An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Mental Health Evaluation for Gender Confirmation Surgery
Affiliation.
- 1 New Health Foundation Worldwide, 1214 Lake Street, Evanston, IL 60201, USA. Electronic address: [email protected].
- PMID: 29908617
- DOI: 10.1016/j.cps.2018.03.002
The requests for medically necessary surgical interventions for transgender individuals have steadily increased over the past several years. So too has the recognition of the diverse nature of this population. The surgeon relies heavily on the mental health provider to assess the readiness and eligibility of the patient to undergo surgery, which the mental health provider documents in a referral letter to the surgeon. The mental health provider explores the individual's preparedness for surgery, expectations, and surgical goals and communicates with the surgeon and other providers to promote positive outcomes and inform multidisciplinary care.
Keywords: Gender; Gender dysphoria; Gender-affirming; Mental health; Surgery.
Copyright © 2018 Elsevier Inc. All rights reserved.
PubMed Disclaimer
Similar articles
- Hormonal and Surgical Treatment Options for Transgender Women and Transfeminine Spectrum Persons. Wesp LM, Deutsch MB. Wesp LM, et al. Psychiatr Clin North Am. 2017 Mar;40(1):99-111. doi: 10.1016/j.psc.2016.10.006. Epub 2016 Dec 22. Psychiatr Clin North Am. 2017. PMID: 28159148 Review.
- Healthcare costs and quality of life outcomes following gender affirming surgery in trans men: a review. Defreyne J, Motmans J, T'sjoen G. Defreyne J, et al. Expert Rev Pharmacoecon Outcomes Res. 2017 Dec;17(6):543-556. doi: 10.1080/14737167.2017.1388164. Epub 2017 Oct 9. Expert Rev Pharmacoecon Outcomes Res. 2017. PMID: 28972413 Review.
- Hormonal and Surgical Treatment Options for Transgender Men (Female-to-Male). Gorton RN, Erickson-Schroth L. Gorton RN, et al. Psychiatr Clin North Am. 2017 Mar;40(1):79-97. doi: 10.1016/j.psc.2016.10.005. Epub 2016 Dec 12. Psychiatr Clin North Am. 2017. PMID: 28159147 Review.
- Gender-affirming hormones and surgery in transgender children and adolescents. Mahfouda S, Moore JK, Siafarikas A, Hewitt T, Ganti U, Lin A, Zepf FD. Mahfouda S, et al. Lancet Diabetes Endocrinol. 2019 Jun;7(6):484-498. doi: 10.1016/S2213-8587(18)30305-X. Epub 2018 Dec 6. Lancet Diabetes Endocrinol. 2019. PMID: 30528161 Review.
- WHOQOL-100 Before and After Sex Reassignment Surgery in Brazilian Male-to-Female Transsexual Individuals. Cardoso da Silva D, Schwarz K, Fontanari AM, Costa AB, Massuda R, Henriques AA, Salvador J, Silveira E, Elias Rosito T, Lobato MI. Cardoso da Silva D, et al. J Sex Med. 2016 Jun;13(6):988-93. doi: 10.1016/j.jsxm.2016.03.370. Epub 2016 Apr 21. J Sex Med. 2016. PMID: 27117529
- Qualitative Assessment of the Experiences of Transgender Individuals Assigned Female at Birth Undergoing Gender-Affirming Mastectomy for the Treatment of Gender Dysphoria. Christiano JG, Punekar I, Patel A, McGregor HA, Moskow M, Anson E. Christiano JG, et al. Transgend Health. 2024 Apr 3;9(2):143-150. doi: 10.1089/trgh.2022.0056. eCollection 2024 Apr. Transgend Health. 2024. PMID: 38585246
- Readiness assessments for gender-affirming surgical treatments: A systematic scoping review of historical practices and changing ethical considerations. Amengual T, Kunstman K, Lloyd RB, Janssen A, Wescott AB. Amengual T, et al. Front Psychiatry. 2022 Oct 20;13:1006024. doi: 10.3389/fpsyt.2022.1006024. eCollection 2022. Front Psychiatry. 2022. PMID: 36339880 Free PMC article.
- Correlations between healthcare provider interactions and mental health among transgender and nonbinary adults. Kattari SK, Bakko M, Hecht HK, Kattari L. Kattari SK, et al. SSM Popul Health. 2019 Nov 29;10:100525. doi: 10.1016/j.ssmph.2019.100525. eCollection 2020 Apr. SSM Popul Health. 2019. PMID: 31872041 Free PMC article.
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- ClinicalKey
- Elsevier Science
- W.B. Saunders
Other Literature Sources
- scite Smart Citations
- MedlinePlus Health Information
Miscellaneous
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Masks Strongly Recommended but Not Required in Maryland
Respiratory viruses continue to circulate in Maryland, so masking remains strongly recommended when you visit Johns Hopkins Medicine clinical locations in Maryland. To protect your loved one, please do not visit if you are sick or have a COVID-19 positive test result. Get more resources on masking and COVID-19 precautions .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Preparing for Gender Affirmation Surgery: Ask the Experts
Preparing for your gender affirmation surgery can be daunting. To help provide some guidance for those considering gender affirmation procedures, our team from the Johns Hopkins Center for Transgender and Gender Expansive Health (JHCTGEH) answered some questions about what to expect before and after your surgery.
What kind of care should I expect as a transgender individual?
What kind of care should I expect as a transgender individual? Before beginning the process, we recommend reading the World Professional Association for Transgender Health Standards Of Care (SOC). The standards were created by international agreement among health care clinicians and in collaboration with the transgender community. These SOC integrate the latest scientific research on transgender health, as well as the lived experience of the transgender community members. This collaboration is crucial so that doctors can best meet the unique health care needs of transgender and gender-diverse people. It is usually a favorable sign if the hospital you choose for your gender affirmation surgery follows or references these standards in their transgender care practices.
Can I still have children after gender affirmation surgery?
Many transgender individuals choose to undergo fertility preservation before their gender affirmation surgery if having biological children is part of their long-term goals. Discuss all your options, such as sperm banking and egg freezing, with your doctor so that you can create the best plan for future family building. JHCTGEH has fertility specialists on staff to meet with you and develop a plan that meets your goals.
Are there other ways I need to prepare?
It is very important to prepare mentally for your surgery. If you haven’t already done so, talk to people who have undergone gender affirmation surgeries or read first-hand accounts. These conversations and articles may be helpful; however, keep in mind that not everything you read will apply to your situation. If you have questions about whether something applies to your individual care, it is always best to talk to your doctor.
You will also want to think about your recovery plan post-surgery. Do you have friends or family who can help care for you in the days after your surgery? Having a support system is vital to your continued health both right after surgery and long term. Most centers have specific discharge instructions that you will receive after surgery. Ask if you can receive a copy of these instructions in advance so you can familiarize yourself with the information.
An initial intake interview via phone with a clinical specialist.
This is your first point of contact with the clinical team, where you will review your medical history, discuss which procedures you’d like to learn more about, clarify what is required by your insurance company for surgery, and develop a plan for next steps. It will make your phone call more productive if you have these documents ready to discuss with the clinician:
- Medications. Information about which prescriptions and over-the-counter medications you are currently taking.
- Insurance. Call your insurance company and find out if your surgery is a “covered benefit" and what their requirements are for you to have surgery.
- Medical Documents. Have at hand the name, address, and contact information for any clinician you see on a regular basis. This includes your primary care clinician, therapists or psychiatrists, and other health specialist you interact with such as a cardiologist or neurologist.
After the intake interview you will need to submit the following documents:
- Pharmacy records and medical records documenting your hormone therapy, if applicable
- Medical records from your primary physician.
- Surgical readiness referral letters from mental health providers documenting their assessment and evaluation
An appointment with your surgeon.
After your intake, and once you have all of your required documentation submitted you will be scheduled for a surgical consultation. These are in-person visits where you will get to meet the surgeon. typically include: The specialty nurse and social worker will meet with you first to conduct an assessment of your medical health status and readiness for major surgical procedures. Discussion of your long-term gender affirmation goals and assessment of which procedures may be most appropriate to help you in your journey. Specific details about the procedures you and your surgeon identify, including the risks, benefits and what to expect after surgery.
A preoperative anesthesia and medical evaluation.
Two to four weeks before your surgery, you may be asked to complete these evaluations at the hospital, which ensure that you are healthy enough for surgery.
What can I expect after gender affirming surgery?
When you’ve finished the surgical aspects of your gender affirmation, we encourage you to follow up with your primary care physician to make sure that they have the latest information about your health. Your doctor can create a custom plan for long-term care that best fits your needs. Depending on your specific surgery and which organs you continue to have, you may need to follow up with a urologist or gynecologist for routine cancer screening. JHCTGEH has primary care clinicians as well as an OB/GYN and urologists on staff.
Among other changes, you may consider updating your name and identification. This list of resources for transgender and gender diverse individuals can help you in this process.
The Center for Transgender and Gender Expansive Health Team at Johns Hopkins
Embracing diversity and inclusion, the Center for Transgender and Gender Expansive Health provides affirming, objective, person-centered care to improve health and enhance wellness; educates interdisciplinary health care professionals to provide culturally competent, evidence-based care; informs the public on transgender health issues; and advances medical knowledge by conducting biomedical research.
Find a Doctor
Specializing In:
- Gender Affirmation Surgery
- Transgender Health
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
Find Additional Treatment Centers at:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital

Request an Appointment

Gender Affirmation Surgeries

Facial Masculinization Surgery

Facial Feminization Surgery (FFS)
Related Topics
- LGBTQ Health
- Gender Affirmation
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
Our systems are now restored following recent technical disruption, and we’re working hard to catch up on publishing. We apologise for the inconvenience caused. Find out more: https://www.cambridge.org/universitypress/about-us/news-and-blogs/cambridge-university-press-publishing-update-following-technical-disruption
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert
- > Journals
- > European Psychiatry
- > Volume 30 Issue S1: Abstracts of the 23rd European...
- > Psychiatric Assessment of Transgender Adults for Sex...

Article contents
Psychiatric assessment of transgender adults for sex reassignment surgery.
Published online by Cambridge University Press: 15 April 2020
While pre-surgical assessments by an internist are relatively common, those by psychiatrists are much more rare. With the exception of bariatric surgery and live donor organ transplantation, sex reassignment surgery (SRS) is the only category of surgeries for which a mental health assessment is routinely done as part of the standard of care. This presentation will outline the assessment process as performed at the Gender Identity Clinic at the Centre for Addiction and Mental Health in Toronto, Canada, which sees and approves individuals in the Canadian province of Ontario seeking to have sex reassignment surgery through the provincial health care insurance plan.
There are three main tasks of the assessment, diagnosis / differential diagnosis, eligibility assessment, and readiness assessment. Diagnosis, while controversial among some in the transgender community, is generally required by most medical professionals and insurance plans that might cover surgical transition procedures. In Ontario diagnosis is a regulated professional activity and can only be done formally by physicians and clinical psychologists.
Eligibility relates to certain specific requirements broadly applied to those seeking surgery that are outlined in international standards of care. For genital surgery, this includes one year of living a full time, continuous gender role experience (GRE) in the chosen gender role.
Readiness is the part of the assessment that most resembles a general psychiatric assessment, in which a full biopsychosocial formulation of the client's current status leads to recommendations for improving readiness for SRS.

This article has been cited by the following publications. This list is generated based on data provided by Crossref .
- Google Scholar
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Volume 30, Issue S1
- C. McIntosh (a1)
- DOI: https://doi.org/10.1016/S0924-9338(15)30128-0
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.

Gender Affirmative Surgery Psychological Evaluations
If you or a loved one are in the process of transitioning or are looking to have a gender affirmative surgery, we want to help .
Deep Eddy Psychotherapy offers psychological evaluations for gender affirmative surgery candidacy for our clients (ages 18 and up). Our clinicians are dedicated to helping the transgender, non-binary, genderqueer, and gender-expansive community by providing this evaluation service along with individual, group, and couples therapy .

We also recognize that transphobia and transmisogyny are interwoven into our society and that the mental health profession has had an unfortunate history of perpetuating these ideas. Our therapists are committed to being part of the change for good and live more fully within our values – you deserve nothing less.
Ready to sign up to get an evaluation? Don’t wait – contact us today. Please read on to learn more about gender affirmative surgery evaluations and answers to common questions.
What is a gender affirmative surgery evaluation?
Under the current guidelines, transgender, non-binary, and gender non-conforming clients seeking gender affirmative surgeries must have letters from mental health providers attesting to whether they meet the guidelines for surgical intervention established by the World Professional Association for Transgender Health (WPATH).
Anyone who is seeking an attestation letter must meet with a mental health provider for an evaluation (typically just an interview, but occasionally more than one session) to determine whether they are good candidates for surgery. Based on the results of the evaluation, the provider will write a letter summarizing your candidacy and their recommendations.
Do you need an evaluation for hormone replacement treatment (HRT)?
No. In Texas (and in most other states), we now use an informed consent model in place for HRT. So, you no longer need letters from mental health providers in order to receive HRT.
What does a gender affirmative surgery evaluation assess for?
At Deep Eddy Psychotherapy, our clinicians recognize the inherent gatekeeping role that mental health providers have in this compulsory letter-writing process, and we seek to reduce any undue gatekeeping while also having to work within the structure of the WPATH Standards of Care.
Our clinicians who provide this service have a welcoming and affirmative stance toward gender-diverse clients and want to help clients receive the gender-affirming medical care they seek. We have training and experience in this area, and we actively consult with each other about the process.
We say all of this so that you can rest easier knowing that our process is designed with your rights in mind. Our goal is not to keep you from getting the surgery you need, but rather to ensure that you are the right fit and have the support you need to succeed.
Some of the things your evaluator might ask about might include:
- Your gender story
- Past and current emotional wellbeing
- Social supports you can lean on
- What sorts of surgical interventions you are seeking
- Your understanding of the risks and benefits of surgery
Our providers understand that there is no one gender story narrative. Your story is unique and does not have to be tied together with a sense of certainty. Likewise, our providers understand that your past and current emotional wellbeing could be impacted by both gender dysphoria and the effects of living in a cisnormative society, and we want to give you the support you deserve.
In addition to us asking you questions, we also welcome questions from the interviewee. We recognize how hard it is to get to this point, and we want to be here for you however we can.
Who can write an attestation letter?
In Texas, some insurance companies require all letters to be written by doctoral level (PhD or PsyD) clinicians. Some insurance companies and surgery centers allow master’s level clinicians (LMFT, LCSW, LPC) to provide letters, but not all will. To make matters a bit more complicated, some insurances and some procedures may require multiple letters from different providers.
Before scheduling a session, it can be helpful to talk with your insurance company and/or surgery center about what they each require in the letter and who can write the letters.
If you do not have insurance, as advocates for equity and social justice, we do not want the ability to pay to keep you from receiving a letter from a mental health professional. Please feel free to reach out to us if you have financial need, and we can let you know which clinicians have sliding scale spots open for this service at the time.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 12 April 2011
Gender reassignment surgery: an overview
- Gennaro Selvaggi 1 &
- James Bellringer 1
Nature Reviews Urology volume 8 , pages 274–282 ( 2011 ) Cite this article
4016 Accesses
153 Citations
41 Altmetric
Metrics details
- Pathogenesis
- Reconstruction
- Urogenital diseases
This article has been updated
Gender reassignment (which includes psychotherapy, hormonal therapy and surgery) has been demonstrated as the most effective treatment for patients affected by gender dysphoria (or gender identity disorder), in which patients do not recognize their gender (sexual identity) as matching their genetic and sexual characteristics. Gender reassignment surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. Genital procedures performed for gender dysphoria, such as vaginoplasty, clitorolabioplasty, penectomy and orchidectomy in male-to-female transsexuals, and penile and scrotal reconstruction in female-to-male transsexuals, are the core procedures in gender reassignment surgery. Nongenital procedures, such as breast enlargement, mastectomy, facial feminization surgery, voice surgery, and other masculinization and feminization procedures complete the surgical treatment available. The World Professional Association for Transgender Health currently publishes and reviews guidelines and standards of care for patients affected by gender dysphoria, such as eligibility criteria for surgery. This article presents an overview of the genital and nongenital procedures available for both male-to-female and female-to-male gender reassignment.
The management of gender dysphoria consists of a combination of psychotherapy, hormonal therapy, and surgery
Psychiatric evaluation is essential before gender reassignment surgical procedures are undertaken
Gender reassignment surgery refers to the whole genital, facial and body procedures required to create a feminine or a masculine appearance
Sex reassignment surgery refers to genital procedures, namely vaginoplasty, clitoroplasty, labioplasty, and penile–scrotal reconstruction
In male-to-female gender dysphoria, skin tubes formed from penile or scrotal skin are the standard technique for vaginal construction
In female-to-male gender dysphoria, no technique is recognized as the standard for penile reconstruction; different techniques fulfill patients' requests at different levels, with a variable number of surgical technique-related drawbacks
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Principles and outcomes of gender-affirming vaginoplasty

Sexual function of transgender assigned female at birth seeking gender affirming care: a narrative review

The effect of early puberty suppression on treatment options and outcomes in transgender patients
Change history, 26 april 2011.
In the version of this article initially published online, the statement regarding the frequency of male-to-female transsexuals was incorrect. The error has been corrected for the print, HTML and PDF versions of the article.
Meyer, W. 3rd. et al . The Harry Benjamin International Gender Dysphoria Association's standards of care for gender identity disorders, sixth version. World Professional Association for Transgender Health [online] , (2001).
Google Scholar
Bakker, A., Van Kesteren, P., Gooren, L. & Bezemer, P. The prevalence of transsexualism in The Netherlands. Acta Psychiatr. Scand. 87 , 237–238 (1993).
Article CAS Google Scholar
Selvaggi, G. et al . Gender identity disorder: general overview and surgical treatment for vaginoplasty in male-to-female transsexuals. Plast. Reconstr. Surg. 116 , 135e–145e (2005).
Article Google Scholar
Benjamin, H. (ed.) The Transsexual Phenomenon (Julian Press Inc., New York, 1966).
World Professional Association for Transgender Health [online] , (2010).
Zhou, J. N., Hofman, M. A., Gooren, L. J. & Swaab, D. F. A sex difference in the human brain and its relation to transsexuality. Nature 378 , 68–70 (1995).
Kruijver, F. P. et al . Male-to-female transsexuals have female neuron numbers in a limbic nucleus. J. Clin. Endocrinol. Metab. 85 , 2034–2041 (2000).
Swaab, D. F., Chun, W. C., Kruijver, F. P., Hofman, M. A. & Ishuina, T. A. Sexual differentiation of the human hypothalamus. Adv. Exp. Med. Biol. 511 , 75–105 (2002).
Garcia-Falgueras, A. & Swaab, D. F. A sex difference in the hypothalamic uncinate nucleus: relationship to gender identity. Brain 131 , 3115–3117 (2008).
Cohen-Kettenis, P. & Kuiper, B. Transseksualiteit en psychotherapie [Dutch]. Tijdschr. Psychoth. 3 , 153–166 (1984).
Kuiper, B. & Cohen-Kettenis, P. Sex reassignment surgery: a study of 141 Dutch transsexuals. Arch. Sex. Behav. 17 , 439–457 (1988).
Kanhai, R. C., Hage, J. J., Karim, R. B. & Mulder, J. W. Exceptional presenting conditions and outcome of augmentation mammoplasty in male-to female transsexuals. Ann. Plast. Surg. 43 , 476–483 (1999).
Kanagalingm, J. et al . Cricothyroid approximation and subluxation in 21 male-to-female transsexuals. Laryngoscope 115 , 611–618 (2005).
Bouman, M. Laparoscopic assisted colovaginoplasty. Presented at the 2009 biennial World Professional Association for Transgender Health meeting, Oslo.
Rubin, S. O. Sex-reassignment surgery male-to-female. Review, own results and report of a new technique using the glans penis as a pseudoclitoris. Scand. J. Urol. Nephrol. Suppl. 154 , 1–28 (1993).
CAS PubMed Google Scholar
Fang, R. H., Chen, C. F. & Ma, S. A new method for clitoroplasty in male-to-female sex reassignment surgery. Plast. Reconstr. Surg. 89 , 679–682 (1992).
Selvaggi, G. et al . Genital sensitivity in sex reassignment surgery. Ann. Plast. Surg. 58 , 427–433 (2007).
Watanayusakul, S. SRS procedures. The Suporn Clinic [online] , (2010).
Melzer, T. Managing complications of male to female surgery. Presented at the 2007 World Professional Association for Transgender Health biennial meeting, Chicago.
Gilleard, O., Qureshi, M., Thomas, P. & Bellringer, J. Urethral bleeding following male to female gender reassignmetn surgery. Presented at the 2009 World Professional Association for Transgender Health biennial meeting, Oslo.
Beckley, I., Thomas, P. & Bellringer, J. Aetiology and management of recto-vaginal fistulas following male to female gender reassignment. Presented at 2008 EAU section of genitourinary surgeons and the EAU section of andrological urology meeting, Madrid.
Monstrey, S. et al . Chest wall contouring surgery in female-to-male (FTM) transsexuals: a new algorithm. Plast. Reconstr. Surg. 121 , 849–859 (2008).
Mueller, A. & Gooren, L. Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. Eur. J. Endocrinol. 159 , 197–202 (2008).
Selvaggi, G., Elander, A. & Branemark, R. Penile epithesis: preliminary study. Plast. Reconstr. Surg. 126 , 265e–266e (2010).
Selvaggi, G. & Elander, A. Penile reconstruction/formation. Curr. Opin. Urol. 18 , 589–597 (2008).
Gilbert, D. A., Jordan, G. H., Devine, C. J. Jr & Winslow, B. H. Microsurgical forearm “cricket bat-transformer” phalloplasty. Plast. Reconstr. Surg. 90 , 711–716 (1992).
Bettocchi, C., Ralph, D. J. & Pryor, J. P. Pedicled pubic phalloplasty in females with gender dysphoria. BJU Int. 95 , 120–124 (2005).
Monstrey, S. et al . Penile reconstruction: is the radial forearm flap really the standard technique? Plast. Reconstr. Surg. 124 , 510–518 (2009).
Selvaggi, G. et al . Donor-site morbidity of the radial forearm free flap after 125 phalloplasties in gender identity disorder. Plast. Reconstr. Surg. 118 , 1171–1177 (2006).
Hoebeke, P. et al . Impact of sex reassignment surgery on lower urinary tract function. Eur. Urol. 47 , 398–402 (2005).
Agrawal, V. & Ralph, D. An audit of implanted penile prosteses in the UK. BJU Int. 98 , 393–395 (2006).
Hoebeke, P. B. et al . Erectile implants in female-to-male transsexuals: our experience in 129 patients. Eur. Urol. 57 , 334–340 (2010).
Vesely, J. et al . New technique of total phalloplasty with reinnervated latissimus dorsi myocutaneous free flap in female-to-male transsexuals. Ann. Plast. Surg. 58 , 544–550 (2007).
Selvaggi, G. et al . Scrotal reconstruction in female-to-male transsexuals: a novel scrotoplasty. Plast. Reconstr. Surg. 123 , 1710–1718 (2009).
Download references
Author information
Authors and affiliations.
Gender Surgery Unit, Charing Cross Hospital, Imperial College NHS Trust, 179–183 Fulham Palace Road, London, W6 8QZ, UK
Gennaro Selvaggi & James Bellringer
You can also search for this author in PubMed Google Scholar
Contributions
G. Selvaggi and J. Bellringer contributed equally to the research, discussions, writing, reviewing, and editing of this article.
Corresponding author
Correspondence to James Bellringer .
Ethics declarations
Competing interests.
The authors declare no competing financial interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Selvaggi, G., Bellringer, J. Gender reassignment surgery: an overview. Nat Rev Urol 8 , 274–282 (2011). https://doi.org/10.1038/nrurol.2011.46
Download citation
Published : 12 April 2011
Issue Date : May 2011
DOI : https://doi.org/10.1038/nrurol.2011.46
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
A bibliometric and visualisation analysis on the research of female genital plastic surgery based on the web of science core collection database.
- Xianling Zhang
Aesthetic Plastic Surgery (2024)
Chest Feminization in Transwomen with Subfascial Breast Augmentation—Our Technique and Results
- James Roy Kanjoor
- Temoor Mohammad Khan
Aesthetic Plastic Surgery (2023)
Vaginoplasty in Male to Female transgenders: single center experience and a narrative review
- Luca Ongaro
- Giulio Garaffa
- Giovanni Liguori
International Journal of Impotence Research (2021)

Urethral complications after gender reassignment surgery: a systematic review
- L. R. Doumanian
Overview on metoidioplasty: variants of the technique
- Marta Bizic
- Borko Stojanovic
- Miroslav Djordjevic
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

This page has been archived and is no longer being updated regularly.
The psychological challenges of gender reassignment surgery
July/August 2007, Vol 38, No. 7
Print version: page 53
Surgery and hormonal therapy are increasingly common treatments for gender dysphoria, but the prejudice and discrimination transgender individuals face post-transition can cause significant psychological distress, says Marci Bowers, MD, a surgeon who performs gender reassignment surgery in Trinidad, Colo., and is herself transgender.
Post-change, many men and women deal with rancorous divorces, custody battles, job loss and rejection by family members, she has found. Some even commit suicide, continues Bowers, who will speak about the psychological impact of transgendersurgery at APA's 2007 Annual Convention.
"It's a wonder that anyone transitions-the penalties are so severe," she says.
Bowers wants to help dispel the myths and misperceptions surrounding transgender surgery-among them that transitioning individuals are really gay men or lesbians in denial or that they are mentally ill.
"Because dysphoria is currently listed as a psychological disorder, transgender [people] are assumed to be mentally ill," she explains. "This doesn't allow them to be treated equally, no matter how visually compelling the change is."
This stigma can have far-reaching psychological effects, Bowers says. "The transition provides great barriers to intimacy, and for a person's psychological well-being, intimacy is very important."
Psychologists can help transgender people overcome such barriers as therapists and also by researching and raising awareness about the social and economic barriers transgender people face.
--L. Meyers
Letters to the Editor
- Send us a letter
SYSTEMATIC REVIEW article
Readiness assessments for gender-affirming surgical treatments: a systematic scoping review of historical practices and changing ethical considerations.

- 1 Department of Psychiatry and Behavioral Sciences, Northwestern Medicine, Chicago, IL, United States
- 2 The Pritzker Department of Psychiatry and Behavioral Health, Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL, United States
- 3 Galter Health Science Library, Northwestern University, Chicago, IL, United States
Transgender and gender diverse (TGD) are terms that refer to individuals whose gender identity differs from sex assigned at birth. TGD individuals may choose any variety of modifications to their gender expression including, but not limited to changing their name, clothing, or hairstyle, starting hormones, or undergoing surgery. Starting in the 1950s, surgeons and endocrinologists began treating what was then known as transsexualism with cross sex hormones and a variety of surgical procedures collectively known as sex reassignment surgery (SRS). Soon after, Harry Benjamin began work to develop standards of care that could be applied to these patients with some uniformity. These guidelines, published by the World Professional Association for Transgender Health (WPATH), are in their 8th iteration. Through each iteration there has been a requirement that patients requesting gender-affirming hormones (GAH) or gender-affirming surgery (GAS) undergo one or more detailed evaluations by a mental health provider through which they must obtain a “letter of readiness,” placing mental health providers in the role of gatekeeper. WPATH specifies eligibility criteria for gender-affirming treatments and general guidelines for the content of letters, but does not include specific details about what must be included, leading to a lack of uniformity in how mental health providers approach performing evaluations and writing letters. This manuscript aims to review practices related to evaluations and letters of readiness for GAS in adults over time as the standards of care have evolved via a scoping review of the literature. We will place a particular emphasis on changing ethical considerations over time and the evolution of the model of care from gatekeeping to informed consent. To this end, we did an extensive review of the literature. We identified a trend across successive iterations of the guidelines in both reducing stigma against TGD individuals and shift in ethical considerations from “do no harm” to the core principle of patient autonomy. This has helped reduce barriers to care and connect more people who desire it to gender affirming care (GAC), but in these authors’ opinions does not go far enough in reducing barriers.
Introduction
Transgender and gender diverse (TGD) are terms that refer to any individual whose gender identity is different from their sex assigned at birth. Gender identity can be expressed through any combination of name, pronouns, hairstyle, clothing, and social role. Some TGD individuals wish to transition medically by taking gender-affirming hormones (GAH) and/or pursuing gender-affirming surgery (GAS) ( 1 ). 1 The medical community’s comfort level with TGD individuals and, consequently, their willingness to provide a broad range of gender affirming care (GAC) 2 has changed significantly over time alongside an increasing understanding of what it means to be TGD and increasing cultural acceptance of LGBTQI people.
Historically physicians have placed significant barriers in the way of TGD people accessing the care that we now know to be lifesaving. Even today, patients wishing to receive GAC must navigate a system that sometimes requires multiple mental health evaluations for procedures, that is not required of cisgender individuals.
The medical and psychiatric communities have used a variety of terms over time to refer to TGD individuals. The first and second editions of DSM described TGD individuals using terms such as transvestism (TV) and transsexualism (TS), and often conflated gender identity with sexuality, by including them alongside diagnoses such as homosexuality and paraphilias. Both the DSM and the International Classification of Diseases (ICD) have continuously changed diagnostic terminology and criteria involving TGD individuals over time, from Gender Identity Disorder in DSM-IV to Gender Dysphoria in DSM-5 to Gender Incongruence in ICD-11.
In 1979, the Harry Benjamin International Gender Dysphoria Association 3 , renamed the World Profession Association for Transgender Health (WPATH) in 2006, was the first to publish international guidelines for providing GAC to TGD individuals. The WPATH Standards of Care (SOC) are used by many insurance companies and surgeons to determine an individual’s eligibility for GAC. Throughout each iteration, mental health providers are placed in the role of gatekeeper and tasked with conducting mental health evaluations and providing required letters of readiness for TGD individuals who request GAC ( 1 ). As part of this review, we will summarize the available literature examining the practical and ethical changes in conducting mental health readiness assessments and writing the associated letters.
While the WPATH guidelines specify eligibility criteria for GAC and a general guide for what information to include in a letter of readiness, there are no widely agreed upon standardized letter templates or semi-structured interviews, leading to a variety of practices in evaluation and letter writing for GAC ( 2 ). To our knowledge, this is the first scoping review to summarize the available research to date regarding the evolution of the mental health evaluation and process of writing letters of readiness for GAS. By summarizing trends in these evaluations over time, we aim to identify best practices and help further guide mental health professionals working in this field.
The review authors conducted a comprehensive search of the literature in collaboration with a research librarian (ABW) according to PRISMA guidelines. The search was comprised of database-specific controlled vocabulary and keyword terms for (1) mental health and (2) TGD-related surgeries. Searches were conducted on December 2, 2020 in MEDLINE (PubMed), the Cochrane Library Databases (Wiley), PsychINFO (EBSCOhost), CINAHL (EBSCOhost), Scopus (Elsevier), and Dissertations and Theses Global (ProQuest). All databases were searched from inception to present without the use of limits or filters. In total, 8,197 results underwent multi-pass deduplication in a citation management system (EndNote), and 4,411 unique entries were uploaded to an online screening software (Rayyan) for title/abstract screening by two independent reviewers. In total, 303 articles were included for full text screening ( Figure 1 ), however, 69 of those articles were excluded as they were unable to be obtained online or through interlibrary loan. Both review authors conducted a full text screen of the remaining 234 articles. Articles were included in the final review if they specified criteria used for mental health screening/evaluation and/or letter writing for GAS, focused on TGD adults, were written in English, and were peer-reviewed publications. Any discrepancies were discussed between the two review authors TA and KK and a consensus was reached. A total of 86 articles met full inclusion criteria. Full documentation of all searches can be found in the Supplementary material .
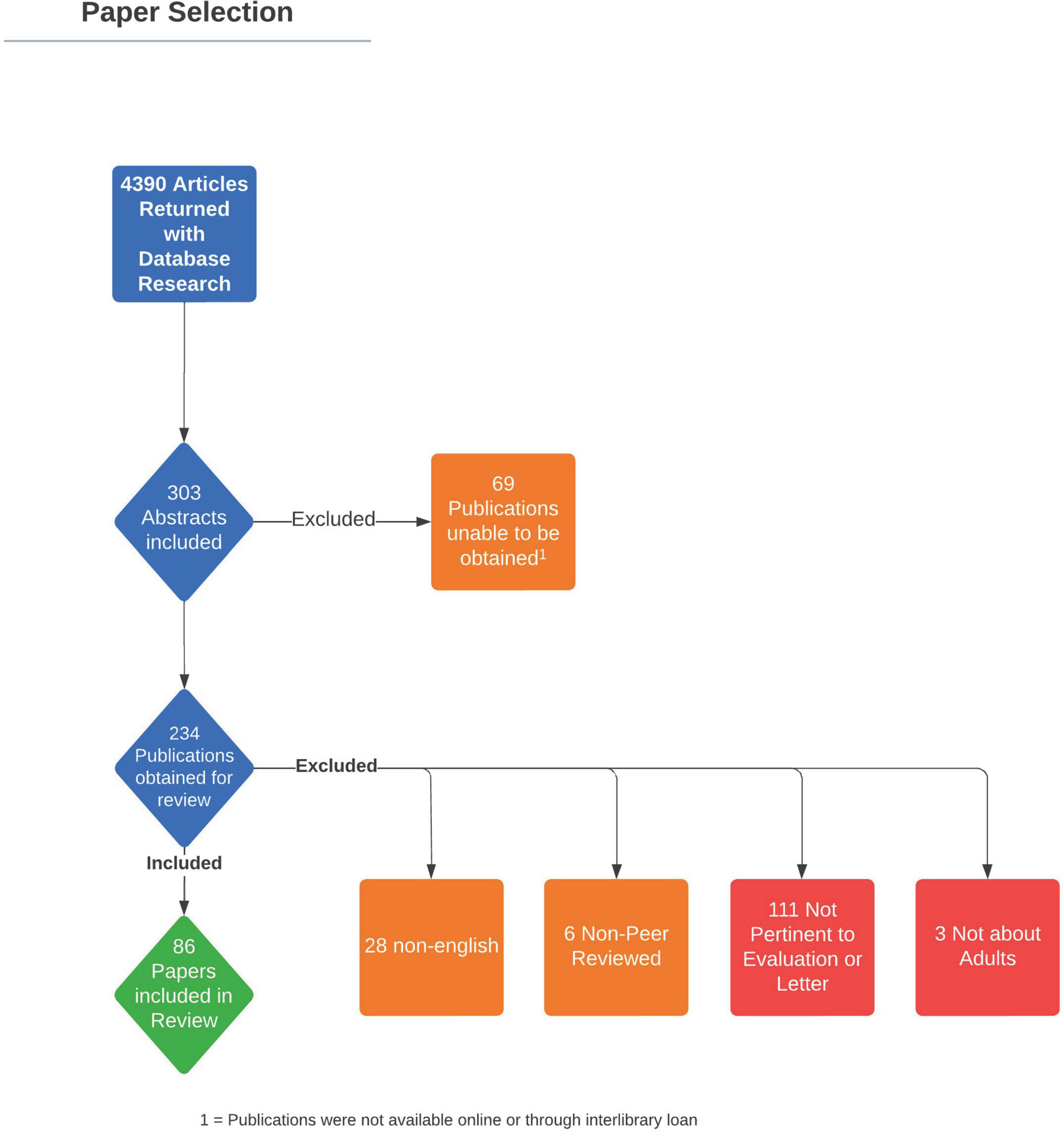
Figure 1. PRISMA flow diagram demonstrating article review process.
In total, 86 articles were included for review. Eleven articles were focused on ethical considerations while the remaining 75 articles focused on the mental health evaluation and process of writing letters of readiness for GAS. Version 8 of the SOC was published in September of 2022 during the review process of this manuscript and is also included as a reference and point of discussion.
Prior to the publication of the standards of care
Fourteen articles were identified in the literature search as published prior to the development of the WPATH SOC version 1 in 1979. Prominent themes included classification, categorization, and diagnosis of TS. Few publications described the components of a mental health evaluation, and inclusion and exclusion criteria, for GAS. Many publications focused exclusively on transgender females, with a paucity of literature examining the experiences of transgender males during this timeframe.
Authors emphasized accurate diagnosis of TS, highlighting elements of the psychosocial history including early life cross-dressing, preference for play with the opposite gender toys and friends, and social estrangement around puberty ( 3 ). One author proposed the term gender dysphoria syndrome, which included the following criteria: a sense of inappropriateness in one’s anatomically congruent sex role, that role reversal would lead to improvement in discomfort, homoerotic interest and heterosexual inhibition, an active desire for surgical intervention, and the patient taking on an active role in exploring their interest in sex reassignment ( 4 ). Many authors attempted to differentiate between the “true transsexual” and other diagnoses, including idiopathic TS; idiopathic, essential, or obligatory homosexuality; neuroticism; TV; schizophrenia; and intersex individuals ( 5 , 6 ).
Money argued that the selection criteria for patients requesting GAS include a psychiatric evaluation to obtain collateral information to confirm the accuracy of the interview, work with the family to foster support of the individual, and proper management of any psychiatric comorbidities ( 5 ). Authors began to assemble a list of possible exclusion criteria for receiving GAS such as psychosis, unstable mental health, ambivalence, and secondary gain (e.g., getting out of the military), lack of triggering major life events or crises, lack of sufficient distress in therapy, presence of marital bonds (given the illegality of same-sex marriage during this period), and if natal genitals were used for pleasure ( 3 – 5 , 7 – 13 ).
Others focused the role of the psychiatric evaluation on the social lives and roles of the patient. They believed the evaluation should include exploring the patient’s motivation for change for at least 6–12 months ( 8 ), facilitating realistic expectations of treatment, managing family issues, providing support during social transition and post-operatively ( 13 ), and encouraging GAH and the “real-life test” (RLT). The RLT is a period in which a person must fully live in their affirmed gender identity, “testing” if it is right for them. In 1970, Green recommended that a primary goal of treatment was that, “the male patient must be able to pass in society as a socially acceptable woman in appearance and to conduct the normal affairs of the day without arousing undue suspicion” ( 14 ). Benjamin also noted concern that “too masculine” features may be a contraindication to surgery so as to not make an “acceptable woman” ( 7 ). Some publications recommended at least 1–2 years of a RLT ( 3 , 7 , 11 , 15 ), while others recommended at least 5 years of RLT prior to considering GAS ( 12 ). Emphasis was placed on verifying the accuracy of reported information from family or friends to ensure “authentic” motivation for GAS and rule out ambivalence or secondary gain (e.g., getting out of the military) ( 10 ).
Ell recommended evaluation to ensure the patient has “adequate intelligence” to understand realistic expectations of surgery and attempted to highlight the patient’s autonomy in the decision to undergo GAS. He wrote, “That is your decision [to undergo surgery]. It’s up to you to prove that you are a suitable candidate for surgery. It’s not for me to offer it to you. If you decide to go ahead with your plans to pass in the opposite gender role, you do it on your own responsibility” ( 8 ). Notably, many authors conceptualized gender transition along a binary, with individuals transitioning from one end to the other.
In these earliest publications, one can start to see the beginning framework of modern-day requirements for accessing GAS, including ensuring an accurate diagnosis of gender incongruence; ruling out other possible causes of presentation such as psychosis; ensuring general mental stability; making sure that the patient has undergone at least some time of living in their affirmed gender; and that they are able to understand the consequences of the procedure.
Standards of care version 1 and 2
Changes to the standards of care.
The first two versions of the WPATH SOC were written in 1979 and 1980, respectively and are substantially similar to one another. SOC version three was the first to be published in an academic journal in 1985 and changes from the first two versions were documented within this publication. The first two versions required that all recommendations for GAC be completed by licensed psychologists or psychiatrists. The first version recommended that patients requesting GAH and non-genital GAS, spend 3 and 6 months, respectively, living full time in their affirmed gender. These recommendations were rescinded in subsequent versions ( 16 ). Figure 2 reviews changes to the recommendations for GAC within the WPATH SOC over time.
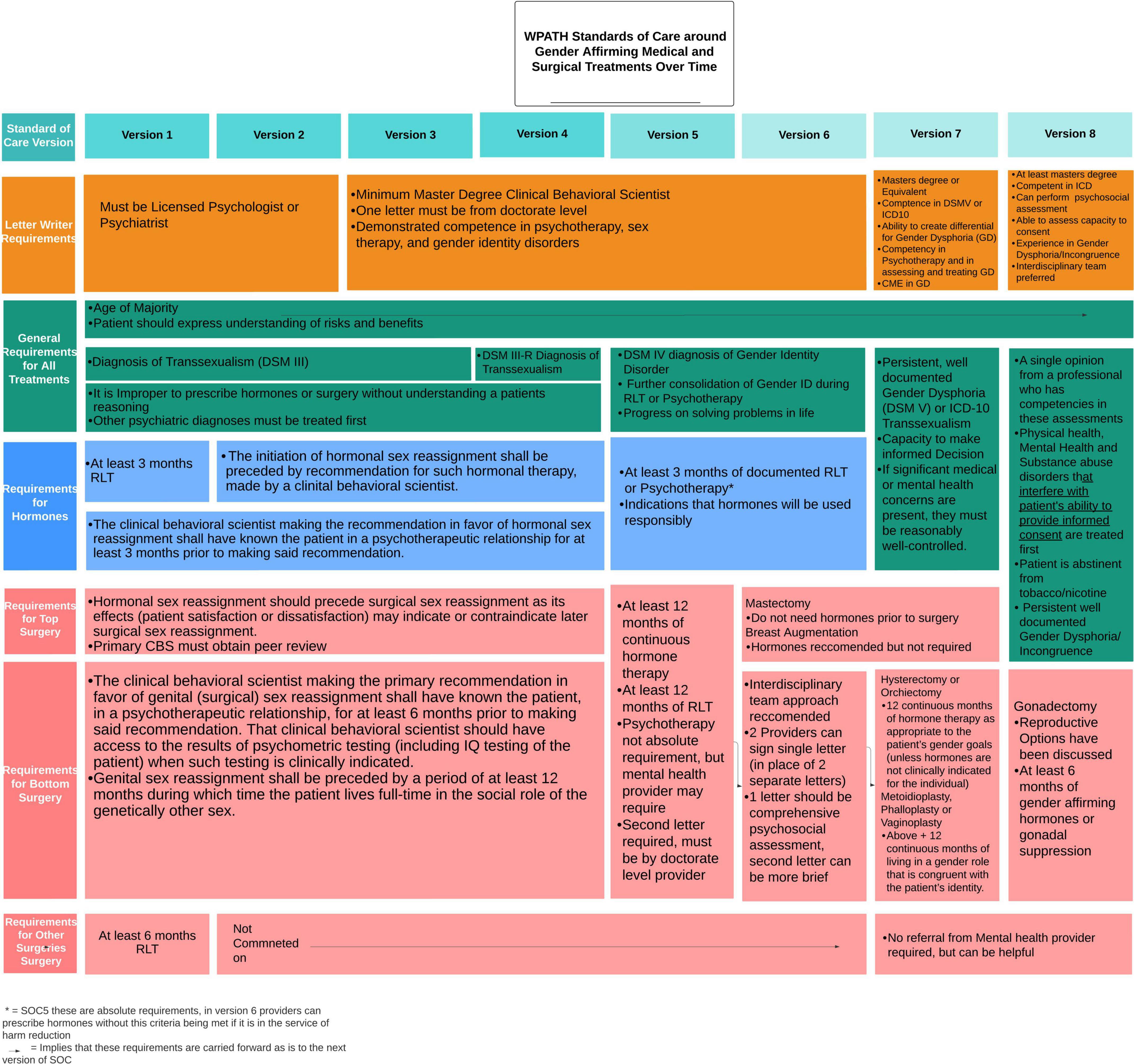
Figure 2. Changes to the World Professional Association for Transgender Health (WPATH) standards of care around gender affirming medical and surgical treatments over time.
Results review
Five articles published between 1979 and 1980 were included in this review. Again, emphasis was placed on proper diagnosis, classification and consistency of gender identity over time ( 17 , 18 ).
Wise and Meyer explored the concept of a continuum between TV and TS, describing that those who experienced gender dysphoria often requested GAS, displayed evidence of strong cross-dressing desires with arousal, history of cross-gender roles, and absence of manic-depressive or psychotic illnesses ( 19 ). Requirements for GAS at the Johns Hopkins Gender Clinic included at least 2 years of cross-dressing, working in the opposite gender role, and undergoing treatment with GAH and psychotherapy ( 19 ). Bernstein identified factors correlated with negative GAS outcomes including presence of psychosis, drug abuse, frequent suicide attempts, criminality, unstable relationships, and low intelligence level ( 18 ). Lothstein stressed the importance of correct diagnosis, “since life stressors may lead some transvestites to clinically present as transsexuals desiring SRS” ( 20 ). Levine reviewed the diagnostic process employed by Case Western Reserve University Gender Identity Clinic which involved initial interview by a social worker to collect psychometric testing, followed by two independent psychiatric interviews to obtain the developmental gender history, understand treatment goals, and evaluate for underlying co-morbid mental health diagnoses, with a final multidisciplinary conference to integrate the various evaluations and develop a treatment plan ( 21 ).
Standards of care version 3
Version 3 broadened the definition of the clinician thereby broadening the scope of providers who could write recommendation letters for GAC. Whereas prior SOC required letters from licensed psychologists or psychiatrists, version 3 allowed initial evaluations from providers with at least a Master’s degree in behavioral science, and when required, a second evaluation from any licensed provider with at least a doctoral degree. Version 3 recommended that all evaluators demonstrate competence in “gender identity matters” and must know the patient, “in a psychotherapeutic relationship,” for at least 6 months ( 16 ). Version 3 relied on the definition of TS in DSM-III, which specified the sense of discomfort with one’s anatomic sex be “continuous (not limited to a period of stress) for at least 2 years” and be independently verified by a source other than the patient through collateral or through a longitudinal relationship with the mental health provider ( 16 ). Recommendation of GAS specifically required at least 6–12 months of RLT, for non-genital and genital GAS, respectively ( 16 ).”
Nine articles were published during the timeframe that the SOC version 3 were active (1981–1990). Themes in these publications included increasing focus on selection criteria for GAS and emphasis on the RLT, which was used to ensure proper diagnosis of gender dysphoria. Recommendations for the duration of the RLT ranged anywhere between 1 and 3 years ( 22 , 23 ).
Proposed components of the mental health evaluation for GAS included a detailed assessment of the duration, intensity, and stability of the gender dysphoria, identification of underlying psychiatric diagnoses and suicidal ideation, a mental status examination to rule out psychosis, and an assessment of intelligence (e.g., IQ) to comment on the individual’s “capacity and competence” to consent to GAC. The Minnesota Multiphasic Personality Inventory (MMPI), Weschler Adult Intelligence Scale (WAIS), and Lindgren-Pauly Body Image Scale were also used during assessments ( 24 ).
Authors developed more specific inclusion and exclusion criteria for undergoing GAS with inclusion criteria including age 21 or older, not legally married, no pending litigation, evidence of gender dysphoria, completion of 1 year of psychotherapy, between 1 and 2 years RLT with ability to “pass convincingly” and “perform successfully” in the opposite gender role, at least 6 months on GAH (if medically tolerable), reasonably stable mental health (including absence of psychosis, depression, alcoholism and intellectual disability), good financial standing with psychotherapy fees ( 25 ), and a prediction that GAS would improve personal and social functioning ( 26 – 29 ). A 1987 survey of European psychiatrists identified their most common requirements as completion of a RLT of 1–2 years, psychiatric observation, mental stability, no psychosis, and 1 year of GAH ( 27 ).
Standards of care version 4
World Professional Association for Transgender Health SOC version four was published in 1990. Between version three and version four, DSM-III-R was published in 1987. Version four relied on the DSM-III-R diagnostic criteria for TS as opposed to the DSM-III criteria in version three. The DSM-III-R criteria for TS included a “persistent discomfort and sense of inappropriateness about one’s assigned sex,” “persistent preoccupation for at least 2 years with getting rid of one’s primary and secondary sex characteristics and acquiring the sex characteristics of the other sex,” and that the individual had reached puberty ( 30 ). Notable changes from the DSM-III criteria include specifying a time duration for the discomfort (2 years) and designating that individuals must have reached puberty.
Six articles were published between 1990 and 1998 while version four was active. Earlier trends continued including emphasizing proper diagnosis of gender dysphoria ( 31 , 32 ), however, a new trend emerged toward implementing more comprehensive evaluations, with an emphasis on decision making, a key element of informed consent.
Bockting and Coleman, in a move representative of other publications of this era, advocated for a more comprehensive approach to the mental health evaluation and treatment of gender dysphoria. Their treatment model was comprised of five main components: a mental health assessment consisting of psychological testing and clinical interviews with the individual, couple, and/or family; a physical examination; management of comorbid disorders with pharmacotherapy and/or psychotherapy; facilitation of identity formation and sexual identity management through individual and group therapy; and aftercare consisting of individual, couple, and/or family therapy with the option of a gender identity consolidation support group. Psychoeducation was a main thread throughout the treatment model and a variety of treatment “subtasks” such as understanding decision making, sexual functioning and sexual identity exploration, social support, and family of origin intimacy were identified as important. The authors advocated for “a clear separation of gender identity, social sex role, and sexual orientation which allows a wide spectrum of sexual identities and prevents limiting access to GAS to those who conform to a heterosexist paradigm of mental health” ( 33 ).
This process can be compared with the Italian SOC for GAS which recommend a multidisciplinary assessment consisting of a psychosocial evaluation and informed consent discussion around treatment options, procedures, and risks. Requirements included 6 months of psychotherapy prior to initiating GAH, 1 year of a RLT prior to GAS, and provision of a court order approving GAS, which could not be granted any sooner than 2 years after starting the process of gender transition. Follow-up was recommended at 6, 12, and 24 months post-GAS to ensure psychosocial adjustment to the affirmed gender role ( 34 ).
Other authors continued to refine inclusion and exclusion criteria for GAS by surveying the actual practices of health centers. Inclusion criteria included those who had life-long cross gender identification with inability to live in their sex assigned at birth; a 1–2 years RLT (a nearly universal requirement in the survey); and ability to pass “effortlessly and convincingly in society”; completed 1 year of GAH; maintained a stable job; were unmarried or divorced; demonstrated good coping skills and social-emotional stability; had a good support system; and were able to maintain a relationship with a psychotherapist. Exclusion criteria included age under 21 years old, recent death of a parent ( 35 ), unstable gender identity, unstable psychosocial circumstances, unstable psychiatric illness (such as schizophrenia, suicide attempts, substance abuse, intellectual disability, organic brain disorder, AIDS), incompatible marital status, criminal history/activity or physical/medical disability ( 36 ).
The survey indicated some programs were more lenient around considering individuals with bipolar affective disorder, the ability to pass successfully, and issues around family support. Only three clinics used sexual orientation as a factor in decision for GAS, marking a significant change in the literature from prior decades. Overall, the authors found that 74% of the clinics surveyed did not adhere to WPATH SOC, instead adopting more conservative policies ( 36 ).
Standards of care version 5
Published in 1998, version five defined the responsibilities of the mental health professional which included diagnosing the gender disorder, diagnosing and treating co-morbid psychiatric conditions, counseling around GAC, providing psychotherapy, evaluating eligibility and readiness criteria for GAC, and collaborating with medical and surgical colleagues by writing letters of recommendation for GAC ( Figure 3 ). Eligibility and readiness criteria were more explicitly described in this version to refer to the specific objective and subjective criteria, respectively, that the patient must meet before proceeding to the next step of their gender transition. The seven elements to include in a letter of readiness were more explicitly listed within this version as well including: the patient’s identifying characteristics, gender, sexual orientation, any other psychological diagnoses, duration and nature of the treatment with the letter writer, whether the author is part of a gender team, whether eligibility criteria have been met, the patient’s ability to follow the SOC and an offer of collaboration. Version five removes the requirement that patients undertake psychotherapy to be eligible for GAC ( 37 ).
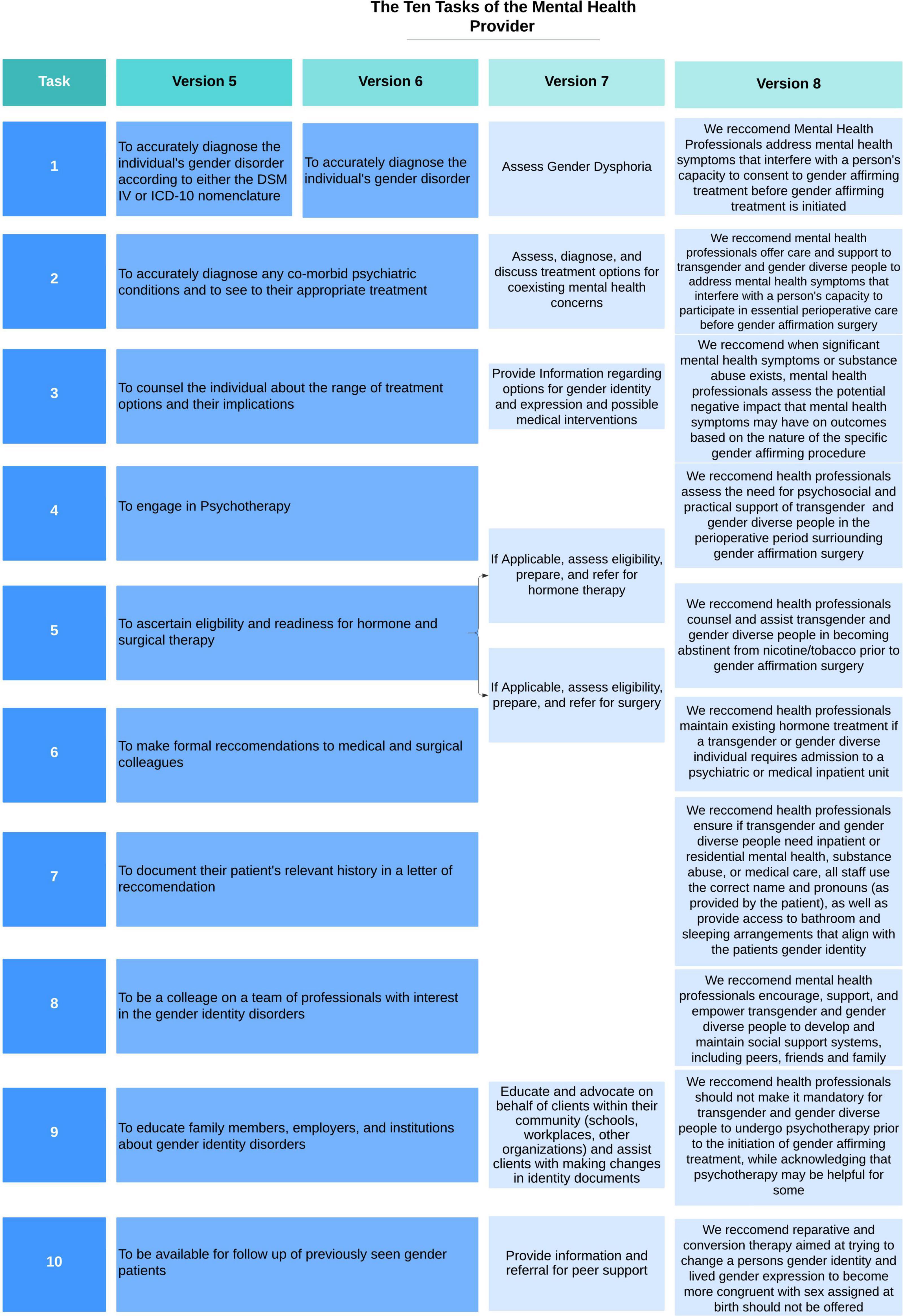
Figure 3. Changes to the ten tasks of the mental health provider within the World Professional Association for Transgender Health (WPATH) standards of care over time.
Five articles were published between 1998 and 2001 while version five was active. Two of these articles were summaries of the SOC ( 37 , 38 ). Themes in these publications included continued attempts to develop comprehensive treatment models for GAS.
Ma reviewed the role of the social worker in a multidisciplinary gender clinic in Hong Kong. Psychosocial assessment for GAS included evaluation of performance in affirmed social roles, adaptation to the affirmed gender role during the 1-year RLT and understanding the patient’s identified gender role and the response to the new gender role culturally and interpersonally within the individual’s support network and family unit. She noted five contraindications to GAS: a history of psychosis, sociopathy, severe depression, organic brain dysfunction or “defective intelligence,” success in parental or marital roles, “successful functioning in heterosexual intercourse,” ability to function in the pretransition gender role, and homosexual or TV history with genital pleasure. She proposed a social work practice model for patients who apply for GAS with categorization of TGD individuals into “better-adjusted” and “poorly-adjusted” with different intervention goals and methods for each. For those who were “better-adjusted,” treatment focused on psychoeducation, building coping tools, and mobilization into a peer counselor role, while treatment goals for those who were “poorly-adjusted” focused on building support and resources ( 39 ).
Damodaran and Kennedy reviewed the assessment and treatment model used by the Monash gender dysphoria clinic in Melbourne, Australia for patients requesting GAS. All referrals for GAS were assessed independently by two psychiatrists to determine proper diagnosis of gender dysphoria, followed by endocrinology and psychology consultation to develop a comprehensive treatment plan. Requirements included RLT of minimum 18 months and GAH ( 40 ).
Miach reviewed the utility of using the Minnesota Multiphasic Personality Inventory-2 (MMPI-2), a revision of the MMPI which was standardized using a more heterogeneous population, in a gender clinic to assess stability of psychopathology prior to GAS, which was only performed on patients aged 21–55 years old. The authors concluded that while the TGD group had a significantly lower level of psychopathology than the control group, they believed that the MMPI-2 was a useful test in assessing readiness for GAC ( 41 ).
Standards of care version 6
Published in 2001, version six of the WPATH SOC did not include significant changes to the 10 tasks of the mental health professional ( Figure 3 ) or in the general recommendations for content of the letters of readiness. An important change in the eligibility criteria for GAH allowed providers to prescribe hormones even if patients had not undergone RLT or psychotherapy if it was for harm reduction purposes (i.e., to prevent patient from buying black market hormones). A notable change in version six separated the eligibility and readiness criteria for top (breast augmentation or mastectomy) and bottom (any gender-affirming surgical alteration of genitalia or reproductive organs) surgery allowing some patients, particularly individuals assigned female at birth (AFAB), to receive a mastectomy without having been on GAH or completing a 12 month RLT ( 42 , 43 ).
Thirteen articles were published between 2001 and 2012. One is a systematic review of evidence for factors that are associated with regret and suicide, and predictive factors of a good psychological and social functioning outcome after GAC. De Cuypere and Vercruysse note that less than one percent of patients regret having GAS or commit suicide, making detection of negative predictive factors in a study nearly impossible. They identified a wide array of positive predictive factors including age at time of request, sex of partner, premorbid social or psychiatric functioning, adequacy of social support system, level of satisfaction with secondary sexual characteristics, and surgical outcomes. Many of these predictive factors were later disproved. They also noted that there were not enough studies to determine whether following the WPATH guidelines was a positive predictive factor. In the end they noted that the evidence for all established evaluation regimens (i.e., RLT, age cut-off, psychotherapy, etc.) was at best indeterminate. They recommended that changes to WPATH criteria should redirect focus from gender identity to psychopathology, differential diagnosis, and psychotherapy for severe personality disorders ( 44 ).
The literature at this time supports two opposing approaches to requests for GAC, those advocating for a set of strictly enforced eligibility and readiness criteria associated with very thorough evaluations and those who advocate for a more flexible approach. Common approaches to the evaluation for GAC include: taking a detailed social history including current relationships, support systems, income, and social functioning; a sexual development history meant to understand when and how the patient began to identify as TGD and how their transition has affected their life; an evaluation of their coping skills, “psychic functions” and general mental well-being; and a focus on assessing the “correct diagnosis” of gender identity disorder ( 44 – 56 ). The use of a multidisciplinary team was also commonly recommended ( 44 , 47 , 48 , 51 , 54 – 56 ).
Those that advocated for a stricter interpretation of the eligibility and readiness criteria emphasized the importance of the RLT ( 45 , 49 , 51 , 53 , 55 , 56 ). One clinic in the UK required a RLT lasting 2 years prior to starting GAH, twice as long as recommended by the SOC ( 49 ). The prevailing view continued to approach gender as a binary phenomenon, rather than as a spectrum of experiences. As a result, treatment recommendations emphasized helping the patient to “pass” in their chosen gender role and did not endorse patients receiving less than the full spectrum of treatment to transition fully from one sex to the other. Several authors indicated that they required some amount of psychotherapy before recommending GAC ( 46 , 47 , 51 , 52 , 55 , 56 ). One author described requirements in Turkey, which unlike the US has the requirements enshrined in law and defines an important role for the courts in granting permission for GAC ( 51 ). In general, these authors supported the gatekeeping role of the mental health provider as a mechanism to prevent cases of regret.
Among groups supporting a flexible interpretation of the SOC, there was a much stronger emphasis on the supportive role of the mental health provider in the gender transition process ( 44 – 46 , 48 , 52 , 53 ). This role included creating a supportive environment for the patient, asking and using the correct pronouns, and helping to guide them through what may be a difficult transition both socially and physically. They emphasized the importance of the psychosocial evaluation including the patient’s connections to others in the TGD community, their social functioning, substance use, and psychiatric history/psychological functioning. While informed consent was mentioned as part of the evaluation, the process was not thoroughly explored and largely focused on patients’ awareness that GAS is an irreversible procedure which removes healthy tissue ( 53 ). One author suggested that a “consumer handbook outlining such rights and responsibilities” related to GAS be made available, but they made no further comment on the informed consent process ( 44 ). There was no further guidance as to the contents of letters of readiness for GAC.
The lack of emphasis on informed consent by both groups of authors mirrors the discussion of informed consent within the SOC, which up through version six, had a relatively narrow definition and role specifically related to risks and benefits of surgery. As far back as version one, the SOC states “hormonal and surgical sex reassignment are procedures which must be requested by, and performed only with the agreement of, the patient having informed consent…[these procedures] may be conducted or administered only after the patient applicant has received full and complete explanations, preferably in writing, in words understood by the patient applicant, of all risks inherent in the requested procedures ( 16 ). “This reflects the dominant concerns of surgeons at the time that they were removing or damaging healthy tissue, which was unethical, and as such wanted to make sure that patients understood the irreversibility of the procedures. It was not until version 7 that there is a change in the discussion of informed consent.
Standards of care version 7
Standards of care version seven was published in 2013. Publication of version seven coincided with the publication of DSM-5, in which the diagnosis required to receive GAC shifted from Gender Identity Disorder to Gender Dysphoria, in an effort to de-pathologize TGD patients. Version seven highlights that these are guidelines meant to be flexible to account for different practices in different places. Compared to version six, a significantly expanded section on the “Tasks of the Mental Health Provider” was added, offering some instructions on what to include in the assessment of the patient for GAS. For the first time the SOC expand on what it means to obtain informed consent and describe a process where the mental health provider is expected to guide a conversation around gender identity and how different treatments and procedures might affect TGD individuals psychologically, socially, and physically. Other recommendations include “at a minimum, assessment of gender identity and gender dysphoria, history and development of gender dysphoric feelings, the impact of stigma attached to gender non-conformity on mental health, and the availability of support from family, friends, and peers.” There is also a change to the recommended content of the letters: switching from “The initial and evolving gender, sexual, and other psychiatric diagnoses” to “Results of the client’s psychosocial assessment, including any diagnoses”, indicating a shift in the focus away from diagnosis toward the psychosocial assessment. Version 7 also adds two new tasks for the mental health provider including “Educate and advocate on behalf of clients within their community (schools, workplaces, other organizations) and assist clients with making changes in identity documents” and “Provide information and referral for peer support”( 2 ).
There were also significant changes to eligibility criteria for GAC. For GAH, version seven eliminates entirely the requirement for a RLT and psychotherapy and adds requirements for “persistent well documented gender dysphoria” and “reasonably well controlled” medical or mental health concerns. Notably, the SOC do not define the meaning of “reasonably well controlled,” leaving providers to interpret this on their own. Version seven delineates separate requirements for top and bottom surgeries. The criteria for both feminizing and masculinizing top surgeries are identical to each other and identical to those laid out for GAH. Version seven explicitly states that GAH is not required prior to top surgery, although GAH is still recommended prior to gender-affirming breast augmentation. Criteria for bottom surgery are more explicitly defined, namely internal (i.e., hysterectomy, orchiectomy) vs. external (i.e., metoidioplasty, phalloplasty, and vaginoplasty). For internal surgeries, criteria are the same as for top surgery with the addition of a required 12 months of GAH. For external surgeries the criteria are the same as for internal, with the addition of required 12 months of living in the patient’s affirmed gender identity ( 2 , 42 ).
Twenty-three articles were published while version 7 of the SOC have been active. Themes include identifying the role of psychometric testing in GAC evaluations, expanding the discussion around informed consent for GAC, and revising the requirements for letter writers.
A systematic review evaluated the accuracy of psychometric tests in those requesting GAC, identifying only two published manuscripts that met their inclusion criteria, both of which were of poor quality; this led them to question the utility of psychometric tests in in TGD patients ( 57 ). Keo-Meir and Fitzgerald provided a detailed narrative review of psychometric and neurocognitive exams in the TGD population and concluded that psychometric testing should not be done unless there is a question about the capacity of the patient to provide informed consent ( 58 ). The only other manuscripts that include a mention of psychological testing describe processes in Iran and China, both of which require extensive psychological testing prior to approval for GAC ( 59 , 60 ). These two manuscripts, in addition to an ethnographic study of the evaluation process in Turkey ( 61 ), are also the only ones that indicate a requirement for psychotherapy prior to approval for treatment. The three international manuscripts described above plus three manuscripts from the US ( 62 – 64 ) are the only ones to include consideration of a RLT, with authors outside the US preferring a long RLT and US authors considering RLT as part of the informed consent process for GAS, and not required at all prior to the initiation of GAH.
Many authors describe the process of informed consent for GAC ( 1 , 58 , 60 , 62 – 76 ). In China, a signature indicating informed consent from the patient’s family is required in addition to that of the patient ( 60 ). Many authors emphasize evaluating for and addressing social determinants of health including housing status, income, transportation, trauma history, etc. ( 1 , 58 , 60 , 67 , 69 – 71 , 75 – 77 ). Deutsch advocated for the psychosocial evaluation being the most important aspect of the evaluation and suggests that one of the letters required for bottom surgery be replaced by a functional assessment (i.e., ADLs/iADLs), which could be repeated as needed or removed entirely for high functioning patients ( 69 ).
Practice patterns and opinions on who should write letters of readiness and how many letters should be required vary widely. Many letters that surgeons receive are cursory, and short and non-personal letters correlate with poor surgical outcomes ( 1 ). Several authors advocate for eliminating the second letter entirely, for at least some procedures, as it is a barrier to care ( 68 , 69 , 74 ). Some support removing the requirement that both letter writers be therapists or psychiatrists, and even suggesting the second letter be written by a urologist ( 72 ) or a social worker who has performed a detailed social assessment ( 69 , 75 ). The evaluation in Turkey requires a report written by an extensive multidisciplinary team and submitted to a court for approval ( 61 ). Surveys of providers indicate that the SOC are not uniformly implemented leading to huge disparities based on the providers knowledge level and personal beliefs ( 77 , 78 ). Additional recommendations include that providers spend significant time discussing the SOC and diagnosis of gender dysphoria with the patients prior to providing a letter to prepare them for the stigma such a diagnosis may confer ( 65 , 66 ), and dropping gender dysphoria entirely in favor the ICD-11 diagnosis of gender incongruence, as it may be less stigmatizing ( 71 ).
The Mount Sinai Gender Clinic describes an integrated multidisciplinary model where a patient will see a primary care doctor, endocrinologist, social worker, psychiatrist, and obtain any necessary lab work in a single visit, significantly reducing barriers to care. The criteria in this model focus on informed consent, the social determinants of health, being physically ready for surgery, and putting measurable goals on psychiatric stability, while deemphasizing the gender dysphoria diagnosis. Their study showed that people who received their evaluation over a 2-year period were more likely to meet their in-house criteria than they were to meet criteria as set forth in WPATH SOC. The Mount Sinai criteria allowed for significantly decreased barriers to care, allowing more people to progress through desired GAC in a timely fashion ( 75 ).
Standards of care version 8
Standards of care version 8, published in September 2022, includes major updates to the guidelines around GAS. This version explicitly highlights the importance of informed decision making, patient autonomy, and harm reduction models of care, as well as emphasizing the flexibility of the guidelines which the authors note can be modified by the healthcare provider in consultation with the TGD individual.
Version 8 lays out the roles of the assessor which are to identify the presence of gender incongruence and any co-existing mental health concerns, provide information on GAC, support the TGD individual in their decision-making, and to assess for capacity to consent to GAC. The authors emphasize the collaborative nature of this decision-making process between the assessor and the TGD individual, as well as recommending TGD care occur in a multidisciplinary team model when possible.
Version 8 recommends that providers who assess TGD individuals for GAC hold at least a Master’s level degree and have sufficient knowledge in diagnosing gender incongruence and distinguishing it from other diagnoses which may present similarly. These changes allow for non-mental health providers to be the main assessors for GAC.
Version 8 recommends reducing the number of evaluations prior to GAS to a single evaluation in an effort to reduce barriers to care for the TGD population. Notably, the authors have removed the recommendations around content of the letter of readiness for GAC. The guidelines note that the complexity of the assessment process may differ from patient to patient, based on the type of GAC requested and the specific characteristics of the patient. Version eight directly states that psychometric testing and psychotherapy are not requirements to pursue GAC. While evaluations should continue to identify co-existing mental health diagnoses, version 8 highlights that the presence of a mental health diagnosis should not prevent access to GAC unless the mental health symptoms directly interfere with capacity to provide informed consent for treatment or interfere with receiving treatment. Version 8 recommends that perioperative matters, such as travel requirements, presence of stable, safe housing, hygiene/healthy living, any activity restrictions, and aftercare optimization, be discussed by the surgeon prior to GAS. In terms of eligibility criteria, the authors recommend a reduced duration of GAH from 12 months (from version 7) to 6 months (in version 8) prior to pursuing GAS involving reproductive organs ( 79 ).
Ethical discussions
A total of eleven articles explored ethical considerations of conducting mental health evaluations and writing letters of readiness for GAS, including a comparison of the ethical principles prioritized within the “gatekeeping” model vs. the informed consent model for GAC and the differential treatment of TGD individuals compared to cisgender individuals seeking similar surgical procedures.
Many authors compare the informed consent model of care for TGD individuals to the WPATH SOC model. In the informed consent model, the role of the health practitioner is to provide TGD patients with information about risks, side effects, benefits, and possible consequences of undergoing GAC, and to obtain informed consent from the patient ( 80 ). Cavanaugh et al. argue that the informed consent model is more patient-centered and elevates the ethical principle of autonomy above non-maleficence, the principle often prioritized in the “gatekeeping” model ( 81 ). They write, “Through a discussion of risks and benefits of possible treatment options with the patient…clinicians work to assist patients in making decisions. This approach recognizes that patients are the only ones who are best positioned, in the context of their lived experience, to assess and judge beneficence (i.e., the potential improvement in their welfare that might be achieved), and it also affords prescribing clinicians a better and fuller sense of how a particular patient balances principles of non-maleficence and beneficence.” Authors note that mental health providers can be particularly helpful in situations where an individual desires additional mental health treatment, which some argue should remain optional, or when an individual’s capacity is in question ( 81 ). Additional ethical considerations include balancing the respect for the dignity of persons, responsible caring, integrity in relationships, and responsibility to society ( 82 ). Other authors argue for a more systematic approach to ethical issues, including consulting the literature and/or experts in the field of TGD mental health for support in making decisions around GAC ( 74 ).
Hale criticizes the WPATH SOC noting that these guidelines create a barrier between patient and mental health provider in establishing trust and a therapeutic relationship, overly pathologize TGD individuals, and unnecessarily impose financial costs to the TGD individual. As a “gatekeeper,” the mental health provider is placed in the position of either granting or denying GAC and must weigh the competing ethical principles of beneficence, non-maleficence, and autonomy. He argues that mental health providers are not surrogate decision makers and that framing requests for GAS as a “phenomenon of incapacity” is “reflective of the overall incapacitating effects of society at large toward the TGD community” ( 83 ). This reflects the broader approach to determining capacity utilized in other medical contexts, namely that patients have capacity until proven otherwise ( 84 ). Additionally, due to the gatekeeping dynamic between patient and clinician, many TGD patients may not mention concerns or fears surrounding GAS out of concern they will be denied services, thereby limiting the quality and utility of the informed consent discussion. Ashley proposes changes to the informed consent model, specifically that the informed consent process should include not only information about whether to go through with a procedure, but how to go through the procedure including relevant information about timeline, side effects, need for perioperative support, and treatment plan ( 85 ). Gruenweld argues for a bottom-up, TGD-led provision of GAC instead of focusing solely on alleviating gender dysphoria through a top-down, medical expert approach via such systems like the WPATH SOC ( 86 ).
MacKinnon et al. conducted an institutional ethnographic study of both TGD individuals undergoing mental health evaluations for GAC and mental health providers to better understand the process of conducting such evaluations ( 87 ). They found that providers cited three concerns with the evaluation: determining the authenticity of an individual’s TGD identity, determining if the individual has the capacity to consent to treatment, and determining the readiness of the individual to undergo treatment. TGD individuals cited concerns around presenting enough distress to be diagnosed with gender dysphoria (a SOC requirement) versus too much distress, and risk being diagnosed with an uncontrolled mental health condition therefore being ineligible for GAC. The authors conclude, “although they are designed to optimize and universalize care… psychosocial readiness assessments actually create a medically risky and arguably unethical situation in which trans people experiencing mental health issues have to decide what is more important – transitioning at the potential expense of care for their mental health or disclosing significant mental health issues at the expense of being rendered not ready to transition (which in turn may produce or exacerbate mental distress)” ( 87 ).
With regards to writing letters of readiness for GAS, authors comment on the differential treatment of TGD compared to cisgender individuals. Bouman argues that requiring two letters for gender-affirming orchiectomy or hysterectomy is unethical given that orchiectomy and hysterectomy for chronic scrotal pain and dysfunctional uterine bleeding, respectively, do not require any mental health evaluation. Requiring a second letter may cause delays in treatment, increase financial costs, and may be invasive to the patient who must undergo two detailed evaluations, while allowing for diffusion of responsibility for the mental health provider ( 88 ).
Changing standards
Starting in the 1950’s with the first successful gender affirming procedure in the US on Christine Jorgenson, TGD people in the US started seeking surgical treatment of what was then called TS. The medical community’s understanding of TGD people, their mental health, and the role of the mental health provider in their medical and surgical transition has progressed and evolved since this time. Prior to the first iteration of what would later be known as WPATH’s SOC, patients were mostly evaluated within a system that viewed gender and sexual minorities as deviants and thereby largely limited access to GAC. We can also see this reflected in the changes to DSM and ICD diagnostic criteria between 1980 and today which demonstrates a trend from pathologizing identity and conflating sexual and gender identity toward pathologizing the distress experienced due to the discordant identity, and finally removing the relevant diagnosis from the chapter of Mental and Behavioral Disorders altogether in the ICD and instead into a new chapter titled “conditions related to sexual health ( 89 ).” These changes have clearly yielded positive benefits for TGD individuals by reducing stigma and improving access to care, but significant problems remain. Requiring TGD people to have a diagnosis at all to obtain care, no matter the terminology used, is pathologizing. The practice of requiring a diagnosis continues to put mental health and other medical providers in the position of gatekeeping, continuing the vestigial historical focus on “confirming” a person’s gender identity, rather than trusting that TGD people understand their identities better than providers do. Version 8 of the SOC put a much heavier emphasis on shared decision making and informed consent, but continue to maintain the requirement of a diagnosis ( 79 ). Many insurance companies and other health care payers require the diagnosis to justify paying for GAC, but providers should continue to advocate for removing such labels as a gatekeeping mechanism for GAC.
With each version of the SOC, guidelines for GAC become more specific, with more explanation of the reasoning behind each recommendation; more flexible requirements, a broadening of the definition of mental health provider, and elimination of the requirement that at least one letter be written by a doctoral level provider. There has been a notable shift in the conceptualization of gender identity, away from a strict gender binary, with individuals transitioning fully from one end to the other, to gender identity and transition as a spectrum of experiences. Over time the SOC became more flexible by removing requirements for psychotherapy, narrowing requirement for the RLT to only those pursuing bottom surgery, eliminating requirements for a mental health evaluation prior to initiating GAH, and eliminating requirements for GAH prior to top surgery. Version 8 of the SOC was even more explicit about removing requirements for psychotherapy and psychometric testing prior to receiving GAC ( 79 ).
Despite these positive changes, those wishing to access GAC still face significant challenges. Access to providers knowledgeable about GAC remains limited, especially in more rural areas, therefore requiring evaluations and letters of readiness for GAC continues to significantly limit access to treatment. By requiring letters of readiness for GAC, adult TGD individuals are not afforded the same level of autonomy present in almost any other medical context, where capacity to provide informed consent is automatically established ( 84 ). The WPATH SOC continue to perpetuate differential treatment of TGD individuals by requiring extensive, and often invasive, evaluations for procedures that their cisgender peers are able to access without such evaluations ( 88 ). The WPATH guidelines apply a one-size-fits-all approach to an extremely heterogeneous community who have varying levels of needs based on a variety of factors including but not limited to age, socioeconomic status, race, natal sex, and geographic location ( 90 ). It should be noted, however, that the version 8 of the SOC does acknowledge that different patients may require evaluations of varying complexity based on the procedure they are requesting as well as a variety of psychosocial factors, although it remains vague about exactly what those different evaluations should entail ( 79 ). We propose that future work be directed toward three primary goals: conducting research to determine the utility of letters of readiness; to better understand factors that impact GAS outcomes; and to develop easily accessible and understandable guides to conducting readiness evaluations and writing letters. These aims will help to further our goals of advocating for this vastly underserved population by further removing barriers to life-saving GAC.
Changing ethics
Early iterations of the SOC were strict, placing the mental health provider within a gatekeeper role, tasked with distinguishing the “true transsexual” that would benefit from GAS from those who would not, which in effect elevated the ethical principal of non-maleficence above autonomy. This created a barrier to forming a therapeutic alliance between the patient and mental health provider as there was little motivation for patients to give any information outside of the expected gender narrative ( 50 , 65 ). Mistrust flowed both ways leading to longer and more involved evaluations then than what is required today, with many providers requiring patients to undergo extensive psychological testing and psychotherapy, provide extensive collateral, and undergo lengthy RLTs, with some focusing on a patient’s ability to “pass” within the desire gender role, before agreeing to write a letter ( 11 , 15 , 19 , 49 , 57 , 58 ).
As understanding around the experiences of TGD individuals has evolved over time, the emphasis has shifted from the reliance on non-maleficence toward elevating patient autonomy as the guiding principle of care. Evaluations within this informed consent model focus much more on the patient’s ability to understand the treatment, its aftercare, and its potential effect on their lives. Informed consent evaluations also shift focus toward other psychosocial factors that will contribute to successful surgical outcomes, for example, housing, transportation, a support system, and treatment of any underlying mental health symptoms. While there is still a lack of consistency in current evaluations and the SOC are enforced unevenly ( 77 ), the use of the informed consent model by some providers has reduced barriers for some patients. Many authors now agree that psychological or neuropsychological testing should not be used when evaluating for surgical readiness unless there is a concern about the patient’s ability to provide informed consent such as in the case of a neurocognitive or developmental disorder ( 58 ). Also important to note here is that while there is a general shift in the focus of the literature from that of gatekeeping toward one of informed consent, neither the informed consent model nor the WPATH SOC more broadly are evenly applied by providers, leading to continued barriers for many patients ( 77 , 78 ).
Within the literature, there is support for further reducing barriers to care by widening the definition of who can conduct evaluations, write letters, or facilitate the informed consent discussion for GAC. Recommending that the physician providing the GAC be the one to conduct the informed consent evaluation would bring GAC practices more in line with practices in place within the broader medical community. It is very rare for mental health providers to be the gatekeepers for medical or surgical procedures, except for transplant surgery, where mental health providers may have a clearer role given the prominence of substance use disorders and the very limited resource of organs. However, even within transplant psychiatry, a negative psychiatric evaluation would not necessarily preclude the patient from receiving the transplant, but instead may be used to guide a treatment plan to improve chances of a successful recovery post-operatively. We then should consider what it means to embrace patient autonomy as our guiding principle, especially with more than 40 years of evidence of the positive effects around GAC behind us. Future guidelines should focus on making sure that TGD individuals are good surgical candidates, not based on their gender identity, but instead on a more holistic understanding of the factors that lead to good and bad gender-affirming surgical outcomes, along the lines of those proposed by Mt. Sinai’s gender clinic for vaginoplasty ( 75 ). Additionally, the physicians providing the GAC should in most cases be the ones to obtain informed consent, while retaining the ability to request a mental health evaluation if specific concerns related to mental health arise. This would both allow mental health providers to adopt a supportive consultant role rather than that of gatekeeper, as well as provide more individualized rather than one-size-fits-all care to patients.
Version 8 of the SOC go a long way toward changing the ethical focus of evaluations toward one of shared decision making and informed consent by removing the requirement of a second letter and the requirement that the letter be written by a mental health provider. This will, in theory, lower barriers to care by allowing other providers (as long as they have at least a master’s degree) to write letters for surgery ( 79 ). In practice, however, this change is likely to only affect a small portion of the patient population. This is because, as noted in the section below in more detail, insurance companies already do not adhere closely to the SOC ( 91 ) and are unlikely to quickly adopt the new guidelines if at all. Further, it is possible that many surgeons will require that the letter of readiness be written by a mental health provider, especially if the patient has any previous mental health problems. While changes to SOC 8 are a step in the direction we propose in this manuscript, it is important to remember that the primary decision makers of who can access GAC in the US are insurance companies with surgeons, primary care providers, and mental health providers as secondary decision makers; this leaves patients with much less real-world autonomy than the SOC state they should have in the process. While insurance companies hold this effective decision-making power in all of US healthcare, it could be at least partially addressed by developing clear, evidence based guidelines for which patients might require a more in-depth evaluation in the first place. Screening out patients that have little or no mental health or social barriers to care would directly reduce those patients’ barriers to receiving GAC, while freeing up mental health and other providers to provide evaluation, resources, and support to those patients who will actually benefit from these services.
Letter writing
There are few published guides for writing letters of readiness for GAC. The WPATH SOC provide vague guidelines as to the information to include within the letter itself, which, in addition to a lack of consistency in implementation of the SOC, lead to a huge variety in current practices around letter writing and limit their usefulness to surgical providers ( 1 ). There is much debate within the literature about how many letters should be required and who should be able to write them. Guidelines from China, Turkey, and Iran recommend much stricter processes requiring input from a wider variety of specialists to comment on a patient’s readiness ( 59 – 61 ). Within the US, the few recent recommendations include having a frank discussion with patients about the gender dysphoria diagnosis and allowing them to have input into the content of the letter itself ( 65 , 66 , 70 , 71 , 75 ). The heterogeneity of current practices around letter writing demonstrates a reality in which many providers do not uniformly operate within the informed consent model, and do not even uniformly adhere to the SOC as written. This heterogeneity in practice by providers also extends to requirements by insurance companies in the US. The lack of clear guidelines about what should go into a letter, especially across different insurance providers, can lead to increased barriers to care due to insurance denials for incorrectly written letters. While direct data examining insurance denials for incorrectly written letters is not available, we can see this indirect effects in the fact that while 90% of insurance providers in the US provide coverage for GAC, only 5–10% of TGD patients had received bottom surgery even though about 50% of TGD patients have reported wanting it ( 91 ). Version 8 of the SOC reduce some of the letter writing requirements as discussed above, but they still do not give clear instructions on exactly how to write a letter of readiness or perform an evaluation ( 79 ). Given the lack of uniformity and limited benefit of such letters to surgical providers, these authors propose that future research be conducted into the need for letters of readiness for GAC, ways to ensure the content of such letters are evidence-based to improve outcomes of GAC, and improve education to providers by creating an easily accessible and free semi-structured interview with letter template.
Limitations
The reviewed articles included opinion manuscripts, published SOC, and proposed models for how to design and operate GAC clinics, however, this narrative review is limited by a lack of peer reviewed clinical trials that assess the evidence for the GAC practices described here. As a result, it is challenging to comment on the effectiveness of various interventions over time.
The WPATH SOC have evolved significantly over time with regards to their treatment of TGD individuals. Review of the literature shows a clear progression of practices from paternalistic gatekeeping toward increasing emphasis on patient autonomy and informed consent. Mental health evaluations, still required by SOC version eight are almost entirely unique as a requirement for GAS, apart from some bariatric and transplant surgeries. Individuals who wish to pursue GAC are required to get approval for treatments that their cisgender peers may pursue without such evaluations. While there may be some benefits from these evaluations in helping to optimize a patient socially, emotionally, and psychologically for GAC, the increased stigma and burden placed on patients by having a blanket requirement for such evaluations leads us to seriously question the readiness evaluation requirements in SOC version 8, despite a reduction in the requirements compared to previous SOC. This burden is made worse by limited access to providers knowledgeable and competent in conducting GAC evaluations, writing letters of readiness, and a lack of consistency in the application and interpretations of the SOC by both providers and insurance companies. Other barriers to care created by multiple letter requirements include the often-prohibitive cost of getting multiple evaluations and the delay in receiving their medical or surgical treatments due to extensive wait times to see a mental health provider. This barrier will in theory be ameliorated by updates to SOC in version 8, but multiple letters are likely to at least be required by insurance companies for some time. Overall, the shift from gate keeping to informed consent has been a net positive for patients by reducing barriers to care and improving patient autonomy, but the mental health evaluation is still an unnecessary barrier for many people. Further research is necessary to develop a standardized evaluation and letter template for providers to access, as well as further study into who can most benefit from an evaluation in the first place.
Data availability statement
The original contributions presented in this study are included in the article/ Supplementary material , further inquiries can be directed to the corresponding author.
Author contributions
TA and KK contributed to the conception and design of the study under the guidance of RL and AJ, reviewed and analyzed the literature, and wrote the manuscript. AW organized the literature search and wrote the “Methods” section. RL and AJ assisted in review and revision of the completed manuscript. All authors approved of the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.1006024/full#supplementary-material
Abbreviations
TGD, transgender and gender diverse; SRS, sex reassignment surgery; WPATH, World Professional Association for Transgender Health; SOC, standards of care; GAC, gender-affirming care; GAS, gender-affirming surgery; GAH, gender-affirming hormones; TS, transsexualism; TV, transvestism; HBIGDA, Harry Benjamin International Gender Dysphoria Association; RLT, Real life test; MMPI, Minnesota Multiphasic Personality Inventory; FTM, female to male; MTF, male to female; LGBTQI, lesbian, gay, bisexual, transgender, queer, intersex; DSM, diagnostic and statistical manual of mental disorders; ICD, international classification of diseases.
- ^ Gender affirming surgery has historically been referred to as sexual reassignment surgery (SRS).
- ^ Gender affirming care is an umbrella term referring to any medical care a TGD individual might pursue that affirms their gender identity, including primary care, mental health care, GAH or GAS.
- ^ The organization will be referred to as WPATH moving forward, even when referring to time periods before the name change.
1. Ettner R. Mental health evaluation for gender confirmation surgery. Clin Plast Surg. (2018) 45:307–11. doi: 10.1016/j.cps.2018.03.002
CrossRef Full Text | Google Scholar
2. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend. (2012) 13:165–232.
Google Scholar
3. Levine C. Social work with transsexuals. Soc Casew. (1978) 59:167–74. doi: 10.1177/104438947805900306
4. Meyer JK. Clinical variants among applicants for sex reassignment. Arch Sex Behav. (1974) 3:527–58. doi: 10.1007/BF01541136
5. Money J. Sex reassignment therapy in gender identity disorders. Int J Psychiatry Clin. (1971) 8:197–210.
6. Socarides CW. The desire for sexual transformation: a psychiatric evaluation of transsexualism. Am J Psychiatry. (1969) 125:1419–25. doi: 10.1176/ajp.125.10.1419
PubMed Abstract | CrossRef Full Text | Google Scholar
7. Benjamin H. Should surgery be performed on transsexuals? Am J Psychother. (1971) 25:74–82. doi: 10.1176/appi.psychotherapy.1971.25.1.74
8. Ell J. Indications for sex reassignment surgery. Arch Sex Behav. (1971) 1:153–61. doi: 10.1007/BF01541059
9. Kirkpatrick M, Freidmann CT. Treatment of requests for sex-change surgery with psychotherapy. Am J Psychiatry. (1976) 133:1194–6. doi: 10.1176/ajp.133.10.1194
10. Knorr NJ, Wolf SR, Meyer E. The transsexual’s request for surgery. J Nerv Mental Dis. (1968) 147:517–24. doi: 10.1097/00005053-196811000-00008
11. Newman LE, Stoller RJ. Nontranssexual men who seek sex reassignment. Am J Psychiatry. (1974) 131:437–41. doi: 10.1176/ajp.1974.131.4.437
12. Stone CB. Psychiatric screening for transsexual surgery. Psychosomatics. (1977) 18:25–7. doi: 10.1016/S0033-3182(77)71100-4
13. Weatherhead AD, Powers S, Rodgers D, Schumacher OP, Ballard LA, Hartwell SW. Sex reassignment program: the cleveland clinic foundation. Arch Sex Behav. (1978) 7:377–81. doi: 10.1007/BF01542046
14. Green R. Persons seeking sex change: psychiatric management of special problems. Am J Psychiatry. (1970) 126:1596–603. doi: 10.1176/ajp.126.11.1596
15. Meyer JK, Hoopes JE. The gender dysphoria syndromes. A position statement on so called “transsexualism”. Plastic Reconstr Surgery. (1974) 54:444–51. doi: 10.1097/00006534-197410000-00009
16. Walker M. Standards of care: the hormonal and surgical sex reassignment of gender dysphoric persons. Harry Benjamin International Gender Dysphonia Association. Arch Sex Behav. (1985) 14:79–90. doi: 10.1007/BF01541354
17. Abel GG. What to do when non transsexuals seek sex reassignment surgery. J Sex Marit Therapy. (1979) 5:374–6. doi: 10.1080/00926237908407082
18. Bernstein S. The psychological measure of man and woman. Ontar Psychol. (1979) 11:13–6.
19. Wise TN, Meyer JK. The border area between transvestism and gender dysphoria: transvestitic applicants for sex reassignment. Arch Sex Behav. (1980) 9:327–42. doi: 10.1007/BF01541358
20. Lothstein LM. The aging gender dysphoria (transsexual) patient. Arch Sex Behav. (1979) 8:431–44. doi: 10.1007/BF01541199
21. Levine SB. Psychiatric diagnosis of patients requesting sex reassignment surgery. J Sex Marital Ther. (1980) 6:164–73. doi: 10.1080/00926238008406081
22. Oppenheim G. The snowball effect of the ‘real-life test’ for sex reassignment. J Sex Educ Therapy. (1986) 12:12–4. doi: 10.1080/01614576.1986.11074872
23. Roberto LG. Issues in diagnosis and treatment of transsexualism. Arch Sex Behav. (1983) 12:445–73. doi: 10.1007/BF01542888
24. Pauly IB. Gender identity disorders: evaluation and treatment. J Sex Educ Therapy. (1990) 16:2–24. doi: 10.1080/01614576.1990.11074975
25. Levine SB, Lothstein L. Transsexualism or the gender dysphoria syndromes. J Sex Marital Ther. (1981) 7:85–113. doi: 10.1080/00926238108406096
26. Mate-Kole C, Freschi M. Psychiatric aspects of sex reassignment surgery. Br J Hosp Med. (1988) 39:153–5.
27. Cohen-Kettenis PT, Wålinder J. Sex reassignment surgery in Europe: a survey. Acta Psychiatr Scand. (1987) 75:176–82. doi: 10.1111/j.1600-0447.1987.tb02771.x
28. Edgerton MTJr., Langman MW, Schmidt JS, Sheppe WJr. Psychological considerations of gender reassignment surgery. Clin Plast Surg. (1982) 9:355–66. doi: 10.1016/S0094-1298(20)30325-4
29. Jones FD, Deeken MG, Eshelman SD. Sexual reassignment surgery and the military: case reports. Mil Med. (1984) 149:271–5. doi: 10.1093/milmed/149.5.271
30. Paul AW, Berger JC, Green R, Laub DR, Reynolds CL Jr., Wollman L. Harry Benjamin Standards of Care Version 4. (1990). Available online at: http://www.genderpsychology.org/transsexual/hbsoc_1990.html (accessed December 16, 2021).
31. de Cuypere G. Schizophrenia and symptomatic trans-sexualism: two case reports. Eur Psychiatry. (1993) 8:163–7. doi: 10.1017/S0924933800001954
32. Modestin J, Ebner G. Multiple personality disorder manifesting itself under the mask of transsexualism. Psychopathology. (1995) 28:317–21. doi: 10.1159/000284944
33. Bockting WO, Coleman E. A comprehensive approach to the treatment of gender dysphoria. J Psychol Hum Sex. (1992) 5:131–55. doi: 10.1300/J056v05n04_08
34. Ravenna AR. Italian standards of care for sex reassignment in gender identity disorder (DSM IV 302.85). Int J Transgend. (1998) 2:287.
35. Lothstein LM. Sex reassignment surgery: current concepts. Integr Psychiatry. (1992) 8:21–30.
36. Petersen ME, Dickey R. Surgical sex reassignment: a comparative survey of international centers. Arch Sex Behav. (1995) 24:135–56. doi: 10.1007/BF01541578
37. Levine SB, Brown GR, Coleman E, Cohen-Kettenis PT, Hage JJ, Maasdam JV, et al. The standards of care for gender identity disorders. J Psychol Hum Sex. (1999) 11:1–34. doi: 10.1300/J056v11n02_01
38. Levine SB. The newly revised standards of care for gender identity disorders. J Sex Educ Ther. (1999) 24:117–27. doi: 10.1080/01614576.1999.11074291
39. Ma JL. Social work practice with transsexuals in Hong Kong who apply for sex reassignment surgery. Soc Work Health Care. (1999) 29:85–103. doi: 10.1300/J010v29n02_05
40. Damodaran SS, Kennedy T. The monash gender dysphoria clinic: opportunities and challenges. Austral Psychiatry. (2000) 8:355–7. doi: 10.1046/j.1440-1665.2000.00278.x
41. Miach PP, Berah EF, Butcher JN, Rouse S. Utility of the MMPI-2 in assessing gender dysphoric patients. J Pers Assess. (2000) 75:268–79. doi: 10.1207/S15327752JPA7502_7
42. Meyer Iii W, Bockting WO, Cohen-Kettenis P, Coleman E, DiCeglie D, Devor H, et al. Harry benjamin international gender dysphoria association’s: the standards of care for gender identity disorders - sixth version. Int J Transg. (2001) 5:1548.
43. Levine SB. Harry benjamin international gender dysphoria association’s the standards of care for gender identity disorders. Int J Transg. (1998) 2:459–569.
PubMed Abstract | Google Scholar
44. De Cuypere G, Vercruysse HJr. Eligibility and readiness criteria for sex reassignment surgery: recommendations for revision of the WPATH Standards of Care. Int J Transg. (2009) 11:194–205. doi: 10.1080/15532730903383781
45. Bockting WO. Psychotherapy and the real-life experience: from gender dichotomy to gender diversity. Sexologies. (2008) 17:211–24. doi: 10.1016/j.sexol.2008.08.001
46. Coolhart D, Provancher N, Hager A, Wang M. Recommending transsexual clients for gender transition: a therapeutic tool for assessing readiness. J GLBT Family Stud. (2008) 4:301–24. doi: 10.1080/15504280802177466
47. de Roche R, Rauchfleisch U, Noelpp B, Dittmann V, Ermer A, Stieglitz RD, et al. A team approach to the indication for gender reassignment surgery in transsexuals resulting in long-term outcome improvement. Eur J Plastic Surgery. (2004) 27:24–8. doi: 10.1007/s00238-004-0596-z
48. Gorin-Lazard A. Gender identity disorder: what is the role of the psychiatrist? Sexologies. (2010) 19:S30–1.
49. Green R. Potholes in the interview road with gender dysphoric patients: contentious areas in clinical practice. Sexologies. (2008) 17:245–57. doi: 10.1016/j.sexol.2008.08.002
50. Lev AI. The ten tasks of the mental health provider: recommendations for revision of the World Professional Association for Transgender Health’s Standards of Care. Int J Transg. (2009) 11:74–99. doi: 10.1080/15532730903008032
51. Özgür Can I, Salaçin S. Legal aspects of gender reassignment surgery in Turkey: a case report. Ind J Gender Stud. (2011) 18:77–88. doi: 10.1177/097152151001800104
52. Rachlin K, Lev AI. Challenging cases for experienced therapists. J Gay Lesb Mental Health. (2011) 15:180–99. doi: 10.1080/19359705.2011.553783
53. Raj R. Towards a transpositive therapeutic model: developing clinical sensitivity and cultural competence in the effective support of transsexual and transgendered clients. Int J Transg. (2002) 6:1689.
54. Schechter LS. The surgeon’s relationship with the physician prescribing hormones and the mental health professional: review for version 7 of the World Professional Association for Transgender Health’s Standards of Care. Int J Transg. (2009) 11:222–5. doi: 10.1080/15532730903439468
55. Sohn M, Bosinski HA. Gender identity disorders: diagnostic and surgical aspects. J Sex Med. (2007) 4:1193–207; quiz 1208. doi: 10.1111/j.1743-6109.2007.00580.x
56. Tugnet N, Goddard JC, Vickery RM, Khoosal D, Terry TR. Current management of male-to-female gender identity disorder in the UK. Postgrad Med J. (2007) 83:638–42. doi: 10.1136/pgmj.2007.060533
57. Lehmann K, Leavey G. Accuracy of psychometric tools in the assessment of personality in adolescents and adults requesting gender-affirming treatments: a systematic review. Eur Psychiatry. (2019) 62:60–7.
58. Keo-Meier CL, Fitzgerald KM. Affirmative psychological testing and neurocognitive assessment with transgender adults. Psychiatr Clin North Am. (2017) 40:51–64. doi: 10.1016/j.psc.2016.10.011
59. Aghabikloo A, Bahrami M, Saberi SM, Emamhadi MA. Gender identity disorders in Iran; request for sex reassignment surgery. Int J Med Toxicol Foren Med. (2012) 2:128–34.
60. Liu N, Lu Z. Challenges in the diagnosis and treatment of transsexualism in contemporary China. Shang Arch Psychiatry. (2014) 26:49–50.
61. Zengin A. Sex for law, sex for psychiatry: pre-sex reassignment surgical psychotherapy in Turkey. Anthropologica. (2014) 56:55–68.
62. Bheem N, Gupta A, Reddy SJ, Mangal M, Gambhir SS, Sudha S. Current concepts in gender affirmation surgery. Curr Med Res Pract. (2017) 7:184–90. doi: 10.1016/j.cmrp.2017.09.009
63. Wylie K, Eden K, Watson E. Gender dysphoria: treatment and outcomes. Adv Psychiatr Treat. (2012) 18:12–6. doi: 10.1192/apt.bp.110.008557
64. Wylie K, Knudson G, Khan SI, Bonierbale M, Watanyusakul S, Baral S. Serving transgender people: clinical care considerations and service delivery models in transgender health. Lancet. (2016) 388:401–11. doi: 10.1016/S0140-6736(16)00682-6
65. Budge SL. Psychotherapists as gatekeepers: an evidence-based case study highlighting the role and process of letter writing for transgender clients. Psychotherapy (Chic). (2015) 52:287–97. doi: 10.1037/pst0000034
66. Budge SL, Dickey LM. Barriers, challenges, and decision-making in the letter writing process for gender transition. Psychiatr Clin North Am. (2017) 40:65–78. doi: 10.1016/j.psc.2016.10.001
67. Byne W, Karasic DH, Coleman E, Eyler AE, Kidd JD, Meyer-Bahlburg HFL, et al. Gender dysphoria in adults: an overview and primer for psychiatrists. Focus (United States). (2020) 18:336–50. doi: 10.1176/appi.focus.18304
68. Colebunders B, De Cuypere G, Monstrey S. New criteria for sex reassignment surgery: WPATH Standards of Care, version 7, revisited. Int J Transg. (2015) 16:222–33. doi: 10.1080/15532739.2015.1081086
69. Deutsch MB. Gender-affirming surgeries in the era of insurance coverage: developing a framework for psychosocial support and care navigation in the perioperative period. J Health Care Poor Underserved. (2016) 27:386–91. doi: 10.1353/hpu.2016.0092
70. Dominguez M, Shrestha A, Ahuja A, Ashley K. Treatment in transition: the rapidly evolving landscape of transgender and gender non-binary care. J Gay Lesb Mental Health. (2020) 24:112–34. doi: 10.1080/19359705.2019.1692387
71. Erasmus J. Monash gender clinic: an overview of the current model of care. Australas Psychiatry. (2020) 28:533–5. doi: 10.1177/1039856220917079
72. Fraser L, Knudson G. Past and future challenges associated with standards of care for gender transitioning clients. Psychiatr Clin North Am. (2017) 40:15–27. doi: 10.1016/j.psc.2016.10.012
73. Karasic DH, Fraser L. Multidisciplinary care and the standards of care for transgender and gender nonconforming individuals. Clin Plast Surg. (2018) 45:295–9. doi: 10.1016/j.cps.2018.03.016
74. LaSala MC, Goldblatt Hyatt ED. A bioethics approach to social work practice with transgender clients. J Gay Lesb Soc Serv. (2019) 31:501–20. doi: 10.1080/10538720.2019.1653804
75. Lichtenstein M, Stein L, Connolly E, Goldstein ZG, Martinson T, Tiersten L, et al. The mount sinai patient-centered preoperative criteria meant to optimize outcomes are less of a barrier to care than WPATH SOC 7 criteria before transgender-specific surgery. Transg Health. (2020) 5:166–72.
76. Levine SB. Informed consent for transgendered patients. J Sex Marital Ther. (2019) 45:218–29. doi: 10.1080/0092623X.2018.1518885
77. Holt NR, Hope DA, Mocarski R, Meyer H, King R, Woodruff N. The provider perspective on behavioral health care for transgender and gender nonconforming individuals in the Central Great Plains: a qualitative study of approaches and needs. Am J Orthopsych. (2020) 90:136–46. doi: 10.1037/ort0000406
78. Whitehead JC. Reluctant gatekeepers: “Trans-positive” practitioners and the social construction of sex and gender. J Gender Stud. (2012) 21:387–400. doi: 10.1080/09589236.2012.681181
79. Coleman E. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transg Health. (2022) 23(Suppl. 1):S1–259.
80. Schulz SL. The informed consent model of transgender care: an alternative to the diagnosis of gender dysphoria. J Human Psychol. (2018) 58:72–92. doi: 10.1177/0022167817745217
81. Cavanaugh T, Hopwood R, Lambert C. Informed consent in the medical care of transgender and gender-nonconforming patients. AMA J Ethics. (2016) 18:1147–55. doi: 10.1001/journalofethics.2016.18.11.sect1-1611
82. Toivonen KI, Dobson KS. Ethical issues in psychosocial assessment for sex reassignment surgery in Canada. Canad Psychol. (2017) 58:178–86. doi: 10.1037/cap0000087
83. Hale CJ. Ethical problems with the mental health evaluation standards of care for adult gender variant prospective patients. Perspect Biol Med. (2007) 50:491–505. doi: 10.1353/pbm.2007.0047
84. Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med. (2006) 357:7. doi: 10.1056/NEJMcp074045
85. Ashley F. Surgical informed consent and recognizing a perioperative duty to disclose in transgender health care. McGill J Law Health. (2019) 13:73–116.
86. Gruenewald AF. Re-assessing the triadic model of care for trans patients using a harm-reduction approach. Health Care Anal. (2020) 28:415–23. doi: 10.1007/s10728-020-00416-8
87. MacKinnon KR I don’t think they thought I was ready: how pre-transition assessments create care inequities for trans people with complex mental health in Canada. Int J Ment Health. (2020) 49:56–80. doi: 10.1080/00207411.2019.1711328
88. Bouman WP. Yes and yes again: are standards of care which require two referrals for genital reconstructive surgery ethical? Sex Relation Therapy. (2014) 29:377–89. doi: 10.1080/14681994.2014.954993
89. WHO. International Statistical Classification of Diseases and Related Health Problems. 11th Edn. Geneva: WHO (2020).
90. Ashmore R, Dip Coun GCE, Collier ME. “Driving to the edge of the cliff”: transgender mental health. J Psychiatr Ment Health Nurs. (2017) 24:2. doi: 10.1111/jpm.12390
91. Ngaage LM, Knighton BJ, Benzel CA, McGlone KL, Rada EM, Coon D, et al. Review of insurance coverage of gender-affirming genital surgery. Plastic Reconstr Surgery. (2020) 145:10. doi: 10.1097/PRS.0000000000006591
Keywords : gender-affirming surgery, standards of care, world professional association for transgender health, ethics, informed consent, transgender and gender diverse (TGD), mental health, scoping review
Citation: Amengual T, Kunstman K, Lloyd RB, Janssen A and Wescott AB (2022) Readiness assessments for gender-affirming surgical treatments: A systematic scoping review of historical practices and changing ethical considerations. Front. Psychiatry 13:1006024. doi: 10.3389/fpsyt.2022.1006024
Received: 28 July 2022; Accepted: 04 October 2022; Published: 20 October 2022.
Reviewed by:
Copyright © 2022 Amengual, Kunstman, Lloyd, Janssen and Wescott. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kaitlyn Kunstman, [email protected]
† These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC11396367

Gender Reassignment and the Role of the Laboratory in Monitoring Gender-Affirming Hormone Therapy
Transgender people experience distress due to gender incongruence (i.e., a discrepancy between their gender identity and sex assigned at birth). Gender-affirming hormone treatment (GAHT) is a part of gender reassignment treatment. The therapeutic goals of the treatment are to develop the physical characteristics of the affirmed gender as far as possible. Guidelines have been developed for GAHT, which recommend dosage as well as different formulations of oestrogen and testosterone for treatment. Questions arise about the metabolic side effects of hormone treatment. Establishing reference ranges for common analytes in transgender individuals remains a task for laboratory medicine. It has been suggested once GAHT is commenced, the reference ranges for affirmed gender are reported for red blood cells, haemoglobin and haematocrit. For transgender assigned-female-at-birth (AFAB) people, testosterone concentrations are recommended to be within the reference interval established for cisgender men and for transgender assigned-male-at-birth (AMAB) people, estradiol concentrations are within the reference range for cisgender women. Sex-specific reference ranges are available for certain laboratory tests, and these may be organ (e.g., heart)-specific. Transgender-specific reference ranges may be a requirement for such tests. Laboratories may need to make decisions on how to report other tests in the transgender population, e.g., eGFR. Interpretation of further tests (e.g., reproductive hormones) can be individualized depending on clinical information. Electronic medical record systems require fields for gender identity/biological sex at birth so that laboratory results can be flagged appropriately. In this review, we aim to summarise the current position of the role of the laboratory in the clinical care of the transgender individual. Prior to the review, we will summarise the genetics of sex determination, the aetiology of gender incongruence, and the recommendations for GAHT and monitoring for the transgender population.
1. Introduction
Gender incongruency (GI) occurs if the gender identity expressed by the individual and the biological sex of the individual are not consistent with each other. GI may be associated with distress, unease, depression, and low quality of life, which in most cases improve during gender-affirming hormonal treatment (GAHT). In many countries, GAHT is prescribed following an initial assessment by multidisciplinary teams. The teams offer initial psychological support prior to prescribing GAHT [ 1 ]. Recent guidelines describe the initial assessment and treatment of GI adolescents and adult individuals. In the scientific literature, transgender people are usually categorised as transgender assigned-male-at-birth (AMAB) people and transgender assigned-female-at-birth (AFAB) people. Guidelines further suggest standard monitoring plans for transgender AFAB and AMAB people treated with GAHT [ 2 , 3 , 4 , 5 ]. GAHT can affect laboratory-based diagnostic measurements. Results can be difficult to interpret for physicians due to the absence of published reference intervals.
In this review, we summarise the genetics of sex development, the possible origins of GI, GI treatment, and suggested monitoring following GAHT. This review has a special focus on laboratory interpretation of common tests following GAHT.
This narrative review covered several topics, and terms (e.g., gender identity, gender-affirming hormone treatment) were used to identify reviews or articles in PubMed, Medline, Google Scholar, and Web of Science over the past 10 years. From each article/review we extracted further references for studies included in this article.
3. Gender Development
Gender incongruence refers to the discordance between biological sex and gender identity, i.e., children or adults who do not identify with their biological sex. Multiple terms have been used for gender incongruence in the scientific literature, such as transsexualism, transgenderism, gender identity disorder, and gender dysphoria. Minor differences in nuances occur in each term, and the term GI is used as a common term in this review [ 6 ]. Prior to examining gender incongruency, this review will first summarise specific genetic signals that ensure sex development in humans. Sex development includes three distinct sequential stages: development of the bipotential gonad; sex determination, gonadal differentiation into testes and ovaries; and sex differentiation, the development of external and internal genitalia, or phenotypic sex. In humans, the bipotential gonads originate at 5 weeks of gestation from the gonadal ridge. The primordial germ cells, precursors to sperm and eggs, actively migrate across the embryo to reach the bipotential gonads [ 7 , 8 ]. Multiple essential genes are involved in bipotential gonadal development. Many of the genes were first reported in animal models. A number of genes (including transcription factors, PBX1, EMX2, and CBX2) [ 7 , 9 ] have been implicated in early gonadal development. Knowledge of factors involved in sex development came from animal models or from case studies in which the genetic or gonadal sex does not equal phenotypical sex, termed disorders of sex development (DSD). As an overall generalisation, factors influencing sex determination are transcriptional regulators, and factors responsible for sex differentiation are secreted hormones and their receptors.
In XY embryos, increasing levels of SF1 (an orphan nuclear receptor) and Wilms Tumour Suppression (WT1) gene, the gonadal development genes, activate the SRY gene expression on the Y chromosome. The SRY gene, the Y chromosomal testis determining gene, initiates the differentiation of Sertoli cells, which develop Leydig cells and germ cells. SRY regulates SOX9 gene expression, which promotes cell differentiation. Several other genes that participate in testicular development are described by Reyes et al. [ 7 ]. In males, sex differentiation begins at 7 weeks gestation. Sertoli cells express factors that differentiate and develop Sertoli cells, Leydig cells, and germ cells [ 10 ]. Anti-Müllerian hormone (AMH) is one of the earliest cell-specific proteins formed by the Sertoli cells. During male fetal development, AMH provokes the regression of the Müllerian duct, the rudiments of the fallopian tubes, the uterus, and the upper part of the vagina [ 11 ]. Human chorionic gonadotrophins (hCG) produced by the placenta in the first trimester of pregnancy and luteinizing hormone (LH) secreted by the pituitary in mid-gestation stimulate Leydig cells to induce testosterone production. Leydig cells respond to hCG/LH, which binds to the LH/hCG receptor and enhances the activity of enzymes that increase testosterone production. Testosterone binds to the androgen receptor in the Wolffian duct to form the male gonaducts. Testosterone is formed into dihydrotestosterone (DHT) by the enzyme 5a-reductase. DHT binds to the androgen receptor with higher affinity than testosterone and drives the differentiation of male external genitalia [ 12 ]. The testes are initially located close to the kidneys and, during development, migrate to the lower abdomen and then through the inguinal canal to the scrotum in a hormone-independent process [ 7 ].
In the absence of the SRY gene, the XX embryo expresses multiple pro-ovarian genes, which include FOXL2, WNT4, and RSPO1. These factors support ovarian differentiation and suppress testis development. FOXL2 maintains granulosa cell differentiation and supports folliculogenesis during development and adulthood. In the female, in the absence of testicular hormones, effective genetic regulation causes Wolffian duct regression and the development of fetal internal genitalia from Müllerian ducts as well as the growth of female external genitalia. The absence of AMH allows the Müllerian ducts to persist and form the fallopian tubes, uterus, and upper third of the vagina. AMH production begins after Müllerian duct differentiation by the counterpart of Sertoli cells, the granulosa cells. AMH is a folliculogenesis regulator and a biomarker of the primordial follicle reserve ( Figure 1 ) [ 7 ].

Germ cells migrate to the gonadal precursor to form the bipotential gonad by 5 weeks of gestation. At 6–8 weeks of gestation, SRY genes, expressed in somatic cells, drive testis determination, and in the absence of the SRY gene, FOXL2 and WNT4 drive ovarian determination. In the XY embryo, testosterone develops the Wolffian duct, and the anti-Müllerian hormone regresses the Müllerian duct. In the XX embryo, the Müllerian duct persists and the Woffian duct regresses. By 12 weeks of gestation, external genitalia are observed. Green shows the development of the male gonad, and purple shows the development of the female gonad.
One of the first hormonal changes in puberty is the pulsatile release of GnRH, which stimulates the release of LH and follicle-stimulating hormone (FSH). LH acts on the theca cells of the ovary to increase estrogen production and the Leydig cells of the testis to increase testosterone. In the female, FSH works on the ovarian follicle to convert oestrogen precursors to oestrogen and within the male Sertoli cells of the testes to form sperm. This results in the formation of the adult male genitalia and in the female development of the breasts. The adrenal gland contributes to the formation of secondary sexual characteristics, particularly the development of pubic and axillary hair, termed pubarche. Tanner staging is an objective classification system that documents the development of secondary sex characteristics in children during puberty [ 13 ] ( Table 1 ).
Tanner staging.
| Tanner Stage | Pubic Hair (Male and Female) | Breast Development (Females) | Testicular Volume (Males) |
|---|---|---|---|
| 1 | No hair | No glandular breast tissue palpable | Testicular volume < 4 mL or long axis < 2.5 cm |
| 2 | Downy hair | Breast bud palpable under the areola (1st pubertal sign in females) | 4–8 mL (or 2.5 to 3.3 cm long), 1st pubertal sign in males |
| 3 | Scant terminal hair | Breast tissue palpable outside areola; no areolar development | 9–12 mL (or 3.4 to 4.0 cm long) |
| 4 | Terminal hair that fills the entire triangle overlying the pubic region | Areola elevated above the contour of the breast, forming a “double scoop” appearance | 15–20 mL (or 4.1 to 4.5 cm long) |
| 5 | Terminal hair that extends beyond the inguinal crease onto the thigh | Areolar mound recedes into single breast contour with areolar hyperpigmentation, papillae development, and nipple protrusion | >20 mL (or >4.5 cm long) |
Genesis of Gender Incongruence
Despite the increase in gender health research, little is known about the timing of gender identity crystallization and the factors that contribute to the development of a gender identity that is not consistent with the sex determined by chromosomal or biological sex. Factors associated with gender incongruence and the scientific evidence in the literature require further exploration. With the advances in neuroimaging, one suggestion is that differences between male and female human brains may be trivial and population-specific [ 14 ]. Ruigrok et al. [ 15 ] report on regional brain differences between males and females, which are due to biological and environmental influences. Sex differences in gene expression have been reported in the brain, and sex hormones can further influence brain morphology [ 16 ]. Despite decades of research, sex differences in brain function are only partly understood. Gender expression is further likely to be a complex interplay of cultural and environmental factors (psychosocial factors) [ 17 ]. Gender identity may be an expression of a complex interplay between biological and environmental pressures.
Publications suggest that the biological origin of transgender identity is based on atypical sexual differentiation of the brain (transgender-specific brain phenotype) [ 18 ] or the hormone milieu during intrauterine development. Twin studies suggest a heritable component in transgender identity [ 19 ]. Foreman et al. [ 20 ] found a significant association between gender incongruence and SRD5A2 and STS alleles, as well as ERα and SULT2A1 genotypes in their cohort of transgender AMAB people. The authors suggest a polygenic basis for the transgender AMAB phenotype. Fernandez et al. [ 21 ] suggest that specific genotypic combinations of oestrogen and androgen receptors are associated with the transgender population.
Currently, there is no objective criterion for gender incongruence, and the literature suggests that GI has multiple aetiologies. Understanding the aetiology of GI would help clinicians decide which type of intervention would help in each individual case.
4. Guidelines for GAHT
4.1. adolescent gi.
One suggestion is that most children develop an ability to label their own and others’ genders between 18 and 24 months, and for the majority of adolescents, gender identity agrees with the assigned gender [ 22 ]. One review suggests that 1.2–2.7% of children and adolescents and 0.3–0.5% of adults identify as transgender [ 23 ]. There is ongoing debate about how children with GI should be treated and how their rights should be respected. The unease with which GI presents in prepubescent children varies; it is often transient and does not continue once puberty begins. Other children with GI exhibit a constant desire to be of the other gender and to match the physical and sexual characteristics of the desired gender. In addition, detransition—or reversing gender transition—can occur in adolescents and young adults [ 24 ].
Treatment follows an all-inclusive multidisciplinary clinical and psychosocial assessment of the GI individual, which includes both counselling and support. Treatment includes the following: (1) suppression of puberty by Gonadotropin-Releasing Hormone analogues (GnRHa, or puberty blockers); (2) administration of gender-affirming cross-sex hormones; and (3) gender-affirming surgery [ 25 ].
The European Academy of Pediatrics (EAP) states that ‘the child’s best interests are the primary consideration.’ The provision of puberty blockers and gender-affirming therapy in children under 18 years old is under critical review [ 24 ]. There has been controversy around the use of GnRHa to block puberty in peri-pubescent children. GnRHa treatment is reversible. GnRHa treatment gives the adolescent time to reconsider while reducing the development of secondary sexual characteristics. Delay may cause psychological and physical harm, though others have stated that there is no evidence for the latter. Studies suggest that the majority who started GnRHa treatment continued with gender-affirming treatment [ 26 , 27 ]. More studies are needed to describe the effect of transgender hormonal treatment on the skeleton and on brain development during adolescence. For the transgender population, while puberty suppression alone does not affect fertility outcomes, the addition of cross steroids does interfere with reproductive potential [ 28 ]. A recent review (Cass review) [ 29 ] of the Bell vs Tavistock High Court Case (UK) states that gender-affirming care is not backed by strong evidence on the natural history of GI and the efficacy of treatment alternatives. The following two critical questions need to be answered for pre-pubertal GI patients: (i) is the transition pathway beneficial for the individual? and (ii) is the pathway consistent with the ‘do no harm’ principle [ 29 ]? A suggestion is that the decision to treat adolescent GI made by a healthcare professional should be based on individual needs and scientific evidence [ 30 ]. It is expected that as experience with puberty suppression in transgender AFAB and AMAB children increases, there will be progress in understanding the best ways to provide endocrine care to transgender GI children, although further studies are needed to investigate adverse events.
4.2. Adult GI
In adult GI, the goals of hormone treatment are to reduce endogenous sex hormone levels and to replace hormones with sex hormone levels consistent with the individual’s gender identity. In transgender AFAB people, several androgen preparations have been used to achieve physiological levels consistent with the individual’s gender identity. Treatment for transgender AMAB people involves either oral or transdermal 17β-estradiol. Other adjunctive therapy is used to reduce endogenous testosterone levels. Progestins with anti-androgen activity, GnRH agonists, and spironolactone are some of the medications available [ 2 ]. A summary of recommendations from three different worldwide organisations’ published guidelines is provided in Table 2 [ 2 , 3 , 4 , 5 ]. It has been suggested that future guidelines might address the holistic healthcare of transpeople by increasing the evidence base, upgrading the quality of clinical practice guidelines, and increasing the number of health topics considered for the transgender population [ 31 ]. Individual goals for non-binary transgender AFAB and AMAB people can be complex, and individualised treatment is suggested. Ideal patient-centered outcomes for GAHT need to be defined for the non-binary population. However, adjusting hormonal treatment to attain some characteristics and not others can be a challenge [ 5 ]. Further research is needed to guide individualised hormonal treatment and clinical care in transgender AFAB/AMAB people.
Summary of guidelines on GAHT of transgender AFAB/AMAB persons.
| Guidelines | Society of Endocrinology | The World Professional Association for Transgender Health (WPATH) | Australian Professional Association for Trans Health (AusPATH) |
|---|---|---|---|
| Evaluation of prospective patients | Clinicians can add gender-affirming hormones after multidisciplinary team (MDT) team has confirmed the persistence of GI and sufficient mental capacity to give informed consent to treatment. The clinicians and mental health practitioners must be trained to diagnose GI. | Health care professionals have competencies in the assessment of transgender and gender diverse people wishing gender-related medical treatment and consider the role of social transition together with the individual. Liaise with professionals from different disciplines within the field of transgender health prior to gender-affirming treatment | |
| Treatment | Unless there is agreement among the parents, the adolescent, and medical practitioner regarding competence, diagnosis, and treatment, a Family Court order is required for access to gender-affirming puberty blockers, hormone treatment, and surgery for adolescents under 18 years old. | ||
| Puberty Induction Regimen | Transgender AMAB people: Increasing doses of oral or transdermal 17β-estradiol, until adult dosage is reached. In postpubertal transgender AMAB people, the dose is increased more rapidly. Transgender AFAB people: Increasing doses of testosterone until adult values are reached. In postpubertal males, the dose is increased more rapidly. Adult maintenance dose is to mimic physiological adult levels. | In eligible youth who have reached the early stages of puberty, the aim is to delay further pubertal progression with GnRHas until an appropriate time when GAHT can be introduced. In these cases, pubertal suppression is considered medically necessary. | |
| Treatment of transgender AFAB/AMAB people | Transgender AFAB people: treatment with both parenteral and transdermal testosterone Transgender AMAB people: Oral, transdermal or parenteral oestrogen. Antiandrogens: spironolactone, cyproterone acetate, GnRH agonist. Estradiol and testosterone are maintained at premenopausal female levels. Gender-affirming hormones are maintained at normal adult ranges | Transgender AFAB people: Masculinising treatment, usually with testosterone. Transgender AMAB people: treatment is usually with oestrogen and androgen-lowering medication. | Transgender AFAB people: masculinising treatment is with different formulations of testosterone Transgender AMAB people: Feminising treatment includes oestrogen and androgen blockers. It is usual to start with low doses and titrate upwards. |
| Monitoring | Periodic monitoring of hormone levels, metabolic parameters, and assessment of prostate gland, gonads, and uterus as well as bone density | Hormone levels are measured during gender-affirming treatment to ensure endogenous sex steroids are lowered and administered sex steroids are maintained at levels appropriate for the treatment goals of transgender people according to the Tanner stage. | For masculinising treatment, total testosterone levels are maintained at the lower male reference range, and for feminising treatment, estradiol is aimed to be within the female reference range. |
| Reference | [ ] | [ ] | [ , ] |
5. Laboratory Tests in Transgender AFAB/AMAB Individuals
Laboratory tests are affected by gender-affirming feminising or masculinising therapy or puberty-suppressing treatment. Laboratory tests are recommended by expert opinion or clinical practice guidelines [ 2 , 3 , 4 , 5 ]. Some tests are baseline tests prior to treatment, and others are used for treatment monitoring ( Table 3 and Table 4 ). In addition, transgender individuals may receive laboratory tests for other clinical indications. Laboratory tests likely affected by gender-affirming treatment are those that have sex-specific reference intervals, which may, additionally, be target-organ-based.
Baseline and follow-up protocols during suppression of puberty.
| Clinical Chemistry Tests | Other Tests | |
|---|---|---|
| LH, FSH, E2/T, 25(OH)D | Anthropometry: height, weight, blood pressure, Tanner stages | |
| Suggested Interval | 6–12 months | 3–6 months |
| Bone density using DXA | ||
| Suggested Interval | 1–2 years | |
| Reference | [ ] |
DXA, dual-energy X-ray absorptiometry; E2, estradiol; FSH, follicle stimulating hormone; LH, luteinizing hormone; T, testosterone; 25(OH)D, 25 hydroxy vitamin D. AusPATH guidelines suggest in addition, full blood count, liver and renal function tests, human chorionic gonadotropin (hCG) (if indicated or requested) vitamin D (if clinically indicated) and ECG, fasting glucose, lipids, HbA1c if cardiovascular risk factors are present. During follow-up protocol following induction of puberty, the following additional clinical chemistry tests are suggested: In transgender AFAB people: haemoglobin/haematocrit, lipids, testosterone, 25OH(D). In transgender AMAB people: prolactin, estradiol, 25OH (D).
Monitoring of transgender AFAB/AMAB individuals following gender-affirming treatment.
| Laboratory Tests | Other Tests | |
|---|---|---|
| Transgender AFAB people | T | Monitor for virilization |
| Suggested Interval | 3 monthly until levels within adult range | Every 3 months the first year and then one or two times per year |
| Haematocrit or haemoglobin | Screening for osteoporosis, cervical screening (if cervical tissue present), breast cancer screening as recommended | |
| Suggested Interval | 3 monthly for first year then one/two times per year | |
| Lipids at regular intervals | ||
| Transgender AFAM people | Serum T and estradiol | Feminisation |
| Suggested Interval | Every 3 months | Every 3 months the first year and then one or two times per year |
| If treated with spironolactone, electrolytes | Routine cancer screening and bone density | |
| Every 3 months the first year and then annually | ||
| Reference | [ ] |
Guidelines concur in that for transgender AMAB people, the suggested estradiol levels are aimed at the adult reference range with suppressed testosterone, and for transgender AFAB people, the suggested testosterone levels are within the adult reference range. Blood tests measure serum estradiol to monitor treatment but cannot monitor synthetic oestrogen use, and clinicians use serum estradiol to monitor treatment. Monitoring frequencies are similar in guidelines developed by WPATH and AusPATH [ 3 , 5 ]. Recommended ranges are used as a guide, and how the patient responds to treatment and associated risk factors that are present may guide GAHT (AusPATH). Other tests suggested are full blood count, electrolytes, renal and liver function tests, glucose, and lipids (AusPATH). Monitoring hormone concentrations as well as physiological changes can be used to optimise gender-affirming therapies and minimise adverse events.
5.1. Red Blood Cell Indices
Several prospective studies have investigated the effect of taking gender-affirming hormones on some analytes. Studies are not always powered to analyse subgroups with differences in medication and dosage and route of hormones or analyte measurement carried out on different analyser platforms. Humble et al. [ 32 ] report on transgender people treated with hormone therapy for at least 6 months. In transgender individuals receiving masculinising hormones, when compared to baseline levels, creatinine, red blood cells (RBC), haematocrit, haemoglobin, and testosterone were increased, similar to previous studies, and HDL decreased. In transgender individuals receiving feminising hormones, RBC, haematocrit, haemoglobin, testosterone, and creatinine levels were decreased when compared to baseline levels. SoRelle et al.’s [ 33 ] study of transgender individuals on hormone therapy for more than 6 months reported similar changes in RBC, haematocrit, haemoglobin and creatinine. In a small study of transgender AFAB people treated with testosterone, the increase in creatinine and RBC indices was stable for 5 years. In transgender AFAB off GAHT, haemoglobin decreased to the female range in 17 weeks. The study suggests that for RBC indices, reference ranges for a person’s affirmed gender apply once on stable GAHT [ 34 ] ( Table 5 ). Other studies have reported similar findings in RBC indices in transgender adolescents following GAHT. The authors did not report other significant laboratory abnormalities in transgender adolescents receiving GAHT [ 35 ].
Women and men have different levels of haemoglobin, which is probably the effect of oestrogens and androgens on erythropoiesis [ 36 ]. Greene et al. [ 37 ] reviewed haematology reference ranges for healthy transgender AMAB/AFAB individuals. The oestrogen-treated cohort had values similar to those of cisgender women, and the testosterone-treated cohort had values similar to those of cisgender men.
5.2. Renal Function
It has been suggested that changes in muscle mass in transgender individuals can contribute to changes in serum creatinine. This raises questions about the calculation of eGFR, which uses sex-based calculations and has implications for the estimation of kidney function. This has consequences for the administration of agents (e.g., intravenous contrast agents) that may impact kidney function, kidney transplant eligibility, or renal failure class allocation. One alternative is to use a more direct measure of GFR estimation such as 24 h urine creatinine clearance [ 38 ].
5.3. Liver Enzymes
Studies on the effect of GAHT on transaminases are conflicting. At least two studies report that changes in transaminases are not likely to be of clinical significance [ 33 , 39 ]. A further study suggests that the interpretation of transaminase and alkaline phosphatase levels are affected by gender-affirming testosterone therapy and recommends the use of affirmed gender reference intervals [ 40 ].
5.4. Lipids
Mixed results across multiple studies have been reported for total cholesterol, triglycerides (TG), LDL, and HDL in transgender individuals receiving GAHT [ 41 , 42 , 43 , 44 ].
5.5. Cardiac Biomarkers
In a further cross-sectional study, similar to healthy cisgender people, transgender AFAB people have higher concentrations of high-sensitivity troponin and lower concentrations of N-terminal pro-brain natriuretic peptide compared with transgender AMAB people [ 45 ]. In a small study with a single cut-off value of high-sensitivity troponin I and gender-specific reference ranges, 1.1% of patients would have been reclassified as acute myocardial infarction if the threshold value was based on the gender assigned at birth instead of their affirmed gender identity [ 46 ].
5.6. Reproductive Hormones
The distribution of endocrine results for estradiol, SHBG, prolactin, AMH, FSH, LH and testosterone for healthy transgender AMAB people differed from that for cisgender men and cisgender women. Treatment with spironolactone had a significant effect on the distribution levels of these hormones [ 47 ]. For transgender AFAB people, the distributions of testosterone and SHBG are similar to those of cisgender men. The distribution of results for estradiol, FSH, LH, progesterone, and prolactin differed from those for cisgender men and women, and AMH and dehydroepiandrosterone (DHEAS) differed from cisgender women [ 48 ]. It is suggested that reproductive hormone results should be interpreted in a manner specific to the transgender population.
5.7. Ferritin
Serum ferritin levels are influenced by dietary intake of iron, alcohol intake, chronic liver disease, and inflammatory disorders. Reference ranges for serum ferritin vary according to age and sex. Ferritin reference ranges are lower in premenopausal women compared to postmenopausal women. Female reference ranges are typically lower than those of men. There are no studies on the effect of GAHT on serum ferritin levels [ 49 ]. When a diagnosis of iron overload is suspected, and secondary causes are excluded, genetic studies for primary haemochromatosis may be indicated.
5.8. Prostate Specific Antigen
In transgender AMAB people, it is rare for the original prostate to be removed during orchiectomy. There is a risk of prostate cancer as long as the prostate remains in situ. Overall, transgender AMAB people showed a lower risk of prostate cancer compared to cisgender women [ 50 ], though it may not be as uncommon as previously supposed [ 51 ]. Reports suggest a more aggressive presentation than in cisgender men, with metastatic disease on presentation [ 52 ]. Little is known about prostate cancer screening in the transgender AMAB population. Future research avenues are the threshold values for prostate-specific antigen (PSA), which should be considered elevated for those on GAHT.
Impact of GAHT on laboratory tests.
| Laboratory Tests | Comments | Reference | ||
|---|---|---|---|---|
| Estradiol treatment | Testosterone treatment | Estradiol GAHT shifts haemoglobin, haematocrit to lower values in line with cisgender women’s reference intervals. Testosterone GAHTshifts reference intervals to higher levels in line with cisgender men’s reference intervals | [ ] | |
| RBC | Decrease | Increase | ||
| Hemoglobin | Decrease | Increase | ||
| Hematocrit | Decrease | Increase | ||
| Creatinine | Decrease | Increase | The most reno protective calculated GFR either male/female is suggested; 24h creatinine clearance if indicated | [ ] |
| High sensitivity troponin I | Report a reference range that would allow critical results to be appropriately followed; an approach of least harm to the patient is suggested | [ ] | ||
| Ferritin | Laboratories use dual reference ranges for cisgender individuals. Interpretation is based on clinical presentation (e.g., pregnancy) in combination with full blood count, liver function test, and markers of inflammation, e.g., CRP. Iron overload: If secondary causes excluded, investigation for primary haemochromatosis gene may be indicated | [ ] | ||
| Reproductive hormones | Testosterone, Estradiol | Following stabilisation of treatment with gender-affirming hormones, guidelines suggest treatment goals are physiological levels of the affirmed gender identity cisgender adults. The time of measurement of the hormone is dependent on the method of administration as well as formulation of the GAHT | [ ] | |
| Reproductive hormones | LH, FSH, AMH, and DHEAS are variable in a transgender population and are interpreted with clinical information | [ , ] | ||
| PSA | Data for reference ranges in transgender AMAB people and from screening for prostatic cancer is not available | [ ] | ||
| Renal function/liver function/lipid profile | Guidelines suggest monitoring of liver function/renal function and lipids during GAHT treatment. Sex-specific reference ranges are not ordinarily stated for the measurements | [ ] |
5.9. Laboratory Test Reference Intervals for Transgender Population
The reference interval for clinical laboratory tests is a requirement. They are necessary for the correct interpretation of tests and direct the care of the intended population. GAHT is medically indicated in transgender patients. To help clinically manage transgender patients, reference intervals have to take the effect of treatment on laboratory results into account. A summary of recent advances is given in Table 5 . Interpretation may still need to be individualized, especially for individuals on a nonstandard treatment regimen of GAHT, during the initial treatment prior to stabilization of therapy, or with co-existing medical conditions.
One principle [ 53 , 54 ] for the selection of different ranges for patients who have started therapy is the organs and physiological hormones influenced by GAHT. Individuals assigned as male at birth have larger organs, such as heart and muscle, following puberty. The reference range for troponin and creatinine may differ. GAHT can influence erythropoiesis, lipid parameters, and reproductive hormones.
6. Electronic Medical Record Systems (EMR)
From the laboratory perspective, the appropriate capture of gender information can have several implications, from test ordering to information gathering on the variation of analytes (i.e., to set up analyte reference ranges). The inclusion of gender identity in the EMR and, if the individual chooses to disclose this information, gender identity at birth can be relevant to individual treatment decisions and help in individual care [ 55 ]. In the USA, electronic medical records and laboratory information systems have the capacity to capture gender identity information. However, the introduction of the system into medical records can be challenging [ 56 ]. As a result of current limitations in the EMR systems, interactions with laboratory services can increase distress to transgender AFAB/AMAB individuals and affect their mental health.
7. GAHT and Other Laboratory Markers
7.1. risk of venous thromboembolism in amab people.
In cisgender females, treatment with oral contraceptives increased the risk of venous thromboembolism 2–4 fold, whereas the transdermal oestrogen formulation used for hormone replacement treatment does not appear to be associated with a significant venous thromboembolism risk. In a meta-analysis, Totaro et al. [ 57 ] suggest that the overall risk of venous thromboembolism in transgender AMAB people undergoing gender affirmation treatment was 2% but was negligible in those <37.5 years. Other studies confirm that the risk of venous thromboembolism during cross-hormone treatment is rare [ 58 ], though the risk may be modified by type, dose, route of oestrogen, duration of treatment, increasing age, high BMI, and smoking [ 59 ]. Prothrombotic variants, Factor V Leiden, prothrombin G2010A mutation, Protein S deficiency, Protein C deficiency, and antithrombin deficiency can increase the risk of hormone treatment. Previous venous thromboembolism and family history of genetic thrombophilia are considered reasons for thrombophilia screening prior to hormone treatment [ 2 ].
7.2. Hyperprolactinemia
Studies report hyperprolactinemia among transgender AMAB people taking both oestrogens and an antiandrogen [ 60 ]. The authors found too few cases of prolactinoma in transgender AMAB people on gender-affirming treatment to draw a conclusion. A threshold value for the definition of hyperprolactinemia in transgender AMAB people needs to be established.
7.3. Other Sex Hormone Dependent Tumours
There is little evidence about the effect of GAHT on the development of hormone-dependent cancer among transgender individuals. The evidence for most aspects of breast cancer in transgender AFAB people is inadequate [ 61 , 62 ]. However, one suggestion is that transgender AFAB people carrying a breast cancer mutation should be investigated further. Specific guidelines for breast cancer screening, intended for transgender AFAB people prior to mastectomy, mimic guidelines for cisgender women [ 61 ].
7.4. Bone Mineral Density
Sex steroids contribute to bone growth and peak bone mass accumulation during puberty and in adults contribute to the maintenance of bone structure. In transgender AFAB/AMAB adolescents, blocking puberty with gonadotropin-releasing hormone analogues decreases bone mineral density (BMD). Commencement of GAHT at least partially reverses the bone loss associated with pubertal suppression [ 63 ]. A review of studies suggests that GAHT in transgender AFAB people does not compromise bone microarchitecture. A summary of several systematic reviews indicates that reports on the effect of GAHT on the bone health of transgender AMAB are inconsistent [ 64 , 65 ]. Some data support the statement that pharmacological oestrogen can increase bone mineral density in transgender AMAB people [ 66 ].
The Endocrine Society clinical practice guidelines for gender-incongruent individuals suggest checking bone density in patients who have risk factors for osteoporosis [ 2 ], such as hyperparathyroidism or steroid use.
It is not certain as to which database to use for the interpretation of BMD although it is possible to use both male and female databases for reference in the DXA report. The official position of the International Society for Clinical Densitometry (ISCD) is that transgender individuals should use the reference data of the gender conforming to the individual’s gender identity. If the referring provider or the individual requests, a set of male or female Z-scores can be provided to calculate the Z-score against male and female reference data, respectively [ 67 , 68 ]. Algorithms used to predict fracture risk, such as FRAX, use data derived from cisgender cohorts. These algorithms may not be able to correctly calculate fracture risk in the transgender population.
8. GAHT, Vascular Health and Cardiovascular Disease, and Impact of Aging in Transgender Adults
In a systematic review, van Leerdam et al. [ 69 ] suggest that GAHT reduces gender dysphoria and body dissatisfaction with a subsequent improvement in psychological well-being and quality of life, though they suggest further studies are indicated. Aggressive modification of cardiovascular risk factors, e.g., optimisation of diabetes, weight, and lipid profile, may be recommended in transgender patients under treatment with GAHT. Case studies suggest thrombotic risk assessment is indicated in at-risk patients [ 70 ]. The effects of GAHT on cardiovascular effects are difficult to assess due to the limited number of studies and contradictory outcomes [ 71 ]. There is a lack of research on treatment with GAHT during menopause and older age. Shared decision-making for treatment with GAHT in older age to minimise potential adverse effects has been suggested [ 72 ].
9. Conclusions
A cascade of complex genetic interactions leads to the formation of male and female phenotypes [ 73 ]. The disparity between the sex assigned at birth and the experienced gender or gender identity in GI individuals can cause distress. GI involves multiple aetiologies, and studies suggest the concept that genetic, endocrine, and neuroanatomic as well as a complex interplay of environmental and cultural factors, contribute to GI [ 2 ]. In some GI individuals, this distress is so great that they seek medical treatment to cause changes which match their gender identity. Guidelines suggest puberty suppression therapy for transgender AFAB/AMAB adolescents and testosterone and estradiol treatment for young adults who require transition treatment. Several guidelines suggest blood examinations and clinical evaluations should be performed at baseline and following GAHT treatment. A number of the recommended laboratory tests have been shown to be affected by GAHT. Laboratory tests impacted by GAHT are predominantly tests that have sex-specific reference intervals or are based on target organs affected by the biological sex of the individual.
10. Future Directions
A future informatics challenge is to use EMR systems to provide reference intervals and interpretative comments for laboratory tests ordered for transgender AFAB/AMAB individuals receiving GAHT. A study to create a comprehensive data set that can be used for a wide range of purposes and to address current controversies and improve care for GI individuals is a further task in this subject [ 74 ].
Funding Statement
The research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
Understanding the Impact of Gender Confirmation Surgery on Mental Health
Heather Lyons, Ph.D.
August 26, 2021
Transgender people with access to gender confirmation surgery experience better mental health outcomes and improved quality of life, according to a new study .
The report, published in April 2021 by JAMA Surgery, found that gender-diverse and transgender patients who underwent gender-affirming surgery reported lower psychological distress levels, suicide risk, and substance use. The authors also found that transgender people who had not yet received gender confirmation surgery were nearly twice as likely to experience severe psychological distress, suicidal thoughts , and substance abuse .
Depending on an individual’s sex assigned at birth, several surgical options are available, including mastectomy, orchiectomy, and hysterectomy. While there are many different types of confirmation surgery, not everyone pursues every option—or any. From overcoming gender dysphoria to improving transgender health outcomes, here’s how gender confirmation surgery and other gender-affirming interventions impact mental health.

What is gender confirmation surgery?
Gender confirmation surgeries aim to give transgender individuals the physical characteristics and functional abilities of the gender they identify with, according to the American Society of Plastic Surgeons . Gender confirmation surgeries are performed by a multi-specialty team, which includes board-certified plastic surgeons.
Some surgical procedures that can help transgender women (MTF) and transgender men (FTM) journey include facial surgery, chest surgery, and genital surgery, such as:
- Facial feminization surgery , which transforms masculine facial features into a more feminine appearance.
- Facial masculinization surgery , which transforms feminine facial features into a more masculine appearance.
- Transfeminine top surgery , which enhances the breasts to provide a more feminine appearance.
- Transmasculine top surgery , which removes breast tissue (mastectomy) to provide a more masculine appearance.
- Transfeminine bottom surgery , which reconstructs male genitalia into that of a female (vaginoplasty).
- Transmasculine bottom surgery , which reconstructs female genitalia into that of a male (phalloplasty).
Find the Right Therapist to Explore Gender Confirmation Surgery
Gender-affirming interventions and mental health.
When transgender people undergo sex reassignment surgery and other gender-affirming interventions, the beneficial effects on their mental health are long-lasting. According to the Standards of Care published by the World Professional Association for Transgender Health (WPATH), gender reassignment surgery is often “the last and most considered step in the treatment process for gender dysphoria.”
In one Swedish study , researchers found that people with gender dysphoria—when biological gender doesn’t match gender identity, resulting in distress—were six times more likely than the general population to visit a mental health professional for mental health concerns. However, transgender people who had undergone gender-affirming surgery experienced less anxiety, depression, and suicidal behavior than those who did not.
In addition to gender affirmation surgery, other gender-affirming interventions have also been shown to improve mental health among the transgender community. According to a 2020 study by the National Institutes of Health, changing one’s legal name and gender marker on government documents is also associated with better mental health outcome measures.
Barriers to Accessing Gender Confirmation Surgery
Treatment for gender dysphoria, including gender-affirmation surgery and hormone therapy, are recognized as medically necessary by the American Medical Association and WPATH . However, in a 2015 National Center for Transgender Equality survey , more than half of transgender people reported being denied insurance coverage for gender confirmation surgery. Unfortunately, only 24 states currently require private insurance companies to cover this type of surgery.
Consequently, continuing research on the impact of gender confirmation surgery on transgender health is key to increasing transgender individuals’ access to such surgery. Hopefully, this research will help raise awareness of the efficacy of gender-affirming surgery.
If you’re experiencing mental health concerns or considering gender affirmation (sometimes still referred to as gender reassignment) surgery, reach out to a therapist through WithTherapy . We’ll connect you to someone you feel comfortable with, regardless of your personal preferences and requirements. One of the compassionate, inclusive therapists on the WithTherapy platform will help you explore your gender expression, understand your options, and live life as your true self.

You’re at the heart of a reimagined therapist search platform.
Explore related articles.

How to Make Friends as an Adult: Overcoming Challenges and Building Connections
June 15, 2024

What Gaslighting Is and Isn’t: A Guide
June 2, 2024
Help! I Can’t Find a Therapist: A User’s Guide to Finding the Right Therapist
April 14, 2024
Find Your Healthier WithTherapy

Psychological Evaluations For Gender Reassignment
Sex reassignment surgery.
Sex reassignment surgery is when transgender person's physical appearance and function of their existing sexual characteristics are altered to resemble that of their identified gender. Mental Health care is required before undergoing elective sex reassignment surgery.
Our experienced mental health specialists assist trans-men and trans-women in dealing with their emotions and the transition between genders and sexes. We provide supportive and sensitive care regardless of sexual orientation, gender identity, race, religion, or socio-economic status.
Verification of Readiness for Surgery
We properly assess our clients mental state and evaluate their readiness for hormone therapy and transgender surgery.Our professional staff is able to provide the required Verification of Readiness for surgery by two experts in the field of Psycholology.
Schedule an Appointment
Attorney referral form.
Este sitio está protegido por reCAPTCHA y aplican las Política de privacidad y los Términos de servicio de Google.
Nogales Psychological Counseling
6230 Wilshire Blvd., Suite 540 Los Angeles CA 90048-5126
(714) 525-8509 or (213) 384-7660
Copyright © 2018 Nogales Psychological Counseling - All Rights Reserved.
Con tecnología de GoDaddy
- Make a Payment
You are using an outdated browser. Please upgrade your browser to improve your experience.
Indiana Judge Rules Sicko Who Murdered His 11-Month-Old Stepdaughter Must Be Granted Transgender Surgery

Autumn Cordellionè
A judge in Indiana has ruled that a prisoner convicted of murdering his 11-month-old stepdaughter back in 2001 must be granted transgender surgery.
The case was originally filed by the American Civil Liberties Union, which argued that the rights of transgender inmate, Jonathan C. Richardson, also known as Autumn Cordellionè, were being violated by an Indiana law prohibiting the Department of Corrections from using taxpayer dollars to fund sex reassignment surgeries for inmates.
ACLU Files Lawsuit Against Indiana For Banning Inmate Sex-Changes — on Behalf of Man Who Murdered 11-Month-Old Stepdaughter
“Accordingly, at this point gender-affirming surgery is necessary so that her physical identity can be aligned with her gender identity and so her gender dysphoria can be ameliorated,” the lawsuit states.
“She believes that the only remedy for her persistent gender dysphoria, and the serious harm it causes her, is to receive gender-affirming surgery, specifically an orchiectomy and vaginoplasty,” it said.
Judge Richard Young, who was appointed to the court by Bill Clinton back in 1998, agreed with this assessment.
“Specifically, Ms. Cordellioné has shown that her gender dysphoria is a serious medical need, and that, despite other treatments Defendant has provided her to treat her gender dysphoria, she requires gender-affirming surgery to prevent a risk of serious bodily and psychological harm,” he wrote in his ruling.
As a result, the Department of Corrections must now take “all reasonable actions” to grant the murderer his desired sex change.
Posting on the X platform, Indiana Attorney General Todd Rokita confirmed he would be appealing the decision and pointed out that taxpayers would rather not fund such an indulgent request.
An Indiana inmate convicted of murder wants taxpayers to fund their gender altering surgery. Last night, on WEHT in Evansville, they aired a story and my interview. My comment? Voters and the Legislature do not want their tax dollars spent on these prisoner gender surgeries.…
— Todd Rokita (@ToddRokitaIN) September 19, 2024
According to court documents , Richardson was sentenced to 55 years in prison after being convicted of strangling his wife’s 11-month-year old daughter to death while she was at work. Detectives who interviewed him at the time said he “unemotional” when questioned about his dastardly crime.
The post Indiana Judge Rules Sicko Who Murdered His 11-Month-Old Stepdaughter Must Be Granted Transgender Surgery appeared first on The Gateway Pundit .

WOW! Barack Obama’s Former Canadian Ambassador Reveals Zoom Call With Hollywood Celebrities and Social...

IMAGES
VIDEO
COMMENTS
A comprehensive assessment for gender dysphoria covers a lot of territory. It includes a gender assessment and a solid basic assessment as well as identifying strengths and resources. Most agencies and clinicians have their own clinical assessment tools. A current Mental Status Exam (MSE) is important for informed consent.
The only other manuscripts that include a mention of psychological testing describe processes in Iran and China, both of which require extensive psychological testing prior to approval for ... Ethical issues in psychosocial assessment for sex reassignment surgery in Canada. Canad Psychol. (2017) 58:178-86. 10.1037/cap0000087 ...
Gender-affirmation care plays an important role in tackling gender dysphoria. 5, 8-10 Gender-affirmation surgeries (GAS) aim to align the patients' appearance with their gender identity and help achieve personal comfort with one-self, which will help decrease psychological distress. 5,10 These interventions should be addressed by a ...
In short, psychological assessment and counseling can be instruments of success in gender transition rather than impediments to the exercise of choice. Still, a skeptic might respond that assessment and counseling are not equally valuable or necessary to all people. If so, these processes should be optional, not obligatory.
Mental Health Evaluation for Gender Confirmation Surgery Clin Plast Surg. 2018 Jul;45(3):307-311. doi: 10.1016/j.cps.2018.03.002. Epub 2018 Apr 19. Author Randi Ettner 1 Affiliation 1 New Health Foundation Worldwide, 1214 Lake Street, Evanston, IL 60201, USA. Electronic address: [email protected]. ... Sex Reassignment Surgery / psychology*
LGBTQ Health Gender Affirmation. Preparing for your gender affirmation surgery can be daunting. To help provide some guidance for those considering gender affirmation procedures, our team from the Johns Hopkins Center for Transgender and Gender Expansive Health (JHCTGEH) answered some questions about what to expect before and after your surgery.
Gender Incongruence (capitalized): A diagnostic category (analogous to Gender Dysphoria in DSM-5) proposed for ICD-11. Gender variance: any variation of experienced or expressed gender from socially ascribed norms within the gender binary. Genderqueer: an identity label used by some individuals whose experienced and/or ex-pressed gender does ...
There is no hormonal therapy requirement for mastectomy only. 5. Member has lived as their reassigned gender full time for 12 months or more. 6. Member's medical and mental health providers document that there are no contraindications for the planned surgery and agree with the plan. 7.
Finn, S. E. (2016). Using therapeutic assessment in psychological assessments required for sex reassignment surgery. In V. M. Brabender & J. L. Mihura (Eds.), Handbook of gender and sexuality in psychological assessment (pp. 511-533). Routledge/Taylor & Francis Group. Abstract
Mental health evaluation: A mental health evaluation is required to look for any mental health concerns that could influence an individual's mental state, and to assess a person's readiness to undergo the physical and emotional stresses of the transition.; Clear and consistent documentation of gender dysphoria; A "real life" test: The individual must take on the role of their gender in ...
With the exception of bariatric surgery and live donor organ transplantation, sex reassignment surgery (SRS) is the only category of surgeries for which a mental health assessment is routinely done as part of the standard of care. ... Presurgical Psychological Evaluation: Risk Factor Identification and Mitigation. Journal of Clinical Psychology ...
Deep Eddy Psychotherapy offers psychological evaluations for gender affirmative surgery candidacy for our clients (ages 18 and up). Our clinicians are dedicated to helping the transgender, non-binary, genderqueer, and gender-expansive community by providing this evaluation service along with individual, group, and couples therapy.
The management of gender dysphoria consists of a combination of psychotherapy, hormonal therapy, and surgery. Psychiatric evaluation is essential before gender reassignment surgical procedures are ...
Article: 0154 Topic: W08 - Workshop 09: Lesbian, gay, bisexual, and transgender affirmative psychiatry: The next generation Psychiatric Assessment of Transgender Adults for Sex Reassignment Surgery C. McIntosh1 1Gender Identity Clinic, Centre for Addiction and Mental Health, Toronto, Canada While pre-surgical assessments by an internist are relatively common, those by psychiatrists are much ...
For people undergoing gender transition, psychological monitoring is organized through all phases of medical treatment. ... were asked a series of open-ended questions related to the decision-making process regarding transition and sex reassignment surgery, their experience of discrimination due to gender dysphoria, social support during the ...
Transgender, gender nonbinary and gender diverse clients may present for psychological assessment for the same reasons as cisgender clients. These assessments may be necessary in order to obtain appropriate supports or treatment. However, in the case of clients who do not identify as cisgender, use of gender in the scoring procedure may harm ...
Surgery and hormonal therapy are increasingly common treatments for gender dysphoria, but the prejudice and discrimination transgender individuals face post-transition can cause significant psychological distress, says Marci Bowers, MD, a surgeon who performs gender reassignment surgery in Trinidad, Colo., and is herself transgender.
The only other manuscripts that include a mention of psychological testing describe processes in Iran and China, both of which require extensive psychological testing prior ... Dobson KS. Ethical issues in psychosocial assessment for sex reassignment surgery in Canada. Canad Psychol. (2017) 58:178-86. doi: 10.1037/cap0000087. CrossRef Full ...
GI may be associated with distress, unease, depression, and low quality of life, which in most cases improve during gender-affirming hormonal treatment (GAHT). In many countries, GAHT is prescribed following an initial assessment by multidisciplinary teams. The teams offer initial psychological support prior to prescribing GAHT . Recent ...
Gender-Affirming Interventions and Mental Health. When transgender people undergo sex reassignment surgery and other gender-affirming interventions, the beneficial effects on their mental health are long-lasting. According to the Standards of Care published by the World Professional Association for Transgender Health (WPATH), gender reassignment surgery is often "the last and most considered ...
Psychological Evaluations For Gender Reassignment. Sex Reassignment Surgery. Sex reassignment surgery is when transgender person's physical appearance and function of their existing sexual characteristics are altered to resemble that of their identified gender. Mental Health care is required before undergoing elective sex reassignment surgery.
Autumn Cordellionè. A judge in Indiana has ruled that a prisoner convicted of murdering his 11-month-old stepdaughter back in 2001 must be granted transgender surgery.. The case was originally filed by the American Civil Liberties Union, which argued that the rights of transgender inmate, Jonathan C. Richardson, also known as Autumn Cordellionè, were being violated by an Indiana law ...