
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
JavaScript appears to be disabled on this computer. Please click here to see any active alerts .

EPA Health Impact Assessment Case Studies
In the news.
[Aug 2022] Read about the latest HIA case study completed for Southwest Rockford, IL .
- Health Impact Assessments
EPA has undertaken several Health Impact Assessment (HIA) case studies to learn how its science can be used in the HIA process and how HIA can be incorporated into its decision-support tools, actions, and mission.
On this page:
- Springfield, MA
- Atlanta, GA
- Suffolk County, NY
- Rockford, IL
HIA Gerena School Renovation Project (Springfield, MA)
- Gerena School HIA Final Report
Gerena Community School, located in Springfield, MA, is undergoing renovations to improve the environmental conditions for its users. The facility functions as an elementary school and community center, serving students and residents of the North End Community. EPA collaborated with stakeholders, including departments within the City of Springfield and community-based groups, to perform an HIA.
The purpose of this HIA is to provide valuable health-focused information to help the City of Springfield narrow down and prioritize those renovation actions that best address the existing environmental conditions and reduce the potential negative health impacts to students, faculty, staff, and community members who use the facility. The HIA also provided an avenue for the community and other stakeholders to be engaged in the decision-making process. Community stakeholders have raised concerns related to Gerena School, which include indoor air quality issues related to motor vehicle emissions, flooding, moisture, mold, and other indoor environment conditions; negative perceptions of the school facilities among the community; differing priorities between school and city administrators; absenteeism; and classroom noise.
The HIA utilized on-site observations, reviewed evidence, and professional expertise to judge each of the proposed renovation options for potential impacts to respiratory health, classroom acoustics, and community perception. Based on the predicted impacts to health, the HIA provided recommendations for renovation actions that aim to maximize potential benefits to health and mitigate and/or avoid potential adverse impacts to health.
HIA Proctor Creek Boone Boulevard Green Street Project (Atlanta, GA)
- Proctor Creek Boone Boulevard Fact Sheet
- Proctor Creek Boone Boulevard HIA Executive Summary
- Proctor Creek Boone Boulevard HIA Final Report
Proctor Creek is one of the most impaired creeks in metro-Atlanta and has been placed on the impaired waters list because it does not meet state water quality standards for fecal coliform. The topography, prevalence of impervious surfaces in the watershed, and a strained combined sewer system have contributed to pervasive flooding in the Proctor Creek community and created environmental, public health, economic, and redevelopment issues. A green infrastructure project, aimed at supporting water quality and revitalization improvement efforts, was proposed in a headwater community of Proctor Creek.
The purpose of this HIA was to help inform the City of Atlanta’s decision on whether to implement the proposed project as designed and to provide an avenue for stakeholders, including state environmental and public health agencies, city and county departments, advocacy groups, and the community, to be engaged in the decision-making process. The HIA evaluated the proposed Boone Boulevard Green Street Project for its potential to impact twelve determinants of health identified by stakeholders ‒ water quality; flood management; climate and temperature; air quality; traffic safety; exposure to greenness; urban noise; access to goods, services, greenspace, and healthcare; crime; social capital; household economics, and community economics.
The results of the HIA suggested that the proposed green infrastructure project would have a positive impact on health overall and provided recommendations for implementation and expansion of green infrastructure projects throughout the watershed. The City of Atlanta is implementing the Boone Boulevard Green Street Project and has decided to expand the length of the green street to maximize its predicted health benefits.
HIA Proposed Code Changes Regarding Individual Sewerage Systems (Suffolk County, NY)
- Fact Sheet for Suffolk County HIA
- Suffolk County HIA Summary Report
- Suffolk County HIA Final Report
As part of the Hurricane Sandy recovery efforts, EPA conducted an HIA to evaluate potential beneficial and adverse health impacts that may result from proposed sanitary code changes regarding individual sewerage systems (ISS) for residential properties in Suffolk County, New York. ISS are an alternative to centralized municipal sewage disposal systems and are the primary mode of sewage disposal for residential properties in the county. The Suffolk County Government proposed the sanitary code changes to address a growing issue of nutrient loading to Suffolk County soil, surface waters, and ground waters. Overloading of nutrients, particularly nitrogen, has been linked to the impairment of surface and ground waters, beach closures, shellfish population die offs, harmful algal blooms, and damage to marine coastlines. Suffolk County agreed to host an HIA, guided by the EPA, to help inform the decision about the code changes. Based on input from stakeholders, community members, and scientific experts, pathways were identified through which the proposed code changes might impact health. Five pathways were prioritized for inclusion in the HIA analysis: individual sewerage system performance and failure; water quality; community and household economics; vector control; and resiliency to natural disaster. This HIA provided evidence-based recommendations to maximize potential benefits and mitigate potential adverse impacts to health that could result from the decision.
- Learn more about the HIA Suffolk County Report .
HIA Former Chesapeake Supply Brownfield Revitalization Assessment (Dover, Delaware)
- Fact Sheet for Dover, Delaware Rapid HIA
- Dover, Delaware Rapid HIA Report
From summer 2017 until early 2018, EPA conducted a rapid Health Impact Assessment (HIA) with the City of Dover and Kent County, Delaware to help the City and County make decisions concerning the redevelopment of a downtown Dover property. This property is a brownfield site – a formerly contaminated property – that has been cleaned up. The City and County are interested in using the property to produce food, including fresh produce and fish. This would help stimulate economic development and increase access to food in downtown Dover.
EPA assisted local and state officials with investigating a plan to use the site to produce food, including the use of aquaponics. Aquaponics is a farming system that grows plants and fish together in a way that benefits them both. To help with the effort, an abbreviated form of HIA (i.e., rapid HIA) was developed with EPA staff along with partners from City of Dover, Kent County, the State of Delaware, U.S. Department of Agriculture, and Delaware State University.
HIA Kingsbury Bay-Grassy Point Habitat Restoration Project (Duluth, MN)
- Helping Preserve and Promote the Cultural Significance of Kingsbury Bay and Grassy Point (Science Matters Publication)
- Kingsbury Bay-Grassy Point Habitat Restoration Project: A health impact assessment (Overview)
- Kingsbury Bay-Grassy Point HIA Fact Sheet (pdf) (335.9 KB)
- Kingsbury Bay-Grassy Point HIA Report (pdf) (22.2 MB)
- Kingsbury Bay-Grassy Point HIA Summary Report (pdf) (8.4 MB)
EPA conducted an HIA in the St. Louis River Areas of Concern (AOC) to examine the potential public health impacts of habitat restoration work and subsequent park improvement projects at two project sites along the St. Louis River – Kingsbury Bay and Grassy Point. The purpose of the HIA was to inform the Minnesota Department of Natural Resources (MNDNR) and City of Duluth’s decisions regarding the design and implementation of these habitat restoration and park improvement projects. Based on input from stakeholders, community members, and scientific experts, pathways were identified through which the proposed projects could potentially impact health. Seven pathways were prioritized for inclusion in the HIA analysis: water quality and habitat; equipment operation, traffic, and transport; air quality; noise and light pollution; crime and safety; recreation, aesthetics, and engagement with nature; and social/cultural aspects.
In examining these pathways, the HIA specifically evaluated the potential health impacts associated with changes in ecosystem services (i.e., benefits people obtain from these ecosystems) and other determinants of health, as a result of the planned sediment remediation, wetland and riparian habitat restoration, and construction of potential waterfront amenities, including trails, boardwalks, bird watching stations, fishing piers, kayak launches, and swimming beaches. The HIA will help inform the decisions regarding habitat restoration and park improvements at these two sites and provide recommendations to maximize potential benefits and mitigate potential adverse impacts to health that may result from the decisions.
Southwest Rockford Revitalization Rapid Health Impact Assessment (Rockford, IL)
- Southwest Rockford Revitalization Rapid Health Impact Assessment (Rockford, Illinois)
Brownfields and Land Revitalization

Brownfields are properties, the expansion, redevelopment, or reuse of which may be complicated by the presence or potential presence of a hazardous substance, pollutant, or contaminant (EPA, 2020a).
The City of Rockford, Illinois was seeking to revitalize the area around South Main Street in southwest Rockford (hereafter referred to as the South Main Corridor Area), along with other areas of the city, as part of its 2020-2024 Neighborhood Revitalization Area Strategy. The City received technical assistance from the EPA Office of Brownfields and Land Revitalization (OBLR) to design a Neighborhood Revitalization Strategy for the South Main Corridor Area.
In combination with the technical assistance contract, city officials agreed to a Health Impact Assessment (HIA), which would assess the health‐relevant social, environmental, and economic conditions in the South Main Corridor Area and identify how neighborhood revitalization could potentially impact health. A rapid HIA, an abbreviated form of HIA, was undertaken by the EPA Office of Research and Development (ORD) in partnership with EPA Office of Brownfields and Land Revitalization (OBLR), with input from EPA Region 5, the City of Rockford, and the Land Revitalization Technical Assistance Contractor.
A mixed methods approach was used in the HIA, including qualitative and quantitative data analysis, geographic information system (GIS) mapping, scientific literature review, and analysis of stakeholder input from multiple efforts that have taken place in the area, to evaluate the potential health impacts of proposed neighborhood revitalization in the South Main Corridor Area.
The HIA did not assess a specific revitalization strategy, program, policy, or decision, as one was not available at the time of the HIA, but rather examined evidence and examples of revitalization concepts being proposed for the South Main Corridor Area and their associations with public health impacts, positive and negative, with a particular emphasis on mental health and social determinants of health. The HIA examined six determinants of health: Housing, Neighborhood and Built Environment, Parks and Greenspace, Crime and Safety, Employment and Economy, and Social and Cultural Well-being.
The assessment identified the existing conditions in the study area related to these determinants of health, took into account community concerns and desires expressed in the City’s public meetings and interviews conducted as part of the Land Revitalization Technical Assistance Contract, and identified how neighborhood revitalization could potentially impact these health determinants and ultimately, human health. The HIA recommended strategies to maximize the potential health benefits and mitigate the potential adverse health impacts of neighborhood revitalization in the South Main Corridor.
- Health Research Home
- Children's Environmental Health Research
- Community Public Health
- Cumulative Impacts Research
- Funding, Resources, & Partnerships
- Health & the Environment
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 18 July 2023
Climate change and health: three grand challenges
- Diarmid Campbell-Lendrum ORCID: orcid.org/0000-0002-2503-7059 1 ,
- Tara Neville 1 ,
- Christian Schweizer 1 &
- Maria Neira 1
Nature Medicine volume 29 , pages 1631–1638 ( 2023 ) Cite this article
19k Accesses
24 Citations
239 Altmetric
Metrics details
- Public health
- Risk factors
Climate change may be the greatest health threat of the twenty-first century, impacting lives both directly and indirectly, through undermining the environmental and social determinants of health. Rapid action to decarbonize economies and build resilience is justified on health, human rights, environmental and economic grounds. While the necessary health response is wide ranging, it can largely be encapsulated within three grand challenges: (i) promote actions that both reduce carbon emissions and improve health; (ii) build better, more climate-resilient and low-carbon health systems; and (iii) implement public health measures to protect from the range of climate risks to health. The health community can make a unique and powerful contribution, applying its trusted voice to climate leadership and advocacy, providing evidence for action, taking responsibility for climate resilience and decarbonization of healthcare systems, and guiding other sectors whose actions impact substantially on health, carbon emissions and climate resilience.
You have full access to this article via your institution.
Similar content being viewed by others

The human right to climate adaptation
Climate change affects multiple dimensions of well-being through impacts, information and policy responses

A systematic global stocktake of evidence on human adaptation to climate change
The world is warming at a faster rate than at any time in human history, due mainly to the burning of fossil fuels—with an important additional contribution through land-use changes, mainly for agriculture and forestry. Unless urgent action is taken to cut carbon emissions, global warming will soon exceed the 1.5 °C limit set in the Paris climate agreement, and current trends are likely to result in over 3 °C of warming by the end of the century 1 .
Climate change has been identified as potentially the greatest health challenge of the twenty-first century 2 , 3 . It is bringing more deadly extreme heat and wildfires, increasing noncommunicable diseases and facilitating the emergence and spread of infectious diseases, contributing to health emergencies. It is impacting the health workforce and infrastructure, reducing capacity to provide universal health coverage. More fundamentally, climate shocks and growing stresses such as droughts and rising sea levels are undermining the environmental and social determinants of physical and mental health, from clean air and water, to sustainable food systems, to livelihoods—and threatening the existence of some nations 1 . Further delay in action will increase the risks, undermine decades of improvements in global health and contravene our collective commitments to ensure the human right to health for all 4 .
The same development pathways and economic choices that are driving the climate crisis are also directly causing large health impacts. These include polluting energy systems that the World Health Organization (WHO) estimates to cause almost 7 million premature deaths from air pollution each year 5 ; environmentally destructive and unhealthy food systems that are contributing to the global increase in noncommunicable disease; and urban planning and transport systems that result in car dependency—contributing to the burdens of physical inactivity and road traffic injuries. The healthcare sector itself is now also a notable contributor to climate change, responsible for almost 5% of global carbon emissions 6 , 7 .
The world is not yet responding to the scale of this challenge. Although the ‘right to health’ is at the core of the United Nations Framework Convention on Climate Change (UNFCCC) and the Paris Agreement, it is largely absent from its operational mechanisms. Less than 0.5% of international climate finance is currently allocated to health projects 8 , and only 30% of nationally determined contributions to the Paris Agreement take account of the large health gains expected from climate change mitigation 9 . Similarly, while health is routinely identified as a top priority for climate action, 70% of countries lack adequate finance to implement a national adaptation plan (NAP) for health, and few national or international health actors allocate meaningful resources to climate action 10 .
As part of their latest annual health monitoring report for the sustainable development goals 11 , the WHO have identified key objectives for the health response to climate change. In line with this, we outline the main connections between climate change and health and summarize three ‘grand challenges’ to protect and promote health in the face of climate change. In addition, we discuss the specific roles of the health community in responding to these challenges and driving change within and beyond the health sector.
Current status of climate change impacts on health
The Sixth Assessment Report of the Intergovernmental Panel on Climate Change estimates that up to 3.6 billion people are living in conditions that are highly vulnerable to the impacts of climate change 12 . Low-income and lower-middle-income countries and Small Island Developing States face the greatest health consequences of climate change, despite contributing the least to historical global emissions 8 , 12 . It is estimated that over the past decade, the mortality rate from extreme weather events was 15 times higher for populations in highly vulnerable regions than in regions with the lowest vulnerability 12 . Within-country disparities also exist; those living in poverty, older people, women, children, indigenous peoples, outdoor workers, the socially isolated and individuals with preexisting medical conditions are typically at highest risk 12 .
The WHO estimates that approximately 2 billion people lack access to safe drinking water 13 . Furthermore, there are about 600 million global cases of foodborne illnesses each year and children under the age of 5 years carry 30% of the burden of foodborne deaths (or 125,000 child deaths every year) 14 . Extreme weather events and climate-related environmental stressors degrade water and soil safety, thereby increasing the risks of waterborne and foodborne illnesses.
In 2020, about 770 million people in the world faced hunger, primarily in Africa and Asia—with women and children at particularly high risk 15 . Higher temperatures, rising sea levels and flooding affect all aspects of food and nutrition security. Consequently, climate-related reductions in agricultural and marine productivity, biodiversity loss, volatility in food prices and disruptions in food imports further impact the quality, quantity and diversity of food consumed, leading to food and nutrition crises.
Changing temperature and precipitation patterns also create conditions that facilitate the transmission of mosquito-borne, tick-borne and rodent-borne diseases in many regions 12 . If prevention methods are not strengthened, this could lead to an increase in deaths from vector-borne diseases (already at over 700,000 each year) 16 .
The health risks of climate change can have both immediate and long-term consequences. Extreme weather events can lead to acute mental health conditions such as anxiety, depression and post-traumatic stress. The cumulative effect of loss of livelihood, displacement, disrupted social cohesion and uncertainty from climate change can also result in longer-term mental health disorders 17 .
Research is ongoing to quantify the current and projected future health effects of climate change. A recent study of 43 countries estimated that 37% of heat-related deaths are attributable to human-induced climate change 18 , and the 2022 Lancet Countdown on Climate Change and Health Report found that heat-related mortality of people older than 65 years increased by almost 70% over the past two decades 7 . The same report estimates 98 million more people reporting moderate-to-severe food insecurity in 2020 than the average in 1981–2010, due to climate change 7 . Advances in the application of detection and attribution studies to health outcomes are also providing greater insight and confidence regarding the magnitude of climate change-related health impacts of extreme weather events 19 .
Providing a single estimate of the overall health burden of climate change is challenging. The WHO has published conservative projections estimating the effect of climate change only on malaria, heat exposure in older people, diarrheal disease in children, undernutrition in children and coastal flood mortality, for the 2030s and 2050s. For example, under a medium-to-high emissions scenario, it was estimated that climate change would cause approximately 250,000 additional deaths per year by the 2030s 20 . While the WHO assessments established that climate change was already having a substantial adverse impact on human health, which was projected to increase into the future, they recognized the inability of existing models to account for major causal pathways for which no reliable quantitative models exist, or that impact a wide range of health outcomes or that may have compounding effects with other health risks. Examples include persistent drought, migration pressures and risk of conflict. Further methodological work is needed to either improve quantitative models or develop alternative assessment approaches to capture these important risks.
The fact that poorer communities tend to have relatively lower carbon emissions, but higher health vulnerabilities to climate change, highlights the need for specific consideration of equity in designing the public health response. A just and equitable response requires that those with both the largest responsibility for carbon emissions, and the greatest means, should bear the largest part of any costs of climate change mitigation and adaptation, and that public measures should be explicitly designed to promote health equity, for example, by prioritizing particularly vulnerable groups.
Three grand challenges for health and climate action
Climate change presents a fundamental threat to human health. It affects the physical environment as well as all aspects of both natural and human systems—including social and economic conditions and the functioning of health systems. It is therefore a ‘threat multiplier’, undermining and potentially reversing decades of health progress.
We identify three ‘grand challenges’ to address the threat of climate change to health.
Promote actions that both reduce carbon emissions and improve health
To stay within the 1.5 °C global warming limit set out in the 2015 Paris Agreement and avoid escalating and intolerable impacts on human health and well-being, the world will need to drastically reduce carbon emissions.
While efforts to achieve this goal are often discussed in terms of paying higher economic costs to protect the global climate, evidence now shows that the global transformation to clean energy would pay for itself through reduced energy costs in as little as 6 years 21 . This transformation would also bring more and better jobs, and greatly improve health 22 . Valuing these societal benefits is estimated to bring the payback time to less than 1 year 21 .
Health has a strong influence on estimates of the benefits of climate action, as the development pathways that are driving climate change also have very large negative effects on human health. Notably, the sectors driving greenhouse gas emissions—including energy, transport, industry, agriculture and waste—are also sources of harmful air pollutants, which increase mortality from cardiovascular disease, respiratory illnesses and cancer 23 . The air quality improvements that would accompany compliance with the Paris Agreement would therefore avoid millions of premature deaths every year by 2050, bringing economic benefits that would equal or exceed the mitigation costs 24 , 25 .
These benefits can also be estimated at the national level, and in relation to specific policies. A 2021 WHO study modeled the health benefits of adjusting Pakistan’s nationally determined contribution to the UNFCCC under the Paris Agreement. The study found that under a high-ambition scenario, Pakistan could reduce greenhouse gas emissions by approximately 27.5% by 2030, compared to a reference case scenario. The accompanying air quality improvements could prevent more than 65,000 annual premature air pollution-related deaths by the same year, with associated annual economic benefits estimated to be about 9 billion USD 26 .
Solutions exist to cut carbon emissions across all sectors 22 and would bring a range of large health gains beyond air quality alone. For example, road transport is estimated to account for almost one-fifth of global CO 2 emissions, while the global food system is responsible for between 21% and 37% of greenhouse gas emissions 27 . Sustainable urban planning that promotes a shift toward safe walking and cycling as well as access to public transport can lead to health benefits from increased physical activity, reduced ambient air pollution and lower noise exposure 28 . In high-income countries, a transition toward plant-based diets, lower red meat consumption and less food waste could help to mitigate climate change while lowering the health burden of diet-related noncommunicable diseases 27 . In low-income and middle-income countries, sustainable agriculture and food production can protect local environments, reduce emissions and promote food and nutrition security 15 .
In support of this, a study of nine countries with high greenhouse gas emissions found that, if these countries followed a sustainable pathway scenario consistent with the goals of the Paris Agreement, this would be expected to bring a total annual reduction of 1.18 million air pollution-related deaths, 5.86 million diet-related deaths and 1.15 million deaths due to physical inactivity by 2040 (ref. 24 ).
The fact that many actions that would reduce carbon emissions would also bring large health benefits has two major implications. Firstly, health should be central to policies in all of these sectors, and in national and international climate policy. Under the Paris Agreement, countries set out their mitigation commitments and adaptation priorities through their nationally determined contributions and NAPs. The 2023 WHO Review of Health in the Nationally Determined Contributions report found that over 90% of countries reflect health priorities in this context 9 . This ensures that health considerations have at least an entry point in national and international climate plans and processes, to be delivered through specific policy measures.
Secondly, health actors should work to identify and accelerate those climate change mitigation actions that bring the greatest health gains, helping to galvanize political and financial support for accelerated climate action, and sustainable development overall. These include a just and inclusive transition to renewable energy, phasing out coal combustion and inefficient fossil fuel subsidies, promoting sustainable and healthy urban transport systems and housing, and sustainable and healthy food systems and diets 4 .
Build better, more resilient and environmentally sustainable health systems
Building climate-resilient and sustainable health systems involves a systematic and comprehensive approach to strengthening all core functions of a health system so it can respond and adapt to the health risks of climate change 29 . This coincides with increased political momentum to transform the provision of universal health coverage in the face of increasing demand and rising costs, with a revitalization of primary healthcare, bringing health services closer to people and communities 30 .
To meet even basic levels of healthcare provision, services including clean energy, water and sanitation, waste management, essential medical equipment and a trained health workforce are essential. To ensure economic and environmental sustainability, this transformation should also support the shift toward a circular economy in health (and in society generally), through rethinking models of care—including optimizing the use of telemedicine, minimizing consumption and wastage and making more sustainable purchasing decisions. All of the above can cut operational costs, reduce losses from climate hazards and increase quality of care—enhancing universal health coverage and primary healthcare. The overall goal for health systems should be to improve delivery of high-quality health services to all, minimize carbon emissions from healthcare, and enhance resilience of health systems to climate and other shocks (Fig. 1 ).
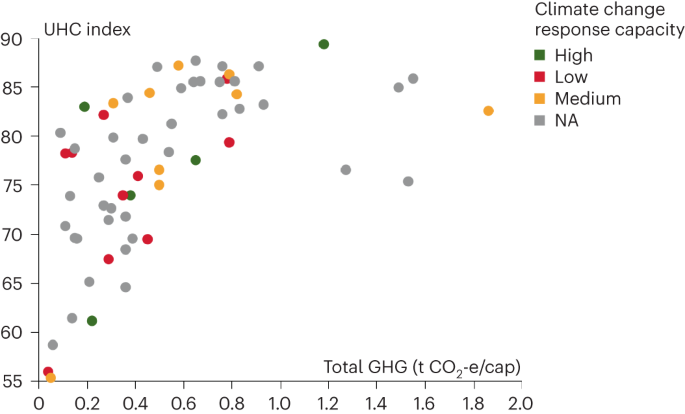
For each country (circle), the graph shows WHO Universal Health Coverage (UHC) Index score (vertical axis), versus estimated carbon emissions from healthcare (in annual tonnes of carbon dioxide equivalent per capita; horizontal axis). Circles are colored by score on an aggregate index of actions taken to build health system resilience to climate change, as measured by the WHO Health and Climate Change Survey Report 10 . The pattern that emerges is one of large differences in all dimensions. Some countries with currently very high health sector carbon emissions need to urgently reduce emissions without sacrificing health performance, while others with currently low health sector carbon emissions need to focus on increasing their health systems performance in a way that ensures a low-carbon future with health equity 45 . Figure adapted from ref. 45 . GHG, greenhouse gas; NA, data not available.
While the health sector is responsible for almost 5% of global greenhouse gas emissions, this contribution is as high as 10% in some high-income nations 6 , 7 , 31 . Health systems can decarbonize through measures such as more efficient or renewable energy sources, as well as through optimizing the use of resources, sustainable procurement practices and waste reduction—as over 70% of carbon emissions from healthcare come from the supply chain. Implementing these measures can bring multiple health system benefits by contributing to a higher quality of care, greater accessibility, more reliable services, reduced occupational hazards from air pollution and waste and reduced costs 31 , 32 .
In particular, health systems in all countries can benefit from the transition to renewable energy which, over the medium term to long term is now cheaper and more reliable than fossil fuel sources and generally well suited to health facilities—especially in remote, off-grid settings. The greatest opportunities for improvement are likely to be in poorly served populations. For example, over 50% of health facilities in some countries in sub-Saharan Africa lack core environmental services including energy, water and sanitation, and many lack any safe management of healthcare waste 33 , 34 . Investments in these settings can allow countries to ‘leapfrog’ directly to better, cheaper, and more resilient services.
In addition, in countries across the entire range of economic development, vulnerabilities in infrastructure, management practices and human resources make health systems vulnerable to climate extremes (such as heatwaves, high winds, dust storms and floods) as well as longer-term threats ranging from persistent droughts and sea level rise, to the spread of infectious diseases to areas that currently lack the public health capacities to address them. This makes it essential to improve the ability to detect, prepare for, respond to and recover from both short-term shocks and long-term stresses.
Increasing climate resilience and controlling carbon emissions in health systems should not result in separate, parallel structures. Instead, it should seek to reinforce and build on existing functions. The 2015 WHO Operational Framework for Building Climate Resilient Health Systems 29 builds on the six core building blocks of health systems (leadership, workforce, information systems, technology, service delivery and finance), and describes how specific actions to build climate resilience can be added to each of these. The framework is now being updated to include complementary actions to control carbon emissions (Fig. 2 ).
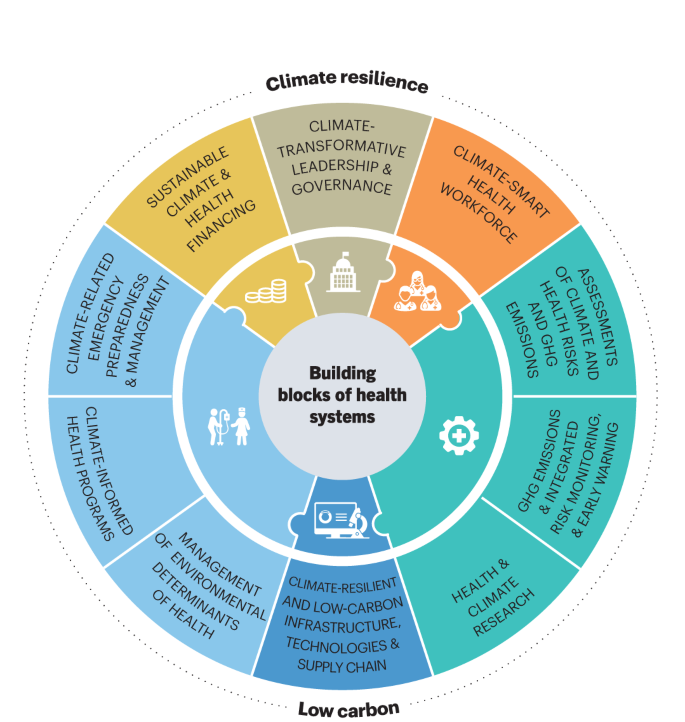
The health system response to climate change should build on the core ‘building blocks’ of health systems: leadership, workforce, information systems, infrastructure and technologies, service delivery and finance (inner ring); adding additional functionality and capacity specifically to build resilience to climate shocks and stresses, while minimizing carbon emissions (outer ring) 45 . Figure adapted from ref. 45 .
Implement public health measures to protect from the range of climate risks to health
The diverse risks that climate change presents to health, many acting through long causal pathways, require action not only within healthcare (that is, curative services), but also on public health functions, including on the environmental and social determinants of health.
The essential first step is to understand the scale and nature of health vulnerabilities to climate variability and change, taking account of important determinants including geography and socioeconomic condition, and considering differential impacts on subpopulations—typically in the form of a climate change and health vulnerability and adaptation assessment. This informs the development of evidence-based NAPs and interventions, most commonly in the form of a health national adaptation plan (HNAP) aligned with the whole-of-government NAP.
Many countries have made substantial progress on assessment and planning in recent years. The 2021 WHO Health and Climate Change Global Survey found that approximately half of all countries surveyed (48 out of 95) reported having conducted a climate change and health vulnerability and adaptation assessment, while 52% (49 out of 95) reported having a national climate change and health strategy in place 10 .
HNAPs generally include intervention measures that are shown to protect against current weather and climate hazards, and that can therefore be expected to provide some level of protection against long-term climate change 35 , 36 . These vary, but typically include three common features. First, implementation of climate-informed surveillance and response systems for key risks, such as extreme heat, infectious disease, and food and nutrition security to improve lead times and accuracy of health early warning systems, and to project the longer-term effects of climate variability and change. Second, integration of climate risk into key ‘vertical’ health programs, targeting a specific disease or population group 35 . This includes emergency preparedness and response, infectious disease control, mental health and programs focusing on groups with particular vulnerabilities to climate risks, such as occupational health, maternal, newborn and child health, climate migrant health and healthy aging. Third, supporting resilience and adaptation in ‘health-determining’ sectors, and within communities 35 . Approximately 25% of the current global burden of disease is attributable to environmental risks—largely determined by decisions outside of health systems 23 . The greatest health gains, and protection from climate risks, may therefore be achieved through collaboration with other sectors, and some HNAPs also include integration of climate resilience into water and sanitation service provision, the built environment, food and nutrition security programs and through supporting community-based health adaptation.
Despite progress on assessment and planning, only a quarter of countries responding in the WHO global survey (11 out of 46) have reached a ‘high’ or ‘very high’ level of implementation. Insufficient finance was a main barrier to implementation of national strategies and plans 10 (Fig. 3 ). In addition to an overall scarcity of resources, action on climate change and health faces an additional financial barrier. While most governments and development agencies identify both health and climate change as top priorities, they generally do so separately, rather than via integrated and mutually reinforcing goals. Meaningful progress on implementation will only come with clear mandates and proportionate resources dedicated specifically to the intersection of climate change and health.
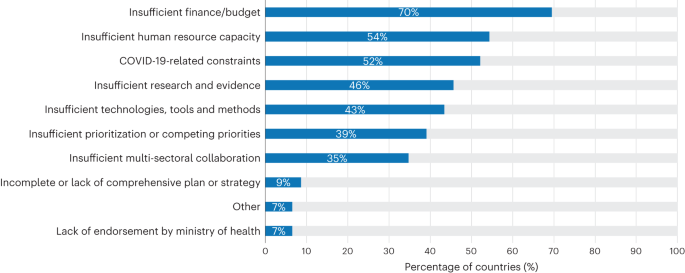
Data from the WHO Climate and Health Country Survey 10 ; 46 country respondents, multiple responses possible.
Ultimately, tackling climate change and protecting health will require effective monitoring and continuous learning and improvement. The interaction between climate change, other environmental and social determinants of health, health interventions and health effects, is constantly evolving. This calls for integrated monitoring systems across these dimensions to improve understanding, track progress and guide health actions.
The unique role of the health community in delivering transformative change
The climate crisis requires transformative action from across society. However, the health community—including frontline health workers, Ministries of Health, intergovernmental and nongovernmental health organizations and health academics—has a unique role to play.
We outline three key functions for the health community in responding to the climate crisis.
Leadership and advocacy
There is increasingly strong evidence from experimental studies from around the world that presenting a positive vision of a healthier, more environmentally sustainable common future, is effective in ensuring public support for climate action, and cutting across political divides 37 , 38 , 39 , 40 .
Health researchers have assembled a large body of evidence on the health benefits of climate action—and the overwhelmingly negative health consequences of inaction. Health is also central to key regulations and legislation, from air quality and emissions standards, to food standards, to protection of the right to health under national and international law and conventions 41 . Health institutions should therefore build not only the applied evidence base, but also their own individual and institutional capacity to engage more directly in policymaking.
At the same time, health professionals are increasingly engaged on climate change in a range of roles, from actions to reduce carbon emissions in their professional work, to organized expressions of support for stronger international climate action ( https://healthyclimateletter.net/ ), to a spectrum of public engagement and nonviolent protests to protect their patients from the impacts of climate change and related threats including air pollution. The large number of health professionals, their direct personal connection to individuals and communities, and their position among the most trusted professions in the world 42 , mean that they have the potential to be among the most powerful advocates for a healthy future through climate action (Box 1 ).
Box 1 Opportunities for the health community to influence climate and health policy
The most direct point of influence is within healthcare settings. Health professionals are increasingly engaged in staff-led and system-wide initiatives to reduce the climate impact of healthcare and extending that role to use their expertise and public trust to advocate for wider societal actions to protect health from climate change.
National and local government health agencies have an important role in leading public health actions to protect from climate risks, providing health assessments of the impacts of policies in key health-determining and carbon-emitting sectors, such as energy, transport, food systems and urban planning, and applying relevant health standards and regulations, for example, on air quality. Health actors should engage fully in relevant national and international climate mechanisms, such as the development of NAPs, and nationally determined contributions to the Paris Agreement. They also have a critical and currently neglected role in accessing climate finance for health, and mainstreaming climate mitigation and adaptation across health investments.
The rapid increase in the number and range of actors now engaging on climate change and health calls for a collective and coordinated effort. The Alliance for Transformative Action on Climate and Health ( https://www.who.int/initiatives/alliance-for-transformative-action-on-climate-and-health/ ), brings together over 65 countries that have committed to build climate-resilient and low-carbon health systems, together with health practitioners, development partners and technical experts in an open partnership to accelerate climate and health action.
Evidence and monitoring
Research on climate change and human health is a rapidly growing field, with the number of articles published each year surging more than sixfold over the past decade 43 . Despite the increase in volume, the research itself remains uneven. Most of the currently available studies are focused on assessing health impacts of climate change, with a particular emphasis on a subset of causal pathways—notably the direct health effects of excessive heat. There is a relative lack of research on other major questions on which health policymakers have expressed demand 44 —notably the effectiveness of health adaptation measures, the diverse range of potential health co-benefits of both adaptation and mitigation measures, the development of decision-support tools and economic assessments of the benefits and costs of climate and health actions. Research output is also highly unevenly distributed across geographical regions, with many more studies conducted in high-income countries compared to low-income and middle-income countries. Often, data are not available at a level of resolution that corresponds to decision-makers’ needs—that is, for national or subnational levels, or disaggregated by gender, age, ethnicity or socioeconomic status—to assess the differential effects of actions on different population groups. In addition, while much applied research focusses on improving capacity to protect populations from current climate risks, there is also a need for research that takes account of the specific characteristics of long-term climate change, including future projections of changes in various determinants of health, such as aging and urbanizing populations that are particularly vulnerable to extreme heat.
Similar considerations apply in the related fields of monitoring and progress tracking. There has been rapid progress in recent years through initiatives such as the triennial WHO Health and Climate Change Global Survey 10 and the annual Lancet countdown on health and climate change 7 . However, as the integrated field of climate change and health is a relatively new one, there are a range of issues that require further development. These include, among others, standards and indicators for climate-resilient health systems and low-carbon healthcare, and comprehensive and coherent indicator frameworks that connect the high-level sustainable development goals on climate change and health with exposures, vulnerabilities, health effects and progress in implementing climate and health interventions. There is also a need for further strengthening of platforms to make emerging evidence more widely accessible and more directly connected to policy, for example, through regional and national climate change observatories connected to policy institutions.
The urgency and existential threat of climate change calls for greater investment in climate and health research and demonstration projects, and implies that it should pursue a more demand-driven approach to evidence generation, involving decision-makers and affected populations as directly as possible. Such research should be focused on the need to limit global warming, protect and improve health, and ensure universal access to high-quality, climate-resilient, environmentally sustainable health services.
Implementation
Guided by its values and mandates, and informed by the available evidence, the health community can drive the necessary transformation through a range of functions: via direct responsibility for the formal healthcare sector, more broadly through public health functions into the wider community, and also in an advisory role capacity for other sectors that have a strong influence on health and climate change.
The most direct effect that health professionals can exert is through their individual and collective actions within their own work, to deliver improved, climate-resilient and low-carbon health systems. The early experience in this emerging field indicates that success factors include a strong legislative basis (for example, a legally binding climate act mandating emissions reductions across sectors), political leadership from senior management from within the health system, investment in analytical and technical support and networking capacity and, above all, the positive engagement and commitment of the health workforce.
The specific actions to be taken will depend on the professional role and institutional context, and particularly at this relatively early stage of the development of the field, will depend heavily on learning from and sharing experience. This is now being supported from the international level through a range of policy and technical guidance, including the WHO’s Conceptual and Operational Framework for Building Climate Resilient and Low Carbon Health Systems 45 , guidance on developing roadmaps for low-carbon healthcare 31 , 32 , as well as tools for assessing and managing carbon emissions 46 , 47 , 48 . It is also supported by new collaborative initiatives, notably the Alliance for Transformative Action on Climate and Health (Box 1 ).
Outside healthcare services, public health agencies have a critical role in strengthening and adapting disease prevention to the new challenges presented by climate change. In addition to assessing health vulnerabilities, developing NAPs for health and building capacity, this should also include implementing specific, high-priority interventions for health security. These could include surveillance and early warning systems for climate-sensitive health risks, as well as broader public health and health promotion functions to reduce harmful exposures and enhance the environmental and social determinants of health 49 .
The third role of the health community in implementation is more indirect but is potentially the most important—to guide policy in sectors other than health, which are driving carbon emissions, and therefore the climate crisis—by providing health analysis, the trusted voice of the health community, and health policy levers. This includes providing health assessments within national climate policies and nationally determined contributions to the UNFCCC, health guidance and impact assessments of policies within key sectors such as energy, transport and food systems, and promoting specific interventions that will bring both climate and health benefits, such as clean energy for households and healthcare facilities. It can also include actions such as behavior change communication around high emission practices, the application of warning labels and marketing restrictions, regulation to control health risks such as air pollution, and pricing mechanisms for products that harm health (which could potentially include fossil fuels).
Cutting across all of the implementation functions above is the issue of finance. While climate change is now recognized as one of the greatest global health threats, there are no dedicated multilateral or bilateral funding mechanisms of the kind that exist for some specific diseases (for example, AIDS, tuberculosis and malaria), health threats (for example, pandemics) or population groups (for example maternal, newborn and child health). There is therefore an important role for the health sector in facilitating simpler, faster and greater access to existing health and climate funding streams, assessing the scale of health impacts which cannot now be avoided and therefore should be supported through any ‘loss and damage’ funds, and proposing improvements in institutional and financial mechanisms for a scale up of investment.
Climate change is already having major negative impacts on public health, and these are increasing rapidly. The societal changes required to stabilize the global climate will entail initial financial cost, but this is outweighed by the health benefits that are projected to result—even before considering the rapid economic payback time—and the fundamental benefit of maintaining the environmental conditions in which humans can survive and thrive.
The range of threats that climate change presents to health is large, diverse and complex, presenting major challenges to health systems, and to the global health architecture, which is largely supported by vertical programs to address individual diseases or health issues. A goal-driven approach to (i) promote actions that both reduce carbon emissions and improve health, (ii) build better, more resilient and environmentally sustainable health systems, and (iii) implement public health measures to protect from the range of climate risks to health, can help to structure and accelerate the health response to climate change.
The scale and scope of the health sector response needs to be commensurate with the size of the health threat. While much progress has been made, much more is still needed. The challenges to delivering this transformation are largely political rather than technical, and require both leadership and public support. The health community has a critical role to play—directly within the health sector by delivering improved services while reducing carbon emissions, as well as through their public health functions to safeguard and improve the environmental and social determinants of health, but also, crucially, through influencing other sectors. The most important role, however, is likely to be as leaders and advocates, changing the narrative from the threat of the climate crisis, to a positive and healthy future through climate action.
Intergovernmental Panel on Climate Change. in Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (eds. Masson-Delmotte, V. et al.) (Cambridge Univ. Press, 2021).
Chan, M. Climate change and health: preparing for unprecedented challenges. David E. Barmes Global Health Lecture. https://www.who.int/director-general/speeches/detail/climate-change-and-health-preparing-for-unprecedented-challenges (2007).
Costello, A. et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 373 , 1693–1733 (2009).
Article PubMed Google Scholar
World Health Organization. COP26 Special Report on Climate Change and Health: the Health Argument for Climate Action . https://apps.who.int/iris/handle/10665/346168 (2021).
Global Health Observatory. Air pollution data portal. https://www.who.int/data/gho/data/themes/air-pollution?lang=en
Health Care Without Harm & ARUP. Health Care Climate Footprint Report https://noharm-global.org/documents/health-care-climate-footprint-report (2019).
Romanello, M. et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet 400 , 1619–1654 (2022).
World Health Organization. C OP24 Special Report: Health and Climate Change . https://apps.who.int/iris/handle/10665/276405 (2018).
World Health Organization. WHO Review of Health in the Nationally Determined contributions (NDCs) (in the press).
World Health Organization. 2021 WHO Health and Climate Change Survey Report . https://apps.who.int/iris/handle/10665/348068 (2021).
World Health Organization. World Health Statistics 2023: Monitoring Health for the SDGs, Sustainable Development Goals . https://apps.who.int/iris/handle/10665/367912 (2023).
Intergovernmental Panel on Climate Change. Summary for Policymakers. in Climate Change 2022: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (eds. Pörtner, H.-O. et al.) 3–33 (Cambridge Univ. Press, 2022).
WHO, UNICEF & World Bank. State of the World’s Drinking Water: an Urgent Call to Action to Accelerate Progress on Ensuring Safe Drinking Water for All . https://apps.who.int/iris/handle/10665/363704 (2022).
World Health Organization. Estimating the burden of foodborne diseases. https://www.who.int/activities/estimating-the-burden-of-foodborne-diseases
FAO, IFAD, UNICEF, WFP & WHO. The State of Food Security and Nutrition in the World 2021: Transforming Food Systems for Food Security, Improved Nutrition and Affordable Healthy Diets for All . https://www.fao.org/documents/card/en/c/cb4474en . https://doi.org/10.4060/cb4474en (2021).
World Health Organization. Vector-borne diseases. https://www.who.int/news-room/fact-sheets/detail/vector-borne-diseases (2020).
Corvalan, C. et al. Mental health and the global climate crisis. Epidemiol. Psychiatr. Sci. 31 , e86 (2022).
Article PubMed PubMed Central Google Scholar
Vicedo-Cabrera, A. M. et al. The burden of heat-related mortality attributable to recent human-induced climate change. Nat. Clim. Chang. 11 , 492–500 (2021).
Article CAS PubMed PubMed Central Google Scholar
Ebi, K. L. et al. Using detection and attribution to quantify how climate change is affecting health. Health Affairs 39 , 2168–2174 (2020).
World Health Organization. Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death , 2030s and 2050s . https://apps.who.int/iris/handle/10665/134014 (2014).
Jacobson, M. Z. et al. Low-cost solutions to global warming, air pollution, and energy insecurity for 145 countries. Energy Environ. Sci. 15 , 3343–3359 (2022).
Article Google Scholar
Intergovernmental Panel on Climate Change. in Climate Change 2022: Mitigation of Climate Change. Contribution of Working Group III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (eds. Shukla, P. R. et al.) (Cambridge Univ.Press, 2022).
Prüss-Üstün, A., Wolf, J., Corvalán, C. F., Bos, R. & Neira, M. P. Preventing Disease through Healthy Environments: a Global Assessment of the Burden of Disease from Environmental Risks . https://apps.who.int/iris/handle/10665/204585 (2016).
Hamilton, I. et al. The public health implications of the Paris Agreement: a modelling study. Lancet Planet. Health 5 , e74–e83 (2021).
Markandya, A. et al. Health co-benefits from air pollution and mitigation costs of the Paris Agreement: a modelling study. Lancet Planet. Health 2 , e126–e133 (2018).
World Health Organization. Health Benefits of Raising Ambition in Pakistan’s Nationally Determined Contribution: WHO Technical Report . https://apps.who.int/iris/handle/10665/347767 (2021).
Romanello, M. et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet 398 , 1619–1662 (2021).
World Health Organization. Walking and Cycling: Latest Evidence to Support Policy-making and Practice . https://apps.who.int/iris/handle/10665/354589 (2022).
World Health Organization. Operational Framework for Building Climate Resilient Health Systems . https://apps.who.int/iris/handle/10665/189951 (2015).
World Health Organization. Declaration of Astana : Global Conference on Primary Health Care: Astana , Kazakhstan, 25 and 26 October 2018 . https://apps.who.int/iris/handle/10665/328123 (2019).
Health Care Without Harm. Global Road Map for Health Care Decarbonization: a navigational tool for achieving zero emissions with climate resilience and health equity. Health Care Climate Action https://healthcareclimateaction.org/roadmap (2020).
World Health Organization . WHO Guidance for Climate Resilient and Environmentally Sustainable Health Care Facilities . https://apps.who.int/iris/handle/10665/335909 (2020).
World Health Organization & United Nations Children’s Fund (UNICEF). Progress on WASH in Health Care Facilities 2000–2021: Special Focus on WASH and Infection Prevention and Control https://apps.who.int/iris/handle/10665/366657 (2023).
World Health Organization. Energizing Health: Accelerating Electricity Access in Health-care Facilities . https://apps.who.int/iris/handle/10665/365588 (2023).
World Health Organization. Quality Criteria for Health National Adaptation Plans . https://apps.who.int/iris/handle/10665/339454 (2021).
World Health Organization. WHO G uidance to Protect Health from Climate Change through Health Adaptation Planning . https://apps.who.int/iris/handle/10665/137383 (2014).
Kotcher, J., Maibach, E., Montoro, M. & Hassol, S. J. How Americans respond to information about global warming’s health impacts: evidence from a national survey experiment. GeoHealth 2 , 262–275 (2018).
Rossa-Roccor, V., Giang, A. & Kershaw, P. Framing climate change as a human health issue: enough to tip the scale in climate policy? Lancet Planet. Health 5 , e553–e559 (2021).
Dasandi, N. et al. Positive, global, and health or environment framing bolsters public support for climate policies. Commun. Earth Environ. 3 , 239 (2022).
Badullovich, N., Grant, W. J. & Colvin, R. M. Framing climate change for effective communication: a systematic map. Environ. Res. Lett. 15 , 123002 (2020).
United Nations General Assembly. The Human Right to a Clean, Healthy and Sustainable Environment . https://digitallibrary.un.org/record/3983329?ln=en (2022).
Clemence, M. & Boyon, N. Doctors and Scientists are seen as the World’s most Trustworthy Professions . https://www.ipsos.com/en/global-trustworthiness-index-2022 (2022).
World Health Organization. Climate Change and Health Research: Current Trends, Gaps and Perspectives for the Future . https://apps.who.int/iris/handle/10665/353062 (2021).
World Health Organization. World Health Assembly, 61. Climate Change and Health . https://apps.who.int/iris/handle/10665/23547 (2008).
World Health Organization. Conceptual and Operational Framework for Building Climate Resilient and Low Carbon Health Systems (in the press).
World Health Organization. Climate Change Mitigation, Air Quality and Health (CLIMAQ-H). https://www.who.int/europe/tools-and-toolkits/climate-change-mitigation--air-quality-and-health-(climaq-h)
World Health Organization. Health Economic Assessment Tool (HEAT) for Walking and Cycling. https://www.who.int/tools/heat-for-walking-and-cycling
World Health Organization. Benefits of Action to Reduce Household Air Pollution Tool (BAR-HAP). https://www.who.int/tools/benefits-of-action-to-reduce-household-air-pollution-tool
International Association of National Public Health Institutes. Roadmap for Action on Health and Climate Change: Engaging and supporting national public health institutes as key climate actors . https://ianphi.org/news/2021/roadmap-climate-change.html (2022).
Download references
Acknowledgements
The authors thank C. Corvalan, A. Sena, E. V. Prats and A. Savage for contributing graphics.
Author information
Authors and affiliations.
Department of Environment, Climate Change and Health, World Health Organization, Geneva, Switzerland
Diarmid Campbell-Lendrum, Tara Neville, Christian Schweizer & Maria Neira
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Diarmid Campbell-Lendrum .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Medicine thanks Kristie Ebi, Matthew Chersich and Sarah Whitmee for their contribution to the peer review of this work. Primary Handling Editor: Karen O’Leary, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Campbell-Lendrum, D., Neville, T., Schweizer, C. et al. Climate change and health: three grand challenges. Nat Med 29 , 1631–1638 (2023). https://doi.org/10.1038/s41591-023-02438-w
Download citation
Received : 08 May 2023
Accepted : 05 June 2023
Published : 18 July 2023
Issue Date : July 2023
DOI : https://doi.org/10.1038/s41591-023-02438-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
A who-led global strategy to control greenhouse gas emissions: a call for action.
- Matthew F Chersich
- Nicholas Brink
- Stanley Luchters
Globalization and Health (2024)
Impact of extreme weather events on healthcare utilization and mortality in the United States
- Renee N. Salas
- Laura G. Burke
- Ashish K. Jha
Nature Medicine (2024)
Building healthy populations
Nature Medicine (2023)
Spatiotemporal change of climate extremes under the projection of CMIP6 model analysis over Awash Basin, Ethiopia
- Mikhael G. Alemu
- Melsew A. Wubneh
- Fasikaw A. Zimale
Sustainable Water Resources Management (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Towards a paradigm shift in environmental health decision-making: a case study of oxybenzone
Affiliations.
- 1 Department of Environmental Health Sciences, School of Public Health and Health Sciences, University of Massachusetts - Amherst, 171C Goessmann, 686 N. Pleasant Street, Amherst, MA, 01003, USA.
- 2 Department of Environmental Health Sciences, School of Public Health and Health Sciences, University of Massachusetts - Amherst, 171C Goessmann, 686 N. Pleasant Street, Amherst, MA, 01003, USA. [email protected].
- PMID: 34998398
- PMCID: PMC8742442
- DOI: 10.1186/s12940-021-00806-y
Background: Technological advancements make lives safer and more convenient. Unfortunately, many of these advances come with costs to susceptible individuals and public health, the environment, and other species and ecosystems. Synthetic chemicals in consumer products represent a quintessential example of the complexity of both the benefits and burdens of modern living. How we navigate this complexity is a matter of a society's values and corresponding principles.
Objectives: We aimed to develop a series of ethical principles to guide decision-making within the landscape of environmental health, and then apply these principles to a specific environmental chemical, oxybenzone. Oxybenzone is a widely used ultraviolet (UV) filter added to personal care products and other consumer goods to prevent UV damage, but potentially poses harm to humans, wildlife, and ecosystems. It provides an excellent example of a chemical that is widely used for the alleged purpose of protecting human health and product safety, but with costs to human health and the environment that are often ignored by stakeholders.
Discussion: We propose six ethical principles to guide environmental health decision-making: principles of sustainability, beneficence, non-maleficence, justice, community, and precautionary substitution. We apply these principles to the case of oxybenzone to demonstrate the complex but imperative decision-making required if we are to address the limits of the biosphere's regenerative rates. We conclude that both ethical and practical considerations should be included in decisions about the commercial, pervasive application of synthetic compounds and that the current flawed practice of cost-benefit analysis be recognized for what it is: a technocratic approach to support corporate interests.
Keywords: Benzophenone 3; Conflicting interests; Endocrine disruptor; Externality; Intergenerational; Melanoma; Skin cancer; Sunscreen.
© 2021. The Author(s).
Publication types
- Research Support, N.I.H., Extramural
- Benzophenones*
- Environmental Health
- Social Justice
- Benzophenones
Grants and funding
- U01ES026140/ES/NIEHS NIH HHS/United States
- Open access
- Published: 31 July 2018
Delayed discovery, dissemination, and decisions on intervention in environmental health: a case study on immunotoxicity of perfluorinated alkylate substances
- Philippe Grandjean ORCID: orcid.org/0000-0003-4046-9658 1 , 2
Environmental Health volume 17 , Article number: 62 ( 2018 ) Cite this article
12k Accesses
59 Citations
640 Altmetric
Metrics details
Identification and characterization of environmental hazards that impact human health must rely on the best possible science to inform and inspire appropriate public health intervention. The perfluorinated alkylate substances (PFASs) are persistent emerging pollutants that are now being recognized as important human health hazards. Although the PFASs have been produced for over 60 years, academic research on environmental health aspects has appeared only in the most recent 10 years or so. In the meantime, these persistent chemicals accumulated in the global environment. Some early studies e.g., on population exposures and toxicity, were not released to the public until after year 2000. Still, the first PFAS risk assessments ignored these reports and relied on scant journal publications. The first guidelines and legal limits for PFAS exposure, e.g., from drinking water, were proposed 10 years ago. They have decreased substantially since then, but remain higher than suggested by data on human adverse effects, especially on the immune system, that occur at background exposure levels. By now, the best-known PFASs are being phased out, and related PFASs are being introduced as substitutes. Given the substantial delays in discovery of PFAS toxicity, in dissemination of findings, and in regulatory decisions, PFAS substitutes and other persistent industrial chemicals should be subjected to prior scrutiny before widespread usage.
Peer Review reports
Late emergence of early evidence
Industrial chemicals are often regarded inert or safe, unless proven otherwise, i.e., the so-called “untested chemicals assumption,” although this belief is of course not logical [ 1 , 2 ]. A high-priority group of environmental chemicals, the perfluorinated alkylate substances (PFASs), constitute a clear example how narrow reliance on published toxicity studies can be misleading and result in insufficient and delayed protection of public health [ 3 ]. New insight on PFAS immunotoxicity shows that the path from discovery of toxicity to decisions on intervention can be stalled for decades (Table 1 ).
After the beginning of commercial PFAS production in the 1950s, a brief review article from 1980 [ 4 ] for the first time mentioned industry-sponsored studies, some of which were carried out in monkeys. Perfluorooctanoic acid (PFOA) showed specific toxicity to the reticuloendothelial system (i.e. immune system) [ 5 ]. In this 90-day study, compound-related microscopic lesions were seen in bone marrow, spleen and lymph nodes, thus clearly suggesting immunotoxicity, although functional tests were not carried out. A parallel study on perfluorooctanoic sulfonic acid (PFOS), also from 1978, was aborted due to mortality of the monkeys at all doses (the lowest being 10 mg/kg/day) [ 6 ]. These two internal reports were eventually shared with the U.S. Environmental Protection Agency (EPA) in 2000 [ 7 ] and then became accessible to the public.
A medical thesis from 1992 mentioned the evidence from the monkey study and noted: “No follow-up studies of these observations have been reported” [ 8 ]. The thesis analyzed clinical examination data from PFOA production workers and found clear associations between increased PFAS concentrations in the blood and decreased leukocyte counts. The results were not reported in a scientific journal. However, in connection with a recent law suit, a draft manuscript on this study has been released (“Peripheral blood lymphocyte count in men occupationally exposed to perfluorooctanoic acid” [ 9 ]). The draft concluded: “PFOA is associated with alterations in peripheral blood lymphocyte numbers in PFOA production workers, suggesting that cell-mediated immunity may be affected by PFOA”. Other company materials outlined in an expert report include the comment “We’re working with [the author] regarding some of the wording” [ 10 ]. Evidently, an agreement was not reached, and the findings were not published.
Human exposure to organofluorine compounds was discovered as early as 1968 [ 11 ] and was later confirmed in a more extensive study [ 12 ]. However, the exact identity and the sources were unknown at the time. Soon thereafter, PFASs were identified in blood from production workers, and in 1981 also in umbilical cord blood at a female worker’s childbirth [ 13 ]. Although the latter finding signified placental passage and prenatal PFAS exposure, this observation was not revealed until 20 years later, after which it was soon confirmed in a larger study [ 14 ]. Of additional public health significance, an unpublished study on goats from 1993 showed that PFOS was transferred into milk [ 10 ], and this pathway was verified in humans, again many years later [ 15 ].
New insight into a hidden hazard
By about 2000, the widespread occurrence and persistence of PFASs in the environment became known [ 7 ], as reflected also by the presence of PFASs in serum samples from blood banks [ 16 ]. Only after this time, and especially during the most recent 10 years, did the scientific literature on PFASs expand (Fig. 1 ) [ 17 ]. Immune system deficits in PFOA-exposed mice were at first observed in studies of peroxisome proliferator activation [ 18 ]. Later, experimental studies of PFOS showed reductions in lymphoid cell numbers and de novo antibody synthesis [ 19 ], and a study in mice from 2009 demonstrated that PFOS exposure reduced the survival after influenza A infection [ 20 ]. Then followed in vitro evidence of adverse effects in human white blood cells [ 21 ]. Although the 1978 monkey study [ 5 ] could have been obtained from the U.S. EPA, none of these studies referred to these original findings.
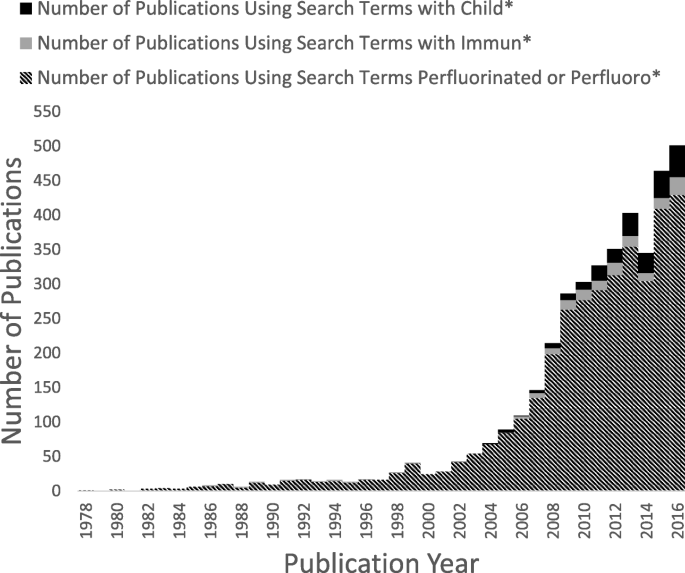
Number of publications on PFASs over time, according to the Web of Science database (between 1978 and 2017), using the search terms “perfluorinated or perfluoro”* and restricting to environmental sciences, toxicology, or public, environmental, and occupational health categories. This search was further refined using the search terms “immun*” and “child*”
Important evidence emerged after the discovery of PFAS contamination in the Mid-Ohio River Valley and the court-mandated health examinations [ 22 ]. In regard to immunotoxicity, an interim report showed that increased PFOA exposure was associated with changes in serum concentrations of immunoglobulins [ 23 ]. A more focused study determined antibody responses to flu vaccination [ 24 ]. Elevated serum-PFOA concentrations were associated with a reduced antibody titer rise, particularly to an A influenza virus strain, with an increased risk of not attaining the antibody level needed to provide long-term protection. A later study on 12 adult volunteers with background exposures showed that two of the subjects failed to respond to a tetanus-diphtheria booster and that the steepness of the antibody responses was negatively associated with the serum-PFAS concentrations [ 25 ]. Cross-sectional data have also suggested lower vaccination antibody concentrations at elevated background PFAS exposures [ 26 ].
The first prospective study assessing children’s antibody responses to routine childhood immunizations reported in 2012 that a doubling in exposure to PFOS and PFOA was associated with an overall decrease by up to 50% in the specific vaccine antibody concentration [ 27 , 28 ]. When mutually adjusted, the regression coefficients for PFOA and PFOS changed only little [ 27 ]. Booster vaccine responses in children at age 5 years were lower at elevated serum-PFAS concentrations [ 28 , 29 ]. A smaller Norwegian study of about 50 children aged 3 years also showed tendencies toward lower vaccination antibody concentrations at higher exposures during pregnancy [ 30 ]. As PFASs are now known to be transferred to the infant via human milk [ 31 ], it seems likely that PFAS exposures in early infancy represent a particular hazard to the adaptive immune system [ 32 ]. If true, the routine modeling of lifetime exposures for risk assessment is inappropriate, as it ignores the presence of vulnerable time windows.
PFAS exposure can also impact the body’s ability to fight off common infections, such as colds and gastroenteritis, as seen in the Norwegian study [ 30 ]. A larger, prospective study in Denmark found that increased maternal serum concentrations of PFOA and PFOS were significantly associated with a higher frequency of fever and symptoms in the children [ 33 ], in agreement with a subsequent study from Japan that relied on retrospective assessment of the disease incidence [ 34 ]. In contrast, a substudy from the Danish National Birth Cohort examined the hospitalization rates for a variety of infections, such as airway infection, middle ear infection, and appendicitis, through to age 11 years and showed no association with PFOS and PFOA in early pregnancy serum from the mother [ 35 ]. However, a recent report from the project team raised doubt about the validity of the PFAS analyses [ 36 ].
Delayed interventions
Despite the support from both experimental and epidemiological data [ 37 ], most regulatory risk assessments of PFASs have focused on other target organs and have emphasized toxicity testing in rodents [ 4 ]. The first opinion from the European Food Safety Authority (EFSA) in 2009 [ 38 ] listed a single report on immunotoxicity under “Other endpoints”. That same year, the EPA issued provisional health advisories and concluded that “epidemiological studies of exposure to PFOA and adverse health outcomes in humans are inconclusive at present” [ 39 ]. Neither report referred to the 1978 monkey study that had become available in 2000. Early and more recent guidelines and recommended limits for PFOS and PFOA are shown in Table 2 .
The EPA prepared more detailed risk assessment reports for PFOA and PFOS in 2014 [ 40 , 41 ]. These drafts conclude that the two major PFASs exhibit immunotoxicity in experimental models and that the epidemiological evidence is additive, although mixed exposures complicate the attribution of effects to specific PFASs. A similar conclusion was reached by an ATSDR ToxProfile on the perfluoroalkyls in 2015 [ 42 ]. The coverage of human immunotoxicity was very brief, and no mention of this potential was made in the sections on public health implications. Although the monkey studies were cited, the risk assessment reports did not refer to the 1992 study of exposure-associated immune cell abnormalities in workers.
More recently, the National Toxicology Program (NTP) in 2016 reviewed the immunotoxicity information on PFOS and PFOA and concluded that both are “presumed” to constitute immune hazards to humans [ 37 ]. The term “presumed” is the strongest below “known” in the NTP vernacular. Both PFASs suppress the antibody response in animal studies, while the evidence in humans is “moderate”, as all studies are observational (not experimental) and refer to mixed PFAS exposures. The revised ATSDR ToxProfile [ 43 ] just released concluded that decreased antibody response to vaccines is a potential outcome from exposure to all five PFASs commonly found in human blood samples. However, ATSDR stopped short of using epidemiology evidence for derivation of exposure limits.
Regulatory agencies frequently use benchmark dose calculations as a basis for generating exposure limits [ 38 ]. This approach relies on fitting a dose-response function to the data, and the benchmark dose (BMD) is defined as the dose that leads to a specific loss (or degree of abnormality) known as the benchmark response (BMR) in the outcome variable. The lower one-sided 95% confidence limit of the BMD is the benchmark dose level (BMDL), which is used as the point of departure for calculation of exposure limits. Relying on the vaccine antibody responses, BMDLs for PFOS and PFOA were calculated in 2013 to be about 1 μg/L serum [ 44 ], i.e., levels that are exceeded by a majority of the general population [ 45 ]. However, at first, these results were disregarded because of the absence of an unexposed control group [ 42 ], a condition that would be impossible to meet. Another concern was the high correlation between exposure components, such as PFOA and PFOS [ 40 , 41 , 43 ]. Still, mutual adjustment is possible and shows clear negative impacts of both of these major PFASs on immune system responses [ 27 ], and other calculations show virtually unchanged BMDLs for PFOA and PFOS after such adjustment [ 46 ].
In an updated opinion on PFOS and PFOA [ 47 ], EFSA used separate BMD calculations for several outcomes in humans, including immunotoxicity, relying on summary data in deciles or quartiles. For the vaccine response data [ 28 ], EFSA assumed that all subjects in the lowest decile exposure group had the same exposure, and the BMDs were similar to the average serum concentration in that group. For this reason, EFSA’s calculated BMDs are several fold higher than the ones obtained from the continuous dose-effect relationship [ 44 ]. Still, the new tolerable intake limits are substantially lower than other published guidelines (Table 2 ), though quite similar to the Minimal Risk Levels developed by ATSDR [ 43 ].
The “untested chemicals assumption”, as highlighted by the National Research Council [ 1 ] has clearly been inappropriately relied upon in past risk assessments of PFASs, and these substances must now be added to the list of environmental hazards [ 48 ] where standard risk assessment has failed. As a major reason, early evidence on PFAS toxicity was kept secret for 20 years or more, and even after its release, it was apparently overlooked. A related reason is the absence of academic PFAS research on the immune system and other sensitive target organs until about 10 years ago. Further, regulatory agencies relied on experimental toxicity studies and disregarded emerging epidemiological evidence. As a result, even some of the current guidelines are orders of magnitude above exposure levels at which associations with adverse effects have been reported.
The PFASs therefore constitute an unfortunate example that risk assessment may be inappropriate to assess human health risks from chemical exposures when crucial documentation has not yet been published. Recognizing the weaknesses of conventional risk assessment, scientists from the U.S. EPA recently recommended to consider the full range of available data and to include health endpoints that reflect the range of subtle effects and morbidities in humans [ 48 ]. The present summary of delayed discovery, dissemination and decision-making on the PFASs indicates that a more comprehensive assessment of adverse health risks is urgently needed and that PFAS substitutes, as well as other persistent industrial chemicals, should not be considered innocuous in the absence of relevant documentation [ 49 ].
Conclusions
Early research on environmental PFAS exposures and their health implications became available at a substantial delay and was not taken into account in initial regulatory decisions on exposure abatement. Only in the last 10 years or so has environmental health research focused on the PFASs and revealed important human health risks, e.g., to the immune system. Although guideline values for PFASs in drinking water have decreased over time, they remain too high to protect against such toxicity. While the most commonly used PFASs will remain in the environment for many years, new PFAS substitutes are being introduced, although little information on adverse health risks is available. Given the serious delays in the discovery of PFAS toxicity, their persistence in the environment, and their public health impact, PFAS substitutes and other persistent industrial chemicals should be subjected to prior research scrutiny before widespread usage.
Abbreviations
Benchmark dose
Benchmark dose level
Benchmark response
European Food Safety Authority
Environmental Protection Agency
National Toxicology Program
Perfluorinated alkylate substance
Perfluorooctanoic acid
Perfluorooctanoic sulfonic acid
National Research Council. Science and decisions: advancing risk assessment. Washington, D.C.: National Academy Press; 2009.
Google Scholar
Grandjean P. Science for precautionary decision-making. In: Gee D, Grandjean P, Hansen SF, van den Hove S, MacGarvin M, Martin J, Nielsen G, Quist D, Stanners D, editors. Late lessons from early warnings, vol. 2. Copenhagen: European Environment Agency; 2013. p. 517–35.
Grandjean P, Clapp R. Perfluorinated alkyl substances: emerging insights into health risks. New Solut. 2015;25(2):147–63.
Article Google Scholar
Griffith FD, Long JE. Animal toxicity studies with ammonium perfluorooctanoate. Am Ind Hyg Assoc J. 1980;41(8):576–83.
Article CAS Google Scholar
Goldenthal EI, Jessup DC, Geil RG, Mehring JS. Final report, ninety day subacute rhesus monkey toxicity study, International Research and Development Corporation, study no. 137–090, November 10, 1978, U.S. EPA Administrative Record, AR226–0447. 1978.
Goldenthal EI, Jessup DC, Geil RG, Mehring JS. Ninety-day subacute rat toxicity study, with Fluorad® Fluorochemical Surfactant FC-95, International Research and Development Corporation, project No. 137–085, December 18, 1978, U.S. EPA Administrative Record, AR226–0137. 1978.
Lindstrom AB, Strynar MJ, Libelo EL. Polyfluorinated compounds: past, present, and future. Environ Sci Technol. 2011;45(19):7954–61.
Gilliland FD. Fluorocarbons and human health: studies in an occupational cohort. Minnesota: University of Minnesota; 1992.
Gilliland FD, Mandel JS: Peripheral blood lymphocyte count in men occupationally exposed to perfluorooctanoic acid. 1992. (unpublished manuscript, available as PTX2498 at https://www.ag.state.mn.us/office/contactus.asp ).
Grandjean P. Expert report. Minneapolis: State of Minnesota District Court for the County of Hennepin Fourth Judicial District; 2017. Civil Action No. 27-cv-10-28862, State of Minnesota, et al. v. 3M company
Taves DR. Evidence that there are two forms of fluoride in human serum. Nature. 1968;217(5133):1050–1.
Guy WS, Taves DR, Brey WS. Organic fluorocompounds in human-plasma - prevalence and characterization. ACS Symp Ser. 1976;28:117–34.
PFCs. Global contaminants: PFOA is a pervasive pollutant in human blood, as are other PFCs [ https://www.ewg.org/research/pfcs-global-contaminants/pfoa-pervasive-pollutant-human-blood-are-other-pfcs ].
Inoue K, Okada F, Ito R, Kato S, Sasaki S, Nakajima S, Uno A, Saijo Y, Sata F, Yoshimura Y, et al. Perfluorooctane sulfonate (PFOS) and related perfluorinated compounds in human maternal and cord blood samples: assessment of PFOS exposure in a susceptible population during pregnancy. Environ Health Perspect. 2004;112(11):1204–7.
Kuklenyik Z, Reich JA, Tully JS, Needham LL, Calafat AM. Automated solid-phase extraction and measurement of perfluorinated organic acids and amides in human serum and milk. Environ Sci Technol. 2004;38(13):3698–704.
Olsen GW, Church TR, Miller JP, Burris JM, Hansen KJ, Lundberg JK, Armitage JB, Herron RM, Medhdizadehkashi Z, Nobiletti JB, et al. Perfluorooctanesulfonate and other fluorochemicals in the serum of American red Cross adult blood donors. Environ Health Perspect. 2003;111(16):1892–901.
Grandjean P, Eriksen ML, Ellegaard O, Wallin JA. The Matthew effect in environmental science publication: a bibliometric analysis of chemical substances in journal articles. Environ Health. 2011;10:96.
Yang Q, Xie Y, Alexson SE, Nelson BD, DePierre JW. Involvement of the peroxisome proliferator-activated receptor alpha in the immunomodulation caused by peroxisome proliferators in mice. Biochem Pharmacol. 2002;63(10):1893–900.
DeWitt JC, Peden-Adams MM, Keller JM, Germolec DR. Immunotoxicity of perfluorinated compounds: recent developments. Toxicol Pathol. 2012;40(2):300–11.
Guruge KS, Hikono H, Shimada N, Murakami K, Hasegawa J, Yeung LW, Yamanaka N, Yamashita N. Effect of perfluorooctane sulfonate (PFOS) on influenza a virus-induced mortality in female B6C3F1 mice. J Toxicol Sci. 2009;34(6):687–91.
Corsini E, Sangiovanni E, Avogadro A, Galbiati V, Viviani B, Marinovich M, Galli CL, Dell'Agli M, Germolec DR. In vitro characterization of the immunotoxic potential of several perfluorinated compounds (PFCs). Toxicol Appl Pharmacol. 2012;258(2):248–55.
Steenland K, Fletcher T, Savitz DA. Epidemiologic evidence on the health effects of perfluorooctanoic acid (PFOA). Environ Health Perspect. 2010;118(8):1100–8.
C8 Science Panel. In: Fletcher T, Steenland K, Savitz D, editors. Status report: PFOA and immune biomarkers in adults exposed to PFOA in drinking water in the mid Ohio valley; 2009.
Looker C, Luster MI, Calafat AM, Johnson VJ, Burleson GR, Burleson FG, Fletcher T. Influenza vaccine response in adults exposed to perfluorooctanoate and perfluorooctanesulfonate. Toxicol Sci. 2014;138(1):76–88.
Kielsen K, Shamim Z, Ryder LP, Nielsen F, Grandjean P, Budtz-Jorgensen E, Heilmann C. Antibody response to booster vaccination with tetanus and diphtheria in adults exposed to perfluorinated alkylates. J Immunotoxicol. 2016;13(2):270–3.
Stein CR, McGovern KJ, Pajak AM, Maglione PJ, Wolff MS. Perfluoroalkyl and polyfluoroalkyl substances and indicators of immune function in children aged 12-19 y: National Health and nutrition examination survey. Pediatr Res. 2016;79(2):348–57.
Mogensen UB, Budtz-Jørgensen E, Heilmann C, Nielsen F, Weihe P, Grandjean P. Structural equation modeling of immunotoxicity associated with exposure to perfluorinated compounds. Environ Health. 2015;14:47.
Grandjean P, Andersen EW, Budtz-Jorgensen E, Nielsen F, Molbak K, Weihe P, Heilmann C. Serum vaccine antibody concentrations in children exposed to perfluorinated compounds. JAMA. 2012;307(4):391–7.
Grandjean P, Heilmann C. Perfluorinated compounds and immunotoxicity in children – reply. JAMA. 2012;307:1910–1.
Granum B, Haug LS, Namork E, Stolevik SB, Thomsen C, Aaberge IS, van Loveren H, Lovik M, Nygaard UC. Pre-natal exposure to perfluoroalkyl substances may be associated with altered vaccine antibody levels and immune-related health outcomes in early childhood. J Immunotoxicol. 2013;10(4):373–9.
Mondal D, Weldon RH, Armstrong BG, Gibson LJ, Lopez-Espinosa MJ, Shin HM, Fletcher T. Breastfeeding: a potential excretion route for mothers and implications for infant exposure to perfluoroalkyl acids. Environ Health Perspect. 2014;122(2):187–92.
Grandjean P, Heilmann C, Weihe P, Nielsen F, Mogensen UB, Timmermann A, Budtz-Jorgensen E. Estimated exposures to perfluorinated compounds in infancy predict attenuated vaccine antibody concentrations at age 5-years. J Immunotoxicol. 2017;14(1):188–95.
Dalsager L, Christensen N, Husby S, Kyhl H, Nielsen F, Host A, Grandjean P, Jensen TK. Association between prenatal exposure to perfluorinated compounds and symptoms of infections at age 1-4years among 359 children in the Odense child cohort. Environ Int. 2016;96:58–64.
Goudarzi H, Miyashita C, Okada E, Kashino I, Chen CJ, Ito S, Araki A, Kobayashi S, Matsuura H, Kishi R. Prenatal exposure to perfluoroalkyl acids and prevalence of infectious diseases up to 4years of age. Environ Int. 2017;104:132–8.
Fei C, McLaughlin JK, Lipworth L, Olsen J. Prenatal exposure to PFOA and PFOS and risk of hospitalization for infectious diseases in early childhood. Environ Res. 2010;110(8):773–7.
Bach CC, Henriksen TB, Bossi R, Bech BH, Fuglsang J, Olsen J, Nohr EA. Perfluoroalkyl acid concentrations in blood samples subjected to transportation and processing delay. PLoS One. 2015;10(9):e0137768.
National Toxicology Program. Immunotoxicity associated with exposure to Perfluorooctanoic acid (PFOA) or Perfluorooctane sulfonate (PFOS). Raleigh: National Toxicology Program; 2016.
European Food Safety Authority. Guidance of the scientific committee on use of the benchmark dose approach in risk assessment. EFSA J. 2009;1150:1–72.
U.S. Environmental Protection Agency. Provisional health advisories for perfluorooctanoic acid (PFOA) and perfluorooctane sulfonate (PFOS). Washington, DC: U.S. Environmental Protection Agency; 2009.
U.S. Environmental Protection Agency. Health effects document for Perfluorooctanoic acid (PFOA). Washington, D.C.: U.S. EPA; 2014.
U.S. Environmental Protection Agency. Health effects document for Perfluorooctane sulfonate (PFOS). Washington, D.C.: U.S. EPA; 2014.
Agency for Toxic Substances and Disease Registry. Draft toxicological profile for perfluoroalkyls. Atlanta: Agency for Toxic Substances and Disease Registry; 2015.
Agency for Toxic Substances and Disease Registry. Draft toxicological profile for perfluoroalkyls. Atlanta: Agency for Toxic Substances and Disease Registry; 2018.
Grandjean P, Budtz-Jorgensen E. Immunotoxicity of perfluorinated alkylates: calculation of benchmark doses based on serum concentrations in children. Environ Health. 2013;12(1):35.
CDC: Fourth National Report on human exposure to environmental chemicals, updated tables. Centers for disease control and prevention; 2015.
Budtz-Joergensen E, Grandjean P. Application of benchmark analysis for mixed contaminant exposures: Mutual adjustment of two perfluoroalkylate substances associated with immunotoxicity: bioRxiv; 2017. p. 198564. https://www.biorxiv.org/content/early/2017/10/06/198564 .
European Food Safety Authority. Risk to human health related to the presence of perfluorooctane sulfonic acid and perfluorooctanoic acid in food (draft). EFSA J. 2018;16(5):1–293.
Gwinn MR, Axelrad DA, Bahadori T, Bussard D, Cascio WE, Deener K, Dix D, Thomas RS, Kavlock RJ, Burke TA. Chemical risk assessment: traditional vs public health perspectives. Am J Public Health. 2017;107(7):1032–9.
Birnbaum LS, Grandjean P. Alternatives to PFASs: perspectives on the science. Environ Health Perspect. 2015;123(5):A104–5.
Dewitt JC, Copeland CB, Strynar MJ, Luebke RW. Perfluorooctanoic acid-induced immunomodulation in adult C57BL/6J or C57BL/6N female mice. Environ Health Perspect. 2008;116(5):644–50.
Download references
The author is supported by the NIEHS Superfund Research Program (P42ES027706).

Author information
Authors and affiliations.
Department of Environmental Health, Harvard T.H. Chan School of Public Health, Boston, MA, USA
Philippe Grandjean
Department of Environmental Medicine, University of Southern Denmark, Odense, Denmark
You can also search for this author in PubMed Google Scholar
Contributions
The author read and approved the final manuscript.
Corresponding author
Correspondence to Philippe Grandjean .
Ethics declarations
Competing interests.
The author is an editor-in-chief of Environmental Health. The author recently served as a health expert for the State of Minnesota in a lawsuit against a PFAS-producing company.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Grandjean, P. Delayed discovery, dissemination, and decisions on intervention in environmental health: a case study on immunotoxicity of perfluorinated alkylate substances. Environ Health 17 , 62 (2018). https://doi.org/10.1186/s12940-018-0405-y
Download citation
Received : 20 June 2018
Accepted : 29 June 2018
Published : 31 July 2018
DOI : https://doi.org/10.1186/s12940-018-0405-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Environmental Health
ISSN: 1476-069X
- General enquiries: [email protected]

Site Search
- How to Search
- Advisory Group
- Editorial Board
- OEC Fellows
- History and Funding
- Using OEC Materials
- Collections
- Research Ethics Resources
- Ethics Projects
- Communities of Practice
- Get Involved
- Submit Content
- Open Access Membership
- Become a Partner
Life and Environmental Science Ethics: Case Studies
This collection of cases covers topics related to Life and Environmental Science ethics including, agriculture ethics, bioethics, environmental ethics, and more. Cases come from a variety of online educational sources, ethics centers, and ethics programs.
Ethics Unwrapped. “Arctic Offshore Drilling.” 2021. https://ethicsunwrapped.utexas.edu/case-study/arctic-offshore-drilling.
- Offshore oil and gas reserves, primarily along coastlines in Alaska, California, Louisiana, and Texas, account for a large proportion of the oil and gas supply in the United States. In August 2015, President Obama authorized Royal Dutch Shell to expand drilling off Alaska’s northwest coast. His decision brought into sharp relief the different, oftentimes competing views on the expansion of offshore drilling.
Ethics Unwrapped. “Climate Change & the Paris Deal.” 2021. https://ethicsunwrapped.utexas.edu/case-study/climate-change-paris-deal.
- In December 2015, representatives from 195 nations gathered in Paris and signed an international agreement to address climate change, which many observers called a breakthrough for several reasons. First, the fact that a deal was struck at all was a major accomplishment, given the failure of previous climate change talks. Second, unlike previous climate change accords that focused exclusively on developed countries, this pact committed both developed and developing countries to reduce greenhouse gas emissions. However, the voluntary targets established by nations in the Paris climate deal fall considerably short of what many scientists deem necessary to achieve the stated goal of the negotiations: limiting the global temperature increase to 2 degrees Celsius. Furthermore, since the established targets are voluntary, they may be lowered or abandoned due to political resistance, short-term economic crises, or simply social fatigue or disinterest.
Ethics Unwrapped. “Patient Autonomy & Informed Consent - Ethics Unwrapped.” 2021. https://ethicsunwrapped.utexas.edu/case-study/patient-autonomy-informed-consent.
- In the context of health care in the United States, the value on autonomy and liberty was cogently expressed by Justice Benjamin Cardozo in Schloendorff v. Society of New York Hospitals (1914), when he wrote, “Every human being of adult years and sound mind has a right to determine what shall be done with his own body.” This case established the principle of informed consent and has become central to modern medical practice ethics . However, a number of events since 1914 have illustrated how the autonomy of patients may be overridden. In Buck v. Bell (1927), Justice Oliver Wendell Holmes wrote that the involuntary sterilization of “mental defectives,” then a widespread practice in the U.S., was justified, stating, “Three generations of imbeciles are enough.” Another example, the Tuskegee Syphilis Study, in which African-American males were denied life-saving treatment for syphilis as part of a scientific study of the natural course of the disease, began in 1932 and was not stopped until 1972.
Ethics Unwrapped. “Prenatal Diagnosis & Parental Choice.” 2021. https://ethicsunwrapped.utexas.edu/case-study/prenatal-diagnosis-parental-choice.
- In the United States, many citizens agree that the government may impose limits on the freedom of individuals when individuals interfere with the rights of others, but the extent of these limits is often a topic of debate. Among the most debated of bioethical issues is the issue of abortion, which hinges on whether the fetus is a person with rights, notably the right to life.
Ethics Unwrapped. “Retracting Research: The Case of Chandok v. Klessig.” 2021. https://ethicsunwrapped.utexas.edu/case-study/retracting-research-case-chandok-v-klessig.
- In 2003, a research team from prominent laboratory the Boyce Thompson Institute (BTI) for Plant Research in Ithaca, New York published an article in the prestigious academic journal Cell. It was considered a breakthrough paper in that it answered a major question in the field of plant cell biology. The first author of this paper was postdoctoral researcher Meena Chandok, working under her supervisor Daniel Klessig, president of BTI at the time.
International Dimensions of Ethics Education in Science & Engineering. “IDEESE Case: GMOs.” University of Massachusetts Amherst, 2009. https://www.umass.edu/sts/ethics/online/cases/GMO/case.html.
- High ethical concern about GM organisms has two sources: concerns for the integrity and sustainability of the natural environment and concern about the social consequences of allowing the supply of seeds or breeding stock to be controlled by developers (mainly though not exclusively large multinational corporations) having 20-year monopolies over the distribution of any particular genetic material as a consequence of patent rights.
International Dimensions of Ethics Education in Science & Engineering. “IDEESE Case: Stem Cell.” University of Massachusetts Amherst, 2009. https://www.umass.edu/sts/ethics/online/cases/StemCell/case.html.
- Stem cells are undifferentiated cells in the human body which are able to replenish themselves by dividing. Under particular natural or medically induced circumstances, they are able to develop into more specialized cells for forming bones, nerves, body tissue, brains, muscles, and blood. Stem cell research has provoked considerable ethical concern; while many welcome the prospect of more effective treatments of birth defects or diseases, using human embryonic stem cells for such treatments, or even in scientific research, is very controversial. The embryo must be destroyed to secure its stem cells, and anyone who believes that human life begins at the moment of conception equates destroying embryos with committing murder. Excitement generated by the first acquisition of human embryonic stem cells in 1998 spread around the world. In South Korea, where scientists and the government had been attuned to advances in genetics, bioscience, and biotechnology since the mid-1980s, there was strong interest in taking up the new possibilities. Four years earlier, the South Korean government had adopted an ambitious "Plan 2000" intended to make South Korea one of the leading sites of bioscience and biotechnology research in the world. In 1990 it provided its national Genetics Research Institute with ample facilities in the new Taedok Science town just outside Seoul; in 1995 it expanded the Institute and renamed it the Korean Research Institute for Bioscience and Biotechnology to better reflect its expanded areas of work.
Iowa State University. “Case Studies.” Bioethics Program, 2021. https://bioethics.las.iastate.edu/a-note-about-case-studies-for-the-classroom/.
- The following are helpful for introducing real-life ethics situations to students. These case studies are designed for teaching purposes, to help students develop critical responses to ethical issues, taking into account a multitude of viewpoints. Please feel free to use these case studies in your classrooms, or modify as necessary for your purposes. Please give credit where credit is due.
Teach the Earth. “Case of GMOs in Environmental Cleanup.” Across the Geoscience Currirulum, 2019. https://serc.carleton.edu/geoethics/activities/84049.html.
- This case represents various agendas, hidden and otherwise, that can come into play during environmental remediation.
Teach the Earth. “Does A River Have Rights?” Across the Geoscience Curriculum, 2019. https://serc.carleton.edu/geoethics/activities/84031.html.
- Individual students have different ethical "lines." This class discussion proceeds with a series of prompts that presents a set of scenarios that explores ethical boundaries. Students discuss right and wrong actions with respect to a river and discuss why those actions are "right" or "wrong" as well as how their ethical viewpoints vary.
Submit Content to the OEC Donate

This material is based upon work supported by the National Science Foundation under Award No. 2055332. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the National Science Foundation.
Health, well-being and education: Building a sustainable future. The Moscow statement on Health Promoting Schools
Health Education
ISSN : 0965-4283
Article publication date: 18 March 2020
Issue publication date: 4 June 2020
The purpose of this paper is to introduce the official statement of the Fifth European Conference on Health-Promoting Schools.
Design/methodology/approach
The Fifth European Conference on Health-Promoting Schools was held on 20–22 November 2019 in Moscow, Russian Federation, with over 450 participants from 40 countries. A writing group was established to prepare a draft version of the statement before the conference. On the basis of an online and offline feedback process, the opinions of the participants were collected during the conference and included in the finalisation of the statement.
The final conference statement comprises six thematic categories (values and principles; environment, climate and health; schools as part of the wider community; non-communicable diseases (NCDs); evidence base; and digital media), with a total of 23 recommendations and calls for action.
Originality/value
The recommendations and calls for action reflect current challenges for Health Promoting Schools in Europe. They are addressed to all actors in governmental, non-governmental and other organisations at international, national and regional levels involved in health promotion in schools and are to be applied for the further development of the concept.
- Health Promoting Schools
- Social change
- Child and adolescent health
- School health promotion
Dadaczynski, K. , Jensen, B.B. , Viig, N.G. , Sormunen, M. , von Seelen, J. , Kuchma, V. and Vilaça, T. (2020), "Health, well-being and education: Building a sustainable future. The Moscow statement on Health Promoting Schools", Health Education , Vol. 120 No. 1, pp. 11-19. https://doi.org/10.1108/HE-12-2019-0058
Emerald Publishing Limited
Copyright © Kevin Dadaczynski, Bjarne Bruun Jensen, Nina Grieg Viig, Marjorita Sormunen, Jesper von Seelen, Vladislav Kuchma and Teresa Vilaça
Published in Health Education . Published by Emerald Publishing Limited. This article is published under the Creative Commons Attribution (CC BY 4.0) licence. Anyone may reproduce, distribute, translate and create derivative works of this article (for both commercial and non-commercial purposes), subject to full attribution to the original publication and authors. The full terms of this licence may be seen at: http://creativecommons.org/licences/by/4.0/legalcode
1. The Health Promoting Schools approach and its development
The Ottawa Charter, adopted in 1986, was a milestone in the development of a holistic and positive understanding of health that requires actions at different levels, from healthy public policy to the development of personal skills, using different strategies, such as enabling and advocacy approaches ( WHO, 1986 ). The charter can also be regarded as marking the birth of whole-school approaches to health that have been established in Europe and internationally under the term Health Promoting Schools ( Stewart Burgher et al. , 1999 ).
A Health Promoting Schools reflects a holistic approach that moves beyond individual behaviour change by also aiming at organisational change through strengthening the physical and social environment, including interpersonal relationships, school management, policy structures and teaching and learning conditions. This approach can be seen as the result of overcoming traditional health education at school, which aimed to influence students' knowledge, attitudes and behaviour ( Clift and Jensen, 2005 ). In accordance with a social-ecological perspective, health is considered to be the result of a complex interplay of individual, social, socio-economic and cultural factors ( Dahlgreen and Whitehead, 1991 ). Since the early 1990, actions on school health promotion have been coordinated in national networks and the European network on Health Promoting Schools as a WHO supported network. The current work on school health promotion on a European level is organised through the Schools for Health in Europe Network Foundation (SHE), with national representatives from 36 countries.
Values of the Health Promoting Schools approach
Health Promoting Schools ensure equal access for all to the full range of educational and health opportunities. This in the long term makes a significant impact in reducing inequalities in health and in improving the quality and availability of lifelong learning.
Sustainability
Health Promoting Schools acknowledge that health, education and development are closely linked. Schools act as places of academic learning. They support and develop a positive view of pupils' future role in society. Health Promoting Schools develop best when efforts and achievements are implemented in a systematic and continuous way. Desirable and sustainable health and educational outcomes occur mostly in the medium or long term.
Health Promoting Schools celebrate diversity and ensure that schools are communities of learning, where all feel trusted and respected. Good relationships among pupils, between pupils and school staff and between school, parents and the school community are important.
Empowerment
Health Promoting Schools enable children and young people, school staff and all members of the school community to be actively involved in setting health-related goals and in taking actions at school and community level to reach the goals.
Health Promoting Schools are based on democratic values and practise the exercising of rights and taking responsibility.
Pillars of the Health Promoting Schools approach
Whole-school approach to health
Taking a participatory and action-oriented approach to health education in the curriculum;
Taking into account the pupil's own concept of health and well-being;
Developing healthy school policies;
Developing the physical and social environment of the school;
Developing life competencies and health literacy;
Making effective links with home and the community; and
Making efficient use of health services.
Participation
A sense of ownership is fostered by pupils, staff and parents through participation and meaningful engagement, which is a prerequisite for the effectiveness of health-promoting activities in schools.
School quality
Health Promoting Schools support better teaching and learning processes. Healthy pupils learn better, and healthy staff work better and have greater job satisfaction. The school's main task is to maximise educational outcomes. Health Promoting Schools support schools in achieving their educational and social goals.
School health promotion in Europe is informed by existing and emerging research and evidence focused on effective approaches and practice in school health promotion, both on health topics (such as mental health, eating and substance use) and on the whole-school approach.
Schools and communities
Health Promoting Schools engage with the wider community. They endorse collaboration between the school and the community and are active agents in strengthening social capital and health literacy.
Since the establishment of the European network of Health Promoting Schools, four European conferences on Health Promoting Schools have been organised. The resolution of the first conference, held in Thessaloniki, Greece, in 1997, stated that every child and young person in Europe had the right to be educated in a Health Promoting Schools and urged governments in all European countries to adopt the Health Promoting Schools approach ( ENHPS, 1997 ). The Egmont Agenda was published in 2002 as a result of the Second European Conference on Health Promoting Schools in The Netherlands and emphasised conditions, programming and evaluation as being essential to developing and sustaining Health Promoting Schools ( ENHPS, 2002 ).
Seven years later, the Third European Conference on Health Promoting Schools was held in Vilnius, Lithuania ( SHE Network, 2009 ). The conference and its resolution marked an important milestone in the development of the Health Promoting Schools approach by highlighting that education and health have shared interests and complement each other. Based on this, joint actions beyond sectoral responsibilities were urged.
The Fourth European Conference was held in Odense, Denmark, in 2013 and resulted in The Odense Statement, which recognised the core values and pillars of school health promotion as a strong contributor to the aims and objectives of the WHO policy framework for health and well-being in Europe, Health 2020 and the EU2020 strategy for inclusive and sustainable growth ( SHE Network, 2013 ).
2. Recent societal challenges
Since the establishment of the Health Promoting School approach in the late 1980s, the world has seen constant societal change, with progressively faster dynamics during recent years. The changes have not only altered substantially the conditions in which people grow up and live, but have also affected behaviours in relation to health, social cohabitation, learning and working. Wars and violence, often rooted in cultural and religious differences or political and economic crisis, and climate change alter significantly the environmental and societal determinants of health ( Mucci et al. , 2016 ; Watts et al. , 2019 ).
Often, it is countries that already are experiencing political and socio-economic instability that feel the effects most ( Reibling et al. , 2017 ). An increase in international migration, commonly in perilous circumstances for migrants and refugees ( Silove et al. , 2017 ), is the consequence, raising social tensions and challenges in many countries, some of which are undergoing political developments characterised by protectionism and isolationism that can partly be seen as a countermovement to the idea, values and principles of Europe ( Harteveld et al. , 2018 ).
In many cases, uncertainty has replaced political, economic, social and individual stability, raising concern and anxiety about the future in young people and adults. This has led to an unprecedented social (grassroots) movement of participation, primarily driven by young people who are demanding social, political, ecological and economic change ( O'Brien, Selboe and Hayward, 2018 ).
These developments should not be seen as being separate from school health promotion, the aim of which is to support young people to develop healthy and self-determined lifestyles and enable them to co-create their social, physical and ecological environments and the determinants of health positively and sustainably ( Clift and Jensen, 2005 ; Simovska and McNamara, 2015 ). As the conditions for growing up and living together change, the question arises of how schools, as places for health-related teaching, learning and development, need to adapt.
Where does the Health Promoting School approach stand today, more than 30 years after the Ottawa Charter on health promotion? Can the Health Promoting School, with its holistic orientation, deliver on its promise of addressing health inequalities and improving children's and young people's health, well-being and academic achievement? To what extent can school health promotion be implemented systematically in schools and be linked to local communities?
These and more questions were raised and discussed during the Fifth European Conference on Health Promoting School, culminating in recommendations for the future development of the Health Promoting School approach.
3. The Fifth European Conference on Health Promoting Schools
The Fifth European Conference on Health Promoting Schools was held on 20–22 November 2019 in Moscow, Russian Federation, with over 450 participants from 40 countries.
A range of topics was addressed through more than 160 contributions and nine keynote presentations focusing on conceptual aspects of the Health Promoting School approach, implementation and dissemination and current social change processes, such as digitisation and heterogeneity.
Holistic approaches to school-based health promotion and health education (such as organizational change and environmental approaches to school health promotion and strategies to promote individual and organizational health literacy in schools);
Implementation and dissemination of school-based health promotion and health education (facilitators and barriers to implementing interventions in school-based health promotion and professional development and capacity-building of, for example, teachers, non-teaching school staff, school health services, parents and external professionals);
Networking and intersectoral collaboration in school-based health promotion and health education (schools as part of the wider community, and multisectoral partnerships at local, national and international levels);
Innovative approaches to dealing with heterogeneity, inclusion and special needs (pupils' and teachers' health in inclusive schooling, school-based health promotion and education for refugees, students with special needs and innovative approaches to school-based health services); and
Digital media and information and communications technology (ICT) in school health promotion and health education (practical approaches to ICT use in school-based health promotion and digital devices and media as a target for interventions and a means to promote health and well-being).
4. Recommendations for action
Be based on democratic processes and foster equal access, active involvement and participation;
Take into account the needs and background of all young people regardless of their gender, geographical, cultural and social background or religious beliefs: in that sense, a Health Promoting School can be seen as an inclusive school that celebrates heterogeneity and diversity as an enriching dimension for mutual learning, respect and acceptance;
Reflect a whole-school approach addressing different target groups and combining classroom activities with development of school policies, the physical, social and cultural environment of the school and the necessary capacities needed: we welcome new and established concepts and approaches within school-based health promotion, such as health literacy, salutogenesis, action competence and life skills, which should complement each other and be integrated in the holistic framework of the Health Promoting School approach; and
Be systematically linked with educational goals and school quality as part of a so-called add-in approach: based on rich evidence, a Health Promoting School can be regarded as a school that not only promotes and maintains health, but also strives for successful learning for pupils and working conditions for teaching and non-teaching staff, and involves parents and families in the school's daily life.
Urge all stakeholders in health and climate/sustainability education to work together systematically to support young people to grow up and live healthily and sustainably;
Urge all stakeholders to support and empower young people to raise their voice and make a lasting contribution to shaping a healthy and sustainable future for themselves and their fellow human beings;
Call for actions to link planetary health and the Health Promoting School approach more explicitly by, for instance, integrating the impact of human action on the environment and its health consequences into school curricula and everyday life; and
Call for realignment of health-promotion research agendas to address environmental challenges in, with and through schools.
All actors to move from a single-setting approach to an integrated multi-setting approach that systematically links actions at school level with actions in the local community: these actions should not be implemented in isolation, but in a coordinated fashion to create synergies and avoid discontinuities;
Intersectoral collaboration among different actors and professions, such as teachers, school health services and social and youth-care services: this requires professional development, and that existing local networks and their leadership capacities be strengthened to align sectoral policies and enable the development of a common vision and language; and
All actors to strengthen links with existing national and regional cooperation mechanisms, such as Health Promoting School networks and healthy city or healthy region networks, by pursuing joint objectives and actions.
A resource-oriented intervention approach (as described in the SHE values and pillars) be taken to tackle NCDs rather than a traditional top-down and disease-oriented approach, which normally dominates interventions related to risk factors;
Young people be viewed as part of the solution and not only as part of the problem of NCDs – we need to work with young people as powerful agents of healthy change and not as victims and recipients of risk factors;
A school environment that promotes healthy practices in areas like healthy eating, physical activity, social and emotional well-being and good hygiene be created; and
Commercial determinants are addressed by empowering young people to become critical and responsible citizens who are able to understand and critically reflect on media advertising and market mechanisms through, for instance, consumer education.
Call for evaluation approaches that reflect the complexity of the Health Promoting School by, for example, applying mixed-methods designs and considering graded health and educational outcomes;
Demand that the available scientific evidence be reviewed and evaluated using existing tools and be translated into recommendations for practical action;
Urge that a one-sided focus on outcomes research be augmented by focusing also on implementation to identify the conditions under which interventions can be effective, systematically linking both research perspectives; and
Call for systematic and strong partnerships between researchers and practitioners who develop and implement innovative interventions in school health promotion and those who conduct empirical surveys on child and adolescent health (such as the Health Behaviour in School-aged Children (HBSC) study) and the health of teaching and non-teaching staff. By sharing available social-epidemiological data, previously untried evaluation potential can be exploited.
Call on all actors in school health promotion to use the possibilities of digital media in the context of research, development, implementation and exchange of innovative interventions and good practice;
Urge all actors to use digital media as a supplement to, and not as a substitute for, non-digital (face-to-face) school health-promotion actions;
Call on all actors to ensure that the use of digital media does not lead to a step back to individual and behavioural prevention, but rather is used at organisational level to, for instance, build capacity, communicate with partners outside the school and promote low-threshold participation in change processes within the school; and
Call for actions to empower individuals and whole-school systems to deal effectively with health information complexity, including its critical assessment, selection and use and to take responsibility for providing suitable and reliable health information.
The Health Promoting School approach
Buijs , G.J. ( 2009 ), “ Better schools through health: networking for health promoting schools in Europe ”, European Journal of Education , Vol. 44 No. 4 , pp. 507 - 520 .
Clift , S. and Jensen , B.B. ( 2005 ), The Health Promoting School: International Advances in Theory, Evaluation and Practice , Danish University of Education Press , Copenhagen .
Dahlgren , G. and Whitehead , M. ( 1981 ), Policies and Strategies to Promote Social Equality in Health , Institute of Future Studies , Stockholm .
European Network of Health Promoting Schools (ENHPS) ( 2002 ), The Egmond Agenda. A New Tool to Help Establish and Develop Health Promotion in Schools and Related Sectors across Europe , available at: https://tinyurl.com/y2py8wzr ( accessed 19 November 2019 ).
European Network of Health Promoting Schools (ENHPS) ( 1997 ), “ Conference resolution ”, available at: https://tinyurl.com/wcunrec ( accessed 19 November 2019 ).
Harteveld , E. , Schaper , J. , De Lange , S.L. and Van Der Brug , W. ( 2018 ), “ Blaming Brussels? the impact of (news about) the refugee crisis on attitudes towards the EU and national politics ”, JCMS: Journal of Common Market Studies , Vol. 56 No. 1 , pp. 157 - 177 .
Mucci , N. , Giorgi , G. , Roncaioli , M. , Perez , J.F. and Arcangeli , G. ( 2016 ), “ The correlation between stress and economic crisis: a systematic review ”, Neuropsychiatric Disease and Treatment , Vol. 12 , pp. 983 - 993 .
O'Brien , K. , Selboe , E. and Hayward , B. ( 2018 ), “ Exploring youth activism on climate change: dutiful, disruptive, and dangerous dissent ”, Ecology and Society , Vol. 23 No. 3 , p. 42 .
Reibling , N. , Beckfield , J. , Huijts , T. , Schmidt-Catran , A. , Thomson , K.H. and Wendt , C. ( 2017 ), “ Depressed during the depression: has the economic crisis affected mental health inequalities in Europe? findings from the European social survey (2014) special module on the determinants of health ”, The European Journal of Public Health , Vol. 27 Suppl 1 , pp. 47 - 54 .
Schools for Health in Europe (SHE) Network ( 2013 ), “ The Odense Statement. Our ABC for equity, education and health ”, available at: https://tinyurl.com/rk8rh5e ( accessed 19 November 2019 ).
Schools for Health in Europe (SHE) Network ( 2009 ), “ Better schools through health: the Third European Conference on Health Promoting Schools. Vilnius resolution ”, available at: https://tinyurl.com/qskr692 ( accessed 19 November 2019 ).
Silove , D. , Ventevogel , P. and Rees , S. ( 2017 ), “ The contemporary refugee crisis: an overview of mental health challenges ”, World Psychiatry , Vol. 16 No. 2 , pp. 130 - 139 .
Simovska , V. and McNamara , P. (Eds) ( 2015 ), Schools for Health and Sustainability , Springer , Dordrecht .
Stewart Burgher , M. , Barnekow , V. and Rivett , D. ( 1999 ), The European Network of Health Promoting Schools. The Alliance of Education and Health , WHO Regional Office for Europe , Copenhagen .
Watts , N. , Amann , M. , Arnell , N. , Ayeb-Karlsson , S. , Belesova , K. , Boykoff , M. , … and Chambers , J. ( 2019 ), “ The 2019 report of the Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate ”, The Lancet , Vol. 394 No. 10211 , pp. 1836 - 1878 .
WHO ( 2016 ), Declaration: Partnerships for the Health and Well-Being of Our Young and Future Generations. Working Together for Better Health and Well-Being: Promoting Intersectoral and Interagency Action for Health and Well-Being in the WHO European Region , WHO Regional Office for Europe , Copenhagen .
WHO ( 1986 ), “ Ottawa Charter for Health Promotion ”, available at: https://tinyurl.com/mohfbn6 ( accessed 19 November 2019 ).
Acknowledgements
This publication has received funding under an operating grant from the European Union's Health Programme.
Corresponding author
Related articles, we’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
Case Studies in Environmental Medicine
Accredited for CE
Trichloroethylene Toxicity – SS4561 – Go to Course Materials – Go to Course PDF [PDF – 586 KB]
Ethylene Glycol and Propylene Glycol Toxicity – WB4342 – Go to Course Materials – Go to Course PDF [ PDF – 954 KB]
CE Unavailable (Informational Purpose Only) (Updates in Progress)
Arsenic – Go to Course Materials – Go to Course PDF [PDF – 1.03 MB]
Asbestos – Go to Course Materials – Go to Course PDF [PDF – 843 KB]
Beryllium – Go to Course Materials – Go to Course PDF [PDF – 463 KB]
Cadmium – Go to Course Materials – Go to Course PDF [PDF – 971 KB]
Carbon Tetrachloride Toxicity – WB2888 – Go to Course Materials – Go to Course Registration and Posttest – Go to Course PDF [PDF – 1.55MB]
Cholinesterase Inhibitors – Go to Course Materials – Go to Course PDF [PDF – 1.87 MB]
Chromium – Go to Course Materials – Go to Course PDF [PDF – 483 KB]
Ethylene Glycol and Propylene Glycol – Go to Course Materials – Go to Course PDF [PDF – 859 KB]
Lead – WB2832 – Go to Course Materials – Go to Course Registration and Posttest
Nitrate/Nitrite – Go to Course Materials – Go to Course PDF [PDF – 917 KB]
Polychlorinated Biphenyls (PCBs) Toxicity – WB2460 – Go to Course Materials – Go to Course PDF [PDF – 522 KB]
Polycyclic Aromatic Hydrocarbons (PAHs) – Go to Course Materials – Go to Course PDF [PDF – 546 KB]
Principles of Pediatric Environmental Health – Go to Course Materials – Go to Course PDF [PDF – 725 KB]
Radon – Go to Course Materials – Go to Course PDF [PDF – 809 KB]
Taking a Pediatric Exposure History – Go to Course Materials – Go to Course PDF [PDF – 866 KB]
Taking an Exposure History – WB2579 – Go to Course Materials – Go to Course Registration and Posttest – Go to Course PDF [PDF – 695 KB]
Tetrachloroethylene – WB4066 – Go to Course Materials – Go to Course Registration and Posttest – Go to Course PDF [PDF – 484 KB]
Trichloroethylene (TCE) – Go to Course Materials – Go to Course PDF [PDF – 392 KB]
Uranium – Go to Course Materials – Go to Course PDF [PDF – 439 KB]
- Medical Disclaimer and Disclosure
- ATSDR Environmental Medicine Education Resources
- PEHSU National Classroom external icon
- Partner and Other Environmental Medicine Resources
- Public Health Statements
- Tox Profiles
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Development of hydrological based physical model for nutrients transport simulation: case study of Makkah city, Saudi Arabia
- Original Paper
- Published: 26 May 2024
Cite this article

- A. M. Al-Areeq ORCID: orcid.org/0000-0003-0618-8190 1 , 2 ,
- M. A. Al-Zahrani 2 ,
- S. Chowdhury 2 , 3 &
- H. O. Sharif 4
Urban flooding poses significant risks to water quality and public health due to inadequate drainage systems, leading to the dispersion of harmful pollutants in the neighborhoods. This study investigates the transport of nutrients during the flood events in Makkah (Saudi Arabia), underlining the city’s vulnerability to such environmental challenges as a pressing concern. The research aims to quantify the impact of non-point source (NPS) pollutant loads resulting from urban floods, emphasizing the need for improved flood control and pollution mitigation strategies. Employing the Gridded Surface/Subsurface Hydrologic Analysis (GSSHA) model, this research simulates the transport and fate of nutrients for variable percentages of manhole overflow (5%, 10%, 15%, and 20%), addressing the challenge of direct measurement and data scarcity in urban environments. This approach allows for the examination of NPS pollution from sewer systems, considering the mixing of contaminants with floodwaters on urban surfaces. To analyze the effects of rainfall intensity on the temporal and spatial distribution of nutrients, the methodology includes the simulation of storm events with 2- and 10-year return periods. This study facilitates the prediction of contaminants’ dispersion, accumulation sites, and potential impacts on groundwater quality, highlighting the model’s utility in urban flood risk management. The findings indicate that while nutrient concentrations from storms with less than a 10-year return period remain within acceptable limits, the infiltration and subsequent potential for groundwater contamination during more severe events pose significant environmental risks. The study reveals critical insights into the dynamics of contaminant distribution and accumulation, especially during the less frequent but more intense flood events. In essence, this paper highlights how the GSSHA model can simulate the intricate relationships between urban drainage systems and floodwaters, providing a strong framework for evaluating the risks of pollution caused by flooding when specific data is lacking. The study presents an innovative approach to managing urban water quality, which aids in the development of efficient flood response plans and pollution control measures. By highlighting the importance of integrating hydrological models in urban planning, the study provides valuable information for enhancing resilience against flood-related public health and environmental hazards.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Availability of data and materials
Not applicable.
Abdelkarim A, Gaber AFD (2019) Flood Risk assessment of the Wadi Nu’man basin, Mecca, Saudi Arabia (during the period, 1988–2019) based on the integration of geomatics and hydraulic modeling: a case Study. Water 11(9):1887. https://doi.org/10.3390/w11091887
Article Google Scholar
Al Jabri N, Alhazmi R (2017) Observing and monitoring the urban expansion of Makkah al-Mukarramah using the remote sensing and GIS. J Eng Sci Inform Technol 1(2):125–203
Google Scholar
Alahmadi M, Atkinson PM (2019) Three-fold urban expansion in Saudi Arabia from 1992 to 2013 observed using calibrated DMSP-OLS night-time lights imagery. Remote Sensing. https://doi.org/10.3390/rs11192266
Al-Areeq AM, Al-Zahrani MA, Sharif HO (2022) Assessment of the performance of satellite rainfall products over Makkah watershed using a physically based hydrologic model. Appl Water Sci 12(11):1–21. https://doi.org/10.1007/S13201-022-01768-3/TABLES/13
Al-Areeq AM, Al-Zahrani MA, Sharif HO (2021a) Physically-based, distributed hydrologic model for Makkah watershed using GPM satellite rainfall and ground rainfall stations. Geomat Nat Hazards Risk 12(1):1234–1257. https://doi.org/10.1080/19475705.2021.1924873
Al-Areeq AM, Al-Zahrani MA, Sharif HO (2021b) The performance of physically based and conceptual hydrologic models: a case study for Makkah Watershed, Saudi Arabia. Water 13(8):1098. https://doi.org/10.3390/W13081098
Al-Baroudi M, Mirza M, Dawood G (2013) The use of GIS in estimating the volumes of floods and the extent of their development at the lower reaches of Wadi Nu’man south of Makkah city by the application of the Snyder model and the model of digital heights. Fac Arts Human Univ Thebes Medina, Saudi Arabia 2013:757–783
Al-Sulttani AO, Al-Mukhtar M, Roomi AB, Farooque AA, Khedher KM, Yaseen ZM (2021) Proposition of new ensemble data-intelligence models for surface water quality prediction. IEEE Access 9:108527–108541. https://doi.org/10.1109/ACCESS.2021.3100490
Asadollah SBHS, Sharafati A, Motta D, Yaseen ZM (2021) River water quality index prediction and uncertainty analysis: a comparative study of machine learning models. J Environ Chem Eng 9(1):104599. https://doi.org/10.1016/J.JECE.2020.104599
Article CAS Google Scholar
Asquith WH, Roussel MC, Thompson DB, Cleveland TG, Fang X (2004) Summary of dimensionless Texas hyetographs and distribution of storm depth developed for Texas department of transportation research project 0–4194 US. Geological survey water resources division, Report 0–4194–4
Chow VT (1951) A general formula for hydrologic frequency analysis. Trans Am Geophys Union 32(2):231. https://doi.org/10.1029/TR032i002p00231
Czemiel Berndtsson J (2010) Green roof performance towards management of runoff water quantity and quality: a review. Ecol Eng 36(4):351–360. https://doi.org/10.1016/J.ECOLENG.2009.12.014
Dawod GM, Mirza MN, Al-Ghamdi KA, Elzahrany RA (2014) Projected impacts of land use and road network changes on increasing flood hazards using a 4D GIS: a case study in Makkah metropolitan area Saudi Arabia. Arab J Geosci 7:1139–1156. https://doi.org/10.1007/s12517-013-0876-7
Downer BCW, Byrd A (2007) Watershed scale TMDL model: multidimensional sediment erosion, transport, and fate. pp. 1–11
Downer CW, Ogden FL (2006) Gridded surface subsurface hydrological analysis (GSSHA) user's manual; version 1.43 for watershed modeling system 6.1
Downer CW, Ogden FL, Neidzialek JLS (2005). Gridded surface/subsurface hydrologic analysis (GSSHA) model: a model for simulating diverse streamflow-producing processes. Watershed model. https://books.google.com.sa/books?hl=en&lr=&id=mn8Foj3rAwQC&oi=fnd&pg=PA131&dq=Gridded+surface/subsurface+hydrologic+analysis+(GSSHA)+model:+A+model+for+simulating+diverse+streamflow-producing+processes.+Watershed+Model&ots=ocMLNWyOry&sig=wm7EwVgDZ4-3gaGadhjlj7wYMYE&redir_esc=y#v=onepage&q=Gridded%20surface%2Fsubsurface%20hydrologic%20analysis%20(GSSHA)%20model%3A%20A%20model%20for%20simulating%20diverse%20streamflow-producing%20processes.%20Watershed%20Model&f=false
Downer CW, Pradhan NR, Ogden FL, Byrd AR (2014) Testing the effects of detachment limits and transport capacity formulation on sediment runoff predictions using the US. Army corps of engineers GSSHA model. J Hydrol Eng 20(7):04014082. https://doi.org/10.1061/(ASCE)HE.1943-5584.0001104
Downer CW, Ogden FL (2004) GSSHA: model to simulate diverse stream flow producing processes. J Hydrol Eng 9(3):161–174. https://doi.org/10.1061/(ASCE)1084-0699(2004)9:3(161)
Downer CW (2008) Demonstration of GSSHA hydrology and sediment at eau galle watershed near. Spring Valley, Wisconsin
Book Google Scholar
Downer C (2009) Simulation of reactive constituent fate and transport in hydrologic simulator GSSHA,ERDC TN-SWWRP-09-2
Egodawatta P, Thomas E, Goonetilleke A (2007) Mathematical interpretation of pollutant wash-off from urban road surfaces using simulated rainfall. Water Res 41(13):3025–3031. https://doi.org/10.1016/J.WATRES.2007.03.037
EMRL (2018) (Environmental modeling research laboratory). Watershed modeling system (WMS) version 11 tutorial. Brigham Young University, Provo, UT, USA
ESRI (2020) (Environmental systems research institute), 2020: ArcGIS : release 10.60. redlands, CA, USA. ArcGIS® is the intellectual property of Esri and are used herein under license. Copyright © Esri. All rights reserved. For more information about Esri® software
Fattahi AM, Hosseini K, Farzin S, Mousavi SF (2023) An innovative approach of GSSHA model in flood analysis of large watersheds based on accuracy of DEM, size of grids, and stream density. Appl Water Sci 13(2):1–19. https://doi.org/10.1007/S13201-022-01838-6/FIGURES/24
Gad M, El-Safa A, Magda M, Farouk M, Hussein H, Alnemari AM, Elsayed S, Khalifa MM, Moghanm FS, Eid EM, Saleh AH (2021) Integration of water quality indices and multivariate modeling for assessing surface water quality in Qaroun lake Egypt. Water 13(16):2258. https://doi.org/10.3390/W13162258
García L, Barreiro-Gomez J, Escobar E, Téllez D, Quijano N, Ocampo-Martinez C (2015) Modeling and real-time control of urban drainage systems: a review. Adv Water Resour 85:120–132. https://doi.org/10.1016/J.ADVWATRES.2015.08.007
GAS (2024a) General authority for statistics. https://www.stats.gov.sa/en/node/10131
GAS (2024b) Population estimates | general authority for statistics. https://www.stats.gov.sa/en/43
GebreEgziabher M, Demissie Y (2020) Modeling urban flood inundation and recession impacted by manholes. Water. https://doi.org/10.3390/W12041160
Gomes MN, Lago CAF, Rápalo LMC, Oliveira PTS, Giacomoni MH, Mendiondo EM (2023) HydroPol2D—distributed hydrodynamic and water quality model: challenges and opportunities in poorly-gauged catchments. J Hydrol. https://doi.org/10.1016/j.jhydrol.2023.129982
Gorgoglione A, Gioia A, Iacobellis V (2019) A framework for assessing modeling performance and effects of rainfall-catchment-drainage characteristics on nutrient urban runoff in poorly gauged watersheds. Sustainability. https://doi.org/10.3390/SU11184933
Han J, He S (2021) Urban flooding events pose risks of virus spread during the novel coronavirus (COVID-19) pandemic. Sci Total Environ 755:142491. https://doi.org/10.1016/J.SCITOTENV.2020.142491
Hengl T, De Jesus JM, Heuvelink GBM, Gonzalez MR, Kilibarda M, Blagotić A, Shangguan W, Wright MN, Geng X, Bauer-Marschallinger B, Guevara MA, Vargas R, MacMillan RA, Batjes NH, Leenaars JGB, Ribeiro E, Wheeler I, Mantel S, Kempen B (2017) SoilGrids250m: global gridded soil information based on machine learning. PLoS ONE. https://doi.org/10.1371/journal.pone.0169748
Jang SH, Oh KD, Jo JW (2020) Application of the GSSHA model for the long-term simulation of discharge and water quality at the Peace dam. J Korea Water Resour Assoc 53(5):357–367. https://doi.org/10.3741/JKWRA.2020.53.5.357
Jamei M, Ahmadianfar I, Karbasi M, Jawad AH, Farooque AA, Yaseen ZM (2021) The assessment of emerging data-intelligence technologies for modeling Mg +2 and SO 4−2 surface water quality. J Environ Manag 300:113774. https://doi.org/10.1016/J.JENVMAN.2021.113774
Johnson BE, Gerald TK (2006) Development of nutrient submodules for use in the gridded surface subsurface hydrologic analysis (GSSHA) distributed watershed model1. JAWRA J Am Water Resour Assoc 42(6):1503–1525. https://doi.org/10.1111/J.1752-1688.2006.TB06017.X
Keller AA, Garner K, Rao N, Knipping E, Thomas J (2023) Hydrological models for climate-based assessments at the watershed scale: a critical review of existing hydrologic and water quality models. Sci Total Environ 867:161209. https://doi.org/10.1016/J.SCITOTENV.2022.161209
Liu Y, Li H, Cui G, Cao Y (2020) Water quality attribution and simulation of non-point source pollution load flux in the Hulan river basin. Sci Rep 10(1):1–15. https://doi.org/10.1038/s41598-020-59980-7
MacroTrends (2020) Mecca, Saudi Arabia metro area population 1950–2020. https://www.macrotrends.net/global-metrics/cities/22426/mecca/population#google_vignette
Ogden FL, Raj Pradhan N, Downer CW, Zahner JA (2011) Relative importance of impervious area, drainage density, width function, and subsurface storm drainage on flood runoff from an urbanized catchment. Water Resour Res 47(12):12503. https://doi.org/10.1029/2011WR010550
Pathirana A, Dikman Maheng M, & Brdjanovic D (2011) A two-dimensional pollutant transport model for sewer overflow impact simulation. In: 12nd international conference on urban drainage, Porto Alegre/Brazil
Paudel M, Nelson EJ, Downer CW, Hotchkiss R (2011) Comparing the capability of distributed and lumped hydrologic models for analyzing the effects of land use change. J Hydroinf 13(3):461–473. https://doi.org/10.2166/HYDRO.2010.100
Peacher RD, Lerch RN, Schultz RC, Willett CD, Isenhart TM (2018) Factors controlling streambank erosion and phosphorus loss in claypan watersheds. J Soil Water Conserv 73(2):189–199. https://doi.org/10.2489/JSWC.73.2.189
Piro P, Saleh MM, Pirouz B, Turco M, Palermo SA (2023) Smart and innovative systems for urban flooding risk management. In: Proceedings—2023 IEEE 8th international conference on information and communication technologies for disaster management, ICT-DM 2023. https://doi.org/10.1109/ICT-DM58371.2023.10286951
Pongmala K, Autixier L, Madoux-Humery AS, Fuamba M, Galarneau M, Sauvé S, Prévost M, Dorner S (2015) Modelling total suspended solids, E. coli and carbamazepine, a tracer of wastewater contamination from combined sewer overflows. J Hydrol 531:830–839. https://doi.org/10.1016/J.JHYDROL.2015.10.042
Pradhan NR, Downer CW, Johnson BE (2014) A Physics based hydrologic modeling approach to simulate non-point source pollution for the purposes of calculating TMDLs and designing abatement measures. Pract Asp Comput Chem III:249–282. https://doi.org/10.1007/978-1-4899-7445-7_9
GSSHA primer—Gsshawiki (2024) https://www.gsshawiki.com/GSSHA_Primer
RCER (2004) Royal Comission for Jubail and Yanbu. I
Salih SQ, Alakili I, Beyaztas U, Shahid S, Yaseen ZM (2021) Prediction of dissolved oxygen, biochemical oxygen demand, and chemical oxygen demand using hydrometeorological variables: case study of Selangor river, Malaysia. Environ Dev Sustain 23(5):8027–8046. https://doi.org/10.1007/S10668-020-00927-3/TABLES/5
Schiff KC, Tiefenthaler LL, Bay SM, Greenstein DJ (2016) Effects of rainfall intensity and duration on the first flush from parking lots. Water 8(8):320. https://doi.org/10.3390/W8080320
Shaikh TA, Adjovu GE, Stephen H, Ahmad S (2023) impacts of urbanization on watershed hydrology and runoff water quality of a watershed: a review. In: World environmental and water resources congress 2023: adaptive planning and design in an age of risk and uncertainty–selected papers from world environmental and water resources congress pp. 1271–1283. https://doi.org/10.1061/9780784484852.116
Sharif HO, Al-Zahrani M, El Hassan A (2017) Physically, fully-distributed hydrologic simulations driven by GPM satellite rainfall over an urbanizing arid catchment in Saudi Arabia. Water 9(3):163. https://doi.org/10.3390/W9030163
Shen D, Huang S, Zhang Y, Zhou Y (2021) The source apportionment of N and P pollution in the surface waters of lowland urban area based on EEM-PARAFAC and PCA-APCS-MLR. Environ Res 197:111022. https://doi.org/10.1016/J.ENVRES.2021.111022
Sith R, Nadaoka K (2017) Comparison of SWAT and GSSHA for high time resolution prediction of stream flow and sediment concentration in a small agricultural watershed. Hydrology 4(2):27. https://doi.org/10.3390/hydrology4020027
Steissberg T, Johnson B, Zhang Z (2023) Eco-hydrology engineering design tool—clearwater capabilities—general constituents, nutrients, and contaminants. EGU23. https://doi.org/10.5194/EGUSPHERE-EGU23-12470
Taheriyoun M, Fallahi A, Nazari-Sharabian M, Fallahi S (2023) Optimization of best management practices to control runoff water quality in an urban watershed using a novel framework of embedding-response surface model. J Hydro-Environ Res 46:19–30. https://doi.org/10.1016/J.JHER.2022.11.003
Teixeira de Mello F, Sierra P, Moi DA, Alonso J, Lucas C, Suárez B, Alvareda E, Alvarez J, Andrade MS, Arimon L, Urtado L, Piperno A (2024) Effects of urbanization and accessibility to sanitation services on water quality in urban streams in Uruguay. Environ Monit Assess 196(2):1–15. https://doi.org/10.1007/S10661-024-12365-Z/METRICS
Tiyasha TTM, Yaseen ZM (2021) Deep learning for prediction of water quality index classification: tropical catchment environmental assessment. Nat Resour Res 30(6):4235–4254. https://doi.org/10.1007/S11053-021-09922-5/TABLES/6
Tsakiridis NL, Samarinas N, Kalopesa E, Zalidis GC (2023) Cognitive soil digital twin for monitoring the soil ecosystem: a conceptual framework. Soil Syst 7(4):88. https://doi.org/10.3390/SOILSYSTEMS7040088
USEPA (2020) Nutrient pollution | US EPA. https://www.epa.gov/nutrientpollution
Wan Mohtar WHM, Abdul Maulud KN, Muhammad NS, Sharil S, Yaseen ZM (2019) Spatial and temporal risk quotient based river assessment for water resources management. Environ Pollut 248:133–144. https://doi.org/10.1016/J.ENVPOL.2019.02.011
Wang S, Rao P, Yang D, Tang L (2020) A combination model for quantifying non-point source pollution based on land use type in a typical urbanized area. Water 12(3):1–18. https://doi.org/10.3390/w12030729
Yan H, Fernandez A, Zhu DZ, Zhang W, Loewen MR, van Duin B, Chen L, Mahmood K, Zhao S, Jia H (2022) Land cover based simulation of urban stormwater runoff and pollutant loading. J Environ Manag 303:114147. https://doi.org/10.1016/J.JENVMAN.2021.114147
Yan H, Zhu DZ, Loewen MR, Zhang W, Liang S, Ahmed S, van Duin B, Mahmood K, Zhao S (2023) Impact of rainfall characteristics on urban stormwater quality using data mining framework. Sci Total Environ 862:160689. https://doi.org/10.1016/J.SCITOTENV.2022.160689
Zahid WM (2007) Cost analysis of trickling-filtration and activated-sludge plants for the treatment of municipal wastewater treatment schemes. In: The 7th Saudi engineering conference, college of engineering, King Saud University, Riyadh
Download references
Acknowledgements
The authors would like to acknowledge the support provided by King Fahd University of Petroleum & Minerals (KFUPM) to complete this study.
No funding was received for conducting this study.
Author information
Authors and affiliations.
Interdisciplinary Research Center for Membranes and, Water Security (IRC-MWS), King Fahd University of Petroleum and Minerals (KFUPM), Dhahran, 31261, Saudi Arabia
A. M. Al-Areeq
Department of Civil and Environmental Engineering, King Fahd University of Petroleum and Minerals (KFUPM), Dhahran, Saudi Arabia
A. M. Al-Areeq, M. A. Al-Zahrani & S. Chowdhury
Interdisciplinary Research Center for Construction and Building Materials (IRC-CBM), King Fahd University of Petroleum and Minerals (KFUPM), Dhahran, Dhahran, 31261, Saudi Arabia
S. Chowdhury
Department of Civil and Environmental Engineering, University of Texas at San Antonio, San Antonio, TX, 78249, USA
H. O. Sharif
You can also search for this author in PubMed Google Scholar
Contributions
Ahmed Al-Areeq: Conceptualization, Methodology, Designed the remote sensing portion, Modeling, Writing—Original draft preparation. Muhammad Al-Zahrani: Supervision, Conceptualization, Modeling, Reviewing, and Editing. Shakhawat Chowdhury: Reviewing and Editing. Hatim Sharif : Reviewing and Editing.
Corresponding author
Correspondence to A. M. Al-Areeq .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Consent to participate
Consent to publish.
The research is scientifically consented to be published.
Ethical approval
The manuscript is conducted in the ethical manner advised by the.
targeted journal.
Additional information
Editorial responsibility: Samareh Mirkia.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Al-Areeq, A.M., Al-Zahrani, M.A., Chowdhury, S. et al. Development of hydrological based physical model for nutrients transport simulation: case study of Makkah city, Saudi Arabia. Int. J. Environ. Sci. Technol. (2024). https://doi.org/10.1007/s13762-024-05745-y
Download citation
Received : 22 May 2023
Revised : 17 February 2024
Accepted : 14 May 2024
Published : 26 May 2024
DOI : https://doi.org/10.1007/s13762-024-05745-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Urban water quality management
- Nutrient runoff simulation
- Hydrological simulation
- Urban flood pollution
- Sewer overflow analysis
- Find a journal
- Publish with us
- Track your research
Improving VOC control strategies in industrial parks based on emission behavior, environmental effects, and health risks: A case study through atmospheric measurement and emission inventory
- Zhang, Sidi
- Lv, Pingjiang
- Zhang, Weidong
- Zhang, Yong
- Zhang, Yunhuai
Industrial parks have a very important impact on regional economic development, but the extremely complex and relatively concentrated volatile organic compound (VOC) emissions from industrial parks also result in it being difficult to control VOCs. In this study, we took a large integrated industrial park in the upper reaches of the Yangtze River as an example, conducted a 1-year monitoring campaign of ambient air VOCs, and established a speciated VOC emission inventory based on the measured chemical profiles of the key industries. The comprehensive control index (CCI) of 125 VOCs was evaluated using the entropy weighting method based on comprehensive consideration of three aspects, namely, emission behavior, environmental effects, and health risks of VOCs, to identify priority VOC species and their key sources for VOC control in industrial parks. The total estimated VOC emissions in the industrial park in 2019 were 6446.96 t. Steel production, sewage treatment, natural gas chemical industry, pharmaceuticals, and industrial boilers were the main sources of VOC emissions. In terms of VOC components, halocarbons, aromatics, and OVOCs were the largest groups of VOCs emitted from the industrial park, accounting for 73.75 % of the total VOC emissions. Using the entropy weighting method, we evaluated the index weights of five parameters: emissions, ozone formation potential, secondary organic aerosol formation potential, hazard quotient, and lifetime cancer risk. Based on the CCI, five control levels for VOC species were further established. The VOC species in Level I and Level II, which contain species such as naphthalene, 2-chlorotoluene, benzene, acrolein, and chloroform, should be considered as extremely important priority control species. These results serve as a reference for the development of precise control strategies for VOCs in industrial parks.
- Speciated emission inventory;
- Health risk;
- Comprehensive control index (CCI);
- Industrial park
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Health Department HAI/AR Programs
- Cleaning in Global Healthcare Settings
- Infection Control Guidance
- Introduction to the Patient Notification Toolkit
HAI Prevention and Control for Healthcare
- Public Health and Policy Strategies
- HAI Prevention, Control and Outbreak Response for Public Health and Healthcare
- Prevention Epicenters
- Healthcare-Associated Infections - Community Interface Activity (HAIC)
HAIs: Reports and Data
- Preventing MDROs
- Laboratory Resources
- Antibiotic Prescribing and Use
- Antimicrobial Resistance
- Infection Control for Healthcare Providers
- Safe Injection Practices and Your Health
Methicillin-resistant Staphylococcus aureus (MRSA) Basics
Healthcare-Associated Infections (HAIs)

Laboratory Resources for HAIs

Research Gaps in Patient and Healthcare Personnel Safety
Related organisms & infections

About Acinetobacter
About Burkholderia cepacia complex
About Carbapenem-resistant Enterobacterales
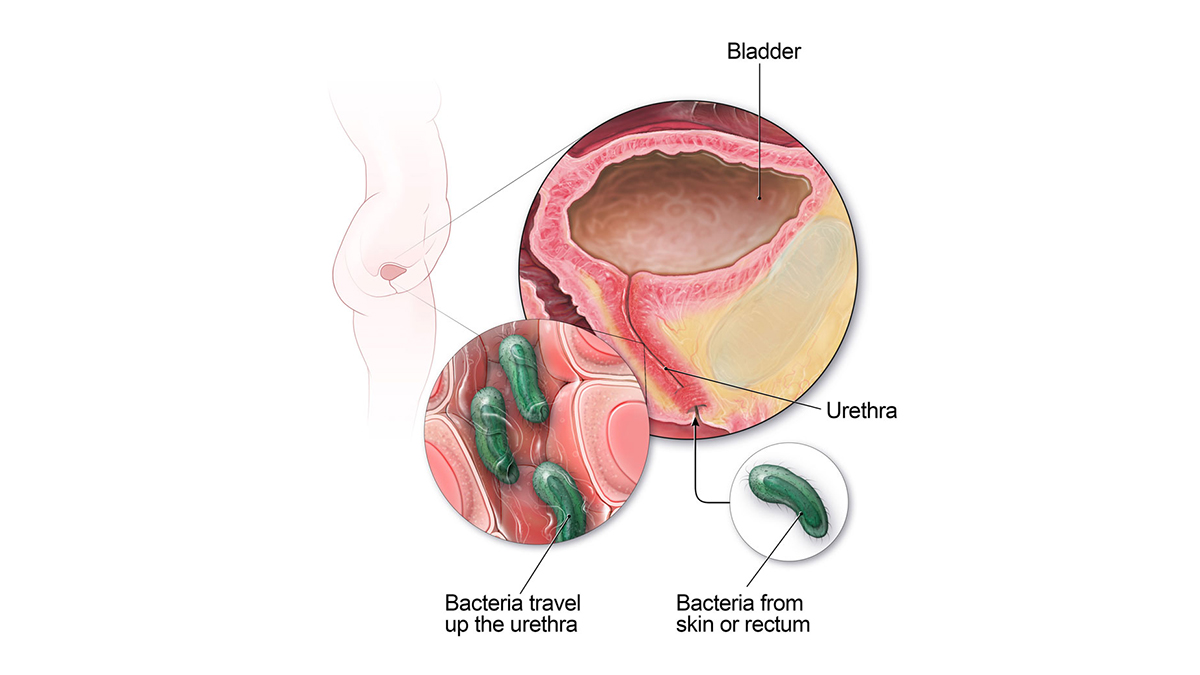
Catheter-associated Urinary Tract Infection Basics

Central Line-associated Bloodstream Infection (CLABSI) Basics
About Clostridium sordellii
About ESBL-producing Enterobacterales
About Gram-negative Bacteria
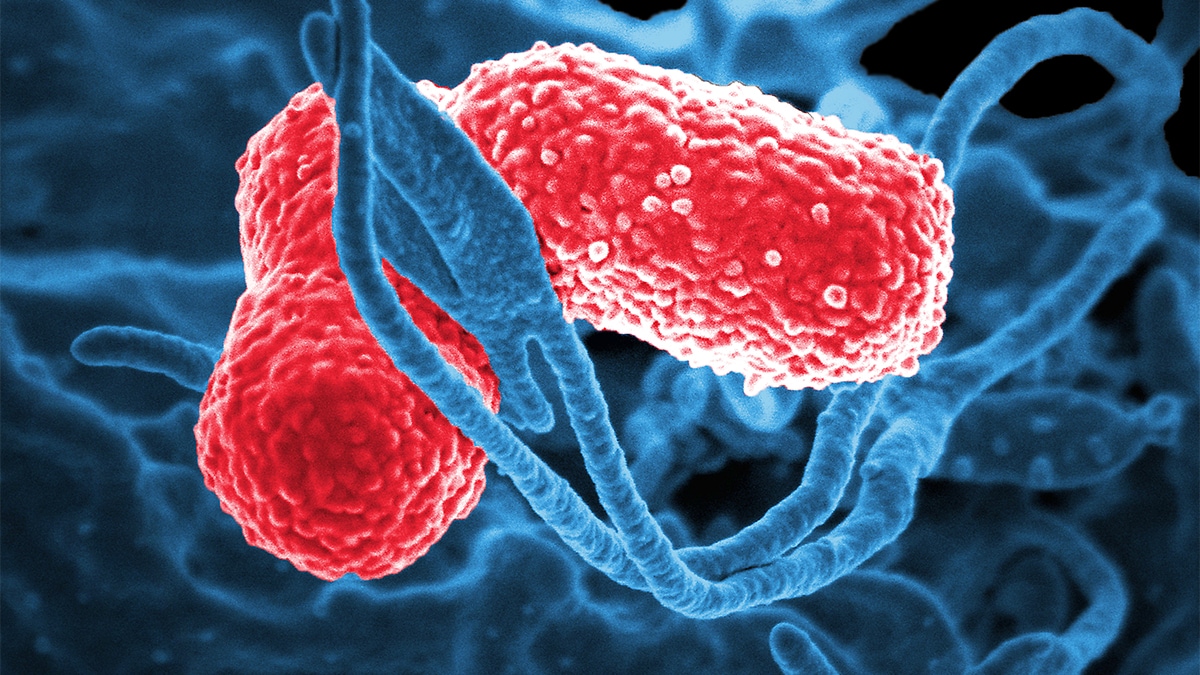
About Klebsiella
Staphylococcus aureus Basics
About Nontuberculous Mycobacteria (NTM) Infections

About Pseudomonas aeruginosa

Surgical Site Infection Basics

Ventilator-associated Pneumonia Basics
HAIs are associated with medical devices, complications following surgery, transmission between patients and healthcare workers, antibiotic overuse, and more.
For Everyone
Health care providers, public health.

COMMENTS
To date, however, an integrative view of environmental health in psychology is lacking, hampering urgently needed progress. In this paper, we review how the environment and human health are intertwined, and that much can be gained through a systemic view of environmental health in psychology. ... A case study of community engagement in mining ...
About the Journal. Case Studies in the Environment is the only journal exclusively devoted to publishing peer-reviewed environmental case study articles, as well as articles that focus on the pedagogy of using studies for in-class instruction or other purposes.The journal's overarching objective is to publish case studies that provide insights on critical environmental issues to students ...
These fourteen (14) case studies illustrate how assessors have developed and interpreted evidence to determine causes of biological impairments. They provide examples of how to organize an assessment report, analyze data, and present results. Most of the cases assess rivers and streams, but a few assess terrestrial ecosystems.
In the news. [Aug 2022] Read about the latest HIA case study completed for Southwest Rockford, IL . Health Impact Assessments. EPA has undertaken several Health Impact Assessment (HIA) case studies to learn how its science can be used in the HIA process and how HIA can be incorporated into its decision-support tools, actions, and mission.
Data are from the Environmental Protection Agency. ... time stratified case crossover study. BMJ 2021;375: ... multicity study. Environ Health Perspect 2019;127:97007-97007. Crossref. PubMed. ISI.
The association between environmental chemical exposures and chronic diseases is of increasing concern. Chemical risk assessment relies heavily on pre-market toxicity testing to identify safe levels of exposure, often known as reference doses (RfD), expected to be protective of human health. Although some RfDs have been reassessed in light of new hazard information, it is not a common practice.
Moreover, the public health motives for action have a strong science basis and are well evidenced and compelling. In this briefing pack, a series of case studies and opportunities for sharing experiences on climate change and health are highlighted across five priority areas of climate action: adaptation & resilience, energy transitions, nature ...
Climate change may be the greatest health threat of the twenty-first century, impacting lives both directly and indirectly, through undermining the environmental and social determinants of health.
Thus, the case of oxybenzone lends an excellent opportunity to apply these six principles of environmental health to a specific chemical that is used in consumer products to meet a specific need (protection from UV-induced damage), but with costs to human and environmental health that have been largely unexplored (Fig. 3). With the framework of ...
What should a climate & health case study look like? •Be solutions-driven:make sure your case study is a concrete and real-life example of progress being made on reducing emissions, building climate-resilient health systems, and/or protecting human health from the negative effects of climate change; •Be visual:share images, video or graphic ...
In conclusion, this study draws on environmental health problems that have been caused by the COVID-19 pandemic and presents the guiding principles for future environmental health research. It is expected that environmental health studies will function as a vigorous tool to safeguard and improve the well-being of the society, environment and ...
We propose six ethical principles to guide environmental health decision-making: principles of sustainability, beneficence, non-maleficence, justice, community, and precautionary substitution. ... Towards a paradigm shift in environmental health decision-making: a case study of oxybenzone Environ Health. 2022 Jan 8;21(1):6. doi: 10.1186/s12940 ...
Abstract. The failure by the city of Flint, Michigan to properly treat its municipal water system after a change in the source of water, has resulted in elevated lead levels in the city's water and an increase in city children's blood lead levels. Lead exposure in young children can lead to decrements in intelligence, development, behavior ...
Identification and characterization of environmental hazards that impact human health must rely on the best possible science to inform and inspire appropriate public health intervention. The perfluorinated alkylate substances (PFASs) are persistent emerging pollutants that are now being recognized as important human health hazards. Although the PFASs have been produced for over 60 years ...
CommunityHealthStudies.org. California DPH EHIB - An interactive website introducing users to environmental health issues and study designs using case studies. The website outlines when health studies may or may not be useful and also suggests alternative activities that can potentially improve the environmental health of a community.
Case-crossover design with daily environmental exposure and health outcomes (e.g., deaths and hospitalisations) is one of the most common study designs. It allows researchers to examine the acute health effects due to short-term environmental exposure. A case-crossover design utilizes the ID as a stratum, comparing individuals to themselves at ...
Description. This collection of cases covers topics related to Life and Environmental Science ethics including, agriculture ethics, bioethics, environmental ethics, and more. Cases come from a variety of online educational sources, ethics centers, and ethics programs.
Case Study in Environmental Medicine: Lead. Course: WB2832. CE Original Date: June 12, 2017. CE Renewal Date: June 12, 2019. CE Expiration Date: June 12, 2021. Introduction. The Lead case study/monograph is one in a series of self-instructional publications designed to increase primary care providers' and other health professional's ...
Cases Studies in Environmental Health and Ethics. 1) A recent study found 200 chemicals in cordblood (residual blood from the fetus following childbirth). The researcher explains that the presence of these chemicals was a surprise since we had always assumed (or hoped!) that the placenta would protect the fetus from any chemicals that the mom ...
In an online environmental health course, undergraduate students worked in teams of five and were immersed in a team-based climate change case study set in the Amazon rainforest. Each student was assigned a character role—a logger, a farmer, a conservation biologist, an environmental activist, and a policymaker. We aimed to understand whether student character assignments influenced their ...
The COVID-19 pandemic and related lockdowns around the world led to a general decline in physical and mental health because of isolation, lack of social interaction, restriction of movement and travel, and dramatic lifestyle changes [].The COVID-19 pandemic also demonstrated the importance of having access to green and blue spaces for human health and well-being during pandemics [2,3,4].
The mission of the National Institute of Environmental Health Sciences is to discover how the environment affects people in order to promote healthier lives. ... A use case working group is intended to be time-limited and comprised of self-selected community members, led by a "champion" who is a subject matter expert, that works ...
As a result of the research and case studies presented and discussions among conference participants, the following recommendations for action have been developed. ... Environmental, climate and health issues are driven by the same fundamental structural determinants in societies. Health promotion and education for sustainable development or ...
Study area. The study area (36° 26′∼36°2 9′ N, 104°1 7′∼104° 22'′ E) is located in the Dongdagou watershed, which is a significant agricultural area in the upper reaches of the Yellow River within the Baiyin district of northwest China (Fig. 1).This area is of great agricultural significance because it is responsible for the production of most of the grains consumed by the ...
Content source: Agency for Toxic Substances and Disease Registry. The Case Studies in Environmental Medicine (CSEM) are self-instructional, continuing-education primers designed to increase primary care providers' knowledge of hazardous substances and aid in the evaluation of patients potentially exposed to hazardous substances.
New study in Nature says last summer was the Northern Hemisphere's hottest in 2,000 years. Experts look at ways to mitigate health effects of extreme heat. ... Michigan reports a human case of ...
Urban flooding poses significant risks to water quality and public health due to inadequate drainage systems, leading to the dispersion of harmful pollutants in the neighborhoods. This study investigates the transport of nutrients during the flood events in Makkah (Saudi Arabia), underlining the city's vulnerability to such environmental challenges as a pressing concern. The research aims to ...
Industrial parks have a very important impact on regional economic development, but the extremely complex and relatively concentrated volatile organic compound (VOC) emissions from industrial parks also result in it being difficult to control VOCs. In this study, we took a large integrated industrial park in the upper reaches of the Yangtze River as an example, conducted a 1-year monitoring ...
Scientists Discover Microplastics Abound in Human Testicles. WEDNESDAY, May 22, 2024 (HealthDay News) -- In a finding that suggests microplastics may pose a special danger to men, a new study has shown that human testicles contain these tiny bits of plastic at levels triple that seen in animal testicles and human placentas.
HAIs: Reports and Data. CDC publishes data reports to help track progress and target areas that need assistance. HAI Prevention and Control for Healthcare. HAI Prevention, Control and Outbreak Response for Public Health and Healthcare. Introduction to the Patient Notification Toolkit. Laboratory Resources for HAIs.