- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
- Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring

Consumer Health Information, Essay Example
Pages: 3
Words: 690
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
Introduction
Consumer health literacy is an important component of modern healthcare practice because it enables patients to be proactive in understanding the issues that impact their health, as well as in recognizing how to best overcome personal health concerns that influence their own perspectives regarding health. It is important to recognize that many consumers who are tech-savvy may have a tendency to self-diagnose using various websites; however, this does not replace truthful and unbiased healthcare information comprised of the facts that is available from reputable sources. It is necessary for consumers to properly decipher and interpret health information effectively in order to identify areas where health information is lacking or is inappropriate in meeting patient needs.
Interpreting health information in the appropriate manner requires a high level of focus and an understanding of the different expectations that consumers have regarding information that is easily accessible on the web and in other locations (Goldberg et.al, 2011). In this context, consumers must be able to obtain health information that is accurate and timely, rather than to rely on information that is untruthful and outdated (Goldberg et.al, 2011). Health information must be properly evaluated and provide useful insight regarding health issues of concern that impact many consumers (Goldberg et.al, 2011). Consumers must also be receptive and willing to learn about health issues through skill development and literacy strategies to improve confidence in health information and in the experts who provide this information to the masses (Car et.al, 2011). These practices require expert knowledge and guidance in advancing health and in supporting preventative and proactive strategies to protect health through improved knowledge and awareness (Car et.al, 2011).
Patients must be adequately prepared to improve their health literacy and to seek out information freely regarding health topics; however, this practice must also take other factors into consideration, such as preventative education that is used to address primary health concerns (Car et.al, 2011). Health literacy is a lifelong phenomenon that requires an effective understanding of the different elements that attract consumers to this practice, such as information that is truthful yet relatively easy to understand (Schnitzer et.al, 2011). These practices require individuals to take the steps that are required to ensure they are health literate and possess knowledge of a variety of health topics from a honest and truthful perspective so that they are able to better understand their own issues more effectively (Schnitzer et.al, 2011). At the same time, it is important for consumers to develop an effective understanding of their needs and to be proactive in recognizing that health literacy is a critical factor in their own growth and maturity (Sheridan et.al, 2011). These factors require experts to educate others regarding health literacy and to be cognizant of the issues that may emerge that impact health knowledge in different ways (Sheridan et.al, 2011).
Consumers must be able to receive and comprehend health information in an effective manner, as this provides a greater sense of accomplishment and an understanding of the different elements that impact their own wellbeing. Health literacy is a lifelong process that requires health knowledge to be accurate and appropriate for consumers so that they are able to identify specific factors related to their own health. This practice also requires a long-term commitment to educating individuals across different age groups so that they are able to actively participate in making decisions regarding their own health that will have a positive impact on their lives throughout the life span.
Car, J., Lang, B., Colledge, A., Ung, C., & Majeed, A. (2011). Interventions for enhancing consumers’ online health literacy. Cochrane Database Syst Rev , 6 .
Goldberg, L., Lide, B., Lowry, S., Massett, H. A., O’Connell, T., Preece, J., … & Shneiderman, (2011). Usability and accessibility in consumer health informatics: current trends and future challenges. American journal of preventive medicine , 40 (5), S187-S197.
Schnitzer, A. E., Rosenzweig, M., & Harris, B. (2011). Health literacy: A survey of the issues and solutions. Journal of Consumer Health on the Internet , 15 (2), 164-179.
Sheridan, S. L., Halpern, D. J., Viera, A. J., Berkman, N. D., Donahue, K. E., & Crotty, K. (2011). Interventions for individuals with low health literacy: a systematic review. Journal of Health Communication , 16 (sup3), 30-54.
Stuck with your Essay?
Get in touch with one of our experts for instant help!
Death of a Sales Man, Movie Review Example
Tips for Online Students, Research Paper Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Relatives, essay example.
Pages: 1
Words: 364
Voting as a Civic Responsibility, Essay Example
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Pages: 2
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Pages: 4
Words: 999
- Search Menu
- Sign in through your institution
- Advance articles
- Author Interviews
- Research Curations
- Author Guidelines
- Open Access
- Submission Site
- Why Submit?
- About Journal of Consumer Research
- Editorial Board
- Advertising and Corporate Services
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, self-drivers, social drivers, solution drivers, service-provider drivers, societal/situational drivers, future directions, author notes.
- < Previous
The 5S's of Consumer Health: A Framework and Curation of JCR Articles on Health and Medical Decision-Making
- Article contents
- Figures & tables
- Supplementary Data
Szu-chi Huang, Leonard Lee, The 5S's of Consumer Health: A Framework and Curation of JCR Articles on Health and Medical Decision-Making, Journal of Consumer Research , Volume 49, Issue 5, February 2023, Pages 926–939, https://doi.org/10.1093/jcr/ucac051
- Permissions Icon Permissions
Every day, consumers make decisions that have both direct and indirect impact on their health. The COVID-19 pandemic, and the long-term physical and mental complications that have ensued, underscores the importance of developing a holistic understanding of drivers of consumers’ health and medical decisions. Without this comprehensive approach, health appeals or interventions are destined to fall short of achieving positive and long-lasting outcomes. Beyond the pandemic, medical and biotechnological advancements can have greater impact on global lifespan when the behavioral sciences offer a critical, complementary lens to enhance the understanding, adoption, and implementation of these new technologies. By illuminating how consumers think, feel, choose, and behave in this multi-faceted decision environment, consumer researchers are well equipped to contribute to the ongoing quest to improve population health.
In this curation, we review many articles published in the Journal of Consumer Research ( JCR ) that focus on a spectrum of health and medical decisions, while highlighting five ( Bolton et al. 2008 ; Botti, Orfali, and Iyengar 2009 ; Briley, Rudd, and Aaker 2017 ; Longoni, Bonezzi, and Morewedge 2019 ; Moorman and Matulich 1993 ). We define consumer health and medical decisions broadly, as those relating to the prevention (e.g., minimizing stress, moderating alcohol consumption), diagnosis (e.g., utilizing health professionals for checkups), remedy and improvement (e.g., taking medication to cure an infection), and maintenance (e.g., monitoring dietary intake) of consumer health ( Moorman and Matulich 1993 ). We build on these articles to propose a new 5S ( S elf, S ocial, S olution, S ervice provider, S ocietal/ S ituational) framework to explain holistic drivers underlying consumers’ health and medical decisions ( figure 1 ). We hope that researchers will find this conceptual framework useful in structuring the existing consumer research literature on health. Furthermore, the 5S framework provides a clear set of four key directions that future researchers will find worthwhile in undertaking research on health and medical decision-making—either by delving deeper into the 5Ss or by going bigger and broader beyond the scope of past research.

THE 5S FRAMEWORK OF DRIVERS OF HEALTH AND MEDICAL DECISIONS
Many “self” variables drive health and medical decisions. Consumers belong to different demographic groups ( Connell, Brucks, and Nielsen 2014 ; Du, Sen, and Bhattacharya 2008 ) and have different health goals, abilities, perceptions, and beliefs. To pursue any action toward health, consumers have to believe that they can do it (i.e., self-efficacy) and that this action will lead to desirable outcomes (i.e., response-outcome expectancies; Bandura 1982 ); consumers’ perception of their own health abilities are thus critical ( Han, Duhachek, and Agrawal 2016 ; Keller 2006 ; Moorman and Matulich 1993 ). Consumers’ existing beliefs and perceptions about diagnoses and remedies are similarly important. For instance, consumers can hold different beliefs about healthy food ( Haws, Reczek, and Sample 2017 ; Raghunathan, Naylor, and Hoyer 2006 ), the accuracy and certainty of a diagnosis ( Wang, Keh, and Bolton 2010 ), and how effective a recommended remedy is ( Keller 2006 ). Consequentially, knowing that a remedy is highly effective can conversely lower consumers’ perception of risk, resulting in a boomerang effect on consumers’ pursuit of overall health ( Bolton, Cohen, and Bloom 2006 ). Below, we highlight three articles, including a focal article from this curation ( Moorman and Matulich 1993 ), that examined health motivation and health ability, self-efficacy and response efficacy, and consumers’ lay beliefs about remedies.
Health Motivation and Health Ability
Moorman and Matulich (1993) proposed a comprehensive framework to theorize how consumers acquire health information and what motivates consumers’ health maintenance behaviors, offering a thorough review of a large set of health models studying a wide variety of behaviors spanning from breast self-examination and nutrition labeling to AIDS information search. The authors propose two key constructs for understanding “self” drivers: (1) health motivation, defined as consumers' goal-directed arousal to engage in preventive health behaviors, and (2) health ability, defined as consumers' resources, skills, or proficiencies for performing preventive health behaviors. The article delineates a host of predictions including how health motivation promotes health behaviors, and how health knowledge, health status, health locus of control, health behavioral control, and demographic variables (education, [young] age, and income) will each promote health behaviors when health motivation is already high. Key among them is the idea that consumers must be motivated to pursue these health actions, and idiosyncratic differences in real and imagined health abilities can all contribute to the ultimate actions taken. Health motivation and health ability thus go hand in hand; policies and interventions that address only one self-driver and neglect the other will be leaving a lot on the table.
Self-Efficacy versus Response Efficacy
Keller’s (2006) influential article investigated successful health messaging and found a matching effect between consumers’ motivational orientation (i.e., regulatory focus) and their perceived effectiveness of a remedy (i.e., whether the remedy uses a self-efficacy or a response-efficacy appeal). For consumers who have a promotion focus, a self-efficacy message featuring an easy means toward a desired health state is more motivating; in contrast, for consumers who have a prevention focus, a response-efficacy message featuring an effective means toward a desired health state will be more motivating.
In one study, Keller recruited 61 students from a middle school. These students were primed to activate either a promotion or a prevention focus; they then saw a full-page sunscreen appeal: one side of the appeal displayed a picture of a young woman with half her face altered to show the negative effects of the sun; the other side of the appeal displayed either a self-efficacy message (“You can do it! It’s as easy as 1–2–3”) or a response-efficacy message (“Sunscreen Works! There is no better way”). The author found that when the students were guided to think about hopes and aspirations (i.e., a promotion focus), the self-efficacy message was more effective; but when the students were guided to think about duties and responsibilities (i.e., a prevention focus), the response-efficacy message worked better. This article highlights the importance of understanding consumers’ motivation orientations—whether they are more concerned about their own abilities or the remedy’s effectiveness in achieving the desired health state. Designing appeals for different motivational orientations goes a long way toward sustaining the effectiveness of these appeals.
Lay Beliefs about Remedy
In addition to health motivation and the perception of ability, consumers also have many existing beliefs about remedies and treatments that are available in the marketplace. Wang et al. (2010) examined the lay theories consumers hold about two aspects of medical decision-making—specifically, lay beliefs about diagnosis and lay beliefs about health remedies.
In a study with 100 Chinese college students, the authors directly manipulated how certain the diagnosis was and whether these students had a class presentation to make in 2 or 10 days. Consistent with the authors’ theory that consumers’ lay beliefs drive their preference for specific remedies, these participants preferred traditional Chinese medicine over Western medicine in all situations except for one condition: when diagnosis uncertainty was low and the class presentation was in two days, participants’ preference shifted toward Western medicine because of their lay belief that Western medicine has higher causal certainty and faster response efficacy.
These beliefs critically drive consumers’ desire to pursue a healthy lifestyle. The authors’ subsequent studies found that traditional Chinese medicine that attends to the whole body are less likely to backfire in the pursuit of a healthy lifestyle because these remedies acknowledge the interaction of treatment with the rest of the body and the mind. In contrast, Western medicine that emphasizes cause–effect sequences tends to narrow consumers’ focus and neglect other health-related actions, leading to a boomerang effect and decreasing consumers’ desire to engage in a healthy lifestyle. Here, the authors highlight the importance of understanding global lay beliefs about diagnosis and remedies so that healthcare practitioners can provide tailored recommendations that minimize backfiring and promote well-rounded health outcomes.
Consumers are social beings; not surprisingly, consumers’ health decisions are heavily driven by social forces. One particularly powerful way that social factors impact health is through social comparison. Other people in our social network serve as meaningful reference points, and we gain self-knowledge by comparing our situations to those of others ( Festinger 1954 ; Tesser 1988 ). For instance, consumers going through medical treatments can affiliate with others undergoing similar procedures for support and knowledge exchange. By assimilating with others who have successfully overcome a health challenge, consumers can feel more optimistic about their own chance of success ( Huang et al. 2015 ; Kulik and Mahler 2000 ). In addition to assimilation, consumers may contrast themselves against undesirable social groups to signal their own identity (e.g., consuming less food than the undesirable social group, McFerran et al. 2010 ). Furthermore, social comparison can either boost or discourage consumers’ adoption of innovative health solutions depending on whether consumers are holistic or analytical thinkers ( Chung and Lee 2019) .
The second powerful way that social others influence us is by sharing and altering our decision-making process ( Dzhogleva and Lamberton 2014 ; Fishbach and Tu 2016 ; Fitzsimons and Finkel 2010 ; Liu, Dallas, and Fitzsimons 2019 ). In the medical context, consumers’ decisions can not only be shared and shaped by others but can also be completely given or delegated to others—in these cases, social others go beyond merely altering our decisions but become the decision-makers themselves. Examples include parents choosing a treatment plan for their child, a person deciding whether to remove life support for their partner who is in a coma, or children choosing a personal-care provider for their aging parent. Below, we discuss these two broad categories of social forces by highlighting two articles, respectively, including one of our focal articles ( Botti et al. 2009 ).
Social Comparison
While assimilation can be easily observed in medical settings such as through various support groups at hospitals, it may be harder to imagine how consumers’ desire to contrast against undesirable social groups would affect their health decisions. Berger and Rand (2008) examined this social factor and leveraged it to increase life-benefiting decisions. They observed that undergraduates at Stanford University were reluctant to wear helmets because graduate students—a group the undergraduates did not identify with—wore helmets. The authors leveraged this insight to reduce risky behaviors such as alcohol consumption by highlighting how these behaviors were popular among out-groups.
In one field experiment, the authors posted flyers to promote responsible drinking in restrooms and on bulletin boards at two freshman dorms. At the treatment dorm, the flyer linked alcohol consumption with graduate students by depicting a graduate student holding an alcoholic beverage; the message ended with “Nobody wants to be mistaken for this guy.” At the control dorm, the flyers provided typical information about negative health effects of alcohol without evoking any social identity. Using follow-up surveys and self-reported alcohol consumption measures, the authors found an interesting interaction between the flyers and freshmen’s existing attitude toward graduate students (i.e., the out-group). For freshmen who did not want to be affiliated with graduate students, the treatment flyers created a strong effect, resulting in significantly less alcohol consumption. This effect did not occur for freshmen who did not mind such an affiliation. Social others thus can serve as powerful facilitators for, or inhibitors to, consumers’ health and medical decisions.
Choosers versus Consumers
When medical decisions are made by others, social forces affect both the “consumers” of the decision (e.g., the patients) and the “choosers” (e.g., the guardians). The award-winning article by Botti et al. (2009) studied this unique decision dynamic through both qualitative and quantitative methodologies. Their focus was on highly consequential and undesirable decisions: parents deciding to discontinue their infants’ life support.
By leveraging a subset of interviews drawn from a large comparative ethnographic study on parents’ experiences in newborn intensive care units, these authors tapped into invaluable insights revealed by parents in two countries—the United States and France—whose babies died after the physicians offered the option to interrupt the life-sustaining treatment and who either autonomously made this tragic decision (American parents) or witnessed the physicians deciding on their behalf (French parents).
The authors found that having autonomy to make tragic choices negatively affected American parents’ psychological pain and grief. While guilt was never mentioned or even indirectly expressed in French parents’ narrative, it was commonly mentioned by American parents. Follow-up lab studies further verified that perceived causality was the driving mechanism: even when most choosers made the “right” decision and reported higher confidence than non-choosers, they felt worse for having made the difficult decision. This research points to the importance of understanding complex medical decision chains in which choosers are not always the consumers of the chosen solution. While the effectiveness of the decision can be lifechanging for the consumers, the process through which these decisions are made can also affect the choosers.
A critical aspect of health and medical decision-making is that this decision process often begins with a health concern/problem, or an anticipation of one. Consumers—driven by self and social factors—seek a solution to address this health concern. The solution can involve (1) human providers such as physicians, (2) non-human providers made available by new technologies such as AI-powered medical assistants, and (3) solution products such as treatment plans and medication. When it comes to human and non-human providers, an interaction between the provider and the patient occurs and a relationship can be developed over time ( Szasz and Hollender 1956 ). Furthermore, providers can express their expertise in various ways, and patients can decide to trust, cooperate, comply, or search for solutions elsewhere. As for the third category of solution products, consumers can hold different beliefs and perceptions about how the products are developed (natural vs. synthetic; Scott, Rozin, and Small 2020 ), how the products actually work (e.g., holistic treatment vs. cause–effect focused, slow vs. fast; Wang et al. 2010 ), and how the products compare with the other options (typical vs. atypical products; Huang and Sengupta 2020 ). Below, we discuss three articles that examined human providers, non-human providers, and product solutions accordingly.
Human Providers
Friedman and Churchill (1987) examined patient–physician relationships from the lens of social power. The authors asked participants to listen to a tape-recorded conversation between a physician and a patient. These recordings featured various medical situations and physicians’ power behaviors and were created based on content analyses of 25 videotaped and 50 transcribed, audiotaped conversations of naturally occurring patient–physician interactions.
The authors found that power behaviors affected patients’ satisfaction and outcomes, but the nature of these influences was rather complex. High (vs. low) expert-legitimate power behaviors led to greater satisfaction and more positive consequences when the medical situation was risky, but these variables were less important in a non-risky situation. High expert-legitimate power behavior also produced greater satisfaction and more positive consequences when the patient and physician had an ongoing relationship but not for new or one-time relationships. Social power behaviors from physicians thus can be effective depending on how serious the patient’s condition is and the nature of the patient–physician relationship.
These results suggest that when a patient interacts with a human provider, the provider’s behaviors and traits (e.g., expertise and power) and the patient’s expectation play important roles in determining whether the patient trusts and follows the provider’s recommendations and the patient’s ultimate health outcome. As it turns out, the patient’s expectation is also a critical driver when the provider is not a human.
Non-Human Providers
With the rapid growth of new technologies and the wide adoption of these technologies in health care, consumers’ receptiveness to medical innovations has emerged as one of the most critical challenges for solution providers to overcome. Through a series of studies, the authors of one of our focal articles ( Longoni et al. 2019 ) demonstrated when consumers are less willing to utilize AI-powered health care, have lower reservation price for it, and derive negative utility from these automated providers.
In one study, the authors informed participants that the analysis of their data could be carried out either by a doctor (human provider) or by a computer (non-human provider) and specified that the two providers had the same accuracy rate of 89%. They further emphasized that there would be no interaction with the provider performing the analysis and that the medical diagnosis would entail the same information and would be delivered according to the same timeline. They found that the participants were willing to pay on average $13.78 USD less to use the non-human provider.
Leveraging the proposed mechanism of “uniqueness neglect,” in another study, the authors manipulated the salience of the provider’s ability to personalize and tailor the analyses and recommendations for the patient (“…the analysis was personalized and tailored to your unique characteristics”). They found that personalized recommendations successfully alleviated consumers’ reluctance to follow the recommendation from the non-human provider. Developing non-human providers that can account for consumers’ unique characteristics and circumstances is thus important in increasing the solutions’ adoption. As medical resources continue to be overtaxed and the need for more efficient, technology-driven providers continues to rise, more research is needed to examine how society can scale up healthcare providers without dampening consumers’ perceptions of the providers’ accuracy and effectiveness, as well as their willingness to follow the recommended actions. We discuss these opportunities further in the Future Directions section.
Solution Products
While medical solutions often involve a certified provider (e.g., meeting with a doctor for diagnosis and prescription), these solutions may eventually be executed through consumers’ purchasing a service (e.g., an fMRI scan) or a product (e.g., a medication). The third category of solutions thus centers on products that consumers purchase to address a health or medical concern. An exemplary article in this category is by Scott et al. (2020) .
These authors showed that natural products—products that do not involve prior human intervention and additives—are preferred when used to prevent a problem than when used to cure a problem. In one study, the authors used publicly available data from the 2012 National Health Interview Survey (NHIS), conducted by the Centers for Disease Control and Prevention (CDC), to explore 9,972 consumers’ reported use of complementary and alternative medicines over the past year. They found that consumers were more likely to prefer natural remedies when using a treatment as a preventative than as a curative.
This preference occurs because consumers believe that natural products are safer and less potent. When seeking prevention (vs. cure) products, consumers care more about safety and thus are more likely to choose a natural product. Leveraging this underlying mechanism, the authors were able to directly reverse this lay belief by framing the natural drug as stronger and having more side effects (more risk), and the synthetic drug as weaker and having fewer side effects (less risk). This framing successfully reversed the pattern, such that consumers preferred the natural drug when choosing a curative.
While solution drivers are essential in shaping consumers’ health and medical decisions, an effective solution cannot be fully understood or judiciously adopted by consumers without effective marketing communication. Accordingly, health messaging and marketing strategies are used ubiquitously by practitioners and organizations to promote healthy behaviors (see Bou-Karroum et al. 2017 for a review). For example, the World Health Organization Framework Convention on Tobacco Control advocates a number of marketing-based recommendations to discourage smoking, whether in terms of promoting the use of plain (standardized) packaging, displaying enlarged graphic health warnings on cigarette packages, or curbing point-of-sale product displays.
In this section, we take a marketing perspective and highlight some articles that have illuminated how the core elements of the marketing mix can influence consumers’ health and medical decisions, including one of our focal articles ( Bolton et al. 2008 ). Findings from these articles not only enable consumers to better understand the antecedents of their decisions but also inform practitioners in both public and private sectors on how they can strategize to improve the physical and psychological wellbeing of target consumers/constituents.
Health Marketing
Marketers and policymakers use a variety of messages and communication strategies to promote health and medical products, services, and practices. Prior research has shown that the degree to which a health message is persuasive depends on how the message is designed and framed, as well as its interaction with consumers’ dispositional tendencies and situational states ( Aaker and Lee 2001 ; Chandran and Menon 2004 ; Keller 2006 ; Menon, Block, and Ramanathan 2002 ).
Following this line of enquiry, Han et al. (2016) demonstrated that the construal level at which a health message is presented interacts with consumers’ coping strategies to affect the message’s effectiveness. For example, in one study, undergraduates at a US university indicated more favorable attitudes toward a government-run educational program designed to promote healthy physical activities when the ad for the program was framed at a high-level construal (i.e., “Why Do You Engage in Physical Activities in This Program”) among participants induced to think about the positive benefits of emotion-focused coping, but when the ad was framed at a low-level construal (i.e., “How Do You Engage in Physical Activities in This Program”) among participants induced to think about the positive benefits of problem-focused coping.
The authors demonstrated in another study that this matching effect was accompanied by actual reduction of stress in terms of cortisol level. The authors further show that different mechanisms underlie this effect for the two groups of consumers, such that response efficacy mediates the effect of a match between emotion-focused coping and the high-construal level of the health message on persuasion, whereas self-efficacy mediates the effect of a match between problem-focused coping and the low-construal level of the health message on persuasion.
Product Marketing
In medical marketing, even well-intentioned product positioning can backfire, as demonstrated by Bolton et al. (2008) . In this research, how a product is positioned and marketed—either as a drug or a health supplement—led to widely different downstream behaviors by changing how consumers think about their health risks and ability to combat these risks. Surprisingly, they found that marketing a product as a drug (rather than a supplement) makes consumers less likely to engage in healthy lifestyle practices.
The researchers posit that this boomerang effect is attributable to two reasons. First, drugs may reduce consumers’ risk perceptions and hence their perceived importance of and motivation to engage in complementary health-protective behaviors, such as eating low-cholesterol foods. Second, drugs may be associated with poor health that reduces self-efficacy to engage in healthy behaviors. By unpacking these potential mechanisms, the authors suggest (and demonstrate empirically) the potential of using a combined intervention—designed to increase health motivation and health ability—to assuage the adverse boomerang effect of drug marketing.
Pricing is another way that marketers can impact consumers’ health and medical decisions. The price of a drug can even affect consumers’ beliefs about its efficacy ( Waber et al. 2008 ) and thus can lead to a placebo effect ( Shiv, Carmon, and Ariely 2005 ).
Samper and Schwartz (2013) offered a unique perspective of the effects of pricing, showing that the price of a medical product can affect how consumers perceive risk, and in turn, how much of the product to consume. They distinguished between sacred and secular products; medical drugs are generally regarded as lifesaving and are hence sacred products—consider a skin ointment that has a lifesaving function (e.g., prevents skin cancer) instead of one that has a cosmetic benefit (e.g., prevents age spots). Lower prices in sacred, lifesaving products signal these products’ greater accessibility to anyone in need, thereby making consumers think they are more at risk, and in turn, increasing consumers’ intention to consume the products. Conversely, higher prices reduce risk assessment and thus consumption.
Since the abovementioned consumption reduction (due to higher prices and lower risk perception) could apply to both necessary and unnecessary care, it may lead to negative effects on consumer welfare if consumers under-consume the drugs that they ought to. Therefore, to the extent that price serves as a simple proxy for risk and that proxy is inaccurate, appropriate “consumer education about communal need and objective risk” (p. 1354) should accompany price transparency to better inform consumption.
While the highlighted articles above shed light on some ways in which the core elements of the marketing mix, particularly marketing messaging and pricing, can affect consumers’ health and medical decisions, other elements may also play an influential role. For instance, it is conceivable that how a product/service is distributed (e.g., intensively, selectively, or exclusively), where it is sold (e.g., online vs. brick-and-mortar store vs. hybrid/omnichannel), and how it is packaged (e.g., where the picture of a product is located on the packaging; Deng and Kahn 2009 ) can also affect consumers’ judgments and decisions.
Furthermore, turning from these direct influences to more indirect/incidental influences, a longstanding debate in our society is how much mass-media advertising and entertainment have led to adverse effects on health (e.g., through advertising of unhealthy foods, movies depicting smoking, drug use, and alcohol consumption—often through product placement), with moralists and capitalists often standing on opposite sides. Using a compelling natural experiment and NHIS data in the United States, Thomas (2019) demonstrated that television had considerable impact on inducing smoking. His analysis revealed that, between 1946 and 1980, television increased the share of smokers in the population by a striking 5–15%, generating roughly 11 million smokers in the United States. This effect was more influential than price fluctuations and was especially dominant among teens. Juxtaposed against an earlier finding from Connell et al. (2014) where childhood advertising can create biased product evaluations that persist into adulthood, Thomas’ finding is at once alarming and sobering.
Beyond internal factors of the self and external influences of social, solution, and service-provider drivers, consumers’ broader societal and situational environment can also affect their health and medical decisions in systematic ways. As Ross and Nisbett (2011) reminded us in their seminal volume “The Person and the Situation,” the context in which consumers find themselves often interact with their dispositions to influence how they think and behave. Here, we consider work on this driver, including our focal article ( Briley et al. 2017 ).
Consumers’ cultural background may not only shape their self-view ( Markus and Kitayama 1991 ) but also affect how they think and process external information. Centering on the question of how consumers confront health challenges in life, Briley et al. (2017) convincingly demonstrated that cultural background plays a pivotal role in cultivating optimism in difficult times. In particular, the authors distinguish between two mental frames that people can adopt in the face of health challenges: an initiator frame (“how will I act, regardless of the situation I encounter”) and a respondent frame (“how will I react to the situations I encounter”). While optimism is essential in helping people cope with health challenges and recover successfully, the authors propose that people with an independent cultural background are more optimistic about their recovery when adopting an initiator (vs. a responder) frame, whereas people with an interdependent cultural background are more optimistic when adopting a responder (vs. initiator) frame, demonstrating these effects for a variety of health challenges (cancer, diabetes, serious injury from a car accident) and health outcomes (e.g., feeling more optimistic and energetic, willingness to take on more challenging physical therapy, sticking to a doctor-recommended diet).
In one study (study 6), undergraduate students were asked to consider having to confront various health threats after experiencing torrential rains and severe flooding where they lived (e.g., communicable diseases spread by contaminated water). They were then exposed to a public health message about a fictitious vaccine, Immunasil, with either initiator language (“Act now to protect yourself—get vaccinated”) or responder language (“Respond now to protect yourself—get vaccinated”). The authors found that participants with a greater independent self-view were more likely to get vaccinated if they were exposed to the initiator-framed health message, while those with a greater interdependent self-view were more likely to get vaccinated if they were exposed to the responder-framed health message; these results were mediated by the ease with which participants imagined getting vaccinated and their optimism toward the vaccine. These findings provide valuable guidance to firms and public health communicators in their design of health products and messages, reminding practitioners of the importance of considering target consumers’ cultural background in fostering greater optimism and improved wellbeing.
Evolutionary Forces
At a more fundamental level, consumers’ incidental exposure to myriad cues in their environment can activate evolutionarily adapted survival instincts and drive their cognition and behavior. Disease cues are an example of such situational triggers (e.g., Galoni, Carpenter, and Rao 2020 ). These cues have been especially prevalent in the last few years as the world wrestles with multiple variants of the COVID-19 virus and consumers are exposed to widespread daily media coverage of the protracted pandemic.
Huang and Sengupta (2020) show how disease cues may activate consumers’ behavioral immune system and cause them to prefer atypical consumer products (e.g., pomegranate juice) and shy away from more typical products (e.g., orange juice), arguing that disease salience triggers the instinctual, unconscious motivation to avoid social others and, consequently, generate aversion to typical products as such products are associated with many (vs. few) people. Accordingly, this effect was attenuated when the disease with which the cues were associated was noncontagious (e.g., cancer), when anti-disease interventions were also made salient (e.g., handwashing), and when the use of the focal product was less likely to carry the risk of infection (e.g., a set of plates used for decoration rather than as dinnerware).
Huang and Sengupta’s (2020) findings suggest that amid the ongoing pandemic, researchers and practitioners could leverage these insights to boost adoption of certain health-related products (e.g., oat milk) and practices (e.g., fitness programs) by highlighting the atypicality and exclusivity of such offerings. Connecting these findings with the earlier discussion on consumers’ lay beliefs ( Wang et al. 2010 ), Western medicine may be perceived as more (or less) typical than traditional Chinese and Ayurvedic medicine depending on consumers’ cultural background. In this vein, an extrapolation of Huang and Sengupta’s (2020) findings may suggest that exposure to disease cues would lead consumers to prefer the type of medicine that they deem more atypical. Furthermore, they observed the hypothesized evolutionary-adaptation effects by activating less immediately threatening disease cues, which were quite different from the highly salient COVID-19 disease cue. Prolonged social isolation arising from the pandemic may instead lead consumers to desire greater social connectedness, and accordingly, prefer more typical products.
Together, these two articles reveal how deep-seated societal (cultural) and situational (evolutionary) drivers could impact consumers’ health and medical decision-making. They add to a growing body of work that has highlighted the critical roles that these drivers play (e.g., how cultural factors affect the effectiveness of health communication with regard to the source, message, and channel of the communication; Kreuter and McClure 2004 ).
The 5S framework offers rich opportunities and fruitful directions for future research on consumer health and medical decision-making. Below, we highlight four major directions. The former two directions call for research that dives deeper into the complexity of consumer health phenomena, to enhance our understanding of how multiple drivers interact, reinforce, or cancel each other, and how a variety of methodologies and unique samples can be leveraged to shed light on complex yet critical nuances involving different decision types.
The latter two directions call for research that goes bigger —beyond the scope of typical consumer health research—challenging consumer researchers to think more broadly about how improving health and medical decisions can (ironically) be a double-edged sword, potentially leading to undesirable consequences on consumers’ wellbeing and the society. In addition, we encourage researchers to examine how health care can be effectively scaled up to address the prevailing challenges in limited supply and to serve the broader and diverse population. Future research along these lines will generate invaluable insights to ensure positive long-term gain on the health of all consumers.
Going Deeper: Cross-Driver Interactions
To truly understand how consumers make health and medical decisions, the five drivers in the 5S framework cannot be studied in isolation. Indeed, many influential articles we have discussed so far explored cross-driver interactions of two key drivers, such as the effect of a service-provider driver (e.g., product marketing) on a self-driver (e.g., health motivation and health ability, Bolton et al. 2008 ) and the effect of a novel solution driver (e.g., AI provider) on a self -driver (e.g., need for uniqueness, Longoni et al. 2019 ). Potential interactions between two self -drivers have also been of considerable interest to consumer researchers, such as studying how lay beliefs and motivational orientations affect consumers’ perceptions of self-efficacy and response efficacy ( Keller 2006 ; Wang et al. 2010 ).
Beyond Two Drivers
In essence, consumer health is an inherently complex topic that often goes beyond two drivers. For instance, the solution driver of an AI provider can interact with social drivers of assimilation and contrast to inform consumers’ perceptions about themselves: seeing a specific group of consumers (e.g., millennials) rely on technology-mediated treatment platforms may turn away consumers of other age groups (e.g., contrast), especially for consumers whose health abilities or self-efficacy beliefs are low. To truly understand and predict the adoption of AI providers, researchers thus need to consider not only the solution drivers of interest but also relevant self and social drivers simultaneously.
It is also important to recognize that one focal construct can affect two drivers at the same time. For instance, power can be both a societal/situational driver (e.g., some societies have a larger power distance) and a solution driver (e.g., the power conveyed by the physicians, Friedman and Churchill 1987 ); power can even be a service-provider driver (e.g., conveying expertise and power through a marketing message or through price). Hence, to examine how power affects consumers’ medical decisions, researchers may need to consider the interaction between the power in consumers’ environment and the power conveyed by the provider, and how these two types of power jointly affect consumers’ expectations, perceived abilities, and motivation ( Moorman and Matulich 1993 ).
There are also significant opportunities for researchers to dive further into the complexity of societal/situational drivers. As modern consumers place greater emphasis on corporates’ social responsibility efforts, companies and medical institutions are becoming more eager to connect their marketing messages with consumers’ values, such as ensuring equal pay of medical staff, increasing energy efficiency, and reducing medical waste (e.g., the Top 25 Environmental Excellence Awards were recently established to recognize healthcare organizations’ environmental achievements). Societal/situational drivers hence interact heavily with consumers’ self-drivers to inform how service providers should communicate and market their healthcare offerings in the 21st century.
Beyond Two Stakeholders
While researchers should consider the complexity of medical decisions that go beyond two drivers, it is similarly important to consider health decisions that involve more than two stakeholders. For instance, as the population ages, greater insights are needed to understand how consumers select care providers for their aging parents, and how these care providers make day-to-day decisions for the wellbeing of these aging clients. The juxtaposition across these stakeholders underscores the complexity of medical decision-making for aging consumers: while one stakeholder is the ultimate recipient of the service, the second stakeholder makes decisions driven by their social relationship (e.g., duty and love), whereas the third stakeholder—driven mostly by a contractual relationship—may have the most intimate knowledge about the patient’s health conditions and changing mental state. A fourth stakeholder may include distant agencies (e.g., policymakers and payment organizations) who impact treatment through accessibility, legislation, and funding. Future research is needed to ask bold questions and explore complex dimensions involving multiple stakeholders and across multiple drivers.
Going Deeper: Complex Decision Types
Decision type considerations.
Health and medical decisions differ widely along various dimensions ( table 1 ). Depending on the specific attributes of the focal decision, different decision processes (e.g., maximizing vs. satisficing, analytical vs. heuristic based vs. feeling based, compensatory vs. non-compensatory) and psychological mechanisms may operate. While most research focuses on specific decision types, extending the focal decision to other (and more complex) decision types along one or more dimensions may prove advantageous in illuminating the unique psychology driving these decisions. In addition, from a practical and substantive perspective, such an approach will help to inspire new research questions (focusing on new decision contexts/types) and novel ideas to address the health or medical issue at hand.
DIMENSIONS OF COMPLEX DECISION TYPES
For example, prior research has shown that high-stake decisions and those that carry a more persistent impact generally entail a more deliberative and analytical decision process than lower-stake and one-time, short-lived decisions. Would the perceived importance of health as a domain (compared to, say, finance) attenuate these differences, such that more categories of drivers (in the 5S framework) are considered by consumers and exert greater impact even for low-stake medical decisions? While persistent (vs. temporary) health issues may lead to habitual decision-making, given the importance of health as a domain, would the longer duration of impact actually prompt consumers to be more deliberative when choosing? Conversely, might the inherent complexity of these decisions result in consumers’ relying more on arguably less-relevant social and incidental situational drivers?
Another example is health lifecycle. Would the weight consumers put on these drivers change as decisions advance from one health-lifecycle stage (e.g., screening) to another (e.g., maintenance)? What about products that could serve both a preventive/maintenance role and a cure/treatment role ( Scott et al. 2020 ), as in some forms of Asian medication (e.g., cordyceps), depending on the dosage amount? How would consumers perceive such dual-purpose products, and how would these perceptions affect their downstream decisions or behaviors?
Furthermore, what if these health and medical decisions were made jointly (e.g., by two partners in a romantic relationship, or by members of a family)? Would this result in a polarizing effect or an averaging effect on consumers’ risk perceptions? And would this social dynamic depend on the heterogeneity of the decision-making unit ( Yaniv 2011 )? A thoughtful consideration of these rich decision dimensions will help consumer researchers deepen their inquiries, enhancing the generalizability of their theories and establishing meaningful boundaries for their proposed effects.
Methodological Considerations
Depending on the nature and complexity of the health decision that researchers intend to study, a diverse set of methodologies and participant samples may be necessary to lend greater relevance as well as confidence to the findings. Accordingly, prior research has employed a variety of methodologies, from lab and field experiments ( Berger and Rand 2008 ; Bolton et al. 2008 ; Cadario and Chandon 2020 ; Haws et al. 2022 ) to qualitative interviews and participatory-action research ( Botti et al. 2009 ; Tian et al. 2014 ), and from natural experiments and econometric modeling ( Thomas 2019 ) to ethnographic methods ( Hirschman 1992 ; Thompson and Troester 2002 ). Besides providing triangulation and ensuring greater robustness in the empirical results, these varied methods may be necessary to inject diverse perspectives that help illuminate the complexity of the decision or issue of interest.
Furthermore, rather than deductive or inductive methods, an abductive approach ( Janiszewski and van Osselaer 2022 ) can prove beneficial for the discovery of novel theories arising from more complex health and medical decisions. This empirical approach prioritizes system validity ( Reiss 2019 ) over internal or external validity, “encourages broad boundary-expanding exploration,” and possesses “the potential to propose original theories that encompass a large set of relationships” ( Janiszewski and van Osselaer 2022 , 175). Advanced quantitative techniques such as systems modeling and simulation, and the use of genetic algorithms may also be useful in capturing the complexity and evolving nature of these multi-faceted and multiply determined relationships.
Going Bigger: Broader and Opposing Consequences
While the two previous research directions relate to deepening our understanding of the core drivers of health and medical decisions, particularly for decisions that possess vastly different attributes along the five dimensions, the next two research directions call for broadening the scope of research on health and medical decisions, and improving understanding of the implications of this expansion.
Although much of the research on consumer health has focused on specific, unilateral consumer decisions and outcomes, some of these decisions and outcomes may have other downstream consequences for consumers, specific communities, or the society at large. These outcomes can have opposing valence or be even unrelated to health, presenting a tradeoff (or double-edged sword) that necessitates the consideration of multiple perspectives and diverse criteria in evaluating the overall impact. (Notably, the five drivers can serve either as enablers/catalysts or detractors/impediments to positive health and medical decision-making.)
Beyond Price and Risk Perception
For instance, consider the findings of Samper and Schwartz (2013) discussed above. While setting a high price for drugs and medicine may discourage consumption through lowering risk perception, this pricing strategy can also help prevent abuse of the drug and over-consumption (as in the case of antibiotics, whose liberal use may result in adverse health consequences in the long run by making everyone less resistant to new bacterial variants or superbugs). To what extent should public health policymakers simply rely on market forces to drive prices down in response to reduced demand? More broadly, might these authors’ findings help to foster greater education efforts and public awareness of health and preventive actions, leading to additional positive spill-over effects?
Beyond Technology and Mass Production
As another example, consider the burgeoning use of AI, synthetic drugs, and other technological innovations that standardize the quality of health care and mass produce these solutions [see Wood and Schulman (2019) on the importance of understanding how patients respond to five types of disruptive healthcare innovations]. While such advances may render healthcare services more efficient and potentially more affordable and accessible, might they also generate consumer overconfidence, resulting in a boomerang or risk compensation effect ( Peltzman 1975 ), such that consumers perceive a false sense of security and take more risks than otherwise warranted (e.g., being more delinquent in adhering to a prescribed medication regime)? From a systemic standpoint, might the increasing use of non-human technology-mediated solutions in health care enhance efficiency and accuracy at the expense of reduced human warmth, empathy, and trust—qualities that may be especially vital for certain medical decisions (e.g., decisions related to terminal illness, psychotherapy) and for some vulnerable groups of patients (e.g., the elderly, people with disabilities)?
Key Questions
In approaching this research direction, it will be worthwhile to consider several pertinent questions. First, to what extent might consumers’ actions and decisions affect other stakeholders (other than consumers themselves), whether these stakeholders belong to the immediate medical ecosystem or beyond, and whether in terms of health-related or health-unrelated outcomes? Second, what criteria should we use to assess the overall welfare impact of consumers’ decisions (the normative or prescriptive view), either at the consumer level or the broader societal and global level? Third, extending beyond the domain of health care, which other domains are most intimately linked to health and medical decisions (e.g., financial decisions, corporate responsibility, environmental sustainability such as food safety and food security) that key stakeholders and policymakers should consider in concert, either to achieve greater effectiveness (to allow for a more holistic evaluation) or efficiency (to conserve scarce resources)?
Going Bigger: Scaling Up Health Care
We live in a world of limited resources. The limitation lies in human resource, natural resource, software and hardware, money and time. The limitations in health care are startling. Many people cannot access health care because of its cost and their income, others cannot access health care because of geographical constraints, and yet others cannot access health care because they are uninsured. In fact, an estimated 9.6% of US residents (i.e., 31.1 million people) lacked health insurance when surveyed in early 2021 by the CDC. To improve consumers’ health and medical outcomes, we need effective solutions driven by behavioral science to scale up healthcare resources: to (1) increase supply, (2) redefine quality, and (3) broaden the reach.
Increase Supply
To increase the “supply” in health care, we need advanced medical research to discover effective procedures, treatments, and medicines, as well as dedicated policy support to ensure sufficient funding and efficient deployment of resources. Equally important, we also need to recruit behavioral science to help overcome erroneous perceptions and beliefs as well as psychological hurdles in implementation.
Take medical innovation as an example. One way to scale up human providers is to deploy non-human providers more broadly. Instead of seeing a physician for every minor health concern, an AI doctor can leverage data to provide quick diagnoses and issue prescriptions at scale. However, prior research has shown that consumers are hesitant to trust non-human service providers ( Longoni et al. 2019 ; Wood and Schulman 2019 ). In addition, even doctors prefer to rely on their own intuition rather than computerized models ( Keeffe et al. 2005 ). What makes matters worse is that doctors who rely on computerized aids may be evaluated as less competent by others ( Palmeira and Spassova 2015 ; Shaffer et al. 2013 ). To scale up automated service providers, therefore, we not only require better technologies but also a much deeper understanding of human psychologies that are holding us back. One such solution is tested in study 9 in Longoni et al. (2019) . The authors tested a theory-driven task allocation between human and non-human providers—having the non-human provider serve the supporting role and not the substitute effectively alleviated consumers’ reservation about AI providers. We encourage future research to explore more innovative and practical ideas and interventions that can help to scale up healthcare accessibility, leading to broader adoption across different segments of consumers and different domains of service providers, so that more patients can benefit from these medical advancements.
Redefine Quality
Scaling up health care also means bringing better-quality care to more consumers. What constitutes “better-quality care,” however, is debatable. Wang et al. (2010) showed that while Western medicine is known for tackling a specific cause effectively and fixing a focal issue quickly, Eastern medicine is known for its holistic approach, which often takes more time for patients to see improvement. Our society has put great emphasis on efficiency and has little patience for solutions that are slow or when progress is less observable; yet slower but more holistic approach may actually help to strengthen consumers’ overall health, leading to long-term improvements and thus reducing future need for medical treatments. In this light, research that helps consumers and service providers re-envision what constitutes better-quality care will go a long way toward solving the demand-versus-supply issue in health care.
Similarly, holistic care, by definition, aims to address patients' physical, emotional, social, and spiritual needs, restore their balance, and enable them to deal with their illnesses, consequently improving their quality of life ( Tjale and Bruce 2007 ). This means that service providers and solution drivers should think carefully about the delicate balance between prolonging one’s life and ensuring one’s wellbeing or general life quality. A shortsighted focus on prolonging life alone not only taxes the healthcare system but can also induce substantial harm to the patient and the patient’s social circle. But unless consumers are made aware of these broader and longer-term costs, they will likely continue to rely on service providers’ recommendations and feel compelled to exhaust all solutions. Research on these psychological obstacles and experiments on smart interventions are needed to increase consumers’ awareness, trust, and knowledge about these intricate and difficult tradeoffs.
Broaden Reach
Finally, scaling up health care means broadening the reach of health and medical resources, especially for vulnerable consumer segments and underserved communities. For instance, Du et al. (2008) studied how a corporate oral health initiative can be beneficial (on both societal and business terms) to disadvantaged Hispanic families by strengthening these children’s beliefs about the physical and psychosocial benefits of oral health behaviors. Research on the health and medical needs of specific ethnic groups is desperately needed to increase adoption and ensure fairness as we scale up healthcare resource.
Another example is the aging consumer. Based on a report by the World Health Organization, by 2030, one in six people in the world will be aged 60 years or over. The number of persons aged 80 years or older is expected to triple between 2020 and 2050 to reach 426 million, and 80% of older people will be living in low- and middle-income countries. The aging population introduces a unique challenge to health care, as recent research has shown that objective and subjective age are often orthogonal ( Amatulli et al. 2018 ; Park et al. 2021 ): whereas geriatric physicians often describe their elderly patients with stereotypical traits associated with old age (e.g., tired and frail), their patients tend to describe themselves instead with traits reflecting young age (e.g., energetic and lively; Kastenbaum et al. 1972 ). Such patient–physician discrepancies can affect the quality of care for the elderly, the patients’ willingness to accept care, and their ultimate health outcomes and life expectancy ( Markides and Pappas 1982 ). More generally, elderly consumers have different health and medical needs than younger adults; on a morbid yet critical note, healthcare systems may have over-emphasized prolonging lives instead of also helping individuals prepare for their exit ( Gawande 2014 ). Accordingly, it would be imperative for consumer researchers to employ behavioral science to better understand the needs and wants of elderly consumers and to help them achieve healthier longevity and lead more fulfilling lives.
Just like many behavioral science domains, research on health and medical decision-making has long suffered from the WEIRD phenomenon, in which the majority of social science studies have focused on participants who are Western, educated, and from industrialized, rich, and democratic countries ( Arnett 2008 ; Henrich, Heine, and Norenzayan 2010 ; Rad, Martingano, and Ginges 2018 ). To meaningfully broaden the reach of health care, our mission as behavioral scientists is to broaden our research—to identify unique psychological barriers as well as unique opportunities to improve health and medical decisions among the consumer segments that are traditionally less studied. Failure in understanding these unique psychologies will prevent an effective scale-up of our medical resources; success in capturing these unique psychologies and decision-making processes, on the other hand, will benefit our society as a whole. The challenge is huge, and we believe that consumer researchers play a critical role in leading this change.
Szu-chi Huang ( [email protected] ) is an associate professor of marketing and an R. Michael Shanahan Faculty Scholar at the Stanford Graduate School of Business, 655 Knight Way, Stanford, CA 94305, USA.
Leonard Lee ( [email protected] ) is a professor of marketing at NUS Business School and Deputy Director at Lloyd's Register Foundation Institute for the Public Understanding of Risk, National University of Singapore (NUS), 15 Kent Ridge Drive, 119245, Singapore. Please address correspondence to Szu-chi Huang.
The authors thank Carolyn Lo and Jason Zhou for their research assistance on this work. The authors also thank the editors, especially Stacy Wood, for the invaluable feedback and comments.
This curation was invited by editors Bernd Schmitt, June Cotte, Markus Giesler, Andrew Stephen, and Stacy Wood.
Aaker Jennifer L. , Lee Angela Y. ( 2001 ), “ I’ Seek Pleasures and ‘We’ Avoid Pains: The Role of Self-Regulatory Goals in Information Processing and Persuasion ,” Journal of Consumer Research , 28 ( 1 ), 33 – 49 .
Google Scholar
Amatulli Cesare , Peluso Alessandro M. , Guido Gianluigi , Yoon Carolyn ( 2018 ), “ When Feeling Younger Depends on Others: The Effects of Social Cues on Older Consumers ,” Journal of Consumer Research , 45 ( 4 ), 691 – 709 .
Arnett Jeffrey J. ( 2008 ), “ The Neglected 95%: Why American Psychology Needs to Become Less American ,” The American Psychologist , 63 ( 7 ), 602 – 14 .
Aubree Shay L. , Lafata Jennifer Elston ( 2015 ), “ Where Is the Evidence? A Systematic Review of Shared Decision Making and Patient Outcomes ,” Medical Decision Making , 35 ( 1 ), 114 – 31 .
Bandura Albert ( 1982 ), “ Self-Efficacy Mechanism in Human Agency ,” American Psychologist , 37 ( 2 ), 122 – 47 .
Berger Jonah , Rand Lindsay ( 2008 ), “ Shifting Signals to Help Health: Using Identity Signaling to Reduce Risky Health Behaviors ,” Journal of Consumer Research , 35 ( 3 ), 509 – 18 .
Bolton Lisa E. , Cohen Joel B. , Bloom Paul N. ( 2006 ), “ Does Marketing Products as Remedies Create ‘Get out of Jail Free Cards’? ,” Journal of Consumer Research , 33 ( 1 ), 71 – 81 .
Bolton Lisa E. , Reed Americus , Volpp Kevin G. , Armstrong Katrina ( 2008 ), “ How Does Drug and Supplement Marketing Affect a Healthy Lifestyle? ,” Journal of Consumer Research , 34 ( 5 ), 713 – 26 .
Botti Simona , Orfali Kristina , Iyengar Sheena S. ( 2009 ), “ Tragic Choices: Autonomy and Emotional Responses to Medical Decisions ,” Journal of Consumer Research , 36 ( 3 ), 337 – 52 .
Bou-Karroum Lama , El-Jardali Fadi , Hemadi Nour , Faraj Yasmine , Ojha Utkarsh , Shahrour Maher , Darzi Andrea , Ali Maha , Doumit Carine , Langlois Etienne V. , Melki Jad , AbouHaidar Gladys Honein , Akl Elie A. ( 2017 ), “ Using Media to Impact Health Policy-Making: An Integrative Systematic Review ,” Implementation Science , 12 ( 1 ), 52 .
Briley Donnel A. , Rudd Melanie , Aaker Jennifer ( 2017 ), “ Cultivating Optimism: How to Frame Your Future during a Health Challenge ,” Journal of Consumer Research , 44 ( 4 ), 895 – 915 .
Cadario Romain , Chandon Pierre ( 2020 ), “ Which Healthy Eating Nudges Work Best? A Meta-Analysis of Field Experiments ,” Marketing Science , 39 ( 3 ), 465 – 86 .
Chandran Sucharita , Menon Geeta ( 2004 ), “ When a Day Means More than a Year: Effects of Temporal Framing on Judgments of Health Risk ,” Journal of Consumer Research , 31 ( 2 ), 375 – 89 .
Chung Jaeyeon (Jae) , Lee Leonard ( 2019 ), “ To Buy or to Resist: When Upward Social Comparison Discourages New Product Adoption ,” Journal of the Association for Consumer Research , 4 ( 3 ), 280 – 92 .
Connell Paul M. , Brucks Merrie , Nielsen Jesper H. ( 2014 ), “ How Childhood Advertising Exposure Can Create Biased Product Evaluations That Persist into Adulthood ,” Journal of Consumer Research , 41 ( 1 ), 119 – 34 .
Deng Xiaoyan , Kahn Barbara E. ( 2009 ), “ Is Your Product on the Right Side? The ‘Location Effect’ on Perceived Product Heaviness and Package Evaluation ,” Journal of Marketing Research , 46 ( 6 ), 725 – 38 .
Du Shuili , Sen Sankar , Bhattacharya C. B. ( 2008 ), “ Exploring the Social and Business Returns of a Corporate Oral Health Initiative Aimed at Disadvantaged Hispanic Families ,” Journal of Consumer Research , 35 ( 3 ), 483 – 94 .
Dzhogleva Hristina , Lamberton Cait Poynor ( 2014 ), “ Should Birds of a Feather Flock Together? Understanding Self-Control Decisions in Dyads ,” Journal of Consumer Research , 41 ( 2 ), 361 – 80 .
Festinger Leon ( 1954 ), “ A Theory of Social Comparison Processes ,” Human Relations , 7 ( 2 ), 117 – 40 .
Fishbach Ayelet , Tu Yanping ( 2016 ), “ Pursuing Goals with Others ,” Social and Personality Psychology Compass , 10 ( 5 ), 298 – 312 .
Fitzsimons Gráinne M. , Finkel Eli J. ( 2010 ), “ Interpersonal Influences on Self-Regulation ,” Current Directions in Psychological Science , 19 ( 2 ), 101 – 5 .
Friedman Margaret L. , Churchill Gilbert A. Jr. ( 1987 ), “ Using Consumer Perceptions and a Contingency Approach to Improve Health Care Delivery ,” Journal of Consumer Research , 13 ( 4 ), 492 .
Galoni Chelsea , , Gregory S. Carpenter , and , Hayagreeva Rao ( 2020 ), “ Disgusted and Afraid: Consumer Choices under the Threat of Contagious Disease ,” Journal of Consumer Research , 47 ( 3 ), 373 – 92 .
Gawande Atul ( 2014 ), Being Mortal: Medicine and What Matters in the End , New York : Metropolitan Books/Henry Holt and Company.
Google Preview
Han Dahee , Duhachek Adam , Agrawal Nidhi ( 2016 ), “ Coping and Construal Level Matching Drives Health Message Effectiveness via Response Efficacy or Self-Efficacy Enhancement ,” Journal of Consumer Research , 43 ( 3 ), 429 – 47 .
Haws Kelly L. , Liu Peggy J. , McFerran Brent , Chandon Pierre ( 2022 ), “ Examining Eating: Bridging the Gap between ‘Lab Eating’ and ‘Free-Living Eating’ ,” Journal of the Association for Consumer Research , 7 ( 4 ), 403 – 18 .
Haws Kelly L. , Reczek Rebecca Walker , Sample Kevin L. ( 2017 ), “ Healthy Diets Make Empty Wallets: The Healthy 5 Expensive Intuition ,” Journal of Consumer Research , 43 ( 6 ), ucw078 .
Henrich Joseph , Heine Steven J. , Norenzayan Ara ( 2010 ), “ The Weirdest People in the World? ,” Behavioral and Brain Sciences , 33 ( 2-3 ), 61 – 83 .
Hirschman Elizabeth C. ( 1992 ), “ The Consciousness of Addiction: Toward a General Theory of Compulsive Consumption ,” Journal of Consumer Research , 19 ( 2 ), 155 – 79 .
Huang Yunhui , Sengupta Jaideep ( 2020 ), “ The Influence of Disease Cues on Preference for Typical versus Atypical Products ,” Journal of Consumer Research , 47 ( 3 ), 393 – 411 .
Huang Szu-Chi , Broniarczyk Susan M. , Zhang Ying , Beruchashvili Mariam ( 2015 ), “ From Close to Distant: The Dynamics of Interpersonal Relationships in Shared Goal Pursuit ,” Journal of Consumer Research , 41 ( 5 ), 1252 – 66 .
Janiszewski Chris , van Osselaer Stijn M. J. ( 2022 ), “ Abductive Theory Construction ,” Journal of Consumer Psychology , 32 ( 1 ), 175 – 93 .
Kastenbaum Robert , Derbin Valerie , Sabatini Paul , Artt Steven ( 1972 ), “ The Ages of Me’: Toward Personal and Interpersonal Definitions of Functional Aging ,” Aging and Human Development , 3 ( 2 ), 197 – 211 .
Keeffe Brian , Subramanian Usha , Tierney William M. , Udris Edmunds , Willems Jim , McDonell Mary , Fihn Stephan D. ( 2005 ), “ Provider Response to Computer-Based Care Suggestions for Chronic Heart Failure ,” Medical Care , 43 ( 5 ), 461 – 5 .
Keller Punam A. ( 2006 ), “ Regulatory Focus and Efficacy of Health Messages ,” Journal of Consumer Research , 33 ( 1 ), 109 – 14 .
Kreuter Matthew W. , McClure Stephanie M. ( 2004 ), “ The Role of Culture in Health Communication ,” Annual Review of Public Health , 25 , 439 – 55 .
Kulik James A. , Mahler Heike I. M. ( 2000 ), “Social Comparison, Affiliation, and Emotional Contagion under Threat,” in Handbook of Social Comparison , ed. Jerry Suls and Ladd Wheeler, Boston, MA : Springer , 295 – 320 .
Liu Peggy , Dallas Steven K. , Fitzsimons Gavan J. ( 2019 ), “ A Framework for Understanding Consumer Choices for Others ,” Journal of Consumer Research , 46 ( 3 ), 407 – 34 .
Longoni Chiara , Bonezzi Andrea , Morewedge Carey K. ( 2019 ), “ Resistance to Medical Artificial Intelligence ,” Journal of Consumer Research , 46 ( 4 ), 629 – 50 .
Markides Kyriakos S. , Pappas Charisse ( 1982 ), “ Subjective Age, Health, and Survivorship in Old Age ,” Research on Aging , 4 ( 1 ), 87 – 96 .
Markus Hazel R. , Kitayama Shinobu ( 1991 ), “ Culture and the Self: Implications for Cognition, Emotion, and Motivation ,” Psychological Review , 98 ( 2 ), 224 – 53 .
McFerran Brent , Dahl Darren W. , Fitzsimons Gavan J. , Morales Andrea C. ( 2010 ), “ I’ll Have What She’s Having: Effects of Social Influence and Body Type on the Food Choices of Others ,” Journal of Consumer Research , 36 ( 6 ), 915 – 29 .
Menon Geeta , Block Lauren G. , Ramanathan Suresh ( 2002 ), “ We’re at as Much Risk as We Are Led to Believe: Effects of Message Cues on Judgments of Health Risk ,” Journal of Consumer Research , 28 ( 4 ), 533 – 49 .
Moorman Christine , Matulich Erika ( 1993 ), “ A Model of Consumers’ Preventive Health Behaviors: The Role of Health Motivation and Health Ability ,” Journal of Consumer Research , 20 ( 2 ), 208 – 28 .
Palmeira Mauricio , Spassova Gerri ( 2015 ), “ Consumer Reactions to Professionals Who Use Decision Aids ,” European Journal of Marketing , 49 ( 3/4 ), 302 – 26 .
Park Jen H , Huang Szu‐chi , Rozenkrants Bella , Kupor Daniella ( 2021 ), “ Subjective Age and the Greater Good ,” Journal of Consumer Psychology , 31 ( 3 ), 429 – 49 .
Peltzman Sam ( 1975 ), “ The Effects of Automobile Safety Regulation ,” Journal of Political Economy , 83 ( 4 ), 677 – 725 .
Rad Mostafa Salari , Martingano Alison Jane , Ginges Jeremy ( 2018 ), “ Toward a Psychology of Homo Sapiens: Making Psychological Science More Representative of the Human Population ,” Proceedings of the National Academy of Sciences of the United States of America , 115 ( 45 ), 11401 – 5 .
Raghunathan Rajagopal , Naylor Rebecca Walker , Hoyer Wayne D. ( 2006 ), “ The Unhealthy = Tasty Intuition and Its Effects on Taste Inferences, Enjoyment, and Choice of Food Products ,” Journal of Marketing , 70 ( 4 ), 170 – 84 .
Reiss Julian ( 2019 ), “ Against External Validity ,” Synthese , 196 ( 8 ), 3103 – 21 .
Ross Lee , Nisbett Richard E. ( 2011 ), The Person and the Situation: Perspectives of Social Psychology , London, UK : Pinter & Martin Publishers.
Samper Adriana , Schwartz Janet A. ( 2013 ), “ Price Inferences for Sacred versus Secular Goods: Changing the Price of Medicine Influences Perceived Health Risk ,” Journal of Consumer Research , 39 ( 6 ), 1343 – 58 .
Scott Sydney E. , Rozin Paul , Small Deborah A. ( 2020 ), “ Consumers Prefer ‘Natural’ More for Preventatives than for Curatives ,” Journal of Consumer Research , 47 ( 3 ), 454 – 71 .
Shaffer Victoria A. , Probst C. Adam , Merkle Edgar C. , Arkes Hal R. , Medow Mitchell A. ( 2013 ), “ Why Do Patients Derogate Physicians Who Use a Computer-Based Diagnostic Support System? ,” Medical Decision Making , 33 ( 1 ), 108 – 18 .
Shiv Baba , Carmon Ziv , Ariely Dan ( 2005 ), “ Placebo Effects of Marketing Actions: Consumers May Get What They Pay For ,” Journal of Marketing Research , 42 ( 4 ), 383 – 93 .
Strull William M. , Lo Bernard , Charles Gerald ( 1984 ), “ Do Patients Want to Participate in Medical Decision Making? ,” JAMA: The Journal of the American Medical Association , 252 ( 21 ), 2990 – 4 .
Szasz Thomas S. , Hollender Marc H. ( 1956 ), “ A Contribution to the Philosophy of Medicine: The Basic Models of the Doctor-Patient Relationship ,” A.M.A. Archives of Internal Medicine , 97 ( 5 ), 585 – 92 .
Tesser Abraham ( 1988 ), “ Toward a Self-Evaluation Maintenance Model of Social Behavior ,” Advances in Experimental Social Psychology , 21 ( C ), 181 – 227 .
Thomas Michael ( 2019 ), “ Was Television Responsible for a New Generation of Smokers? ,” Journal of Consumer Research , 46 ( 4 ), 689 – 707 .
Thompson Craig J. , Troester Maura ( 2002 ), “ Consumer Value Systems in the Age of Postmodern Fragmentation: The Case of the Natural Health Microculture ,” Journal of Consumer Research , 28 ( 4 ), 550 – 71 .
Tian Kelly , Sautter Pookie , Fisher Derek , Fischbach Sarah , Luna-Nevarez Cuauhtemoc , Boberg Kevin , Kroger Jim , Vann Richard ( 2014 ), “ Transforming Health Care: Empowering Therapeutic Communities through Technology-Enhanced Narratives ,” Journal of Consumer Research , 41 ( 2 ), 237 – 60 .
Tjale A. A. , Bruce J. ( 2007 ), “ A Concept Analysis of Holistic Nursing Care in Paediatric Nursing ,” Curationis , 30 ( 4 ), 45 – 52 .
Ubel Peter A. , Spranca Mark D. , Dekay Michael L. , Hershey John C. , Asch David A. ( 1998 ), “ Public Preferences for Prevention versus Cure: What If an Ounce of Prevention Is Worth Only an Ounce of Cure? ,” Medical Decision Making , 18 ( 2 ), 141 – 8 .
Vig Elizabeth K. , Starks Helene , Taylor Janelle S. , Hopley Elizabeth K. , Fryer-Edwards Kelly ( 2007 ), “ Surviving Surrogate Decision-Making: What Helps and Hampers the Experience of Making Medical Decisions for Others ,” Journal of General Internal Medicine , 22 ( 9 ), 1274 – 9 .
Waber Rebecca L. , Shiv Baba , Carmon Ziv , Ariely Dan ( 2008 ), “ Commercial Features of Placebo and Therapeutic Efficacy ,” JAMA—Journal of the American Medical Association , 299 ( 9 ), 1016 – 7 .
Wang Wenbo , Keh Hean Tat , Bolton Lisa E. ( 2010 ), “ Lay Theories of Medicine and a Healthy Lifestyle ,” Journal of Consumer Research , 37 ( 1 ), 80 – 97 .
Wendler David , Rid Annette ( 2011 ), “ Systematic Review: The Effect on Surrogates of Making Treatment Decisions for Others ,” Annals of Internal Medicine , 154 ( 5 ), 336 – 46 .
Wood Stacy , Schulman Kevin ( 2019 ), “ The Doctor-of-the-Future Is In: Patient Responses to Disruptive Health-Care Innovations ,” Journal of the Association for Consumer Research , 4 ( 3 ), 231 – 43 .
Yaniv Ilan ( 2011 ), “ Group Diversity and Decision Quality: Amplification and Attenuation of the Framing Effect ,” International Journal of Forecasting , 27 ( 1 ), 41 – 9 .
Zikmund-Fisher Brian J. , Sarr Brianna , Fagerlin Angela , Ubel Peter A. ( 2006 ), “ A Matter of Perspective: Choosing for Others Differs from Choosing for Yourself in Making Treatment Decisions ,” Journal of General Internal Medicine , 21 ( 6 ), 618 – 22 .
Email alerts
Citing articles via.
- X (formerly Twitter)
- Recommend to your Library
Affiliations
- Online ISSN 1537-5277
- Print ISSN 0093-5301
- Copyright © 2024 Journal of Consumer Research Inc.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Consumerism and Implications for Good Health and Well-Being
- Living reference work entry
- First Online: 11 July 2020
- Cite this living reference work entry

- Dmitry Tikhaze 7 &
- Anastassia Kurilova 7
Part of the book series: Encyclopedia of the UN Sustainable Development Goals ((ENUNSDG))
271 Accesses
Consumerism as a culture of overconsumption and a system of values and standards with the core focus on consumption is found to be in close correlation with human health and well-being. On the one hand, growing consumption contributes substantially to the reduction of poverty, hunger, and diseases, that is, to the health and well-being of the global population. On the other hand, the growth of consumption entails increased demand for natural resources, and consumer product manufacturing is one of the major sources of environmental pollution seriously affecting human health. The concept of sustainable development has emerged as a response to these challenges, vectoring product consumption toward human and environmental well-being, and the consumer society is making every effort to mitigate the negative impact.
Consumerism
Consumption has become one of the major factors of economic growth in modern societies (Miller and Rose 2008 ; Ritzer and Miles 2019 ). Modern economies...
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Ahuvia AC (2005) Beyond the extended Self: loved objects and consumers’ identity narratives. J Consum Res 32(1):171–184. https://doi.org/10.1086/429607
Article Google Scholar
Ahuvia AC (2008) If money doesn’t make us happy, why do we act as if it does? J Econ Psychol 29(4):491–507. https://doi.org/10.1016/j.joep.2007.11.005
Ahuvia AC (2018) Consumption, income and happiness. In: Lewis A (ed) The Cambridge handbook of psychology and economic behavior. Cambridge University Press, Cambridge, MA, pp 307–339. https://doi.org/10.1017/9781316676349.011
Chapter Google Scholar
Ahuvia AC, Izberk-Bilgin E (2013) Well-being in consumer societies. In: Boniwell I, David SA, Conley Ayers A (eds) Oxford handbook of happiness. Oxford University Press, Oxford, pp 483–497. https://doi.org/10.1093/oxfordhb/9780199557257.013.0037
Angus A, Westbrook G (2019) Top 10 global consumer trends 2019. Euromonitor International, London
Google Scholar
Baudrillard J (2006) The consumer society: myths and structures. SAGE, London
Bauman Z (1987) Legislators and interpreters: on modernity, post-modernity, and intellectuals. Polity Press, Cambridge, UK
Bauman Z (2008) Consuming life. Polity Press, Cambridge, MA
Baumann S, Szabo M, Johnston J (2019) Understanding the fool preference of people of low socioeconomic status. J Consum Cult 19(3):316–339. https://doi.org/10.1177/1469540517717780
Beck U (2010) Risk society: towards a new modernity. SAGE, London
Belton T (2016) Whey becoming a “happily modest consumer” could help save the planet. https://www.weforum.org/agenda/2016/12/want-to-protect-the-planet-pursue-personal-happiness . Accessed 12 Aug 2019
Boumphrey S, Brehmer Z (2017) Megatrend analysis: putting the consumer at the heart of business. Euromonitor International, London
Brown KW, Kasser T, Ryan RM et al (2016) Materialism, spending, and affect: an event-sampling study of marketplace behavior and its affective costs. J Happiness Stud 17(6):2277–2292. https://doi.org/10.1007/s10902-015-9694-9
Campbell C (2010) What is wrong with consumerism? An assessment of some common criticisms. Anu Filosofico 43(2):279–296
Carlisle S, Hanlon P (2007) Well-being and consumer culture: a different kind of public health problem? Health Promot Int 22(3):261–268. https://doi.org/10.1093/heapro/dam022
Chalasani N, Szabo G (eds) (2016) Alcoholic and non-alcoholic fatty liver disease. Springer, Cham. https://doi.org/10.1007/978-3-319-20538-0
Book Google Scholar
Charlton E (2019) You eat a credit card’s worth of plastic a week, research says. https://www.weforum.org/agenda/2019/06/you-eat-a-credit-card-s-worth-of-plastic-a-week-research-says/ . Accessed 12 Aug 2019
Chelekis J (2011) Consumer illnesses and maladies. In: Southerton D (ed) Encyclopedia of consumer culture, vol 1. SAGE, Thousand Oaks, pp 269–272. https://doi.org/10.4135/9781412994248.n105
Chiarelli N, Yang S, Gallob S (eds) (2016) Lifestyle trends and tourism – how changing consumer behavior impacts travel to Europe. European Travel Commission, Brussels
Clarke TC, Black LI, Stussman BJ et al (2015) Trends in the use of complementary health approaches among adults: United States, 2002–2012. National Center for Health Statistics, Hyattsville
Cook DT (2010) Commercial enculturation: moving beyond consumer socialization. In: Buckigham D, Tingstad V (eds) Childhood and consumer culture. Palgrave Macmillan, London, pp 63–79. https://doi.org/10.1057/9780230281844_5
Csikszentmihalyi M (2014) Reflections and reviews. In: Applications of flow in human development and education. Springer, Dordrecht, pp 117–127. https://doi.org/10.1007/978-94-017-9094-9_5
Danziger PN (2017) Why instant gratification isn’t so gratifying. Forbes. https://www.forbes.com/sites/pamdanziger/2017/09/19/why-instant-gratification-isnt-so-gratifying/#1a205f575725 . Accessed 12 Aug 2019
Deloitte (2017) Global mobile consumer trends, 2nd edition: mobile continues its global reach into all aspects of consumers’ lives. Deloitte
Deloitte (2018) Global mobile consumer survey, US edition: overview of results. Deloitte
Deloitte (2019) Global powers of luxury goods 2019: bridging the gap between the old and the new. Deloitte
Development Initiatives (2018) 2018 global nutrition report: shining a light to spur action on nutrition. Development Initiatives, Bristol
Di Meglio E, Kaczmarek-Firth A, Litwinska A et al (2018) Living conditions in Europe – 2018 edition. Eureostat, Luxembourg
Dittmar H, Bond R, Hurst M et al (2014) The relationship between materialism and personal well-being: a meta-analysis. J Pers Soc Psychol 107(5):879–924. https://doi.org/10.1037/a0037409
Dowman JK, Farrell GC, Newsome P (2016) NAFLD: a worldwide problem. In: Williams R, Taylor-Robinson SD (eds) Clinical dilemmas in non-alcoholic fatty liver disease. Wiley-Blackwell, Chichester, pp 8–14
Drucker PF, Maciariello JA (2009) Management. Collins, London
Ellen MacArthur Foundation (2017) The new plastics economy: rethinking the future of plastics & catalysing action. Ellen MacArthur Foundation. https://www.ellenmacarthurfoundation.org/assets/downloads/publications/NPEC-Hybrid_English_22-11-17_Digital.pdf . Accessed 12 Aug 2019
Ellen MacArthur Foundation (2018) Circular consumer electronics: an initial exploration. Ellen MacArthur Foundation. https://www.ellenmacarthurfoundation.org/assets/downloads/Circular-Consumer-Electronics-2704.pdf . Accessed 12 Aug 2019
Ellen MacArthur Foundation (2019a) Circular economy in cities: project guide. Ellen MacArthur Foundation. https://www.ellenmacarthurfoundation.org/assets/downloads/CE-in-Cities-Project-Guide_Mar19.pdf . Accessed 12 Aug 2019
Ellen MacArthur Foundation (2019b) Cities and circular economy for food. Ellen MacArthur Foundation. https://www.ellenmacarthurfoundation.org/assets/downloads/Cities-and-Circular-Economy-for-Food_280119.pdf . Accessed 12 Aug 2019
Erner G (2004) Victimes de la mode? Comment on la crée, pourquoi on la suit. Éditions La Découverte, Paris
Euromonitor Research (2017) Wellness as status symbol: a top consumer trend for 2017. Euromonitor International, London. https://blog.euromonitor.com/wellness-status-symbol-top-consumer-trend-2017/ . Accessed 12 Aug 2019
Faber RJ (2004) Self-control and compulsive buying. In: Kasser T, Kanner AD (eds) Psychology and consumer culture: the struggle for a good life in a materialistic world. American Psychological Association, Washington, DC, pp 169–187
Fiolet T, Srour B, Sellem L (2018) Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ 360. https://doi.org/10.1136/bmj.k322
Gilinsky YI (2012) Deviantnost’ v obshchestve potrebleniya: kratkiy obzor (Deviation in the consumer society: a short review). In: Gilinsky YI, Shipunova TV (eds) Deviantnost’ v obshchestve potrebleniya (Deviation in the consumer society). Alef-Press, St. Petersburg, pp 101–127
Grossmann GN (2007) Teoreticheskiye osnovy biokompensatsionnogo podkhoda k lecheniyu alimentarnogo ozhireniya (The theoretical base of the biocompensating approach to the therapy of alimentary obesity). https://sites.google.com/site/galinagross2/o-doktore-galine-grossmann . Accessed 12 Aug 2019
Hanlon P, Carlisle S (2009) Is “modern culture” bad for our health and well-being? Glob Health Promot 16(4):27–34. https://doi.org/10.1177/1757975909348113
Helliwell J, Layard R, Sachs J (2018) World happiness report 2018. Sustainable Development Solutions Network, New York
Hilton M (2008) The death of a consumer society. Trans R Hist Soc 18:211–236. https://doi.org/10.1017/S0080440108000716
Hodgson A (2018) Meeting the demands of high net-worth individuals. Euromonitor International, London
Holbrook MB (ed) (1999) Consumer value: a framework for analysis and research. Routledge, London
Huikari N (2016) The consumption of well-being: developing consumption practices of well-being in the context of medicalized water. Aalto University, Helsinki. https://aaltodoc.aalto.fi/handle/123456789/20631 . Accessed 12 Aug 2019
Il’in VI (2011) Kreativnyy konsyumerizm kak trend sovremennogo obshchestva potrebleniya (Creative consumerism as a trend of a modern consumer society). Zhurnal sotsiologii i sotsial’noy antropologii (J Sociol Soc Anthr) 5:41–54
Il’in VI (2012) Deviantnost’ v obshchestve potrebleniya: prostranstvo vozmozhnostey, prostranstvo zhelaniy (Deviation in the consumer society: the space of possibilities, the space of desires). In: Gilinsky YI, Shipunova TV (eds) Deviantnost’ v obshchestve potrebleniya (Deviation in the consumer society). Alef-Press, St. Petersburg, pp 9–24
Il’in VI (2014) Dual’nost’ struktur individual’nogo potrebleniya v istoricheskoy dinamike: ot sovetskogo k postsovetskomu obshchestvu (Duality of structures of individual consumption: from the soviet to the post-soviet society). Labirint (Labyrinth) 2:9–18
Il’in VI (2018) Sotsiologiya potrebleniya (Sociology of consumption). Urait, Moscow
Kahle LR (1986) The nine nations of North America and the value basis of geographic segmentation. J Mark 50(2):37–47. https://doi.org/10.2307/1251598
Kasser T (2002) The high price of materialism. The MIT Press, Cambridge, MA
Kasser T (2016) Materialistic values and goals. Annu Rev Psychol 67:489–514. https://doi.org/10.1146/annurev-psych-122414-033344
Kosyakova VA (2018) Apokalipsis Sednevekov’ya. Iyeronim Boskh, Ivan Groznyy, Konets Sveta (The Apocalypse of the Middle Ages. Hieronimus Bosch, Ivan the Terrible, End of the World). AST, Moscow
Lee L, Böttger TM (2018) The therapeutic utility of shopping: retail therapy, emotion regulation, and well-being. In: Solomon MR, Lowrey TM (eds) The Routledge companion to consumer behavior. Routledge, New York, pp 38–61. https://doi.org/10.4324/9781315526935
Levy SL (2018) A history of the study of consumer behavior. In: Solomon MR, Lowrey TM (eds) The Routledge companion to consumer behavior. Routledge, New York, pp 3–13. https://doi.org/10.4324/9781315526935
Li D, Suh S (2019) Health risks of chemicals in consumer products: a review. Environ Int 123:580–587. https://doi.org/10.1016/j.envint.2018.12.033
Article CAS Google Scholar
Lipovetsky G, Serroy J (2016) L’esthétisation du monde: vivre à l’âge du capitalisme artiste. Gallimard, Paris
Liu LU, Schiano TD (2007) Hepatotoxicity of herbal medicines, vitamins, and natural hepatotoxins. In: Kaplowitz N, DeLeve LD (eds) Drug-induced liver disease. Informa Healthcare, New York, pp 733–754
Lobaugh KM, Stephens B, Simpson J (2019) The consumer is changing, but perhaps not how you think. Deloitte. https://www2.deloitte.com/us/en/insights/industry/retail-distribution/the-consumer-is-changing.html . Accessed 12 Aug 2019
Mascaraque M (2019) Top 5 trends in health and wellness. Euromonitor International, London
Miles S (2018) The emergence of contemporary consumer culture. In: Kravets O, Maclaran P, Miles S, Venkatesh A (eds) The SAGE handbook of consumer culture. SAGE, London, pp 13–26. https://doi.org/10.4135/9781473998803.n2
Miller P, Rose N (1997) Mobilizing the consumer: assembling the subject of consumption. Theory Cult Soc 14(1):1–36. https://doi.org/10.1177/026327697014001001
Miller P, Rose N (2008) Governing the present: administering economic, social and personal life. Polity Press, Cambridge, UK
Mind (2008) Debt and mental health. Mind, London
OECD (2019) Main economic indicators, vol 2019, issue 8. OECD Publishing, Paris. https://doi.org/10.1787/mei-v2019-8-en
Patient@Home (2018) Health consumerism: when health becomes a consumer good. Patient@Home, Odense
PlasticsEurope (2018) Plastics – the facts 2018: an analysis of European plastics production, demand and waste data. PlasticsEurope, Brussels
Reith G (2018) Addictive consumption: capitalism, modernity and excess. Routledge, London. https://doi.org/10.4324/9780429464447
Reynolds A, Mann J, Cummings J et al (2019) Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet 393:434–445. https://doi.org/10.1016/S0140-6736(18)31809-9
Rico-Campà A, Martínez-González MA, Alvarez-Alvarez I et al (2019) Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ 365. https://doi.org/10.1136/bmj.l1949
Ritzer G (2014) Prosumption: evolution, revolution, or eternal return of the same? J Consum Cult 14(1):3–24. https://doi.org/10.1177/1469540513509641
Ritzer G (2015) The dehumanized consumer: does the prosumer offer some hope? In: Garcia Martinez AN (ed) Being human in a consumer society. Ashgate, Farnham, pp 25–40
Ritzer G (2019) The McDonaldization of society. SAGE, Thousand Oaks
Ritzer G, Miles S (2019) The changing nature of consumption and the intensification of McDonaldization in the digital age. J Consum Cult 19(1):3–20. https://doi.org/10.1177/1469540518818628
Rodriguez M (2019) Planet fitness. Health Club Manag 271:50–55
Rustagi N, Shrum LJ (2018) Materialism: conceptualizations, antecedents, and consequences. In: Solomon MR, Lowrey TM (eds) The Routledge companion to consumer behavior. Routledge, New York, pp 21–37. https://doi.org/10.4324/9781315526935
Sarkar C, Webster C, Gallacher J (2018) Lancet Planet Health 2(10):438–450. https://doi.org/10.1016/S2542-5196(18)30208-0
Schneider Electric, Global Footprint Network (2019) The business case for one-planet prosperity. Schneider Electric, Global Footprint Network, Rueil-Malmaison, Oakland
Seeff L, Stickel F, Navarro VJ (2013) Hepatotoxicity of herbals and dietary supplements. In: Kaplowitz N, DeLeve L (eds) Drug-induced liver disease. Elsevier, London, pp 631–657
Shridhar A (2019) Top consumer trends impacting health and nutrition. Euromonitor International, London
Slater D (2005) Consumer culture. In: Ritzer G (ed) Encyclopedia of social theory. SAGE, Thousand Oaks, pp 139–145
Solomon S, Greenberg J, Pyszczynski T (2004) Lethal consumption: death-denying materialism. In: Kasser T, Kanner AD (eds) Psychology and consumer culture: the struggle for a good life in a materialistic world. American Psychological Association, Washington, DC, pp 127–146
Sortheix FM, Schwartz SH (2017) Values that underlie and undermine well-being: variability across countries. Eur J Personal 31(2):187–201. https://doi.org/10.1002/per.2096
Stearns PN (2001) Consumerism in world history: the global transformation of desire. Routledge, New York
Swinburn BA, Kraak VI, Allender S et al (2019) The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet 393:791–846. https://doi.org/10.1016/S0140-6736(18)32822-8
Trentmann F (2009) Crossing divides: consumption and globalization in history. J Consum Cult 9(2):187–220. https://doi.org/10.1177/1469540509104374
United Nations (2017a) 2017 HLPF on sustainable development: expert group meeting on integrated approaches to implementing Sustainable Development Goal 3. United Nations, New York
United Nations (2017b) 2017 HLPF thematic review of SDG3: ensure healthy lives and promote well-being for all at all ages. https://sustainabledevelopment.un.org/content/documents/14367SDG3format-rev_MD_OD.pdf . Accessed 12 Aug 2019
United Nations (2017c) President’s summary of 2017 High-level political forum on sustainable development. United Nations. https://www.sustainabledevelopment.un.org/content/documents/16673HLPF_2017_Presidents_summary.pdf . Accessed 15 Aug 2019
United Nations (2018) World economic and social survey 2018: frontier technologies for sustainable development. United Nations, New York
United Nations (2019a) Goal 12: ensure sustainable consumption and production patterns. United Nations. https://www.un.org/sustainabledevelopment/sustainable-consumption-production . Accessed 12 Aug 2019
United Nations (2019b) Microplastic pollution is everywhere, but not necessarily a risk to human health. United Nations. https://news.un.org/en/story/2019/08/1044661 . Accessed 23 Aug 2019
United Nations (2019c) Progress towards the Sustainable Development Goals. Report of the Secretary-General. United Nations. https://sustainabledevelopment.un.org/content/documents/22700E_2019_XXXX_Report_of_the_SG_on_the_progress_towards_the_SDGs_Special_Edition.pdf . Accessed 12 Aug 2019
United Nations (2019d) The Sustainable Development Goals report 2019. United Nations, New York
United Nations (2019e) World economic situation and prospects 2019. United Nations, New York
United Nations Department of Economic and Social Affairs (2019) World urbanization prospects: the 2018 revision. United Nations, New York
United Nations Development Programme (1998) Human development report 1998. Oxford University Press, New York
United Nations Development Programme, Oxford Poverty and Human Development Initiative (2019) Global Multidimensional Poverty Index 2019: illuminating inequalities. United Nations Development Programme, Oxford Poverty and Human Development Initiative. https://www.hdr.undp.org/sites/default/files/mpi_2019_publication_0.pdf . Accessed 1 Aug 2019
United Nations Environment Programme (2019) Global resources outlook 2019: natural resources for the future we want. United Nations Environment Programme, Paris
Warde A (2017) Consumption: a sociological analysis. Palgrave Macmillan, London
Wertz J (2018) Why instant gratification is the one marketing tactic companies should focus on right now. Forbes. https://www.forbes.com/sites/jiawertz/2018/04/30/why-instant-gratification-is-the-one-marketing-tactic-companies-should-focus-on-right-now/#74e82a2ae91b . Accessed 12 Aug 2019
Willett W, Rockström J, Loken B et al (2019) Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet 393:447–492. https://doi.org/10.1016/S0140-6736(18)31788-4
Williams RJ (1973) Nutrition against disease: environmental prevention. Bantam Books, New York
World Economic Forum (2017) Shaping the future of global food systems: a scenarios analysis. World Economic Forum, Geneva
World Economic Forum (2019a) Accelerating consumer health and well-being. https://www.weforum.org/projects/accelerating-consumer-health-and-well-being . Accessed 20 Aug 2019
World Economic Forum (2019b) Health and healthcare in the fourth industrial revolution: Global Future Council on the Future of Health and Healthcare 2016–2018. World Economic Forum, Geneva
World Health Organization (2017a) Incentives and disincentives for reducing sugar in manufactured foods: an exploratory supply chain analysis. World Health Organization Regional Office for Europe, Copenhagen
World Health Organization (2017b) Ten years in public health, 2007–2017: report by Dr. Margaret Chan, Director-General, World Health Organization. World Health Organization, Geneva
World Health Organization (2018a) Using dietary intake modelling to achieve population salt reduction: a guide to developing a country-specific salt reduction model. World Health Organization Regional Office for Europe, Copenhagen
World Health Organization (2018b) World health statistics 2018: monitoring health for the SDGs, sustainable development goals. World Health Organization, Geneva
World Health Organization (2019) Global health observatory data: risk factors. https://who.int/gho/ncd/risk_factors/en/ . Accessed 12 Aug 2019
World Health Organization, Secretariat of the Convention on Biological Diversity (2015) Connecting global priorities: biodiversity and human health: a state of knowledge review. World Health Organization/Secretariat of the Convention on Biological Diversity, Geneva/Quebec
WWF (2019) Solving plastic pollution through accountability. WWF International, Glan
Download references

Author information
Authors and affiliations.
Moscow, Russia
Dmitry Tikhaze & Anastassia Kurilova
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Dmitry Tikhaze .
Editor information
Editors and affiliations.
European School of Sustainability, Hamburg University of Applied Sciences, Hamburg, Hamburg, Germany
Walter Leal Filho
International Centre for Thriving, University of Chester, Chester, UK
Center for Neuroscience & Cell Biology, University of Coimbra, Coimbra, Portugal
Anabela Marisa Azul
Faculty of Engineering and Architecture, Passo Fundo University Faculty of Engineering and Architecture, Passo Fundo, Brazil
Luciana Brandli
Istinye University, Istanbul, Turkey
Pinar Gökcin Özuyar
Section Editor information
Department of Economics, Asian University for Women, Chattogram, Bangladesh
Meherun Ahmed
Rights and permissions
Reprints and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this entry
Cite this entry.
Tikhaze, D., Kurilova, A. (2020). Consumerism and Implications for Good Health and Well-Being. In: Leal Filho, W., Wall, T., Azul, A., Brandli, L., Özuyar, P. (eds) Good Health and Well-Being. Encyclopedia of the UN Sustainable Development Goals. Springer, Cham. https://doi.org/10.1007/978-3-319-69627-0_122-1
Download citation
DOI : https://doi.org/10.1007/978-3-319-69627-0_122-1
Received : 12 November 2019
Accepted : 14 November 2019
Published : 11 July 2020
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-69627-0
Online ISBN : 978-3-319-69627-0
eBook Packages : Springer Reference Earth and Environm. Science Reference Module Physical and Materials Science Reference Module Earth and Environmental Sciences
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Editorial: Consumer Engagement in Health and Well-being: Theoretical and Empirical Perspectives in Patient Centered Medicine
Guendalina graffigna, elena vegni.
- Author information
- Article notes
- Copyright and License information
Edited by: Gianluca Castelnuovo, Università Cattolica del Sacro Cuore, Italy
Reviewed by: Go Yoshizawa, Osaka University, Japan
*Correspondence: Guendalina Graffigna [email protected]
This article was submitted to Clinical and Health Psychology, a section of the journal Frontiers in Psychology
Received 2017 Mar 22; Accepted 2017 Sep 29; Collection date 2017.
Keywords: consumer engagement, health, well-being, patient-centered medicine, health behavior
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
The growing understanding of the key role of people in improving healthy behaviors and clinical outcomes has led healthcare to search for innovative ways to foster individuals' roles in the care and health promotion processes. It comes as no surprise, therefore, that making consumers active agents in their health and care is up today recognized as a key priority for services' innovation. In the era of participatory health, the concept of “engagement” may be particularly promising to give consumers a starring role in managing their health and well-being.
The healthcare field has recently introduced the term “engagement” in its lexicon to call for a renewed partnership among the actors (i.e., patients, caregivers, practitioners, decision makers…) implied in the health and care management. Overall, the concept of engagement attempts to offer a compass for action in the current complex and uncertain context of healthcare design and health promotion initiatives. The main aim is giving (back) a leading role to patients and taking them on board for a more efficient and effective process of care delivery and of health promotion initiatives. Furthermore, consumer health engagement can be the key to systematically diagnose and make sense of the different organizational, relational, and psychological components in play in the dynamic exchange between “demand” and “supply” of health and care. This challenge could or even should be integrated with a complex attempt coming from the literature on medicine and regarding a new medical model that should be offered to patients/clients/consumers: that of a patient centered medicine, based on a biopsychological epistemology.
Patient engagement may be defined as an umbrella term that qualifies the systemic relation that occurs between the demand and the supply of healthcare, at different levels and in different situation. If considered according to this meaning, patient engagement overarches the other terms more traditionally used to denote the active role of patients in their care such as patient adherence, patient compliance, patient involvement, patient participation, and patient activation (Graffigna et al., 2016 ).
Precisely, the concept of “activation” differs from the concept of “engagement” since it is mainly referred to the knowledge, attitude, and skills of patients in their self-management; while the concept of “engagement” is also applicable to the patients' proactive role in other settings, such as health promotion and prevention. Furthermore, the motivational and emotional nature of “engagement” is crucial and differentiates this concept from activation which is rather more cognitive and behavioral in its nature.
Other concepts are strongly anchored to the area of disease management. For instance, the classical concepts of “adherence” and “compliance” express a hierarchical representation of the clinical consultation, where the healthcare professional is considered as “the expert” and he/she prescribes to the patient (not expert) the rules to manage his/her disease. These concepts imply the implicit evaluation of the patient behavior in self-management such as more or less good, more or less able to respond adequately to the expert's requirements (Haynes et al., 1979 ; Vlasnik et al., 2005 ). Furthermore, these concepts evoke a medicalizing idea of the patient such as passive and needing to be correct in order to better functioning, not only at the clinical but also at the psychosocial level. It is evident how the concept of “engagement” move from a very different philosophy and representation of the patient role along the healthcare journey. From this perspective, the different actors implied in the healthcare journey are considered “experts” based on their specific subjective experience of illness and of its management. The concept of “engagement” aims at democratizing the clinical consultation and at legitimizing care receivers in a more starring role.
On the other hand, the concepts of “involvement” and “participation,” refers instead to the dyadic context of the medical consultation and the cognitive/emotional attitude of the patient to the negotiation of clinical decision making. There is an evident conceptual link between the concepts of “involvement,” “participation,” and the concept of “engagement.” All of these concepts advocate for the proactive role of patients in the decisions about care. However, these concepts relate to different levels of healthcare services demand-supply exchange (Murray et al., 2006 ; Thompson, 2007 ), since the concepts of “involvement” and “participation” are mostly limited to the dyadic context of the doctor-patient consultation in shared decision making, whereas the concept of “engagement,” refers to the role of patients and to how he/she approaches the healthcare system in its complexity (where medical consultation is one of the possible settings).
Finally, the concept of “empowerment” entertains evident areas of overlapping and potential synergies with the concept of “engagement,” although with a different breadth. The concept of “empowerment” relates to the level of patients' power and of agency upon their healthcare condition. Particularly, “empowerment” refers to patients' reacquisition of the subjective sense of control over their disease (Aujoulat et al., 2007 ). Given this definition, “empowerment” may be defined as a potential prerequisite for the process of engagement, although in turn it is fed by the good experiences that the patient makes in his evolutionary journey of exchange with the healthcare system, and thus along the “patient engagement journey” itself. Furthermore, if “empowerment” is primarily a cognitive and behavioral condition, “engagement” is nurtured by the emotional and motivational components of patients experiences along the care pathway.
Alongside with this desire to engage patients a tendency toward a more patient centered clinical intervention has developed. At the end of the 60 s, Balint introduced the term of patient centered medicine focusing the attention, during the medical encounter, not only to the biological-technical aspects but also on the emotional and relational dimensions (Balint, 1964 ). The patient-centered medicine is a large concept variously described, till to the proposal of a “transformed clinical method” by the Canadian group: they suggested to involve the patient and consider his/her own perspective (Stewart et al., 2003 ) not only in the clinical encounter but in the process of care. The patient centered medicine is conceptualized as a clinical method of a bio-psycho-social model of care and has the aim to transform the clinical approach to patients and enhance their involvement. So far, patient engagement and the patient-centered medicine seem to have a common ground and similar aims, but their overlapping is not clear and not frequently explored in the literature. Furthermore, shared guidelines about how to translate into the clinical practice the imperative of patient engagement have still to come. In this light, this Frontiers Research Topics has been conceived as an arena to bridge research and theoretical expertise mastered in different disciplinary domains in order to set the ground for a shared definition of what consumer engagement in health and well-being is and on useful guidelines for practice a consumer engagement in a patient centered medicine.
We invited authors from different disciplinary domains to contribute original as well as review article in order to set a debate about patient engagement applications and its conceptual relationship with patient centered medicine.
In the present issue, readers will find the two concepts differently approached. The importance of engagement in health and well-being increased in the last years outlining the role of patient and legitimizing the starring role in the care receivers is described in the contribution by Bigi : in particular the issue that engagement involves a profound change in the doctor's behavior is discussed. The increase of chronic diseases has highlighted the need for increased engagement in patients ( Menichetti and Graffigna Zhang et al. ). Menichetti and Graffigna underlined the importance of intervention (PHEinAction) to support patient engagement and lifestyle change and maintenance, facilitating emotional and psychological processes. The relevance of emotion in engagement process appears also in the study conducted on patients with HIV by Leone et al . The importance of this construct in cancer studies ( Villani et al. Saita et al. ), and mental health studies ( Degli Stefani and Biasutti Singh et al. Oliveira-Maia et al. ) seems to suggest the usefulness of psychosocial interventions in addressing the care, for patients and the family. Last but not least, the training for health care workers appears to be crucial in order to enable cares to engage patient, particularly for nurses to learn strategies and assessment measures in clinical practice are key points in supporting the realization of patient engagement in healthcare ( Barello et al. ).
Author contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The handling Editor declared a shared affiliation, though no other collaboration, with one of the authors, GG.
- Aujoulat I., d'Hoore W., Deccache A. (2007). Patient empowerment in theory and practice: polysemy or cacophony? Patient Educ. Couns. 66, 13–20. 10.1016/j.pec.2006.09.008 [ DOI ] [ PubMed ] [ Google Scholar ]
- Balint M. (1964). The Doctor, His Patient and the Illness. Pitman Medical Publishing Co., LTD [ Google Scholar ]
- Graffigna G., Barello S., Triberti S. (2016). Patient Engagement: a Consumer-Centered Model to Innovate Healthcare. Walter de Gruyter GmbH & Co. KG. [ Google Scholar ]
- Haynes R. B., Taylor D. W., Sackett D. L. (eds.). (1979). Compliance in Health Care. Baltimore, MD: Johns Hopkins University Press. [ Google Scholar ]
- Murray E., Charles C., Gafni A. (2006). Shared decision-making in primary care: tailoring the Charles et al. model to fit the context of general practice. Patient Educ. Couns. 62, 205–211. 10.1016/j.pec.2005.07.003 [ DOI ] [ PubMed ] [ Google Scholar ]
- Stewart M., Brown J. B., Weston W. W., McWhinney I. R., McWilliam C. L., Freeman T. R. (2003). Patient Centered Medicine Transforming the Clinical Method. Oxon: Redcliffe Medical Press. [ Google Scholar ]
- Thompson A. G. (2007). The meaning of patient involvement and participation in health care consultations: a taxonomy. Soc. Sci. Med. 64, 1297–1310. 10.1016/j.socscimed.2006.11.002 [ DOI ] [ PubMed ] [ Google Scholar ]
- Vlasnik J. J., Aliotta S. L., DeLor B. (2005). Medication adherence: factors influencing compliance with prescribed medication plans. Case Manager 16, 47–51. 10.1016/j.casemgr.2005.01.009 [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (178.1 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Making Sense of “Consumer Engagement” Initiatives to Improve Health and Health Care: A Conceptual Framework to Guide Policy and Practice
Jessica n mittler, grant r martsolf, shannon j telenko, dennis p scanlon.
- Author information
- Article notes
- Copyright and License information
Address correspondence to : Jessica Mittler, Pennsylvania State University, 601L Ford Building, University Park, PA 16802 (email: [email protected] ).
Issue date 2013 Mar.
Policymakers and practitioners continue to pursue initiatives designed to engage individuals in their health and health care despite discordant views and mixed evidence regarding the ability to cultivate greater individual engagement that improves Americans’ health and well-being and helps manage health care costs. There is limited and mixed evidence regarding the value of different interventions.
Based on our involvement in evaluating various community-based consumer engagement initiatives and a targeted literature review of models of behavior change, we identified the need for a framework to classify the universe of consumer engagement initiatives toward advancing policymakers' and practitioners' knowledge of their value and fit in various contexts. We developed a framework that expanded our conceptualization of consumer engagement, building on elements of two common models, the individually focused transtheoretical model of behavior and the broader, multilevel social ecological model. Finally, we applied this framework to one community's existing consumer engagement program.
Consumer engagement in health and health care refers to the performance of specific behaviors (“engaged behaviors”) and/or an individual's capacity and motivation to perform these behaviors (“activation”). These two dimensions are related but distinct and thus should be differentiated. The framework creates four classification schemas, by (1) targeted behavior types (self-management, health care encounter, shopping, and health behaviors) and by (2) individual, (3) group, and (4) community dimensions. Our example illustrates that the framework can systematically classify a variety of consumer engagement programs, and that this exercise and resulting characterization can provide a structured way to consider the program and how its components fit program goals both individually and collectively.
Conclusions
Applying the framework could help advance the field by making policymakers and practitioners aware of the wide range of approaches, providing a structured way to organize and characterize interventions retrospectively, and helping them consider how they can meet the program's goals both individually and collectively.
Keywords: consumer engagement, patient activation, health behavior, conceptual framework
The ongoing pursuit of policies and programs to engage individuals in their health and health care is in large part based on their conceptual appeal. This is both the philosophical argument that individuals should have more say in their care (e.g., patient centeredness) and the performance-based argument that if obstacles to being engaged are removed (e.g., lack of information or motivation), then these active consumers will make informed decisions to behave in ways, such as selecting high-quality providers or helping design a care plan to follow, that improve the quality of their health care, their health, and their well-being and also may help contain their health care costs (e.g., Arnold 2007 ; DHHS 2008 ; Duggan et al. 2006 ; Epstein and Street 2011 ). Some people are skeptical about the power of this pathway to achieve all these desired results, especially system transformation (e.g., Berenson 2005 ; Hurley et al. 2009 ; Nichols et al. 2004 ), as the existing evidence for successful interventions is still limited and mixed, especially for efforts to stimulate behavior change in large numbers of consumers (e.g., Haynes et al. 2008 ; Ketelaar et al. 2011 ). When one community leader was asked about his community's efforts to improve consumer engagement, he said, “I think consumer engagement is the wild card. On the one hand, I think a lot of people are hopeful and see it as the missing link [to improving quality and controlling costs]. … On the other hand, I think it's a new enough topic that there's probably a fair amount of skepticism. I'll tell you [there is] skepticism; [colleagues ask,] ‘Is that even possible? Why should we be spending our time on that?’” (Alexander et al. 2009 ). This debate suggests the need for additional research into consumer engagement and for an evaluation of consumer engagement initiatives.
Meanwhile, public and private entities continue to experiment with consumer engagement initiatives. For example, the 2010 Patient Protection and Affordable Care Act (ACA) included multiple provisions to support consumer engagement, such as increasing the availability of information and assistance to consumers for decision making and resources for wellness and self-management programs (DHHS 2012 ). Private purchasers’ efforts, such as offering personal health coaching or consumer-directed health plans, also continue to grow: from 11 percent and 13 percent in 2008 to 27 percent and 23 percent in 2011, respectively (KFF-HRET 2008 , 2011 ). The $300-million Aligning Forces for Quality (AF4Q) initiative, supported by the Robert Wood Johnson Foundation, is another large national program whose goal is to improve the quality of health and health care for individuals (12.5% of the U.S. population) residing in sixteen communities nationwide by, in part, implementing community-based interventions to improve consumer engagement (AF4Q 2012 ; Painter and Lavizzo-Mourey 2008 ).
We are part of the independent team hired by the Robert Wood Johnson Foundation to evaluate the AF4Q initiative, which began in 2006 (Scanlon et al. 2012 ). Our early efforts to “make sense of” the AF4Q communities’ varied consumer engagement activities revealed that consumer engagement is multidimensional and that these dimensions need to be made explicit and to be distinguished from one another in order to describe and compare them. We needed a framework to systematically characterize the diverse and evolving array of interventions that the AF4Q communities were piloting. While there were a range of thoughtful and useful conceptual models addressing important elements of consumer engagement in the literature, none on its own could be used to characterize the diversity of strategies reflected in the current consumer engagement initiatives. The need for such a framework was revealed in our in-depth interviews with AF4Q participants, who suggested that “everyone comes at [consumer engagement] differently,” which contributed to difficulties to “thinking through … and bring[ing] some cohesion to [the consumer engagement piece]” (Alexander et al. 2009 ).
In this article we present a conceptual framework that distills the multifaceted concept of consumer engagement in health and health care into the critical analytic components that characterize community-based efforts to improve consumer engagement and help stimulate productive discussions about advancing health and health care through consumer engagement initiatives. After a brief discussion of our data and methods, we examine the meaning of the term “consumer engagement” and related concepts; offer a conceptual framework to typify and differentiate initiatives and to serve as a foundation for broad thinking and debate about the consumer engagement universe; and apply the framework to one community's consumer engagement initiative.
Data and Methods
In January 2009, we searched and reviewed the health services literature available through the PubMed database for existing conceptual models of consumer engagement in health. The phrase “consumer engagement” generated citations for twelve papers (Barraclough and Birch 2006 ; Brown et al. 2005 ; Draper and Claxton 2004 ; Fronstin 2008 ; Hibbard 2009b ; Hurley et al. 2009 ; Jones et al. 2006 ; Lee and Hoo 2006 ; Maillet and Halterman 2004 ; Northrop, Pittam, and Caan 2008 ; Rolfe, Sheehan, and Davidson 2008 ; Shaller 2007 ), of which only three (Hibbard 2009b ; Hurley et al. 2009 ; Shaller 2007 ) discussed multiple aspects of consumer engagement, and only one discussed a conceptual framework that linked higher patient “activation” to the performance of more “productive health behaviors” (Hibbard 2009b , 10).
We then turned to the gray literature, using Google to search for the phrase “‘consumer engagement’ definition health,” reviewing the first twenty web links, of which only Gruman and colleagues’ 2009 report, “A New Definition of Patient Engagement: What Is Engagement and Why Is It Important?” was useful. It alone provided a definition and a framework of consumer engagement behaviors based on a review of the literature on “patient engagement” and on environmental scans of organizations and recent conferences likely to address patient engagement.
These materials showed consumer engagement to be multidimensional and fundamentally about individual behavior change. We used Gruman and colleagues’ ( 2009 ) and Hibbard's ( 2009a , 2009b ) papers as the basis for our consumer engagement framework. These two papers suggested two core dimensions of consumer engagement: (1) behavioral (e.g., what do engaged individuals do?), represented by four types of behaviors (consumer/consumeristic, patient/medical encounter, self-management, healthy), and (2) cognitive (e.g., what are individuals’ capacity and motivation to change?), represented by activation. We built our framework from these elements and expanded it with additional, targeted review of the literature about how activation and behaviors relate to one another and how individual change is related to community change (which is the ultimate goal of AF4Q).
First, we investigated Hibbard's patient activation concept more closely, reviewing the six articles generated from a new PubMed search of “patient activation” and “Hibbard” (Hibbard and Cunningham 2008 ; Hibbard et al. 2004 , 2005 , 2007a , 2007b ; Mosen et al. 2007 ). Second, we identified and reviewed key models of behavior change in the social sciences for how the behavioral and cognitive dimensions of consumer engagement were treated. We began by searching PubMed with “‘behavior change’ models literature review,” which resulted in 114 articles, reduced to 65 by eliminating those published before 2000. Mittler reviewed the abstracts for the 65 papers, reading in full the one systematic review of models used in health behavior research (Painter et al. 2008 ). This paper identified five main theories based on their use: the transtheoretical model, social cognitive theory, health belief model, theory of reasoned action / planned behavior, and social networks / social support theory. We then investigated these five models, plus the microeconomic consumer choice theory, using textbooks and handbooks in which the literature is synthesized and distilled (Culyer and Newhouse 2000 ; Fiske, Gilbert, and Lindzey 2010 ; Glanz, Rimer, and Viswanath 2008 ; Schumaker, Ockene, and Riekert 2009 ). Martsolf wrote one-page overviews of these models, highlighting their logic, key variables, and use and findings to date. Then Mittler reviewed and further clarified these summaries, using seminal references identified as those that established and/or reviewed the theories and models being investigated.
Although Mittler was responsible for developing the framework, all of us discussed the framework's logic, variables, linkages, and scope during the first year of its development. We debated the framework's gaps, clarity, and level of detail, and our desire to develop a parsimonious framework for classifying the wide array of consumer engagement behaviors. Throughout the process, we also drew on knowledge gained from our interviews of AF4Q community members about their consumer engagement strategies and on other program materials, such as the AF4Q communities’ reports to the national program office and the Robert Wood Johnson Foundation (Scanlon et al. 2012 ).
Recognizing the lack of group- and community-level elements in the six initial models explored and based on Mittler's subsequent reading of eight review chapters (Glanz and Rimer 2008 ; Glanz and Schwartz 2008 ; Heaney and Israel 2008 ; Kegeler and Glanz 2008 ; McAlister, Perry, and Parcel 2008 ; Minkler, Wallerstein, and Wilson 2008 ; Sallis, Owen, and Fisher 2008 ; Viswanath 2008 ) about interpersonal, group, and community theories and evidence, and Painter and colleagues’ (2008) review of the model's use, we settled on the social ecological model. We decided to use this nested, multilevel model to structure the overall framework because of its ability to accommodate the universe of consumer intervention approaches. To better understand the group and community levels and dynamics, we reviewed the social cognitive, social network, and support theories and also read several updated syntheses of the social-psychology literature (Fiske 2010 ; Leary 2010 ; Swann and Bosson 2010 ; Yzerbyt and Demoulin 2010 ) and other selected, social science treatments of these levels (Helman 2001 ; Herrmann-Pillath 2010 ; Kleinman 1980 ; Kleinman and Hall-Clifford 2009 ; Lynch et al. 2002 ; Parsons 1951 ; Roblin and Becker 2009 ).
To answer questions as they arose and to keep abreast of new developments, we periodically searched for new reviews in PubMed and Google Scholar, using the terms “‘consumer engagement’ health” with “review” or “model,” and “behavior change” with “review.” In addition, when looking up seminal papers or searching for answers to questions as they arose, we used a “snowballing” process, looking at references that appeared in search engines’ “article cited by” and “articles like these” features, in order to identify relevant new or updated publications. Here we cite the most recent updated versions of materials wherever possible.
We “tested” and improved the framework by applying it to different types of engagement activities being implemented by AF4Q participants. We further refined the framework using feedback on the schematic and draft explanation by the other AF4Q evaluation investigators, several AF4Q consumer engagement leaders, and ultimately from reviewers during the publication process. Finally, we applied the framework to one AF4Q community, Washington State's Puget Sound Health Alliance, which had many consumer engagement activities of different scope, used a variety of approaches, and targeted different engaged behaviors. Its consumer engagement program in 2008/2009 provided a good opportunity to show how the framework could be used to help make sense of existing consumer engagement initiatives by classifying the program's activities. Information about the Puget Sound Health Alliance's current program can be found on its website: http://www.pugetsoundhealthalliance.org .
Consumer Engagement: What Are We Talking About?
Community members who are developing and operating consumer engagement programs have many definitions of consumer engagement (Hurley et al. 2009 ), ranging from “educating the public about quality and healthcare initiatives and overall health and wellness” to “involving consumers in the process … [of] deciding [about care]” to “empower[ing] people to be their own personal health care managers” (Alexander et al. 2009 ). Our review of the literature, however, revealed few explicit definitions and several different conceptualizations. Later we discuss the different meanings of the terms “consumer” and “engagement” and conclude with a suggested vocabulary meant to distinguish between the two key dimensions of consumer engagement that emerged: the capacity and motivation to act and the actual behaviors. Most important, we call for a clearer articulation of what these or other shorthand terms mean when used to characterize consumer engagement.
Consumer versus Patient
As we mentioned earlier, clear definitions of the “consumer” component of “consumer engagement” were scarce. “Consumer” most often referred to the dictionary definition of “one that utilizes economic goods” (Merriam-Webster 2012b ), but its contextual use implied an economics-based depiction of a consumer as an individual who makes autonomous, informed, rational decisions that maximize his or her individual welfare (Culyer and Newhouse 2000 ). This contrasts with the historical interpretation of “patient” as one who relies on his or her providers to make health-related decisions on his or her behalf (Brody 1980 ; Charles, Gafni, and Whelan 1997 ; Parsons 1951 ).
Some definitions differentiated consumers from patients. Whereas Longo ( 2005 ) distinguished a consumer from a patient based on whether the individual was healthy or sick, Gruman and colleagues ( 2010 , 351) labeled individuals as consumers when they were “making decisions about obtaining health care—choosing among plans, providers and hospitals, for example,” and applied the term “patients” when individuals were “interacting directly with health care providers and services about personal health concerns.”
Engagement: Individual Capacity and Motivation to Act versus Acting
We found that the “engagement” component of “consumer engagement” was used unsystematically to describe a person's “emotional involvement and commitment” to his or her health and role in health care and/or to the act of being “involved in an activity” (Merriam-Webster 2012c ), including behavior related to one's health and health care. Examples of the former describe engaged consumers as individuals “empowered to be in control of their care” (Leape et al. 2009 , 426) or “valu[ing] clinical quality, insist[ing] on shared decision-making, and accept[ing] the responsibility to bear results of choosing lower-quality treatment options” (Schaeffer and McMurtry 2004 , 119). Examples of the latter refer to behaviors to manage one's health and health care, such as participating in “fully” shared decisions about treatments (Gruman et al. 2010 ; Leape et al. 2009 ), including discussing “various lifestyle choices associated with … treatment” (Maillet and Halterman 2004 , 1); undertaking “responsible individual behaviors … [such as] selecting competent physicians and safe hospitals [and] interacting successfully with health providers and institutions” (Shaller 2007 , 309); and talking about “actions individuals must take to obtain the greatest benefit from the health care services available to them” (Gruman et al. 2010 , 351). Although these two dimensions are related, they are not the same: the former describes an individual's capacity to act and his or her degree of motivation (cognitive and emotional elements), and the latter is about behavior.
Engagement as Individual Capacity and Motivation
When engagement is used to characterize an individual's capacity and commitment to taking an active role in his or her own health and health care, those who are more “engaged” are perceived as being more emotionally invested and dedicated to taking charge of their health (Hibbard and Mahoney 2010 ), as well as being more motivated, willing, and able to undertake a constructive role in their health and care. In this context, an individual's degree of engagement is expected to affect the likelihood that he or she will perform engaged behaviors, although this use of the term “engagement” does not refer to any particular behavior.
This dimension of engagement has come to be synonymous with the term “patient activation,” which emerged primarily from the work of Judith Hibbard and her colleagues (e.g., Hibbard and Cunningham 2008 ; Hibbard et al. 2004 ). Hibbard and Cunningham ( 2008 , 2) defined patient activation as “people's ability and willingness to take on the role of managing their health and health care.” This refers not only to people's technical capacity to be active but also to how much they are “disposed to action” (Merriam-Webster 2012a ). People's degree of activation is thus related to their personal beliefs, attitudes, knowledge, confidence, and positive feelings toward their role in their own health and health care (Hibbard and Cunningham 2008 ; Hibbard and Mahoney 2010 ), but it is not equivalent to any one of these attributes. Rather, “activation” is a separate quality reflecting one's overall predilection to engage in certain behaviors.
Engagement as a Set of Behaviors
Some scholars define consumer engagement as an individual's performance of specific behaviors. Gruman and colleagues’ ( 2009 ) typology classifies behaviors into two overarching domains: (1) “managing health” behaviors, which is both the self-management of chronic disease and the adoption of healthy behaviors, and (2) “managing health care” behaviors, which can be both patient and “consumeristic” behaviors. We modified this typology by renaming “patient behaviors” as “health care encounter behaviors” to make clear that this category refers to individuals’ interactions with health care providers. We also renamed “consumeristic behaviors” as “shopping behaviors.” The term “shopping”—“examin[ing] goods or services with the intent to buy” (Merriam-Webster 2012d )—provides a more precise description of the type of behavior being referenced and thus avoids interpreting “consumer” as referring to both a person and a behavior type. Finally, we described the difference between self-management and healthy behaviors.
Self-Management Behaviors
Self-management behaviors are the “day-to-day tasks an individual must undertake to control or reduce the impact of disease on physical health status” (Clark et al. 1991 , 5). These behaviors, such as diabetics monitoring their blood sugar, are believed either to help prevent the deterioration of health or to improve the well-being of individuals with chronic conditions. For conceptual clarity, we classified behaviors related to an individual's acute or chronic illness as “self-management.” For example, a person with diabetes engaging in healthy eating to control his or her blood sugar is undertaking a self-management behavior, whereas healthy eating by an individual with no chronic illnesses would be classified as a healthy behavior.
Healthy Behaviors
Healthy behaviors are undertaken by individuals to maintain their health and well-being and to prevent the development of illness. These behaviors include healthy eating, not smoking or stopping smoking, and getting regular exercise, all of which are known to improve health (Schumaker, Ockene, and Riekert 2009 ).
Health Care Encounter Behaviors
Health care encounter behaviors refer to activities that individuals perform to become more effective self-advocates with their health care providers. Patients engaging in such behaviors ask their providers more and better-informed questions about their care, more effectively communicate their health goals and wishes to their providers, and participate in decisions about their care.
Shopping Behaviors
Shopping behaviors refer to the activities that individuals perform in order to become more effective purchasers of health care. These behaviors include using quality reports to choose a physician, hospital, or health plan, as well as seeking out and using information to help select among treatment options.
In Sum: Proposed Vocabulary for Consumer Engagement
In this section we suggest some terms to help differentiate the meanings of “consumer engagement” and to communicate the intended meanings more clearly. These suggestions are based on the terms just defined. Strict adherence to a particular set of terms is not required to advance our understanding of consumer engagement, so regardless of the terms chosen, we are arguing for a clearer articulation of assumptions and meanings in developing, assessing, and discussing consumer engagement interventions.
To differentiate between the two main dimensions of engagement just described, we propose that the degree to which individuals (i.e., “patients” or “consumers”) are inclined to take an active role in managing their health and health care be referred to as the degree of “activation.” Our tracking of the consumer engagement field suggests that “activation” (coined by Hibbard and colleagues) is becoming the favored term. We propose that “engaged behaviors” be used as a general term to refer to actions to manage health and health care and that self-management, healthy, health care encounter, and shopping behaviors be used to describe the four general kinds of engaged behavioral domains defined earlier.
When selecting a term to represent the individual (or individuals as a class), neither “consumer” nor “patient” is objectively superior to the other. As described earlier, the normative interpretations of each of these terms reflect different values and assumptions regarding an individual's role in his or her health and health care. But the language is continuously evolving, and so even these interpretations are not absolute or universal. For example, discussions about promoting individuals’ greater involvement in their care plans and treatment decisions often refer to individuals as “patients.” However, the intent of this shared decision-making movement is for individuals to partner with providers, thereby contradicting the common meaning of “patient” as a person who relies on the provider to make treatment decisions on his or her behalf and passively accepts the provider's instructions. Thus, we contend that it is very important to be mindful of the language used to communicate about “consumer engagement” concepts, especially by those outside academic circles, whose assumptions may vary but may not be communicated (e.g., in an office visit, in an issue brief). Overall, we found that the literature and the conversations we conducted for the AF4Q evaluation implicitly reflected Gruman and colleagues’ ( 2010 ) distinctions. “Patient” was used when an individual was interacting directly with health care providers (and provider entities) about personal health concerns, and “consumer” was used when an individual was making decisions about obtaining health care. We endorse following this trend and do so for the remainder of this article.
A Framework for Consumer Engagement
We found no single conceptual model or framework that satisfactorily accounted for the key dimensions of consumer engagement; depicted individual, group, and community dynamics; and was applicable to all four behavior types (self-management, health care encounter, shopping, and healthy). First, most of the existing models addressing individual health behavior change do not consider group and community elements or a variety of behavior types, even though this is important for classifying and evaluating programs like AF4Q that involve multiple and diverse consumer engagement interventions (Glanz, Rimer, and Viswanath 2008 ; Painter et al. 2008 ). The models of individual behavior, which focus almost exclusively on intrapersonal dimensions, are the health belief model, the microeconomic consumer choice theory, the theory of planned behavior, and the transtheoretical model ( table 1 ).
Selected Behavior Change Models
The health belief model explains why large numbers of individuals do not obtain beneficial health services, such as preventive screenings (Janz and Becker 1984 ). It assumes that individuals value their health very highly and that their decision to act is based on their perceptions of the gravity of the threat to their health and the benefits and costs of action ( table 1 ). But it does not delineate the process for individual decision making and does not take into account that people do not always value health above almost everything else (e.g., smoking to “fit in” with one's friends). The microeconomic consumer choice theory is also based on an individual's cost-benefit assessment of the expected value of acting in a particular way, but the influences on the assessment of value are defined rather broadly as one's “preferences” (Kolstad and Chernew 2009 ).
The transtheoretical model (Prochaska et al. 1994 ) posits that individuals progress through five stages while considering, undertaking, and possibly maintaining a new behavior: precontemplation, contemplation, and preparation (stages 1 through 3); taking action (stage 4); and maintaining the behavior (stage 5). Neither this model nor the theory of planned behavior depicts the relationships with contextual influences. The theory of planned behavior (Ajzen 1991 ; Armitage and Conner 1999 ), which is an extension of the theory of reasoned action (Fishbein 1979 ), posits that a person's intention to perform a behavior drives his or her actions and that a person's beliefs about behavioral outcomes, behavior norms, and perceptions of his or her control over the behavior converge to create this intent ( table 1 ). Although this model includes the role of normative beliefs, it does not go beyond this to connect individual attributes to broader contextual factors.
Models based on social support and network theory, social cognitive theory, and social ecological theory emphasize the influence of interpersonal, group and/or community dimensions on behavior ( table 1 ). The first two theories are built on social learning. Models of social support and networks associate characteristics of relationships (e.g., closeness, number of relationships) with behaviors (Berkman and Kawachi 2000 ; Christakis and Fowler 2012 ; Uchino et al. 2012 ); models based on social cognitive theory also account for interpersonal factors but place a greater emphasis on the interaction between individual factors (most notably, self-efficacy, which was developed as part of this theory) and the social environment (Bandura 1986 , 2004 ). Finally, while the social ecological model clearly illustrates that multiple levels of factors influence health behaviors, nesting individuals in their intrapersonal environment and then within the larger contexts of community and even society, it does not depict individual mechanisms (Bronfenbrenner 1979 ; Richard, Gauvin, and Raine 2011 ).
None of these models alone served our need to classify and understand the wide variety of consumer engagement interventions with which the AF4Q communities were experimenting (e.g., directly or indirectly targeting individuals, targeting different sets of behaviors, targeting different stages of “readiness”). However, to develop a framework for such varied consumer engagement programs, which we titled the Engaging Consumers in Health and Health Care in Communities (ECHC) framework, we drew collectively on these existing models. Before examining the ECHC's particulars, we provide a brief overview of the framework's structure.
The ECHC's Structure
The overall structure of the ECHC framework ( figure 1 ) is drawn from social ecology, which posits that factors outside the individual influence his or her behavior (Bronfenbrenner 1979 ). That is, individuals are nested within groups, which are embedded in the broader community. We selected this multilevel structure because consumer engagement interventions can take group or population approaches, and contextual factors influence individual behavior and the success of interventions. The ECHC's structure of concentric circles shows that individuals, groups, and communities may influence one another at any point in time, but not necessarily in a linear fashion or with equal importance.
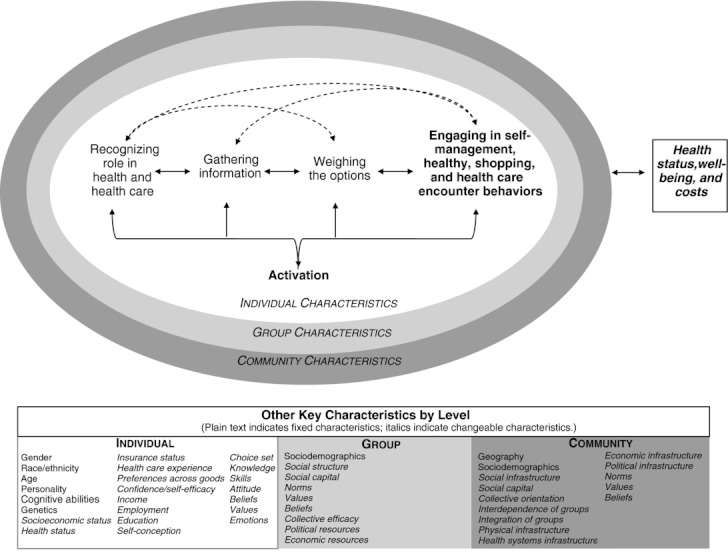
The Engaging Consumers in Health and Health Care in Communities (ECHC) framework.
The first level is concerned with individuals’ engagement in their health and health care and is the most detailed because, as we noted earlier, consumer engagement is fundamentally about individual behaviors. Although groups and communities can have unique identities and act collectively, most consumer engagement is ultimately acted out by individuals (Hibbard 2009a ). The surrounding group level focuses on individuals’ interactions with and influences on one another (i.e., interpersonal relationships and behaviors). Thus, in the ECHC framework, the term “group” refers to relationships among two or more individuals whose relationship may be based, for example, on friendship, family, religion, ethnicity, exchange of services, or employment. 1 The community level represents the larger geographic space, consisting of the physical, economic, sociocultural, and political structures in which individuals (and the groups with which they identify) navigate (Buttimer 1969 ; Hunter 1975 ). Although some literature uses the term “community” to describe a large group of people with a common attribute (e.g., the breast cancer community), the ECHC framework considers these collections of people as groups. Finally, at the bottom of the framework we list those characteristics identified in the literature as likely influencing consumer engagement within and across levels.
Next we examine more closely each of the framework's three levels and the relationships within and among them. Our goal was to develop a framework for classifying consumer engagement interventions, specifically interventions sponsored by or put in place by a community's multistakeholder entities, to facilitate dialogue about their logic and role. Here, however, we cannot present an exhaustive set of specific hypotheses about how any or all of a level's characteristics could impact an individual's engagement.
Individual Level
At the center of the ECHC framework is an adapted version of the transtheoretical model of individual behavior change (Prochaska 2008 ; Prochaska et al. 1994 ). The transtheoretical model is not, however, a theory but a model that reflects a common, but not universal (e.g., see Herzog 2010 ), conceptualization of behavior change as an individual's progression through a series of stages and processes that can be targeted by interventions (Prochaska 2008 ; Prochaska et al. 1994 ). For example, in the precontemplation and contemplation stages, a key process may be becoming increasingly aware of how a particular behavior affects an individual's health and well-being (Prochaska et al. 1994 ). Because of its widespread use in the literature (Glanz, Rimer, and Viswanath 2008 ; Painter et al. 2008 ) and its intuitive, staged approach (Munro et al. 2007 ; Prochaska, Redding, and Evers 2008 ), we chose this model as a starting point, modifying it to incorporate the role of activation and to emphasize the dynamic nature and varied time horizon of change.
The original transtheoretical model consists of five stages of change: (1) precontemplation (no change intended within six months), (2) contemplation (change intended within next six months), (3) preparation (change intended within a month), (4) action (already has made changes), and (5) maintenance (sustaining change beyond six months) (Prochaska et al. 1994 ); the time frames reflect the original focus on using the model to design interventions to guide the planned behavior change. The ECHC framework specifies activation as a distinct characteristic that influences an individual's decision-making process and actions taken to change his or her behavior. This decision-making process has four stages: (1) recognizing one's role in health and health care, (2) gathering information, (3) weighing the options, and (4) engaging in healthy, self-management, shopping, or health care encounter behaviors. In figure 1 , the two core conceptual dimensions of consumer engagement discussed earlier in this article—activation and one or more of the four behavior types—are denoted in boldface. In addition, we eliminated any reference to specific time frames and added bidirectional links to better reflect the dynamic nature of decision making and behaviors over time. For various reasons, individuals may implicitly or explicitly (re)consider their behaviors.
To improve activation and the performance of engaged behaviors, individuals must be aware of, acknowledge, and embrace the idea that there is room to improve their own health and that they have an important, active role in doing so. This step primarily concerns individuals’ self-perception of their role and ability to be engaged in their health and health care (Bandura 1986 , 2004 ; Prochaska et al. 1994 ; Swann and Bosson 2010 ; Terry 2005 ). Recognizing their role provides motivation to pursue behavior change, and how individuals perceive this role affects their motivation to pursue behavior change, including the scope and types of information sought. Individuals’ effort in looking for information and where they seek it can vary greatly and include searching the Internet, asking friends or family for advice, reading pamphlets in their provider's office or at the pharmacy, and talking to their provider about their health and health care. The information gathered and how it is interpreted can further shape how an individual perceives his or her role.
The next step is weighing the options, or understanding, assessing, and synthesizing information to evaluate the direct or indirect benefits and costs of engagement alternatives. In economics, this process is known as estimating trade-offs to maximize utility, or assessing the “opportunity costs” when choosing one's behavior (Culyer and Newhouse 2000 ). In the transtheoretical model of behavioral change, this concept is referred to as individuals’ “decisional balance sheet” of pros and cons (Prochaska et al. 1994 ). Weighing the options may be executed as an intrinsic, unconscious process or as one that is more explicit and deliberate. If individuals conclude that the benefits of change sufficiently outweigh the costs, they will be expected to perform and maintain the engaged behaviors. Individuals’ choosing to take (or not to take) action may affect their health and well-being over time. Finally, the framework indicates that an individual's degree of activation is associated with the behavior change and that his or her degree of activation can change over time (Fowles et al. 2009 ; Greene and Hibbard 2011 ; Harvey et al. 2012 ; Hibbard 2009b ; Hibbard et al. 2007a; Mosen et al. 2007 ; Remmers et al. 2009 ).
The ECHC framework assumes that individuals may progress (or regress) among these stages at different rates. Individuals have different capacities, and different constraints on their capacities, that affect motivation and movement. For example, a diagnosis of diabetes may prompt individuals to rethink their role in managing their own health and instigate information gathering about diabetes-specific management recommendations. However, these same people may not view themselves as active “shoppers” for high-quality providers and may not look for information about their provider's record on diabetes care. Or they may not have “real” choices because of insurance restrictions or because other providers are not taking new patients. Since we designed our framework to accommodate these variations, defined time periods are not assigned to a stage.
In addition, although we presented our framework linearly, we recognize that the consumer engagement process is dynamic (Hibbard and Mahoney 2010 ; Prochaska 2008 ). The bidirectional arrows indicate the potential to progress or regress in linear and nonlinear ways over time. For example, an individual who exercises regularly may move from taking action to gathering information to understanding better why he or she has not seen a change in weight or decrease in blood pressure. In another case, an individual may believe that the costs associated with using performance reports and switching physicians are prohibitively high but may revisit this calculus when he or she moves to another town or his or her physician retires.
While the process is dynamic, individuals may pause at any point. For instance, individuals may gather information about one of their providers or possible treatments but stall and do nothing because they find the information hard to understand and believe that the additional effort to comprehend the information (e.g., time, potential embarrassment in seeking help, likely relevance) outweighs expected benefits. Or an individual who did not lose weight despite exercising may not return to gather more information but move back to role recognition because this feedback altered his or her self-conception as a confident, apt manager of his or her own health. One factor affecting progress is the source of an individual's motivation to change. Individual change that is more intrinsically than extrinsically motivated is thought to be more powerful, especially when people are experiencing stress, because the intention and motivation is grounded in their own values and interests, not in others’ (Anderson and Funnell 2010 ; Ryan and Deci 2000 ).
As indicated by our examples, static traits like age, gender, personality, cognitive abilities, race, and ethnicity and more variable states such as health status, income, socioeconomic status, self-efficacy, emotions, experiences, self-conception, degree of self-regulation, knowledge, awareness of choices, skills, and beliefs and values can influence the engagement process and degree of engagement (Hibbard and Mahoney 2010 ; IOM 2001 ; Protheroe, Nutbeam, and Rowlands 2009 ; Rosen, Anell, and Hjortsberg 2001 ; Schumaker, Ockene, and Riekert 2009 ; Swann and Bosson 2010 ).
Group Level
Group membership affects access to potentially beneficial information, social support, and material resources (Berkman and Kawachi 2000 ; Granovetter 1973 ; Hermann-Pillath 2010). Most individuals are members of social networks and psychologically identify with one or more groups, each of which has its own identity and culture (Charles et al. 2006 ; Leary 2010 ; Tajfel and Turner 1979 ). Group culture, which is made up of the values, attitudes, and beliefs that are learned and transmitted among group members, is expressed through implicit and explicit rules that regulate and reinforce appropriate, socially sanctioned behavior and punish unacceptable displays of values and beliefs (Kreuter and Haughton 2006 ; Leary 2010 ; Link and Phalen 2001 ). This ongoing socialization can impede or enhance consumer engagement, depending on how consumer engagement in health and health care is defined and valued (Swann and Bosson 2010 ).
For example, some groups of consumers might not trust specific sources of information or might believe it is disrespectful to question providers about treatment (Cutilli 2010 ; Hesse et al. 2005 ; Kleinman 1980 ). Members of these groups also may disregard institutionally sponsored campaign materials encouraging people to ask their providers specific questions about their health care or prevent a family member from asking questions during a visit with a provider. Alternatively, groups that strongly value being “informed” or “not pushed around” may be positively affected by the same campaign efforts, if the campaign affirms these core elements of their identity. Instead of automatically discarding these materials, members of these groups may bring them to their next office visit for easy reference. For their part, providers may adhere to and reinforce nonactivated consumer roles in health care encounters, for example, by repeatedly interrupting patients and outwardly dismissing their concerns, or they may affirm activated roles by soliciting patients’ input in a collaborative manner and making them aware of any options (Dy and Purnell 2012 ; Emanuel and Emanuel 1992 ).
A group's influence on a consumer's engagement is likely to be greater if a member strongly identifies with, is attached to, and is embedded in the group; the group has a strong identity; and it has a high degree of cohesiveness and interdependence (Berkman and Kawachi 2000 ; Friedkin 2004 ; Lau 1989 ; Swann and Bosson 2010 ). For example, Ahern and colleagues ( 2009 ) found that the same high degree of collective efficacy was associated with more smoking in neighborhoods having permissive smoking norms and with less smoking in neighborhoods having strong antismoking norms. The forces that prevail may depend on the issue and situation. For example, if a minority woman with diabetes identifies with her ethnic group more strongly than she does as a diabetic, she may hesitate to discuss alternative medicine treatments with her mainstream medical providers (Graham et al. 2005 ; Shelley et al. 2009 ), even if others in her diabetes support group encourage this discussion.
Other group-level characteristics that can shape consumer engagement are sociodemographic makeup, integration into mainstream culture, and economic, political, and social 2 resources (Fiske 2010 ; Link and Phalen 2001 ; Reitz and Sklar 1997 ; Yzerbyt and Demoulin 2010 ).
Community Level
A community's economic, political, social, and physical infrastructures influence (1) the relevance and role of consumer engagement in improving the community's health and health care; (2) the will and ability to take collective action with respect to consumer engagement; and (3) the legitimate, acceptable options for consumer engagement initiatives in the community. Although scholars and practitioners disagree on the relative influence of these factors (Helman 2001 ; Lynch et al. 2002 ; McLeroy et al. 1988 ; Roblin and Becker 2009 ), powerful individuals and entities can have tremendous influence over community agendas, including how resources are distributed (Fiske 2010 ; Gradstein and Schiff 2006 ). Context is important to understanding the opportunities for and characteristics of community consumer engagement initiatives (Hibbard 2009a , 2009b ; Larson et al. 2009 ).
A community's economic infrastructure affects both the total amount of resources available for improving a community's health and the locus of power. For example, if a few large purchasers have significant economic power in a community's health care sector, they may use this power to compel providers to supply performance data for their employees to use in choosing providers or for the employer to use in deciding payments. The purchasers may also pursue this performance-reporting agenda, regardless of the providers’ readiness. In turn, providers may use their social power to persuade patients to maintain their existing provider relationships, despite any purported quality differences.
Likewise, a community's “mainstream culture” represents historically powerful groups’ values and beliefs, such as the role of collectivism versus individualism in community life or the role of folk medicine versus Western medicine. The importance of the mainstream culture is its power to set norms that influence behavior, as observed in the evolution of smoking behavior and the treatment of depression (Kleinman and Hall-Clifford 2009 ; Stuber, Meyer, and Link 2008 ). Its influence may vary with the matter being considered and how embedded a group is in the mainstream (Swann and Bosson 2010 ; Wolff et al. 2010 ). Finally, geography and physical infrastructure affect consumer engagement by shaping the connections among people, groups, and resources (Sampson, Morenoff, and Gannon-Rowley 2002 ; Williams and Collins 2001 ). Geography affects access to resources that can reduce the costs of engagement like social support, healthy food, safe places to exercise, and the accessibility and availability of high-quality providers (Cohen, Inagami, and Finch 2008 ; Larson, Story, and Nelson 2009 ; Nemet and Bailey 2000 ; Stanley, Cantor, and Guarnaccia 2008 ).
Applying the Framework: An Example from the Aligning Forces for Quality (AF4Q) Initiative
In this section, we show how policymakers and practitioners can “make sense” of existing consumer engagement initiatives by applying the ECHC framework to a real program. Our intent is to show how the framework can be used to systematically classify different program elements that can contribute to discussions of the purpose, value, fit, and realistic potential of consumer engagement initiatives in particular contexts.
The case is Washington State's Puget Sound Health Alliance's (“the Alliance”) consumer engagement program in 2008/2009. It is one of the communities participating in the Aligning Forces for Quality (AF4Q) program, which provides resources to grantee communities to develop localized, multistakeholder, communitywide efforts to improve health care quality and overall health through several mechanisms, including improving consumer engagement (Painter and Lavizzo-Mourey 2008 ). We chose to apply the ECHC framework to this program because it included several activities with varied scopes, mechanisms, and purposes and thus provided a good test of the framework's utility in effectively understanding complex consumer engagement initiatives and generating a productive dialogue among policymakers and practitioners.
We begin with a brief description of the Alliance's four program activities in 2008/2009, followed by our examination of the program by the ECHC framework's targeted behaviors, individual stages and processes, and levels (i.e., individual, group, and community).
Overview of Activities
In 2008/2009 the Alliance's four main consumer engagement activities were (1) a public, communitywide, Internet-based performance report on physicians, hospitals, and health plans known as the Community Checkup; (2) a monthly health column by a local physician for use in newspapers and local organizations’ websites and newsletters; (3) Rx for Information, in which physicians in a small number of practices wrote “prescriptions” for patients with diabetes, congestive heart failure, or depression to go to the library to learn about their conditions from trained librarians; and (4) Healthy Incentives, one public employer's employee incentive program to engage in healthy and shopping behaviors. Table 2 provides additional details.
Description of Puget Sound Health Alliance's Consumer Engagement Activities in 2008–2009
Source : Authors’ analysis.
Analysis by Engaged Behavior Type
The four activities tackle multiple types of engaged behavior ( figure 2 ): three address healthy behaviors (Community Checkup, health columns, and Healthy Incentives); three speak to self-management and shopping behaviors (Community Checkup, health columns, and Rx for Information); and two take up health care encounter behaviors (Community Checkup and health columns). The activities do not emphasize engaged behaviors equally. For example, although the Community Checkup is predominantly focused on shopping behaviors (i.e., comparing and selecting providers), this report could influence the other three behavior types by increasing awareness of what is involved in preventing and managing chronic illnesses and stimulating discussions with providers. The heart of Rx for Information is improving self-management behaviors by connecting individuals with information about their conditions, but this activity also may encourage discussion of their care with their physicians (health care encounter behavior) or comparison of providers’ performance (shopping behavior).
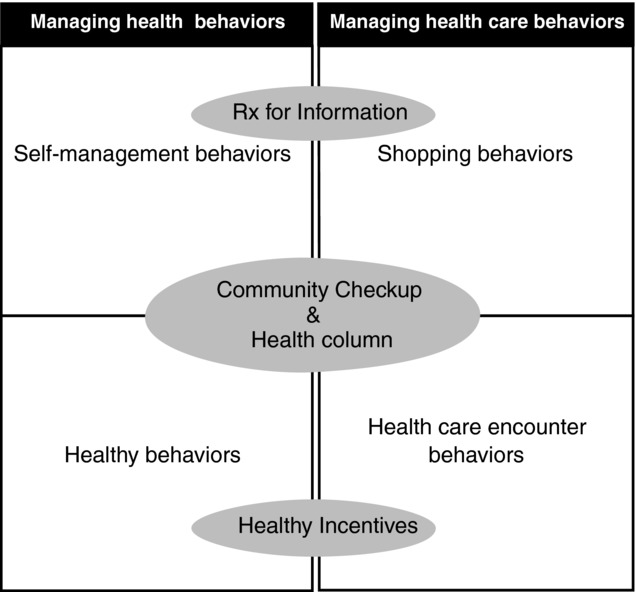
Classification of Puget Sound Health Alliance's consumer engagement program activities by consumer behavior type, 2008–2009.
Our review of this classification of activity by type generated several questions that the Alliance could use to structure a dialogue about how these activities work individually and together to meet Alliance's goals, including
Is it important to have activities that collectively address all four types of engaged behaviors? How does this fit into the Alliance's overall strategy for consumer engagement? How do these behaviors correspond to the needs of the targeted populations and the community as a whole?
Do certain activities effectively address more than one behavior (e.g., do they provide evidence? Existing infrastructure in the community?) Are activities intended to be independent or interdependent?
Is there evidence of the activities’ potential success? What would success look like in Puget Sound, and how would the Alliance measure it (e.g., more “hits” on the Alliance's website? More employees eligible for the workplace incentive? More individuals reporting that they consult the performance information?)
Analysis by Individual Stage
The Alliance's consumer engagement program as a whole emphasizes the information-gathering stage of the individual engagement process; all four activities address this aspect, and most prioritize it ( figure 3 ). The Community Checkup targets information gathering for selecting providers through its performance metrics and searchable website; the health column offers information related to all four engagement behaviors; Rx for Information tries to make information gathering easier by helping with accessing and using existing resources; and Healthy Incentives offers several opportunities in the workplace to gather general and more individualized information about healthy living in multiple forms (e.g., print resources, Internet, and classes). Finally, the Community Checkup and the health column reflect a cognitive approach to change (i.e., if minds are changed, behavior will follow), whereas Rx for Information and Healthy Incentives take a behavioral approach (i.e., if behavior is changed, beliefs will follow).
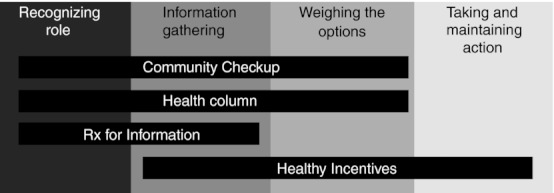
Classification of the Puget Sound Health Alliance's consumer engagement program by individual change process, 2008–2009.
This description led us to several more questions that could guide our discussion about the program's priorities (e.g., selection of targeted populations) and operating assumptions (e.g., logic, evidence, and expectations for different types of changes), such as
Is it important to serve consumers’ needs across the continuum of change? Does this continuum differ by degree of activation, engaged behavior type, or population (e.g., persons with diabetes, low literacy, no Internet access, no provider choice)?
Are the targeted stages consistent with the target population's capacity and needs? Do these activities adequately consider consumers’ capacity, interest, and willingness to use these resources?
What is known about the approach to and effectiveness of these activities for the target population(s)? Is a cognitive or a behavioral approach better suited to some people or behaviors? Has the timing and sequencing of activities been taken into account?
How will the Alliance know if the activities are working and which activities should be modified, sustained, or eliminated? How do assumptions about how individual change occurs and how the selected interventions work affect expectations for success?
Analysis by Level: Individuals, Groups, and Communities
The scope and reach of the Alliance's consumer engagement elements vary widely. Rx for Information focuses on individual-level change for consumers with specific chronic illnesses through one-on-one interactions with a physician and librarian. This program was implemented in only a few physicians’ practices. However, it was the only activity to explicitly use individual physicians’ influence with consumers, which can be a very powerful force for activating consumers (Becker and Roblin 2008 ; Cutilli 2010 ; Hesse et al. 2005 ). Healthy Incentives targets the individual and group levels, offers individual financial incentives for meeting program goals, and supports new and naturally existing employee subgroups to reinforce activation and engaged behaviors. Examples are on-site support groups for specific health issues (e.g., weight loss) and organized group exercise activities. Focused, narrower efforts like these reach many fewer people and are more costly to operate per consumer. But some would argue that these approaches may more effectively motivate engagement than do the aforementioned broad-audience interventions, since they are more personalized and delivered by proximal, influential sources.
Alternatively, the Community Checkup and health columns take a “top-down,” communitywide approach; they were designed for broad dissemination and use by Puget Sound's consumers, providers, employers, and insurers to create a community environment that encourages activation and engaged behaviors. These activities have the potential to reach large numbers of people but may not be helpful for consumers who, for example, do not already recognize their role, trust the Internet, or know how to interpret performance measures. The Alliance addressed community diversity and population scope in several ways. The health column was made available in multiple lengths and reading levels. The Alliance's websites allow some customization in their search capabilities (e.g., for certain conditions) and provide resources in Spanish, access to a dictionary of health terms, and a link to EthnoMed ( http://ethnomed.org ), which offers health and medical information on and for various cultural groups in several languages.
The process of categorizing the activities by level raised questions for reviewing the Alliance's strategy for consumer engagement, including the appropriate level(s) for interventions:
Do the activities complement or reinforce one another across levels? What are the trade-offs of taking narrow and/or broad approaches? What is desirable and realistic for this particular community?
Are activities deliberately matched and tailored to level? Are certain activities better suited to certain goals and levels? For example, are activities to improve recognition of an active role more effective at the individual, group, or community level? Is there an optimal order of interventions? What are the comparative advantages of different approaches for the Alliance's targeted populations?
Will the Alliance know if these activities are increasing activation or engaged behaviors? Is it important to establish the cost-effectiveness of any or all of the activities?
In sum, this example illustrates how the ECHC framework can be used to differentiate among consumer engagement program components and to catalyze thinking about the purpose, scope, potential, and fit of these initiatives for specific contexts. While we applied the framework retrospectively, we also think that this framework could have value prospectively when planning consumer engagement interventions. Even though it is not a self-contained analytic tool that produces an optimal solution, it could help policymakers and practitioners successfully develop and assess the fit of their consumer engagement programs by providing a structure for discussion and prompting broad thinking about vital program dimensions.
Defining consumer engagement and understanding its role in generating better health and improving the value of health care is especially important as the United States implements health reform and as the number and types of consumer engagement initiatives continue to grow. Employers will provide consumer-directed health plans; Medicare and private employer coalitions will offer consumers reports on hospital quality; cities will implement a broad health education campaign urging individuals to ask their providers about their care, participate in treatment choices, or make healthy behavior choices; and hospitals or community organizations will add small, peer-led classes to help patients manage their chronic diseases (CDC 2010 ; Fronstin 2010 ; Galvin et al. 2005 ; Harris and Buntin 2008 ; Lorig et al. 2001 , 2009 ; National Patient Safety Foundation 2009 ).
A key question confronting policymakers and practitioners is how to achieve effective, widespread change. For consumer engagement, consensus on the most effective approaches is still elusive. For example, some stage-specific interventions targeting individuals have been more effective in moving individuals toward more physical exercise than have interventions not matched to stage (Lippke et al. 2010 ), but others have not been able to do so (Jepson et al. 2010 ; Van Sluijs, Van Poppel, and Van Mechelen 2004 ). The relatively scant evidence for community-level change also is mixed. For example, cigarette taxes and smoking bans in workplaces and restaurants have proved effective, but the effect on consumer behavior of environmental changes like the production and wide dissemination of provider performance reports or providing caloric information on fast food and restaurant items is debatable (e.g., Elbel et al. 2009 ; Harris and Buntin 2008 ; Ketelaar et al. 2011 ; Kolstad and Chernew 2009 ; Roberto et al. 2010 ).
In addition, the effectiveness of community coalitions in improving health, focused mostly on public health issues, has been “modest at best” (Glanz, Rimer, and Viswanath 2008 , 395), with the exception of antismoking efforts (Warner and Mendez 2010 ). From the existing knowledge, we cannot confidently state that the most prudent strategy to improve engagement is somehow to “scale up” individual interventions or to take a fundamentally different approach targeting broader environmental factors, or some combination of the two. Accordingly, some argue that the implementation of consumer engagement programs may be ahead of the research, suggesting the need for more scientific evidence that consumer engagement initiatives work and can improve the quality of health care (Arnold and Scanlon 2009 ).
In this article we identified the need for a framework to classify the wide array of consumer engagement interventions to help “make sense” of them as an important step to advancing knowledge of their value in improving the quality of health care through community-based efforts, or otherwise. The Puget Sound Health Alliance example illustrated how applying the framework could advance the field by making policymakers and practitioners aware of the wide range of approaches, providing a structured way to organize interventions retrospectively, and, perhaps prospectively, to help consider how they can meet program goals both individually and collectively.
Acknowledgments
The authors thank their AF4Q evaluation team colleagues and the anonymous reviewers for their thoughtful and valuable feedback during this manuscript's development. This work was supported by a grant from the Robert Wood Johnson Foundation.
Unless noted, we use the terms “group” and “social network” interchangeably in this article because we are primarily concerned with the individual's interactions with other people, ranging from a dyad to a much larger collection of people. In some fields, however, the terms “group” and “social network” carry different connotations, with “group” suggesting a clearly bounded collection of people (e.g., class, geography, religion), whereas “social networks” typically cut across these groups (Berkman and Kawachi 2000 , 140–41). Finally, we consider an organization (employment or otherwise) to be a group.
Social capital is intangible resources, such as trust and reciprocity, generated by the social structure for use by individuals and collectives. Because it is a public good, social capital is a characteristic of a collective, not an individual (Berkman and Kawachi 2000 ; Coleman 1990 ; Putnam 1995 ). Social capital facilitates action and coordination, shaping the “obligations and expectations for transactions” (Berkman and Kawachi 2000 , 175–76) among people and in markets (Herrmann-Pillath 2010 ), thereby reinforcing existing structures.
- AF4Q (Aligning Forces for Quality) About Us. 2012. Available at http://forces4quality.org/about-us (accessed July 9, 2012)
- Ahern J, Galea S, Hubbard A, Syme SL. Neighborhood Smoking Norms Modify the Relation between Collective Efficacy and Smoking Behavior. Drug and Alcohol Dependency. 2009;100(1–2):138–45. doi: 10.1016/j.drugalcdep.2008.09.012. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ajzen I. The Theory of Planned Behavior. Organizational Behavior and Human Decision Processes. 1991;50(2):179–211. [ Google Scholar ]
- Alexander JA, Beich J, Christianson JB, Hasnain-Wynia R, Hurley R, Keenan PS, Mittler JN, Scanlon DP. Confidential Interviews with Aligning Forces for Quality Participants. 2009. Verbatim Transcripts.
- Anderson RM, Funnell MM. Patient Empowerment: Myths and Misconceptions. Patient Education and Counseling. 2010;79:277–82. doi: 10.1016/j.pec.2009.07.025. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Armitage CJ, Conner M. Efficacy of the Theory of Planned Behavior: A Meta-Analytic Review. British Journal of Social Psychology. 1999;38:195–222. doi: 10.1348/014466601164939. [ DOI ] [ PubMed ] [ Google Scholar ]
- Arnold SB. Improving Quality Health Care: The Role of Consumer Engagement. 2007. Available at http://www.academyhealth.org/files/issues/ConsumerEngagement.pdf (accessed November 16, 2009)
- Arnold SB, Scanlon DP. Realizing True Consumer Directed Health Care: What the Policy Community Needs. Medical Care Research and Review. 2009;66(1):3S–8S. doi: 10.1177/1077558708327579. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Saddle River, NJ: Prentice Hall; 1986. [ Google Scholar ]
- Bandura A. Health Promotion by Social Cognitive Means. Health Education and Behavior. 2004;31:143–64. doi: 10.1177/1090198104263660. [ DOI ] [ PubMed ] [ Google Scholar ]
- Barraclough JH, Birch J. Health Care Safety and Quality: Where Have We Been and Where Are We Going. Medical Journal of Australia. 2006;184(suppl. 10):S48–50. doi: 10.5694/j.1326-5377.2006.tb00362.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Becker ER, Roblin DW. Translating Primary Care Practice Climate into Patient Activation: The Role of Patient Trust in Physician. Medical Care. 2008;46(8):795–805. doi: 10.1097/MLR.0b013e31817919c0. [ DOI ] [ PubMed ] [ Google Scholar ]
- Berenson RA. Which Way for Competition? None of the Above. Health Affairs. 2005;24(6):1536–42. doi: 10.1377/hlthaff.24.6.1536. [ DOI ] [ PubMed ] [ Google Scholar ]
- Berkman L, Kawachi I. Social Epidemiology. Oxford: Oxford University Press; 2000. [ Google Scholar ]
- Brody DS. The Patient's Role in Clinical Decision-Making. Annals of Internal Medicine. 1980;93:718–22. doi: 10.7326/0003-4819-93-5-718. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979. [ Google Scholar ]
- Brown AD, Alikhan LM, Sandoval GA, Seeman N, Baker GR, Pink GH. Acute Care Hospital Strategic Priorities: Perceptions of Challenges, Control, Competition and Collaboration in Ontario's Evolving Healthcare System. Healthcare Quarterly. 2005;8(3):36–47. [ PubMed ] [ Google Scholar ]
- Buttimer A. Social Space in Interdisciplinary Perspective. Geographical Review. 1969;59(2):417–26. [ Google Scholar ]
- CDC (Centers for Disease Control and Prevention) Communities Putting Prevention to Work: CDC Awards $372.8 Million to 44 Communities. 2010. Available at http://www.cdc.gov/Features/ChronicPreventionGrants/ (accessed January 3, 2010)
- Charles C, Gafni A, Whelan T. Shared Decision-Making in the Medical Encounter: What Does It Mean? (Or It Takes Two to Tango) Social Science & Medicine. 1997;44(5):681–92. doi: 10.1016/s0277-9536(96)00221-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- Charles C, Gafni A, Whelan T, O'Brien A. Cultural Influences on the Physician-Patient Encounter: The Case of Shared Treatment Decision-Making. Patient Education and Counseling. 2006;63:262–67. doi: 10.1016/j.pec.2006.06.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- Christakis NA, Fowler JH. Social Contagion Theory: Examining Dynamic Social Networks and Human Behavior. Statistics in Medicine. 2012 doi: 10.1002/sim.5408. June 18 (e-pub before print) [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Clark NM, Becker MH, Janz NK, Lorig K, Rakowski W, Anderson L. Self-Management of Chronic Disease by Older Adults: A Review and Questions for Research. Journal of Aging and Health. 1991;3(1):3–27. [ Google Scholar ]
- Cohen DA, Inagami S, Finch B. The Built Environment and Collective Efficacy. Health Place. 2008;14(2):198–208. doi: 10.1016/j.healthplace.2007.06.001. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Coleman JS. Social Capital in the Creation of Human Capital. American Journal of Sociology. 1990;94(suppl):S95–S120. [ Google Scholar ]
- Culyer A, Newhouse JP. The Handbook of Health Economics. Amsterdam: North Holland; 2000. [ Google Scholar ]
- Cutilli CC. Seeking Health Information: What Sources Do Your Patients Use? Orthopedic Nursing. 2010;29(3):214–19. doi: 10.1097/NOR.0b013e3181db5471. [ DOI ] [ PubMed ] [ Google Scholar ]
- DHHS (Department of Health and Human Services) Value-Driven Health Care. 2008. Available at http://archive.hhs.gov/valuedriven/#top (accessed November 16, 2009)
- DHHS (Department of Health and Human Services) Key Features of the Affordable Care Act, by Year. 2012. Available at http://www.healthcare.gov/law/timeline/full.html (accessed July 5, 2012) [ Google Scholar ]
- Draper DA, Claxton G. Managed Care Redux: Health Plans Shift Responsibilities to Consumers. Center for Studying Health System Change: Issue Brief. 2004;(79):1–4. [ PubMed ] [ Google Scholar ]
- Duggan PS, Geller G, Cooper LA, Beach MC. The Moral Nature of Patient-Centeredness: Is It “Just the Right Thing to Do”? Patient Education and Counseling. 2006;62(20):271–76. doi: 10.1016/j.pec.2005.08.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- Dy SM, Purnell TS. Key Concepts Relevant to Quality of Complex and Shared Decision-Making in Health Care: A Literature Review. Social Science & Medicine. 2012;74(4):582–87. doi: 10.1016/j.socscimed.2011.11.015. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Elbel B, Kersh R, Brescoll VL, Dixon B. Calorie Labeling and Food Choices: A First Look at the Effects on Low-Income People in New York City. Health Affairs. 2009;28(6):1110–21. doi: 10.1377/hlthaff.28.6.w1110. [ DOI ] [ PubMed ] [ Google Scholar ]
- Emanuel EJ, Emanuel LL. Four Models of the Physician-Patient Relationship. JAMA. 1992;267(16):2221–26. [ PubMed ] [ Google Scholar ]
- Epstein RM, Street RL. The Values and Value of Patient-Centered Care. Annals of Family Medicine. 2011;9(2):100–103. doi: 10.1370/afm.1239. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fishbein M. A Theory of Reasoned Action: Some Applications and Implications. Nebraska Symposium on Motivation. 1979;27:65–116. [ PubMed ] [ Google Scholar ]
- Fiske ST. Interpersonal Stratification: Status, Power, and Subordination. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of Social Psychology. Hoboken, NJ: Wiley; 2010. pp. 941–82. [ Google Scholar ]
- Fiske ST, Gilbert DT, Lindzey G. Handbook of Social Psychology. Hoboken, NJ: Wiley; 2010. [ Google Scholar ]
- Fowles JB, Terry P, Xi M, Hibbard J, Bloom CT, Harvey L. Measuring Self-Management of Patients’ and Employees’ Health: Further Validation of the Patient Activation Measure (PAM) Based on Its Relation to Employee Characteristics. Patient Education Counseling. 2009;77(1):116–22. doi: 10.1016/j.pec.2009.02.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- Friedkin N. Social Cohesion. Annual Review of Sociology. 2004;30:409–25. [ Google Scholar ]
- Fronstin P. Findings from the 2008 EBRI Consumer Engagement Health Care Survey. ERBI Issue Brief. 2008;323:1–42. [ PubMed ] [ Google Scholar ]
- Fronstin P. Findings from the 2010 EBRI/MGA Consumer Engagement Health Care Survey. EBRI Issue Brief. 2010;352:1–42. [ PubMed ] [ Google Scholar ]
- Galvin RS, Delbanco S, Milstein A, Belden G. Has the Leapfrog Group Had an Impact on the Health Care Market? Health Affairs. 2005;24(1):228–33. doi: 10.1377/hlthaff.24.1.228. [ DOI ] [ PubMed ] [ Google Scholar ]
- Glanz K, Rimer BK. Perspectives on Using Theory: Past, Present, and Future. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 509–18. [ Google Scholar ]
- Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. San Francisco: Jossey-Bass; 2008. [ Google Scholar ]
- Glanz K, Schwartz MD. Stress, Coping and Health Behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 211–36. [ Google Scholar ]
- Gradstein M, Schiff M. The Political Economy of Social Exclusion with Implications for Immigration Policy. Journal of Population Economics. 2006;19:327–44. [ Google Scholar ]
- Graham RE, Ahn RC, Davis RB, O'Connor BB, Eisenbers DM, Phillips RS. Use of Complementary and Alternative Medical Therapies among Racial and Ethnic Minority Adults: Results from the 2002 National Health Interview Survey. Journal of the National Medical Association. 2005;97(3):535–45. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Granovetter M. The Strength of Weak Ties. American Journal of Sociology. 1973;78(6):1360–80. [ Google Scholar ]
- Greene J, Hibbard J. Why Does Patient Activation Matter? An Examination of the Relationships between Patient Activation and Health-Related Outcomes. Journal of General Internal Medicine. 2011 doi: 10.1007/s11606-011-1931-2. November 30 (e-pub before print) [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gruman J, Rovner MH, French ME, Jeffress D, Sofaer S, Shaller D, Prager DJ. From Patient Education to Patient Engagement. Patient Education and Counseling. 2010;78:350–56. doi: 10.1016/j.pec.2010.02.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- Gruman J, Rovner MH, Jeffress D, Sofaer S, Shaller D, Prager D. A New Definition of Patient Engagement: What Is Engagement and Why Is It Important? Washington, DC: Center for the Advancement of Health; 2009. [ Google Scholar ]
- Harris KM, Buntin MB. Choosing a Health Care Provider: The Role of Quality Information. Research Synthesis Report: Robert Wood Johnson Foundation. 2008;14:1–26. [ PubMed ] [ Google Scholar ]
- Harvey L, Fowles JB, Xi M, Terry P. When Activation Changes, What Else Changes? The Relationship between Change in Patient Activation Measure (PAM) and Employees’ Health Status and Health Behaviors. Patient Education and Counseling. 2012 doi: 10.1016/j.pec.2012.02.005. March 26 (e-pub before print) [ DOI ] [ PubMed ] [ Google Scholar ]
- Haynes RB, Ackloo E, Sahota N, MacDonald HP, Yao X. Interventions for Enhancing Medication Adherence. Cochrane Database of Systematic Reviews. 2008;16(2):CD000011. doi: 10.1002/14651858.CD000011.pub3. [ DOI ] [ PubMed ] [ Google Scholar ]
- Heaney CH, Israel BA. Social Networks and Social Support. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 189–210. [ Google Scholar ]
- Helman C. Culture, Health, & Illness. London: Arnold; 2001. [ Google Scholar ]
- Herrmann-Pillath C. What Have We Learnt from 20 Years of Economic Research into Culture? International Journal of Cultural Studies. 2010;13(4):317–35. [ Google Scholar ]
- Herzog TA. A Welcomed and Overdue Debate. Health Psychology. 2010;29(1):102–3. [ Google Scholar ]
- Hesse BW, Nelson DE, Kreps GL, Croyle RT, Arora NK, Rimer BK, Viswanath K. Trust and Sources of Health Information. Archives of Internal Medicine. 2005;165(22):2618–24. doi: 10.1001/archinte.165.22.2618. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hibbard JH. Community-Based Participation Approaches and Individual Health Activation. Journal of Ambulatory Care Management. 2009a;32(4):275–77. doi: 10.1097/JAC.0b013e3181ba6f63. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hibbard JH. Using Systematic Measurement to Target Consumer Activation Strategies. Medical Care Research and Review. 2009b;66(suppl. 1):9S–27S. doi: 10.1177/1077558708326969. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hibbard JH, Cunningham PJ. How Engaged Are Consumers in Their Health and Health Care, and Why Does It Matter? Research Brief: Center for Studying Health System Change. 2008;8:1–9. [ PubMed ] [ Google Scholar ]
- Hibbard JH, Mahoney ER. Toward a Theory of Patient and Consumer Activation. Patient Education and Counseling. 2010;78:377–81. doi: 10.1016/j.pec.2009.12.015. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hibbard JH, Mahoney ER, Stock R, Tusler M. Do Increases in Patient Activation Result in Improved Self-Management Behaviors? Health Services Research. 2007a;42(4):1443–63. doi: 10.1111/j.1475-6773.2006.00669.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and Testing of a Short Form of the Patient Activation Measure. Health Services Research. 2005;40(6, part 1):1918–30. doi: 10.1111/j.1475-6773.2005.00438.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hibbard JH, Peters E, Dixon A, Tusler M. Consumer Competencies and the Use of Comparative Quality Information: It Isn't Just about Literacy. Medical Care Research and Review. 2007b;64(4):379–94. doi: 10.1177/1077558707301630. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health Services Research. 2004;39(4, part 1):1005–26. doi: 10.1111/j.1475-6773.2004.00269.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hunter A. The Loss of Community: An Empirical Test through Replication. American Sociology Review. 1975;40(5):537–52. [ Google Scholar ]
- Hurley RE, Keenan PS, Martsolf GR, Maeng DD, Scanlon DP. Early Experiences with Consumer Engagement Initiatives to Improve Chronic Care. Health Affairs. 2009;28(1):277–83. doi: 10.1377/hlthaff.28.1.277. [ DOI ] [ PubMed ] [ Google Scholar ]
- IOM (Institute of Medicine), Committee on Health and Behavior. Health and Behavior: The Interplay of Biological, Behavioral, and Societal Influences. Washington, DC: National Academies Press; 2001. [ PubMed ] [ Google Scholar ]
- Janz NK, Becker MH. The Health Belief Model: A Decade Later. Health Education Quarterly. 1984;11:1–47. doi: 10.1177/109019818401100101. [ DOI ] [ PubMed ] [ Google Scholar ]
- Jepson RG, Harris FM, Platt S, Tannahill C. The Effectiveness of Interventions to Change Six Health Behaviors: A Review of Reviews. BMC Public Health. 2010;10:538–54. doi: 10.1186/1471-2458-10-538. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jones JA, Meehan-Andrews TA, Smith KB, Humphreys JS, Griffin L, Wilson B. “There's No Point in Complaining, Nothing Changes”: Rural Disaffection with Complaints as an Improvement Method. Australian Health Review. 2006;30(3):322–32. doi: 10.1071/ah060322. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kegeler MC, Glanz K. Perspectives on Group, Organization, and Community Interventions. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 389–404. [ Google Scholar ]
- Ketelaar NA, Faber MJ, Flottorp S, Rygh LH, Deane KH, Eccles MP. Public Release of Performance Data in Changing Behavior of Consumers, Health Care Professionals or Organisations. Cochrane Database of Systematic Reviews. 2011;9(11):CD004538. doi: 10.1002/14651858.CD004538.pub2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- KFF-HRET (Kaiser Family Foundation and Health Research and Education Trust) Employer Health Benefits: 2008 Annual Survey, September 24. 2008. Available at http://ehbs.kff.org/pdf/7790.pdf (accessed July 3, 2012)
- KFF-HRET (Kaiser Family Foundation and Health Research and Education Trust) Employer Health Benefits: 2011 Annual Survey, September 27. 2011. Available at http://ehbs.kff.org/pdf/2011/8225.pdf (accessed July 3, 2012)
- Kleinman A. Patients and Healers in the Context of Culture: An Exploration of the Borderland between Anthropology, Medicine, and Psychiatry. Berkeley: University of California Press; 1980. [ Google Scholar ]
- Kleinman A, Hall-Clifford R. Stigma: A Social, Cultural and Moral Process. Journal of Epidemiology and Community Health. 2009;63(6):418–19. doi: 10.1136/jech.2008.084277. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kolstad JT, Chernew ME. Quality and Consumer Decision Making in the Market for Health Insurance and Health Care Services. Medical Care Research & Review. 2009;66(suppl.1):28S–52S. doi: 10.1177/1077558708325887. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kreuter MW, Haughton LT. Integrating Culture into Health Information for African American Women. American Behavioral Scientist. 2006;49(6):794–811. [ Google Scholar ]
- Larson C, Schlundt D, Patel K, Goldzweig I, Hargreaves M. Community Participation in Health Initiatives for Marginalized Populations. Journal of Ambulatory Care Management. 2009;32(4):264–70. doi: 10.1097/JAC.0b013e3181ba6f74. [ DOI ] [ PubMed ] [ Google Scholar ]
- Larson NI, Story MT, Nelson MC. Neighborhood Environments: Disparities in Access to Healthy Foods in the U.S. American Journal of Preventive Medicine. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lau R. Individual and Contextual Influences on Group Identification. Social Psychology Quarterly. 1989;52(3):220–31. [ Google Scholar ]
- Leape L, Berwick D, Clancy C, Conway J, Gluck P, Guest J, Lawrence D, Morath J, O'Leary D, O'Neill P, Pinakiewicz D, Isaac T. Transforming Health Care: A Safety Imperative. Quality Safety in Health Care. 2009;28(6):424–28. doi: 10.1136/qshc.2009.036954. [ DOI ] [ PubMed ] [ Google Scholar ]
- Leary M. Affiliation, Acceptance, and Belonging: The Pursuit of Interpersonal Connection. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of Social Psychology. Hoboken, NJ: Wiley; 2010. pp. 864–97. [ Google Scholar ]
- Lee PV, Hoo E. Beyond Consumer-Driven Health Care: Purchasers’ Expectations of All Plans. Health Affairs. 2006;25(6):w544–48. doi: 10.1377/hlthaff.25.w544. [ DOI ] [ PubMed ] [ Google Scholar ]
- Link BG, Phalen JC. Conceptualizing Stigma. Annual Review of Sociology. 2001;27:363–85. [ Google Scholar ]
- Lippke S, Schwarzer R, Ziegelmann JP, Scholz U, Schuz B. Targeting Stage-Specific Effects of a Stage-Matched Intervention: A Randomized Controlled Trial Targeting Physical Exercise and Its Predictors. Health Education Behavior. 2010;37(4):533–46. doi: 10.1177/1090198109359386. [ DOI ] [ PubMed ] [ Google Scholar ]
- Longo DR. Understanding Health Information, Communication, and Information Seeking of Patients and Consumers: A Comprehensive & Integrated Model. Health Expectations. 2005;8:189–94. doi: 10.1111/j.1369-7625.2005.00339.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lorig K, Ritter PL, Villa FJ, Armas J. Community-Based Peer-Led Diabetes Self-Management: A Randomized Trial. Diabetes Education. 2009;35(4):641–51. doi: 10.1177/0145721709335006. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a Self-Management Program on Patients with Chronic Disease. Effective Clinical Practice. 2001;4(6):256–62. [ PubMed ] [ Google Scholar ]
- Lynch J, Smith GD, Harper S, Hillemeier M, Ross N, Kaplan GA, Wolfson M. Is Income Inequality a Determinant of Population Health? Part 1: A Systematic Review. The Milbank Quarterly. 2002;82(1):5–99. doi: 10.1111/j.0887-378X.2004.00302.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Maillet P, Halterman S. The Consumer-Driven Approach: Defining and Measuring Success. Benefits Quarterly. 2004;2:1–9. [ PubMed ] [ Google Scholar ]
- Merriam-Webster. Activate. 2012a. Available at http://merriam-webster.com/dictionary/activate (accessed January 7, 2012)
- Merriam-Webster. Consumer. 2012b. Available at http://merriam-webster.com/dictionary/consumer (accessed January 7, 2012)
- Merriam-Webster. Engagement. 2012c. Available at http://merriam-webster.com/dictionary/engagement (accessed January 7, 2012)
- Merriam-Webster. Shopping. 2012d. Available at http://merriam-webster.com/dictionary/shopping (accessed January 7, 2012)
- McAlister AL, Perry CL, Parcel GS. How Individuals, Environments and Health Behaviors Interact: Social Cognitive Theory. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 167–88. [ Google Scholar ]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An Ecological Perspective on Health Promotion Programs. Health Education Quarterly. 1988;15:351–77. doi: 10.1177/109019818801500401. [ DOI ] [ PubMed ] [ Google Scholar ]
- Minkler M, Wallerstein N, Wilson N. Improving Health through Community Organization and Community Building. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 283–309. [ Google Scholar ]
- Mosen DM, Schmittdiel J, Hibbard J, Sobel D, Remmers C, Bellows J. Is Patient Activation Associated with Outcomes of Care for Adults with Chronic Conditions? Journal of Ambulatory Care Management. 2007;30(1):21–29. doi: 10.1097/00004479-200701000-00005. [ DOI ] [ PubMed ] [ Google Scholar ]
- Munro S, Lewin S, Swart T, Volmink J. A Review of Health Behaviour Theories: How Useful Are These for Developing Interventions to Promote Long-Term Medication Adherence for TB and HIV/AIDS? BMC Public Health. 2007;7:104–20. doi: 10.1186/1471-2458-7-104. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- National Patient Safety Foundation. Ask-Me-Three. 2009. Available at http://www.npsf.org/askme3/ (accessed November 20, 2009)
- Nemet GF, Bailey AJ. Distance and Health Care Utilization among the Rural Elderly. Social Science & Medicine. 2000;50(9):1197–1208. doi: 10.1016/s0277-9536(99)00365-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- Nichols LM, Ginsburg PB, Berenson RA, Christianson J, Hurley BE. Are Market Forces Strong Enough to Deliver Efficient Health Care Systems? Confidence Is Waning. Health Affairs. 2004;23(2):8–21. doi: 10.1377/hlthaff.23.2.8. [ DOI ] [ PubMed ] [ Google Scholar ]
- Northrop M, Pittam G, Caan W. The Expectations of Families and Patterns of Participation in a Trailblazer Sure Start. Community Practitioner. 2008;81(2):24–28. [ PubMed ] [ Google Scholar ]
- Painter JE, Borba CP, Hynes M, Mays D, Glanz K. The Use of Theory in Health Behavior Research from 2000 to 2005: A Systematic Review. Annals of Behavioral Medicine. 2008;33(3):358–62. doi: 10.1007/s12160-008-9042-y. [ DOI ] [ PubMed ] [ Google Scholar ]
- Painter MW, Lavizzo-Mourey R. Aligning Forces for Quality: A Program to Improve Health and Health Care in Communities across the United States. Health Affairs. 2008;27(5):1461–63. doi: 10.1377/hlthaff.27.5.1461. [ DOI ] [ PubMed ] [ Google Scholar ]
- Parsons T. The Social System. Glencoe, IL: Free Press; 1951. [ Google Scholar ]
- Prochaska JO. Decision Making in the Transtheoretical Model of Behavior Change. Medical Decision Making. 2008;28(6):845–49. doi: 10.1177/0272989X08327068. [ DOI ] [ PubMed ] [ Google Scholar ]
- Prochaska JO, Redding CA, Evers KE. The Transtheoretical Model and Stages of Change. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 97–122. [ Google Scholar ]
- Prochaska JO, Velcier W, Rossi J, Goldstein M, Marcus B, Rakowski W, Fiore C, Harlow L, Redding C, Rosenbloom D, Rossi S. Stages of Change and Decisional Balance for 12 Problem Behaviors. Health Psychology. 1994;13(1):39–46. doi: 10.1037//0278-6133.13.1.39. [ DOI ] [ PubMed ] [ Google Scholar ]
- Protheroe J, Nutbeam D, Rowlands G. Health Literacy: A Necessity for Increasing Participation in Health Care. British Journal of General Practice. 2009;59(567):721–23. doi: 10.3399/bjgp09X472584. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Putnam RD. Bowling Alone. New York: Simon & Schuster; 1995. [ Google Scholar ]
- Reitz JG, Sklar SM. Culture, Race, and Economic Assimilation of Immigrants. Sociological Forum. 1997;12(2):233–77. [ Google Scholar ]
- Remmers C, Hibbard J, Mosen DM, Wagenfield M, Hoye RE, Jones C. Is Patient Activation Associated with Future Health Outcomes and Healthcare Utilization among Patients with Diabetes? Journal of Ambulatory Care Management. 2009;32(4):320–27. doi: 10.1097/JAC.0b013e3181ba6e77. [ DOI ] [ PubMed ] [ Google Scholar ]
- Richard L, Gauvin L, Raine K. Ecological Models Revisited: Their Uses and Evolution in Health Promotion over Two Decades. Annual Review of Public Health. 2011;32:307–26. doi: 10.1146/annurev-publhealth-031210-101141. [ DOI ] [ PubMed ] [ Google Scholar ]
- Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the Impact of Menu Labeling on Food Choices and Intake. American Journal of Public Health. 2010;100:312–18. doi: 10.2105/AJPH.2009.160226. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Roblin DW, Becker ER. The Community Counts! But the Question Remains, How Much? Journal of Ambulatory Care Management. 2009;32(4):292–94. doi: 10.1097/JAC.0b013e3181ba6e62. [ DOI ] [ PubMed ] [ Google Scholar ]
- Rolfe T, Sheehan B, Davidson R. Are Consumers on Community Treatment Orders Informed of Their Legal and Human Rights? A West Australian Study. International Journal of Mental Health Nursing. 2008;17(1):36. doi: 10.1111/j.1447-0349.2007.00509.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Rosen P, Anell A, Hjortsberg C. Patient Views on Choice and Participation in Primary Health Care. Health Policy. 2001;55:121–128. doi: 10.1016/s0168-8510(00)00122-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ryan RM, Deci EL. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. American Psychologist. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [ DOI ] [ PubMed ] [ Google Scholar ]
- Sallis JF, Owen N, Fisher EB. Ecological Models of Health Behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 465–86. [ Google Scholar ]
- Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “Neighborhood Effects”: Social Processes and New Directions in Research. Annual Review of Sociology. 2002;28:443–78. [ Google Scholar ]
- Scanlon DP, Alexander JA, Beich J, Christianson JB, Hasnain-Wynia R, McHugh MC, Mittler JN, Shi Y, Bodenschatz LJ. Evaluating a Community-Based Program to Improve Healthcare Quality: Research Design for the Aligning Forces for Quality Initiative. American Journal of Managed Care. 2012;18(6):eS165–eS176. [ PubMed ] [ Google Scholar ]
- Schaeffer LD, McMurtry DE. When Excuses Run Dry: Transforming the U.S. Health Care System. Health Affairs. 2004:117–20. doi: 10.1377/hlthaff.var.117. web suppl.:VAR. [ DOI ] [ PubMed ] [ Google Scholar ]
- Schumaker S, Ockene J, Riekert K. The Handbook of Health Behavior Change. New York: Springer; 2009. [ Google Scholar ]
- Seven R. King County's “Health Incentives” Program Relies on the Power of Preventative Care. 2009. Seattle Times, March 1.
- Shaller D. Consumer Engagement: Whose Responsibility Is It? American Journal of Medical Quality. 2007;22(5):309–10. doi: 10.1177/1062860607305596. [ DOI ] [ PubMed ] [ Google Scholar ]
- Shelley BM, Sussman AL, Williams RL, Crabtree BF. “They Don't Ask Me So I Don't Tell Them”: Patient-Clinician Communication about Traditional, Complementary, and Alternative Medicine. Annals of Family Medicine. 2009;7(2):139–47. doi: 10.1370/afm.947. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stanley A, Cantor JC, Guarnaccia P. Holes in the Safety Net: A Case Study of Access to Prescription Drugs and Specialty Care. Journal of Urban Health. 2008;85(4):555–71. doi: 10.1007/s11524-008-9282-y. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stuber J, Meyer I, Link B. Stigma, Prejudice, Discrimination, and Health. Social Science & Medicine. 2008;67(3):351–57. doi: 10.1016/j.socscimed.2008.03.023. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Swann WB, Bosson JK. Self and Identity. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of Social Psychology. Hoboken, NJ: Wiley; 2010. pp. 589–628. [ Google Scholar ]
- Tajfel H, Turner J. An Integrative Theory of Intergroup Conflict. In: Austin WG, Worchel S, editors. The Social Psychology of Intergroup Relations. Monterey, CA: Brooks/Cole; 1979. pp. 33–48. [ Google Scholar ]
- Terry M. Health Care Consumerism: Engaging the Real Buyers—Employees. Benefits Quarterly. 2005;21(2):18–21. [ PubMed ] [ Google Scholar ]
- Uchino BN, Bowen K, Carlisle M, Birmingham W. Psychological Pathways Linking Social Support to Health Outcomes: A Visit with the “Ghosts” of Research Past, Present and Future. Social Science & Medicine. 2012;74:949–57. doi: 10.1016/j.socscimed.2011.11.023. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Van Sluijs EMF, van Poppel MNM, van Mechelen W. Stage-Based Lifestyle Interventions in Primary Care: Are They Effective? American Journal of Preventive Medicine. 2004;26(4):330–43. doi: 10.1016/j.amepre.2003.12.010. [ DOI ] [ PubMed ] [ Google Scholar ]
- Viswanath K. Perspectives on Models of Interpersonal Health Behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 271–82. [ Google Scholar ]
- Warner K, Mendez D. Tobacco Control Policy in Developed Countries: Yesterday, Today, and Tomorrow. Nicotine & Tobacco Research. 2010;12(9):876–87. doi: 10.1093/ntr/ntq125. [ DOI ] [ PubMed ] [ Google Scholar ]
- Williams D, Collins C. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Reports. 2001;116:404–16. doi: 10.1093/phr/116.5.404. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wolff LS, Subramanian SV, Acevedo-Garcia D, Weber D, Kawachi I. Compared to Whom? Subjective Social Status, Self-Rated Health, and Referent Group Sensitivity in a Diverse US Sample. Social Science and Medicine. 2010;70(12):2019–28. doi: 10.1016/j.socscimed.2010.02.033. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yzerbyt V, Demoulin S. Intergroup Relations. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of Social Psychology. Hoboken, NJ: Wiley; 2010. pp. 1024–83. [ Google Scholar ]
- View on publisher site
- PDF (681.3 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
COMMENTS
One of the key benefits of consumer health is its impact on public health and safety. Through consumer health information, individuals are educated about food safety, drug safety, and product safety, ensuring that they are aware of potential risks and can take necessary precautions.Moreover, consumer health organizations raise awareness about disease prevention and control, promoting vaccines ...
Essays.io ️ Consumer Health Information, Essay Example from students accepted to Harvard, Stanford, and other elite schools ... Consumer health literacy is an important component of modern healthcare practice because it enables patients to be proactive in understanding the issues that impact their health, as well as in recognizing how to best ...
This essay offers two new lenses for studying consumer health. Theories of psycholmmunology and institutional environments bring a wider array of individual, social, cultural, and organizational ...
INTRODUCTION. Every day, consumers make decisions that have both direct and indirect impact on their health. The COVID-19 pandemic, and the long-term physical and mental complications that have ensued, underscores the importance of developing a holistic understanding of drivers of consumers' health and medical decisions.
Private consumption is an important factor of economic growth in most parts of the world (United Nations 2019e), so consumption will be developed further.The problem of achieving a basic level of life is acute for many global consumers (Hilton 2008).The need for novelty inherent in people will also remain as is (Lipovetsky and Serroy 2016).. The consumer society is not a fixed phenomenon; it ...
Furthermore, consumer health engagement can be the key to systematically diagnose and make sense of the different organizational, relational, and psychological components in play in the dynamic exchange between "demand" and "supply" of health and care. ... The importance of this construct in cancer studies (Villani et al. Saita et al ...
Consumers are now ever more concerned about the quality, safety, and environmental-friendliness of food. The growing need for a healthier diet caused a rapid increase in organic food consumption worldwide (Al-Swidi et al., 2014; Kushwah et al., 2019; Waqas & Hong, 2019).The industry of organic or natural food has nurtured exponentially in recent years with a growth rate of approximately 10% to ...
Model Description Selected Citations; Focus on the Individual: Health belief model: Originally developed to predict adoption of preventive behaviors, this model posits that an individual's decision to act stems from people's perceptions of (1) the severity of the threat to their health, (2) their susceptibility to this threat, and (3) the benefits of and barriers to action.
Consumer health is important because it is directly related to the overall health of the population. When individuals are able to access healthcare, understand health information, make healthy choices, and achieve good health outcomes, the overall health of the population improves. The internet has made searching for consumer health information ...
Food is both privately and socially consumed and is an important part of consumers' buying decisions. In recent decades, consumption of fast food and food away from home has increased in the United States (Krieger et al., 2013).According to Poti and Popkin (2011) and Powell et al. (2012), in 2007 to 2008, fast-food and full-service restaurants accounted for an estimated per day consumption ...