Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals

You are here
- Volume 78, Issue 10
- Intergenerational transmission of health inequalities: research agenda for a life course approach to socioeconomic inequalities in health
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-6090-4376 Tanja A J Houweling 1 ,
- http://orcid.org/0000-0002-7034-1922 Ilona Grünberger 2
- 1 Department of Public Health , Erasmus MC, University Medical Center Rotterdam , Rotterdam , The Netherlands
- 2 Department of Public Health Sciences , Stockholm University , Stockholm , Sweden
- Correspondence to Dr Tanja A J Houweling, Department of Public Health, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands; a.j.houweling{at}erasmusmc.nl
Explanations for socioeconomic inequalities in adult health are usually sought in behaviours and environments in adulthood. Yet, there is compelling evidence that the first two decades of life contribute substantially to both adult socioeconomic position (SEP) and adult health. This has implications for explanatory health inequalities research.
We propose an analytical framework to advance research on the intergenerational transmission of health inequalities, that is, on intergenerational transmission of socioeconomic and associated health (dis)advantages at the family level, and its contribution to health inequalities at the population level. The framework distinguishes three transmission pathways: (1) intergenerational transmission of SEP, with effects on offspring health fully mediated by offspring SEP; (2) intergenerational transmission of health problems affecting SEP and (3) intergenerational transmission of both SEP and health, without a causal relationship between offspring adult SEP and health. We describe areas for future research along this framework and discuss the challenges and opportunities to advance this field.
- Health inequalities
- Life course epidemiology
- CHILD HEALTH
- PUBLIC HEALTH
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/jech-2022-220163
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
A framework for research
Traditionally, explanations for socioeconomic inequalities in adult health are sought in behaviours and environments in adulthood. 1 Figure 1 visualises this relationship between adult socioeconomic position (SEP) and adult health. In this framework, SEP is causally related to proximal health determinants, such as smoking, and health outcomes in adulthood; and there is some reverse causation between health (determinants) and SEP (also called ‘selection’).
- Download figure
- Open in new tab
- Download powerpoint
Traditional framework for explaining socioeconomic health inequalities. SEP, socioeconomic position.
Yet, from a broad range of disciplines, there is evidence that the early years of life contribute substantially to both adult SEP and adult health. In a companion paper, we have described how socioeconomic and health (dis)advantages are intergenerationally transmitted at the family level, and contribute to the persistence of socioeconomic health inequalities at the population level. 2 We found evidence that broadly the same mechanisms, in the fetal and postnatal environment, shape both adult SEP and adult health. This has implications for explanatory research on socioeconomic inequalities in health.
Figure 2 provides a framework for studying socioeconomic health inequalities from an intergenerational perspective. The pathways through which health inequalities are intergenerationally transmitted, can be grouped into three models.
Conceptual framework for the intergenerational transmission of health inequalities. Three models of intergenerational transmission of socioeconomic health inequalities: (1) socioeconomic transmission: intergenerational transmission of SEP, combined with an effect of offspring adult SEP on health; (2) health transmission: intergenerational transmission of parental health problems that affect SEP; (3) sociobiological transmission: parental SEP influences both offspring SEP and offspring health (determinants). SEP, socioeconomic position.
In the first model (socioeconomic transmission, red arrows), the SEP-health link is transmitted across generations as a result of intergenerational transmission of SEP. 3 Intergenerational transmission of SEP occurs through (in)direct transfers (eg, of wealth), and via the fetal and postnatal environment—through the influence of parental SEP, parental proximal health determinants and parental health outcomes associated with SEP. As long as offspring adult SEP influences health, there needs to be no direct causal relationship between parental SEP and offspring health (determinants) for health inequalities to be intergenerationally transmitted. In this model, the relationship between parental SEP and offspring health, is fully mediated by offspring SEP. Consequently, statistical adjustment for offspring SEP would lead to severe underestimation of the contribution of intergenerational transmission to adult health inequalities.
In the second model (health transmission, blue arrows), the SEP-health link is transmitted across generations through intergenerational transmission of health problems that affect SEP, such as mental health problems. There is substantial evidence that such parental problems affect child development and well-being, but there is a paucity of evidence about their role in explaining offspring adult health inequalities.
The third model (sociobiological transmission, green arrows) consists of a purely intergenerational causal effect of SEP on adult health. Here, parental SEP influences both offspring SEP and offspring health (determinants), without a causal relationship between offspring adult SEP and health. 3 This is sometimes called indirect selection. The fetal environment, the learning and psychosocial environment, and childhood and adolescent socialisation, affect offspring adult SEP and health by influencing child and adolescent cognitive, socialemotional, and physical health and development, and patterns of beliefs, values and behavioural habits.
In practice, SEP and health are causally related within and across generations—their contributions varying with the health outcome studied—such that the three above models reinforce each other. The relative importance of the three models, and how this varies over historical time and across societal contexts, remains largely unknown. Yet, this is crucial information for designing interventions and determining the appropriate timing of policies to reduce health inequalities. 4
Research agenda based on the framework
Our framework can be used as basis for asking relevant questions to advance this field, including questions around how policies and other societal conditions affect the different pathways in this framework.
Intergenerational transmission of SEP
A first set of questions relates to the intergenerational transmission of SEP. What proportion of adult health inequalities is attributable to the effect of parental SEP on offspring SEP? A rough calculation can be analogous to that of population attributable fractions. So, with what percentage would health inequalities reduce if offspring of low SEP parents had the same educational (wealth, income) distribution as offspring of high SEP parents? Next, what is the impact of structural determinants of intergenerational social mobility, for example, social protection policies and education systems, on adult health inequalities? Intergenerational social mobility is larger in some cohorts and countries than in others, 5 arguably affecting the proportion of health inequalities attributable to intergenerational SEP persistence. This suggests room for policy-making, by ensuring that all children can develop to their full potential, irrespective of parental SEP. It also suggests the need to better understand these structural factors and their political and historical determinants.
The effect of parental and offspring SEP on offspring health
A second set of questions relates to the effect of parental and offspring SEP on offspring health. Does parental SEP have an independent effect on offspring adult health, that is, not mediated by offspring adult SEP? 6–8 To what extent is the health effect of offspring adult SEP explained by parental SEP? What is the relative importance of the independent effects of offspring and parental SEP? Three methodological problems complicate answering these questions. The first is intermediate confounding. Important determinants of both offspring SEP and offspring health—including cognitive ability, socialemotional well-being and habits—are strongly influenced by parental SEP. When examining the independent health effects of offspring SEP, these factors, shaped in early life, could be important confounders. 9 The second problem is mediator-outcome confounding (collider bias). Independent effects of parental and offspring SEP are mostly examined in discordant parent-offspring pairs, that is, in cases of intergenerational upward or downward mobility. 6–8 But these may be selective groups. Analyses should, therefore, be adjusted for factors influencing both intergenerational mobility and offspring adult health. Third, intergenerational social mobility may have health effects itself, requiring the inclusion of interaction terms between parental SEP and offspring adult SEP. Modern causal mediation analyses can partly address these problems and be used to decompose the effect of parental SEP on offspring health into direct effects, and indirect effects via offspring SEP, even in the presence of interaction. 10 Also, structured approaches to compare life course models have been applied to these questions. 4 11 Howe et al have linked causal mediation analysis to a structured life course approach. 3 A next step would be to address intermediate confounding and mediator-outcome confounding in such models.
While the above models and mechanisms could be seen as acting within relatively stable social and policy contexts, another way forward would be through research on the health effects of exogenous changes in parental and offspring adult SEP, for example, income changes due to new social security policies. A possible strategy would be to focus on determinants of adult health that are largely shaped in early life—including cognitive ability, executive functions, social-emotional well-being, habits and beliefs 12 13 —and examine to which extent these explain adult health inequalities. 14 Such a strategy could also include research on (1) stability of the association between SEP on the one hand, and cognitive ability, executive functions, behavioural habits and beliefs on the other, throughout childhood, adolescence and beyond 15 ; (2) their contribution to inequalities in health behaviours in adulthood and (3) and their interaction with the environment in both childhood and adulthood (eg, Are changes in school policies affecting children from disadvantaged backgrounds disproportionately? Is a health promoting environment more important for individuals with lower executive functions?)
Intergenerational transmission of health problems associated with SEP
A third set of questions relate to the intergenerational transmission of health problems that are associated with SEP. What is the contribution of parental health problems, such as mental health problems, which affect both parental SEP and their offspring’s development and life course outcomes, to the intergenerational transmission of health inequalities? And what is the relative importance of fetal and postnatal environmental pathways to this transmission? A first step would be to describe what proportion of parents with low SEP suffer from such health problems. In social epidemiological research, low SEP tends to be treated as a uniform category. 16 Unpacking this to understand the complex set of problems underlying low SEP, and how these problems cluster and interact, and are transmitted intergenerationally in different societal and policy contexts, is important, also for policy-making.
The first two decades of life, from the prenatal period to early adulthood, play an important role in the development of socioeconomic inequalities in adult health and help explain the persistence of these inequalities in welfare states. It is time to give more attention to these early years in research on and policies to tackle adult health inequalities. It is important to recognise that SEP, and many determinants of health and health behaviour, are formed early in life. SEP and health determinants that are shaped in these early years—including cognitive development, executive functions, beliefs and habits—should not be taken as a given. Rather, understanding their development and intergenerational transmission should be squarely rooted within health inequalities research, thereby providing a basis for preventive policies.
Methodological advances and the coming of age of many birth cohorts provide opportunities for empirical research across multiple generations. We have provided a framework to advance this research field. It will require interdisciplinary research to not only understand the complexities of the physiological processes that lead to intergenerational transmission of health inequalities, but also the social complexities that often remain hidden behind the term ‘SEP’. Importantly, our framework also describes new opportunities for action. There is a lot to be gained.
Ethics statements
Patient consent for publication.
Not applicable.
Acknowledgments
We thank Prof. Johan P. Mackenbach for his comments on an outline of this paper and for helpful discussions during preparation of the International Symposium on the Intergenerational Transmission of Health Inequalities that TAJH organised with him on 25 October 2018 –26 October 2018, Rotterdam, the Netherlands. We thank presenters and participants at this symposium for their presentations and their contributions to the discussions.
- Mackenbach JP
- Houweling TAJ ,
- Grünberger I
- Macdonald-Wallis C , et al
- Mishra GD ,
- Goodman A , et al
- Galobardes B ,
- Hossin MZ ,
- Falkstedt D
- Loucks EB ,
- Rogers ML , et al
- VanderWeele TJ
- Black S , et al
- Early Child Development Knowledge Network of the Commission on the Social Determinants of Health
- Sehmi R , et al
- Hemmingsson T ,
- v Essen J ,
- Melin B , et al
- Hackman DA ,
- Evans GW , et al
X @TanjaHouweling
Contributors TAJH conceived of and drafted the manuscript. IG critically reviewed the draft manuscript and contributed to revisions. Both authors have approved of the final manuscript before submission.
Funding TAJH is supported by NWO grant number NWA.1238.18.001 and though a grant awarded by the Norwegian Research Council (project number 288638) to the Centre for Global Health Inequalities Research (CHAIN) at the Norwegian University for Science and Technology (NTNU). The International Symposium on the Intergenerational Transmission of Health Inequalities was financially supported by the Royal Dutch Academy of Sciences (KNAW) and a EUR Research Excellence initiative grant obtained by TAJH. TAJH is also member of a ZonMW funded project on socioeconomic inequalities in child development (grant number 531003013). IG is supported by a grant from the Swedish Research Council for Health, Working Life and Welfare (FORTE project number 2018-00211).
Disclaimer The funders had no role in study design; in the collection, analysis and interpretation of data; in the writing of the articles; and in the decision to submit it for publication.
Competing interests None declared.
Provenance and peer review Not commissioned; internally peer reviewed.
Read the full text or download the PDF:

- Create new account
- Reset your password
- Translation
- Alternative Standpoint
- HT Parekh Finance Column
- Law and Society
- Strategic Affairs
- Perspectives
- Special Articles
- The Economic Weekly (1949–1965)
- Economic and Political Weekly
- Open Access
- Notes for contributors
- Style Sheet
- Track Your Submission
- Resource Kits
- Discussion Maps
- Interventions
- Research Radio
Advanced Search
A + | A | A -
Violence against Women in India
Understanding trends in the extent of violence against women can be helpful in challenging violence against women and gender inequality. In this paper, we compare the incidence of violence, as measured in the National Family Health Surveys, to the reporting of violence, as compiled by the National Crime Records Bureau. We also shed light on heterogeneity in incidence and reporting across India’s states. We find that violence against women is common, that most violence against women is not reported to the police, that violence by husbands is less likely to be reported than violence by others, and that the reporting of violence has not improved over the last decade and a half. These concerning findings highlight the urgent need for social and legal interventions to reduce violence against women, and to improve its reporting.
The authors would like to thank Vipul Paikra for helpful research assistance.
Sexual and physical violence against women is one of the clearest and most detrimental manifestations of gender inequa lity. The United Nations Sustainable Development Goals aim at “eliminating violence against women and girls” (UNWomen 2022). And violence against women remains one of the core concerns of movements against patriarchy in India and globally (Kannabiran and Menon 2007). Despite this recogn ition, public discussions on violence against women in India are c onstrained by the lack of reliable information on the magnitude of violence against women, the extent to which cases are reported to the police, or trends in incidence and reporting (Bhattacharya 2013; Gupta 2014; Rukmini 2021).

Dear Reader,
To continue reading, become a subscriber.
Explore our attractive subscription offers.
To gain instant access to this article (download).
(Readers in India)
(Readers outside India)
Your Support will ensure EPW’s financial viability and sustainability.
The EPW produces independent and public-spirited scholarship and analyses of contemporary affairs every week. EPW is one of the few publications that keep alive the spirit of intellectual inquiry in the Indian media.
Often described as a publication with a “social conscience,” EPW has never shied away from taking strong editorial positions. Our publication is free from political pressure, or commercial interests. Our editorial independence is our pride.
We rely on your support to continue the endeavour of highlighting the challenges faced by the disadvantaged, writings from the margins, and scholarship on the most pertinent issues that concern contemporary Indian society.
Every contribution is valuable for our future.
- About Engage
- For Contributors
- About Open Access
- Opportunities
Term & Policy
- Terms and Conditions
- Privacy Policy
Circulation
- Refund and Cancellation
- User Registration
- Delivery Policy
Advertisement
- Why Advertise in EPW?
- Advertisement Tariffs
Connect with us
320-322, A to Z Industrial Estate, Ganpatrao Kadam Marg, Lower Parel, Mumbai, India 400 013
Phone: +91-22-40638282 | Email: Editorial - [email protected] | Subscription - [email protected] | Advertisement - [email protected]
Designed, developed and maintained by Yodasoft Technologies Pvt. Ltd.
September National Health Observances: Healthy Aging, Sickle Cell Disease, and More
Each month, we feature select National Health Observances (NHOs) that align with our priorities for improving health across the nation. In September, we’re raising awareness about healthy aging, sickle cell disease, substance use recovery, and HIV/AIDS.
Below, you’ll find resources to help you spread the word about these NHOs with your audiences.
- Healthy Aging Month Each September, we celebrate Healthy Aging Month to promote ways people can stay healthy as they age. Explore our healthy aging resources , bookmark the Healthy People 2030 and Older Adults page , share our Move Your Way® materials for older adults , and check out the Physical Activity Guidelines for Americans Midcourse Report . You can also share resources related to healthy aging from the National Institute on Aging — and register for the 2024 National Healthy Aging Symposium to hear from experts on innovations to improve the health and well-being of older adults.
- National Recovery Month The Substance Abuse and Mental Health Services Administration (SAMHSA) sponsors National Recovery Month to raise awareness about mental health and addiction recovery. Share our MyHealthfinder resources on substance use and misuse — and be sure to check out Healthy People 2030’s evidence-based resources related to drug and alcohol use .
- National Sickle Cell Awareness Month National Sickle Cell Awareness Month is a time to raise awareness and support people living with sickle cell disease. Help your community learn about sickle cell disease by sharing these resources from the National Heart, Lung, and Blood Institute (NHLBI) . You can also encourage new and expecting parents to learn about screening their newborn baby for sickle cell . And be sure to view our Healthy People 2030 objectives on improving health for people who have blood disorders .
- National HIV/AIDS and Aging Awareness Day (September 18) On September 18, we celebrate HIV/AIDS and Aging Awareness Day to encourage older adults to get tested for HIV. Share CDC’s Let’s Stop HIV Together campaign to help promote HIV testing, prevention, and treatment. MyHealthfinder also has information for consumers about getting tested for HIV and actionable questions for the doctor about HIV testing . Finally, share these evidence-based resources on sexually transmitted infections from Healthy People 2030.
- National Gay Men’s HIV/AIDS Awareness Day (September 27) National Gay Men’s HIV/AIDS Awareness Day on September 27 highlights the impact of HIV on gay and bisexual men and promotes strategies to encourage testing. Get involved by sharing CDC’s social media toolkit and HIV information to encourage men to get tested — and share our MyHealthfinder resources to help people get tested for HIV and talk with their doctor about testing .
We hope you’ll join us in promoting these important NHOs with your networks to help improve health across the nation!
The Office of Disease Prevention and Health Promotion (ODPHP) cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Why a health...
Why a health inequalities white paper is still so vital and should not be scrapped
Linked news.
Health inequalities: Government must not abandon white paper, health leaders urge
- Related content
- Peer review
- Layla McCay , director of policy
- NHS Confederation
Health inequalities across the country have been widening for many years, and if they had ever not been obvious before, the covid-19 pandemic served to shine a spotlight on the health inequalities which are so keenly apparent in so many communities across the UK.
A significant and growing gap in life expectancy for people living in areas with the highest and lowest levels of deprivation means there is now an urgent need to create opportunities for health and care systems to drive improvements in population health outcomes at pace. So, if the rumours are to be believed and the new secretary of state for health and social care has decided to shelve the work of her predecessor and abandon the long-awaited health inequalities white paper this will deal a huge blow to the health and life chances of millions of people across the country.
The newly created Integrated Care Systems (ICSs) provide a fresh opportunity for central government and local leaders to share power locally in a flexible and dynamic way which, over time, should really help reduce inequalities in health outcomes. Through integrated care partnerships (ICPs), local leaders can embrace community power and they will have a mechanism to develop services according to the priorities of their local communities.
To improve population health, NHS, local government and social care leaders alike are urging the government not to perform such a significant and damaging volte-face, but to build on existing knowledge of what works and to consider holistically the social, economic, and commercial determinants of health when addressing inequalities. Their view is that a system-wide approach is fundamental and breaking down siloed ways of working within local systems will be crucial.
They say that the government must commit to this white paper which should consider action in four key areas to really shift the dial and reduce health inequalities once and for all.
First, leaders want to see health equity in all policies. Up to 80 per cent of what affects health—both physical and mental—is from outside of the health system, so the impact of a white paper that fails to outline a cross-government approach that looks beyond the remit of the Department of Health and Social Care (DHSC), will be drastically constrained.
The need to adopt a cross-Whitehall approach to reduce health inequalities is widely accepted. The NHS Confederation, as a member of the Inequalities in Health Alliance, a coalition of over 150 healthcare organisations, is calling for a cross-government strategy to reduce inequalities. They have written to the new Secretary of State urging her to keep the commitment to publish it before the end of this year. A health equity in all policies approach recommends action beyond the health sector, taking into account all the drivers of ill health and promoting actions that contribute to good health and wellbeing.
Secondly, leaders want prevention to be incentivised so that local systems can allocate resources according to health need and deprivation. This will require the government to make use of the structural and regulatory levers at its disposal, such as taxes and levies, to create a society where the healthy choice is the easy choice for everyone.
Last year’s Government Spending Review which failed to commit to a real-terms increase in the public health grant and soaring inflation rates which currently stand at 9 per cent, mean the Spending Review’s commitments represent a significant real-terms cut in funding. The white paper must reinstate real-terms funding increases at the level seen before 2015.
Thirdly inclusive innovation, integration, and access will be key to driving down national and local inequalities in health. The covid-19 pandemic showed that innovation in health and care services could be delivered including remote consultation. However, while very positive, there is a real risk that without concerted action to ensure these new approaches reach the country’s most deprived areas and communities, they will exacerbate inequalities.
The white paper is needed and must set out funding proposals to close the digital gap, and a strategy for the provision of health services on the high street. A plan is also needed for a population health management approach to general practice data to enable primary prevention to begin in primary care.
Equitable innovation will mean that communities are involved and engaged in defining what it looks like and that results are monitored and evaluated over the long term. Deep partnership working with the voluntary, community, and social enterprise sector will also provide valuable links into those communities.
Finally, there needs to be real concerted action on the cost-of-living crisis for communities.
A record number of working families now find themselves living in poverty. Government support must be targeted towards those who need it most in our communities. For health and care staff, this means a fully funded, generous pay rise for healthcare staff on the lowest pay, and a national care workers’ minimum wage of £10.50. The white paper must also encourage a flexible approach to the Apprenticeship Levy, using widening participation principles to enable more people from disadvantaged or excluded communities to get into work.
With concerted action it is possible to make real inroads in tackling the increasingly disparate health outcomes experienced across the country to create the conditions for a healthier population, with no-one left behind.
Moving from silo to system in our approach to population health outcome improvement will not just allow local health and care leaders to mind the health inequity gap but will engage and empower them to mend and reduce it.
Competing interests: none declared.
Provenance and peer review: not commissioned, not peer reviewed.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Income, Poverty, and Health Inequality
- 1 Chief population health officer of New York City Health + Hospitals, and clinical associate professor of population health and medicine at the New York University School of Medicine
The health of people with low incomes historically has been a driver of public health advances in the United States. For example, in New York City, cholera deaths during outbreaks in 1832 and 1854 concentrated among the poor helped push forward the Metropolitan Health Law, which allowed for regulation of sanitary conditions in the city. The law was an exemplar for other municipalities across the United States, saving countless lives during subsequent cholera epidemics as well as from typhus, dysentery, and smallpox.
Health inequality persists today, though our public health response—our modern Metropolitan Health Laws—must address more insidious causes and conditions of illness. There is a robust literature linking income inequality to health disparities —and thus widening income inequality is cause for concern. US Census data show a steady increase in summary measures of income inequality over the past 50 years. The association between income and life expectancy, already well established, was detailed in a landmark 2016 JAMA study by Raj Chetty, PhD, of Stanford University, and colleagues. This study found a gap in life expectancy of about 15 years for men and 10 years for women when comparing the most affluent 1% of individuals with the poorest 1%. To put this into perspective, the 10-year life expectancy difference for women is equal to the decrement in longevity from a lifetime of smoking.
Probing the Income-Health Relationship
In an editorial that accompanied the article by Chetty et al, Angus Deaton, PhD, of Princeton University, commented on the study’s geographical findings: “It is as if the top income percentiles belong to one world of elite, wealthy US adults, whereas the bottom income percentiles each belong to separate worlds of poverty, each unhappy and unhealthy in its own way.” Prior research had tried to identify these separate worlds, describing “ Eight Americas ” defined by sociodemographic characteristics, such as low-income white people in Appalachia and the Mississippi Valley, Western Native Americans, and Southern low-income rural black people. To improve health, interventions may need to account for starkly different lived experiences across different geographic contexts.
Educational attainment, sex, and race interact with and complicate the income-health relationship. Two additional dimensions add complexity: thinking beyond income to wealth and thinking beyond mortality to morbidity. Wealth refers to the total value of assets (and debts) possessed by an individual, not just the flow of money defined as income. Wealth is even more unequally divided than income : while the top 10% of the income distribution received a little more than half of all income, the top 10% of the wealth distribution held more than three-quarters of all wealth. This matters because it is one way that inequities persist over time —through, for instance, legacy effects of Jim Crow laws or discriminatory housing policy that affect family wealth and health over generations .
Studies on inequality and mortality may garner the most attention, but disparities in morbidity and quality of life are also evident. Low-income adults are more than 3 times as likely to have limitations with routine activities (like eating, bathing, and dressing) due to chronic illness, compared with more affluent individuals. Children living in poverty are more likely to have risk factors such as obesity and elevated blood lead levels, affecting their future health prospects.
Inequality or Inequity?
Is it the role of physicians and other health professionals to address poverty? Is it a “modifiable” risk factor, or should we focus on more proximate causes of illness, such as health behaviors? Our answers to these questions determine whether wealth gradients lead only to health inequality—or whether they contribute to health inequity , which is inequality that is avoidable and unfair.
Two arguments favor paying attention to income and wealth distributions as part of advancing health equity. First, health care spending—the realm of medical professionals—can worsen income inequality, at both individual and systemic levels. Individually, poor people have to spend a much greater proportion of their income on health care than richer people do. In 2014, medical outlays lowered the median income for the poorest decile of US individuals by 47.6% vs 2.7% for the wealthiest decile. Systemically, medical spending can crowd out other government spending on social services , drawing resources away from education and environmental improvement, for example. Taken together, this supports the case that “first do no harm” must extend to the financial impact of delivering health care. Clinicians who care about the social determinants of health must also pay heed to the cost (and opportunity cost) of health care.
Second, we are in a period when declines in key public health indicators may be wrought by policies that ostensibly have little to do with health—such as tax policy. The Centers for Disease Control and Prevention reported that average life expectancy decreased for the second year in a row in 2016. But mean mortality changes may obscure the full picture , which is more about increasing mortality being concentrated in lower-income groups. Meanwhile, the recent Tax Cuts and Jobs Act is likely to exacerbate income inequality. This is particularly true if the tax cuts trigger cuts in government spending , as Republican leaders have signaled. Medicaid and the Supplemental Nutrition Assistance Program (SNAP, also known as food stamps) are 2 programs for low-income individuals that are likely to be targeted for cuts. Even if Medicare and Social Security are spared, life expectancy differences by income means that more affluent US adults can expect to claim those benefits over a longer lifespan.
What would be today’s analog to the Metropolitan Health Law of 1866? Addressing the root causes of health inequity requires interrupting the vicious cycle of poverty leading to illness leading to poverty—what Jacob Bor, ScD, and Sandro Galea, MD, of Boston University School of Health, have termed a “21st century health-poverty trap.” Although there are many root causes to address, perhaps the place to begin is the health of children. For instance, economic policy like the Earned Income Tax Credit has been associated with decreases in low birth weight.
Congress’ recent reauthorization of the Children’s Health Insurance Program offers a glimmer of hope for such bipartisan paths toward health equity nationally. Focusing on resources to support children—such as nurse home visits to pregnant women, prekindergarten programs, and adolescent mental health care— can directly improve health while influencing intergenerational economic mobility. The city of Philadelphia offers a concrete example of how to do this: a tax on sugary drinks was used to fund prekindergarten, social services in neighborhood schools, and parks and libraries. In this way, health might lead to economic opportunity, leading to better health.
Corresponding Author: Dave A. Chokshi, MD, MSc ( [email protected] ).
Published Online: February 21, 2018, at https://newsatjama.jama.com/category/the-jama-forum/ .
Disclaimer: Each entry in The JAMA Forum expresses the opinions of the author but does not necessarily reflect the views or opinions of JAMA, the editorial staff, or the American Medical Association.
Additional Information: Information about The JAMA Forum, including disclosures of potential conflicts of interest, is available at https://newsatjama.jama.com/about/ .
Note: Source references are available through embedded hyperlinks in the article text online.
See More About
Chokshi DA. Income, Poverty, and Health Inequality. JAMA. 2018;319(13):1312–1313. doi:10.1001/jama.2018.2521
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Open access
- Published: 25 April 2023
Social inequality, social networks, and health: a scoping review of research on health inequalities from a social network perspective
- Sylvia Keim-Klärner 1 ,
- Philip Adebahr 2 ,
- Stefan Brandt 3 ,
- Markus Gamper 4 ,
- Andreas Klärner 1 ,
- André Knabe 5 ,
- Annett Kupfer 6 ,
- Britta Müller 7 ,
- Olaf Reis 8 ,
- Nico Vonneilich 9 ,
- Maxi A. Ganser 10 ,
- Charlotte de Bruyn 11 &
- Holger von der Lippe 10
International Journal for Equity in Health volume 22 , Article number: 74 ( 2023 ) Cite this article
5872 Accesses
4 Citations
4 Altmetric
Metrics details
This review summarises the present state of research on health inequalities using a social network perspective, and it explores the available studies examining the interrelations of social inequality, social networks, and health.
Using the strategy of a scoping review, as outlined by Arksey and O’Malley (Int J Sci Res Methodol 8:19–32, 2005), our team performed two searches across eight scientific, bibliographic databases including papers published until October 2021. Studies meeting pre-defined eligibility criteria were selected. The data were charted in a table, and then collated, summarised, and reported in this paper.
Our search provided a total of 15,237 initial hits. After deduplication ( n = 6,168 studies) and the removal of hits that did not meet our baseline criteria ( n = 8,767 studies), the remaining 302 full text articles were examined. This resulted in 25 articles being included in the present review, many of which focused on moderating or mediating network effects. Such effects were found in the majority of these studies, but not in all. Social networks were found to buffer the harsher effects of poverty on health, while specific network characteristics were shown to intensify or attenuate the health effects of social inequalities.
Conclusions
Our review showed that the variables used for measuring health and social networks differed considerably across the selected studies. Thus, our attempt to establish a consensus of opinion across the included studies was not successful. Nevertheless, the usefulness of social network analysis in researching health inequalities and the employment of health-promoting interventions focusing on social relations was generally acknowledged in the studies. We close by suggesting ways to advance the research methodology, and argue for a greater orientation on theoretical models. We also call for the increased use of structural measures; the inclusion of measures on negative ties and interactions; and the use of more complex study designs, such as mixed-methods and longitudinal studies.
Introduction
This scoping review departs from two meta-analytically substantiated insights into the sociological and psychological determinants of people’s health and health behaviour. First, there is broad evidence that social inequality engenders health inequality : the fewer economic and educational resources individuals possess, the less healthy they typically are, and the fewer – or less effective – health behaviours they exhibit [ 34 , 50 ].
Second, the literature also indicates that networks of personal relationships are important for individuals’ health and health behaviour [ 3 , 44 ]. Analyses of social networks take the structural and compositional features of people’s networks into account. These networks impact people’s health and health behaviour, with the effects ranging from helpful to harmful. For instance, networks that provide individuals with a high degree of social integration typically foster their well-being and promote social learning from their network members [ 44 ]. While these network relationships might lead people to adopt healthy behaviours, they might also push or entice people to engage in unhealthy risk behaviours. Thus, recent studies have examined all three aspects and their interrelationships,that is, they have addressed both social inequality and social networks in the context of research on health differences and inequalities.
In recent years, a large and growing number of empirical studies have examined the interrelationships between social networks and health. Although these findings are promising, research gaps have been pointed out [ 35 , 38 , 41 ]. What has so far been missing in this strand of research is a systematic exploration of how the social network perspective contributes to our understanding of the correlation between social and health inequalities.
From a theoretical point of view, the social network perspective has been identified as having the potential to improve our understanding of health inequalities [ 23 ]. This perspective may be particularly valuable when it focuses on the structures and the mechanisms that influence health outcomes, while also analysing how individual differences are multiplied by social networks, and how social inequalities are reproduced.
Therefore, this paper is guided by two leading questions:
To what extent have existing studies examined social inequality, social networks, and health inequality using a single empirical approach?
What have the findings of these studies revealed about the effects of the structural and the compositional characteristics of social networks on the association between social inequalities and health?
The topic: social networks, health, and social inequalities
Today, the term “social network” is widely used, often in reference to online networks. However, our focus is on the research perspective of social network analysis that defines social networks broadly as “webs of social relationships that surround an individual and the characteristics of those ties” ([ 3 ], p. 145). Such relationships and their interconnections are not volatile,instead, they are arranged in “lasting structures” that are constantly produced and reproduced by interactions ([ 6 ], p. 6). It is this “overall configuration or pattern of relationships” ([ 44 ], p. 6) that is of interest in network research. This configuration may, for example, be captured by:
homogeneity and homophily measures of one’s network members (indices of, respectively, the similarity of one’s network partners and their resemblance to oneself);
measures of the density or redundancy of one’s network (indices that show to what extent a network is or is not loosely knit); or
the presence and the number of bonding ties (the core network of close contacts) or bridging ties (which provide access to resources and information not available within the core network).
While these measures describe specific structural features, network indices form composite measures of different types of relations. An index that is often applied in this context is the Berkman-Syme Social Network Index (SNI), which focuses on the isolation/integration of a person, and collects information on the individual’s marital status, number and frequency of contacts with children, close relatives and close friends, church group membership, and membership in other community organisations. By means of such indices, subjects can be categorised into different network types, which are often characterised as having high to low levels of social integration [ 4 ].
An assumption that underlies many network approaches is that social networks “have emergent properties not explained by the constituent parts and not present in the parts” ([ 41 ], p. 407). Thus, network research combines an interest in the specific contacts individuals have in different areas of life (e.g., relatives, friends, colleagues,plus their characteristics) with a focus on their interactions and the functional aspects of these relationships (e.g., social support). Moreover, network research is interested in the larger structure that emerges based on these single ties. Drawing on this perspective, network research goes beyond other measures and concepts of social contacts and interpersonal influences by collecting information not only on the characteristics of the individuals in the network, but also on their relationships and their interconnections.
Social capital research from Bourdieu [ 8 ] to Coleman [ 13 ] or Putnam [ 36 ] has often referred to social networks in defining social capital. However, social capital studies have used structural network measures and network theory to varying degrees, from “building a network theory of social capital” [ 27 ], to focusing exclusively on the aggregate level, by, for example, measuring involvement in organisations and associations (yes/no) and general norms of trust [ 36 ]. These aggregate measures were often based on network theoretical thinking, with the aim of measuring network variables efficiently. For example, involvement in organisations can be used as an indicator of bridging ties without the need to collect complex network data.
Given the inconsistent and often metaphorical use of the term “social networks”, we have provided a definition of social networks that guides us in this review in Table 1 . It specifies that social networks are characterised by relationship characteristics (focusing on different types of relations), by information on the function of relationships (e.g., support), and by structural information on the patterns the relationships form (e.g., density).
In health research, network studies examine the direct impacts of networks on people’s behaviour, as well as the diffusion of ideas, diseases, and behaviours within these structures [ 3 , 44 ].
Unlike in health research, social network studies are not very common in inequality research [ 16 ], even though their concepts have much to offer in investigations of inequality [ 28 ]. Network characteristics such as homophily (“birds of a feather flock together”) or transitivity (“my friend’s friend is also my friend”) can lead to segregated networks of individuals who have either high or low resources, and can therefore not just reproduce social affiliations, but also foster social inequality and inhibit social mobility. People’s social status can affect their opportunities for engaging in beneficial social contacts. For example, an individual with higher social status has access to places (e.g., clubs, business meetings, societal events) where other people in higher social positions meet, and the person can use this access to social resources to advance his/her own career. In contrast, the homogenous network of an individual with lower social status cannot provide him/her with access to such resources [ 7 ]. These dynamics can be directly connected to an individual’s health and health behaviour, as people with higher social status are known to adopt healthier behaviours, and to form relationships with similar individuals, which may also have a positive impact on their health. This pattern can lead to the widening of health disparities [ 33 ]. However, the interrelations of social networks and social inequality are complex. Social networks can also help to reduce social inequality, by, for example, buffering individuals from the detrimental effects of financial deprivation [ 18 ]. The mechanisms involved in how social networks impact individual health or buffer or foster health inequalities are complex and manifold [ 24 ]. It is therefore far beyond the scope of this paper to go into all these possible mechanisms in more detail. In what follows, we focus on moderator and mediator effects of social networks on health inequalities.
Figure 1 illustrates the most commonly identified types of interconnections between social networks and social and health inequalities. Part A of the figure displays a so-called moderator model. In this model, social networks do not have direct correlations with social or with health inequalities, but they can influence the correlations between these inequalities, by, for instance, having a buffer effect, as was mentioned above. Part B of the figure shows a so-called mediation model. Here, the baseline correlation between social and health inequalities is – fully or partially – altered (“mediated”) by the characteristics of a person’s social networks. In this model, the empirical question of whether the baseline correlation is attenuated (“statistical mediation”) or increased (“statistical suppression”) when social networks are included as a mediating variable remains open.
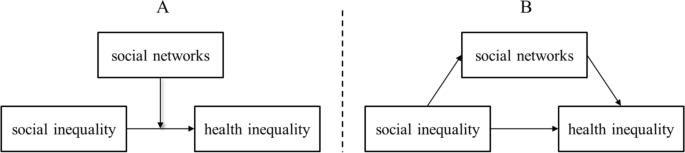
Schematic representation of moderator ( A ) and mediator ( B ) effects of social networks on health inequality. Source: own display
In the present scoping review, we examine to what extent existing studies have analysed the interconnections of social inequality, social networks, and health inequality using a single empirical approach. We also intend to summarise what the findings of these existing studies have revealed about the effects of the structural and the compositional characteristics of social networks on the association between social inequalities and health.
Methods: reviewing studies using a social network perspective on health inequalities
The literature reviewing process was conducted by the members of a research network on social networks and health inequalities “Soziale Netzwerke und gesundheitliche Ungleichheiten (SoNegU)” funded by the German Research Foundation. The 25 members of this group discussed, scrutinised, and critically assessed the methodological approach and the proceedings of the review on several occasions, a total of 18 members were involved in the article screening. Although we did not strictly follow the PRESS strategy [ 30 ], we employed a third party review of our search strategy by two renowned experts in the field. Given the broad nature of our research questions and the heterogeneity of the studies in the field, we used the method of a scoping review. This method is especially applicable in contexts in which concepts are blurry or heterogeneously understood (as is the case for social networks, social support, social capital), and in which there are a variety of definitions, operationalisation approaches, and research designs that are difficult to compare systematically [ 1 ].
This scoping review strategy follows the method created and outlined by Arksey and O’Malley [ 1 ]. Their methodological framework describes five steps that must be taken to adequately perform a scoping review: 1. Identifying the research question; 2. Identifying relevant studies; 3. Selecting studies; 4. Charting the data; and 5. Collating, summarising, and reporting the results.
Identifying relevant studies: data sources and search terms
The initial literature search was limited to peer-reviewed journal articles in English or German language, using the following international and German medical and social science data bases: Pubmed; PsycINFO and MEDLINE via Ovid; Solis (until 2017), SA (Sociological Abstracts, from 2017), SSA (Social Services Abstracts), ASSIA (Applied Social Sciences Index and Abstracts), and Scopus. The restriction to peer-reviewed articles was made for qualitative and time-efficiency reasons. Because the term "social networks" was often used metaphorically, we had to screen a large number of articles. A restriction to peer-reviewed articles ensured both a high-quality standard and a manageable number of hits. The search was conducted until October 2021. Articles were deemed eligible for inclusion only if they contained at least one search term from each of the following three topics: health, social inequality, and social network analysis. Table 2 displays the search terms that were applied to titles , abstracts, keyword, or MeSH terms of empirical studies . Additional information on how we translated these search terms into MeSH terms is provided in Appendix 1 .
Selecting studies: article screening and eligibility criteria
Eligibility criteria were consensually determined by the research group. Various preparatory steps (including a pilot trial) were taken to homogenise the evaluation of the literature in the research group (a two-stage pretest, discussion sessions for dissent, etc.). Through this process, a final eligibility list was generated.
Due to the large number of resulting findings, we needed to limit the scope of research to specific contexts. Given our interest in population health, studies focusing on health service use, on specific health issues (e.g., AIDS), or on specific groups (such as homeless individuals, or men who have sex with men) were excluded, as these works may require a separate review. A clear regional focus on OECD countries was also included in the criteria. Table 3 displays all of the study exclusion criteria.
While we began the initial selection process by reviewing titles and abstracts, we then proceeded to review full texts (see Fig. 2 ). We recorded the selected texts, using a spreadsheet, indicating included or excluded texts as well as the reasons for exclusion. After reviewing full texts, it became obvious that some articles used the term “social network” in a rather metaphorical way, and often as a synonym for one-item measurements of social relations or support. We decided to exclude the studies that did not report on more advanced relational, functional, or structural indicators (see the aforementioned social network perspective). Additionally, the empirical connections the studies made between social inequality and social networks were evaluated. Papers that did not relate social inequalities to social networks, but instead treated them as independent controls, were excluded. Figure 2 displays the full sequence of the selection process.
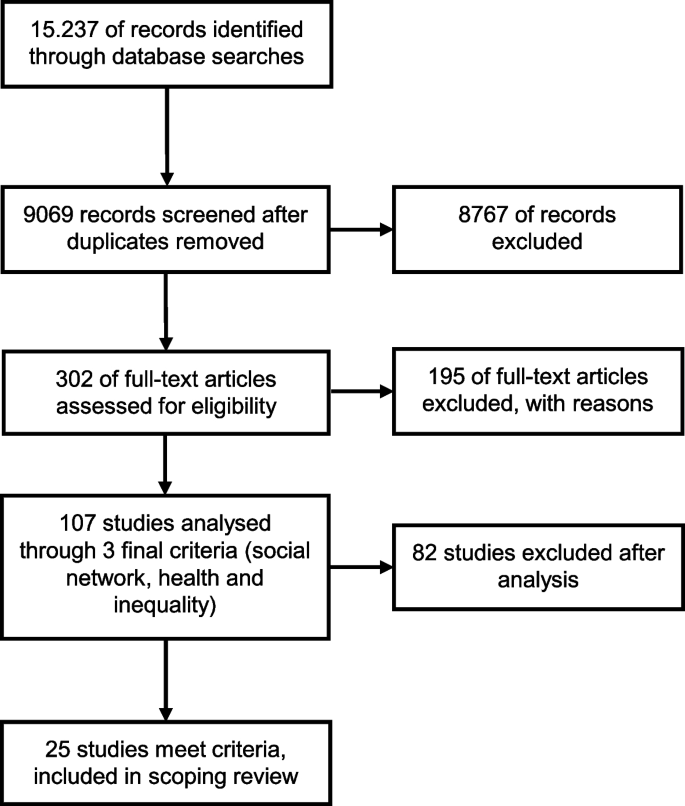
Flowchart of paper selection process (adapted from [ 1 ]). Source: own display
Data charting and final extraction
A resulting and refined 17-column spreadsheet indicated the relevant variables for extraction. This spreadsheet was pilot-tested with 20 papers, discussed in the working group and then provided to all involved in data charting along with examples and an explanatory text. The selected studies were evaluated with regard to characteristics such as research questions, study designs, methods and variables used, and central findings. Appendix 2 illustrates this procedure using the final study selection of this review.
Results: characteristics and main findings of the eligible studies
General characteristics of the final body of studies.
The resulting 25 studies were conducted between 1999 and 2021. Of those, more than half were performed after 2010. Thus, a steady increase in the publication of relevant articles can be observed over the years, with only four of the studies being published before 2005. Of the selected studies, 15 were conducted in Europe, five were conducted in the US, two were conducted in Canada, two were conducted in Australia, and one was conducted in New Zealand.
Given our selection criteria, all 25 studies stem from academic journals, typically from health sector journals such as “Social Science and Medicine” (e.g., [ 9 *, 45 *]) and “Health & Place” (e.g., [ 2 *, 15 *, 46 *]). None of the selected articles had been published in a journal on social network research. Although network journals publish various articles on health issues, these articles did not deal with social inequalities.
Methodological characteristics of the final body of studies
Study design and methodology.
Of the 25 included studies, 24 used quantitative data and performed one or more types of regression analyses. The studies were predominantly cross-sectional, and only seven papers used longitudinal data sets. One study used a mixed-methods design [ 2 *] that began by collecting quantitative data through a postal questionnaire, followed by face-to-face interviews with participants from the questionnaire part. Cattell [ 9 *] was the only purely qualitative study included in this review. Adopting a Grounded Theory approach, this study focused on in-depth face-to-face interviews in two impoverished London neighbourhoods, and developed a typology of social networks in relation to social and health inequalities.
Types of health measurements
The numbers and the types of variables collected in order to quantitatively depict health differentials varied between the studies (cf. also Appendix 2 ). A measure for self-rated, self-reported, subjective, or perceived health was most commonly used, appearing in 11 studies. Nine studies combined three or more health measures; e.g., on physical functioning, mental health, well-being, or vitality. Other studies focused on single measures of general interest, such as BMI (two studies) or resting heart rate (one study). Measures of health behaviour, such as smoking, alcohol consumption, or physical activity, were used as dependent variables in five studies.
Types of social inequality measurements
The included studies showed less variation in their approaches to measuring vertical social inequality. Most common were measures of education and income. Among the other measures used were wealth, perceived income adequacy, employment, occupation, social class, and economic living standard.
Types of social network measurements
The studies included in this review utilised a wide array of variables measuring social networks, including relational, functional, and structural measures (see Appendix 2 ). The relationship characteristics they collected were diverse, and most commonly referred to partnerships, family and friends, and contact frequency. In contrast, one functional characteristic, social support, was used in 15 of the studies. However, these studies varied considerably in the types of support they measured (e.g., emotional, instrumental), and in whether they assumed that the support was needed, perceived, received, or provided. Structural network measures were used in 15 studies, with the variable of network size being the most frequently used (11 studies). In contrast, the use of other structural network measures was rare, and those that were included were diverse. Network density was measured in three studies, and the homogeneity of networks was also measured in three studies. One study focused on homogeneity in terms of ethnicity and gender [ 20 *], while another study focused on homogeneity of belonging to a small number of membership groups [ 9 *], and a third study measured homogeneity of income, age, race, education, being employed, living in the local area, and being family members [ 26 *]. Verhaeghe and colleagues [ 46 *] studied the occupational composition of social networks. Homophily was measured in one study using the I-E Index, which indicated the similarity of alters with ego regarding smoking, age, and education [ 31 *]. The structural constructs of bridging or bonding social relations were applied in three studies. In addition to network measures, 13 studies also used aggregate social capital measures such as trust, neighbourhood cohesion, or community activities.
Most studies covered two of the three named network characteristics: i.e., either relational and functional measures or relational and structural measures. Nine studies were more complex and used variables on multiple types of relationships, network functions, and structural information. For example, Nemeth and colleagues [ 31 *] collected information on the persons the respondent spends the most time with and the persons whom the respondent asks for advice, including information on the characteristics of these persons (e.g., age, smoking status). They also used measures of perceived support (by partner, family, and friends), network size, and density. Four studies reduced complexity by using the Social Network Index (SNI) by Berkman and Syme [ 4 ] and the Social Integration Index (SII), a modified version of the SNI [ 5 ]. These indices captured different types of relations, and they were enriched with additional support or loneliness measures [ 25 *, 29 *, 47 *, 48 *, 49 *].
Main findings of included studies on the interconnections between social inequality, social networks, and health inequality
The interconnections between the crucial three constructs of interest were predominantly analysed using statistical moderator analyses (11 studies) and mediator analyses (nine studies), but multivariate regressions were also applied (six studies). Footnote 1
Social networks as moderators of health inequalities (moderator analysis “type 1”)
Regarding the moderating effect of social networks on the correlation of social inequalities and health inequalities (here termed “type 1”; see Fig. 1 A in the introductory section), the results of four out of five studies showed the relevance of different kinds of social network measures. Richards [ 37 *] and Gele and Harsløff [ 20 *] described moderator effects. Both focused on strong and weak network ties: on close ties, activities in organisations, and having a doctor as a friend [ 20 *], and on friends, support, activities in organisations, and their frequency [ 37 *]. Gele and Harsløff [ 20 *] showed that in their sample, social networks were significant brokers of social resources. For example, they found that being linked to higher educated network partners was beneficial for the respondents’ health, particularly for those with low education. Richards [ 37 *] observed that a high level of social integration acted as a buffer for the negative correlation of well-being and financial strains. Specifically, they found that financial problems impacted a person’s happiness less severely when the person had strong and supportive informal ties as well as extensive weak ties. In the studies by Baum et al. [ 2 *] and Craveiro [ 15 *], neither the relational, structural, nor functional network characteristics under study (e.g., contact frequency, support, network size) were shown to be relevant,but aggregate measures, such as perceived neighbourhood cohesion and safety, social participation, and general network satisfaction, were found to have a moderating effect on health inequalities. However, Craveiro [ 15 *] observed these effects in central and southern Europe only. By contrast, Chappell and Funk [ 10 *] found no similar moderator effects for network size, group membership, community activities, service use, or trust. Emotional support was only used as a control variable in this study.
SES as moderators of network impact on health (moderator analysis “type 2”)
In contrast to the model displayed in Fig. 1 A, and somewhat surprisingly, six studies of the review sample also examined whether social inequality moderated the relationship between social networks and health (here termed “type 2” moderation). Four of these six studies found such moderating effects.
Schöllgen and colleagues [ 40 *] reported that SES had a moderator effect on the relationship between social resources and health. Specifically, they found that network support was more beneficial for the subjective health of individuals with lower than with higher income levels. In a similar vein, Vonneilich et al. [ 47 *] reported that the health risks associated with the lack of emotional and instrumental support were higher for subjects with lower than with higher SES. Focusing and bonding social capital, Kim et al. [ 22 *] showed that the association between social capital and health was moderated by income, with higher bonding social capital being linked with better health for low-income households only. However, the measure of network density, in combination with the health measure BMI, was found to be associated with higher health risks for persons with lower levels of education [ 12 *]. The authors explained this finding by noting that lower educated individuals tend to have less resourceful/supportive and more homophilic social networks. Unfortunately, measures of network homophily or support were not included in this study.
While Unger and colleagues [ 43 *] and Weyers and colleagues [ 49 *] did not find any “type 2” moderator effects in their data, they do no reject the relevance of social networks. The former authors assumed that it could be a mediator effect, and the latter authors stated that having a lower socio-economic position strengthens the influence of social networks on adverse health behaviour.
Social networks as mediators of health inequalities
Regarding the mediating effect of social networks on the correlation of social inequalities with health inequalities (see Fig. 1 B), seven out of nine studies reported such findings. This mediating effect was found in cross-sectional studies as well as in longitudinal studies. The study by Li [ 26 *] found that people of a higher social class were more likely to mobilise their social resources and networks for their own well-being than people of a lower social class. The authors noted, however, that these partial mediation effects of network size and diversity on health and well-being were numerically small compared to the effects of social class. In addition, Verhaeghe et al. [ 46 *] found a prevalent class effect as well as a mediator effect of social networks, with lower levels of social support contributing to a reduction in self-rated health. In a longitudinal study, Klein and colleagues [ 25 *] found that social networks mediated up to 35% of the social inequality effect on self-rated health. They showed that low SES was associated with lower levels of social integration and poorer social support, which in turn led to adverse effects on health. In their longitudinal study, Vonneilich et al. and colleagues [ 48 *] also found a considerable mediating effect, stating that “social relationships substantially contribute to the explanation of SES differences in subjective health” ([ 48 *]: 1/11).
In her qualitative study, Cattell [ 9 *] described how being financially restricted or living in a poor area impeded social participation, which in turn led to a higher risk of social exclusion (smaller networks, less support) and poor health. She also showed that structural social network features (such as density and reciprocity) and functional characteristics (such as support) reduced the harsher effects of poverty on health.
While the mediation studies discussed so far dealt with some indicator of perceived or self-rated health, [ 29 *] demonstrated that social isolation mediated the relationship between SES and resting heart rate by increasing the latter when subjects felt socially isolated and had smaller networks. Looking at different welfare regimes, Craveiro [ 14 *] found that social networks mediated the effects of SES on health, but also that the mediating variables varied across different welfare regimes. However, social support and network satisfaction were found to be consistent mediators in all regions under study.
Two studies did not find any mediating effects. Chappell and Funk [ 10 *] analysed the effects of network size, emotional support, group membership, and community activities on the perceived mental and physical health of individuals with different levels of education and income, while Sabbah and colleagues [ 39 *] researched the mediating effects of support and network size on dental health. However, while the latter authors did not reject the idea that social networks could play a role in inequality in dental health in general, they critically evaluated their applied support measures. Among other measures, they used the subjects’ “need for emotional support”, instead of the more commonly used receipt of support.
Social networks in multivariate models of health inequalities
Another strand of studies refrained from formulating explicit moderator or mediator models. Instead, these six studies investigated social and health inequalities together with social networks in multivariate models without statistical interaction terms. All of these studies showed the relevance of social networks for health inequalities. Stephens and colleagues [ 42 *] found that having a lower income was associated with having less social support, having a more restricted social network, and being less socially integrated, which in turn had detrimental health effects. Moreover, they found these social factors led to a higher risk of loneliness, which was strongly related to several adverse health effects. Similarly, Chavez et al. [ 11 *] demonstrated that people who reported having trust and feelings of reciprocity in their social context had better self-reported health. Although Veenstra [ 45 *] found that income and education were the strongest predictors for health, this author also showed that being socially integrated at work contributed to better self-reported health.
Two of these studies focused on health behaviours. Nemeth and colleagues [ 31 *] showed that when strong neighbourhood cohesion was combined with the belief in the general acceptability of smoking in a deprived neighbourhood, and when social networks contained many smokers, it was more difficult for smokers to quit, as doing so would jeopardise their social acceptance. Kamphuis and colleagues [ 21 *] showed that social networks played an important role in differences in sports participation, as people with lower SES, smaller networks, and less network cohesion had lower levels of sports participation.
The longitudinal study by Novak and colleagues [ 32 *] introduced network characteristics from past study waves as “parental control in school” and “not being popular in school”. They showed that people who had low education as well as these social network characteristics during their school years were more likely to be obese in adulthood.
Discussion and conclusion
Health inequalities have been investigated and discussed in research for many decades, and form an established research topic. Social network analysis, by contrast, is a novel research approach, but one that is gaining in popularity. Thus, the present scoping review was guided by two main questions: to what extent have existing studies examined social inequality, social networks, and health inequality using a joint empirical approach; and what have the findings of these studies revealed about the effects of the structural and the compositional characteristics of social networks on the association between social and health inequalities?
Despite the large number of initial hits in the literature research (9,064), after we reviewed the papers’ contents in more detail, we found a comparatively small number of publications (25) that fitted the aim of this review. A typical phenomenon that occurred during the selection process was that at first glance, many articles seemed suitable based on the term “social networks” in their abstract. At second glance, however, we found that the authors often used this term rather metaphorically for some unspecified kind of social relations or support. In these articles, which we excluded from this review, the authors neither made connections to the theoretical concepts or to methods of social network analysis; nor explored different types of relationships, analysed network functions, or measured structural network characteristics. Thus, despite the recent prominence of the term “social network”, there are only a few studies on health inequalities that can clearly be identified as social network analyses.
Among the studies considered for this review, the majority were published less than 10 years ago, and this set of studies exemplifies the growing popularity of network studies in research on health inequalities. From a theoretical and a statistical point of view, analyses of mediator, moderator, and multivariate models were the most common. Table 4 summarises the central results of this scoping review, which we will discuss in the following sections.
The empirical basis of statements 1 and 2 in Table 4 is provided by Table 5 . When summarising the studies that applied statistical mediation or “type 1 moderation” models, we observed that 11 out of 14 empirical studies successfully located social networks conceptually between social and health inequalities. From our perspective, this approach also appears to be particularly valid, because networks temporally arise more frequently from a person's social class than vice versa. The models we termed “moderation type 2” models appeared to be less plausible to us for that reason. The 11 studies mentioned above showed that social networks are a relevant explanatory tool for improving our understanding of the complex relationships between socially unequal industrialised societies and health outcomes.
Another finding that we deem particularly interesting – including for future research – is that social networks appeared to be particularly relevant for attenuating the detrimental effects on health of deprived social contexts or statuses (statements 3 and 4 in Table 4 ). When the structure, function, or composition of social networks provide health-related resources to people, the health of deprived individuals typically benefits. However, we also found evidence of the often overlooked “dark side” of networks: studies that focused their research on behavioural variables to describe health (e.g., BMI, smoking, and alcohol consumption) often found a negative correlation between these behaviours and social inequality due to the power and influence of social networks . For instance, the study by Child et al. [ 12 *] demonstrated that social networks could have reinforcing effects on the behaviour of people with both low and high incomes, resulting in higher predicted BMI for people in low-income communities and lower BMI for people in high-income communities. These results were echoed by Nemeth et al. [ 31 *] in their study of smoking cessation and by Weyers et al. [ 49 *] in their study of social relations’ overall impact on behaviour. In other words, depending on the variables used to describe health and networks, the intervening effects of networks on health changed, but the value of social network analysis within this research framework did not.

Methodological discussion and future research directions
If the reported level of interest in the role of social networks in health research continues as was previously described, within the next few decades, more studies will be conducted using social network analysis as a mediator and moderator between health and social inequalities. This projected growth in the literature will provide a broader set of precedents and more consistency in both the variables collected and the results produced in this research field. While the 25 studies included in this scoping review provide an illuminating introduction to this topic, they should ultimately represent only the beginning of research into what we hope will become a very useful explanatory tool for studying these complex relationships in the years to come. Many of the studies in this review started out by stating that the body of knowledge on the role of social networks in health inequalities is small (e.g., [ 15 *, 25 *, 47 *]), indeed, it appears that the authors of these studies were often unaware of other research on this topic, as the studies seldom cite each other in the text or in the references. This could reflect the strength of disciplinary boundaries; the centredness of the authors on specific health topics, populations, or specific countries; or the authors’ reading habits, which led them to focus on a small number of journals in the large landscape of health-related journals. This review can help scholars overcome these boundaries by bringing together evidence from various research streams.
Looking more closely at the methodological approaches and the network measures used in the presented studies provides us with valuable insights for formulating future directions for researching the role of social networks in health inequalities.
A first critical issue is the large amount of heterogeneity that the selected studies displayed, and especially the diversity of their network measures. Even a comparatively simple network variable such as size was measured in many different ways (number of close ties, number of supportive ties, etc.), and the studies often combined very different relational, functional, structural, and even aggregate measures into one empirical approach. This heterogeneity currently impedes quantitative meta-analyses in terms of systematic reviews. In future research on social and health inequalities, all network analyses could benefit by orienting empirical measures on theoretical models, such as the notions of supportive, integrating, influencing (norming), or contagious network ties. The current literature is still far from having reached a consensus on these issues. For instance, studies grounded in the theoretical considerations of social capital did not automatically enter this review because their network-related variables were typically too broad and too aggregate. While many of the included studies found that social networks could partially explain the association between socio-economic position and health, the researchers often did not observe the expected interrelations of social networks, social inequality, and health. These authors suggested [ 10 *, 39 *], or even insisted, that better measures should be used to clarify these interrelations [ 11 *]. Apart from orienting measures on theoretical models in general, using structural network indicators may be one step in this direction, as the studies using multiple network variables indicated. The best examples of this approach were provided in the studies by Li [ 26 *], who found mediating effects of network size and diversity, by [ 12 *], who found a moderating effect of network density, and by [ 31 *], who showed the relevance of homophily for smoking behaviour. One way of dealing with the complexities of collecting and analysing network measures is the development of tools such as the Social Network Index (SNI), which was created and developed by Berkman and Syme [ 4 ], or its successor, the Social Integration Index (SII) [ 5 ]. These tools were included in four of the studies presented here. They provide important precedents that constitute essential tools for increasing the consistency of studies in this field. In the future, the use of more standardised research tools would enhance the reliability and consistency of social network analysis within this research field. The benefits of using these tools would be compounded by the establishment of a set of baseline variables collected through precedent and testing.
Second, as social network research builds on a rich tradition of quantitative studies, it is not surprising that quantitative social network analysis emerges so strongly in the articles we reviewed. However, the single qualitative study included in the present study shows the valuable contributions qualitative methods can make in identifying the pathways through which social networks affect health, and the role of social inequality in this association. An especially interesting approach for future network research on social and health inequalities could be to conduct mixed-methods studies, which have received increased attention in recent years [ 17 , 19 ]. Only one mixed-methods study entered this review, and the qualitative aspect of this study did not, unfortunately, focus on social networks.
Third, the studies we reviewed were mostly cross-sectional, and several of the authors explicitly asked for the use of more longitudinal data (e.g., [ 10 *, 12 *, 22 *]). Fourth, another limitation of these studies that became apparent is the focus on the social gradient and the decision not to include certain socially excluded groups such as the homeless. Future studies could examine whether exploring the social networks of such groups would lead to similar conclusions.
Lastly, this research, which demonstrated how networks can buffer the detrimental health effects of having lower socio-economic status, or how networks pertain to the reproduction of health inequalities, can inform health policies in general, and health interventions more specifically. Many of the authors suggested focusing on social networks and on interventions aimed at helping socially disadvantaged individuals increase their contact with others. However, other researchers insisted that if we want to reduce health inequalities, we need to start by reducing social inequalities, given the evidence that accumulating ties that have detrimental effects on health (e.g., getting acquainted with other smokers) will not reduce health inequalities. Thus, when examining the effects of social networks on health inequalities, the role of negative ties and the negative effects of social relations on health inequalities should be considered more often.
Availability of data and materials
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Numbers sum up to more than 25 or 100 percent, respectively, because one study presented more than one analytical approach.
* Studies are part of the final selection of this scoping review
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Science Research Methodology. 2005;8:19–32. https://doi.org/10.1080/1364557032000119616 .
Article Google Scholar
*Baum FE, Ziersch AM, Zhang G, Osborne K. Do perceived neighbourhood cohesion and safety contribute to neighbourhood differences in health? Health Place. 2009;15:925–34. https://doi.org/10.1016/j.healthplace.2009.02.013 .
Berkman LF, Glass T. Social integration, social networks, social support, and health. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2000. p. 137–73.
Google Scholar
Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. https://doi.org/10.1093/oxfordjournals.aje.a112674 .
Article CAS PubMed Google Scholar
Berkman LF, Melchior M, Chastang J-F, Niedhammer I, Leclerc A, Goldberg M. Social integration and mortality: A prospective study on French employees of electricity of France-Gas of France. The GAZEL Cohort Am J Epidemiol. 2004;159:167–74. https://doi.org/10.1093/aje/kwh020 .
Article PubMed Google Scholar
Bidart C, Degenne A, Grossetti M. Living in networks. The dynamics of social relations (Structural analysis in the social sciences, Bd. 49). Cambridge: Cambridge University Press; 2020.
Böhnke P, Link S. Poverty and the dynamics of social networks. An analysis of german panel data. Eur Sociol Rev. 2017;33(4):615–32. https://doi.org/10.1093/esr/jcx063 .
Bourdieu P. The forms of capital. In: Richardson JG, editor. The Handbook of Theory: Research for the Sociology of Education. New York: Greenwood Press; 1986. p. 241–58.
*Cattell V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Sc Sci Med. 2001;52:1501–16. https://doi.org/10.1016/S0277-9536(00)00259-8 .
*Chappell NL, Funk LM. Social capital: does it add to the health inequalities debate? Soc Indic Res. 2010;99:357–73. https://doi.org/10.1007/s11205-010-9597-4 .
*Chavez R, Kemp L, Harris E. The social capital: health relationship in two disadvantaged neighbourhoods. J Health Serv Res Policy. 2004;9:29–34. https://doi.org/10.1258/1355819042349871 .
*Child ST, Walsemann KM, Kaczynski AT, Fleischer NL, Mclain AC, Moore S. Personal network characteristics and body mass index: the role of education among Black Americans. J Public Health. 2018;41:130–7. https://doi.org/10.1093/pubmed/fdy020 .
Coleman JS. Social capital in the creation of human capital. Am J Sociol. 1998;94:S95-120.
*Craveiro D. Ties and inequalities in later life: welfare state regime and the role of social networks in health inequalities in later life in Europe. Eur Soc. 2016;19:268–91. https://doi.org/10.1080/14616696.2016.1258084 .
*Craveiro D. The role of personal social networks on health inequalities across European regions. Health Place. 2017;45:24–31. https://doi.org/10.1016/j.healthplace.2017.02.007 .
DiMaggio P, Garip F. Network Effects and Social Inequality. Ann Rev Sociol. 2012;38:93–118. https://doi.org/10.1146/annurev.soc.012809.102545 .
Dominguez S, Hollstein B. Mixed Methods Social Networks Research. Cambridge University Press, Cambridge. 2014. https://doi.org/10.1017/CBO9781139227193 .
Domínguez S, Watkins C. Creating networks for survival and mobility: social capital among African-American and Latin-American low-income mothers. Soc Probl. 2003;50(1):111–35. https://doi.org/10.1525/sp.2003.50.1.111 .
Gamper M, Schoenhuth M. Visual network research (VNR)–a theoretical and methodological appraisal of an evolving field. Vis Stud. 2020;35(4):374–93. https://doi.org/10.1080/1472586X.2020.1808524 .
*Gele AA, Harsløff I. Types of social capital resources and self-rated health among the Norwegian adult population. Int J Equity Health. 2010;9. https://doi.org/10.1186/1475-9276-9-8 .
*Kamphuis CBM, Van Lenthe FJ, Giske K, Huisman M, Brug J, Mackenbach JP. Socioeconomic status, environmental and individual factors, and sports participation. Med Sci Sports Ecers. 2008;40:71–81. https://doi.org/10.1249/mss.0b013e318158e467 .
*Kim Y, Schneider T, Faß E, Lochbaum M. Personal social capital and self-rated health among middle-aged and older adults: a cross-sectional study exploring the roles of leisure-time physical activity and socioeconomic status. BMC Public Health. 2021;21:48. https://doi.org/10.1186/s12889-020-10043-6 .
Klärner A, Gamper M, Keim-Klärner S, Moor I, von der Lippe H, Vonneilich N. Social Networks and Health Inequalities. Cham: Springer International Publishing; 2022. https://doi.org/10.1007/978-3-030-97722-1 .
Book Google Scholar
Klärner A, von der Lippe H. Social Network Mechanisms. In: Klärner A, Gamper M, Keim-Klärner S, Moor I, von der Lippe H, Vonneilich N, editors. Social Networks and Health Inequalities. Cham: Springer International Publishing; 2022. p. 49–56. https://doi.org/10.1007/978-3-030-97722-1_4 .
Chapter Google Scholar
*Klein J, Vonneilich N, Baumeister SE, Kohlmann T, von dem Knesebeck O. Do social relations explain health inequalities? Evidence from a longitudinal survey in a changing eastern German region. Int J Public Health. 2012;57:619–27. https://doi.org/10.1007/s00038-012-0356-y .
*Li Y. Social mobility, social network and subjective well-being in the UK. Contemp Soc Sci. 2016;11:222–37. https://doi.org/10.1080/21582041.2016.1190860 .
Lin N. Building a Network Theory of Social Capital. Connections. 1999;22(1):28–51 http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.96.3792&rep=rep1&type=pdf .
Martin JL, Murphy JP. Networks, status, and inequality. In: Light R, Moody J, editors. The Oxford handbook of social networks (Oxford handbooks. New York NY: Oxford University Press; 2020. p. 98–115.
*McCrory C, Finuacane C, OHare C, Frewn J, Nolan H, Layte R, Kearney PM, Kenny RA. Social Disadvantage and Social Isolation Are Associated With a Higher Resting Heart Rate: Evidence From The Irish Longitudinal Study on Ageing. J Gerontol B Psychol Sci Soc Sci. 2016;71:463–73. https://doi.org/10.1093/geronb/gbu163 .
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6. https://doi.org/10.1016/j.jclinepi.2016.01.021 .
*Nemeth JM, Thomson TL, Peng J, Krebs V, Doogan NJ, Ferketich AK, Post DM, Browning CR, Paskett ED, Wewers ME. A social -contextual investigation of smoking among rural women: multilevel factors associated with smoking status and considerations for cessation. Rural Remote Health. 2018;18:4338. https://doi.org/10.22605/RRH4338 .
*Novak M, Ahlgren C, Hammarström A. A life-course approach in explaining social inequity in obesity among young adult men and women. International J Obes. 2006;30:191–200. https://doi.org/10.1038/sj.ijo.0803104 .
Pampel FC, Krueger PM, Denney JT. Socioeconomic Disparities in Health Behaviors. Ann Rev Sociol. 2010;36:349–70. https://doi.org/10.1146/annurev.soc.012809.102529 .
Pathirana TI, Jackson CA. Socioeconomic status and multimorbidity: a systematic review and meta-analysis. Aust N Z J Public Health. 2018;42:186–94. https://doi.org/10.1111/1753-6405.12762 .
Perkins JM, Subramanian SV, Christakis NA. Social networks and health: a systematic review of sociocentric network studies in low- and middle-income countries. Soc Sci Med. 2015;1982(125):60–78. https://doi.org/10.1016/j.socscimed.2014.08.019 .
Putnam R. Bowling Alone: The Collapse and Revival of American Community. New York: Simon & Schuster; 2000.
*Richards L. For Whom Money Matters Less: Social Connectedness as a Resilience Resource in the UK. Soc Indic Res. 2016;125:509–35. https://doi.org/10.1007/s11205-014-0858-5 .
Roth AR. Social networks and health in later life: a state of the literature. Sociol Health Illn. 2020;42(7):1642–56. https://doi.org/10.1111/1467-9566.13155 .
*Sabbah W, Tsakos G, Chandola T, Newton T, Kawachi I, Sheiham A, Marmot MG, Watt RG. The relationship between social network, social support and periodontal disease among older Americans. J Clin Periodontol. 2011;38:547–525. https://doi.org/10.1111/j.1600-051X.2011.01713.x .
*Schöllgen I, Huxhold O, Schüz B, Tesch-Römer C. Resources for health: differential effects of optimistic self-beliefs and social support according to socioeconomic status. Health Psychol. 2011;30:326–35. https://doi.org/10.1037/a0022514 .
Smith KP, Christakis NA. Social Networks and Health. Ann Rev Sociol. 2008;34:405–29. https://doi.org/10.1146/annurev.soc.34.040507.134601 .
*Stephens C, Alpass F, Towers A, Stevenson B. The effects of types of social networks, perceived Social Support, and loneliness on the health of older people: accounting for the social context. J Aging Health. 2011;23:887–911. https://doi.org/10.1177/0898264311400189 .
*Unger JB, McAvay G, Bruce ML, Berkmann L, Seeman T. Variation in the impact of social network characteristics on physical functioning in elderly persons: MacArthur studies of successful aging. J Gerontol B Psychol Sci Soc Sci. 1999;54:245–51. https://doi.org/10.1093/geronb/54B.5.S245 .
Valente TW. Social Networks and Health: Models, Methods, and Applications. New York: Oxford University Press; 2010.
*Veenstra G. Social capital, SES and health: an individual-level analysis. Soc Sci Med. 2000;50:619–29. https://doi.org/10.1016/S0277-9536(99)00307-X .
*Verhaeghe P, Pattyn E, Bracke P, Verhaeghe M, Van De Putte B. The association between network social capital and self-rated health: Pouring old wine in new bottles? Health & Place. 2012;18:358–65. https://doi.org/10.1016/j.healthplace.2011.11.005 .
*Vonneilich N, Jöckel KH, Erbel R, Klein J, Dragano N, Weyers S, Moebus S, Siegrist J, von dem Knesebeck O. Does socioeconomic status affect the association of social relationships and health? A moderator analysis. Int J Equity Health. 2011;10:43. https://doi.org/10.1186/1475-9276-10-43 .
*Vonneilich N, Jöckel KH, Erbel R, Klein J, Dragano N, Siegrist J, von dem Knesebeck O. The mediating effect of social relationships on the association between socioeconomic status and subjective health - results from the Heinz Nixdorf Recall cohort study. BMC Public Health. 2012;12:285. https://doi.org/10.1186/1471-2458-12-285 .
*Weyers S, Dragano N, Möbus S, Beck E, Stang A, Möhlenkamp S, Jöckel KH, Erbel R, Siegrist J. Poor social relations and adverse health behavior: stronger associations in low socioeconomic groups? Int J Public Health. 2010;55:17–23. https://doi.org/10.1007/s00038-009-0070-6 .
Zell E, Strickhouser JE, Krizan Z. Subjective social status and health: A meta-analysis of community and society ladders. Health Psychol. 2018;37:979–87. https://doi.org/10.1037/hea0000667 .
Download references
Acknowledgements
The authors would like to thank all members of the DFG research network “SoNegU” for the inspiring meetings and discussions. Special thanks are extended to Lea Ellwardt, Irene Moor, Eike Quilling, Nancy Reims and Katharina Seebaß for their contributions to reviewing articles for this paper. Emily LeCouvie Nantel was very helpful in the final polishing of the paper.
Open Access funding enabled and organized by Projekt DEAL. This publication emerged from meetings of the research network on “Social Networks and Health Inequalities”, funded by the German Research Foundation (DFG), Project number 280679966. This foundation was not involved in the preparation of this research article. We acknowledge institutional and financial support for this research by the Thuenen Institute of Rural Studies and the Medical School Berlin.
Author information
Authors and affiliations.
Thünen Institute of Rural Studies, Bundesallee 64, Brunswick, Germany
Sylvia Keim-Klärner & Andreas Klärner
Institute of Sociology, University of Technology Chemnitz, Chemnitz, Germany
Philip Adebahr
Landesfrauenrat Mecklenburg-Vorpommern e.V., Rostock, Germany
Stefan Brandt
Institut für vergleichende Bildungsforschung und Sozialwissenschaften, University of Cologne, Cologne, Germany
Markus Gamper
Rostocker Institut für Sozialforschung und gesellschaftliche Praxis e.V., Rostock, Germany
André Knabe
Institute of Social Pedagogy, Social Work and Welfare Studies, Technische Universität Dresden, Dresden, Germany
Annett Kupfer
Institute of Medical Psychology and Medical Sociology, Rostock University Medical Center, Rostock, Germany
Britta Müller
Klinik für Psychiatrie, Neurologie, Psychosomatik und Psychotherapie im Kindes- und Jugendalter, Rostock University Medical Center, Rostock, Germany
Institute of Medical Sociology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
Nico Vonneilich
MSB Medical School Berlin, Berlin, Germany
Maxi A. Ganser & Holger von der Lippe
Alumna of MSB Medical School Berlin, Berlin, Germany
Charlotte de Bruyn
You can also search for this author in PubMed Google Scholar
Contributions
All authors were involved in the reviewing process, they discussed eligibility criteria, reviewed literature regarding their eligibility and summarized the contents of the eligible studies. This work forms the basis of the results section. All authors drafted and reviewed the full manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Sylvia Keim-Klärner .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Table 6 Translating search terms into mesh terms
|
|
|---|---|
| |
health, well-being | health |
life satisfaction | no MeSH term |
illness | disease attributes |
disease, disorder | disease |
health status | health status |
health behavior | health behavior |
risk behavior | risk-taking |
coping | adaptation, psychological |
mortality | mortality |
morbidity | morbidity |
life expectancy | life expectancy |
quality of life | quality of life |
| |
social status, socioeconomic status, SES, social class, income, education, occupation, poverty, low-income, deprivation | socioeconomic factors |
prestige | social class |
wealth | - no MeSH term |
financial strain | - no MeSH term |
inequalities | socioeconomic factors, healthcare disparities |
disparities | healthcare disparities, health status disparities |
| |
social network, support network, informal network | social support |
personal network, egocentered, egonet, friendship network, egocentric network, whole network, network chart, sociogram | - no MeSH term |
|
|
- Comment: For our interest in Social Network Analysis (SNA), the MeSH terms social support and family are not sufficiently specific, therefore we did not use MeSH terms for the third topic SNA and rather performed our search with the search terms indicated above within titles and abstracts
Table 7 Data charting sheet: the 25 selected studies: study design and measurements
|
|
|
|
|
|
|
| |
|---|---|---|---|---|---|---|---|---|
1 | Baum | 2009 | cross-sectional mixed methods | 3: smoking, exercise, self-reported health | 2: education, income | 1) contact frequency 2) support 4)associational membership, reciprocity and 3 more | moderator analysis (type 1) | of aggregate measures (neighbourhood cohesion, neighbourhood safety) |
2 | Cattell | 2001 | cross-sectional, qualitative | qualitative accounts on health and wellbeing | qualitative accounts on poverty | 1) tie characteristics, contact frequency/duration 2) support given/ received 3) size, subgroups, density, homo/heterogeneity | qualitative mediator analysis | (size, density, homogeneity, reciprocity, support) |
3 | Chappell | 2010 | cross-sectional, quantitative | 3: perceived and mental health, physical function | 2: education, income | 3) size 4) trust, group membership, community activities, service use | moderator (type 1), mediator analysis | no moderating effect no mediating effect |
4 | Chavez | 2004 | cross-sectional, quantitative | 1: self-reported health | 3: housing, education, employment status | 1) family/friends in neighbourhood (bonding ties) 2) support 4) trust, local participation/ membership and 8 more | multivariate analysis | trust is of relevance for health in disadvantaged neighbourhoods |
5 | Child | 2018 | cross-sectional, quantitative | 1: BMI | 2: education, income | 1) up to three close ties, their educational level and residence 3) density | moderator analysis (type 2) | of education on the association between network (density) and health |
6 | Craveiro | 2016 | cross-sectional, quantitative | 3: chronic disease, perceived health, ADL limitation | 4: education, income, wealth, perceived income adequacy | 1) close ties, daily contact 2) support 3) size 4) social participation, network satisfaction | mediator analysis | (participation, daily contact, support); mediator effects of size only in eastern countries |
7 | Craveiro | 2017 | cross-sectional, quantitative | 3: chronic disease, perceived health, ADL limitation | 4: education, income, wealth, perceived income adequacy | 1) partner, children, daily contacts, closeness 2) support 3) size 4) participation in activities, network satisfaction | moderator analysis (type 1) | in central and southern Europe for aggregate measures (mainly: social participation, network satisfaction), not in northern Europe |
8 | Gele | 2010 | cross-sectional, quantitative | 1: self-rated health | 3: occupation, income group and education | 1)strong and weak ties, contact frequency w/ family and friends, nurses/medical doctors as friends 3)size, ethnic/gender diversity, bonding/bridging ties 4)activities in organisations | moderator analysis (type 1) | (strong ties, activities in organisations, one friend is a doctor) |
9 | Kamphuis | 2008 | cross-sectional, quantitative | 3: sports frequency, duration, intensity | 2: education, income | 3) neighbourhood network (small, medium, large) 4) social cohesion, opinion of neighbourhood, disorganisation, frequency of social gathering | mediator analysis | (network size, neighbourhood attractiveness and neighbourhood safety, social cohesion) |
10 | Kim | 2021 | cross-sectional, quantitative | 2: Self-rated health, physical activities | 2: education, income | 3) bonding and bridging ties (Personal Social Capital Scale) | moderator analysis (type 2) | of income on the association of network (bridging and bonding ties) and health |
11 | Klein | 2012 | longitudinal, quantitative | 1: self-rated health | 3: income, education, profession | 1 + 4) Social Integration Index: living with a partner, number of close ties, affiliation in associations 2) support | mediator analysis | (SII and support) |
12 | Li | 2016 | longitudinal, quantitative | 3: perceived health, happiness, satisfaction | 3: degree and employment, parents’ class | 3) size, diversity (income, age, race, education, employment, place of living, family member) 4) civic engagement, neighbourhood cohesion | mediator analysis | significant but small (size, diversity, neighbourhood cohesion, civic engagement) |
13 | McCrory | 2014 | cross-sectional, quantitative | 1: resting heartrate, | 1: household income | 1 + 4) Social Network Index: marital status, number of children, contact frequency, close relatives/friends, church group/ organisational membership 4) loneliness | mediator analysis | (SNI, loneliness) |
14 | Nemeth | 2018 | cross-sectional, quantitative | 2: smoking, depression | 3: education, income, employment status | 1) partner, persons spending time with/asking for advice, their characteristics (e.g., smoking status) 2) perceived support, social influence scale, 3) size, density, E/I index (similarity of Ego and Alter in smoking, age and education) 4) participation, neighbourhood cohesion and 3 more | multivariate analysis | perception of social acceptability of smoking, homophily on smoking and neighbourhood cohesion are associated with current smoking in a disadvantaged population, cessation interventions need to acknowledge the social context |
15 | Novak | 2006 | longitudinal, quantitative | 1: BMI | 2: occupation (parents’ and own) and education | 1) marital status, number of children, social network index, contact with parents; 2) social support index, parental support in adolescence 4) participation in associations; popularity in school | multivariate analysis | educational gradient in BMI at middle age is explained by support (men), popularity (women) in adolescence and nonparticipation in associations in young adulthood (men) |
16 | Richards | 2015 | longitudinal study, quantitative | 2: long-term illness, subjective well being | 2: financial situation, employment status | 1) friends (strong ties) 2) support in 5 dimensions (strong ties) 4) activities in organisations, their frequency (weak ties) | moderator analysis (type 1) | (weak ties, supportive strong ties) |
17 | Sabbah | 2011 | cross-sectional study, quantitative | 2: damaged teeth, paradontose | 2: education, income | 1) close friends, marital status 2) support 3) size | mediator analysis | no mediating effect |
18 | Schöllgen | 2011 | cross-sectional study, quantitative | 3: physical, functional, subjective health | 2: education, income | 2) emotional support, informational support 3) size | moderator analysis (type 2) | (supportive network) |
19 | Stephens | 2011 | cross-sectional, qualitative | 8: physical function, mental health, pain and more | 2: economic living standard, education | 1) living distance from relatives, contact frequency to family, neighbours, friends 2) support, 4) involvement in community, loneliness | multivariate analysis | social network and social support explain 33% of mental health and 15% of physical health, social gradients in health can be partially explained by social networks |
20 | Unger | 1999 | longitudinal, quantitative | 1: physical functioning | 2: education, income | 1) marital status 2) emotional and instrumental support by spouse, children, friends and relatives 3) size | moderator analysis (type 2) | no moderating effect of income on the association of networks/support and functional decline |
21 | Veenstra: | 2000 | cross-sectional, quantitative | 1: self reported health | 2: income, education | 1) contact frequency (family, workmates, neighbours…) 4) trust, religious attendance, civic participation | multivariate analysis | income and education were strongest predictors for health, social integration at work and attending religious services additionally contributed to better health |
22 | Verhaeghe | 2012 | cross-sectional, quantitative | 1: self-rated health | 3: education, occupation, social class | 1) friends, family, acquaintances w/ different occupations 2) perceived support 3) volume of social capital, occupational composition | mediator analysis | positive associations between network social capital and health beyond the influence of social class. Support only partially mediated the association of network social capital and health |
23 | Vonneilich | 2011 | longitudinal, quantitative | 2: self-rated health, depressive symptoms | 2: income, education | 1 + 4) Social Integration index: living with a partner, number of close ties, affiliation in associations 2) emotional/instrumental, perceived/received support | moderator analysis (type 2) | of SES on the association between networks (SII, support) and health |
24 | Vonneilich | 2012 | longitudinal, quantitative | 1: General subjective Health | 3: income, education | 1 + 4) Social Integration index: living with a partner, number of close ties, affiliation in associations ( 2) emotional/instrumental, perceived/received support | mediator analysis | (SII, support)—> network interventions fostering relationships can help lower SES groups to enhance health and buffer health inequalities |
25 | Weyers | 2010 | cross-sectional, quantitative | 3: smoking, nutrition, physical exercise | 2 income, education | 1) Social Integration index: living with a partner, number of close ties, affiliation in associations 2) emotional/instrumental, perceived/received support | moderator analysis (type 2) | no moderating effect; additive effect (SII, support) |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Keim-Klärner, S., Adebahr, P., Brandt, S. et al. Social inequality, social networks, and health: a scoping review of research on health inequalities from a social network perspective. Int J Equity Health 22 , 74 (2023). https://doi.org/10.1186/s12939-023-01876-9
Download citation
Received : 17 October 2022
Accepted : 28 March 2023
Published : 25 April 2023
DOI : https://doi.org/10.1186/s12939-023-01876-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social network
- Socioeconomic status
- Social support
- Scoping review
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- West J Emerg Med
- v.24(5); 2023 Sep
- PMC10527840
Race, Healthcare, and Health Disparities: A Critical Review and Recommendations for Advancing Health Equity
Wendy l. macias-konstantopoulos.
* Center for Social Justice and Health Equity, Department of Emergency Medicine, Boston, Massachusetts
† Harvard Medical School, Department of Emergency Medicine, Boston, Massachusetts
Kimberly A. Collins
‡ Tampa General Hospital, Tampa, Florida
Rosemarie Diaz
§ University of California-Los Angeles, Department of Emergency Medicine, Los Angeles, California
Herbert C. Duber
∥ University of Washington School of Medicine, Department of Emergency Medicine, Seattle, Washington
¶ Washington State Department of Health, Tumwater, Washington
Courtney D. Edwards
# Samford University, Moffett & Sanders School of Nursing, Birmingham, Alabama
Antony P. Hsu
** Trinity Health Ann Arbor Hospital, Department of Emergency Medicine, Ypsilanti, Michigan
Megan L. Ranney
†† Yale University, Yale School of Public Health, New Haven, Connecticut
Ralph J. Riviello
‡‡ University of Texas Health San Antonio, Department of Emergency Medicine, San Antonio, Texas
Zachary S. Wettstein
§§ University of Washington School of Medicine, Department of Emergency Medicine, Seattle, Washington
Carolyn J. Sachs
∥∥ Ronald Reagan-UCLA Medical Center and David Geffen School of Medicine at University of California-Los Angeles, Department of Emergency Medicine, Los Angeles, California
An overwhelming body of evidence points to an inextricable link between race and health disparities in the United States. Although race is best understood as a social construct, its role in health outcomes has historically been attributed to increasingly debunked theories of underlying biological and genetic differences across races. Recently, growing calls for health equity and social justice have raised awareness of the impact of implicit bias and structural racism on social determinants of health, healthcare quality, and ultimately, health outcomes. This more nuanced recognition of the role of race in health disparities has, in turn, facilitated introspective racial disparities research, root cause analyses, and changes in practice within the medical community. Examining the complex interplay between race, social determinants of health, and health outcomes allows systems of health to create mechanisms for checks and balances that mitigate unfair and avoidable health inequalities.
As one of the specialties most intertwined with social medicine, emergency medicine (EM) is ideally positioned to address racism in medicine, develop health equity metrics, monitor disparities in clinical performance data, identify research gaps, implement processes and policies to eliminate racial health inequities, and promote anti-racist ideals as advocates for structural change. In this critical review our aim was to (a) provide a synopsis of racial disparities across a broad scope of clinical pathology interests addressed in emergency departments—communicable diseases, non-communicable conditions, and injuries—and (b) through a race-conscious analysis, develop EM practice recommendations for advancing a culture of equity with the potential for measurable impact on healthcare quality and health outcomes.
INTRODUCTION
Social determinants of health (SDoH) as defined by the US Centers for Disease Control and Prevention (CDC) are the conditions in which people live, learn, work, and play that are determined by the distribution of money, power, and resources and that affect a wide range of health and quality-of-life risks and outcomes. 1 Influenced by the social construct of race, SDoH exert disparate impacts on the health of subpopulations. Economic disparities disproportionately place Black, indigenous, and people of color (BIPOC) within zones marked by substandard health promotion and excessive health risks. The compounding nature of adverse SDoH, such as housing instability, food insecurity, poor healthcare access, and hazardous exposures, has serious health implications. Health disparities are the profound downstream effect of the socioeconomic disadvantages that BIPOC endure under the moniker structural racism .
In addition to structural racism, implicit bias —defined as unconscious attitudes, positive or negative, toward a person, group, or idea—often leads to differential treatment based on perceived race. 2 , 3 Implicit bias further restricts quality healthcare as a separate factor above and beyond inequities of structural racism. Emergency department (ED) data indicates that Black (vs White) patients have longer treatment wait times, 4 longer lengths of stay, 5 and lower triage acuity levels. 6 Additionally, Black ED patients have a 10% lower likelihood of admission and 1.26 times higher odds of ED or hospital death than White patients. 7 Research also suggests that physicians’ own implicit racial biases may contribute to disparities in healthcare quality and delivery. 8 – 10
In this critical review we explore the complex effects of race, implicit bias, and structural racism on SDoH, healthcare quality and, ultimately, health outcomes. Although not intended as a comprehensive literature review on health disparities, this exercise informs a conceptual framework through which actionable steps and practice recommendations for emergency medicine (EM) are proposed as one part of a larger systemwide effort that requires thoughtful action and transformative policy to dismantle the hard-wired inequities of structural racism and advance health equity.
Critical Review Methodology
We conducted a broad-scope critical review of the extant health disparities literature across three areas of clinical pathology interest: communicable diseases; non-communicable conditions; and injuries. The review was conducted through a race-conscious lens to examine the impact of race on health outcomes and inform a conceptual framework for the development of actionable steps and practice recommendations.
Critical reviews include “a degree of analysis and conceptual innovation” resulting in a product capable of launching a new phase of evaluation. 11 According to Grant and Booth, the critical review does not call for a systematic evaluation of all the literature related to a topic, but rather the emphasis is on the contribution of each piece of evidence included to the review’s conceptual product. 11 As described by the Search, Appraisal, Synthesis, and Analysis framework, critical reviews are designed to identify key findings in the field of interest (health disparities literature), evaluate the evidence in accordance with its contribution (racial health disparities attributable to SDoH), synthesize the evidence in organized fashion (clinical pathology interests relevant to EM), and provide a conceptual output of analysis that contributes to the literature (actionable steps and practice recommendations). 11
In this review we aimed to examine racial health disparities through the SDoH model and apply socioenvironmental theory 12 and resource deprivation theory 13 as race-conscious filters through which racial disparities data is analyzed and synthesized ( Table 1 ). The analysis informed the conceptual framework through which we developed and propose actionable steps and practice recommendations.
Race-conscious analysis tools employed in critical review.
| Socioenvironmental theory | Resource deprivation theory |
|---|---|
| holds that racial residential segregation is central to racial and ethnic health disparities. According to this theory, racial/ethnic minority groups have considerably different levels of health risk due to the multiple social and environmental factors that detrimentally impact their health within the context of longstanding residential segregation and its deeply rooted socioeconomic disadvantages. | holds that the longstanding deprivation of resources experienced by racial/ethnic minority groups is central to racial and ethnic disparities. Due to chronic deprivation, racial/ethnic minority groups lack the necessary infrastructure to support health. Resources are not restricted to material possessions; they include education, employment, housing, neighborhood safety, and psychological wellbeing. According to evidence-based interpretations of this theory, gap closure cannot be achieved through equal distribution of resources, but rather targeted differential distribution of resources that levels the playing field for racial/ethnic minority groups. |
Communicable Diseases
Racial and ethnic disparities in the incidence and prevalence of HIV infection and AIDS have been documented in the US since the 1980s. 14 Despite prevention, identification, and treatment advances, Black-White and Hispanic-White disease incidence disparities have increased since 1984. In 2013, Blacks and Hispanics accounted for 46% and 21% of new HIV infections and 49% and 20% of new AIDS diagnoses despite representing 12% and 16% of the total US population, respectively. 14 Although HIV incidence rates have improved in recent decades, Blacks and Hispanics have benefitted less from antiretroviral therapy advancements. 15 Incidence rates (IR) have declined with the advent of pre-exposure prophylaxis (PrEP); however, PrEP usage remains disparately low among Black (5.9%) and Hispanic (10.9%) adults with an indication as compared to Whites (42.1%). 16 , 17
ED Actionable Steps: Increase access to HIV testing and referrals to PrEP and post-exposure prophylaxis.
Viral Hepatitis
Hepatitis C virus (HCV) is the leading cause of liver disease-related death in the US. 18 Racial disparities in disease prevalence exist at a rate greater than twice that of Whites; Blacks in the US have the highest prevalence ratio (PR) of disease (PR 2.29, 95% confidence interval [CI] 1.94–2.70). 18 Rates of treatment for chronic hepatitis C are also higher among Whites as compared to Black, Hispanic, and Asian individuals. 19 Direct-acting antivirals (DAA) became available in 2014 and are achieving greater than 90% cure rates. 20 Early research found that Black and Hispanic patients were less likely than Whites to benefit from DAA initiation (adjusted rate ratio [aRR] 0.7, 95% CI 0.7–0.8 and 0.8, 95% CI 0.7–0.9, respectively). 21 Follow-up data from a national cohort found that these racial-ethnic gaps had closed by 2016; however, more recent data is needed to determine whether equitable access has persisted beyond initial evidence-driven efforts. 20
ED Actionable Steps: Increase access to HCV testing and referrals to DAA treatment.
Sexually Transmitted Infections
Disparities in sexually transmitted infections (STI) have been described extensively in the literature. Rates of primary and secondary syphilis, HIV/AIDS, chlamydia, and gonorrhea among Blacks range from 5.4 to 17.8 times the rates among Whites in the US. 22 The SDoH associated with increased STI prevalence have been discussed extensively, ranging from inequities in healthcare, income, incarceration, residential segregation, and substance use, among others. 23 , 24 Importantly, prevalence must be interpreted within the context of STI screening, the odds of which are higher among Black and Hispanic women than their White counterparts (adjusted odds ratio [aOR] 2.56, 95% CI 2.60–3.10 and 1.42, 95% CI 1.39–1.46, respectively). 25
ED Actionable Steps: Increase access to STI testing and ED-based treatment.
Diarrheal Disease
An estimated 500,000 cases of shigellosis occur annually in the US. 26 Incidence rates of infection per 100,000 are greatest among Black (7.2) and Hispanic (5.6) individuals as compared to Whites (2.6). 26 Despite the preventable nature of shigellosis, an analysis of over 25,000 laboratory-confirmed cases reported to the CDC found a strong association between its incidence and residence in areas marked by US Census Tract-level poverty and household crowding. Racial and ethnic IR disparities, however, persisted even after controlling for these socioeconomic indicators, 26 and the rates of severe infection among adults are highest among Black persons. 27 Similarly, Black (vs non-Black) infants <6 months in age had higher rates of diarrhea-associated hospitalizations that persisted even after the introduction of the rotavirus vaccines in 2006. 28
ED Actionable Steps: Educate patients and parents about transmission mechanisms and mitigation strategies (eg, hand hygiene, low-cost water treatment options, vaccination), and consider offering vaccination in the ED when necessary and reasonable.
Pandemic Respiratory Viral Infection
Disparities exist among pandemic respiratory viral infections, including influenza H1N1 and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), resulting in higher disease incidence and mortality among minority groups. 29 – 31 Coronavirus disease 2019 (COVID-19) cases and hospitalization rates were 2.5-4.5 times higher among Black, Hispanic, and Native American populations than Whites. Through May 2021, COVID-19 deaths among Hispanic and Black populations were 17% and 10% greater, respectively, than expected by US population representation after controlling for age. 32 Elevated COVID-19 infection and death rates have also been observed in socially disadvantaged counties with larger proportions of BIPOC. 32 , 33 Among residents of a predominantly Black and Hispanic COVID-19 hotspot, very high and disparate positivity rates were observed among Black (68.5%) and Hispanic (65.3%) patients as compared to Whites (53%). 34 Higher hospitalization rates for Blacks (60.2%) and Hispanics (62.3%) as compared to Whites (47.7%) were also observed, although there were no differences in admission rates to the intensive care unit. 34
Mortality rates among COVID-19 inpatients also show BIPOC disparities. 35 , 36 Recent CDC data shows higher mortality risk ratios for Native Americans (2.4), Hispanics (2.3), and Blacks (1.9) compared to Whites. 37 There are several reasons cited to explain the higher out-of-hospital mortality rates, disease burden, and severity of illness among BIPOC. 36 , 38 – 40 Several authors have concluded that population-based disparities in COVID-19 hospital mortality are best explained by differential disease incidence, prevalence of comorbid conditions, and socioeconomic marginalization among Black and Hispanic individuals. 34 , 39 , 40
Overall racial and ethnic disparities in COVID-19 risk, severity, morbidity, and mortality arise from a combination of social, economic, and health determinants. 36 , 38 Due to economic strain, BIPOC are more likely to live in crowded housing (multigenerational or communal households) and densely populated neighborhoods. They are also more likely to work in consumer-facing public service industries and rely on public transportation, increasing their exposure risk. Additionally, higher rates of comorbidities (eg, heart disease, diabetes, hypertension, and obesity) increase BIPOC’s risk for severe COVID-19 disease. Barriers to health insurance and health services limit access to treatments and to accurate knowledge regarding SARS-CoV-2 transmission, prevention strategies, disease symptoms, and reasons for seeking care. 41 – 43 Interestingly, despite the positive impact of Medicaid expansion on healthcare access, mortality, and disparities, one study failed to find an association between COVID-19 mortality and expansion vs non-expansion, 44 , 45 likely reflecting a benefit negated by the heightened social risk of structural racism.
Disparities in vaccination coverage were evident by the end of April 2021. When all adult age groups were eligible, vaccination rates among Black (46.3%) and Hispanic (47.3%) adults were lower than among Whites (59%) and Asians (69.6%). 46 Despite policies to ensure equitable COVID-19 vaccine access, vaccination hesitancy—originating from distrust in the medical establishment and resulting from longstanding systemic racism in healthcare and research—required community partnerships and concerted efforts by trusted sources of information to overcome the slower rates of vaccination among BIPOC. 46
ED Actionable Steps: Increase access to viral testing, educate patients and parents about transmission mechanisms and mitigation strategies (eg, masks, isolation, vaccination), and consider offering vaccination in the ED when necessary and reasonable.
Non-Communicable Conditions
Acute coronary syndrome and acute myocardial infarction.
Disparities in acute coronary syndrome (ACS) care have been well-documented. Compared to White patients with door-to-balloon (DTB) times of 103.4 minutes, Black and Hispanic patients experience significantly longer DTB times (122.3 and 114.8 minutes, respectively). 47 Over the last decade, DTB times have improved significantly across all groups; however, Black Americans have a lower likelihood of experiencing DTB times <90 minutes 48 and have experienced only a modest decline in recurrent hospitalization for acute myocardial infarction (AMI) compared to Whites. 49 Black patients experience worse AMI outcomes with a five-year mortality rate of 29% compared to 18% among Whites. 50
ED Actionable Steps: Consider protocolized ED triage and early management of potential ACS/AMI-related complaints beyond chest pain.
Type 2 Diabetes Mellitus
Type 2 diabetes prevalence rates among Black (13.2%) and Hispanic (12.8%) Americans are similar and higher than rates among Whites (7.6%). 51 Well-controlled glycemia and hospitalization rates, quality indicators, are both worse among Black patients (37.6% and 26.5%, respectively) compared to Whites (44% and 16.1%, respectively). 51 The marker of glycemic control, hemoglobin A 1c (HgbA 1c ), is statistically worse among Black vs White patients (HgbA 1c 9.1 ± 2.9% vs. 8.5 ± 2.2%, P = 0.001). 52 Black and Hispanic patients have higher odds of diabetes-related ED visits (odds ratio [OR] 1.84, 95% confidence interval [CI] 1.7–2.0 and 1.60, 95% CI 1.4–1.8, respectively) than Whites. 53
ED Actionable Steps: Educate patients about the complications of poor glycemic control and consider navigation partnerships with primary care for expedited post-ED visit, outpatient follow-up of patients with diabetes-related chief complaints and complications.
Hypertension
Racial and ethnic disparities in hypertension are likely multifactorial related to upstream SDoH, including access to healthcare, affordable medications, low-sodium foods, and safe green spaces for physical activity. 54 Unique to Black patients, race-consciousness significantly increases diastolic blood pressure (BP), and the self-perception of having a lower social standing as a function of race is associated with medication non-adherence and higher systolic BP. 54 Research has also demonstrated that Black and Asian patients have higher odds of a high BP reading at their last clinic visit (OR 0.36, 95% CI 0.21–0.60 and 0.40, 95% CI 0.16–0.97, respectively) and Black and American Indian/Alaska Native patients have higher odds of an ED visit or hospitalization (OR 3.61, 95% CI 1.88–6.91 and 5.31, 95% CI 2.13–13.20, respectively). 55
ED Actionable Steps: Educate patients about the complications of poor BP control and consider navigation partnerships with primary care for expedited post-ED visit, outpatient follow-up of patients with hypertension-related chief complaints and complications.
End-stage Renal Disease
Racial and ethnic disparities are profound in renal disease. Black patients experience higher IRs of end-stage renal disease (ESRD) in adolescence, greater probability of progression to advanced disease stages before initiation of dialysis, lower likelihood of peritoneal vs hemodialysis treatment, lower likelihood of transplant waitlist placement, and longer waiting times for transplantation. 56 Pediatric nephrology registry data found that among children who progressed to ESRD, 41.8% of White children received transplants compared to 16.3% and 27% of Black and Hispanic children, respectively, and 70% of White children were transplanted within two years of waitlist placement compared to 44% of Black pediatric patients. 57 Subsequent analyses confirm the persistence of these disparities with Black and Hispanic less likely than White children to receive preemptive transplants (8.7% and 14.2% vs 27.4%, respectively), and Black pediatric transplant recipients were less likely than White to experience allograft survival at five years (63% vs 80.8%, respectively). 58
Similar disparities among non-White adult ESRD patients include lower rates of transplant referrals, delayed times to transplant waitlist placement, and longer wait times for transplant. 56 National mortality statistics indicate Blacks experience significantly higher death rates from ESRD than Hispanic and White Americans (24.6 vs 11.1 and 12.1 age-adjusted death rate per 100,000, respectively). 59
ED Actionable Steps: Advocate for increased access to dialysis, particularly for the uninsured, and consider navigation partnerships with nephrology and local dialysis centers for expedited post-ED visit, outpatient follow-up of patients with ESRD-related chief complaints and complications.
As a risk factor for heart disease, type 2 diabetes, hypertension, and other chronic conditions, obesity poses a real challenge to population health management efforts. National data demonstrates that the highest prevalence of adult obesity occurs among Black Americans (38.4%) followed by Hispanics (32.6%) and Whites (28.6%). 60 Much like hypertension, racial and ethnic disparities in obesity are multifactorial and require a multifaceted intervention to target social (food deserts), biological (hormone dysregulation secondary adverse childhood events), and behavioral (physical activity) determinants. 61 Research has revealed a high burden of fast- food establishments within predominantly Black communities. 62 – 64 Treatment disparities are also present with BIPOC demonstrating decreased responsiveness to weight-loss pharmacotherapy, decreased likelihood weight- loss center referral, and decreased likelihood of bariatric surgery. 65
ED Actionable Steps: Consider partnerships with community programs focused on healthy lifestyle change and prescribe vouchers to patients whose health would benefit from weight loss.
Mental Health
Racial disparities in the management of psychiatric illness have also come to the forefront in recent years. Rates of depression treatment are lower among Black and Hispanic patients as compared to White patients, who are half as likely and a third as likely, respectively, to receive care than White patients. 66 According to the CDC, Black adults had the highest rates of mental health-related ED visits in 2018-2020, had longer ED wait times, and were less likely to be admitted or transferred to another hospital. 67 An analysis of national data found that Black patients presenting to the ED with a psychiatric emergency have a greater probability of chemical sedation than White patients. 68 , 69 Additionally, single- and multisite studies have found that Black 69 – 71 and Hispanic patients 71 are more likely to be physically restrained in the ED than White patients.
ED Actionable Steps: Use an equity lens to conduct a thorough review of policies related to restraint use, consider protocolized screening and management of agitation inclusive of early oral medication and withdrawal treatment, and consider navigation partnerships with hospital-based and community-based counseling services.
Environmental Hazard-Related Injuries
Ambient fine-particulate matter exposure (PM 2.5) is a risk factor for a host of conditions including reactive airway disease, coronary artery disease, and cerebrovascular disease. 72 The inequitable distribution of hazardous sites, namely industrial facilities, utilities, and landfills, is one of the greatest concerns in the field of environmental justice. Extensive literature has demonstrated that non-Whites are more likely to reside near stationary sources of PM, with Black Americans experiencing a higher burden of PM exposure than Whites and the general population. 73
Racial disparities in hazardous exposure burden are not a recent phenomenon. The 1987 groundbreaking study that first exposed the disproportionate co-location of toxic waste sites and minority communities found that three of every five Black and Hispanic Americans lived in such conditions. 74 The National Research Council conducted a study that observed greater prevalence of health problems—spontaneous abortions, birth defects, heart disease, gastric cancer, leukemia, and Hodgkin’s lymphoma—among those living in proximity to highly toxic chemicals and carcinogens (eg, benzene, polychlorinated biphenyls, mercury, arsenic, and lead). 75 Geo-mapping of hazardous sites found that a disproportionate number of towns overburdened by toxic sources were also home to high proportions of BIPOC, a robust positive predictor of hazardous waste site locations. 76
ED Actionable Steps: Increase syndromic surveillance collaborations with public health departments for early detection and community notification of hazardous conditions, and advocate for targeted policy interventions by highlighting the harmful health impacts on local communities.
Long-bone Fractures
Black and Hispanic patients are less likely to receive opioid analgesia for acute pain in the ED and opioid prescriptions at discharge compared to White counterparts. 77 – 79 Research shows that although average pain scores do not differ between White and non-White patients with long-bone fractures (LBF), White patients are more likely to receive opiates (70% vs 50%, P < 0.001). 78 Among children presenting for ED management of LBF, the data is similar: Black and Hispanic children were less likely to receive opioid analgesics (aOR 0.86, 95% CI 077–0.95 and 0.86, 95% CI 0.76–0.96, respectively) and less likely to achieve optimal pain reduction (aOR 0.78, 95% CI 0.67–0.90 and 0.80, 95% CI 0.67–0.95, respectively). 80
ED Actionable Steps: Consider protocolized ED triage and early management of LBF, including adequate analgesia dosing schedules.
Firearm Injuries
Firearm violence is a public health epidemic in the US. In 2018, firearms were the leading method of homicide and suicide, major causes of premature death. Per the CDC, 39,707 Americans died from firearm violence in 2019, averaging 109 deaths per day and comprising 60% suicides, 35% homicides, and 1.4% law enforcement interventions. 81 While most firearm suicide deaths impact Whites and American Indian/Alaska Natives, homicides disproportionately plague Black Americans. In 2018, firearm homicides were highest among Blacks. Black males and females aged 20–34 years died by firearm homicide at nearly 17 times higher and nearly six times higher rates than their White counterparts, respectively. Among youth aged 0–19, Black males had the highest firearm homicide rate at 14 times higher than their White peers. American Indian/Alaska Native male youth had the second highest youth homicide rate. Black males are disproportionately killed by law enforcement intervention with firearms at a rate 1.71 times that of non-Hispanic White males. 82
ED Actionable Steps: Remain informed of local firearm injury statistics and advocate for adequate policy responses by highlighting the harmful health impacts on local communities.
Across clinical pathology interests and in almost every area studied, BIPOC communities experience worse patient care and health outcomes. Contrary to historical medical teachings, there is no biological evidence for the concept of race as a genomic human subspecies to explain health disparities. 83 , 84 Rather, it is the social interpretation of people in a race-conscious society that disparately impacts health. 85 The system of structuring opportunity and assigning value, based on assumptions about groups of people with certain physical attributes, systematically privileges some while disadvantaging others and undergirds the deadly problem of structural racism. Compounding the well-recognized theory of resource deprivation among racially/ethnically segregated communities (eg, quality primary education, adequate housing, green space) is socioenvironmental theory, which points to acts of commission that inequitably pose health risks (eg, air pollution, 72 , 73 toxic waste, 74 – 76 and fast- food, 62 – 64 alcohol, 86 and tobacco outlets 87 ).
Physicians must acknowledge the insidious health threat that implicit biases and structural racism pose. Disproportionate levels of socioeconomic disadvantage, social vulnerability, and poor health outcomes are manifestations of long-established and deeply entrenched racial segregation and racial deprivation. One could argue that the adverse health effects of structural racism over the centuries have created a far greater public health crisis than the COVID-19 pandemic, and yet beyond their identification, they have not received the attention they demand. Perhaps, in future years, our collective response to the volatile sociopolitical events of the last five years will be viewed as the force that changed the narrative. Many academic medical centers have created executive positions focused on equity, diversity, and inclusion and have worked to implement educational curricula aimed at dismantling structural racism. 88
The question that remains today— how do we as individuals and collectively as an institution and specialty best advance social justice and health equity? —demands thoughtful actions and transformative policies. A recent scoping review found 37 published intervention papers with only a third including empirical research. 89 Clearly, the implementation science behind this massive multi-pronged process will take time to develop, 90 but there appears to be sufficient direction to propose potential actionable steps ( Table 2 ) and practice recommendations.
Potential actionable steps for emergency physicians.
BIPOC , Black, indigenous and people of color; DPH , Department of Public Health; ED , emergency department; EP , emergency physician; PM , particulate matter; STIs , sexually transmitted infections.
LIMITATIONS
As critical reviews focus on advancing thought through conceptual innovation following an analysis of the literature, the methodology, by design, does not necessitate an exhaustive comprehensive review of the literature nor the same systematicity and quality assessment as in other more structured review approaches. 11 Additionally, the objective of the conceptual product of a critical review is to propose a new phase of research within the field in question, 11 and as a result, the actionable steps and practice recommendations made have yet to be proven effective but instead serve as a starting point for a new phase of implementation science.
The suggested actionable steps and following practice recommendations constitute the conceptual product of this critical review, demanding a new phase of implementation and evaluation research that identifies effective strategies and best practices for mitigating racial health inequities. Emergency physicians, as individuals and organizational leaders, can act from several positions in the social structure:
- a. Affordable, safe housing
- b. Food security (ie, sufficient, safe, and nutritious sustenance)
- c. Firearm safety, neighborhood safety, and support for survivors of violence
- d. Health-promoting lifestyle (eg, green space and density restrictions on fast-food, tobacco, and alcohol outlets)
- e. Comprehensive community health centers with expanded hours of operations
- 2. Develop meaningful individual and organizational partnerships with antiracist stakeholders and communities (ie, Black Lives Matter, White Coats for Black Lives, etc).
- 3. Engage leadership and representatives of first responder agencies in upholding the value of every human life.
- 1. Engage medical leadership in changing organizational culture to one that consistently prioritizes equity, addresses inequities in clinical and professional spaces, and recognizes the systematic advantage of privilege.
- 2. Create permanent positions accountable to equity, diversity, and inclusion initiatives 91 and ensure core leadership articulates diversity as an institutional priority and dialogues constructively with all relevant stakeholders. 92
- 3. Increase BIPOC representation within the pipeline and across all organizational strata. 93
- 4. Identify racial disparities and their sources within the system, conduct root cause analyses, and implement strategies to remedy inequities. 94 Describe, document, and proactively work to mitigate the health impact of racism. 95
- 5. Draft policies and enforce protocols for dealing with race-based aggression by patients and other staff.
- 6. Educate medical personnel through multimodal continuous medical education on trauma-informed care, anti-racism practice, and cultural humility. 96
- a. SDoH: Although the prospective, patient-oriented outcome is sparse, many medical schools and residency programs have adopted SDoH curriculum, which may lead to measurable changes in the future 98 and is a stated priority of the Institute of Medicine. 99 Comprehensive training materials are free and available on the web. 100
- b. Cultural humility training to address implicit bias, stereotypes, and prejudice. 101
- c. Anti-racism and trauma-informed care training to improve patient care communication and bedside skills.
- 8. Evaluate the impact of educational programs on patient care and health outcomes to curate efforts. 102 Disseminate evidence-based best practices.
- 9. Endeavor as an institution and specialty to eliminate racialized conceptions of disease susceptibility (eg, casting Blacks as innately diseased and dehumanizing their suffering). 103
- 1. Develop equity metrics, monitor clinical performance data, identify clinical and research gaps, and implement process and policy changes to eliminate health disparities.
- 2. Abandon the practice of stating the patient’s race in the narrative of the history and physical as it has minimal benefit, risks introducing bias, and is offensive to minority physicians. 104
- 3. Cease the use of correction formulas that use race as a proxy for pathology when their use furthers health inequities. 105
- 4. Make deliberate efforts to treat racial groups similarly on individual and population levels as a concrete first step in ameliorating racial health disparities. Although physicians undoubtedly carry implicit racial biases equal to the general population, there is some evidence that emergency physicians show less implicit racial bias than the general population. 106
- 5. Address racist patient attitudes professionally even when these cause moral distress. 107 Addressing racism and attempting to rebuild therapeutic alliances is part of the leadership and professionalism that emergency physicians must emulate.
- D. Hospital executives
- Institutional leaders must assure appropriate ED ancillary staffing and address hospital policies (eg, inpatient census levels, direct and transfer admissions) that result in ED crowding, medical error, morbidity and mortality, and staff demoralization. 108 Emergency physicians are experts in rapid cognition or thin-slicing, but with that practice comes the expression of latent stereotypes and biases that require a deliberate “bias-check” pause to better understand the patient and, thus, achieve better outcomes. 109 Research has demonstrated that overstressing physicians beyond reasonable levels is associated with increases in implicit bias. 110
- a. Abandon power imbalances common in traditional, paternalistic doctor-patient dynamics.
- b. Empower patients to be partners in treatment decisions.
- c. Offer patients validation, explanation, and choice.
- d. Practice cultural humility, an orientation to care that is based on self-reflexivity, appreciation of patients' lay expertise, openness to sharing power and knowledge with patients, and desire to learn from patients. 114
- a. Follow evidence-based race-blind admission and surgical criteria.
- b. Provide professional peer-to-peer feedback with coaching on delivery of difficult conversations. 115
- c. Build race-blind analgesia protocols. 116
- d. Create policies to address interprofessional microaggressions and patient-to-clinician racism. Micro- and macroaggressions contribute to burnout and must be combated to ensure inclusion and career longevity. 117 , 118
In conclusion, from a medical standpoint, there is only one race—the human race—and we must recognize and counter our implicit biases. As fellow humans, we must acknowledge that structural racism drives health inequities, and as emergency physicians we can choose to address it by employing any or all the actions and recommendations proposed herein.
Section Editors: David Thompson, MD and Shahram Lotfipour, MD, MPH
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest : By the West JEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Maternal and Infant Health Inequality: New Evidence from Linked Administrative Data
We use linked administrative data that combines the universe of California birth records, hospitalizations, and death records with parental income from Internal Revenue Service tax records to provide novel evidence on economic inequality in infant and maternal health. We find that birth outcomes vary non-monotonically with parental income, and that children of parents in the top ventile of the income distribution have higher rates of low birth weight and preterm birth than those in the bottom ventile. However, unlike birth outcomes, infant mortality varies monotonically with income, and infants of parents in the top ventile of the income distribution—who have the worst birth outcomes—have a death rate that is half that of infants of parents in the bottom ventile. When studying maternal health, we find that although mothers in the top and bottom income ventiles have similar rates of severe maternal morbidity, the former group are three times less likely to die than the latter. At the same time, these disparities by parental income are small when compared to racial disparities, and we observe virtually no convergence in health outcomes across racial and ethnic groups as income rises. Indeed, infant and maternal health in Black families at the top of the income distribution is markedly worse than that of white families at the bottom of the income distribution. Lastly, we benchmark the health gradients in California to those in Sweden, finding that infant and maternal health is worse in California than in Sweden for most outcomes throughout the entire income distribution.
This research was conducted as a part of the U.S. Census Bureau’s Evidence Building Project Series. Any opinions and conclusions expressed herein are those of the authors and do not represent the views of the U.S. Census Bureau. The Census Bureau has ensured appropriate access and use of confidential data and has reviewed these results for disclosure avoidance protection (Project P-7523134: CBDRB-FY22-CES018-005, CBDRB-FY22-CES018-012, CBDRB-FY22-CES018-016, CBDRB-FY22-420, CBDRB-FY23-0405, and CBDRB-FY23- 0464). We would like to thank Joshua Bricker and Iriliana Shala for excellent research assistance. We are also grateful to Janet Currie, Daniel Dench, Maria Perez-Patron, and Heather Royer for valuable feedback, as well as seminar and conference participants at Columbia University School of Public Health, Duke University, Harvard University (Opportunity Insights), Illinois Institute of Technology, the Los Angeles Guild of Reproductive Health, NBER New York, NBER Summer Institute (Children’s and Health Care Meetings), NYU Langone Department of Adolescent and Child Psychiatry, Stanford University, UC Berkeley (Health Policy), University of Kentucky, University of Utah School of Business, the USC Center for Health Journalism, and Weill Cornell Medicine. We are grateful to Jennifer Troyan and staff at the California Maternal, Child, and Adolescent Health Division for providing additional information regarding health statistics published by the California Department of Public Health. We would also like to thank Ellen Badley, Sandra Bannerman, Colin Chew, Heather Fukushima, Steven Hoang, Amanda Jackson, Michelle Miles, Eric Neuhauser, Jenn Rico, and other staff at the California Department of Public Health (CDPH) for their help in accessing restricted California birth records, as well as Chris Crettol, Betty Henderson-Sparks, Jasmine Neeley, and other staff at the California Department of Health Care Access and Information (formerly the Office of Statewide Health Planning and Development) for help in accessing hospital discharge data, and Victoria McCoy-Cosentino at NYU for help with data use agreements. We would also like to thank Ashley Austin, Casey Blalock, Scott Boggess, Clint Carter, Melissa Chiu, Diane Cronkite, Denise Flanagan-Doyle, Adam Galemore, Katie Genadek, Katlyn King, Shawn Klimek, Shirley Liu, Kathryn Mcnamara, Bonnie Moore, John Sullivan and other staff at Census, Robert Goerge and Leah Gjertson at Chapin Hall, and the Laura and John Arnold Foundation’s support under their initiative to use linked data to advance evidence-based policymaking for help with the linkages to Census-held data. This research was supported by the National Institute on Aging under R01-AG059731. The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research.
MARC RIS BibTeΧ
Download Citation Data
- February 13, 2023
Mentioned in the News
More from nber.
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .

IMAGES
VIDEO
COMMENTS
Explanations for socioeconomic inequalities in adult health are usually sought in behaviours and environments in adulthood. Yet, there is compelling evidence that the first two decades of life contribute substantially to both adult socioeconomic position (SEP) and adult health. This has implications for explanatory health inequalities research. We propose an analytical framework to advance ...
Understanding trends in the extent of violence against women can be helpful in challenging violence against women and gender inequality. In this paper, we compare the incidence of violence, as measured in the National Family Health Surveys, to the reporting of violence, as compiled by the National Crime Records Bureau. We also shed light on heterogeneity in incidence and reporting across India ...
Each month, we feature select National Health Observances (NHOs) that align with our priorities for improving health across the nation. In September, we're raising awareness about healthy aging, sickle cell disease, substance use recovery, and HIV/AIDS. Below, you'll find resources to help you spread the word about these NHOs with your audiences.
The purpose of this paper is to define health inequality, health disparity, and health inequity from a population health perspective and to illustrate the meaning of each term by presenting authentic real-world examples. ... However, National Institutes of Health research funding for cystic fibrosis, which occurs in only a third of the number ...
The February issue of 2018 addressed the role of theory in health inequality research, the relationship between socio-political context and health [], and it also highlighted the recent turn in social epidemiology towards studying the impact of institutional arrangements, social policy and political context on population health [].Moreover, the issue suggested that moving forward from where we ...
Eliminating racial health inequities requires a movement away from disparities as the focus of research and toward a research agenda centered on achieving equity by dismantling structural racism.
Motivation for studying health inequalities. Despite considerable attention to the problem of health inequalities since the 1980s (), striking differences in health still exist among and within countries today ().In 2010, for example, Haitian men had a healthy life expectancy of 27.8 years, while men in Japan could expect 70.6 years, over twice as long, in full health ().
On April 20, 2023, WHO released the largest global collection of publicly available inequality data with the launch of the Health Inequality Data Repository.1 As members of the technical team developing the resource, we highlight its potential contribution to advancing health equity by creating opportunities for health inequality monitoring, including tracking progress towards the Sustainable ...
One major criticism of health inequalities research and policy is that there has been too much effort put into describing the problem, rather than finding solutions. The National Health Inequalities Strategy in England 1999-2010 provides a key international example of the latter. ... Paper: Aim: Study design: Data sources: Time period ...
Motivation for studying health inequalities. Despite considerable attention to the problem of health inequalities since the 1980s (Citation 8), striking differences in health still exist among and within countries today (Citation 9).In 2010, for example, Haitian men had a healthy life expectancy (Citation 10) of 27.8 years, while men in Japan could expect 70.6 years, over twice as long, in ...
In this essay, we focus on the potential and promise that intersectionality holds as a lens for studying the social determinants of health, reducing health disparities, and promoting health equity and social justice. Research that engages intersectionality as a guiding conceptual, methodological, and praxis-oriented framework is focused on power dynamics, specifically the relationships between ...
Introduction. Strong efforts to tackle health inequalities can be seen at international and national level since the 1980s. In early 2008, the World Health Organization's (WHO) Global Commission on Social Determinants of Health called for action on the social determinants of health, the conditions in which persons are born, grow, work, live, and age, to "close the gap in a generation" [].
This Series paper examines how the health-care system in the USA contributes and responds to inequality. We focus our attention on the association between inequality and the medical care system. We first review how social position influences Americans' access to medical services and the quality of those services.
The white paper must reinstate real-terms funding increases at the level seen before 2015. Thirdly inclusive innovation, integration, and access will be key to driving down national and local inequalities in health. The covid-19 pandemic showed that innovation in health and care services could be delivered including remote consultation.
Health inequalities research and health disparities research (hereafter 'health equity research') aims to understand, explain and reduce the unequal distribution of health across groups defined by social demographic factors, such as education, income and ethnicity. ... 29,212 papers containing relevant keywords were extracted, representing ...
This study found a gap in life expectancy of about 15 years for men and 10 years for women when comparing the most affluent 1% of individuals with the poorest 1%. To put this into perspective, the 10-year life expectancy difference for women is equal to the decrement in longevity from a lifetime of smoking. Probing the Income-Health Relationship.
This review summarises the present state of research on health inequalities using a social network perspective, and it explores the available studies examining the interrelations of social inequality, social networks, and health. Using the strategy of a scoping review, as outlined by Arksey and O'Malley (Int J Sci Res Methodol 8:19-32, 2005), our team performed two searches across eight ...
research efforts. In this paper, we discuss some of the challenges in performing research around inequalities in health, health care access and quality, and health care coverage and costs, and we provide suggestions for future research. When designing a statistical approach, selecting data, conducting health and health care research and
Referred to as a "cause of causes" or "fundamental cause" of health outcomes, income shapes the resources at our disposal, the disease risks we are exposed to, and our ability to mitigate these risks. 7 Decades of research have shown that low-income people have poorer self-reported health and higher rates of communicable and ...
We found evidence of wide ethnic inequalities in HRQoL and five determinants of health for older adults in England. Outcomes varied between minority ethnic groups, highlighting heterogeneity in the direction and magnitude of associations. We recommend further research to understand the drivers of inequalities, together with policy changes to improve equity of socioeconomic opportunity and ...
Advisor Analysis. Covid-19 is taking a toll on health care organizations' ability to provide equitable access to care, revealing that much work needs to be done to overcome disparities in care, according to a recent NEJM Catalyst Insights Council survey on health equity. "The Covid-19 pandemic has magnified issues to the extent that ...
We will likely look back on 2020 as a turning point. The pandemic put a spotlight on existing societal issues, accelerated the pace of change in others, and created some new ones too. For example, concerns about inequalities in health by income and race are not new, but they became more apparent to a larger number of people during 2020. The speed and starkness of broadening societal ...
The issue of "doing something" about inequality has become an important question in policy and academic realms. In the past few years the Ford Foundation, the Russell Sage Foundation, and the William T. Grant Foundation (Gamoran 2013) have all launched initiatives on "reducing inequality" and call for new research that might lead to concrete knowledge-based strategies for achieving ...
The purpose of this Review is to provide evidence for why gender equality in science, medicine, and global health matters for health and health-related outcomes. We present a high-level synthesis of global gender data, summarise progress towards gender equality in science, medicine, and global health, review the evidence for why gender equality in these fields matters in terms of health and ...
INTRODUCTION. Social determinants of health (SDoH) as defined by the US Centers for Disease Control and Prevention (CDC) are the conditions in which people live, learn, work, and play that are determined by the distribution of money, power, and resources and that affect a wide range of health and quality-of-life risks and outcomes. 1 Influenced by the social construct of race, SDoH exert ...
DOI 10.3386/w30693. Issue Date November 2022. Revision Date September 2023. We use linked administrative data that combines the universe of California birth records, hospitalizations, and death records with parental income from Internal Revenue Service tax records to provide novel evidence on economic inequality in infant and maternal health.