Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- What Is Peer Review? | Types & Examples

What Is Peer Review? | Types & Examples
Published on December 17, 2021 by Tegan George . Revised on June 22, 2023.
Peer review, sometimes referred to as refereeing , is the process of evaluating submissions to an academic journal. Using strict criteria, a panel of reviewers in the same subject area decides whether to accept each submission for publication.
Peer-reviewed articles are considered a highly credible source due to the stringent process they go through before publication.
There are various types of peer review. The main difference between them is to what extent the authors, reviewers, and editors know each other’s identities. The most common types are:
- Single-blind review
- Double-blind review
- Triple-blind review
Collaborative review
Open review.
Relatedly, peer assessment is a process where your peers provide you with feedback on something you’ve written, based on a set of criteria or benchmarks from an instructor. They then give constructive feedback, compliments, or guidance to help you improve your draft.
Table of contents
What is the purpose of peer review, types of peer review, the peer review process, providing feedback to your peers, peer review example, advantages of peer review, criticisms of peer review, other interesting articles, frequently asked questions about peer reviews.
Many academic fields use peer review, largely to determine whether a manuscript is suitable for publication. Peer review enhances the credibility of the manuscript. For this reason, academic journals are among the most credible sources you can refer to.
However, peer review is also common in non-academic settings. The United Nations, the European Union, and many individual nations use peer review to evaluate grant applications. It is also widely used in medical and health-related fields as a teaching or quality-of-care measure.
Peer assessment is often used in the classroom as a pedagogical tool. Both receiving feedback and providing it are thought to enhance the learning process, helping students think critically and collaboratively.
Prevent plagiarism. Run a free check.
Depending on the journal, there are several types of peer review.
Single-blind peer review
The most common type of peer review is single-blind (or single anonymized) review . Here, the names of the reviewers are not known by the author.
While this gives the reviewers the ability to give feedback without the possibility of interference from the author, there has been substantial criticism of this method in the last few years. Many argue that single-blind reviewing can lead to poaching or intellectual theft or that anonymized comments cause reviewers to be too harsh.
Double-blind peer review
In double-blind (or double anonymized) review , both the author and the reviewers are anonymous.
Arguments for double-blind review highlight that this mitigates any risk of prejudice on the side of the reviewer, while protecting the nature of the process. In theory, it also leads to manuscripts being published on merit rather than on the reputation of the author.
Triple-blind peer review
While triple-blind (or triple anonymized) review —where the identities of the author, reviewers, and editors are all anonymized—does exist, it is difficult to carry out in practice.
Proponents of adopting triple-blind review for journal submissions argue that it minimizes potential conflicts of interest and biases. However, ensuring anonymity is logistically challenging, and current editing software is not always able to fully anonymize everyone involved in the process.
In collaborative review , authors and reviewers interact with each other directly throughout the process. However, the identity of the reviewer is not known to the author. This gives all parties the opportunity to resolve any inconsistencies or contradictions in real time, and provides them a rich forum for discussion. It can mitigate the need for multiple rounds of editing and minimize back-and-forth.
Collaborative review can be time- and resource-intensive for the journal, however. For these collaborations to occur, there has to be a set system in place, often a technological platform, with staff monitoring and fixing any bugs or glitches.
Lastly, in open review , all parties know each other’s identities throughout the process. Often, open review can also include feedback from a larger audience, such as an online forum, or reviewer feedback included as part of the final published product.
While many argue that greater transparency prevents plagiarism or unnecessary harshness, there is also concern about the quality of future scholarship if reviewers feel they have to censor their comments.
In general, the peer review process includes the following steps:
- First, the author submits the manuscript to the editor.
- Reject the manuscript and send it back to the author, or
- Send it onward to the selected peer reviewer(s)
- Next, the peer review process occurs. The reviewer provides feedback, addressing any major or minor issues with the manuscript, and gives their advice regarding what edits should be made.
- Lastly, the edited manuscript is sent back to the author. They input the edits and resubmit it to the editor for publication.

In an effort to be transparent, many journals are now disclosing who reviewed each article in the published product. There are also increasing opportunities for collaboration and feedback, with some journals allowing open communication between reviewers and authors.
It can seem daunting at first to conduct a peer review or peer assessment. If you’re not sure where to start, there are several best practices you can use.
Summarize the argument in your own words
Summarizing the main argument helps the author see how their argument is interpreted by readers, and gives you a jumping-off point for providing feedback. If you’re having trouble doing this, it’s a sign that the argument needs to be clearer, more concise, or worded differently.
If the author sees that you’ve interpreted their argument differently than they intended, they have an opportunity to address any misunderstandings when they get the manuscript back.
Separate your feedback into major and minor issues
It can be challenging to keep feedback organized. One strategy is to start out with any major issues and then flow into the more minor points. It’s often helpful to keep your feedback in a numbered list, so the author has concrete points to refer back to.
Major issues typically consist of any problems with the style, flow, or key points of the manuscript. Minor issues include spelling errors, citation errors, or other smaller, easy-to-apply feedback.
Tip: Try not to focus too much on the minor issues. If the manuscript has a lot of typos, consider making a note that the author should address spelling and grammar issues, rather than going through and fixing each one.
The best feedback you can provide is anything that helps them strengthen their argument or resolve major stylistic issues.
Give the type of feedback that you would like to receive
No one likes being criticized, and it can be difficult to give honest feedback without sounding overly harsh or critical. One strategy you can use here is the “compliment sandwich,” where you “sandwich” your constructive criticism between two compliments.
Be sure you are giving concrete, actionable feedback that will help the author submit a successful final draft. While you shouldn’t tell them exactly what they should do, your feedback should help them resolve any issues they may have overlooked.
As a rule of thumb, your feedback should be:
- Easy to understand
- Constructive
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

Below is a brief annotated research example. You can view examples of peer feedback by hovering over the highlighted sections.
Influence of phone use on sleep
Studies show that teens from the US are getting less sleep than they were a decade ago (Johnson, 2019) . On average, teens only slept for 6 hours a night in 2021, compared to 8 hours a night in 2011. Johnson mentions several potential causes, such as increased anxiety, changed diets, and increased phone use.
The current study focuses on the effect phone use before bedtime has on the number of hours of sleep teens are getting.
For this study, a sample of 300 teens was recruited using social media, such as Facebook, Instagram, and Snapchat. The first week, all teens were allowed to use their phone the way they normally would, in order to obtain a baseline.
The sample was then divided into 3 groups:
- Group 1 was not allowed to use their phone before bedtime.
- Group 2 used their phone for 1 hour before bedtime.
- Group 3 used their phone for 3 hours before bedtime.
All participants were asked to go to sleep around 10 p.m. to control for variation in bedtime . In the morning, their Fitbit showed the number of hours they’d slept. They kept track of these numbers themselves for 1 week.
Two independent t tests were used in order to compare Group 1 and Group 2, and Group 1 and Group 3. The first t test showed no significant difference ( p > .05) between the number of hours for Group 1 ( M = 7.8, SD = 0.6) and Group 2 ( M = 7.0, SD = 0.8). The second t test showed a significant difference ( p < .01) between the average difference for Group 1 ( M = 7.8, SD = 0.6) and Group 3 ( M = 6.1, SD = 1.5).
This shows that teens sleep fewer hours a night if they use their phone for over an hour before bedtime, compared to teens who use their phone for 0 to 1 hours.
Peer review is an established and hallowed process in academia, dating back hundreds of years. It provides various fields of study with metrics, expectations, and guidance to ensure published work is consistent with predetermined standards.
- Protects the quality of published research
Peer review can stop obviously problematic, falsified, or otherwise untrustworthy research from being published. Any content that raises red flags for reviewers can be closely examined in the review stage, preventing plagiarized or duplicated research from being published.
- Gives you access to feedback from experts in your field
Peer review represents an excellent opportunity to get feedback from renowned experts in your field and to improve your writing through their feedback and guidance. Experts with knowledge about your subject matter can give you feedback on both style and content, and they may also suggest avenues for further research that you hadn’t yet considered.
- Helps you identify any weaknesses in your argument
Peer review acts as a first defense, helping you ensure your argument is clear and that there are no gaps, vague terms, or unanswered questions for readers who weren’t involved in the research process. This way, you’ll end up with a more robust, more cohesive article.
While peer review is a widely accepted metric for credibility, it’s not without its drawbacks.
- Reviewer bias
The more transparent double-blind system is not yet very common, which can lead to bias in reviewing. A common criticism is that an excellent paper by a new researcher may be declined, while an objectively lower-quality submission by an established researcher would be accepted.
- Delays in publication
The thoroughness of the peer review process can lead to significant delays in publishing time. Research that was current at the time of submission may not be as current by the time it’s published. There is also high risk of publication bias , where journals are more likely to publish studies with positive findings than studies with negative findings.
- Risk of human error
By its very nature, peer review carries a risk of human error. In particular, falsification often cannot be detected, given that reviewers would have to replicate entire experiments to ensure the validity of results.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Normal distribution
- Measures of central tendency
- Chi square tests
- Confidence interval
- Quartiles & Quantiles
- Cluster sampling
- Stratified sampling
- Thematic analysis
- Discourse analysis
- Cohort study
- Ethnography
Research bias
- Implicit bias
- Cognitive bias
- Conformity bias
- Hawthorne effect
- Availability heuristic
- Attrition bias
- Social desirability bias
Peer review is a process of evaluating submissions to an academic journal. Utilizing rigorous criteria, a panel of reviewers in the same subject area decide whether to accept each submission for publication. For this reason, academic journals are often considered among the most credible sources you can use in a research project– provided that the journal itself is trustworthy and well-regarded.
In general, the peer review process follows the following steps:
- Reject the manuscript and send it back to author, or
- Send it onward to the selected peer reviewer(s)
- Next, the peer review process occurs. The reviewer provides feedback, addressing any major or minor issues with the manuscript, and gives their advice regarding what edits should be made.
- Lastly, the edited manuscript is sent back to the author. They input the edits, and resubmit it to the editor for publication.
Peer review can stop obviously problematic, falsified, or otherwise untrustworthy research from being published. It also represents an excellent opportunity to get feedback from renowned experts in your field. It acts as a first defense, helping you ensure your argument is clear and that there are no gaps, vague terms, or unanswered questions for readers who weren’t involved in the research process.
Peer-reviewed articles are considered a highly credible source due to this stringent process they go through before publication.
Many academic fields use peer review , largely to determine whether a manuscript is suitable for publication. Peer review enhances the credibility of the published manuscript.
However, peer review is also common in non-academic settings. The United Nations, the European Union, and many individual nations use peer review to evaluate grant applications. It is also widely used in medical and health-related fields as a teaching or quality-of-care measure.
A credible source should pass the CRAAP test and follow these guidelines:
- The information should be up to date and current.
- The author and publication should be a trusted authority on the subject you are researching.
- The sources the author cited should be easy to find, clear, and unbiased.
- For a web source, the URL and layout should signify that it is trustworthy.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
George, T. (2023, June 22). What Is Peer Review? | Types & Examples. Scribbr. Retrieved August 21, 2024, from https://www.scribbr.com/methodology/peer-review/
Is this article helpful?
Tegan George
Other students also liked, what are credible sources & how to spot them | examples, ethical considerations in research | types & examples, applying the craap test & evaluating sources, get unlimited documents corrected.
✔ Free APA citation check included ✔ Unlimited document corrections ✔ Specialized in correcting academic texts

- Science Notes Posts
- Contact Science Notes
- Todd Helmenstine Biography
- Anne Helmenstine Biography
- Free Printable Periodic Tables (PDF and PNG)
- Periodic Table Wallpapers
- Interactive Periodic Table
- Periodic Table Posters
- Science Experiments for Kids
- How to Grow Crystals
- Chemistry Projects
- Fire and Flames Projects
- Holiday Science
- Chemistry Problems With Answers
- Physics Problems
- Unit Conversion Example Problems
- Chemistry Worksheets
- Biology Worksheets
- Periodic Table Worksheets
- Physical Science Worksheets
- Science Lab Worksheets
- My Amazon Books
Understanding Peer Review in Science

Peer review is an essential element of the scientific publishing process that helps ensure that research articles are evaluated, critiqued, and improved before release into the academic community. Take a look at the significance of peer review in scientific publications, the typical steps of the process, and and how to approach peer review if you are asked to assess a manuscript.
What Is Peer Review?
Peer review is the evaluation of work by peers, who are people with comparable experience and competency. Peers assess each others’ work in educational settings, in professional settings, and in the publishing world. The goal of peer review is improving quality, defining and maintaining standards, and helping people learn from one another.
In the context of scientific publication, peer review helps editors determine which submissions merit publication and improves the quality of manuscripts prior to their final release.
Types of Peer Review for Manuscripts
There are three main types of peer review:
- Single-blind review: The reviewers know the identities of the authors, but the authors do not know the identities of the reviewers.
- Double-blind review: Both the authors and reviewers remain anonymous to each other.
- Open peer review: The identities of both the authors and reviewers are disclosed, promoting transparency and collaboration.
There are advantages and disadvantages of each method. Anonymous reviews reduce bias but reduce collaboration, while open reviews are more transparent, but increase bias.
Key Elements of Peer Review
Proper selection of a peer group improves the outcome of the process:
- Expertise : Reviewers should possess adequate knowledge and experience in the relevant field to provide constructive feedback.
- Objectivity : Reviewers assess the manuscript impartially and without personal bias.
- Confidentiality : The peer review process maintains confidentiality to protect intellectual property and encourage honest feedback.
- Timeliness : Reviewers provide feedback within a reasonable timeframe to ensure timely publication.
Steps of the Peer Review Process
The typical peer review process for scientific publications involves the following steps:
- Submission : Authors submit their manuscript to a journal that aligns with their research topic.
- Editorial assessment : The journal editor examines the manuscript and determines whether or not it is suitable for publication. If it is not, the manuscript is rejected.
- Peer review : If it is suitable, the editor sends the article to peer reviewers who are experts in the relevant field.
- Reviewer feedback : Reviewers provide feedback, critique, and suggestions for improvement.
- Revision and resubmission : Authors address the feedback and make necessary revisions before resubmitting the manuscript.
- Final decision : The editor makes a final decision on whether to accept or reject the manuscript based on the revised version and reviewer comments.
- Publication : If accepted, the manuscript undergoes copyediting and formatting before being published in the journal.
Pros and Cons
While the goal of peer review is improving the quality of published research, the process isn’t without its drawbacks.
- Quality assurance : Peer review helps ensure the quality and reliability of published research.
- Error detection : The process identifies errors and flaws that the authors may have overlooked.
- Credibility : The scientific community generally considers peer-reviewed articles to be more credible.
- Professional development : Reviewers can learn from the work of others and enhance their own knowledge and understanding.
- Time-consuming : The peer review process can be lengthy, delaying the publication of potentially valuable research.
- Bias : Personal biases of reviews impact their evaluation of the manuscript.
- Inconsistency : Different reviewers may provide conflicting feedback, making it challenging for authors to address all concerns.
- Limited effectiveness : Peer review does not always detect significant errors or misconduct.
- Poaching : Some reviewers take an idea from a submission and gain publication before the authors of the original research.
Steps for Conducting Peer Review of an Article
Generally, an editor provides guidance when you are asked to provide peer review of a manuscript. Here are typical steps of the process.
- Accept the right assignment: Accept invitations to review articles that align with your area of expertise to ensure you can provide well-informed feedback.
- Manage your time: Allocate sufficient time to thoroughly read and evaluate the manuscript, while adhering to the journal’s deadline for providing feedback.
- Read the manuscript multiple times: First, read the manuscript for an overall understanding of the research. Then, read it more closely to assess the details, methodology, results, and conclusions.
- Evaluate the structure and organization: Check if the manuscript follows the journal’s guidelines and is structured logically, with clear headings, subheadings, and a coherent flow of information.
- Assess the quality of the research: Evaluate the research question, study design, methodology, data collection, analysis, and interpretation. Consider whether the methods are appropriate, the results are valid, and the conclusions are supported by the data.
- Examine the originality and relevance: Determine if the research offers new insights, builds on existing knowledge, and is relevant to the field.
- Check for clarity and consistency: Review the manuscript for clarity of writing, consistent terminology, and proper formatting of figures, tables, and references.
- Identify ethical issues: Look for potential ethical concerns, such as plagiarism, data fabrication, or conflicts of interest.
- Provide constructive feedback: Offer specific, actionable, and objective suggestions for improvement, highlighting both the strengths and weaknesses of the manuscript. Don’t be mean.
- Organize your review: Structure your review with an overview of your evaluation, followed by detailed comments and suggestions organized by section (e.g., introduction, methods, results, discussion, and conclusion).
- Be professional and respectful: Maintain a respectful tone in your feedback, avoiding personal criticism or derogatory language.
- Proofread your review: Before submitting your review, proofread it for typos, grammar, and clarity.
- Couzin-Frankel J (September 2013). “Biomedical publishing. Secretive and subjective, peer review proves resistant to study”. Science . 341 (6152): 1331. doi: 10.1126/science.341.6152.1331
- Lee, Carole J.; Sugimoto, Cassidy R.; Zhang, Guo; Cronin, Blaise (2013). “Bias in peer review”. Journal of the American Society for Information Science and Technology. 64 (1): 2–17. doi: 10.1002/asi.22784
- Slavov, Nikolai (2015). “Making the most of peer review”. eLife . 4: e12708. doi: 10.7554/eLife.12708
- Spier, Ray (2002). “The history of the peer-review process”. Trends in Biotechnology . 20 (8): 357–8. doi: 10.1016/S0167-7799(02)01985-6
- Squazzoni, Flaminio; Brezis, Elise; Marušić, Ana (2017). “Scientometrics of peer review”. Scientometrics . 113 (1): 501–502. doi: 10.1007/s11192-017-2518-4
Related Posts
You are using an outdated browser . Please upgrade your browser today !
What Is Peer Review and Why Is It Important?
It’s one of the major cornerstones of the academic process and critical to maintaining rigorous quality standards for research papers. Whichever side of the peer review process you’re on, we want to help you understand the steps involved.
This post is part of a series that provides practical information and resources for authors and editors.
Peer review – the evaluation of academic research by other experts in the same field – has been used by the scientific community as a method of ensuring novelty and quality of research for more than 300 years. It is a testament to the power of peer review that a scientific hypothesis or statement presented to the world is largely ignored by the scholarly community unless it is first published in a peer-reviewed journal.
It is also safe to say that peer review is a critical element of the scholarly publication process and one of the major cornerstones of the academic process. It acts as a filter, ensuring that research is properly verified before being published. And it arguably improves the quality of the research, as the rigorous review by like-minded experts helps to refine or emphasise key points and correct inadvertent errors.
Ideally, this process encourages authors to meet the accepted standards of their discipline and in turn reduces the dissemination of irrelevant findings, unwarranted claims, unacceptable interpretations, and personal views.
If you are a researcher, you will come across peer review many times in your career. But not every part of the process might be clear to you yet. So, let’s have a look together!
Types of Peer Review
Peer review comes in many different forms. With single-blind peer review , the names of the reviewers are hidden from the authors, while double-blind peer review , both reviewers and authors remain anonymous. Then, there is open peer review , a term which offers more than one interpretation nowadays.
Open peer review can simply mean that reviewer and author identities are revealed to each other. It can also mean that a journal makes the reviewers’ reports and author replies of published papers publicly available (anonymized or not). The “open” in open peer review can even be a call for participation, where fellow researchers are invited to proactively comment on a freely accessible pre-print article. The latter two options are not yet widely used, but the Open Science movement, which strives for more transparency in scientific publishing, has been giving them a strong push over the last years.
If you are unsure about what kind of peer review a specific journal conducts, check out its instructions for authors and/or their editorial policy on the journal’s home page.
Why Should I Even Review?
To answer that question, many reviewers would probably reply that it simply is their “academic duty” – a natural part of academia, an important mechanism to monitor the quality of published research in their field. This is of course why the peer-review system was developed in the first place – by academia rather than the publishers – but there are also benefits.
Are you looking for the right place to publish your paper? Find out here whether a De Gruyter journal might be the right fit.
Besides a general interest in the field, reviewing also helps researchers keep up-to-date with the latest developments. They get to know about new research before everyone else does. It might help with their own research and/or stimulate new ideas. On top of that, reviewing builds relationships with prestigious journals and journal editors.
Clearly, reviewing is also crucial for the development of a scientific career, especially in the early stages. Relatively new services like Publons and ORCID Reviewer Recognition can support reviewers in getting credit for their efforts and making their contributions more visible to the wider community.
The Fundamentals of Reviewing
You have received an invitation to review? Before agreeing to do so, there are three pertinent questions you should ask yourself:
- Does the article you are being asked to review match your expertise?
- Do you have time to review the paper?
- Are there any potential conflicts of interest (e.g. of financial or personal nature)?
If you feel like you cannot handle the review for whatever reason, it is okay to decline. If you can think of a colleague who would be well suited for the topic, even better – suggest them to the journal’s editorial office.
But let’s assume that you have accepted the request. Here are some general things to keep in mind:
Please be aware that reviewer reports provide advice for editors to assist them in reaching a decision on a submitted paper. The final decision concerning a manuscript does not lie with you, but ultimately with the editor. It’s your expert guidance that is being sought.
Reviewing also needs to be conducted confidentially . The article you have been asked to review, including supplementary material, must never be disclosed to a third party. In the traditional single- or double-blind peer review process, your own anonymity will also be strictly preserved. Therefore, you should not communicate directly with the authors.
When writing a review, it is important to keep the journal’s guidelines in mind and to work along the building blocks of a manuscript (typically: abstract, introduction, methods, results, discussion, conclusion, references, tables, figures).
After initial receipt of the manuscript, you will be asked to supply your feedback within a specified period (usually 2-4 weeks). If at some point you notice that you are running out of time, get in touch with the editorial office as soon as you can and ask whether an extension is possible.
Some More Advice from a Journal Editor
- Be critical and constructive. An editor will find it easier to overturn very critical, unconstructive comments than to overturn favourable comments.
- Justify and specify all criticisms. Make specific references to the text of the paper (use line numbers!) or to published literature. Vague criticisms are unhelpful.
- Don’t repeat information from the paper , for example, the title and authors names, as this information already appears elsewhere in the review form.
- Check the aims and scope. This will help ensure that your comments are in accordance with journal policy and can be found on its home page.
- Give a clear recommendation . Do not put “I will leave the decision to the editor” in your reply, unless you are genuinely unsure of your recommendation.
- Number your comments. This makes it easy for authors to easily refer to them.
- Be careful not to identify yourself. Check, for example, the file name of your report if you submit it as a Word file.
Sticking to these rules will make the author’s life and that of the editors much easier!
Explore new perspectives on peer review in this collection of blog posts published during Peer Review Week 2021

[Title image by AndreyPopov/iStock/Getty Images Plus
David Sleeman
David Sleeman worked as a Senior Journals Manager in the field of Physical Sciences at De Gruyter.
You might also be interested in
Academia & Publishing
Taking Libraries into the Future, Part 4: How IFLA Harnesses Social Media
10 summer reads for the intellectually curious, how to maximize your message through social media: a global masterclass from library professionals, visit our shop.
De Gruyter publishes over 1,300 new book titles each year and more than 750 journals in the humanities, social sciences, medicine, mathematics, engineering, computer sciences, natural sciences, and law.
Pin It on Pinterest
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Methodology
- What Is Peer Review? | Types & Examples
What Is Peer Review? | Types & Examples
Published on 6 May 2022 by Tegan George . Revised on 2 September 2022.
Peer review, sometimes referred to as refereeing , is the process of evaluating submissions to an academic journal. Using strict criteria, a panel of reviewers in the same subject area decides whether to accept each submission for publication.
Peer-reviewed articles are considered a highly credible source due to the stringent process they go through before publication.
There are various types of peer review. The main difference between them is to what extent the authors, reviewers, and editors know each other’s identities. The most common types are:
- Single-blind review
- Double-blind review
- Triple-blind review
Collaborative review
Open review.
Relatedly, peer assessment is a process where your peers provide you with feedback on something you’ve written, based on a set of criteria or benchmarks from an instructor. They then give constructive feedback, compliments, or guidance to help you improve your draft.
Table of contents
What is the purpose of peer review, types of peer review, the peer review process, providing feedback to your peers, peer review example, advantages of peer review, criticisms of peer review, frequently asked questions about peer review.
Many academic fields use peer review, largely to determine whether a manuscript is suitable for publication. Peer review enhances the credibility of the manuscript. For this reason, academic journals are among the most credible sources you can refer to.
However, peer review is also common in non-academic settings. The United Nations, the European Union, and many individual nations use peer review to evaluate grant applications. It is also widely used in medical and health-related fields as a teaching or quality-of-care measure.
Peer assessment is often used in the classroom as a pedagogical tool. Both receiving feedback and providing it are thought to enhance the learning process, helping students think critically and collaboratively.
Prevent plagiarism, run a free check.
Depending on the journal, there are several types of peer review.
Single-blind peer review
The most common type of peer review is single-blind (or single anonymised) review . Here, the names of the reviewers are not known by the author.
While this gives the reviewers the ability to give feedback without the possibility of interference from the author, there has been substantial criticism of this method in the last few years. Many argue that single-blind reviewing can lead to poaching or intellectual theft or that anonymised comments cause reviewers to be too harsh.
Double-blind peer review
In double-blind (or double anonymised) review , both the author and the reviewers are anonymous.
Arguments for double-blind review highlight that this mitigates any risk of prejudice on the side of the reviewer, while protecting the nature of the process. In theory, it also leads to manuscripts being published on merit rather than on the reputation of the author.
Triple-blind peer review
While triple-blind (or triple anonymised) review – where the identities of the author, reviewers, and editors are all anonymised – does exist, it is difficult to carry out in practice.
Proponents of adopting triple-blind review for journal submissions argue that it minimises potential conflicts of interest and biases. However, ensuring anonymity is logistically challenging, and current editing software is not always able to fully anonymise everyone involved in the process.
In collaborative review , authors and reviewers interact with each other directly throughout the process. However, the identity of the reviewer is not known to the author. This gives all parties the opportunity to resolve any inconsistencies or contradictions in real time, and provides them a rich forum for discussion. It can mitigate the need for multiple rounds of editing and minimise back-and-forth.
Collaborative review can be time- and resource-intensive for the journal, however. For these collaborations to occur, there has to be a set system in place, often a technological platform, with staff monitoring and fixing any bugs or glitches.
Lastly, in open review , all parties know each other’s identities throughout the process. Often, open review can also include feedback from a larger audience, such as an online forum, or reviewer feedback included as part of the final published product.
While many argue that greater transparency prevents plagiarism or unnecessary harshness, there is also concern about the quality of future scholarship if reviewers feel they have to censor their comments.
In general, the peer review process includes the following steps:
- First, the author submits the manuscript to the editor.
- Reject the manuscript and send it back to the author, or
- Send it onward to the selected peer reviewer(s)
- Next, the peer review process occurs. The reviewer provides feedback, addressing any major or minor issues with the manuscript, and gives their advice regarding what edits should be made.
- Lastly, the edited manuscript is sent back to the author. They input the edits and resubmit it to the editor for publication.

In an effort to be transparent, many journals are now disclosing who reviewed each article in the published product. There are also increasing opportunities for collaboration and feedback, with some journals allowing open communication between reviewers and authors.
It can seem daunting at first to conduct a peer review or peer assessment. If you’re not sure where to start, there are several best practices you can use.
Summarise the argument in your own words
Summarising the main argument helps the author see how their argument is interpreted by readers, and gives you a jumping-off point for providing feedback. If you’re having trouble doing this, it’s a sign that the argument needs to be clearer, more concise, or worded differently.
If the author sees that you’ve interpreted their argument differently than they intended, they have an opportunity to address any misunderstandings when they get the manuscript back.
Separate your feedback into major and minor issues
It can be challenging to keep feedback organised. One strategy is to start out with any major issues and then flow into the more minor points. It’s often helpful to keep your feedback in a numbered list, so the author has concrete points to refer back to.
Major issues typically consist of any problems with the style, flow, or key points of the manuscript. Minor issues include spelling errors, citation errors, or other smaller, easy-to-apply feedback.
The best feedback you can provide is anything that helps them strengthen their argument or resolve major stylistic issues.
Give the type of feedback that you would like to receive
No one likes being criticised, and it can be difficult to give honest feedback without sounding overly harsh or critical. One strategy you can use here is the ‘compliment sandwich’, where you ‘sandwich’ your constructive criticism between two compliments.
Be sure you are giving concrete, actionable feedback that will help the author submit a successful final draft. While you shouldn’t tell them exactly what they should do, your feedback should help them resolve any issues they may have overlooked.
As a rule of thumb, your feedback should be:
- Easy to understand
- Constructive
Below is a brief annotated research example. You can view examples of peer feedback by hovering over the highlighted sections.
Influence of phone use on sleep
Studies show that teens from the US are getting less sleep than they were a decade ago (Johnson, 2019) . On average, teens only slept for 6 hours a night in 2021, compared to 8 hours a night in 2011. Johnson mentions several potential causes, such as increased anxiety, changed diets, and increased phone use.
The current study focuses on the effect phone use before bedtime has on the number of hours of sleep teens are getting.
For this study, a sample of 300 teens was recruited using social media, such as Facebook, Instagram, and Snapchat. The first week, all teens were allowed to use their phone the way they normally would, in order to obtain a baseline.
The sample was then divided into 3 groups:
- Group 1 was not allowed to use their phone before bedtime.
- Group 2 used their phone for 1 hour before bedtime.
- Group 3 used their phone for 3 hours before bedtime.
All participants were asked to go to sleep around 10 p.m. to control for variation in bedtime . In the morning, their Fitbit showed the number of hours they’d slept. They kept track of these numbers themselves for 1 week.
Two independent t tests were used in order to compare Group 1 and Group 2, and Group 1 and Group 3. The first t test showed no significant difference ( p > .05) between the number of hours for Group 1 ( M = 7.8, SD = 0.6) and Group 2 ( M = 7.0, SD = 0.8). The second t test showed a significant difference ( p < .01) between the average difference for Group 1 ( M = 7.8, SD = 0.6) and Group 3 ( M = 6.1, SD = 1.5).
This shows that teens sleep fewer hours a night if they use their phone for over an hour before bedtime, compared to teens who use their phone for 0 to 1 hours.
Peer review is an established and hallowed process in academia, dating back hundreds of years. It provides various fields of study with metrics, expectations, and guidance to ensure published work is consistent with predetermined standards.
- Protects the quality of published research
Peer review can stop obviously problematic, falsified, or otherwise untrustworthy research from being published. Any content that raises red flags for reviewers can be closely examined in the review stage, preventing plagiarised or duplicated research from being published.
- Gives you access to feedback from experts in your field
Peer review represents an excellent opportunity to get feedback from renowned experts in your field and to improve your writing through their feedback and guidance. Experts with knowledge about your subject matter can give you feedback on both style and content, and they may also suggest avenues for further research that you hadn’t yet considered.
- Helps you identify any weaknesses in your argument
Peer review acts as a first defence, helping you ensure your argument is clear and that there are no gaps, vague terms, or unanswered questions for readers who weren’t involved in the research process. This way, you’ll end up with a more robust, more cohesive article.
While peer review is a widely accepted metric for credibility, it’s not without its drawbacks.
- Reviewer bias
The more transparent double-blind system is not yet very common, which can lead to bias in reviewing. A common criticism is that an excellent paper by a new researcher may be declined, while an objectively lower-quality submission by an established researcher would be accepted.
- Delays in publication
The thoroughness of the peer review process can lead to significant delays in publishing time. Research that was current at the time of submission may not be as current by the time it’s published.
- Risk of human error
By its very nature, peer review carries a risk of human error. In particular, falsification often cannot be detected, given that reviewers would have to replicate entire experiments to ensure the validity of results.
Peer review is a process of evaluating submissions to an academic journal. Utilising rigorous criteria, a panel of reviewers in the same subject area decide whether to accept each submission for publication.
For this reason, academic journals are often considered among the most credible sources you can use in a research project – provided that the journal itself is trustworthy and well regarded.
Peer review can stop obviously problematic, falsified, or otherwise untrustworthy research from being published. It also represents an excellent opportunity to get feedback from renowned experts in your field.
It acts as a first defence, helping you ensure your argument is clear and that there are no gaps, vague terms, or unanswered questions for readers who weren’t involved in the research process.
Peer-reviewed articles are considered a highly credible source due to this stringent process they go through before publication.
In general, the peer review process follows the following steps:
- Reject the manuscript and send it back to author, or
- Lastly, the edited manuscript is sent back to the author. They input the edits, and resubmit it to the editor for publication.
Many academic fields use peer review , largely to determine whether a manuscript is suitable for publication. Peer review enhances the credibility of the published manuscript.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
George, T. (2022, September 02). What Is Peer Review? | Types & Examples. Scribbr. Retrieved 21 August 2024, from https://www.scribbr.co.uk/research-methods/peer-reviews/
Is this article helpful?
Tegan George
Other students also liked, what is a double-blind study | introduction & examples, a quick guide to experimental design | 5 steps & examples, data cleaning | a guide with examples & steps.
- Harvard Library
- Research Guides
- Faculty of Arts & Sciences Libraries
Engineering and Applied Sciences Research Guide
What is peer review.
- Get Started
- Find Books in the SEC Library This link opens in a new window
- How to get the full-text
- Find Conference Proceedings
- Find Dissertations and Theses
- Find Patents This link opens in a new window
- Why use Standards?
- Find Technical Reports
- Find Videos
- ENG-SCI 298R Woodward Yang
- Master in Design Engineering Resources
- Environmental Science & Engineering (ESE)
- Research Data Management
- Ask a Librarian This link opens in a new window
| The tries to ensure that the highest quality research gets published. When an article is submitted to a peer-reviewed journal, the editor after deciding if the article meets the basic requirements for inclusion, sends it to be reviewed by other scholars (the author's peers) within the same field. These reviewers provide feedback to the editor to reject the paper, accept the paper as is, or accept the paper with author revisions. informs the public when articles are retracted due to various reasons, including plagiarism, error, and fraud. |
|
|
| Peer-reviewed articles may include some or all of these elements (individual mileage may vary):
|
| An article may be considered scholarly, for example, a conference proceeding or technical report, but you cannot assume it was peer-reviewed. Need help? Talk to a librarian! |
- << Previous: Find Articles
- Next: Find Books in the SEC Library >>
- Last Updated: Mar 6, 2024 5:16 PM
- URL: https://guides.library.harvard.edu/es
Harvard University Digital Accessibility Policy
- USU Library
Articles: Finding (and Identifying) Peer-Reviewed Articles: What is Peer Review?
- What is Peer Review?
- Finding Peer Reviewed Articles
- Databases That Can Determine Peer Review
Peer Review in 3 Minutes
What is "Peer-Review"?
What are they.
Scholarly articles are papers that describe a research study.
Why are scholarly articles useful?
They report original research projects that have been reviewed by other experts before they are accepted for publication, so you can reasonably be assured that they contain valid information.
How do you identify scholarly or peer-reviewed articles?
- They are usually fairly lengthy - most likely at least 7-10 pages
- The authors and their credentials should be identified, at least the company or university where the author is employed
- There is usually a list of References or Works Cited at the end of the paper, listing the sources that the authors used in their research
How do you find them?
Some of the library's databases contain scholarly articles, either exclusively or in combination with other types of articles.
Google Scholar is another option for searching for scholarly articles.
Know the Difference Between Scholarly and Popular Journals/Magazines
Peer reviewed articles are found in scholarly journals. The checklist below can help you determine if what you are looking at is peer reviewed or scholarly.
- Both kinds of journals and magazines can be useful sources of information.
- Popular magazines and newspapers are good for overviews, recent news, first-person accounts, and opinions about a topic.
- Scholarly journals, often called scientific or peer-reviewed journals, are good sources of actual studies or research conducted about a particular topic. They go through a process of review by experts, so the information is usually highly reliable.
| Author is an expert on the specific topic of the article | Author is usually a journalists who might or might not have particular expertise in the topic |
| Articles are "peer-reviewed" or evaluated by experts in the field | Reviewed by an editor and fact checker. |
| A list of references or citations appears at the end of the article | References usually aren't formally cited |
| Goal is to present results of research | Goal may be to inform, entertain, or persuade |
| Examples: ; | Examples: ; |

- Next: Finding Peer Reviewed Articles >>
- Last Updated: May 21, 2024 8:45 AM
- URL: https://libguides.usu.edu/peer-review

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
Unfortunately we don't fully support your browser. If you have the option to, please upgrade to a newer version or use Mozilla Firefox , Microsoft Edge , Google Chrome , or Safari 14 or newer. If you are unable to, and need support, please send us your feedback .
We'd appreciate your feedback. Tell us what you think! opens in new tab/window
What is peer review?
Reviewers play a pivotal role in scholarly publishing. The peer review system exists to validate academic work, helps to improve the quality of published research, and increases networking possibilities within research communities. Despite criticisms, peer review is still the only widely accepted method for research validation and has continued successfully with relatively minor changes for some 350 years.
Elsevier relies on the peer review process to uphold the quality and validity of individual articles and the journals that publish them.
Peer review has been a formal part of scientific communication since the first scientific journals appeared more than 300 years ago. The Philosophical Transactions opens in new tab/window of the Royal Society is thought to be the first journal to formalize the peer review process opens in new tab/window under the editorship of Henry Oldenburg (1618- 1677).
Despite many criticisms about the integrity of peer review, the majority of the research community still believes peer review is the best form of scientific evaluation. This opinion was endorsed by the outcome of a survey Elsevier and Sense About Science conducted in 2009 opens in new tab/window and has since been further confirmed by other publisher and scholarly organization surveys. Furthermore, a 2015 survey by the Publishing Research Consortium opens in new tab/window , saw 82% of researchers agreeing that “without peer review there is no control in scientific communication.”
To learn more about peer review, visit Elsevier’s free e-learning platform Researcher Academy opens in new tab/window and see our resources below.

The peer review process
Types of peer review.
Peer review comes in different flavours. Each model has its own advantages and disadvantages, and often one type of review will be preferred by a subject community. Before submitting or reviewing a paper, you must therefore check which type is employed by the journal so you are aware of the respective rules. In case of questions regarding the peer review model employed by the journal for which you have been invited to review, consult the journal’s homepage or contact the editorial office directly.
Single anonymized review
In this type of review, the names of the reviewers are hidden from the author. This is the traditional method of reviewing and is the most common type by far. Points to consider regarding single anonymized review include:
Reviewer anonymity allows for impartial decisions, as the reviewers will not be influenced by potential criticism from the authors.
Authors may be concerned that reviewers in their field could delay publication, giving the reviewers a chance to publish first.
Reviewers may use their anonymity as justification for being unnecessarily critical or harsh when commenting on the authors’ work.
Double anonymized review
Both the reviewer and the author are anonymous in this model. Some advantages of this model are listed below.
Author anonymity limits reviewer bias, such as on author's gender, country of origin, academic status, or previous publication history.
Articles written by prestigious or renowned authors are considered based on the content of their papers, rather than their reputation.
But bear in mind that despite the above, reviewers can often identify the author through their writing style, subject matter, or self-citation – it is exceedingly difficult to guarantee total author anonymity. More information for authors can be found in our double-anonymized peer review guidelines .
Triple anonymized review
With triple anonymized review, reviewers are anonymous to the author, and the author's identity is unknown to both the reviewers and the editor. Articles are anonymized at the submission stage and are handled in a way to minimize any potential bias towards the authors. However, it should be noted that:
The complexities involved with anonymizing articles/authors to this level are considerable.
As with double anonymized review, there is still a possibility for the editor and/or reviewers to correctly identify the author(s) from their writing style, subject matter, citation patterns, or other methodologies.
Open review
Open peer review is an umbrella term for many different models aiming at greater transparency during and after the peer review process. The most common definition of open review is when both the reviewer and author are known to each other during the peer review process. Other types of open peer review consist of:
Publication of reviewers’ names on the article page
Publication of peer review reports alongside the article, either signed or anonymous
Publication of peer review reports (signed or anonymous) with authors’ and editors’ responses alongside the article
Publication of the paper after pre-checks and opening a discussion forum to the community who can then comment (named or anonymous) on the article
Many believe this is the best way to prevent malicious comments, stop plagiarism, prevent reviewers from following their own agenda, and encourage open, honest reviewing. Others see open review as a less honest process, in which politeness or fear of retribution may cause a reviewer to withhold or tone down criticism. For three years, five Elsevier journals experimented with publication of peer review reports (signed or anonymous) as articles alongside the accepted paper on ScienceDirect ( example opens in new tab/window ).
Read more about the experiment
More transparent peer review
Transparency is the key to trust in peer review and as such there is an increasing call towards more transparency around the peer review process . In an effort to promote transparency in the peer review process, many Elsevier journals therefore publish the name of the handling editor of the published paper on ScienceDirect. Some journals also provide details about the number of reviewers who reviewed the article before acceptance. Furthermore, in order to provide updates and feedback to reviewers, most Elsevier journals inform reviewers about the editor’s decision and their peers’ recommendations.
Article transfer service: sharing reviewer comments
Elsevier authors may be invited to transfer their article submission from one journal to another for free if their initial submission was not successful.
As a referee, your review report (including all comments to the author and editor) will be transferred to the destination journal, along with the manuscript. The main benefit is that reviewers are not asked to review the same manuscript several times for different journals.
Tools & resources
Elsevier researcher academy modules.
The certified peer reviewer course opens in new tab/window
Transparency in peer review opens in new tab/window
Reviewers’ Update articles
Peer review using today’s technology
Lifting the lid on publishing peer review reports: an interview with Bahar Mehmani and Flaminio Squazzoni
How face-to-face peer review can benefit authors and journals alike
Innovation in peer review: introducing “volunpeers”
Results masked review: peer review without publication bias
Interesting reads
"Is Peer Review in Crisis?" Perspectives in Publishing No 2, August 2004, by Adrian Mulligan opens in new tab/window
“The history of the peer-review process” Trends in Biotechnology, 2002, by Ray Spier opens in new tab/window
Publishing Research Consortium Peer review survey . 2015. Elsevier; 2015
Explainer: what is peer review?
Professor of Organisational Behaviour, Cass Business School, City, University of London
Novak Druce Research Fellow, University of Oxford
Disclosure statement
Thomas Roulet does not work for, consult to, own shares in or receive funding from any company or organisation that would benefit from this article, and has no relevant affiliations.
Andre Spicer does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
City, University of London provides funding as a founding partner of The Conversation UK.
University of Oxford provides funding as a member of The Conversation UK.
View all partners

We’ve all heard the phrase “peer review” as giving credence to research and scholarly papers, but what does it actually mean? How does it work?
Peer review is one of the gold standards of science. It’s a process where scientists (“peers”) evaluate the quality of other scientists’ work. By doing this, they aim to ensure the work is rigorous, coherent, uses past research and adds to what we already knew.
Most scientific journals, conferences and grant applications have some sort of peer review system. In most cases it is “double blind” peer review. This means evaluators do not know the author(s), and the author(s) do not know the identity of the evaluators. The intention behind this system is to ensure evaluation is not biased.
The more prestigious the journal, conference, or grant, the more demanding will be the review process, and the more likely the rejection. This prestige is why these papers tend to be more read and more cited.
The process in details
The peer review process for journals involves at least three stages.
1. The desk evaluation stage
When a paper is submitted to a journal, it receives an initial evaluation by the chief editor, or an associate editor with relevant expertise.
At this stage, either can “desk reject” the paper: that is, reject the paper without sending it to blind referees. Generally, papers are desk rejected if the paper doesn’t fit the scope of the journal or there is a fundamental flaw which makes it unfit for publication.
In this case, the rejecting editors might write a letter summarising his or her concerns. Some journals, such as the British Medical Journal , desk reject up to two-thirds or more of the papers.
2. The blind review
If the editorial team judges there are no fundamental flaws, they send it for review to blind referees. The number of reviewers depends on the field: in finance there might be only one reviewer, while journals in other fields of social sciences might ask up to four reviewers. Those reviewers are selected by the editor on the basis of their expert knowledge and their absence of a link with the authors.
Reviewers will decide whether to reject the paper, to accept it as it is (which rarely happens) or to ask for the paper to be revised. This means the author needs to change the paper in line with the reviewers’ concerns.
Usually the reviews deal with the validity and rigour of the empirical method, and the importance and originality of the findings (what is called the “contribution” to the existing literature). The editor collects those comments, weights them, takes a decision, and writes a letter summarising the reviewers’ and his or her own concerns.
It can therefore happen that despite hostility on the part of the reviewers, the editor could offer the paper a subsequent round of revision. In the best journals in the social sciences, 10% to 20% of the papers are offered a “revise-and-resubmit” after the first round.
3. The revisions – if you are lucky enough
If the paper has not been rejected after this first round of review, it is sent back to the author(s) for a revision. The process is repeated as many times as necessary for the editor to reach a consensus point on whether to accept or reject the paper. In some cases this can last for several years.
Ultimately, less than 10% of the submitted papers are accepted in the best journals in the social sciences. The renowned journal Nature publishes around 7% of the submitted papers.
Strengths and weaknesses of the peer review process
The peer review process is seen as the gold standard in science because it ensures the rigour, novelty, and consistency of academic outputs. Typically, through rounds of review, flawed ideas are eliminated and good ideas are strengthened and improved. Peer reviewing also ensures that science is relatively independent.
Because scientific ideas are judged by other scientists, the crucial yardstick is scientific standards. If other people from outside of the field were involved in judging ideas, other criteria such as political or economic gain might be used to select ideas. Peer reviewing is also seen as a crucial way of removing personalities and bias from the process of judging knowledge.
Despite the undoubted strengths, the peer review process as we know it has been criticised . It involves a number of social interactions that might create biases – for example, authors might be identified by reviewers if they are in the same field, and desk rejections are not blind.
It might also favour incremental (adding to past research) rather than innovative (new) research. Finally, reviewers are human after all and can make mistakes, misunderstand elements, or miss errors.
Are there any alternatives?
Defenders of the peer review system say although there are flaws, we’re yet to find a better system to evaluate research. However, a number of innovations have been introduced in the academic review system to improve its objectivity and efficiency.
Some new open-access journals (such as PLOS ONE ) publish papers with very little evaluation (they check the work is not deeply flawed methodologically). The focus there is on the post-publication peer review system: all readers can comment and criticise the paper.
Some journals such as Nature, have made part of the review process public (“open” review), offering a hybrid system in which peer review plays a role of primary gate keepers, but the public community of scholars judge in parallel (or afterwards in some other journals) the value of the research.
Another idea is to have a set of reviewers rating the paper each time it is revised. In this case, authors will be able to choose whether they want to invest more time in a revision to obtain a better rating, and get their work publicly recognised.
- Peer review

OzGrav Postdoctoral Research Fellow

Student Administration Officer

Casual Facilitator: GERRIC Student Programs - Arts, Design and Architecture

Senior Lecturer, Digital Advertising

Manager, Centre Policy and Translation

Peer review
Psychological Services reviewer guidelines
Psychological Services guidelines for reviewers.

Nick Bowman, PhD
Nick Bowman, PhD, associate editor for Technology, Mind, and Behavior sheds light on registered reports, outlining key features, misconceptions, and benefits of this unique article type.

Part three, peer review
In this part of the series, we examine the role of peer reviewers.
How to become a journal editor
The psychology field is looking for fresh voices—why not add yours?
Reviewer mentorship programs
Explore and join reviewer mentorship programs offered by various APA journals.
How to review manuscripts
Peer review is an integral part of science and a valuable contribution to our field. Browse these resources and consider joining the community of APA reviewers.
Peer Review Recognition
Publons is a service that provides instant recognition for peer review and enables APA reviewers and action editors to maintain a verified record of their contributions for promotion and funding applications.
Little-known secrets for how to get published
Advice from seasoned psychologists for those seeking to publish in a journal for the first time
How to review a manuscript
Journal editors identify 10 key steps for would-be reviewers
How to find reviewer opportunities
What if you want to review journal manuscripts but the editors aren’t beating down your door?
Webinars and training

Standards, guidelines, and regulations

Guidelines for responsible conduct regarding scientific communication

APA Style Journal Article Reporting Standards
National Science Foundation (NSF) Grant Proposal Guide
The Proposal & Award Policies & Procedures Guide (PAPPG) is the source for information about NSF's proposal and award process. Each version of the PAPPG applies to all proposals or applications submitted while that version is effective.
National Institutes of Health (NIH) Peer Review Policies and Practices
NIH resources about the regulations and processes that govern peer review, including management of conflicts of interest, applicant and reviewer responsibilities in maintaining the integrity in peer review, appeals, and more.
Office of Management and Budget (OMB) Final Information Quality Bulletin for Peer Review
Peer review at APA Journals

APA Journals Peer Review Process
Like other scientific journals, APA journals utilize a peer review process to guide manuscript selection and publication decisions.

APA reviewers get recognized through Web of Science Reviewer Recognition Service
Web of Science Reviewer Recognition Service™ enables APA reviewers and action editors to maintain a verified record of their contributions.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Saudi J Anaesth
- v.13(Suppl 1); 2019 Apr
The peer review process
Dmitry tumin.
1 Department of Anesthesiology and Pain Medicine, Nationwide Children's Hospital, Columbus, Ohio, USA
2 Department of Pediatrics, Nationwide Children's Hospital and The Ohio State University, Columbus, Ohio, USA
Joseph Drew Tobias
3 Department of Anesthesiology and Pain Medicine, The Ohio State University College of Medicine, Columbus, Ohio, USA
The peer review process provides a foundation for the credibility of scientific findings in medicine. The following article discusses the history of peer review in scientific and medical journals, the process for the selection of peer reviewers, and how journal editors arrive at a decision on submitted manuscripts. To aid authors who are invited to revise their manuscripts for further consideration, we outline steps for considering reviewer comments and provide suggestions for organizing the author's response to reviewers. We also examine ethical issues in peer review and provide recommendations for authors interested in becoming peer reviewers themselves.
Introduction
The review of research articles by peer experts prior to their publication is considered a mainstay of publishing in the medical literature.[ 1 , 2 ] This peer review process serves at least two purposes. For journal editors, peer review is an important tool for evaluating manuscripts submitted for publication. Reviewers assess the novelty and importance of the study, the validity of the methods, including the statistical analysis, the quality of the writing, the presentation of the data, and the connections drawn between the study findings and the existing literature. For authors, peer review is an important source of feedback on scientific writing and study design, and may aid in professionalization of junior researchers still learning the conventions of their field. Nevertheless, peer review can be frustrating, intimidating, or mysterious. This can deter authors from publishing their work or lead them to seek publication in less credible venues that use less rigorous peer review or do not subject manuscripts to peer review at all. In this article, we trace the origins of the scientific peer review system, explain its contemporary workings, and present authors with a brief guide on shepherding their manuscripts through peer review in medical journals.
The History of Scientific Peer Review
The introduction of peer review has been popularly attributed to the Royal Society of Edinburg, which compiled a collection of articles that had undergone peer review in 1731.[ 2 , 3 ] However, this initial process did not meet the criteria of peer review in its modern form, and well into the twentieth century, external and blinded peer review was still far from a requisite for scientific publication. Albert Einstein protested to the editor of an American journal in 1936 that his article was sent out for review, whereas this was not the practice of the German journals to which he had previously contributed.[ 4 ] Nevertheless, by the 1960s, the scientific value of peer review was becoming widely accepted, and in recent years, publication in a peer-reviewed journal has become a standard metric of scientific productivity (for the researchers) and validity (for the study).[ 5 , 6 ] In fact, publication in peer-reviewed quality journals is used to evaluate the quality of research during the academic promotion process. Today, peer review continues to evolve with the introduction of open review (reviewer comments posted publicly with the final article), postpublication review (reviews solicited from readers in an open forum after article publication), and journal review networks (where reviews are transferred from one journal to another when an article is rejected).[ 7 , 8 , 9 ] The constant at the center of this change remains the individual reviewer, who is asked to contribute their expertise to evaluating a manuscript that may or may not ever be shared with a wider scientific audience.
Reviewer Selection
The opacity of the peer review process is due, in part, to the anonymity of the reviewers and authors' lack of familiarity with how reviewers are selected. Typically, reviewers are selected by an editor of the journal, although depending on the size and organization of the journal, this may be the Editor-in-Chief, an Associate Editor, a Managing Editor, or an Editorial Assistant. Some journals permit authors to suggest their own reviewers, although the extent to which editors use these suggestions is variable. Authors may also be asked specifically or allowed to oppose reviewers, if they feel that certain scholars cannot grant their manuscript an unbiased hearing. Again, it is at the editors' discretion whether these requests are heeded. It has been suggested that these “opposed” reviewers may even be deliberately selected to ensure critical evaluation of a controversial manuscript. Alternatively, for very specific and narrow subject areas, there may be a limited number of appropriately qualified reviewers.
In general, reviewers may be of any academic rank and from a wide range of medical disciplines. A reviewer may be selected for their expertise in the topic of the study, but also for their general methodological expertise, or because they have been a reliable reviewer for the journal in the past. Qualified reviewers may not be invited if they cannot be reached by the editorial team, if they tend to submit late or uninformative reviews, or if they are too closely connected with the manuscript authors (e.g., colleagues at the same institution) and therefore may not provide an unbiased review. The reviewers initially selected by the editors may decline the invitation to review, mandating that the editors seek other reviewers. Unfortunately, this process of waiting for a response from the initial invitation to review (aside from the time taken to review) is one of the more common causes resulting in a delay in getting a response from the journal when a manuscript is submitted. The invited reviewer may pass the review on to a junior faculty member to allow them to participate and experience the academic peer review process. This may be performed with the permission of the editor, and noted after the review is submitted to the editor when the invited reviewer identifies that another person has participated in the process.
The initially received reviews may conflict with one another, leading the editors to cast a wider net for experts who will agree to review a submission. Because many factors may delay the completion of the review process, editors may proactively invite more reviews than they require and decide on the manuscript after a minimum number of reviews have been completed. The use of email and the internet has greatly facilitated communication for the review process, which used to be accomplished via telephone and postal mail. In most instances, an initial email is sent to the reviewer inquiring regarding their availability and interest. They are then asked to agree to review, at which time, a secondary email with a link to the journal site, the manuscript, and the review forms is sent.
How Reviewers Assess a Manuscript
From the reviewer's perspective, participation in the review process begins with an invitation from the journal editors to consider reviewing a submitted manuscript. If they accept, the reviewers will be able to access the submitted manuscript files, and sometimes the authors' cover letter, and other article metadata (e.g., the authors' list of preferred reviewers, figures, tables, etc.). Some journals ask reviewers to complete a structured questionnaire regarding the manuscript, rating its attributes on a numeric scale, or answering specific questions about each article section. All journals permit the submission of free-response evaluations. It is these evaluations that typically carry the greatest weight in the editors' final decision. The free-text reviewer reports also give the authors specific instructions about revising their manuscript and responding to the concerns that are raised. Reviewers may also submit confidential free-response comments to the editors (not seen by the authors) and indicate to the editors if they would be willing to review a revised version of the manuscript. In the end, the reviewer is asked to indicate their final recommendation to accept the manuscript without changes, accept after minor revisions, reconsider after major revisions, or reject. Some journals may offer additional variations on these recommendations, such as “reject but allow resubmission,” discussed below.
Regardless of the requested format for reviews, reviewers will typically evaluate several key aspects of submitted manuscripts. For original research studies, these will include the importance of the research question, the rigor of the methods, the completeness, accuracy, and novelty of the study and its results, and the validity of conclusions drawn from the data. The presentation of the manuscript, including the writing style, structure, grammar, and syntax also determine how the manuscript is received by the reviewers. Although the study design and results may be valid, these findings may be lost if the presentation is not precise or if there are grammar and spelling errors.
Reviewers also consider whether the study adds to existing knowledge in the field, whether it was ethically conducted, and whether it may be subject to any conflicts of interest. The editor and the reviewers also evaluate the study content and decide whether it is valuable and relevant to the readers of the journal. Although the study may be valid and well performed, it may be decided that the subject matter fits more appropriately in a journal of a different specialty. Along those lines, there may be overlap in the interests and fit of journals in different specialties, so that common topics in anesthesiology research may be of interest to journals from surgical specialties, pain medicine, or healthcare quality and patient safety, depending on the article content.
Some reviewers may submit their comments in paragraph form, building a narrative of the study's strengths and weaknesses section by section, whereas others may submit a short summary of the study followed by a list of criticisms or suggested corrections. Less commonly, reviewers may annotate the original manuscript with specific changes and questions or using the track-changes function of the word-processing software. Although the reviewers may recommend a specific editorial decision (e.g., recommend accepting an article with revisions, recommend rejection) in their comments to authors, this is generally discouraged by most journals and does not override the final decision reached by the editorial team. The ultimate decision generally resides with the section editor or the editor-in-chief, once they have seen and evaluated the comments of the reviewers. Depending on the format of the journal, the manuscript may be reviewed by one to five individuals. When there are specific statistical questions or advanced methods used, a separate review of the analytic methods may be required. For high-profile journals with high Impact Factors, a recommendation to accept may be required from all reviewers to receive a favorable editorial decision. At times, if there is a split decision, an additional reviewer or member of the editorial board may be asked to evaluate the manuscript to break the tie.
Almost all journals practice blinded review, where the reviewers' identities are not revealed to the authors. Double-blind review, where authors' identities are concealed from reviewers, although previously uncommon in medical journals, has been increasingly used. The editors communicate their decision and reviewers' evaluations to the authors in a decision letter (e-mail), informing of manuscript acceptance or rejection.
Reviews and the Editorial Decision
The comments submitted by external reviewers are collected by the editorial team and considered when determining the overall decision on the submitted article. The reviews may be read directly by the Editor-in-Chief, or by one or more Associate or Section Editors. The first editor reading the reviews might provide a recommendation that is then considered by the more senior editor; or the editors may convene to discuss the reviews and reach a decision as a group. In some journals, editors may write their own summary of the reviewers' criticism (sometimes adding their own) or may point out the critiques they consider most important to their decision. In other journals, editors weigh the number of positive and negative reviews or may reject an article unless all reviewers endorse its acceptance or revision.
Based on the external reviews and their own reading of the manuscript, the editors will reach one of several options regarding the manuscript. Unconditional acceptance of an article on its first submission to a journal (without any requested revisions) is very rare. Sometimes, articles will be conditionally accepted or accepted with minor revisions, meaning that the editors wish the authors to make changes to their manuscript based on the reviewers' comments but will not send the revised manuscript for a further round of external review. Rather, if the comments are generally minor, the editor will ensure that the comments are appropriately addressed in the authors' revision. The more common decision is “major revision,” where editors are willing to consider a revised version of the article but will subject it to further external review, by the original reviewers, a new set of reviewers, or a combination of both. Some journals also use a “reject and resubmit” decision, indicating lower enthusiasm for a resubmitted version of the article but still permitting resubmission, perhaps in an alternative format (e.g., brief report or letter to the editor, vs. full article) or with extensive revisions. For this latter decision, a full review will be accomplished as the revised manuscript is handled in much the same way as a new submission.
If the editors feel an article is a poor fit for their journal or falls too far below its standards, they may reject submissions outright without sending the manuscript for external review. This “desk reject” should not be confused with articles being “unsubmitted” by a managing editor or editorial assistant. The latter can happen due to style or formatting issues with the initial submission, which the author is asked to correct before the manuscript proceeds to review. Having a manuscript “unsubmitted” does not preclude resubmission of a corrected manuscript and is unlikely to affect reviewer assessment and, eventually, editorial decision.
Revising the Manuscript
When the initial editorial decision is positive, but not an unconditional acceptance, authors may elect to revise their manuscript and resubmit it to the same journal with a point-by-point response to the reviewers (discussed in the next section). The primary aim of the authors for this revision should be to address the criticisms and concerns raised during the initial review. Yet, this may be easier said than done when faced with conflicting recommendations, hostile reviews, or simply a large number of suggestions to be accommodated within a strict manuscript word limit. To streamline the process of responding to reviews, we offer the following roadmap as a suggestion.
Address the “fatal flaws”
Reviewers or editors may point out critical weaknesses of the study that prevent it from drawing the intended conclusions or even any conclusions at all. For example, an inaccuracy in the data, a bias in patient recruitment, a limitation of sample size, or a lack of follow-up may be so severe that the manuscript cannot provide credible evidence on the treatment or exposure it is meant to study. In particular, a lack of appropriate ethical approval would disqualify a study from publication, no matter how methodologically rigorous it may have been. In systematic reviews and analyses of existing databases, prior publication of a near-identical paper by a different group may also fundamentally preclude a paper from acceptance. On the rare occasions when the paper's central conclusions are found invalid and cannot be corrected through new analysis or a different framing of the authors' argument, reconceiving the study may be a better approach than attempting to revise and resubmit. At other times, some of these issues may be approached and the editor and reviewers satisfied by adding text to the discussion outlining the limitations of the current study. This may allow authors to acknowledge the concerns expressed by the reviewers and yet not redo their study from the beginning.
Amend the data analysis
More commonly, reviewers ask for changes to the data analysis without implying that these requests invalidate the entire study. We recommend making these changes before any further edits to the manuscript, because the intent is often to see if the paper's original findings are robust. In the best case scenario, any additional analysis will only confirm and strengthen the central conclusions. However, additional analyses sometimes reveal contradicting findings, which the authors should frankly address in the revised manuscript, by pointing out the contradiction and speculating about why different analyses of their data may have reached different conclusions. Especially when the study design was prospectively registered, the authors should explain in the manuscript which analyses were planned a priori and which were added post hoc . In these studies, authors should also avoid changing the pre-specified primary outcome, which would have been used for any a priori power or sample size calculation.
Decline infeasible or inappropriate suggestions
Some requests may not be feasible, for example, when requested data were not collected for a prospective study, or when collecting the data would mean starting chart review from scratch for a retrospective study. At other times, it may not be feasible to comply with the reviewers' requests if they disagree with the study type, the study cohort, or make other requests that would require a new or different study to address. Reviewers could also request changes to the statistical analysis that are not appropriate for the data at hand or for the study aims. In these cases, authors have the choice of rebutting the reviewers' comments while making no change in their manuscript, but an argumentative revision that leans too heavily on this option may be received poorly on re-review, resulting in rejection of the manuscript. In our experience, authors may be successful in responding to the reviews while rebutting one or two of the reviewers' suggestions, but a legitimate argument must be made for the rebuttal, and the reasons clearly stated.
Explain the study rationale and methods
Having completed the revision of the data analysis, authors should check that their methods section includes a complete and correct explanation of how the data were collected and explains how the analysis was performed. It may be appropriate to end the introduction by stating the hypothesis of the study. In the methods section, reviewers will often ask about the ethical committee approval of the study, the site(s) where the study was conducted, patient inclusion and exclusion criteria, the consent process, the procedures involved and the protocol for anesthetic management, and the specific data points that were collected during the study. For prospective clinical studies, authors should also indicate whether the study was submitted to a trial registry (such as ClinicalTrials.gov), and whether this was done before or after study enrollment had started. Clearly stated ethical approval and trial registration information must be provided for all submissions. Explanations may be sought if the editors and reviewers believe that the study did not meet standards for ethical approval, patient consent, or trial registration. Other requests related to methods may ask to clarify how the primary and secondary aims outlined in the introduction were addressed in the analysis, and how the sample size was determined, whether based on a statistical power analysis or logistical considerations (e.g., how many patients could be recruited with available resources). When a statistical power analysis is performed, reviewers may ask for more detail about the assumptions of this analysis and any supporting data from pilot studies or previous publications.
Check the conclusions and limitations
Having revised the introduction, methods, and results, the authors should revise the discussion to make any changes to the conclusions required by new or different study findings. We recommend that authors start the discussion with a review of what the study found, and then discuss how the study findings relate to similar work that has been previously published. An excessively long discussion does not ensure that a study will be published and, in fact, may detract from the quality of the manuscript. For a scientific study (retrospective or prospective), the discussion should not read like a comprehensive review of the literature. Typically, the discussion of study limitations will be expanded in the revised manuscript to include additional study weaknesses pointed out by reviewers, acknowledge suggested changes that could not be made to the study methods, and mention other suggestions for future studies that would build on the current results or answer questions left unanswered by the current study. Reviewers may ask that the conclusions be more specific in addressing the primary aim or hypothesis of the study (stated in the introduction), but they may also encourage authors to go further afield in their discussion, connecting their findings to results from previous publications and describing how their findings support or challenge current clinical practice.
Writing the Response to Reviewers
As seen above, manuscript revision can require more writing and (re)analysis than even the initial submission. Therefore, the aim of the revision memo (response to reviewers) is to summarize for the editors and reviewers how each change addresses the concerns raised on the initial review. This document is handled differently by different journals; some require it to be uploaded as a separate file, others require that the revision memo be entered in a text-box during the online submission process, and still others require that the response to review be included in the cover letter for the resubmitted manuscript. Therefore, authors should pay close attention to the decision letter and its instructions as to how they should submit their response to reviewers and how they should refer to manuscript edits in the revision memo (e.g., by page number, by line number, or copying sections of the revised manuscript into the memo).
Typically, the reviewers' comments should be copied and entered in the response memo so that each comment is numbered and the response clearly listed after it, in a different font style or color. It is equally important to determine how the journal would like the changes tracked in the revised manuscript. Some journals will ask that the authors use the track-changes mode in the word processing software, whereas others may ask for changes to be highlighted or be added in a different color font. Deleted manuscript text may need to be shown in strike-through font or simply removed from the revised submission, depending on the journal. Journals may ask for two copies of the revised manuscript: one showing the changes and one in a clean format that is ready for copyediting.
A typical revision memo will include a short paragraph acknowledging the editorial decision and reviewer comments and briefly summarizing key changes made to the manuscript. This would be followed by a numbered list of comments from the editors and reviewers (as received in the decision letter), with the authors' response to each one. Although not all reviewers and editors submit their comments as a numbered list, the authors may want to break up long sections or paragraphs of the reviews into shorter, numbered comments, to separately describe how each one was addressed in the revision. The authors' responses need not be excessively ingratiating but should respect the reviewers' effort in evaluating the manuscript, and concisely explain what was changed or why a change was not or could not be made. Different reviewers may have conflicting recommendations for revision. This may be as simple as one asking for a more concise definition of a method while another asking for a more detailed explanation. With conflicting reviews, the authors may consider taking the recommendation that is endorsed in the editor's comments (if this is provided), the one that is best aligned with the study aims, or the one that best matches the methods and writing style used in other contemporary papers in the field; and explaining this rationale when responding to the reviewers.
What to Do with a Rejected Manuscript
Based on reviewer reports or their own judgment, editors may reject a manuscript with no option to resubmit. It is essential to read the decision letter closely as some journals will state that they cannot publish a manuscript in its current form but offer to consider a new submission of a substantially revised manuscript (“reject and resubmit,” as mentioned above, in contrast to “revise and resubmit”). When the manuscript is rejected with no option of resubmission, authors may appeal this decision, but this option is rarely exercised and may not change the editors' decision. Appeals are also generally only successful when made by experienced and recognized scholars in the field.
Unless the study is discovered to be so flawed as to preclude publication in any venue, authors will usually consider submitting it to another journal after the initial rejection. Taking a single rejection and tabling a manuscript without further submission is rarely a good option. It is possible that multiple rejections will precede an eventual acceptance for valuable work. Given the amount of time taken to devise, implement, and up a study, we encourage authors to consider resubmission to a new journal, if the study is well conceived and addresses an important problem or question. In this case, the criticisms in the initial review are not binding, but still worth the authors' consideration. Particularly, authors should address any major flaws in the study's approach and conclusions (distinct from reviewers' preferences for additional data analysis unrelated to the primary aims), and correct any factual, spelling, or grammatical errors prior to resubmission. Adding recommended secondary analyses could sometimes strengthen the next submission, although just as often, the reviewers at the next journal may find these additional analyses superfluous, and will have their own set of analyses to recommend.
Becoming a Reviewer
Like any complex skill, navigating the peer review process is best learned through repetition. Becoming a peer reviewer for scientific journals is an important way to hone this skill, as well as providing a service to the scientific community, and adding to one's academic credentials as an expert whose opinion is sought by journal editors. The most common entry point to becoming a reviewer is through scientific publication; the authors of published articles can be contacted by another journal to provide a review on a related submission. One's expertise in a specific area may be noted by the editor who performs a topic search of key words when looking for reviewers. Alternatively, editors and associate editors may call on colleagues who they know are recognized experts in a particular field. Academic mentorship is also important, as mentors may ask junior colleagues and faculty to help them with reviewing article submissions, or may pass their name along to journal editors to be considered for inclusion in the reviewer pool. Once one has successfully reviewed for a journal, they are frequently called upon to review other submissions, especially if their review was returned in a timely manner. Many journals will give a specific timeframe within which the review is to be completed, while others will not. In most cases, a response within 2–4 weeks is considered acceptable. Some journals have now started editorial fellowships that aim to provide an immersive experience in the peer review and publishing process for early-career scientists. Lastly, researchers wishing to become peer reviewers may contact journal editors themselves, or register reviewer accounts in journal online submission systems. Although the general structure of peer review reports is described above, more specific guidance on performing peer review is available in other publications.[ 10 , 11 ]
Peer Review Ethics
Authors, reviewers, and editors have a shared responsibility for the ethical conduct of peer review. This is necessary to sustain the professional and public trust in peer review, as a system of evaluation that is accurate, constructive, and free from bias. Recently reported ethics violations have included authors misrepresenting the identity of suggested reviewers, reviewers plagiarizing a manuscript sent to them for review or recommending its rejection and then conducting a similar study, and editors inappropriately pressuring authors to cite articles published in their journal.[ 12 , 13 , 14 ] Some journals and publishers have also been criticized for circumventing the peer review process for submitted manuscripts.[ 15 ] For reviewers, it is most important that they be unbiased and not have any hidden agendas or personal vendettas to settle. For authors, ethical conduct in peer review includes disclosing the study's ethics committee approval, trial registration, and consent process; disclosing any related or overlapping prior publications; disclosing any actual or potential conflicts of interest; and submitting the manuscript only to one journal. These requirements are typically stated in the journal's guidelines for authors, and may need to be acknowledged in the cover letter accompanying the manuscript. In responding to reviews, authors should also carefully consider whether their revisions still fall within the scope of the ethics committee approval for the study and the informed consent that was obtained, and whether the revised manuscript remains faithful to the aims and study design of any pre-registered trial protocol.
Scientific research is not complete until it is published, but not all research can or should be published. It falls to peer-review to determine the difference. By engaging with the process of peer review, authors can improve the quality of their work as well as gain confidence that it is published in a reputable medium. Furthermore, the fact that a study has been peer reviewed will increase its stature and potential for recognition. However, the peer review process does not assure this. Although responding to reviews can be challenging, we hope that the suggestions sketched out in this article will help authors plan their approach to manuscript revision and resubmission. We also encourage authors to participate in this process as reviewers, so that the labor of peer review is properly shared among the community of scientists.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
The peer review process
The peer review process can be broadly summarized into 10 steps, although these steps can vary slightly between journals. Explore what’s involved, below.
Editor Feedback: “Reviewers should remember that they are representing the readers of the journal. Will the readers of this particular journal find this informative and useful?”
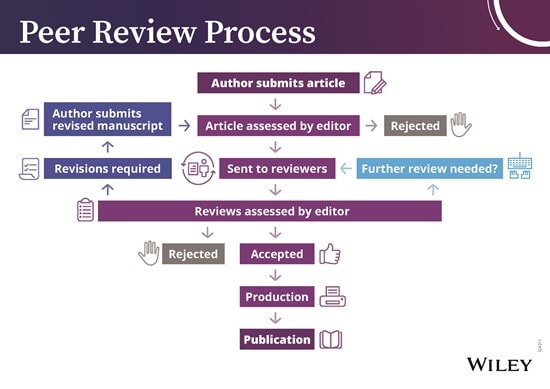

1. Submission of Paper
The corresponding or submitting author submits the paper to the journal. This is usually via an online system such as ScholarOne Manuscripts. Occasionally, journals may accept submissions by email.
2. Editorial Office Assessment
The Editorial Office checks that the paper adheres to the requirements described in the journal’s Author Guidelines. The quality of the paper is not assessed at this point.
3. Appraisal by the Editor-in-Chief (EIC)
The EIC checks assesses the paper, considering its scope, originality and merits. The EiC may reject the paper at this stage.
4. EIC Assigns an Associate Editor (AE)
Some journals have Associate Editors ( or equivalent ) who handle the peer review. If they do, they would be assigned at this stage.
5. Invitation to Reviewers
The handling editor sends invitations to individuals he or she believes would be appropriate reviewers. As responses are received, further invitations are issued, if necessary, until the required number of reviewers is secured– commonly this is 2, but there is some variation between journals.
6. Response to Invitations
Potential reviewers consider the invitation against their own expertise, conflicts of interest and availability. They then accept or decline the invitation to review. If possible, when declining, they might also suggest alternative reviewers.
7. Review is Conducted
The reviewer sets time aside to read the paper several times. The first read is used to form an initial impression of the work. If major problems are found at this stage, the reviewer may feel comfortable rejecting the paper without further work. Otherwise, they will read the paper several more times, taking notes to build a detailed point-by-point review. The review is then submitted to the journal, with the reviewer’s recommendation (e.g. to revise, accept or reject the paper).
8. Journal Evaluates the Reviews
The handling editor considers all the returned reviews before making a decision. If the reviews differ widely, the editor may invite an additional reviewer so as to get an extra opinion before making a decision.
9. The Decision is Communicated
The editor sends a decision email to the author including any relevant reviewer comments. Comments will be anonymous if the journal follows a single-anonymous or double-anonymous peer review model. Journals with following an open or transparent peer review model will share the identities of the reviewers with the author(s).
10. Next Steps
An editor's perspective.
Listen to a podcast from Roger Watson, Editor-in-Chief of Journal of Advanced Nursing, as he discusses 'The peer review process'.
If accepted , the paper is sent to production. If the article is rejected or sent back for either major or minor revision , the handling editor should include constructive comments from the reviewers to help the author improve the article. At this point, reviewers should also be sent an email or letter letting them know the outcome of their review. If the paper was sent back for revision , the reviewers should expect to receive a new version, unless they have opted out of further participation. However, where only minor changes were requested this follow-up review might be done by the handling editor.
Peer review process
Introduction to peer review, what is peer review.
Peer review is the system used to assess the quality of a manuscript before it is published. Independent researchers in the relevant research area assess submitted manuscripts for originality, validity and significance to help editors determine whether a manuscript should be published in their journal.
How does it work?
When a manuscript is submitted to a journal, it is assessed to see if it meets the criteria for submission. If it does, the editorial team will select potential peer reviewers within the field of research to peer-review the manuscript and make recommendations.
There are four main types of peer review used by BMC:
Single-blind: the reviewers know the names of the authors, but the authors do not know who reviewed their manuscript unless the reviewer chooses to sign their report.
Double-blind: the reviewers do not know the names of the authors, and the authors do not know who reviewed their manuscript.
Open peer: authors know who the reviewers are, and the reviewers know who the authors are. If the manuscript is accepted, the named reviewer reports are published alongside the article and the authors’ response to the reviewer.
Transparent peer: the reviewers know the names of the authors, but the authors do not know who reviewed their manuscript unless the reviewer chooses to sign their report. If the manuscript is accepted, the anonymous reviewer reports are published alongside the article and the authors’ response to the reviewer.
Different journals use different types of peer review. You can find out which peer-review system is used by a particular journal in the journal’s ‘About’ page.
Why do peer review?
Peer review is an integral part of scientific publishing that confirms the validity of the manuscript. Peer reviewers are experts who volunteer their time to help improve the manuscripts they review. By undergoing peer review, manuscripts should become:
More robust - peer reviewers may point out gaps in a paper that require more explanation or additional experiments.
Easier to read - if parts of your paper are difficult to understand, reviewers can suggest changes.
More useful - peer reviewers also consider the importance of your paper to others in your field.
For more information and advice on how to get published, please see our blog series here .
How peer review works
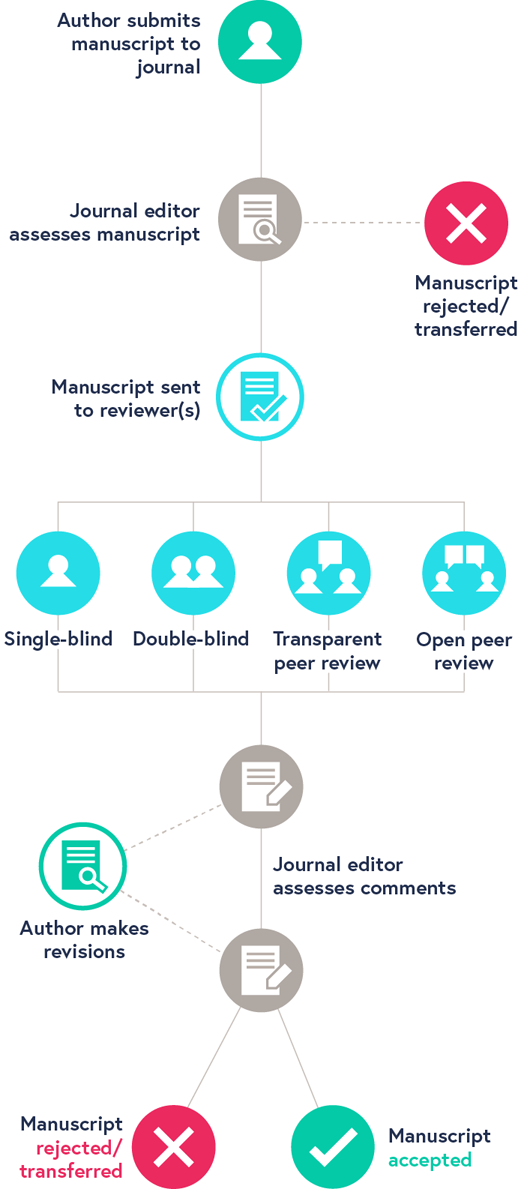
The peer review process can be single-blind, double-blind, open or transparent.
You can find out which peer review system is used by a particular journal in the journal's 'About' page.
N. B. This diagram is a representation of the peer review process, and should not be taken as the definitive approach used by every journal.
Understanding the peer-review process
The peer-review process is used to assess scholarly articles. Experts in a discipline similar to the author critique an article’s methodology, findings, and reasoning to evaluate it for possible publication in a scholarly journal. Editors of scholarly journals use the peer-review process to decide which articles to publish, and the academic world relies on the peer review process to validate scholarly articles.
Peer review process steps
- A researcher writes an article and submits it for publication to a scholarly journal.
- The journal editor gives the article an initial read to see whether it fits within the journal’s scope.
- If the article passes this phase, the editor selects reviewers who are experts in the same field as that of the author (which is why they are called “peers”). The reviewers may also be referred to as referees because they make judgments about the article’s quality. The reviewers often do not know who the author is, and the author does not know who the reviewers are.
- The reviewers evaluate the article on the basis of its quality, methodology, potential bias, ethical issues, and any other factors that would affect the research.
- The reviewers make a recommendation on whether the article should be published, including whether the article needs major or minor revisions. The editor makes a final decision on whether the article should be rejected, rejected with the request for revisions, or accepted.
- If an author is asked to make revisions, the author can resubmit the article after addressing the reviewers’ comments. This process may go through several rounds before an article is ultimately accepted.
- If an article is published in a subscription-based journal, the article is available to subscribers of that journal. Subscribers are usually university and college libraries, as subscriptions are expensive. If an article is published in an open access journal, the article is available for anyone to read for free online.
- The peer-review process may continue even after an article has been published. Authors and editors may make corrections to the article or even retract it if serious concerns arise.
Many professors will require you to use only peer-reviewed research for your assignments. View our guide to finding peer-reviewed articles to learn more about this process.
Peer review in 3 minutes
This video by the North Carolina State University Library describes the peer-review process.
View Video on Peer Review Process
- Open access
- Published: 19 August 2024
If health organisations and staff engage in research, does healthcare improve? Strengthening the evidence base through systematic reviews
- Annette Boaz 1 ,
- Belinda Goodenough 2 ,
- Stephen Hanney 3 &
- Bryony Soper 3
Health Research Policy and Systems volume 22 , Article number: 113 ( 2024 ) Cite this article
56 Accesses
7 Altmetric
Metrics details
There is an often-held assumption that the engagement of clinicians and healthcare organizations in research improves healthcare performance at various levels. Previous reviews found up to 28 studies suggesting a positive association between the engagement of individuals and healthcare organizations in research and improvements in healthcare performance. The current study sought to provide an update.
We updated our existing published systematic review by again addressing the question: Does research engagement (by clinicians and organizations) improve healthcare performance? The search covered the period 1 January 2012 to March 2024, in two phases. First, the formal updated search ran from 1 January 2012 to 31 May 2020, in any healthcare setting or country and focussed on English language publications. In this phase two searches identified 66 901 records. Later, a further check of key journals and citations to identified papers ran from May 2020 to March 2024. In total, 168 papers progressed to full-text appraisal; 62 were identified for inclusion in the update. Then we combined papers from our original and updated reviews.
In the combined review, the literature is dominated by papers from the United States (50/95) and mostly drawn from the Global North. Papers cover various clinical fields, with more on cancer than any other field; 86 of the 95 papers report positive results, of which 70 are purely positive and 16 positive/mixed, meaning there are some negative elements (i.e. aspects where there is a lack of healthcare improvement) in their findings.
Conclusions
The updated review collates a substantial pool of studies, especially when combined with our original review, which are largely positive in terms of the impact of research engagement on processes of care and patient outcomes. Of the potential engagement mechanisms, the review highlights the important role played by research networks. The review also identifies various papers which consider how far there is a “dose effect” from differing amounts of research engagement. Additional lessons come from analyses of equity issues and negative papers. This review provides further evidence of contributions played by systems level research investments such as research networks on processes of care and patient outcomes.
Peer Review reports
There is an often-held assumption that the engagement of clinicians and healthcare organizations in research improves healthcare performance at various levels. This assumption contributed to policy documents from various health organizations promoting research engagement by healthcare providers as a way of improving healthcare, for example, in the United Kingdom [ 1 , 2 , 3 ]. Therefore, it was believed that policy-makers who make relevant decisions, such as on the allocation of resources for health and health research systems, should have access to evidence on the validity of the assumption. In the United Kingdom, two programmes of the National Institute for Health Research (now called the National Institute for Health and Care Research) (NIHR) decided to commission reviews of the global evidence on this [ 1 , 2 , 3 ].
The wide-ranging brief provided for the second review, which was the original review by the authors of this present paper (published in full as Hanney et al. in 2013 [ 3 ] and more succinctly as Boaz et al. in 2015 [ 2 ]), included the additional aim of conducting a theoretically grounded synthesis to explore the mechanisms by which research engagement might improve healthcare [ 3 ]. The protocol for that study considered pertinent global literature, including on accelerating the adoption of evidence in health systems, and ways to enhance the relevance of the research conducted to the needs of health systems. The final protocol published as part of the Hanney et al. report [ 3 ] then used these ideas to identify possible mechanisms that would be worth analysing to help understand the processes that might be at work when research engagement leads to improved health. Among these was the idea that engaging in conducting research increases the ability and willingness of clinicians to use research findings from the global pool of knowledge, and here the concept of “absorptive capacity” was expected to be useful [ 3 ].
Some analyses focussed on the importance of exploring the relationship between research engagement and improved healthcare to contribute towards understanding of the benefits for healthcare performance in the context of a strong research culture. These papers were reviewed in Australia by Harding et al. in 2017 [ 4 ].
As far as we are aware, these three systematic literature reviews published in the second decade of this century provided the first analyses of the empirical evidence available to support the assumption of improved healthcare from research engagement [ 1 , 2 , 3 , 4 ]. Their differing scopes and approaches are summarized briefly in Table 1 .
All three of the reviews reported some evidence of a positive association between research engagement and healthcare performance, but the available evidence was not mature enough to support statements about causality [ 2 ]. Our review [ 2 , 3 ] had the widest scope of the three, reflecting the broad brief given by our NIHR funder. It included an extensive initial mapping exercise, a formal focussed review, and a wider review which drew on the earlier stages to explore, as noted above, the mechanisms by which research engagement might improve healthcare [ 3 ]. Our review identified 33 papers from 9 countries (15 from the United States), 28 of which reported positive findings [ 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ]. Even our review concluded, however, that there did not appear to be a well-structured, steadily accumulating body of knowledge about the benefits associated with research engagement.
In the succeeding years, we have identified a continuing and growing interest in this general topic, therefore an updated review seemed desirable to gather more evidence about how far research engagement might lead to improved healthcare and the mechanisms involved. In addition to these general questions, our original review had identified two specific issues that could usefully be considered further. These were research networks as potentially important mechanisms through which research engagement might improve healthcare, and whether greater amounts of research engagement would have a larger beneficial effect. Our original review also covered some aspects of a third issue (health equity) that has subsequently become increasingly important [ 2 , 3 ].
The growing development of research networks has been associated with efforts to move towards more formalized attempts to boost the role of health research systems in accelerating science and facilitating the translation of research into practice [ 2 , 3 ]. However, at the time of our original review, the evidence was still emerging and its availability was heavily skewed by the different timing of the establishment of formal research networks in different countries.
In the United States, various research networks had been set up in the second half of the last century, and most of the early papers on networks and their role came from there [ 2 ]. These networks in the United States are described in the “Glossary of the United States of America and United Kingdom Research Organizations and Networks Discussed in the Papers” (see Additional file 1 ). They include the National Cancer Institute (NCI)-funded Cancer Community Oncology Program (CCOP), established to encourage outreach and improve equity by bringing the advantages of clinical research to cancer patients in their own communities [ 37 ]. In the United Kingdom in contrast, national research networks were not formally created until this century, too late for any potential benefits to patient outcomes to be fully researched and reported prior to our review which started in 2011. However, even in our original review we were aware of concurrent United Kingdom work to measure those outcomes and to improve patient access to clinical research, and identified a need for further evaluations (see Hanney et al. [ 3 ], pp. 48, 83).
Subsequently, we also became increasingly aware of new studies on the effects of the developing research networks, especially in the United Kingdom, and Boaz et al. identified a promising approach in statistical analysis that could help further analysis [ 2 ]. As set out in the Glossary, there have been policy shifts and organizational changes in the United States and the United Kingdom, and there have been further ones elsewhere, which are designed to promote research networks to address the time lag between the production of research and its use in practice, including various efforts to strengthen links between academic centres and community services. There has also been an increasing emphasis, including within research networks, on the potential research contribution of healthcare professionals other than medical professionals.
Our original review had also noted a partly related second issue as worthy of further attention. This is the question of whether the association between research engagement by healthcare providers and improved healthcare outcomes increases with greater amounts of research participation. There was early evidence that it did. This came, in particular, from the 2008 paper by Majumdar et al. [ 26 ] that compared outcomes for patients with angina in hospitals in the United States having a high level of angina research activity with hospitals with low research activity, and those with no research activity. Other papers compared centres with different levels of research activity within a research network [ 23 ]. However, there was little certainty about extent and implications around this issue at that time, although it has become increasingly important with the development of the comprehensive research networks that we summarize in the Glossary. It also has theoretical implications for the exact nature of the association between research engagement and improved healthcare: in our original review we argued that further data on this effect, and on the time an institution was research active, “are needed to provide evidence of causation” (p. 12) [ 2 ].
These findings also have implications for health equity, the third unresolved issue. More outreach by research networks means more access to clinical research and its benefits for more patients. The United States CCOP has been rightly lauded for achieving this [ 37 ], but can that be squared with the emerging finding that higher levels of research participation in specific provider institutions bring greater benefit to the patients in those centres?
Reflection on these uncertainties further strengthened the argument that with all the developments since our original review, it seemed timely in 2020 to revisit this topic to explore and collate what additional understanding had been gained. While conducting the resulting update, we became aware of some more recent developments. A United Kingdom qualitative systematic review was published in 2021 that explored the impact of research activity by healthcare professionals other than medical professionals [ 38 ], and another UK review published in 2023 focussed on research engagement by allied health professionals (AHPs) [ 39 ]. With few exceptions, the papers specifically on nursing and AHPs in these reviews were typically smaller scale than the papers included in our formal review, and/or usually did not include the quantifiable comparisons that featured in most of our included papers. Nevertheless, these reviews usefully illustrate the growing interest in the contribution of these healthcare professionals in countries such as Australia, Canada and the United Kingdom.
In addition, we identified a large-scale study from the United States by Shahian et al. [ 40 ] that was published in 2022 and examined the link between research engagement and improved healthcare performance in 5 major medical fields across 1604 Medicare-participating hospitals. A noticeable facet of the paper by Shahian et al. was their referencing of a large number of papers that we had identified either in our original review, or in the first phase of our updated review [ 40 ].
To ensure our updated review adequately reflected all such developments since May 2020, we conducted a further search in March 2024. The review presented here is based on papers identified in both phases of the updated review, the findings of which are then combined with those from our original review.
Review question
To identify studies, the primary research question used the same approach as Boaz et al. [ 2 , 3 ].
Does research engagement (by clinicians and organizations) improve healthcare performance?
By research engagement, we mean, as in our original review, engagement in research rather than the broader concept of engagement with research, and we are referring to participation in research by healthcare organizations and staff rather than patient participation in trials. Engagement in research is taken to mean, “a deliberate set of intellectual and practical activities undertaken by healthcare staff (including conducting research and playing an active role in the whole research cycle) and organizations (including playing an active role in research networks, partnerships or collaborations)” (p. 2) [ 2 ].
The 2020 decision to complete an update of the previous review [ 2 , 3 ] was informed by a published decision framework for updating systematic reviews [ 41 ]. After completion in 2024 of the comprehensive initial phase of the updated review, including the two searches and considerable subsequent analysis, we recognized, as noted above, that while we had been conducting the review some important further papers had been published. We wanted to incorporate such papers, and so decided to conduct a further search for papers. The design of this final phase (which included a third search) was informed both by the fact that we had already identified a considerable number of papers for the updated review, and by the way new papers in this field were by now much more likely to cite earlier papers, with Shahian et al. [ 40 ] being a prime example. Therefore, we thought it was reasonable to rely to a much greater extent on checking citations to the papers already identified, as explained below.
Search strategy and information sources
Search 1 (update).
The first step in syntax development used the Medline Ovid strategy published by Boaz et al. [ 2 ].
Initial diagnostic testing indicated issues preventing code execution. Due to the syntax comprising several nested terms and Boolean operators, it was rebuilt using recommendations for “single-line” optimization for debugging complex code [ 42 ].
Search 2 (modified)
The syntax for Search 2 was a term modification to capture papers that more explicitly indexed research networks and collaborations. Search 2 necessitated a deeper dive into the full-text content of papers. The decision to search full-text articles reflected observations that the sensitivity of Search 1 was potentially affected by the variable quality (and relevance for our review) of abstracts, a consistent challenge for reviewers [ 43 ]. As a second search also adapted published syntax, the Preferred Reporting Items for Systematic reviews and Meta-Analyses Literature Search—Extension Checklist (PRISMA-S) reporting protocol was followed [ 44 ]. (The full text for search strategies is provided in “Search Strategy and Syntax Sensitivity”; see Additional file 2 ).
Electronic databases
Nine electronic records collections were used in Search 1: Medline (OVID and EBSCO), EMBASE, PsycInfo (OVID and EBSCO), CINAHL, Web of Science, Health Management and Information Consortium and British Nursing Institute. The mix provided parity with previous reviews and mitigated risk of missed papers by combining general and specialized databases. Different interfaces (e.g. OVID, EBSCO) for the same collection were also included to offset variations due to platform [ 45 ]. Grey literature was not searched: these collections failed to uniquely identify papers in previous reviews on this topic. Search 2 was restricted to the Medline EBSCO Full Text records, which was the collection which yielded the highest hit ratio for relevant papers (see Additional file 2 ).
Other sources
Manual and snowball searching were used in three ways. Firstly, a range of search engines (Google Scholar, PubMed, ProQuest Central, Scopus, the Web of Science Cited Reference Search) were used to track citations for (a) prior reviews as whole papers, (b) the individual studies within these reviews and (c) article reference lists. Secondly, key journals that published studies shortlisted in the previous reviews were hand-checked, including: Implementation Science, PLOS One, BMJ Open and BMC Health Services Research. Thirdly, topic experts suggested papers for consideration.
Search 3 (final phase)
As explained above, we subsequently conducted a further search covering May 2020–March 2024. This consisted of: a hand-search of three of the journals in which papers from the first phase of the updated review had been published (Health Research Policy and Systems, Implementation Science and Medical Care); a check of papers in the two reviews published in this period [ 38 , 39 ]; and a check of citations in this period to all the papers identified both in our original review and in the update’s initial phase.
Eligibility criteria
The following limiters were applied:
Timeframe: 1 January 2012 to 20 March 2024 (inclusive of eprint)
Population: Human (any setting)
Language: English (any country)
Paper type: Academic Journals (scholarly works). Conference papers were admitted as flags for accessible peer-reviewed works (e.g. pre-print) or key teams.
Three criteria were defined, guided by definitions from the original review [ 3 ].
Criterion A: study design
Empirical studies using method/s aligned with health services research, including clinical trials, retrospective cohort and survey methods. Studies with only patient reported outcomes (e.g. satisfaction) were excluded.
Criterion B: healthcare performance
Studies must report an outcome indexing performance assessment for a care process or healthcare improvement. The following were excluded: staff-specific reports alone, (e.g. job satisfaction or morale), policy impacts alone (no flow through to healthcare), descriptions of networks without outcomes data.
Criterion C: research engagement
Explicit demonstration of engagement in research including: agenda-setting, conducting research, participation in action research or in networks where the research involvement is noted. This criterion also allowed engagement implicitly through research network membership, even if a specific study was not recorded, but there was a comparison of healthcare between member and non-member settings. More details about examples that were in scope can be found in Hanney et al. [ 3 , p. 2].
Records management
To efficiently manage the export of the large records for the first two searches, Endnote X9 (Clarivate) was used to combine downloads from different databases and discard software detected duplicates. The endnote library was imported into Rayyan, a free multi-collaborator online screening tool [ 46 ]. Study selection procedures for Searches 1 and 2 followed the same screening/eligibility check sequence.
Screening and eligibility/quality checking
In Rayyan, titles were scanned to exclude papers that were irrelevant, did not meet criteria or were non-exact duplicates. Abstracts of retained records were then screened and classified as “include”, “exclude” or “maybe”. A third screening of “maybe” classifications forced a binary coding of “include” or “exclude”, with comment flags on issues. A final records’ sweep with the Rayyan query function checked for misclassified studies. This four-step screening process was completed by a single reviewer (BG).
Full-text for each provisionally included study was uploaded into Rayyan. The initial eligibility check was completed by three experts who were involved in article screening for Hanney et al. [ 3 ]. As a criterion check and to orient reviewers to the Rayyan platform, a practice phase used 10 randomly sampled records. The abstract was the primary source for expert reviewers, with full-text also available. After the practice task and consensus discussion of criteria, a batch of records (alphabet determined) was assigned to each expert reviewer, to rate each paper as “include”, “exclude” or “maybe” (ratings were unblinded). If the rating pair (i.e. B.G. and an expert from the original review) were both “include”, the paper was progressed to full-text appraisal. If there was disagreement, papers rated as “maybe” were reassigned to another expert reviewer for an opinion, and those rated as “exclude” by an expert reviewer were marked for discard. If consensus for a “maybe” paper could not be reached by discussion, it was progressed to a full text appraisal, conducted by a single reviewer (B.G.) using all available information sources and reviewer ratings.
A final review of all potential “includes” was jointly conducted by team members, including a few papers identified by other sources such as continued manual snowballing from key papers. The study selection procedures for Search 3 mirrored this final step, and so consisted of a review of all potential “includes” conducted jointly by team members.
Study quality was assessed using the mixed-methods appraisal tool (MMAT v2018), on a scale of 1 (low) to 5 (high) [ 47 ]. The MMAT accommodated all designs in the paper set. The majority of the papers have a design which fitted into the MMAT category of quantitative non-randomized. All papers scored good to high quality on the five questions in their relevant MMAT subscale. The lower end of ratings (good) was typically due to lack of information in the article, such as whether and/or how confounding factors may have been identified or managed. Quality ratings were not used to exclude papers, but formed part of the discussion about the quality and contribution of the papers.
Data extraction, coding and ethics
As Rayyan is only a screening platform, a data extraction sheet was created in Excel (v2016) for each included paper. A university research ethics committee deemed the project as not requiring formal ethical approval, due to secondary data mining on anonymized aggregated records.
A large and methodologically diverse mix of papers was identified with a range of different outcomes and outcome measures. The papers were combined through a process of critical interpretive synthesis inspired, as in our original review, by the approach outlined by Dixon-Woods et al. [ 48 ]. This involves adopting an iterative approach to refining the research question, searching the literature and defining and applying codes and categories. It enables the generation and development of theory with strong explanatory power and uses relevance as one measure of quality. Following analysis of the papers in the updated review, we collated the results from the updated review with those from our original review to create one combined set of papers for overall analysis.
Figure 1 summarizes the review literature flow. The two formal searches identified 66 901 records, with 68 further papers coming from other sources, including the March 2024 extension. From these, 168 papers progressed to full-text appraisal, and 62 were identified for inclusion [ 40 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 ].

Flow diagram for literature search
This review updates the previous review conducted by the team [ 2 ]. Table 2 outlines the 95 papers in our combined review: the 62 additional papers in the updated review along with the 33 papers in our original review. The latter 33 papers are shown in italics in Table 2 , which includes details about the study characteristics of all 95 included papers as well as key dimensions of the findings. To complement Table 2 , brief notes on the development and scope of key United States and United Kingdom research networks/organizations discussed in the papers are provided in the “Glossary of the United States of America and United Kingdom Research Organizations and Networks Discussed in the Papers” (see Additional file 1 ).
Study characteristics
Across the 95 papers, 12 countries are either the location for the research engagement described in a single-country study, or the location from which a multi-country study was led, with one paper led from South Africa having authors from a range of African countries (and Yemen) [ 88 ]. The 12 countries are: United States (50 papers), United Kingdom (17), Canada (7), Spain (5), Germany (4), the Netherlands (3), Australia (2), Denmark (2), South Africa (2), China (1), Finland (1) and Sweden (1).
Cancer was the most common field, with 32/95 papers overall. Next came hospital care in general/multi-field/acute care with 16 papers, cardiovascular/stroke (12), substance use disorder (7), dentistry (3), mental health/psychiatry (3) and obstetrics (3).
Main findings
As presented in Table 2 , the key findings from the combined review are presented in terms of the four pairs of binary options, though inevitably some papers did not neatly fit into one category. The first categorization is in terms of the level of analysis explored in different papers; 23 papers compare clinicians, but 72 compare organizations. There is an even higher proportion in the updated review at the organizational level (50/62, 81%) than in our original review (22/33, 67%).
A total of 86 of the 95 papers report positive results, of which 70 are purely positive and 16 are positive/mixed meaning that there are some key negative elements in their findings, that is, important parts of the analysis where a lack of healthcare improvement is identified. Nine papers are negative, of which four are negative-mixed.
The final two pairs of binary options consider just the 86 positive papers. In total, 37/86 report improved health outcomes in terms of reduced mortality or morbidity. A higher proportion of the positive papers in the updated review (30/58, 52%) than in our original review (7/28, 25%) describe such improved health outcomes. There is a corresponding reduction from three quarters (21/28) to a half (28/58) in the proportion of papers solely describing improved processes in terms such as applying proven interventions.
Finally, in terms of the type of impact, 55/86 of the papers describe research engagement leading to a broader impact on healthcare performance. Broad impacts arise when the improved healthcare goes more widely than just being linked to clinicians or healthcare organizations implementing the findings, or processes, from their own research more rapidly/extensively than do others. When the improved healthcare is linked to the results or processes of their own research, that is categorized as specific impact, which is the case in 31/86 papers. Using these various categories, Fig. 2 outlines the findings from the combined review, alongside the findings from our original review, and the updated review. This highlights various trends in terms of the main findings.

Results from Boaz et al. systematic reviews of whether research engagement by health organizations and staff improves healthcare: analysis of original; updated; and combined reviews (and of the 86 positive papers). Green rows (top): original review; Brown rows (middle): updated review; blue rows (bottom): combined review
One further trend in terms of the type of analysis is seen in the 11/95 papers that used bibliometric analysis as an indicator of the extent, and/or quality, of research engagement compared with some measure of the healthcare performance, in terms of processes and/or outcomes [ 30 , 40 , 50 , 51 , 56 , 65 , 76 , 95 , 96 , 97 , 100 ]; 10 of these papers are in the updated review, with just 1 [ 30 ] from our original review. All these 11 papers are positive, but various types of bibliometric analysis are used. The broad categories of academic indicators applied include publication volume [ 95 , 96 ], publication “quality” (for example, as measured by citations) [ 51 ] and a combination of volume and “quality” [ 30 , 40 , 50 , 56 , 65 , 76 , 97 , 100 ]. Of the latter, five relatively small studies suggest that the association with “quality” was stronger than with volume. The bibliometric studies also illustrate the varying levels of analysis at which the included studies in the review are conducted; 4 of the 11 papers compare the academic outputs of clinicians [ 50 , 56 , 96 , 97 ] and 7 make comparisons at an organizational level [ 30 , 40 , 51 , 65 , 76 , 95 , 100 ], focussing variously on academic outputs at ward, department or hospital/trust level.
The combined review allows for a range of issues to be analysed more thoroughly than they had been in our original review. These include issues highlighted in the background such as the role of networks and the “dose effect”. These are examined in turn below, followed by consideration of how far the included studies have addressed various aspects of health equity, and finally an analysis of lessons from the overall portfolio of positive and negative studies.
The role of research networks
The full significance of papers on research networks is seen in the combined review. Using the inclusive definition developed by Laliberte et al. [ 24 ], we have applied the term to various arrangements that, however loosely, give some measure of commonality to the research of multiple healthcare organizations that not only enhance science production, but also share a concern to transfer research findings into clinical practice. About half the papers in the combined review analysed research activity by clinicians or healthcare organizations who were part of research networks of various types.
In the United States, the NCI cancer research networks include the NCI-designated Comprehensive Cancer Centres, the NCI Cooperative Groups and collaborative groups of community hospitals affiliated to the NCI’s CCOP- see the Glossary for its new name. In various ways these networks all include outreach and the engagement of community physicians in their brief; see the Glossary for more details. Their potential was recognized early in the 2005 study by Laliberte et al. [ 24 ] that looked at these networks and concluded that network membership may influence compliance with treatment guidelines, and should therefore be taken into account in predictive models of compliance.
Seven included papers illustrated various aspects of this issue by comparing the processes and outcomes for patients treated at NCI-designated (comprehensive) cancer centres with those treated elsewhere, six of these studies showed better outcomes for patients treated at NCI centres [ 52 , 64 , 80 , 84 , 86 , 106 ], while one paper suggested that despite better processes, patient outcomes were worse at NCI centres. This paper is considered in the section on negative papers below [ 81 ]. Of the positive papers, Paulson et al. showed how the NCI designation was “associated with lower risk of postoperative death and improved long-term survival” (p. 675) [ 86 ], identified possible factors such as better adherence to guidelines, and demonstrated that the better outcomes at NCI-designated centres remained even when compared with non-NCI designated centres with a similar high volume of cases [ 86 ]. Wolfson et al. identified the requirements that underpin the positive association between high-quality research and high-quality care [ 106 ]. These included the mandate NCI centres have to “lead clinical trials, exchange ideas, disseminate findings” (p. 3892), which showed how the centres could act as part of a network. Wolfson et al. continued: “The NCI operates on the belief that a culture of discovery, scientific excellence, transdisciplinary research, and collaboration yields tangible benefits extending far beyond the generation of new knowledge” [ 106 ].
Building on Laliberte et al. [ 24 ], Carpenter et al. demonstrated an association between CCOP membership and accelerated innovation adoption but added the important codicil that it was not possible to “definitively ascertain whether there is a direct causal relationship between the two” [ 54 ].
Improved healthcare has also been associated with membership of the United States practice-based research networks (PBRNs). These networks cover family practice/primary care, dentistry, mental health and substance abuse. Like the CCOP and its affiliates, PBRNs involve practising clinicians in the community who conduct research. The combined review includes seven PBRN papers covering primary care and dentistry, all of which are positive [ 32 , 36 , 66 , 78 , 83 , 92 , 108 ] and one of which describes an international dental PBRN led from the United States that includes three Scandinavian countries [ 66 ].
A total of seven papers from another PBRN, the National Institute on Drug Abuse’s Clinical Trials Network (CTN), also provided evidence of accelerated translation, identified mechanisms through which this might work, and discussed the theoretical frameworks within which those operated [ 5 , 14 , 23 , 49 , 63 , 90 , 91 ]. Thus, Ducharme et al. [ 14 ] and Knudsen et al. [ 23 ] explored Rogers’ notion of the “trialability” [ 110 ] of innovations, that is, how far an innovation may be experimented with on just a limited basis, and Abraham et al. [ 5 ] discussed the role of absorptive capacity [ 111 , 112 ], which they summarized as an organization’s ability to assess and use information [ 5 ]. Rieckmann et al. noted that although the mechanisms involved were not fully understood they appeared “to be influenced by core experiences from network participation” (p. 894) [ 91 ], and Fields et al. [ 63 ] used insights from implementation science to explore the influence of a set of organizational characteristics (including network membership) on innovation adoption [ 113 ].
In an analysis of data on 12 993 transplants conducted in 162 US centres, the 32 centres in the Bone Marrow Transplant trials network were found to have significantly better survival rates than others [ 77 ]. Marmor et al. reported that there was not an association between procedure volume and survival. Rather, they suggested, the better outcomes for those treated in centres in this network could be linked to the nature of trials that required “higher levels of national clinical collaboration and standardization of protocols”, and such collaboration was “likely to generate higher levels of innovation and excellence among clinical colleagues” (p. 92) [ 77 ].
In Germany, one team produced three papers on the improved healthcare performance of hospitals that were part of clinical trials organizations [ 13 , 34 , 94 ]. Two papers described the improved outcomes for patients with ovarian cancer if they were treated in a hospital that belonged to one of two German ovarian cancer clinical trials organizations, in effect research networks [ 13 , 34 ]. They noted that the improved outcomes were not related to patient volume, suggesting instead that possible factors may include hospitals’ participation in the study group’s quality assurance programs and team members attending regular and scientific and educational meetings [ 13 ]. In a follow-up study, the data were analysed in more detail using mediation analysis that showed not just that the research participation of a hospital contributed to superior patient survival, but also began to unpick how it happened, including through better use of surgery and chemotherapy [ 94 ].
Downing et al. noted that, following the 2006 establishment of the NIHR in the United Kingdom, the increase in research activity in networks throughout the English NHS also increased the scope for analysing the benefits of research engagement [ 58 ]. The role of NIHR networks in boosting research engagement, which is then linked to improved healthcare, also covers clinicians such as nurses and AHPs who had traditionally had limited research opportunities. Studies are now showing how they can play an important role by engaging in research because, according to Trusson et al. reporting on a research network for nurses and AHPs, people working in such roles “have opportunities to explore possible solutions to issues that they encounter in their clinical role through academic study” (p. 1) [ 101 ]. Such opportunities can also enhance their clinical skills. More broadly, Downing et al. claimed that, in relation to the NIHR’s clinical trials network, “this natural experiment, presented by the rapid expansion of trial activity across a whole national health system, is perhaps the best opportunity to address the subject though outcomes research” (p. 95) [ 58 ]. This development is discussed in the next section.
The “dose effect” of the extent of research engagement
Evidence indicating a link between the extent of research engagement and the degree of improved healthcare has been accumulating for some time. In the United States, the 1996 study by Brown and Griffiss found that the average acute length of stay (LoS) in Department of Veteran Affairs hospitals was inversely related to the size of research programmes [ 53 ]. Majumdar et al. [ 26 ] used a tertile approach to show that in-hospital mortality decreased as the rate of trial participation increased in the area of unstable angina. In the substance abuse field, early CTN studies also contributed: thus Knudsen et al. [ 23 ] noted that the adoption of buprenorphine therapy by practitioners within the trials’ network was much greater in those programmes in the network that participated in the specific buprenorphine trial than those that had not. In a 2006 study of a sexual health trial in Australia, Morton et al. [ 28 ] identified improved post-trial clinical practice by high-recruiting clinicians, but not by low-recruiting ones.
In our combined set of papers the first use of the specific term “dose effect” to describe the effects of differing amounts of research engagement occurred in Downing et al., who tested the hypothesis that for colorectal cancer (CRC) “high, sustained hospital-level participation in interventional clinical trials improves outcomes for all patients with CRC managed in those research-intensive hospitals” (p. 89) [ 58 ]. They found that high participation in such clinical trials was independently associated with better outcomes and that these effects were not restricted to academic centres or large institutions but were seen across all the NHS Trusts that conducted research on and treated patients with colorectal cancer. They extended their analysis to look at the effects of different levels of research participation and found that the highest levels of participation led to the highest levels of improved outcomes. However, in relation to these findings, Downing et al. were careful to say that, in the absence of the possibility of an RCT, caution was needed if attempting “to infer a causal contribution” (p. 89) from participation in research activity to improved healthcare [ 58 ].
Other United Kingdom database studies support the findings of Downing et al. For example, Ozdemir et al. [ 85 ] compared mortality with research funding per hospital bed in hospitals with high, medium and low levels of research funding and showed that not only was mortality lower in high-funded research hospitals than in other hospitals, but also, on average, hospitals in the middle category had a lower mortality rate than ones with the least research funding. In two studies using NIHR research study activity data from different years, Jonker and Fisher [ 68 , 69 ] showed an inverse correlation between the number of clinical trials/patient participation levels in United Kingdom hospitals and the mortality rate. Lin et al. [ 73 ] used retrospective data to examine the survival rate of the 465 patients (recruited by 60 hospitals) who had participated in an RCT in the NIHR Clinical Research Network (CRN). While they identified a significant association between low trial recruitment and lower survival rates, looking at the volume of patients treated in the disease area by the respective hospitals they report that “no significance was found between hospital throughput and outcomes” (p. 40) [ 73 ].
Further support for the “dose effect” concept comes from the United States and elsewhere. According to Abraham et al., in the substance abuse field “treatment programs participating in a greater number of CTN protocols had significantly higher levels of treatment quality, an association that held after controlling for key organizational characteristics” (p. 232) [ 49 ]. Similarly, Gilbert et al. [ 66 ] reported that members of a dental PBRN who fully participated in the network were more likely to move evidence-based care into everyday practice than members who only partially participated. Seaburg et al. [ 96 ] showed an association between the quantity of resident physicians’ publications and their clinical performance scores during training, and García-Romero et al. claimed that increases in the scientific output of Spanish hospitals made a significant contribution to a reduction of hospital LoS [ 65 ].
In Canada, Tsang et al. [ 103 ] conducted a pre-planned observational study nested within a clinical trial to test how well traditionally non-research active community hospitals could participate in an RCT alongside the traditional RCT sites in academic hospitals. However, while that aspect of the study did show that, in terms of adherence to trial metrics, the community hospitals could successfully participate in studies, outcomes for patients in the trial were significantly better in the traditional research hospitals, although the full reasons for this will need further exploration [ 103 ].
- Health equity
Various aspects of health equity are considered in the included papers, and some of these report attempts to improve health equity. Some population groups are particularly vulnerable. In the United States, for example, Wolfson et al. listed the following groups: “underrepresented minorities, those with low socio-economic status (SES), those with public or no insurance, and those with a significant distance to care” (p. 3886) [ 106 ]. On the basis of its long-held assumption that patient access to research active healthcare providers is beneficial, the NCI has attempted to reduce geographic inequalities in access. In a 1995 paper, Warneke et al. noted that the CCOP was established by the NCI in 1983 with the deliberate intention of spreading the benefits of the clinical research conducted in NCI centres: “The program was designed with the assumption that by participating as equals in the research process, community physicians would be more likely to accept and implement the results in their practices with non-protocol patients” (p. 336) [ 37 ].
Similar moves to encourage wider participation in clinical trials have recently been made in Canada in the nested study described above [ 103 ]. A recent analysis showing higher levels of research activity within the English healthcare system were associated with lower mortality, noted that although the NIHR CRN was established to promote research participation across England, there was still some way to go to ensure greater geographical equity [ 69 ].
Other initiatives, such as the United States minority-based CCOPs described in the Glossary, addressed racial inequalities in relation to access to research engagement and timely evidence-based healthcare. These sometimes overlap with geographic inequalities. Some of the papers on the NCI-designated cancer centres observed with concern that the proportion of certain racial/ethnic groups, including African Americans, who received treatment at these centres compared with non-NCI centres, was lower than for other racial groups [ 64 , 80 , 106 ]. Having noted that African Americans with colon cancer experienced worse outcomes than Caucasian Americans, and suggested that this was partly due to differential treatment, a study by Penn et al. found evidence that African Americans receiving treatment from CCOP providers had benefitted from a seemingly deliberate attempt to boost early access to a recently recommended innovative treatment [ 87 ]. In Australia, Young et al. [ 109 ] reported that the health services, and health research system, of the Aboriginal community work together to try to ensure health research is embedded into activities that improve health, and described a specific example in relation to ear, nose and throat surgery and speech-language pathology services.
Lessons from the overall collection of studies: positive and negative
A wide variety of papers contribute to the combined review’s overall finding that the included studies are overwhelmingly positive. As the section on the “dose effect” illustrates, throughout the time covered by the combined review, individual papers have contributed to a wider understanding that goes beyond specific issues about research networks. Many papers contribute to the analysis of both the strength of the association between research engagement and improved healthcare, and the mechanisms involved. For example, a 2019 US positive study by Fanaroff et al. [ 60 ] identified improved care and outcomes for patients with acute myocardial infarction who were treated at research active hospitals, even after accounting for potential confounders. The authors encapsulated some of the key thinking on research engagement with their conclusion that participation in clinical trials by hospitals “may be emblematic of a culture that embraces novel therapeutics, engages both clinicians and patients, and incentivizes continuous improvement in care” (p. 191) [ 60 ].
While overall the 95 studies included in the combined review are positive, about 10% are categorized as negative. These nine negative papers also provide important insights [ 7 , 11 , 15 , 20 , 25 , 67 , 79 , 81 , 99 ]. For example, existing widespread use of one proven intervention prior to a company-sponsored clinical trial exploring physicians’ adherence to international treatment recommendations meant that the trial had no significant impact on that adherence, although it did increase use of the trial sponsor’s drug [ 7 ]; physicians adopted another trial intervention before it was proven one way or another [ 11 ]; more positively, a unique policy and regulatory environment governing the adoption of another intervention ensured that all hospitals benefitted, not just those in the trial [ 79 ]. Two teams with negative results later conducted further, more comprehensive studies with positive conclusions [ 25 , 26 , 67 , 68 , 69 ]. Six of the seven papers examining whether NCI-designated cancer centres provided patients with better healthcare processes and outcomes are positive [ 52 , 64 , 80 , 84 , 86 , 106 ]. However, one paper suggested that outcomes were worse in these accredited hospitals despite the better healthcare and, in seeking to explain this, drew attention to the factors considered in the accreditation processes used by different organizations and how far they accurately captured the most relevant data [ 81 ].
Our original review set out to find whether there was empirical evidence that supported the often-held assumption that engagement by clinicians and healthcare organizations in research improves healthcare performance at various levels. It concluded that there was some positive evidence but that systematic analysis of the data related to this engagement was in its infancy [ 2 ]. The 62 papers in the updated review, 58 of which are positive, provide further empirical evidence to support the positive conclusions of the original review.
When the papers from both reviews are considered together, they provide a more complete dataset than previously available [ 1 , 2 , 3 , 4 ], and an updated picture of this literature in which the trends identified in our initial analyses [ 3 ] become more apparent. With more than a third of the papers in the combined review (32/95) focussing on aspects of cancer, this is the field overall in which there is the most comprehensive analysis of the link between research engagement and improved healthcare. While the individual cancer papers differ in the strength of the association identified, and most of the papers focus one or other of the main cancer sites, many of the cancer papers analyse the role of research networks – one of the main mechanisms through which it is claimed research engagement improves healthcare.
The combined review reflects policy shifts and organizational changes that occurred first in the United States and later in the United Kingdom and elsewhere, and were designed to address the time lag between the production of research and its use in practice. These include the development of research networks and their associated databases over several decades (accompanied by an improved understanding of their strengths and limitations [ 54 , 64 , 77 , 106 , 108 ]) and efforts to strengthen links between academic centres and community services [ 61 , 87 ]. More recent developments, especially in the United Kingdom, encouraged further deliberate attempts to identify and explore the impacts of research engagement. Research teams were, for example, better able to study the real-world impacts of system-level mechanisms such as research networks as they became more formalized and embedded in national health and science structures [ 58 , 67 , 68 , 69 , 85 , 93 , 101 ].
Across the board, within and beyond networks, there is also further evidence about the mechanisms by which research engagement might improve healthcare, including the ones identified in our original review. The role of strong evidence-based protocols developed for RCTs, but contributing to improved healthcare more widely in research active healthcare sites, was highlighted in various studies [ 77 , 98 , 105 ]. Papers also identified the importance of providing evidence-based/guideline consistent care, which could also be linked to a culture of discovery, excellence and collaboration [ 40 , 60 , 62 , 64 , 77 , 84 , 86 , 87 , 106 ]. There were also more nuanced mechanisms at the speciality and clinician levels, such as the use of multi-disciplinary coordination of care in radiation therapy treatment [ 107 ] and practitioner skill development in substance abuse work [ 90 ]. Similar practitioner skill development was also reported among nurses and AHPs, including in the wider literature [ 31 , 38 , 39 , 62 , 70 , 101 ].
In the combined review it also became easier to see connections across this diverse literature. It was possible to identify research teams that had worked together on multiple studies and to explore the extent of cross referencing. In the United States, for example, the CTN of the drug abuse institute had been created to emulate the CCOP, and a centre was established to assess the CTN’s impact [ 114 ]. Analysis of this research network highlighted its role both in conducting research that was relevant to the “real-world” needs of clinical settings, and in enhancing evidence-adoption by healthcare organizations and staff [ 114 ]. Many of the papers from this substance abuse CTN [ 23 , 49 , 90 ] referenced each other and also cross-referenced key cancer papers [ 8 , 24 , 54 ], and there was common use of the same early sources [ 110 , 112 , 115 , 116 ]. These interactions prompted ongoing methodological development, strengthened understanding of theoretical concepts, and supported shared learning across the specialities. Additionally, themes that had been recognized in the original review, including concepts such as absorptive capacity [ 5 , 111 ], were further explored and tested in new contexts, even if the same literature was not always drawn upon [ 40 , 65 ].
In the combined review, the nature and strength of the association found between research engagement and improved health varies enormously among the 86 positive papers, even among those that describe the role of research networks. One approach that begins to identify where evidence might be strongest was noted in the original review as being the important concept of the “dose effect”, even if it was not specifically labelled as such [ 26 ]. However, the combined review can now more fully consider the concept because evidence about this greatly increased as the scope of the papers included has increased. There are many more studies where all the clinicians or organizations compared are engaged in research but to varying extents and/or with different levels of resources, for example within a trial [ 28 , 50 , 59 , 73 , 93 , 103 , 107 ] or within a network [ 23 , 33 , 49 , 51 , 66 , 68 , 69 , 85 , 95 ]. The inclusion of papers regarding differences within trials, and the emergence of the importance of the “dose effect”, have implications for both (a) how the issue of research engagement is analysed and (b) how far efforts to enhance research engagement should be concentrated or spread widely across a system.
In relation to the first of these issues, when considering how research engagement is analysed, the key question morphs somewhat: it is no longer simply whether research engagement improves healthcare performance compared with no research engagement, rather, it is whether a larger amount of research engagement improves healthcare performance by more than a smaller level of engagement (and, if so, by how much). Answers to these questions could then feed back to strengthen the evidence for a positive association between research engagement and improved healthcare performance.
In relation to the second question, about the concentration or wide distribution of research funding, analyses might have to consider the context and trade-offs in terms of benefits for improved health and health equity. The widespread distribution of research funding across the health system could maximize the number of patients who might benefit, but a more concentrated approach, with a higher dose of research engagement in a smaller number of hospitals, could maximize the benefit for patients in such centres.
Research infrastructures in countries such as the United States and United Kingdom have been developed to enhance the relationship between health and health research systems, and the evidence from our combined review suggests that these changes have been positive. In both systems, but particularly in the United Kingdom, there have been deliberate attempts to fund major centres of research in leading healthcare facilities, as well as to spread research funding more widely to healthcare organizations across the country, but this impetus needs to be maintained if the full benefits of research engagement are to be realized.
Such an argument is reinforced by the conclusions of a major recent analysis of progress in the United Kingdom in engaging healthcare staff in research and building research capacity. The findings from the study suggest that many healthcare staff in the United Kingdom are interested in being involved in research, there are supportive national policies and strategies in place and there has been some important progress. However, achieving widespread involvement “will only be possible by focusing more on how healthcare organizations embed and support research activity through organizational policies which are supported by the wider research support and funding infrastructure. This is an essential part of a system-based approach to developing and supporting research engagement” (p. 356) [ 117 ]. The progress possible, and the potential benefits of trying to build a health research system embedded into a healthcare system, but also the full range of substantial challenges, have also recently been explored in a hospital and regional healthcare system in northern Queensland, Australia [ 118 , 119 ]. Studies such as these indicate that this combined review could provide timely evidence to further the challenging task of improving healthcare by boosting engagement in health research.
Strengths and limitations
The combined review contains a considerable number of papers from diverse perspectives, but the literature is drawn predominantly from the United States and the Global North, thus the conclusions may not be appropriate in different contexts, including in the Global South. This, perhaps, partly reflects the inclusion criteria of papers in English only. While the increasing use of bibliometrics as an indicator of research engagement has widened the range of positive studies available, differing claims as to the most appropriate measure of research publications challenge consistent interpretation of the data and indicate there is more work to do. Furthermore, it is important to recognize that the national policy, noted in one paper, of attaching promotion and bonuses for clinicians to publish in journals with an impact factor of at least three [ 97 ] runs contrary to the internationally widely endorsed Declaration on Research Assessment [ 120 ].
The complexity of this literature (with many generic terms such as “research” and “engagement”), and the tangential approach of some papers to the broad question of whether research engagement improves performance, posed considerable challenges. It helped enormously that this time around, we were able to build on our experience in the original review. We adopted a somewhat more extensive approach to the formal search in the updated review, and we identified some papers that we had missed in the original review. We were aided by the generally greater clarity in later papers. We are now able, therefore, to present a more nuanced understanding of this field, building on our experience in the original review. In particular, we have found considerably more evidence on two topics identified as important in our original review, and on their implications for health equity: the role of research networks and consideration of how far there is a dose effect with regard to the degrees of research engagement. On both topics the combined review has strong papers showing important healthcare improvements even after considering potential confounders such as patient volume [ 8 , 13 , 26 , 40 , 58 , 73 , 77 , 84 , 85 , 86 ]. However, the failure of some papers to address such confounders [ 59 , 107 ] means some weaknesses in the overall analysis remain, and we are still not able to undertake any meta-analysis as the included literature remains very diverse.
We have now included a significant range of largely positive papers in the combined review. However, lack of resources meant we were not able to replicate our original review’s [ 2 , 3 ] structured analysis of the wider range of papers identified as making many relevant and illuminating points related to the topic, but not meeting the review’s inclusion criteria. For example, while the combined review does include some consideration of health equity issues, there were papers taken to full paper review that were not in the end included but which provide considerably more evidence [ 121 , 122 ].
Future possible work
The system-based approaches for expanding the amount of research in healthcare systems that are mentioned above continue to provide important opportunities for further work on exploring the relationship between research engagement and improved healthcare, including the implications for health equity. Likewise, improvements in the identification and collection of relevant data and developments in statistics have prompted increasingly sophisticated analyses, sometimes using approaches developed in other fields, and could continue to do so [ 65 , 90 , 94 ]. There has also been increasingly sophisticated use of bibliometrics, and there are likely to be continuing opportunities to apply such approaches to more countries. However, the warning from Downing et al. that caution is needed if attempting “to infer a causal contribution” from research participation to improved health outcomes [ 58 ], as well as frequent mention of similar disclaimers in other papers [ 8 , 40 , 54 , 59 , 69 , 74 ], is a reminder that more work is needed.
While some of our papers have claimed that the costs of research engagement are broadly covered by the associated reduced LoS [ 53 , 65 ], further research might be useful around the costs associated with research engagement and how these relate to reported benefits. Such studies could add to the existing large-scale studies showing the considerable monetary value of the health and economic gains resulting from health research [ 123 ].
The insights revealed by the negative papers, particularly in relation to the contexts in which research and research networks operate [ 99 ], could usefully be further explored. Merkow et al. [ 81 ], the one negative paper out of seven papers included on the NCI-designated centres, raises issues about the accuracy, or perhaps appropriateness, of the measurement used by various organizations to accredit cancer centres. These issues have also been explored by various teams [ 122 , 124 , 125 ] but could perhaps be worth further examination because the findings from Merkow et al. are so starkly different from those of other papers included in our review.
Finally, there are increasing opportunities, as well as a growing need, to address the limitations identified above (and also noted in the review by Chalmers et al. [ 39 ]) and go beyond the formal inclusion criteria of this review. A major area that could usefully be incorporated into an overall analysis of the field relates to the impact of the growing interest in research engagement strategies [ 126 ]. This includes the efforts to enhance research roles for healthcare professionals other than medical professionals [ 38 ], and the increasing number of organizational arrangements within health and health research systems for partnerships that seek to boost the production and use of relevant evidence [ 127 , 128 ].
Previous reviews [ 1 , 2 , 3 , 4 ] have investigated the association between research engagement and improvements in healthcare performance. This study updates and extends the most comprehensive of these reviews [ 2 , 3 ], and combines its findings with those from that original review to produce a more substantial pool of studies, which are largely positive in terms of the impact of research engagement on processes of care and patient outcomes. Of potential mechanisms, the combined review highlights the important role played by research networks and further identifies the various ways the research engagement facilitated by them operates to improve healthcare. The review also draws together a set of papers which consider how far there is a research engagement “dose effect”. Given the difficulty of conducting randomized controlled trials of large-scale research engagement initiatives, studies of the dose effect offer another approach to understanding the potential contribution and complexities of research engagement, including the implications for health equity. This review provides further evidence of the important contribution played by systems-level research investments such as research networks on processes of care and patient outcomes.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
Allied health professionals
Clinical research network
Clinical trials network
Community Clinical Oncology Program
Length of stay
Mixed-methods appraisal tool
National Cancer Institute
National Health Service
National Institute for Health (and Care) Research
Practice-based research network
Research and development
Randomized controlled trials
Clarke M, Loudon K. Effects on patients of their healthcare practitioner’s or institution’s participation in clinical trials: a systematic review. Trials. 2011;12:16. https://doi.org/10.1186/1745-6215-12-16 .
Article PubMed PubMed Central Google Scholar
Boaz A, Hanney S, Jones T, Soper B. Does the engagement of clinicians and organisations in research improve healthcare performance: a three-stage review. BMJ Open. 2015;5: e009415. https://doi.org/10.1136/bmjopen-2015-009415 .
Hanney S, Boaz A, Jones T, Soper B. Engagement in research: an innovative three-stage review of the benefits for health-care performance. Health Serv Deliv Res. 2013;1:8. https://doi.org/10.3310/hsdr01080 .
Article Google Scholar
Harding K, Lynch L, Porter J, Taylor NF. Organisational benefits of a strong research culture in a health service: a systematic review. Aust Health Rev. 2017;41:45–53. https://doi.org/10.1071/AH15180 .
Article PubMed Google Scholar
Abraham AJ, Knudsen HK, Rothrauff TC, Roman PM. The adoption of alcohol pharmacotherapies in the clinical trials network: the influence of research network participation. J Subst Abuse Treat. 2010;38:275–83. https://doi.org/10.1016/j.jsat.2010.01.003 .
Adler MW. Changes in local clinical practice following an experiment in medical care: evaluation of evaluation. J Epidemiol Community Health. 1978;32:143–6. https://doi.org/10.1136/jech.32.2.143 .
Article CAS PubMed PubMed Central Google Scholar
Andersen M, Kragstrup J, Sondergaard J. How conducting a clinical trial affects physicians’ guideline adherence and drug preferences. JAMA. 2006;295:2759–64. https://doi.org/10.1001/jama.295.23.2759 .
Article CAS PubMed Google Scholar
Carpenter WR, Reeder-Hayes K, Bainbridge J, Meyer A-M, Amos KD, Weiner BJ, et al. The role of organizational affiliations and research networks in the diffusion of breast cancer treatment innovation. Med Care. 2011;49:172–9. https://doi.org/10.1097/MLR.0b013e3182028ff2 .
Chaney EF, Rubenstein LV, Liu C-F, Yano EM, Bolkan C, Lee M, et al. Implementing collaborative care for depression treatment in primary care: a cluster randomized evaluation of a quality improvement practice redesign. Implement Sci. 2011;6:121. https://doi.org/10.1186/1748-5908-6-121 .
Chen AY, Schrag N, Hao Y, Flanders WD, Kepner J, Stewart A, et al. Changes in treatment of advanced laryngeal cancer 1985–2001. Otolaryngol Head Neck Surg. 2006;135:831–7. https://doi.org/10.1016/j.otohns.2006.07.012 .
Clark WF, Garg AX, Blake PG, Rock GA, Heidenheim AP, Sackett DL. Effect of awareness of a randomized controlled trial on use of experimental therapy. JAMA. 2003;290:1351–5. https://doi.org/10.1001/jama.290.10.1351 .
Das D, Ishaq S, Harrison R, Kosuri K, Harper E, Decaestecker J, et al. Management of Barrett’s esophagus in the UK: overtreated and underbiopsied but improved by the introduction of a national randomised trial. Am J Gastroenterol. 2008;103:1079–89. https://doi.org/10.1111/j.1572-0241.2008.01790.x .
du Bois A, Rochon J, Lamparter C, Pfisterer J, for the Organkommission OVAR. Pattern of care and impact of participation in clinical studies on the outcome in ovarian cancer. Int J Gynecol Cancer. 2005;15:183–91. https://doi.org/10.1111/j.1525-1438.2005.15202.x .
Ducharme LJ, Knudsen HK, Roman PM, Johnson JA. Innovation adoption in substance abuse treatment: exposure, trialability, and the clinical trials network. J Subst Abuse Treat. 2007;32:321–9. https://doi.org/10.1016/j.jsat.2006.05.021 .
Goldberg HI, Neighbor WE, Hirsch IB, Cheadle AD, Ramsey SD, Gore E. Evidence-based management: using serial firm trials to improve diabetes care quality. Jt Comm J Qual Improv. 2002;28:155–66.
PubMed Google Scholar
Hall C, Sigford B, Sayer N. Practice changes associated with the Department of Veterans Affairs’ Family Care Collaborative. J Gen Int Med. 2010;25(Suppl. 1):18–26. https://doi.org/10.1007/s11606-009-1125-3 .
Hébert-Croteau N, Brisson J, Latreille J, Blanchette C, Deschenes L. Variations in the treatment of early-stage breast cancer in Quebec between 1988 and 1994. CMAJ. 1999;161:951–5.
PubMed PubMed Central Google Scholar
Janni W, Kiechle M, Sommer H, Rack B, Gauger K, Heinrigs M, et al. Study participation improves treatment strategies and individual patient care in participating centers. Anticancer Res. 2006;26:3661–7. https://doi.org/10.1016/S0960-9776(05)80107-9 .
Jha P, Deboer D, Sykora K, Naylor CD. Characteristics and mortality outcomes of thrombolysis trial participants and nonparticipants: a population-based comparison. J Am Coll Cardiol. 1996;27:1335–42. https://doi.org/10.1016/0735-1097(96)00018-6 .
Jones B, Ratzer E, Clark J, Zeren F, Haun W. Does peer-reviewed publication change the habits of surgeons? Am J Surg. 2000;180:566–9. https://doi.org/10.1016/S0002-9610(00)00495-5 .
Karjalainen S, Palva I. Do treatment protocols improve end results? A study of survival of patients with multiple myeloma in Finland. BMJ. 1989;299:1069–72. https://doi.org/10.1136/bmj.299.6707.1069 .
Kizer JR, Cannon CP, McCabe CH, Mueller HS, Schweiger MJ, Davis VG, et al. Trends in the use of pharmacotherapies for acute myocardial infarction among physicians who design and/or implement randomized trials vs physicians in routine clinical practice: the MILIS-TIMI experience. Am Heart J. 1999;137:79–92. https://doi.org/10.1016/s0002-8703(99)70462-x .
Knudsen HK, Abraham AJ, Johnson JA, Roman PM. Buprenorphine adoption in the national drug abuse treatment clinical trials network. J Subst Abuse Treat. 2009;37:307–12. https://doi.org/10.1016/j.jsat.2008.12.004 .
Laliberte L, Fennell ML, Papandonatos G. The relationship of membership in research networks to compliance with treatment guidelines for early-stage breast cancer. Med Care. 2005;43:471–9. https://doi.org/10.1097/01.mlr.0000160416.66188.f5 .
Majumdar SR, Chang W-C, Armstrong PW. Do the investigative sites that take part in a positive clinical trial translate that evidence into practice? Am J Med. 2002;113:140–5. https://doi.org/10.1016/S0002-9343(02)01166-X .
Majumdar SR, Roe MT, Peterson ED, Chen AY, Gibler WB, Armstrong PW. Better outcomes for patients treated at hospitals that participate in clinical trials. Arch Intern Med. 2008;168:657–62. https://doi.org/10.1001/archinternmed.2007.124 .
Meineche-Schmidt V, Hvenegaard A, Juhl HH. Participation in a clinical trial influences the future management of patients with gastro-oesophageal reflux disease in general practice. Aliment Pharmacol Ther. 2006;24:1117–25. https://doi.org/10.1111/j.1365-2036.2006.03046.x .
Morton AN, Bradshaw CS, Fairley CK. Changes in the diagnosis and management of bacterial vaginosis following clinical research. Sex Health. 2006;3:183–5. https://doi.org/10.1071/SH06024 .
Pancorbo-Hidalgo PL, Garcia-Fernandez FP, Lopez-Medina IM, Lopez-Ortega J. Pressure ulcer care in Spain: nurses’ knowledge and clinical practice. J Adv Nurs. 2007;58:327–38. https://doi.org/10.1111/j.1365-2648.2007.04236.x .
Pons J, Sais C, Illa C, Méndez R, Suñen E, Casas M, et al. Is there an association between the quality of hospitals’ research and their quality of care? J Health Serv Res Policy. 2010;15:204–9. https://doi.org/10.1258/jhsrp.2010.009125 .
Puoane T, Sanders D, Ashworth A, Chopra M, Strasser S, McCoy D. Improving the hospital management of malnourished children by participatory research. Int J Qual Health Care. 2004;16:31–40. https://doi.org/10.1093/intqhc/mzh002 .
Rhyne R, Sussman AL, Fernald D, Weller N, Daniels E, Williams RL, et al. Reports of persistent change in the clinical encounter following research participation: a report from the primary care multiethnic network (PRIME Net). J Am Board Fam Med. 2011;24:496–502. https://doi.org/10.3122/jabfm.2011.05.100295 .
Rich AL, Tata LJ, Free CM, Stanley RA, Peake MD, Baldwin DR, et al. How do patient and hospital features influence outcomes in small-cell lung cancer in England? Br J Cancer. 2011;105:746–52. https://doi.org/10.1038/bjc.2011.310 .
Rochon J, du Bois A. Clinical research in epithelial ovarian cancer and patients’ outcome. Ann Oncol. 2011;22(Suppl. 7):vii16–9. https://doi.org/10.1093/annonc/mdr421 .
Salbach NM, Guilcher SJ, Jaglal SB, Davis DA. Determinants of research use in clinical decision making among physical therapists providing services post-stroke: a cross-sectional study. Implement Sci. 2010;5:77. https://doi.org/10.1186/1748-5908-5-77 .
Siegel RM, Bien J, Lichtenstein P, Davis J, Khoury JC, Knight JE, et al. A safety-net antibiotic prescription for otitis media: the effects of a PBRN study on patients and practitioners. Clin Pediatr. 2006;45:518–24. https://doi.org/10.1177/0009922806290567 .
Warnecke R, Johnson T, Kaluzny A, Ford L. The community clinical oncology program: its effect on clinical practice. Jt Comm J Qual Improv. 1995;21:336–9.
CAS PubMed Google Scholar
Newington L, Wells M, Adonis A, Bolton L, Bolton Saghdaoui L, et al. A qualitative systematic review and thematic synthesis exploring the impacts of clinical academic activity by healthcare professionals outside medicine. BMC Health Serv Res. 2021;21:400. https://doi.org/10.1186/s12913-021-06354-y .
Chalmers S, Hill J, Connell L, Ackerley S, Kulkarni A, Roddam H. The value of allied health professional research engagement on healthcare performance: a systematic review. BMC Health Serv Res. 2023;23:766. https://doi.org/10.1186/s12913-023-09555-9 .
Shahian DM, McCloskey D, Liu X, Schneider E, Cheng D, Mort EA. The association of hospital research publications and clinical quality. Health Serv Res. 2022;57(3):587–97. https://doi.org/10.1111/1475-6773.13947 .
Garner P, Hopewell S, Chandler J, MacLehose H, Akl EA, Bayene J, et al. When and how to update systematic reviews: consensus and checklist. BMJ. 2016;354: i3507. https://doi.org/10.1136/bmj.i3507 .
Bramer WM, De Jonge GB, Rethlefsen ML, Mast F, Kleijnen J. A systematic approach to searching: an efficient and complete method to develop literature searches. J Med Libr Assoc. 2018;106:531–41. https://doi.org/10.1136/bmj.i3507 .
Beller EM, Glasziou PP, Altman DG, Hopewell S, Bastian H, Chalmers I, et al. PRISMA for abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med. 2013;10:e1001419. https://doi.org/10.1371/journal.pmed.1001419 .
Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, et al. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Sys Rev. 2021;10:39. https://doi.org/10.1186/s13643-020-01542-z .
Younger P, Boddy K. When is a search not a search? A comparison of searching the AMED complementary health database via EBSCOhost, OVID and DIALOG. Health Info Libr J. 2009;26:126–35. https://doi.org/10.1111/j.1471-1842.2008.00785.x .
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—A web and mobile app for systematic reviews. Syst Rev. 2016;5:210. https://doi.org/10.1186/s13643-016-0384-4 .
Hong QN, Pluye P, Fàbregues S, Bartlett G, et al. The mixed methods appraisal tool (MMAT) version 2018. User guide. http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf . Accessed 7 July 2024.
Dixon-Woods M, Cavers D, Agarwal S, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35. https://doi.org/10.1186/1471-2288-6-35 .
Abraham AJ, Knudsen HK, Roman PM. The relationship between clinical trial network protocol involvement and quality of substance use disorder treatment. J Subst Abuse Treat. 2014;46:232–7. https://doi.org/10.1016/j.jsat.2013.08.021 .
Alotaibi NM, Ibrahim GM, Wang J, Guha D, Mamdani M, Schweizer TA, et al. Neurosurgeon academic impact is associated with clinical outcomes after clipping of ruptured intracranial aneurysms. PLoS ONE. 2017;12: e0181521. https://doi.org/10.1371/journal.pone.0181521 .
Bennett WO, Bird JH, Burrows SA, Counter PR, Reddy VM. Does academic output correlate with better mortality rates in NHS trusts in England? Public Health. 2012;126(Suppl 1):S40–3. https://doi.org/10.1016/j.puhe.2012.05.021 .
Birkmeyer NJ, Goodney PP, Stukel TA, Hillner BE, Birkmeyer JD. Do cancer centers designated by the National Cancer Institute have better surgical outcomes? Cancer. 2005;103(3):435–41. https://doi.org/10.1002/cncr.20785 .
Brown A, Griffiss M. Effect of integrated research programs on health care systems and costs. Mil Med. 1996;161:691–5. https://doi.org/10.1093/milmed/161.11.691 .
Carpenter WR, Meyer AM, Wu Y, Qaqish B, Sanoff HK, Goldberg RM, et al. Translating research into practice: the role of provider-based research networks in the diffusion of an evidence-based colon cancer treatment innovation. Med Care. 2012;50:737–48. https://doi.org/10.1097/MLR.0b013e31824ebe13 .
Corrigan MH, Glass HE. Physician participation in clinical studies and subsequent prescribing of new drugs. Pharm Ther. 2005;30(1):60–6.
Google Scholar
de Arriba-Enriquez J, Sanz-Casado E, Vieta E, Rapado-Castro M, Arango C. Quality of care in psychiatry is related to research activity. Eur Psychiatry. 2021;64(1): e53. https://doi.org/10.1192/j.eurpsy.2021.16 .
de Lange TS, Roos C, Bloemenkamp KW, Bolte AC, Duvekot JJ, Franssen MT, et al. Impact of a randomized trial on maintenance tocolysis on length of hospital admission of women with threatened preterm labor in the Netherlands. Eur J Obstet Gynecol Reprod Biol. 2015;186:8–11. https://doi.org/10.1016/j.ejogrb.2014.12.003 .
Downing A, Morris EJ, Corrigan N, Sebag-Montefiore D, Finan PJ, Thomas JD, et al. High hospital research participation and improved colorectal cancer survival outcomes: a population-based study. Gut. 2017;66:89–96. https://doi.org/10.1136/gutjnl-2015-311308 .
Eaton BR, Pugh SL, Bradley JD, Masters G, Kavadi VS, Narayan S, et al. Institutional enrollment and survival among NSCLC patients receiving chemoradiation: NRG oncology radiation therapy oncology group (RTOG) 0617. J Natl Cancer Inst. 2016;108(9): djw034. https://doi.org/10.1093/jnci/djw034 .
Fanaroff AC, Vora AN, Chen AY, Mathews R, Udell JA, Roe MT, et al. Hospital participation in clinical trials for patients with acute myocardial infarction: results from the National Cardiovascular Data Registry. Am Heart J. 2019;214:184–93. https://doi.org/10.1016/j.ahj.2019.05.011 .
Farquhar DR, Masood MM, Lenze NR, Sheth S, Patel SN, Lumley C, et al. Academic affiliation and surgical volume predict survival in head and neck cancer patients receiving surgery. Laryngoscope. 2021;131:E479–88. https://doi.org/10.1002/lary.28744 .
Fernández-Domínguez JC, De Pedro-Gómez JE, Jiménez-López R, Romero-Franco N, Bays Moneo AB, Oliva-Pascual-Vaca Á, et al. Physiotherapists’ evidence-based practice profiles by HS-EBP questionnaire in Spain: a cross-sectional normative study. PLoS ONE. 2022;17(6): e0269460. https://doi.org/10.1371/journal.pone.0269460 .
Fields D, Knudsen HK, Roman PM. Implementation of network for the improvement of addiction treatment (NIATx) processes in substance use disorder treatment centers. J Behav Health Serv Res. 2016;43:354–65. https://doi.org/10.1007/s11414-015-9466-7 .
Fong ZV, Chang DC, Hur C, et al. Variation in long-term oncologic outcomes by type of cancer center accreditation: an analysis of a SEER-Medicare population with pancreatic cancer. Am J Surg. 2020;220(1):29–34. https://doi.org/10.1016/j.amjsurg.2020.03.035 .
García-Romero A, Escribano Á, Tribó JA. The impact of health research on length of stay in Spanish public hospitals. Res Policy. 2017;46:591–604. https://doi.org/10.1016/j.respol.2017.01.006 .
Gilbert GH, Gordan VV, Funkhouser EM, Rindal DB, Fellows JL, Qvist V, et al. Caries treatment in a dental practice-based research network: movement toward stated evidence-based treatment. Community Dent Oral Epidemiol. 2013;41:143–53. https://doi.org/10.1111/cdoe.12008 .
Jonker L, Fisher SJ. NHS Trusts’ clinical research activity and overall CQC performance—Is there a correlation? Public Health. 2015;129:1491–5. https://doi.org/10.1016/j.puhe.2015.07.026 .
Jonker L, Fisher SJ. The correlation between National Health Service trusts’ clinical trial activity and both mortality rates and care quality commission ratings: a retrospective cross-sectional study. Public Health. 2018;157:1–6. https://doi.org/10.1016/j.puhe.2017.12.022 .
Jonker L, Fisher SJ, Badgett RG. Relationship between staff thriving, through engagement and research activity, and hospital-related outcome measures: a retrospective cross-sectional study. J Healthc Qual Res. 2021;36(3):128–35.
Kirby K, Brandling J, Robinson M, Thomas M, Voss S, Benger J. The experiences of EMS providers taking part in a large randomised trial of airway management during out of hospital cardiac arrest, and the impact on their views and practice. Results of a survey and telephone interviews. Resuscitation. 2020;149:1–9. https://doi.org/10.1016/j.resuscitation.2020.01.034 .
Kirwan CC, Al Sarakbi W, Loncaster J, Chan HY, Thompson AM, Wishart GC. Tumour bed clip localisation for targeted breast radiotherapy: compliance is proportional to trial-related research activity: tumour bed clip localisation in breast radiotherapy. Eur J Surg Oncol. 2014;40:158–62. https://doi.org/10.1016/j.ejso.2013.11.016 .
Levan JM, Brion LP, Wrage LA, Gantz MG, Wyckoff MH, Sánchez PJ, et al. Change in practice after the surfactant, positive pressure and oxygenation randomised trial. Arch Dis Child Fetal Neonatal Ed. 2014;99:F386–90. https://doi.org/10.1136/archdischild-2014-306057 .
Lin DJ, McConkey CC, Nankivell P, Dunn J, Mehanna H. The impact of institutional clinical trial recruitment versus hospital volume on survival outcomes of patients with head and neck cancer: an analysis of the PET-NECK trial outcomes, UKCRN portfolio, and Hospital Episode Statistics (HES) in England. Oral Oncol. 2018;85:40–3. https://doi.org/10.1016/j.oraloncology.2018.08.006 .
Litjens RJ, Oude Rengerink K, Danhof NA, Kruitwagen RF, Mol BW. Does recruitment for multicenter clinical trials improve dissemination and timely implementation of their results? A survey study from the Netherlands. Clin Trials. 2013;10:915–23. https://doi.org/10.1177/1740774513504150 .
Ljunggren M, Weibull CE, Rosander E, et al. Hospital factors and metastatic surgery in colorectal cancer patients, a population-based cohort study. BMC Cancer. 2022;22:907. https://doi.org/10.1186/s12885-022-10005-8 .
Manes E, Tchetchik A, Tobol Y, Durst R, Chodick G. An empirical investigation of “physician congestion” in US University Hospitals. Int J Environ Res Public Health. 2019;16:761. https://doi.org/10.3390/ijerph16050761 .
Marmor S, Begun J, Abraham J, et al. The impact of center accreditation on hematopoietic cell transplantation (HCT). Bone Marrow Transplant. 2015;50:87–94. https://doi.org/10.1038/bmt.2014.219 .
McBride R, Leroux B, Lindblad A, Williams OD, Lehmann M, Rindal DB, et al. Measuring the impact of practice-based research networks on member dentists in the Collaboration on Networked Dental and Oral Health Research, CONDOR. J Dent. 2013;41:393–403. https://doi.org/10.1016/j.jdent.2013.03.005 .
McCarthy FH, Groeneveld PW, Kobrin D, Mcdermott KM, Wirtalla C, Desai ND. Effect of clinical trial experience on transcatheter aortic valve replacement outcomes. Circ Cardiovasc Interv. 2015;8: e002234. https://doi.org/10.1161/CIRCINTERVENTIONS.114.002234 .
McDaniels-Davidson C, Feng CH, Martinez ME, Canchola AJ, Gomez SL, Nodora JN, et al. Improved survival in cervical cancer patients receiving care at National Cancer Institute—Designated cancer centers. Cancer. 2022;128:3479–86. https://doi.org/10.1002/cncr.34404 .
Merkow RP, Chung JW, Paruch JL, Bentrem DJ. Center accreditation and performance on publicly reported quality measures. Ann Surg. 2014;259(6):1091–7. https://doi.org/10.1097/SLA.0000000000000542 .
Meyer AM, Reeder-Hayes KE, Liu H, Wheeler SB, Penn D, Weiner BJ, et al. Differential receipt of sentinel lymph node biopsy within practice-based research networks. Med Care. 2013;51:812–8. https://doi.org/10.1097/MLR.0b013e31829c8ca4 .
Mold JW, Aspy CB, Smith PD, Zink T, Knox L, Lipman PD, et al. Leveraging practice-based research networks to accelerate implementation and diffusion of chronic kidney disease guidelines in primary care practices: a prospective cohort study. Implement Sci. 2014;9:169. https://doi.org/10.1186/s13012-014-0169-x .
Murimwa GZ, Karalis JD, Meier J, et al. Hospital designations and their impact on guideline-concordant care and survival in pancreatic cancer. Do they matter? Ann Surg Oncol. 2023;30:4377–87. https://doi.org/10.1245/s10434-023-13308-7 .
Ozdemir BA, Karthikesalingam A, Sinha S, Poloniecki JD, Hinchliffe RJ, Thompson MM, et al. Research activity and the association with mortality. PLoS ONE. 2015;10: e0118253. https://doi.org/10.1371/journal.pone.0118253 .
Paulson EC, Mitra N, Sonnad S, Armstrong K, Wirtalla C, Kelz RR, et al. National cancer institute designation predicts improved outcomes in colorectal cancer surgery. Ann Surg. 2008;248:675–86. https://doi.org/10.1097/SLA.0b013e318187a757 .
Penn DC, Chang Y, Meyer AM, Defilippo Mack C, Sanoff HK, Stitzenberg KB, et al. Provider-based research networks may improve early access to innovative colon cancer treatment for African Americans treated in the community. Cancer. 2015;121:93–101. https://doi.org/10.1002/cncr.29028 .
Prendergast EA, Perkins S, Engel ME, Cupido B, Francis V, Joachim A, et al. Participation in research improves overall patient management: insights from the global rheumatic heart disease registry (REMEDY). Cardiovasc J Afr. 2018;29:98–105. https://doi.org/10.5830/CVJA-2017-054 .
Rai A, Nastoupil LJ, Williams JN, Lipscomb J, Ward KC, Howard DH, et al. Patterns of use and survival outcomes of positron emission tomography for initial staging in elderly follicular lymphoma patients. Leuk Lymphoma. 2017;58:1570–80. https://doi.org/10.1080/10428194.2016.1253836 .
Rieckmann TR, Abraham AJ, Bride BE. Implementation of motivational interviewing in substance use disorder treatment: research network participation and organizational compatibility. J Addict Med. 2016;10:402–7. https://doi.org/10.1097/ADM.0000000000000251 .
Rieckmann TR, Abraham AJ, Kovas AE, Mcfarland BH, Roman PM. Impact of research network participation on the adoption of buprenorphine for substance abuse treatment. Addict Behav. 2014;39:889–96. https://doi.org/10.1016/j.addbeh.2014.01.016 .
Rindal DB, Flottemesch TJ, Durand EU, Godlevsky OV, Schmidt AM, Gilbert GH. Practice change toward better adherence to evidence-based treatment of early dental decay in the National Dental PBRN. Implement Sci. 2014;9:177. https://doi.org/10.1186/s13012-014-0177-x .
Robinson TG, Wang X, Durham AC, Ford GA, Liao J, Littlewood S, et al. The National Institute for Health Research Hyperacute Stroke Research Centres and the ENCHANTED trial: the impact of enhanced research infrastructure on trial metrics and patient outcomes. Health Res Policy Syst. 2019;17:19. https://doi.org/10.1186/s12961-019-0417-2 .
Rochon J, Du Bois A, Lange T. Mediation analysis of the relationship between institutional research activity and patient survival. BMC Med Res Methodol. 2014;14:9. https://doi.org/10.1186/1471-2288-14-9 .
Salge TO, Vera A. Hospital innovativeness and organizational performance: evidence from English public acute care. Health Care Manag Rev. 2009;34:54–67. https://doi.org/10.1097/01.HMR.0000342978.84307.80 .
Seaburg LA, Wang AT, West CP, Reed DA, Halvorsen AJ, Engstler G, et al. Associations between resident physicians’ publications and clinical performance during residency training. BMC Med Educ. 2016;16:22. https://doi.org/10.1186/s12909-016-0543-2 .
Shen M, Liang X, Li L, Wu Y, Yang Y, Zingg R. The association of attending physicians’ publications and patients’ readmission rates: evidence from tertiary hospitals in china using a retrospective data analysis. Int J Environ Res Public Health. 2022;19(15):9760. https://doi.org/10.3390/ijerph19159760 .
Siracuse JJ, Goodney PP, Menard MT, Rosenfield K, Van Over M, Hamza T, et al. Participation in a chronic limb threatening ischemia randomized trial is inversely correlated with regional amputation rate in limb threatening ischemia patients. Ann Surg. 2021;274(4):621–6. https://doi.org/10.1097/SLA.0000000000005058 .
Tan HJ, Meyer AM, Kuo TM, Smith AB, Wheeler SB, Carpenter WR, et al. Provider-based research networks and diffusion of surgical technologies among patients with early-stage kidney cancer. Cancer. 2015;121:836–43. https://doi.org/10.1002/cncr.29144 .
Tchetchik A, Grinstein A, Manes E, Shapira D, Durst R. From research to practice: which research strategy contributes more to clinical excellence? Comparing high-volume versus high-quality biomedical research. PLoS ONE. 2015;10: e0129259. https://doi.org/10.1371/journal.pone.0129259 .
Trusson D, Rowley E, Bramley L. A mixed-methods study of challenges and benefits of clinical academic careers for nurses, midwives and allied health professionals. BMJ Open. 2019;9: e030595. https://doi.org/10.1136/bmjopen-2019-030595 .
Tsang Y, Ciurlionis L, Kirby AM, Locke I, Venables K, Yarnold JR, et al. Clinical impact of IMPORT HIGH trial (CRUK/06/003) on breast radiotherapy practices in the United Kingdom. Br J Radiol. 2015;88:20150453. https://doi.org/10.1259/bjr.20150453 .
Tsang JLY, Binnie A, Duan EH, Johnstone J, Heels-Ansdell D, Reeve B. Academic and community ICUs participating in a critical care randomized trial: a comparison of patient characteristics and trial metrics. Crit Care Explor. 2022;4(11): e0794. https://doi.org/10.1097/CCE.0000000000000794 .
Van Der Tuuk K, Koopmans CM, Groen H, Mol BW, Van Pampus MG. Impact of the HYPITAT trial on doctors’ behaviour and prevalence of eclampsia in the Netherlands. BJOG. 2011;118:1658–60. https://doi.org/10.1111/j.1471-0528.2011.03138.x .
Venables K, Tsang Y, Ciurlionis L, Coles CE, Yarnold JR. Does participation in clinical trials influence the implementation of new techniques? A look at changing techniques in breast radiotherapy in the UK. Clin Oncol (R Coll Radiol). 2012;24:e100–5. https://doi.org/10.1016/j.clon.2012.06.010 .
Wolfson JA, Sun CL, Wyatt LP, Hurria A, Bhatia S. Impact of care at comprehensive cancer centers on outcome: results from a population-based study. Cancer. 2015;121(21):3885–93. https://doi.org/10.1002/cncr.29576 .
Wuthrick EJ, Zhang Q, Machtay M, Rosenthal DI, Nguyen-Tan PF, Fortin A, et al. Institutional clinical trial accrual volume and survival of patients with head and neck cancer. J Clin Oncol. 2015;33(2):156–64. https://doi.org/10.1200/JCO.2014.56.5218 .
Yawn BP, Pace W, Dietrich A, Bertram S, Kurland M, Graham D, et al. Practice benefit from participating in a practice-based research network study of postpartum depression: a national research network (NRN) report. J Am Board Fam Med. 2010;23:455–64. https://doi.org/10.3122/jabfm.2010.04.090246 .
Young C, Gunasekera H, Kong K, Purcell A, Muthayya S, Vincent F, et al. A case study of enhanced clinical care enabled by Aboriginal health research: the Hearing, EAr health and Language Services (HEALS) project. Aust N Z J Public Health. 2016;40:523–8. https://doi.org/10.1111/1753-6405.12586 .
Rogers E. Diffusion of innovations. 5th ed. New York: Free Press; 2003.
Cohen WM, Levinthal DA. Absorptive capacity: a new perspective on learning and innovation. Adm Sci Q. 1990;35(1):128–52.
Zahra SA, George G. Absorptive capacity: a review, reconceptualization, and extension. Acad Manag Rev. 2002;27:185–203. https://doi.org/10.5465/AMR.2002.6587995 .
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. https://doi.org/10.1186/1748-5908-4-50 .
Roman PM, Abraham AJ, Rothrauff TC, Knudsen HK. A longitudinal study of organizational formation, innovation adoption, and dissemination activities within the national drug abuse treatment clinical trials network. J Subst Abuse Treat. 2010;38(Suppl 1):S44-52. https://doi.org/10.1016/j.jsat.2009.12.008 .
Minasian LM, Carpenter WR, Weiner BJ, Anderson DE, McCaskill-Stevens W, Nelson S, et al. Translating research into evidence-based practice: the National Cancer Institute Community Clinical Oncology Program. Cancer. 2010;116:4440–9. https://doi.org/10.1002/cncr.25248 .
Fennell M, Warneke R. The diffusion of medical innovations: an applied network analysis: environment, development, and public policy and social services. Boston: Springer; 1988. https://doi.org/10.1007/978-1-4684-5436-9 .
Book Google Scholar
Peckham S, Eida T, Hashem F, Kendall S. Research engagement and research capacity building: a priority for healthcare organisations in the UK. J Health Organ Manag. 2023;37(3):343–59. https://doi.org/10.1108/JHOM-12-2021-0436 .
Edelman A, Brown A, Pain T, Larkins S, Harvey G. Evaluating research investment and impact at a regional Australian hospital and health service: a programme theory and conceptual framework. Health Res Policy Sys. 2020;18:30. https://doi.org/10.1186/s12961-020-0542-y .
Brown A, Edelman A, Pain T, Larkins S, Harvey G. “We’re not providing the best care if we are not on the cutting edge of research”: a research impact evaluation at a regional Australian hospital and health service. Int J Health Policy Manag. 2022;11(12):3000–11. https://doi.org/10.34172/IJHPM.2022.6529 .
San Francisco declaration on research assessment. https://sfdora.org/ . Accessed 18 Apr 2024.
Ailawadhi S, Advani P, Yang D, Ghosh R, Swaika A, et al. Impact of access to NCI- and NCCN-designated cancer centers on outcomes for multiple myeloma patients: a SEER registry analysis. Cancer. 2016;122:618–25. https://doi.org/10.1002/cncr.29771 .
Tsilimigras DI, Hyer JM, Diaz A, Moris D, Abbas A, Dillhoff M, et al. Impact of cancer center accreditation on outcomes of patients undergoing resection for hepatocellular carcinoma: a SEER-Medicare analysis. Am J Surg. 2021;222(3):570–6. https://doi.org/10.1016/j.amjsurg.2021.01.015 .
Grant J, Buxton MJ. Economic returns to medical research funding. BMJ Open. 2018;8: e022131. https://doi.org/10.1136/bmjopen-2018-022131 .
Schlick CJ, Yang AD. Is there value in cancer center accreditation? Am J Surg. 2023;220(1):27–8. https://doi.org/10.1016/j.amjsurg.2020.05.001 .
Hussein M, Pavlova M, Ghalwash M, Groot W. The impact of hospital accreditation on the quality of healthcare: a systematic literature review. BMC Health Serv Res. 2021;21:1057.
Yoong SL, Bolsewicz K, Reilly K, et al. Describing the evidence-base for research engagement by health care providers and health care organisations: a scoping review. BMC Health Serv Res. 2023;23:75. https://doi.org/10.1186/s12913-022-08887-2 .
Soper B, Yaqub O, Hinrichs S, Marjanovich S, Drabble S, Hanney S, et al. CLAHRCs in practice: combined knowledge transfer and exchange strategies, cultural change, and experimentation. J Health Serv Res Policy. 2013;18:53–64. https://doi.org/10.1177/1355819613499903 .
Kislov R, Wilson PM, Knowles S, Boaden R. Learning from the emergence of NIHR Collaborations for Leadership in Applied Health Research and Care (CLAHRCs): a systematic review of evaluations. Implement Sci. 2018;13:111. https://doi.org/10.1186/s13012-018-0805-y .
Download references
Acknowledgements
The authors would like to thank Teresa Jones for her expert advice on the search strategy. The review was completed as partial fulfilment of Belinda Goodenough’s Masters dissertation at King’s College London. In the original full report for our first review [ 3 ], we gratefully acknowledged the valuable help we had received from our expert advisory group. The members included two patient representatives who were consulted at various stages throughout the project, especially around the necessity of having our systematic review focus on the complexities of benefits from research engagement by healthcare organizations and staff, while separate reviews and analyses focussed on the benefits of PPI in health research.
Author information
Authors and affiliations.
Health and Social Care Workforce Research Unit, King’s Policy Institute, King’s College London, Virginia Woolf Building, 20 Kingsway, London, United Kingdom
Annette Boaz
The Sax Institute, Sydney, NSW, Australia
Belinda Goodenough
Brunel University London, Uxbridge, United Kingdom
Stephen Hanney & Bryony Soper
You can also search for this author in PubMed Google Scholar
Contributions
All authors were involved in planning the study. B.G. conducted the searches, with all authors involved in screening and analysis. B.G. produced an initial draft of the paper. The final version of the paper was produced collaboratively by all the authors.
Corresponding author
Correspondence to Annette Boaz .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Boaz, A., Goodenough, B., Hanney, S. et al. If health organisations and staff engage in research, does healthcare improve? Strengthening the evidence base through systematic reviews. Health Res Policy Sys 22 , 113 (2024). https://doi.org/10.1186/s12961-024-01187-7
Download citation
Received : 14 May 2024
Accepted : 22 July 2024
Published : 19 August 2024
DOI : https://doi.org/10.1186/s12961-024-01187-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical trials
- Healthcare organizations
- Patient outcomes
- Processes of care
- Research engagement
- Systematic review
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 19 August 2024
The impact of study habits and personal factors on the academic achievement performances of medical students
- Mohammed A. Aljaffer 1 ,
- Ahmad H. Almadani 1 ,
- Abdullah S. AlDughaither 2 ,
- Ali A. Basfar 2 ,
- Saad M. AlGhadir 2 ,
- Yahya A. AlGhamdi 2 ,
- Bassam N. AlHubaysh 2 ,
- Osamah A. AlMayouf 2 ,
- Saleh A. AlGhamdi 3 ,
- Tauseef Ahmad 4 &
- Hamza M. Abdulghani 5
BMC Medical Education volume 24 , Article number: 888 ( 2024 ) Cite this article
61 Accesses
2 Altmetric
Metrics details
Academic achievement is essential for all students seeking a successful career. Studying habits and routines is crucial in achieving such an ultimate goal.
This study investigates the association between study habits, personal factors, and academic achievement, aiming to identify factors that distinguish academically successful medical students.
A cross-sectional study was conducted at the College of Medicine, King Saud University, Riyadh, Saudi Arabia. The participants consisted of 1st through 5th-year medical students, with a sample size of 336. The research team collected study data using an electronic questionnaire containing three sections: socio-demographic data, personal characteristics, and study habits.
The study results indicated a statistically significant association between self-fulfillment as a motivation toward studying and academic achievement ( p = 0.04). The results also showed a statistically significant correlation between recalling recently memorized information and academic achievement ( p = 0.05). Furthermore, a statistically significant association between preferring the information to be presented in a graphical form rather than a written one and academic achievement was also found ( p = 0.03). Students who were satisfied with their academic performance had 1.6 times greater chances of having a high-grade point average (OR = 1.6, p = 0.08).
The results of this study support the available literature, indicating a correlation between study habits and high academic performance. Further multicenter studies are warranted to differentiate between high-achieving students and their peers using qualitative, semi-structured interviews. Educating the students about healthy study habits and enhancing their learning skills would also be of value.
Peer Review reports
Introduction
Academic performance is a common indicator used to measure student achievement [ 1 , 2 ]. It is a compound process influenced by many factors, among which is study habits [ 2 , 3 ]. Study habit is defined as different individual behavior in relation to studying, and is a combination of study methods and skills [ 2 , 3 , 4 ]. Put differently, study habits involve various techniques that would increase motivation and transform the study process into an effective one, thus enhancing learning [ 5 ]. Students’ perspectives and approaches toward studying were found to be the key factors in predicting their academic success [ 6 , 7 ]. However, these learning processes vary from one student to another due to variations in the students’ cognitive processing [ 8 ].
The study habits of students are the regular practices and habits they exhibit during the learning process [ 9 , 10 ]. Over time, several study habits have been developed, such as time management, setting appropriate goals, choosing a comfortable study environment, taking notes effectively, choosing main ideas, and being organized [ 11 ]. Global research shows that study habits impact academic performance and are the most important predictor of it [ 12 ]. It is difficult for medical students to organize and learn a lot of information, and they need to employ study skills to succeed [ 1 , 2 , 5 , 13 ].
Different lifestyle and social factors could affect students’ academic performance. For instance, Jafari et al. found that native students had better study habits compared to dormitory students [ 1 ]. This discrepancy between native and dormitory students was also indicated by Jouhari et al. who illustrated that dormitory students scored lower in attitude, test strategies, choosing main ideas, and concentration [ 10 ]. Regarding sleeping habits, Curcio G et al. found that students with a regular and adequate sleeping pattern had higher Grade Point Average (GPA) scores [ 14 ]. Lifestyle factors, such as watching television and listening to music, were shown to be unremarkable in affecting students’ grades [ 15 , 16 ]. Social media applications, including WhatsApp, Facebook, and Twitter, distract students during learning [ 16 , 17 ].
Motivation was found to be a major factor in students’ academic success. Bonsaksen et al. found that students who chose “to seek meaning” when studying were associated with high GPA scores [ 18 ]. In addition, low scores on “fear of failure” and high scores on “achieving” correlated with a higher GPA [ 8 , 18 ].
Resource-wise, Alzahrani et al. found that 82.7% of students relied on textbooks assigned by the department, while 46.6% mainly relied on the department’s lecture slides [ 19 ]. The study also indicated that 78.8% perceived that the scientific contents of the lectures were adequate [ 19 ]. Another study found that most students relied on the lecture slides (> 83%) along with their notes, followed by educational videos (76.1%), and reference textbooks (46.1%) [ 20 ]. Striking evidence in that study, as well as in another study, indicated that most students tended to avoid textbooks and opted for lecture slides, especially when preparing for exams [ 20 , 21 ].
Several researchers studied the association between different factors and academic performance; however, more is needed to know about this association in the process of education among medical students [ 15 , 20 , 22 ], with some limitations to the conducted studies. Such limitations include the study sample and using self-reported questionnaires, which may generate inaccurate results. Moreover, in Saudi Arabia in particular, the literature concerning the topic remains limited. Since many students are unsatisfied with their performance and seek improvement [ 10 ], the present study was designed and conducted.
Unlike other studies in the region, this study aims to investigate the relationship between study habits and personal factors and measure their influence on academic achievement. The results of this study could raise awareness regarding the effect of study habits and personal factors on students’ performance and would also guide them toward achieving academic success. The study also seeks to identify the factors that distinguish academically successful students from their peers.
Study design, setting, and participants
This observational cross-sectional study, which took place between June and December 2022, was conducted among students attending the College of Medicine at King Saud University (KSU), Riyadh, Saudi Arabia. Its targeted population included all male and female medical students (first to fifth years) attending KSU during the academic year 2021/2022. Whereas, students at other colleges and universities, those who failed to complete the questionnaire, interns (the students who already graduated), and those who were enrolled in the university’s preparatory year, were all excluded from the current study. The sample size was calculated based on a study conducted in 2015 by Lana Al Shawwa [ 15 ]. Using the sample size formula for a single proportion (0.79), the required sample size was 255 using a confidence interval of 95% and a margin of error of 5%. After adding a 20% margin to accommodate non-responses and incomplete responses, the calculated sample size required for this study was 306. However, our research team collected a total of 336 participants for this study to ensure complete representation.
Study instrument
The research team developed and used an electronic questionnaire. The rationale is that no standardized questionnaire measuring the study objectives was found in the literature. However, the questionnaire was tested on a pilot of 15 students to test its clarity and address any possible misconceptions and ambiguity. The study questionnaire was distributed randomly to this cohort, who were asked to fill out the questionnaire. The students reported a complete understanding of the questionnaire’s contents, so the same questionnaire was used without any modifications. The questionnaire, written in English, consisted of three parts. The first part included eleven questions about the socio-demographic status of the participants. The second part contained twenty-one questions examining personal factors such as sleep and caffeine consumption. The last part included twenty-one questions regarding students’ study habits. The questionnaire was constructed based on an ordinal Likert scale which had: strongly agree, agree, neutral, disagree, and strongly disagree as possible answers. The questionnaire was sent to participants through email and social media applications like Twitter and WhatsApp to increase the study response. An informed consent that clearly states the study’s purpose was taken from all participants at the beginning of the questionnaire. In addition, all participants were assured that the collected data would be anonymous and confidential. Each participant was represented by a code for the sole purpose of analyzing the data. Furthermore, no incentives or rewards were given to the participants for their participation.
Study variables
Socio-demographic information (such as age, gender, and academic year), and personal factors (such as motivation, sleeping status, caffeine consumption, and self-management) were the independent variables. Study habits such as attendance, individual versus group study, memorization techniques, revision, learning style, and strategies were also independent variables.
Academic achievement refers to a student’s success in gaining knowledge and understanding in various subjects, as well as the ability to apply that knowledge effectively [ 23 ]. It is a measure of the student’s progress throughout the educational journey, encompassing both academic achievements and personal growth [ 3 , 24 ]. Academic achievement is judged based on the student’s GPA or performance score. In this study, students’ GPA scores, awareness, and satisfaction regarding their academic performance were the dependent variables.
We divided the study sample into two groups based on the GPA. We considered students with high GPAs to be exposed (i.e. exposed to the study habits we are investigating), and students with low GPAs to be the control group. The purpose of this study was to determine why an exposed group of students gets high grades and what study factors they adopt. Based on this exposure (high achieving students), we concluded what methods they used to achieve higher grades. Those in the first group had a GPA greater or equal to 4.5 (out of 5), while those in the second group had a GPA less than 4.5. The students’ data were kept confidential and never used for any other purpose.
Data analysis
The data collected were analyzed by using IBM SPSS Statistical software for Windows version 24.0. Descriptive statistics such as frequency and percentage were used to describe the socio-demographic data in a tabular form. Furthermore, data for categorical variables, including different study habits, motivation factors, memorizing and revising factors, and lifestyle factors, were tabulated and analyzed using the odds ratio test. Finally, we calculated the odds ratio statistic and a p-value of 0.05 to report the statistical significance of our results.
Ethical approval and consent to Participate
Before conducting the study, the research team obtained the Ethics Committee Approval from the Institutional Review Board of the College of Medicine, KSU, Riyadh, Saudi Arabia (project No. E-22-7044). Participants’ agreement/consent to participate was guaranteed by choosing “agree” after reading the consent form at the beginning of the questionnaire. Participation was voluntary, and consent was obtained from all participants. The research team carried out all methods following relevant guidelines and regulations.
The total 336 medical students participated in the study. All participants completed the study questionnaire, and there were no missing or incomplete data, with all of them being able to participate. As shown in Table 1 9.3% of participants were between 18 and 20, 44.9% were between the ages of 21 and 22, and 35.8% were 23–28 years old. In the current study, 62.5% of the participants were males and 37.5% were females. The proportion of first-year students was 21.4%, 20.8% of second-year students, 20.8% of third-year students, 18.2% of fourth-year students, and 18.8% of fifth-year students, according to academic year levels. Regarding GPA scores, 36.9% scored 4.75-5 and 32.4% scored 4.5–4.74. 23.8% achieved 4-4.49, 6.5% achieved 3-3.99, and only 0.4% achieved 2.99 or less. Participants lived with their families in 94.6% of cases, with friends in 1.2% of cases, and alone in 4.2% of cases. For smoking habits, 86.3% did not smoke, 11% reported using vapes, 2.1% used cigarettes, and 0.6% used Shisha. 91.4% of the participants did not report any chronic illnesses; however, 8.6% did. In addition, 83% had no mental illness, 8.9% had anxiety, 6% had depression, and 2.1% reported other mental illnesses.
Table 2 shows motivational factors associated with academic performance. There was a clear difference in motivation factors between students with high and low achievement in the current study. Students with high GPAs were 1.67 times more motivated toward their careers (OR = 1.67, p = 0.09) than those with low GPAs. Furthermore, significant differences were found between those students who had self-fulfillment or ambitions in life they had ~ 2 times higher (OR = 1.93, p = 0.04) GPA scores than low GPA students. Exam results did not motivate exposed or high GPA students (46%) or control students with low GPA students (41%), but the current study showed test results had little impact on low achiever students (OR = 1.03, p = 0.88). Furthermore, 72.6% of high achievers were satisfied with their academic performance, while only 41% of low achiever students were satisfied. Therefore, students who were satisfied with their academic performance had 1.6 times greater chances of a higher GPA (OR = 1.6, p = 0.08). Students who get support and help from those around them are more likely to get high GPAs (OR = 1.1, p = 0.73) than those who do not receive any support. When students reported feeling a sense of family responsibility, the odds (odds ratio) of their receiving higher grades were 1.15 times higher (OR = 1.15, p = 0.6) compared to those who did not feel a sense of family responsibility. The p-value, which indicates the level of statistical significance, was 0.6.
Table 3 shows the study habits of higher achiever students and low achiever students. Most of the high-achieving students (79.0%) attended most of the lectures and had 1.6 times higher chances of getting higher grades (OR = 1.6, p = 0.2) than those who did not attend regular lectures. The current study found that studying alone had no significant impact on academic achievement in either group. However, those students who had studied alone had lower GPAs (OR = 1.07, p = 0.81). The current study findings reported 29.8% of students walk or stand while studying rather than sit, and they had 1.57 times higher GPA chances compared to students with lower GPAs (OR = 0.73, p = 0.27). High achievers (54.0%) preferred studying early in the morning, and these students had higher chances of achieving good GPAs (OR = 1.3, p = 0.28) than low achiever groups of students. The number of students with high achievement (39.5%) went through the lecture before the lesson was taught. These students had 1.08 times higher chances of achieving than low achiever groups of students. Furthermore, students who made a weekly study schedule had 1.3 times higher chances of being good academic achievers than those who did not (OR = 1.3, p = 0.37). Additionally, high-achieving students paid closer attention to the lecturer (1.2 times higher). In addition, students with high GPAs spent more time studying when exam dates approached (OR = 1.3, p = 0.58).
Table 4 demonstrates the relationship between memorizing and revising with high and low GPA students. It was found that high achiever students (58.9%) studied lectures daily and had 1.4 times higher chances of achieving high grades (OR = 1.4, p = 0.16) than the other group. It was found that most of the high achievers (62.1%) skim the lecture beforehand before memorizing it, which led to 1.8 times higher chances of getting good grades in this exam (OR = 1.8, p = 0.06). One regular activity reported by high GPA students (82.3%) was recalling what had just been memorized. For this recalling technique, we found a significant difference between low-achieving students (OR = 0.8, p = 0.63) and high-achieving students (OR = 1.83, p = 0.05). A high achiever student writes notes before speaking out for the memorizing method, which gives 1.2 times greater chances of getting high grades (OR = 1.2, p = 0.55) than a student who does not write notes. A major difference in the current study was that high GPA achievers (70.2%) revise lectures more frequently than low GPA achievers (57.1%). They had 1.5 times more chances of getting high grades if they practiced and revised this method (OR = 1.5, p = 0.13).
Table 5 illustrates the relationship between negative lifestyle factors and students’ academic performance. The current study found that students are less likely to get high exam grades when they smoke. Students who smoke cigarettes and those who vape are 1.14 and 1.07 times respectively more likely to have a decrease in GPA than those who do not smoke. Those students with chronic illnesses had 1.22 times higher chances of a downgrade in the exam (OR = 1.22, p = 0.49). Additionally, students with high GPAs had higher mental pressures (Anxiety = 1.2, Depression = 1.18, and other mental pressures = 1.57) than those with low GPAs.
Learning is a multifaceted process that evolves throughout our lifetimes. The leading indicator that sets students apart is their academic achievement. Hence, it is crucial to investigate the factors that influence it. The present study examined the relationship between different study habits, personal characteristics, and academic achievement among medical students. In medical education, and more so in Saudi Arabia, there needs to be more understanding regarding such vital aspects.
Regarding motivational factors, the present study found some differences between high and low achievers. Students with high GPA scores were more motivated toward their future careers (OR = 1.67, p = 0.09). The study also indicated that students who had ambitions and sought self-fulfillment were more likely to have high GPA scores, which were statistically significant (OR = 1.93, p = 0.04). This was consistent with Bin Abdulrahman et al. [ 20 ], who indicated that the highest motivation was self-fulfillment and satisfying family dreams, followed by a high educational level, aspirations to join a high-quality residency program, and high income. Their study also found that few students were motivated by the desire to be regarded as unique students. We hypothesize that this probably goes back to human nature, where a highly rewarding incentive becomes the driving force of our work. Hence, schools should utilize this finding in exploring ways to enhance students’ motivation toward learning.
The present study did not find a significant effect of previous exam results on academic performance (OR = 1.03, p = 0.88). However, some studies reported that more than half of the high-achieving students admitted that high scores acquired on previous assessments are an important motivational factor [ 15 , 25 , 26 ]. We hypothesize that as students score higher marks, they become pleased and feel confident with their study approach. This finding shows how positive measurable results influence the students’ mentality.
The present study also explored the social environment surrounding medical students. The results indicated that those who were supported by their friends or family were slightly more likely to score higher GPAs (OR = 1.1, p = 0.73); however, the results did not reach a statistical significance. We hypothesize that a supportive and understanding environment would push the students to be patient and look for a brighter future. Our study results were consistent with previous published studies, which showed an association [ 3 , 27 , 28 , 29 , 30 ]. We hypothesize that students who spend most of their time with their families had less time to study, which made their study time more valuable. The findings of this study will hopefully raise awareness concerning the precious time that students have each day.
The association of different study habits among medical students with high and low GPAs was also studied in our study. It was noted that the high-achieving students try to attend their lectures compared to the lower achievers. This was in line with the previous published studies, which showed that significant differences were observed between the two groups regarding the attendance of lectures, tutorials, practical sessions, and clinical teachings [ 31 , 32 ]. The present study found that most students prefer to study alone, regardless of their level of academic achievement (82.1%). This finding is consistent with the study by Khalid A Bin Abdulrahman et al., which also showed that most students, regardless of their GPA, favored studying alone [ 20 ].
The present study findings suggest that a small number of students (29.8%) prefer to walk or stand while studying rather than sit, with most being high achievers (OR = 1.57, P = 0.15). A study reported that 40.3% of students with high GPAs seemed to favor a certain posture or body position, such as sitting or lying on the floor [ 15 ]. These contradictory findings might indicate that which position to adopt while studying should come down to personal preference and what feels most comfortable to each student. The present study also found that high achievers are more likely to prefer studying early in the morning (OR = 1.3, P = 0.28). The authors did not find similar studies investigating this same association in the literature. However, mornings might allow for more focused studying with fewer distractions, which has been shown to be associated with higher achievement in medical students [ 3 , 15 , 33 ].
Our study also found that 39.5% of the academically successful students reviewed pre-work or went through the material before they were taught it (OR = 1.08, p = 0.75), and 25% were neutral. Similar findings were reported in other studies, showing that academically successful students prepared themselves by doing their pre-work, watching videos, and revising slides [ 3 , 9 , 34 ]. Our study showed that 75% of high-achieving students tend to listen attentively to the lecturer (OR = 1.2, p = 0.48). Al Shawa et al. found no significant differences between the high achievers and low achievers when talking about attending lectures [ 15 ]. This could be due to the quality of teachers and the environment of the college or university.
Regarding the relationship between memorizing and revising with high and low GPA students, the present study found that students who study lectures daily are more likely to score higher than those who do not (OR = 1.4, p = 0.16). This finding is consistent with other studies [ 3 , 19 , 35 ]. For skimming lectures beforehand, an appreciable agreement was noted by high GPA students (62.1%), while only (42%) of low GPA students agreed to it. Similarly, previous published studies also found that highlighting and reading the content before memorization were both common among high-achieving students [ 15 , 36 ]. Furthermore, the present study has found recalling what has just been memorized to be statistically significantly associated with high GPA students (OR = 1.83, p = 0.05). Interestingly, we could not find any study that investigated this as an important factor, which could be justified by the high specificity of this question. Besides, when it comes to writing down/speaking out what has just been memorized, our study has found no recognizable differences between high-achieving students (75%) and low-achieving students (69%), as both categories had remarkably high percentages of reading and writing while studying.
The present study has found no statistical significance between regularly revising the lectures and high GPA ( p > 0.05), unlike the study conducted by Deborah A. Sleight et al. [ 37 ]. The difference in findings between our study and Deborah A. Sleight et al. might be due to a limitation of our study, namely the similar backgrounds of our participants. Another explanation could be related to curricular differences between the institutions where the two studies were conducted. Moreover, a statistically significant correlation between not preferring the data being presented in a written form instead of a graphical form and high GPA scores have been found in their study ( p < 0.05). However, a study conducted by Deborah A. Sleight et al. indicated that 66% of high achievers used notes prepared by other classmates compared to 84% of low achievers. Moreover, their study showed that only 59% of high achievers used tables and graphs prepared by others compared to 92% of low achievers. About 63% and 61% of the students in their study reported using self-made study aids for revision and memory aids, respectively [ 37 ].
The present study also examined the effects of smoking and chronic and mental illness, but found no statistical significance; the majority of both groups responded by denying these factors’ presence in their life. A similar finding by Al Shawwa et al. showed no statistical significance of smoking and caffeine consumption between low GPA and high GPA students [ 15 ]. We hypothesize that our findings occurred due to the study’s broad approach to examining such factors rather than delving deeper into them.
High-achieving students’ habits and factors contributing to their academic achievement were explored in the present study. High-achieving students were found to be more motivated and socially supported than their peers. Moreover, students who attended lectures, concentrated during lectures, studied early in the morning, prepared their weekly schedule, and studied more when exams approached were more likely to have high GPA scores. Studying techniques, including skimming before memorizing, writing what was memorized, active recall, and consistent revision, were adopted by high-achievers. To gain deeper insight into students’ strategies, it is recommended that qualitative semi-structured interviews be conducted to understand what distinguishes high-achieving students from their peers. Future studies should also explore differences between public and private university students. Additionally, further research is needed to confirm this study’s findings and provide guidance to all students. Future studies should collect a larger sample size from a variety of universities in order to increase generalizability.
Limitations and recommendations
The present study has some limitations. All the study’s findings indicated possible associations rather than causation; hence, the reader should approach the results of this study with caution. We recommend in-depth longitudinal studies to provide more insight into the different study habits and their impact on academic performance. Another limitation is that the research team created a self-reported questionnaire to address the study objectives, which carries a potential risk of bias. Hence, we recommend conducting interviews and having personal encounters with the study’s participants to reduce the risk of bias and better understand how different factors affect their academic achievement. A third limitation is that the research team only used the GPA scores as indicators of academic achievement. We recommend conducting other studies and investigating factors that cannot be solely reflected by the GPA, such as the student’s clinical performance and skills. Lastly, all participants included in the study share one background and live in the same environment. Therefore, the study’s findings do not necessarily apply to students who do not belong to such a geographic area and point in time. We recommend that future studies consider the sociodemographic and socioeconomic variations that exist among the universities in Saudi Arabia.
Availability of data materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Grade Point Average
King Saud University
Institutional review board
Statistical package for the social sciences
Jafari H, Aghaei A, Khatony A. Relationship between study habits and academic achievement in students of medical sciences in Kermanshah-Iran. Adv Med Educ Pract. 2019;10:637–43.
Article Google Scholar
Abid N, Aslam S, Alghamdi AA, Kumar T. Relationships among students’ reading habits, study skills, and academic achievement in English at the secondary level. Front Psychol. 2023;14:1020269.
Abdulghani HM, Al-Drees AA, Khalil MS, Ahmad F, Ponnamperuma GG, Amin Z. What factors determine academic achievement in high achieving undergraduate medical students? A qualitative study. Med Teach. 2014;36(Suppl 1):S43–48.
Muntean LM, Nireștean A, Sima-Comaniciu A, Mărușteri M, Zăgan CA, Lukacs E. The relationship between personality, motivation and academic performance at Medical students from Romania. Int J Environ Res Public Health 2022, 19(15).
Reza HM, Alireza HJIJME. Investigating study Habits of Library and Information Sciences Students of Isfahan University and Isfahan University of Medical Sciences. 2014, 14:751–757.
Kurtz SM, Silverman JD. The Calgary-Cambridge Referenced Observation guides: an aid to defining the curriculum and organizing the teaching in communication training programmes. Med Educ. 1996;30(2):83–9.
Pun J, Kong B. An exploratory study of communication training for Chinese medicine practitioners in Hong Kong to integrate patients’ conventional medical history. BMC Complement Med Ther. 2023;23(1):10.
İlçin N, Tomruk M, Yeşilyaprak SS, Karadibak D, Savcı S. The relationship between learning styles and academic performance in TURKISH physiotherapy students. BMC Med Educ. 2018;18(1):291.
McKeirnan KC, Colorafi K, Kim AP, Stewart AS, Remsberg CM, Vu M, Bray BS. Study behaviors Associated with Student pharmacists’ academic success in an active Classroom Pharmacy Curriculum. Am J Pharm Educ. 2020;84(7):ajpe7695.
Jouhari Z, Haghani F, Changiz T. Assessment of medical students’ learning and study strategies in self-regulated learning. J Adv Med Educ Professionalism. 2016;4(2):72–9.
Google Scholar
Proctor BE, Prevatt FF, Adams KSS, Reaser A, Petscher Y. Study skills profiles of normal-achieving and academically-struggling College students. J Coll Student Dev. 2006;47(1):37–51.
Kyauta AMASY, Garba HS. The role of guidance and counseling service on academic performance among students of umar suleiman college of education, Gashua, Yobe State, Nigeria. KIU J Humanit. 2017;2(2):59–66.
Eva KW, Bordage G, Campbell C, Galbraith R, Ginsburg S, Holmboe E, Regehr G. Towards a program of assessment for health professionals: from training into practice. Adv Health Sci Education: Theory Pract. 2016;21(4):897–913.
Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10(5):323–37.
Al Shawwa L, Abulaban AA, Abulaban AA, Merdad A, Baghlaf S, Algethami A, Abu-Shanab J, Balkhoyor A. Factors potentially influencing academic performance among medical students. Adv Med Educ Pract. 2015;6:65–75.
Ibrahim NK, Baharoon BS, Banjar WF, Jar AA, Ashor RM, Aman AA, Al-Ahmadi JR. Mobile Phone Addiction and its relationship to Sleep Quality and Academic Achievement of Medical students at King Abdulaziz University, Jeddah, Saudi Arabia. J Res Health Sci. 2018;18(3):e00420.
Alkhalaf AM, Tekian A, Park YS. The impact of WhatsApp use on academic achievement among Saudi medical students. Med Teach. 2018;40(sup1):S10–4.
Bonsaksen T, Brown T, Lim HB, Fong K. Approaches to studying predict academic performance in undergraduate occupational therapy students: a cross-cultural study. BMC Med Educ. 2017;17(1):76.
Alzahrani HA, Alzahrani OH. Learning strategies of medical students in the surgery department, Jeddah, Saudi Arabia. Adv Med Educ Pract. 2012;3:79–87.
Bin Abdulrahman KA, Khalaf AM, Bin Abbas FB, Alanazi OT. Study habits of highly effective medical students. Adv Med Educ Pract. 2021;12:627–33.
Jameel T, Gazzaz ZJ, Baig M, Tashkandi JM, Alharenth NS, Butt NS, Shafique A, Iftikhar R. Medical students’ preferences towards learning resources and their study habits at King Abdulaziz University, Jeddah, Saudi Arabia. BMC Res Notes. 2019;12(1):30.
Abdulghani HM, Alrowais NA, Bin-Saad NS, Al-Subaie NM, Haji AM, Alhaqwi AI. Sleep disorder among medical students: relationship to their academic performance. Med Teach. 2012;34(Suppl 1):S37–41.
Hwang G-J, Wang S-Y, Lai C-L. Effects of a social regulation-based online learning framework on students’ learning achievements and behaviors in mathematics. Comput Educ. 2021;160:104031.
Gamage KAA, Dehideniya D, Ekanayake SY. The role of personal values in learning approaches and student achievements. Behav Sci (Basel Switzerland) 2021, 11(7).
Linn Z, Tashiro Y, Morio K, Hori H. Peer evaluations of group work in different years of medical school and academic achievement: how are they related? BMC Med Educ. 2022;22(1):102.
Avonts M, Michels NR, Bombeke K, Hens N, Coenen S, Vanderveken OM, De Winter BY. Does peer teaching improve academic results and competencies during medical school? A mixed methods study. BMC Med Educ. 2022;22(1):431.
Topor DR, Keane SP, Shelton TL, Calkins SD. Parent involvement and student academic performance: a multiple mediational analysis. J Prev Interv Community. 2010;38(3):183–97.
Veas A, Castejón JL, Miñano P, Gilar-Corbí R. Relationship between parent involvement and academic achievement through metacognitive strategies: a multiple multilevel mediation analysis. Br J Educ Psychol. 2019;89(2):393–411.
Núñez JC, Regueiro B, Suárez N, Piñeiro I, Rodicio ML, Valle A. Student Perception of teacher and parent involvement in Homework and Student Engagement: the mediating role of motivation. Front Psychol. 2019;10:1384.
Abdulghani AH, Ahmad T, Abdulghani HM. The impact of COVID-19 pandemic on anxiety and depression among physical therapists in Saudi Arabia: a cross-sectional study. BMC Med Educ. 2022;22(1):751.
Park KH, Park JH, Kim S, Rhee JA, Kim JH, Ahn YJ, Han JJ, Suh DJ. Students’ perception of the educational environment of medical schools in Korea: findings from a nationwide survey. Korean J Med Educ. 2015;27(2):117–30.
Ahrberg K, Dresler M, Niedermaier S, Steiger A, Genzel L. The interaction between sleep quality and academic performance. J Psychiatr Res. 2012;46(12):1618–22.
Dikker S, Haegens S, Bevilacqua D, Davidesco I, Wan L, Kaggen L, McClintock J, Chaloner K, Ding M, West T, et al. Morning brain: real-world neural evidence that high school class times matter. Soc Cognit Affect Neurosci. 2020;15(11):1193–202.
Pittenger AL, Dimitropoulos E, Foag J, Bishop D, Panizza S, Bishop JR. Closing the Classroom Theory to practice gap by simulating a Psychiatric Pharmacy Practice Experience. Am J Pharm Educ. 2019;83(10):7276.
Walck-Shannon EM, Rowell SF, Frey RF. To what extent do Study habits relate to performance? CBE Life Sci Educ. 2021;20(1):ar6.
Abdulghani HM, Alanazi K, Alotaibi R, Alsubeeh NA, Ahmad T, Haque S. Prevalence of potential dropout thoughts and their influential factors among Saudi Medical Students. 2023, 13(1):21582440221146966.
Sleight DA, Mavis BE. Study skills and academic performance among second-Year Medical students in Problem-based learning. Med Educ Online. 2006;11(1):4599.
Download references
Acknowledgements
The authors are grateful to the Deanship of Scientific Research, King Saud University, for.
support through the Vice Deanship of Scientific Research Chairs.
Author information
Authors and affiliations.
Department of Psychiatry, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Mohammed A. Aljaffer & Ahmad H. Almadani
College of Medicine, King Saud University, Riyadh, Saudi Arabia
Abdullah S. AlDughaither, Ali A. Basfar, Saad M. AlGhadir, Yahya A. AlGhamdi, Bassam N. AlHubaysh & Osamah A. AlMayouf
Department of Psychiatry, College of Medicine, Imam Mohammad Ibn Saud Islamic University, Riyadh, Saudi Arabia
Saleh A. AlGhamdi
Department of Medical Education, College of Medicine, King Saud University, P.O. Box: 230155, Riyadh, 11321, Saudi Arabia
Tauseef Ahmad
Department of Medical Education and Family Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Hamza M. Abdulghani
You can also search for this author in PubMed Google Scholar
Contributions
Conception or design: AHA, MAA, and HMA. Acquisition, analysis, or interpretation of data: AAB, SMA, ASA, YAA, BNA, OAA and SAA. Drafting the work or revising: TA, AHA, ASA AAB. Final approval of the manuscript: MAA, HMA., AHA, and TA. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Tauseef Ahmad .
Ethics declarations
Conflict of interest.
The Authors declare that they have no conflict of interest.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Human ethics and consent to participate declarations
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Aljaffer, M.A., Almadani, A.H., AlDughaither, A.S. et al. The impact of study habits and personal factors on the academic achievement performances of medical students. BMC Med Educ 24 , 888 (2024). https://doi.org/10.1186/s12909-024-05889-y
Download citation
Received : 26 September 2023
Accepted : 12 August 2024
Published : 19 August 2024
DOI : https://doi.org/10.1186/s12909-024-05889-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical students
- Study habits
- Academic achievement
- Saudi Arabia
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
- Open access
- Published: 20 August 2024
Psychosocial interventions for improving the physical health of young people and adults with attention deficit hyperactivity disorder: a scoping review
- John Headley Ward ORCID: orcid.org/0000-0002-9108-7900 1 , 2 , 3 , 4 ,
- Audrey McBride ORCID: orcid.org/0009-0003-9000-6667 1 ,
- Anna Price ORCID: orcid.org/0000-0001-9147-1876 1 &
- Tamsin Newlove Delgado ORCID: orcid.org/0000-0002-5192-3724 1
BMC Psychiatry volume 24 , Article number: 569 ( 2024 ) Cite this article
2 Altmetric
Metrics details
Young people and adults with ADHD are at risk of a range of physical health problems. There is limited guidance on how to approach health problems in ADHD, and especially around 16-25 year olds who will be transitioning from paediatric to adult care. The aim of this scoping review was to identify psychosocial interventions that target physical health in young people and adults with ADHD.
We constructed searches in MEDLINE, PsycInfo, EMBASE of adolescents, young people and adults. Inclusion criteria were; studies of psychosocial interventions examining a component of physical health, applicable to people aged 16-25, with clinical or research diagnoses of ADHD. Data were extracted using a data extraction tool and tabulated, including study intervention framing/aims, population, intervention, and relevant outcomes (including specific statistics where relevant).
Our search identified 22 unique papers covering, psychosocial interventions targeting at least one of sleep ( n= 7), smoking ( n= 3), substance/alcohol use ( n= 4), physical health/exercise ( n= 6) and general health ( n= 3). Studies examined psychotherapy/behaviour interventions ( n= 12), psychoeducation ( n= 4), digital ( n= 2) and social interventions ( n= 4). There was significant heterogeneity in intervention framing, outcome measures and population.
Further work on the impact of targeted physical health interventions, with explicit reference to a conceptual framework of poor health in ADHD is required. Furthermore, future work standardising reporting of physical health outcomes in ADHD is crucial for the development of an evidence base in this field.
Peer Review reports
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental condition characterised by combinations of hyperactivity, impulsivity, and inattention, thought to affect 5.6% of 12-18 year olds and 2.58% of adults [ 1 , 2 ]. Whilst traditionally thought of as a disorder of childhood, with a typical onset before the age of 12, it is now understood that symptoms can persist into adulthood and have a significant impact on many aspects of life, including physical health [ 3 , 4 , 5 , 6 ].
In respect to the links in research between ADHD and physical health, firstly there is a wealth of literature on the association between ADHD and higher rates of health risk behaviours, including smoking, alcohol abuse, substance misuse, risk-taking behaviour, self-harm, obesity and sleep disorders [ 6 , 7 , 8 , 9 , 10 , 11 ]. These findings are reproduced in studies using various methods including traits-based approaches, mendelian randomisation, case-control and longitudinal follow-up studies.
Secondly, there is a growing body of evidence demonstrating links between ADHD and non-communicable diseases. A large genetically informed Swedish registry study found that participants with ADHD were at higher risk for 34 out the 35 conditions studied compared to those without ADHD, including nervous system and respiratory disorders [ 12 ]. Other studies have also demonstrated high rates of neurological and respiratory disease, as well as gastrointestinal disorders and cardiovascular disease [ 13 , 14 , 15 ]. Furthermore, Stickley and colleagues [ 15 ] demonstrated that multimorbidity was predictive of whether study participants had ADHD. In respect to mortality, several longitudinal studies have noted increased mortality rates amongst people with ADHD. Whilst these appear to be driven by accidental and unnatural deaths, the cause remains contested [ 6 , 16 , 17 , 18 ].
There have been various attempts to explain the inequalities in physical health outcomes for this population. It has previously been suggested that people with ADHD may be less likely to follow government recommendations on health promotion, even when controlling for socioeconomic status [ 19 ]. This is echoed in work by Cherkasova et al , who reported that the persistence of ADHD symptoms into adulthood mediated poorer functional outcomes [ 6 ]. However, the large sibling analysis study of DuRietz et al highlights the importance of genetic risk factors in the association between ADHD and physical health, supported by their finding that shared genetic factors explained 60-69% of the relationship between ADHD and respiratory, musculoskeletal and metabolic disorders in their sample [ 20 ].
There have been previous studies suggesting that some of the health risks in ADHD may be mitigated by appropriate treatment of ADHD using medication (e.g., meta-analyses demonstrating the efficacy of medication in improving sleep or substance misuse [ 7 , 21 , 22 ]). In addition to medication, psychosocial interventions are likely to be important in the prevention and mitigation of health risks in ADHD, when provided as part of a holistic approach. Importantly, psychosocial interventions can also constitute health promotion and support health autonomy, which may be of particular significance to young adults transitioning to adult care [ 23 , 24 , 25 , 26 , 27 ]. There is a small and heterogenous body of research examining the efficacy of psychosocial interventions in the management of physical health problems associated with ADHD [ 28 , 29 , 30 , 31 , 32 , 33 ]. However, this has not yet been synthesised to identify the nature and extent of existing research or indicate targets for future research and intervention development. This is a significant evidence gap given the poorer physical health of people with ADHD, which adversely affects quality of life and economic, social and health outcomes [ 34 , 35 , 36 , 37 ].
This scoping review aims to identify and describe existing psychosocial interventions for physical health in young people and adults with ADHD, including those in preliminary stages (e.g. feasibility trials).
Given the lack of previous reviews in this field, and the need to provide a broad overview of available evidence, a scoping review was chosen to identify psychosocial interventions addressing physical health in ADHD. Scoping reviews are suitable for identifying research gaps, summarising research findings, clarifying concepts, and making recommendations for future research [ 38 ]. This scoping review aimed to identify relevant literature using an inclusive approach incorporating different methodologies and reflecting varying levels of quality [ 39 ].
The review followed a five-stage process as described by Arksey and O'Malley: identifying the question, identifying relevant studies, study selection, charting the data and collating, summarising and reporting the results [ 40 , 41 ]. We found no previous scoping reviews or systematic reviews examining this topic. We have reported our scoping review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Scoping Review Extension checklist (see supplementary materials) [ 42 ]. We did not pre-register this review protocol.
Eligibility criteria
Studies were eligible for inclusion in the review if they met four key eligibility criteria: a population aged 16 years or older (or including substantial representation of this group), diagnosed with ADHD (either clinically diagnosed, self-reported, or using a standardised diagnostic measure) (population and context), the introduction of a form of structured psychosocial intervention within an experimental trial (concept) and the measurement of a physical health outcome (outcome).
In respect to defining the population of interest, we sought interventions that would be relevant to young people and adults, of a transition care age group (16-25 year olds). This age bracket is important for two reasons. Firstly, it is well-understood that ADHD care begins to decline for older adolescents, as medication adherence and service access decline [ 25 , 26 ]. Secondly, the transition to adulthood is when adolescents begin to take responsibility for their own health and health behaviour, and therefore support around independent health management would be timely [ 23 , 24 , 27 ].
To meet the scoping review’s aim of identifying all interventions relevant to the population, we included studies of under 16s, and some studies of adults over 25 years old. This was the case where the proposed intervention had methods or findings that were clearly applicable to 16–25-year-olds. ‘Applicable’ in this context was defined as interventions that could be utilised in our population of interest without need for modification of the intervention itself. Given that this was a scoping review, we judged this was an appropriately inclusive approach to exploring a limited literature, with similar expanded definitions of age categories having been used in previous scoping reviews [ 43 , 44 , 45 ]. We did however exclude school-based interventions, (e.g., those which use a school or classroom-based approach in childhood) [ 46 ]. This was because our team considered that interventions set within classroom environments would not be replicable in young adults. Where inclusion criteria were borderline, decisions were made on a case-by-case basis and discussed by at least two reviewers (TND and JW).
For the purposes of this review, psychosocial interventions were defined as structured interventions that adopt a psychological, educational, or social framework. This definition was adapted from Ruddy and House, adapting the definition to include digital health interventions, which have taken prominence since the publication of their definition in 2005 [ 47 , 48 , 49 ]. In this review, we included search terms pertaining to psychotherapeutic interventions, behavioural interventions, digital interventions, peer/support groups, exercise-based interventions, and psychoeducational interventions.
Study outcomes were checked during the screening process to identify physical health outcomes. We defined physical health broadly as a chronic physical health problem and/or a current behaviour that confers a long-term physical health risk (e.g., unprotected sex, smoking). This definition was formed in collaboration with the Managing Young People with ADHD in Primary Care (MAP) study academic team and research advisory group (RAG) which was composed of people with lived experience [ 50 ]. Physical health outcomes included scales (e.g., sleep indices, health-related quality of life), objective measures (e.g., reductions in alcohol consumption, abstinence) and subjective measures (e.g., sleep diaries). Studies were excluded if there was no clear physical health outcome recorded in either the published paper or its supplementary materials. We deliberately did not pre-define specific physical health concerns in our search. This was because, in conjunction with our MAP study advisory team, we felt this would be a more appropriate approach for an initial exploration aimed at capturing the breadth of health problems being addressed. In pre-defining health problems, we considered there would be a risk of excluding studies which incidentally notes physical health outcomes.
Studies from the grey literature were excluded, as well as studies not written in the English language, due to resource limitations. We also excluded non peer-reviewed scientific literature (e.g. dissertations, preprints, conference proceedings). We did not exclude studies where participants received a biological therapy (e.g. medication, bright light therapy), if they also received a psychosocial intervention. This approach enabled a broad spread of relevant included studies and met the review’s objective of identifying feasible interventions.
Search strategy
The search strategy was developed with information specialists at the at the University of Exeter. Searches were performed using MEDLINE (1946 onwards), Embase (1974 onwards ) and PsycInfo (1803 onwards ), via the Ovid © platform.
Searching took place in two phases, to ensure adequate inclusion of young people/youths and adults (Fig. 1 ). In the first phase, we used our young people/youth search terms and our adult terms (search dates 7 th October 2022 and 24 th November 2022 respectively). The process of search design through the completion of title and abstract screening was from September 2022 to December 2022, with full-text inclusions from this search decided by January 2023.

Flow diagram of database searches, title/abstract screening and full text screening
In order to ensure that we included publications relating to applicable interventions that were tested in a younger population (i.e. 13-17 year olds), a second phase included a search using adolescent search terms, conducted in February 2024, with title/abstract and full text-screening screening completed in March 2024. This search included literature published up until February 2024. Full details of all searches can be seen in supplementary materials.
ADHD search terms were adapted from the search terms used by the National Institute for Care and Health Excellence (NICE) in their development of ADHD guidance [ 51 ]. Search terms for psychosocial interventions were adapted from the search terms used by NICE in the development of their guidance for lower back pain and diabetes [ 52 , 53 ]. These were adapted as appropriate for our search and are available in supplementary materials.
Study selection
The study selection process is highlighted in Figure 1 . The first set of searches (young people/adults, October-November 2022) yielded 5258 results, and the second (adolescents, February 2024) 4293.
These studies were then screened by title and abstract independently by two reviewers (JW, TND), against inclusion criteria, with disagreements resolved by discussion. Where disagreements were not resolved, this was taken to the wider study team and MAP study principal investigator (PI) (AP). Citation chasing was also performed by examining references from relevant review and protocol studies to identify any further studies not found in our search.
This left 61 records for full-text screening. These were again double-screened (JW, TND), with disagreements resolved by discussion, and where necessary the wider study team, and principal investigator (AP), leaving 22 articles which were included at full-text screening. Reasons for full-text exclusions are given in Figure 1 .
Data extraction and charting
Studies were collated using a data extraction form and shared spreadsheet in which the data could be recorded. This data extraction tool was piloted on five papers initially, reviewed and then used for all papers. These were single entered by researchers (JW, AM), with all entries were re-reviewed after first entry (JW). The data extraction tool can be found in supplementary materials.
The data extraction process used narrative synthesis to collate information on what the intervention was targeting (and rationale), what outcomes were measured and how these were measured. This involved extracting study details (i.e., title, author), study design (comparator, methodology), population characteristics (age, gender, location of study), intervention framing of study (i.e. rationale for intervention chosen), ADHD definition (e.g., meeting DSM-V criteria, clinically diagnosed ADHD), relevant additional inclusion/exclusion criteria, primary and secondary outcomes of the studies and measures used, physical health findings, attendance reporting and ADHD symptom findings. Where studies had noted qualitative feedback on the interventions used, this was also collated and charted under outcomes.
Data were then charted in tabular form, by physical health problem addressed, with the extracted details on the studies provided alongside this.
Twenty-two studies met our inclusion criteria (Table 1 ). Physical health outcomes targeted or reported included sleep (seven studies), smoking (three studies), substance misuse (four studies), physical activity and/or weight (six studies) and more general/broad physical health outcomes (three studies). It should be noted that one study (Bjork et al .) covered two health outcomes (smoking, physical activity) [ 54 ]. Studies covered an overall age range of 11-65. Of these, eleven studies examined adolescents, ten studies examined adults (although four did not provide a precise age range), and one study examined both (14–30-year-olds) [ 55 ]. Only one included study had participants exclusively between 16-25, but this was a college-based study [ 56 ].
In respect to ADHD concept, 14/22 studies were based on clinical diagnosis, whilst 6/22 were criteria based, 1/22 used self-reported ADHD and 1/22 used ‘documented’ ADHD (Table 1 ). Where studies reported gender ( n= 16), 10 studies were at least 50% female, ranging from a 32% to 83% male sample. 14/22 studies included a physical health outcome as a primary outcome or target, whilst 5/22 studies included physical health as a secondary outcome [ 55 , 56 , 60 , 61 , 74 , 75 ]. 12/22 of the studies were of a psychotherapeutic or behavioural intervention, 4/22 of psychoeducation, 4/22 social/exercise interventions and 2/22 digital interventions. Most of the studies were conducted in the USA (8/22), followed by Sweden (5/22), the Netherlands (2/22) and Germany (2/22), with the others located in Brazil, Norway, Belgium, Denmark and China.
In respect to methodology, 13/22 studies were randomised controlled trials (RCTs) [ 56 , 63 , 66 , 67 , 68 , 70 , 75 , 76 , 77 ], 6/22 studies were single group (before and after) comparisons [ 54 , 57 , 59 , 60 , 69 , 73 ], one study was secondary analysis of RCT data [ 58 ], one study compared a single-group pre/post intervention with a previous study data [ 74 ], and finally one study compared two groups before and after comparison (not RCT) [ 64 ]. Apart from one study which was unfunded [ 73 ], and one study which did not clarify its funding [ 54 ], 20/22 studies were funded from non-commercial sources.
Sleep was examined as a health outcome in seven included studies, as described below in Table 2 [ 55 , 57 , 58 , 59 , 60 , 61 , 77 ]. All used different interventions, which can be broadly divided into psychoeducational interventions and psychotherapeutic interventions (e.g., adapted cognitive or dialectical behavioural therapy). One study examined primarily bright light therapy, however used psychoeducation around sleep in their methodology for both active arms and the placebo arm (hence its inclusion). Only one study included people with diagnosed sleep problems and ADHD, with the others including either a general ADHD population or those with self-reported sleep problems. Four of the studies included are completed or ongoing RCTs, with the rest being pilot/feasibility studies or single group intervention studies. Included studies had small sample sizes (three had fewer than 20 participants, only one had a sample size greater than 100) and covered a wide age range (13-63). Three studies suggested a rationale for their intervention within ADHD in relation to health needs; ADHD symptoms/executive dysfunction impacting on habits and sleep hygiene as the mechanism of sleep problems in ADHD [ 58 , 59 , 62 ] and delayed circadian rhythm/preference [ 58 , 59 ]. Whilst Becker et al referenced problems of adolescence in sleep, they did not explain the rationale within ADHD [ 57 ]. Van Andel et al (RCT (melatonin versus placebo versus melatonin and bright light therapy, where all arms received psychoeducation) did not find improvements in sleep for any group [ 58 ]. Meyer et al (RCT) also did not find sustained improvements in sleep for either their behavioural or control (psychoeducation group) [ 55 ]. However, the single group intervention and pilot studies did find evidence supporting behavioural and psychosocial interventions, including pilot feasibility data from Keuppens et al RCT [ 77 ]. Results also demonstrated tolerability and feasibility of these sleep interventions in ADHD; all completed studies noted good attendance at and compliance with interventions, whilst Becker et al. , Jernelov et al . and Keuppens et al. noted participants’ satisfaction with interventions. The subjective positive feedback received in Becker et al. included increased responsibility for health, working with a therapist and increased knowledge [ 57 ]. In Jernelov et al ., feedback received was the use of routines and structure [ 59 ]. For Keuppens et al. , thematic analysis generated themes for adolescents around having more control and independence around sleep, and that both parents and adolescents had better understanding of the impact of ADHD on sleep [ 77 ].
Smoking was examined as a health outcome in three studies, as presented in Table 3 [ 54 , 63 , 64 ]. These studies had an average sample size of 45 and covered both adolescents and adults. One of the studies was a randomised controlled trial (RCT), whilst the other two were a single-group intervention study and an ADHD vs non-ADHD single intervention study, neither with control groups. Two of the studies used psychoeducation, including components about smoking, whilst one of the studies used monetary incentives to encourage participants to stop smoking. In respect to mechanisms, two of the three studies suggested a rationale for their choice of intervention; targeting executive dysfunction in ADHD that may perpetuate smoking [ 54 , 64 ] and mental health difficulties in ADHD precipitating poor health behaviour [ 54 ]. The results were variable. The two studies examining tobacco use (Kollins et al ., Bjork et al .—non-randomised group trials) found no interventions with sustained effects, reporting that participants largely went back to smoking (irrespective of ADHD). Corona et al.’s study (also an RCT) found that the attitudes of participants towards substance misuse changed significantly following specific work around tobacco, however they did not examine tobacco use directly. Bjork et al and Corona et al both noted that participants generally adhered well to the intervention [ 54 , 63 ]. In respect to specific positives of interventions, Björk et al. cite peer support dynamics in their group [ 54 ].
Substance misuse
Outcomes related to alcohol and substance misuse were examined in four studies, as seen in Table 4 [ 65 , 66 , 67 , 68 ]. These all had relatively larger sample sizes (range=70-303) and were RCTs. They all included participants who had diagnosable substance misuse disorders, rather than subclinical problematic substance use, (in contrast to the studies of sleep). Two of the studies examined cognitive behavioural therapy (CBT) paradigms, whilst one study evaluated at motivational interviewing (MI) and behavioural action and one used both CBT/MI. Two studies identified a rationale for their choice of intervention; untreated ADHD symptoms being associated with poorer outcomes in substance use disorder [ 67 , 68 ], and the challenges of people with ADHD within a college environment putting them at greater risk for long-term substance misuse [ 66 ]. All four studies (RCTs) reported significant improvements in measured outcomes with a psychotherapeutic intervention, including Riggs et al. and Thurstone et al. which found that behavioural therapy and medication had comparable effects in the treatment of substance use disorder in patients with ADHD [ 67 , 68 ].
Physical activity/weight
Studies reporting physical activity or weight outcomes were much more heterogenous in their design, including two RCT protocols, two completed RCTs and two single group interventions (Table 5 ). Studies in this category had generally small sample sizes (n<50), except Lindvall et al ( N= 120) [ 71 ] and comprised a younger adult demographic (11-30). Only two studies provided a rationale for intervention explicitly highlighting health in ADHD (both referencing poor health behaviour in ADHD) [ 54 , 71 ]. All involved promoting physical activity, through structured exercise classes, wearable technology/social media and psychoeducation respectively. Furthermore, Schoenfelder et al. report qualitative feedback that the intervention increased awareness of activity levels and ADHD symptoms [ 69 ]. Both RCTs (Silva et al, Converse et al [ 56 , 72 ]) reported improved physical functioning (Converse et al using a questionnaire, Silva et al using objective biometrics), as did both single group intervention studies (Schoenfelder et al finding an increase in step count, Bjork et al in weekly physical activity [ 54 , 69 ]).
Unspecified physical health outcomes
Three studies examined unspecified physical health outcomes related to quality of life and did not fit well into other categories (Table 6 ) [ 73 , 74 , 75 ]. Enggaard et al. reported a study of adolescents with a comorbid physical health disorder, examining guided self-determination as a way of improving their engagement in physical healthcare, given the association of ADHD with physical comorbidity. They found that guided self-determination was effective in improving patients’ self-confidence in managing their conditions, and that adolescents were positively engaged in creating the self-management strategies. The second study examined effects of medication versus cognitive behavioural therapy in 124 young adults on core ADHD symptoms and secondarily recorded improvements in physical health as part of questions on the World Health Organisation (WHO) quality of life scale [ 78 ]. This study [ 74 ] did not identify a rationale for their intervention’s impact physical health. Thirdly, Geissler et al developed a modular treatment programme for adolescents with continual ADHD-related impairment (under routine care). Their rationale was the breadth of functional impairment faced by adolescents with ADHD, and the lack of related interventions. Their developed RCT protocol includes a health-related quality of life questionnaire as a secondary outcome, and their intervention includes a module on substance use [ 75 ].
This scoping review aimed to identify psychosocial interventions that have been designed for physical health problems in ADHD, and which physical health problems they target. We found 22 studies of interventions which measured at least one physical health outcome, with 16 specifically targeting physical health outcomes. In the other studies, measures of physical health (including sleep quality or health-related quality of life measures) were included as secondary outcomes of interventions primarily targeting reduction of core ADHD symptoms [ 55 , 56 , 60 , 61 , 74 , 75 ]. Included studies were grouped under five categories, dependent on the outcomes explored. These were sleep, smoking, substance misuse, physical activity/weight, and general health outcomes, utilising psychoeducational, behavioural and social paradigms (Table 1 ).
The main finding from this scoping review is a relative paucity of research into interventions targeting physical health outcomes in ADHD, and furthermore the lack of larger programmes of research aiming to address the health problems identified. Generally, the included studies lacked detail on the framing and theoretical basis both of individual health problems (who is affected, and how that health problem is quantified) as well as of health problems in ADHD in general (the 'mechanism' of ill health targeted by such interventions). Fortunately, there is some similarity amongst the identified literature explored in respect to the psychosocial interventions used and identified positive aspects of interventions, which may form a basis for the development of a more coherent evidence base in this field.
Framing of health problems
There is substantial heterogeneity in this literature in respect to how health problems were defined and measured, with variable inclusion criteria and outcome measures between studies. For example, when exploring sleep, some studies examined those with formal sleep diagnoses [ 58 ], whilst others specifically excluded those with diagnosed sleep problems [ 59 , 62 ]. In relation to outcome measures, smoking was conceptualised in a different way by each of the studies included (attitudes to tobacco, carbon monoxide levels and self-reported reductions). Some studies used standardised quality of life measures, such as the WHOQL-BREF, SF-36, and KIDSCREEN-10 [ 56 , 74 , 75 ]. However, quality of life measures are of limited utility in assessing physical health outcomes, often being too broad and multi-factorial. We also note a recent scoping review finding that the SF-36 is frequently erroneously reported as a global measure of quality of life, which although Converse and colleagues did not do, highlights a wider problem with the misapplication of quality-of-life measures [ 79 ]. The heterogeneity of included studies’ outcome measures highlights the need for consensus in respect to measures used in assessing the physical health outcomes of populations with ADHD. It was interesting that three of the six studies that did not explicitly target a health problem used sleep outcome measures in behavioural interventions [ 55 , 60 , 61 ], which may highlight the importance of sleep to young people and families, and the impact poor sleep has on symptoms and functioning [ 80 , 81 ].
Such extensive variability in inclusion criteria and outcome measurements limits both the clinical and academic applicability of studies’ findings. This variability is likely to result from the absence of a common framework that mechanistically relates ADHD and physical health outcomes.
Whilst there was some commonality in intervention modalities (e.g., behavioural interventions, educational interventions), authors tended not to explain clearly which mechanism within ADHD their health intervention was targeting, beyond a select few [ 54 , 57 , 58 , 59 , 62 , 64 , 66 , 71 , 73 ]. Challenges surrounding poor conceptual framework of mechanisms of ADHD in relation to health are alluded to in the discussions of some of the included studies [ 54 , 58 , 59 , 64 , 66 , 67 , 73 ]. As mentioned in the introduction, the ‘causal pathway’ of increased health risk in ADHD is likely to be complex and multifactorial, however a sound understanding and explicit logic model is an important basis for the development of preventative interventions in this population. Findings from this scoping review suggest that that clearer framing of the problem is required to properly develop interventions, through better definition of health problems with inputs from existing research and stakeholder perspectives (which may explain the currently disjointed view of this field) [ 82 ].
Positive aspects of interventions
Psychoeducation was common amongst health interventions studied, with 4/22 solely examining a psychoeducational intervention, and Meyer et al comparing a behavioural intervention with psychoeducation as control [ 55 ]. These studies tended to recruit younger participants who were ‘at risk of’ particular health problems, with only Bjork et al using psychoeducation in an adult context. This raises questions about where future research work should focus, primary or secondary prevention in young people and adults with ADHD.
‘Self-efficacy’ or independence over one’s health was also a concept referenced explicitly in the qualitative feedback from participants included in several of the studies we reviewed [ 57 , 73 , 77 ]. Furthermore, all the interventions in included studies all required commitment to interventions and required people to actively engage in their own care, the importance of which has been studied previously in patients with chronic conditions [ 83 , 84 , 85 ]. Self-efficacy is widely cited as being important in ADHD management [ 86 , 87 ]. This is explicitly highlighted by Enggaard et al. , who demonstrated that their guided self-determination intervention promoted efficacy and strategy formation amongst patients with ADHD [ 73 ].
Regular and consistent interventions (regular sessions, commitment to a regimen), were explicitly highlighted in the qualitative participant feedback on several interventions [ 59 , 69 ]. This is particularly pertinent in ADHD, where difficulty with day-to-day structure and organisation is something that people highlight as a contributor to health and social outcome inequalities [ 88 , 89 , 90 ].
Peer dynamics were also referenced by several papers [ 54 , 56 ]. Bjork et al. reported that participants found the peer support dynamic of such interventions useful, whilst Converse et al. reported that participants from an earlier survey used in the development of their intervention would have preferred a mixed ADHD/non-ADHD group [ 91 ]. From a brief review of the literature, the perspectives on peer support in adult ADHD have not yet been formally studied but could be looked at in future work. It should be noted that, in discussions about ADHD in online spaces, community and identity appear to be important themes in living with ADHD [ 87 , 92 ].
If the literature in this field were more coherent, it would make it easier to explore facets of interventions in this field more rigorously, using methods such as intervention component analysis. This would be especially interesting given the findings of Meyer et al, which suggest comparable effects between psychoeducation and behavioural intervention [ 55 ].
Strengths and limitations
This study addresses a novel research question in the literature and our search strategy identified papers in line with research aims. By not defining physical health in our search strategy, we were able to identify a broad range of interventions, targeting for example sleep, smoking, alcohol/substance misuse, physical activity, weight, and physical comorbidity.
Limitations of our scoping review include challenges around defining population age range. Of the 22 studies included, only one study explicitly fell within the 16-25 age range [ 56 ]. Whilst it may have been preferable to strictly apply the lower age limit of 16 years, doing so would have risked losing studies with applicability to our 16-25 age group (e.g., Schoenfelder and colleague’s study of digital health, many of the sleep behavioural interventions) [ 57 , 61 , 69 ]. The same would apply to the upper age limit, where studies such as Björk et al would be excluded if a strict age basis was applied (despite this study having clear relevance to our question) [ 54 ]. Therefore, we adopted a pragmatic approach, informed by consultation with MAP study colleagues and our RAG. We accept that the interventions would likely have different effects than those reported by the studies, if they were to be repeated in a strictly 16-25 age group. This would be an important subject of future work, supported by framework development.
By defining ‘types’ of interventions we were interested in for our search (psychotherapeutic, behavioural, technological, support groups, exercise-based, psychoeducational) we may have inadvertently precluded the inclusion of other interventions in the field. However, to deliver the review with the resources available, and following consultation with our RAG, it was decided to prioritise an open approach to defining physical health problems, which came at the cost of being more restrictive in terms of types of intervention reviewed. As this research area matures, and concepts related to ADHD and physical health become more clearly defined, it will become easier to conduct evidence syntheses of literature on this topic.
Furthermore, it was notable that there were limited interventions surrounding established chronic physical disorders targeted at adults with ADHD, given the known associations of ADHD with chronic health problems [ 12 , 14 , 93 ]. However, this is likely because our search filters examining psychosocial interventions would not have been inclusive of tailored medical interventions (e.g. if a study were examining supporting people with ADHD and diabetes in their medication compliance). A focussed review of chronic disease management in ADHD in adults would be useful in exploring this important area.
This scoping review set out to identify existing psychosocial interventions for physical health in ADHD, with a focus on interventions applicable to a transition care age range (16-25 year olds). Findings demonstrate that whilst such interventions have been developed and reported, the small evidence base surrounding them limits their current application. Future work in this field needs to focus on the development of a conceptual framework for the origins of the physical health challenges and linked health inequalities we see in ADHD. Alongside this, more research is needed into creating standardising how health outcomes are measured and reported in ADHD research in this field, such that evidence can be better synthesised and ultimately realised into clinical applications.
Availability of data and materials
The datasets generated and/or analysed during the current study are available via the MEDLINE ( https://www.nlm.nih.gov/medline/medline_overview.html ), APA PsycInfo ( https://www.apa.org/pubs/databases/psycinfo ) and EMBASE ( https://www.embase.com/ ) databases.
Abbreviations
Attention deficit hyperactivity disorder
Cognitive Behavioural Therapy
Diagnostic and Statistical Manual of Mental Disorders Fifth Edition
Kiddie Schedule for Affective Disorders and Schizophrenia Present and Lifetime
Mapping ADHD services in Primary Care Study
National Institute of Health and Care Excellence
Research Advisory Group
Randomised Control Trial
36-item Short Form Survey
World Health Organisation
World Health Organisation Quality of Life (Brief) Scale
Song P, Zha M, Yang Q, Zhang Y, Li X, Rudan I. The prevalence of adult attention-deficit hyperactivity disorder: A global systematic review and meta-analysis. J Glob Health. 2021;11:1–9.
Article Google Scholar
Salari N, Ghasemi H, Abdoli N, Rahmani A, Shiri MH, Hashemian AH, Akbari H, Mohammadi M. The global prevalence of ADHD in children and adolescents: a systematic review and meta-analysis. Ital J Pediatr. 2023;49:1–12.
Biederman J, Petty CR, Woodworth KY, Lomedico A, Hyder LL, Faraone S, v. Adult Outcome of Attention-Deficit/Hyperactivity Disorder: A Controlled 16-Year Follow-Up Study. J Clin Psychiatry. 2012;73:577.
Arnold LE, Hodgkins P, Kahle J, Madhoo M, Kewley G. Long-Term Outcomes of ADHD: Academic Achievement and Performance. J Atten Disord. 2020;24:73–85.
Article PubMed Google Scholar
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602.
Cherkasova MV, Roy A, Molina BSG, et al. Review: Adult Outcome as Seen Through Controlled Prospective Follow-up Studies of Children With Attention-Deficit/Hyperactivity Disorder Followed Into Adulthood. J Am Acad Child Adolesc Psychiatry. 2022;61:378–91.
Taubin D, Wilson JC, Wilens TE. ADHD and Substance Use Disorders in Young People: Considerations for Evaluation, Diagnosis, and Pharmacotherapy. Child Adolesc Psychiatr Clin N Am. 2022;31:515–30.
Ward JH, Curran S. Self-harm as the first presentation of attention deficit hyperactivity disorder in adolescents. Child Adolesc Ment Health. 2021;26:303–9.
Ricketts EJ, Sturm A, McMakin DL, McGuire JF, Tan PZ, Smalberg FB, McCracken JT, Colwell CS, Piacentini J. Changes in Sleep Problems Across Attention-Deficit/Hyperactivity Disorder Treatment: Findings from the Multimodal Treatment of Attention-Deficit/Hyperactivity Disorder Study. J Child Adolesc Psychopharmacol. 2018;28:690–8.
Article PubMed PubMed Central Google Scholar
Leppert B, Riglin L, Wootton RE, Dardani C, Thapar A, Staley JR, Tilling K, Davey Smith G, Thapar A, Stergiakouli E. The Effect of Attention Deficit/Hyperactivity Disorder on Physical Health Outcomes: A 2-Sample Mendelian Randomization Study. Am J Epidemiol. 2021;190:1047.
Brook JS, Balka EB, Zhang C, Brook DW. Longitudinal Smoking Patterns: Do They Predict Symptoms of ADHD in Adults? J Atten Disord. 2020;24:86–93.
Du Rietz E, Brikell I, Butwicka A, et al. Mapping phenotypic and aetiological associations between ADHD and physical conditions in adulthood in Sweden: a genetically informed register study. Lancet Psychiatry. 2021;8:774–83.
Semeijn EJ, Kooij † J J Sandra, Comijs HC, Michielsen M, Dorly †, Deeg JH, Beekman ATF,. Attention-Deficit/Hyperactivity Disorder. Physical Health, and Lifestyle in Older Adults. 2013. https://doi.org/10.1111/jgs.12261 .
Pan PY, Bölte S (2020) The association between ADHD and physical health: a co-twin control study. Scientific Reports 2020 10:1 10:1–13.
Stickley A, Koyanagi A, Takahashi H, Ruchkin V, Inoue Y, Kamio Y. Attention-deficit/hyperactivity disorder and physical multimorbidity: A population-based study. Eur Psychiatry. 2017;45:227–34.
Article CAS PubMed Google Scholar
London AS, Landes SD. Attention Deficit Hyperactivity Disorder and adult mortality. Prev Med (Baltim). 2016;90:8–10.
Schiavone N, Virta M, Leppämäki S, Launes J, Vanninen R, Tuulio-Henriksson A, Järvinen I, Lehto E, Michelsson K, Hokkanen L. Mortality in individuals with childhood ADHD or subthreshold symptoms – a prospective perinatal risk cohort study over 40 years. BMC Psychiatry. 2022;22:1–10.
Klein RG, Mannuzza S, Ramos Olazagasti MA, Roizen E, Hutchison JA, Lashua EC, Castellanos FX. Clinical and Functional Outcome of Childhood Attention-Deficit/Hyperactivity Disorder 33 Years Later. Arch Gen Psychiatry. 2012;69:1295–303.
Loewen OK, Maximova K, Ekwaru JP, Ohinmaa A, Veugelers PJ. Adherence to Life-Style Recommendations and Attention-Deficit/Hyperactivity Disorder: A Population-Based Study of Children Aged 10 to 11 Years. Psychosom Med. 2020;82:305–15.
Du Rietz E, Barker AR, Michelini G, Rommel A-S, Vainieri I, Asherson P, Kuntsi J. Beneficial effects of acute high-intensity exercise on electrophysiological indices of attention processes in young adult men. Behavioural brain research. 2019;359:474–84.
Kidwell KM, van Dyk TR, Lundahl A, Nelson TD. Stimulant Medications and Sleep for Youth With ADHD: A Meta-analysis. Pediatrics. 2015;136:1144–53.
Zulauf CA, Sprich SE, Safren SA, Wilens TE. The complicated relationship between attention deficit/hyperactivity disorder and substance use disorders. Curr Psychiatry Rep. 2014;16:436.
Singh SP, Tuomainen H. Transition from child to adult mental health services: needs, barriers, experiences and new models of care. World Psychiatry. 2015;14:358.
Schuiteman S, Chua KP, Plegue MA, Ilyas O, Chang T. Self-Management of Health Care Among Youth: Implications for Policies on Transitions of Care. J Adolesc Health. 2020;66:616.
Eke H, Ford T, Newlove-Delgado T, Price A, Young S, Ani C, Sayal K, Lynn RM, Paul M, Janssens A. Transition between child and adult services for young people with attention-deficit hyperactivity disorder (ADHD): findings from a British national surveillance study. The British Journal of Psychiatry. 2020;217:616–22.
Young S, Adamou M, Asherson P, et al. Recommendations for the transition of patients with ADHD from child to adult healthcare services: A consensus statement from the UK adult ADHD network. BMC Psychiatry. 2016;16:1–10.
Rigby E, Hagell A, Davis M, Gleeson H, Mathews G, Turner G. Getting health services right for 16–25 year-olds. Arch Dis Child. 2021;106:9–13.
Waldron HB, Turner CW (2008) Evidence-Based Psychosocial Treatments for Adolescent Substance Abuse. https://doi.org/10.1080/15374410701820133 37:238–261.
Alfonso JP, Caracuel A, Delgado-Pastor LC, Verdejo-García A. Combined Goal Management Training and Mindfulness meditation improve executive functions and decision-making performance in abstinent polysubstance abusers. Drug Alcohol Depend. 2011;117:78–81.
Pagoto SL, Curtin C, Bandini LG, Anderson SE, Schneider KL, Bodenlos JS, Ma Y (2013) Weight loss following a clinic-based weight loss program among adults with attention deficit/hyperactivity disorder symptoms. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity 2010 15:3 15:e166–e172.
Hiscock H, Sciberras E, Mensah F, Gerner B, Efron D, Khano S, Oberklaid F. Impact of a behavioural sleep intervention on symptoms and sleep in children with attention deficit hyperactivity disorder, and parental mental health: randomised controlled trial. BMJ. 2015. https://doi.org/10.1136/BMJ.H68 .
Sciberras E, Fulton M, Efron D, Oberklaid F, Hiscock H. Managing sleep problems in school aged children with ADHD: a pilot randomised controlled trial. Sleep Med. 2011;12:932–5.
Keshavarzi Z, Bajoghli H, Mohamadi MR, Salmanian M, Kirov R, Gerber M, Holsboer-Trachsler E, Brand S. In a randomized case-control trial with 10-years olds suffering from attention deficit/hyperactivity disorder (ADHD) sleep and psychological functioning improved during a 12-week sleep-training program. World Journal of Biological Psychiatry. 2014;15:609–19.
Libutzki B, Ludwig S, May M, Jacobsen RH, Reif A, Hartman CA. Direct medical costs of ADHD and its comorbid conditions on basis of a claims data analysis. European Psychiatry. 2019;58:38–44.
Kittel-Schneider S, Arteaga-Henriquez G, Vasquez AA, et al. Non-mental diseases associated with ADHD across the lifespan: Fidgety Philipp and Pippi Longstocking at risk of multimorbidity? Neurosci Biobehav Rev. 2022;132:1157–80.
Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2005;90:i2–7.
Harpin V, Mazzone L, Raynaud JP, Kahle J, Hodgkins P. Long-Term Outcomes of ADHD: A Systematic Review of Self-Esteem and Social Function. J Atten Disord. 2016;20:295–305.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:1–7.
Peterson J, Pearce PF, Ferguson LA, Langford CA. Understanding scoping reviews: Definition, purpose, and process. J Am Assoc Nurse Pract. 2017;29:12–6.
Arksey H, O’Malley L (2007) Scoping studies: towards a methodological framework. https://doi.org/10.1080/1364557032000119616 8:19–32.
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–73.
PRISMA. http://www.prisma-statement.org/Extensions/ScopingReviews . Accessed 3 Nov 2023.
Mitchell DL, Shlobin NA, Winterhalter E, Lam SK, Raskin JS. Gaps in transitional care to adulthood for patients with cerebral palsy: a systematic review. Child’s Nervous System. 2023;39:3083–101.
Nesbitt AE, Sabiston CM, deJonge ML, Barbic SP, Kozloff N, Nalder EJ (2023) A scoping review of resilience among transition-age youth with serious mental illness: tensions, knowledge gaps, and future directions. BMC Psychiatry 2023 23:1 23:1–27.
McCrory A, Best P, Maddock A. The relationship between highly visual social media and young people’s mental health: A scoping review. Child Youth Serv Rev. 2020;115: 105053.
(2018) School-based interventions. The Association for Child and Adolescent Mental Health. https://doi.org/10.13056/ACAMH.1088 .
Guan Lim C, Lim-Ashworth NSJ, Fung DSS. Updates in technology-based interventions for attention deficit hyperactivity disorder. Curr Opin Psychiatry. 2020;33:577.
Lakes KD, Cibrian FL, Schuck SEB, Nelson M, Hayes GR. Digital health interventions for youth with ADHD: A mapping review. Computers in Human Behavior Reports. 2022;6: 100174.
Ruddy R, House A. Psychosocial interventions for conversion disorder. Cochrane Database of Systematic Reviews. 2005. https://doi.org/10.1002/14651858.CD005331.PUB2/MEDIA/CDSR/CD005331/REL0002/CD005331/IMAGE_N/NCD005331-CMP-003-05.PNG .
Price A, Smith JR, Mughal F, Salimi A, Melendez-Torres GJ, Newlove-Delgado T. Protocol for the mixed methods, Managing young people (aged 16–25) with Attention deficit hyperactivity disorder in Primary care (MAP) study: mapping current practice and co-producing guidance to improve healthcare in an underserved population. BMJ Open. 2023;13: e068184.
National Institute for Care and Health Excellence (2021) Search strategy | How this topic was developed | Attention deficit hyperactivity disorder | CKS | NICE. https://cks.nice.org.uk/topics/attention-deficit-hyperactivity-disorder/how-this-topic-was-developed/search-strategy/ . Accessed 30 Sep 2022.
National Institute for Health and Care Excellence (2022) Search strategy | How this topic was developed | Back pain - low (without radiculopathy) | CKS | NICE. In: National Institute for Health and Care Excellence. https://cks.nice.org.uk/topics/back-pain-low-without-radiculopathy/how-this-topic-was-developed/search-strategy/ . Accessed 30 Sep 2022.
National Institute for Health and Care Excellence (2017) Type 2 diabetes: prevention in people at high risk [A] Evidence reviews for interventions for people at high risk of type 2 diabetes.
Björk A, Rönngren Y, Wall E, Vinberg S, Hellzen O, Olofsson N (2020) A nurse-led lifestyle intervention for adult persons with attention-deficit/hyperactivity disorder (ADHD) in Sweden. https://doi.org/10.1080/0803948820201771768 74:602–612.
Meyer J, Ramklint M, Hallerbäck MU, Lööf M, Isaksson J. Evaluation of a structured skills training group for adolescents with attention-deficit/hyperactivity disorder: a randomised controlled trial. Eur Child Adolesc Psychiatry. 2022;31:1–13.
Converse AK, Barrett BP, Chewning BA, Wayne PM. Tai Chi training for attention deficit hyperactivity disorder: A feasibility trial in college students. Complement Ther Med. 2020;53: 102538.
Becker SP, Duraccio KM, Sidol CA, Fershtman CEM, Byars KC, Harvey AG. Impact of a Behavioral Sleep Intervention in Adolescents With ADHD: Feasibility, Acceptability, and Preliminary Effectiveness From a Pilot Open Trial. J Atten Disord. 2022;26:1051–66.
van Andel E, Bijlenga D, Vogel SWN, Beekman ATF, Kooij JJS. Attention-Deficit/Hyperactivity Disorder and Delayed Sleep Phase Syndrome in Adults: A Randomized Clinical Trial on the Effects of Chronotherapy on Sleep. J Biol Rhythms. 2022;37:673–89.
Jernelov S, Larsson Y, Llenas M, Nasri B, Kaldo V. Effects and clinical feasibility of a behavioral treatment for sleep problems in adult attention deficit hyperactivity disorder (ADHD): a pragmatic within-group pilot evaluation. BMC Psychiatry. 2019;19:226.
Morgensterns E, Alfredsson J, Hirvikoski T. Structured skills training for adults with ADHD in an outpatient psychiatric context: an open feasibility trial. Atten Defic Hyperact Disord. 2016;8:101–11.
Nøvik TS, Haugan ALJ, Lydersen S, Thomsen PH, Young S, Sund AM. Cognitive-behavioural group therapy for adolescents with ADHD: study protocol for a randomised controlled trial. BMJ Open. 2020;10: e032839.
Keuppens L, Marten F, Baeyens D, Boyer B, Danckaerts M, Van Der Oord S. Protocol: Sleep IntervEntion as Symptom Treatment for ADHD (SIESTA)-Blended CBT sleep intervention to improve sleep, ADHD symptoms and related problems in adolescents with ADHD: Protocol for a randomised controlled trial. BMJ Open. 2023;13:65355.
Corona R, Dvorsky MR, Romo S, Parks AM, Bourchtein E, Smith ZR, Avila M, Langberg J. Integrating Tobacco Prevention Skills into an Evidence-Based Intervention for Adolescents with ADHD: Results from a Pilot Efficacy Randomized Controlled Trial. J Abnorm Child Psychol. 2020;48:1439–53.
Kollins SH, McClernon FJ, Van Voorhees EE. Monetary Incentives Promote Smoking Abstinence in Adults With Attention Deficit Hyperactivity Disorder (ADHD). Exp Clin Psychopharmacol. 2010;18:221.
van Emmerik-van Oortmerssen K, Vedel E, Kramer FJ, Blankers M, Dekker JJM, van den Brink W, Schoevers RA. Integrated cognitive behavioral therapy for ADHD in adult substance use disorder patients: Results of a randomized clinical trial. Drug Alcohol Depend. 2019;197:28–36.
Meinzer MC, Oddo LE, Vasko JM, Murphy JG, Iwamoto D, Lejuez CW, Chronis-Tuscano A. Motivational interviewing plus behavioral activation for alcohol misuse in college students with ADHD. Psychol Addict Behav. 2021;35:803–16.
Riggs PD, Winhusen T, Davies RD, et al. Randomized controlled trial of osmotic-release methylphenidate with cognitive-behavioral therapy in adolescents with attention-deficit/hyperactivity disorder and substance use disorders. J Am Acad Child Adolesc Psychiatry. 2011;50:903–14.
Thurstone C, Riggs PD, Salomonsen-Sautel S, Mikulich-Gilbertson SK. Randomized, controlled trial of atomoxetine for attention-deficit/hyperactivity disorder in adolescents with substance use disorder. J Am Acad Child Adolesc Psychiatry. 2010;49:573–82.
PubMed PubMed Central Google Scholar
Schoenfelder E, Moreno M, Wilner M, Whitlock KB, Mendoza JA. Piloting a mobile health intervention to increase physical activity for adolescents with ADHD. Prev Med Rep. 2017;6:210–3.
Mayer JS, Hees K, Medda J, et al. Bright light therapy versus physical exercise to prevent co-morbid depression and obesity in adolescents and young adults with attention-deficit / hyperactivity disorder: study protocol for a randomized controlled trial. Trials. 2018;19:140.
Lindvall MA, Holmqvist KL, Svedell LA, Philipson A, Cao Y, Msghina M. START – physical exercise and person-centred cognitive skills training as treatment for adult ADHD: protocol for a randomized controlled trial. BMC Psychiatry. 2023;23:1–14.
Da Silva LA, Doyenart R, Henrique Salvan P, Rodrigues W, Felipe Lopes J, Gomes K, Thirupathi A, De Pinho RA, Silveira PC. Swimming training improves mental health parameters, cognition and motor coordination in children with Attention Deficit Hyperactivity Disorder. Int J Environ Health Res. 2020;30:584–92.
Enggaard H, Laugesen B, DeJonckheere M, Fetters MD, Dalgaard MK, Lauritsen MB, Zoffmann V, Jørgensen R. Impact of the Guided Self-Determination Intervention among Adolescents with Co-Existing ADHD and Medical Disorder: A Mixed Methods Study. Issues Ment Health Nurs. 2021;42:1–12.
Mei-Rong P, Huang F, Zhao M-J, Wang Y-F, Wang Y-F, Qian Q-J. A comparison of efficacy between cognitive behavioral therapy (CBT) and CBT combined with medication in adults with attention-deficit/hyperactivity disorder (ADHD). Psychiatry Res. 2019;279:23–33.
Geissler J, Jans T, Banaschewski T, et al. Individualised short-term therapy for adolescents impaired by attention-deficit/hyperactivity disorder despite previous routine care treatment (ESCAadol)-Study protocol of a randomised controlled trial within the consortium ESCAlife. Trials. 2018. https://doi.org/10.1186/S13063-018-2635-2 .
van Emmerik-van Oortmerssen K, Blankers M, Vedel E, Kramer F, Goudriaan AE, van den Brink W, Schoevers RA. Prediction of drop-out and outcome in integrated cognitive behavioral therapy for ADHD and SUD: Results from a randomized clinical trial. Addictive Behaviors. 2020. https://doi.org/10.1016/j.addbeh.2019.106228 .
Keuppens L, Marten F, Baeyens D, Boyer BE, Danckaerts M, van der Oord S. A Pilot Study of a Cognitive-Behavioral Sleep Intervention Specifically for Adolescents With ADHD and Sleep Problems: A Qualitative and Quantitative Evaluation. Cogn Behav Pract. 2024;31:367–82.
Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310.
Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016. https://doi.org/10.1177/2050312116671725 .
Arias-Mera C, Paillama-Raimán D, Lucero-González N, Leiva-Bianchi M, Avello-Sáez D. Relation between sleep disorders and attention deficit disorder with hyperactivity in children and adolescents: A systematic review. Res Dev Disabil. 2023. https://doi.org/10.1016/J.RIDD.2023.104500 .
Hvolby A. Associations of sleep disturbance with ADHD: implications for treatment. Atten Defic Hyperact Disord. 2015;7:1–18.
O’Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, Yardley L, Hoddinott P. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019. https://doi.org/10.1136/BMJOPEN-2019-029954 .
Rees S, Williams A. Promoting and supporting self-management for adults living in the community with physical chronic illness: A systematic review of the effectiveness and meaningfulness of the patient-practitioner encounter. JBI Libr Syst Rev. 2009;7:492–582.
PubMed Google Scholar
Aboumatar H, Pitts S, Sharma R, Das A, Smith BM, Day J, Holzhauer K, Yang S, Bass EB, Bennett WL. Patient engagement strategies for adults with chronic conditions: an evidence map. Syst Rev. 2022. https://doi.org/10.1186/S13643-021-01873-5 .
Smith BM, Sharma R, Das A, Aboumatar H, Pitts SI, Day J, Holzhauer K, Bass E, Bennett WL. Patient and family engagement strategies for children and adolescents with chronic diseases: A review of systematic reviews. Patient Educ Couns. 2021;104:2213–23.
Wenderlich AM, Baldwin CD, Fagnano M, Jones M, Halterman J. Responsibility for Asthma Management among Adolescents with and without ADHD. J Adolesc Health. 2019;65:812.
Gajaria A, Yeung E, Goodale T, Charach A. Beliefs about attention-deficit/hyperactivity disorder and response to stereotypes: youth postings in Facebook groups. J Adolesc Health. 2011;49:15–20.
Knox E, Muros JJ. Association of lifestyle behaviours with self-esteem through health-related quality of life in Spanish adolescents. Eur J Pediatr. 2017;176:621.
Schrevel SJC, Dedding C, van Aken JA, Broerse JEW. ‘Do I need to become someone else?’ A qualitative exploratory study into the experiences and needs of adults with ADHD. Health Expectations. 2016;19:39–48.
Ginapp CM, Macdonald-Gagnon G, Angarita GA, Bold KW, Potenza MN. The lived experiences of adults with attention-deficit/hyperactivity disorder: A rapid review of qualitative evidence. Front Psychiatry. 2022;13:1853.
Sulzer SH, Trueba C, Converse AK. The appeal of tai chi and complementary therapies for college students with ADHD. J Am Coll Health. 2023. https://doi.org/10.1080/07448481.2021.1990071 .
Yeung A, Ng E, Abi-Jaoude E. TikTok and Attention-Deficit/Hyperactivity Disorder: A Cross-Sectional Study of Social Media Content Quality. Can J Psychiatry. 2022;67:899–906.
Landes SD, London AS (2018) Self-Reported ADHD and Adult Health in the United States. 25:3–13. https://doi.org/10.1177/1087054718757648 .
Download references
Acknowledgements
we would like to express our thanks to our public patient involvement group and research advisory group, who facilitated our approach to this important research topic. We would also like to thank Reviewer 2, whose detailed and thoughtful comments have greatly strengthened the content and form of this manuscript.
AP is funded by a National Institute for Health and Care Research (NIHR) Three Research Schools’ Mental Health Research Fellowship (located within the Exeter NIHR School for Primary Care Research (SPCR); Grant Reference Number MHF008). Tamsin Newlove-Delgado was funded by a NIHR Advanced Fellowship (NIHR300056) whilst undertaking this work. The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS or the UK Department of Health and Social Care.
JW is supported by the NIHR Oxford Health Biomedical Research Centre (BRC)
Author information
Authors and affiliations.
2.05 South Cloisters, 2.05 South Cloisters, St Luke’s Campus, University of Exeter Medical School, Heavitree Road, Exeter, EX2 4TH, UK
John Headley Ward, Audrey McBride, Anna Price & Tamsin Newlove Delgado
Royal Devon University NHS Foundation Trust, Exeter, UK
John Headley Ward
Department of Psychiatry, University of Oxford, Oxford, UK
Oxford Health NHS Foundation Trust, Oxford, UK
You can also search for this author in PubMed Google Scholar
Contributions
JW was responsible for hypothesis generation, design of literature search, title/abstract screening, data extraction, analysis and manuscript preparation. AM was responsible for data extraction and manuscript preparation. AP was responsible for design of literature search and manuscript preparation, as well as project oversight. TND was responsible for title/abstract screening and manuscript preparation, as well as project oversight.
Corresponding author
Correspondence to John Headley Ward .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1, supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ward, J.H., McBride, A., Price, A. et al. Psychosocial interventions for improving the physical health of young people and adults with attention deficit hyperactivity disorder: a scoping review. BMC Psychiatry 24 , 569 (2024). https://doi.org/10.1186/s12888-024-06009-2
Download citation
Received : 12 September 2023
Accepted : 08 August 2024
Published : 20 August 2024
DOI : https://doi.org/10.1186/s12888-024-06009-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preventative medicine
- Psychosocial intervention
BMC Psychiatry
ISSN: 1471-244X
- General enquiries: [email protected]

IMAGES
COMMENTS
Peer review, sometimes referred to as refereeing, is the process of evaluating submissions to an academic journal. Using strict criteria, a panel of
The peer review process is essential for evaluating the quality of scholarly works, suggesting corrections, and learning from other authors' mistakes. The principles of peer review are largely based on professionalism, eloquence, and collegiate attitude. As such, reviewing journal submissions is a privilege and responsibility for 'elite ...
Peer review is designed to assess the validity, quality and often the originality of articles for publication. Its ultimate purpose is to maintain the integrity of science by filtering out invalid or poor quality articles. From a publisher's perspective, peer review functions as a filter for content, directing better quality articles to ...
Peer review is an essential element of the scientific publishing process that helps ensure that research articles are evaluated, critiqued, and improved before release into the academic community. Take a look at the significance of peer review in scientific publications, the typical steps of the process, and and how to approach peer review if you are asked to assess a manuscript.
Peer review is a mutual responsibility among fellow scientists, and scientists are expected, as part of the academic community, to take part in peer review. If one is to expect others to review their work, they should commit to reviewing the work of others as well, and put effort into it. 2) Be pleasant. If the paper is of low quality, suggest ...
It is also safe to say that peer review is a critical element of the scholarly publication process and one of the major cornerstones of the academic process. It acts as a filter, ensuring that research is properly verified before being published. And it arguably improves the quality of the research, as the rigorous review by like-minded experts ...
Peer review. A key convention in the publication of research is the peer review process, in which the quality and potential contribution of each manuscript is evaluated by one's peers in the scientific community. Like other scientific journals, APA journals utilize a peer review process to guide manuscript selection and publication decisions.
This article, based on that session, presents an overview of the processes and practices — good, bad, and terrible — in peer review for academic journals. Peer review of research grant proposals was beyond the scope of this presentation and is not discussed.
Peer review, sometimes referred to as refereeing, is the process of evaluating submissions to an academic journal. Using strict criteria, a panel of reviewers in the same subject area decides whether to accept each submission for publication.
What is Peer Review? The peer-review process tries to ensure that the highest quality research gets published. When an article is submitted to a peer-reviewed journal, the editor after deciding if the article meets the basic requirements for inclusion, sends it to be reviewed by other scholars (the author's peers) within the same field.
Scholarly journals, often called scientific or peer-reviewed journals, are good sources of actual studies or research conducted about a particular topic. They go through a process of review by experts, so the information is usually highly reliable.
Peer review is the independent assessment of your research paper by experts in your field. The purpose of peer review is to evaluate the paper's quality and suitability for publication. As well as peer review acting as a form of quality control for academic journals, it is a very useful source of feedback for you.
Reviewers play a pivotal role in scholarly publishing. The peer review system exists to validate academic work, helps to improve the quality of published research, and increases networking possibilities within research communities. Despite criticisms, peer review is still the only widely accepted method for research validation and has continued ...
PLOS ONE. part of the review process public. We've all heard the phrase "peer review" as giving credence to research and scholarly papers, but what does it actually mean? How does it work?
Positive peer reviews contribute to increased funding opportunities, academic advancement and a good reputation. Learn how to review, get mentored, and get published.
The review of research articles by peer experts prior to their publication is considered a mainstay of publishing in the medical literature. [ 1, 2] This peer review process serves at least two purposes. For journal editors, peer review is an important tool for evaluating manuscripts submitted for publication.
The peer review process. The peer review process can be broadly summarized into 10 steps, although these steps can vary slightly between journals. Explore what's involved, below. Editor Feedback: "Reviewers should remember that they are representing the readers of the journal. Will the readers of this particular journal find this ...
The peer review process can be single-blind, double-blind, open or transparent. You can find out which peer review system is used by a particular journal in the journal's 'About' page. N. B. This diagram is a representation of the peer review process, and should not be taken as the definitive approach used by every journal. Advertisement.
Peer review cannot improve poor research, but it can often "correct, enhance and strengthen the statistical analysis of data and can markedly improve presentation and clarity" [ 4 ]. Why should you volunteer to be a referee and review papers? The noblest motive is altruism, to help others to improve their papers.
The peer-review process is used to assess scholarly articles. Experts in a discipline similar to the author critique an article's methodology, findings, and reasoning to evaluate it for possible publication in a scholarly journal. Editors of scholarly journals use the peer-review process to decide which articles to publish, and the academic ...
How to Write a Peer Review When you write a peer review for a manuscript, what should you include in your comments? What should you leave out? And how should the review be formatted? This guide provides quick tips for writing and organizing your reviewer report.
Peer review is the first stage of a discussion among scientists as to whether the methods of the study support the conclusions made. Critical evaluation of the paper by external peers helps add clarity and acknowledge and report uncertainties and limitations, place new work in the context of the totality of available evidence and prevent over ...
Scientific peer review has existed for centuries and is a cornerstone of the scientific publication process. Because the number of scientific publications has rapidly increased over the past decades, so has the number of peer reviews and peer reviewers. In this paper, drawing on the relevant medical literature and our collective experience as peer reviewers, we provide a user guide to the peer ...
Of the potential engagement mechanisms, the review highlights the important role played by research networks. The review also identifies various papers which consider how far there is a "dose effect" from differing amounts of research engagement. Additional lessons come from analyses of equity issues and negative papers.
The participants consisted of 1st through 5th-year medical students, with a sample size of 336. The research team collected study data using an electronic questionnaire containing three sections: socio-demographic data, personal characteristics, and study habits. ... Peer Review reports. Introduction. Academic performance is a common indicator ...
The main finding from this scoping review is a relative paucity of research into interventions targeting physical health outcomes in ADHD, and furthermore the lack of larger programmes of research aiming to address the health problems identified. ... Peer dynamics were also referenced by several papers ... This study addresses a novel research ...