fluid intake [ 28 , 33 , 35 , 37 , 38 , 39 , 40 , 47 ], is essential. Furthermore, it’s necessary to investigate the impact of gender (both women and men) [ 16 , 33 , 35 , 38 , 39 , 40 , 41 , 46 , 47 ] and aging on heat tolerance and psychophysiological adaptation during work in hot-dry and hot-humid environmental conditions. This is especially crucial since elderly workers [ 38 , 40 , 43 , 44 , 46 , 47 ] display increased susceptibility to HRI in future studies, even if they haven’t engaged in prolonged or strenuous physical labor [ 31 ]. Pogačar et al.‘s study revealed that the most common symptoms of heat stress include excessive sweating, thirst, and fatigue. Interestingly, there was a significant difference among age groups regarding thirst and excessive sweating [ 35 ]. Gender differences in temperature regulation become more apparent under varying heat loads [ 8 ]. In general, women lose more heat through convection [ 11 ], which is advantageous in hot-humid environments [ 57 ], while men lose more heat through evaporation, which is more pronounced in hot-dry environments [ 58 ]. The resilience of vulnerable worker groups to heat stress can be compromised despite existing standards and knowledge. This vulnerability is particularly relevant when considering outdoor workers exposed to different climate conditions in tropical and subtropical countries [ 12 , 38 , 47 ]. Kjellstrom et al.‘s study underscores that mine workers remain the most significant population in terms of preventing the impact of thermal stress. This also extends to many construction workers, agricultural workers, and individuals laboring in warm workplaces without effective cooling systems [ 20 ]. Lui et al. demonstrated that wildland firefighters experience heat acclimatization across the thermal stress and fire season, leading to significant decreases in physiological and perceptual responses. These adaptations can reduce the risk of HRI [ 32 ]. Implementing acclimatization [ 26 , 29 , 30 , 31 , 32 , 33 , 34 , 36 , 37 , 40 , 47 ] and adaptation programms [ 13 , 48 , 49 ] for workers exposed to thermal stress is crucial. Adaptation policies aim to increase climate change resilience and reduce climate vulnerability [ 48 ]. Managers and occupational health professionals should also assess workers’ health status and individual habits, such as sleep deprivation [ 33 , 34 , 40 , 47 ], dehydration, and alcohol consumption before work [ 34 ]. International agencies have proposed various climate change adaptation and prevention strategies, including conducting training and awareness programs, using cooling mechanisms [ 13 , 16 , 26 , 38 , 39 , 40 , 41 , 44 , 47 ], and ensuring the availability of cool drinking water [ 13 , 16 , 20 , 25 , 44 , 47 , 49 ]. The most effective solutions at mitigating occupational heat strain were heat acclimation [ 26 , 29 , 30 , 31 , 32 , 33 , 34 , 36 , 37 , 40 , 47 ], wearing specialized cooling garments [ 27 , 47 ], cold water immersion [ 59 ], improving aerobic fitness [ 15 ], and applying ventilation [ 49 ]. Extending the exposure time to thermal stress leads to an increase in core body temperature and dehydration levels [ 60 ]. Acclimatized workers, with beneficial physiological adaptations like an efficient sweating system, lower heart rate, and core body temperature, can tolerate higher levels of dehydration and lose more water through sweat per shift. This means that the maximum allowable exposure time is greater for acclimatized workers compared to non-acclimatized workers [ 38 , 42 , 47 ]. Venugopal et al. demonstrated a strong correlation between physical workload, thermal stress exposures, Heat Strain Indicators (HSIs), and HRIs, leading to adverse health outcomes among outdoor workers [ 46 ]. There is a pressing need for evidence-based reviews and interventions to prevent occupational heat stress and enhance comprehensive resilience labor policies for outdoor workers in low and middle-income countries as climate change progresses. Increased awareness and consciousness among workers can lead to better adaptability to climate change risks [ 31 ]. Workers often implement conscious and flexible behavioral attitudes to manage their heat stress, especially in extremely hot workplaces, such as outdoor work [ 49 ]. Understanding the relationship between endurance time and WBGT values is crucial for training workers in very hot environments and ensuring their health and safety [ 43 ]. Elevated carbon emissions in the atmosphere contribute to extremely hot environments and climate changes, exacerbating occupational heat strains for outdoor workers [ 61 ]. A high-quality air and work environment can enhance worker safety, health, productivity, and company profitability [ 37 , 49 ]. Sustainable adaptation to warming climatic conditions [ 13 ] and social protection strategies during exposure to occupational heat stress depend on the availability of financial resources and collaborative efforts to overcome adaptation barriers [ 48 ]. The severity of occupational heat stress caused by climate change depends on workers’ sensitivity and vulnerability to different weather conditions. Additionally, the extent of adaptation capacity and resilience planning plays a crucial role [ 33 , 38 ]. Also, establishing a program that can assess how thermal stress due to climate change may increase heat-related effects on outdoor workers and document future heat-related events leading to relevant occupational health and safety regulations, seems essential [ 15 ].
The HEAT-SHIELD project is a customized occupational heat stress-related warning system that provides short- and long-term heat warnings to safeguard workers’ health and productivity. This project represents a useful adaptation strategy aimed at protecting workers, particularly those exposed to the effects of climate change [ 55 , 62 , 63 , 64 , 65 , 66 ].
The findings of this study are valuable for policymakers and professionals in the field of occupational health. They can use this information to develop guidelines and regulations aimed at preventing occupational heat stress and strengthening the resilience of outdoor workers during exposure to heat stress caused by climate change. However, it’s important to note that developing countries face a higher risk of negative occupational health outcomes compared to developed countries due to their lower adaptive capacity [ 46 ], increased poverty, and insufficient technological progress to combat climate change-induced temperature increases [ 6 , 47 ]. Outdoor workers often lack awareness of heat-related risks and HRI due to global warming [ 67 , 68 ]. Therefore, there is a critical need to raise awareness of heat-related hazards, bolster heat stress education, and update existing heat prevention measures. This includes optimizing current heat-related laws and adaptation policies to ensure effective implementation and compliance, especially in hot-dry and hot-humid work environments, particularly in low-middle-income countries [ 44 , 48 ]. Studies of this nature are essential among workers in these countries to provide health professionals and senior managers with the necessary knowledge to inform occupational heat stress adaptation policies, social protection measures, and resilience strategies for sustainable development.
Limitations
One limitation of this systematic review was the limited focus on female workers. Consequently, the results may not accurately represent the perspectives of women working outdoors, which is an important demographic to consider. Another significant limitation of this study is its heavy reliance on cross-sectional and experimental studies. Incorporating clinical aspects into data collection could greatly enhance and advance occupational health interventions. Furthermore, there is an evident scarcity of research exploring the social dimensions and the broader effects of occupational heat stress. Additionally, there is insufficient investigation into the adaptation strategies employed by workers in the context of increasing thermal stress and climate change, particularly in tropical and subtropical countries. These research gaps highlight the need for further studies to provide a more comprehensive understanding of this critical occupational health issue.
Addressing the health risks associated with occupational thermal stress among outdoor workers requires a multi-level approach that includes standard procedures and safety interventions. Currently, there is a lack of formal guidelines for outdoor workers, and most advisory systems do not adequately support this workforce in implementing solutions to mitigate occupational heat stress and enhance climate change resilience. While many workers acknowledge the importance of increased hydration and clothing adjustments during hot-dry and hot-humid climate conditions, a smaller proportion attempt to modify the nature of their work or seek rest in cooler areas. It is crucial to recognize that occupational heat stress remains a prevalent issue among these populations. To address these challenges, we recommend conducting further research to enhance our understanding of strategies aimed at bolstering the resilience of outdoor workers against heat stress resulting from climate change. This research should encompass diverse fields such as medicine, climatology, occupational health, and epidemiology. Additionally, there is a need to improve information dissemination, develop relevant regulations, and implement protective strategies among outdoor workers. These efforts will aid in identifying and preventing heat stress-related policies, including mitigation and adaptation measures.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on request.
Huang C, Barnett AG, Xu Z, Chu C, Wang X, Turner LR, et al. Managing the health effects of temperature in response to climate change: challenges ahead. Environ Health Perspect. 2013;121(4):415–9.
Article PubMed PubMed Central Google Scholar
Hall SA. Heat stress in outdoor manual workers in east Africa. Ergonomics. 1971;14(1):91–4.
Article CAS PubMed Google Scholar
Seo SN, Mendelsohn R. Measuring impacts and adaptations to climate change: a structural Ricardian model of African livestock management. Agric Econ. 2008;38(2):151–65.
Google Scholar
Brenkert AL, Malone EL. Modeling vulnerability and resilience to climate change: a case study of India and Indian states. Clim Change. 2005;72(1–2):57–102.
Article CAS Google Scholar
Alongi DM. Mangrove forests: resilience, protection from tsunamis, and responses to global climate change. Estuar Coast Shelf Sci. 2008;76(1):1–13.
Article Google Scholar
Habibi P, Ostad SN, Heydari A, Monazzam MR, Foroushani AR, Ghazi-Khansari M, et al. Diagnostic biomarkers of heat stress Induced-DNA in Occupational exposure: a systematic review. J Health Saf Work. 2023;12(4):800–19.
Yi W, Chan APC. Optimal work pattern for construction workers in Hot Weather: a Case Study in Hong Kong. J Comput Civil Eng. 2015;29(5).
Dehghan H, Habibi E, Habibi P, Maracy MR. Validation of a questionnaire for heat strain evaluation in women workers. Int J Prev Med. 2013;4(6):631.
PubMed PubMed Central Google Scholar
Thomas RJ. Opportunities to reduce the vulnerability of dryland farmers in Central and West Asia and North Africa to climate change. Agric Ecosyst Environ. 2008;126(1–2):36–45.
Habibi P, Ostad SN, Heydari A, Aliebrahimi S, Montazeri V, Foroushani AR, et al. Effect of heat stress on DNA damage: a systematic literature review. Int J Biometeorol. 2022;66(11):2147–58.
Article PubMed Google Scholar
Habibi P, Dehghan H, Haghi A, Shakerian M. The relationship between wet bulb globe temperature and physiological strain index in muslim women in hot-dry condition in the climatic chamber. Health Scope. 2015;4(1).
Kim D, Lee J. Spatial changes in work capacity for occupations vulnerable to heat stress: potential regional impacts from global climate change. Saf Health Work. 2020;11(1):1–9.
Hunt AP, Brearley M, Hall A, Pope R. Climate Change effects on the predicted heat strain and Labour Capacity of Outdoor Workers in Australia. Int J Environ Res Public Health. 2023;20(9):5675.
Samaniego-Rascón D, da Silva MCG, Ferreira AD, Cabanillas-Lopez RE. Solar energy industry workers under climate change: a risk assessment of the level of heat stress experienced by a worker based on measured data. Saf Sci. 2019;118:33–47.
Habibi P, Heydari A, Dehghan H, Moradi A, Moradi G. Climate Change and Occupational Heat Strain among Women Workers: a systematic review. Indian J Occup Environ Med. 2024;28(1):4–17.
Nunfam VF, Oosthuizen J, Adusei-Asante K, Van Etten EJ, Frimpong K. Perceptions of climate change and occupational heat stress risks and adaptation strategies of mining workers in Ghana. Sci Total Environ. 2019;657:365–78.
Odonkor ST, Adams S. Climate change-mediated heat stress vulnerability and adaptation strategies among outdoor workers. Clim Dev. 2022;14(7):591–9.
Pathak H. Impact, adaptation, and mitigation of climate change in Indian agriculture. Environ Monit Assess. 2023;195(1).
Amir S, Saqib Z, Khan MI, Khan MA, Bokhari SA, Zaman-Ul-haq M, et al. Farmers’ perceptions and adaptation practices to climate change in rain-fed area: a case study from district chakwal, Pakistan. Pak J Agric Sci. 2020;57(2):465–75.
Kjellstrom T, Lemke B, Hyatt O, Otto M. Climate change and occupational health: a South African perspective. South Afr Med J. 2014;104(8):586.
Schulte PA, Bhattacharya A, Butler CR, Chun HK, Jacklitsch B, Jacobs T, et al. Advancing the framework for considering the effects of climate change on worker safety and health. J Occup Environ Hyg. 2016;13(11):847–65.
Article CAS PubMed PubMed Central Google Scholar
Dehury RK, DeHuRy P. A review of measures against increasing temperature and climate change for the Safeguard of workers in India. J Clin Diagn Res. 2017;11(10).
Shamseer LMD, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;2:7647.
Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract. 2012;18(4):746–52.
Bates GP, Miller VS, Joubert DM. Hydration status of Expatriate Manual workers during Summer in the Middle East. Ann Occup Hyg. 2010;54(2):137–43.
PubMed Google Scholar
Hanna EG, Kjellstrom T, Bennett C, Dear K. Climate change and rising heat: population health implications for working people in Australia. Asia Pac J Public Health. 2011;23(2suppl):S14–26.
Kim JH, Coca A, Williams WJ, Roberge RJ. Effects of Liquid cooling garments on recovery and performance time in individuals performing strenuous work wearing a Firefighter Ensemble. J Occup Environ Hyg. 2011;8(7):409–16.
Chan APC, Yi W, Wong DP, Yam MCH, Chan DWM. Determining an optimal recovery time for construction rebar workers after working to exhaustion in a hot and humid environment. Build Environ. 2012;58:163–71.
Yokota M, Berglund LG, Bathalon GP. Female anthropometric variability and their effects on predicted thermoregulatory responses to work in the heat. Int J Biometeorol. 2012;56(2):379–85.
Chan APC, Yi W, Chan DWM, Wong DP. Using the thermal work limit as an environmental determinant of heat stress for construction workers. J Manage Eng. 2013;29(4):414–23.
Yamazaki F. Effectiveness of exercise-heat acclimation for preventing heat illness in the workplace. J UOEH. 2013;35(3):183–92.
Lui B, Cuddy JS, Hailes WS, Ruby BC. Seasonal heat acclimatization in wildland firefighters. J Therm Biol. 2014;45:134–40.
Hatvani-Kovacs G, Belusko M, Skinner N, Pockett J, Boland J. Drivers and barriers to heat stress resilience. Sci Total Environ. 2016;571:603–14.
Park J, Kim Y, Oh I. Factors affecting heat-related diseases in outdoor workers exposed to extreme heat. Annals Occup Environ Med. 2017;29:1–6.
Pogačar T, Črepinšek Z, Kajfež Bogataj L, Nybo L. Comprehension of climatic and occupational heat stress amongst agricultural advisers and workers in Slovenia. Acta Agric Slov. 2017;109(3):545–54.
Yang YC, Wei MC, Hong SJ, EVALUATION OF OCCUPATION HOT, EXPOSURE IN INDUSTRIAL WORKPLACES IN A SUBTROPICAL COUNTRY. Int J Occup Med Environ Health. 2017;30(3):379–95.
Kemala ITS, Yuliani S, editors. Acclimatization, Water Intake Adequacy Rate, Individual Characteristics and Heat Strain: A Cross-Sectional Study on Heat Exposed Workers. E3S Web of Conferences; 2018: EDP Sciences.
Nunfam VF, Adusei-Asante K, Van Etten EJ, Oosthuizen J, Frimpong K. Social impacts of occupational heat stress and adaptation strategies of workers: a narrative synthesis of the literature. Sci Total Environ. 2018;643:1542–52.
Nunfam VF. Social impacts of climate change and occupational heat stress and adaptation strategies of mining workers in Ghana. 2019.
Nunfam VF, Adusei-Asante K, Van Etten EJ, Oosthuizen J, Adams S, Frimpong K. The nexus between social impacts and adaptation strategies of workers to occupational heat stress: a conceptual framework. Int J Biometeorol. 2019;63(12):1693–706.
Nunfam VF, Adusei-Asante K, Frimpong K, Van Etten EJ, Oosthuizen J. Barriers to occupational heat stress risk adaptation of mining workers in Ghana. Int J Biometeorol. 2020;64:1085–101.
Talebi E, Sunkpal M, Sharizadeh T, Roghanchi P. The effects of Clothing Insulation and Acclimation on the Thermal Comfort of Underground Mine workers. Min Metall Explor. 2020;37(6):1827–36.
Tigchelaar M, Battisti DS, Spector JT. Work adaptations insufficient to address growing heat risk for US agricultural workers. Environ Res Letters: ERL [Web site]. 2020;15(9):094035.
Han S-R, Wei M, Wu Z, Duan S, Chen X, Yang J, et al. Perceptions of workplace heat exposure and adaption behaviors among Chinese construction workers in the context of climate change. BMC Public Health. 2021;21(1):1–16.
Tang TW, Zhang YC, Zheng ZM, Zhou XQ, Fang ZS, Liu WW. Detailed thermal indicators analysis based on outdoor thermal comfort indices in construction sites in South China. Build Environ. 2021;205.
Venugopal V, Shanmugam R, Kamalakkannan LP. Heat-health vulnerabilities in the climate change context—comparing risk profiles between indoor and outdoor workers in developing country settings. EnvironResLett. 2021;16(8):085008.
Habibi P, Moradi G, Dehghan H, Moradi A, Heydari A. The impacts of climate change on occupational heat strain in outdoor workers: a systematic review. Urban Clim. 2021;36:100770.
Butt MS, Saleem J, Ishaq M, Bukhari GMJ, Faryal J. Climate change vulnerability, adaptation assessment, and policy development for occupational health. Avicenna. 2022;2022(2):8.
Pal G, Patel T, Banik T. Effect of Climate Change Associated hazards on Agricultural workers and approaches for assessing heat stress and its mitigation strategies–review of some Research Significances. Int J Curr Microbiol App Sci. 2021;10(02):2947–75.
Habibi P, Momeni R, Dehghan H. Relationship of environmental, physiological, and perceptual heat stress indices in Iranian men. Int J Prev Med. 2015;6.
Saidi A, Gauvin C, Ladhari S, Nguyen-Tri P. Advanced functional materials for intelligent thermoregulation in personal protective equipment. Polym. 2021;13(21):3711.
Li J, Zhu W, Wang Y, Li J. Efficacy of cooling garments on exertional heat strain recovery in firefighters: a systematic review and meta-analysis. Text Res J. 2022;92(21–22):4521–35.
CAS Google Scholar
Itani M, Ghaddar N, Ghali K, Ouahrani D, Khater B. Significance of PCM arrangement in cooling vest for enhancing comfort at varied working periods and climates: modeling and experimentation. Appl Therm Eng. 2018;145:772–90.
Habibi P, Moradi G, Moradi A, Golbabaei F. A review on advanced functional photonic fabric for enhanced thermoregulating performance. Environ Nanatechnol Monit Manage. 2021;16:100504.
Ioannou LG, Foster J, Morris NB, Piil JF, Havenith G, Mekjavic IB, et al. Occupational heat strain in outdoor workers: a comprehensive review and meta-analysis. Temperature. 2022;9(1):67–102.
Flouris AD, Dinas PC, Ioannou LG, Nybo L, Havenith G, Kenny GP, et al. Workers’ health and productivity under occupational heat strain: a systematic review and meta-analysis. Lancet Planet Health. 2018;2(12):e521–31.
Soleimani N, Habibi P, Dehghan H. Effect of air blowing inside isolated hospital clothing on perceptual and physiological heat strain in laboratory conditions. Int J Biometeorol. 2023:1–12.
Kaciuba-Uscilko H, Grucza R. Gender differences in thermoregulation. Curr Opin Clin Nutr Metabolic Care. 2001;4(6):533–6.
Morris NB, Jay O, Flouris AD, Casanueva A, Gao C, Foster J, et al. Sustainable solutions to mitigate occupational heat strain–an umbrella review of physiological effects and global health perspectives. Environ Health. 2020;19:1–24.
Habibi P, Ostad SN, Monazzam MR, Foroushani AR, Ghazi-Khansari M, Aliebrahimi S, et al. Thermal stress and TiO2 nanoparticle–induced oxidative DNA damage and apoptosis in mouse hippocampus. Environ Sci Pollut Res. 2022;29(60):90128–39.
Sahoo SK, Lenka B, Raj A, Jhariya MK. Climate Change impacts and Mitigation through Sustainable Agroforestry practices. Advances in Sustainable Development and Management of Environmental and Natural resources: Economic Outlook and opinions: volume 1. Volume 1. Apple Academic; 2021. pp. 265–308.
Morris NB, Piil JF, Morabito M, Messeri A, Levi M, Ioannou LG, et al. The HEAT-SHIELD project—perspectives from an inter-sectoral approach to occupational heat stress. J Sci Med Sport. 2021;24(8):747–55.
Morabito M, Messeri A, Noti P, Casanueva A, Crisci A, Kotlarski S, et al. An occupational heat–health warning system for Europe: the HEAT-SHIELD platform. Int J Environ Res Public Health. 2019;16(16):2890.
Ciuha U, Valenčič T, Ioannou LG, Mekjavic IB. Efficacy of cooling vests based on different heat-extraction concepts: the HEAT-SHIELD project. J Therm Biol. 2023;112:103442.
Vanos J, Guzman-Echavarria G, Baldwin JW, Bongers C, Ebi KL, Jay O. A physiological approach for assessing human survivability and liveability to heat in a changing climate. Nat Commun. 2023;14(1):7653.
Nelson GC, Vanos J, Havenith G, Jay O, Ebi KL, Hijmans RJ. Global reductions in manual agricultural work capacity due to climate change. Glob Change Biol. 2024;30(1):e17142.
Pisello A, Rosso F, Castaldo V, Piselli C, Fabiani C, Cotana F. The role of building occupants’ education in their resilience to climate-change related events. Energy Build. 2017;154:217–31.
Wagner H. The management of heat flow in deep mines. Min Rep. 2013;149(2):88–100.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Occupational Health Engineering, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
Peymaneh Habibi & Farank Mahdavi
Health, Safety & Environment (HSE), Shahid Beheshti University of Medical Sciences and Health Services, Tehran, Iran
Jaleh Razmjouei
Safety and Risk Engineering, Faculty of Engineering and Applied Science, Memorial University of Newfoundland, St. John’s, Newfoundland, NL, Canada
Amirhossein Moradi
Department of Health in Emergencies and Disasters, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Saeed Fallah-Aliabadi
Accident Prevention and Crisis Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Department of Health in Disaster and Emergencies, School of Medicine, Kurdistan University of Medical Sciences, Sanandaj, Iran
Ahad Heydari
You can also search for this author in PubMed Google Scholar
Contributions
AH and PH were participated in the study design, data collection, data analysis. JR, AM, FM, SFA were participated manuscript writing, revising and editing. Study was done under the supervision of AH and PH. All authors read, revised and approved the final manuscript.
Corresponding author
Correspondence to Ahad Heydari .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Habibi, P., Razmjouei, J., Moradi, A. et al. Climate change and heat stress resilient outdoor workers: findings from systematic literature review. BMC Public Health 24 , 1711 (2024). https://doi.org/10.1186/s12889-024-19212-3
Download citation
Received : 02 September 2023
Accepted : 20 June 2024
Published : 26 June 2024
DOI : https://doi.org/10.1186/s12889-024-19212-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Climate change
- Outdoor workers
- Adaptation strategies
- Occupational heat stress
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Working on the COVID frontline inspired Northeastern research on the moral injury suffered by health care professionals
- Search Search
Rory Gleeson, an assistant professor of English at Northeastern University in London, is writing a novel based on his experience as a non-registered support worker, a role designed to assist under-pressure nurses.
- Copy Link Link Copied!

LONDON — Rory Gleeson knows what a beautiful death looks like. And he knows that patients he cared for while covered head to toe in protective personal equipment during the COVID-19 pandemic were not being afforded the life ending they deserved.
Gleeson is a novelist and assistant professor of English at Northeastern University in London. But, in an experience echoed the world over during the coronavirus pandemic , repeated lockdowns killed his creative spirit and the writing dried up.
Having interviewed senior staff at the hospital in Codogno — a town in Italy’s Lombardy region that was at the epicenter of the first European COVID-19 wave in spring 2020 — about the turmoil they had endured and the abandonment they felt, he was determined to put himself to practical use if the virus struck again.
And it did.
The second wave rocked the United Kingdom that autumn, encouraging the writer to apply for a job with the country’s National Health Service (NHS) as a non-registered support worker, a role designed to assist under-pressure nurses.
Now, Gleson is producing a novel based on his and others’ experience working on the frontlines.
“I had two grandparents of mine die in hospice in a very beautiful way,” Gleeson recalls. “They were cared for, they were spoiled rotten and they were given love, attention and kindness as they died.”
He says it was “important” for his family to see their loved ones “go with dignity” and know that the medical workers were “doing the best for their patients as they leave.”
But that experience was a world apart from when he started his three-month stint working in Hammersmith Hospital, west London, in early 2021 during the period when the third COVID wave in Britain was not long past its peak.
What he went through during shifts could be “upsetting” while also leaving him feeling shame and guilt at being unable to provide the level of care he wanted to at all times.

In more normal times, intensive care units will often see a nurse deployed with a single patient on a daily basis for the entirety of their weekly shift pattern, a deployment that allows strong bonds to form, Gleeson explains. He says during COVID overloads, nurses could be given as many as three high-dependency patients to care for, with support workers like him assisting them by helping with the physical labor of turning patients, washing them and changing beds, while also running ward errands.
“There were a number of things that were upsetting that you see and that you do,” he tells Northeastern Global News . “A lot of people in ICUs are uncomfortable, they’re in pain, they’re delirious or they’re in a very dazed state. And you are there to try to console that person and to try to make things easier for them — and a lot of times you can’t.
“Sometimes you don’t have the time and sometimes you have to move to other people or sometimes you have to do other things. So you literally don’t have the time and the space to give them the compassion, dignity and care that you would want, which is your job. A lot of the time there is a great sense of failure when you are watching somebody get worse or watching somebody suffer needlessly when you could help that person if the circumstances were different, if circumstances in the hospital were different,” he says.
The pace of the work could be so frantic and disconnected, especially because having to wear personal protective equipment like gloves and face masks fractured the personal relationship between coronavirus patient and caregiver, that the sick Gleeson had cared for died without him knowing.
“At one stage, somebody asked me about a patient and I thought, ‘Actually, I haven’t seen them in a while.’ I did a database search for them and I realized that the patient had died — he died two weeks before without me knowing,” he remembers.
“And then I looked through the list and I realized that there were seven or eight different patients that I had known who had actually passed. I’d never known, and that hit quite hard. Nobody had told you they had died because nobody knew who anybody was, nobody knew what the relationships were.”
It was while speaking to a staff member who was training ICU nurses that he became “struck” by a term she used to describe what health care professionals were experiencing — moral injury.
“She said there were a lot of nurses who felt that their patients had gotten worse under their care and that it was their fault,” says the screenwriter and novelist. “Those nurses had found that very emotionally damaging and they were ashamed and deeply offended by watching patients decline unnecessarily under their care and feeling personally responsible for it.”
The trainer had told him that this form of moral injury was causing many to “abandon their profession,” having felt let down by the health care system and the governments in charge.
Featured Stories

This music technology class takes students back through history — way, way back

US homicides and violent crime overall are down significantly, according to FBI data

Amazon is improving the autonomy capabilities of its Proteus robot with the help of this Northeastern fellow and grad student

Northeastern’s own version of ‘Shark Tank’ is helping create the next generation of C-suite executives
Moral injury has tended to have been associated with the guilt and shame that soldiers can return with from war after potentially having witnessed or been privy to something that offended their moral character, such as the killing of a prisoner of war.
But COVID instilled those same feelings of regret and betrayal in those who served on their own type of frontline during the pandemic. NHS Wales says moral dilemmas that some staff faced during coronavirus included being “unable to optimize end of life care” and “providing care with constrained or inadequate resources: for example, insufficient ventilators.”
“Health and social care workers may be exposed to morally injurious events, from instances where they are asked to act, or in some cases instructed not to, which go against their training and sense of right and wrong, or where they may experience betrayal at work,” according to the NHS.
Gleeson says he became intrigued by the concept of moral injury in health care.
“I found that very interesting,” he says, “because it was about how giving bad care impacts the person who ends up giving it. It is not something you think about a lot.”
Gleeson wants to speak to ICU workers and hear their stories. He will then use these conversations as inspiration for a novel that he will write as part of his three-and-a-half years of research for his PhD in creative writing.
He believes fiction, in this context, can be used to “express core emotional truths and new knowledge, but in a very emotionally impactful way.”
What Gleeson especially wants is for those to come forward who feel their story or account has not been heard in the media or through other mediums.
He says there is a “superhero narrative” in the NHS that puts medical workers up on a pedestal. But this, he argues, has cultivated a culture whereby these workers’ vocations are used against them, imposing long hours and low pay. “You can treat them poorly, because they’re supposed to take it, because they’re superheroes,” he says.
Gleeson continues: “But they’re people and they’re people who get tired, they’re people who make mistakes and they are people who have a variety of very complicated feelings about their job.
“So what I’m hoping to express with this is the amount of complication and complexity that a job of being a health care professional entails by getting people’s unspoken or less spoken about feelings about their jobs, their experience in their jobs and their experience of things they’ve done that they might not necessarily be immediately willing to tell people.”
He is hoping that his own travails of working in a major hospital during the pandemic will help him to connect and empathize with interviewees. “What I’ve learned when conducting some of the early interviews is you have to make it two-way,” he says.
“They are semi-structured interviews. But if it comes up during conversation that I have an example of something that I did or something I saw on a ward and you tell somebody about your own experience, that can give them a context and an idea of the way that you’re gathering information and the way that you’re processing stories.
“And the one thing I know about health care workers is they all have stories and they love telling them — they are very good storytellers. It is about getting the story they haven’t told somebody before.”
Those wanting to speak to Gleeson about their personal ICU experiences can email him at [email protected]

Recent Stories

Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Sex work and parenthood: the experiences of female sex workers who are also parents or caregivers: a scoping review.

Share and Cite
Winter, M.L.; Olivia, S.G. Sex Work and Parenthood: The Experiences of Female Sex Workers Who Are also Parents or Caregivers: A Scoping Review. Int. J. Environ. Res. Public Health 2024 , 21 , 852. https://doi.org/10.3390/ijerph21070852
Winter ML, Olivia SG. Sex Work and Parenthood: The Experiences of Female Sex Workers Who Are also Parents or Caregivers: A Scoping Review. International Journal of Environmental Research and Public Health . 2024; 21(7):852. https://doi.org/10.3390/ijerph21070852
Winter, Mokhwelepa Leshata, and Sumbane Gsakani Olivia. 2024. "Sex Work and Parenthood: The Experiences of Female Sex Workers Who Are also Parents or Caregivers: A Scoping Review" International Journal of Environmental Research and Public Health 21, no. 7: 852. https://doi.org/10.3390/ijerph21070852
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Influenza vaccination of healthcare workers: a literature review of attitudes and beliefs
Affiliation.
- 1 Bergische Universität Wuppertal, Fachbereich D-Abteilung Sicherheitstechnik, FG Arbeitsphysiologie, Arbeitsmedizin und Infektionsschutz, Gaussstrasse 20, 42097 Wuppertal, Germany. [email protected]
- PMID: 16804657
- DOI: 10.1007/s15010-006-5109-5
Background: Influenza vaccination coverage among healthcare workers (HCW) is insufficient despite health authority recommendations in many countries. Numerous vaccination campaigns encouraging HCW to be vaccinated have met with resistance. We reviewed published influenza vaccination programs in healthcare settings to understand the reasons for their success and failure, as well as the attitudes and beliefs of HCW.
Methods: Relevant articles published up to June 2004 were identified in the MEDLINE/Pubmed database.
Results: Thirty-two studies performed between 1985 and 2002 reported vaccination rates of 2.1-82%. Vaccination campaigns including easy access to free vaccine and an educational program tended to obtain the highest uptake, particularly in the USA. Yet, even this type of campaign was not always successful. Two main barriers to satisfactory vaccine uptake were consistently reported: (1) misperception of influenza, its risks, the role of HCW in its transmission to patients, and the importance and risks of vaccination (2) lack of (or perceived lack of) conveniently available vaccine.
Conclusion: To overcome these barriers and increase uptake, vaccination campaigns must be carefully designed and implemented taking account of the specific needs at each healthcare institution.
PubMed Disclaimer
Similar articles
- Influenza vaccine and healthcare workers. Aguilar-Díaz Fdel C, Jiménez-Corona ME, Ponce-de-León-Rosales S. Aguilar-Díaz Fdel C, et al. Arch Med Res. 2011 Nov;42(8):652-7. doi: 10.1016/j.arcmed.2011.12.006. Epub 2012 Jan 4. Arch Med Res. 2011. PMID: 22227045 Review.
- [Influence of knowledge and attitude on the uptake of influenza vaccine by healthcare workers]. Nativ T, Paz A, Peterfreund I, Potasman I. Nativ T, et al. Harefuah. 2010 Oct;149(10):626-9, 685. Harefuah. 2010. PMID: 21568055 Hebrew.
- Knowledge, attitudes and beliefs regarding influenza vaccination among healthcare workers in a Saudi hospital. Rehmani R, Memon JI. Rehmani R, et al. Vaccine. 2010 Jun 11;28(26):4283-7. doi: 10.1016/j.vaccine.2010.04.031. Epub 2010 May 2. Vaccine. 2010. PMID: 20441803
- Influenza vaccination of health care workers in hospitals--a review of studies on attitudes and predictors. Hollmeyer HG, Hayden F, Poland G, Buchholz U. Hollmeyer HG, et al. Vaccine. 2009 Jun 19;27(30):3935-44. doi: 10.1016/j.vaccine.2009.03.056. Epub 2009 Apr 8. Vaccine. 2009. PMID: 19467744 Review.
- Health care worker beliefs about influenza vaccine and reasons for non-vaccination--a cross-sectional survey. Canning HS, Phillips J, Allsup S. Canning HS, et al. J Clin Nurs. 2005 Sep;14(8):922-5. doi: 10.1111/j.1365-2702.2005.01190.x. J Clin Nurs. 2005. PMID: 16102143
- Physical health and mental health functional status during and following hospitalization for an acute respiratory illness. Nowalk MP, Balasubramani GK, Sax TM, Eng H, Saul S, Susick M, Zimmerman RK. Nowalk MP, et al. Brain Behav Immun Health. 2019 Nov 14;1:100004. doi: 10.1016/j.bbih.2019.100004. eCollection 2020 Jan. Brain Behav Immun Health. 2019. PMID: 38377430 Free PMC article.
- Health Belief Model in studies of influenza vaccination among health care workers. Silva SB, Souza FO, Pinho PS, Santos DV. Silva SB, et al. Rev Bras Med Trab. 2023 Aug 8;21(2):e2022839. doi: 10.47626/1679-4435-2022-839. eCollection 2023 Apr-Jun. Rev Bras Med Trab. 2023. PMID: 38313093 Free PMC article. Review.
- The effectiveness of interventions to improve the seasonal influenza vaccination uptake among nurses: A systematic review. Flanagan P, Dowling M, Sezgin D, Mereckiene J, Murphy L, Giltenane M, Carr P, Gethin G. Flanagan P, et al. J Infect Prev. 2023 Nov;24(6):268-277. doi: 10.1177/17571774231208115. Epub 2023 Oct 20. J Infect Prev. 2023. PMID: 37969468 Free PMC article. Review.
- Changes in Students' Perceptions Regarding Adolescent Vaccinations through a Before-After Study Conducted during the COVID-19 Pandemic: GIRASOLE Project Study. Restivo V, Bruno A, Minutolo G, Pieri A, Riggio L, Zarcone M, Candiloro S, Caldarella R, Immordino P, Amodio E, Casuccio A. Restivo V, et al. Vaccines (Basel). 2023 Sep 25;11(10):1524. doi: 10.3390/vaccines11101524. Vaccines (Basel). 2023. PMID: 37896928 Free PMC article.
- Vaccination Attitudes Examination (VAX) Scale: a Bifactor-ESEM approach in a youth sample (15-24 years). Jovanović V, Lazić M. Jovanović V, et al. BMC Psychol. 2023 Oct 23;11(1):351. doi: 10.1186/s40359-023-01388-9. BMC Psychol. 2023. PMID: 37872642 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- MedlinePlus Health Information
Miscellaneous
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- West J Emerg Med
- v.21(5); 2020 Sep
The Impact of COVID-19 on Healthcare Worker Wellness: A Scoping Review
Jacob shreffler.
* University of Louisville, Department of Emergency Medicine, Louisville, Kentucky
Jessica Petrey
† University of Louisville, Kornhauser Library, Louisville, Kentucky
Martin Huecker
Associated data.
At the heart of the unparalleled crisis of COVID-19, healthcare workers (HCWs) face several challenges treating patients with COVID-19: reducing the spread of infection; developing suitable short-term strategies; and formulating long-term plans. The psychological burden and overall wellness of HCWs has received heightened awareness in news and research publications. The purpose of this study was to provide a review on current publications measuring the effects of COVID-19 on wellness of healthcare providers to inform interventional strategies. Between April 6–May 17, 2020, we conducted systematic searches using combinations of these keywords and synonyms in conjunction with the controlled vocabulary of the database: “physician,” “wellness, “wellbeing,” “stress,” “burnout,” “COVID-19,” and “SARS-CoV-2.” We excluded articles without original data, research studies regarding the wellness of non-healthcare occupations or the general public exclusively, other outbreaks, or wellness as an epidemic. A total of 37 studies were included in this review. The review of literature revealed consistent reports of stress, anxiety, and depressive symptoms in HCWs as a result of COVID-19. We describe published data on HCW distress and burnout but urge future research on strategies to enhance HCW well-being.
INTRODUCTION
The COVID-19 pandemic has resulted in significant burdens globally. Detrimental effects include high rates of infection and death, financial hardships faced by individuals, stress related to known and particularly unknown information, and fear of the uncertainty regarding continued impact. Healthcare workers (HCWs), at the heart of the unparalleled crisis of COVID-19, face challenges treating patients with COVID-19: reducing the spread of infection; developing suitable short-term strategies; and formulating long-term plans. HCWs must also continue to successfully treat non-COVID patients and maintain personal responsibilities, including taking care of their families and themselves. The psychological burden and overall wellness of HCWs has received heightened awareness, with research continuing to show high rates of burnout, psychological stress, and suicide. 1
HCWs experience emotional exhaustion, which may lead to medical errors, lack of empathy in treating patients, lower productivity, and higher turnover rates. 2 The ability of HCWs to adequately cope with stressors is important for their patients, their families, and themselves. Providers vary in levels of psychological resilience, the ability to positively adapt to adversity to protect themselves from stress. 3 Prior to COVID-19, wide-ranging research had established the multifactorial nature of stressors in healthcare: electronic health record duties; insurance and billing issues; any patient dissatisfaction; and balancing busy work-life schedules. 4
HCWs must continue to balance these existing obstacles to wellness while facing the unique challenges of a pandemic. Literature from severe acute respiratory syndrome and Middle East respiratory syndrome can provide insight on the stress, trauma, psychological morbidities, and successful interventions, but the body of evidence for the impact COVID-19 on HCW wellness is evolving alongside the pathogen. The purpose of this study was to provide a review of current publications measuring the effects of COVID-19 on wellness of the HCWs to inform interventional strategies.
Between April 6–May 17, 2020, we conducted systematic searches in PubMed, Embase, Cochrane, Clinical Key, and Web of Science using combinations of these keywords and synonyms in conjunction with the controlled vocabulary of the database: “physician,” “wellness,” “wellbeing,” “stress,” “burnout,” “COVID-19,” and “SARS-CoV-2.” Results were filtered to English-language publications, retrieving a total of 107 references. We examined references in included papers and relevant excluded papers for additional studies, and a non-systematic search in Google Scholar was conducted as well. After those selections were added and duplicates were removed, 185 distinct references remained for screening.
To reduce risk of bias, titles and abstracts were screened for eligibility by two independent reviewers, with a third available in the event of disagreements. Papers presenting original data regarding the evaluation or management of physicians’ well-being during the COVID-19 pandemic were included for full analysis. Some publications indexed as correspondence did contain data, so article type was not an automatic exclusion criterion, nor was study design and quality of methodology. While papers on infection control practices, personal protective equipment (PPE), or wellness in other types of HCWs were not actively sought out, any retrieved by the strategies were retained. We excluded articles without original data, research studies regarding the wellness of non-healthcare occupations or the general public exclusively, other outbreaks, or wellness as an epidemic ( Figure ).

Process of systematic searches using combinations of “physician,” “wellness,” “wellbeing,” “stress,” “burnout,” “COVID-19,” and “SARS-CoV-2” to provide a scoping review on publications measuring the effects of novel coronavirus 2019 on wellness of healthcare workers.
We included 37 studies in this review. Multiple themes emerged from the current literature on how COVID-19 has impacted HCW wellness. The majority of studies focused on the psychological impact of COVID-19, including stress and anxiety measurements. Some evaluated burnout and sleep quality. A small portion of the studies used qualitative methodology. We have provided a summary of the articles below.
Stress, Fear, Anxiety, Depression
In light of the many known and unknown effects of COVID-19, exploration of stress, fear, anxiety and symptoms of depression were prevalent in the included studies, with many focusing on frontline HCWs.
Frontline Workers
Researchers assessed anxiety levels in 512 frontline healthcare workers in China, finding a prevalence of 12.5%. 5 The authors found HCWs who had direct contact with COVID-19 patients were at higher risk for anxiety. 5 Frontline workers were also a focus by Lu et al in 2299 HCWs (2042 medical staff and 257 administrative staff). The authors found that medical staff had greater fear, anxiety, and depression levels than administrative staff. Additionally, the investigators found that HCWs working on frontlines in departments more impacted by COVID-19 (ie, emergency department, intensive care unit, infections disease) were at greater risk for anxiety and depression and psychological disorder. 6
A total of 5062 HCWs were surveyed by Zhu et al to measure psychological impact of COVID-19. 7 The authors measured stress, depression, and anxiety, discovering that 29.8% of respondents reported stress, 24.1% reported anxiety, and 13.5% reported depression. Women, individuals with history of mental disorders, and HCWs with infected family members were more vulnerable to undesirable health consequences of stress, anxiety, and depression. 7
Liu et al measured distress, anxiety, and symptoms of depression in 4679 Chinese HCWs. 8 Results showed the prevalence of anxiety and distress was about 16% each; 34.6% of respondents experienced depressive symptoms. The investigators discovered that risk factors for developing the mental health concerns aforementioned included living alone, being a nurse, being on the frontline, and middle age. 8
Li et al measured the vicarious traumatization phenomenon in three groups: frontline nurses, non-frontline nurses, and general population. Frontline nurses had lower levels of trauma than both the general public and non-frontline nurses. The authors hypothesized that frontline nurses have better training to deal with crisis. 9 Similar findings were discovered in 470 HCWs in Singapore. 10 Results showed non-medical workers had greater anxiety and stress compared to medical workers. Among the 470 HCWs, 14.5% experienced anxiety with 7.7% experiencing levels of concern for post-traumatic stress disorder. 10
Liang et al compared HCWs in COVID-19 associated departments to other HCWs. They found a significant portion of HCWs experienced clinically depressive symptoms, but no significant differences between frontline HCWs and non-frontline HCWs. 11 A study by Cai et al measured the psychological impact of COVID-19 on 534 frontline medical-staff members. 12 The authors found that HCWs experienced anxiety about their own and their family’s safety (along with their patients) but maintained the professional obligation to effectively complete their work. The authors found that older staff had increased stress related to (lack of) PPE and longer work hours. Coping strategies used by the HCWs included adhering to strict protective measures, following isolation guidelines, and exhibiting a positive mindset. 13
Guo et al studied 11,118 HCWs in China. Results showed that risk factors for anxiety and depression were being younger, employed as a nurse, and being a frontline HCW. Within the sample, about 5% experienced middle to high levels of anxiety and about 13.5% experience middle to high depression levels. 13 Lai et al found that female gender predicted greater risk of psychological stress in a study that examined depression, anxiety, insomnia, and distress in 1257 HCWs. 14 HCWs experienced high incidence of depression (50.4%), anxiety (44.6%), and insomnia (34%). The majority of HCWs reported distress (71.5%), with women, nurses, frontline workers, and those working in Wuhan, China, having higher negative health outcomes. 14
Dai et al discovered that geographic location was a risk factor for distress in 4357 HCWs. The results showed that 39.1% of HCWs experienced distress; living in Wuhan, being isolated, worrying about family members and working on the frontline were risk factors for experiencing distress. 15 HCWs were chiefly concerned about infection in colleagues or family members. 15 Geographic location was also a risk factor in a study in Italy comparing stress and anxiety in healthcare workers (n = 167) to the general population (n = 186). Likelihood of exposure to disease (HCWs and individuals in highly affected Northern Italy) predicted increased stress and anxiety. Overall, HCWs reported higher levels of worry compared to the general population. 16
In a letter to the editor, Du et al reported smartphone survey data on frontline HCWs in Wuhan. HCWs from two hospitals and one outreach team answered multiple questions during a five-day period. The outreach team members appeared more prepared psychologically, had more supplies, and had improved sleep, stress, and levels of depression compared to frontline workers. Fifty-nine percent of respondents had moderate to severe perceived stress, with 12.7% having at least mild depressive symptoms and 20.1% having anxiety. Those at greatest risk were HCWs who felt less prepared, had less family support, felt less self-efficacy, perceived a higher level of stress, and those with poor sleep quality. Fear of self and colleague infection represented a top source of stress. 17
Unspecified/Other Healthcare Workers
Access to PPE was a key focus by Zhang et al, who surveyed 304 HCWs in Iran. The authors found that 28% of HCWs experienced anxiety, 20.1% experienced distress, and 30.6% experienced depression. Furthermore, the study revealed that access to PPE resulted in both improved physical health and job gratification and ultimately led to less distress among HCWs. 18 Delgado et al measured HCW personal safety perception in 936 workers in Latin America. Overall, HCWs lacked sufficient PPE and felt limited support from human resources and public officials. 19
Preparedness to fight COVID-19 was examined in 158 HCWs in England. The authors found that HCWs desired more actions (including proper education) to feel confident to fight COVID-19, particularly in the collection and management of samples. 20 Suleiman et al conducted a similar study on preparedness for the COVID-19 outbreak, surveying 308 physicians in Jordan. Individuals with protocols in place and accessible PPE reported higher levels of readiness. Furthermore, 90.9% of respondents reported feelings of anxiousness regarding the transmission of the disease and fear of the increase of the volume of infected patients. The large majority (96.4%) of HCWs were worried about transmitting COVID-19 to loved ones. 21
Chew et al measured stress and anxiety in HCWs in 906 HCWs in Singapore and India. The results showed that 48 (5.3%) HCWs faced moderate to very severe depression and 79 (8.7%) had moderate to extremely severe depression. Additionally, 54 (6%) HCWs experienced moderate to extremely severe stress or moderate to severe distress. After correcting for confounders, the authors noted an association between incidence of prior month physical symptoms and emotional distress during COVID-19. 22
In Wuhan, China, Kang et al measured mental health and psychological wellbeing using a survey in 994 HCWs. The study revealed that 28.6% of the sample had moderate to severe mental disturbances, with young women affected the most. Within the study population, subjects who accessed mental health amenities had improved relationship between exposure risks and mental health. 23
Jiang et al measured psychological impact by comparing self-efficacy and loneliness of 205 HCWs in Hubei, China. Medical staff with lower self-efficacy had higher likelihood of loneliness. The authors noted that individuals experiencing loneliness may choose undesirable coping tactics (eg, substance use). 24 The protective effect of a committed relationship surfaced in 194 physicians surveyed in Oman. The researchers revealed that individuals who were married and older experienced less stress compared to other HCWs. Additionally, the authors found that females may be more susceptible to stress. 25
Some physician-specific studies occurred in the included literature. Chen et al surveyed pediatricians on outcomes of stress and anxiety. Of 105 respondents, 90.5% of the sample were female and 18.1% reported working in high-risk areas. The authors noted particularly high self-reported depression and anxiety during the COVID-19 outbreak. 26 In a study completed by Xu et al, the researchers surveyed 60 surgical staff during a period of COVID-19 outbreak and compared them with a separate group of 60 surgical staff in a non-outbreak period in China. The results showed that HCWs surveyed during the outbreak period had significantly higher levels of anxiety and depression. 27 One researcher used the Beck Anxiety Inventory to measure anxiety in multiple sclerosis fellows in Iran. The authors had 14 respondents and only two individuals had mild levels of anxiety. 28
A focused look at dentists and dental hygienists assessed the COVID-19 impact in Israel. Among the 338 surveyed, individuals with previous illness and those worried about infection from patients were inclined to higher levels of distress. HCWs in committed relationships and those with superior levels of self-efficacy reported less stress. 29
Wu et al specifically measured burnout in 220 oncology medical staff working in Wuhan, China. Using the validated and widely deployed Maslach Burnout Inventory-Medical Personnel (MBI), they compared levels of burnout in frontline and other HCW groups. Frontline HCWs had significantly lower levels of burnout and were less worried about becoming ill compared to those in the “usual ward” group. The authors noted two possible explanations: frontline HCWs may perceive more control over their situation and may appreciate a closer proximity to decision-makers (with more timely provided information) compared with the other HCWs. 30
Cao et al used the MBI to measure burnout and emotional distress in 37 HCWs. They found that the levels of burnout and emotional distress were not highly elevated within their sample. Connecting with family members via technology or telephone was the most prevalent coping mechanism. The study showed that 29.7% of the sample had issues obtaining proper sleep. 31
Some researchers focused specifically on COVID-19’s impact on HCW sleep. Xiao et al surveyed 180 medical staff members on social support, anxiety, stress, self-efficacy, and sleep quality to determine the effects of COVID-19. 32 The authors found that social support correlated significantly with both self-efficacy and quality of sleep. Anxiety and stress were significantly associated, leading to negative impacts on both self-efficacy and sleep. The authors recommended HCWs to take advantage of support systems, including family and friends to stabilize emotions, share experiences, and maintain social connections, thus reducing anxiety intensities and enabling quality sleep. 32
Huang and Zhao measured sleep, anxiety, and depressive symptoms in 2250 HCWs. The authors compared HCWs’ results to individuals from the general population. Results showed that HCWs were more likely to experience poor quality sleep and develop psychological issues. 33 Qi et al also measured sleep in their survey of 1306 (801 frontline) HCWs in China. The authors found that frontline HCWs had advanced anxiety, depression, and prevalence of sleep disturbances compared to non-frontline HCWs. Furthermore, the authors found that female frontline HCWs had higher prevalence of sleep disturbances compared with male frontline HCWs. 34
Zhang W et al found that medical HCWs had higher levels of insomnia, anxiety, depression, somatization, and obsessive-compulsive symptoms compared to non-medical HCWs in 2182 respondents in China. Risk factors for worsened mental health included living in a rural area, being female, and having contact with infected COVID-19 patients. 35 Finally, insomnia was measured in HCWs in China involved in the COVID-19 outbreak. Of the 1563 respondents, 36.1% reported insomnia symptoms. Insomnia risk factors included lower levels of education, working in a unit with isolation, being a physician, lack of support, having high levels of uncertainty, and being worried about infection. The authors called for interventions for insomnia for HCWs. 36
Qualitative Approach
Some researchers used qualitative methods to gain better insight into the impact of COVID-19 on HCW wellness. Liu et al interviewed nine nurses and four physicians in Hubei. Respondents described many challenges of COVID-19 including fear of infection, exhaustion, and working in a new context. Despite these challenges, the HCWs felt that they were fully responsible to care for their patients as it was part of their duty, demonstrating an immense vow to their profession. The authors noted that workplace safety including access to PPE was a top priority. 37
Sun et al interviewed 20 nurses who provided care for COVID-19 patients in China. The study results indicated that anxiety and fear were prevalent in the early stages of the outbreak, leading to feelings of helplessness. The authors noted some healthy coping strategies, including team encouragement and rational thinking. Furthermore, the authors found that reflection and developing a sense of professional responsibility resulted in growth. Finally, the researchers discovered that the nurses experienced both negative and positive emotions concurrently. 38
Sethi et al also used a qualitative approach to develop open-ended questions for 290 HCWs in Pakistan. They found that HCWs were anxious, overworked, and felt financially unstable. Furthermore, HCWs reported challenges in taking care of both their professional lives and their households. 39
Healthcare Workers Who Became Ill
This review did not intend to describe exposure, infection rate, or mortality of healthcare providers during the COVID-19 pandemic. Two publications that appeared in our literature search described providers who became infected with the virus, but we refer readers to reviews focused on this topic. 40 , 41 Ran et al examined risk factors for HCWs who developed acute respiratory infection in Wuhan China. The authors found that longer hours, higher risk clinical setting, and suboptimal hand cleanliness were risk factors for infection. 42
Researchers in Wuhan, China, studied 103 HCWs who had become infected with COVID-19. These HCWs answered questions on perceived cause of infection and psychological changes. Results showed that the large majority (84.5%) of HCWs who became infected felt it was due to their work setting, with nurses’ top three perceived causes being suction care, swab collection, and other nursing requirements. Physicians perceived highest risk in physical examination and tracheal or manual ventilations. During the isolation period, 88.3% of these HCWs experienced stress or emotional deviations. The study showed that persons who were experiencing distress were apprehensive about their own health in addition to transmitting it to loved ones. 43
The review of literature revealed consistent reports of stress, anxiety, and depressive symptoms in HCWs as a result of COVID-19. Multiple studies confirmed significant anxiety regarding patient care in addition to the possibility of infecting their families. 12 , 16 , 30 Access to appropriate PPE remains of paramount importance to help physicians feel physically safe. With sufficient PPE, individuals feel more protected from infection, which may lessen fear of infecting loved ones. Women and individuals in high-risk areas may have more negative psychological health outcomes. Furthermore, both individuals on the frontline and other HCWs are susceptible to distress and negative health outcomes including anxiety, poor quality sleep, and feelings of isolation. Interestingly, some frontline workers experienced better mental health outcomes. The sense of vocation / purpose in work, along with greater control of environment, could explain these findings.
Given the relative novelty of this crisis, no published studies have collected data on interventions to improve psychological health and overall wellness for HCWs who face COVID-19 specific challenges. Suggestions to alleviate the burden on HCW mental health have been provided by researchers both for COVID-19 and in other crises. We found no studies that measured the same sample before and after COVID-19 to determine how wellness or stress changed within the same individuals. Researchers could compare previous datasets on provider wellness to measure and quantify effects of COVID-19.
Generally recognized for their emotional resilience, HCWs must now face additional layers of responsibilities and mental and physical hardships. 1 We remain uncertain about the timeline and actions needed to effectively combat this virus but hope to reduce severity of current and future waves of infection. 44 Targeted individual and organizational strategies for mental health and overall wellness for HCWs are critical for these courageous individuals. Based on the narrative review of the literature, we believe the following are necessary strategies for HCW wellness provided in the Table .
Strategies for healthcare worker wellness.
PPE , personal protective equipment; HCW , healthcare worker.
LIMITATIONS
The research on effects of COVID-19, and physician wellness in general, continues to rapidly evolve.
Therefore, updated reviews will be necessary in the coming months. The present review was limited by search strategies designed to retrieve publications with a focus on overall well-being, burnout, or stress; thus, studies exclusively about the physical protection, infection, and transmission rates within this population may not have been retrieved. Future research should consider assessing the psychological burden placed upon HCWs by practical and physiological aspects of disease. Finally, there was limited literature from US providers due to this scoping review being conducted in the earlier stages of the pandemic.
We recognize the obstacles to implementing strategies to improve HCW wellness: financial barriers; worker engagement; etc. 2 Burnout, stress, and the emotional burden of caring for sick patients were already affecting HCWs before COVID-19. Long-term effects of the worldwide pandemic remain unknown. We described published data on HCW distress and burnout but urge future research on strategies to enhance HCW wellbeing. To continue to provide uninterrupted, quality care, the healthcare workforce – human beings – must be empowered and encouraged to take care of themselves. 4
Supplementary Information
Section Editor: Patrick J. Maher, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Disclaimer: Due to the rapidly evolving nature of this outbreak, and in the interests of rapid dissemination of reliable, actionable information, this paper went through expedited peer review. Additionally, information should be considered current only at the time of publication and may evolve as the science develops.
Conflicts of Interest : By the West JEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.

IMAGES
VIDEO
COMMENTS
The shortage of healthcare workers is a growing concern. The COVID-19 pandemic and retirement wave have accelerated turnover rates. This systematic review aimed to identify and analyse the existing interventions for job retention of healthcare workers, in terms of nurses and physicians, in a hospital setting.
Background: Acquisition of a health care-associated infection is a substantial risk to patient safety. When health care workers comply with hand hygiene guidelines, it reduces this risk. Despite a growing body of qualitative research in this area, a review of the qualitative literature has not been published.
A summative content analysis was used to analyze the data. Healthcare workers described three types of stressors: work stressors (49% of total stressors), personal life stressors (32% of total stressors), and stressors that intersect work and personal life (19% of total stressors). Future research and clinical practice should consider the multi ...
Healthcare personnel shortages are a problem across the globe. With a lack of 4.3 million doctors in 2016 1 and 5.9 million nurses in 2020 2 globally, the shortage was already critical. The World Health Organization (WHO) reports that by 2030, there will be a global shortage of almost 14 million healthcare workers, in terms of nurses, physicians, midwives and other cadres. 3 These challenges ...
Conclusion. A significant number of HCW were reported to be infected with COVID-19 during the first 6 months of the COVID-19 pandemic, with a prevalence of hospitalisation of 15.1% and mortality of 1.5%. Further data are needed to track the continued risks in HCW as the pandemic evolves and health systems adapt.
Background. Mental health is declining in health care workers. Objectives. To provide a comprehensive assessment of intervention literature focused on the support and treatment of mental health within the health care workforce. Search Methods. We searched online databases (e.g., Medline, PsycINFO). Selection Criteria. We selected manuscripts published before March 2022 that evaluated the ...
This review of the qualitative literature enabled the researchers to take an inductive approach allowing for all factors affecting the phenomenon of interest to be explored. Two core concepts seem to influence health care workers' compliance with hand hygiene guidelines. ... Health care workers' compliance with hand hygiene guidelines was ...
The shortage of healthcare workers is a growing problem across the globe. Nurses and physicians, in particular, are vulnerable as a result of the COVID-19 pandemic. ... The Race to Retain Healthcare Workers: A Systematic Review on Factors that Impact Retention of Nurses and Physicians in Hospitals Inquiry. 2023 Jan-Dec:60:469580231159318. doi ...
The psychological burden and overall wellness of HCWs has received heightened awareness in news and research publications. The purpose of this study was to provide a review on current publications measuring the effects of COVID-19 on wellness of healthcare providers to inform interventional strategies. Between April 6-May 17, 2020, we conducted ...
Acquisition of a health care-associated infection is a substantial risk to patient safety. When health care workers comply with hand hygiene guidelines, it reduces this risk. Despite a growing body of qualitative research in this area, a review of the qualitative literature has not been published.
COVID-19 has challenged health systems worldwide, especially the health workforce, a pillar crucial for health systems resilience. Therefore, strengthening health system resilience can be informed by analyzing health care workers' (HCWs) experiences and needs during pandemics. This review synthesizes qualitative studies published during the first year of the COVID-19 pandemic to identify ...
This literature review focused on the mental health and coping strategies of healthcare workers amidst pandemic. Coronavirus disease 2019 (COVID-19) has produced a worldwide health catastrophe ...
FACTORS IMPACTING THE EFFECTIVENESS OF HEALTH CARE WORKER BEHAVIOR CHANGE A LITERATURE REVIEW. May 20, 2016. ACKNOWLEDGEMENTS. The USAID-funded Health Communication Capacity Collaborative (HC3) - based at the Johns Hopkins Center for Communication Programs - would like to acknowledge Erin Kurtz for authoring this report with input from ...
In the current period of global public health crisis due to the COVID-19, healthcare workers are more exposed to physical and mental exhaustion - burnout - for the torment of difficult decisions, the pain of losing patients and colleagues, and the risk of infection, for themselves and their families. The very high number of cases and deaths ...
The COVID-19 pandemic has challenged and, in many cases, exceeded the capacity of hospitals and intensive care units (ICUs) worldwide. Health-care workers have continued to provide care for patients despite exhaustion, personal risk of infection, fear of transmission to family members, illness or death of friends and colleagues, and the loss of many patients. Sadly, health-care workers have ...
Professional quality of life is a crucial aspect of healthcare professionals' well-being and job satisfaction. Job satisfaction, on the other hand, encompasses fulfillment of desired needs within the work environment, happiness or gratifying emotional response towards working conditions, and job values or equity. Existing literature tends to address job satisfaction and professional quality ...
The community health worker (CHW) workforce in the United States has grown substantially since it was established in the 1960s, with the goal of effectively linking underserved communities to vital health services [].CHWs—also known as promotores/as de salud, peer health educators, and lay health advocates—are frontline public health workers who help community members overcome barriers to ...
Abstract. Aim: The aim of this scoping literature review was to examine and summarize the factors, context, and processes that influence work motivation of health care workers. Methods: A scoping literature review was done to answer the question: What is known from the existing empirical literature about factors, context, and processes that ...
Healthcare workers (HCWs) rely on personal protective equipment (PPE) to reduce exposure to infectious diseases while treating patients. Guidance documents, such as the 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, inform PPE selection for HCWs. ... This literature review aims to ...
Background While many populations struggle with health literacy, those who speak Spanish preferentially or exclusively, including Hispanic, immigrant, or migrant populations, may face particular barriers, as they navigate a predominantly English-language healthcare system. This population also faces greater morbidity and mortality from treatable chronic diseases, such as hypertension and ...
Background Attracting and supporting a sustainable long-term care (LTC) workforce has been a persistent social policy challenge across the globe. To better attract and retain a sustainable LTC workforce, it is necessary to adopt a unified concept of worker well-being. Meaning of work is an important psychological resource that buffers the negative impacts of adverse working conditions on ...
During the COVID-19 pandemic, this systematic review and meta-analysis aims to provide a complete assessment of the prevalence of burnout across various healthcare personnel. Until January 2021, systematic searches for English language papers were conducted using PubMed, Scopus, EMBASE, Web of Science, Cochrane Library, and ProQuest.
A review conducted in 2013 showed only nine papers examining the role of support workers in providing end-of-life care, eight of which studied assistant healthcare workers and only one examined social homecare workers.13 However, the available literature confirms challenges regarding a lack of training about the specific needs of this client ...
Global warming has led to an increase in the number and intensity of extreme heat events, posing a significant threat to the health and safety of workers, especially those working outdoors, as they often have limited access to cooling strategies. The present systematic literature review (a) summarizes the current knowledge on the impacts of climate change on outdoor workers, (b) provides ...
In the current period of global public health crisis due to the COVID-19, healthcare workers are more exposed to physical and mental exhaustion - burnout - for the torment of difficult decisions, the pain of losing patients and colleagues, and the risk of infection, for themselves and their families. The very high number of cases and deaths ...
Working on the COVID frontline inspired Northeastern research on the moral injury suffered by health care professionals. Rory Gleeson, an assistant professor of English at Northeastern University in London, is writing a novel based on his experience as a non-registered support worker, a role designed to assist under-pressure nurses.
A questionnaire-based cross sectional study was conducted during November and December 2019 among health care workers working in wards and Intensive Care Unit (ICU) of Medicine Department at a tertiary care centre in New Delhi, India. Health care workers included doctors and nurses. ... Review of the literature. J Infect Dev Ctries 2015; 9 (10 ...
Complex interactions exist between sex work and parenthood, impacting the lives of those in sex work who also provide care for others. This scoping review aims to review the experiences and challenges of female sex workers who are parents or caregivers, highlighting the socioeconomic, psychological, and legal dimensions of their dual roles. The rationale for this review stems from the ...
We reviewed published influenza vaccination programs in healthcare settings to understand the reasons for their success and failure, as well as the attitudes and beliefs of HCW. Methods: Relevant articles published up to June 2004 were identified in the MEDLINE/Pubmed database. Results: Thirty-two studies performed between 1985 and 2002 ...
We included 37 studies in this review. Multiple themes emerged from the current literature on how COVID-19 has impacted HCW wellness. The majority of studies focused on the psychological impact of COVID-19, including stress and anxiety measurements. Some evaluated burnout and sleep quality.